Infections in the immunocompromised patient Inger Karin Lgreid



- Slides: 56
Infections in the immunocompromised patient. Inger Karin Lægreid Avd for nyresykdommer St. Olavs Hospital Desember 2011
Immunocompromised patients: • Organtransplanted – immunosuppressive medications • Cancerpatients – cytotoxic drugs + xray • Systemic illnesses – ex. Vasculitis, Lupus, RA - immunosuppressive medications + cytotoxic drugs • HIV pos / AIDS
Risk factors for infections • 1. High dosis of immunosuppressive medications - Because of treatment failure or rejection - Repeating treatments - Cumulative dosis • 2. Leucopenia - Induced by a. medications: - Most often cytotoxic drugs and - azathioprine(Imurel), mycophenalate (Cell Cept or Myfortic) - or b. virus: CMV
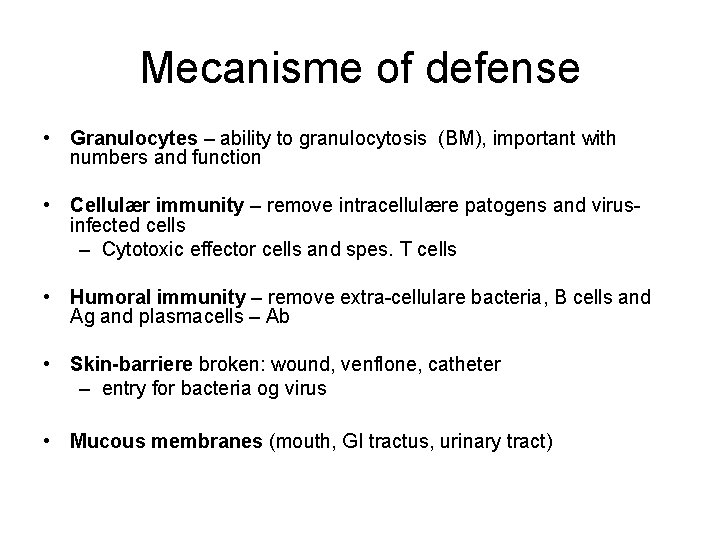
Mecanisme of defense • Granulocytes – ability to granulocytosis (BM), important with numbers and function • Cellulær immunity – remove intracellulære patogens and virusinfected cells – Cytotoxic effector cells and spes. T cells • Humoral immunity – remove extra-cellulare bacteria, B cells and Ag and plasmacells – Ab • Skin-barriere broken: wound, venflone, catheter – entry for bacteria og virus • Mucous membranes (mouth, GI tractus, urinary tract)
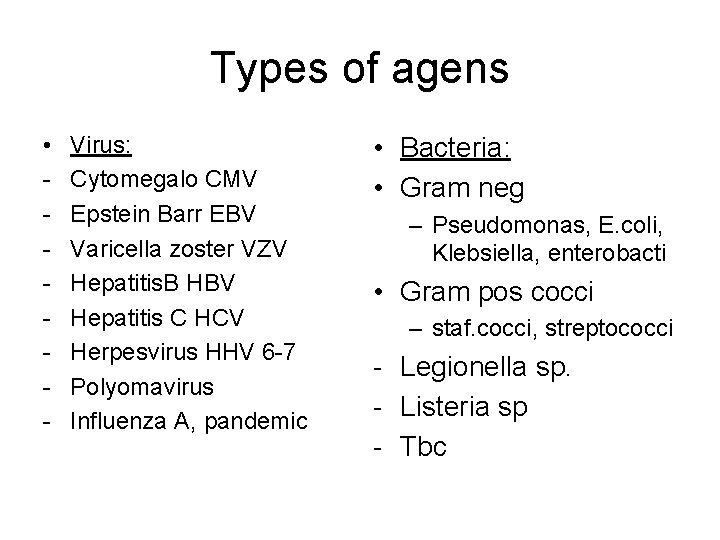
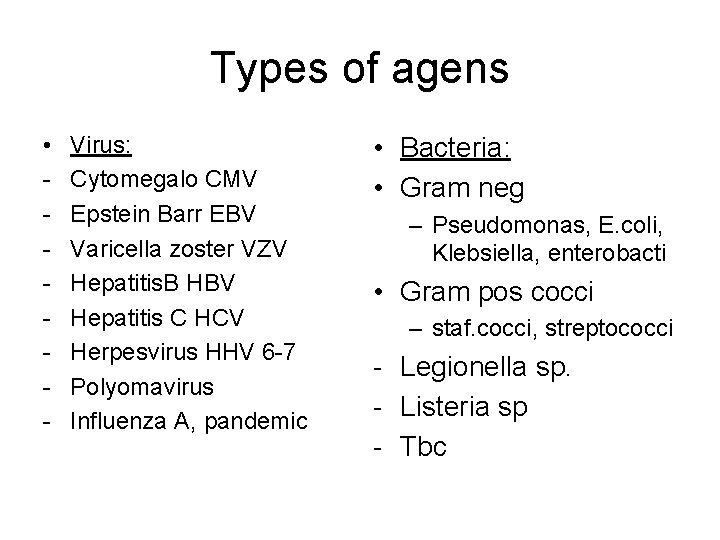
Types of agens • - Virus: Cytomegalo CMV Epstein Barr EBV Varicella zoster VZV Hepatitis. B HBV Hepatitis C HCV Herpesvirus HHV 6 -7 Polyomavirus Influenza A, pandemic • Bacteria: • Gram neg – Pseudomonas, E. coli, Klebsiella, enterobacti • Gram pos cocci – staf. cocci, streptococci - Legionella sp. - Listeria sp - Tbc
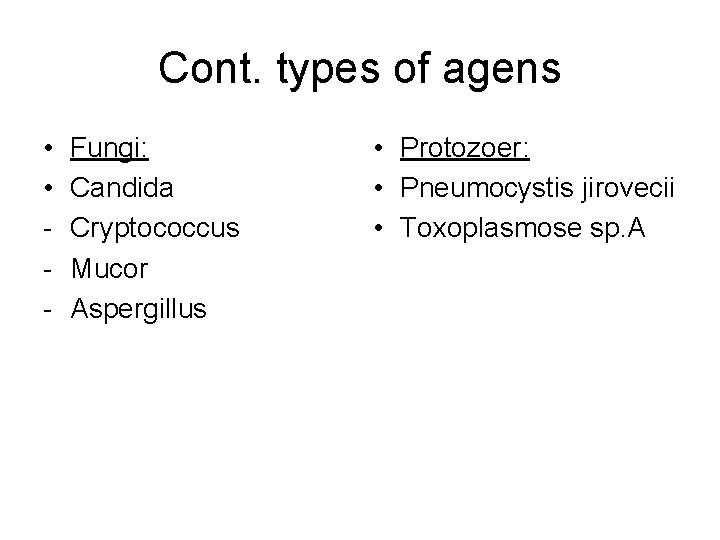
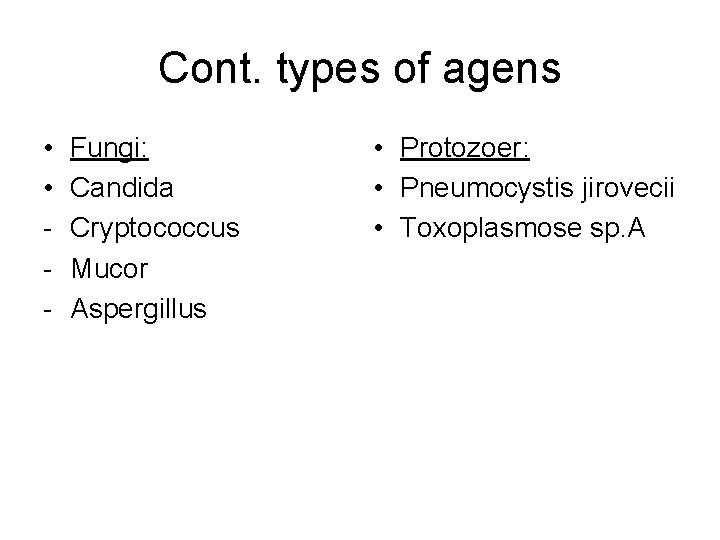
Cont. types of agens • • - Fungi: Candida Cryptococcus Mucor Aspergillus • Protozoer: • Pneumocystis jirovecii • Toxoplasmose sp. A

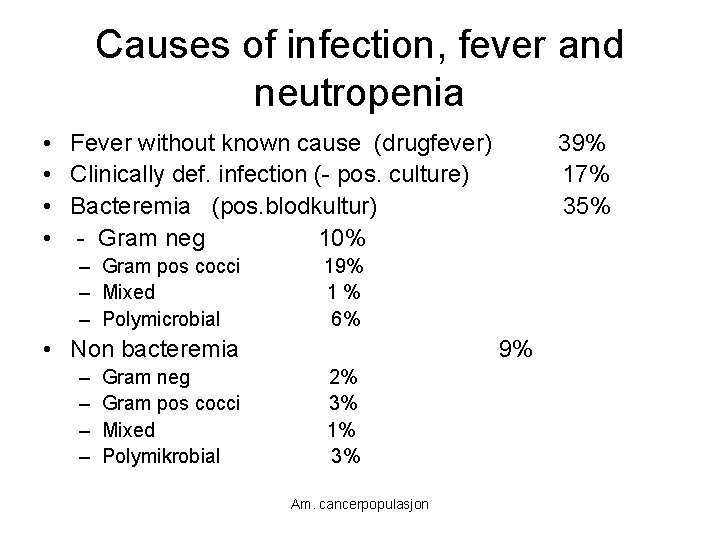
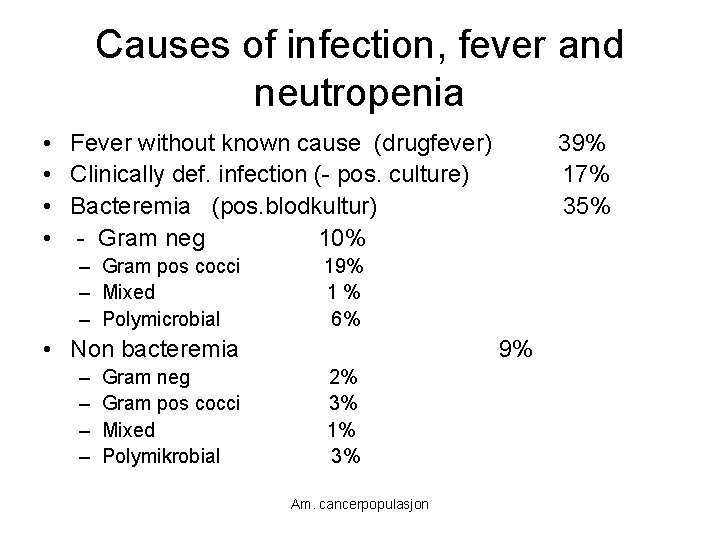
Causes of infection, fever and neutropenia • Fever without known cause (drugfever) • Clinically def. infection (- pos. culture) • Bacteremia (pos. blodkultur) • - Gram neg 10% – Gram pos cocci – Mixed – Polymicrobial 19% 1% 6% • Non bacteremia – – Gram neg Gram pos cocci Mixed Polymikrobial 39% 17% 35% 9% 2% 3% 1% 3% Am. cancerpopulasjon

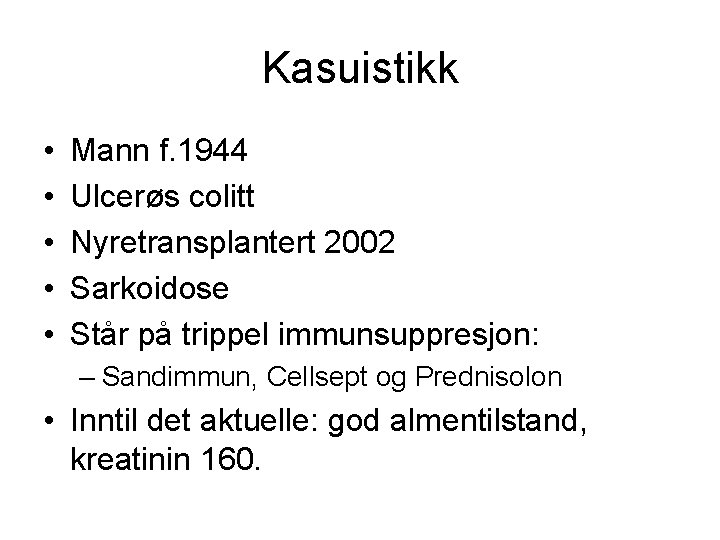
Kasuistikk • • • Mann f. 1944 Ulcerøs colitt Nyretransplantert 2002 Sarkoidose Står på trippel immunsuppresjon: – Sandimmun, Cellsept og Prednisolon • Inntil det aktuelle: god almentilstand, kreatinin 160.
Kasuistikk • Feber, tørrhoste, slapphet frå 3. 12 • Opps fastlege , får Ciproxin • Ny kontakt pga ingen effekt/ forverring av symptomer → innlegges. • Ved innk 10. 12: feber, hoste, tungpust, CRP: 130, kreatinin 204 (e. GFR 28 ml/min) • Rtg. thoraks: småflekka infiltrat bilat, mest utbredt perihilært. Atypisk pneumoni? ? • Starter Rocephalin (cephalosporin)
Kasuistikk • Trass i Rocephalin – tilstanden forverres, økende dyspnoe, stigende CRP • Utifrå klinikk, CT thoraks og rtg. thorax funn – atypisk pneumoni: ? ? Pneumocystis Jirovecii • Planlagt bronkoskopi med BAL – pas for dårlig. • Starter Trim Sulfa (TMS) på mistanke, red dose pga nyresvikt • Forverring → Respirator • Bronkoskopi med BAL: Pneumoc J → høg dose TMS
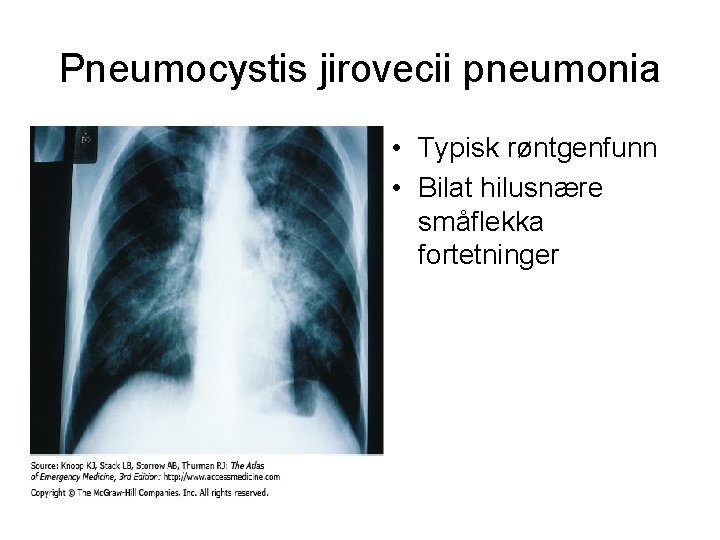
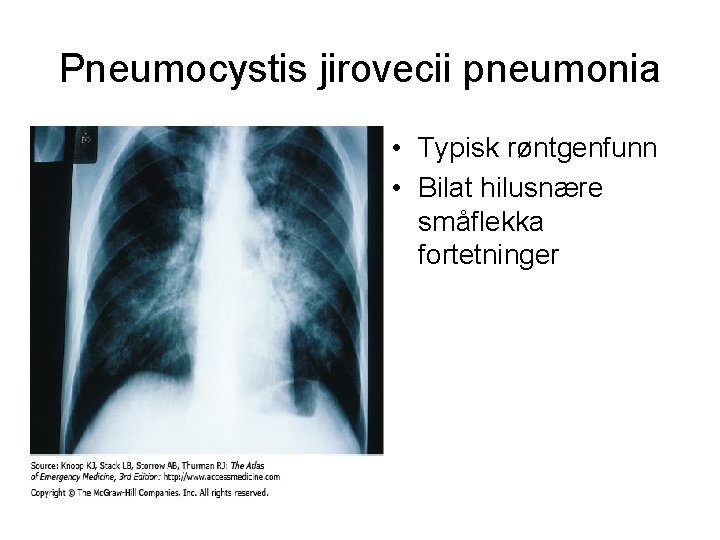
Pneumocystis jirovecii pneumonia • Typisk røntgenfunn • Bilat hilusnære småflekka fortetninger
Kasuistikk • • • Uendra resp. status over fleire dager Terapisvikt pga initial låg TMS dose? Høg dose → økende nyresvikt + rhabdomyolyse Red TMS, må seponeres. 04. 01. 11: fortsatt på respirator, betring i nyrefunksjon (kreat 125), CRP 102, svært usikker prognose. • Får spontan pneumothorax – vanskelig å ventilere • Har ARDS, lungefibrose. • Avslutter respiratorbehandling 5. 1 –pas sovner inn samme dag
Pneumocystis jirovecii • Incidens hos organ tranplanterte: 5 – 15% • Reservoir: barn, symp og asympt immunkomprimerte pasienter • Luftsmitte via mennesker – opptrer ofte i ”cluster” • Riskofaktorer: alder, CMV infeksjoner, rejeksjoner, ↓ lymfocytter • Obs. coinfection (Herpesvirus)
Listeria monocytogenes • Listeria sepsis in adults nonpregnant: – Most are immunocompromised or elderly – Symptoms: fever and chills – Septic shock – Seeding of the brain and/or meninges – Meningoencephalitis or cerebritis – Diagnosis: culture of blood and cerebrospinal fluid (CSF) – Cerebral MRI
Listeria M • Listeria RH autum 2007: – Kantine serverte upasteurisert gårdsost – 15 persons got the disease – 5 died, 3 immunocompromised and 2 unborn childs(twins) • Eng. studie 10 års materiale (1999 – 2009): – Cancerpas har 5 X større risiko for Listeria M – Hematologisk cancer mest utsatt (17 x) – I tillegg til cancer: lever, nyresykdommer, bindevevssykdommer(Lupus) og inflammatoriske sykdommer (Crohns sykdom) Piers Mook et al; Em Inf Dis 2011 Jan
Listeria M • Treatment: – Ampicillin – Gentamycin ( in combination the first days) • Prognosis: – Total mortality: 25% – Higher by menigitis and sepsis
Legionella • Pneumonia – predominantly clinical manifestation • Cough – initially mild • Chest pain • High fever > 39 • Gastrointestinal symptoms • Headache
Legionella • Diagnosis: – Xray of lungs: patchy infiltrates – Culture of blood ( specific medium) – BAL – Direct immunfluorescens – Antigen- test in urine
Legionella • Treatment: –Erythromycin –In combination with ciprofloxacin or rifampicin • Prognosis: • Mortality: 5 – 30%
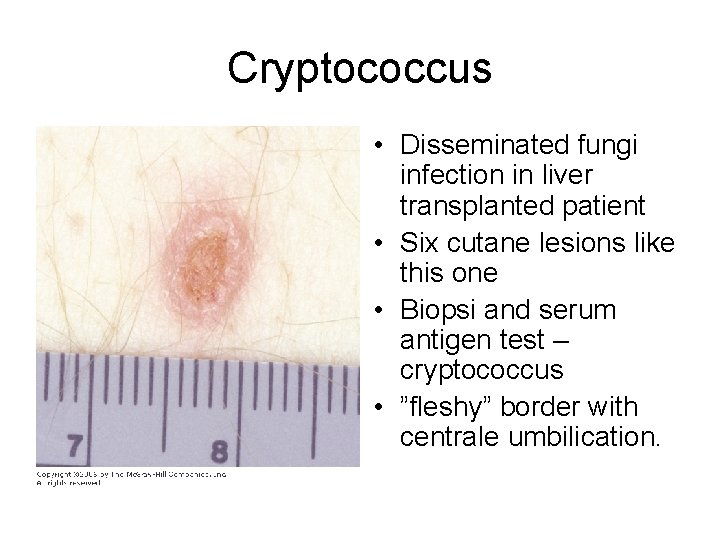
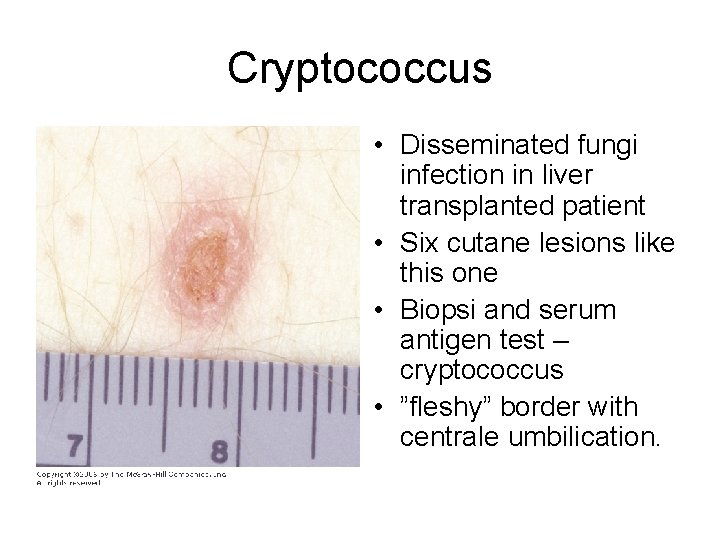
Cryptococcus • Disseminated fungi infection in liver transplanted patient • Six cutane lesions like this one • Biopsi and serum antigen test – cryptococcus • ”fleshy” border with centrale umbilication.
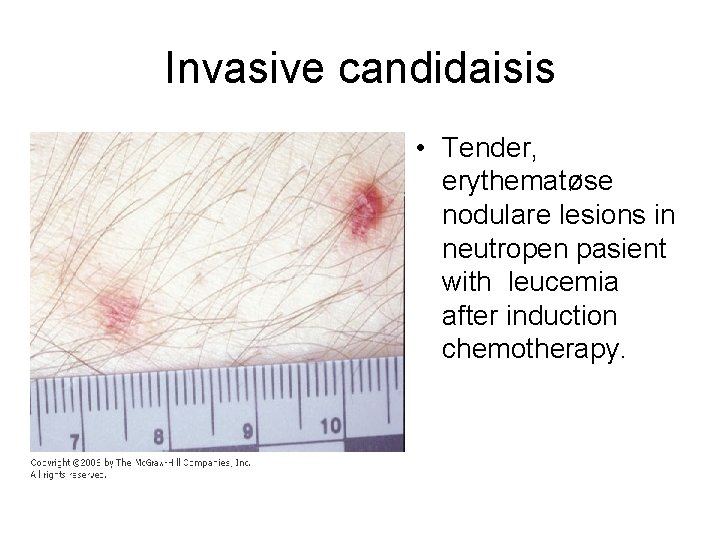
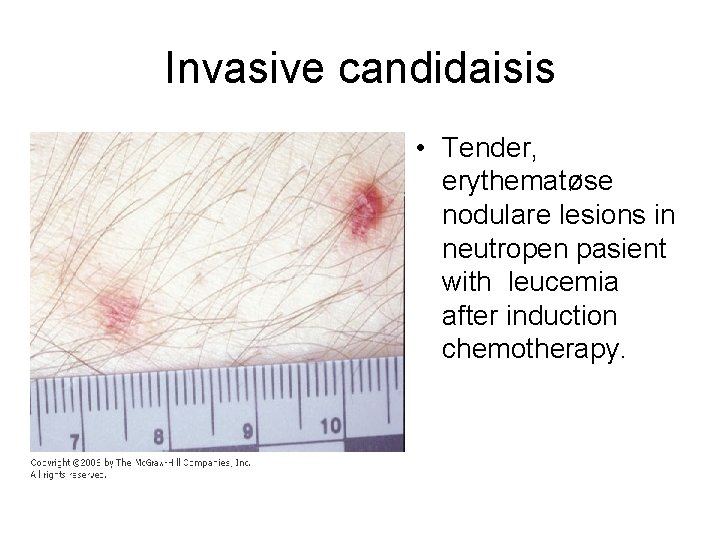
Invasive candidaisis • Tender, erythematøse nodulare lesions in neutropen pasient with leucemia after induction chemotherapy.
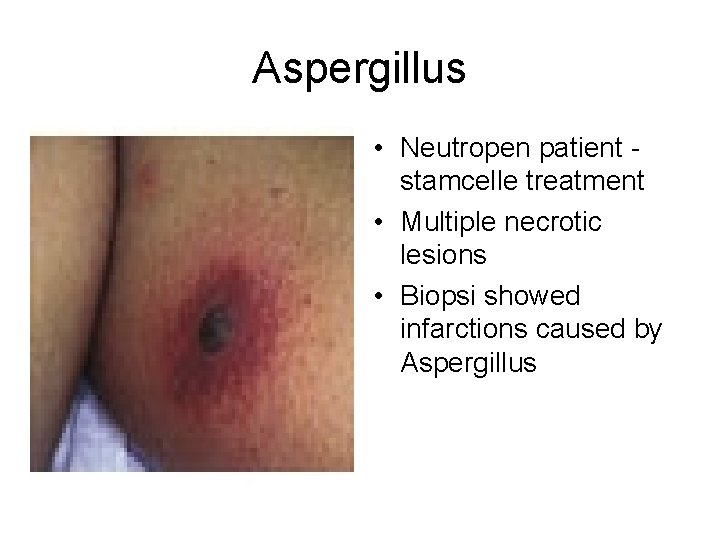
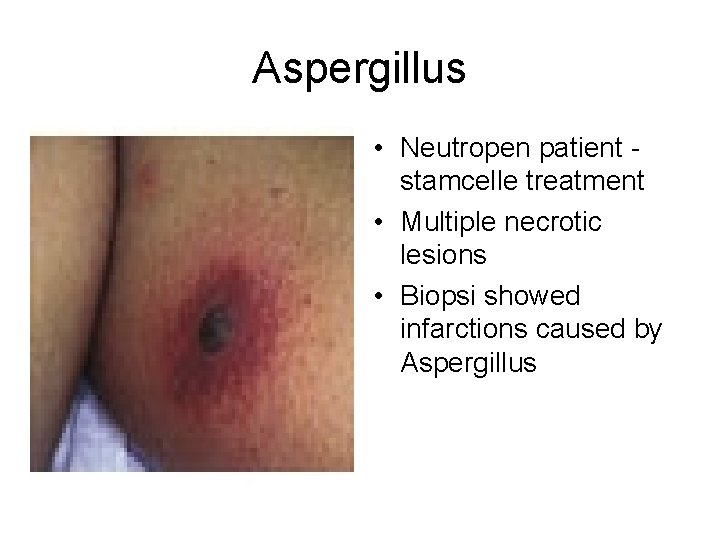
Aspergillus • Neutropen patient stamcelle treatment • Multiple necrotic lesions • Biopsi showed infarctions caused by Aspergillus
Herpes Zoster • 1. primær infeksjon: vannkopper • 2. Herpes Zoster – reaktivering av endogent latente varizella zoster virus i sensoriske ganglier – Følger dermatomer • 75% har prodromale smerter før utslettet • Starter ofte med små røde flekker → blemmer • Varizella zoster pneumonitt – alvorlig prognose
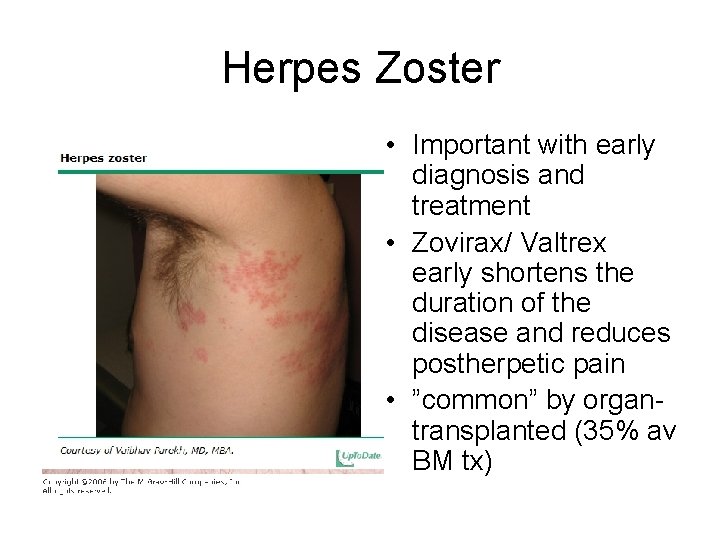
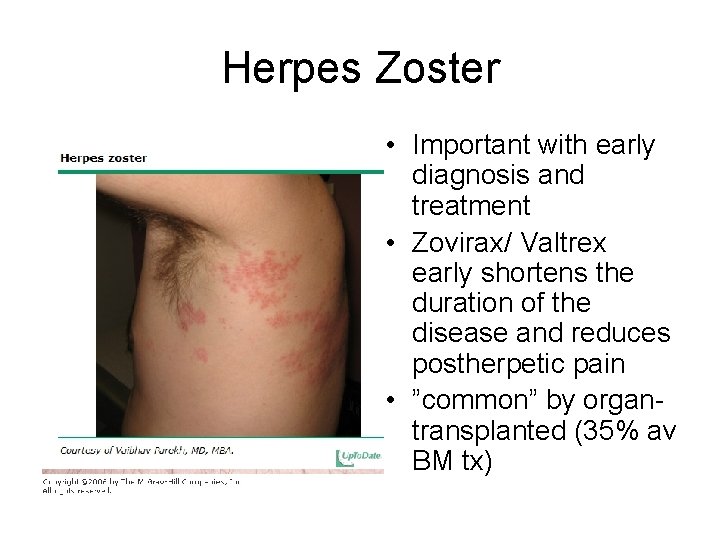
Herpes Zoster • Important with early diagnosis and treatment • Zovirax/ Valtrex early shortens the duration of the disease and reduces postherpetic pain • ”common” by organtransplanted (35% av BM tx)
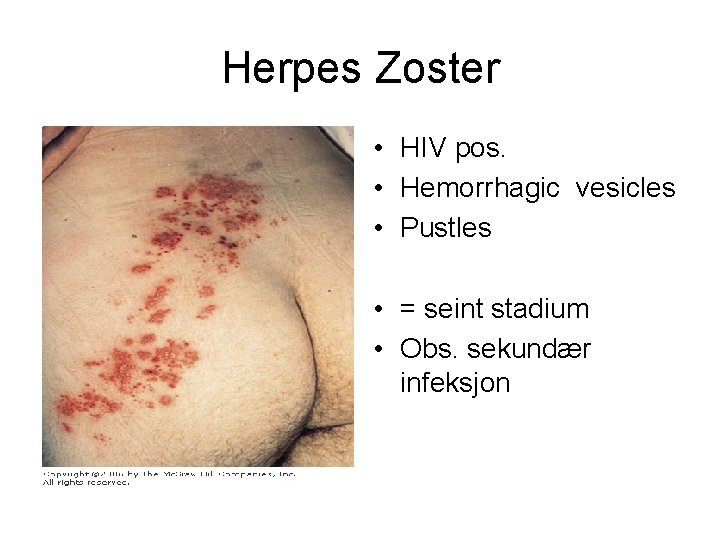
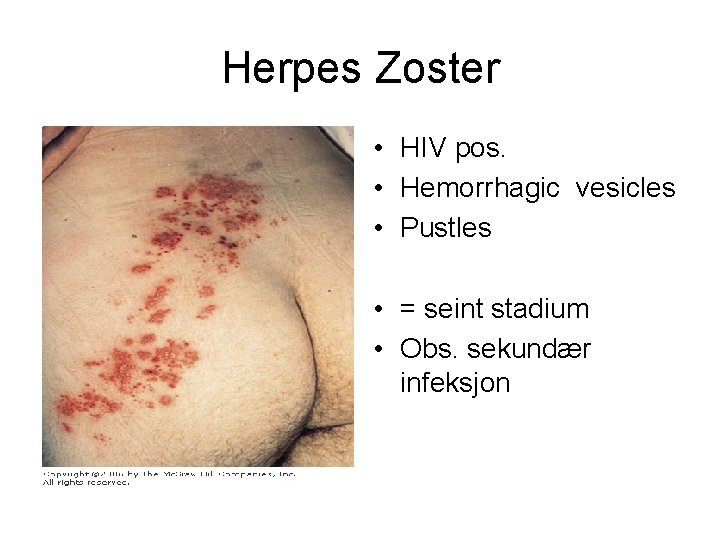
Herpes Zoster • HIV pos. • Hemorrhagic vesicles • Pustles • = seint stadium • Obs. sekundær infeksjon
Herpes Zoster • Male b. 1960. Refugee from Vietnam • Cystic kidney disease, - renal transplanted april 98 • Rejection – Solumedrole + Thymoglobuline • Creatinine at discharge from RH july 98 : 320 • Aug -98: pain at left eye and ear. Opthalmoscopy: Shows vesicles, diagnosed as HZ optalmicus, gets general eyedrops.
Herpes Zoster II • 1 week later- hospitalizes with widespread Herpes Zoster Oftalmicus with affection of left part of the face incl. left ear • Zovirax (in reduced dosis because of reduced renal function) • Discharged from hospital after 2 weeks.
Herpes Zoster III • • 1 week later – new hosp : fever, dyspnoe og cough Blood tests: High CRP og leucopenia Xray lungs: diffuse infiltrate – agents? Broncoskopi with BAL: stafylococcus aureus + CMV Sepsis- multiorgan failure – respirator – dialysis Sep 2 of 3 immunosuppressive medications Survives with a rel. good outcome • status nov 2007: -- creat 130, chronic pain in left part of face, got perforation of tympanic membrane in -98, relapsing otitis later, planned operative treatment (myringoplastic surgery)

Herpes Zoster ophtalmicus • Rammer Trigeminus dermatom • Kan føre til corneal affeksjon og føre til synstap
Cytomegalovirus CMV • Member of B-herpes family • big ds DNA virus. Transmitted by : -contact (sexually, nursing) - blood / organ (CMV pos til CMV neg) - mother to child (in utero, perinatal, lactation) • Asymptomatic primary infection, followed by lifelong latency, can be reactivated • Age related increase in seroprevalence: - by age 20: - 40% -by age 30: - 50% -by age 50: - 65% -by age 80: - 90%
CMV • The most common viral infection in organ-transplanted • Lungs>heart>liver>pancreas>kidney ”CMV- syndrome” (viremi): - fever, malaise, ( ”influenza-symptoms”), leucopenia, trombocytopenia, hepatic aminotransferase elevations Tissue – invasive CMV: - GI – duodenitis, gastritis, colitis, ulcus - Lungs – pneumonitis - Transplantat – nephritis, hepatitis, pneumonitis - Eye - retinitis
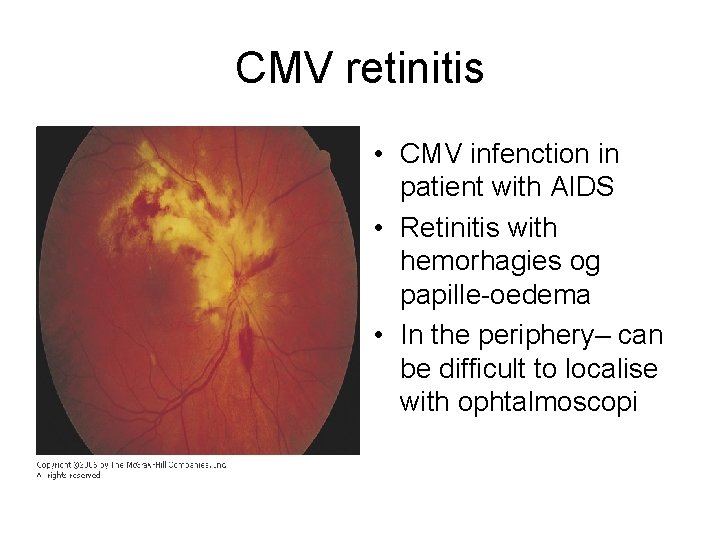
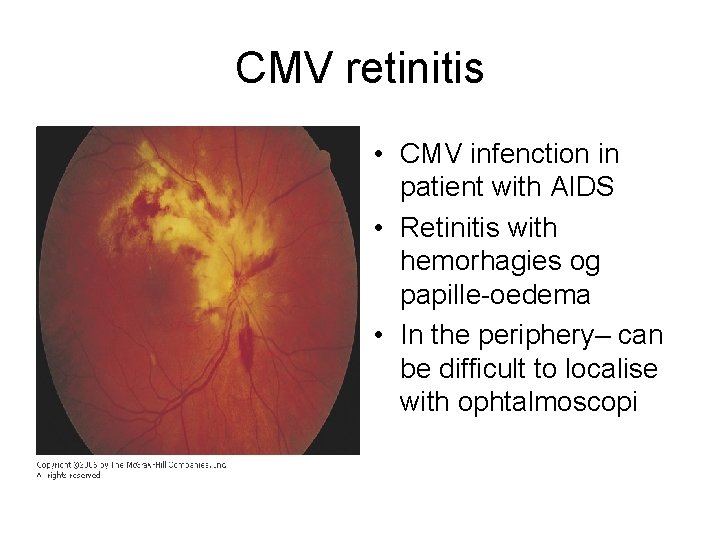
CMV retinitis • CMV infenction in patient with AIDS • Retinitis with hemorhagies og papille-oedema • In the periphery– can be difficult to localise with ophtalmoscopi
Epstein Barr virus EBV • 20 -30% of organtransplanted has active replication of EBV • 80% of these have got antilymfocytt- antibodies (because of serious rejection). • Cyclosporine A (Sandimmun), tacrolimus (Prograf) + Antilymfocytt-antibodies reactivate latent EBV infection • EBV can give mononucleosis • Important: the role of EBV in the pathogenesis of development of post-tx lymfoproliferative disease.
EBV II • B celle lymfoproliferativ process – can change from benign polyclonale process to a highly malignant monoclonal lymphoma which is resistante to treatment. • Post-tx disease – extranodale – brain, bonemarrow, organtransplant, GI-tractus and liver • Important to reduce or take away immunsuppressive medications • Most important that the patient survives, on the behalf of the transplanted organ.
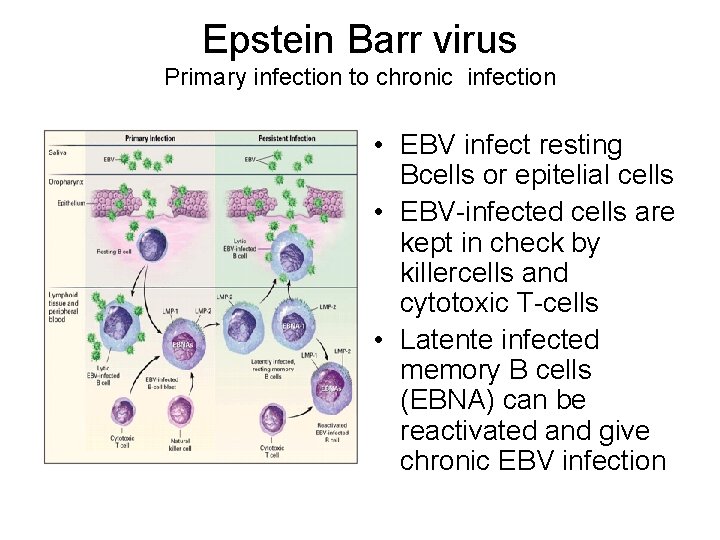
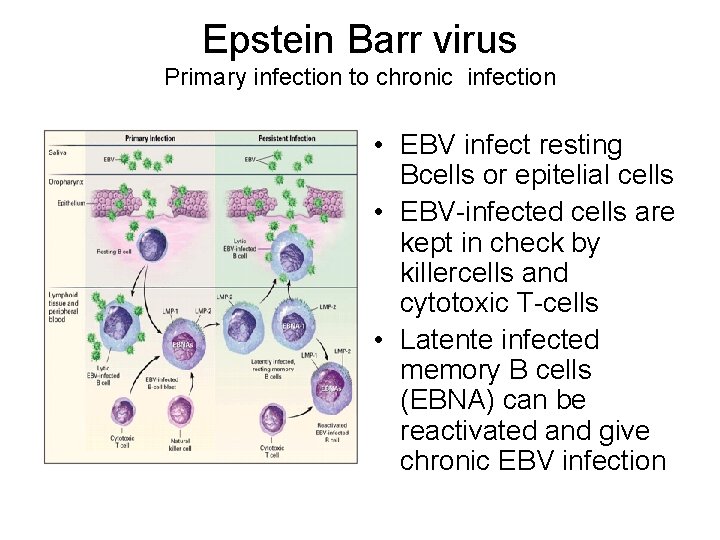
Epstein Barr virus Primary infection to chronic infection • EBV infect resting Bcells or epitelial cells • EBV-infected cells are kept in check by killercells and cytotoxic T-cells • Latente infected memory B cells (EBNA) can be reactivated and give chronic EBV infection
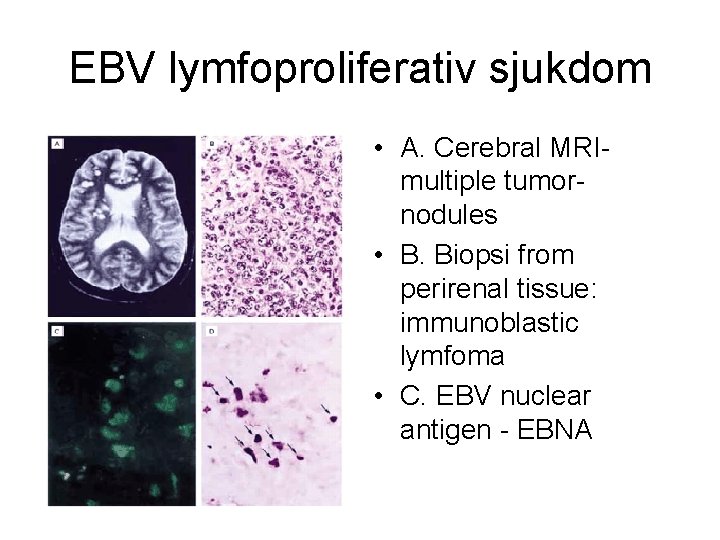
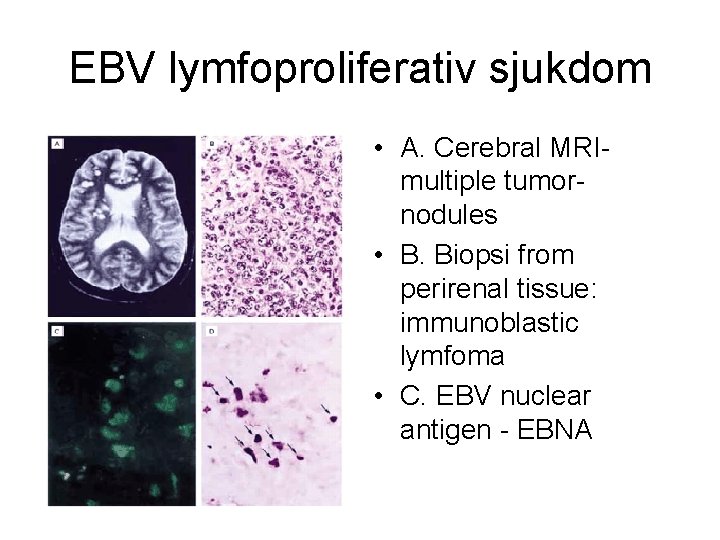
EBV lymfoproliferativ sjukdom • A. Cerebral MRImultiple tumornodules • B. Biopsi from perirenal tissue: immunoblastic lymfoma • C. EBV nuclear antigen - EBNA
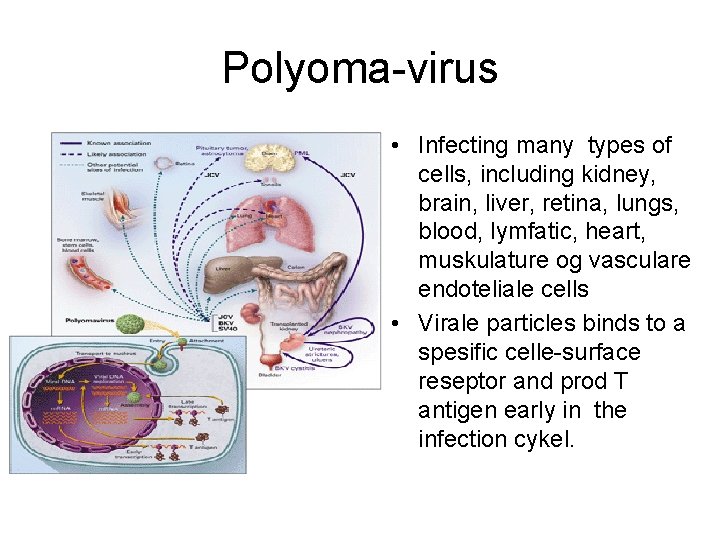
Polyoma virus PV • Ds DNA virus, two types ass. with humane disease: • BK virus • JK virus • 60 -80% av immuncompetente adults are seropos for PV • Renal transplanted: --PV-BK can give acute tubulo-intestitiell nephritis, ureter stenosis, hemorragic cystitis, serious transplantat dysfunction --PV-JK reactivation can give progressive multifokal leukoencephalopati
Polyomavirus • Diagnosis: ---cells who contains virale inclutionsbodies (”decoy cells”) in urine or biopsi of the transplant • Treatment: ---- reduction in immunsuppression --- cidofovir – seldom in use, highly nephrotoksic
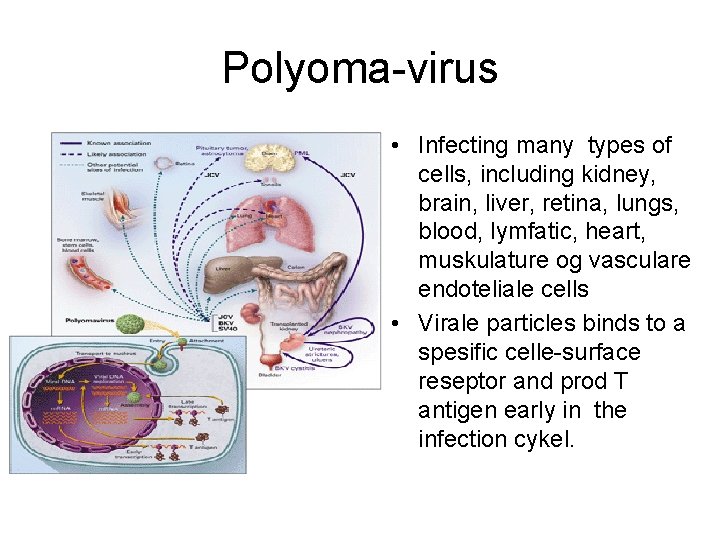
Polyoma-virus • Infecting many types of cells, including kidney, brain, liver, retina, lungs, blood, lymfatic, heart, muskulature og vasculare endoteliale cells • Virale particles binds to a spesific celle-surface reseptor and prod T antigen early in the infection cykel.
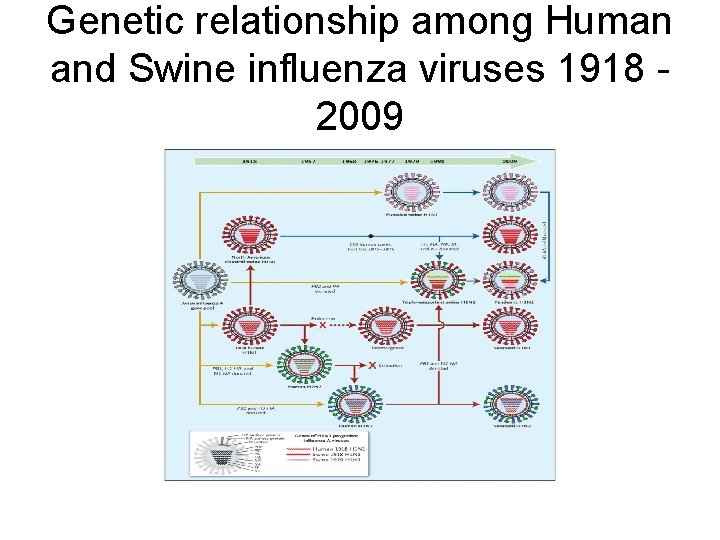
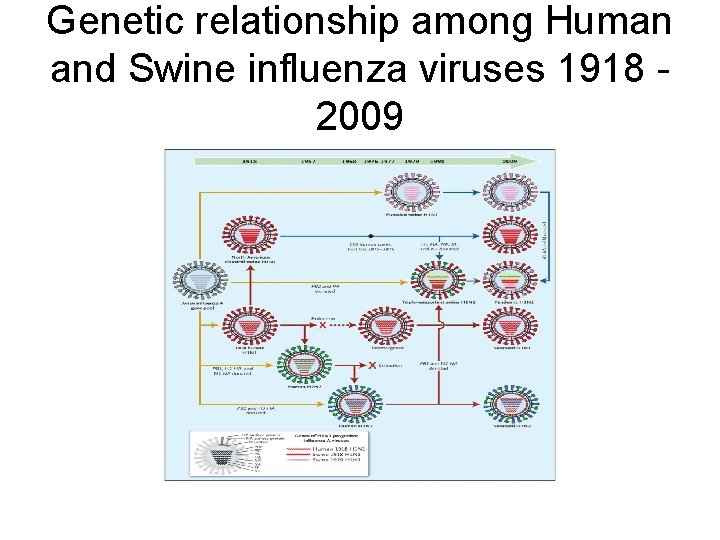
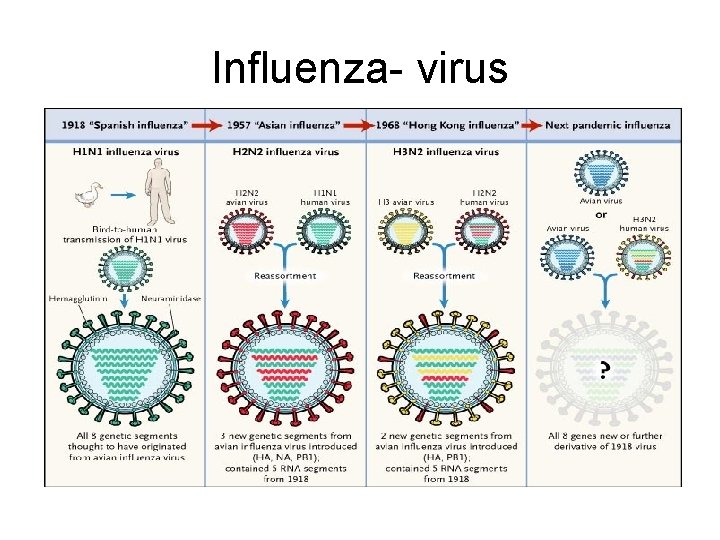
Genetic relationship among Human and Swine influenza viruses 1918 2009
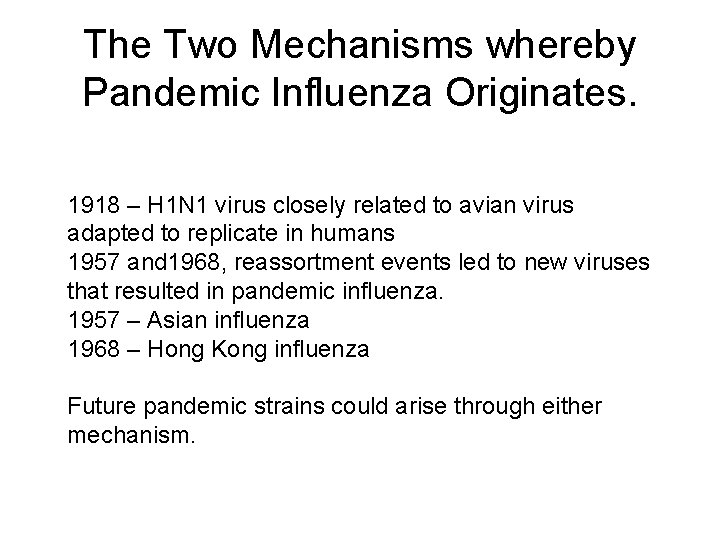
The Two Mechanisms whereby Pandemic Influenza Originates. 1918 – H 1 N 1 virus closely related to avian virus adapted to replicate in humans 1957 and 1968, reassortment events led to new viruses that resulted in pandemic influenza. 1957 – Asian influenza 1968 – Hong Kong influenza Future pandemic strains could arise through either mechanism.
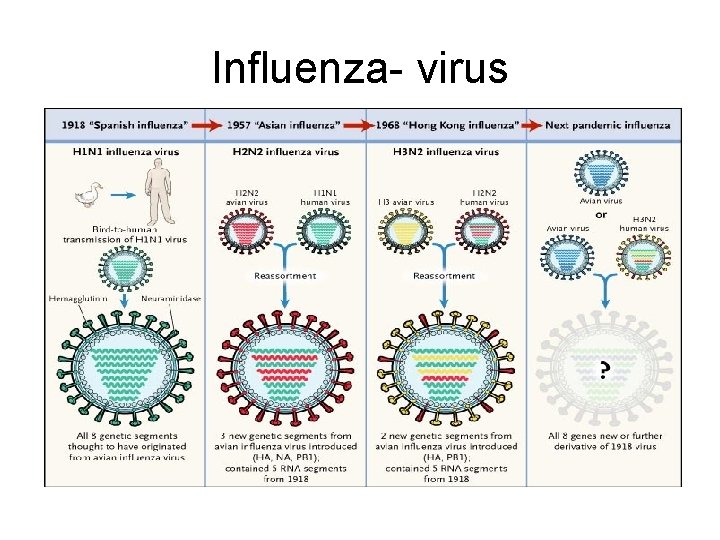
Influenza- virus
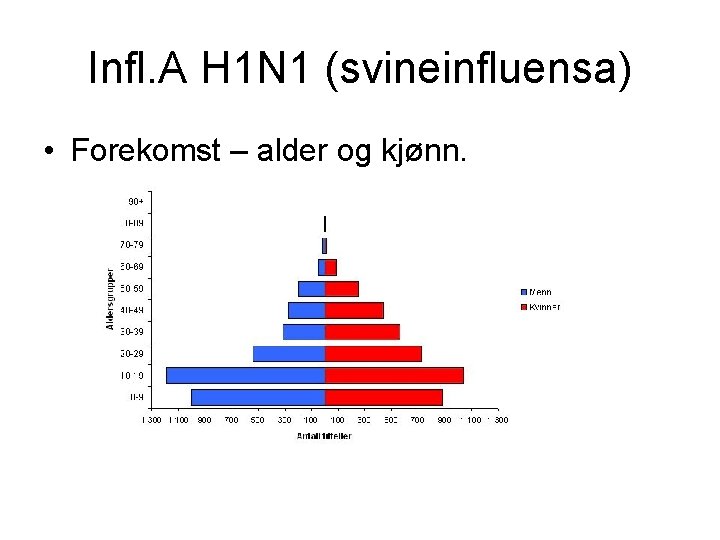
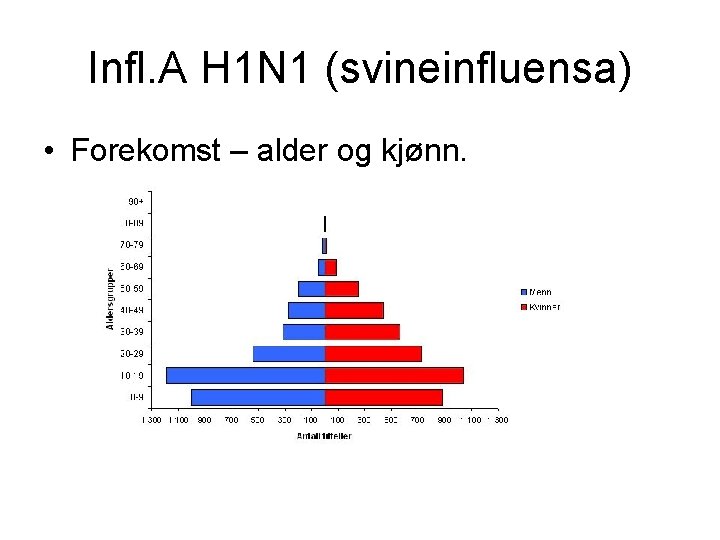
Infl. A H 1 N 1 (svineinfluensa) • Forekomst – alder og kjønn.
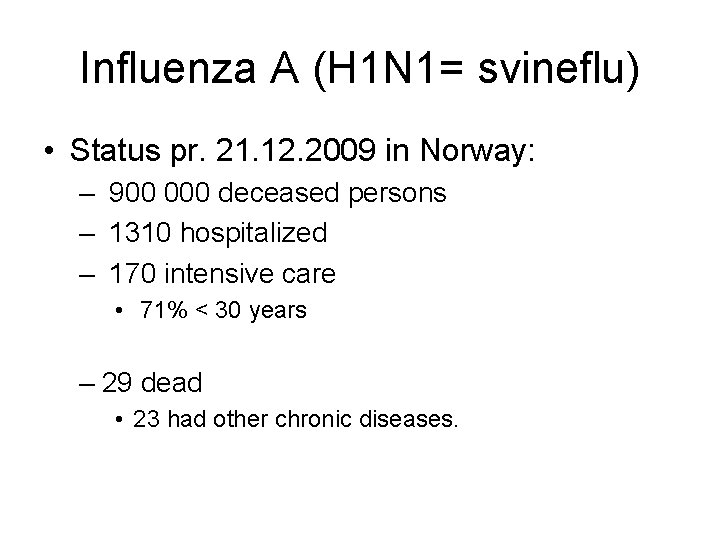
Influenza A (H 1 N 1= svineflu) • Status pr. 21. 12. 2009 in Norway: – 900 000 deceased persons – 1310 hospitalized – 170 intensive care • 71% < 30 years – 29 dead • 23 had other chronic diseases.
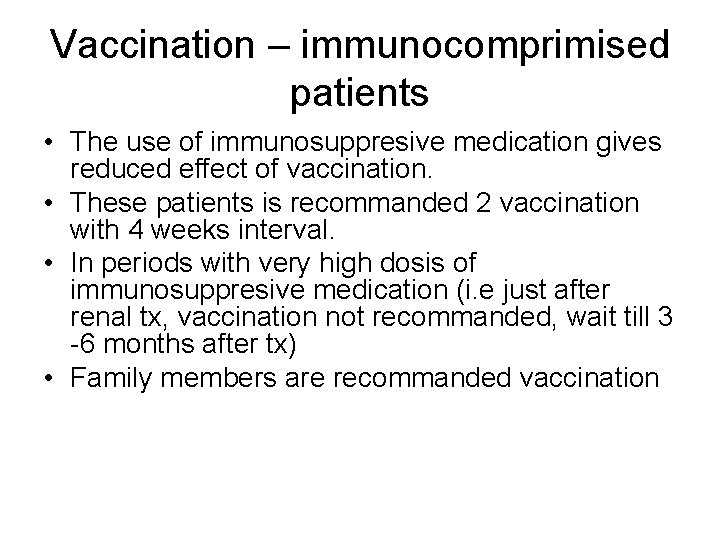
Vaccination – immunocomprimised patients • The use of immunosuppresive medication gives reduced effect of vaccination. • These patients is recommanded 2 vaccination with 4 weeks interval. • In periods with very high dosis of immunosuppresive medication (i. e just after renal tx, vaccination not recommanded, wait till 3 -6 months after tx) • Family members are recommanded vaccination
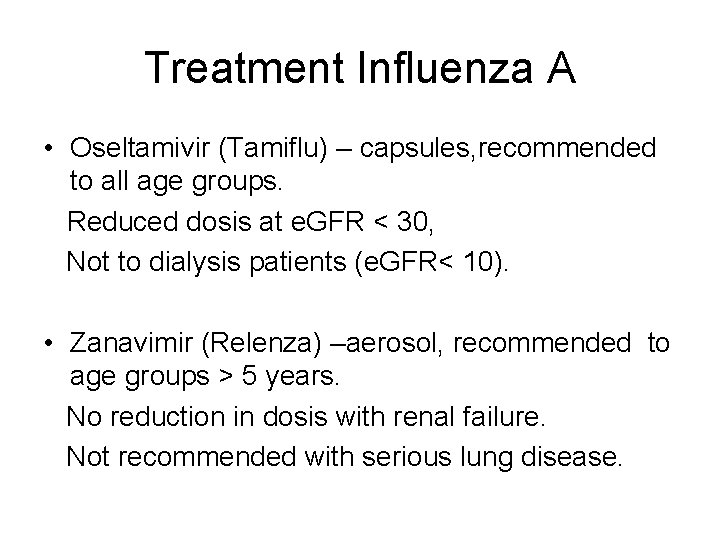
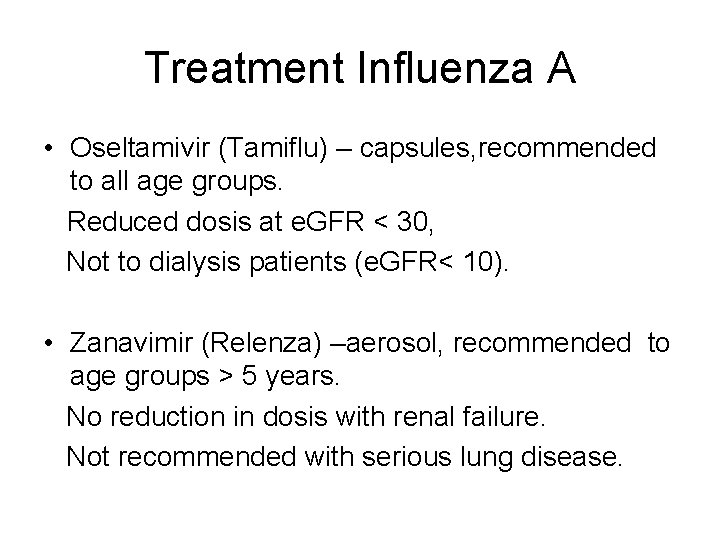
Treatment Influenza A • Oseltamivir (Tamiflu) – capsules, recommended to all age groups. Reduced dosis at e. GFR < 30, Not to dialysis patients (e. GFR< 10). • Zanavimir (Relenza) –aerosol, recommended to age groups > 5 years. No reduction in dosis with renal failure. Not recommended with serious lung disease.
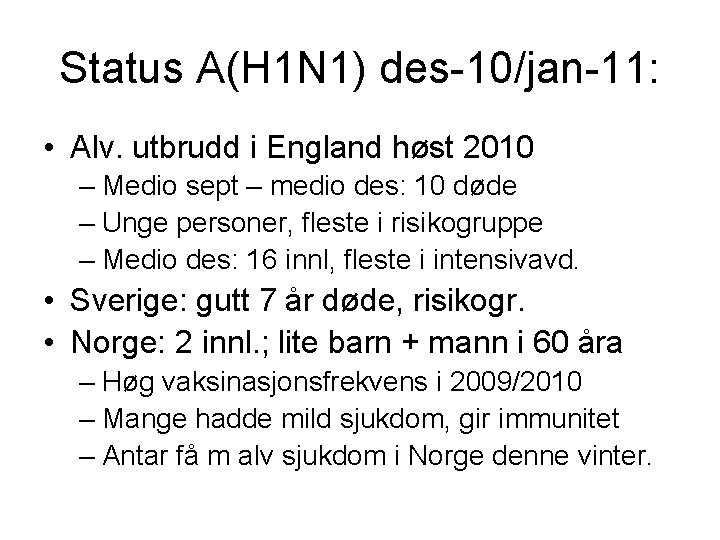
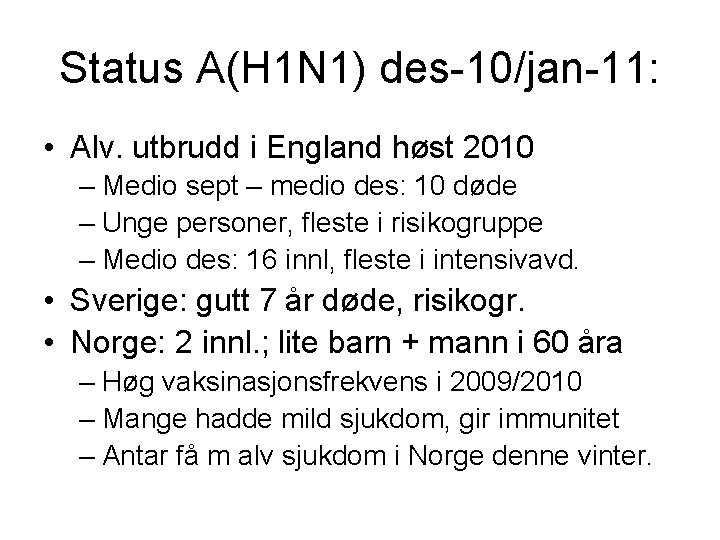
Status A(H 1 N 1) des-10/jan-11: • Alv. utbrudd i England høst 2010 – Medio sept – medio des: 10 døde – Unge personer, fleste i risikogruppe – Medio des: 16 innl, fleste i intensivavd. • Sverige: gutt 7 år døde, risikogr. • Norge: 2 innl. ; lite barn + mann i 60 åra – Høg vaksinasjonsfrekvens i 2009/2010 – Mange hadde mild sjukdom, gir immunitet – Antar få m alv sjukdom i Norge denne vinter.
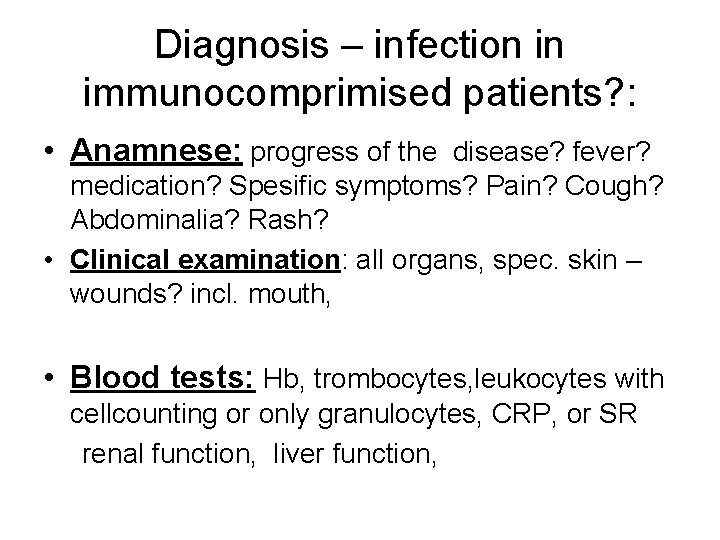
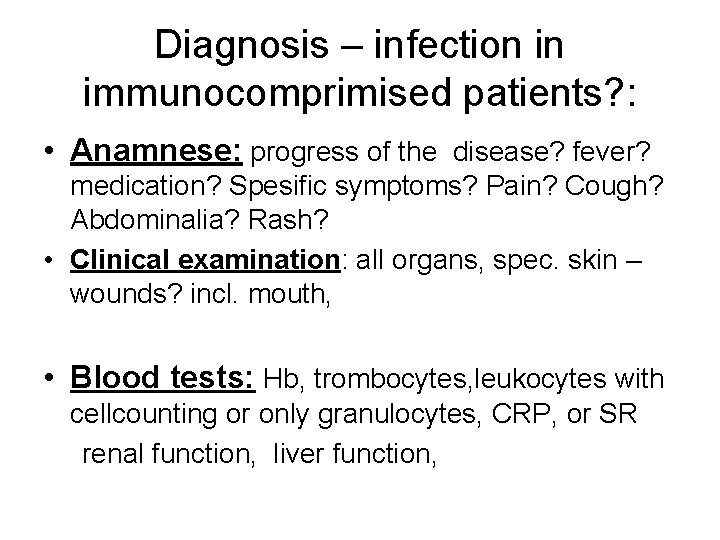
Diagnosis – infection in immunocomprimised patients? : • Anamnese: progress of the disease? fever? medication? Spesific symptoms? Pain? Cough? Abdominalia? Rash? • Clinical examination: all organs, spec. skin – wounds? incl. mouth, • Blood tests: Hb, trombocytes, leukocytes with cellcounting or only granulocytes, CRP, or SR renal function, liver function,
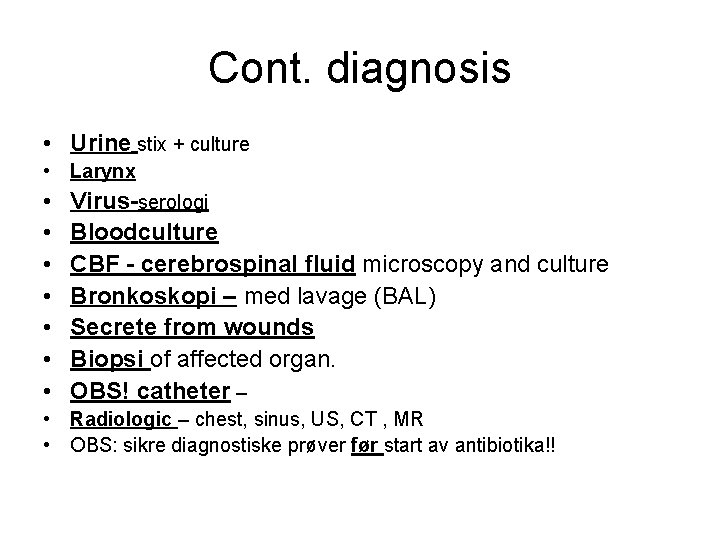
Cont. diagnosis • Urine stix + culture • Larynx • • Virus-serologi Bloodculture CBF - cerebrospinal fluid microscopy and culture Bronkoskopi – med lavage (BAL) Secrete from wounds Biopsi of affected organ. OBS! catheter – • Radiologic – chest, sinus, US, CT , MR • OBS: sikre diagnostiske prøver før start av antibiotika!!
Principles for antimicrobielle therapy • Treatment of established clinically disease • Prophylaxis – treat the entire patient-population prophylactic, fex all renal-transplant pat. get TMS as prophylaxis against Pneumocystis carini in 6 months post-tx • Preemptive therapy – treat subpopulations fex renaltx with pos CMV test, before clinically symptoms. • Obs. Studier må vise stor gevinst for å vege opp for risiko for resistensutvikling.
Anti-microbielle treatment Fever and neutropenia ( neutrophile < 0. 5 x 10 9 cells /L): (ex: nadirperiode etter tøffe cytostatika-kurer) • Big risk for lifethreathening infections, spec. gram. neg bacteria • Start with: benzylpenicillin + gentamicin • With clear abdominal symptoms: piperacillin/ tazobactam (Tazocin) • Dont hesitate – important with early start!!
Antifungal treatment • After 3 -5 days with neutropenia and fever –the risk for invasive mycosis is 25 -30% • The most common: candidasis • Treatment: fluconazol (Diflucan) • Suspicious for aspergillus and notflucanozol- sensitive candidasis: voriconazol (VFEND)
Antiviral treatment • Herpes simplex – valgancyclovir(Valcyte) -- acyclovir (Zovirax) -- valacyclovir (Valtrex) • CMV –gancyclovir ( Cymvene) – valgancyclovir • Herpes Zoster – acyclovir (Zovirax) • Diagnostikk: PCR- test in blood IF (immunofluorescens) Biopsi = gold standard
Conclusions • Immunocompromised pasients: – More vulnerable for infections – More often atypical infections, remember: virus, fungi, tbc – Can reacte different upon infections: • Less fever • Later signs on x-ray – Obs neutropenia – Obs medications • EARLY DIAGNOSIS and SPESIFIC TREATMENT is important for a good outcome!
 Inger karin lægreid
Inger karin lægreid Immunocompromised diseases list
Immunocompromised diseases list Food safety for immunocompromised patients
Food safety for immunocompromised patients 1 es típusú diabetes
1 es típusú diabetes Inger langseth
Inger langseth Inger nordby grønn
Inger nordby grønn Inger kraav
Inger kraav Stlan
Stlan Inger midmo
Inger midmo Inger merete terp
Inger merete terp Inger james
Inger james Adventsvers
Adventsvers Inger lise kaldhol
Inger lise kaldhol Kétpontküszöb térkép
Kétpontküszöb térkép Inger langseth
Inger langseth Kulcsinger fogalma
Kulcsinger fogalma Mi ez
Mi ez Patient 2 patient
Patient 2 patient Storch infections
Storch infections Eye infections
Eye infections Genital infections
Genital infections Opportunistic infections
Opportunistic infections Storch infections
Storch infections Genital infections
Genital infections Postpartum infections
Postpartum infections Chapter 25 sexually transmitted infections and hiv/aids
Chapter 25 sexually transmitted infections and hiv/aids Bone and joint infections
Bone and joint infections Opportunistic infections
Opportunistic infections Opsonization
Opsonization Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Understanding the mirai botnet
Understanding the mirai botnet Infections opportunistes digestives
Infections opportunistes digestives Can methotrexate cause yeast infections
Can methotrexate cause yeast infections Acute gingival infections
Acute gingival infections Diễn thế sinh thái là
Diễn thế sinh thái là Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau 101012 bằng
101012 bằng Công thức tính độ biến thiên đông lượng
Công thức tính độ biến thiên đông lượng Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Lời thề hippocrates
Lời thề hippocrates đại từ thay thế
đại từ thay thế Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Môn thể thao bắt đầu bằng chữ đua
Môn thể thao bắt đầu bằng chữ đua Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Sự nuôi và dạy con của hươu
Sự nuôi và dạy con của hươu Các loại đột biến cấu trúc nhiễm sắc thể
Các loại đột biến cấu trúc nhiễm sắc thể Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ độ dài liên kết
độ dài liên kết Gấu đi như thế nào
Gấu đi như thế nào Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan điện thế nghỉ
điện thế nghỉ Fecboak
Fecboak Một số thể thơ truyền thống
Một số thể thơ truyền thống Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất