Power Point Lecture Slides prepared by Meg Flemming

Power. Point® Lecture Slides prepared by Meg Flemming Austin Community College CHAPTER 13 The Cardiovascular System: Blood Vessels and Circulation © 2013 Pearson Education, Inc.
Chapter 13 Learning Outcomes • 13 -1 • Distinguish among the types of blood vessels based on their structure and function. • 13 -2 • Explain the mechanisms that regulate blood flow through blood vessels, and discuss the mechanisms that regulate movement of fluids between capillaries and interstitial spaces. • 13 -3 • Describe the control mechanisms that interact to regulate blood flow and pressure in tissues, and explain how the activities of the cardiac, vasomotor, and respiratory centers are coordinated to control blood flow through tissues. © 2013 Pearson Education, Inc.
Chapter 13 Learning Outcomes • 13 -4 • Explain the cardiovascular system's homeostatic response to exercising and hemorrhaging. • 13 -5 • Describe three general functional patterns in the pulmonary and systemic circuits. • 13 -6 • Identify the major arteries and veins of the pulmonary circuit. • 13 -7 • Identify the major arteries and veins of the systemic circuit. © 2013 Pearson Education, Inc.
Chapter 13 Learning Outcomes • 13 -8 • Identify the differences between fetal and adult circulation patterns, and describe the changes in the patterns of blood flow that occur at birth. • 13 -9 • Discuss the effects of aging on the cardiovascular system. • 13 -10 • Give examples of interactions between the cardiovascular system and the other organ systems. © 2013 Pearson Education, Inc.
Vascular Pathway of Blood Flow (13 -1) • Arteries leave the heart and branch into: • Arterioles feed parts of organs and branch into: • Capillaries, where chemical and gaseous exchange occurs, and which drain into: • Venules, the smallest vessels of the venous system, which drain into: • Veins, which return blood to the atria of the heart © 2013 Pearson Education, Inc.
Three Layers of Vessel Walls (13 -1) 1. Tunica intima (or tunica interna) • Has endothelial lining and elastic connective tissue 2. Tunica media • Has smooth muscle with collagen and elastic fibers • Controls diameter of vessel 3. Tunica externa (or tunica adventitia) • Sheath of connective tissue may anchor to other tissues © 2013 Pearson Education, Inc.
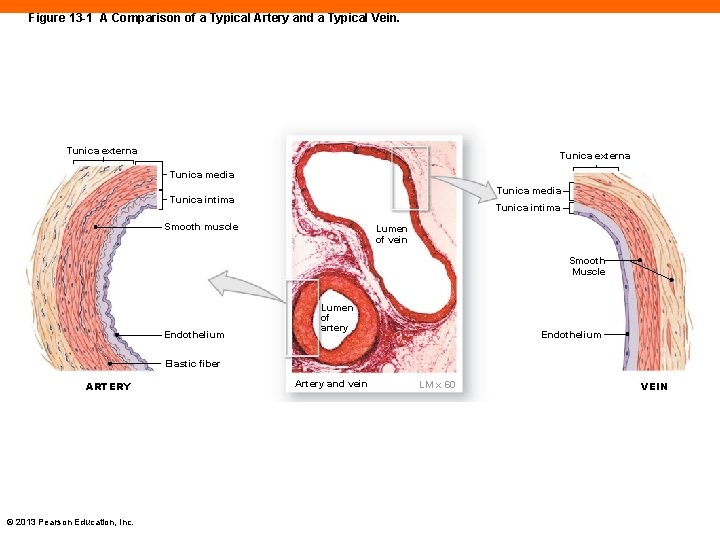
Figure 13 -1 A Comparison of a Typical Artery and a Typical Vein. Tunica externa Tunica media Tunica intima Smooth muscle Lumen of vein Smooth Muscle Endothelium Lumen of artery Endothelium Elastic fiber ARTERY © 2013 Pearson Education, Inc. Artery and vein LM x 60 VEIN
Elastic Arteries (13 -1) • First type of arteries leaving the heart • Examples are pulmonary trunk, aorta, and major branches • Have more elastic fibers than smooth muscle • Absorb pressure changes readily • Stretched during systole, relaxed during diastole • Prevent very high pressure during systole • Prevent very low pressure during diastole © 2013 Pearson Education, Inc.
Muscular Arteries and Arterioles (13 -1) • Muscular arteries • Examples are external carotid arteries • Tunica media contains high proportion of smooth muscle, little elastic fiber • Arterioles • Tunica media has only 1– 2 layers of smooth muscle • Ability to change diameter controls BP and flow © 2013 Pearson Education, Inc.
Capillaries (13 -1) • Tunica interna only • Endothelial cells with basement membrane • Ideal for diffusion between plasma and IF • Thin walls provide short diffusion distance • Small diameter slows flow to increase diffusion rate • Enormous number of capillaries provide huge surface area for increased diffusion © 2013 Pearson Education, Inc.
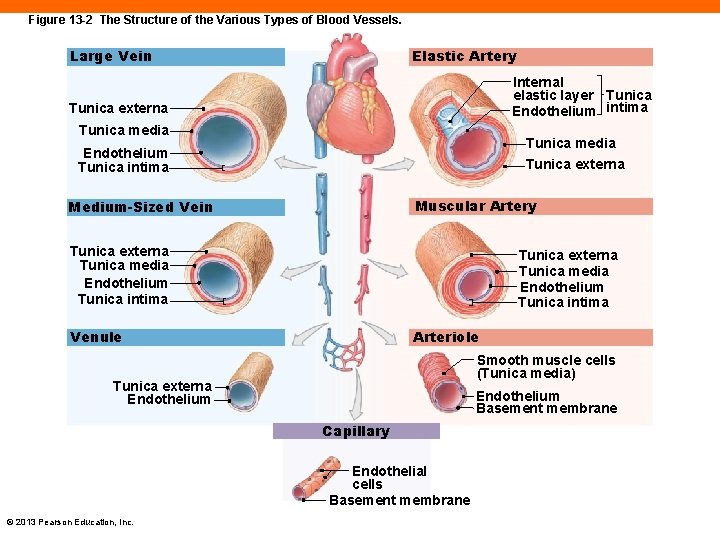
Figure 13 -2 The Structure of the Various Types of Blood Vessels. Large Vein Elastic Artery Internal elastic layer Tunica Endothelium intima Tunica externa Tunica media Endothelium Tunica intima Tunica externa Muscular Artery Medium-Sized Vein Tunica externa Tunica media Endothelium Tunica intima Arteriole Venule Smooth muscle cells (Tunica media) Tunica externa Endothelium Basement membrane Capillary Endothelial cells Basement membrane © 2013 Pearson Education, Inc.
Capillary Beds (13 -1) • An interconnected network of capillaries • Entrance to bed is regulated by precapillary sphincter, a band of smooth muscle • Relaxation of sphincter allows for increased flow • Constriction of sphincter decreases flow • This occurs cyclically, referred to as vasomotion • Control is local through autoregulation © 2013 Pearson Education, Inc.
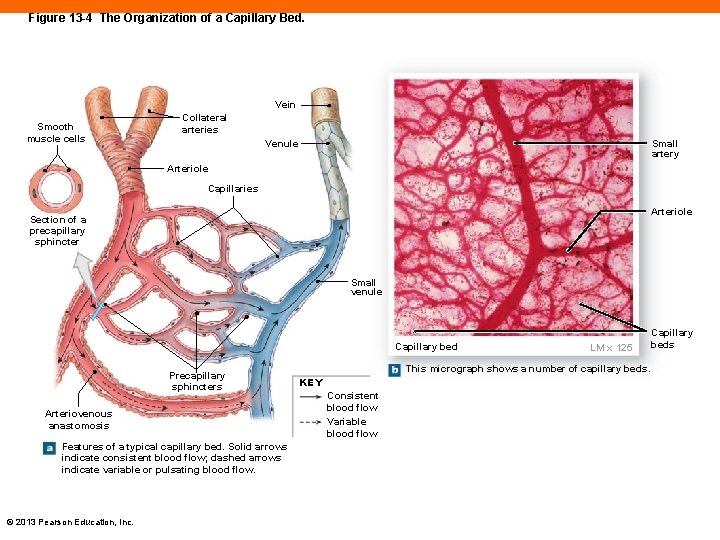
Figure 13 -4 The Organization of a Capillary Bed. Vein Smooth muscle cells Collateral arteries Venule Small artery Arteriole Capillaries Arteriole Section of a precapillary sphincter Small venule Capillary bed Precapillary sphincters Arteriovenous anastomosis Features of a typical capillary bed. Solid arrows indicate consistent blood flow; dashed arrows indicate variable or pulsating blood flow. © 2013 Pearson Education, Inc. LM x 125 This micrograph shows a number of capillary beds. KEY Consistent blood flow Variable blood flow Capillary beds
Alternate Routes for Blood Flow (13 -1) • Formed by anastomosis, a joining of blood vessels • Arteriovenous anastomosis bypasses capillary bed, connecting arteriole to venule • Arterial anastomosis occurs where arteries fuse before branching into arterioles • Ensures delivery of blood to key areas, brain, and heart © 2013 Pearson Education, Inc.
Veins (13 -1) • Collect blood from tissues and organs and return it to the heart • Venules are the smallest and some lack tunica media • Medium-sized veins • Tunica media has several smooth muscle layers • In limbs, contain valves • Prevent backflow of blood toward the distal ends • Increase venous return © 2013 Pearson Education, Inc.
Veins (13 -1) • Large veins • Thin tunica media and thick collagenous tunica externa • Thinner walls than arteries because of low pressure © 2013 Pearson Education, Inc.
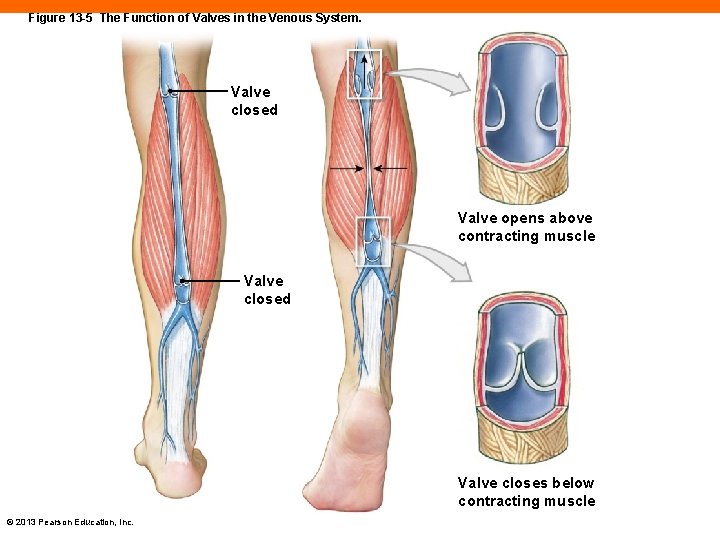
Figure 13 -5 The Function of Valves in the Venous System. Valve closed Valve opens above contracting muscle Valve closed Valve closes below contracting muscle © 2013 Pearson Education, Inc.
Checkpoint (13 -1) 1. List the five general classes of blood vessels. 2. A cross section of tissue shows several small, thin-walled vessels with very little smooth muscle tissue in the tunica media. Which type of vessels are these? 3. What effect would relaxation of precapillary sphincters have on blood flow through a tissue? 4. Why are valves found in veins, but not in arteries? © 2013 Pearson Education, Inc.
Maintaining Adequate Blood Flow (13 -2) • Flow maintains adequate perfusion of tissues • Normally, blood flow equals cardiac output (CO) • Increased CO leads to increased flow through capillaries • Decreased CO leads to reduced flow • Capillary flow influenced by pressure and resistance • Increased pressure increases flow • Increased resistance decreases flow © 2013 Pearson Education, Inc.
Pressure (13 -2) • Liquids exert hydrostatic pressure in all directions • A pressure gradient exists between high and low pressures at different points • Circulatory pressure, high in aorta vs. low in venae cavae • Arterial pressure is blood pressure • Capillary pressure • Venous pressure • Flow is proportional to pressure gradients © 2013 Pearson Education, Inc.
Resistance (13 -2) • Any force that opposes movement • Circulatory pressure must be high enough to overcome total peripheral resistance • Highest pressure gradient exists in arterioles due to high peripheral resistance • Vascular resistance • Viscosity • Turbulence © 2013 Pearson Education, Inc.
Vascular Resistance (13 -2) • Largest component of peripheral resistance • Caused mostly by friction between blood and vessel walls • Amount of friction due to length and diameter of vessel • Length doesn't normally change • The longer the vessel, the higher the resistance • Arteriolar diameter is primary source of vascular resistance • The smaller the diameter, the greater the resistance © 2013 Pearson Education, Inc.
Viscosity (13 -2) • Due to interactions between molecules and suspended materials in a liquid • Low-viscosity fluids flow at low pressures • High-viscosity fluids flow only under high pressures • Blood viscosity is normally stable • Changes in plasma proteins or hematocrit can alter viscosity and, therefore, flow © 2013 Pearson Education, Inc.
Turbulence (13 -2) • Eddies and swirls in fluid flow • In smooth-walled vessels turbulence is low • Slow flow near the walls, faster flow in center • Injured or diseased vessels or heart valves show increase in turbulence and decrease in flow • Turbulent blood flow across valves produces the sound of heart murmurs © 2013 Pearson Education, Inc.
Interplay of Pressure and Resistance (13 -2) • Blood pressure is maintained by hormonal and neural mechanisms • Adjusting diameter of arterioles to specific organs: • Regulates peripheral resistance • Regulates flow • Allows for matching flow and perfusion to tissue needs © 2013 Pearson Education, Inc.
Blood Pressure (13 -2) • Arterial pressures fluctuate • Systolic pressure (SP) is peak and occurs during ventricular contraction • Diastolic pressure (DP) is the minimum and occurs at the end of ventricular relaxation • Recorded as systolic over diastolic (e. g. , 120/80 mm Hg) • Pulse is alternating changes in pressures © 2013 Pearson Education, Inc.
Pulse Pressure (13 -2) • The difference between systolic and diastolic pressures • Pulse pressure = SP – DP • Diminishes over distance, eliminated at the capillary level • Arterial recoil or elastic rebound occurs during diastole • Adds additional push or squeeze on blood • Results in fluctuation of pressures © 2013 Pearson Education, Inc.
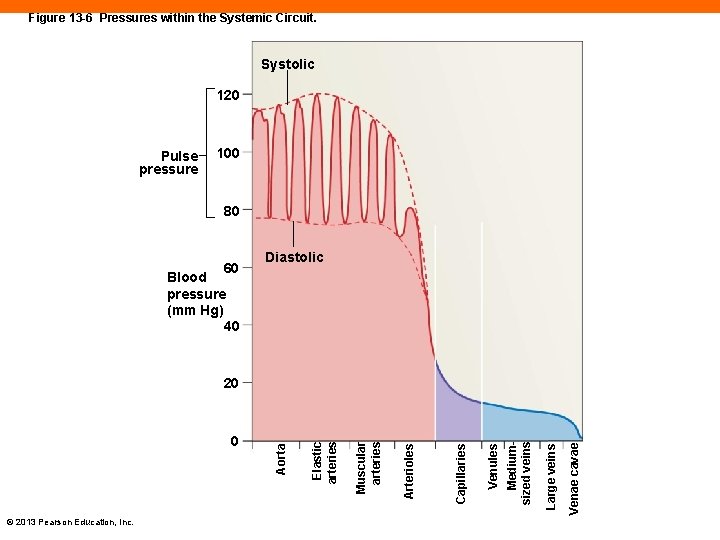
Figure 13 -6 Pressures within the Systemic Circuit. Systolic 120 Pulse pressure 100 80 60 Diastolic Blood pressure (mm Hg) 40 © 2013 Pearson Education, Inc. Venae cavae Large veins Mediumsized veins Venules Capillaries Arterioles Muscular arteries Elastic arteries 0 Aorta 20
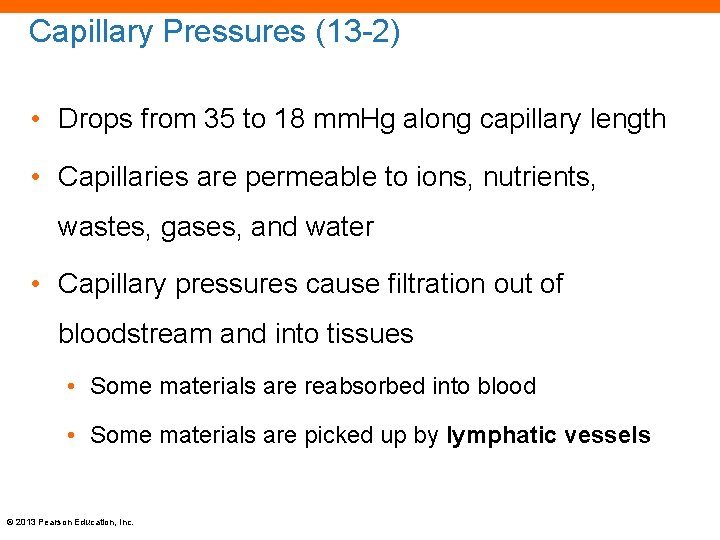
Capillary Pressures (13 -2) • Drops from 35 to 18 mm. Hg along capillary length • Capillaries are permeable to ions, nutrients, wastes, gases, and water • Capillary pressures cause filtration out of bloodstream and into tissues • Some materials are reabsorbed into blood • Some materials are picked up by lymphatic vessels © 2013 Pearson Education, Inc.
Four Functions of Capillary Exchange (13 -2) 1. Maintains constant communication between plasma and IF 2. Speeds distribution of nutrients, hormones, and gases 3. Assists movement of insoluble molecules 4. Flushes bacterial toxins and other chemicals to lymphatic tissues for immune response © 2013 Pearson Education, Inc.
Mechanisms of Capillary Exchange (13 -2) • Diffusion of solutes down concentration gradients • Filtration down fluid pressure gradients • Osmosis down osmotic gradient • Water is filtered out of capillary by fluid or hydrostatic pressures • Water is reabsorbed into capillary due to osmotic pressure © 2013 Pearson Education, Inc.
Capillary Exchange and Pressure Balances (13 -2) • Capillary hydrostatic pressure (CHP) is high at arteriolar end, low at venous end • Tends to push water out of plasma into tissues at arteriolar end, favoring filtration • Blood osmotic pressure (BOP) is higher than in interstitial fluid • As CHP drops over length of capillary, BOP remains the same, favoring reabsorption © 2013 Pearson Education, Inc.
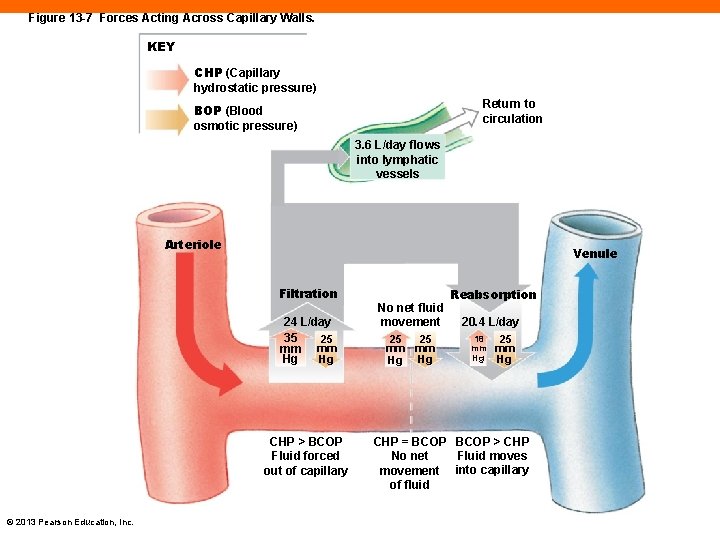
Figure 13 -7 Forces Acting Across Capillary Walls. KEY CHP (Capillary hydrostatic pressure) Return to circulation BOP (Blood osmotic pressure) 3. 6 L/day flows into lymphatic vessels Arteriole Venule Filtration 24 L/day 35 25 mm mm Hg Hg CHP > BCOP Fluid forced out of capillary © 2013 Pearson Education, Inc. No net fluid movement 25 25 mm mm Hg Hg Reabsorption 20. 4 L/day 18 mm Hg 25 mm Hg CHP = BCOP > CHP Fluid moves No net movement into capillary of fluid
Venous Pressure (13 -2) • Gradient is low compared to arterial side • Large veins provide low resistance ensuring increase in flow despite low pressure • When standing, blood flow must overcome gravity • Muscular compression pushes on outside of veins • Venous valves prevent backflow • Respiratory pump due to thoracic pressures © 2013 Pearson Education, Inc.
Checkpoint (13 -2) 5. Identify the factors that contribute to total peripheral resistance. 6. In a healthy individual, where is blood pressure greater: at the aorta or at the inferior vena cava? Explain. 7. While standing in the hot sun, Sally begins to feel light-headed and then faints. Explain what happened. © 2013 Pearson Education, Inc.
Homeostatic Regulation of Perfusion (13 -3) • Affected by: • Cardiac output, peripheral resistance, and blood pressure • Regulated to ensure blood flow changes occur at: • Appropriate time, in right location, and without negative effect on pressure and flow to vital organs • Accomplished through: • Autoregulation, neural and hormonal input © 2013 Pearson Education, Inc.
Autoregulation of Perfusion (13 -3) • Immediate and localized changes in: • Vasoconstrictors, factors that stimulate constriction • Vasodilators, factors that promote dilation • Tissue temperature, low O 2 or p. H, high CO 2 cause: • Capillary sphincter dilation causing: • Peripheral resistance decrease causing: • Increase in flow through capillary beds © 2013 Pearson Education, Inc.
Neural Control of Blood Pressure and Perfusion (13 -3) • Triggered by changes in arterial pressure or blood gas levels • Cardiovascular (CV) centers in medulla oblongata • Adjust cardiac output • Vasomotor center in medulla oblongata • Controls diameter of arterioles and peripheral resistance • Controls venoconstriction © 2013 Pearson Education, Inc.
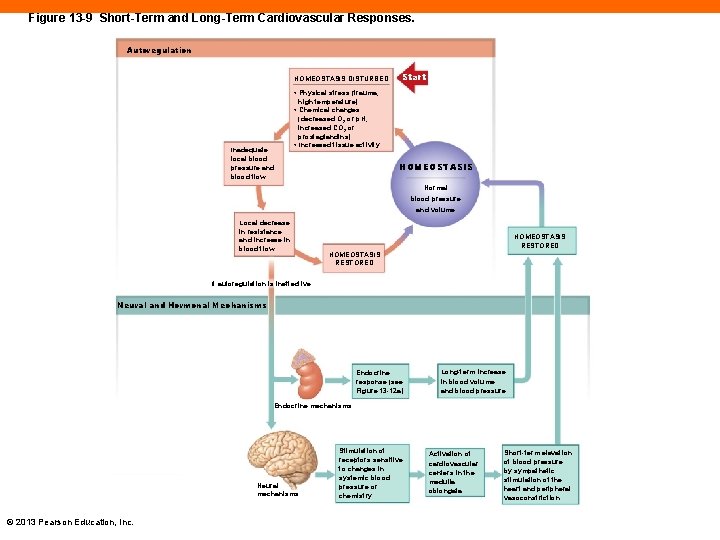
Figure 13 -9 Short-Term and Long-Term Cardiovascular Responses. Autoregulation HOMEOSTASIS DISTURBED Inadequate local blood pressure and blood flow Start • Physical stress (trauma, high temperature) • Chemical changes (decreased O 2 or p. H, increased CO 2 or prostaglandins) • Increased tissue activity. HOMEOSTASIS Normal blood pressure and volume Local decrease in resistance and increase in blood flow HOMEOSTASIS RESTORED If autoregulation is ineffective Neural and Hormonal Mechanisms Endocrine response (see Figure 13 -12 a) Long-term increase in blood volume and blood pressure Endocrine mechanisms Neural mechanisms © 2013 Pearson Education, Inc. Stimulation of receptors sensitive to changes in systemic blood pressure or chemistry Activation of cardiovascular centers in the medulla oblongata Short-term elevation of blood pressure by sympathetic stimulation of the heart and peripheral vasoconstriction
Baroreceptor Reflexes (13 -3) • Receptors monitor degree of stretch • Aortic sinuses • Located in pockets in walls of ascending aorta • Aortic reflex adjusts flow through systemic circuit • Carotid sinuses • Very sensitive to ensure adequate flow to, and perfusion of, brain © 2013 Pearson Education, Inc.

Figure 13 -10 The Baroreceptor Reflexes of the Carotid and Aortic Sinuses. Cardioinhibitory centers stimulated Responses to Increased Baroreceptor Stimulation Cardioacceleratory centers inhibited Vasomotor center inhibited Vasodilation occurs Baroreceptors stimulated HOMEOSTASIS RESTORED HOMEOSTASIS DISTURBED Blood pressure declines Rising blood pressure Start HOMEOSTASIS Start Normal range of blood pressure HOMEOSTASIS DISTURBED HOMEOSTASIS RESTORED Falling blood pressure Blood pressure rises Vasoconstriction occurs Baroreceptors inhibited Responses to Decreased Baroreceptor Stimulation Vasomotor center stimulated Cardioacceleratory centers stimulated Cardioinhibitory centers inhibited © 2013 Pearson Education, Inc. Decreased cardiac output Increased cardiac output
Chemoreceptor Reflexes (13 -3) • Receptors • Sensitive to changes in carbon dioxide, oxygen, and p. H in blood and CSF • Located in carotid and aortic bodies, medulla oblongata • Decrease in p. H or plasma O 2, increase in plasma CO 2 stimulate increase in heart rate and arteriolar constriction • Result is increase in BP © 2013 Pearson Education, Inc.
Hormonal Control of Cardiovascular Performance (13 -3) • Short-term • E and NE trigger rapid increase of cardiac output and vasoconstriction • Long-term • Antidiuretic hormone (ADH), angiotensin II, EPO • Raise BP when too low • Atrial natriuretic peptide (ANP) • Lowers BP when too high © 2013 Pearson Education, Inc.
Antidiuretic Hormone and Cardiovascular Regulation (13 -3) • Released from posterior pituitary in response to: • Decrease in blood volume • Increase in blood osmolarity • Presence of angiotensin II • Results in: • Vasoconstriction • Conserving water by kidneys, increasing blood volume © 2013 Pearson Education, Inc.
Angiotensin II and Cardiovascular Regulation (13 -3) • When BP decreases, kidney secretes renin • Cascade of reactions forms angiotensin II • Angiotensin II • Stimulates CO, arteriolar constriction • Immediately increases BP • Stimulates release of ADH and aldosterone • Stimulates thirst center © 2013 Pearson Education, Inc.
Erythropoietin and Cardiovascular Regulation (13 -3) • Released by kidney when: • BP drops • Plasma oxygen drops • Stimulates: • RBC production • Increases blood volume © 2013 Pearson Education, Inc.
Atrial Natriuretic Peptide and Cardiovascular Regulation (13 -3) • Released by atrial walls when BP increases • From stretch of atrial wall due to more venous return • Effects • Increases sodium (and therefore water) loss by kidneys • Reduces thirst • Blocks release of ADH, aldosterone, E, NE • Stimulates arteriolar dilation © 2013 Pearson Education, Inc.
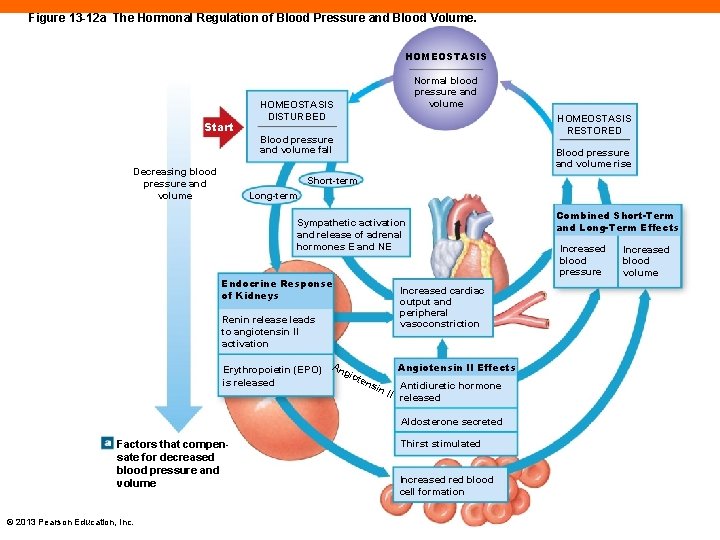
Figure 13 -12 a The Hormonal Regulation of Blood Pressure and Blood Volume. HOMEOSTASIS Start Decreasing blood pressure and volume Normal blood pressure and volume HOMEOSTASIS DISTURBED HOMEOSTASIS RESTORED Blood pressure and volume fall Blood pressure and volume rise Short-term Long-term Sympathetic activation and release of adrenal hormones E and NE Endocrine Response of Kidneys Increased cardiac output and peripheral vasoconstriction Renin release leads to angiotensin II activation Erythropoietin (EPO) is released An gio Angiotensin II Effects ten sin Antidiuretic hormone II released Aldosterone secreted Factors that compensate for decreased blood pressure and volume © 2013 Pearson Education, Inc. Thirst stimulated Increased red blood cell formation Combined Short-Term and Long-Term Effects Increased blood pressure Increased blood volume
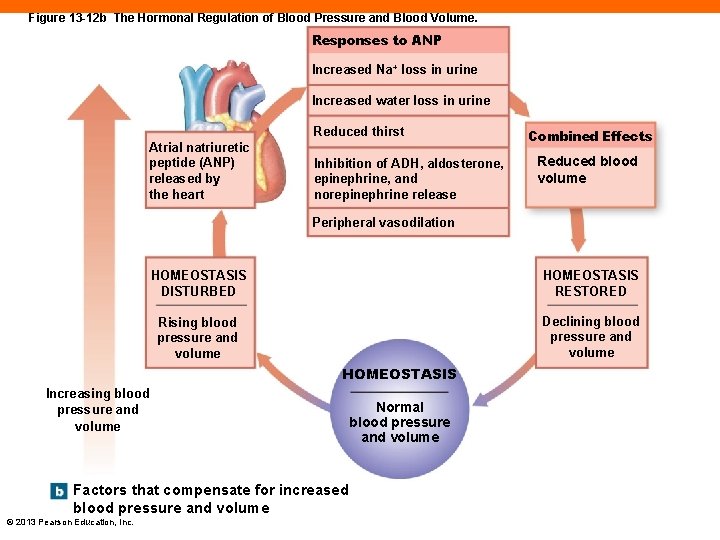
Figure 13 -12 b The Hormonal Regulation of Blood Pressure and Blood Volume. Responses to ANP Increased Na+ loss in urine Increased water loss in urine Reduced thirst Atrial natriuretic peptide (ANP) released by the heart Inhibition of ADH, aldosterone, epinephrine, and norepinephrine release Combined Effects Reduced blood volume Peripheral vasodilation HOMEOSTASIS DISTURBED HOMEOSTASIS RESTORED Rising blood pressure and volume Declining blood pressure and volume HOMEOSTASIS Increasing blood pressure and volume Factors that compensate for increased blood pressure and volume © 2013 Pearson Education, Inc. Normal blood pressure and volume
Checkpoint (13 -3) 8. Describe the actions of vasodilators and vasoconstrictors. 9. How would slightly compressing the common carotid artery affect your heart rate? 10. What effect would vasoconstriction of the renal artery have on systemic blood pressure and blood volume? © 2013 Pearson Education, Inc.
Four Cardiovascular Responses to the Stress of Exercise (13 -4) 1. Extensive vasodilation • Increased O consumption • Causes lower peripheral resistance • Resulting in increased flow 2. Increased venous return • Due to skeletal muscle and respiratory "pumps" © 2013 Pearson Education, Inc.
Four Cardiovascular Responses to the Stress of Exercise (13 -4) 3. Increased cardiac output • Frank-Starling principle due to increased venous return • Arterial pressures are maintained • Increased CO balances out decrease in peripheral resistance 4. Shunting of blood flow away from nonessential organs • Ensures adequate perfusion of heart and skeletal muscles © 2013 Pearson Education, Inc.
Short-Term Cardiovascular Response to Hemorrhage (13 -4) • Loss of blood causes decrease in BP • Carotid and aortic reflexes increase cardiac output and peripheral resistance • Venoconstriction accesses venous reserve • Sympathetic activation triggers arteriolar constriction • All mechanisms function to elevate BP © 2013 Pearson Education, Inc.
Long-Term Cardiovascular Response to Hemorrhage (13 -4) • May take several days to restore blood volume to normal • Fluids are accessed from interstitial space • ADH and aldosterone promote fluid retention • Thirst increases • EPO triggers RBC production • All mechanisms lead to increase in volume and BP © 2013 Pearson Education, Inc.
Checkpoint (13 -4) 11. Why does blood pressure increase during exercise? 12. Name the immediate and long-term problems related to the cardiovascular response to hemorrhaging. 13. Explain the role of aldosterone and ADH in long-term restoration of blood volume. © 2013 Pearson Education, Inc.
Three Functional Patterns of the Cardiovascular System (13 -5) 1. Distribution of arteries and veins nearly identical except near heart 2. Single vessel may undergo name changes as it crosses anatomical boundaries 3. Anastomoses of arteries and veins reduce threat of temporary blockage of vessel to organ © 2013 Pearson Education, Inc.
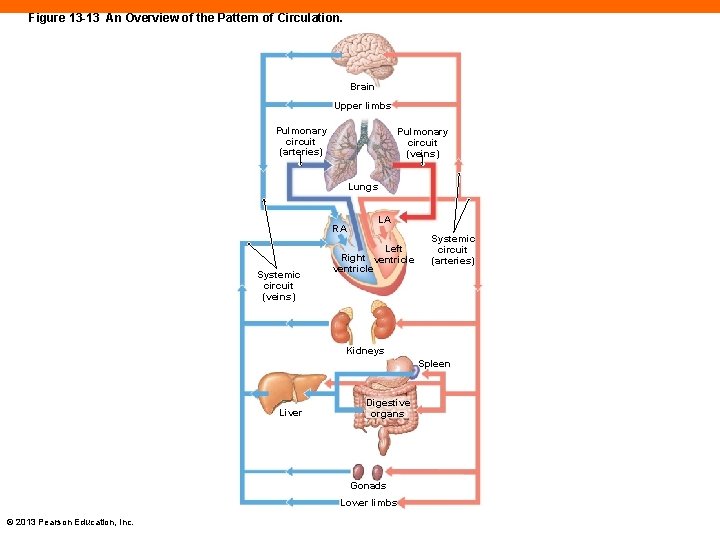
Figure 13 -13 An Overview of the Pattern of Circulation. Brain Upper limbs Pulmonary circuit (arteries) Pulmonary circuit (veins) Lungs RA Systemic circuit (veins) LA Left Right ventricle Systemic circuit (arteries) Kidneys Spleen Liver Digestive organs Gonads Lower limbs © 2013 Pearson Education, Inc.
Checkpoint (13 -5) 14. Identify the two circuits of the cardiovascular system. 15. Identify the three general functional patterns of the body's blood vessels. © 2013 Pearson Education, Inc.
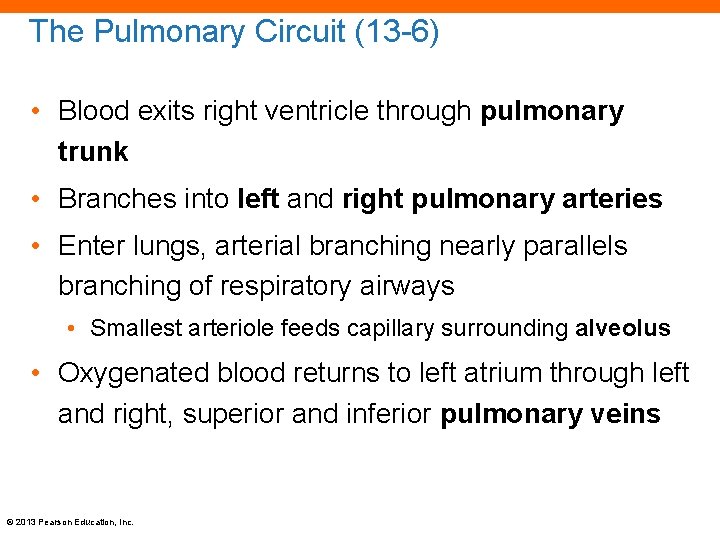
The Pulmonary Circuit (13 -6) • Blood exits right ventricle through pulmonary trunk • Branches into left and right pulmonary arteries • Enter lungs, arterial branching nearly parallels branching of respiratory airways • Smallest arteriole feeds capillary surrounding alveolus • Oxygenated blood returns to left atrium through left and right, superior and inferior pulmonary veins © 2013 Pearson Education, Inc.
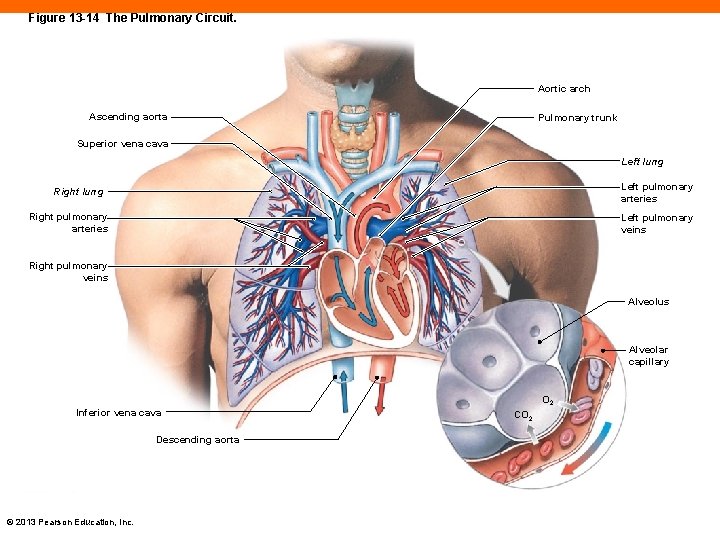
Figure 13 -14 The Pulmonary Circuit. Aortic arch Ascending aorta Pulmonary trunk Superior vena cava Left lung Left pulmonary arteries Right lung Right pulmonary arteries Left pulmonary veins Right pulmonary veins Alveolus Alveolar capillary Inferior vena cava Descending aorta © 2013 Pearson Education, Inc. O 2 CO 2
Checkpoint (13 -6) 16. Name the blood vessels that enter and exit the lungs, and indicate the relative oxygen content of the blood in each. 17. Trace the path of a drop of blood through the lungs, beginning at the right ventricle and ending at the left atrium. © 2013 Pearson Education, Inc.
The Systemic Circuit (13 -7) • Supplies oxygenated blood to all non-pulmonary tissues • Oxygenated blood leaves left ventricle through aorta • Returns deoxygenated blood to right atrium through superior and inferior venae cavae, and coronary sinus • Contains about 84 percent of total blood volume © 2013 Pearson Education, Inc.
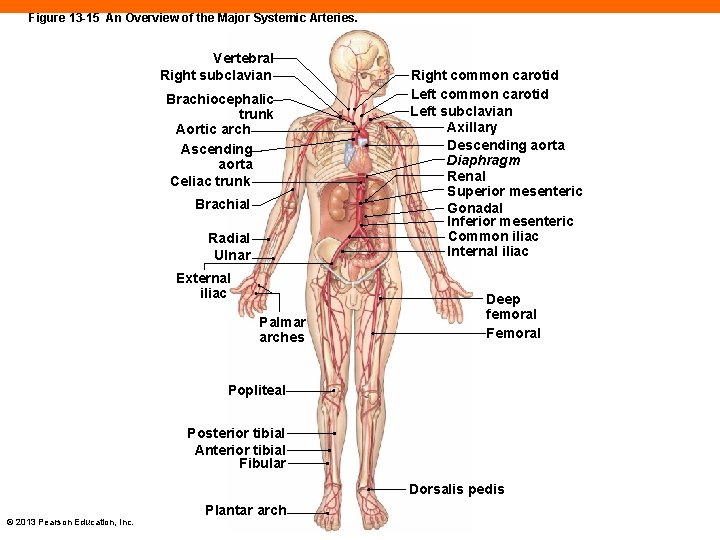
Figure 13 -15 An Overview of the Major Systemic Arteries. Vertebral Right subclavian Brachiocephalic trunk Aortic arch Ascending aorta Celiac trunk Brachial Radial Ulnar External iliac Palmar arches Right common carotid Left subclavian Axillary Descending aorta Diaphragm Renal Superior mesenteric Gonadal Inferior mesenteric Common iliac Internal iliac Deep femoral Femoral Popliteal Posterior tibial Anterior tibial Fibular Dorsalis pedis © 2013 Pearson Education, Inc. Plantar arch
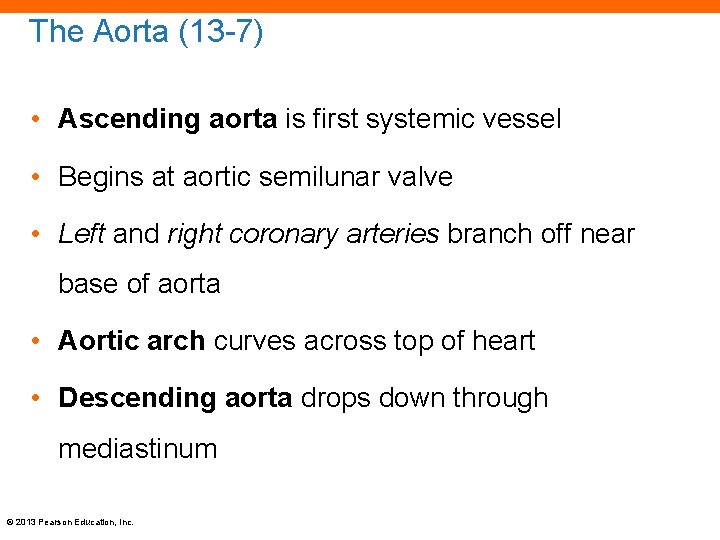
The Aorta (13 -7) • Ascending aorta is first systemic vessel • Begins at aortic semilunar valve • Left and right coronary arteries branch off near base of aorta • Aortic arch curves across top of heart • Descending aorta drops down through mediastinum © 2013 Pearson Education, Inc.
Three Elastic Arteries of the Aortic Arch (13 -7) 1. Brachiocephalic trunk • Branches to form right common carotid artery and right subclavian artery 2. Left common carotid 3. Left subclavian • This is an example of non-mirror-image arrangement • From here on, arteries are the same on both sides of the body • Designation of right and left not necessary © 2013 Pearson Education, Inc.
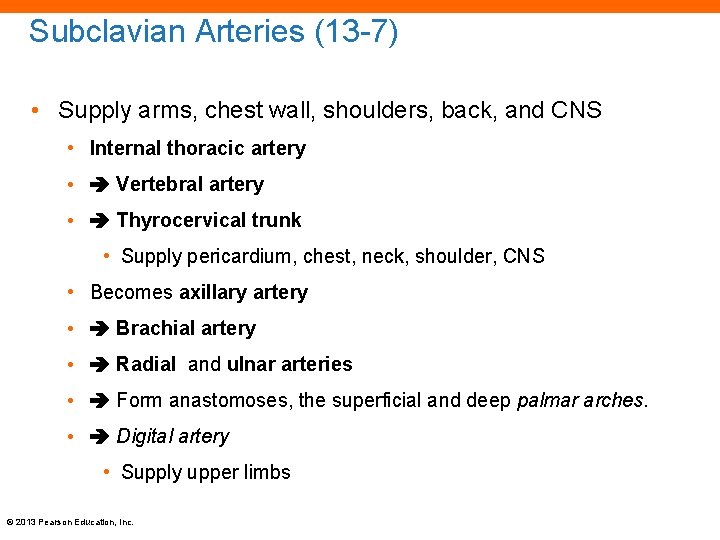
Subclavian Arteries (13 -7) • Supply arms, chest wall, shoulders, back, and CNS • Internal thoracic artery • Vertebral artery • Thyrocervical trunk • Supply pericardium, chest, neck, shoulder, CNS • Becomes axillary artery • Brachial artery • Radial and ulnar arteries • Form anastomoses, the superficial and deep palmar arches. • Digital artery • Supply upper limbs © 2013 Pearson Education, Inc.
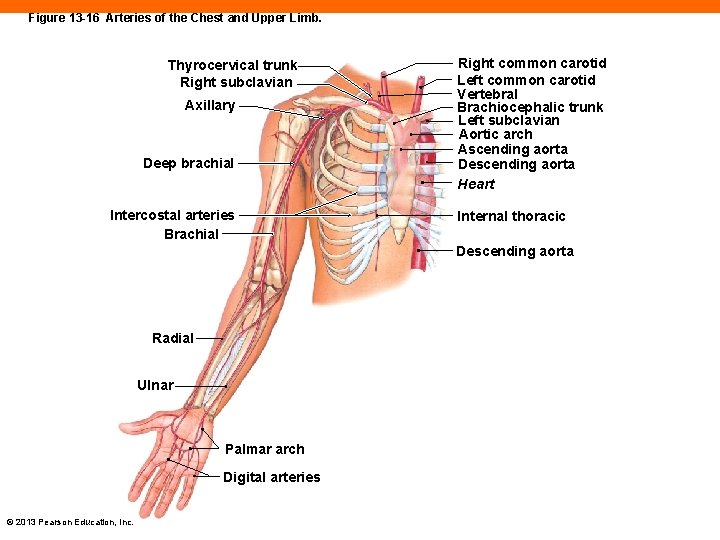
Figure 13 -16 Arteries of the Chest and Upper Limb. Thyrocervical trunk Right subclavian Axillary Deep brachial Intercostal arteries Brachial Right common carotid Left common carotid Vertebral Brachiocephalic trunk Left subclavian Aortic arch Ascending aorta Descending aorta Heart Internal thoracic Descending aorta Radial Ulnar Palmar arch Digital arteries © 2013 Pearson Education, Inc.
The Carotid Arteries (13 -7) • Common carotids ascend up into the neck and divide • External carotid artery • Supplies pharynx, esophagus, larynx, and face • Internal carotid artery • Enters skull, supplies brain and eyes © 2013 Pearson Education, Inc.
Blood Supply to the Brain (13 -7) • Two pathways • Vertebral arteries enter skull and fuse to form one basilar artery • Posterior cerebral artery • Posterior communicating artery • Cerebral arterial circle • Ring-shaped anastomosis encircling the infundibulum of the pituitary © 2013 Pearson Education, Inc.
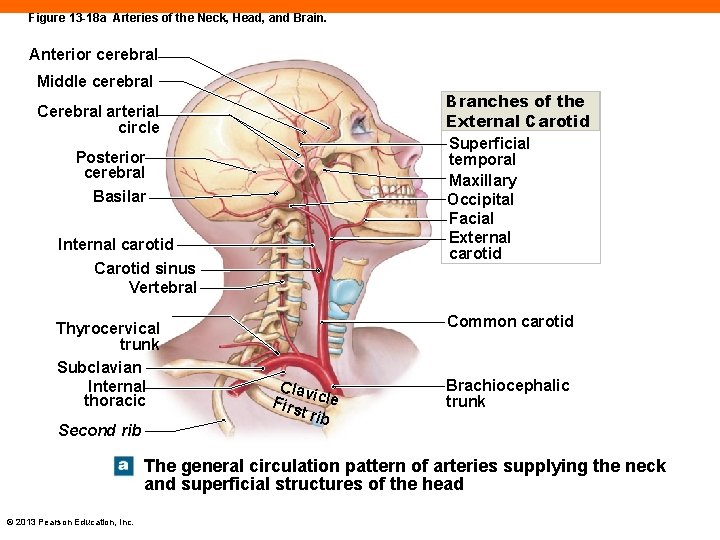
Figure 13 -18 a Arteries of the Neck, Head, and Brain. Anterior cerebral Middle cerebral Branches of the External Carotid Superficial temporal Maxillary Occipital Facial External carotid Cerebral arterial circle Posterior cerebral Basilar Internal carotid Carotid sinus Vertebral Thyrocervical trunk Subclavian Internal thoracic Second rib Common carotid Clav Firs icle t rib Brachiocephalic trunk The general circulation pattern of arteries supplying the neck and superficial structures of the head © 2013 Pearson Education, Inc.
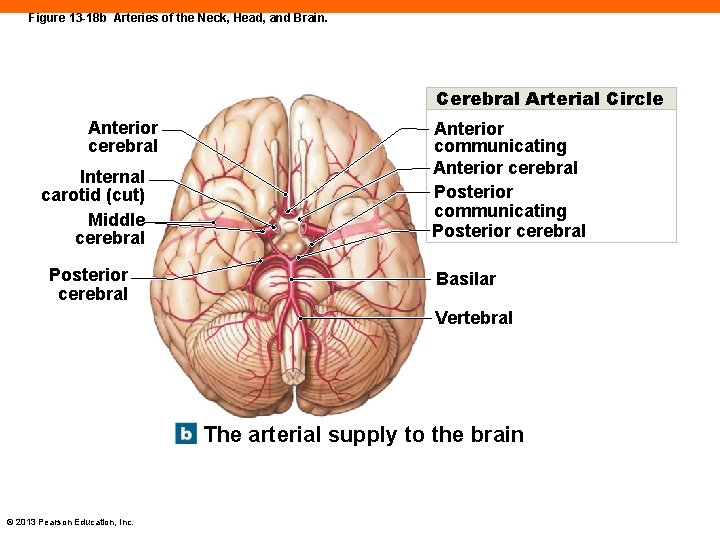
Figure 13 -18 b Arteries of the Neck, Head, and Brain. Cerebral Arterial Circle Anterior cerebral Internal carotid (cut) Middle cerebral Posterior cerebral Anterior communicating Anterior cerebral Posterior communicating Posterior cerebral Basilar Vertebral The arterial supply to the brain © 2013 Pearson Education, Inc.
Major Arteries of the Trunk (13 -7) • Descending aorta • Thoracic aorta within thoracic cavity • Abdominal aorta after passing through diaphragm • Phrenic artery • First branch off abdominal aorta • Supplies diaphragm © 2013 Pearson Education, Inc.
Unpaired Arteries of Digestive Organs (13 -7) • Supply blood to all digestive organs • Celiac trunk • Left gastric artery • Splenic artery • Common hepatic artery • Superior mesenteric artery • Inferior mesenteric artery © 2013 Pearson Education, Inc.
Paired Major Arteries of the Trunk (13 -7) • Gonadal arteries • Testicular in male, ovarian in female • Adrenal arteries • Supply adrenal glands • Renal arteries • Supply kidneys • Lumbar arteries • Supply spinal cord and abdominal wall © 2013 Pearson Education, Inc.
Iliac Arteries (13 -7) • Abdominal aorta branches to the: • Common iliac artery • Branches to: • Internal iliac artery • Supplies pelvis • External iliac artery • Supplies lower limbs © 2013 Pearson Education, Inc.
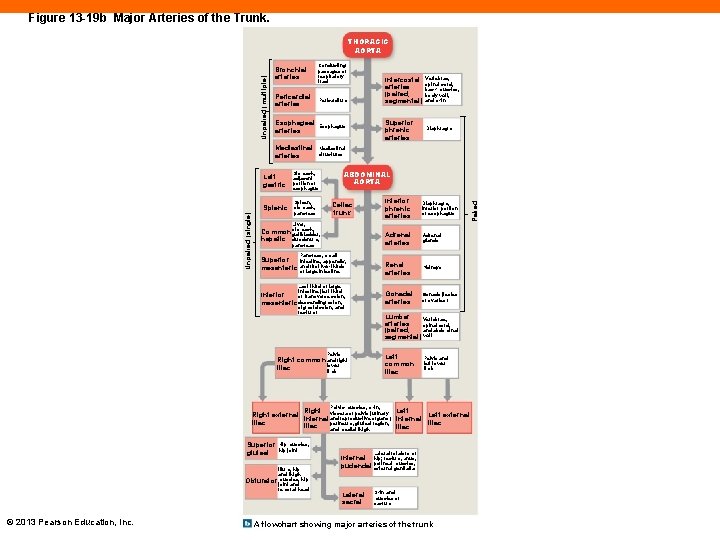
Figure 13 -19 b Major Arteries of the Trunk. Bronchial arteries Conducting passages of respiratory tract Pericardial arteries Pericardium Esophageal arteries Esophagus Mediastinal arteries Mediastinal structures Left gastric Stomach, adjacent portion of esophagus Splenic Spleen, stomach, pancreas Intercostal arteries (paired, segmental) Vertebrae, spinal cord, back muscles, body wall, and skin Superior phrenic arteries Diaphragm ABDOMINAL AORTA Celiac trunk Inferior phrenic arteries Diaphragm, inferior portion of esophagus Adrenal arteries Adrenal glands Renal arteries Kidneys Gonadal arteries Gonads (testes or ovaries) Liver, Common stomach, gallbladder, hepatic duodenum, pancreas Superior mesenteric Pancreas, small intestine, appendix, and first two-thirds of large intestine Last third of large intestine (left third Inferior of transverse colon, mesenteric descending colon, sigmoid colon, and rectum) Lumbar Vertebrae, arteries spinal cord, and abdominal (paired, segmental) wall Pelvis Left common iliac Right common and right lower iliac limb Pelvis and left lower limb Pelvic muscles, skin, Right viscera of pelvis (urinary Left Right external Left external internal and reproductive organs), internal iliac perineum, gluteal region, iliac and medial thigh Superior gluteal Hip muscles, hip joint Ilium, hip and thigh Lateral rotators of Internal hip; rectum, anus, muscles, pudendal perineal external genitalia hip Obturator muscles, joint and femoral head © 2013 Pearson Education, Inc. Lateral sacral Skin and muscles of sacrum A flowchart showing major arteries of the trunk Paired Unpaired (single) Unpaired (multiple) THORACIC AORTA
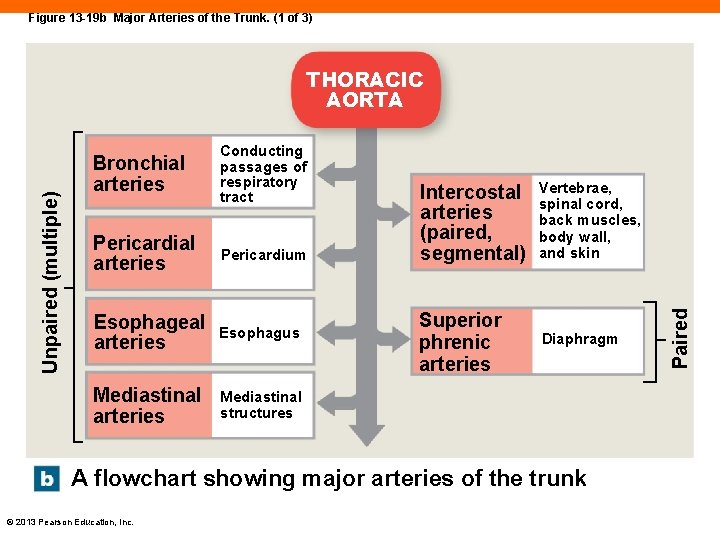
Figure 13 -19 b Major Arteries of the Trunk. (1 of 3) Bronchial arteries Conducting passages of respiratory tract Pericardial arteries Pericardium Esophageal arteries Esophagus Mediastinal arteries Mediastinal structures Intercostal arteries (paired, segmental) Vertebrae, spinal cord, back muscles, body wall, and skin Superior phrenic arteries Diaphragm A flowchart showing major arteries of the trunk © 2013 Pearson Education, Inc. Paired Unpaired (multiple) THORACIC AORTA
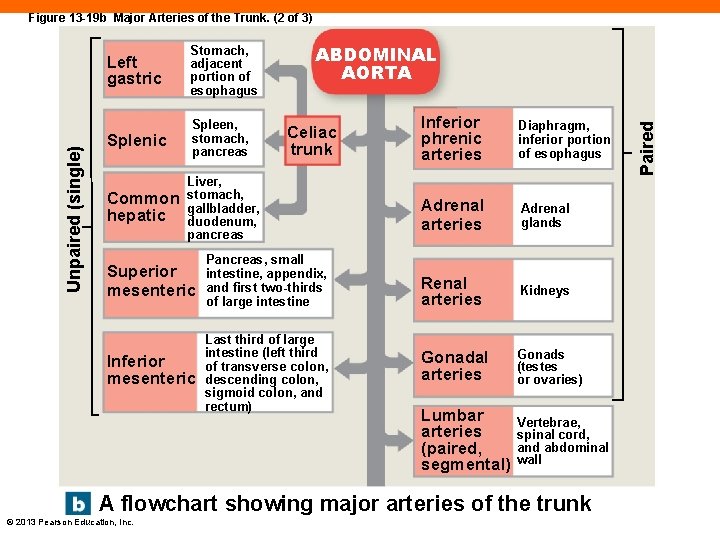
Left gastric Stomach, adjacent portion of esophagus Splenic Spleen, stomach, pancreas Common hepatic ABDOMINAL AORTA Celiac trunk Liver, stomach, gallbladder, duodenum, pancreas Superior mesenteric Pancreas, small intestine, appendix, and first two-thirds of large intestine Inferior mesenteric Last third of large intestine (left third of transverse colon, descending colon, sigmoid colon, and rectum) Inferior phrenic arteries Diaphragm, inferior portion of esophagus Adrenal arteries Adrenal glands Renal arteries Kidneys Gonadal arteries Gonads (testes or ovaries) Lumbar arteries (paired, segmental) Vertebrae, spinal cord, and abdominal wall A flowchart showing major arteries of the trunk © 2013 Pearson Education, Inc. Paired Unpaired (single) Figure 13 -19 b Major Arteries of the Trunk. (2 of 3)
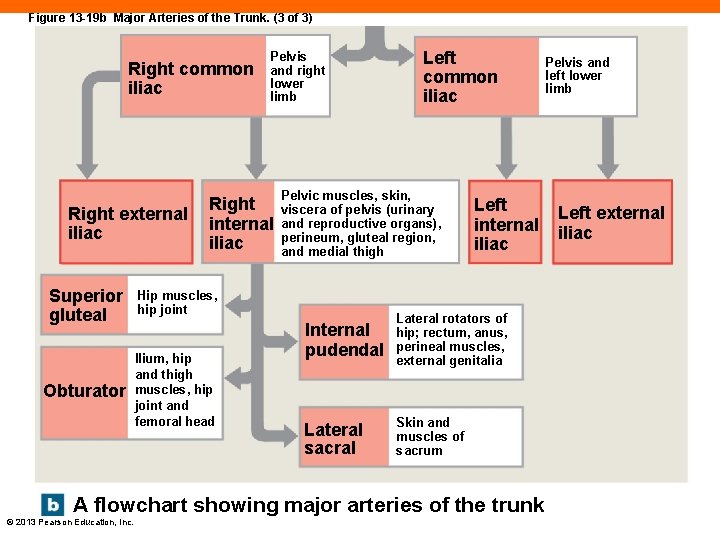
Figure 13 -19 b Major Arteries of the Trunk. (3 of 3) Right common iliac Right external iliac Pelvis and right lower limb Right internal iliac Superior gluteal Hip muscles, hip joint Obturator Ilium, hip and thigh muscles, hip joint and femoral head Left common iliac Pelvic muscles, skin, viscera of pelvis (urinary and reproductive organs), perineum, gluteal region, and medial thigh Left internal iliac Internal pudendal Lateral rotators of hip; rectum, anus, perineal muscles, external genitalia Lateral sacral Skin and muscles of sacrum A flowchart showing major arteries of the trunk © 2013 Pearson Education, Inc. Pelvis and left lower limb Left external iliac
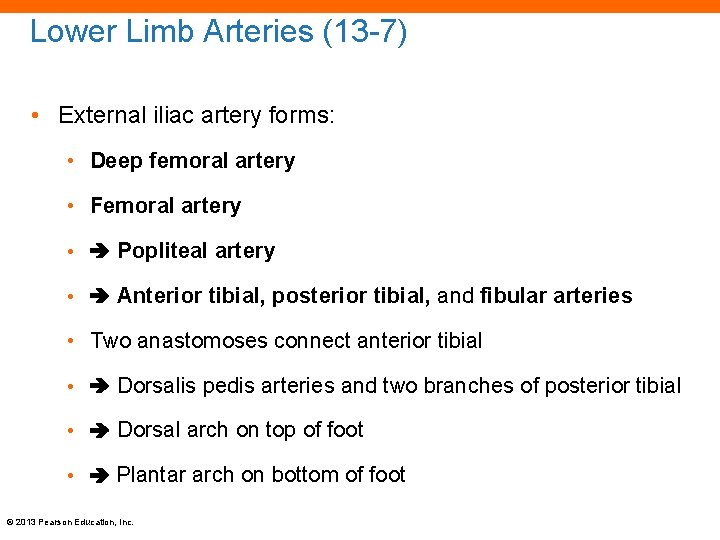
Lower Limb Arteries (13 -7) • External iliac artery forms: • Deep femoral artery • Femoral artery • Popliteal artery • Anterior tibial, posterior tibial, and fibular arteries • Two anastomoses connect anterior tibial • Dorsalis pedis arteries and two branches of posterior tibial • Dorsal arch on top of foot • Plantar arch on bottom of foot © 2013 Pearson Education, Inc.
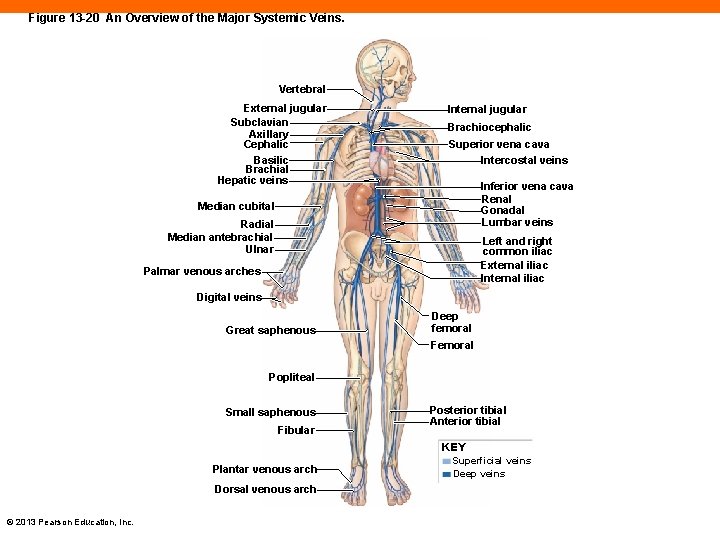
Figure 13 -20 An Overview of the Major Systemic Veins. Vertebral External jugular Subclavian Axillary Cephalic Basilic Brachial Hepatic veins Internal jugular Brachiocephalic Superior vena cava Intercostal veins Inferior vena cava Renal Gonadal Lumbar veins Median cubital Radial Median antebrachial Ulnar Left and right common iliac External iliac Internal iliac Palmar venous arches Digital veins Great saphenous Deep femoral Femoral Popliteal Small saphenous Fibular Posterior tibial Anterior tibial KEY Plantar venous arch Dorsal venous arch © 2013 Pearson Education, Inc. Superficial veins Deep veins
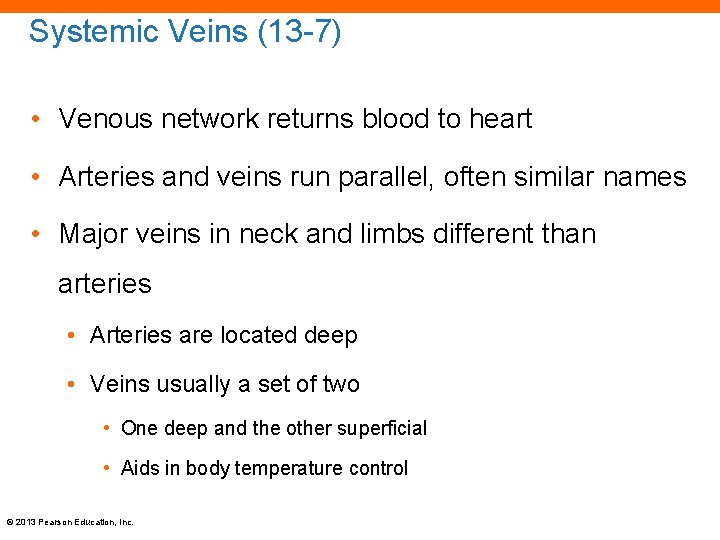
Systemic Veins (13 -7) • Venous network returns blood to heart • Arteries and veins run parallel, often similar names • Major veins in neck and limbs different than arteries • Arteries are located deep • Veins usually a set of two • One deep and the other superficial • Aids in body temperature control © 2013 Pearson Education, Inc.
The Superior Vena Cava (13 -7) • SVC • Receives blood from: • Head and neck • Upper limbs, shoulders, and chest © 2013 Pearson Education, Inc.
Venous Return from Head and Neck (13 -7) • Small veins in brain drain into dural sinuses • Largest is superior sagittal sinus • Internal jugular veins • External jugular veins • Collect blood from superficial head and neck • Vertebral veins • Collect blood from cervical spinal cord and posterior skull © 2013 Pearson Education, Inc.
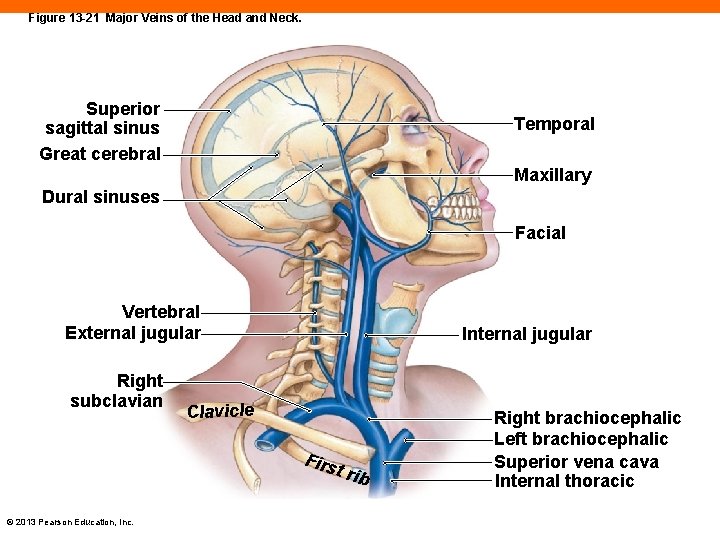
Figure 13 -21 Major Veins of the Head and Neck. Superior sagittal sinus Great cerebral Temporal Maxillary Dural sinuses Facial Vertebral External jugular Right subclavian Internal jugular Clavicle Firs t rib © 2013 Pearson Education, Inc. Right brachiocephalic Left brachiocephalic Superior vena cava Internal thoracic
Venous Return from the Upper Limbs and Chest (13 -7) • Digital vein drains into venous network in palms • Cephalic vein • Basilic vein • Median cubital • Connects cephalic and basilic veins • Site of venous blood sample tap © 2013 Pearson Education, Inc.
Venous Return from the Upper Limbs and Chest (13 -7) • Deeper forearm veins are radial veins and ulnar veins • Brachial vein joins basilic vein to form: • Axillary vein • Subclavian vein • Meet and merge with internal and external jugular veins • Creates large brachiocephalic vein SVC • Azygos vein drains chest wall SVC © 2013 Pearson Education, Inc.
Inferior Vena Cava (13 -7) • IVC • Collects blood from organs below diaphragm © 2013 Pearson Education, Inc.
Venous Return from the Lower Limbs (13 -7) • Plantar veins on the sole of the foot • Plantar venous arch drains into: • Anterior tibial vein • Posterior tibial vein • Fibular vein • Dorsal venous arch drains into: • Great saphenous vein and small saphenous vein © 2013 Pearson Education, Inc.
Venous Return from the Lower Limbs (13 -7) • Behind knee small saphenous, tibial, and fibular veins connect • Popliteal vein • Femoral vein • Great saphenous and deep femoral vein join femoral vein • External iliac vein • Joins internal iliac vein to become common iliac vein • IVC © 2013 Pearson Education, Inc.
Veins of the Abdominopelvic Organs (13 -7) • As IVC ascends toward heart it collects blood from: • Lumbar vein • Gonadal vein • Renal and adrenal veins • Phrenic vein • Hepatic vein © 2013 Pearson Education, Inc.
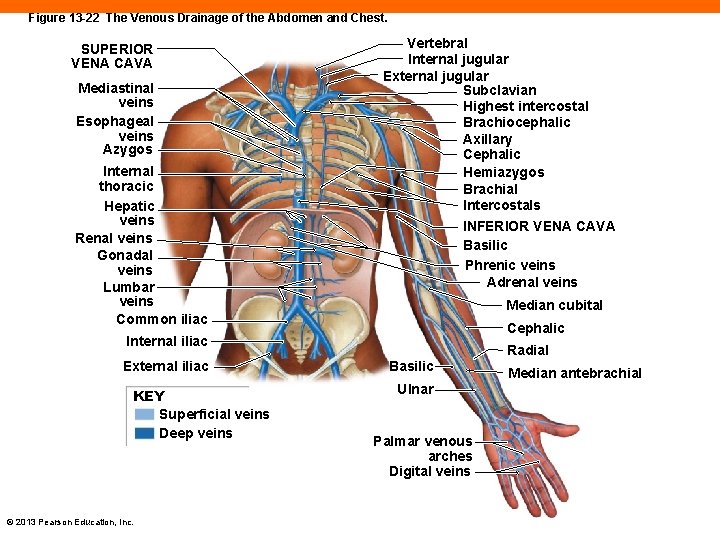
Figure 13 -22 The Venous Drainage of the Abdomen and Chest. SUPERIOR VENA CAVA Mediastinal veins Esophageal veins Azygos Internal thoracic Hepatic veins Renal veins Gonadal veins Lumbar veins Common iliac Vertebral Internal jugular External jugular Subclavian Highest intercostal Brachiocephalic Axillary Cephalic Hemiazygos Brachial Intercostals INFERIOR VENA CAVA Basilic Phrenic veins Adrenal veins Median cubital Cephalic Internal iliac External iliac KEY Superficial veins Deep veins © 2013 Pearson Education, Inc. Radial Basilic Ulnar Palmar venous arches Digital veins Median antebrachial
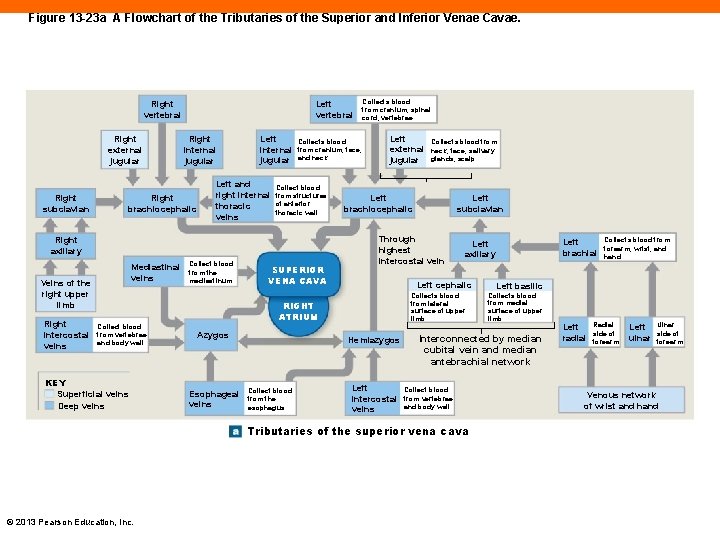
Figure 13 -23 a A Flowchart of the Tributaries of the Superior and Inferior Venae Cavae. Left vertebral Right external jugular Right subclavian Right internal jugular Right brachiocephalic Left internal jugular Left and right internal thoracic veins Collects blood from cranium, face, and neck Collect blood from structures of anterior thoracic wall Right axillary Mediastinal veins Veins of the right upper limb Right intercostal veins Collect blood from vertebrae and body wall KEY Superficial veins Deep veins Collect blood from the mediastinum SUPERIOR VENA CAVA Collects blood from cranium, spinal cord, vertebrae Left external jugular Left brachiocephalic Esophageal veins Left cephalic Left intercostal veins Collect blood from vertebrae and body wall Collects blood from forearm, wrist, and hand Left basilic Collects blood from medial surface of upper limb Interconnected by median cubital vein and median antebrachial network Tributaries of the superior vena cava © 2013 Pearson Education, Inc. Left brachial Left axillary Collects blood from lateral surface of upper limb Hemiazygos Collect blood from the esophagus Left subclavian Through highest intercostal vein RIGHT ATRIUM Azygos Collects blood from neck, face, salivary glands, scalp Left radial Radial side of forearm Left ulnar Ulnar side of forearm Venous network of wrist and hand
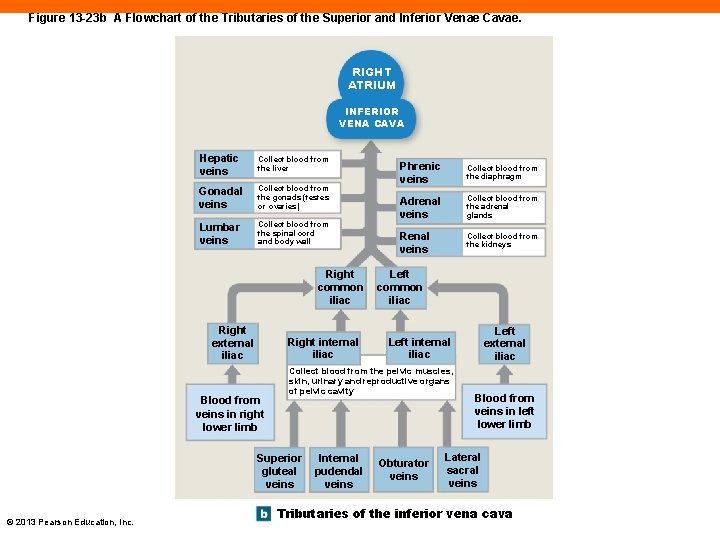
Figure 13 -23 b A Flowchart of the Tributaries of the Superior and Inferior Venae Cavae. RIGHT ATRIUM INFERIOR VENA CAVA Hepatic veins Collect blood from the liver Gonadal veins Collect blood from the gonads (testes or ovaries) Lumbar veins Collect blood from the spinal cord and body wall Right common iliac Right external iliac Right internal iliac Blood from veins in right lower limb Collect blood from the diaphragm Adrenal veins Collect blood from the adrenal glands Renal veins Collect blood from the kidneys Left common iliac Internal pudendal veins Left external iliac Left internal iliac Collect blood from the pelvic muscles, skin, urinary and reproductive organs of pelvic cavity Superior gluteal veins © 2013 Pearson Education, Inc. Phrenic veins Obturator veins Blood from veins in left lower limb Lateral sacral veins Tributaries of the inferior vena cava
Hepatic Portal System (13 -7) • Portal system is two capillary beds in series connected by portal vessel • Blood going through capillaries of digestive organs absorbs nutrients, some wastes, some toxins • Blood is processed by liver before entering general circulation © 2013 Pearson Education, Inc.
Hepatic Portal System (13 -7) • Capillaries from: • Lower large intestine inferior mesenteric vein • Spleen, stomach, pancreas splenic vein • Stomach, small and large intestines superior mesenteric vein • All three hepatic portal vein • Blood from gastric vein and cystic vein added • Blood enters liver capillaries hepatic vein IVC © 2013 Pearson Education, Inc.
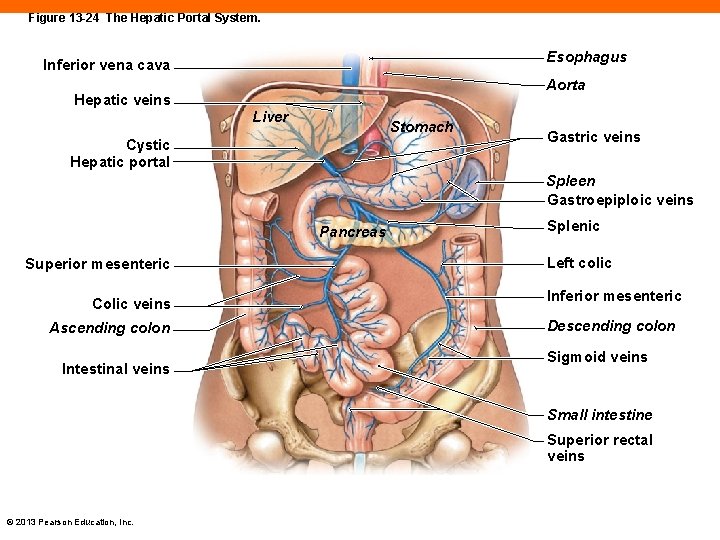
Figure 13 -24 The Hepatic Portal System. Esophagus Inferior vena cava Aorta Hepatic veins Liver Stomach Cystic Hepatic portal Gastric veins Spleen Gastroepiploic veins Pancreas Superior mesenteric Colic veins Ascending colon Intestinal veins Splenic Left colic Inferior mesenteric Descending colon Sigmoid veins Small intestine Superior rectal veins © 2013 Pearson Education, Inc.
Checkpoint (13 -7) 18. A blockage of which branch of the aortic arch would interfere with blood flow to the left arm? 19. Why would compression of the common carotid arteries cause a person to lose consciousness? 20. Grace is in an automobile accident, and her celiac trunk is ruptured. Which organs will be affected most directly by this injury? 21. Describe the general distribution of major arteries and veins in the neck and limbs. What functional advantage does this distribution provide? © 2013 Pearson Education, Inc.
Fetal Circulation (13 -8) • Biggest difference is sources of respiratory and nutritional support • All nutrients and blood gases supplied from mother through diffusion across placenta • Placenta is unique part of uterine wall • Maternal and fetal circulatory systems in close contact © 2013 Pearson Education, Inc.
Placental Blood Supply (13 -8) • Low O 2 fetal blood flows through umbilical arteries • At placenta: • CO 2 and wastes cross to mother • O 2 diffuses into fetal blood • Returns to fetal circulation through umbilical vein • Some blood goes to liver • Rest goes to IVC through ductus venosus © 2013 Pearson Education, Inc.
Fetal Circulation in the Heart and Great Vessels (13 -8) • Foramen ovale • An interatrial opening • Flap that acts as one-way valve from right to left atrium • Allows blood to bypass pulmonary circuit • Ductus arteriosus • Short vessel that takes most of blood from right ventricle directly to aortic arch of systemic circuit © 2013 Pearson Education, Inc.
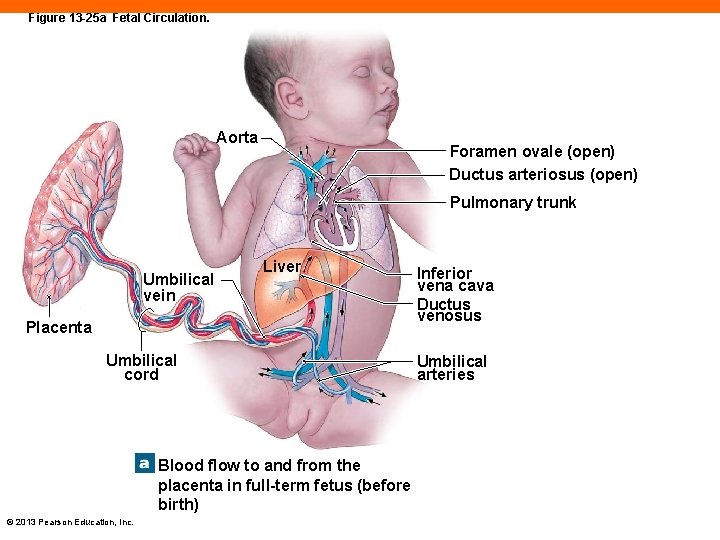
Figure 13 -25 a Fetal Circulation. Aorta Foramen ovale (open) Ductus arteriosus (open) Pulmonary trunk Umbilical vein Liver Placenta Umbilical cord Blood flow to and from the placenta in full-term fetus (before birth) © 2013 Pearson Education, Inc. Inferior vena cava Ductus venosus Umbilical arteries
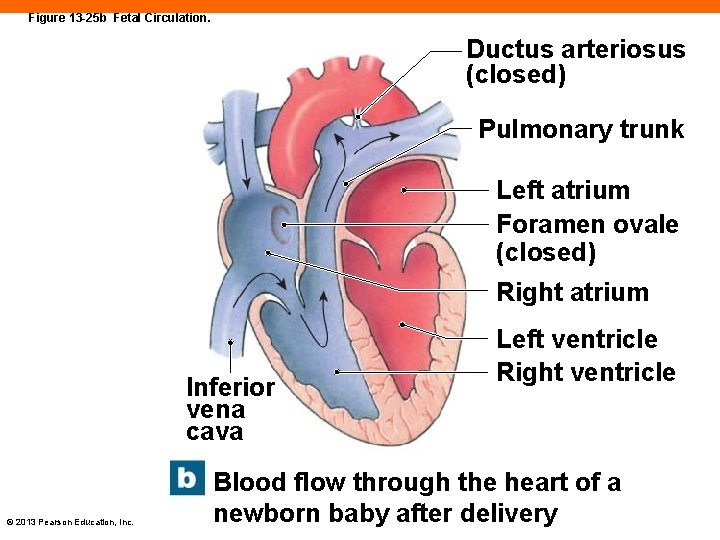
Figure 13 -25 b Fetal Circulation. Ductus arteriosus (closed) Pulmonary trunk Left atrium Foramen ovale (closed) Right atrium Inferior vena cava © 2013 Pearson Education, Inc. Left ventricle Right ventricle Blood flow through the heart of a newborn baby after delivery
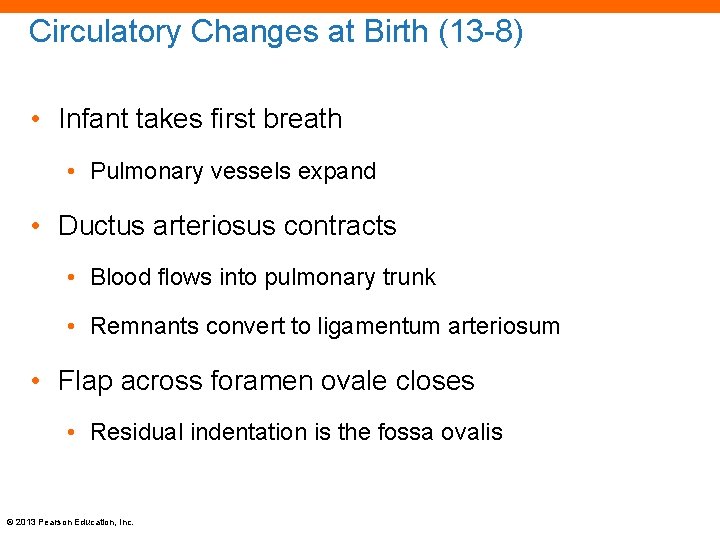
Circulatory Changes at Birth (13 -8) • Infant takes first breath • Pulmonary vessels expand • Ductus arteriosus contracts • Blood flows into pulmonary trunk • Remnants convert to ligamentum arteriosum • Flap across foramen ovale closes • Residual indentation is the fossa ovalis © 2013 Pearson Education, Inc.
Checkpoint (13 -8) 22. Name the umbilical vessels that constitute the placental blood supply. 23. A blood sample taken from the umbilical cord contains high levels of oxygen and nutrients, and low levels of carbon dioxide and waste products. Is this sample from an umbilical artery or from the umbilical vein? Explain. 24. Name the structures that are vital to fetal circulation but cease to function at birth. What becomes of each of these structures? © 2013 Pearson Education, Inc.
Effects of Aging on Blood (13 -9) • Lower hematocrit • Formation of a thrombus, or stationary blood clot • Can detach becoming an embolism • Pooling of blood in veins of leg • Due to ineffective venous valves © 2013 Pearson Education, Inc.
Effects of Aging on the Heart (13 -9) • Reduction in maximum cardiac output • Changes in nodal and conducting cells • Reduction of elasticity of cardiac skeleton • Progressive atherosclerosis • Serious if found in coronary circulation • Replacement of damaged cardiac muscle with scar tissue © 2013 Pearson Education, Inc.
Effects of Aging on the Vessels (13 -9) • Arteriosclerosis or thickening and toughening of wall • Inelastic walls of arteries less tolerant of pressure increase • Can lead to local dilation, an aneurysm • Calcium salts deposited on walls • Can lead to stroke or myocardial infarction • Thrombi can form at atherosclerotic plaques © 2013 Pearson Education, Inc.
Checkpoint (13 -9) 25. Identify components of the cardiovascular system that are affected by age. 26. Define thrombus. 27. Define aneurysm. © 2013 Pearson Education, Inc.
Cardiovascular System Linked to All Other Systems (13 -10) • Cardiovascular system supplies all others with: • Oxygen • Hormones • Nutrients • White blood cells • Removes: • Carbon dioxide and metabolic wastes © 2013 Pearson Education, Inc.
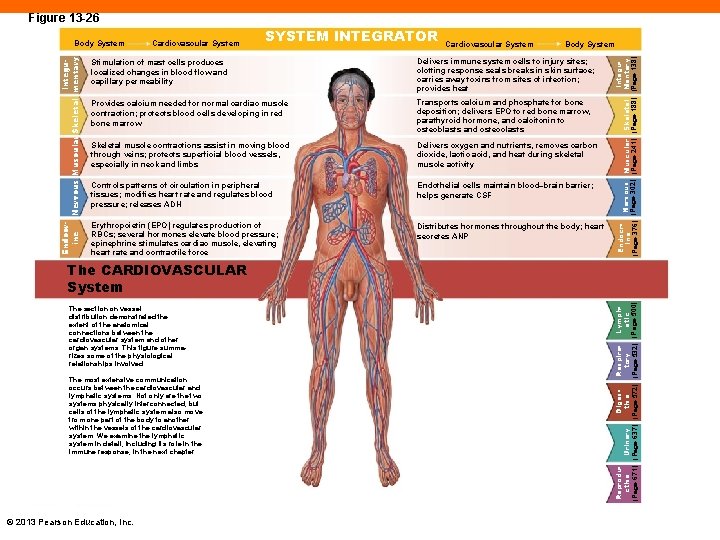
Figure 13 -26 Cardiovascular System SYSTEM INTEGRATOR Cardiovascular System Body System Stimulation of mast cells produces localized changes in blood flow and capillary permeability Delivers immune system cells to injury sites; clotting response seals breaks in skin surface; carries away toxins from sites of infection; provides heat Provides calcium needed for normal cardiac muscle contraction; protects blood cells developing in red bone marrow Transports calcium and phosphate for bone deposition; delivers EPO to red bone marrow, parathyroid hormone, and calcitonin to osteoblasts and osteoclasts Skeletal muscle contractions assist in moving blood through veins; protects superficial blood vessels, especially in neck and limbs Delivers oxygen and nutrients, removes carbon dioxide, lactic acid, and heat during skeletal muscle activity Controls patterns of circulation in peripheral tissues; modifies heart rate and regulates blood pressure; releases ADH Endothelial cells maintain blood–brain barrier; helps generate CSF Erythropoietin (EPO) regulates production of RBCs; several hormones elevate blood pressure; epinephrine stimulates cardiac muscle, elevating heart rate and contractile force Distributes hormones throughout the body; heart secretes ANP Integu. Endocr. Nervous Muscular Skeletal Mentary Ine (Page 302) (Page 241) (Page 188) (Page 138) (Page 376) Endocr. Integuine Nervous Muscular Skeletal mentary Body System The section on vessel distribution demonstrated the extent of the anatomical connections between the cardiovascular system and other organ systems. This figure summarizes some of the physiological relationships involved. The most extensive communication occurs between the cardiovascular and lymphatic systems. Not only are the two systems physically interconnected, but cells of the lymphatic system also move from one part of the body to another within the vessels of the cardiovascular system. We examine the lymphatic system in detail, including its role in the immune response, in the next chapter. © 2013 Pearson Education, Inc. Reprodu. Diges. Respira. Lymph. Urinary ctive tory atic (Page 671) (Page 637) (Page 572) (Page 532) (Page 500) The CARDIOVASCULAR System
Checkpoint (13 -10) 28. Describe what the cardiovascular system provides for all other body systems. 29. What is the relationship between the skeletal system and the cardiovascular system? © 2013 Pearson Education, Inc.
- Slides: 112