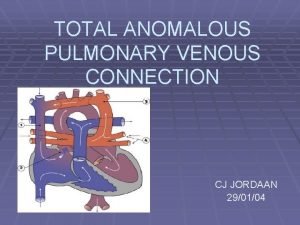
TOTAL ANOMALOUS PULMONARY VENOUS CONNECTION CJ JORDAAN 290104





- Slides: 38

TOTAL ANOMALOUS PULMONARY VENOUS CONNECTION CJ JORDAAN 29/01/04
Definition: § Uncommon congenital cardiac defect (13%) in which there is no direct communication between the pulmonary venous drainage and the Left Atrium. § All the pulmonary veins connect/drain to the Right atrium.
Embryology: § Total anomalous pulmonary venous connection (TAPVC) develops when the primordial pulmonary vein fails to unite with the plexus of veins surrounding the lung buds. § This results in return of pulmonary venous blood to the heart via a systemic vein, and subsequently to the right atrium.
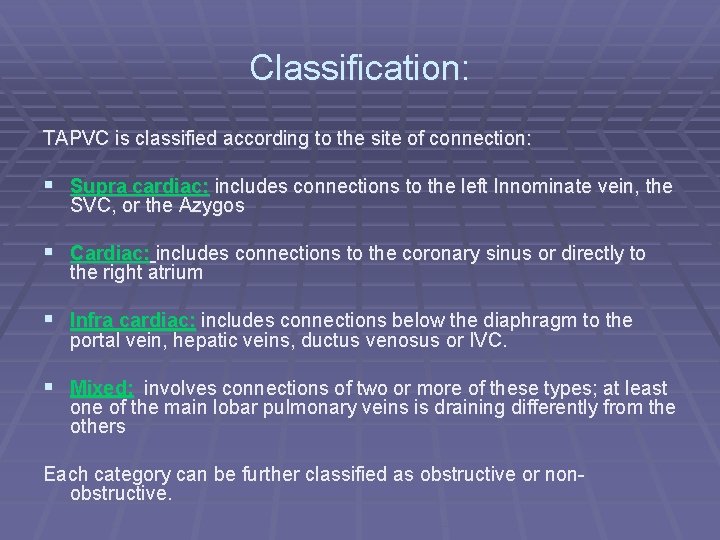
Classification: TAPVC is classified according to the site of connection: § Supra cardiac: includes connections to the left Innominate vein, the SVC, or the Azygos § Cardiac: includes connections to the coronary sinus or directly to the right atrium § Infra cardiac: includes connections below the diaphragm to the portal vein, hepatic veins, ductus venosus or IVC. § Mixed: involves connections of two or more of these types; at least one of the main lobar pulmonary veins is draining differently from the others Each category can be further classified as obstructive or nonobstructive.
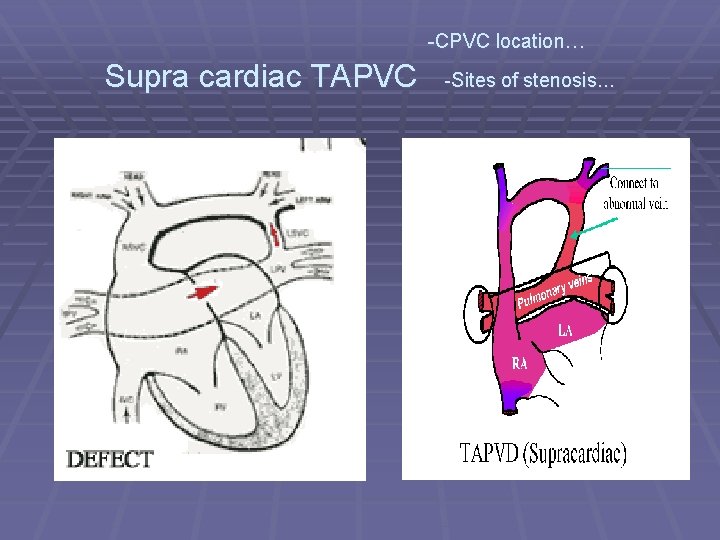
1. Supra cardiac TAPVC: § Most common form of TAPVC---45% § Bilat draining of pulmonary veins (PV) to Common Pulmonary Venous Sinus (CPVS). § This confluence drains via Vertical Vein (VV) to Innominate vein, SVC or Azygos. § Stenosis common ( +/- 40 -60%): Pulmonary vein systemic connection, Vascular vice or Long thin VV
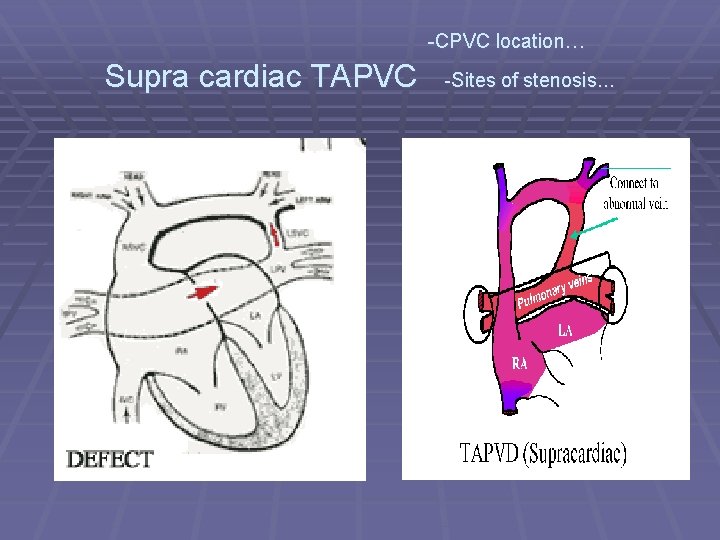
-CPVC location… Supra cardiac TAPVC -Sites of stenosis…
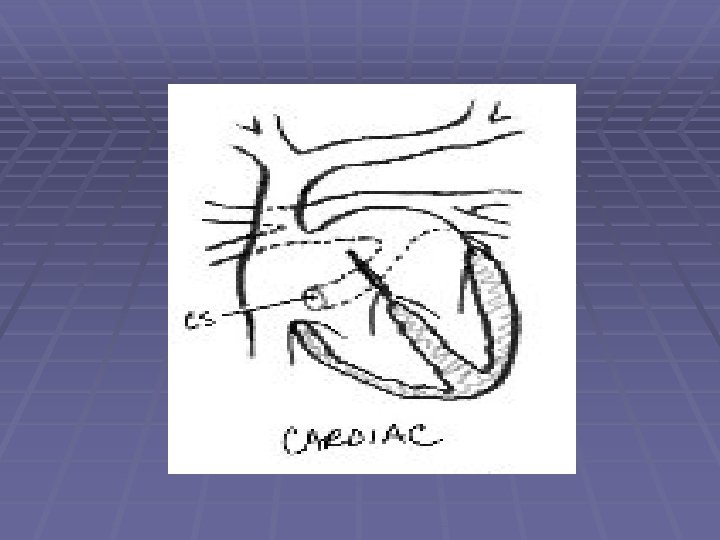
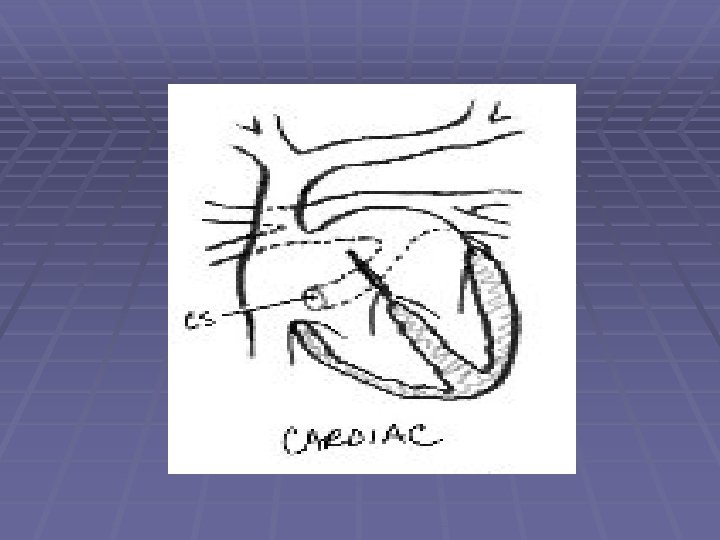
2. Cardiac TAPVC: § Accounts for 25% of TAPVC § VV drains mostly to Coronary Sinus, seldom directly to § § § Right atrium. Enlarged coronary sinus acts as the CPVS with only a thin wall of myocardium separating sinus and the Left atrium. Right atrial draining: Seen in RA isomerism. Associated with absent Coronary sinus, huge or absent intra atrial septum. VV opens as a fibrous midline confluence. STENOSIS: Rare. May occur where the CPVS joins the Coronary sinus, or at the mouth of the coronary sinus (persisting Thebesian valve)
3. Infra cardiac TAPVC: § Accounts for 25% of TAPVC § The common pulmonary vein drains through the § diaphragm to the portal vein, ductus venosus or seldom to the IVC. Has the greatest propensity for STENOSIS: -May be compressed where it penetrates the Diaphragm, -Connecting vein is narrowed at its junction with the portal vein, -VV has a thickened wall with intimal proliferation, -portal sinusoids (Liver) offer additional obstruction to venous return

Infra cardiac TAPVC:
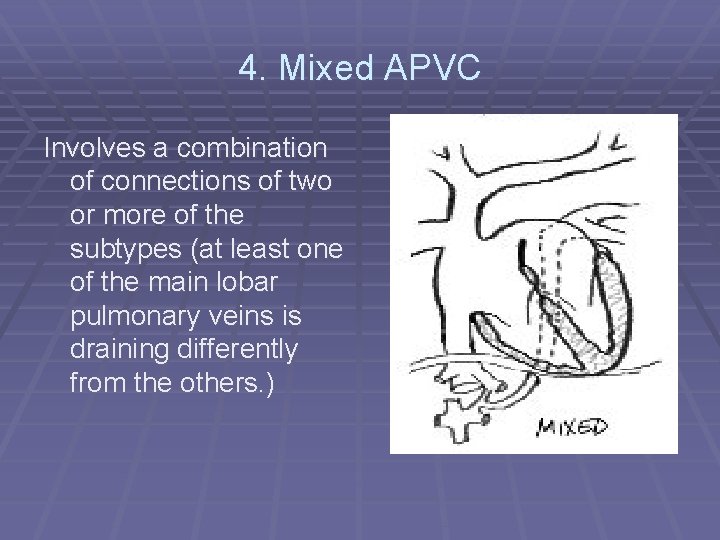
4. Mixed APVC Involves a combination of connections of two or more of the subtypes (at least one of the main lobar pulmonary veins is draining differently from the others. )
Anatomy § RA: Enlarged and thick walled. Decreased compliance. § LA: Volume 53% less than predicted. LA auricle is normal in size, decrease in LA can be explained by the absence of the pulmonary vein component. § ASD: ASD or PFO must exist for survival. Usually of adequate size and not obstructive. Obstruction leads to a decreased R to L shunt with pulmonary venous obstruction and Pulm. Hypertension. Presents as a severely sick neonate.
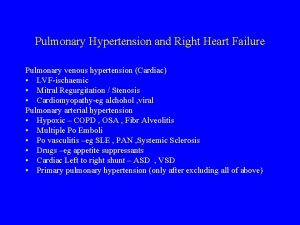
Anatomy § LV: Normal in size, wall thickness and mass, but decreased LV cavity ( due to leftward displacement of septum secondary to right ventricle pressure-volume overload. ) § RV: Varies in size, depends on magnitude of pulmonary blood flow, pulmonary venous stenosis, point of PV connection. (Infra cardiac connection- RV not dilated or hypertrophied) § PA: Most infants have marked pulmonary hypertension. Structural changes are usually found in the lungs even in the youngest infants dying of TAPVC. Increase in pulm. Arterial muscularity-increase in wall thickness and extension of muscle into smaller and peripheral arteries. Vein wall thickness is also increased.
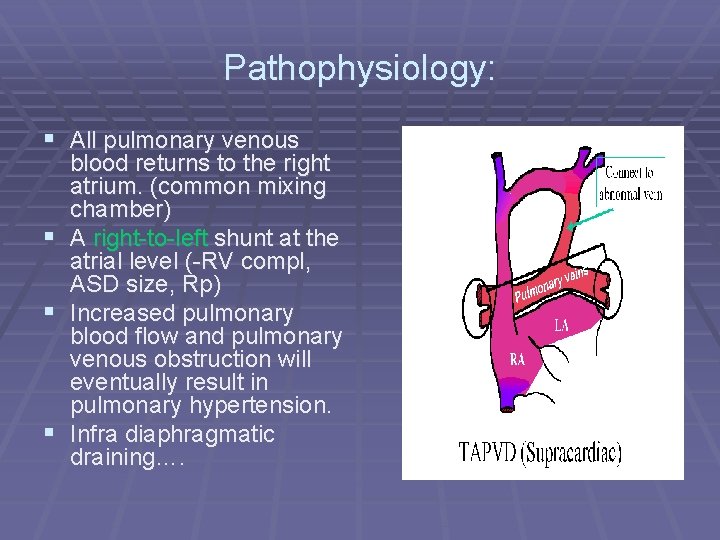
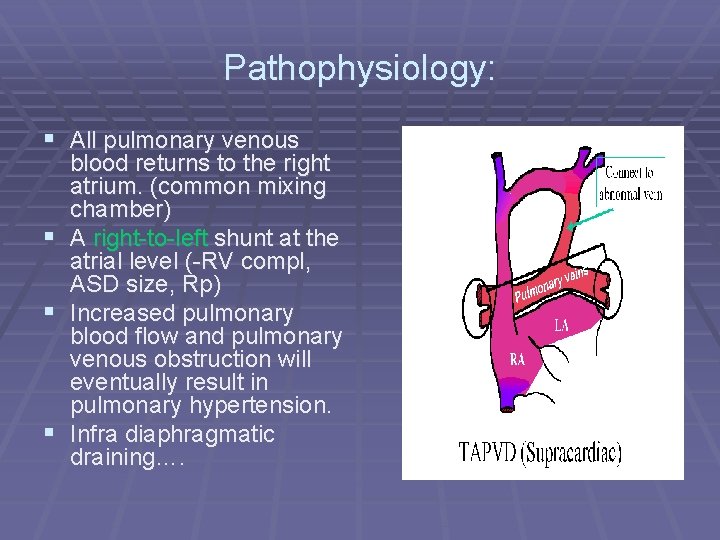
Pathophysiology: § All pulmonary venous blood returns to the right atrium. (common mixing chamber) § A right-to-left shunt at the atrial level (-RV compl, ASD size, Rp) § Increased pulmonary blood flow and pulmonary venous obstruction will eventually result in pulmonary hypertension. § Infra diaphragmatic draining….
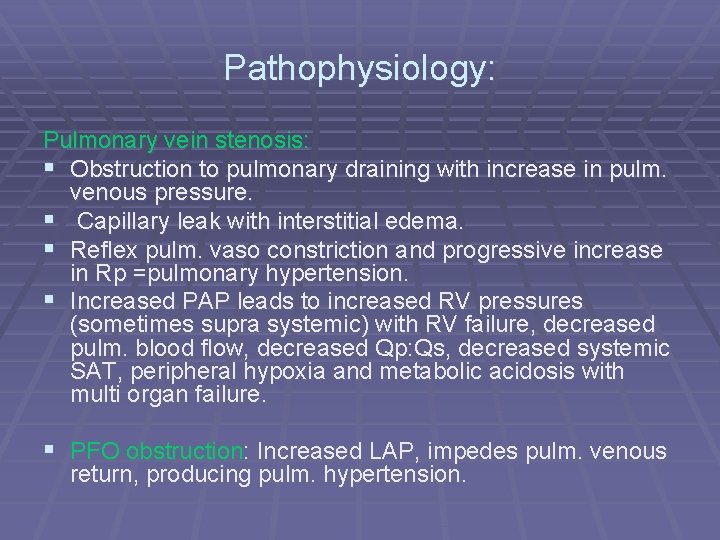
Pathophysiology: Pulmonary vein stenosis: § Obstruction to pulmonary draining with increase in pulm. venous pressure. § Capillary leak with interstitial edema. § Reflex pulm. vaso constriction and progressive increase in Rp =pulmonary hypertension. § Increased PAP leads to increased RV pressures (sometimes supra systemic) with RV failure, decreased pulm. blood flow, decreased Qp: Qs, decreased systemic SAT, peripheral hypoxia and metabolic acidosis with multi organ failure. § PFO obstruction: Increased LAP, impedes pulm. venous return, producing pulm. hypertension.

Burchell principle: § A direct relationship exists between the magnitude of pulm. blood flow and systemic saturation. § The Qp: Qs is determined by magnitude of pulmonary blood flow, pulm. blood flow is inversely related to Rp. § Thus an increase in PAP and Rp leads to a decrease in pulm blood flow with a decreased systemic SAT. § SAT less than 80%: Qp: Qs likely to be < 1. 4 and Rp > 10 !!!!!!!
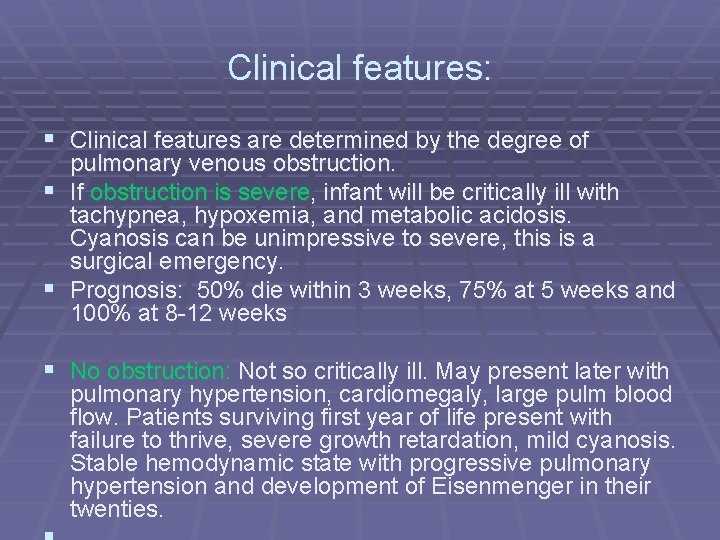
Clinical features: § Clinical features are determined by the degree of pulmonary venous obstruction. § If obstruction is severe, infant will be critically ill with tachypnea, hypoxemia, and metabolic acidosis. Cyanosis can be unimpressive to severe, this is a surgical emergency. § Prognosis: 50% die within 3 weeks, 75% at 5 weeks and 100% at 8 -12 weeks § No obstruction: Not so critically ill. May present later with pulmonary hypertension, cardiomegaly, large pulm blood flow. Patients surviving first year of life present with failure to thrive, severe growth retardation, mild cyanosis. Stable hemodynamic state with progressive pulmonary hypertension and development of Eisenmenger in their twenties.
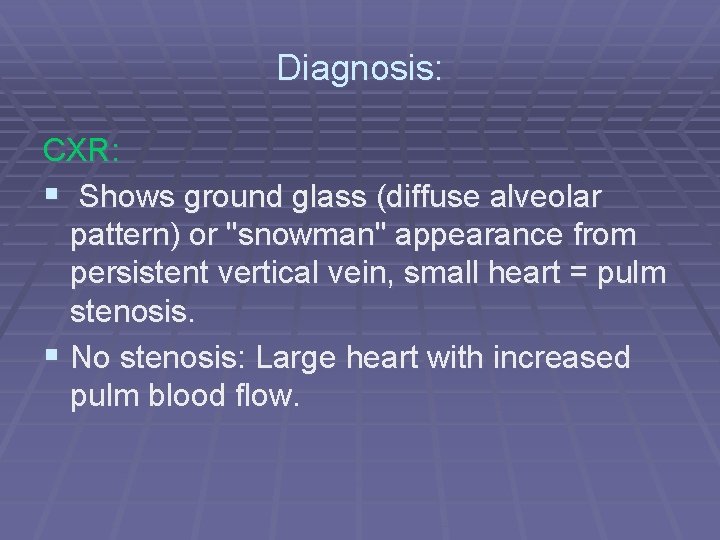
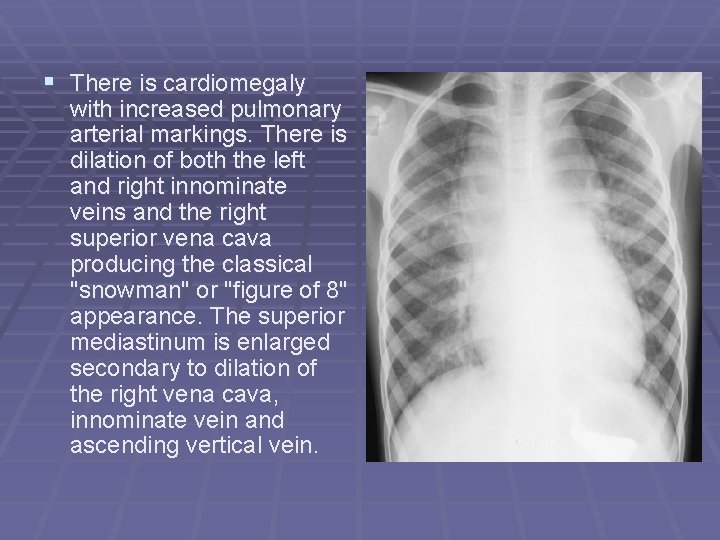
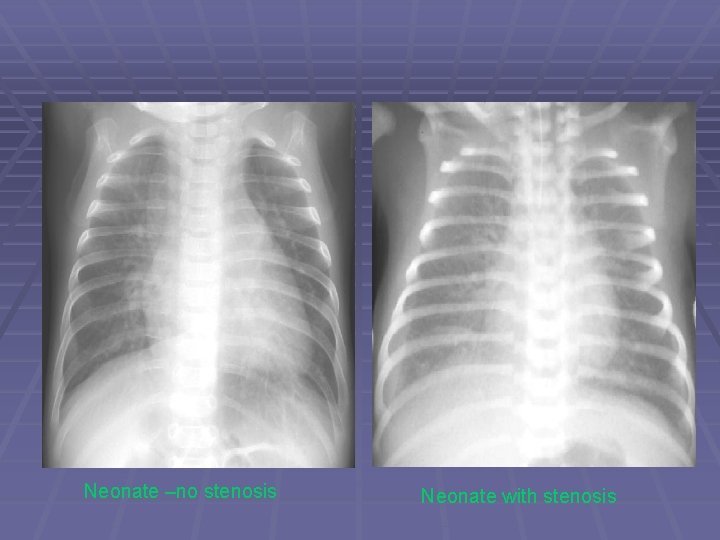
Diagnosis: CXR: § Shows ground glass (diffuse alveolar pattern) or "snowman" appearance from persistent vertical vein, small heart = pulm stenosis. § No stenosis: Large heart with increased pulm blood flow.
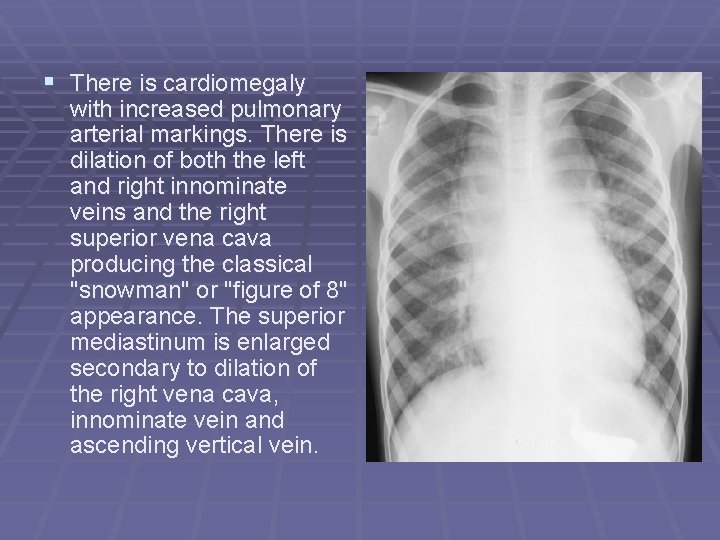
§ There is cardiomegaly with increased pulmonary arterial markings. There is dilation of both the left and right innominate veins and the right superior vena cava producing the classical "snowman" or "figure of 8" appearance. The superior mediastinum is enlarged secondary to dilation of the right vena cava, innominate vein and ascending vertical vein.
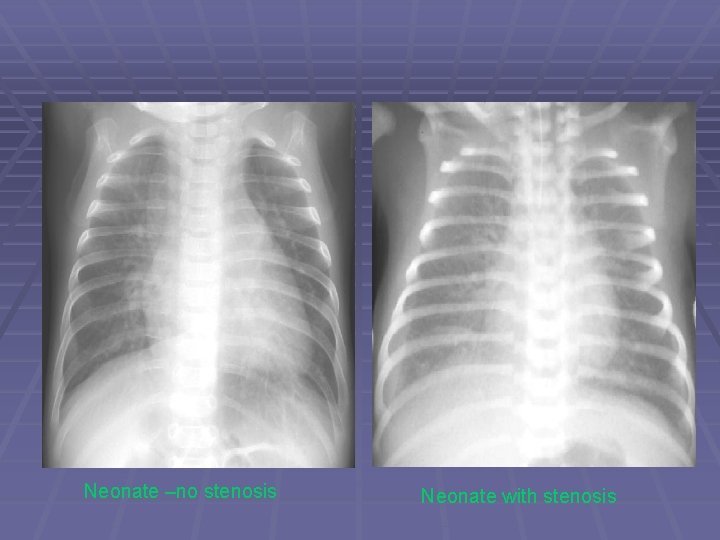
Neonate –no stenosis Neonate with stenosis
Diagnosis: Echo: Diagnostic in most infants. Evaluation of cardiac chambers, Echo free space posterior to LA with abnormal drainage
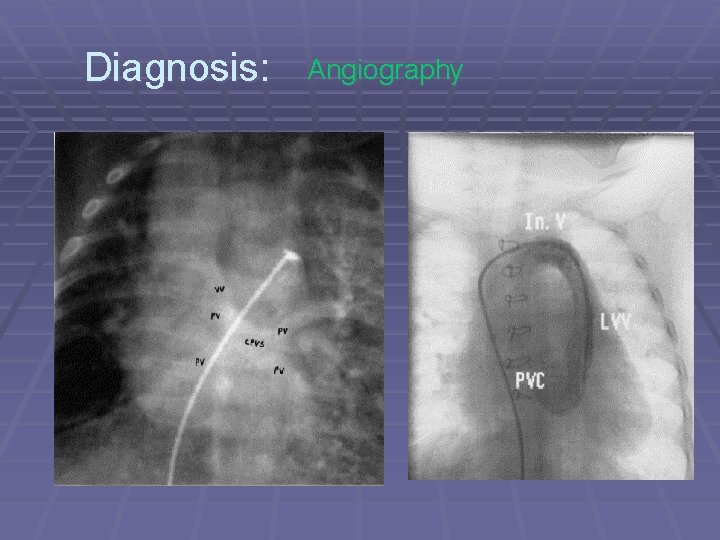
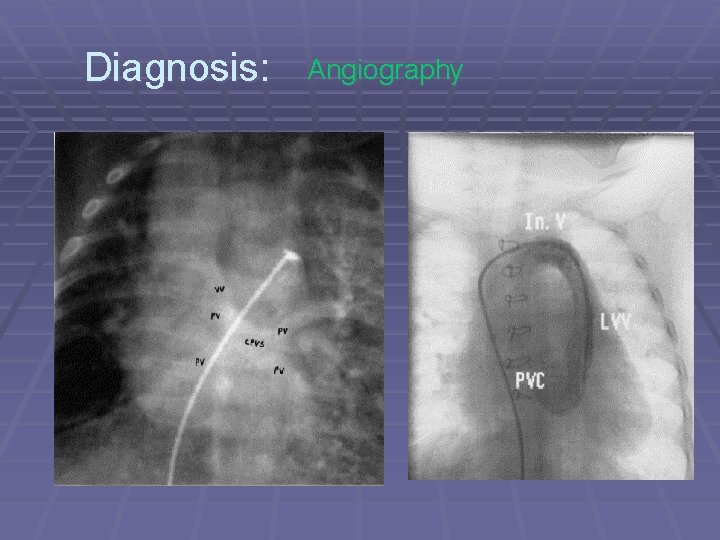
Diagnosis: Angiography
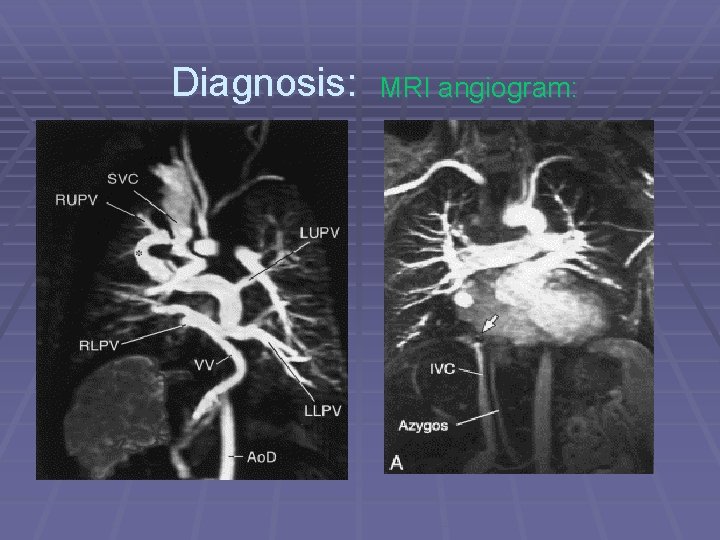
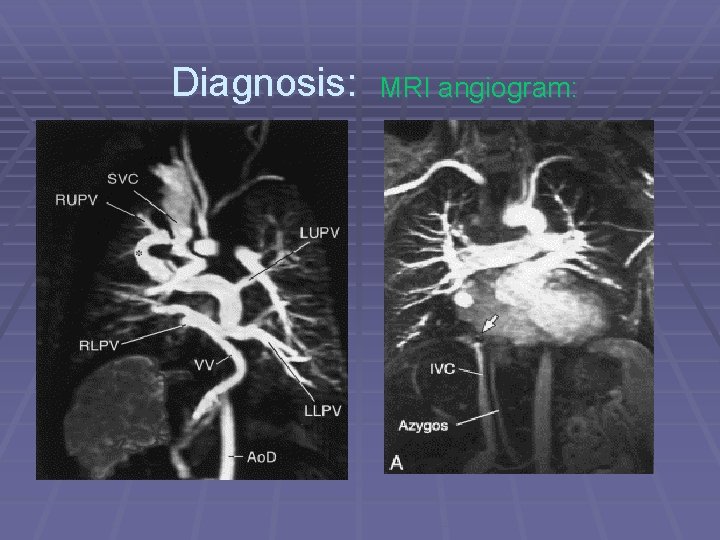
Diagnosis: MRI angiogram:
TREATMENT: § Patients with TAPVC should undergo operative § § § repair when the diagnosis is made Obstructed TAPVC is a surgical emergency Non-obstructed TAPVC should have prompt repair as well, as the clinical status of these patients can deteriorate rapidly Early repair of non-obstructed TAPVC also prevents the adverse squeal of cyanosis and volume overload of the heart and lungs
Treatment: Pre operatively: § Admit in PICU § Intubation and ventilation § Tolazoline, PGE 1 IVI § Stabilize, correct metabolic acidosis, confirm diagnosis § Prepare for emergent theatre.
Operative Technique § Cardiopulmonary bypass with hypothermic circulatory arrest is the preferred approach in critically ill infants § Surgical goals are: eliminating all anomalous connections, draining the pulmonary veins into the left atrium, and closing intracardiac shunts, small PFO is left for RV decompression § The PV-LA anastomosis must be large and undistorted. § Problems: Small aorta Hypothermic CPB response
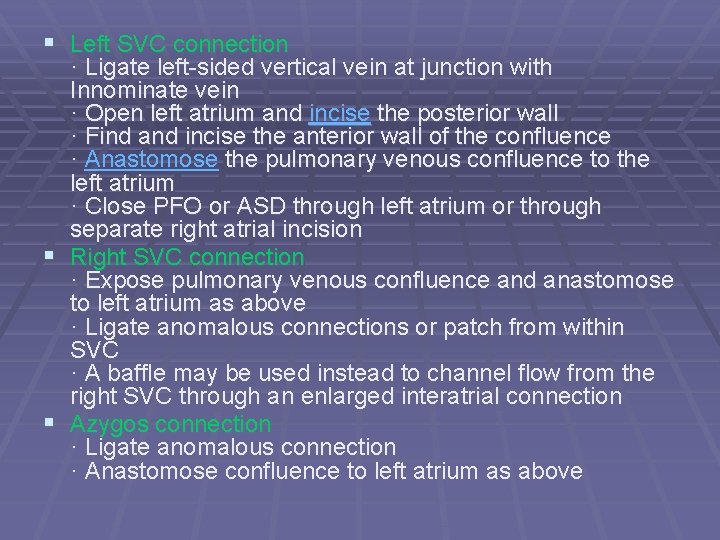
§ Left SVC connection · Ligate left-sided vertical vein at junction with Innominate vein · Open left atrium and incise the posterior wall · Find and incise the anterior wall of the confluence · Anastomose the pulmonary venous confluence to the left atrium · Close PFO or ASD through left atrium or through separate right atrial incision § Right SVC connection · Expose pulmonary venous confluence and anastomose to left atrium as above · Ligate anomalous connections or patch from within SVC · A baffle may be used instead to channel flow from the right SVC through an enlarged interatrial connection § Azygos connection · Ligate anomalous connection · Anastomose confluence to left atrium as above

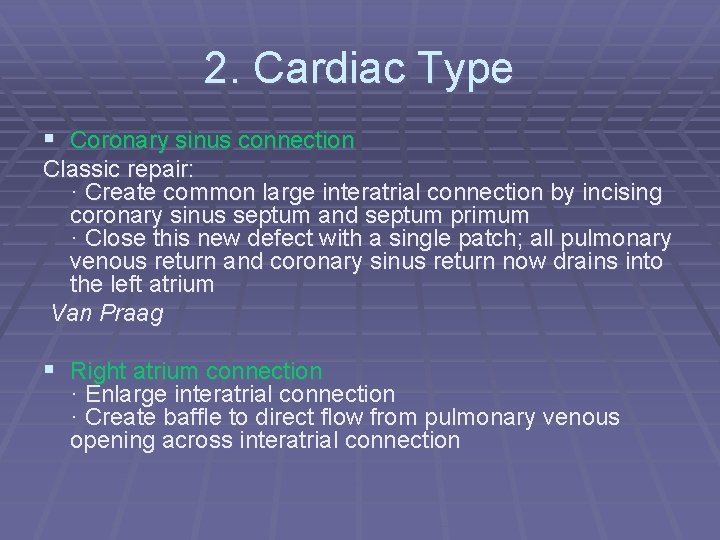
2. Cardiac Type § Coronary sinus connection Classic repair: · Create common large interatrial connection by incising coronary sinus septum and septum primum · Close this new defect with a single patch; all pulmonary venous return and coronary sinus return now drains into the left atrium Van Praag § Right atrium connection · Enlarge interatrial connection · Create baffle to direct flow from pulmonary venous opening across interatrial connection

3. Infracardiac Type § · Ligate PDA once CPB is established · Identify and ligate anomalous descending vertical vein at the diaphragm · Initiate circulatory arrest · Open left atrium and incise the posterior wall · Find and incise the anterior wall of the confluence · Anastomose the pulmonary venous confluence to the left atrium · Close the interatrial communication
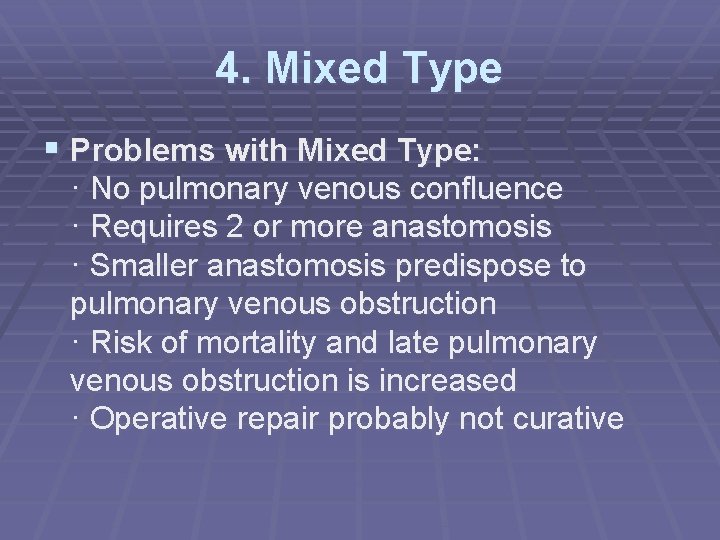
4. Mixed Type § Problems with Mixed Type: · No pulmonary venous confluence · Requires 2 or more anastomosis · Smaller anastomosis predispose to pulmonary venous obstruction · Risk of mortality and late pulmonary venous obstruction is increased · Operative repair probably not curative
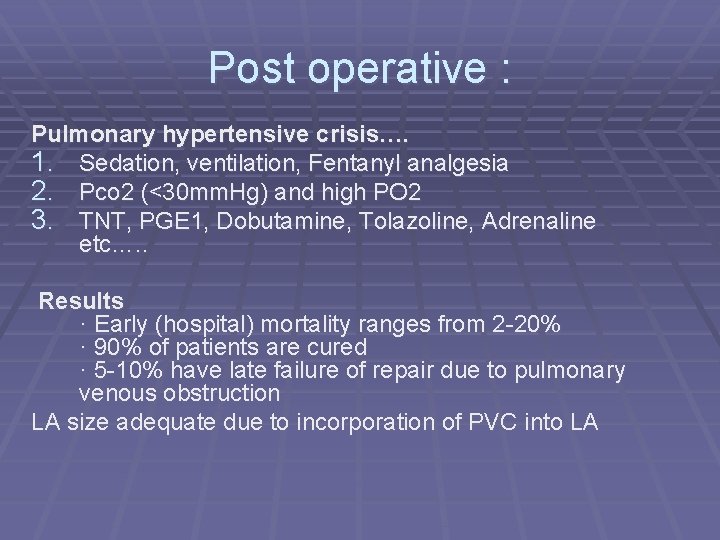
Post operative : Pulmonary hypertensive crisis…. 1. Sedation, ventilation, Fentanyl analgesia 2. Pco 2 (<30 mm. Hg) and high PO 2 3. TNT, PGE 1, Dobutamine, Tolazoline, Adrenaline etc…. . Results · Early (hospital) mortality ranges from 2 -20% · 90% of patients are cured · 5 -10% have late failure of repair due to pulmonary venous obstruction LA size adequate due to incorporation of PVC into LA
Post operative : Risk Factors: · Poor pre-operative status (acidosis) · Pulmonary venous obstruction, small PFO · High pulmonary vascular resistance, pre operative SAT <80% · Young age · Small left ventricle · Major associated anomalies · Infracardiac or mixed type
Literature: Bu’Lock FA et al. Balloon dilatation of vein stenosis in obstructed TAPVC. Ped Cardio 1998; 15: 78 Balloon atrial septostomy: Risk factor for death, not an ameliorating factor. Balloon dilatation of left vertical vein in obstructive supracardiac TAPVC may provide important clinical improvement and short term hemodinamic stability before operation Kiziltepe U et al. Acute pulm hypertensive crisis after TAPVC repair…treatment. Internat J of Cardio 2002: 87; 107 -109 Treatment of recurrent severe pulm hypertension refractive to medical treatment can be dealt with inflow occlusion and creation of large intra atrial connection. Chest left open post operatively.
Post operative PV stenosis: Stark J, De Leval MR. Management of pulm venous obstruction after TAPVC repair. Eur J Cardio-Thorac Surg. 2003: 24: 28 -36 § Complicates surgery in 5 -10% § Classification of PV stenosis: Discrete stenosis Tubular focal stenosis Diffuse hypoplasia § May be severe anastomotic stenosis or pulmonary vein stenosis.
Post operative PV stenosis: § Predominate after correction of Infracardiac and cardiac § § TAPVC. Vary from Fibrosis and neo-intimal proliferation at the anastomotic site, to segmental or diffuse intimal hyperplasia with extension to the individual pulm veins Abnormal architecture of pulm venous wall leads to increased tendency to neo intimal proliferation with increase in intimal and muscular media. Obstruction involving individual PV occurring early post op – Very difficult to treat with high re-stenosis rate. Poor prognosis. 66% early mortality.
Post operative PV stenosis § Risk factors: Use of Gore-tex patches Early presentation difficult anastomosis small pulmonary venous confluence § Diagnosis: 1. 2. 3. 4. 5. § Pulm venous flow patterns which does not reach baseline throughout the cardiac and resp cycles Absence of pulm venous return from one lung TR jet velocity > 3 m per sec. RV pressure >40 mm. Hg Increase in pulm blood flow>1. 8 m per second Scrupulous and atraumatic technique still remain the best option for success. Use of absorbable sutures controversial.
Post operative PV stenosis: § Repair: 100% success rate achievable in anastomotic stenosis. Patch enlargement relieves stenosis and re stenosis is uncommon, No surgical approach including: patch augmentation, longitudinal incision with transverse plication, balloon dilatation or placement of stents has shown any improvement in patient outcome. Goldenar syndrome: (Infracardiac TAPVC, R lung hypoplasia, sub arterial VSD and ost secundum ASD) has a particular tendency to PV stenosis irrespective of type of repair. End with near atresia of PV’s
 Total anomalous venous return
Total anomalous venous return Nedbank classic credit card travel medical insurance
Nedbank classic credit card travel medical insurance Dr johan jordaan
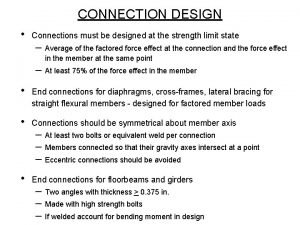
Dr johan jordaan Slip critical connection vs bearing connection
Slip critical connection vs bearing connection A307 bolt shear strength
A307 bolt shear strength Slip critical bolted connection
Slip critical bolted connection Text to world connections examples
Text to world connections examples Total pulmonary ventilation
Total pulmonary ventilation Protein structure determination
Protein structure determination Dinitrogen complex ppt
Dinitrogen complex ppt Anomalous picture
Anomalous picture Anomalous
Anomalous Anomalous verb
Anomalous verb Anomalous expansion of water
Anomalous expansion of water Anomalous mirage archer
Anomalous mirage archer Abrupt blunt with no formalities
Abrupt blunt with no formalities Anomalous zeeman effect
Anomalous zeeman effect Anmalo
Anmalo Christianne beekman
Christianne beekman Total revenues minus total costs equals
Total revenues minus total costs equals Pasivo total sobre activo total
Pasivo total sobre activo total Total revenue minus total expenses
Total revenue minus total expenses Total revenues minus total costs equals
Total revenues minus total costs equals Total revenues minus total costs equals
Total revenues minus total costs equals Most common complication of central venous catheter
Most common complication of central venous catheter Keith and wagner classification
Keith and wagner classification Suboccipital triangle roof
Suboccipital triangle roof Capillary bed labeled
Capillary bed labeled Lymphatic and venous drainage
Lymphatic and venous drainage Venous loop
Venous loop Precapillary sphincter
Precapillary sphincter Epicranial aponeurosis
Epicranial aponeurosis Common femoral vein
Common femoral vein Perforators of leg
Perforators of leg Cardiovascular changes
Cardiovascular changes Hepatic portal system
Hepatic portal system Optic
Optic Systemic veins
Systemic veins Hard exudates vs cotton wool spots
Hard exudates vs cotton wool spots