Presentation Management Of Common Thoracic Diseases Dr Waseem


























- Slides: 87
Presentation &Management Of Common Thoracic Diseases Dr. Waseem HAJJAR MD, FRCS, Assistant Professor & Consultant thoracic surgeon edited by: Rowayda Mishiddi Revised by: Bilal Marwa

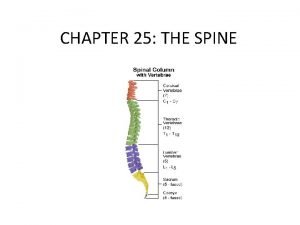
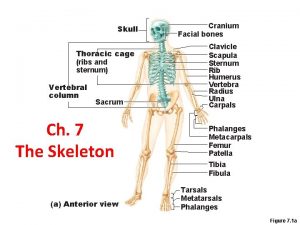
The Lung Ø Embryology § Bronchial system § Alveolar system Ø Anatomy § Lobes § Fissures § Segments § Blood supply
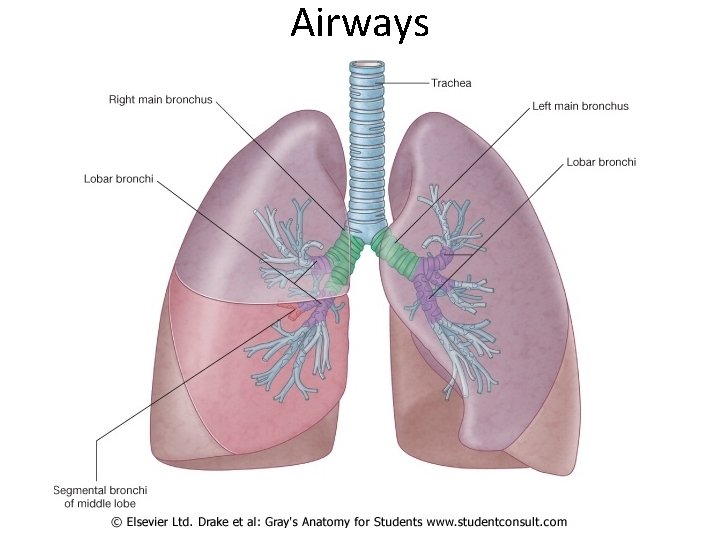
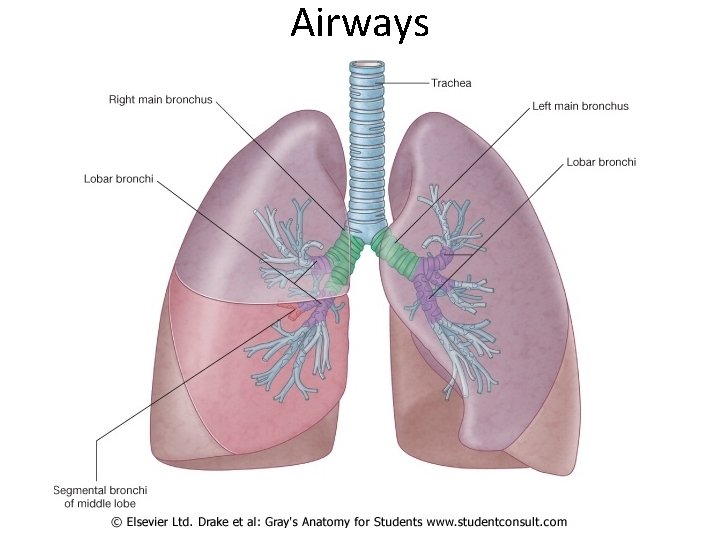
Airways
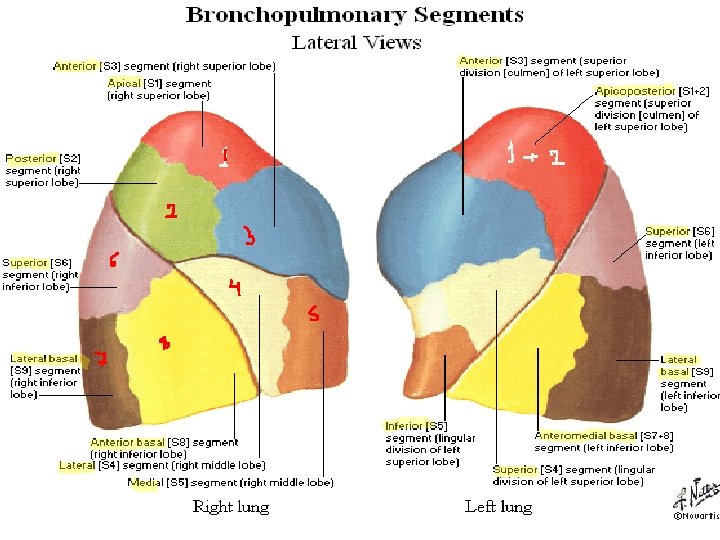
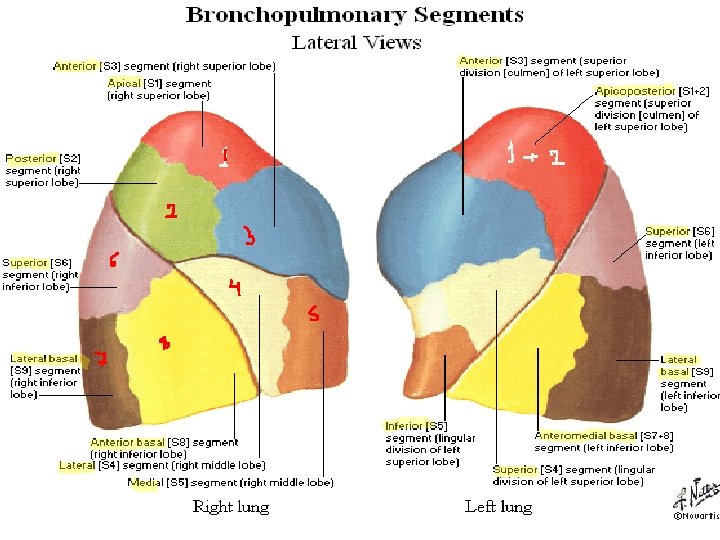
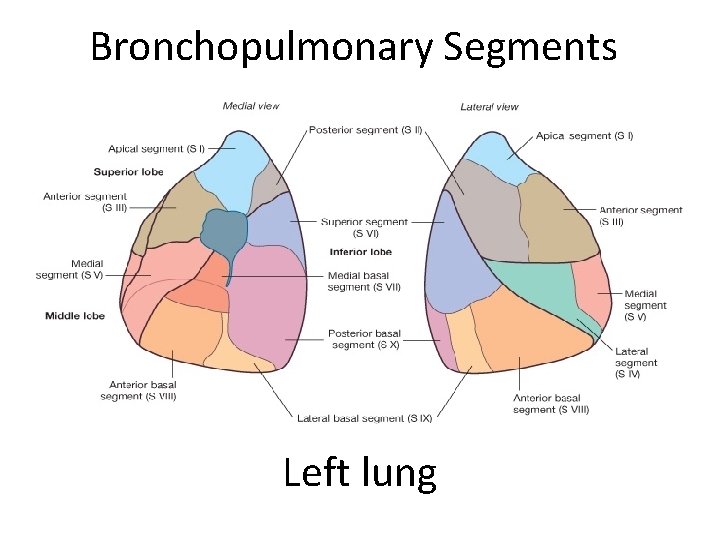
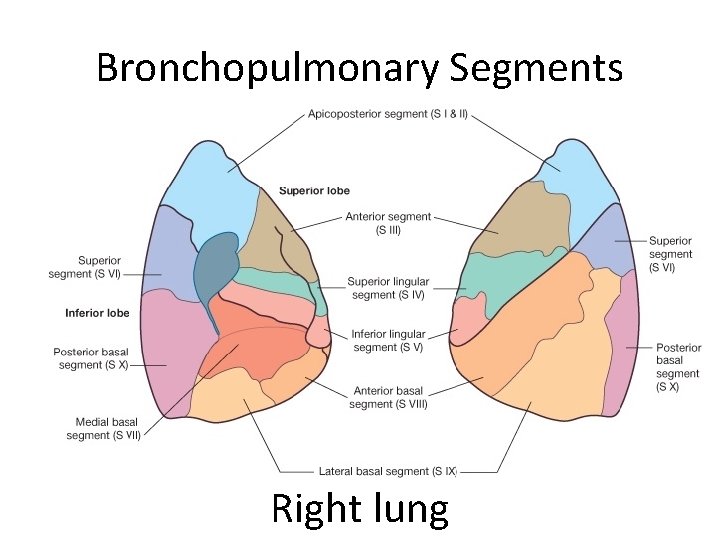
Bronchopulmonary Segments
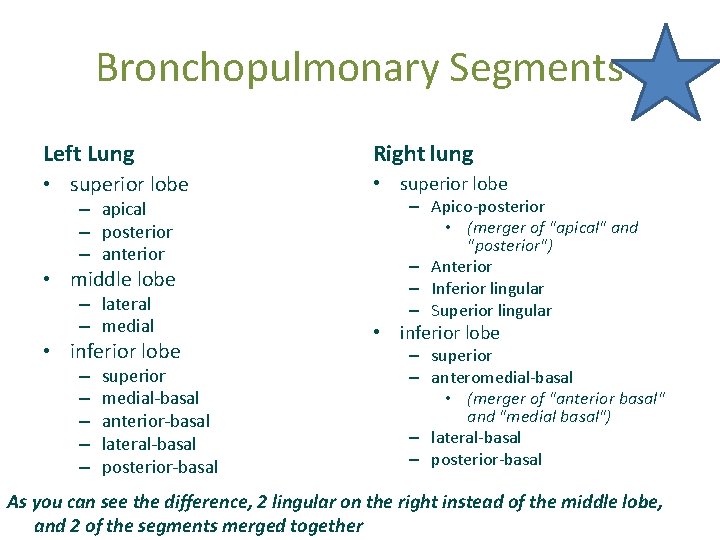
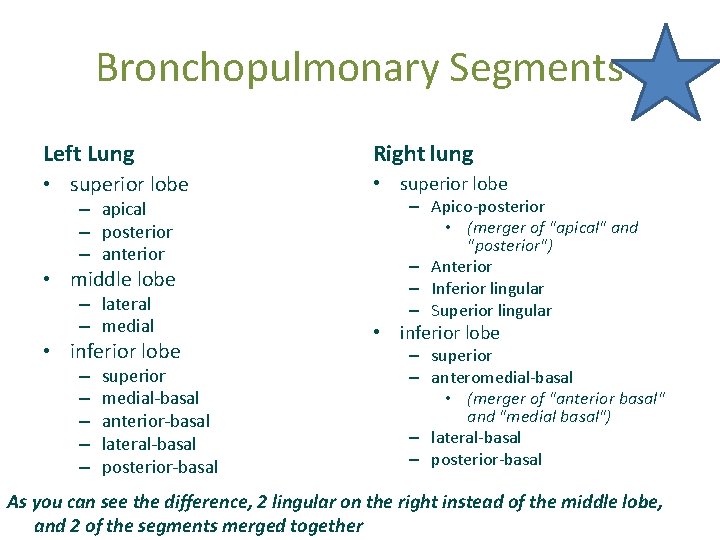
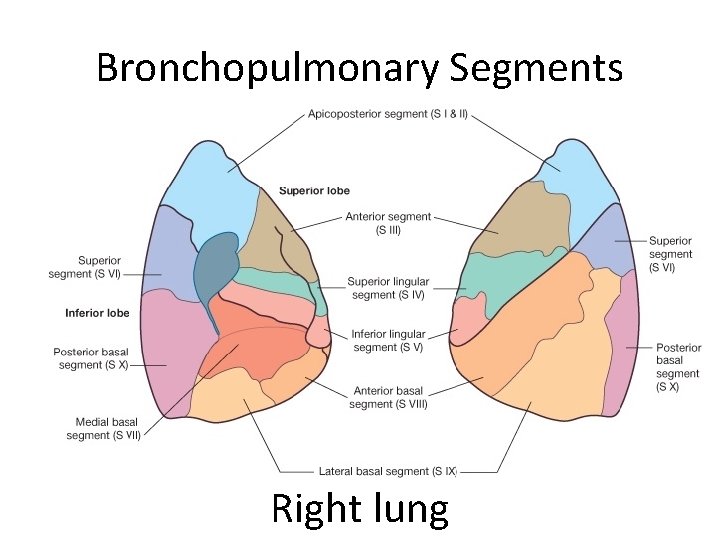
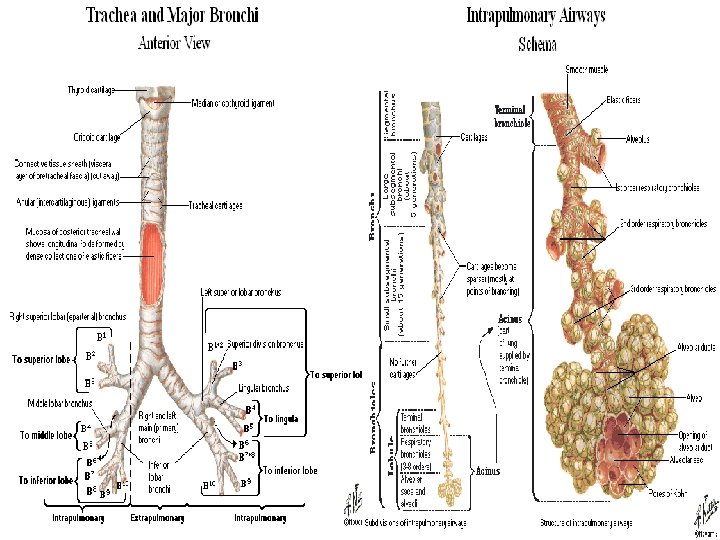
Bronchopulmonary Segments Left Lung Right lung • superior lobe – apical – posterior – anterior • middle lobe – lateral – medial • inferior lobe – – – superior medial-basal anterior-basal lateral-basal posterior-basal – Apico-posterior • (merger of "apical" and "posterior") – Anterior – Inferior lingular – Superior lingular • inferior lobe – superior – anteromedial-basal • (merger of "anterior basal" and "medial basal") – lateral-basal – posterior-basal As you can see the difference, 2 lingular on the right instead of the middle lobe, and 2 of the segments merged together
Bronchopulmonary Segments Right lung
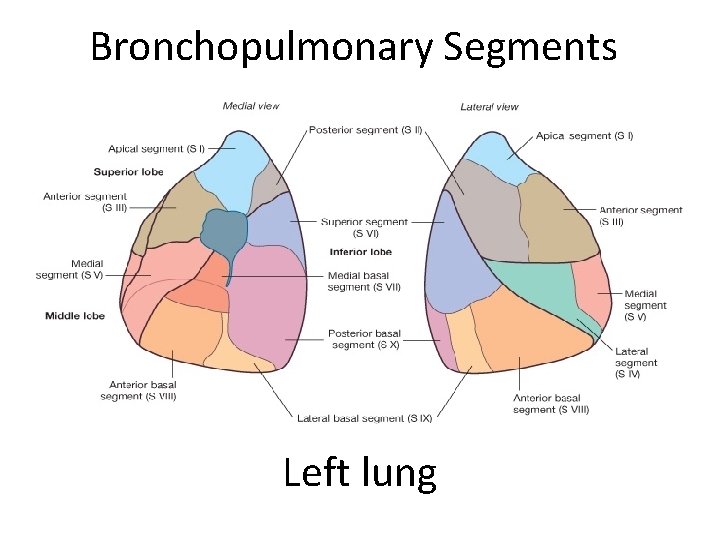
Bronchopulmonary Segments Left lung
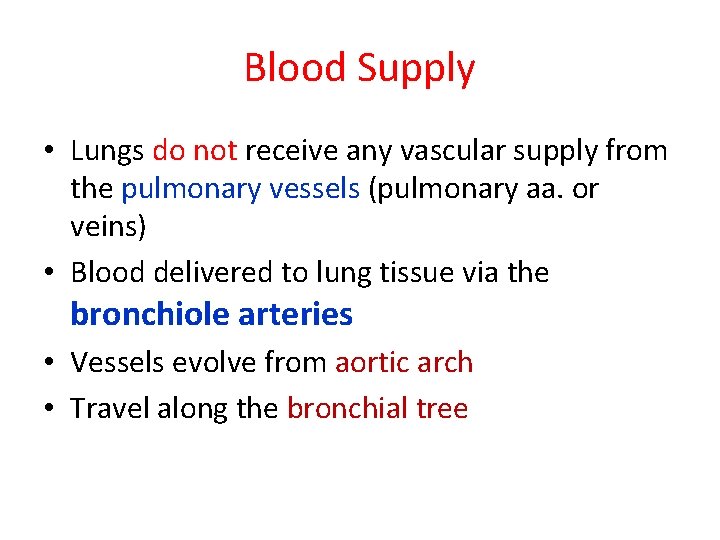
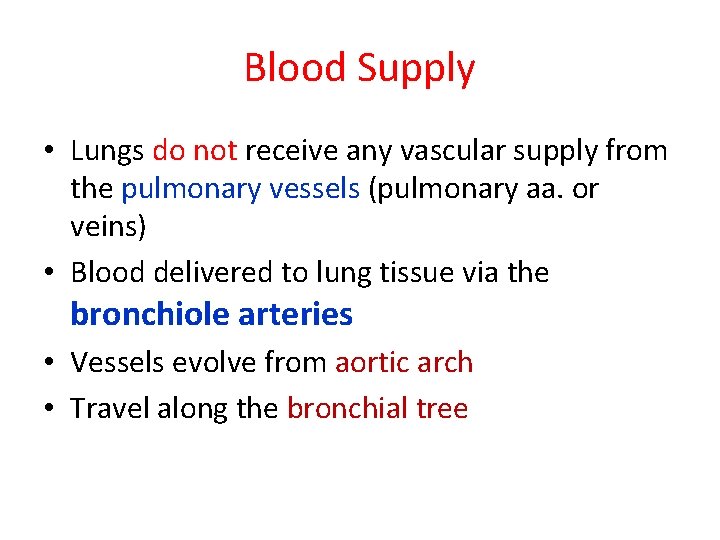
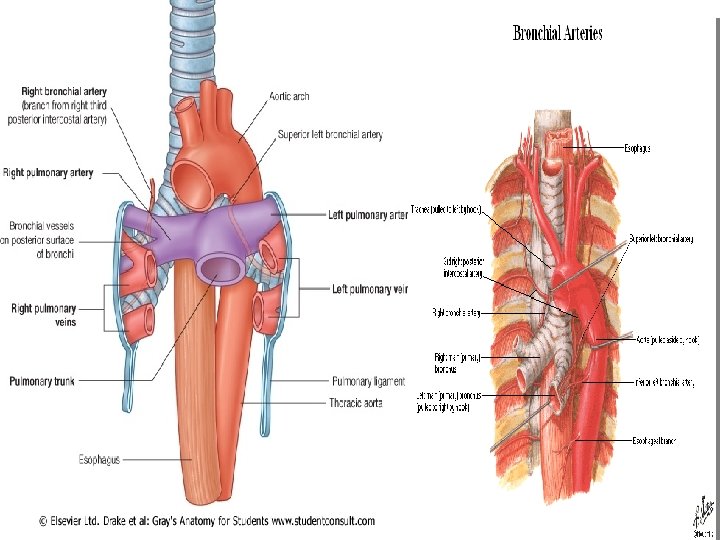
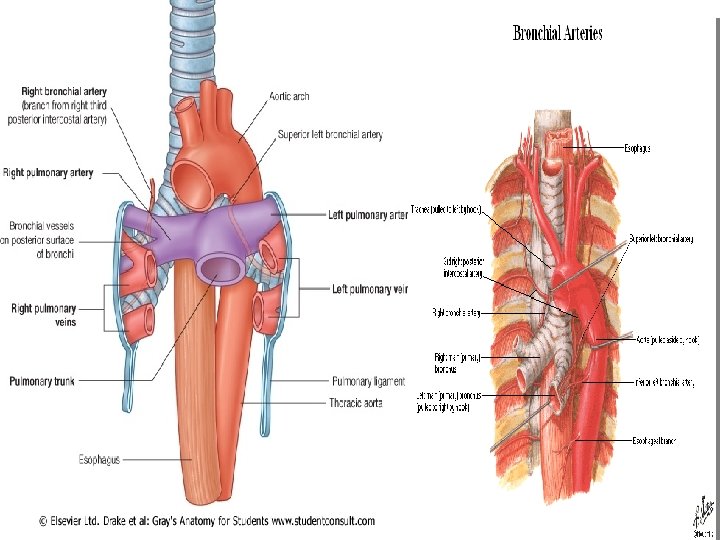
Blood Supply • Lungs do not receive any vascular supply from the pulmonary vessels (pulmonary aa. or veins) • Blood delivered to lung tissue via the bronchiole arteries • Vessels evolve from aortic arch • Travel along the bronchial tree
Blood Supply
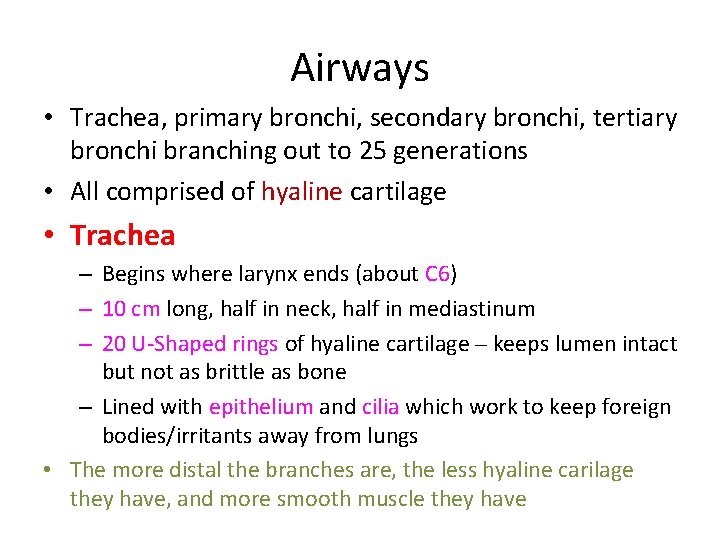
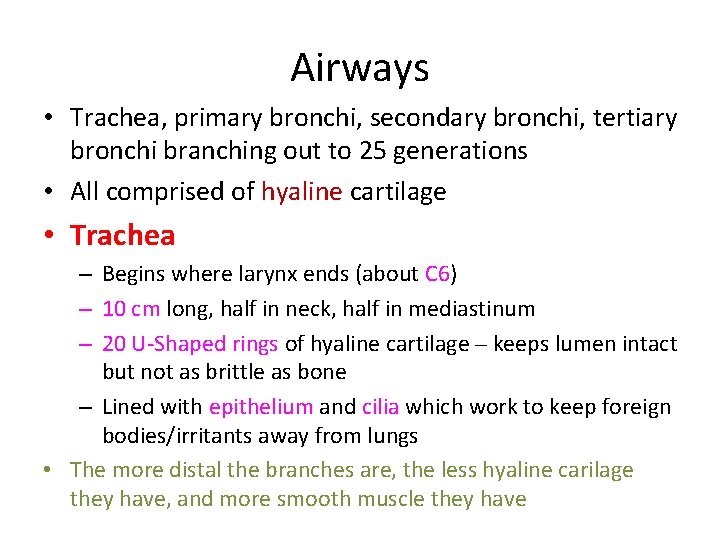
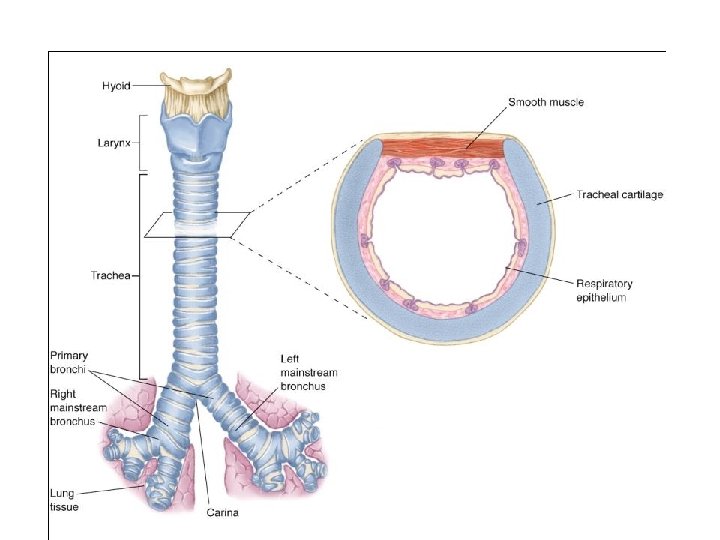
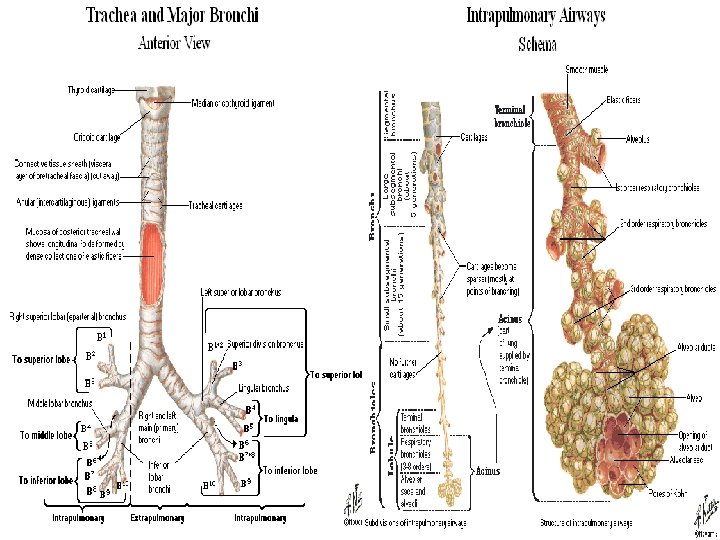
Airways • Trachea, primary bronchi, secondary bronchi, tertiary bronchi branching out to 25 generations • All comprised of hyaline cartilage • Trachea – Begins where larynx ends (about C 6) – 10 cm long, half in neck, half in mediastinum – 20 U-Shaped rings of hyaline cartilage – keeps lumen intact but not as brittle as bone – Lined with epithelium and cilia which work to keep foreign bodies/irritants away from lungs • The more distal the branches are, the less hyaline carilage they have, and more smooth muscle they have
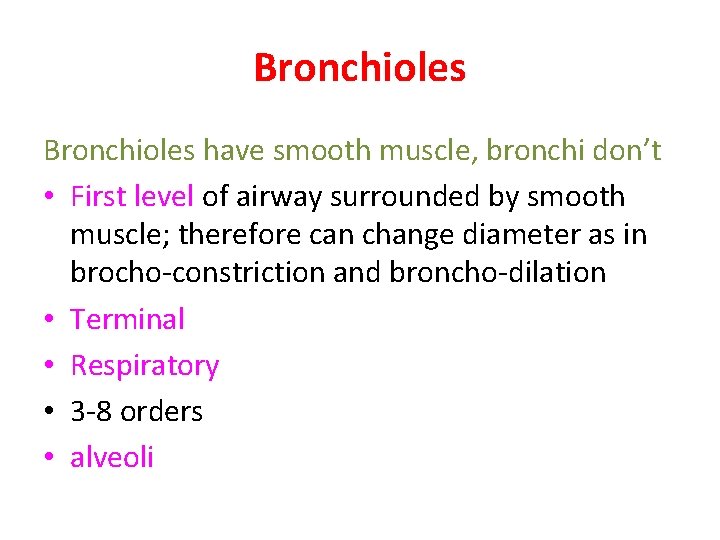
Bronchioles have smooth muscle, bronchi don’t • First level of airway surrounded by smooth muscle; therefore can change diameter as in brocho-constriction and broncho-dilation • Terminal • Respiratory • 3 -8 orders • alveoli
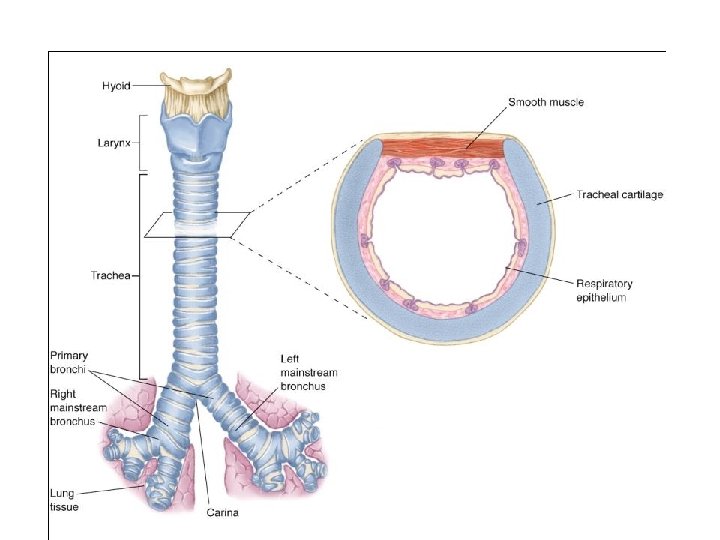

Carina and primary bronchi • Right Primary Bronchus is shorter, wider, and more steep. • Left Primary Bronchus is longer, more narrow, and less steep.
Airways
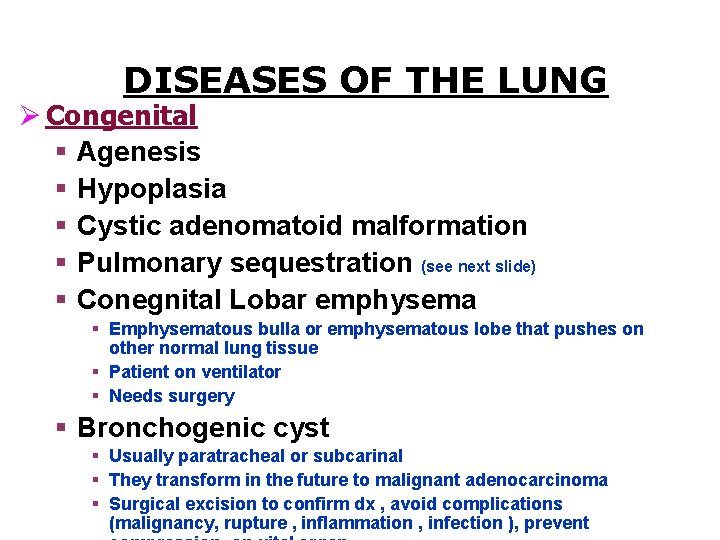
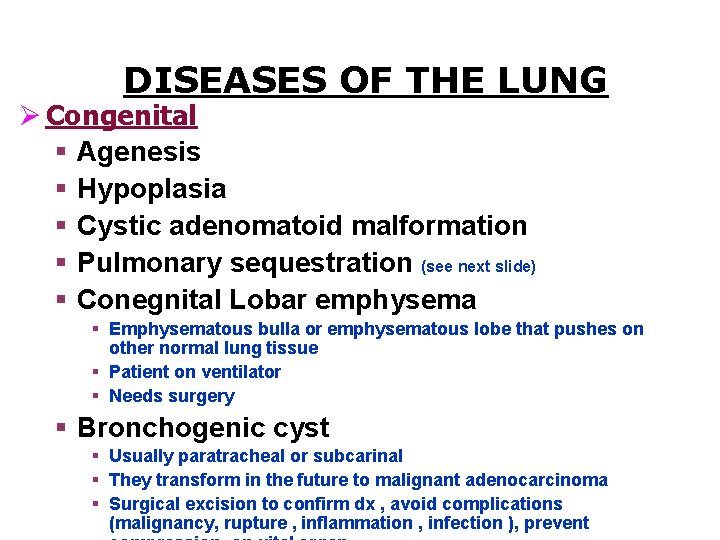
DISEASES OF THE LUNG Ø Congenital § Agenesis § Hypoplasia § Cystic adenomatoid malformation § Pulmonary sequestration (see next slide) § Conegnital Lobar emphysema § Emphysematous bulla or emphysematous lobe that pushes on other normal lung tissue § Patient on ventilator § Needs surgery § Bronchogenic cyst § Usually paratracheal or subcarinal § They transform in the future to malignant adenocarcinoma § Surgical excision to confirm dx , avoid complications (malignancy, rupture , inflammation , infection ), prevent
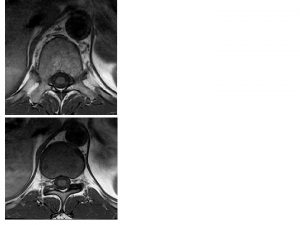
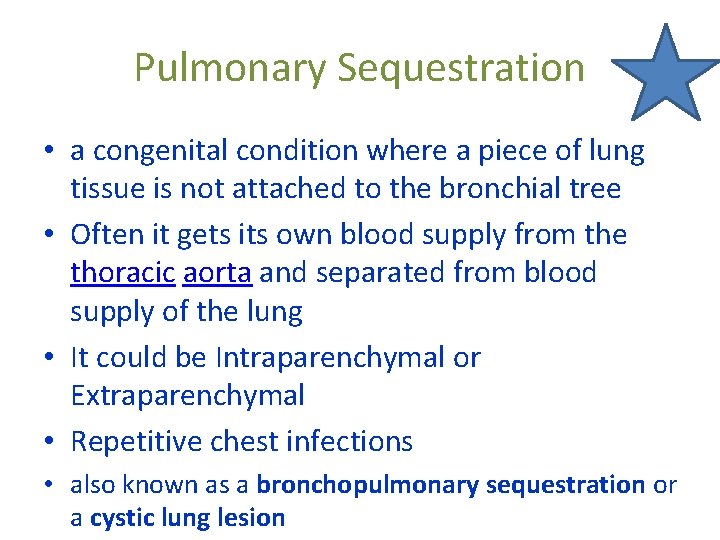
Pulmonary Sequestration • a congenital condition where a piece of lung tissue is not attached to the bronchial tree • Often it gets its own blood supply from the thoracic aorta and separated from blood supply of the lung • It could be Intraparenchymal or Extraparenchymal • Repetitive chest infections • also known as a bronchopulmonary sequestration or a cystic lung lesion

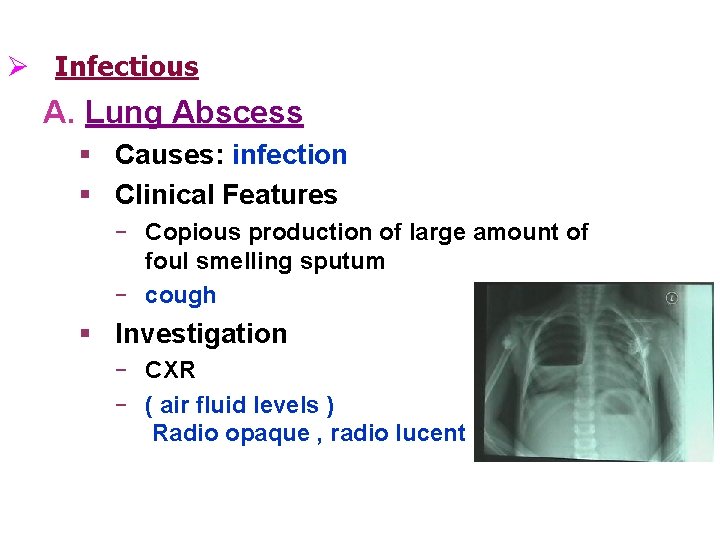
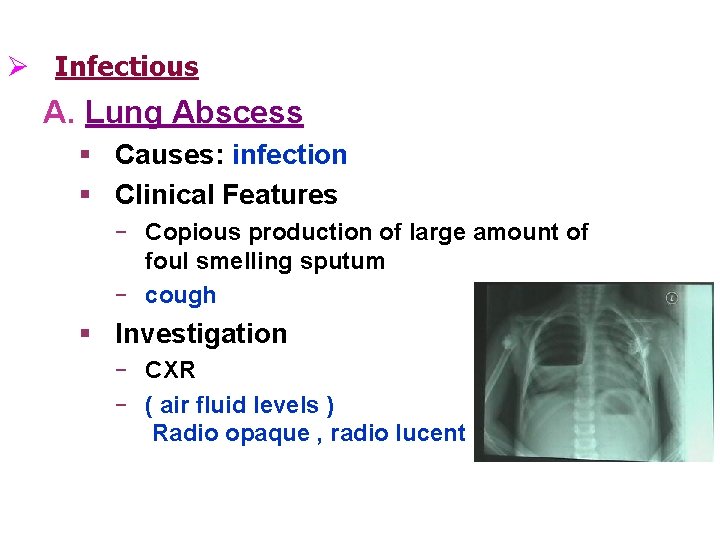
Ø Infectious A. Lung Abscess § Causes: infection § Clinical Features ‒ Copious production of large amount of foul smelling sputum ‒ cough § Investigation ‒ CXR ‒ ( air fluid levels ) Radio opaque , radio lucent
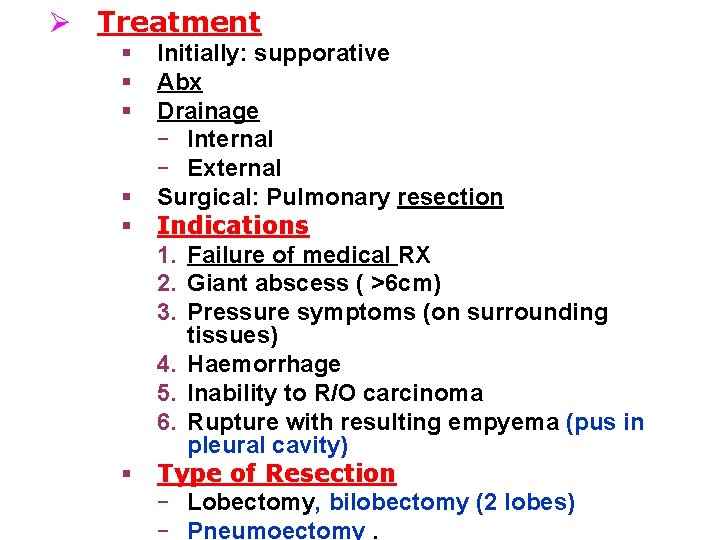
Ø Treatment § § § Initially: supporative Abx Drainage ‒ Internal ‒ External Surgical: Pulmonary resection Indications 1. Failure of medical RX 2. Giant abscess ( >6 cm) 3. Pressure symptoms (on surrounding tissues) 4. Haemorrhage 5. Inability to R/O carcinoma 6. Rupture with resulting empyema (pus in pleural cavity) Type of Resection ‒ Lobectomy, bilobectomy (2 lobes) ‒ Pneumoectomy.
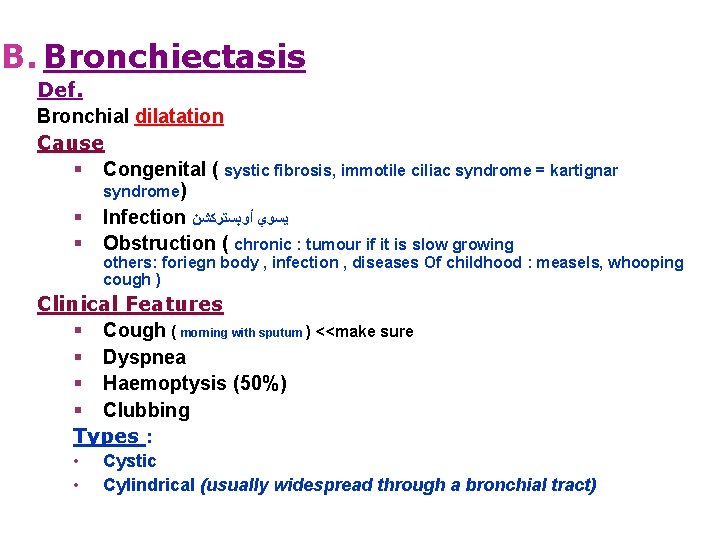
B. Bronchiectasis Def. Bronchial dilatation Cause § Congenital ( systic fibrosis, immotile ciliac syndrome = kartignar syndrome) § Infection ﻳﺴﻮﻱ ﺃﻮﺑﺴﺘﺮﻛﺸﻦ § Obstruction ( chronic : tumour if it is slow growing others: foriegn body , infection , diseases Of childhood : measels, whooping cough ) Clinical Features § Cough ( morning with sputum ) <<make sure § Dyspnea § Haemoptysis (50%) § Clubbing Types : • • Cystic Cylindrical (usually widespread through a bronchial tract)
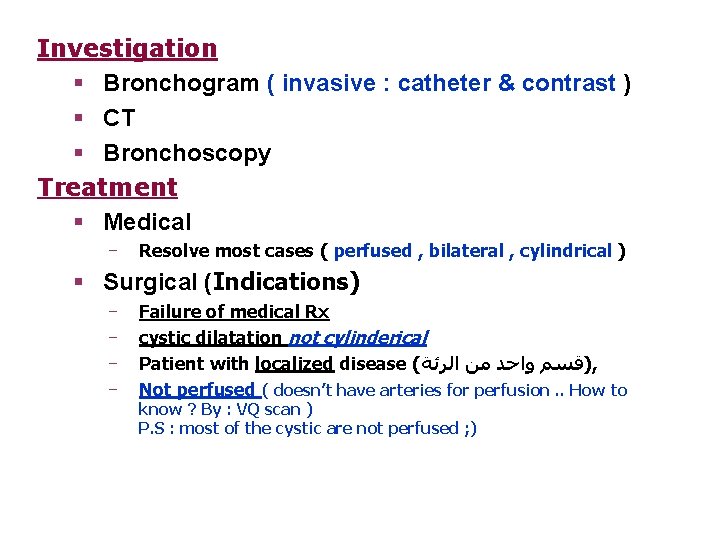
Investigation § Bronchogram ( invasive : catheter & contrast ) § CT § Bronchoscopy Treatment § Medical ‒ Resolve most cases ( perfused , bilateral , cylindrical ) § Surgical (Indications) ‒ ‒ Failure of medical Rx cystic dilatation not cylinderical Patient with localized disease ( )ﻗﺴﻢ ﻭﺍﺣﺪ ﻣﻦ ﺍﻟﺮﺋﺔ , Not perfused ( doesn’t have arteries for perfusion. . How to know ? By : VQ scan ) P. S : most of the cystic are not perfused ; )


Indications for surgery in this case of Left Lower Bronchiectasis ‒ ‒ ‒ cystic dilatation. localized Not perfused ( by VQ scan )
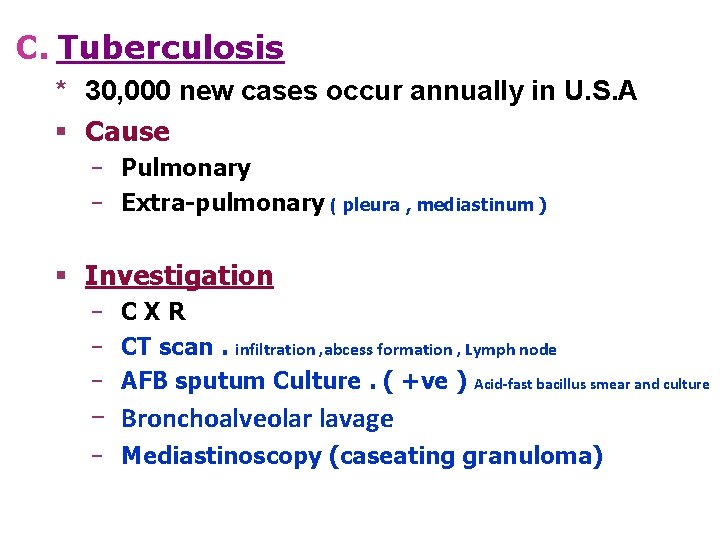
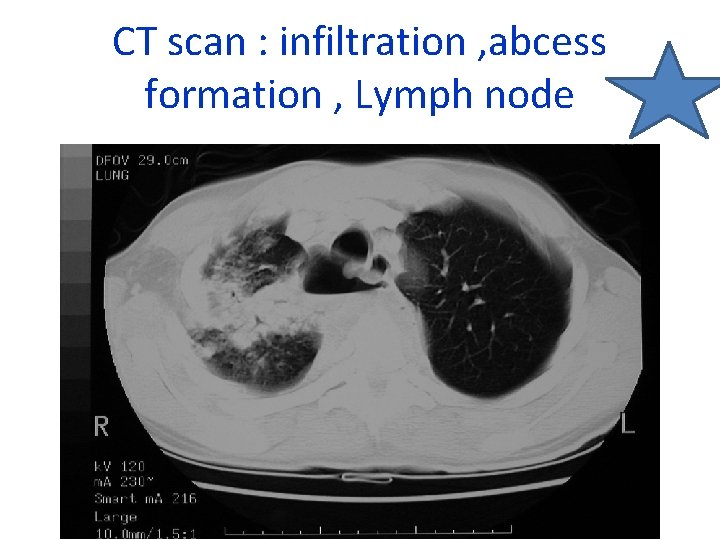
C. Tuberculosis * 30, 000 new cases occur annually in U. S. A § Cause ‒ Pulmonary ‒ Extra-pulmonary ( pleura , mediastinum ) § Investigation ‒ CXR ‒ CT scan. infiltration , abcess formation , Lymph node ‒ AFB sputum Culture. ( +ve ) Acid-fast bacillus smear and culture ‒ Bronchoalveolar lavage ‒ Mediastinoscopy (caseating granuloma)
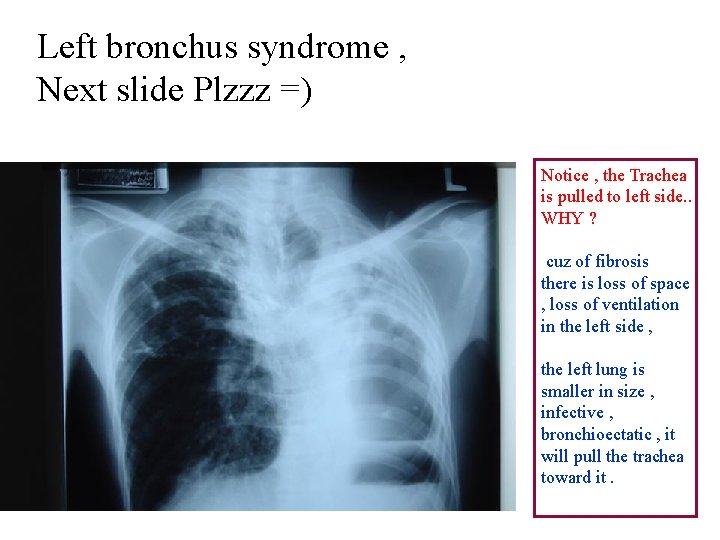
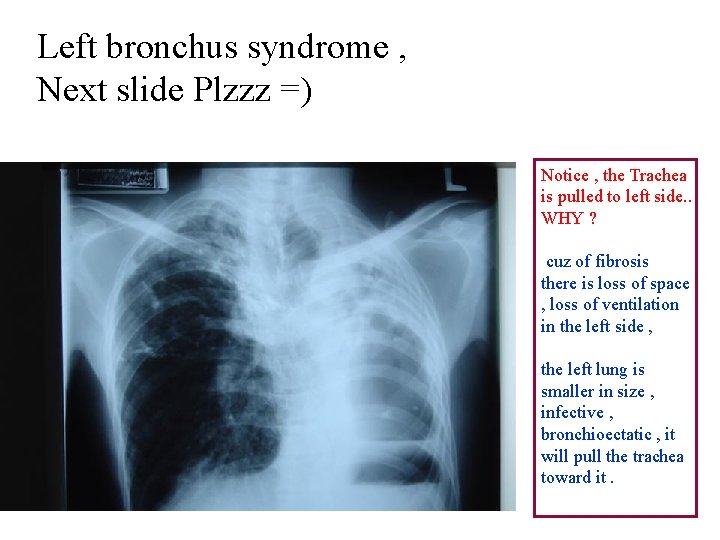
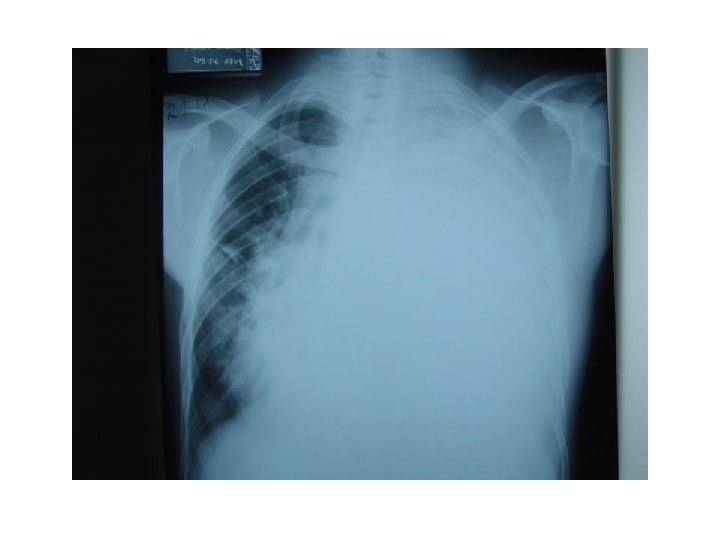
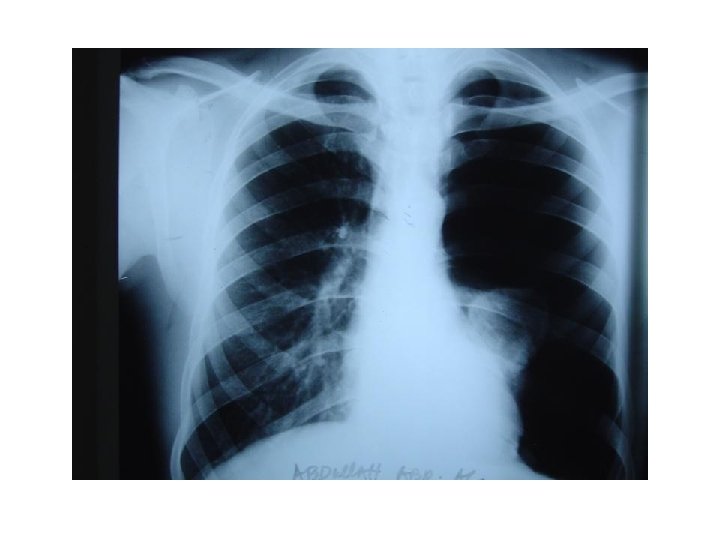
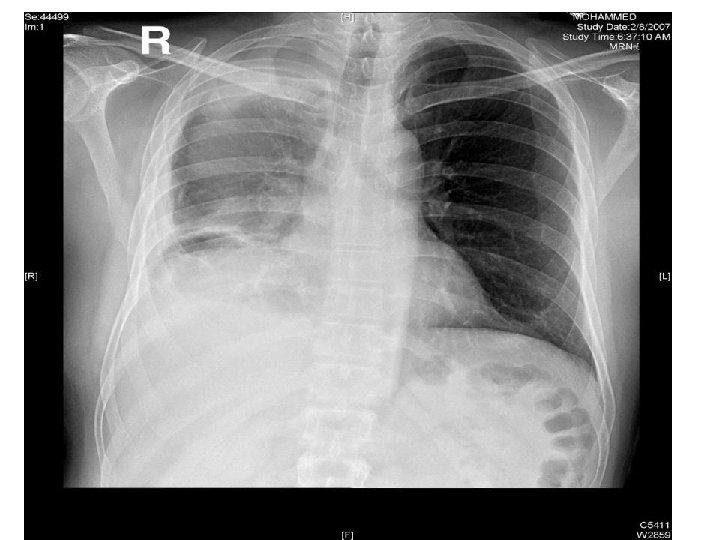
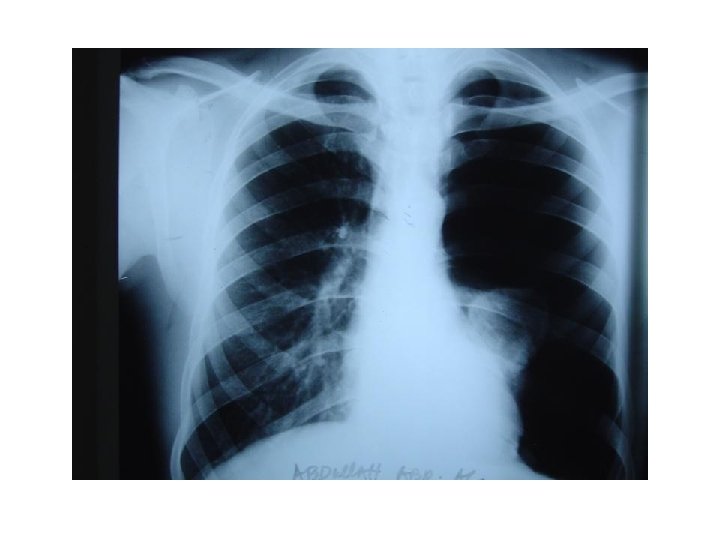
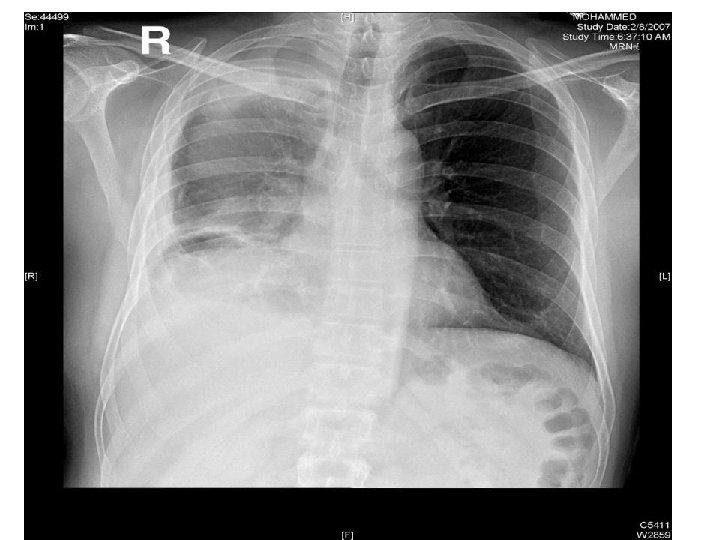
Left bronchus syndrome , Next slide Plzzz =) Notice , the Trachea is pulled to left side. . WHY ? cuz of fibrosis there is loss of space , loss of ventilation in the left side , the left lung is smaller in size , infective , bronchioectatic , it will pull the trachea toward it.
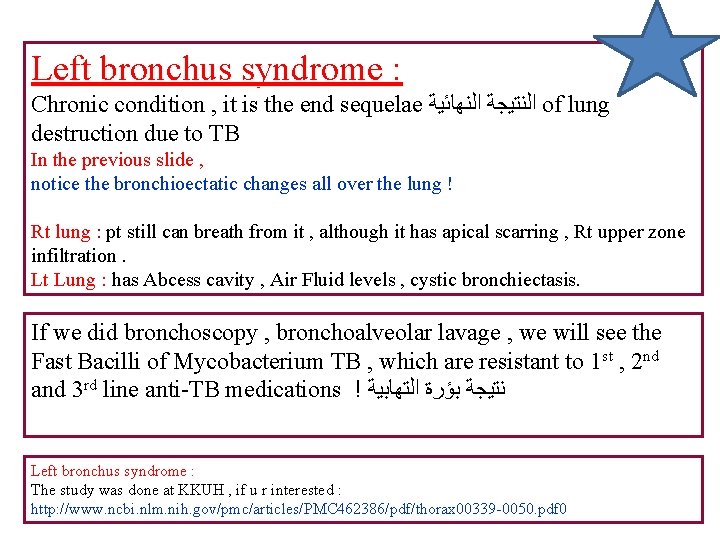
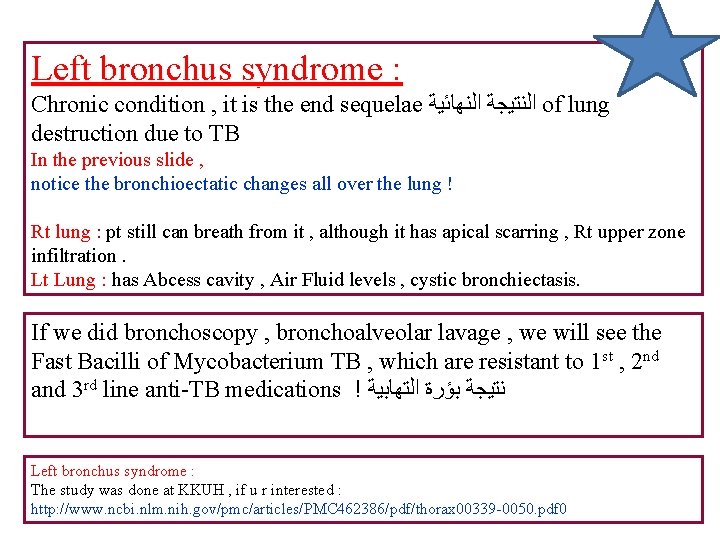
Left bronchus syndrome : Chronic condition , it is the end sequelae ﺍﻟﻨﺘﻴﺠﺔ ﺍﻟﻨﻬﺎﺋﻴﺔ of lung destruction due to TB In the previous slide , notice the bronchioectatic changes all over the lung ! Rt lung : pt still can breath from it , although it has apical scarring , Rt upper zone infiltration. Lt Lung : has Abcess cavity , Air Fluid levels , cystic bronchiectasis. If we did bronchoscopy , bronchoalveolar lavage , we will see the Fast Bacilli of Mycobacterium TB , which are resistant to 1 st , 2 nd and 3 rd line anti-TB medications ! ﻧﺘﻴﺠﺔ ﺑﺆﺮﺓ ﺍﻟﺘﻬﺎﺑﻴﺔ Left bronchus syndrome : The study was done at KKUH , if u r interested : http: //www. ncbi. nlm. nih. gov/pmc/articles/PMC 462386/pdf/thorax 00339 -0050. pdf 0
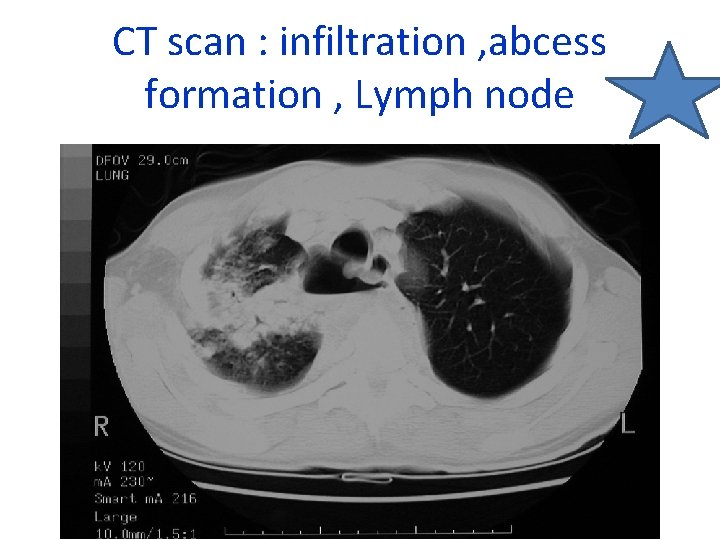
CT scan : infiltration , abcess formation , Lymph node
§ Treatment ‒ Medical ‒ Surgical ü Failure of medical Rx ( Resist. 1 st , 2 nd , 3 rd Line of ttt) ü Destroyed lobe or lung ( left bronchus syndrome ) cuz can lead to ( inflammation , infection , abcess formation , septic state. . Pt needs to be admitted continueously due to chest infection or TB ! ü Pulmonary haemorrhage ü Persistent open cavity with + ve sputum ü Persistent broncho pulmonary fistula )
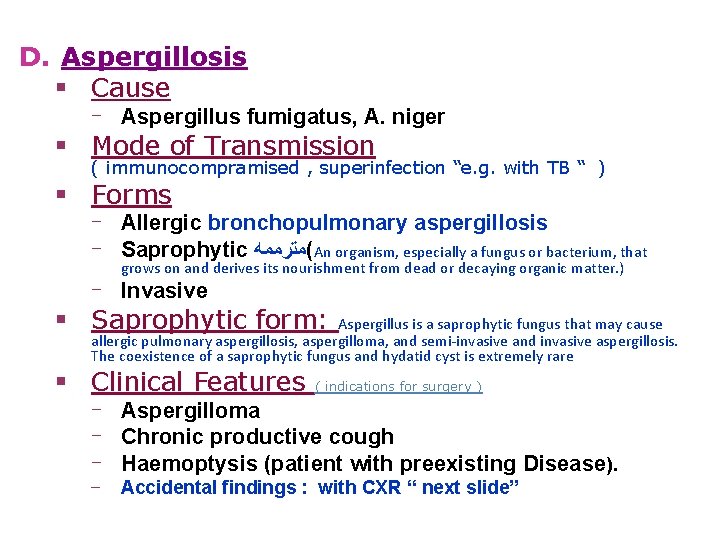
D. Aspergillosis § Cause ‒ Aspergillus fumigatus, A. niger § Mode of Transmission ( immunocompramised , superinfection “e. g. with TB “ ) § Forms ‒ Allergic bronchopulmonary aspergillosis ‒ Saprophytic (ﻣﺘﺮﻣﻤﻪ An organism, especially a fungus or bacterium, that grows on and derives its nourishment from dead or decaying organic matter. ) ‒ Invasive § Saprophytic form: Aspergillus is a saprophytic fungus that may cause allergic pulmonary aspergillosis, aspergilloma, and semi-invasive and invasive aspergillosis. The coexistence of a saprophytic fungus and hydatid cyst is extremely rare § Clinical Features ( indications for surgery ) ‒ Aspergilloma ‒ Chronic productive cough ‒ Haemoptysis (patient with preexisting Disease). ‒ Accidental findings : with CXR “ next slide”
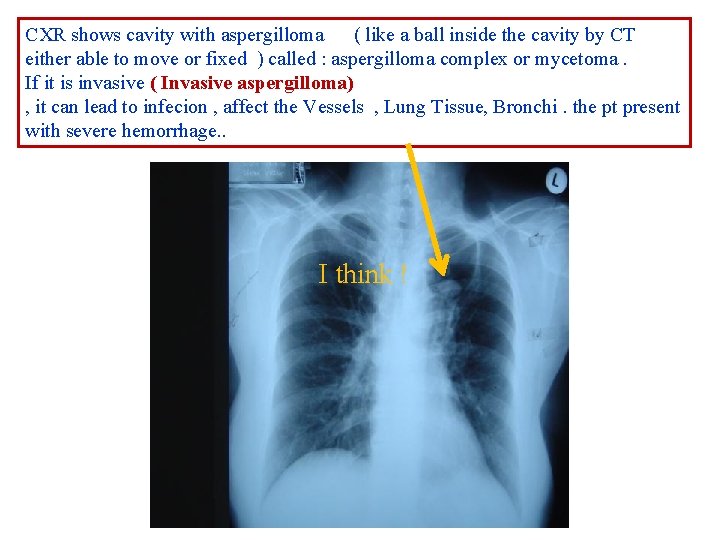
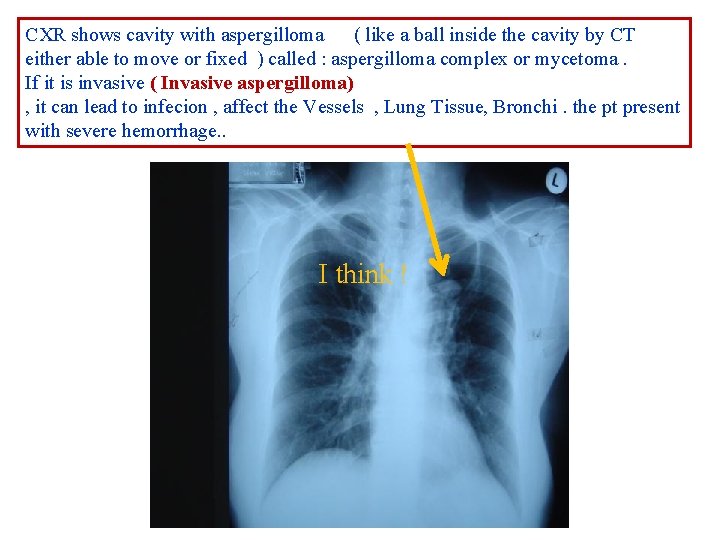
CXR shows cavity with aspergilloma ( like a ball inside the cavity by CT either able to move or fixed ) called : aspergilloma complex or mycetoma. If it is invasive ( Invasive aspergilloma) , it can lead to infecion , affect the Vessels , Lung Tissue, Bronchi. the pt present with severe hemorrhage. . I think !

§ Investigations ‒ ‒ § Skin test Sputum ( fungal culture) Biopsy (Invasive) ( by CT scan ) CXR Treatment ‒ Medical ( anti fungal ) ‒ Surgical § Indications ‒ A significant aspergilloma ‒ Haemoptysis ‒ Clinical features such as Chronic productive cough , SOB , § Type of resection ‒ Lobectomy ( mainly ) ‒ Pneumonectomy ( Rarely ) ‒ Segmentectomy ( very rarely )
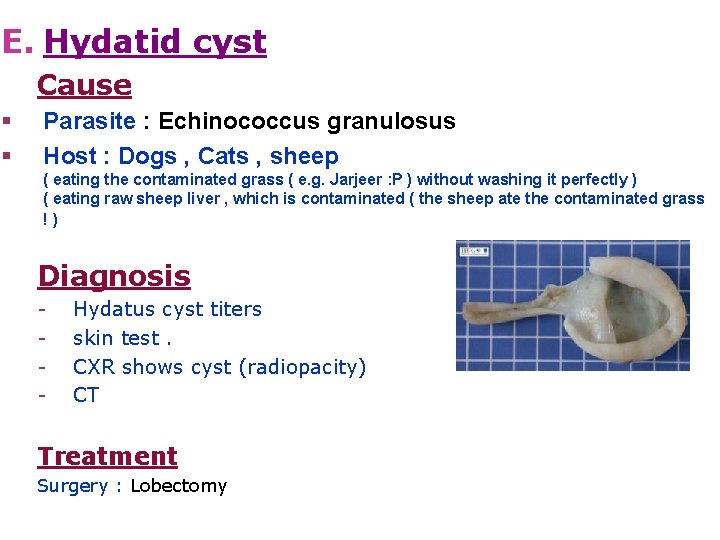
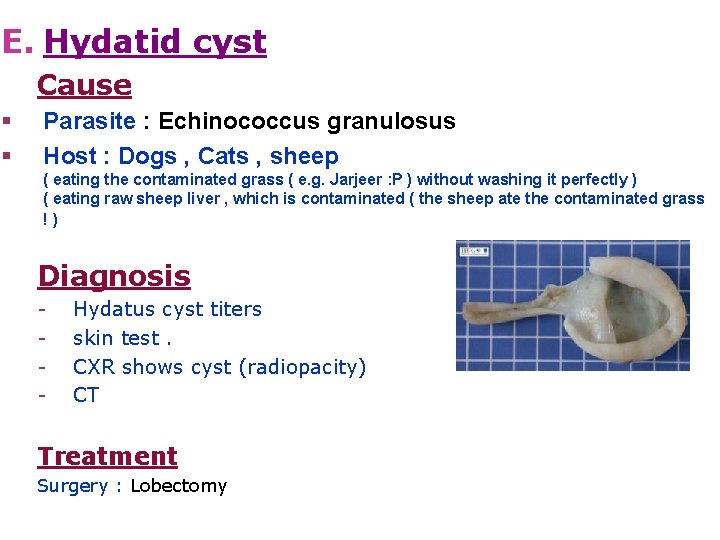
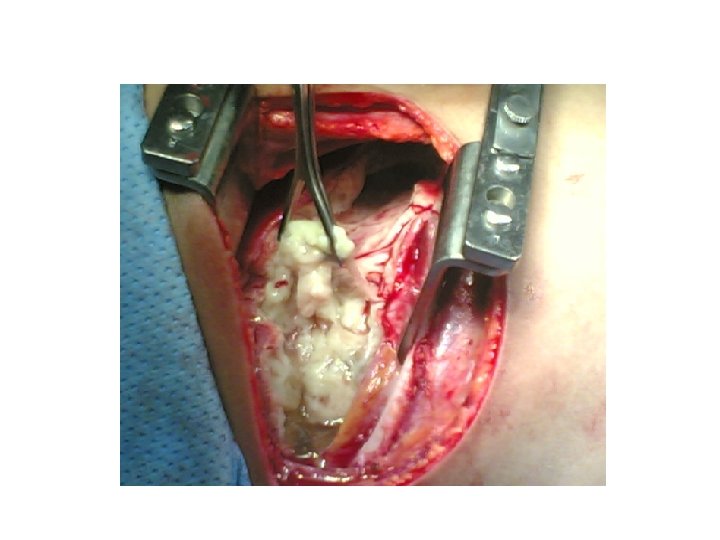
E. Hydatid cyst Cause § § Parasite : Echinococcus granulosus Host : Dogs , Cats , sheep ( eating the contaminated grass ( e. g. Jarjeer : P ) without washing it perfectly ) ( eating raw sheep liver , which is contaminated ( the sheep ate the contaminated grass !) Diagnosis - Hydatus cyst titers skin test. CXR shows cyst (radiopacity) CT Treatment Surgery : Lobectomy
Hydatid cyst q hydatid cyst consists of three layers and hydatid fluid. ü The first layer is the pericyst or adventitia which is the host tissue formed by the lung as a reaction to the foreign body (parasite). (false layer ﻃﺒﻘﺔ ﺛﺎﺑﺘﻪ üThe other two layers, the laminated membrane (ﺍﻟﻄﺒﻘﺔ ﺍﻟﺤﻘﻴﻘﻴﺔ external layer of the cyst) and the germinative layer (inner layer of the cyst), belong to the parasite scolex ﺍﻟﻄﺒﻘﺔ ﺍﻟﻤﻮﻟﺪﺓ ﺗﻌﻄﻲ ﺍﻷﺠﻨﺔ ” ﺍﻝ “ ﻭ ﻣﻤﻜﻦ ﺗﻨﺘﺸﺮ ﻋﻦ ﻃﺮﻳﻖ ﺍﻟﺪﻡ ﺇﻟﻰ ﺃﻲ ﻣﻜﺎﻥ ﻟﻠﺠﺴﻢ hydatid cyst in the brain , parotid , abdomen …. But the commonest sites are liver and lungs. üThe cyst fluid resembles water in appearance which may contain daughter vesicles.
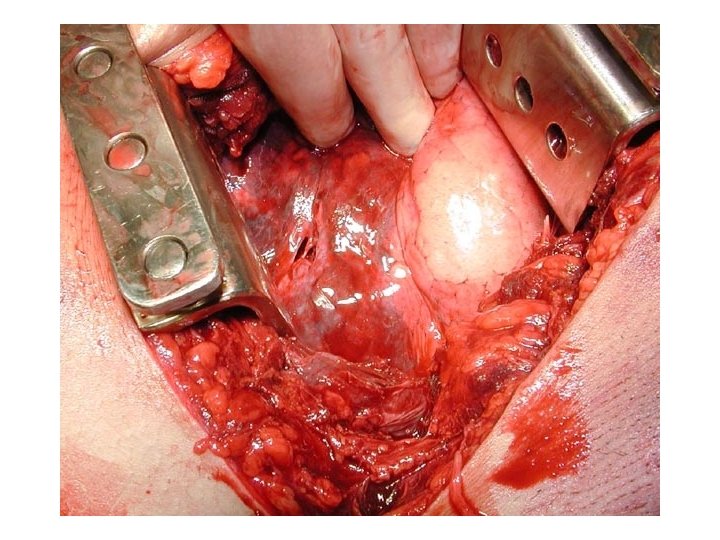
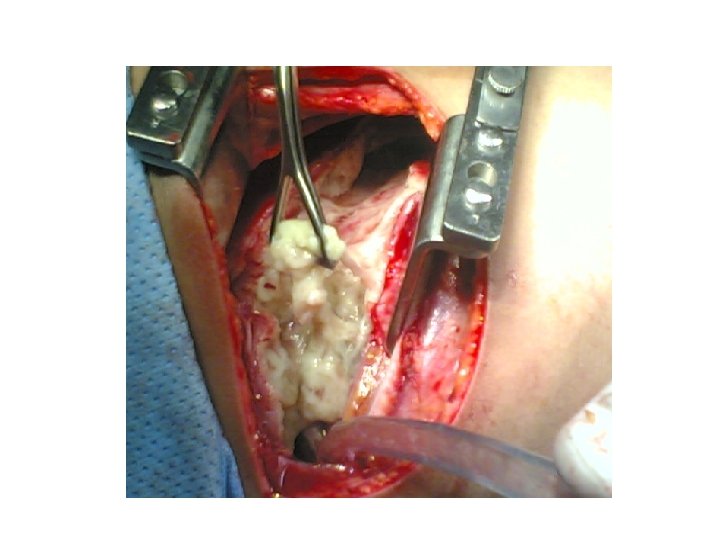
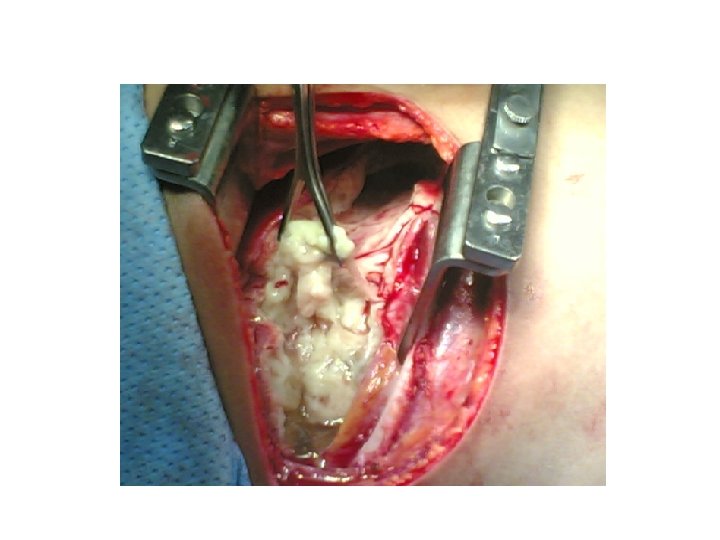
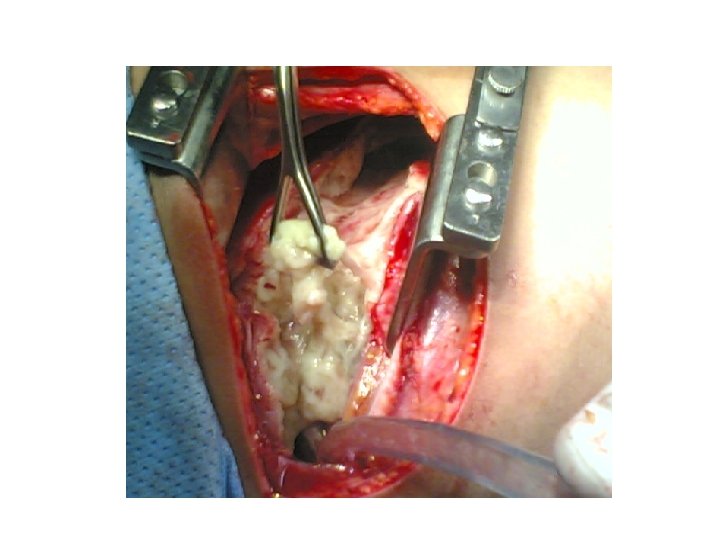
ü - ( Sometimes we see the cyst ruptured to the pleural cavity ) Why some of the cyst rupture and others do not rupture even if they are big cysts ? It depends on the feeding bronchus , if the feeding bronchus is big , the cyst will rupture even if it is small. And if the feeding brochus is small , it will not rupture Treatment Surgery : Lobectomy Injection of concentrated saline 20% for 2 -4 mins ( usually the used Saline is 0. 9%) , to kill the scolex ﺍﻷﺠﻨﺔ which are able to rupture to the pleural cavity and form new cysts ! We cover the whole area with sterile towels , to prevent contamination. Apendazole is given after or before the surgery Saline is injected during the surgery ( they used to inject formaline “ aminarol ? “ ) : ﻓﻴﻪ ﺗﻘﺮﻳﺒﺎ ﻛﻞ ﺍﻟﻠﻲ ﺷﺎﺭﺣﻪ ﺍﻟﺪﻛﺘﻮﺭ ﺑﺎﻟﺼﻮﺭ , ﻣﻮﻗﻊ ﺣﻠﻮ http: //mmcts. ctsnetjournals. org/cgi/content/full/2005/0425/mmcts. 2004. 000307#SEC 2 Cyst can be anywhere, but mainly in the liver or lung

Tumor ØBenign ØMalignant § Primary § Secondary

A. Primary lung carcinoma Incidence Worldwide, lung cancer is the most common cause of cancer death. The 3 rd most common cause of death overall. The incidence is rising in women as well ( after breast ca ). Risk Factor § Smoking § Diet § Genetic factors § Others - air pollution, radiation and industrial chemicals, radon , and asbestos
Pathology 1. Adenocarcinoma 2. Squamous cell carcinoma 3. Large cell carcinoma 4. Small cell carcinoma, § NSCLC vs. SCLC (Small cell lung cancer): derived from neuroendocrine – nonsurgical NSCLC (Non small) : derived from epithelial origin - surgical
Clinical Features § Asymptomatic § Symptomatic ü General : loss of appetite , fever , loss of weight , fatigue. ü Lung : cough is the commonest , occures in half of the pt !, Haemoptysis , sputum production , SOB, pain ü Pressure symptomes on Surrounding structures : § Rec. L. nerve : chocking ( )ﺗﺘﺸﺮﺩﻕ on drinking , hoarsness. § Oesophagus : dysphagia. § C 8, T 1 nerve : arm pain or numbness , brachial plexus § Sympathetic especially injury to satellite ganglion (1 st sympathetic ganglion): Horner's syndrome ( ptosis , Anhidrosis , enophthalmos … etc ) § Pleura § SVC : superior vena cava obstruction syndrome , Shortness of breath is the most common symptom, followed by face or arm swelling § Para. Neoplastic Syndrome (next slide)
§ distal (para-neoplastic syndrome) - Squemous cell carcinoma. § § § PTH ADH ACTH Hypertrophic pulmonary osteoathropathy (HPOA) : pain and swelling of joints. not responsive for any ttt. Once the tumor removed , all the symp. Improved Hypercalcemia , hyponatremia , fluid retention. (cushing syndrome) Investigations § § § CXR Trans-thoracic needle aspiration CT Scan Bronchoscopy MRI : Poor modality in Lung cancers in general ! If there is involvement of the major structures in the apex ( brachial plexus , vertebral column , spinal canal , apex , spine ) Staging : ﻧﻌﺘﻤﺪ ﻋﻠﻴﻪ (see table)

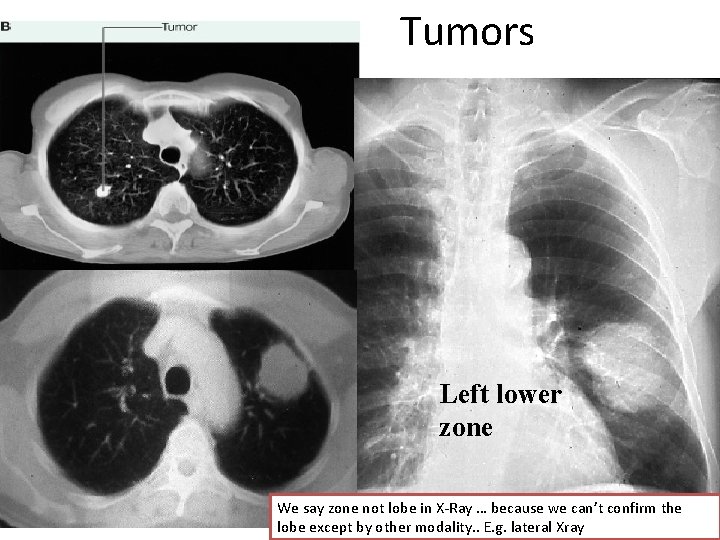
MRI is used in Cancox tumor , or superior sulcus tumor ( in the Apex of the Lung ) cuz we can see the involvement of the spinal canal and vertebrea Tumor
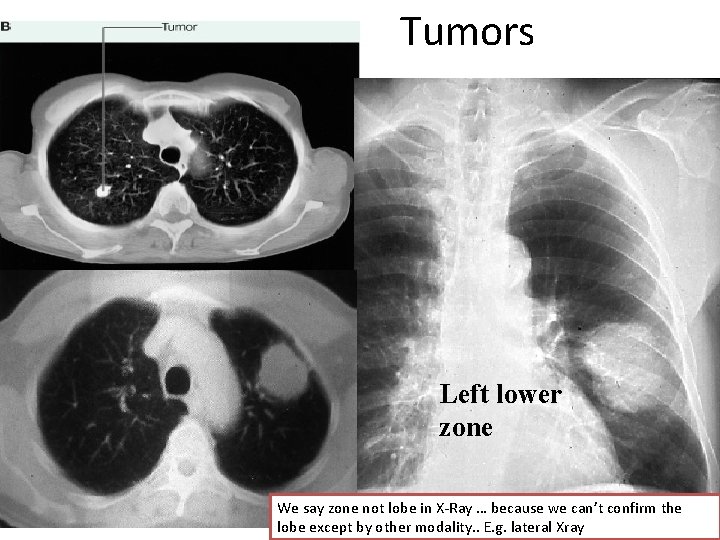
Tumors Left lower zone We say zone not lobe in X-Ray … because we can’t confirm the lobe except by other modality. . E. g. lateral Xray
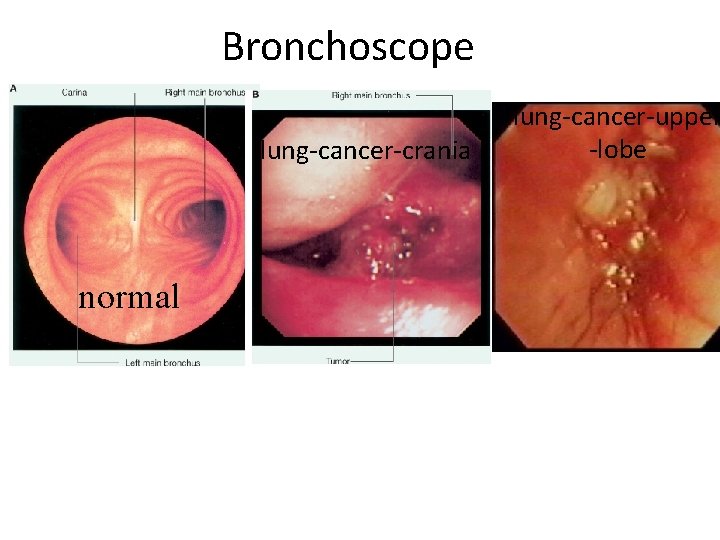
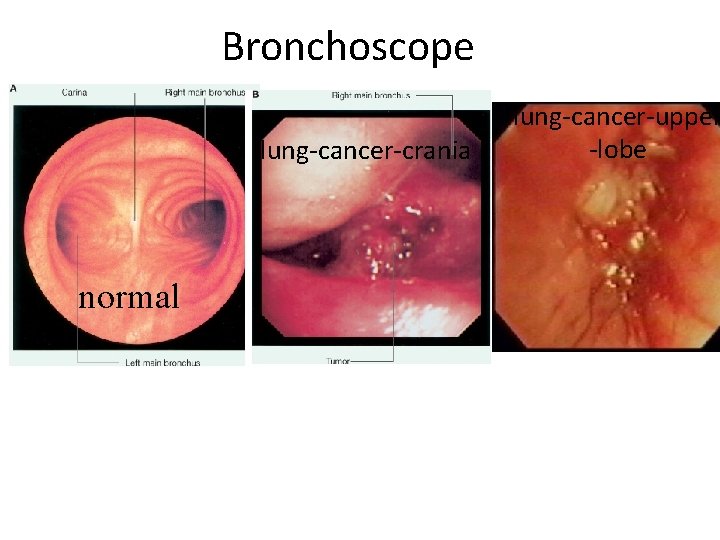
Bronchoscope lung-cancer-crania normal lung-cancer-upper -lobe
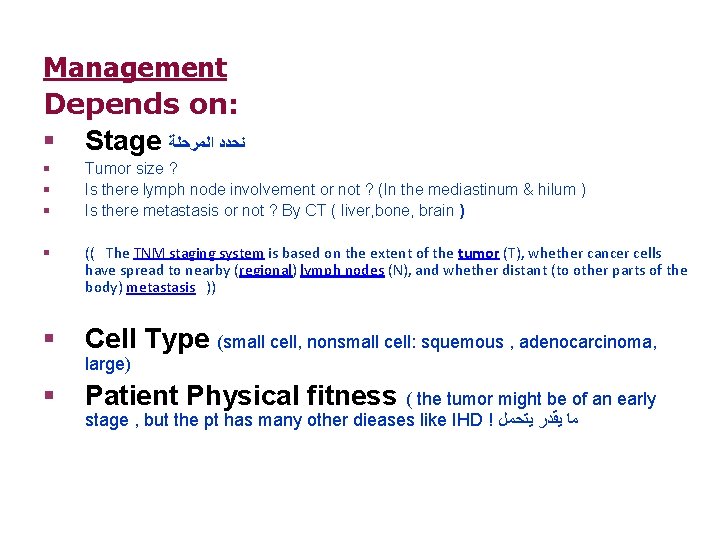
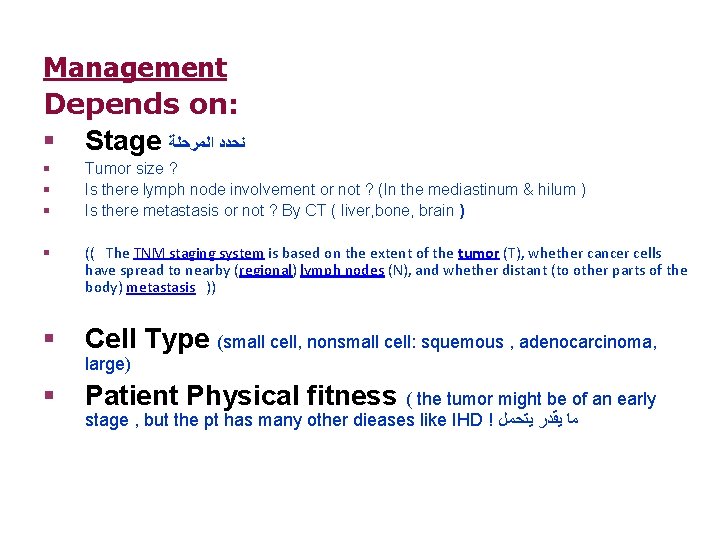
Management Depends on: § Stage ﻧﺤﺪﺩ ﺍﻟﻤﺮﺣﻠﺔ § § § Tumor size ? Is there lymph node involvement or not ? (In the mediastinum & hilum ) Is there metastasis or not ? By CT ( liver, bone, brain ) § (( The TNM staging system is based on the extent of the tumor (T), whether cancer cells have spread to nearby (regional) lymph nodes (N), and whether distant (to other parts of the body) metastasis )) § Cell Type (small cell, nonsmall cell: squemous , adenocarcinoma, § Patient Physical fitness ( the tumor might be of an early large) stage , but the pt has many other dieases like IHD ! ﻣﺎ ﻳﻘﺪﺭ ﻳﺘﺤﻤﻞ
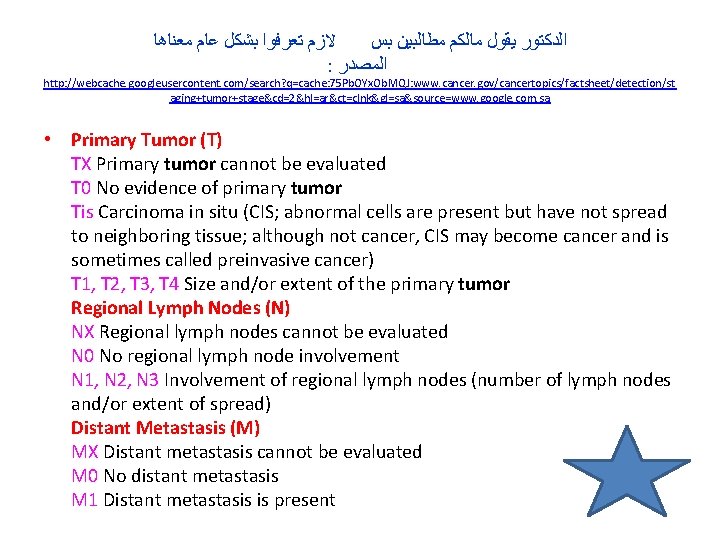
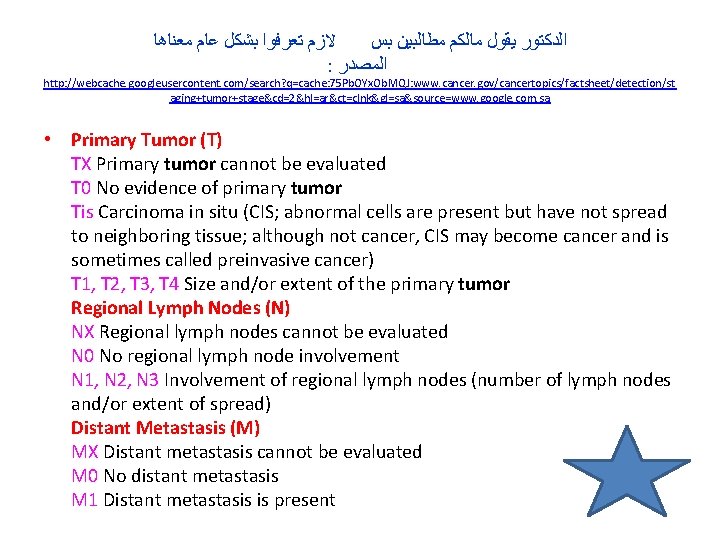
ﻻﺯﻡ ﺗﻌﺮﻓﻮﺍ ﺑﺸﻜﻞ ﻋﺎﻡ ﻣﻌﻨﺎﻫﺎ ﺍﻟﺪﻛﺘﻮﺭ ﻳﻘﻮﻝ ﻣﺎﻟﻜﻢ ﻣﻄﺎﻟﺒﻴﻦ ﺑﺲ : ﺍﻟﻤﺼﺪﺭ http: //webcache. googleusercontent. com/search? q=cache: 75 Pb. OYx. Ob. MQJ: www. cancer. gov/cancertopics/factsheet/detection/st aging+tumor+stage&cd=2&hl=ar&ct=clnk&gl=sa&source=www. google. com. sa • Primary Tumor (T) TX Primary tumor cannot be evaluated T 0 No evidence of primary tumor Tis Carcinoma in situ (CIS; abnormal cells are present but have not spread to neighboring tissue; although not cancer, CIS may become cancer and is sometimes called preinvasive cancer) T 1, T 2, T 3, T 4 Size and/or extent of the primary tumor Regional Lymph Nodes (N) NX Regional lymph nodes cannot be evaluated N 0 No regional lymph node involvement N 1, N 2, N 3 Involvement of regional lymph nodes (number of lymph nodes and/or extent of spread) Distant Metastasis (M) MX Distant metastasis cannot be evaluated M 0 No distant metastasis M 1 Distant metastasis is present
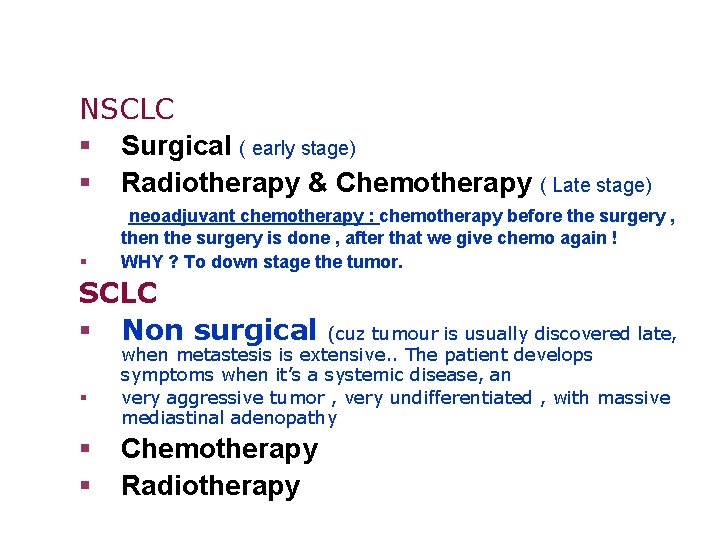
NSCLC § Surgical ( early stage) § Radiotherapy & Chemotherapy ( Late stage) § neoadjuvant chemotherapy : chemotherapy before the surgery , then the surgery is done , after that we give chemo again ! WHY ? To down stage the tumor. SCLC § Non surgical § § § (cuz tumour is usually discovered late, when metastesis is extensive. . The patient develops symptoms when it’s a systemic disease, an very aggressive tumor , very undifferentiated , with massive mediastinal adenopathy Chemotherapy Radiotherapy

N 3 : supraclavicular or to the other side N 2: out the lung to mediastinum , hilum N 1 : inside the lung
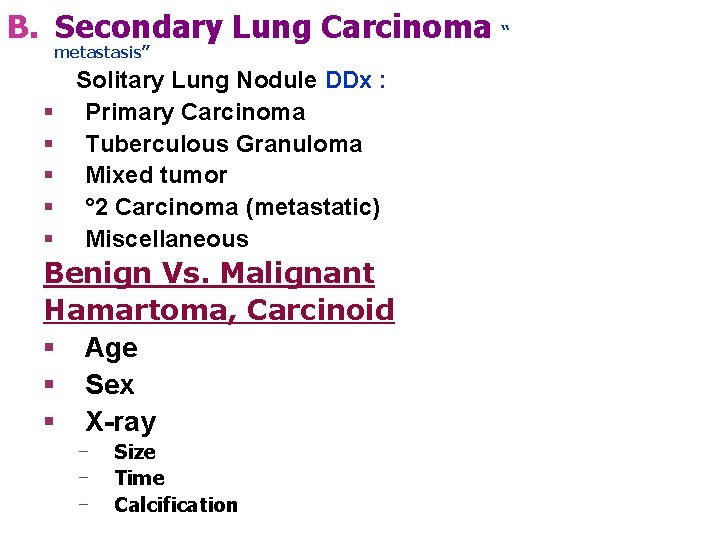
B. Secondary Lung Carcinoma “ metastasis” § § § Solitary Lung Nodule DDx : Primary Carcinoma Tuberculous Granuloma Mixed tumor ° 2 Carcinoma (metastatic) Miscellaneous Benign Vs. Malignant Hamartoma, Carcinoid § Age § Sex § X-ray ‒ ‒ ‒ Size Time Calcification
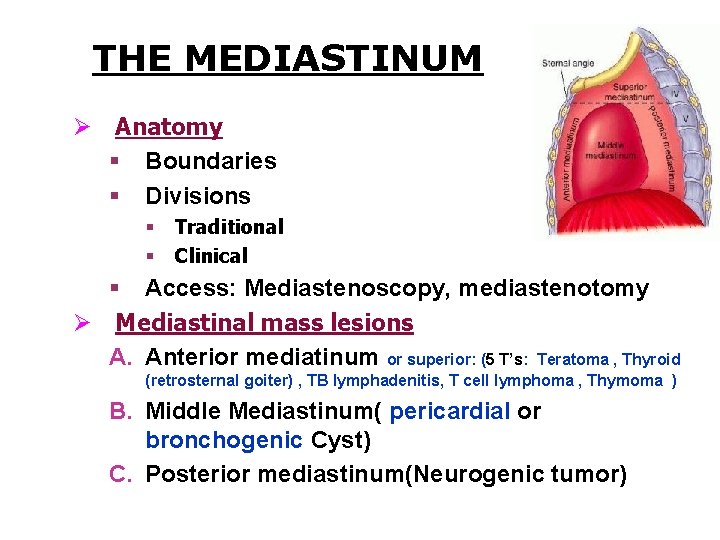
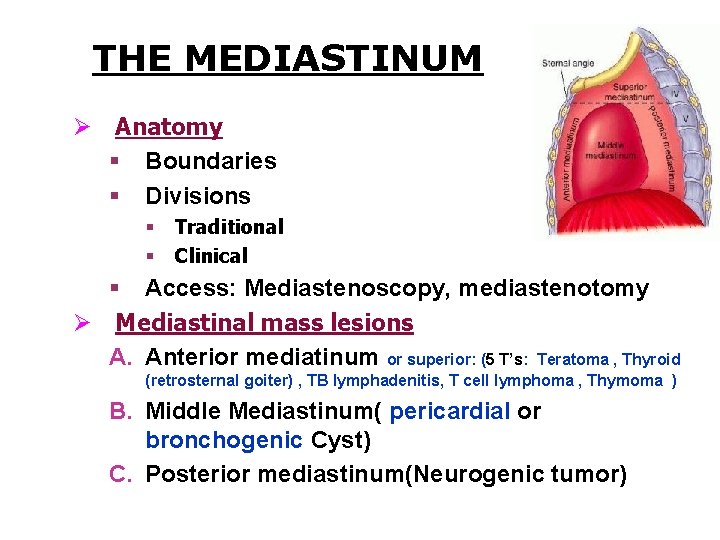
THE MEDIASTINUM Ø Anatomy § Boundaries § Divisions § § Traditional Clinical § Access: Mediastenoscopy, mediastenotomy Ø Mediastinal mass lesions A. Anterior mediatinum or superior: (5 T’s: Teratoma , Thyroid (retrosternal goiter) , TB lymphadenitis, T cell lymphoma , Thymoma ) B. Middle Mediastinum( pericardial or bronchogenic Cyst) C. Posterior mediastinum(Neurogenic tumor)
Thymoma • • • Commonest tumor in the anterior mediastinum. Age 40 – 60. Can be benign or malignant. Stages 1 -2 surgical 3 -4 needs chemo. Thymoma is a tumor originating from the epithelial cells of the thymus. It also contains lymphocytes (thymocytes) that are often abundant and non-neoplastic. All thymomas should be considered as malignant as even the encapsulated ones may recur and metastasize. Thymoma is an uncommon tumor, best known for its association with the neuromuscular disorder myasthenia gravis • • • 40% of Thymoma pt have Mysthenia graves symptoms. 15% of MG , have thymoma ! The ttt is surgery , to get out the MG symps.
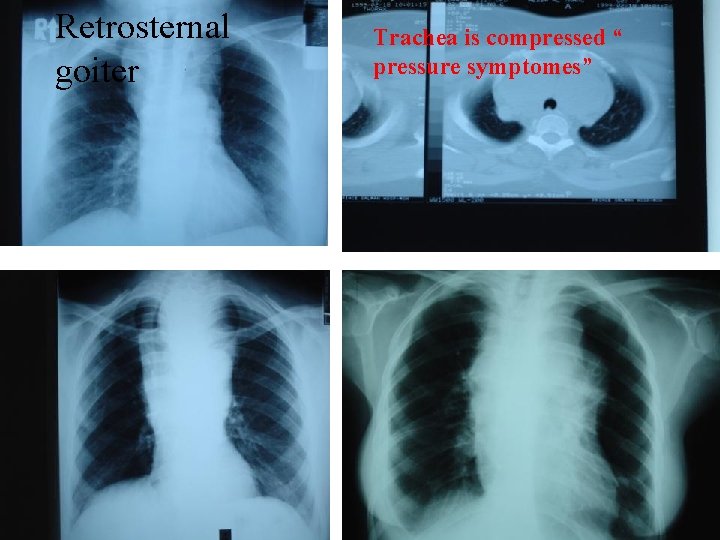
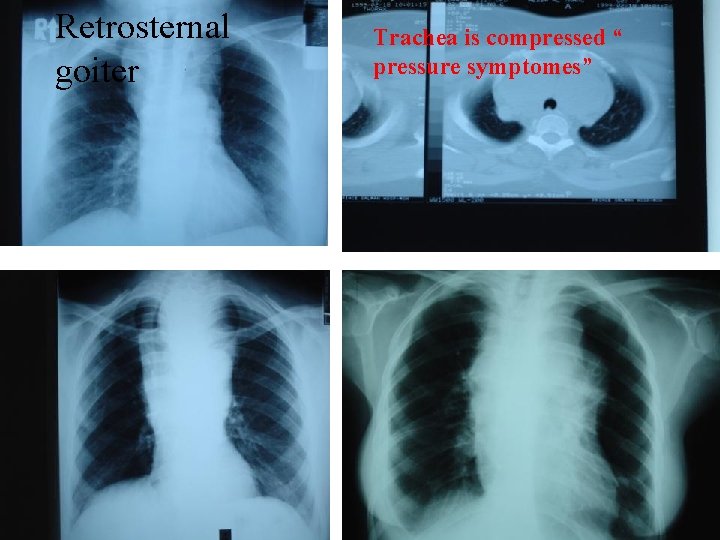
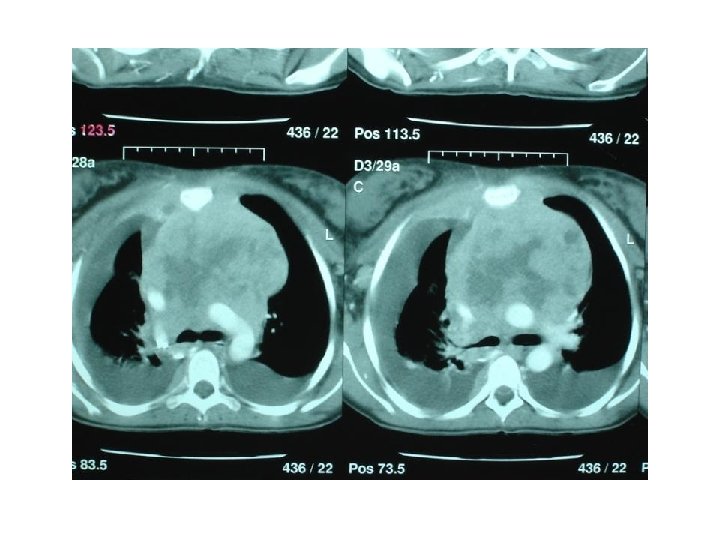
Retrosternal goiter Trachea is compressed “ pressure symptomes”
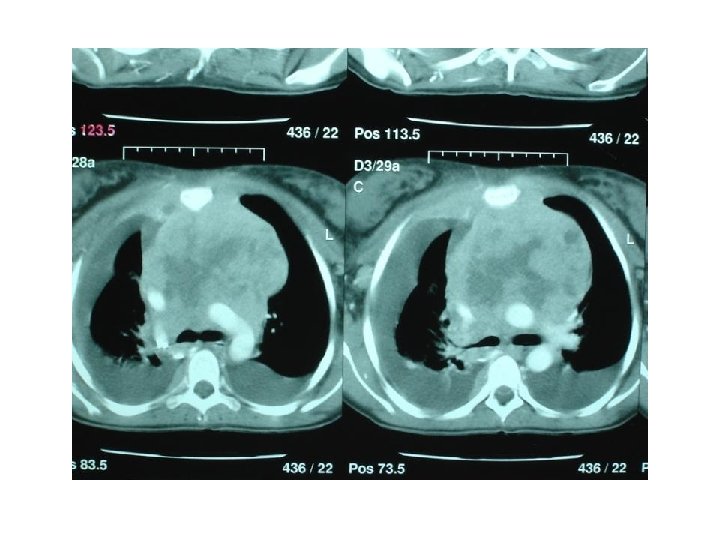
Investigations : • CXR • CT scan • Biopsy. • Angiogram. • Bronchoscopy • Mediastinoscopy Treatment : • Benign : complete excise ( surgery) • Malignant : chemo , Radio , Surgery “chemo b 4 surg, then surg m then chemo radio after. ”
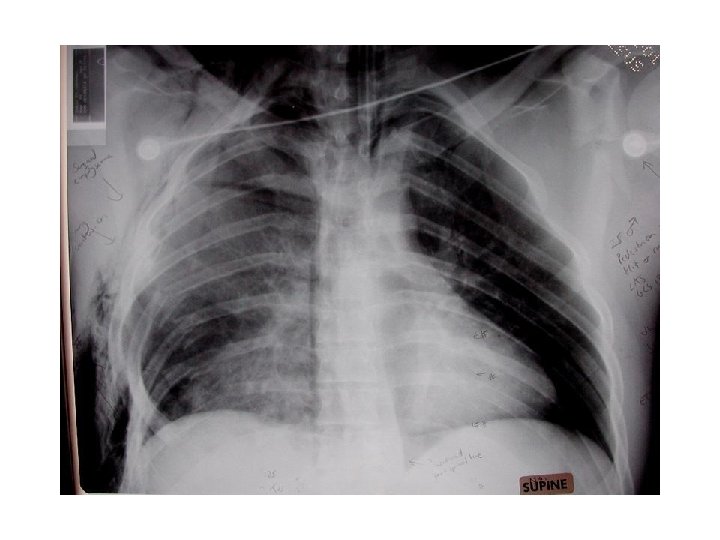
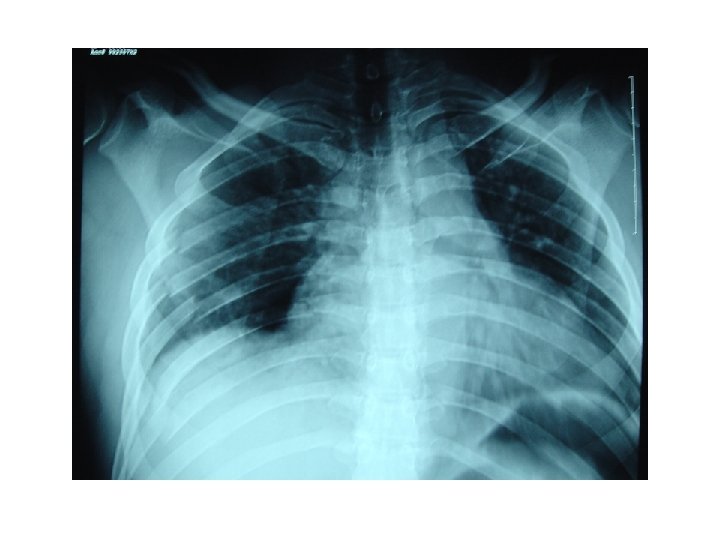
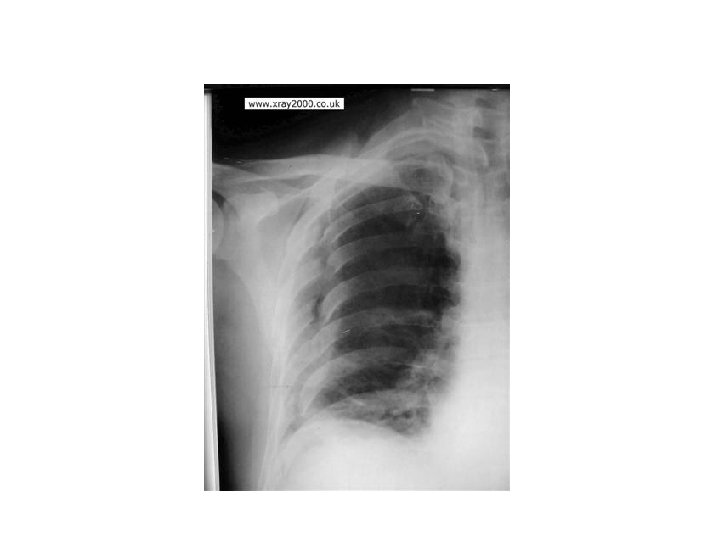
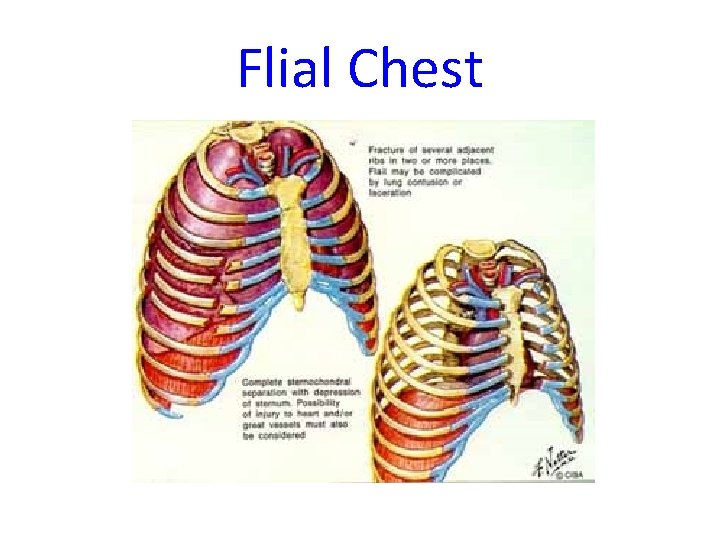
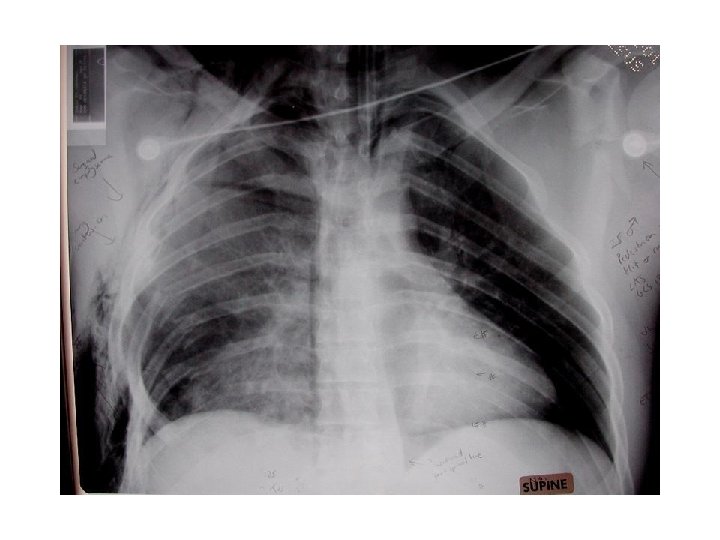
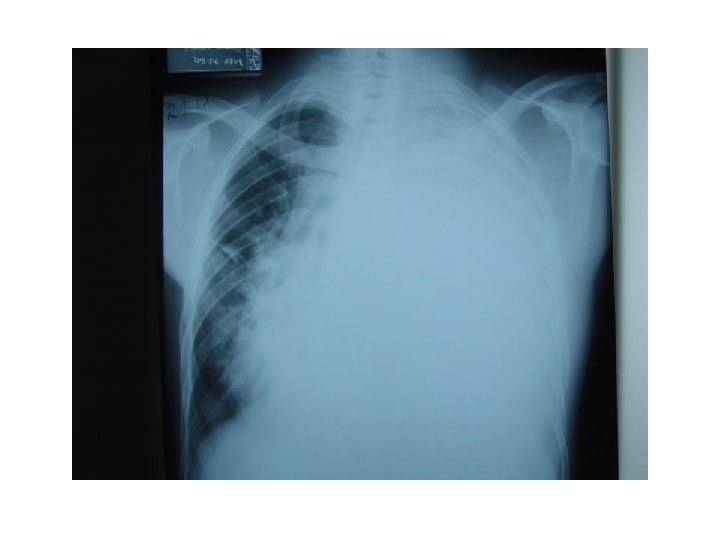
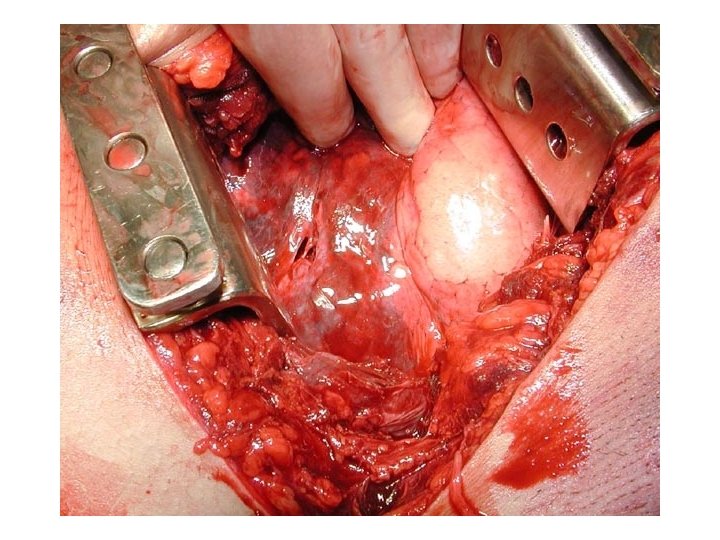
Trauma. . ﺑﻌﺪ ﻛﺪﺍ ﻣﺎ ﺷﺮﺡ ﺍﻟﺪﻛﺘﻮﺭ § § § RTA Fracture Ribs Simple – Complicated Haemothorax Pneumothorax Flail chest Lung Contusion and ARDS
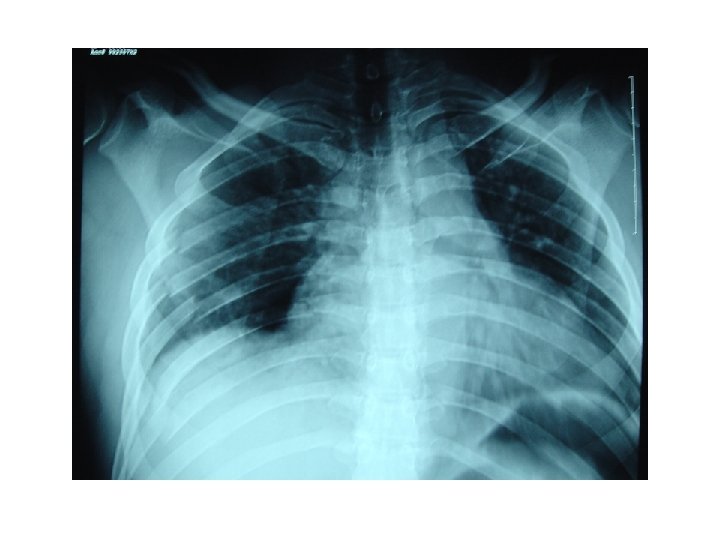
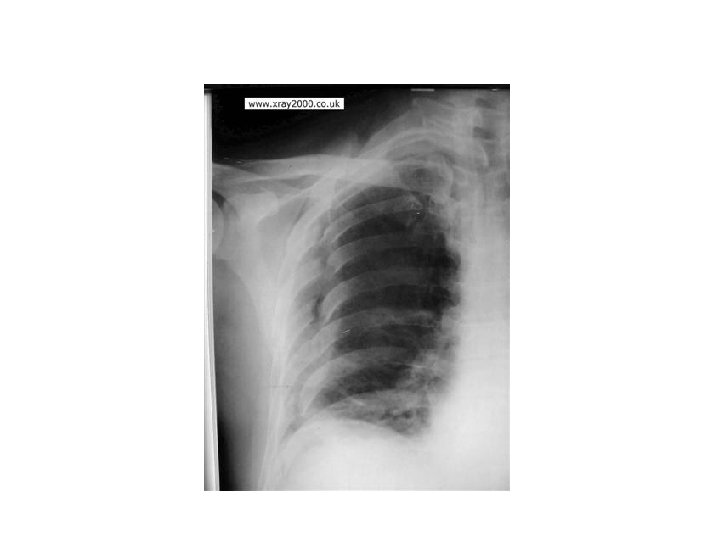
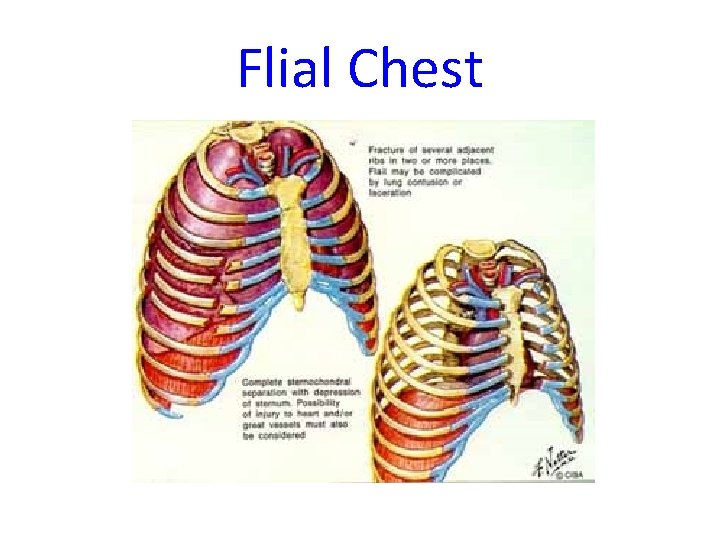
Flial Chest






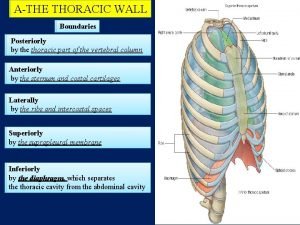
Chest Wall § Deformity: ‒ Pectus excavatum ‒ Pectus Carniatum § Infection § Chest wall tumor § Thoracic outlet Syndrome.



Pleura § § Spontaneous preumothorax Pleural effusion Empyema Mesothelioma.




Surgery: § § Thoracotomy Thoracoscopy Sternotomy Analgesia

Position of skin incisions, showing camera port and working port anteriorly

Use of a retractor to hold open the working port.

 Waseem ahmad khan
Waseem ahmad khan Waseem ikram
Waseem ikram Waseem ikram
Waseem ikram Personality disorder
Personality disorder Waseem ikram
Waseem ikram Chapter 23 lesson 1 understanding communicable diseases
Chapter 23 lesson 1 understanding communicable diseases Non common communicable diseases
Non common communicable diseases Genu recurvatum
Genu recurvatum Blood supply to thoracic wall
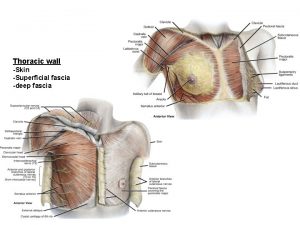
Blood supply to thoracic wall Fascia of thoracic wall
Fascia of thoracic wall Salvador dali chest of drawers
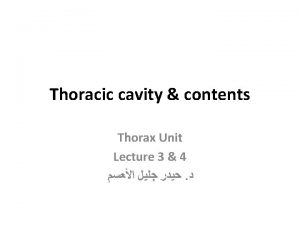
Salvador dali chest of drawers Chest cavity
Chest cavity Lymph nodes legs
Lymph nodes legs Body cavity
Body cavity Tfl counterstrain
Tfl counterstrain Venous drainage of thoracic wall
Venous drainage of thoracic wall Where is the sternal notch
Where is the sternal notch Cervical facet referral patterns
Cervical facet referral patterns Pig thoracic cavity diagram
Pig thoracic cavity diagram Extrinsic muscles
Extrinsic muscles Thyroid isotope scan
Thyroid isotope scan Cupola in diaphragm
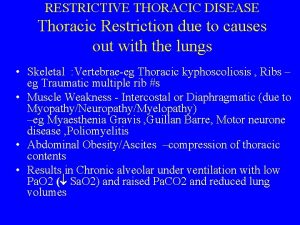
Cupola in diaphragm Thoracic kyphoscoliosis definition
Thoracic kyphoscoliosis definition Horizontal fissure of left lung
Horizontal fissure of left lung Branches of aorta
Branches of aorta Thoracic membranes
Thoracic membranes Venturi mask uses
Venturi mask uses Dorsal and ventral body cavities
Dorsal and ventral body cavities Thoracic cavity and abdominal cavity
Thoracic cavity and abdominal cavity Arteries of thoracic wall
Arteries of thoracic wall Thoracic cage configuration
Thoracic cage configuration Popularly called lymph glands
Popularly called lymph glands Thoracic vertebrae not labeled
Thoracic vertebrae not labeled Thoracic aortic aneurysm
Thoracic aortic aneurysm Layers of chest wall
Layers of chest wall Posterior mediastinum contents
Posterior mediastinum contents Thoracic outlet wedge pillow
Thoracic outlet wedge pillow Neurogeen thoracic outlet syndroom
Neurogeen thoracic outlet syndroom Rajesh shah thoracic surgeon
Rajesh shah thoracic surgeon Thoracic cage anterior view
Thoracic cage anterior view Thoracic cage anterior view
Thoracic cage anterior view Auscultatory triangle
Auscultatory triangle Muscles of thoracic spine
Muscles of thoracic spine Kati mori
Kati mori Chyle leak
Chyle leak Thoracic cage anterior view
Thoracic cage anterior view Volume of thoracic cavity
Volume of thoracic cavity Inferior articular process
Inferior articular process Thoracic duct
Thoracic duct Thoracic cavity
Thoracic cavity Thoracic lumbar fascia
Thoracic lumbar fascia Bones of thorax
Bones of thorax Cervical lateral flexion
Cervical lateral flexion Posterior wall of the axilla
Posterior wall of the axilla Jugular notch
Jugular notch Thoracic surgeon
Thoracic surgeon Soft spongy cone shaped organs in the thoracic cavity
Soft spongy cone shaped organs in the thoracic cavity Atheromatous thoracic aorta
Atheromatous thoracic aorta Thoracic mri images
Thoracic mri images Is aortic atherosclerosis dangerous
Is aortic atherosclerosis dangerous Lumbar vertebrae characteristics
Lumbar vertebrae characteristics Which ventral cavity subdivision has no bony protection
Which ventral cavity subdivision has no bony protection Thoracic surgery
Thoracic surgery Thoracic nerves
Thoracic nerves Highest common factor of 12 and 42
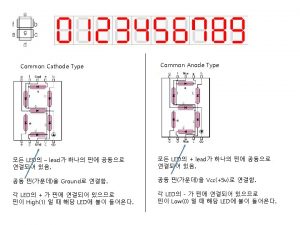
Highest common factor of 12 and 42 Common anode and common cathode
Common anode and common cathode Factor tree of 28
Factor tree of 28 How to find lowest common factor
How to find lowest common factor Gcf of 72 and 90
Gcf of 72 and 90 Multiples of 9 and 21
Multiples of 9 and 21 Sinciput presentation
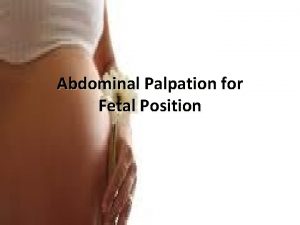
Sinciput presentation Leopold maneuver
Leopold maneuver Type of disease
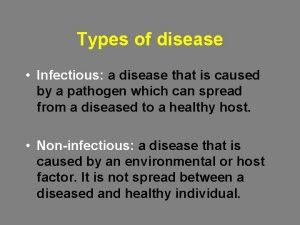
Type of disease Philip crosby formulated the seven deadly diseases
Philip crosby formulated the seven deadly diseases Protein deficiency diseases
Protein deficiency diseases Diagram of natural history of disease
Diagram of natural history of disease Modern lifestyle and hypokinetic diseases
Modern lifestyle and hypokinetic diseases Major nutritional deficiency diseases in emergencies
Major nutritional deficiency diseases in emergencies Inflammation of mfa ppt
Inflammation of mfa ppt Iceberg phenomenon
Iceberg phenomenon Human diseases a systemic approach
Human diseases a systemic approach Communicable and noncommunicable diseases venn diagram
Communicable and noncommunicable diseases venn diagram Chapter 24 lesson 1 sexually transmitted diseases
Chapter 24 lesson 1 sexually transmitted diseases Define periradicular disease
Define periradicular disease Section 19-3 diseases caused by bacteria and viruses
Section 19-3 diseases caused by bacteria and viruses Chapter 8 skin disorders and diseases review questions
Chapter 8 skin disorders and diseases review questions Chapter 6 musculoskeletal system diseases and disorders
Chapter 6 musculoskeletal system diseases and disorders Chapter 32 childhood communicable diseases bioterrorism
Chapter 32 childhood communicable diseases bioterrorism