Mycoplasma Pneumonia in an Immunocompromised Patient 12110 HPI





- Slides: 32
Mycoplasma Pneumonia in an Immunocompromised Patient 12_1_10
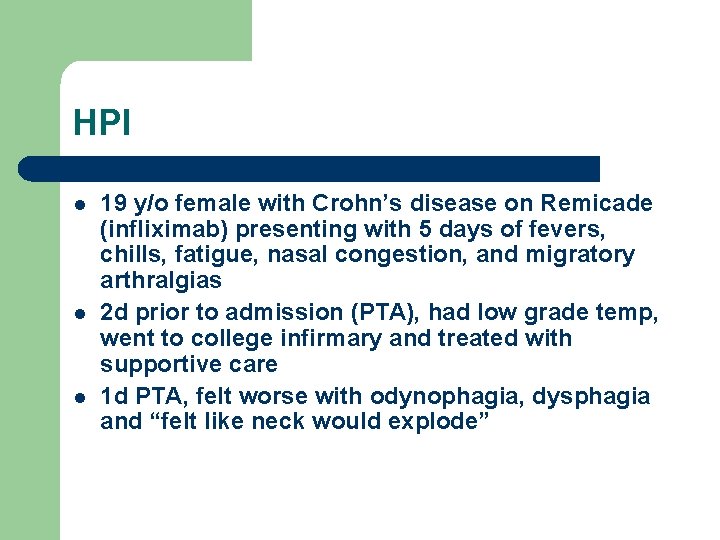
HPI l l l 19 y/o female with Crohn’s disease on Remicade (infliximab) presenting with 5 days of fevers, chills, fatigue, nasal congestion, and migratory arthralgias 2 d prior to admission (PTA), had low grade temp, went to college infirmary and treated with supportive care 1 d PTA, felt worse with odynophagia, dysphagia and “felt like neck would explode”
Review of Systems l l Pertinent positives -fever -fatigue -migratory arthralgias (jaw, neck, shoulders), -sore posterior neck -nausea -mild dry cough and congestion -hoarse voice Pertinent negatives: no respiratory symptoms apart from mild cough
PMH l Crohn’s disease -Diagnosed 11/09 (several months abdominal pain) -Initially was on Azathioprine (Imuran) and infliximab (Remicade, anti-TNF-a monoclonal antibody) -PPD negative prior to Remicade initiation -Now receiving Remicade every 7 -8 weeks (last dose 10/22/10)
PMH l l l Admitted 7/2010 for fever, arthralgia, LAN -workup (cx, EBV, CMV, Lyme, syphilis) all negative -CXR normal -presumed viral etiology Rheumatologic workup -saw rheum for swollen knees - had positive Anti. Smith Abs and elevated complement levels per report Birth: previously FT, NSVD, no complications
PSH l l s/p ear tubes as a baby for recurrent otitis media s/p inguinal hernia repair (age 8)
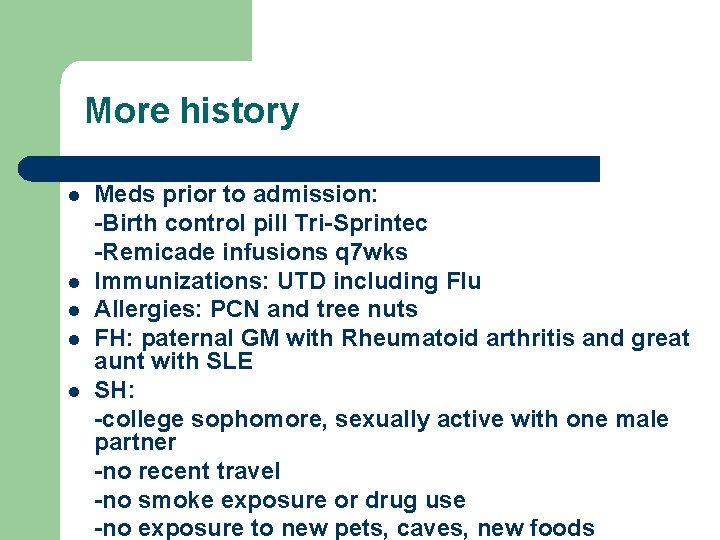
More history l l l Meds prior to admission: -Birth control pill Tri-Sprintec -Remicade infusions q 7 wks Immunizations: UTD including Flu Allergies: PCN and tree nuts FH: paternal GM with Rheumatoid arthritis and great aunt with SLE SH: -college sophomore, sexually active with one male partner -no recent travel -no smoke exposure or drug use -no exposure to new pets, caves, new foods
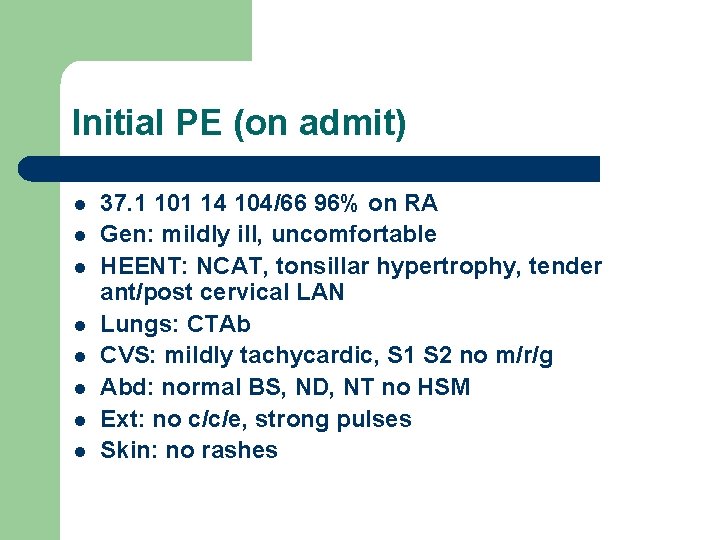
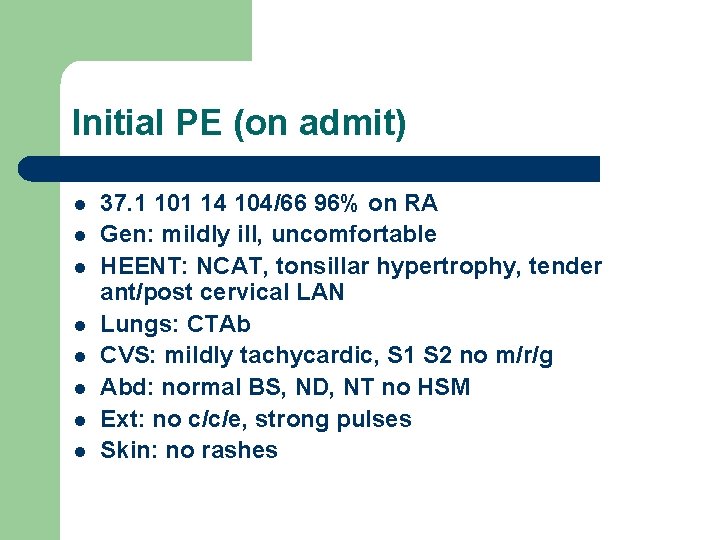
Initial PE (on admit) l l l l 37. 1 101 14 104/66 96% on RA Gen: mildly ill, uncomfortable HEENT: NCAT, tonsillar hypertrophy, tender ant/post cervical LAN Lungs: CTAb CVS: mildly tachycardic, S 1 S 2 no m/r/g Abd: normal BS, ND, NT no HSM Ext: no c/c/e, strong pulses Skin: no rashes
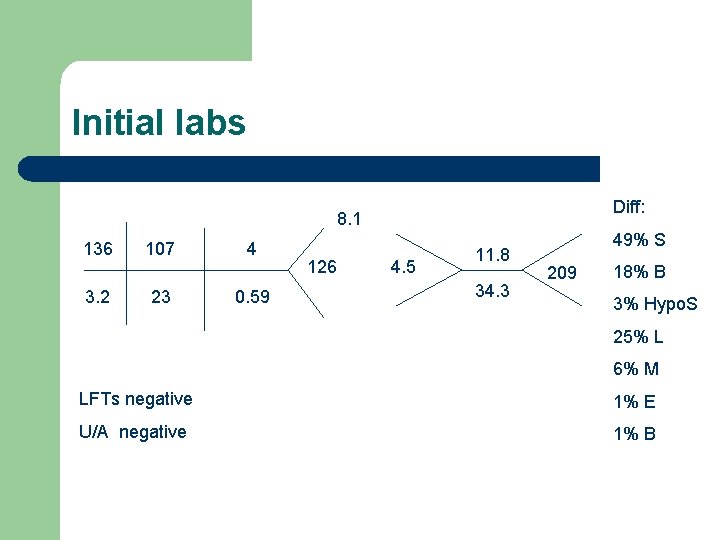
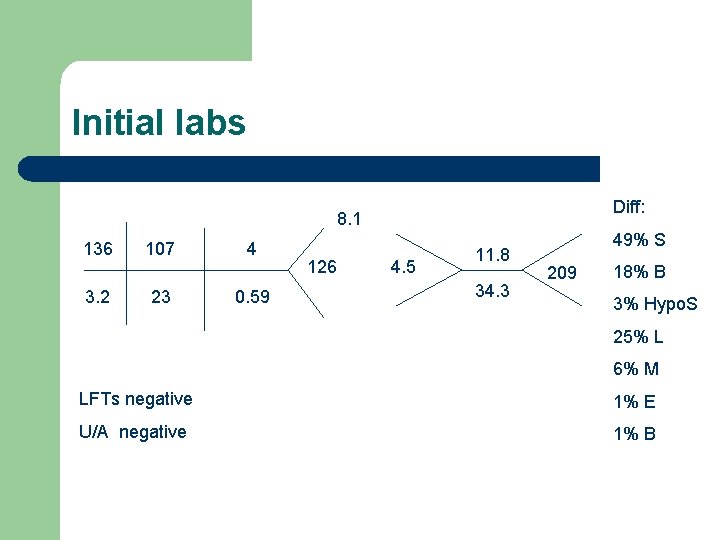
Initial labs Diff: 8. 1 136 3. 2 107 23 4 0. 59 126 4. 5 11. 8 34. 3 49% S 209 18% B 3% Hypo. S 25% L 6% M LFTs negative 1% E U/A negative 1% B

Initial CXR Clear lungs
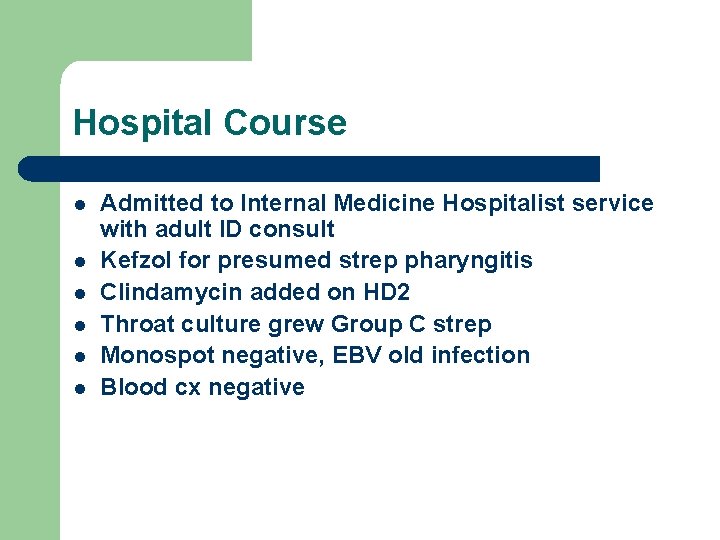
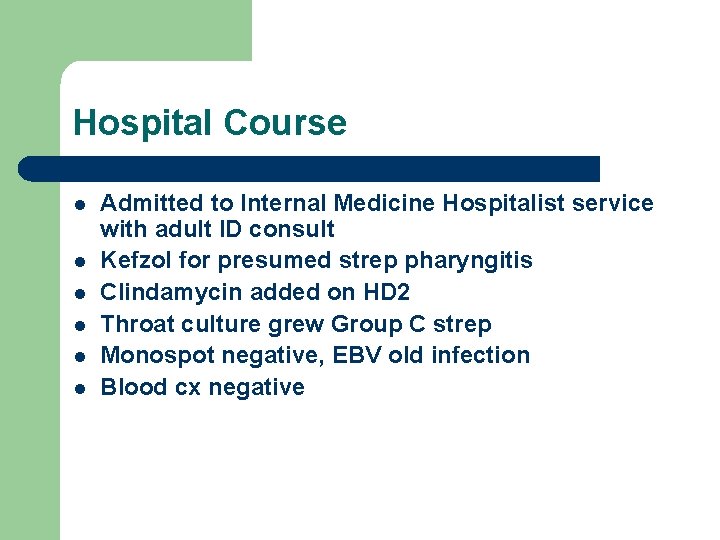
Hospital Course l l l Admitted to Internal Medicine Hospitalist service with adult ID consult Kefzol for presumed strep pharyngitis Clindamycin added on HD 2 Throat culture grew Group C strep Monospot negative, EBV old infection Blood cx negative
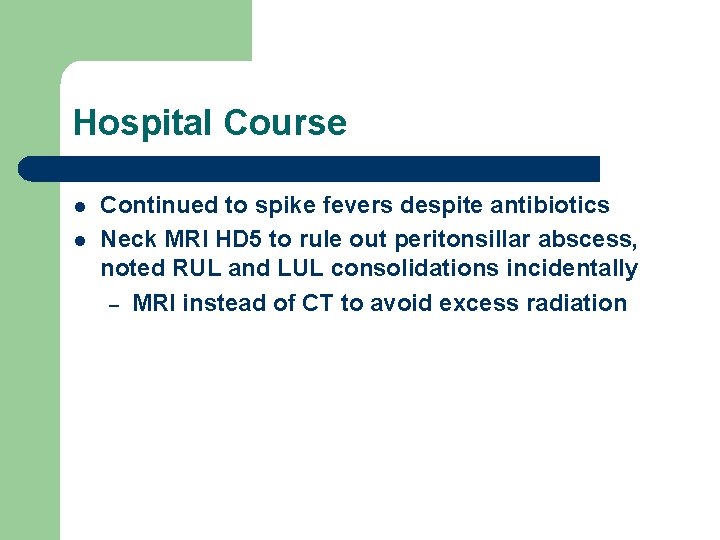
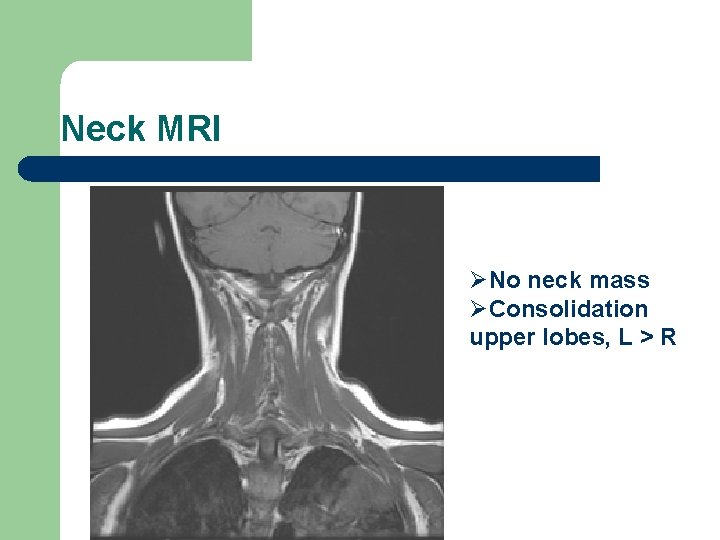
Hospital Course l l Continued to spike fevers despite antibiotics Neck MRI HD 5 to rule out peritonsillar abscess, noted RUL and LUL consolidations incidentally – MRI instead of CT to avoid excess radiation
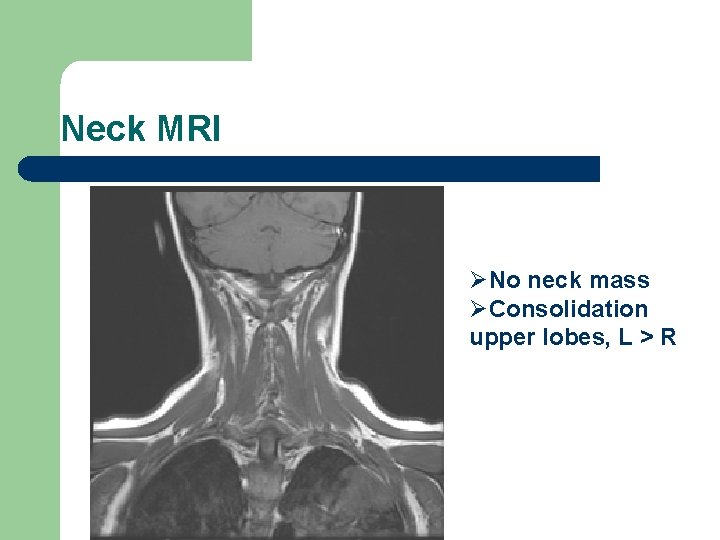
Neck MRI ØNo neck mass ØConsolidation upper lobes, L > R
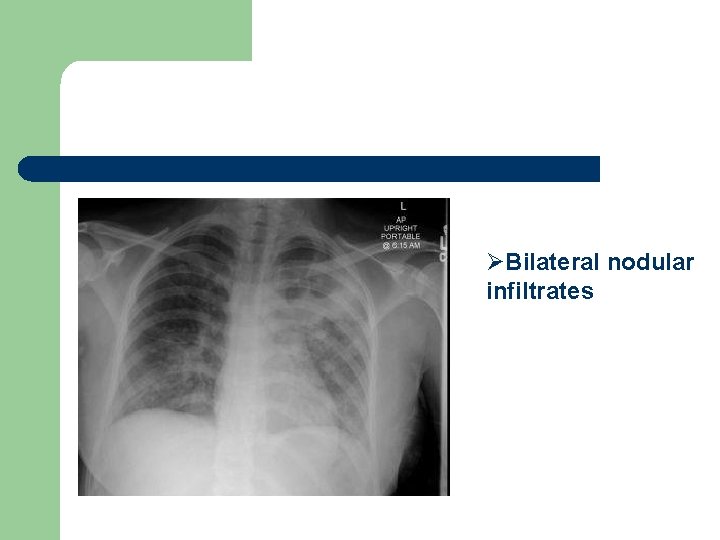
Respiratory distress ensues l l l l HD 6 desats to high 80 s, requiring O 2 (1. 5 L->3 L) Fevers to 40. 3 Chest “heavy” Lung exam: bibasilar inspiratory crackles WBC 5. 3 ID re-consulted for new infiltrates on cxr Blood, sputum, urine cx, CMV titers sent Vancomycin and Imipenem started
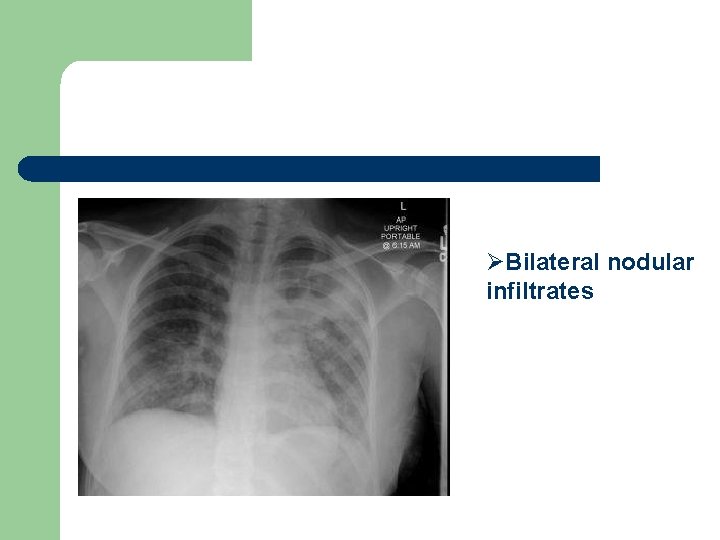
ØBilateral nodular infiltrates
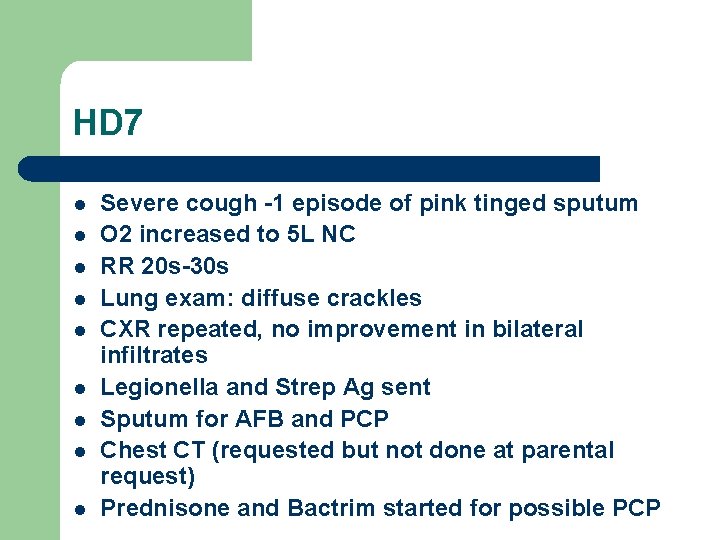
HD 7 l l l l l Severe cough -1 episode of pink tinged sputum O 2 increased to 5 L NC RR 20 s-30 s Lung exam: diffuse crackles CXR repeated, no improvement in bilateral infiltrates Legionella and Strep Ag sent Sputum for AFB and PCP Chest CT (requested but not done at parental request) Prednisone and Bactrim started for possible PCP
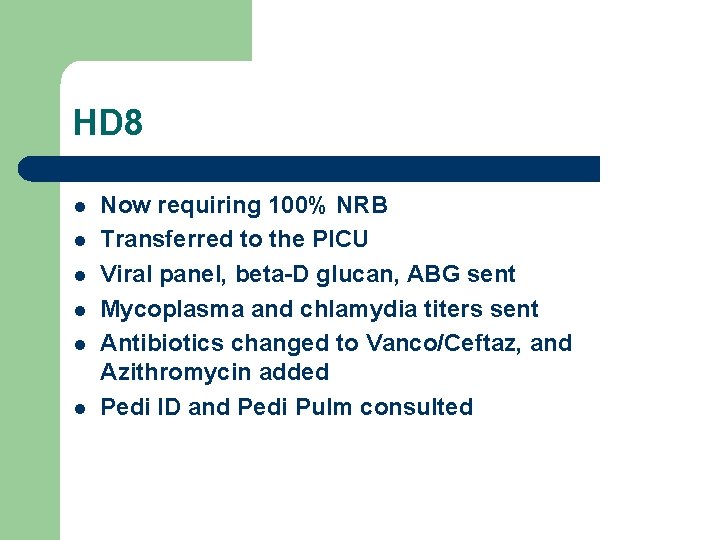
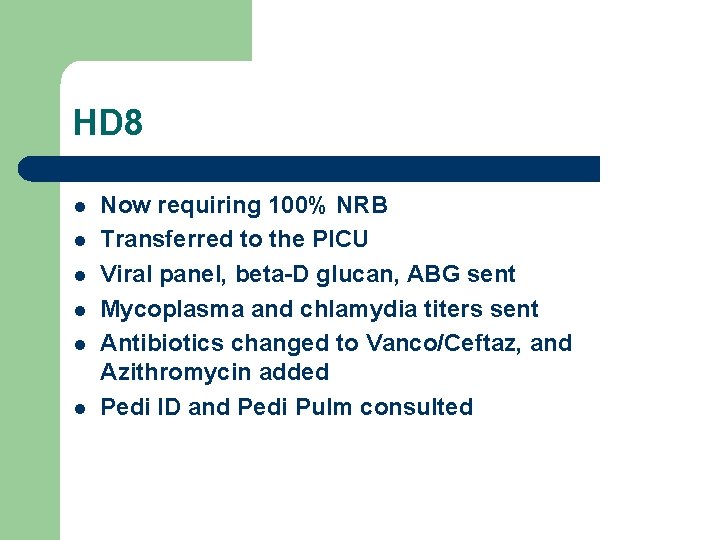
HD 8 l l l Now requiring 100% NRB Transferred to the PICU Viral panel, beta-D glucan, ABG sent Mycoplasma and chlamydia titers sent Antibiotics changed to Vanco/Ceftaz, and Azithromycin added Pedi ID and Pedi Pulm consulted

To review l 19 year old female with Crohn’s on Remicade initially admitted with fevers, arthralgias, cervical LAN on Kefzol with positive Group C Strep in pharynx, now with bilateral infiltrates, desats requiring a 100% non-rebreather mask not improving with broad-spectrum antibiotics.

Clinical Pearl Ø A patient on prolonged inhaled corticosteroids and broad spectrum antibiotics can be susceptible to invasive fungal infections – Our patient was not on inhaled steroids
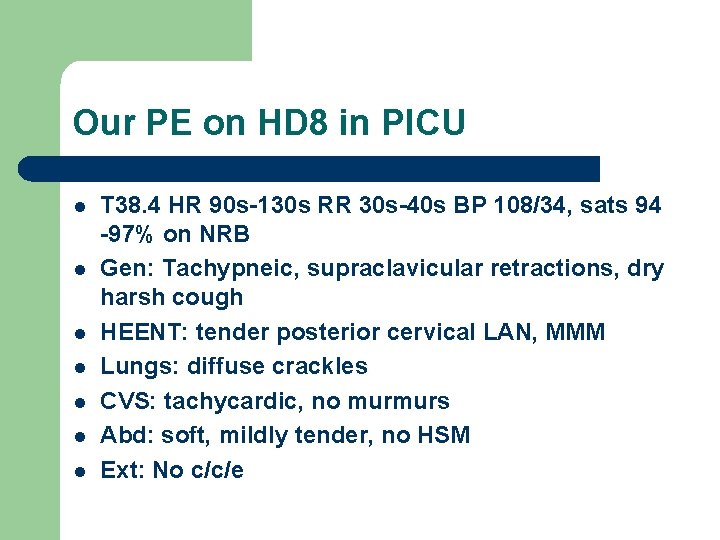
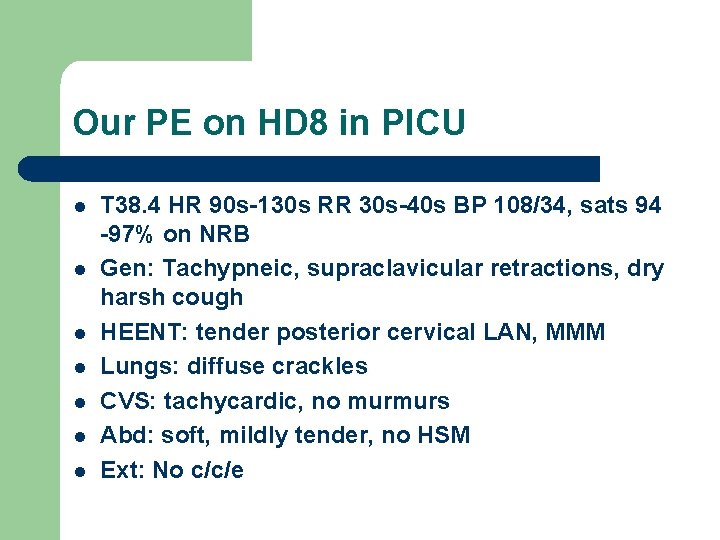
Our PE on HD 8 in PICU l l l l T 38. 4 HR 90 s-130 s RR 30 s-40 s BP 108/34, sats 94 -97% on NRB Gen: Tachypneic, supraclavicular retractions, dry harsh cough HEENT: tender posterior cervical LAN, MMM Lungs: diffuse crackles CVS: tachycardic, no murmurs Abd: soft, mildly tender, no HSM Ext: No c/c/e
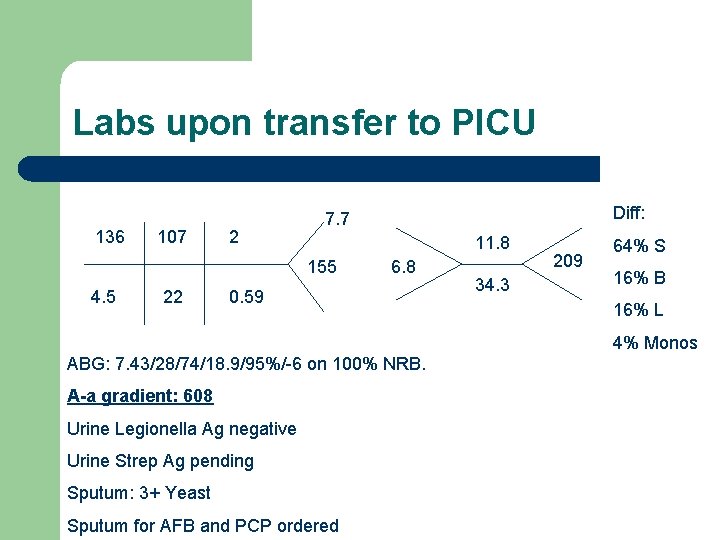
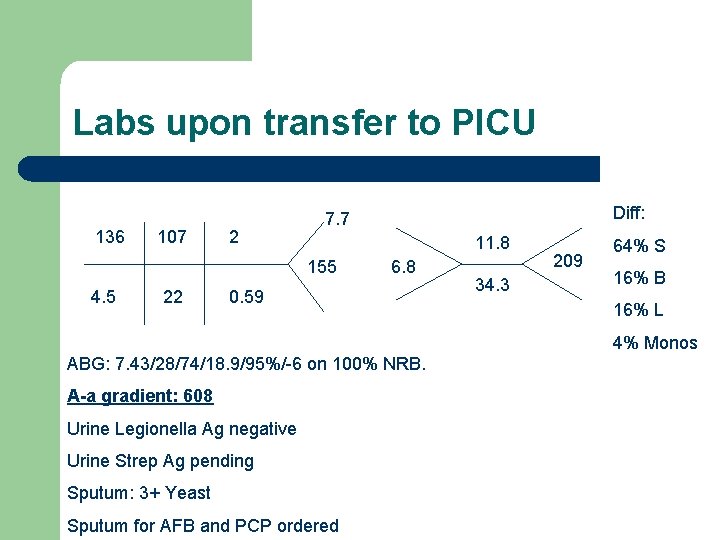
Labs upon transfer to PICU 136 107 2 11. 8 155 4. 5 22 Diff: 7. 7 6. 8 0. 59 34. 3 209 64% S 16% B 16% L 4% Monos ABG: 7. 43/28/74/18. 9/95%/-6 on 100% NRB. A-a gradient: 608 Urine Legionella Ag negative Urine Strep Ag pending Sputum: 3+ Yeast Sputum for AFB and PCP ordered

CXR ØInterstitial and alveolar infiltrates Pearl: ØWith this pattern on CXR – always think about mycoplasma infection
Differential for this 19 yo F with ARDS l l l Infectious Eosinophilic pneumonitis 2/2 Infliximab Extra-intestinal Crohn’s manifestation Pulmonary hemosiderosis Drug induced lupus
DDx-Infectious -Bacterial: on broad-spectrum antibiotics -Atypical bacterial: started on Azithro, Mycoplasma/Chlamydia titers sent -Viral: viral panel sent -Fungal: no exposures, sputum Cx sent -PCP: none seen on induced sputum -Tb: had negative PPD prior to Remicade and no exposures. PPD repeated, and AFB sent on induced sputum.
DDx-Eosinophilic pneumonitis l l l Case report of 33 yo M with Crohn’s on Remicade developing ARDS after 2 nd infusion. – 10 days after infusion developed dyspnea, fevers, found to have b/l interstitial infiltrates – Bronch: airway inflammation – Open lung biopsy: eosinophilic pneumonia – Improved with steroids Seemed less likely in our patient since her infusion was 4 weeks ago Wanted to avoid bronchoscopy and lung bx since she was starting to improve
DDx-Extra-intestinal Crohn’s l Also possible, but such an acute onset made infection seem more likely
DDx-Hemosiderosis l l l H/H remained stable Only 1 episode of mild hemoptysis Had negative Celiac workup last year
Hospital course, continued l l Continued on broad-spectrum antibiotics and Azithromycin P/F ratio improved to 130 from 71 on HD 9 Respiratory status improved, NRB was weaned to 60% and then to NC by HD 11 Discharged home HD 15, will follow-up in clinic
Lab Follow-up l l l l Viral panel negative Urine Ag (Legionella, Strep, and Histoplasma) negative AFB negative x 1 PCP negative x 1 Sputum cx: 3+ Candida Albicans Chlamydia Ab negative (pneumonia and psittaci) Beta-D glucan positive, but 82 (threshold is 80), so low positive Mycoplasma Ig. M positive

Mycoplasma and Crohn’s l l Increased prevalence of Mycoplasma pneumonia in intestinal biopsy specimens in Crohn’s (59. 2%) compared to UC (26. 3%) or non-IBD controls (37. 7%). Significance of this for our patient? – Could she develop post infectious BOOP? l Needs to be followed in clinic with spirometry and DLCO – Could take months before she reaches her new baseline
Further Questions l l Did the remicade contribute to the severity of the mycoplasma infection? l Should she continue Remicade infusions? Should all patients undergo pulmonary function testing prior to starting any drug with potential pulmonary complications?
References l l “Delayed hypersensitivity reaction and acute respiratory distress syndrome following infliximab infusion. ” Riegert. Johnson et al. Inflammatory Bowel Disease 2002 8(3) 186 -191. “High prevalence of mycoplasma pneumoniae in intestinal mucosal biopsies from patients with inflammatory bowel disease and controls. ” Chen et al. Digestive Diseases and Sciences. 2001. 2529 -35. “Mesalamine-Related Lung Disease: Clinical, Radiographic, and Pathologic Manifestations. ” Foster et al. Inflammatory Bowel Diseases 2003. 9(5) 308 -315. “Pentasa-induced Lung Injury. ” Presented 10/27/10 from NE Pedi Pulm Consortium website (www. Nepedipulm. com)
 Immunocompromised diseases list
Immunocompromised diseases list Jack in the box
Jack in the box Mycoplasma pneumoniae
Mycoplasma pneumoniae Rocky mountain fever
Rocky mountain fever Vagninitis
Vagninitis Swollen lymph nodes
Swollen lymph nodes Patient 2 patient
Patient 2 patient Present illness example
Present illness example History of present illness example nursing
History of present illness example nursing Pasal 163 is
Pasal 163 is Teori statuta adalah
Teori statuta adalah Bushco hpi
Bushco hpi Cc chief complaint
Cc chief complaint Pemakaian hukum asing adalah
Pemakaian hukum asing adalah Renvoi dalam hpi
Renvoi dalam hpi Contoh kasus renvoi
Contoh kasus renvoi Review of systems example
Review of systems example Perbedaan icrc dan ifrc
Perbedaan icrc dan ifrc Penyelundupan hukum hpi
Penyelundupan hukum hpi Ruang lingkup hpi
Ruang lingkup hpi Locates hpi
Locates hpi Hpi in medical terms
Hpi in medical terms Pqrst hpi
Pqrst hpi Hpi pmh
Hpi pmh Tb pneumonia
Tb pneumonia Pneumonia tipica e atipica
Pneumonia tipica e atipica Ap diameter of chest
Ap diameter of chest Nursing care plan for pneumonia
Nursing care plan for pneumonia Radiografia
Radiografia Copd medical abbreviation
Copd medical abbreviation Core measures for pneumonia
Core measures for pneumonia Hepatization
Hepatization Anatomical classification of pneumonia
Anatomical classification of pneumonia