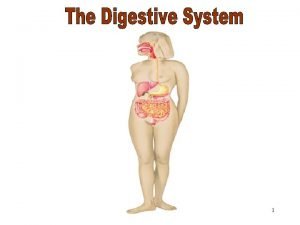
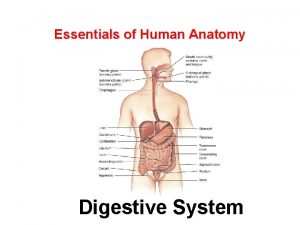
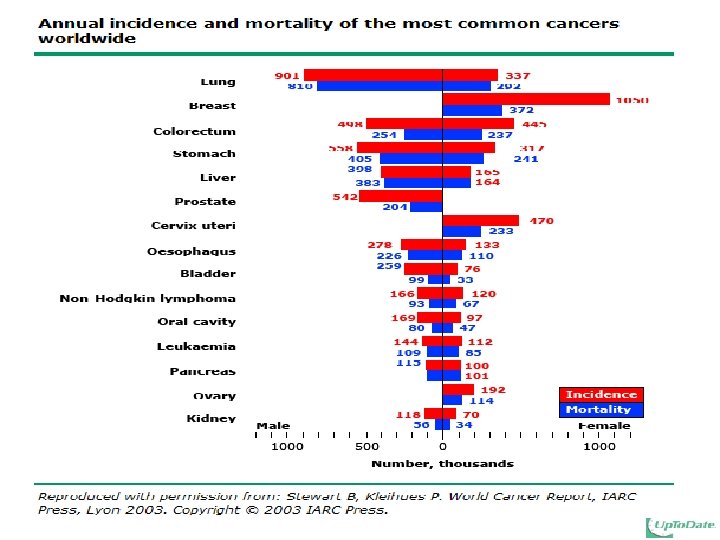
STOMACH ANATOMY The stomach The stomach is a









- Slides: 87

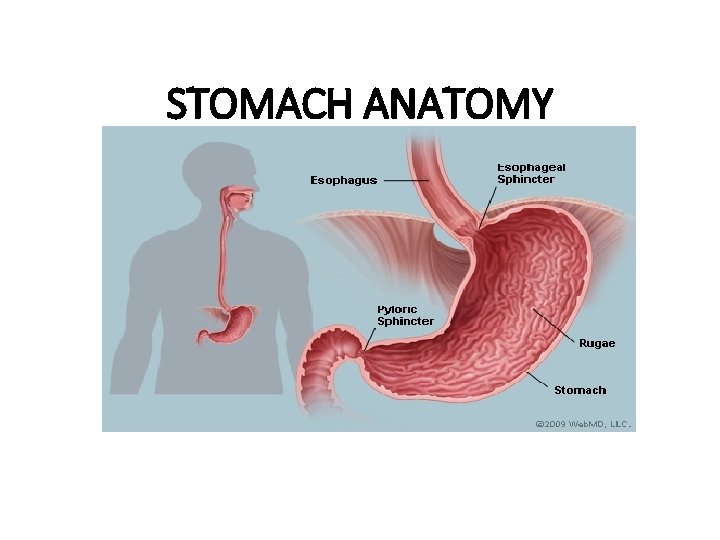
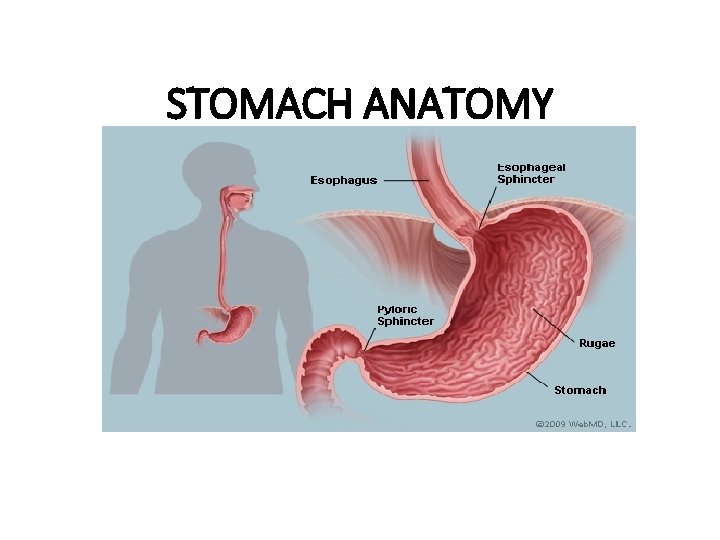
STOMACH ANATOMY
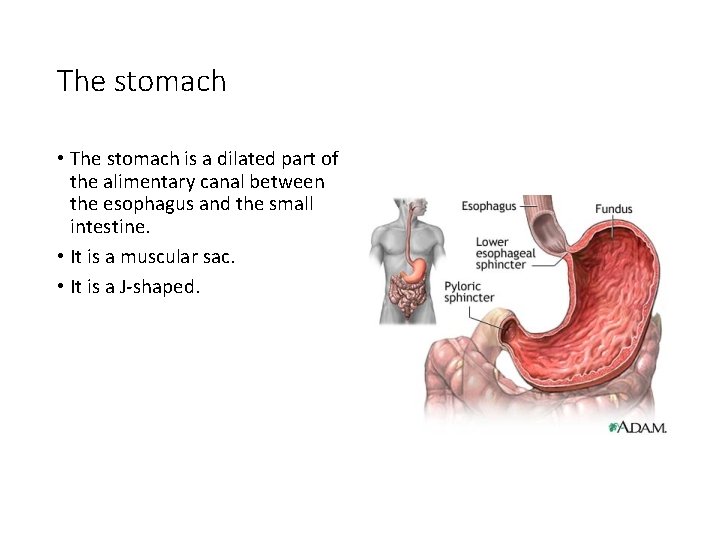
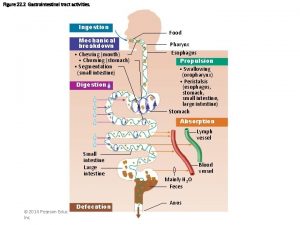
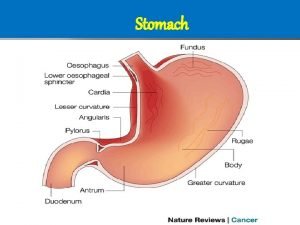
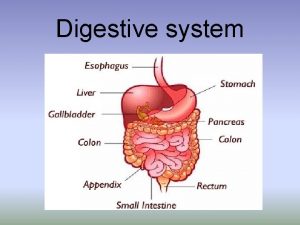
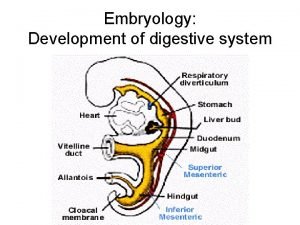
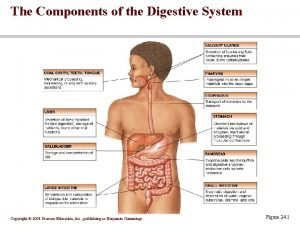
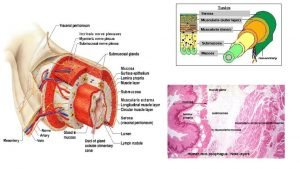
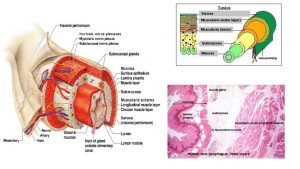
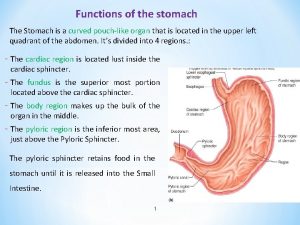
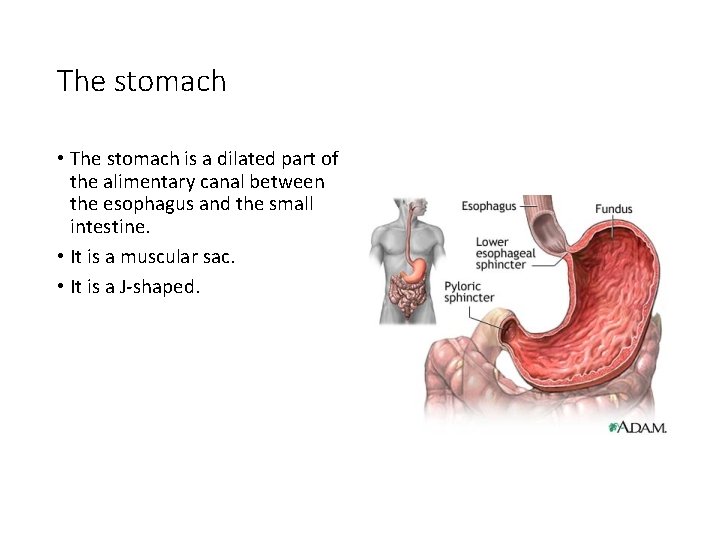
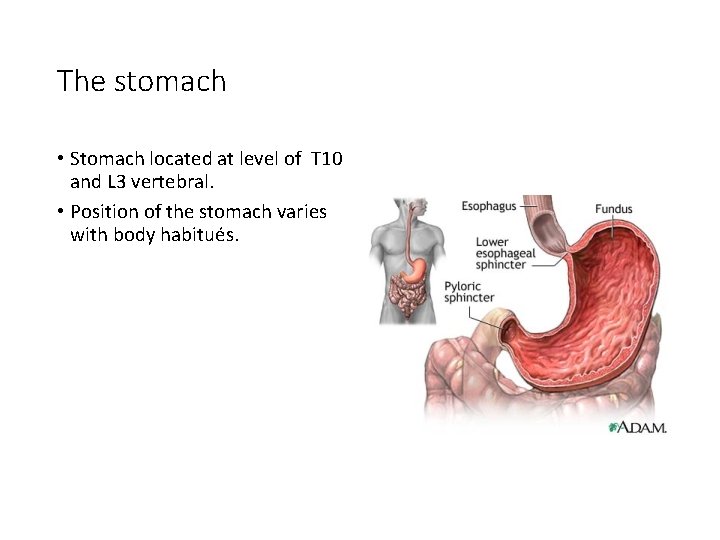
The stomach • The stomach is a dilated part of the alimentary canal between the esophagus and the small intestine. • It is a muscular sac. • It is a J-shaped.
The stomach • Stomach located at level of T 10 and L 3 vertebral. • Position of the stomach varies with body habitués.
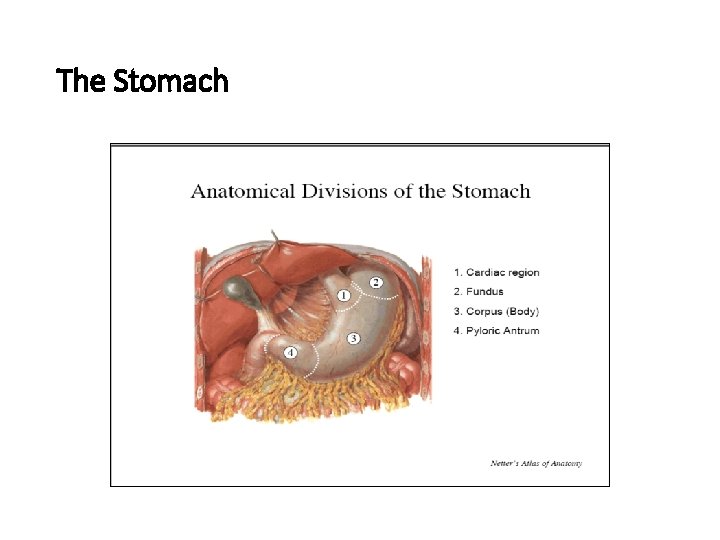
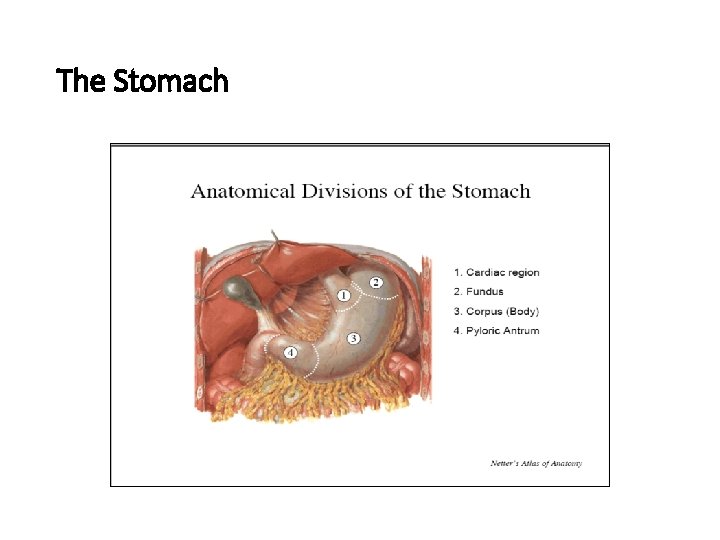
The Stomach
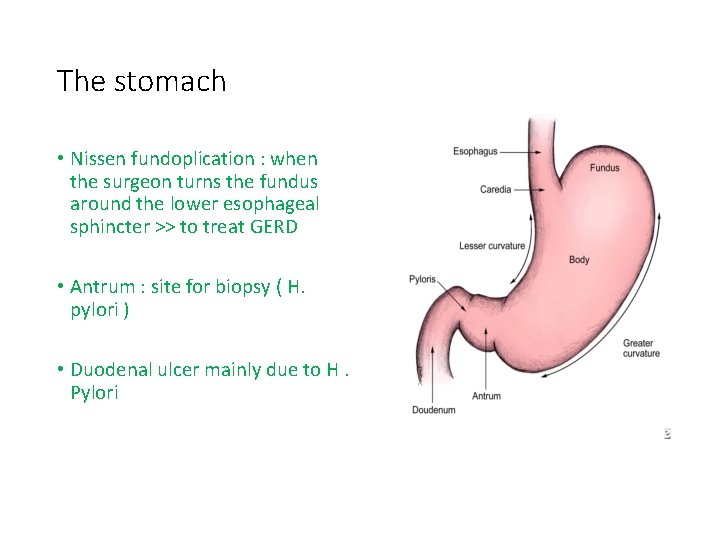
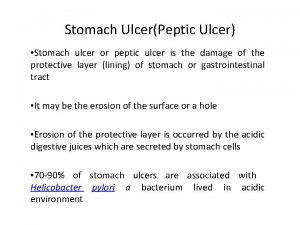
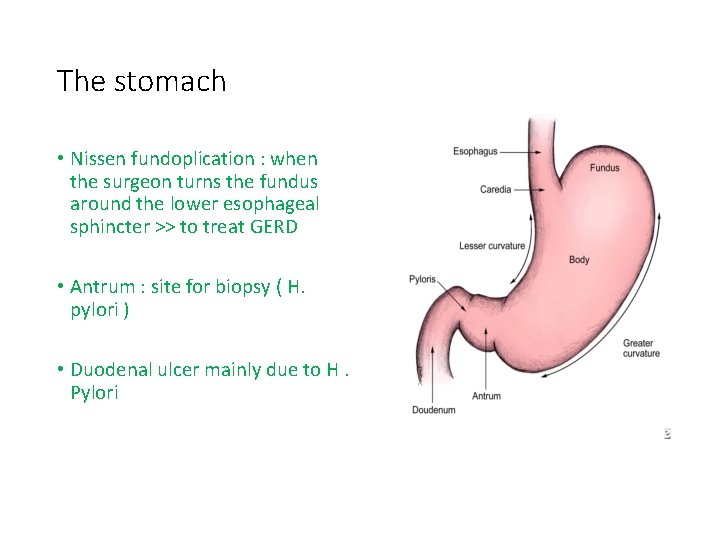
The stomach • Nissen fundoplication : when the surgeon turns the fundus around the lower esophageal sphincter >> to treat GERD • Antrum : site for biopsy ( H. pylori ) • Duodenal ulcer mainly due to H. Pylori
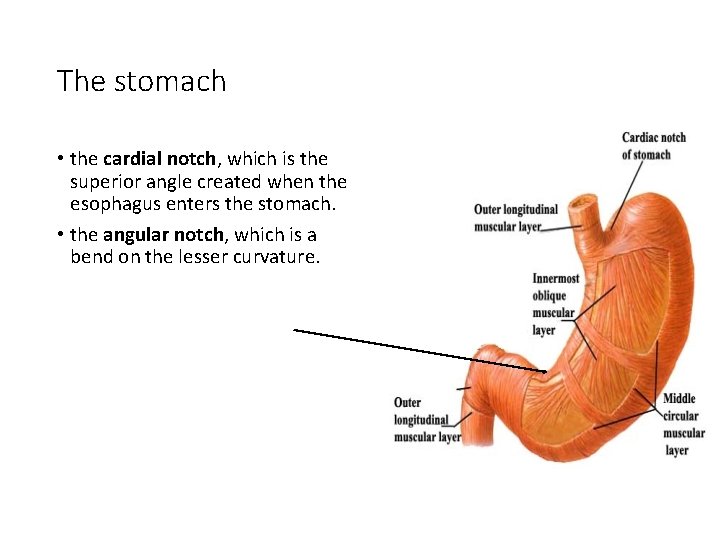
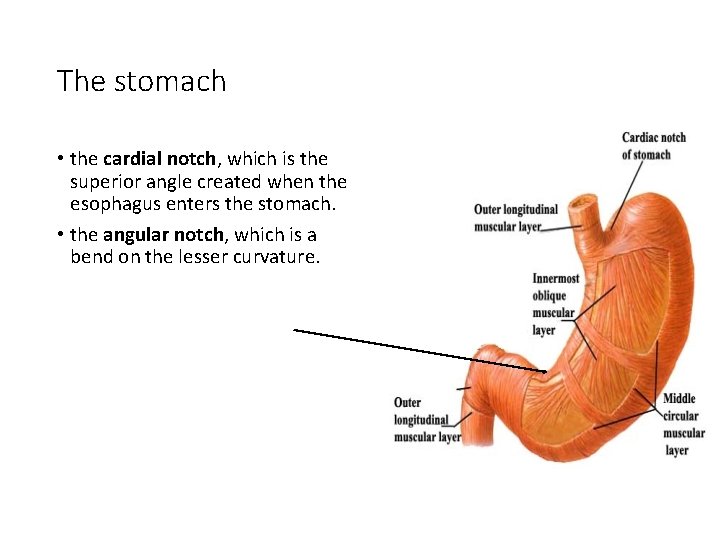
The stomach • the cardial notch, which is the superior angle created when the esophagus enters the stomach. • the angular notch, which is a bend on the lesser curvature.
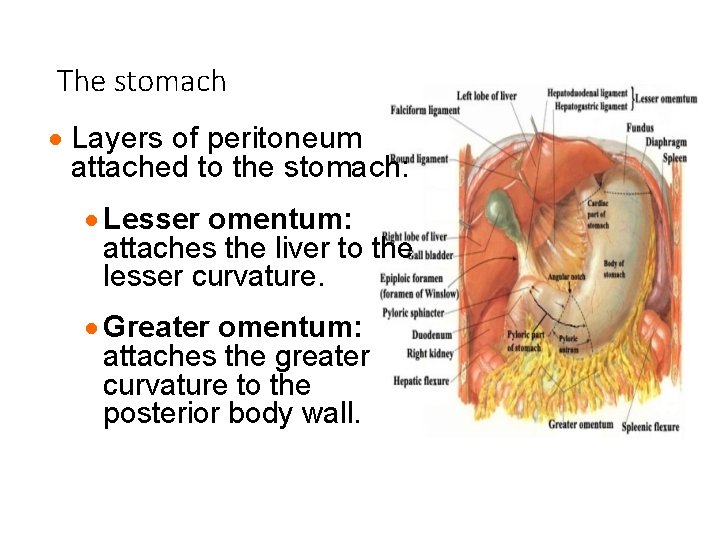
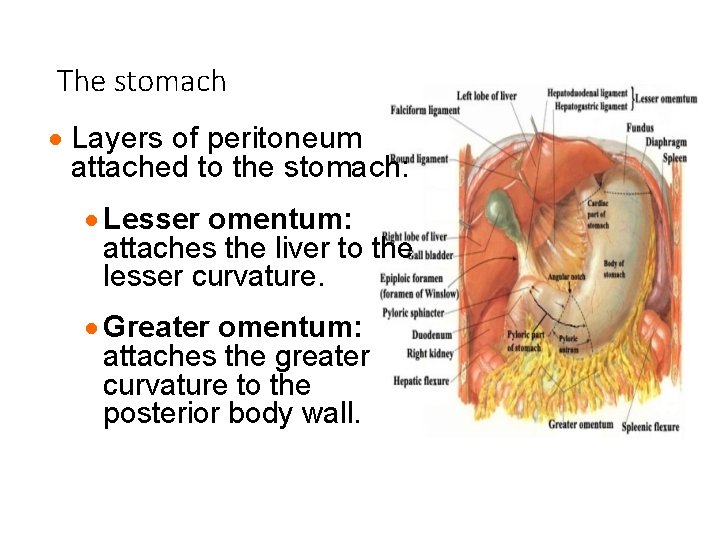
The stomach · Layers of peritoneum attached to the stomach: · Lesser omentum: attaches the liver to the lesser curvature. · Greater omentum: attaches the greater curvature to the posterior body wall.
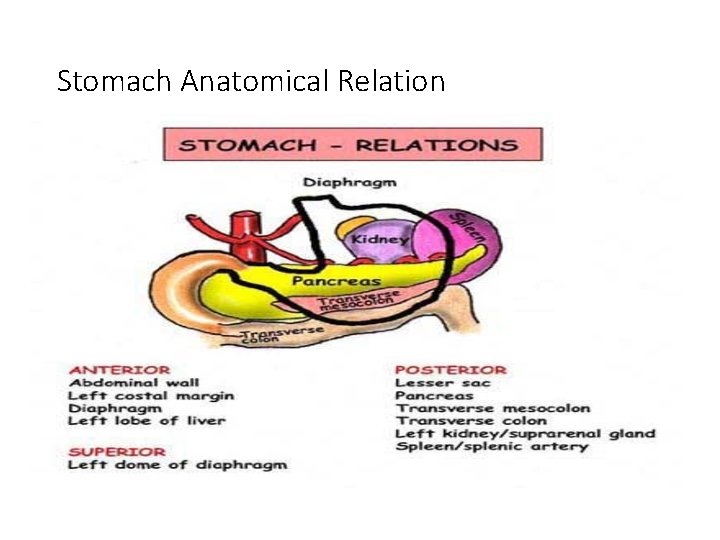
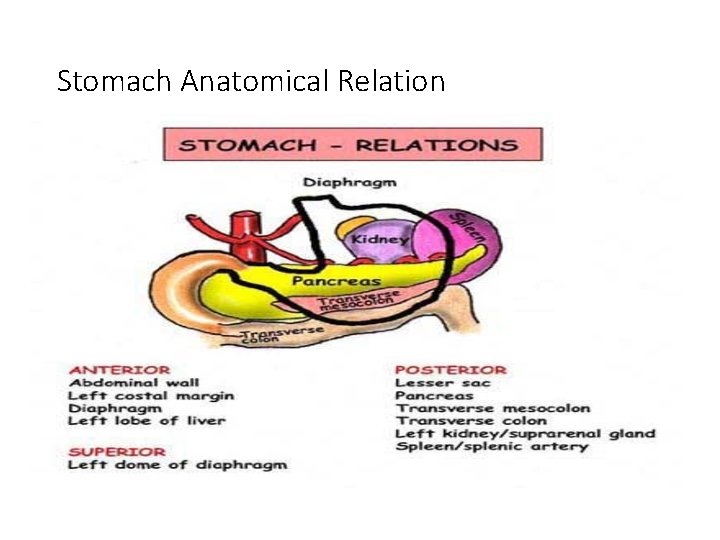
Stomach Anatomical Relation
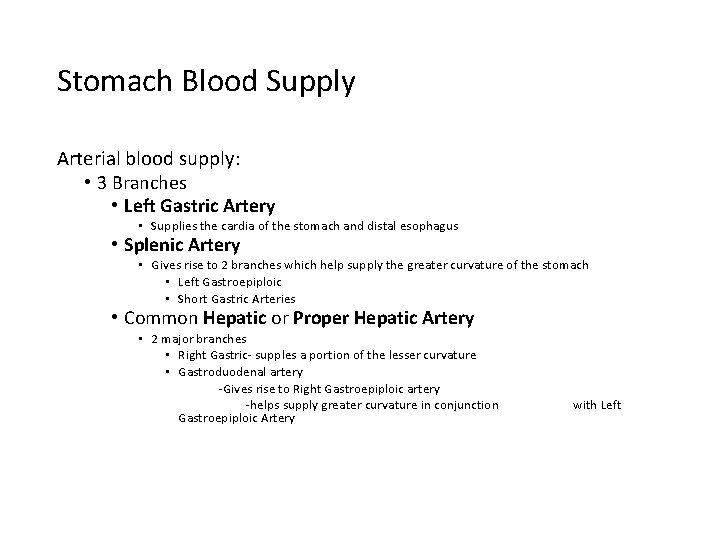
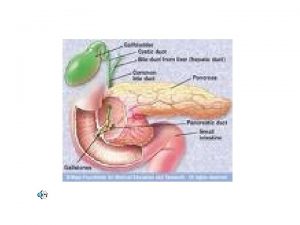
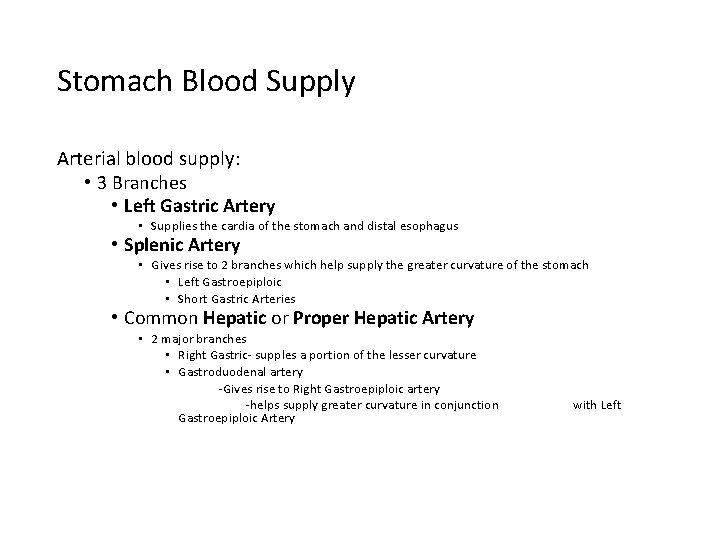
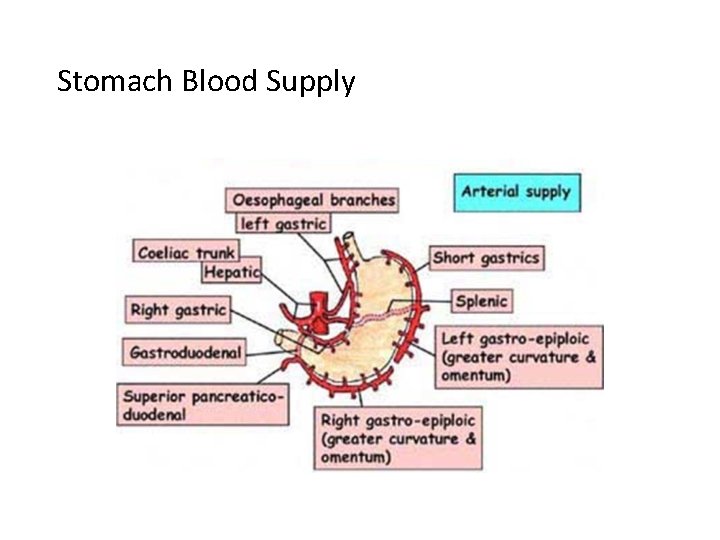
Stomach Blood Supply Arterial blood supply: • 3 Branches • Left Gastric Artery • Supplies the cardia of the stomach and distal esophagus • Splenic Artery • Gives rise to 2 branches which help supply the greater curvature of the stomach • Left Gastroepiploic • Short Gastric Arteries • Common Hepatic or Proper Hepatic Artery • 2 major branches • Right Gastric- supples a portion of the lesser curvature • Gastroduodenal artery -Gives rise to Right Gastroepiploic artery -helps supply greater curvature in conjunction Gastroepiploic Artery with Left
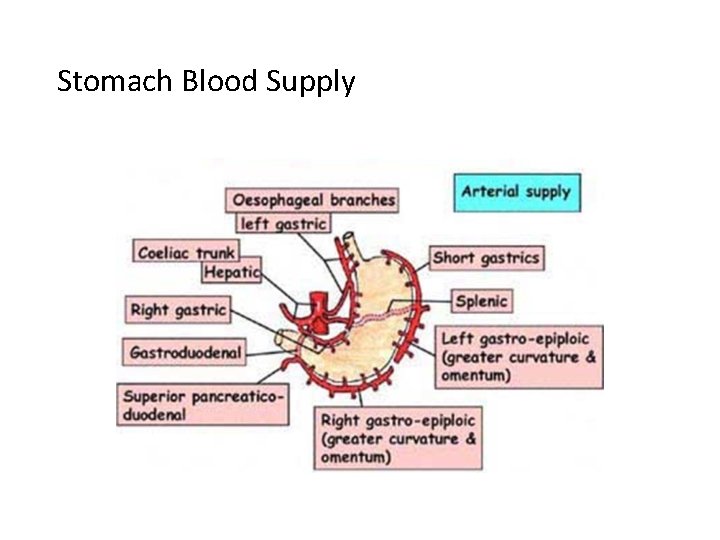
Stomach Blood Supply
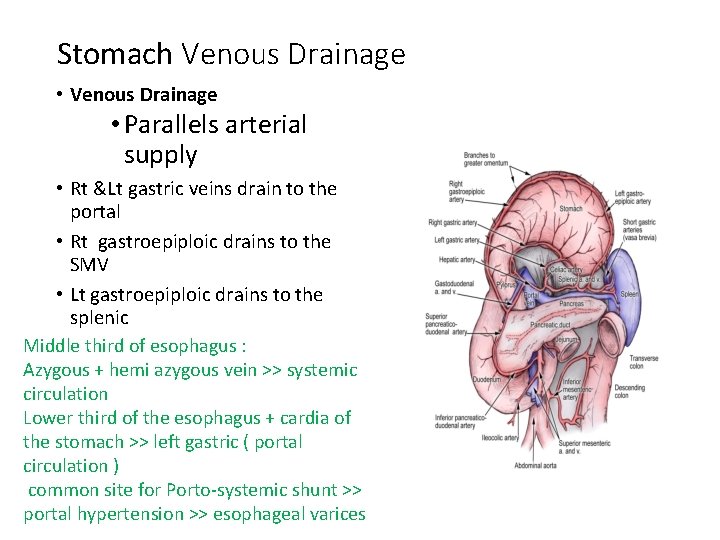
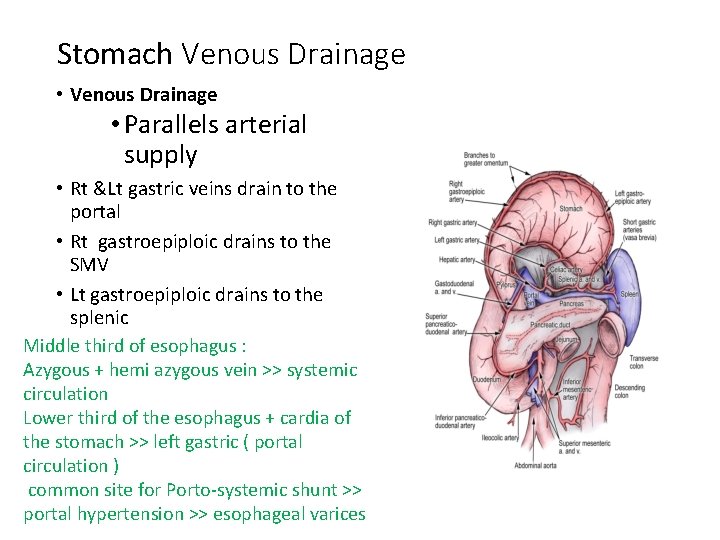
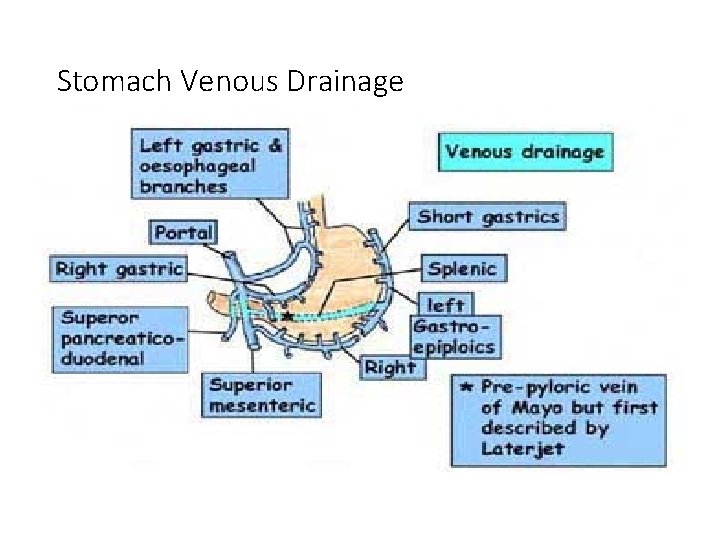
Stomach Venous Drainage • Venous Drainage • Parallels arterial supply • Rt &Lt gastric veins drain to the portal • Rt gastroepiploic drains to the SMV • Lt gastroepiploic drains to the splenic Middle third of esophagus : Azygous + hemi azygous vein >> systemic circulation Lower third of the esophagus + cardia of the stomach >> left gastric ( portal circulation ) common site for Porto-systemic shunt >> portal hypertension >> esophageal varices
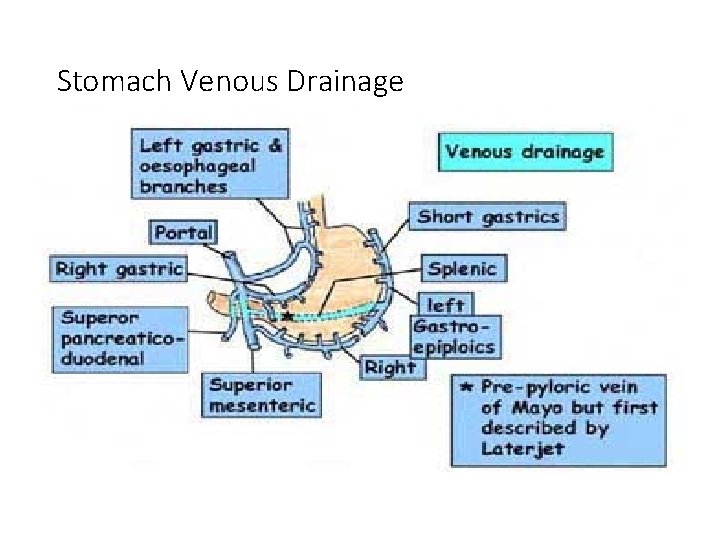
Stomach Venous Drainage
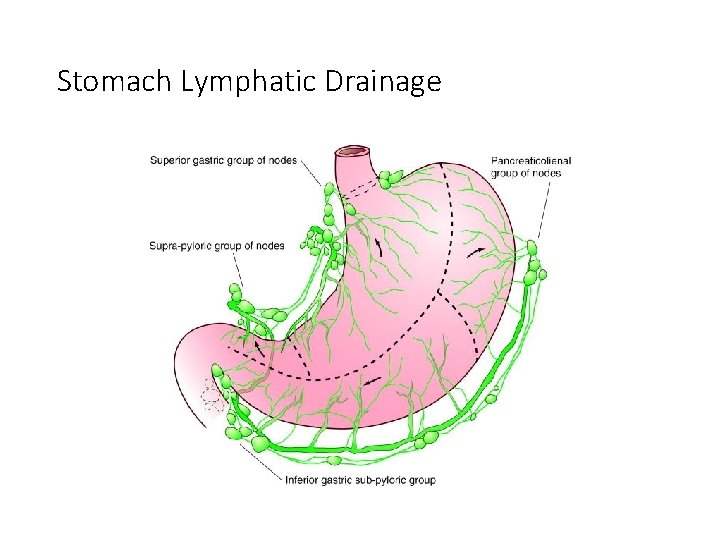
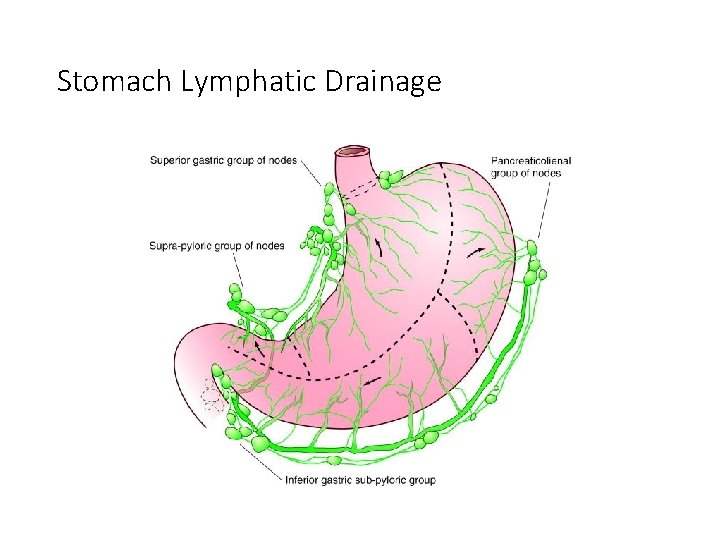
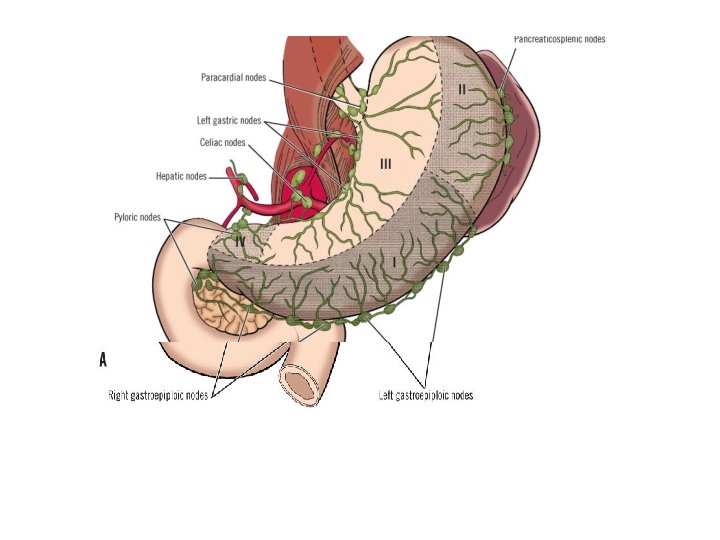
Stomach Lymphatic Drainage
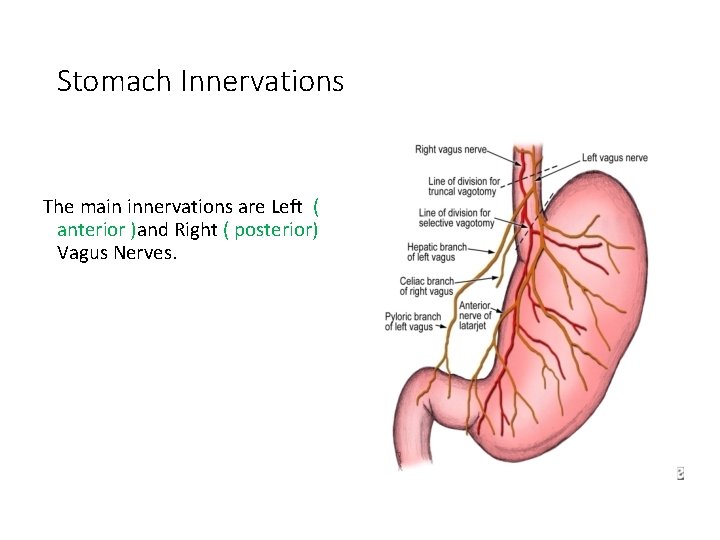
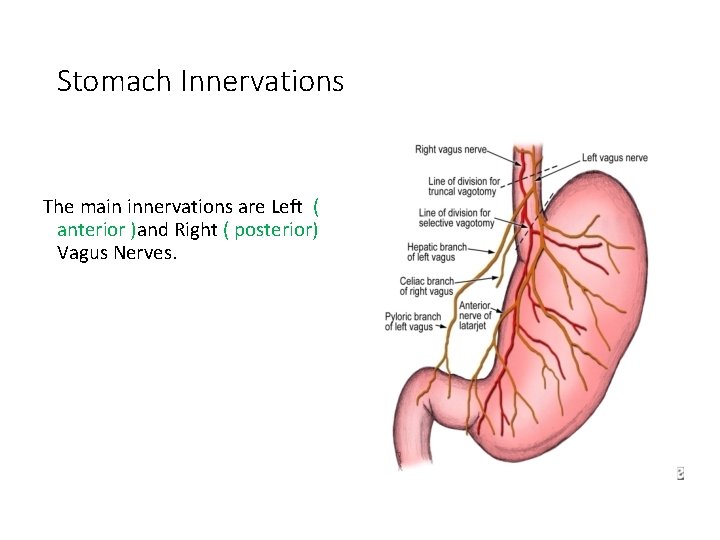
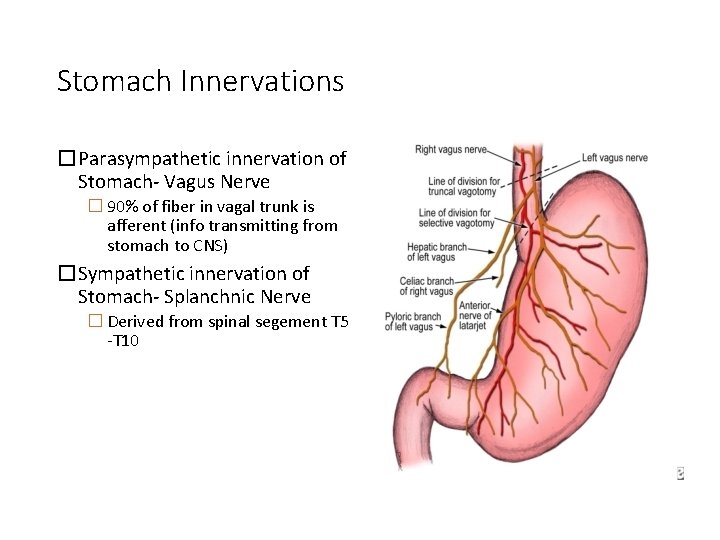
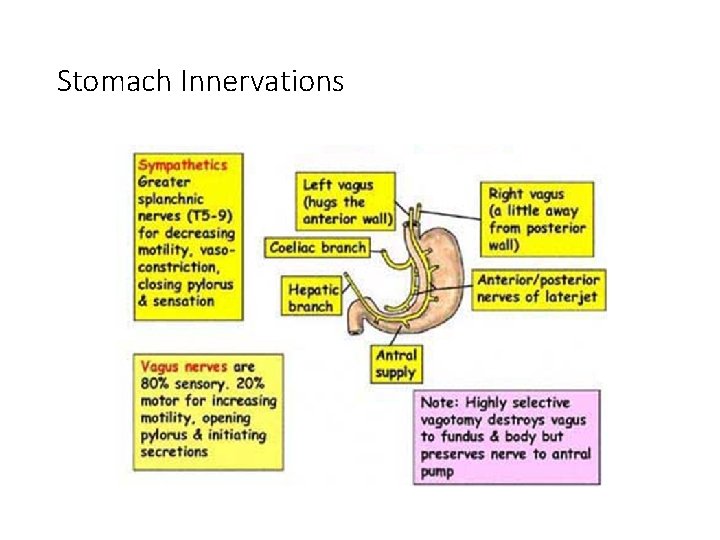
Stomach Innervations The main innervations are Left ( anterior )and Right ( posterior) Vagus Nerves.
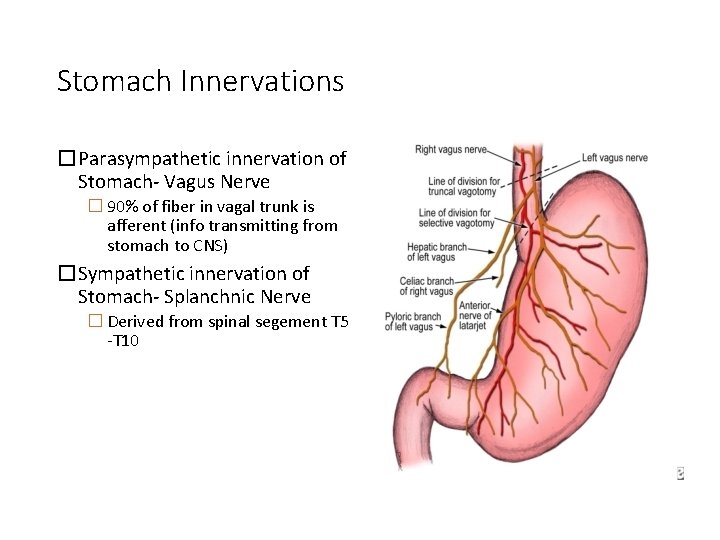
Stomach Innervations �Parasympathetic innervation of Stomach- Vagus Nerve � 90% of fiber in vagal trunk is afferent (info transmitting from stomach to CNS) �Sympathetic innervation of Stomach- Splanchnic Nerve � Derived from spinal segement T 5 -T 10
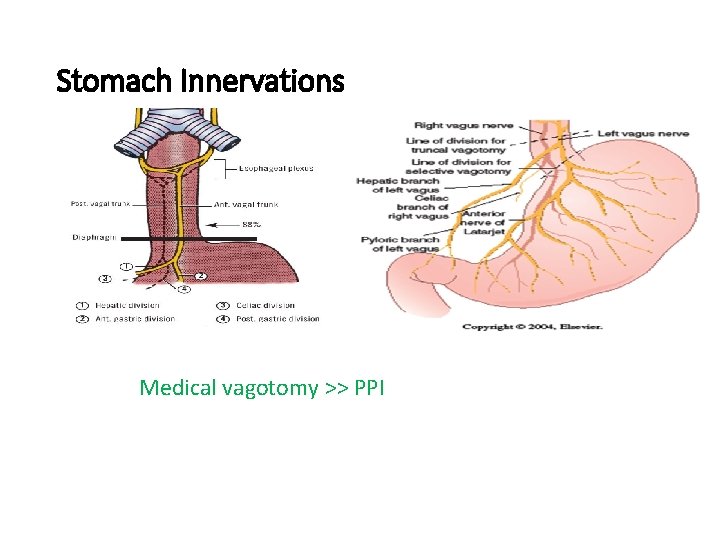
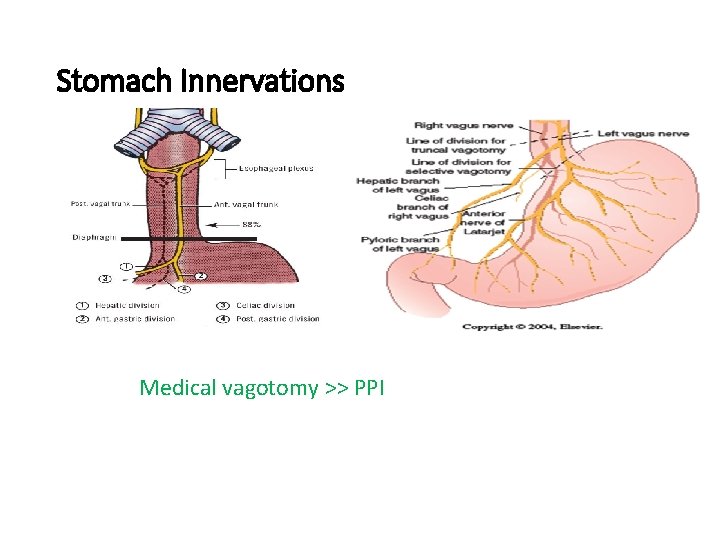
Stomach Innervations Medical vagotomy >> PPI
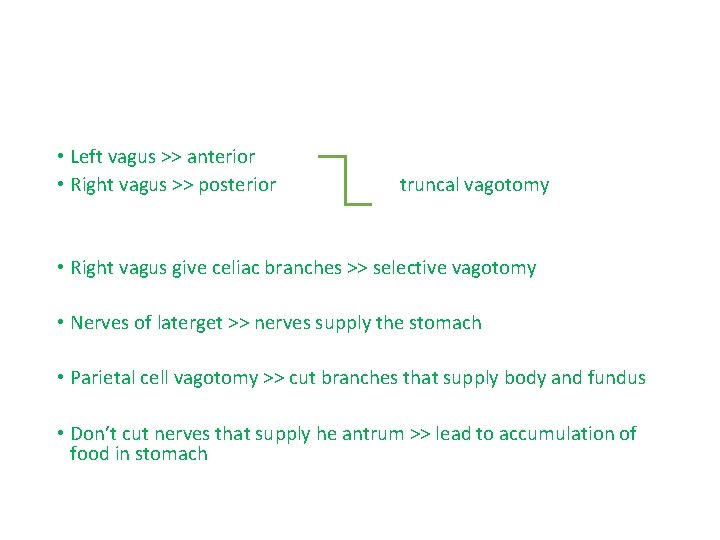
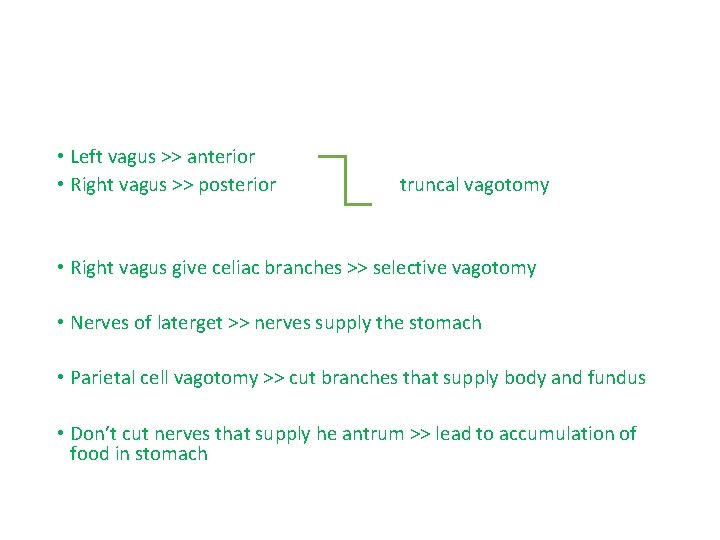
• Left vagus >> anterior • Right vagus >> posterior truncal vagotomy • Right vagus give celiac branches >> selective vagotomy • Nerves of laterget >> nerves supply the stomach • Parietal cell vagotomy >> cut branches that supply body and fundus • Don’t cut nerves that supply he antrum >> lead to accumulation of food in stomach
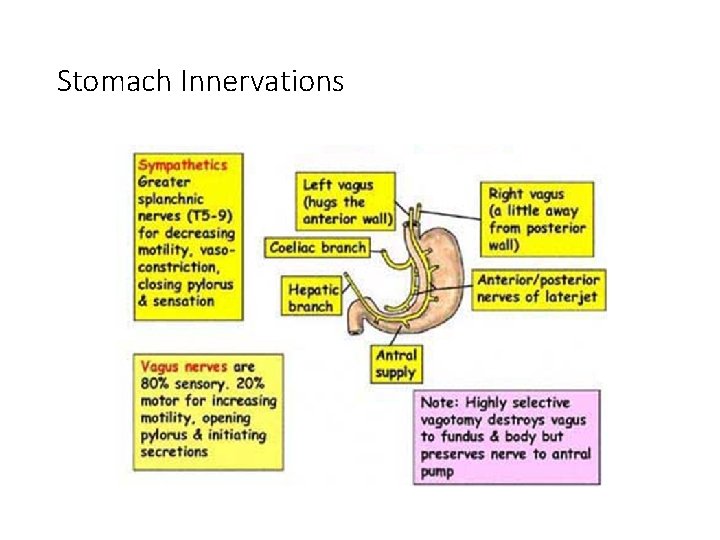
Stomach Innervations
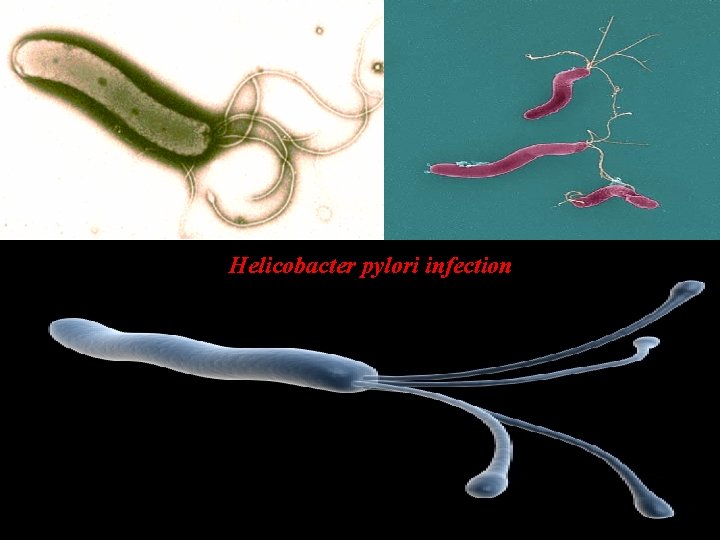
Helicobacter pylori infection
• Early stage of lymphoma can be treated by triple assessment : ( PPI and 2 antibiotics )

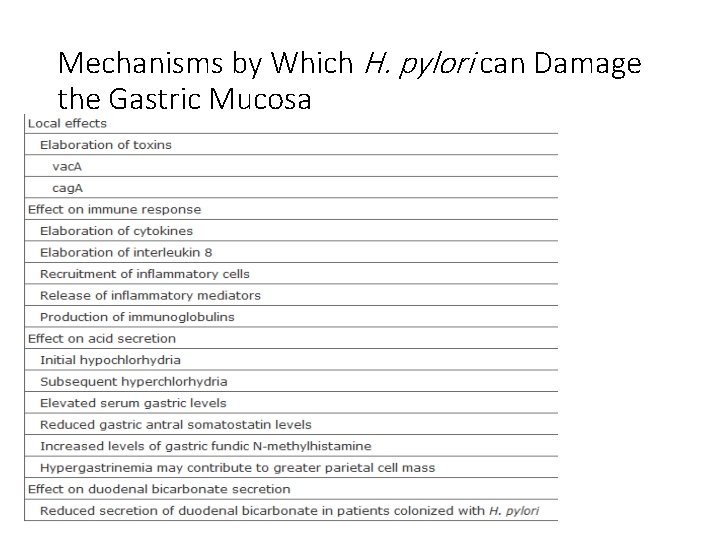
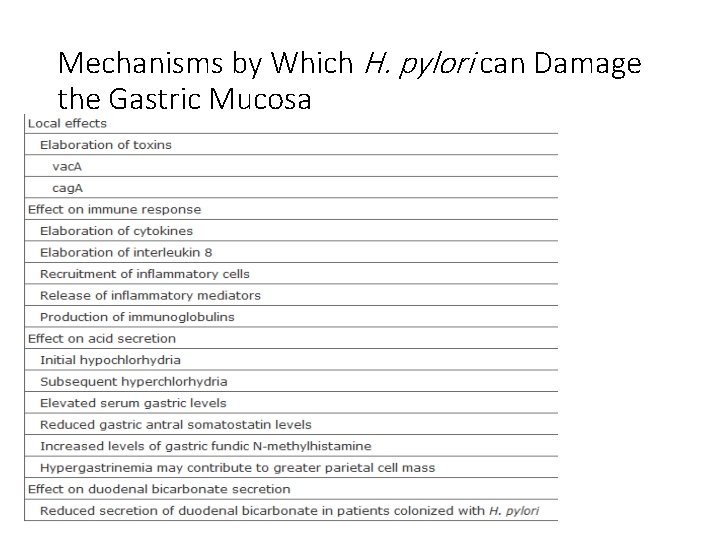
Mechanisms by Which H. pylori can Damage the Gastric Mucosa
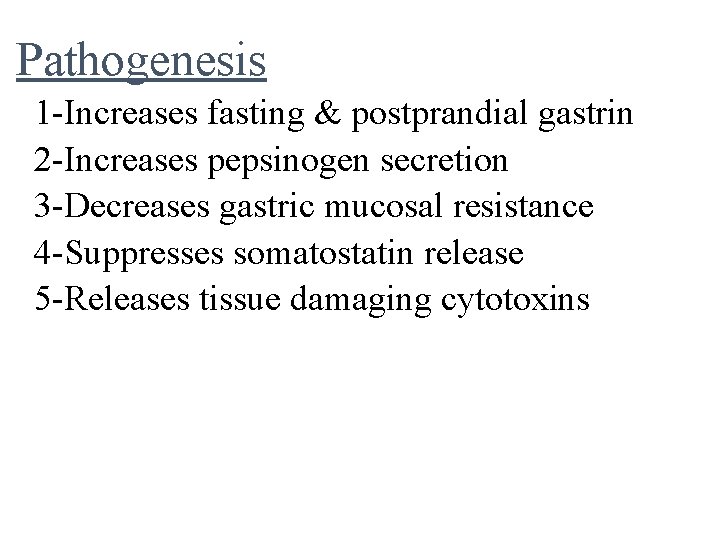
Pathogenesis 1 -Increases fasting & postprandial gastrin 2 -Increases pepsinogen secretion 3 -Decreases gastric mucosal resistance 4 -Suppresses somatostatin release 5 -Releases tissue damaging cytotoxins
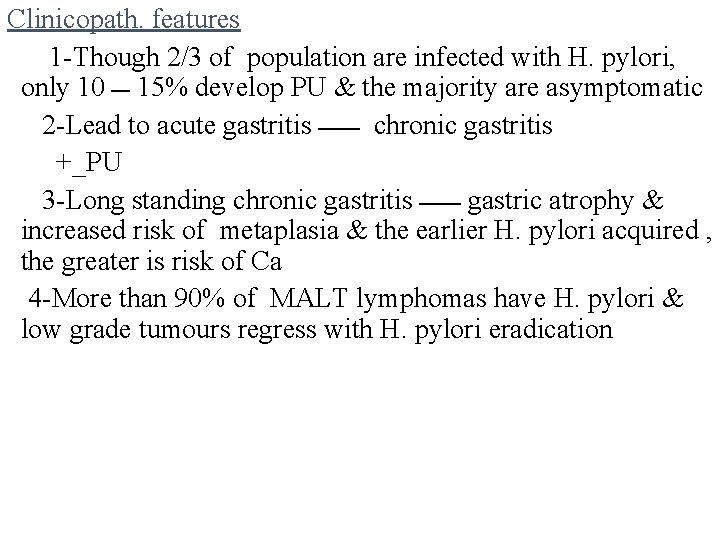
Clinicopath. features 1 -Though 2/3 of population are infected with H. pylori, only 10 ـــ 15% develop PU & the majority are asymptomatic 2 -Lead to acute gastritis ـــــــ chronic gastritis +_PU 3 -Long standing chronic gastritis ـــــــ gastric atrophy & increased risk of metaplasia & the earlier H. pylori acquired , the greater is risk of Ca 4 -More than 90% of MALT lymphomas have H. pylori & low grade tumours regress with H. pylori eradication
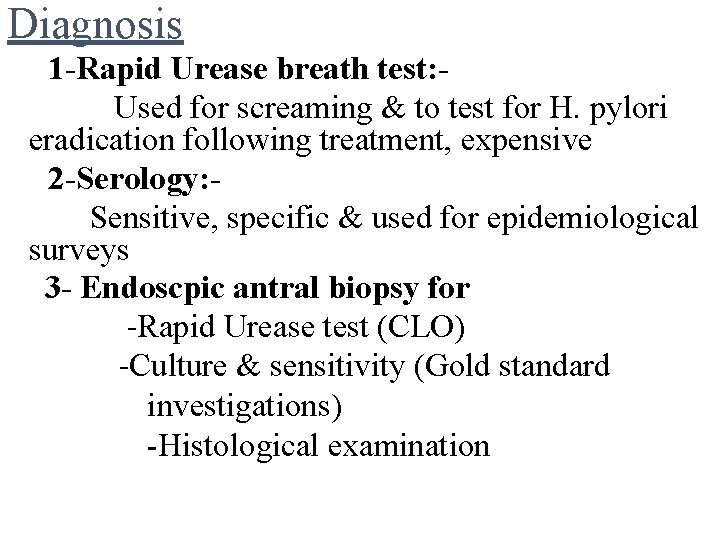
Diagnosis 1 -Rapid Urease breath test: Used for screaming & to test for H. pylori eradication following treatment, expensive 2 -Serology: Sensitive, specific & used for epidemiological surveys 3 - Endoscpic antral biopsy for -Rapid Urease test (CLO) -Culture & sensitivity (Gold standard investigations) -Histological examination
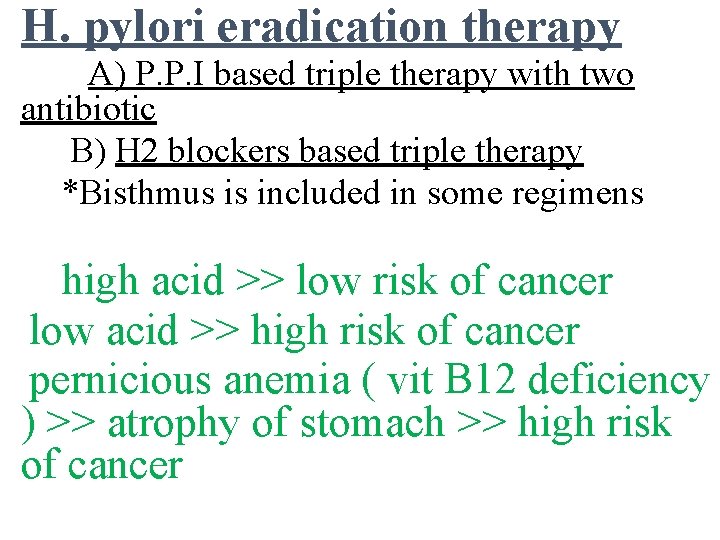
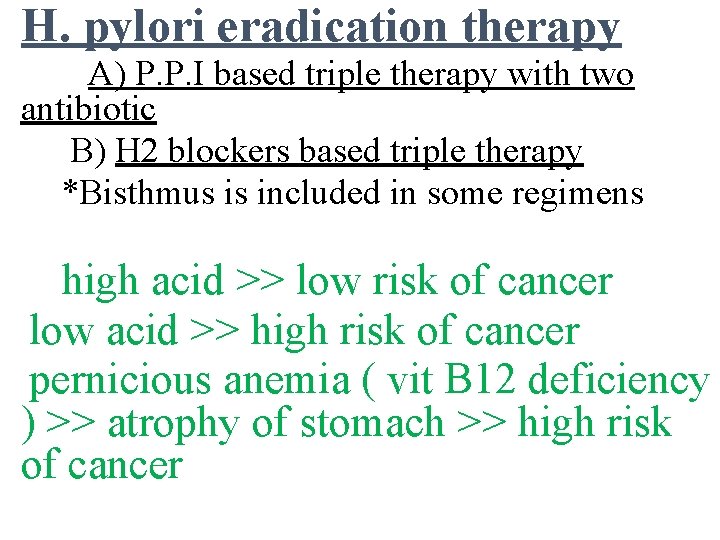
H. pylori eradication therapy A) P. P. I based triple therapy with two antibiotic B) H 2 blockers based triple therapy *Bisthmus is included in some regimens high acid >> low risk of cancer low acid >> high risk of cancer pernicious anemia ( vit B 12 deficiency ) >> atrophy of stomach >> high risk of cancer
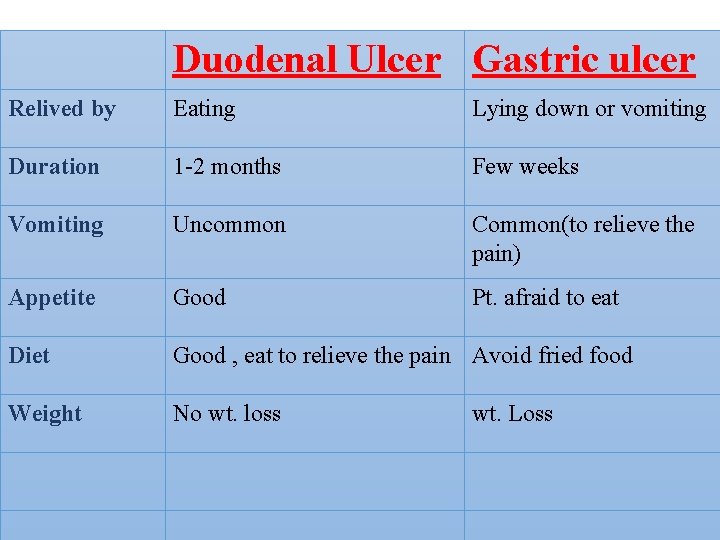
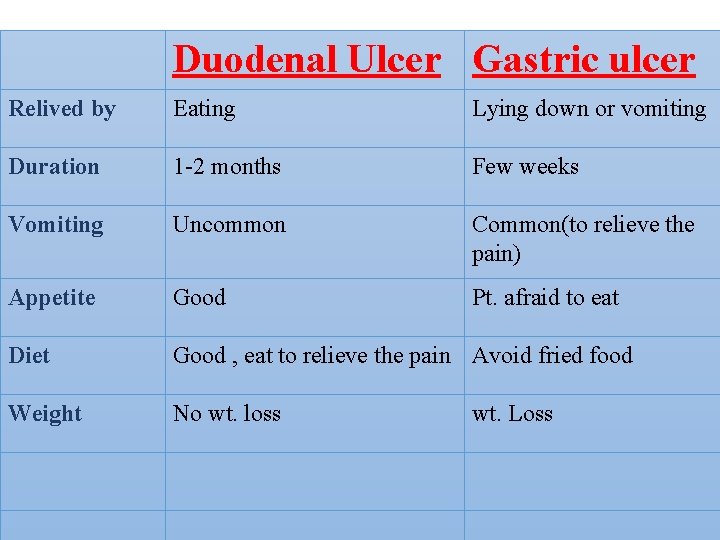
Duodenal Ulcer Gastric ulcer Relived by Eating Lying down or vomiting Duration 1 -2 months Few weeks Vomiting Uncommon Common(to relieve the pain) Appetite Good Pt. afraid to eat Diet Good , eat to relieve the pain Avoid fried food Weight No wt. loss wt. Loss
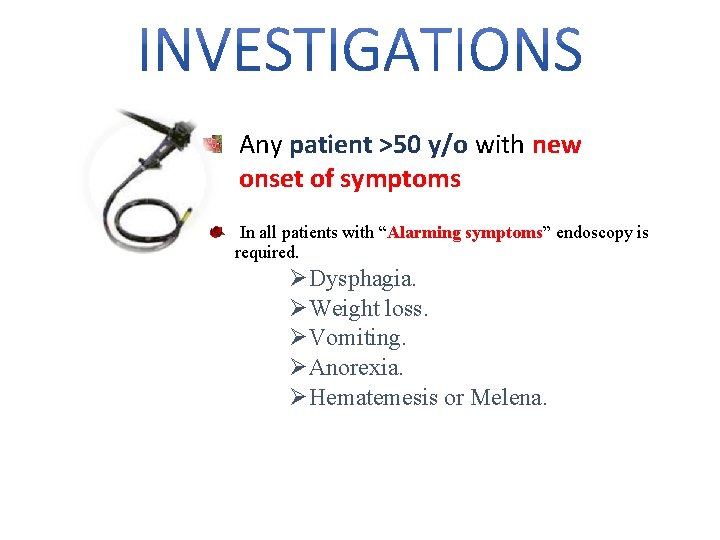
Any patient >50 y/o with new onset of symptoms In all patients with “Alarming symptoms” endoscopy is required. ØDysphagia. ØWeight loss. ØVomiting. ØAnorexia. ØHematemesis or Melena.
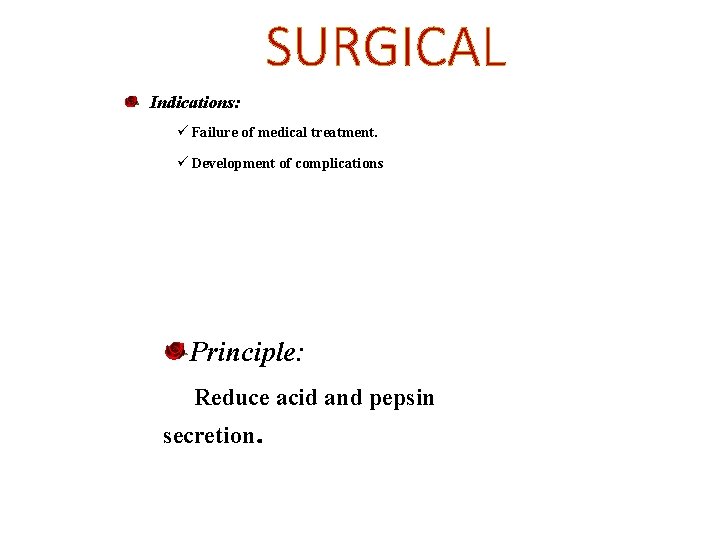
SURGICAL Indications: ü Failure of medical treatment. ü Development of complications Principle: Reduce acid and pepsin secretion.
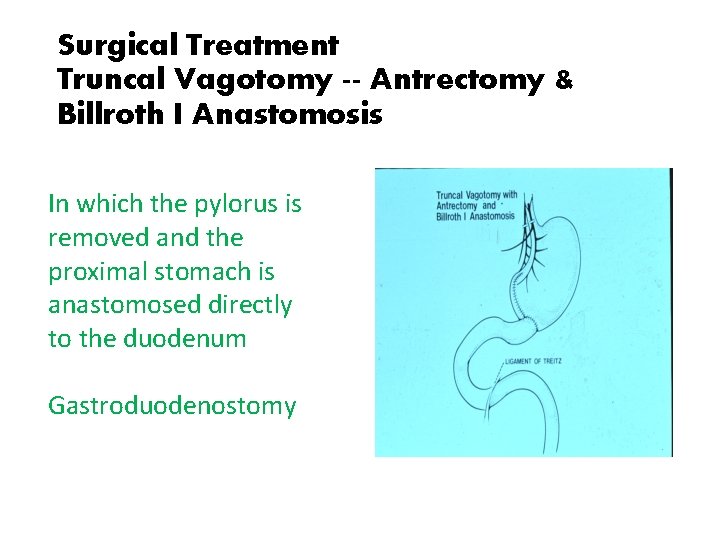
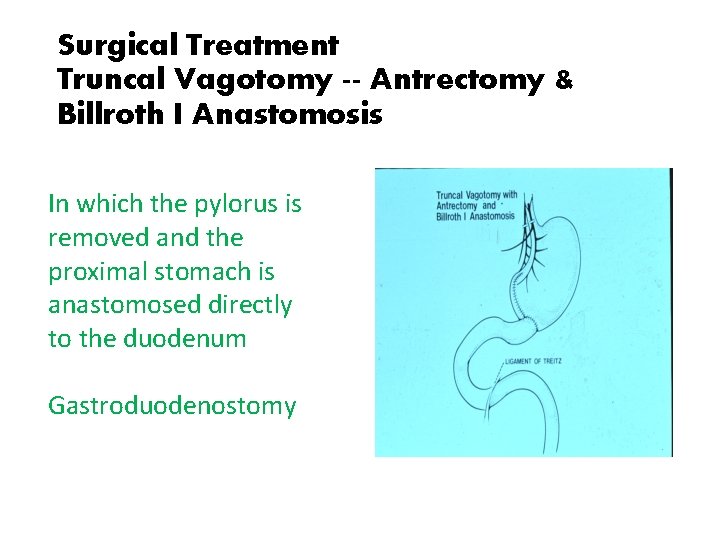
Surgical Treatment Truncal Vagotomy -- Antrectomy & Billroth I Anastomosis In which the pylorus is removed and the proximal stomach is anastomosed directly to the duodenum Gastroduodenostomy
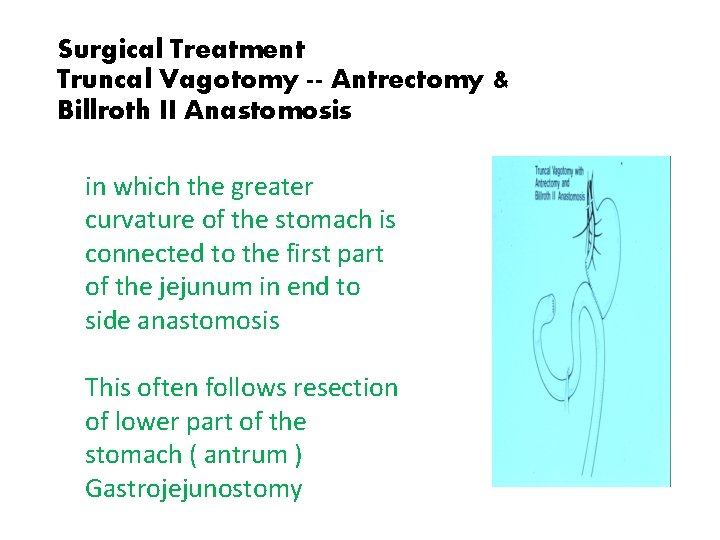
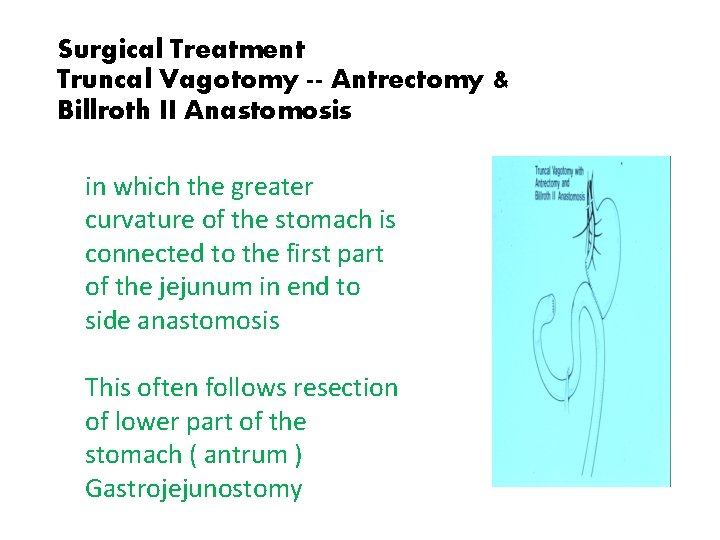
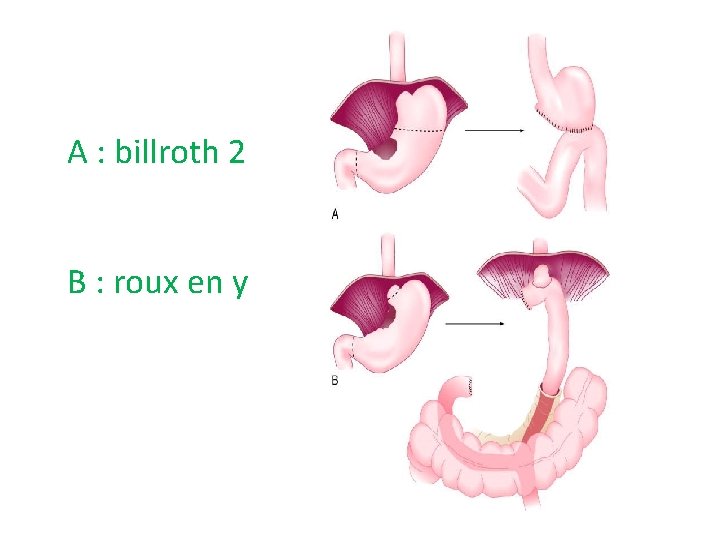
Surgical Treatment Truncal Vagotomy -- Antrectomy & Billroth II Anastomosis in which the greater curvature of the stomach is connected to the first part of the jejunum in end to side anastomosis This often follows resection of lower part of the stomach ( antrum ) Gastrojejunostomy
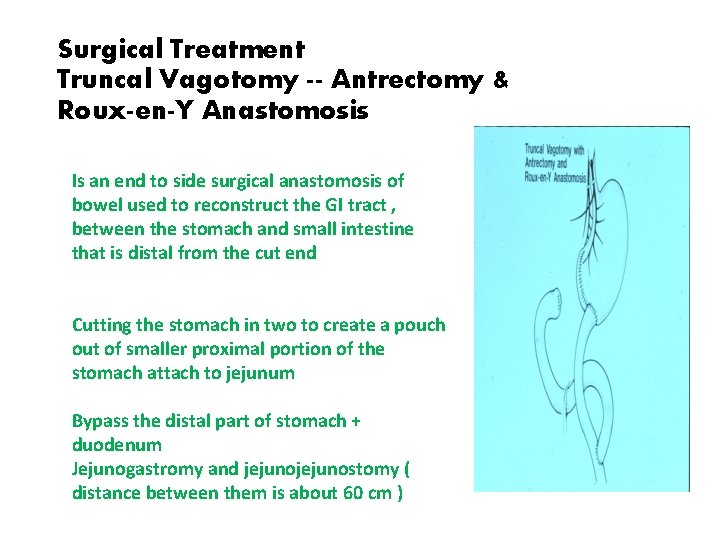
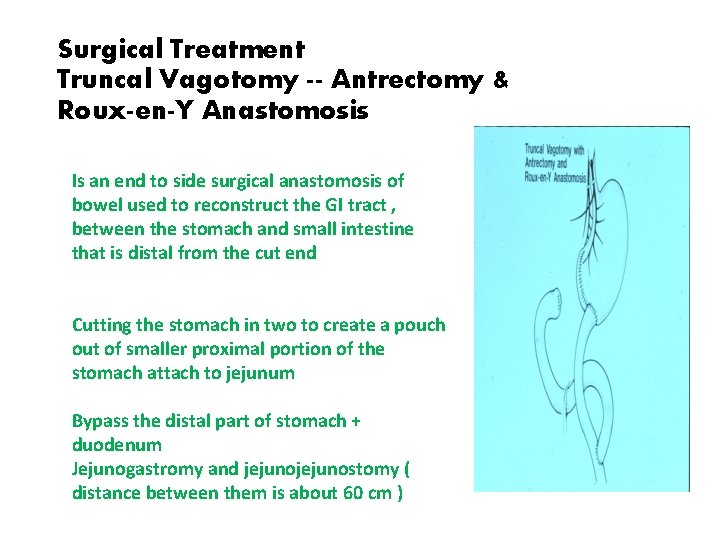
Surgical Treatment Truncal Vagotomy -- Antrectomy & Roux-en-Y Anastomosis Is an end to side surgical anastomosis of bowel used to reconstruct the GI tract , between the stomach and small intestine that is distal from the cut end Cutting the stomach in two to create a pouch out of smaller proximal portion of the stomach attach to jejunum Bypass the distal part of stomach + duodenum Jejunogastromy and jejunostomy ( distance between them is about 60 cm )

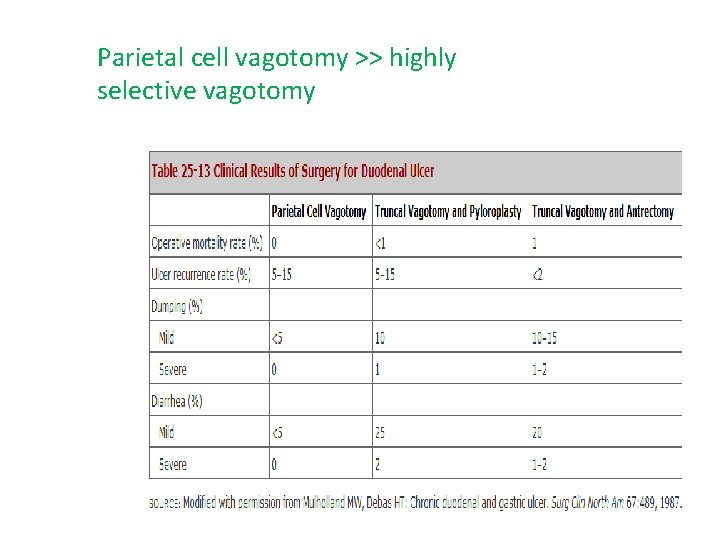
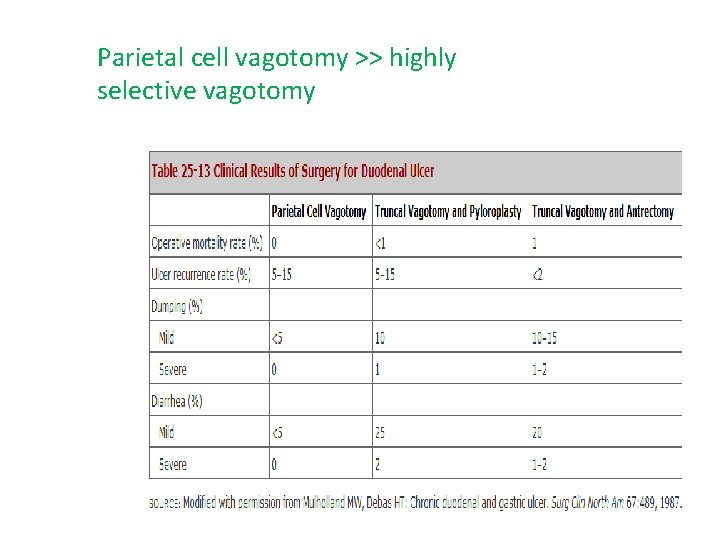
Parietal cell vagotomy >> highly selective vagotomy

Stomach Postgastrectomy Syndromes • Due to denervation of stomach the pyloric mechanism becomes incompetent and the control of stomach emptying is abolish. If we add the re-anastomotic of duodenum, posgastrectomy syndromes are the consequence. • Early Dumping syndrome • Late dumping syndrome • Post-vagotomy Diarrhea • Afferent loop obstruction • Blind loop syndrome • Alkaline Reflux gastritis • Recurrent ulcer Ds • Gastric atony • Metabolic disturbances
Stomach Early Dumping Syndrome � Symptoms occurs 15 minutes after meal. � S/S: � Anxiety, extreme weakness, tachycardia, diaphoresis, palpitations, and desire to lie down. Also borborygmi are heard and diarrhea is common. Symptoms disappear gradually. � Pathophysiology: � it is an uncontrolled emptying of hypertonic fluid into small intestine. � Fluid moves rapidly from intravascular space into intraluminal space producing acute intravascular volume depletion. � As simple sugars are absorbed and dilution of hypertonic solution occurs the symptoms decreased. � Substances like serotonin, neurotensin, histamine, glucagon, vasoactive intestinal peptide, kinins. � Treated by fluid

Stomach Early dumping syndrome • • • MCC are Billroth I and II. Tx: Somatostatin analogue, may be of benefit, and Beta blockers. Avoid hypertonic liquid meals. Altering the volume of meals. Ingest some fat to slow gastric emptying Liquids should be ingested before meals or 30’ after meals. Billroth I and II are MCC. Roux en Y is sometimes indicated b/c delays emptying.
Stomach Late dumping syndrome • Symptoms begin 3 hours after meals. • S/S: • Sudden anxiety, diaphoresis, tachycardia, palpitations, weakness, fatigue, and desire to lie down. • It is not associated with borborygm or diarrhea. • Pathophysiology: • Rapid changes in serum glucose and insulin levels. • Large glucose-bolus containing chyme presented to small intestine has a lot of glucose in it, glucose is absorbed faster than when the intact pylorus controls emptying of stomach. This causes high levels of serum glucose shortly after meal and causes a big released of insulin. Insulin response exceeds what is necessary to clear glucose from blood and hypoglycemia symptoms happens. Symptoms are due to rapid fluctuations in serum glucose levels. • ( hypoglycemia + hypovolemia )
Stomach Late Dumping syndrome • • Tx: Conservative Small snacks 2 hours after meals If symptoms can not be controlled then the previous procedure has to be converted to Billroth I or Roux en Y gastrojejunostomy.
Complication of peptic ulcer : • 1 - bleeding : Stabilized by cauterization , adrenaline , clipping Sclerosing agent just in case of venous bleeding We cant stop bleeding by endoscopy , we do surgery >> open longitudinal and close transverse to prevent stenosis or leak 2 - perforation : lead to chemical peritonitis then due to dilution of the chemicals ( subside ) then super added by infection ( purulent peritonitis ) Purulent peritonitis stabilized by ( iv fluid , correction of electrolytes , open abdomen or laparoscopy )
• Duodenal ulcer treated by Graham patch surgical technique >> piece of omentum is used to cover the perforation • Gastric outlet obstruction : edema with fibrosis , recurrent Treatment : Conservative , iv fluid , NPO , correction of acid base balance and electrolytes , endoscopy , surgery : billroth 1 , 2 Duodenal ulcer >> no transformation to malignancy Gastric ulcer >> littlie transformation

Gastric Cancer(GC)
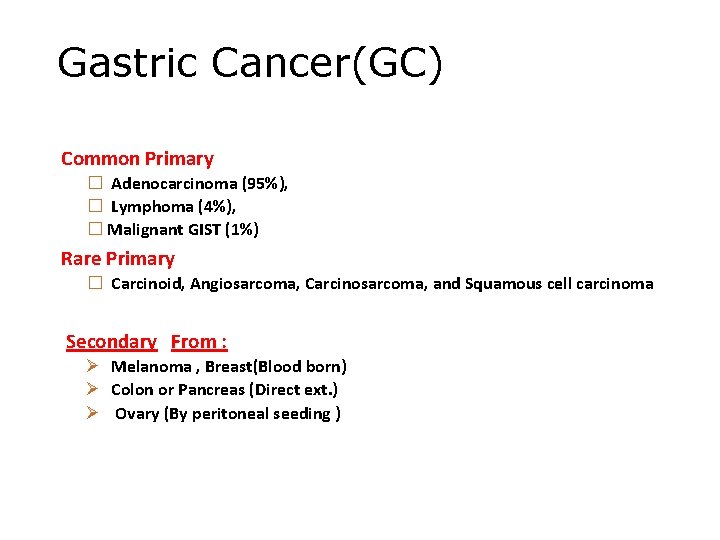
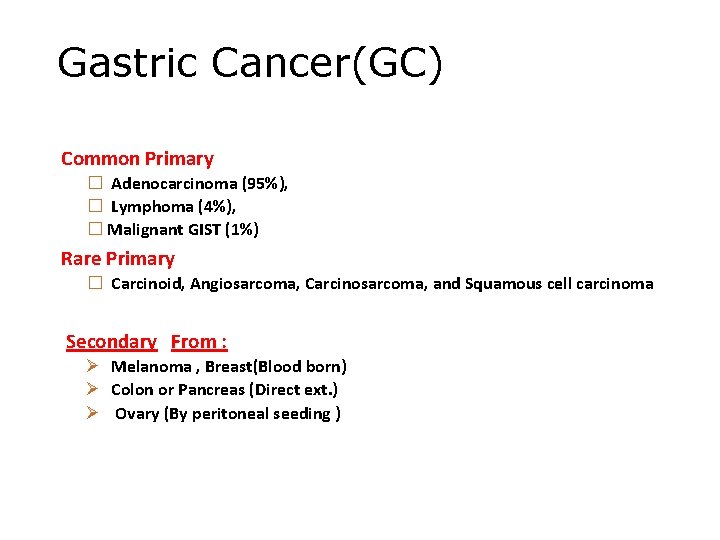
Gastric Cancer(GC) Common Primary � Adenocarcinoma (95%), � Lymphoma (4%), � Malignant GIST (1%) Rare Primary � Carcinoid, Angiosarcoma, Carcinosarcoma, and Squamous cell carcinoma Secondary From : Ø Melanoma , Breast(Blood born) Ø Colon or Pancreas (Direct ext. ) Ø Ovary (By peritoneal seeding )
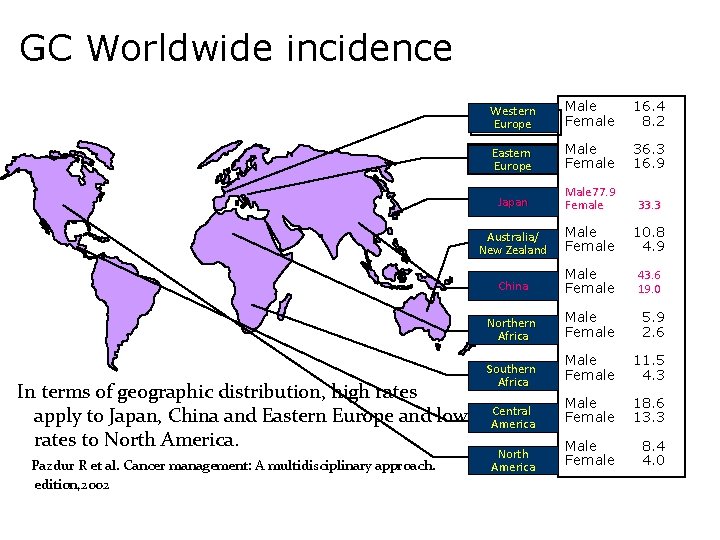
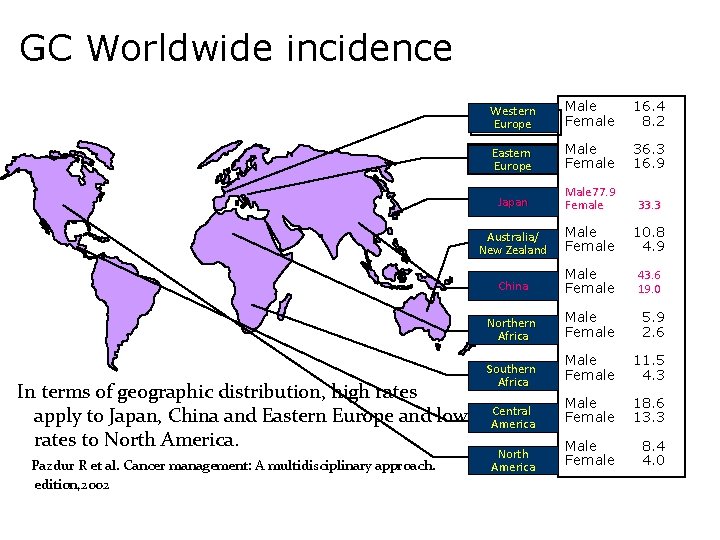
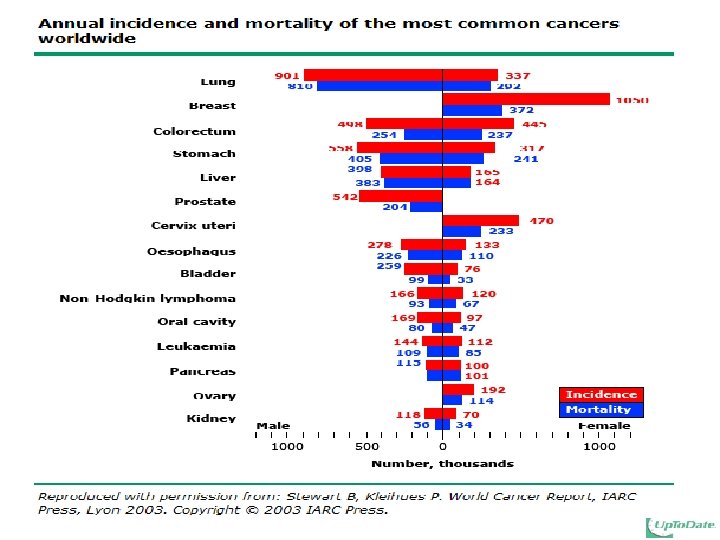
GC Worldwide incidence In terms of geographic distribution, high rates apply to Japan, China and Eastern Europe and low rates to North America. Pazdur R et al. Cancer management: A multidisciplinary approach. edition, 2002 Western Europe Male Female 16. 4 8. 2 Eastern Europe Male Female 36. 3 16. 9 Japan Male 77. 9 Female 33. 3 Australia/ New Zealand Male Female 10. 8 4. 9 China Male Female 43. 6 19. 0 Northern Africa Male Female 5. 9 2. 6 Male Female 11. 5 4. 3 Male Female 18. 6 13. 3 Male Female 8. 4 4. 0 Southern Africa Central America North America
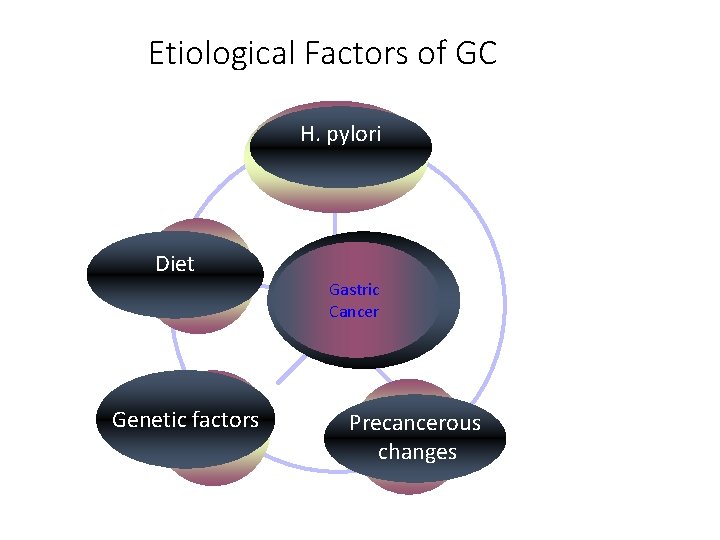
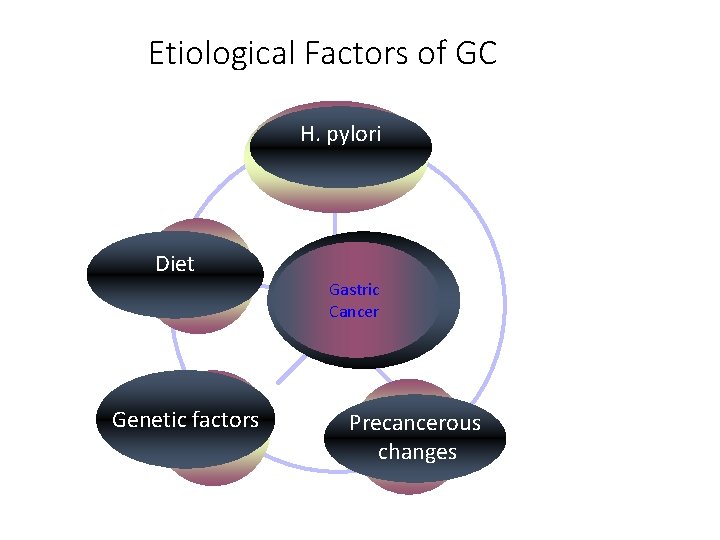
Etiological Factors of GC H. pylori Diet Gastric Cancer Genetic factors Precancerous changes
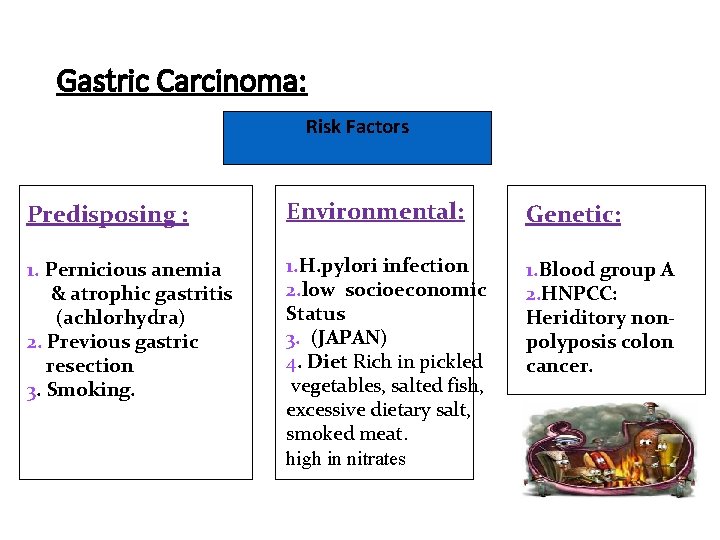
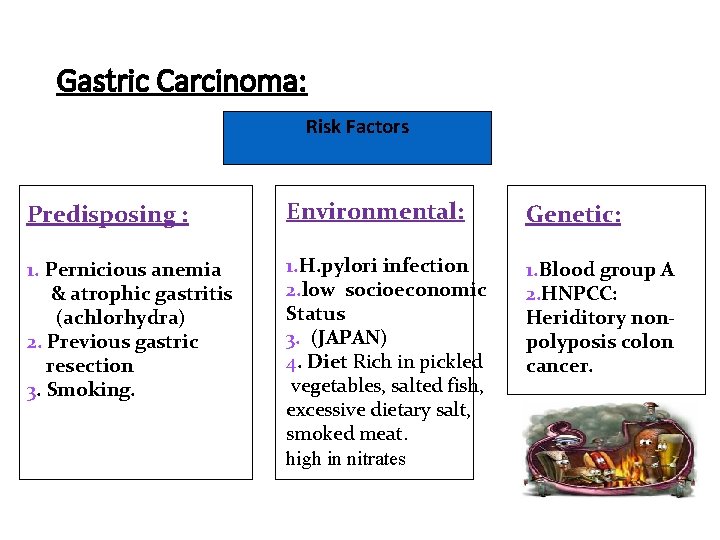
Gastric Carcinoma: Risk Factors Predisposing : Environmental: Genetic: 1. Pernicious anemia & atrophic gastritis (achlorhydra) 2. Previous gastric resection 3. Smoking. 1. H. pylori infection 2. low socioeconomic Status 3. (JAPAN) 4. Diet Rich in pickled vegetables, salted fish, excessive dietary salt, smoked meat. high in nitrates 1. Blood group A 2. HNPCC: Heriditory nonpolyposis colon cancer.
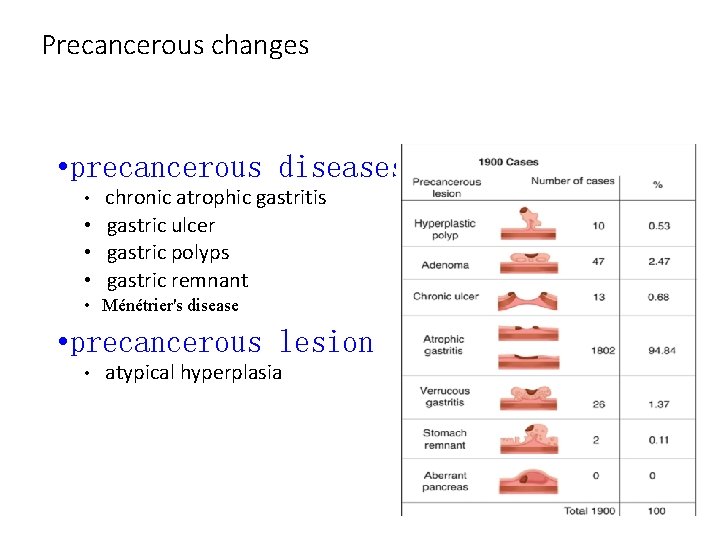
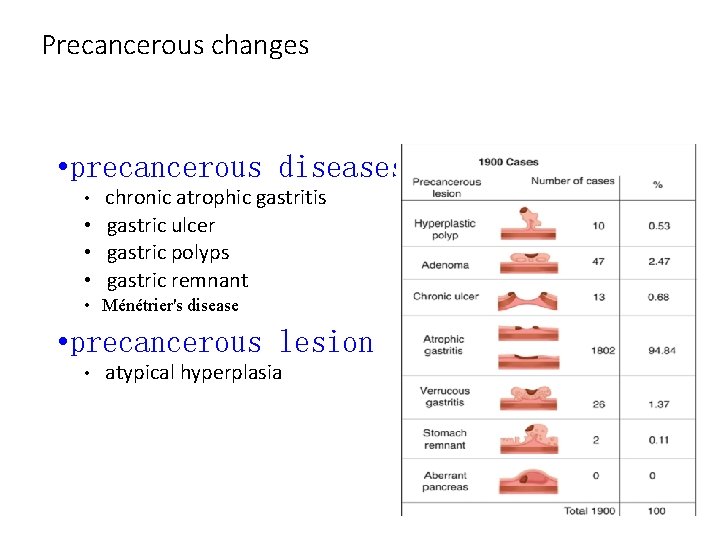
Precancerous changes • precancerous diseases • chronic atrophic gastritis • gastric ulcer • gastric polyps • gastric remnant • Ménétrier's disease • precancerous lesion • atypical hyperplasia
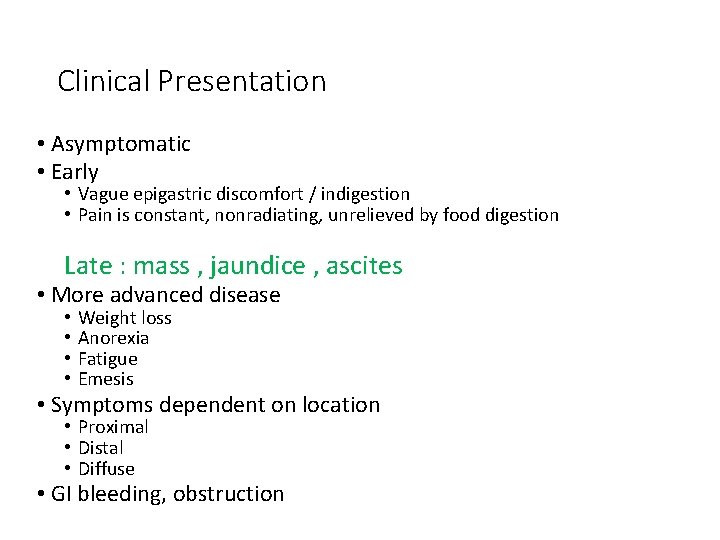
Clinical Presentation • Asymptomatic • Early • Vague epigastric discomfort / indigestion • Pain is constant, nonradiating, unrelieved by food digestion Late : mass , jaundice , ascites • More advanced disease • • Weight loss Anorexia Fatigue Emesis • Symptoms dependent on location • Proximal • Distal • Diffuse • GI bleeding, obstruction
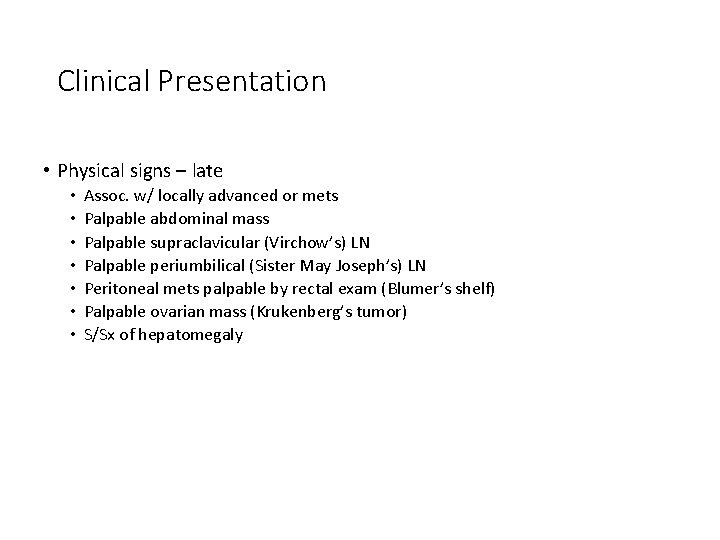
Clinical Presentation • Physical signs – late • • Assoc. w/ locally advanced or mets Palpable abdominal mass Palpable supraclavicular (Virchow’s) LN Palpable periumbilical (Sister May Joseph’s) LN Peritoneal mets palpable by rectal exam (Blumer’s shelf) Palpable ovarian mass (Krukenberg’s tumor) S/Sx of hepatomegaly
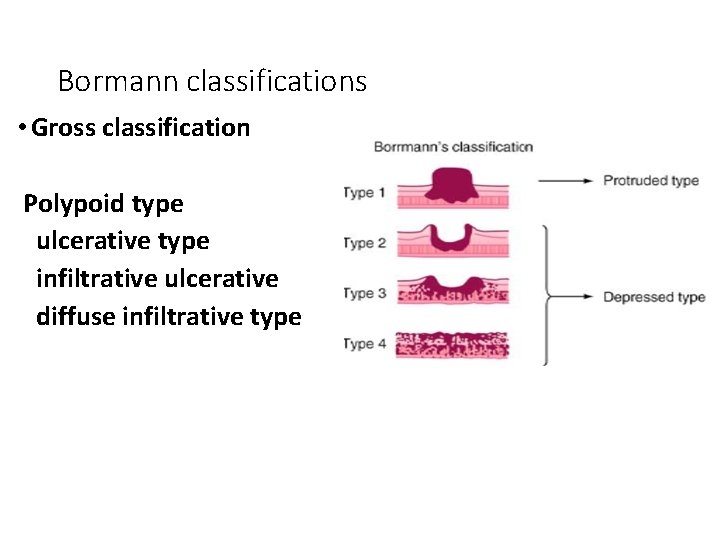
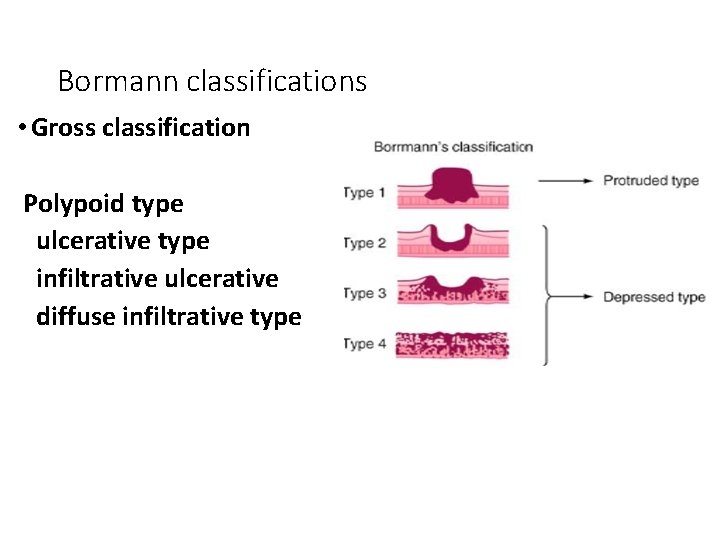
Bormann classifications • Gross classification Polypoid type ulcerative type infiltrative ulcerative diffuse infiltrative type
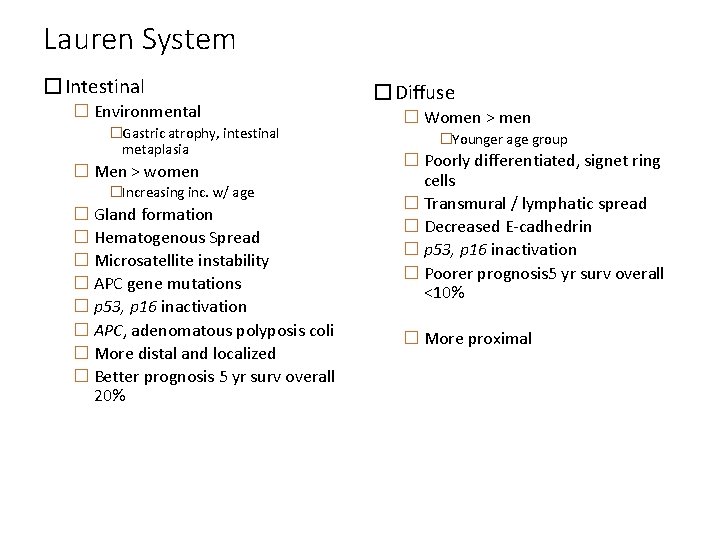
Lauren System �Intestinal � Environmental �Gastric atrophy, intestinal metaplasia � Men > women �Increasing inc. w/ age � Gland formation � Hematogenous Spread � Microsatellite instability � APC gene mutations � p 53, p 16 inactivation � APC, adenomatous polyposis coli � More distal and localized � Better prognosis 5 yr surv overall 20% �Diffuse � Women > men �Younger age group � Poorly differentiated, signet ring cells � Transmural / lymphatic spread � Decreased E-cadhedrin � p 53, p 16 inactivation � Poorer prognosis 5 yr surv overall <10% � More proximal
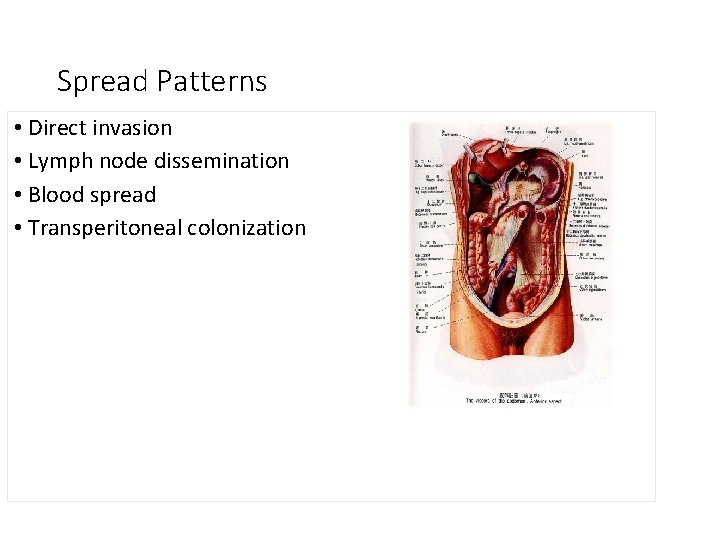
Spread Patterns • Direct invasion • Lymph node dissemination • Blood spread • Transperitoneal colonization
Laboratory tests �Assists in determining optimal therapy. �CBC identifies anemia , with maybe caused by bleeding , liver dysfunction, or poor nutrition. � 15 -20% have anemia. �Tumor markers : 1 -CEA : carcino-embryonic antigen 2 -CA 19 -9: carbohydrte Antigen 3 -CA 724: carbohydrate Antigen
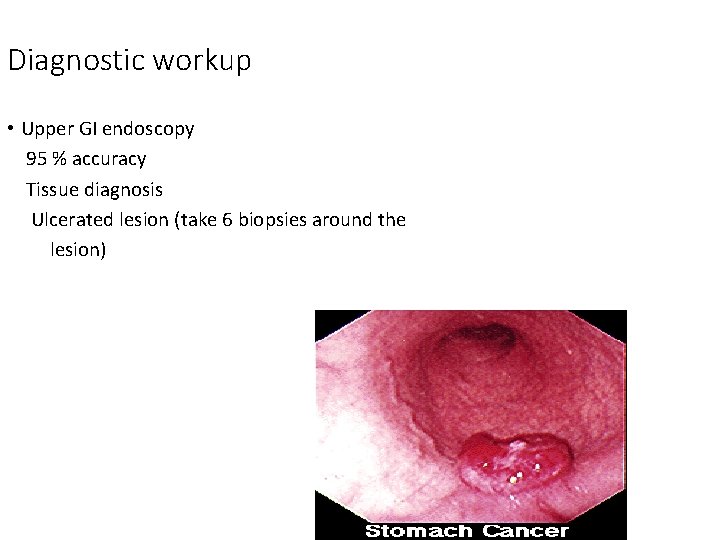
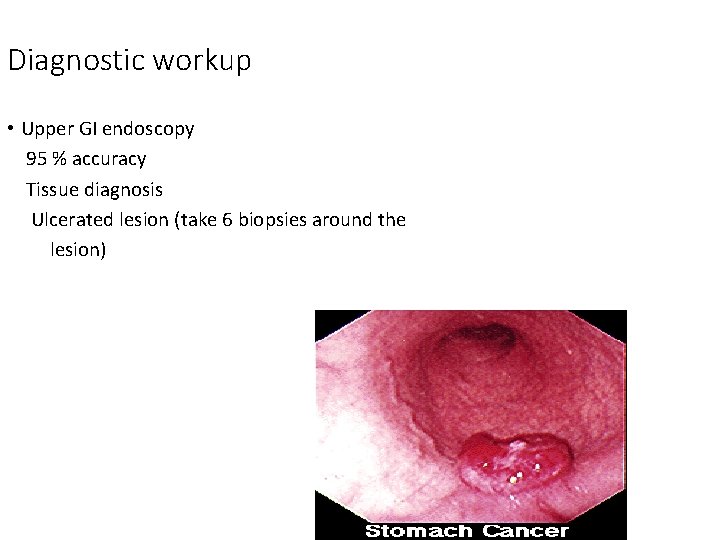
Diagnostic workup • Upper GI endoscopy 95 % accuracy Tissue diagnosis Ulcerated lesion (take 6 biopsies around the lesion)
Contd: • Double contrast upper GI series And Barium swallow 75% accuracy for obstructive lesions only
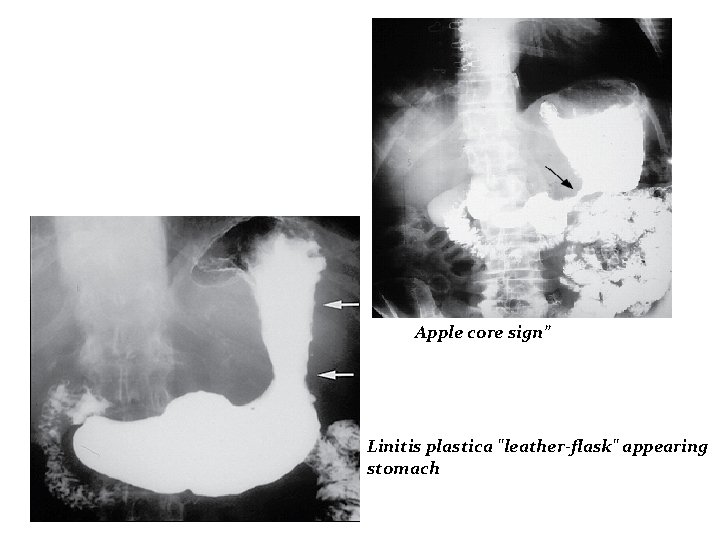
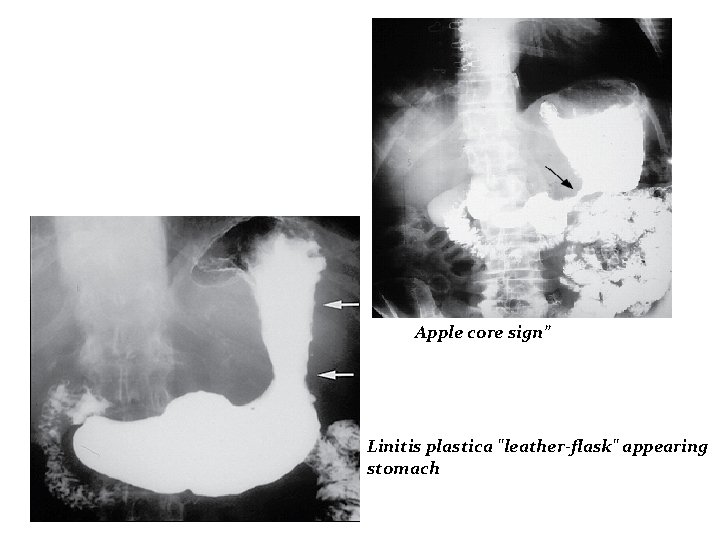
Apple core sign” Linitis plastica "leather-flask" appearing stomach
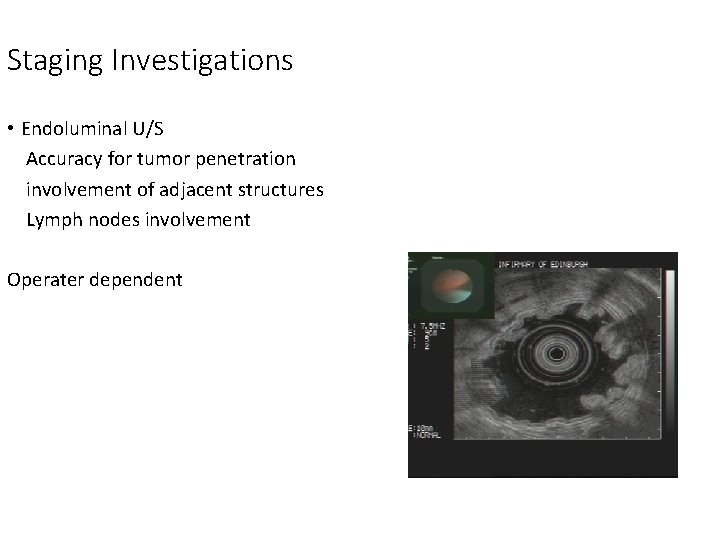
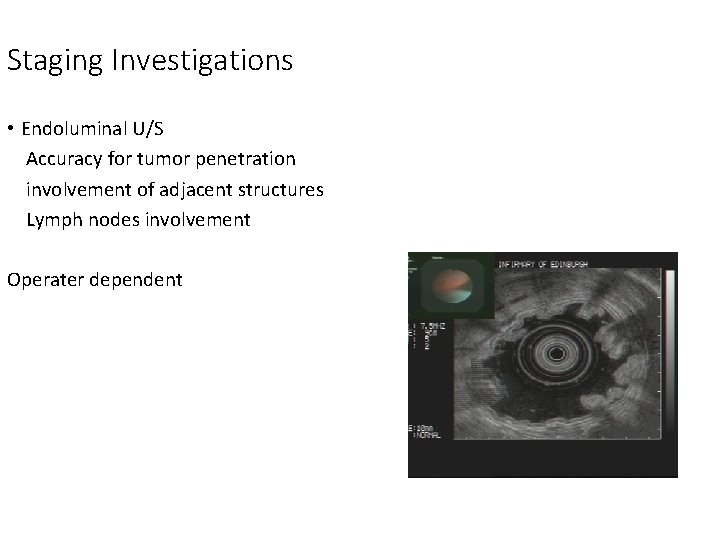
Staging Investigations • Endoluminal U/S Accuracy for tumor penetration involvement of adjacent structures Lymph nodes involvement Operater dependent
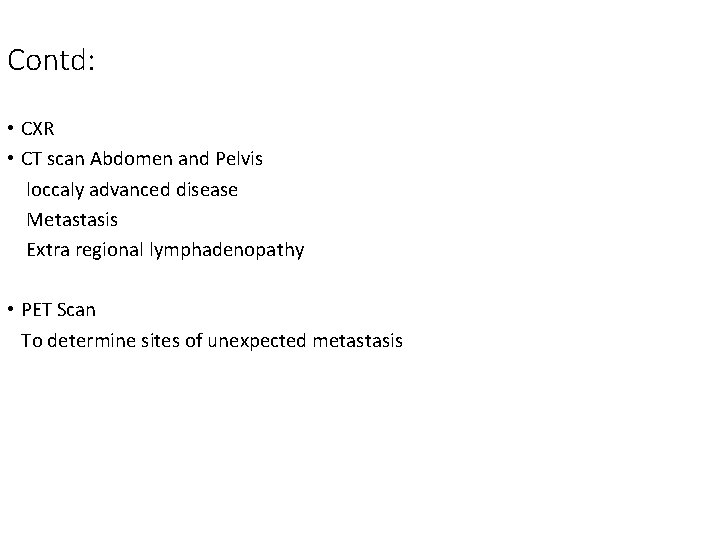
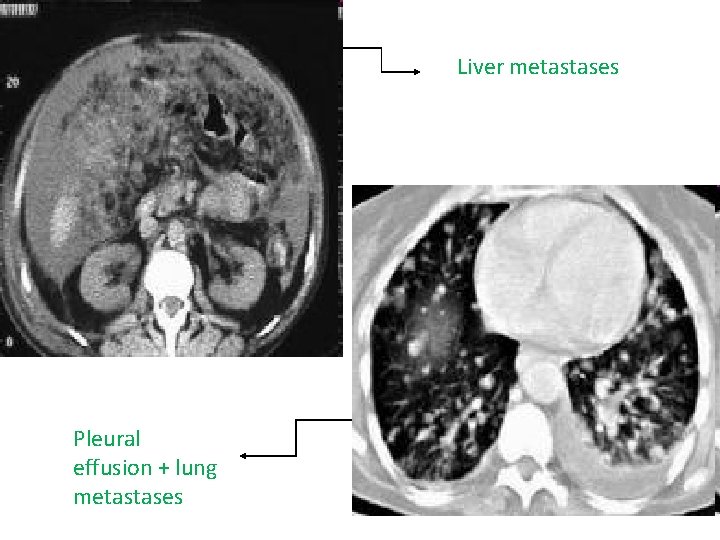
Contd: • CXR • CT scan Abdomen and Pelvis loccaly advanced disease Metastasis Extra regional lymphadenopathy • PET Scan To determine sites of unexpected metastasis
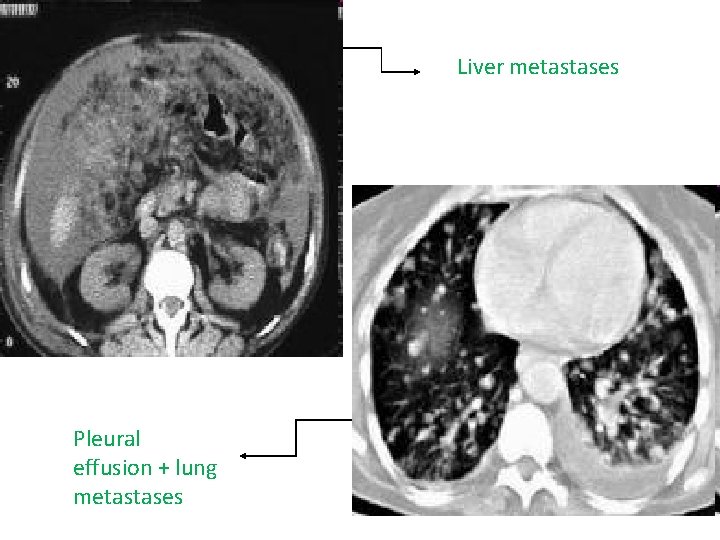
Liver metastases Pleural effusion + lung metastases
Contd: • Staging Laproscopy To determine possibilty of curitive lesion look for peritoneal and hepatic mets Curative surgery : safety margin , resume the continuity of the bowel , resection of tumor and lymph node TLC : tender love and care
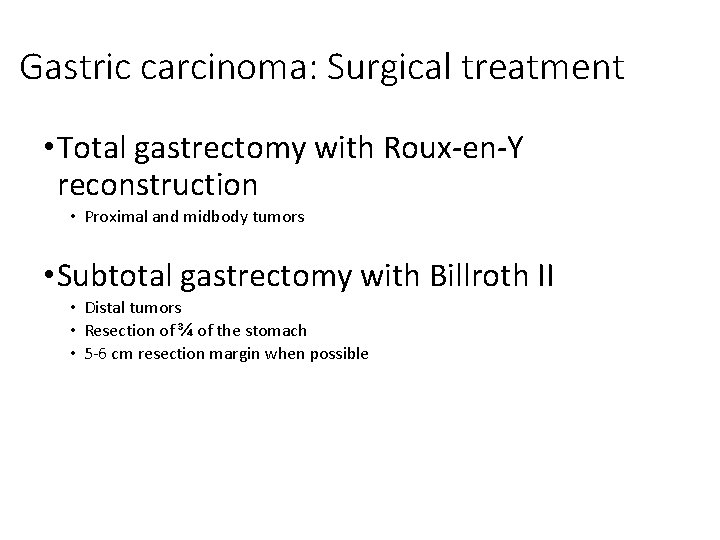
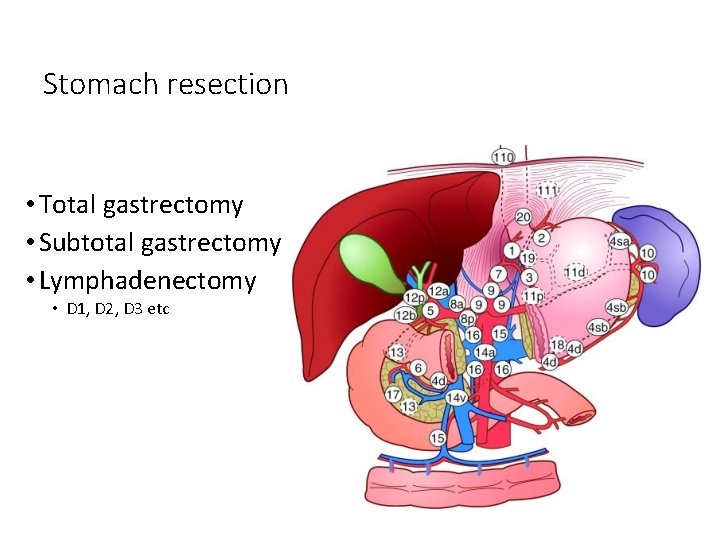
Gastric carcinoma: Surgical treatment • Total gastrectomy with Roux-en-Y reconstruction • Proximal and midbody tumors • Subtotal gastrectomy with Billroth II • Distal tumors • Resection of ¾ of the stomach • 5 -6 cm resection margin when possible
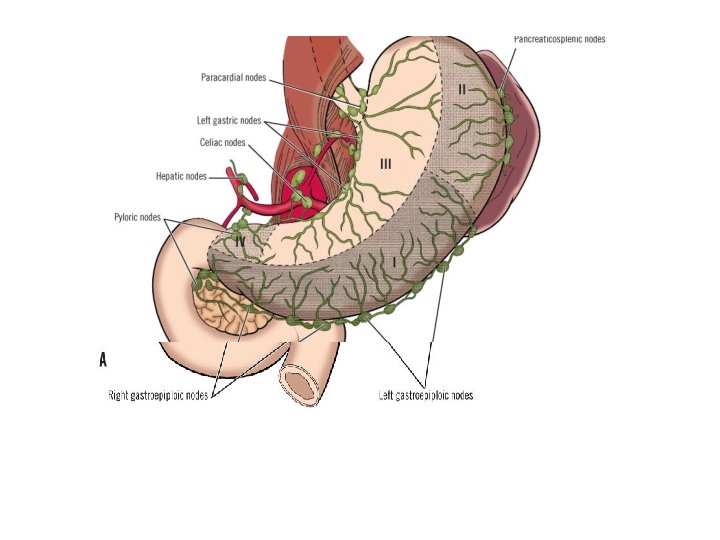
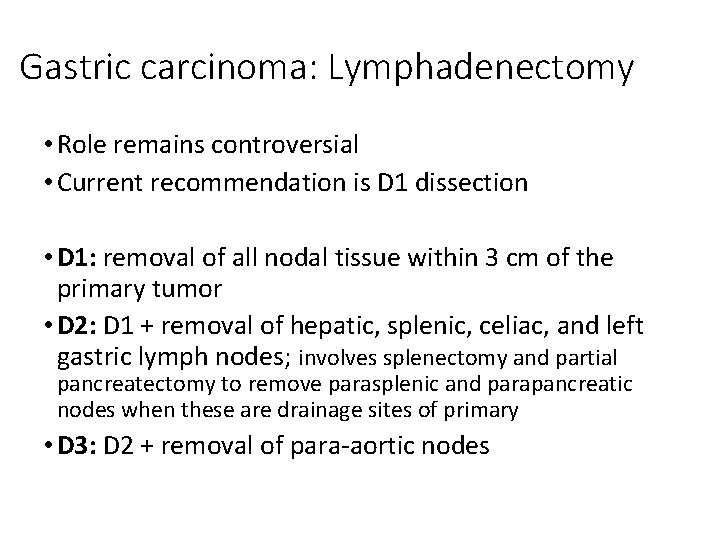
Gastric carcinoma: Lymphadenectomy • Role remains controversial • Current recommendation is D 1 dissection • D 1: removal of all nodal tissue within 3 cm of the primary tumor • D 2: D 1 + removal of hepatic, splenic, celiac, and left gastric lymph nodes; involves splenectomy and partial pancreatectomy to remove parasplenic and parapancreatic nodes when these are drainage sites of primary • D 3: D 2 + removal of para-aortic nodes

Lymph node metastasis • Radial spread • D 1 nodes • Perigastric nodes • D 2 nodes • Hepatic, splenic, coeliac • D 3 nodes • Para-aortic nodes
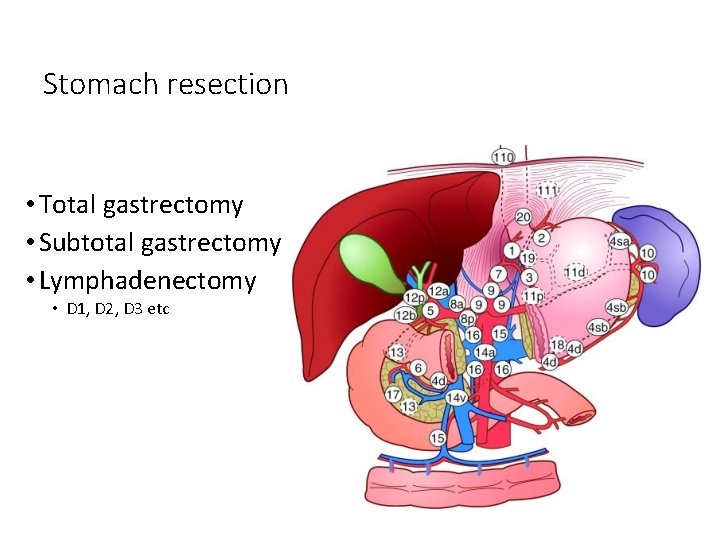
Stomach resection • Total gastrectomy • Subtotal gastrectomy • Lymphadenectomy • D 1, D 2, D 3 etc

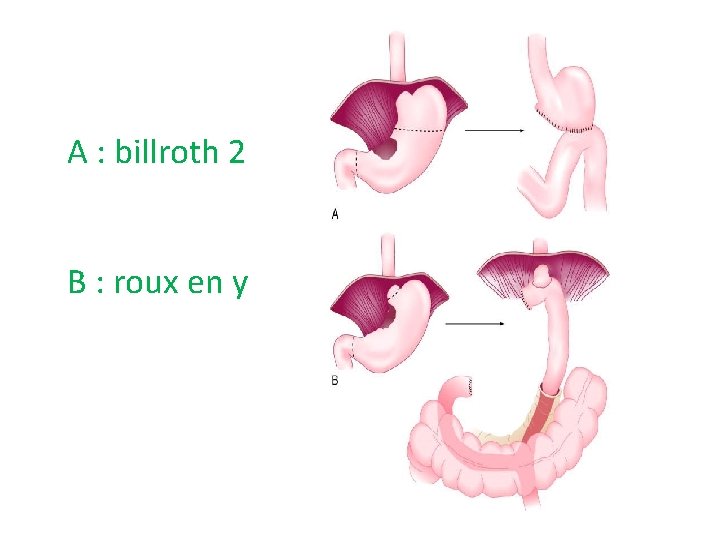
A : billroth 2 B : roux en y
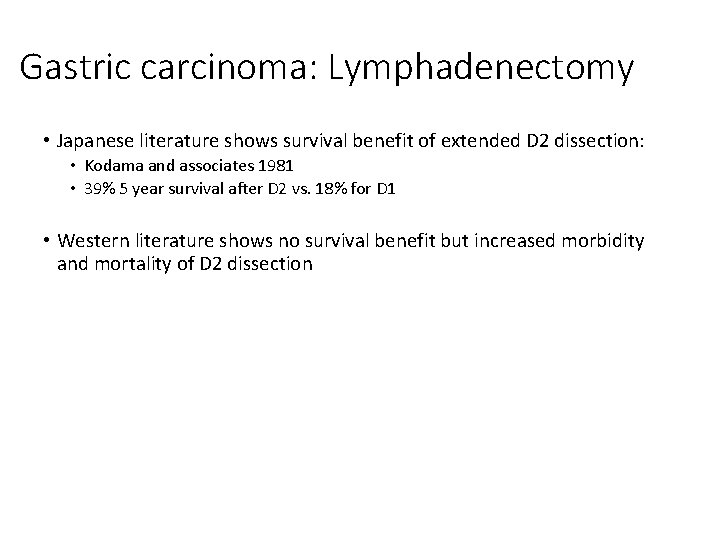
Gastric carcinoma: Lymphadenectomy • Japanese literature shows survival benefit of extended D 2 dissection: • Kodama and associates 1981 • 39% 5 year survival after D 2 vs. 18% for D 1 • Western literature shows no survival benefit but increased morbidity and mortality of D 2 dissection
Results of therapy – stomach cancer • Surgery with curative intent • 42% of patients • 5 year survival – 60% • Node positive - 35% • Node negative - 88% Sue Ling et al (1993) BMJ
Multimodal therapy • Adjuvant chemotherapy • Radiotherapy • Neo-adjuvant chemotherapy
Consequences of surgery • Weight loss • Food restriction • B 12, calcium, iron deficiency • Dumping • Early • Late hypoglycaemic • Diarrhoea • Gallstones • Stomal ulceration
Gastric lymphoma • The Stomach is the commonest extranodal primary site for non-Hodgkin's lymphoma • Secondary Lymphoma is commonly seen in stomach from another site • Accounts for less than 5% of gastric malignancies • Presentation is similar to gastric carcinoma • Anaemia and epigastric mass are common • Age of presentation is approx 60 years • Investigations • Endoscopy • EUS is the best modality
Gastric Lymphoma • Treatment • 70% of tumours are resectable • 5 -year survival is approximately 25% • Treatments range from chemotherapy alone, H pylori eradication or surgery and chemotherapy may be useful
MALT lymphoma • A type of primary gastric lymphoma • The stomach does not usually contain lymphoid tissue • MALT follicles found in the stomach are associated with H pylori infection • Patients can be completely cured by H pylori eradication or else use it in conjunction with chemotherapy
Gastrointestinal Stromal Tumor ‘GIST’ Previously leiomyoma & leomyosarcoma. <1 % Rarly cause bleeding or obstruction. originate in interstitial cells of Cajal (regulate peristalsis) 95% stain with Ab against c-KIT (CD 117) 70% stain for CD 34 The distinction bw benign & malignant is unclear. In general terms, the larger the tumor & greater mitotic activity, the more likely to metastases. The stomach is the most common site of GIST. Common presentation is bleeding Wide local incision is enough no need for lymphonodectomy Depend on the size and mitotic figure
GIST tumours • Presentation • Haemetemsis • Melaena • Epigastric mass • Investigation • EUS + biopsy • Endoscopy
GIST tumours • Treatment • • Surgery-local excision of tumor Lymph node clearance unnecessary as spread is not common Large tumors may need formal gastrectomy+/- adjuvant therapy Trials on a new drug Imatinib( Gleevec) have been shown to be effective
Duodenum • 4 regions: • Duodenal bulb (1 st part) • Descending duodenum (2 nd part) • Transverse duodenum (3 rd part) • Ascending duodenum (4 th part) • It ends at ligament of Treitz • Absorptive, goblet, granular, endocrine, intestinal and duodenal glands called Brunner’s glands which protect mucosa. • Blood supply
Duodenum Duodenal bicarbonate Secretion These are several mechanism that protect duodenum mucosa: 1) Brunner’s glands secrete mucus that protects mucosa. 2) duodenal cells secrete NAHCO 3, that neutralizes all H ions in duodenal bulb, secreted by stimulation produce by irritation. • 3) Additional HCO 3 comes from pancreas, in response to Secretin. • •
Adenocarcinoma of Duodenum MC site for ADC. 2/3 are located in 2 nd part of duodenum around peri-ampullar y region. presents late in its course. S/S: Nonespecific abdominal pain, weight loss, gastric outlet obstruction, melena, hematochezia (due to ulceration of lesion), jaundice • Dx is made by Upper endoscopy and Bx. • CT for local invasion or mets spread. • • •
ADC of Duodenum • Surgery: • excision when is possible resection of disease pancreaticoduodenectomy if tumor is in 1 st or 2 nd portion • if tumor is in 3 rd or 4 th portion small bowel resection c duodenojejunostomy • if tumor is unresectable or mets are presented then gastroenterostomy is indicated • Post surgery radiation can be helpful. • (+) nodes poor prognosis, • 5 y survival less than 15%
Duodenal Lymphoma • • • Very rare in duodenum MC in ileum. S/S: same as those of ADC of duodenum Nonespecific abdominal pain, weight loss, gastric outlet obstruction, melena, hematochezia (ulceration of lesion), fatigue. Complications: perforation, bleeding, and obstruction. Dx: Endoscopy CT for Ds extent. Follow same guidelines for any lymphoma. Adjuvant chemo post operatory Disseminated Ds only chemo + local radiation.

 Ruminant digestive system
Ruminant digestive system Degluttination
Degluttination Transverse mesocolon
Transverse mesocolon Lymphatic drainage of stomach diagram
Lymphatic drainage of stomach diagram Flap at bottom of esophagus
Flap at bottom of esophagus Transtubercular plane
Transtubercular plane Antrum of stomach
Antrum of stomach Gastric ulcer differential diagnosis
Gastric ulcer differential diagnosis Stomach anatomy
Stomach anatomy Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Khi nào hổ mẹ dạy hổ con săn mồi
Khi nào hổ mẹ dạy hổ con săn mồi điện thế nghỉ
điện thế nghỉ Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ Một số thể thơ truyền thống
Một số thể thơ truyền thống Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Số.nguyên tố
Số.nguyên tố Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Phối cảnh
Phối cảnh Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Hệ hô hấp
Hệ hô hấp Tư thế ngồi viết
Tư thế ngồi viết Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Cái miệng bé xinh thế chỉ nói điều hay thôi
Cái miệng bé xinh thế chỉ nói điều hay thôi Cách giải mật thư tọa độ
Cách giải mật thư tọa độ ưu thế lai là gì
ưu thế lai là gì Tư thế ngồi viết
Tư thế ngồi viết Gấu đi như thế nào
Gấu đi như thế nào Thẻ vin
Thẻ vin Thể thơ truyền thống
Thể thơ truyền thống Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Diễn thế sinh thái là
Diễn thế sinh thái là Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thế nào là giọng cùng tên?
Thế nào là giọng cùng tên? Phép trừ bù
Phép trừ bù Chúa yêu trần thế alleluia
Chúa yêu trần thế alleluia Khi nào hổ mẹ dạy hổ con săn mồi
Khi nào hổ mẹ dạy hổ con săn mồi Lời thề hippocrates
Lời thề hippocrates đại từ thay thế
đại từ thay thế Glasgow thang điểm
Glasgow thang điểm Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Công thức tính thế năng
Công thức tính thế năng Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Các loại đột biến cấu trúc nhiễm sắc thể
Các loại đột biến cấu trúc nhiễm sắc thể Bổ thể
Bổ thể Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Phản ứng thế ankan
Phản ứng thế ankan Môn thể thao bắt đầu bằng chữ f
Môn thể thao bắt đầu bằng chữ f Stomach function
Stomach function Digestive system helpers
Digestive system helpers What assimilates dissolved food
What assimilates dissolved food Gastric folds
Gastric folds Barium x ray stomach
Barium x ray stomach Stomach clock
Stomach clock Are lipids digested in the stomach
Are lipids digested in the stomach Sabrina domingues
Sabrina domingues Orifices of stomach
Orifices of stomach Pprotozoa
Pprotozoa Upper limb artery
Upper limb artery Stomach
Stomach Symptoms of worms in children pictures
Symptoms of worms in children pictures Ruminant stomach diagram
Ruminant stomach diagram Parts of a cows stomach
Parts of a cows stomach Digestion of food in stomach
Digestion of food in stomach Stomach region
Stomach region Stomach virus
Stomach virus Cardiac orifice of stomach
Cardiac orifice of stomach 9 parts of stomach
9 parts of stomach Gastric
Gastric Yakult stomach pain
Yakult stomach pain 4 chambers of the ruminant stomach
4 chambers of the ruminant stomach Stomachitis
Stomachitis Carcinoid tumor stomach
Carcinoid tumor stomach Stomodeum
Stomodeum Bacterial infection in stomach
Bacterial infection in stomach Stomach pain chart
Stomach pain chart Parts of stomach histology
Parts of stomach histology Epigastric region
Epigastric region Pearson
Pearson Layers of esophagus
Layers of esophagus Eric carle stomach ache
Eric carle stomach ache Pancreatic juice
Pancreatic juice Stomach
Stomach Chapter 55 care of patients with stomach disorders
Chapter 55 care of patients with stomach disorders Esophagus and stomach junction histology
Esophagus and stomach junction histology