Pulmonary Artery Pressure Monitoring 1 of 3 Central


























- Slides: 114
Pulmonary Artery Pressure Monitoring (1 of 3) ßCentral venous catheter passed through right atrium, right ventricle, past tricuspid valve, and into pulmonary artery ßAllows monitoring of: – Right ventricular function – Pulmonary vascular status – Left ventricular function (indirectly) PAP Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Pulmonary Artery Pressure Monitoring (2 of 3) ßSpecific parameters measured – CO – Right arterial pressure – Right ventricular pressure – Pulmonary artery wedge pressure (PAWP) PAP Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
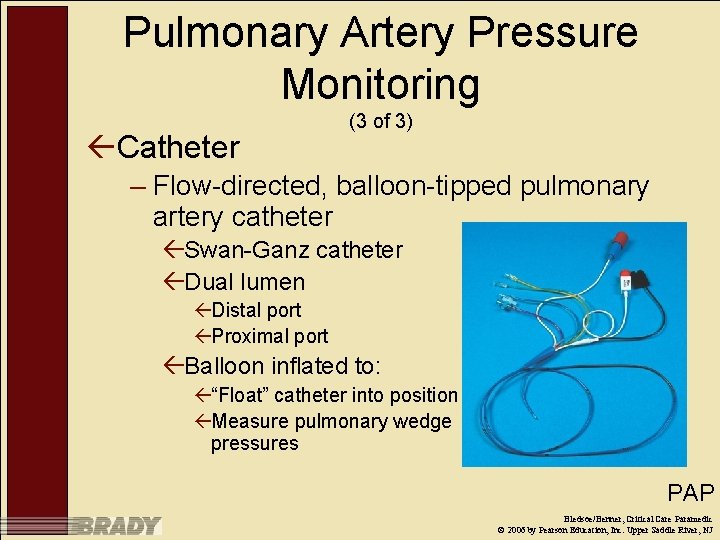
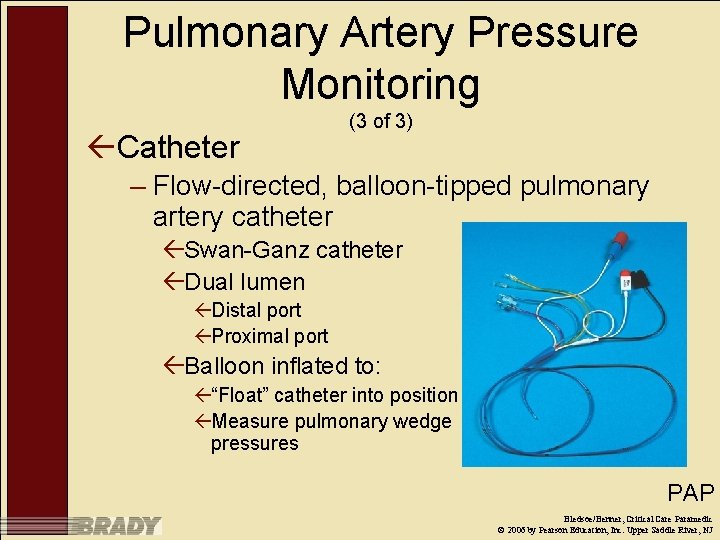
Pulmonary Artery Pressure Monitoring ßCatheter (3 of 3) – Flow-directed, balloon-tipped pulmonary artery catheter ßSwan-Ganz catheter ßDual lumen ßDistal port ßProximal port ßBalloon inflated to: ß“Float” catheter into position ßMeasure pulmonary wedge pressures PAP Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Waveform Interpretation ßPressure changes during systole and diastole ßWaveforms classified as: – Right atrial – Right ventricular – Pulmonary artery pressure – Pulmonary artery wedge pressure PAP Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Indications of PA Catheter Placement (1 of 2) ßDiagnosis of shock states and shock types ßDiagnosis of high-pressure versus lowpressure pulmonary edema ßAssessment of vascular tone ßAssessment of myocardial contractility, including determination of cardiac output ßAssessment of intravascular fluid balance Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ

Indications of PA Catheter Placement (2 of 2) ßAnalysis of mixed venous oxygen saturation ßMonitoring and management of complicated AMI ßAssessment of hemodynamic response to therapies ßManagement of hemodynamic instability after cardiac surgery Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ

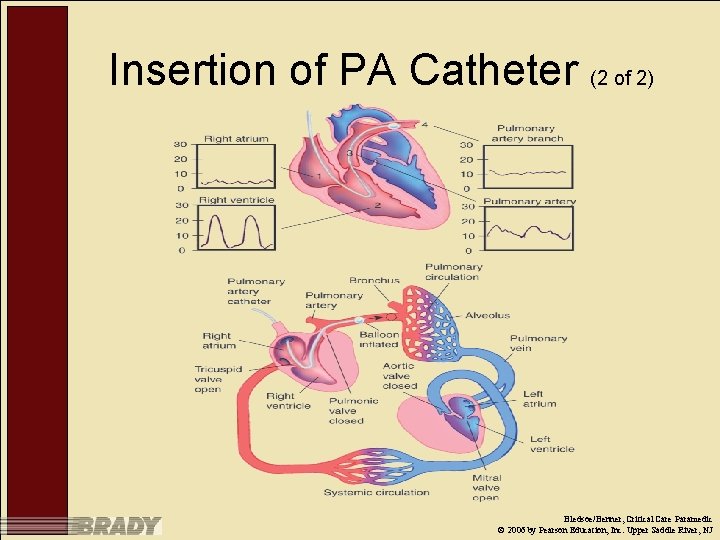
Insertion of PA Catheter (1 of 2) ßCatheter placed in vein ßCatheter fed into vein until distal tip in right atrium ßDistal balloon inflated with 1. 5 cc of air ßDistal tip “floated” through tricuspid, into right ventricle, through pulmonic valve, and into pulmonary artery ßBalloon allowed to “wedge” itself in branch of pulmonary artery Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
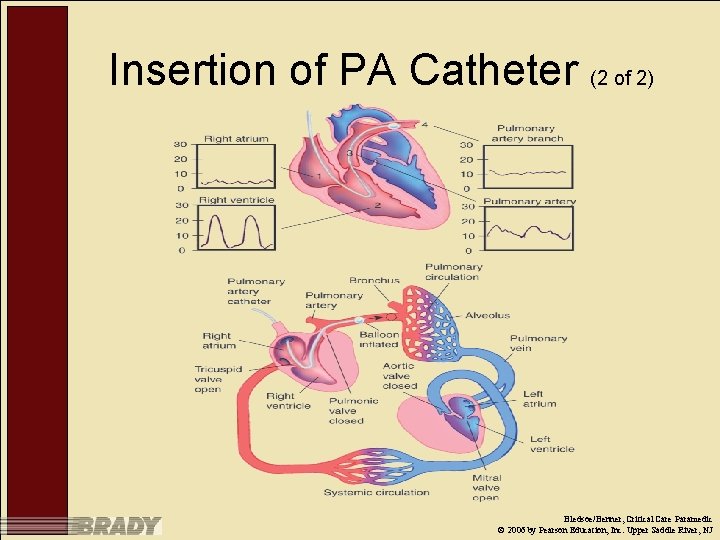
Insertion of PA Catheter (2 of 2) Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Right Atrial Pressure ßMean right atrial pressure – 8 mm. Hg Right Atrial Pressu Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Right Ventricular Pressure (1 of 2) ßRight-atrial end-diastolic pressure – 0– 8 mm. Hg – Equal to right atrial pressure when tricuspid valve opens Right Ventricular Press Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Right Ventricular Pressure (2 of 2) ßRight-atrial systolic pressure – 15– 30 mm. Hg – Opens pulmonic valve ßPropels blood into pulmonary artery – Higher-pressure chamber Right Ventricular Press Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ

Pulmonary Artery Pressure (2 of 4) ßSystolic – 15– 30 mm. Hg – Equal to right ventricular systolic pressure PAP Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Pulmonary Artery Pressure (3 of 4) ßDiastolic – 8– 15 mm. Hg – Reflects resistance of pulmonary vascular bed ßLeft-ventricular end-diastolic pressure also ßPA diastolic pressure is indirect measurement of left ventricular pressure PAP Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
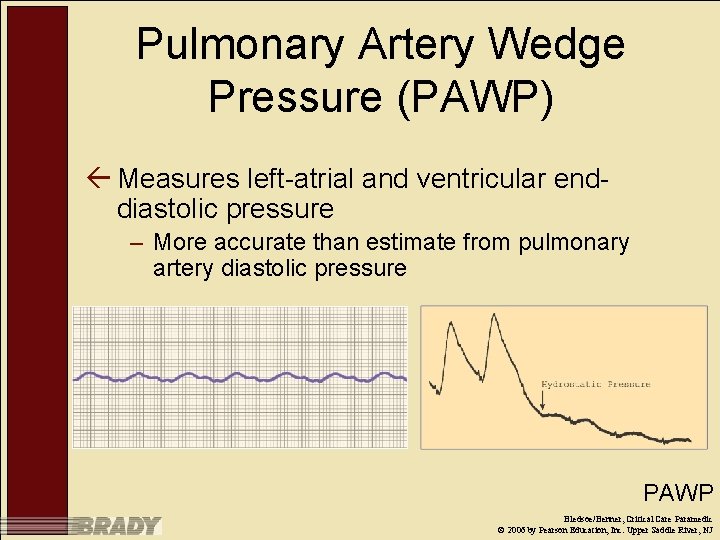
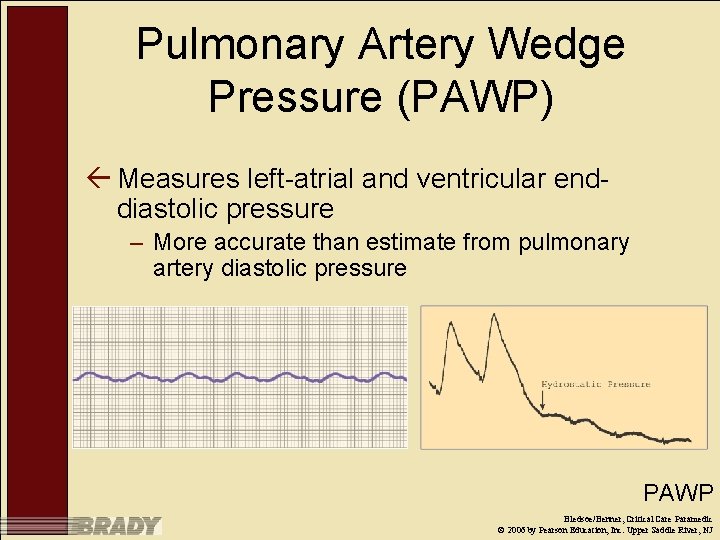
Pulmonary Artery Wedge Pressure (PAWP) ß Measures left-atrial and ventricular enddiastolic pressure – More accurate than estimate from pulmonary artery diastolic pressure PAWP Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
PAWP ß 8– 12 mm. Hg ß Catheter tip placed in pulmonary artery – In-place pulmonary artery catheter used – Balloon on distal tip inflated – Balloon advanced until it lodges in branch of pulmonary artery ß Forward blood flow stopped ß Static column of blood created ßBranch of artery ßPulmonary capillaries ßPulmonary vein ßLeft atrium ßOpen mitral valve ßDuring diastole ßLeft ventricle PAWP ß Balloon deflated after Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ measurements
Complications of PA Catheterization ßPulmonary injury – During needle puncture ßDysrhythmias ßInfection ßPulmonary artery rupture PAWP Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Preparation for Hemodynamic Monitoring ßPrime the flush system ßConnect the transducer to the monitor ßLeveling the transducer ßZero the pressure system to atmospheric pressure ßCalibrate the pressure system Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Intra-aortic Balloon Pump (IABP) (1 of 6) ß Augments weakened heart’s cardiac output ß Percutanous placement of balloon catheter in aorta – Insertion site: Femoral – Balloon placed about 2 cm distal to aortic arch Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Intra-Aortic Balloon Pump (IABP) (1 of 3) ß Provides mechanical circulatory support for failing heart ß Catheter – 30 -cm balloon on distal end ß Balloons sized according to height – Placed in aorta distal to left of subclavian artery – Inserted in femoral artery – During operation, rapidly inflated and deflated with 35– 40 ml of helium IABP Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
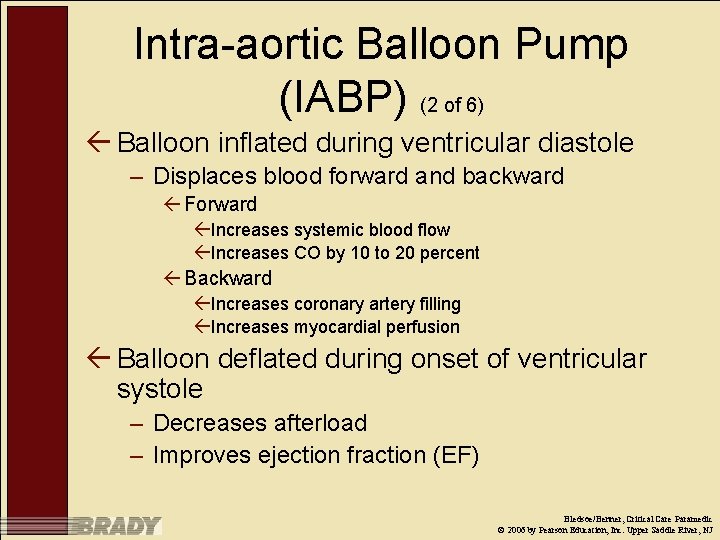
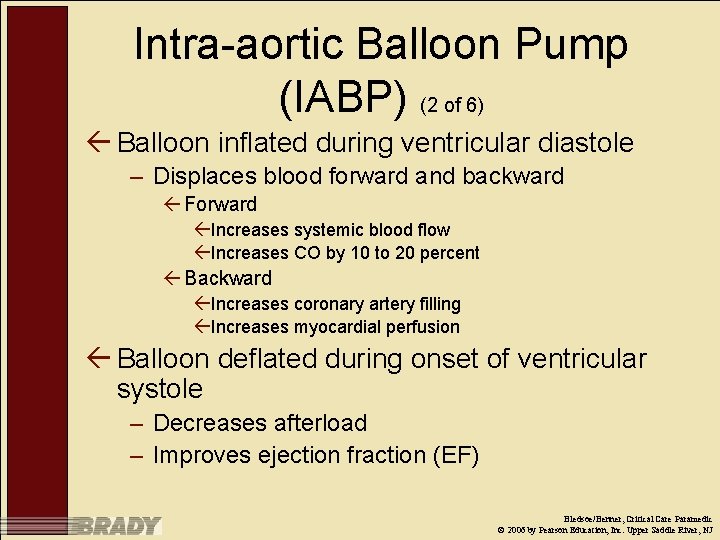
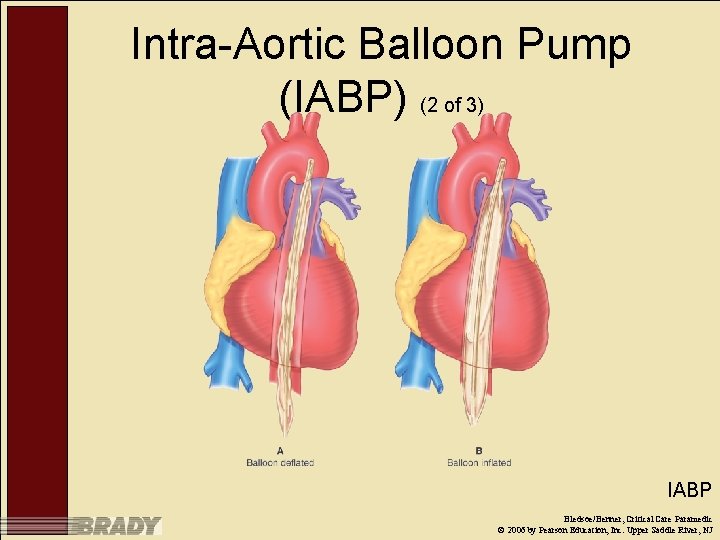
Intra-aortic Balloon Pump (IABP) (2 of 6) ß Balloon inflated during ventricular diastole – Displaces blood forward and backward ß Forward ßIncreases systemic blood flow ßIncreases CO by 10 to 20 percent ß Backward ßIncreases coronary artery filling ßIncreases myocardial perfusion ß Balloon deflated during onset of ventricular systole – Decreases afterload – Improves ejection fraction (EF) Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
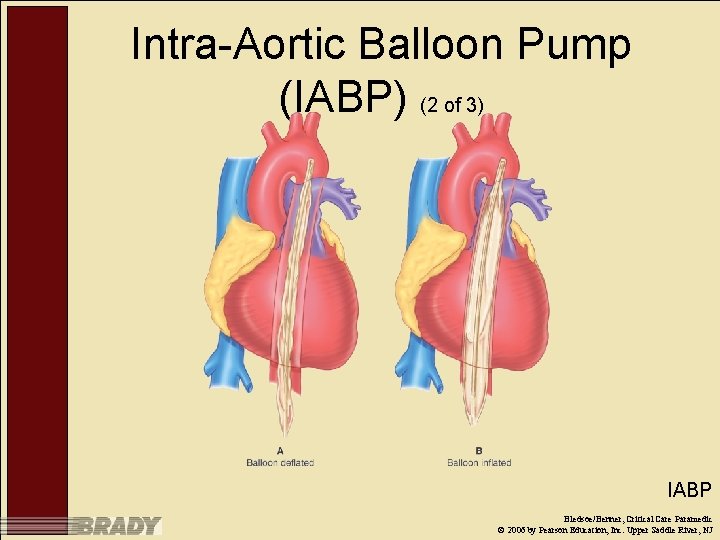
Intra-Aortic Balloon Pump (IABP) (2 of 3) IABP Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Indications for IABP Therapy ßCardiogenic shock ßLeft ventricular failure ßDrug-induced cardiovascular failure ßSeptic shock ßCardiac surgery preparation IABP Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
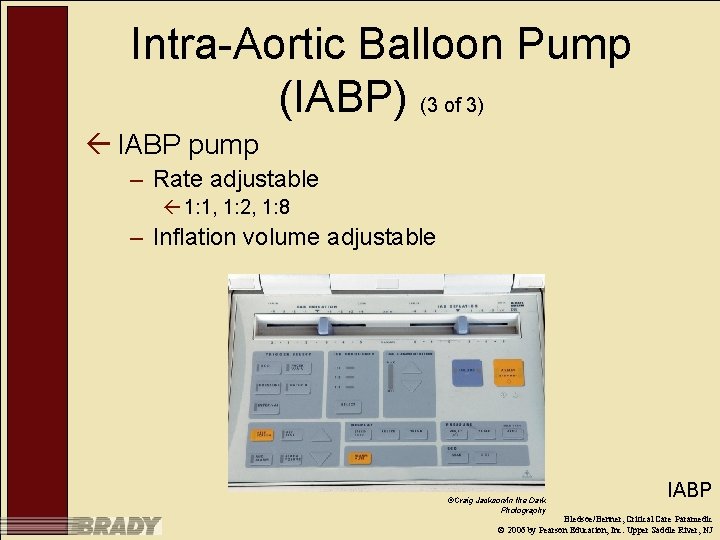
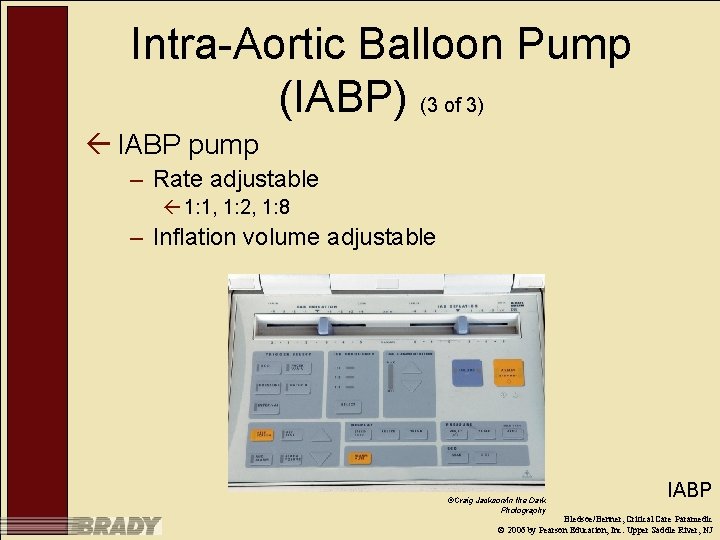
Intra-Aortic Balloon Pump (IABP) (3 of 3) ß IABP pump – Rate adjustable ß 1: 1, 1: 2, 1: 8 – Inflation volume adjustable ©Craig Jackson/In the Dark Photography IABP Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ

Intra-aortic Balloon Pump (IABP) (3 of 6) ß Transport management of patient on IABP includes: – Evaluating patient response to treatment in terms of: ß Hemodynamic status ß Dysrhythmia control ß Systemic perfusion ß Relief of symptoms of cardiac ischemia Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ

Intra-aortic Balloon Pump (IABP) (4 of 6) ß Transport management of patient on IABP includes: – Observing such early signs of complications from IABP therapy as: ß Limb ischemia ß Bleeding ß Infection ß Thrombus formation ß Displacement of balloon catheter ß Arterial damage Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Intra-aortic Balloon Pump (IABP) (5 of 6) ß Ensure proper IABP functioning, including: – – Correct timing Consistent triggering Appropriate troubleshooting of all alarm situations Safe operation Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ

Intra-aortic Balloon Pump (IABP) (6 of 6) ß Air medical transport considerations ß Hypobaric environment can impeded IABP functioning – Volume decreases on ascent – Volume decreases on descent ß IABP must be reprimed – During ascent – At altitude – During descent Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
IABP Contraindications ßGross aortic insufficiency ßPeripheral vascular disease with poor femorals ßIrreversible brain damage ßChronic end state heart disease ßDissecting aortic or thoracic aneurysms ßPeripheral vascular disease IABP Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Side Effects and Complications ß Limb ischemia ß Bleeding at insertion site ß Thrombocytopenia ß Immobility of balloon catheter ß Balloon leak or rupture – Helium embolization – Thrombus formation ß Infection ß Aortic dissection ß Compartment syndrome IABP Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Summary ßCritical care paramedics will most likely not be required to establish/insert hemodynamic monitoring catheters – Must be familiar with insertion technique, however ßMust be prepared to: – Interpret data – Use data in differential diagnosis and treatment decisions ßManage complications of devices Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Shock Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Introduction to Shock (1 of 2) ß Shock is often unrecognized in early stages – Clinical signs and symptoms can vary – Clinical signs and symptoms can be subtle – Many different presentations ß Shock is not a primary diagnosis – Physiologic adaptation to an insult – Body is attempting to preserve vital functions Shock is a “rude unhinging of the machinery of life” Samuel Gross, 1862 Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ

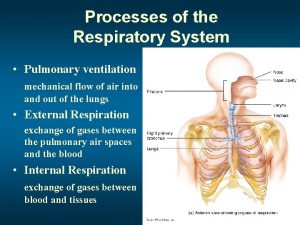
Introduction to Shock (2 of 2) ß Shock results from changes in: – Circulating volume – Cardiac function – Peripheral vascular resistance ß Shock can cause changes in organ systems – – Cardiovascular Respiratory Renal Gastrointestinal ß Classified in stages – Compensatory – Progressive – Irreversible Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Shock Defined ßLocal or systemic hypoperfusion resulting in an inability to meet cellular demands – Can affect tissue, organs, or organ systems – Can result from insult to: ßHeart ßLungs ßBlood vessels ßBlood ßNervous system Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ

Compensatory Mechanisms ßCounter effects of shock state ßInability to correct insult may lead to death Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ

Cell Physiology C 6 H 12 O 6 + 6 O 2 >> 6 CO 2 + 6 H 2 O Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
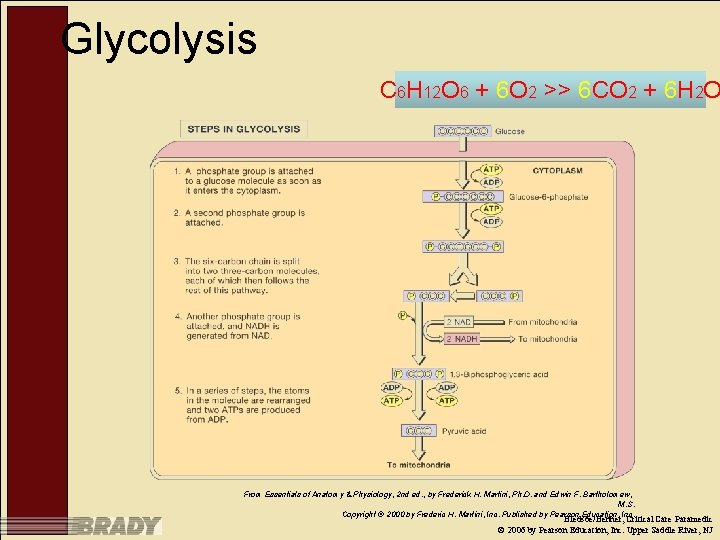
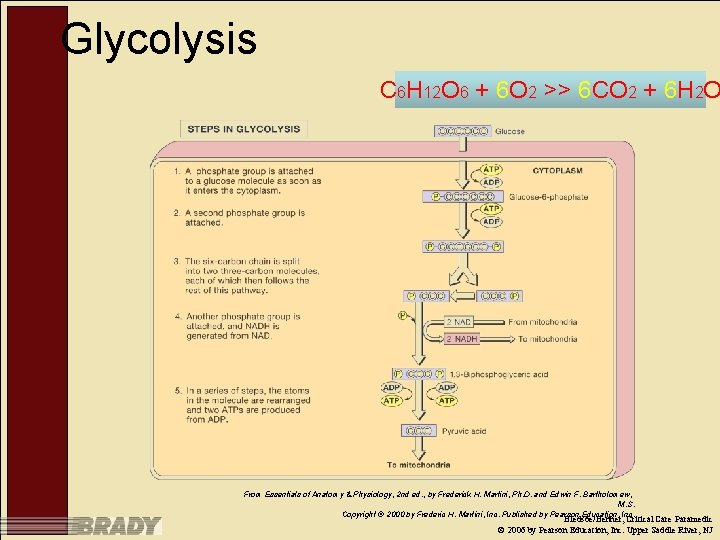
Glycolysis C 6 H 12 O 6 + 6 O 2 >> 6 CO 2 + 6 H 2 O From Essentials of Anatomy & Physiology, 2 nd ed. , by Frederick H. Martini, Ph. D. and Edwin F. Bartholomew, M. S. Copyright © 2000 by Frederic H. Martini, Inc. Published by Pearson Education, Inc. Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
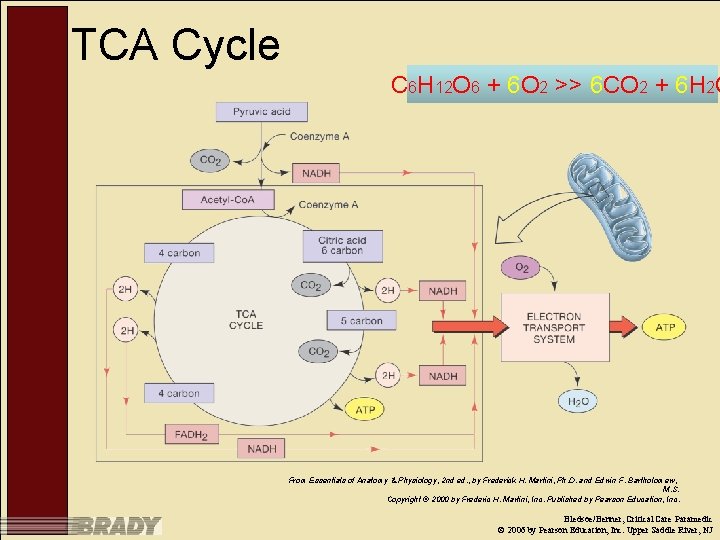
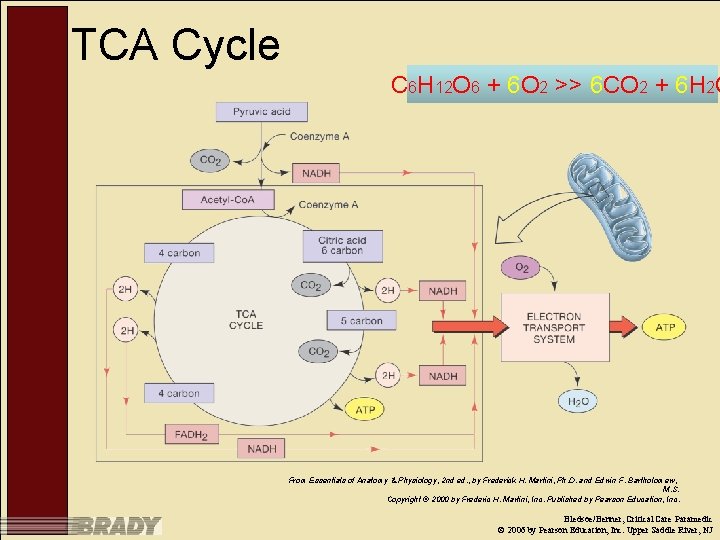
TCA Cycle C 6 H 12 O 6 + 6 O 2 >> 6 CO 2 + 6 H 2 O From Essentials of Anatomy & Physiology, 2 nd ed. , by Frederick H. Martini, Ph. D. and Edwin F. Bartholomew, M. S. Copyright © 2000 by Frederic H. Martini, Inc. Published by Pearson Education, Inc. Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Pathophysiology Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
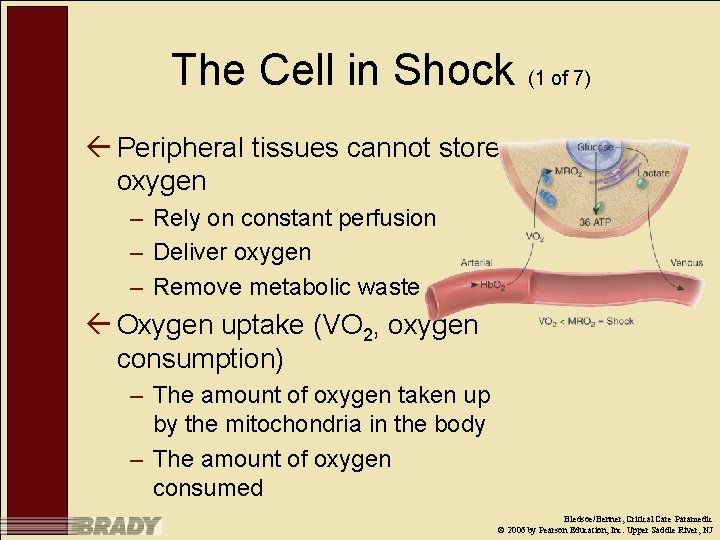
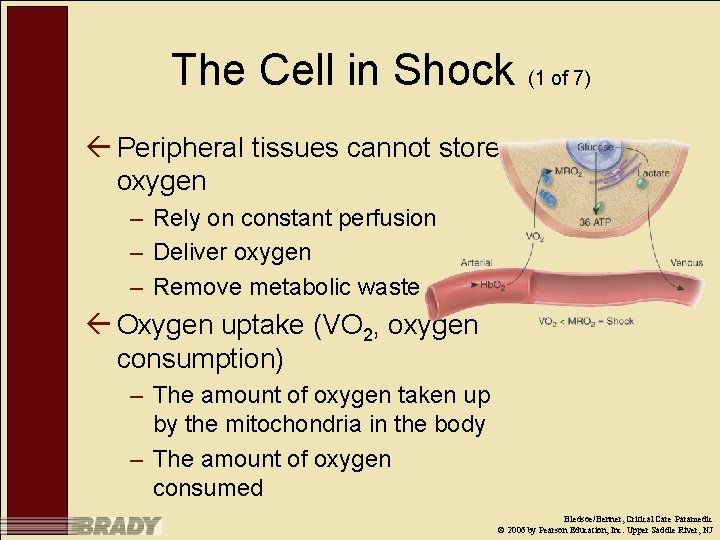
The Cell in Shock (1 of 7) ß Peripheral tissues cannot store oxygen – Rely on constant perfusion – Deliver oxygen – Remove metabolic waste ß Oxygen uptake (VO 2, oxygen consumption) – The amount of oxygen taken up by the mitochondria in the body – The amount of oxygen consumed Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ

The Cell in Shock (2 of 7) ß Metabolic requirement for oxygen (MRO 2) – Rate at which oxygen is metabolized to water in the mitochondria – Water is byproduct of the TCA (Krebs) cycle Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
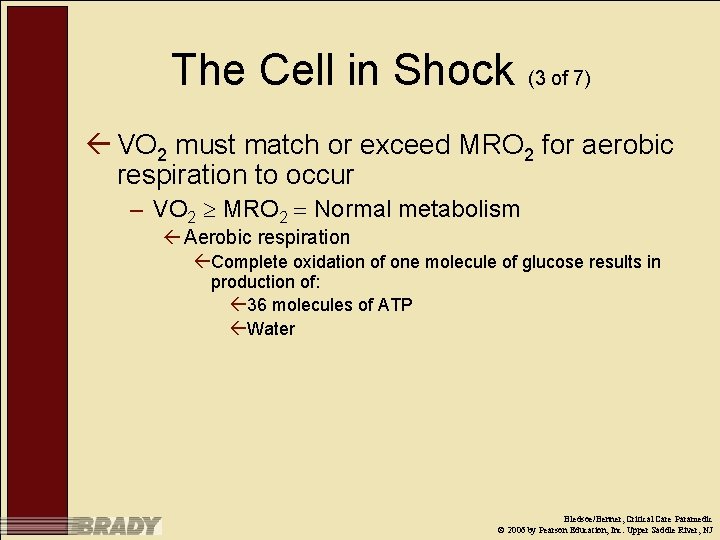
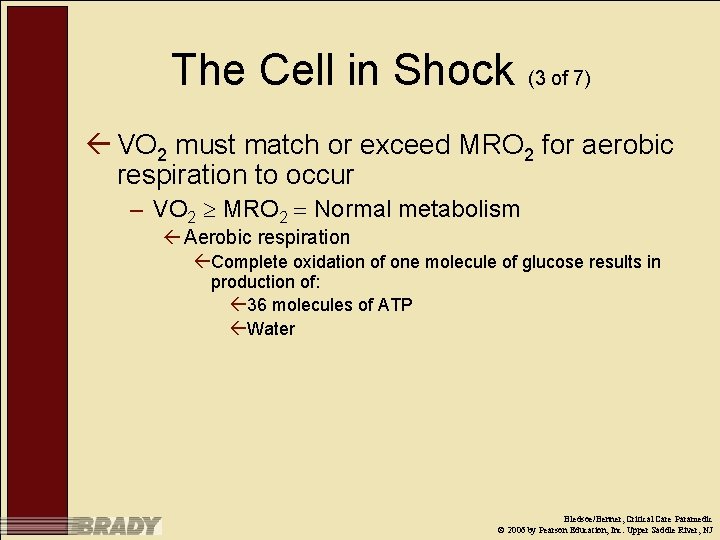
The Cell in Shock (3 of 7) ß VO 2 must match or exceed MRO 2 for aerobic respiration to occur – VO 2 MRO 2 Normal metabolism ß Aerobic respiration ßComplete oxidation of one molecule of glucose results in production of: ß 36 molecules of ATP ßWater Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ

The Cell in Shock (4 of 7) ß When VO 2 falls below MRO 2, anaerobic metabolism occurs – Oxygen uptake fails to meet metabolic demand for oxygen – VO 2 MRO 2 anaerobic metabolism ß Anaerobic respiration results in production of: ßTwo molecules of ATP ßPyruvic acid converted to lactic acid Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
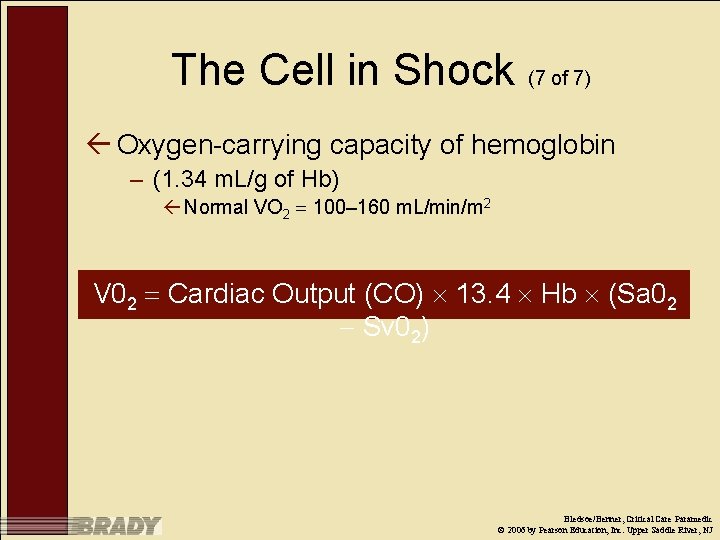
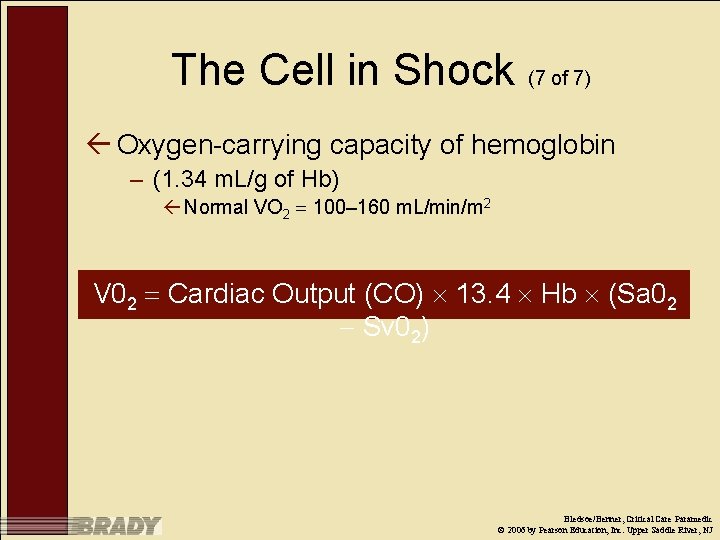
The Cell in Shock (7 of 7) ß Oxygen-carrying capacity of hemoglobin – (1. 34 m. L/g of Hb) ß Normal VO 2 100– 160 m. L/min/m 2 V 02 Cardiac Output (CO) 13. 4 Hb (Sa 02 Sv 02) Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Precursors to Shock ßInadequate CO ßInadequate Hb concentration or oxygencarrying capacity ßInadequate arterial oxygen saturation Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
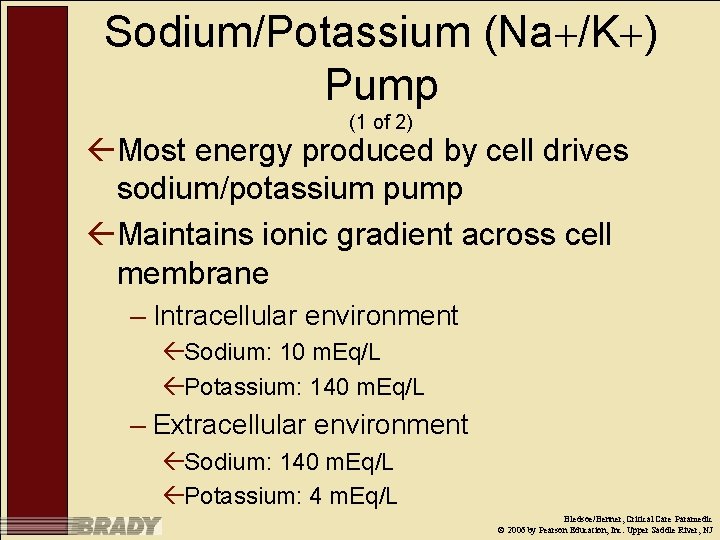
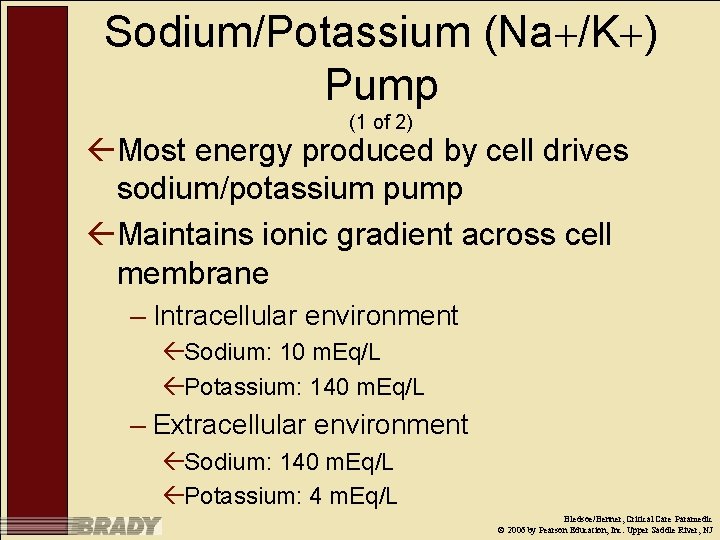
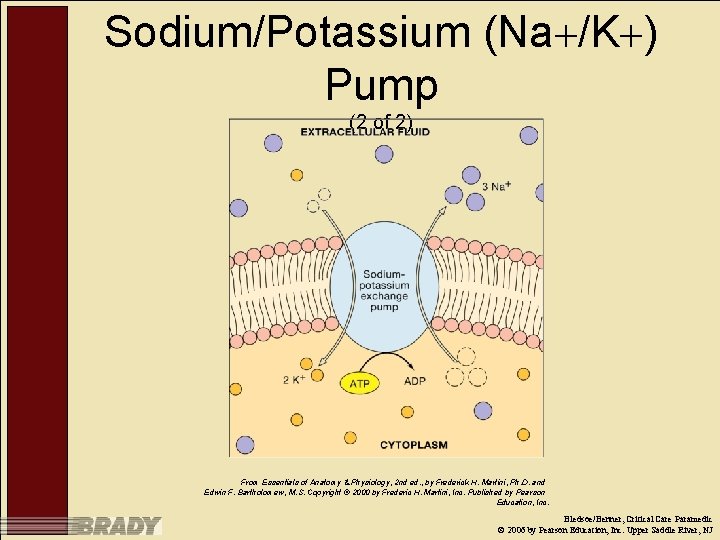
Sodium/Potassium (Na /K ) Pump (1 of 2) ßMost energy produced by cell drives sodium/potassium pump ßMaintains ionic gradient across cell membrane – Intracellular environment ßSodium: 10 m. Eq/L ßPotassium: 140 m. Eq/L – Extracellular environment ßSodium: 140 m. Eq/L ßPotassium: 4 m. Eq/L Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
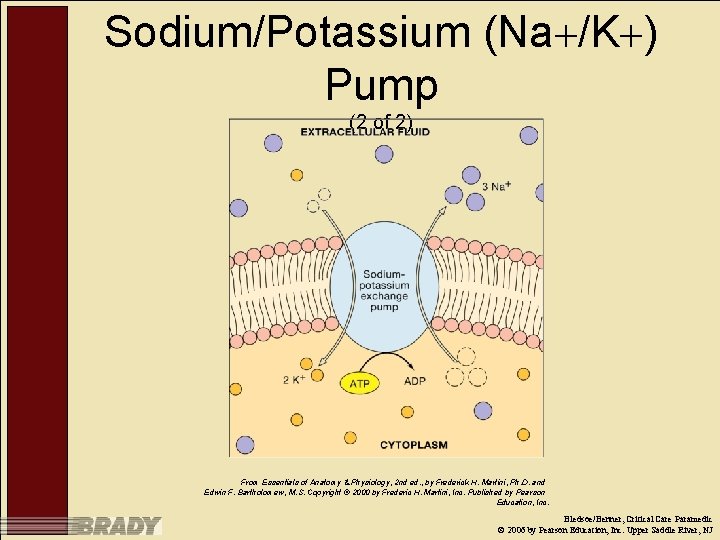
Sodium/Potassium (Na /K ) Pump (2 of 2) From Essentials of Anatomy & Physiology, 2 nd ed. , by Frederick H. Martini, Ph. D. and Edwin F. Bartholomew, M. S. Copyright © 2000 by Frederic H. Martini, Inc. Published by Pearson Education, Inc. Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ

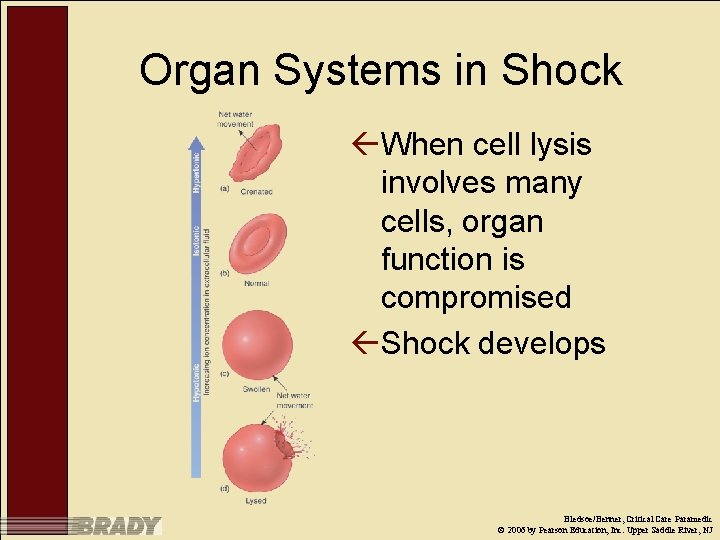
Sodium/Potassium Pump Dysfunction ßLack of ATP production in anaerobic metabolism results in failure of the Na /K pump – Sodium moves to the intracellular environment ßOsmotic shift of water into cell – Swelling – Lysis ßClinically significant organ damage may occur Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
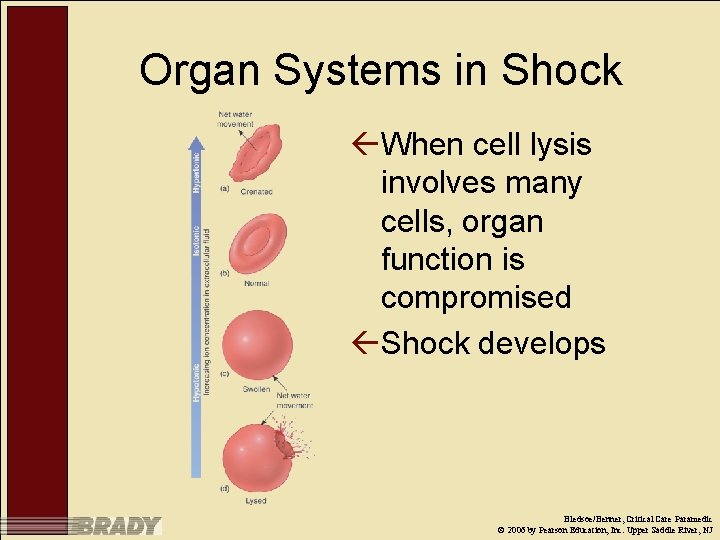
Organ Systems in Shock ßWhen cell lysis involves many cells, organ function is compromised ßShock develops Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ

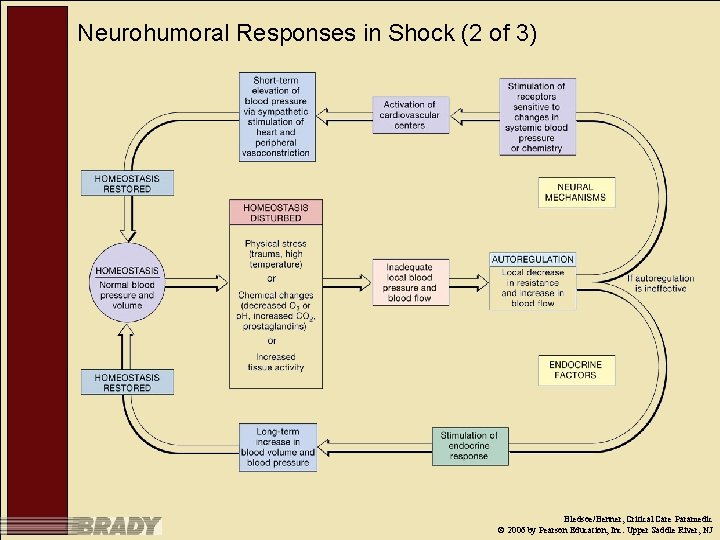
Neurohumoral Responses in Shock (1 of 3) ßOverall effects termed compensatory mechanisms – Increased heart rate – Increased myocardial contractility – Increased peripheral vasoconstriction – Renal retention of salt and water to maintain plasma volume – Assembling of metabolic fuels Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
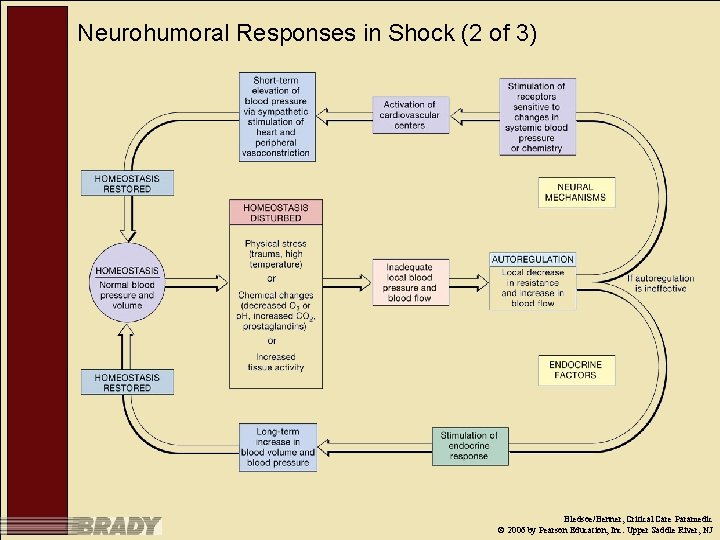
Neurohumoral Responses in Shock (2 of 3) Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Neurohumoral Responses in Shock (3 of 3) ßCompensatory mechanisms can only be tolerated for a short period due to: – Myocardial stress – Decreased blood flow to nonvital organs ßIschemia ßLactic-acid production and accumulation (metabolic acidosis) Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ

Symptoms of Shock Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ

Neurohumoral Agents and Effects Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
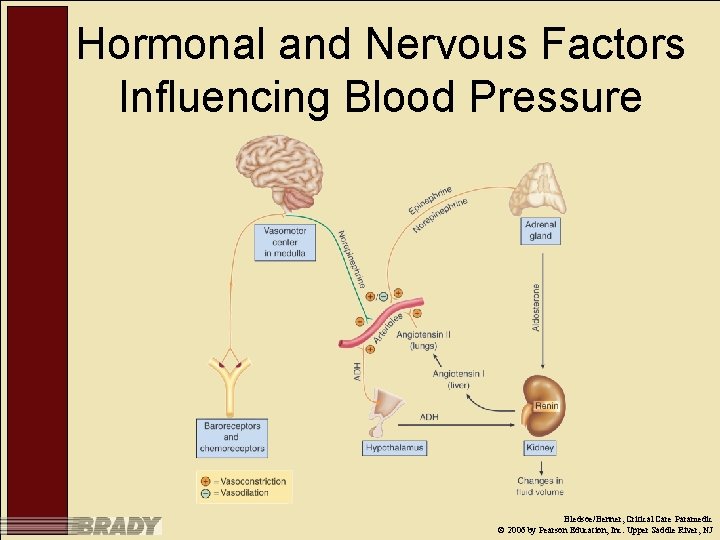
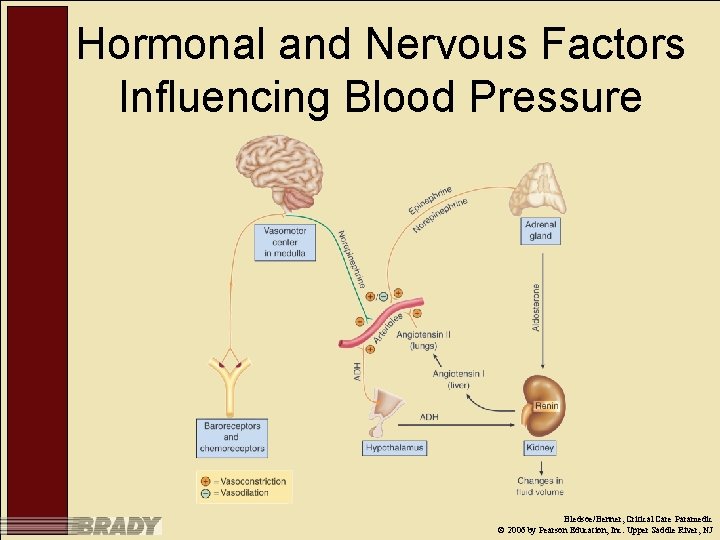
Hormonal and Nervous Factors Influencing Blood Pressure Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
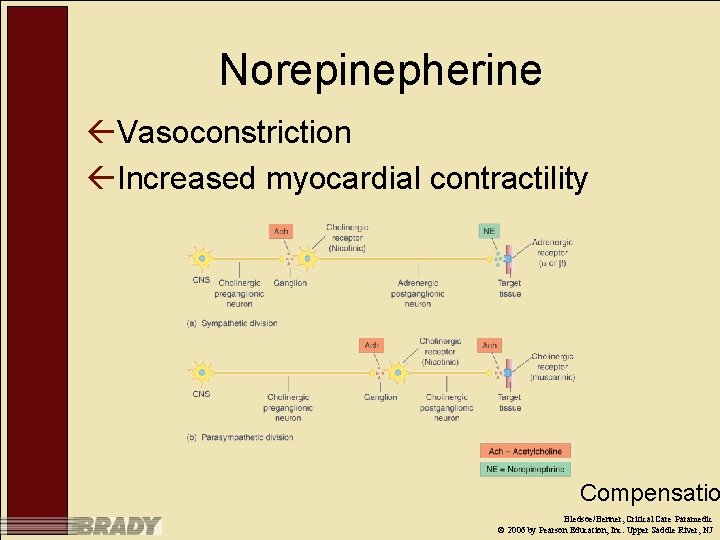
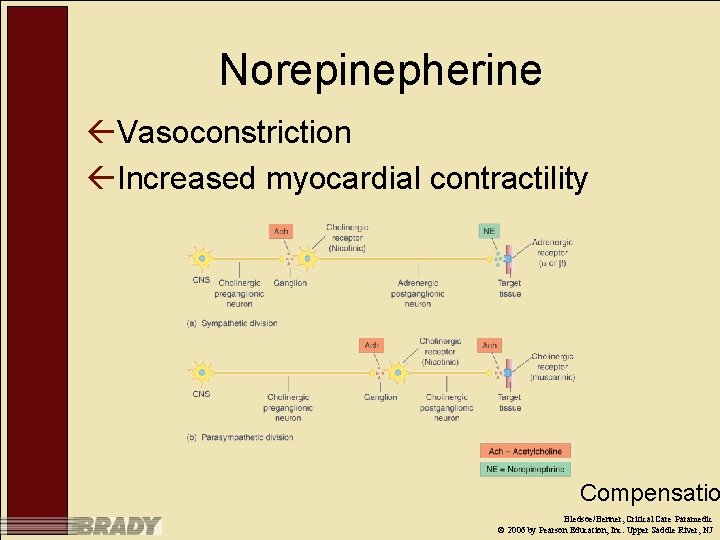
Norepinepherine ßVasoconstriction ßIncreased myocardial contractility Compensatio Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ

Epinephrine ßIncreased heart rate ßIncreased myocardial contractility Compensatio Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
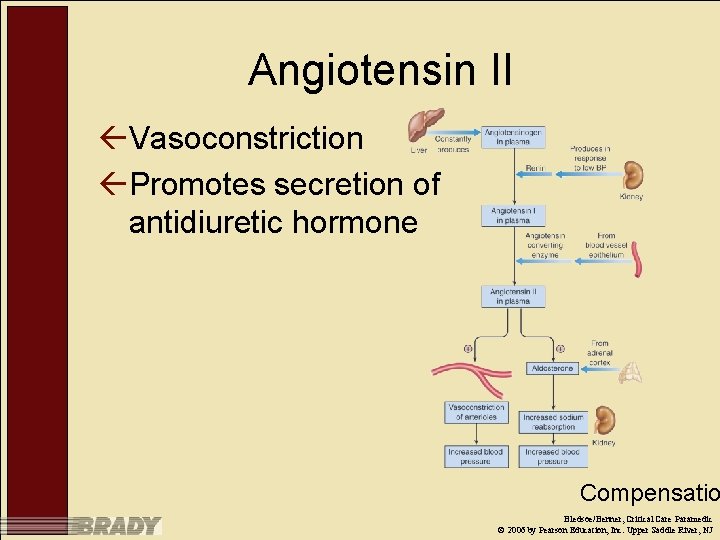
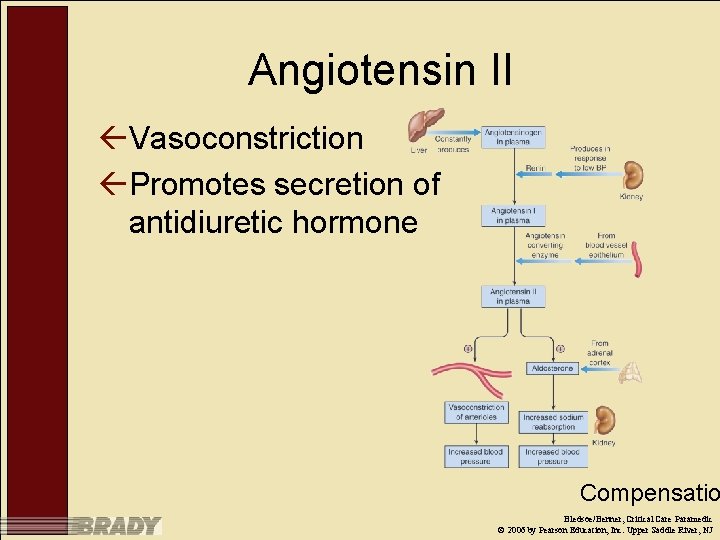
Angiotensin II ßVasoconstriction ßPromotes secretion of antidiuretic hormone Compensatio Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
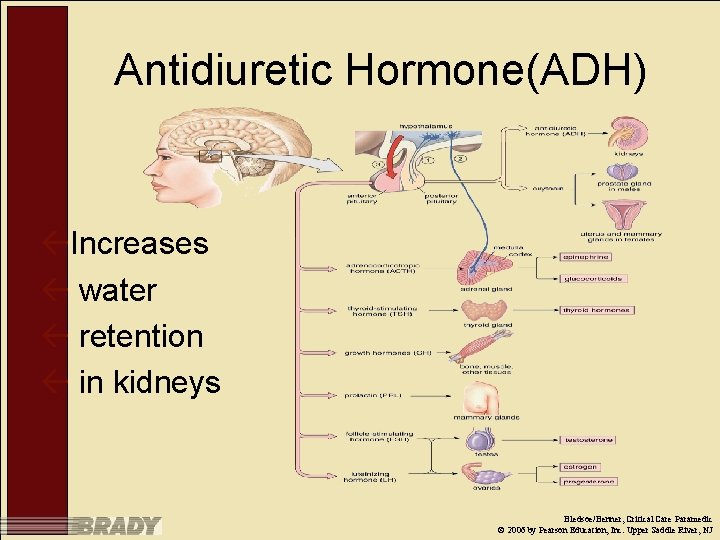
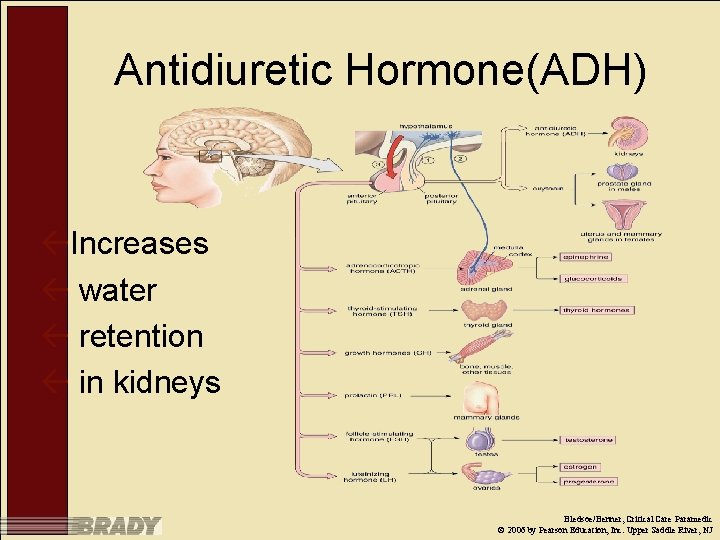
Antidiuretic Hormone(ADH) ßIncreases ß water ß retention ß in kidneys Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
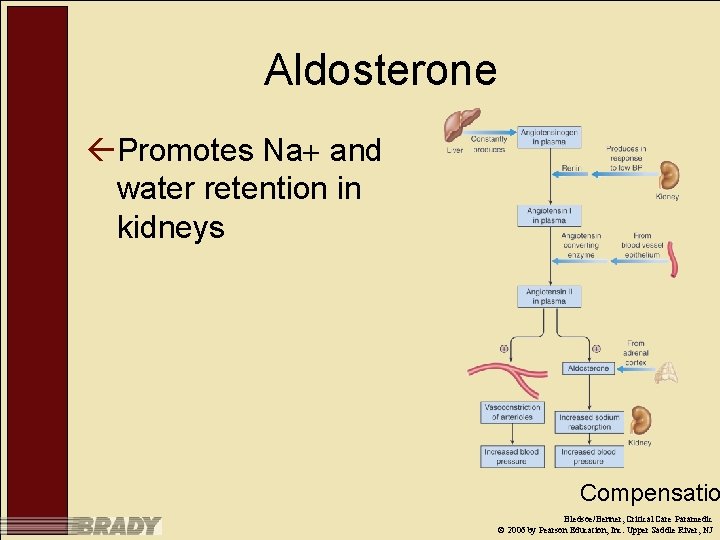
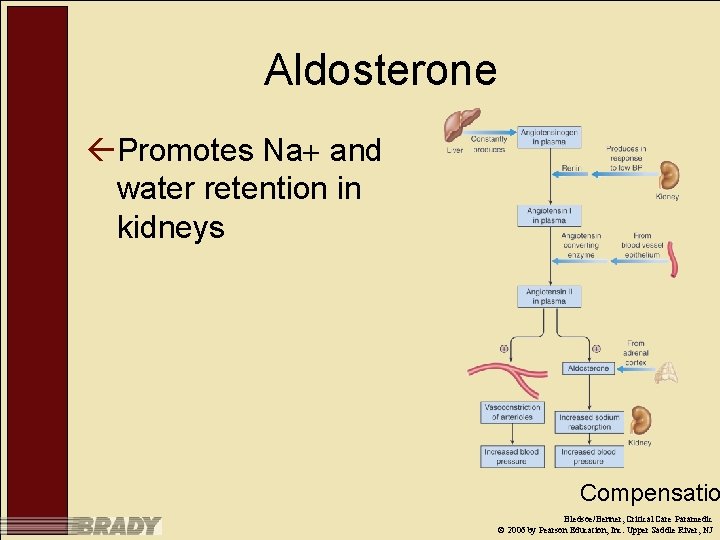
Aldosterone ßPromotes Na and water retention in kidneys Compensatio Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Cortisol ßSuppresses immune and inflammatory response ßPromotes protein catabolism ßIncreases blood glucose Compensatio Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ

Stages of Shock Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
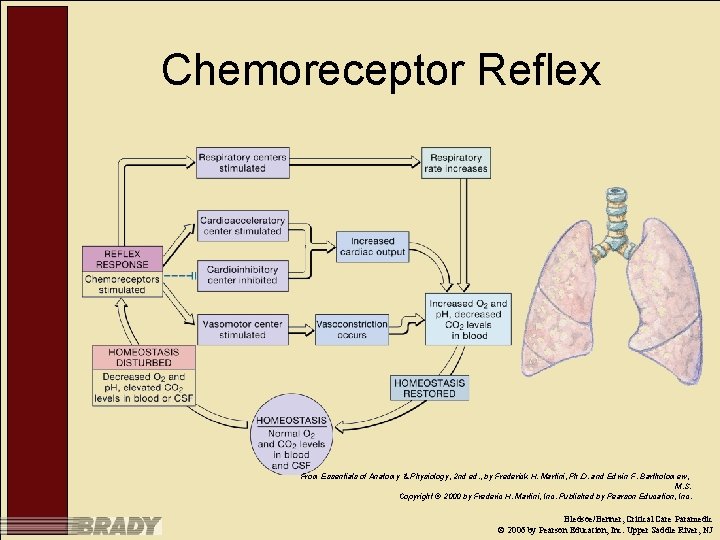
Compensated Shock ßBody able to detect decrease in CO – Baroreceptors – Chemoreceptors Stages of Shoc Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
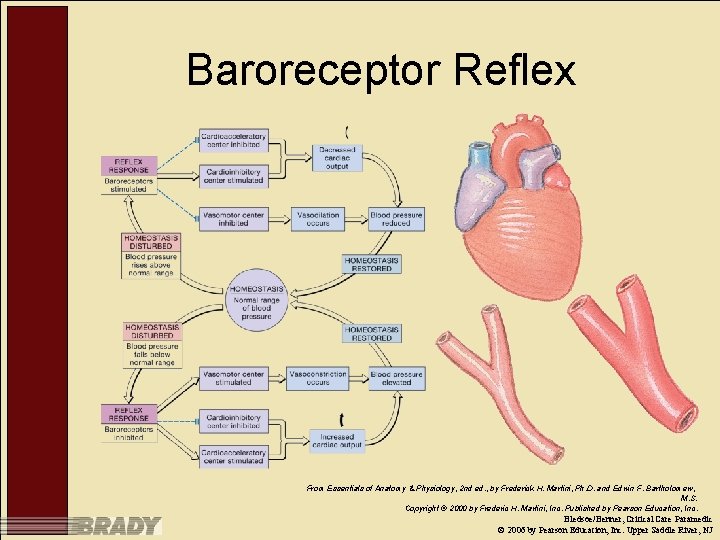
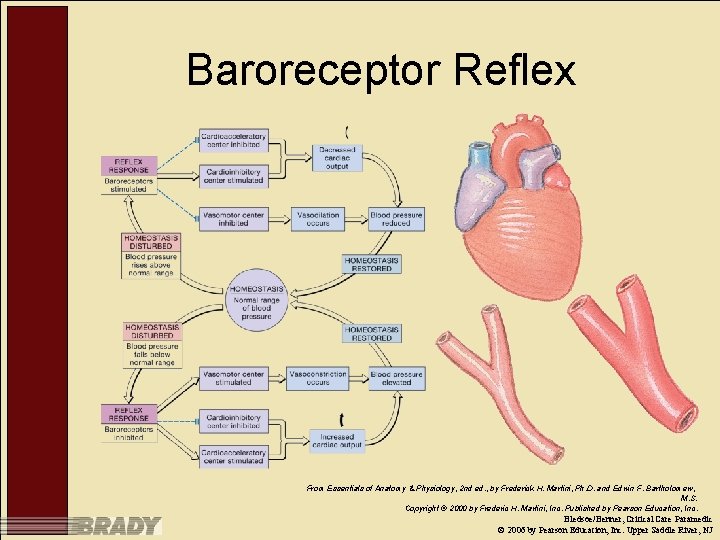
Baroreceptor Reflex From Essentials of Anatomy & Physiology, 2 nd ed. , by Frederick H. Martini, Ph. D. and Edwin F. Bartholomew, M. S. Copyright © 2000 by Frederic H. Martini, Inc. Published by Pearson Education, Inc. Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
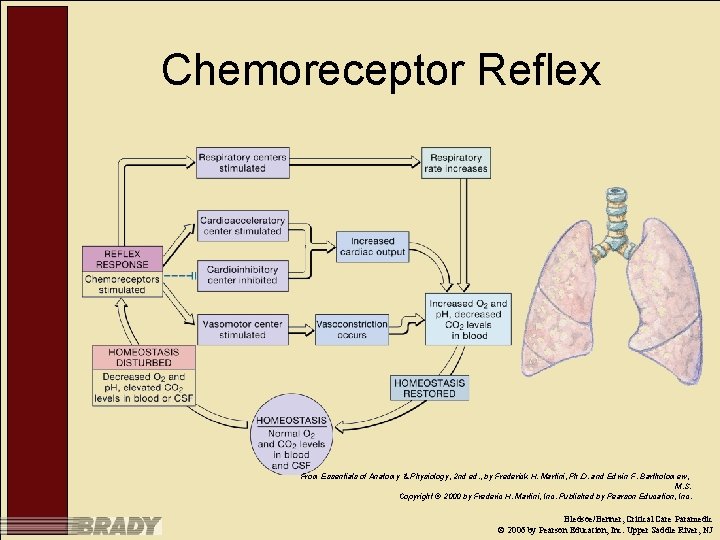
Chemoreceptor Reflex From Essentials of Anatomy & Physiology, 2 nd ed. , by Frederick H. Martini, Ph. D. and Edwin F. Bartholomew, M. S. Copyright © 2000 by Frederic H. Martini, Inc. Published by Pearson Education, Inc. Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Compensated Shock ßBody able to compensate for decrease in CO – Compensatory mechanisms activated ßIncreased peripheral vasoconstriction ßIncreased heart rate ßIncreased myocardial contractility – Maintenance of blood pressure – If insult not recognized and corrected, will proceed to progressive stage of shock Stages of Shoc Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Progressive Shock ßAnaerobic metabolism, tissue hypoxia appreciated ßAdditional compensatory mechanisms activated – Water retention in kidney – Profound vasoconstriction – Increased heart rate – Increased myocardial contractility Stages of Shoc Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Decompensated Shock ßCellular death – Can occur suddenly or over days ßPrognosis poor Stages of Shoc Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
General Management of Shock ß Correct the underlying problem ß Provide supportive care while attempting to identify the insult – Airway ß Ensure patency – Breathing ß Adequate ventilation, oxygenation – Circulation ß Ensure adequate tissue perfusion ßVolume resuscitation ßVasoactive medications – Correct acid-base abnormalities – Conserve body temperature Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ

Initial Assessment and Management ßSame as any other critically ill patient ßGoal is to identify and treat any potentially life-threatening injuries Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
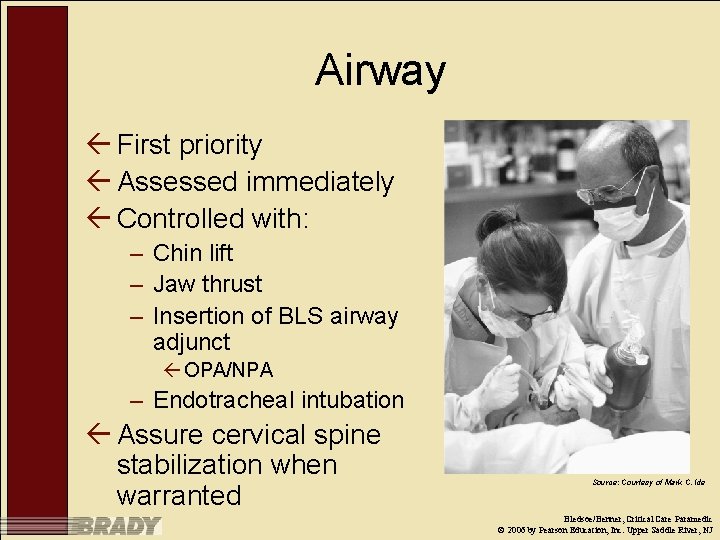
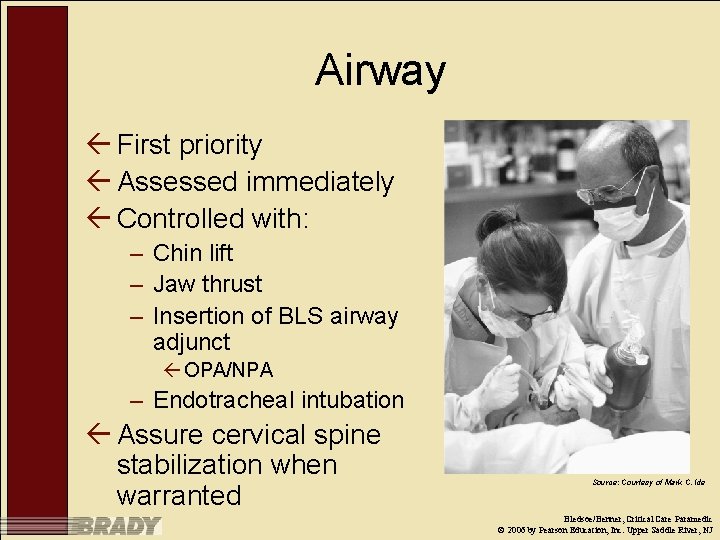
Airway ß First priority ß Assessed immediately ß Controlled with: – Chin lift – Jaw thrust – Insertion of BLS airway adjunct ß OPA/NPA – Endotracheal intubation ß Assure cervical spine stabilization when warranted Source: Courtesy of Mark C. Ide Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Breathing and Ventilation ß Assessment – Verify presence of bilateral breath sounds on auscultation – Assess rate and depth of respirations – Expose chest and inspect for signs of trauma ß Anterior, lateral, and posterior ß Management – Administer 100 percent oxygen via appropriate method – Assess ventilatory status with capnography Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Circulation (1 of 2) ßAssessment – Blood pressure – Pulse rate and quality – Skin color/temperature – Capillary refill time Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Circulation (2 of 2) ßManagement – BLS maneuvers ßRaise legs – IV cannulation ßFluid administration ßVasopressors ßDopamine ßDobutamine ßEpinephrine ßNorepinephrine Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Disability, Neurologic Deficit ßAssessment – AVPU – GCS – Level of consciousness – Motor, sensation – If altered, rule out: ßTrauma ßSubstance abuse Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Examine/Exposure ßRemove all clothing to fully expose patient ßCover with blankets to preserve heat once exam is complete Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Detailed Exam/History ßRe-evaluation of initial assessment followed by complete head-to-toe exam ßNecessary to ensure that all acute and chronic insults/disease is identified and considered ßAllows for trend identification ßReview of studies – Imaging – Laboratory Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ

Patient History ß Understand the circumstances surrounding the injury/illness – Mechanism of injury (MOI) – History of present illness (HPI) ß Medical history important to identify comorbidities – – Pre-existing disease Medications/alcohol/illicit drugs Allergies Tetanus immunization history ß AMPLE Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ

Performing the Detailed Exam ß Head-to-toe exam – Head/face – Neck/cervical spine – Chest ß Anterior, lateral, posterior – – – Abdomen Perineum/genitalia Back/spine Extremities Vascular Neurological Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Management and Further Evaluation ßManagement is same as for any critically ill patient ßABCDE method for prioritizing the management of life threats ßSpecific management for shock can occur after management of potential life threats – Management of potential life threat may help manage shock as well Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
General Treatment Considerations ßAirway management and ventilation key – Begin aggressive airway management early – Endotracheal intubation when necessary ßUse of NMBAs when necessary ßConfirm placement with ETCO 2 detection ßETCO 2 monitoring ßMechanical ventilation ßMust be familiar with patient needs, available vent settings Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Fluid Resuscitation (1 of 2) ßIV access – Peripheral IV access ßTwo large-bore IV lines – Central venous cannulation if: ßPeripheral IV access cannot be obtained ßAdministration of large volumes of fluid are anticipated ßHemodynamic monitoring is required Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Fluid Resuscitation (2 of 2) ßGoal is to achieve no more than 75 percent of preinjury blood pressure – Permissive hypotension ßPrevents: ßExcessive bleeding ßLoss of coagulation factors ß 200 m. L fluid boluses ßRe-evaluate, repeat as needed Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Hemoglobin-Based, Oxygen. Carrying Solutions (HBOCs) ß Major development in emergency and critical care medicine ß Differ from traditional IV volume expanders – Can transport oxygen – Contain polymerized hemoglobin ß Obtained from human, bovine blood ß Removed from red blood cells ß Isolated ßNo infectious agents, antigenic proteins, other blood constituents ß Hemoglobin molecules joined into large chains ßPolymerization ß Compatible with all blood types ßDoes not require: ßTyping ßTesting ßCross-matching Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Volume Expanders (1 of 3) ßHypertonic saline – Showed potential initially – Recent evidence suggests it is no more effective than standard isotonic crystalloids Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Volume Expanders (2 of 3) ßColloids – Popular outside the United States ßAustralia – No more or less effective than crystalloids Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Volume Expanders (3 of 3) ßBlood and blood products – O negative used if time for typing and cross -matching does not exist ßTyped and cross-matched products preferred – Whole blood versus packed red blood cells Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Pharmacological Agents ßFor shock unresponsive to fluid bolus administration – Dopamine – Dobutamine – Epinephrine – Norepinepherine Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Hemodynamic Monitoring ßNoninvasive means initially – Heart rate – Heart rhythm – Blood pressure ßInvasive monitoring: Normal values – Urine output: 0. 5– 1. 0 m. L/hr ßVia foley Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
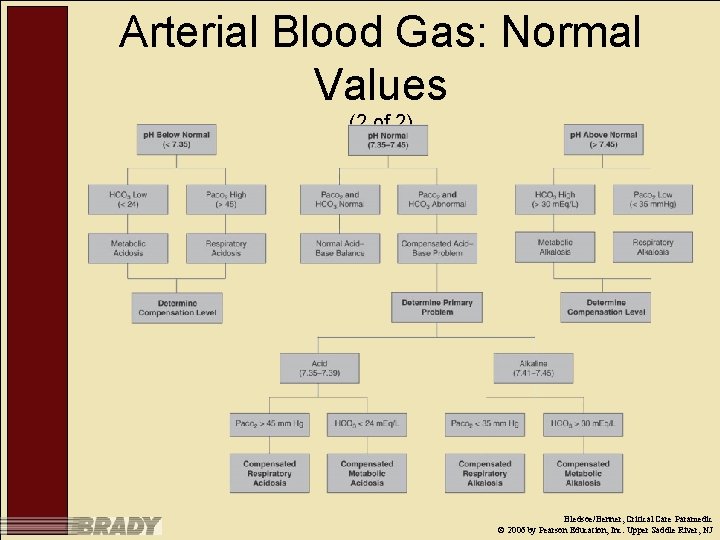
Arterial Blood Gas: Normal Values (1 of 2) ßp. H: 7. 35– 7. 45 ßPa. O 2: 80– 100 mm. Hg ßOxygen saturation: 96 to 98 percent ßPa. CO 2: 35– 45 ßHCO 3 : 22– 26 m. Eq/L ßBase/excess: 3 m. Eq/L Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
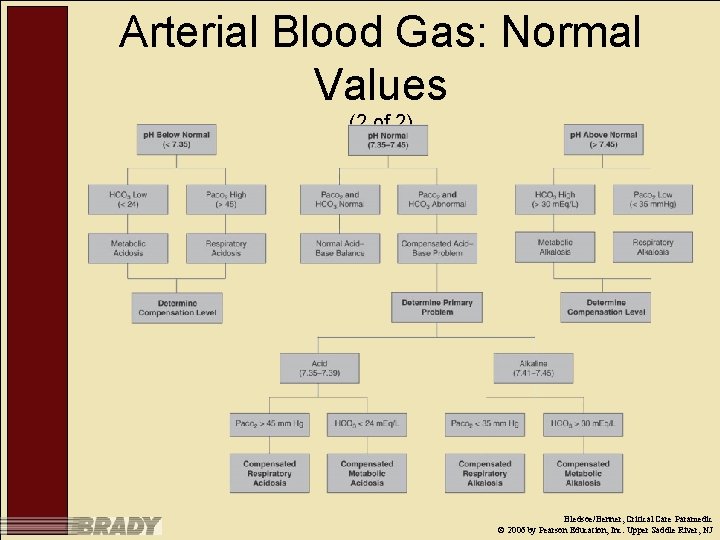
Arterial Blood Gas: Normal Values (2 of 2) Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
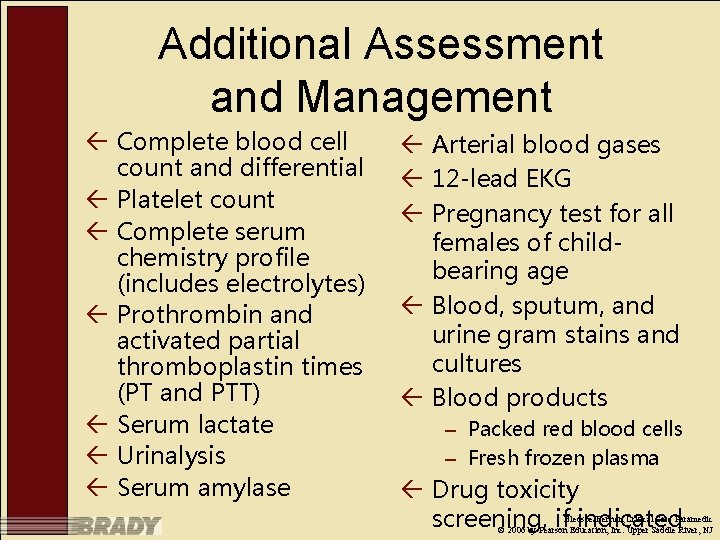
Additional Assessment and Management ß Complete blood cell count and differential ß Platelet count ß Complete serum chemistry profile (includes electrolytes) ß Prothrombin and activated partial thromboplastin times (PT and PTT) ß Serum lactate ß Urinalysis ß Serum amylase ß Arterial blood gases ß 12 -lead EKG ß Pregnancy test for all females of childbearing age ß Blood, sputum, and urine gram stains and cultures ß Blood products – Packed red blood cells – Fresh frozen plasma ß Drug toxicity screening, if indicated Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Imaging Tests ßCT ßUltrasound ßX-rays ßEchocardiogram Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Classifications of Shock ßHypovolemic ßObstructive ßDistributive ßCardiogenic Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ

Hypovolemic Shock ß Secondary to decrease in circulating blood volume – Etiologies include: ß Hemorrhage ßTrauma ßGI bleeding ß Other methods of fluid loss ßDehydration ßExcess diuretic use ßGI loss ßSweating ßBurns ßFluid shift ßSepsis Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ

Signs/Symptoms of Hypovolemic Shock ß Altered mental status ß Diaphoresis ß Tachycardia, tachypnea ß Pallor, mottling ß Thirst ß Collapsed veins, increased skin turgor ß Decreased urine output, oliguria, concentrated urine ß Hypotension Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Management of Hypovolemic Shock ßVolume resuscitation – Crystalloids – Colloids – Vasopressors only after volume resuscitation Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Obstructive Shock ßSecondary to impedance of normal blood flow – Etiologies ßCardiac tamponade ßTension pneumothorax ßPericarditis ßCompression of great vessels ßSupine hypotension syndrome ßPulmonary embolism ßAortic dissection Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Signs and Symptoms of Obstructive Shock ßMirror those of hypovolemic and cardiogenic shock – Signs and symptoms specific to etiology ßTension pneumothorax ßCardiac tamponade ßPulmonary embolism ßAortic dissection ßManagement ßSpecific to etiology Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Management of Obstructive Shock ßSpecific to etiology Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Distributive Shock ßCharacterized by: – Decrease in vascular resistance or – Increased venous capacity secondary to vasomotor dysfunction ßCan be further classified as: – Septic shock – Anaphylactic shock – Neurogenic shock Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Septic Shock ßOccurs secondary to systemic infection ßPredisposing factors – Immunoinsufficiency – Nosocomial infection ßRelease of endotoxins by infecting organism – Vasodilation – Increased cell membrane permeability Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Signs and Symptoms of Septic Shock ßFever ßChills, diaphoresis ßPetechial rash ßPulmonary edema Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ

Management of Septic Shock ßIdentification and removal of infection source ßFluid therapy ßVasopressors Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Anaphylactic Shock ß Exaggerated, systemic response to an allergen – Profound vasodilation – Third spacing of fluid – Bronchospasm ß Etiologies – Food, drug allergies – Administration of blood products – Envenomation ß Speed and severity of symptoms vary – Can occur over minutes or days Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Signs and Symptoms of Anaphylactic Shock ßDyspnea ßBronchospasm ßDysphagia ßRashes, flushing Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ

Management of Anaphylactic Shock ßEpinephrine ßAntihistamine Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Neurogenic Shock ß Results from disruption of sympathetic nervous system secondary to cervical or thoracic spinal injury – Can also occur secondary to: ß Severe head injury ß Migration of spinal anesthesia – Reduction in peripheral vascular resistance ß Widespread vasodilation below level of insult – If insult below level of T 6, bradycardia develops ß Secondary to unopposed vagal tone ß Prevents compensatory tachycardia Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Signs and Symptoms of Neurogenic Shock ßBradycardia – If insult below T 6 ßHypotension ßWarm, flushed skin Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Management of Neurogenic Shock ßFluid administration ßVasopressors Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Cardiogenic Shock ß Results from hearts inability to maintain sufficient CO ß Often result of myocardial insult – Ischemia secondary to: ß AMI ß Trauma ßMyocardial contusion – Dysrhythmia – Vascular insufficiency ß Left ventricular failure results in pulmonary hypertension and edema ß Treatment goal is to restore cardiac output Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
Signs and Symptoms of Cardiogenic Shock ßVary with etiology Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ

Management of Cardiogenic Shock ßVolume replacement ßVasopressors ßIABP placement ßVentricular assist devices ßPacemaker ßCABG Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ

Summary ßEarly identification of shock and aggressive management are important ßClinical trends guide continued treatment ßAppreciation of resources and proficiency with pharmacology and equipment important Bledsoe/Benner, Critical Care Paramedic © 2006 by Pearson Education, Inc. Upper Saddle River, NJ
 Normal pulmonary artery pressure
Normal pulmonary artery pressure Pulmonary artery and aorta
Pulmonary artery and aorta Pig dissection
Pig dissection Pac pulmonary artery catheter
Pac pulmonary artery catheter Swan ganz catheter ports
Swan ganz catheter ports Pmi
Pmi Aorta and pulmonary artery
Aorta and pulmonary artery Conduction delay
Conduction delay Heart valves labeled
Heart valves labeled Central venous pressure monitoring for nurses
Central venous pressure monitoring for nurses Square wave test arterial line
Square wave test arterial line Sma origin
Sma origin Mean pulmonary arterial pressure
Mean pulmonary arterial pressure Holtech
Holtech Downhole pressure monitoring
Downhole pressure monitoring Cushing's triad vitals
Cushing's triad vitals Elmslie trillat
Elmslie trillat Pressure support vs pressure control
Pressure support vs pressure control Continuous bedside pressure mapping
Continuous bedside pressure mapping Intrapleural pressure
Intrapleural pressure Describing edema
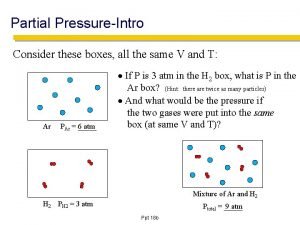
Describing edema How to find partial pressure from total pressure
How to find partial pressure from total pressure Transpulmonary pressure meaning
Transpulmonary pressure meaning Regional metamorphism
Regional metamorphism Pressure support vs pressure control
Pressure support vs pressure control Bernoulli equation pipe flow
Bernoulli equation pipe flow Oncotic pressure vs hydrostatic pressure
Oncotic pressure vs hydrostatic pressure Interstitial fluid hydrostatic pressure
Interstitial fluid hydrostatic pressure Hydrostatic pressure and osmotic pressure
Hydrostatic pressure and osmotic pressure Hydrostatic oncotic pressure
Hydrostatic oncotic pressure Dynamothermal
Dynamothermal Blood pressure regulation
Blood pressure regulation How to find partical pressure
How to find partical pressure Pressure support vs pressure control
Pressure support vs pressure control High pressure and low pressure
High pressure and low pressure High pressure area
High pressure area Central statistical monitoring
Central statistical monitoring Intervention central behavior report card
Intervention central behavior report card Total anomalous venous return
Total anomalous venous return Sibsons fascia
Sibsons fascia Major arteries and veins of the systemic circuit
Major arteries and veins of the systemic circuit Neurogenic shock
Neurogenic shock Right atrium
Right atrium Priyanka breathing
Priyanka breathing Pulmonary surfactant function
Pulmonary surfactant function Cvs xray
Cvs xray Pulmonary function test results
Pulmonary function test results Abnormal vq scan images
Abnormal vq scan images Pulmonary embolism diagnosis
Pulmonary embolism diagnosis Medslide
Medslide Pneumothorax
Pneumothorax Pleural adhesions
Pleural adhesions Windpipe cells
Windpipe cells Pulmonary vascular resistance normal range
Pulmonary vascular resistance normal range Pulmonary toilet
Pulmonary toilet Pulmonary edema
Pulmonary edema Sheep heart
Sheep heart Pulmonary toilet
Pulmonary toilet Cardiac vs pulmonary dyspnea
Cardiac vs pulmonary dyspnea Pulmonary hypertension severity
Pulmonary hypertension severity Tetralogy of fallot murmur
Tetralogy of fallot murmur Pulmonary systemic
Pulmonary systemic Pulmonary gas exchange and transport diagram
Pulmonary gas exchange and transport diagram Pulmonary capillary bed
Pulmonary capillary bed Pearson education heart diagram
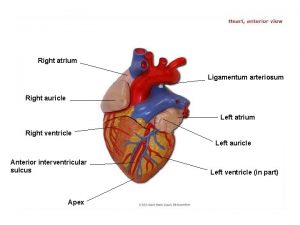
Pearson education heart diagram Pulmonary vascular resistance normal range
Pulmonary vascular resistance normal range Pulmonary aortic window
Pulmonary aortic window Pulmonary hypertension differential diagnosis
Pulmonary hypertension differential diagnosis Flail chest definition
Flail chest definition Hypoventilation
Hypoventilation Pulmonary embolism diagnosis
Pulmonary embolism diagnosis Thin
Thin Pulmonary hangout interval
Pulmonary hangout interval Cardiogenic vs noncardiogenic pulmonary edema
Cardiogenic vs noncardiogenic pulmonary edema Pulmonary hypertension definition
Pulmonary hypertension definition Pah groups
Pah groups How to calculate systemic vascular resistance
How to calculate systemic vascular resistance Mitral stenosis pulmonary hypertension
Mitral stenosis pulmonary hypertension Westermark sign
Westermark sign Normal pulmonary vascular resistance
Normal pulmonary vascular resistance Chest pediatric pulmonary board review
Chest pediatric pulmonary board review Pulmonary embolism case study
Pulmonary embolism case study Copd exacerbation nursing management
Copd exacerbation nursing management Septae
Septae Pulmonary embolism nursing diagnosis
Pulmonary embolism nursing diagnosis Southwest pulmonary associates
Southwest pulmonary associates Heart failure cells are seen in lungs
Heart failure cells are seen in lungs Difference between right and left bronchus
Difference between right and left bronchus Pulmonary ventilation
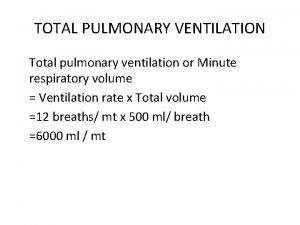
Pulmonary ventilation Layers of the heart
Layers of the heart Upper respiratory tract
Upper respiratory tract Pulmonary capillary
Pulmonary capillary Arteriosum
Arteriosum Auricle of atrium
Auricle of atrium Pulmonary ventilation
Pulmonary ventilation Tuberculosis
Tuberculosis Prof.dr.yesari karter
Prof.dr.yesari karter Vq scan
Vq scan Pulmonary ventilation
Pulmonary ventilation Pulmonary valve
Pulmonary valve Miliary pulmonary tuberculosis
Miliary pulmonary tuberculosis Coronary sinus
Coronary sinus Pulmonary embolism
Pulmonary embolism Pulmonary score pediatria
Pulmonary score pediatria Pulmonary embolism ppt
Pulmonary embolism ppt Miliary tuberculosis
Miliary tuberculosis Pulmonary hypoplasia with anasarca
Pulmonary hypoplasia with anasarca Pulmonary circulation system
Pulmonary circulation system Pictures of lungs with copd
Pictures of lungs with copd Intimal hyperplasia
Intimal hyperplasia Sachin gupta md
Sachin gupta md Pulmonary function test slideshare
Pulmonary function test slideshare X ray of pulmonary embolism
X ray of pulmonary embolism Pulmonary segments
Pulmonary segments Pulmonary hypertension
Pulmonary hypertension