Principles of Mechanical Ventilation Aimes Ventilator settings Modes




- Slides: 51
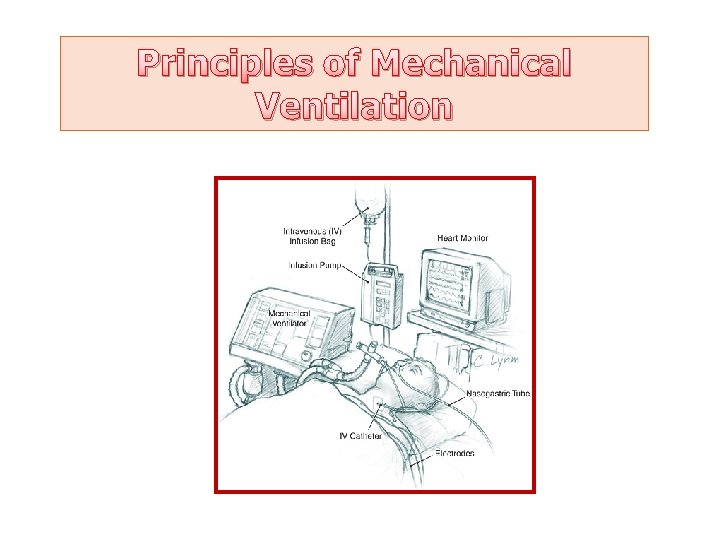
Principles of Mechanical Ventilation
Aimes ØVentilator settings ØModes of ventilation ØMonitoring of the patient ØTrouble shooting
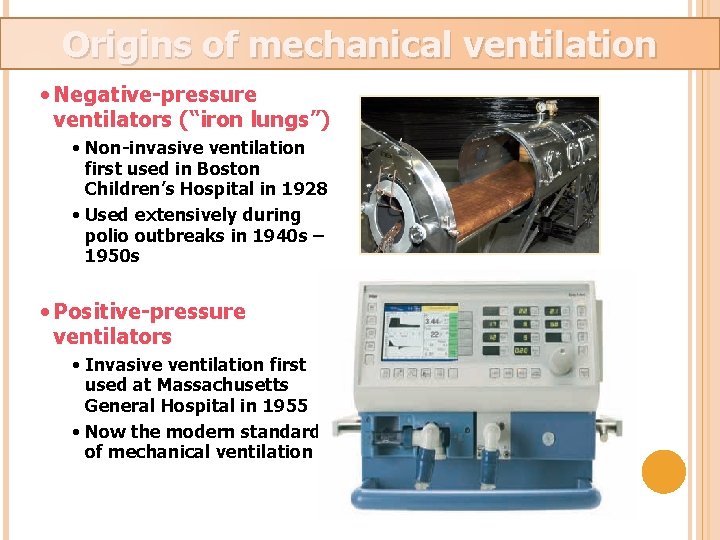
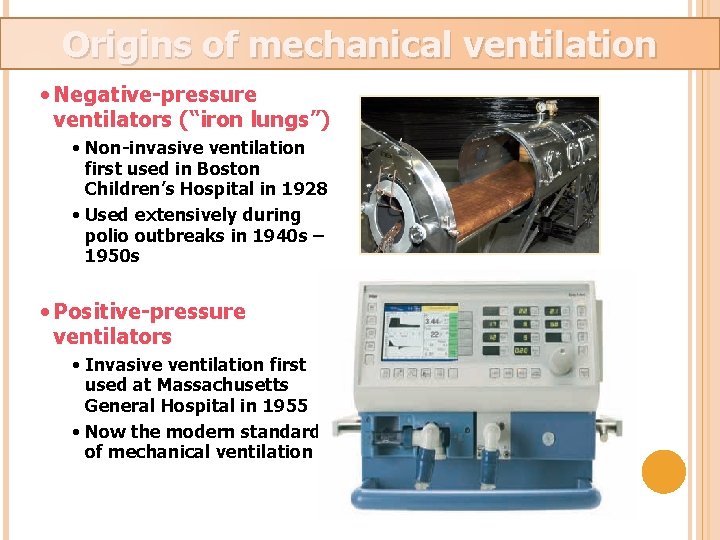
Origins of mechanical ventilation • Negative-pressure ventilators (“iron lungs”) • Non-invasive ventilation first used in Boston Children’s Hospital in 1928 • Used extensively during polio outbreaks in 1940 s – 1950 s • Positive-pressure ventilators • Invasive ventilation first used at Massachusetts General Hospital in 1955 • Now the modern standard of mechanical ventilation
VENTILATOR SETTINGS
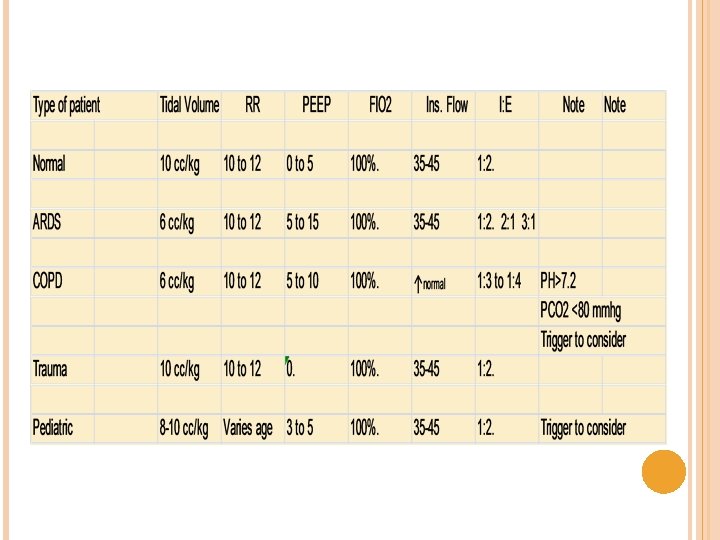
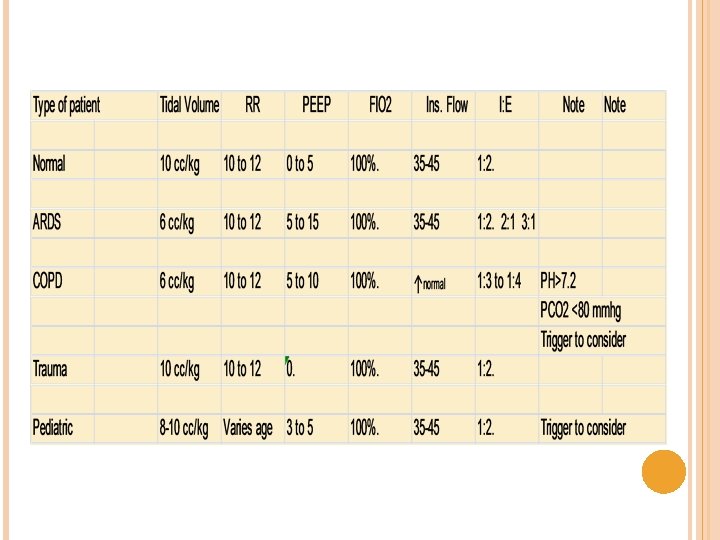
Ø Ø Ø Ø Ventilator mode Respiratory rate Tidal volume or pressure settings Inspiratory flow I: E ratio PEEP Fi. O 2 Inspiratory trigger
Respiratory rate • What is the pt actual rate demand?
Inspiratory time Set as: % of respiratory cycle RR: 10 I: E =1/2 Total respiratory time=60/10 TCT=6 Sec I: E ratio Expiratory time not set Remaining time after inspiration before next breath
TIDAL VOLUME OR PRESSURE SETTING Maximum volume/pressure to achieve good ventilation and oxygenation without producing alveolar overdistention Max cc/kg? = 10 cc/kg Some clinical exceptions

Inspiratory flow Varies with the Vt, I: E and RR Normally about 35 -45 l/min
I: E RATIO 1: 2 Prolonged Inverse at 1: 3, 1: 4, … ratio
FIO 2 The usual goal is to use the minimum Fio 2 required to have a Pa. O 2 > 60 mmhg or a sat >90% Start at 100% Oxygen toxicity normally with Fio 2 >40%
INSPIRATORY TRIGER 2 modes: Airway pressure Flow triggering
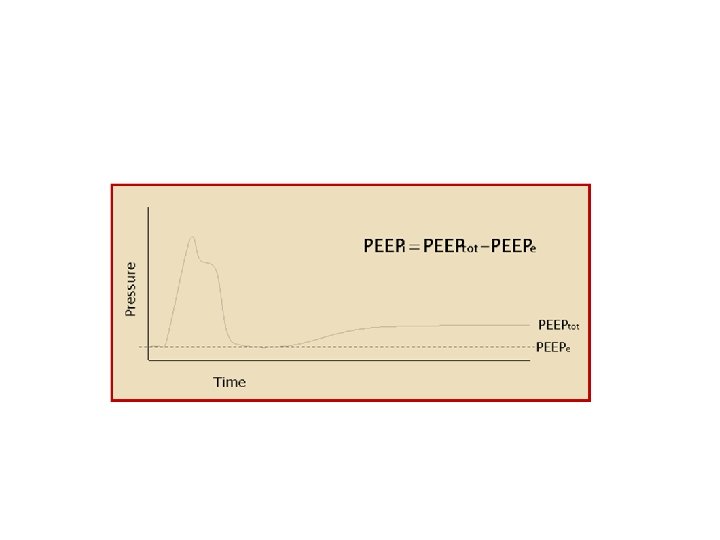
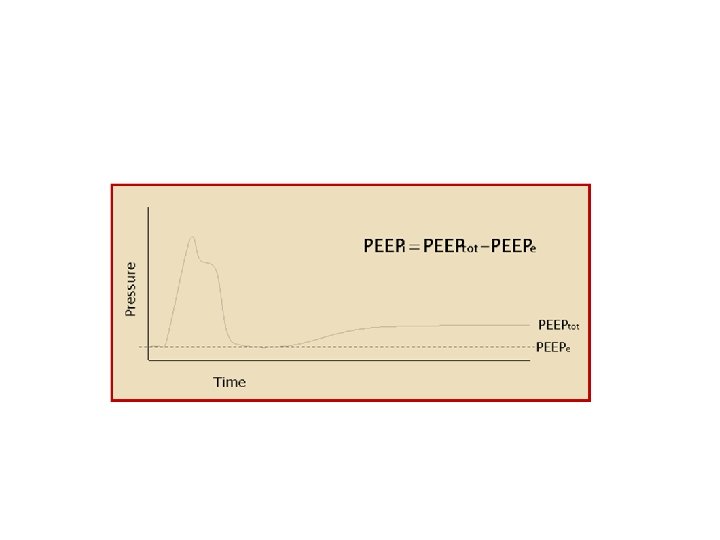
Positive End-expiratory Pressure (PEEP) v What is PEEP? v What is the goal of PEEP? v. Improve oxygenation v. Diminish the work of breathing
PEEP Barotrauma Diminish cardiac output Regional hypoperfusion Na. Cl retention Augmentation of I. C. P. ? Paradoxal hypoxemia

PEEP Contraindication: No absolute CI Barotrauma Airway trauma Hemodynamic instability I. C. P. ? Bronchospasm?
PEEP WHAT PEEP DO YOU WANT? Usually, 5 -10 cm. H 2 O
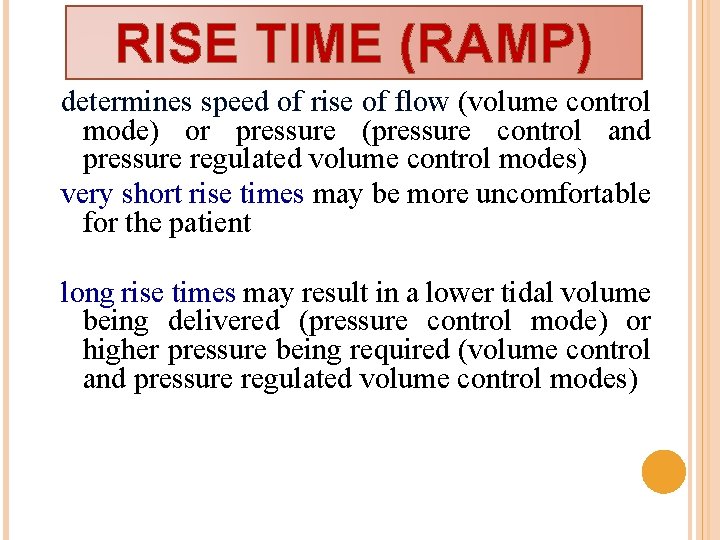
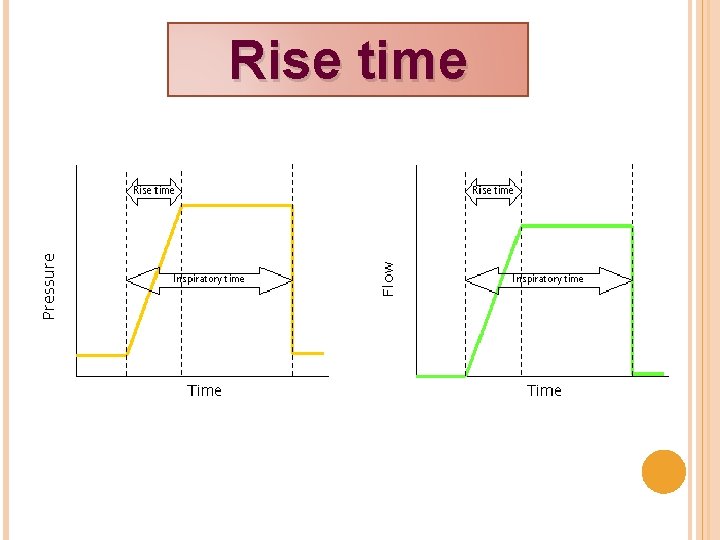
RISE TIME (RAMP) determines speed of rise of flow (volume control mode) or pressure (pressure control and pressure regulated volume control modes) very short rise times may be more uncomfortable for the patient long rise times may result in a lower tidal volume being delivered (pressure control mode) or higher pressure being required (volume control and pressure regulated volume control modes)
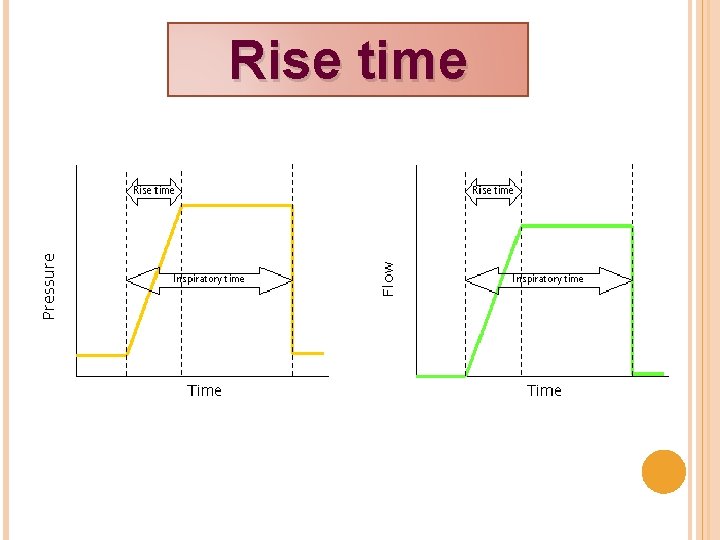
Rise time
Theory • Ventilation vs. Oxygenation • Pressure Cycling vs. Volume Cycling
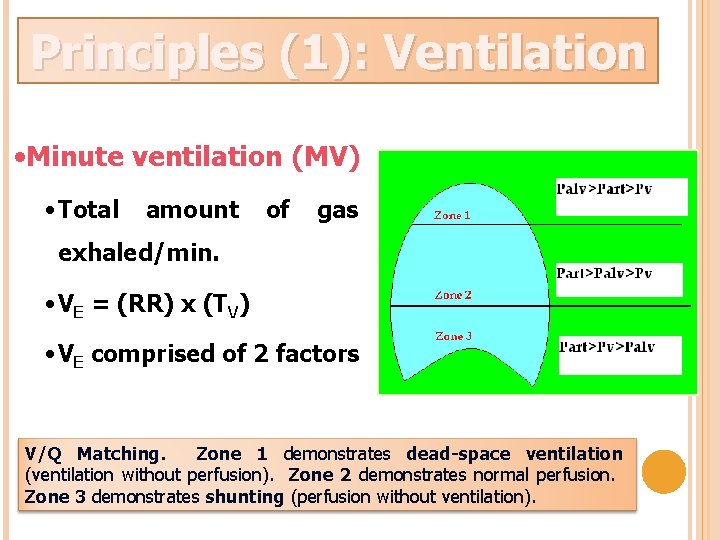
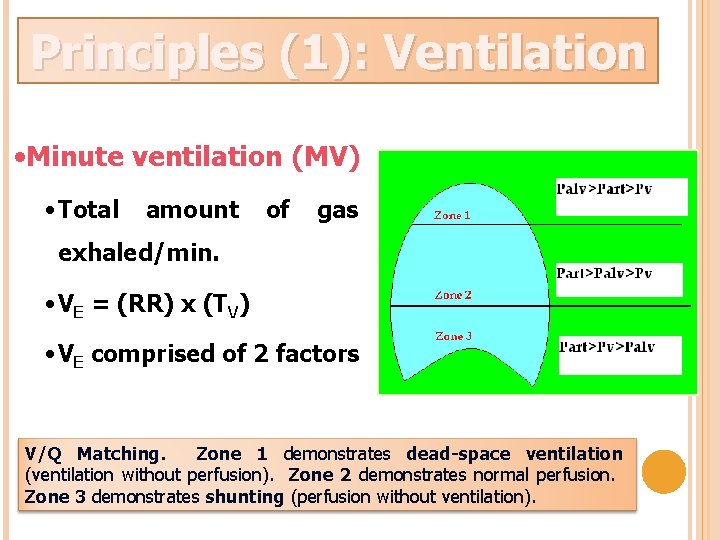
Principles (1): Ventilation The goal of ventilation is to facilitate CO 2 release and maintain normal Pa. CO 2 • Minute ventilation (MV) • Total amount of gas exhaled/min. • VE = (RR) x (TV) • VE comprised of 2 factors V/Q Matching. Zone 1 demonstrates dead-space ventilation (ventilation without perfusion). Zone 2 demonstrates normal perfusion. Zone 3 demonstrates shunting (perfusion without ventilation).
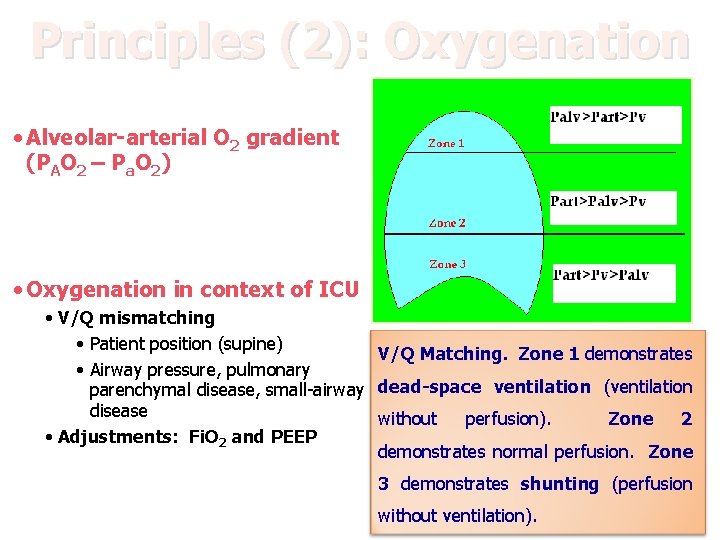
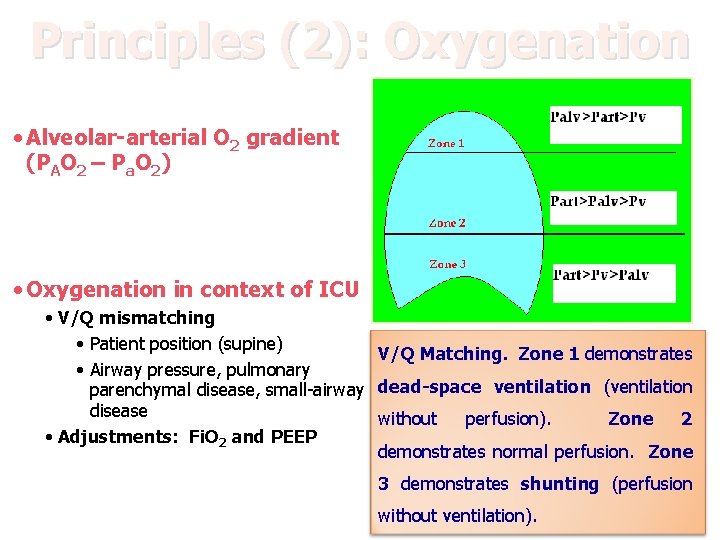
Principles (2): Oxygenation The primary goal of oxygenation is to maximize O 2 delivery to blood (Pa. O 2) • Alveolar-arterial O 2 gradient (PAO 2 – Pa. O 2) • Oxygenation in context of ICU • V/Q mismatching • Patient position (supine) V/Q Matching. Zone 1 demonstrates • Airway pressure, pulmonary parenchymal disease, small-airway dead-space ventilation (ventilation disease without perfusion). Zone 2 • Adjustments: Fi. O 2 and PEEP demonstrates normal perfusion. Zone 3 demonstrates shunting (perfusion without ventilation).
Pressure ventilation vs. volume ventilation Pressure-cycled modes deliver a fixed pressure at variable volume (neonates) Volume-cycled modes deliver a fixed volume at variable pressure (adults)
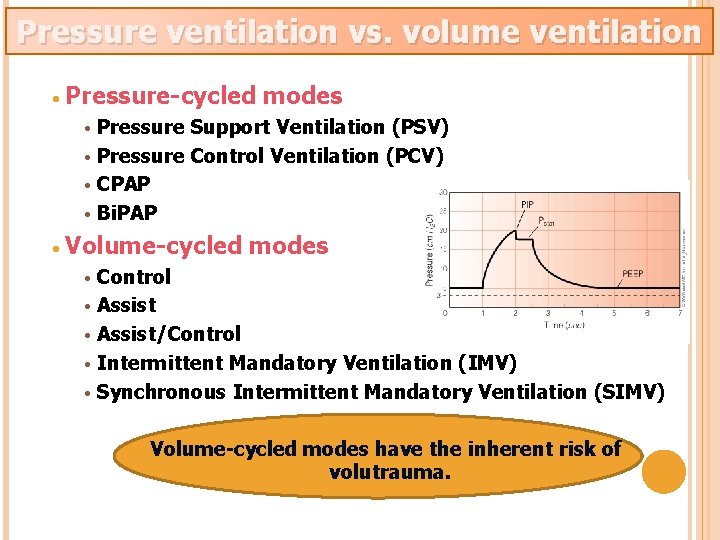
Pressure ventilation vs. volume ventilation • Pressure-cycled modes Pressure Support Ventilation (PSV) • Pressure Control Ventilation (PCV) • CPAP • Bi. PAP • • Volume-cycled modes Control • Assist/Control • Intermittent Mandatory Ventilation (IMV) • Synchronous Intermittent Mandatory Ventilation (SIMV) • Volume-cycled modes have the inherent risk of volutrauma.
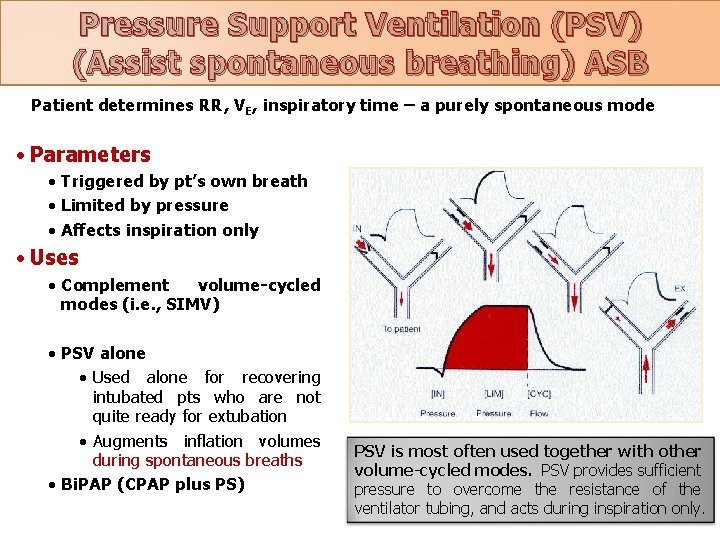
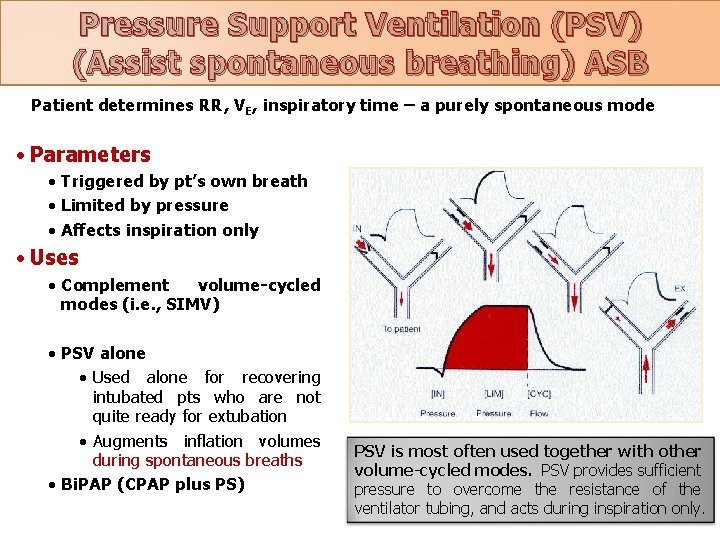
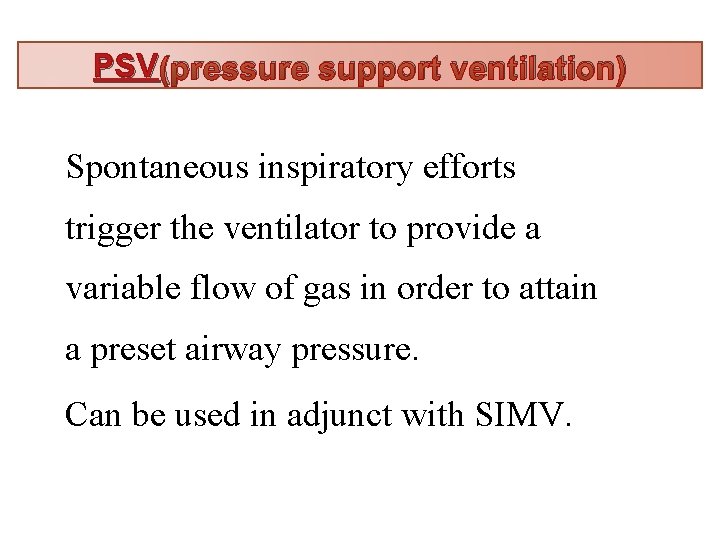
Pressure Support Ventilation (PSV) (Assist spontaneous breathing) ASB Patient determines RR, VE, inspiratory time – a purely spontaneous mode • Parameters • Triggered by pt’s own breath • Limited by pressure • Affects inspiration only • Uses • Complement volume-cycled modes (i. e. , SIMV) • PSV alone • Used alone for recovering intubated pts who are not quite ready for extubation • Augments inflation volumes during spontaneous breaths • Bi. PAP (CPAP plus PS) PSV is most often used together with other volume-cycled modes. PSV provides sufficient pressure to overcome the resistance of the ventilator tubing, and acts during inspiration only.
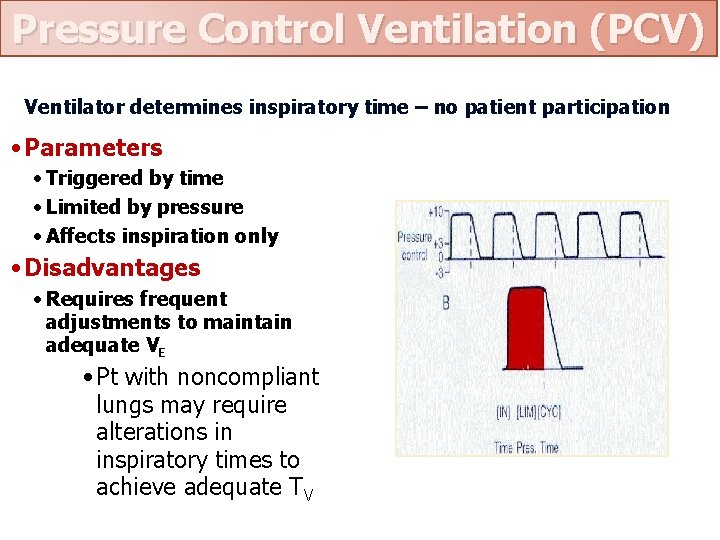
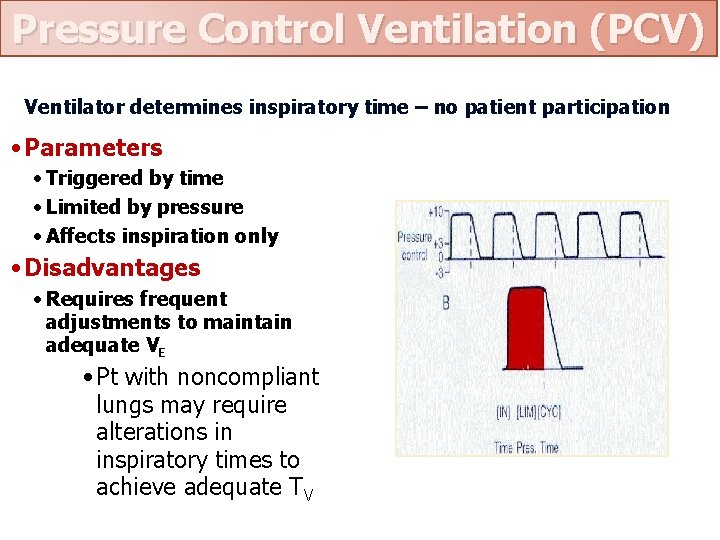
Pressure Control Ventilation (PCV) Ventilator determines inspiratory time – no patient participation • Parameters • Triggered by time • Limited by pressure • Affects inspiration only • Disadvantages • Requires frequent adjustments to maintain adequate VE • Pt with noncompliant lungs may require alterations in inspiratory times to achieve adequate TV
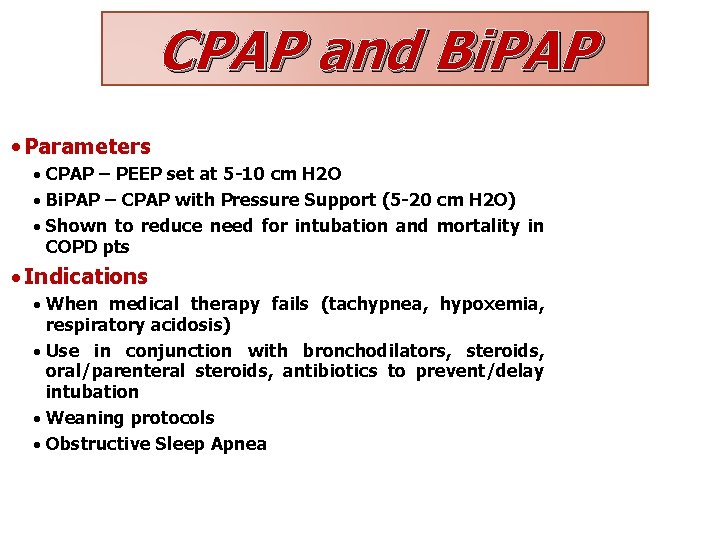
CPAP and Bi. PAP CPAP is essentially constant PEEP; Bi. PAP is CPAP plus PS • Parameters · CPAP – PEEP set at 5 -10 cm H 2 O · Bi. PAP – CPAP with Pressure Support (5 -20 cm H 2 O) · Shown to reduce need for intubation and mortality in COPD pts · Indications · When medical therapy fails (tachypnea, hypoxemia, respiratory acidosis) · Use in conjunction with bronchodilators, steroids, oral/parenteral steroids, antibiotics to prevent/delay intubation · Weaning protocols · Obstructive Sleep Apnea
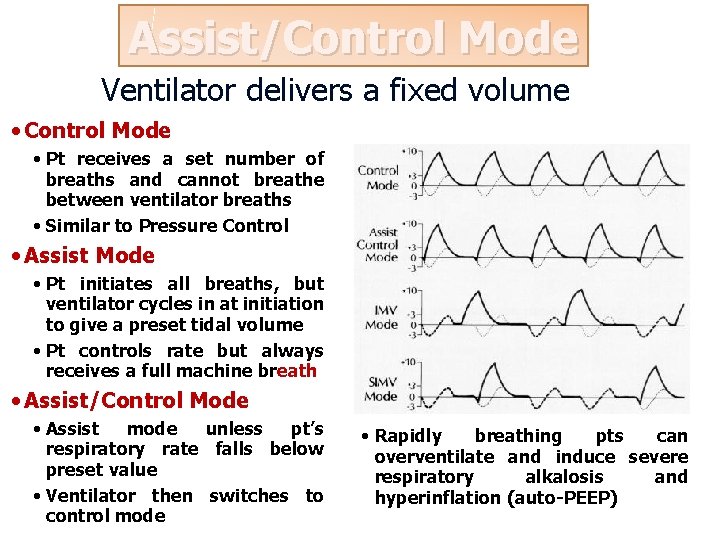
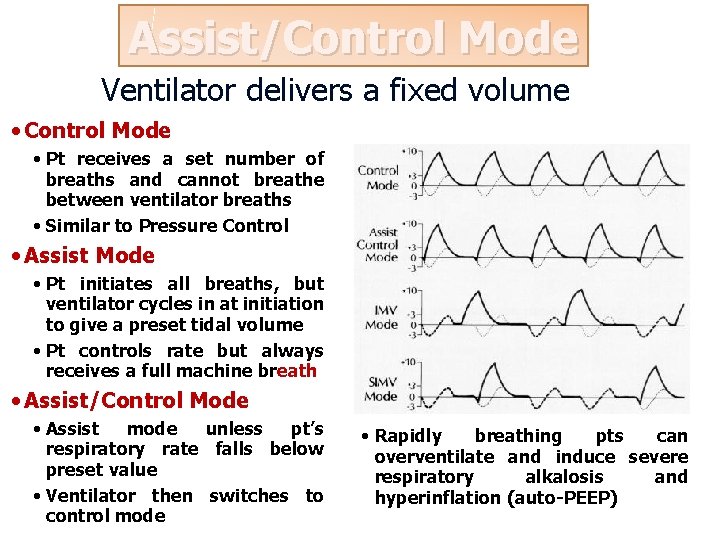
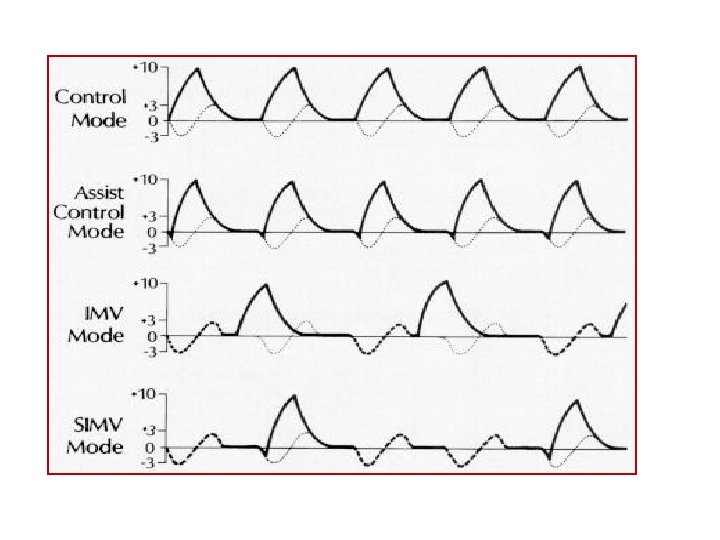
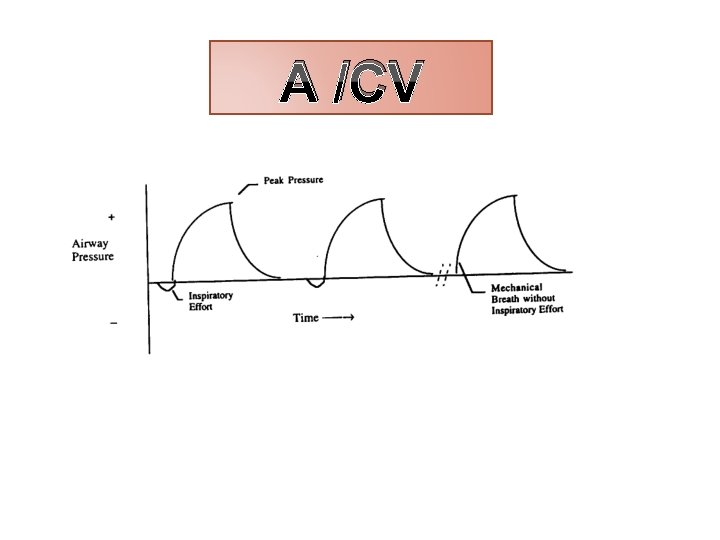
Assist/Control Mode Ventilator delivers a fixed volume • Control Mode • Pt receives a set number of breaths and cannot breathe between ventilator breaths • Similar to Pressure Control • Assist Mode • Pt initiates all breaths, but ventilator cycles in at initiation to give a preset tidal volume • Pt controls rate but always receives a full machine breath • Assist/Control Mode • Assist mode unless pt’s respiratory rate falls below preset value • Ventilator then switches to control mode • Rapidly breathing pts can overventilate and induce severe respiratory alkalosis and hyperinflation (auto-PEEP)
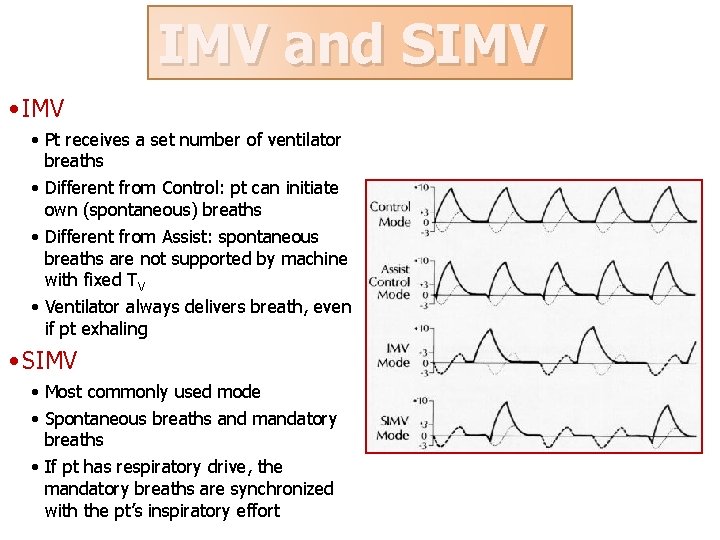
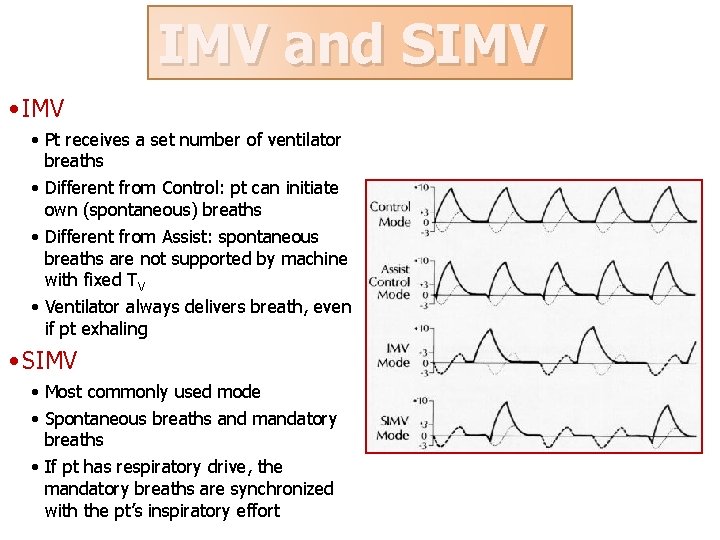
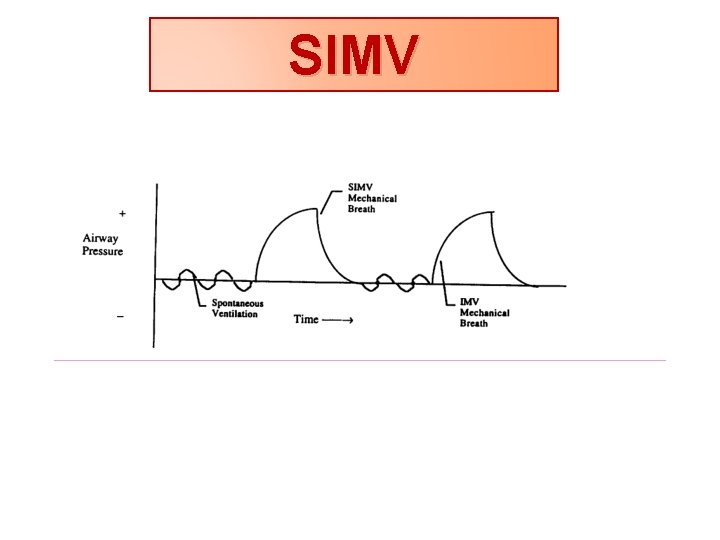
IMV and SIMV • Pt receives a set number of ventilator breaths • Different from Control: pt can initiate own (spontaneous) breaths • Different from Assist: spontaneous breaths are not supported by machine with fixed TV • Ventilator always delivers breath, even if pt exhaling • SIMV • Most commonly used mode • Spontaneous breaths and mandatory breaths • If pt has respiratory drive, the mandatory breaths are synchronized with the pt’s inspiratory effort
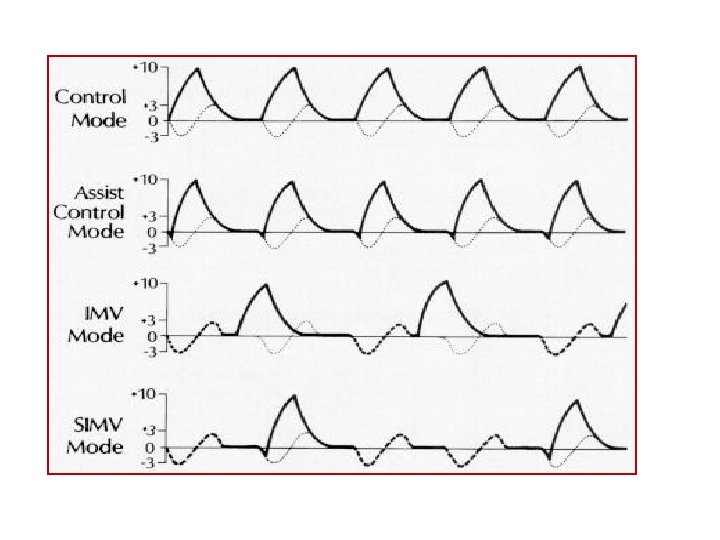
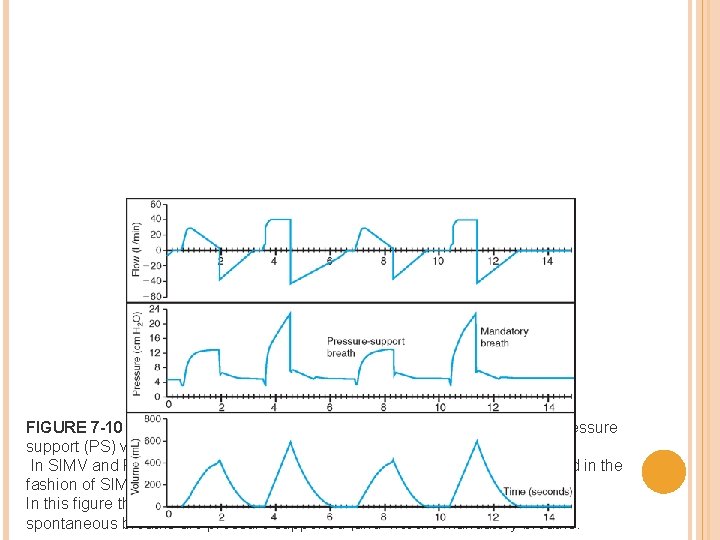
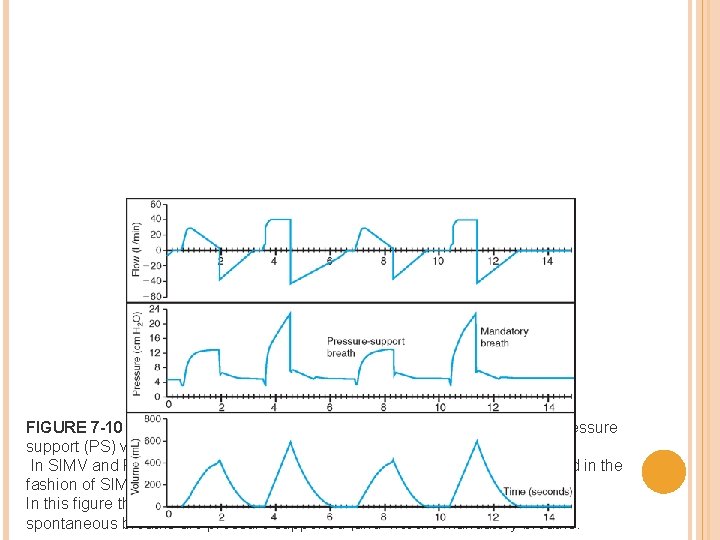
FIGURE 7 -10 Synchronized intermittent mandatory ventilation (SIMV) with pressure support (PS) ventilation. In SIMV and PS, mandatory breaths of a preset tidal volume are administered in the fashion of SIMV. In this figure the square waveform is applied to the mandatory breaths. Only spontaneous breaths are pressure supported , and not the mandatory breaths.
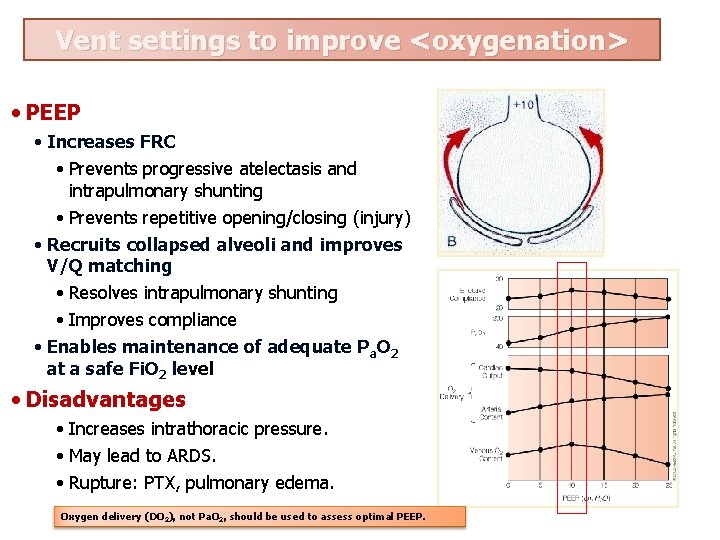
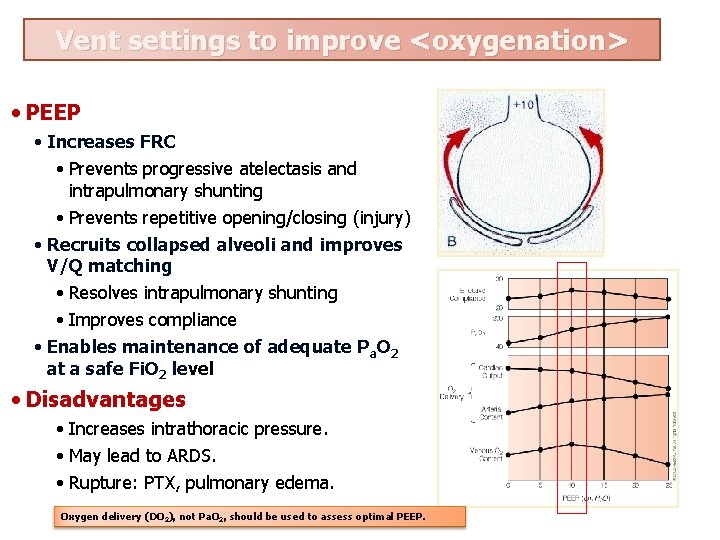
Vent settings to improve <oxygenation> • PEEP • Increases FRC • Prevents progressive atelectasis and intrapulmonary shunting • Prevents repetitive opening/closing (injury) • Recruits collapsed alveoli and improves V/Q matching • Resolves intrapulmonary shunting • Improves compliance • Enables maintenance of adequate Pa. O 2 at a safe Fi. O 2 level • Disadvantages • Increases intrathoracic pressure. • May lead to ARDS. • Rupture: PTX, pulmonary edema. Oxygen delivery (DO 2), not Pa. O 2, should be used to assess optimal PEEP.
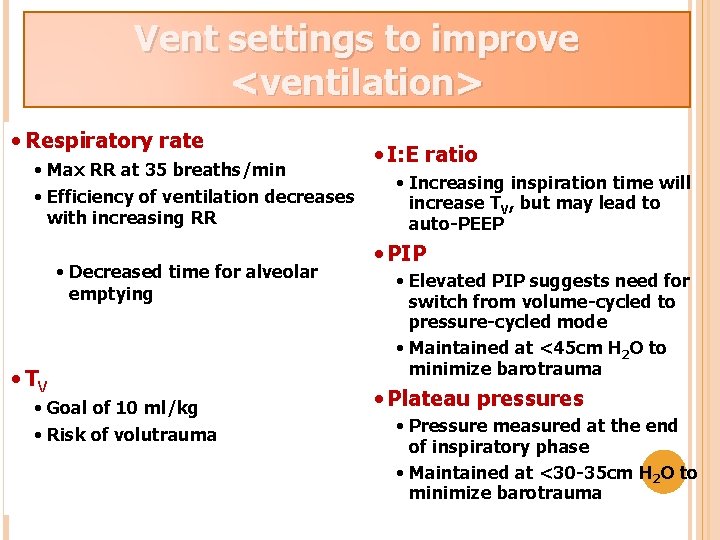
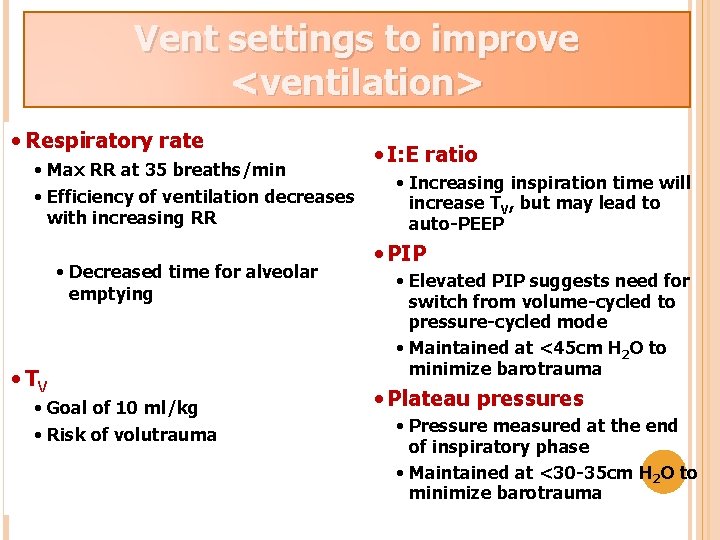
Vent settings to improve <ventilation> RR and T are adjusted to maintain V and P CO V • Respiratory rate • Max RR at 35 breaths/min • Efficiency of ventilation decreases with increasing RR • Decreased time for alveolar emptying • TV • Goal of 10 ml/kg • Risk of volutrauma E a 2 • I: E ratio • Increasing inspiration time will increase TV, but may lead to auto-PEEP • PIP • Elevated PIP suggests need for switch from volume-cycled to pressure-cycled mode • Maintained at <45 cm H 2 O to minimize barotrauma • Plateau pressures • Pressure measured at the end of inspiratory phase • Maintained at <30 -35 cm H 2 O to minimize barotrauma
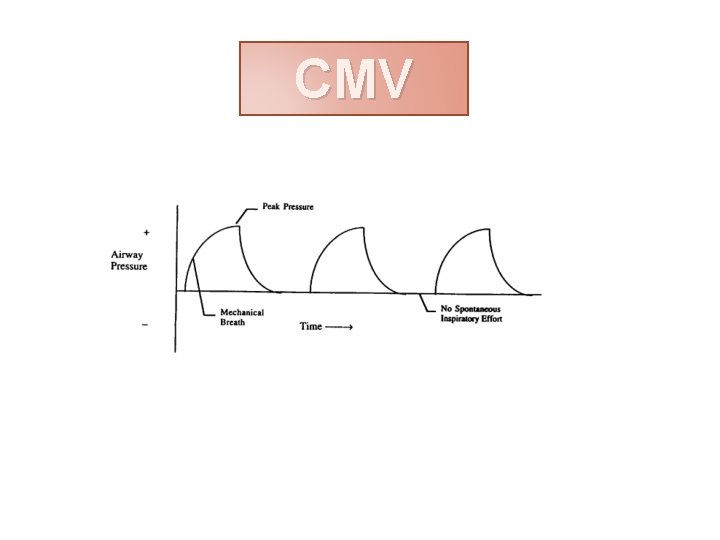
CMV
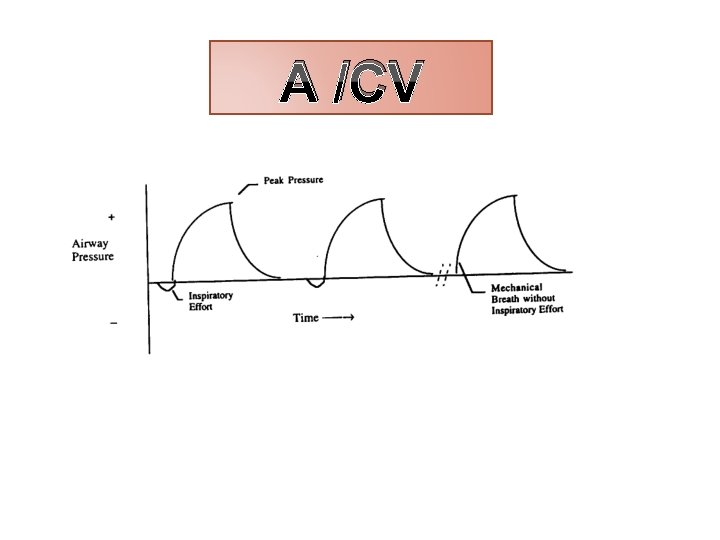
A /CV
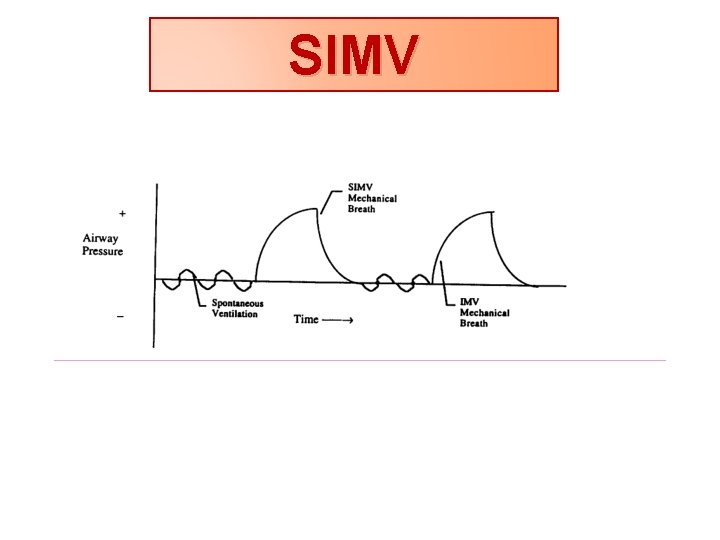
SIMV
PSV (pressure support ventilation) Spontaneous inspiratory efforts trigger the ventilator to provide a variable flow of gas in order to attain a preset airway pressure. Can be used in adjunct with SIMV.
MONITORING OF THE PATIENT
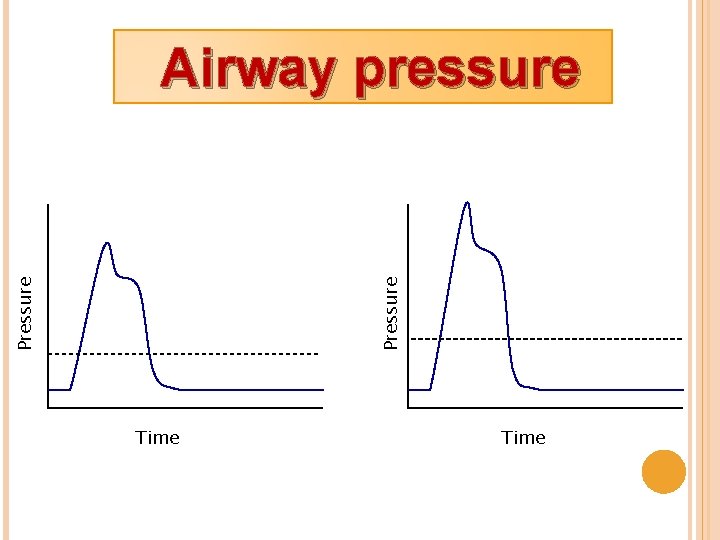
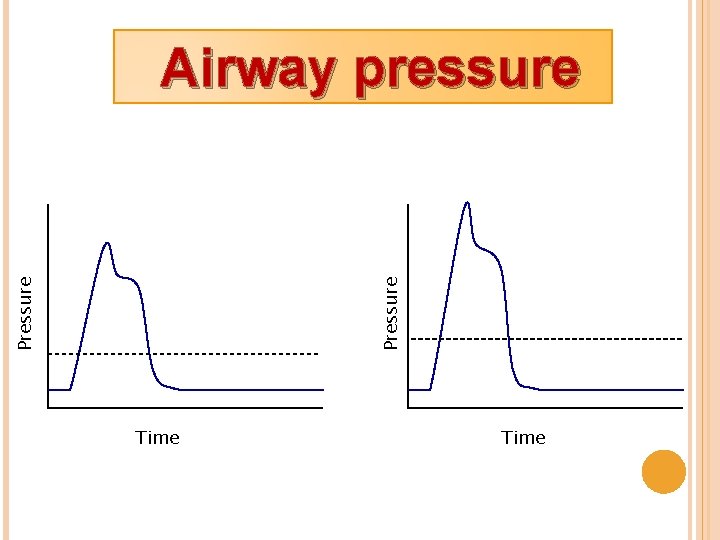
Pressure Airway pressure Time
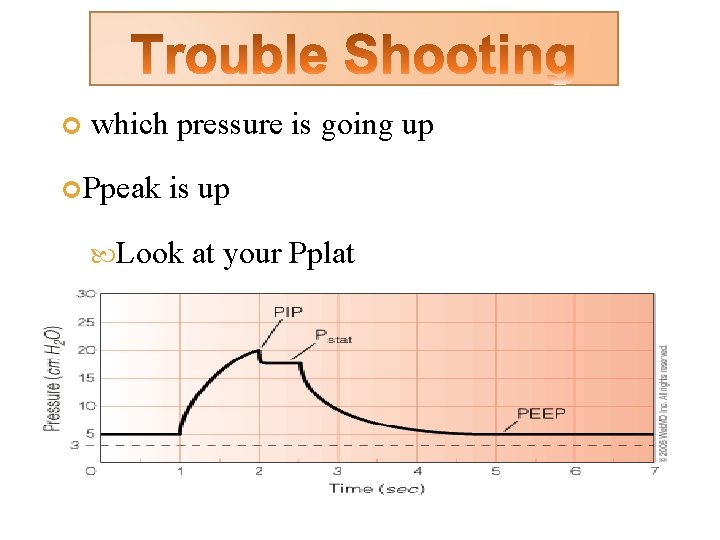
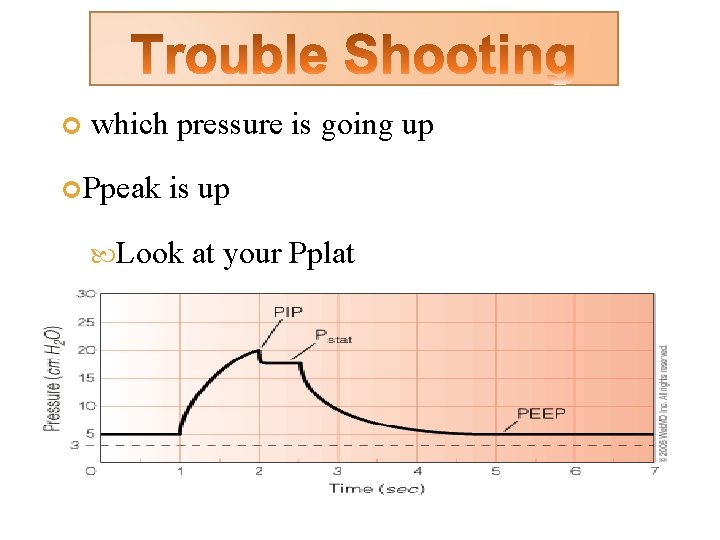
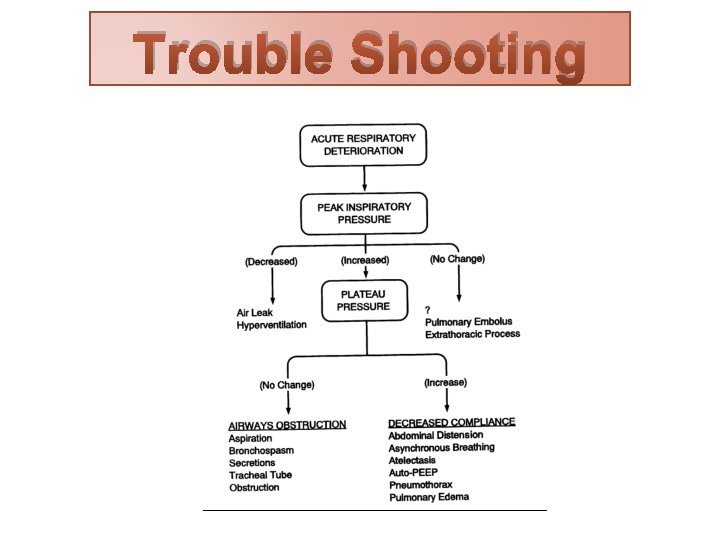
which pressure is going up Ppeak is up Look at your Pplat
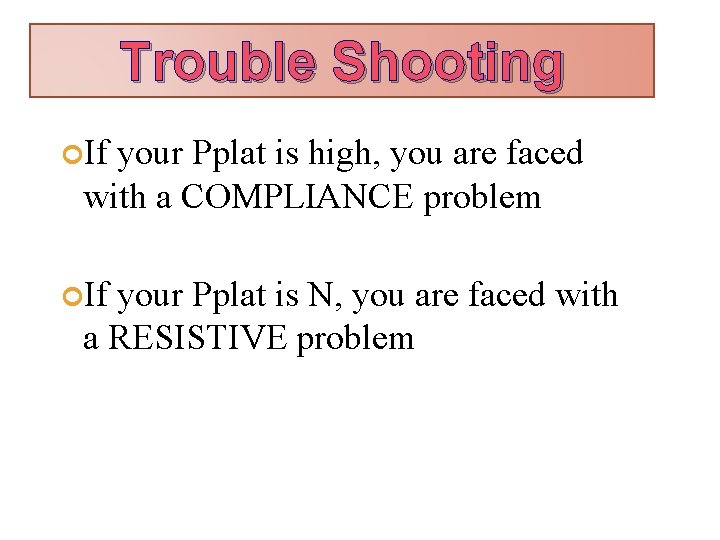
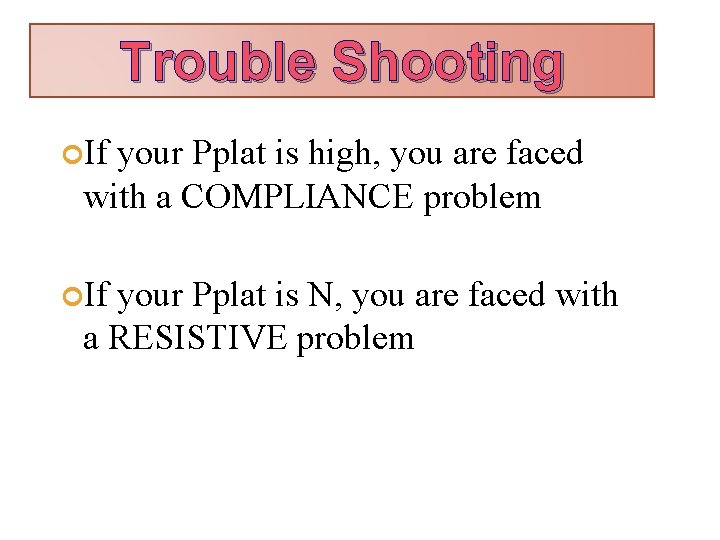
Trouble Shooting If your Pplat is high, you are faced with a COMPLIANCE problem If your Pplat is N, you are faced with a RESISTIVE problem
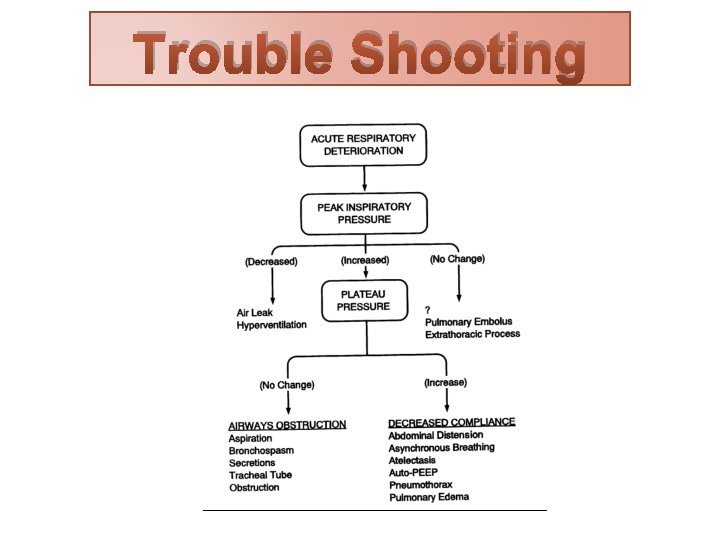
Trouble Shooting
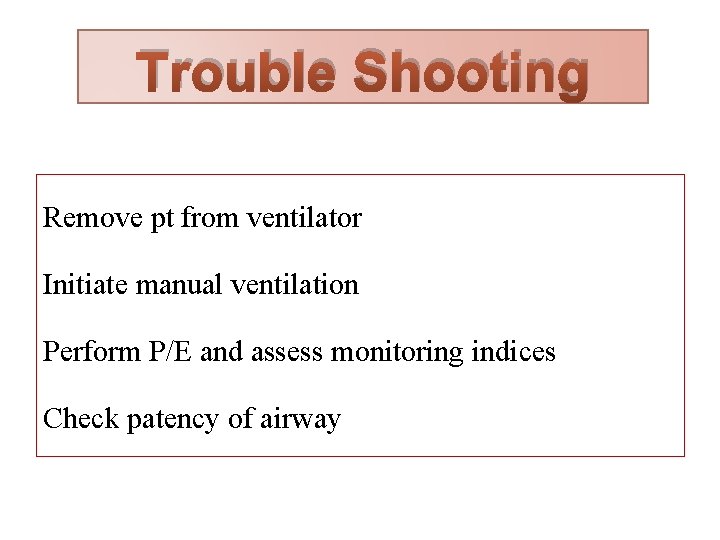
Trouble Shooting Remove pt from ventilator Initiate manual ventilation Perform P/E and assess monitoring indices Check patency of airway
Conclusion Ventilator settings Monitoring Trouble of the patient shooting

Chronic Obstructive Pulmonary Disease and Weaning of Difficult-to -wean Patients from Mechanical Ventilation: Randomized Prospective Study. Croat Med J 2007; 48: 51 -58

Thanks For Your Atention