Mechanical Ventilation in Adult Patients A July Guide


- Slides: 71
Mechanical Ventilation in Adult Patients A July Guide to Ventilators Joshua R. Rosenberg M. D.
Disclosure o I have no knowledge of stock in pharmaceutical companies, medical device companies, or any company affiliated with the Medical Industry. o Any stock owned is through the Continuum retirement plan with Fidelity. It is rapidly loosing money. o I am not a paid speaker, lecturer, consultant for any company. o Brand name products will be discussed. o Proprietary and copyrighted ventilator modes will be discussed.
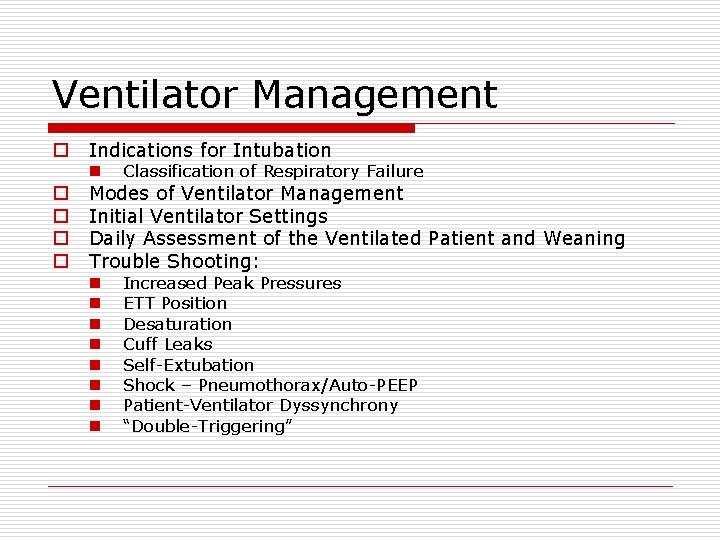
Ventilator Management o o o Indications for Intubation n Classification of Respiratory Failure n n n n Increased Peak Pressures ETT Position Desaturation Cuff Leaks Self-Extubation Shock – Pneumothorax/Auto-PEEP Patient-Ventilator Dyssynchrony “Double-Triggering” Modes of Ventilator Management Initial Ventilator Settings Daily Assessment of the Ventilated Patient and Weaning Trouble Shooting:
The Greatest Quotable Yankee “If you don't know where you are going, you might wind up someplace else. ” Try to figure out ‘why’ the patient is requiring intubation. “In theory there is no difference between theory and practice. In practice there is. ” Hearing the information is nice but no substitute for gaining experience in ventilator management.
General “Rules” of Mechanical Ventilation o Indications for Intubation…. n “The Look” o “Rest”… n Get rid of “The Look” o o Keep the Pressures Low… n Peak < 45 cm H 2 O n Plateau < 32 cm H 2 O Keep the Fi. O 2 Low n Pa. O 2 70 -80 o Keep the Tidal Volumes near 6 ml/kg IBW o You don’t have to correct it all at once n Permit some hypercapnea initially to lower airway and lung pressures.
Ventilator Management: Stepwise 1. 2. 3. 4. 5. Recognize Respiratory Failure Stabilize on the Vent Figure out why? Talk with your nurse! Trouble Shooting o Initial assessment of common problems 6. Weaning
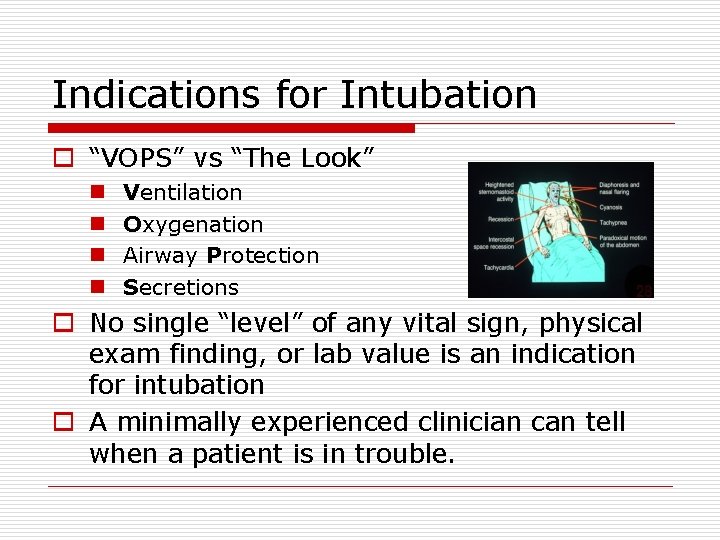
Indications for Intubation o “VOPS” vs “The Look” n n Ventilation Oxygenation Airway Protection Secretions o No single “level” of any vital sign, physical exam finding, or lab value is an indication for intubation o A minimally experienced clinician can tell when a patient is in trouble.
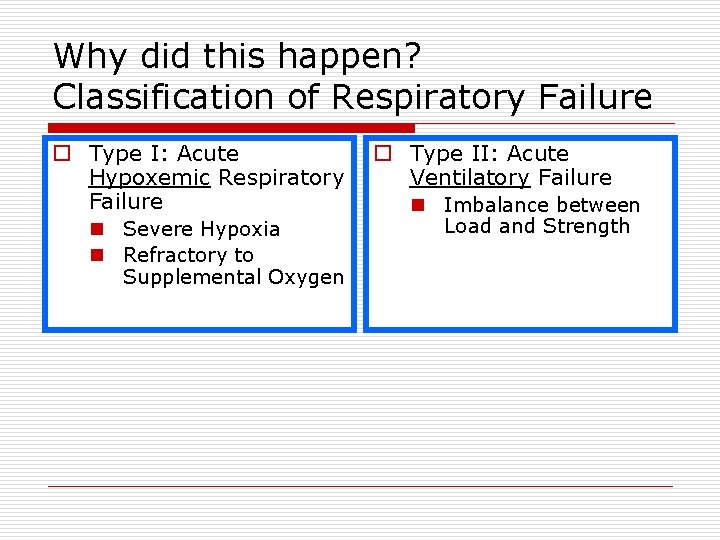
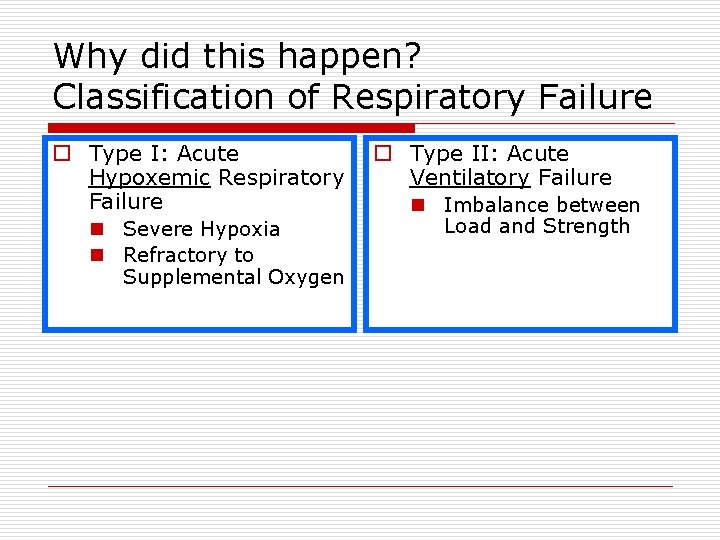
Why did this happen? Classification of Respiratory Failure o Type I: Acute Hypoxemic Respiratory Failure n Severe Hypoxia n Refractory to Supplemental Oxygen o Type II: Acute Ventilatory Failure n Imbalance between Load and Strength
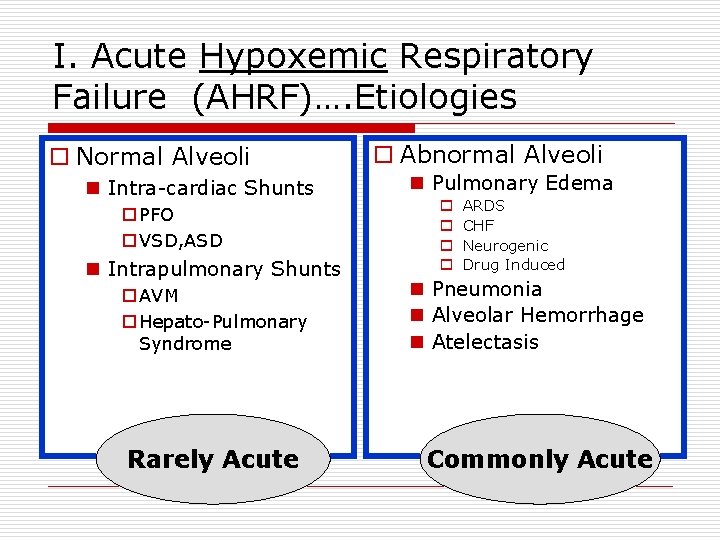
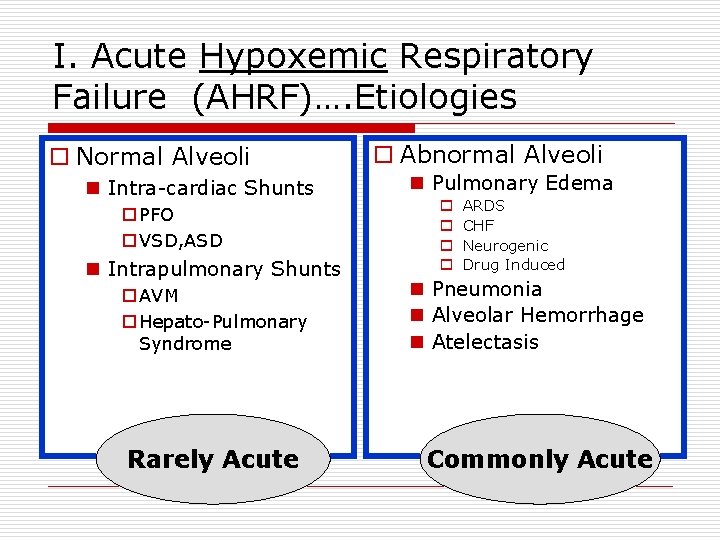
I. Acute Hypoxemic Respiratory Failure (AHRF)…. Etiologies o Normal Alveoli n Intra-cardiac Shunts o PFO o VSD, ASD n Intrapulmonary Shunts o AVM o Hepato-Pulmonary Syndrome Rarely Acute o Abnormal Alveoli n Pulmonary Edema o o ARDS CHF Neurogenic Drug Induced n Pneumonia n Alveolar Hemorrhage n Atelectasis Commonly Acute
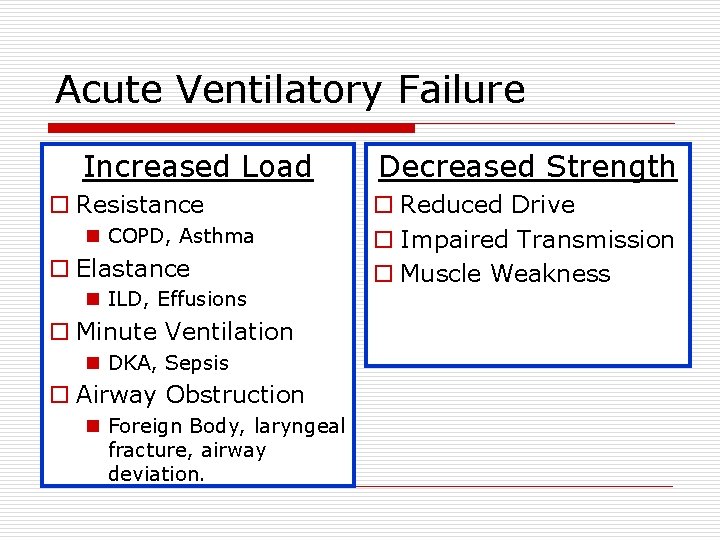
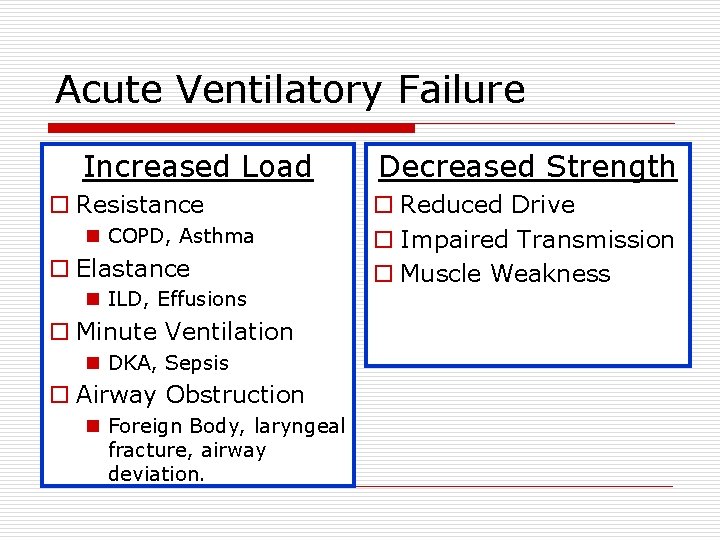
Acute Ventilatory Failure Increased Load o Resistance n COPD, Asthma o Elastance n ILD, Effusions o Minute Ventilation n DKA, Sepsis o Airway Obstruction n Foreign Body, laryngeal fracture, airway deviation. Decreased Strength o Reduced Drive o Impaired Transmission o Muscle Weakness
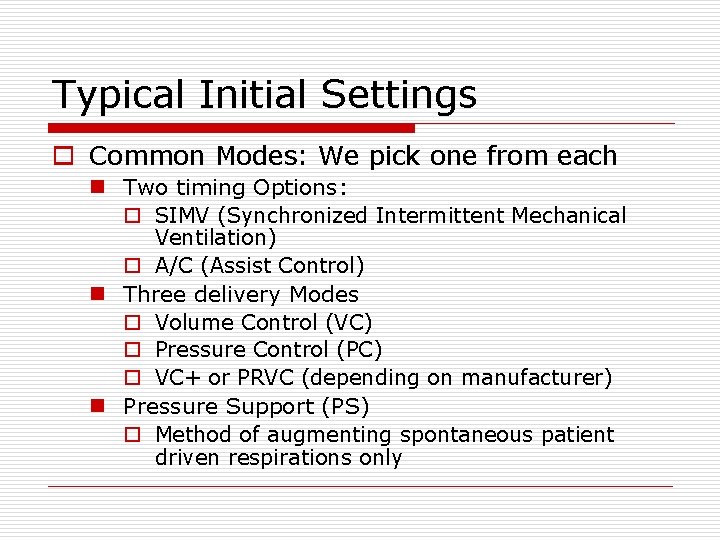
Typical Initial Settings o Common Modes: We pick one from each n Two timing Options: o SIMV (Synchronized Intermittent Mechanical Ventilation) o A/C (Assist Control) n Three delivery Modes o Volume Control (VC) o Pressure Control (PC) o VC+ or PRVC (depending on manufacturer) n Pressure Support (PS) o Method of augmenting spontaneous patient driven respirations only
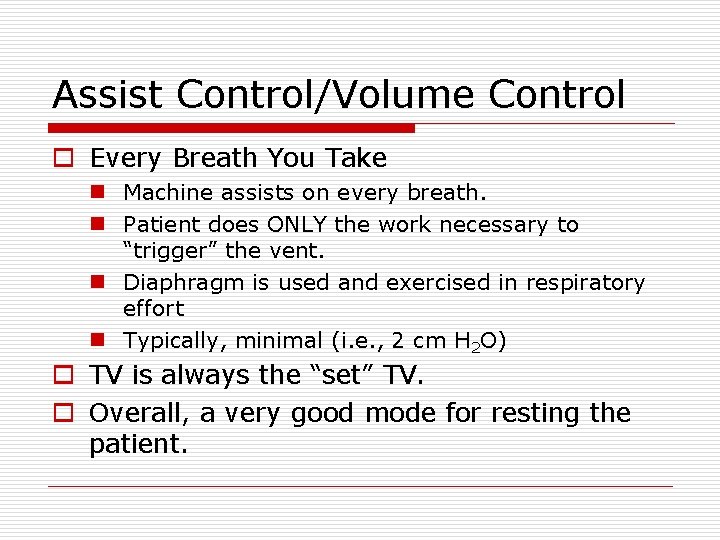
Assist Control o Machine assists on every single breath o Assists on patient initiated breaths o Assists on machine driven breaths o Set Rate is the Minimum rate of ventilation o Can be combined with VC, PC, or VC+
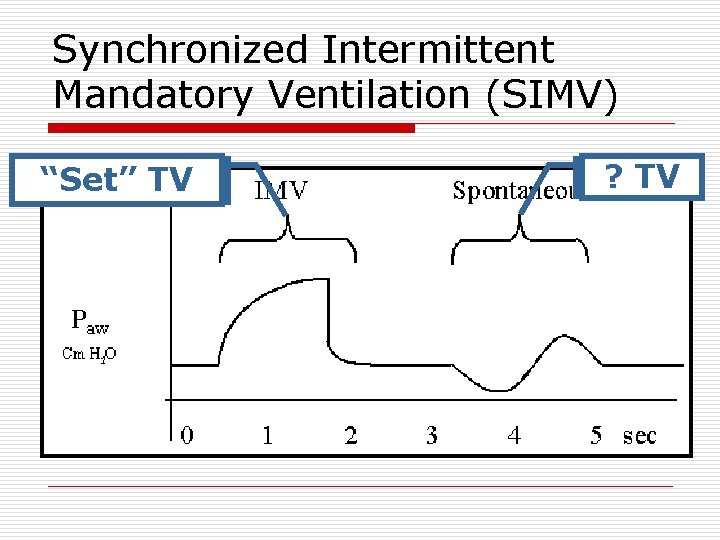
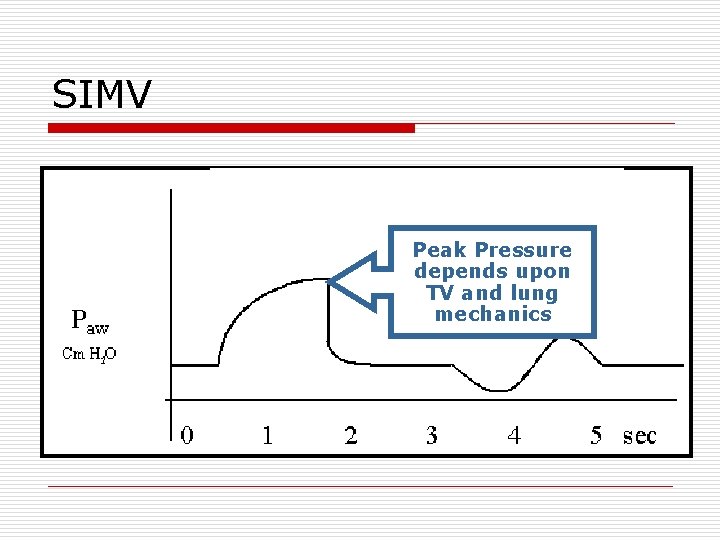
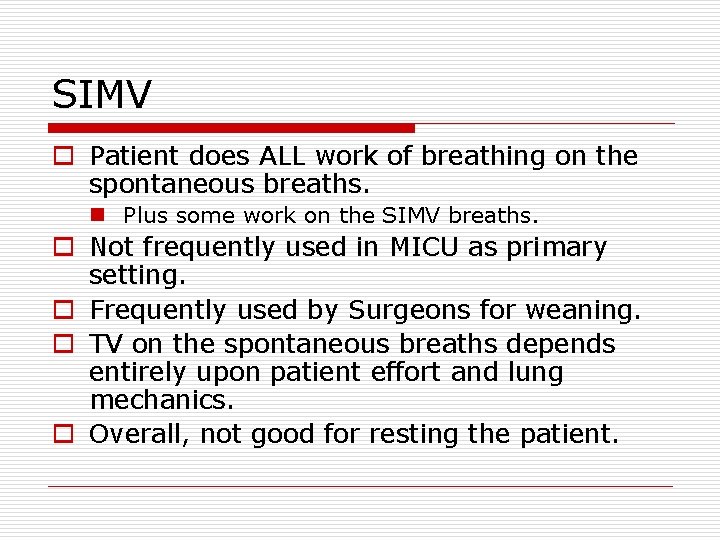
SIMV o Machine assists for set number of breaths only. o Other breaths patient is on their own with or without pressure support. o For machine delivered breaths can be combined with VC, PC, or VC+ o Spontaneous breaths – PS only!
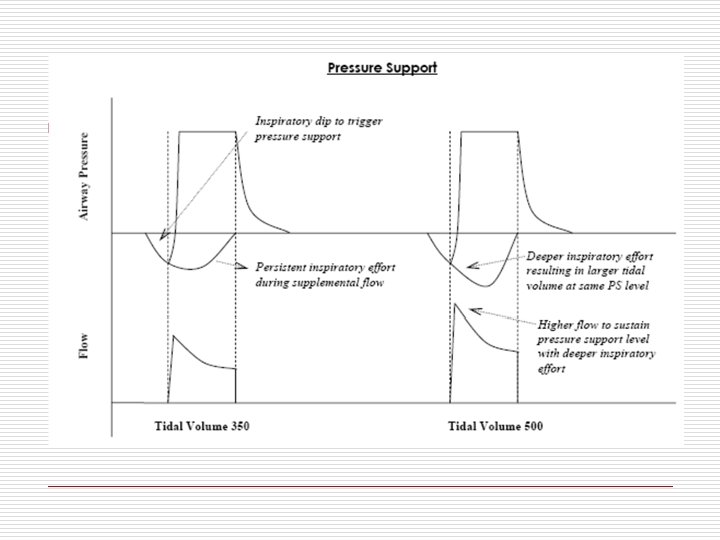
Pressure Support o Respiratory rate is completely patient dependent o Machine augments the patient’s breath by at a flow rate which adjusts itself to the patient’s effort. o A relatively constant, preset airway pressure is sustained during inspiration. o This added flow is terminated when the patient exhales. o Can deliver high or low level support.
Volume Control o We set the Tidal volume (TV) delivered o We set the Respiratory Rate (RR) o We set the Flow (V) o We do not control Airway Pressures
Pressure Control o We set the airway pressure o We set the Time of inspiration Ti o We do not have control of tidal volume o We must closely monitor to ensure adequate tidal volumes are achieved.
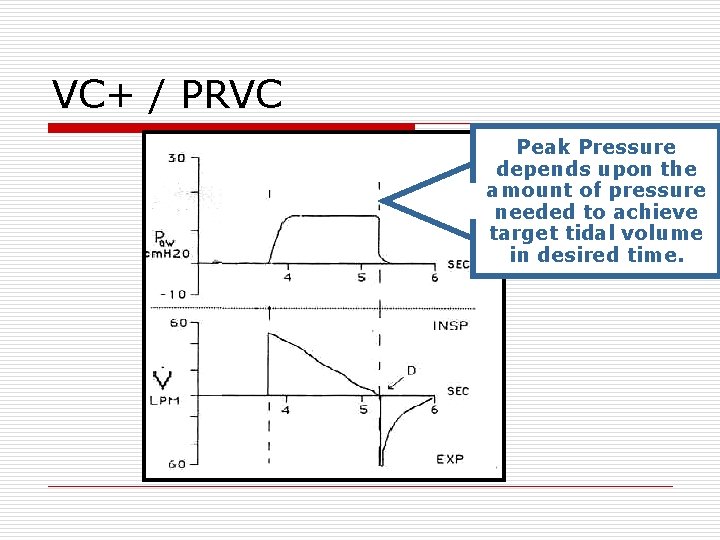
VC+ / PRVC o Pressure Control Ventilation to a Specific Volume Target o We set target TV o We set Ti o Machine adjusts pressure needed to achieve TV in set Ti. o It uses the returned TV of recent past breaths to constantly fine tune required pressure o Physiologically closest to normal breathing outside of Pressure Support.
PEEP o Positive End Expiratory Pressure o Helps keep aveoli inflated o High peep can help recruitment in ARDS and has been shown to have no negative impact on mortality. o PEEP can affect blood pressure and contribute to hypotension.
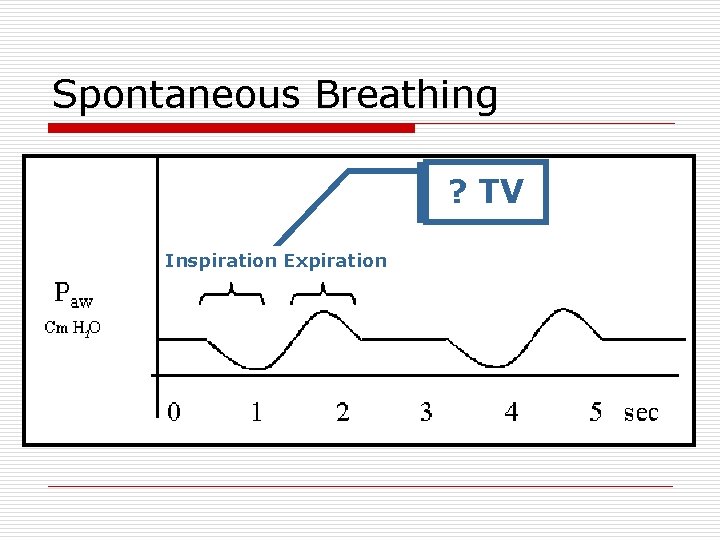
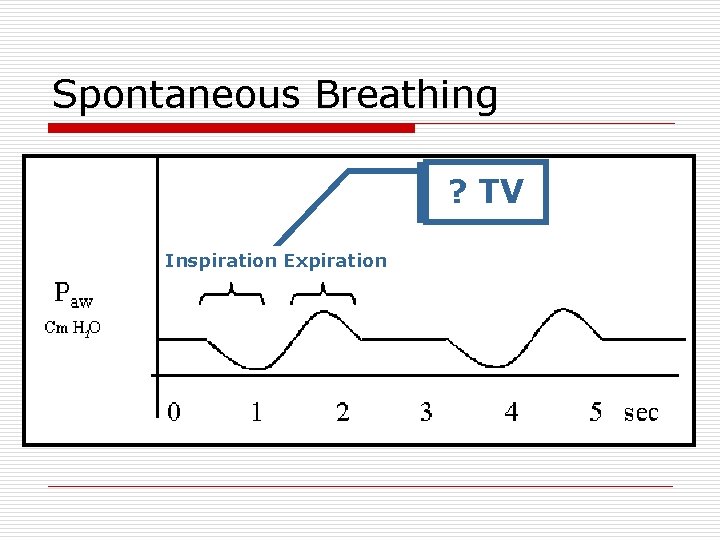
Spontaneous Breathing ? TV Inspiration Expiration
Spontaneous Breathing o Patient does ALL work of breathing o TV depends entirely upon patient effort and lung mechanics
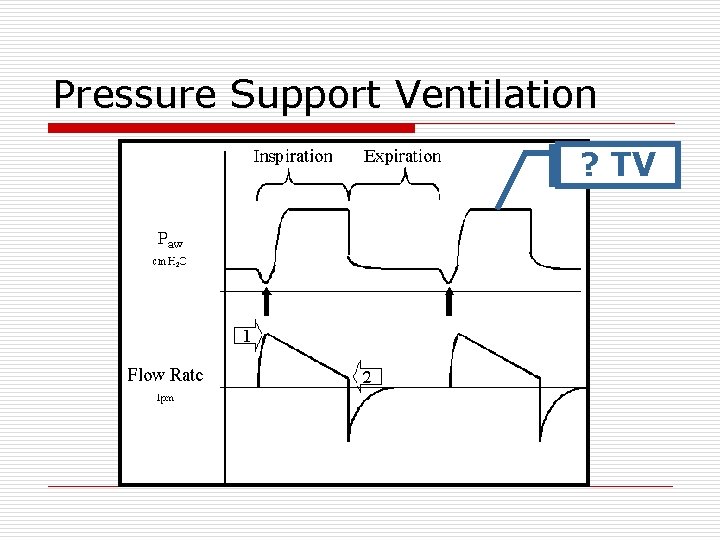
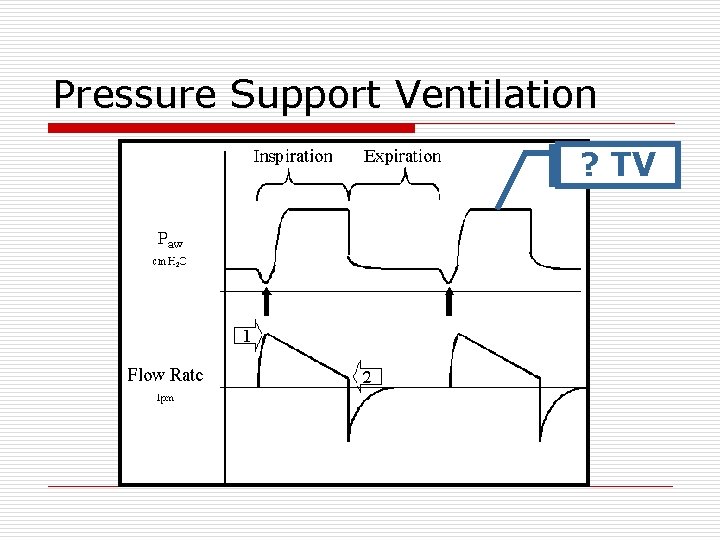
Pressure Support Ventilation ? TV
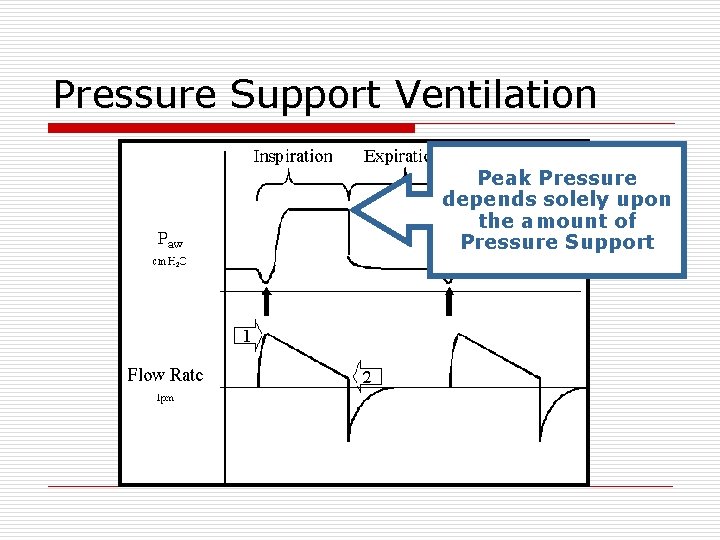
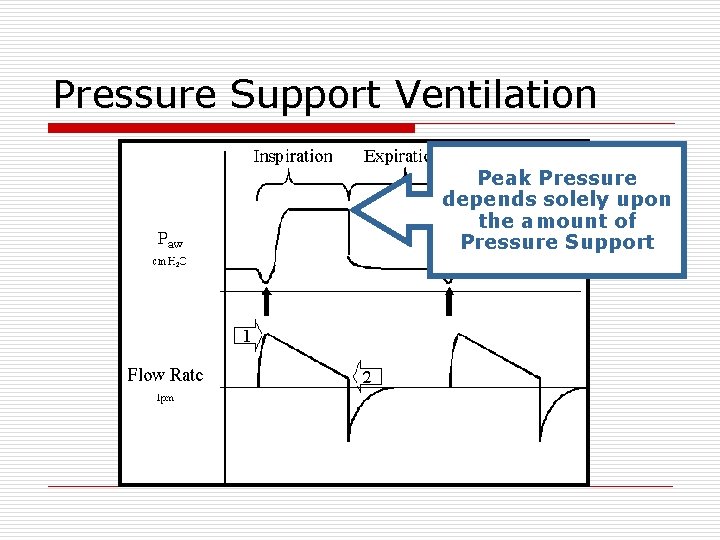
Pressure Support Ventilation Peak Pressure depends solely upon the amount of Pressure Support
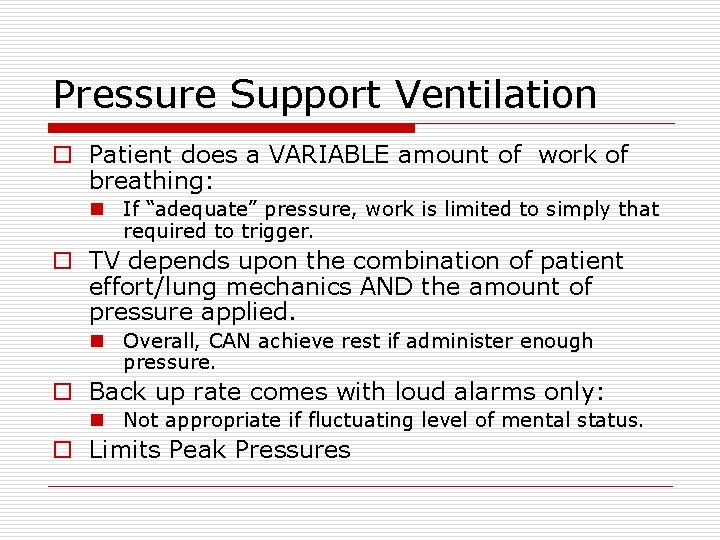
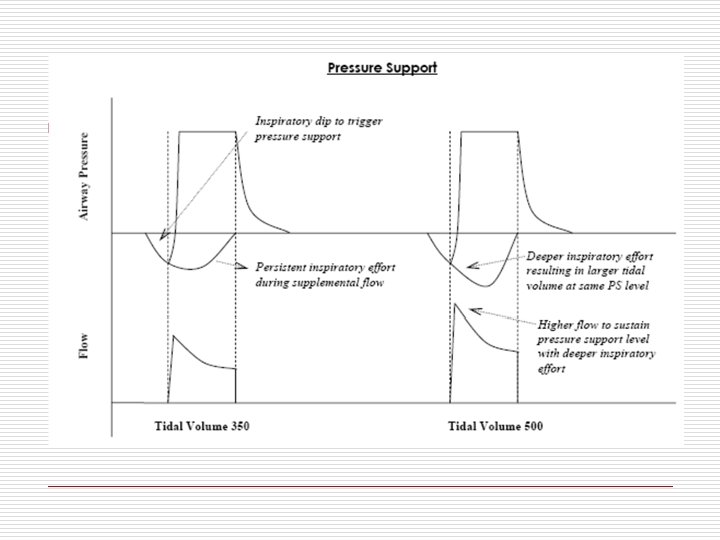
Pressure Support Ventilation o Patient does a VARIABLE amount of work of breathing: n If “adequate” pressure, work is limited to simply that required to trigger. o TV depends upon the combination of patient effort/lung mechanics AND the amount of pressure applied. n Overall, CAN achieve rest if administer enough pressure. o Back up rate comes with loud alarms only: n Not appropriate if fluctuating level of mental status. o Limits Peak Pressures
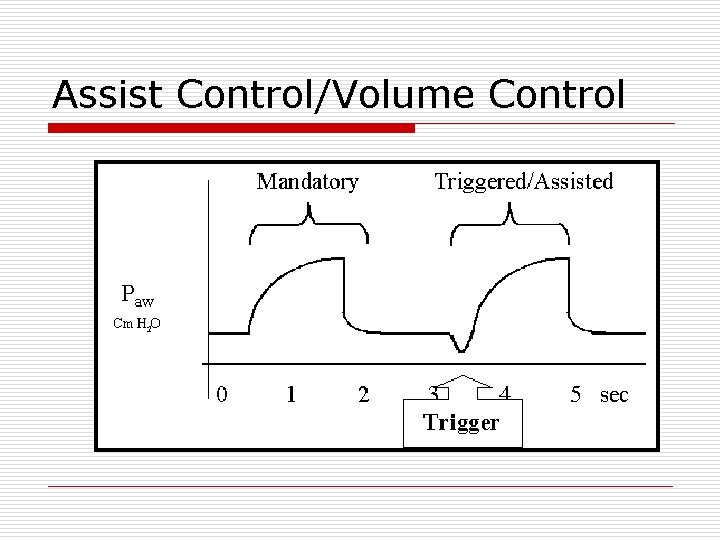
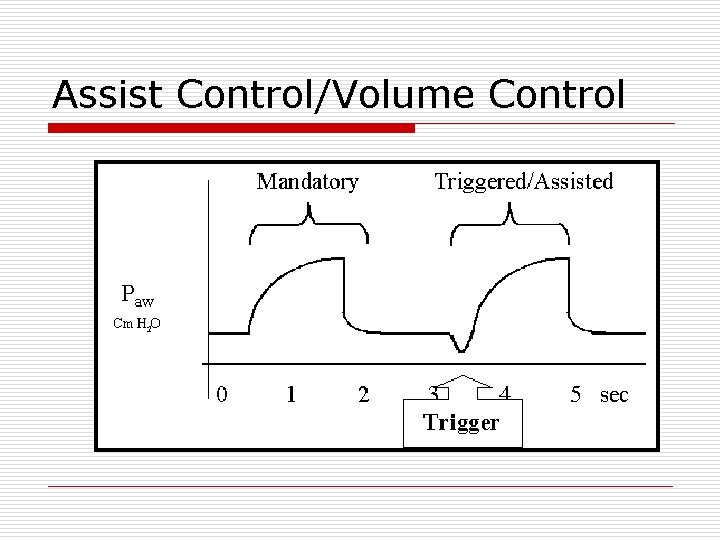
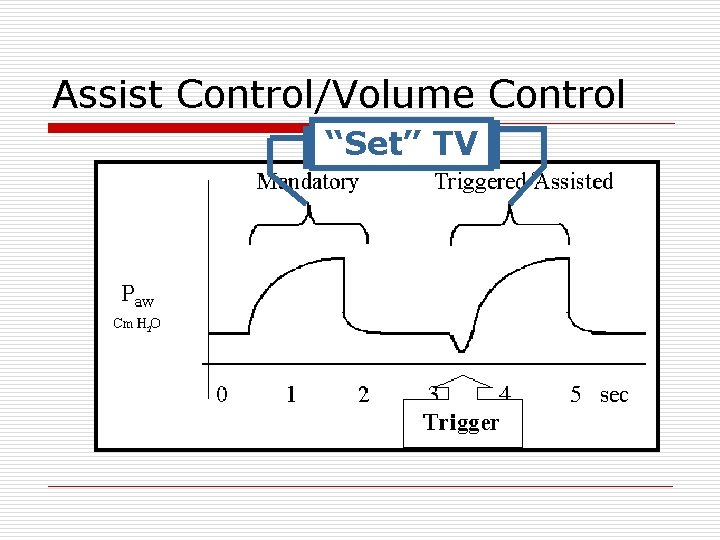
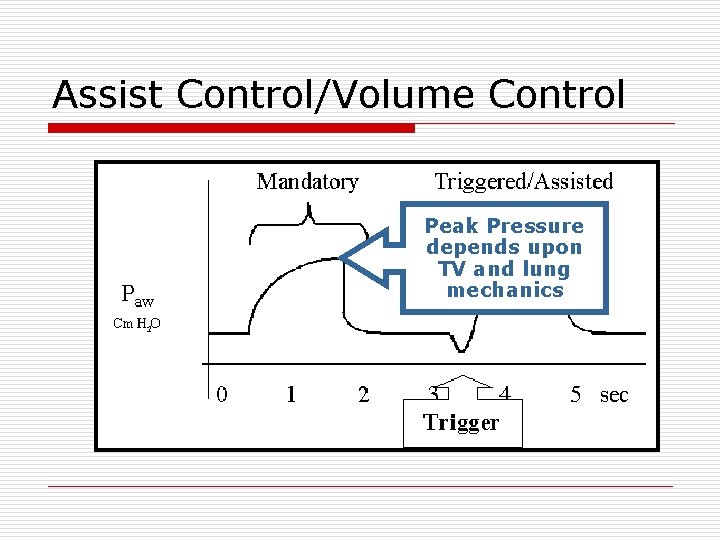
Assist Control/Volume Control
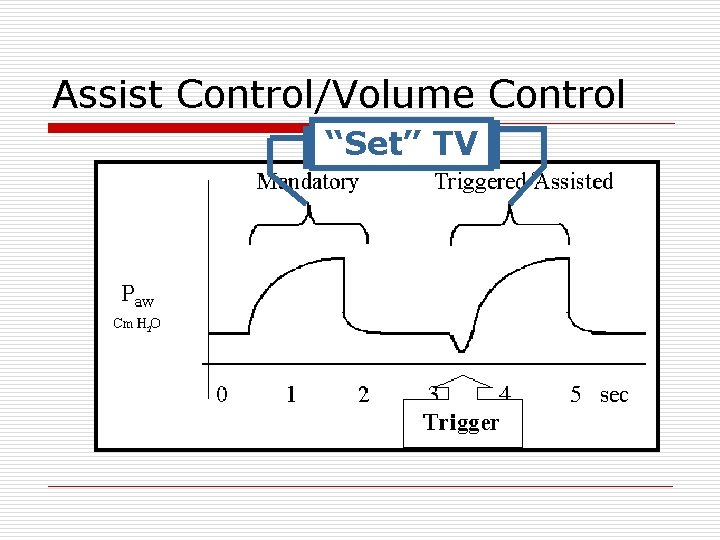
Assist Control/Volume Control “Set” TV
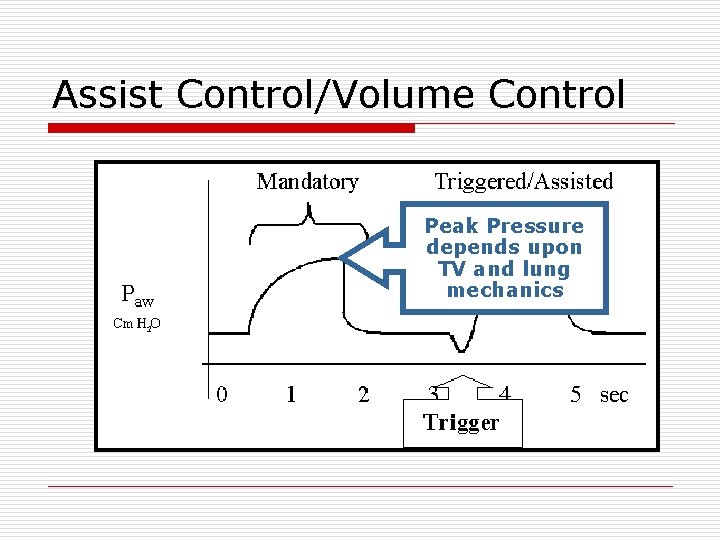
Assist Control/Volume Control Peak Pressure depends upon TV and lung mechanics
Assist Control/Volume Control o Every Breath You Take n Machine assists on every breath. n Patient does ONLY the work necessary to “trigger” the vent. n Diaphragm is used and exercised in respiratory effort n Typically, minimal (i. e. , 2 cm H 2 O) o TV is always the “set” TV. o Overall, a very good mode for resting the patient.
Flow Rates o “Normal” ~ 1 L/sec or 60 L/min n “Abnormal” Flow Rates o May be uncomfortable and increase WOB o May induce tachypnea, double-triggering, auto-PEEP, ALARMS! o May be adjusted directly or indirectly n By changing the flow profile
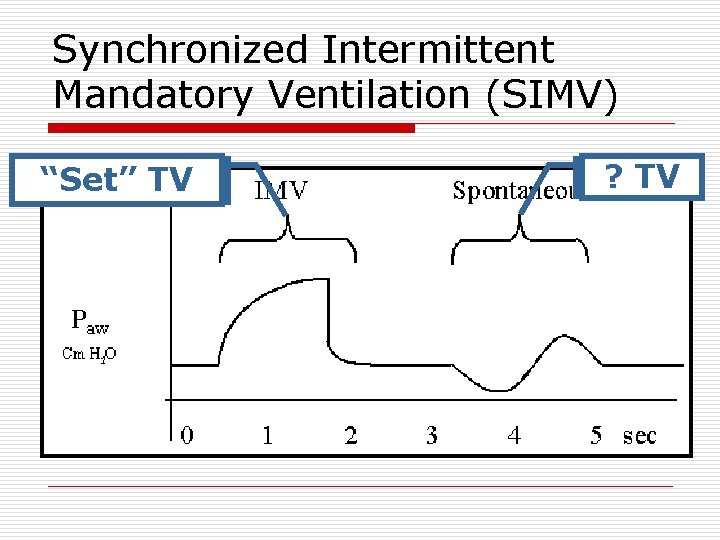
Synchronized Intermittent Mandatory Ventilation (SIMV) “Set” TV ? TV
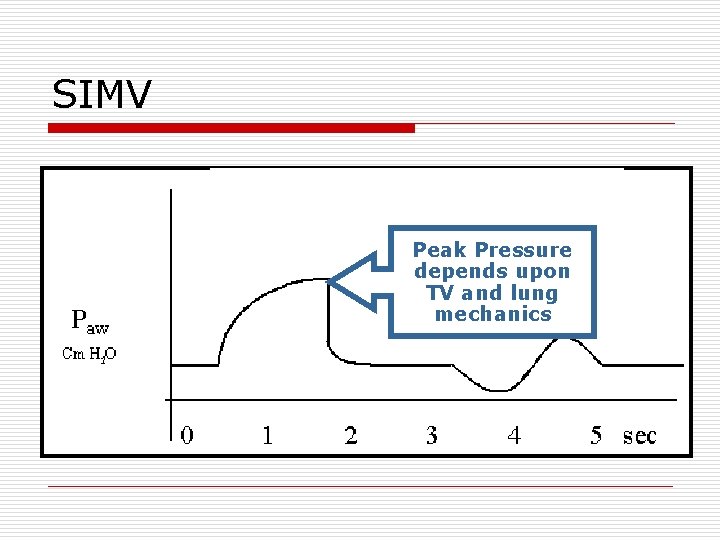
SIMV Peak Pressure depends upon TV and lung mechanics

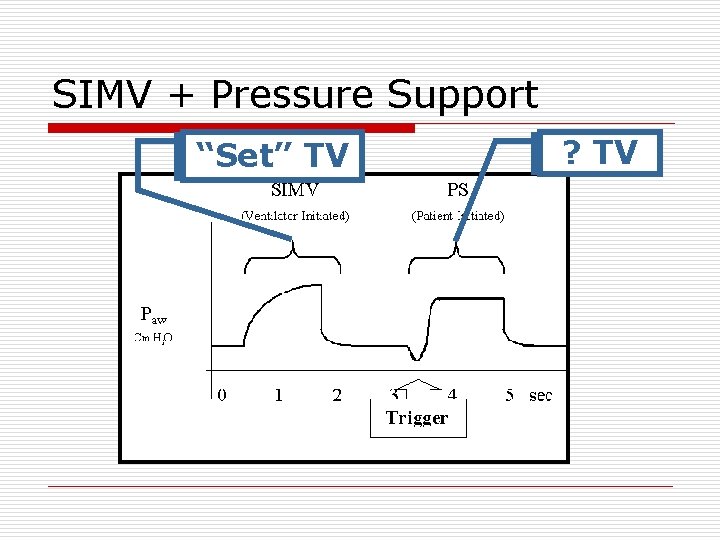
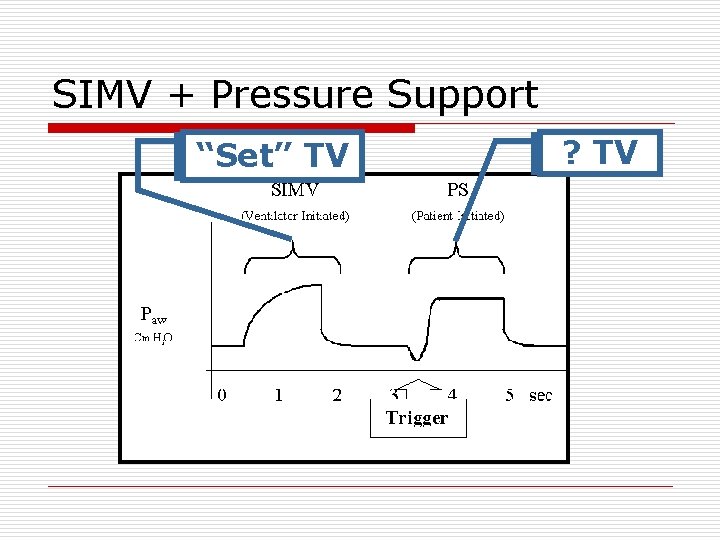
SIMV + Pressure Support “Set” TV ? TV
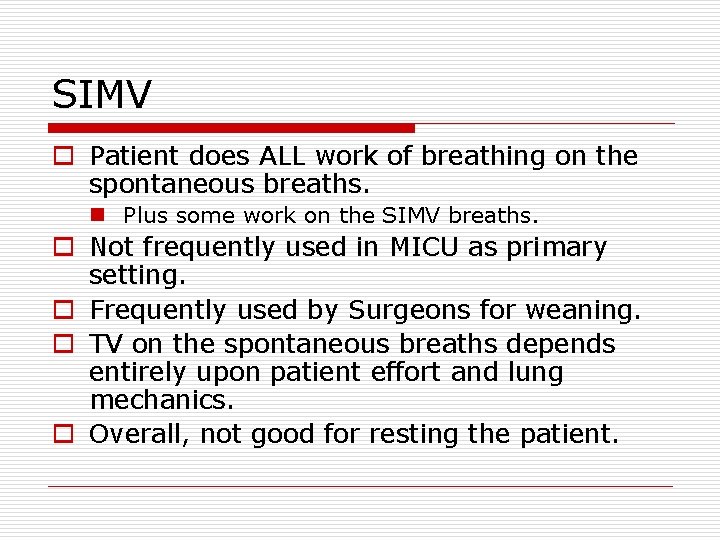
SIMV o Patient does ALL work of breathing on the spontaneous breaths. n Plus some work on the SIMV breaths. o Not frequently used in MICU as primary setting. o Frequently used by Surgeons for weaning. o TV on the spontaneous breaths depends entirely upon patient effort and lung mechanics. o Overall, not good for resting the patient.
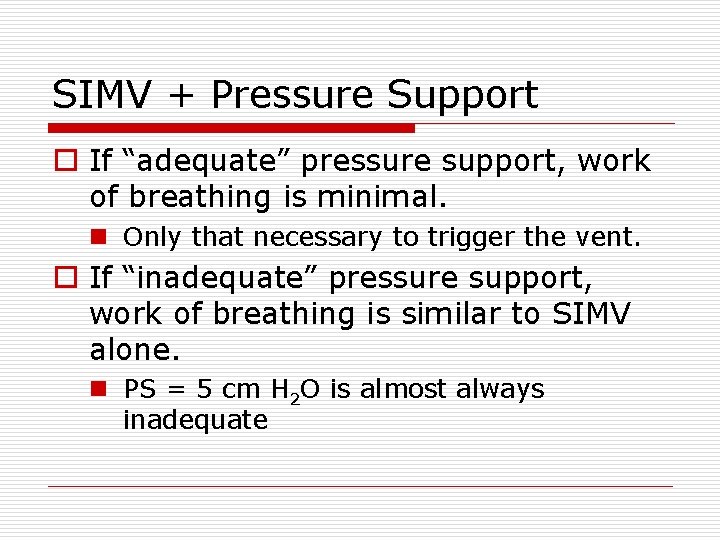
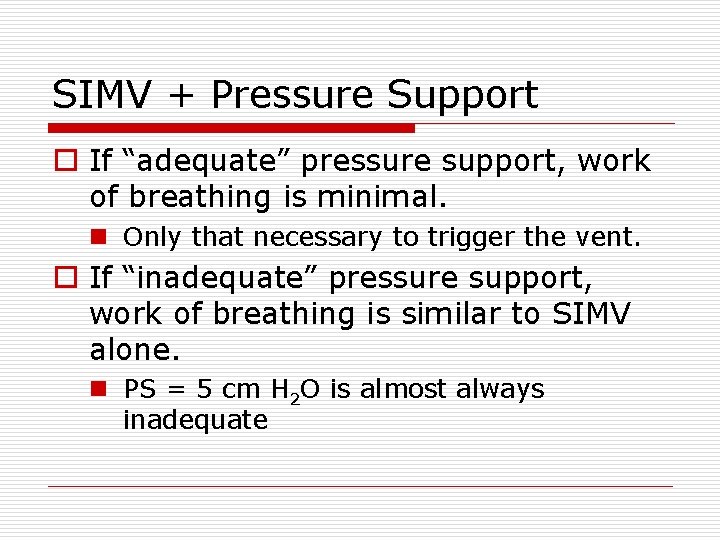
SIMV + Pressure Support o If “adequate” pressure support, work of breathing is minimal. n Only that necessary to trigger the vent. o If “inadequate” pressure support, work of breathing is similar to SIMV alone. n PS = 5 cm H 2 O is almost always inadequate
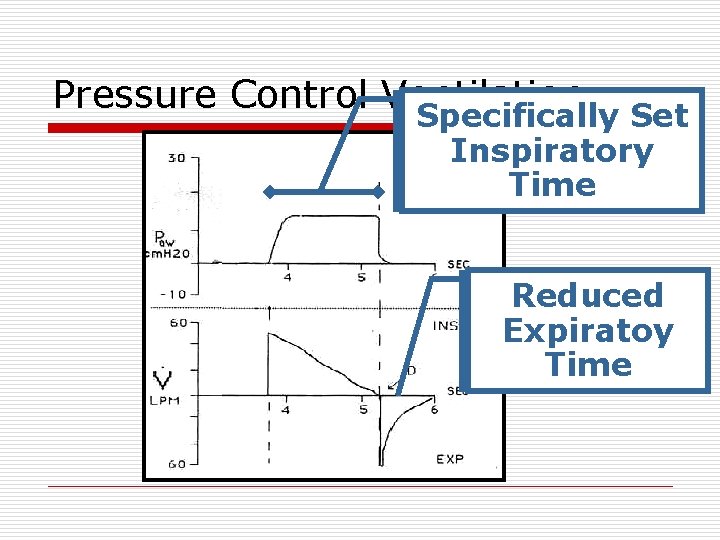
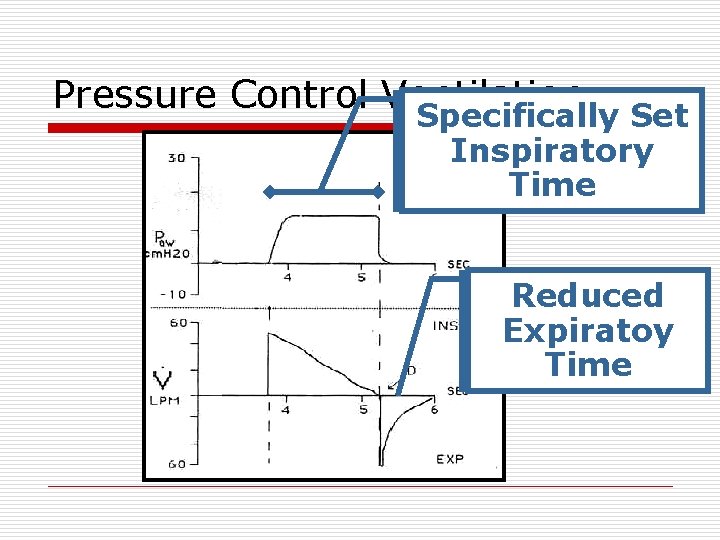
Pressure Control Ventilation Specifically Set Inspiratory Time Reduced Expiratoy Time
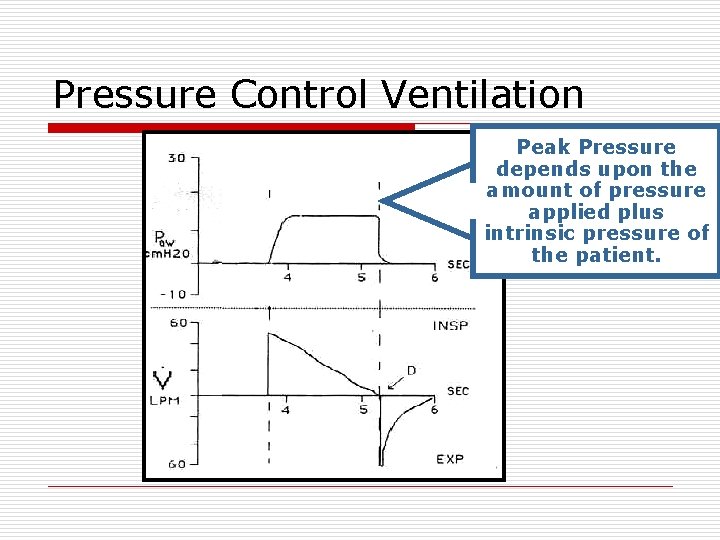
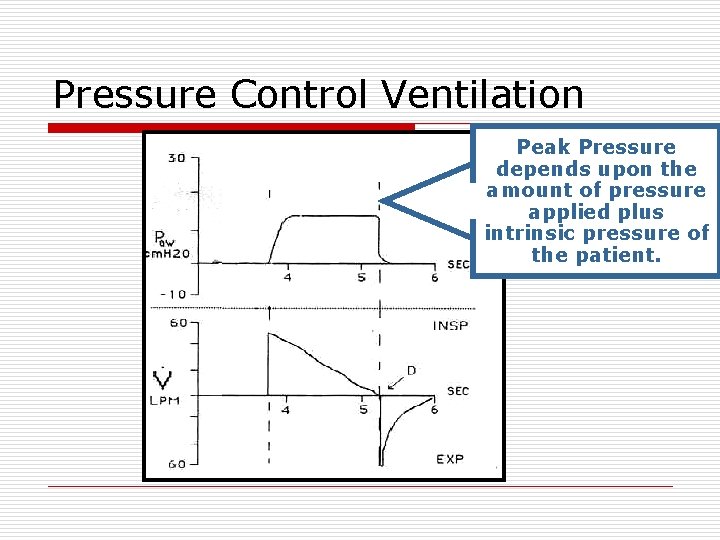
Pressure Control Ventilation Peak Pressure depends upon the amount of pressure applied plus intrinsic pressure of the patient.
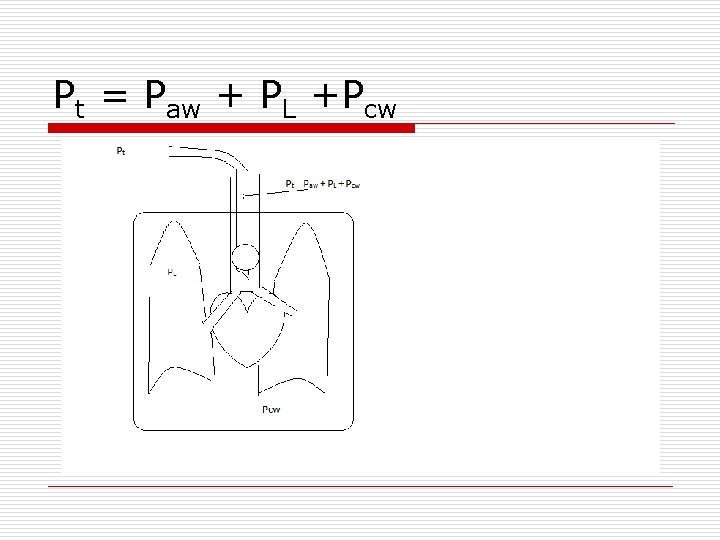
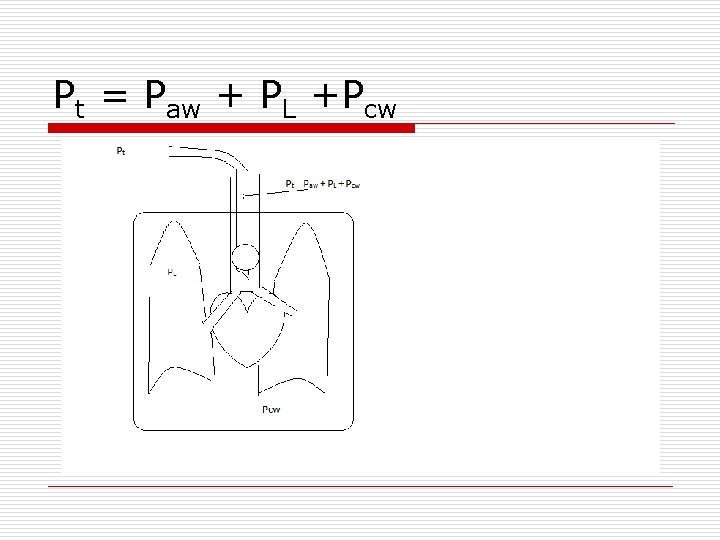
Pt = Paw + PL +Pcw
Pressure Control Ventilation o Almost never used as initial setting: n n Reserved for refractory hypoxemia. MAY increase gas exchange. Limits Peak Pressure. Very useful in ARDS settings.
Pressure Control Ventilation o Prolonged Inspiratory Time results in Reduced Expiratory Time n Potential for auto-PEEP o Requires constant monitoring as changes in patient status will dramatically affect tidal volumes. o As the patient improves it will be necessary to decrease the inspiratory pressure.
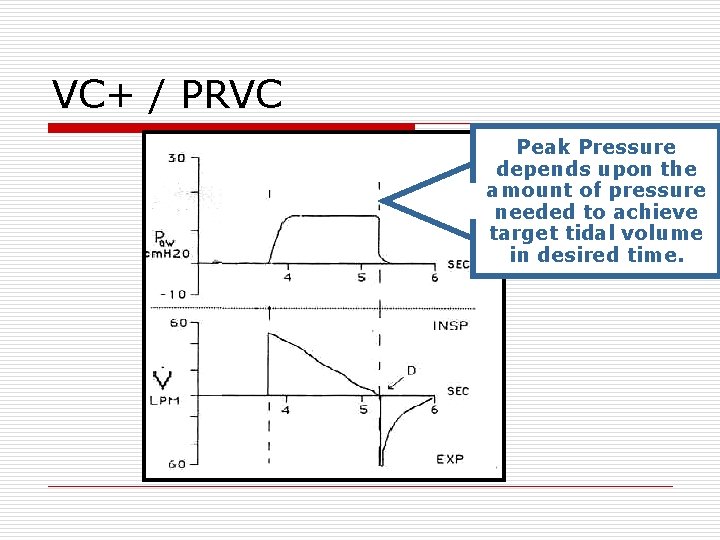
VC+ / PRVC Peak Pressure depends upon the amount of pressure needed to achieve target tidal volume in desired time.
Typical Initial Settings o Mode: A/C assist control or VC+ o RR: 12 -16 n Higher if patient has acidosis o Tidal Volumes n 6 – 8 cc/kg Ideal body weight n 6 cc/kg Ideal body weight strict if ARDS n If VC+ Ti of approx 0. 8 - 1. 25 seconds. o Oxygen n If severe hypoxia Fi. O 2 80 -100% n Titrate FIO 2 to Pa. O 2 of 70 -80 o Peep of 5 unless severely hypotensive.
Talk with your nurse! o Sedation/Pain Control: n Versed o (100 mg in 100 cc) o Start 1 mg/hr and titrate to Richmond Agitation Sedation Score = 0 n Fentanyl o (2500 mcg/50 cc) o Start 1 mcg/kg/hr and titrate to relief of pain o CXR n immediate and daily o Restraints o Dobhoff n CNU consult for TF’s o Change meds to suspension or IV o Titrate FIO 2 to maintain Sp. O 2 > 92% o ? ABG ? o ? MDI’s o NOTIFY FAMILY
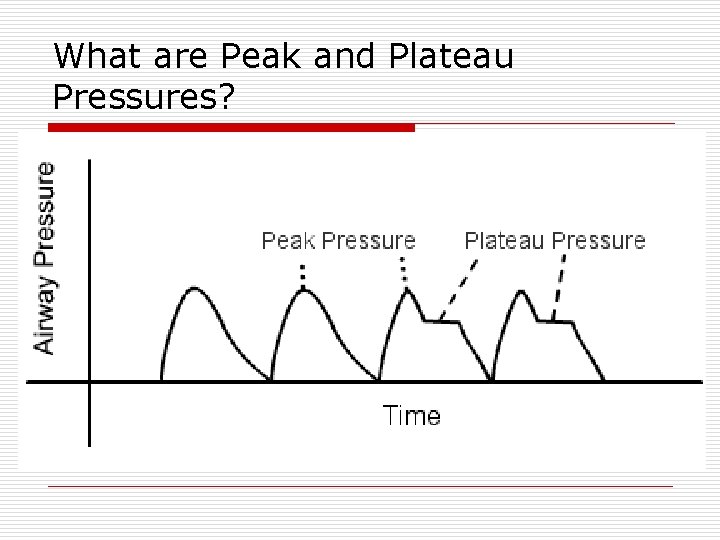
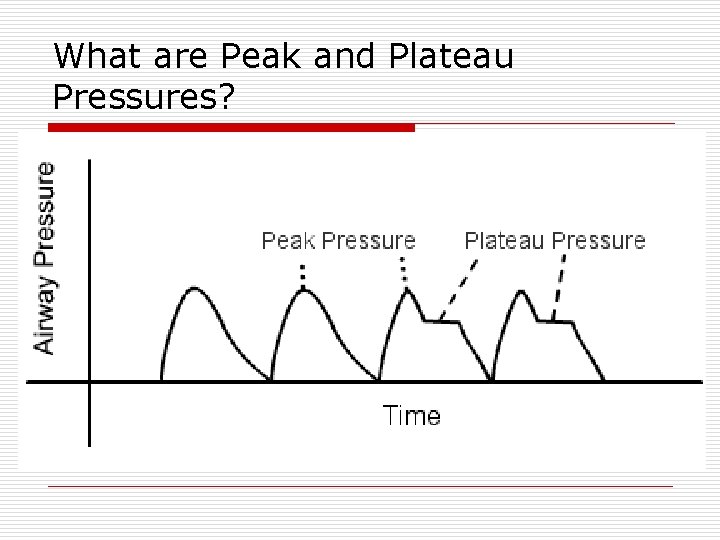
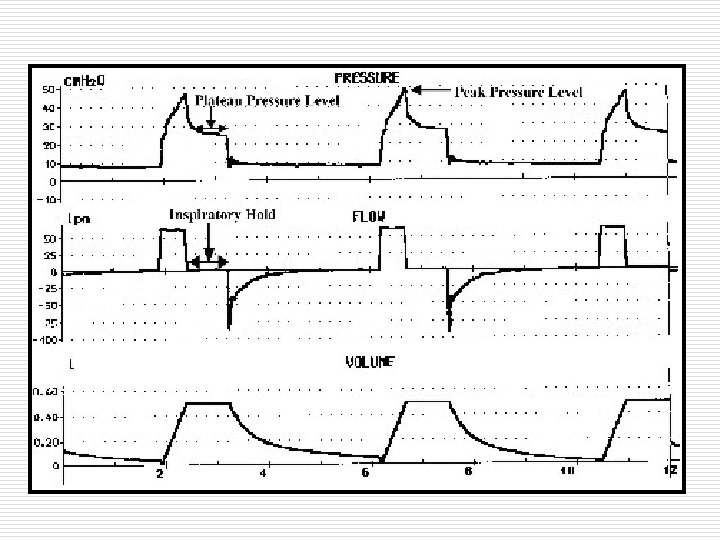
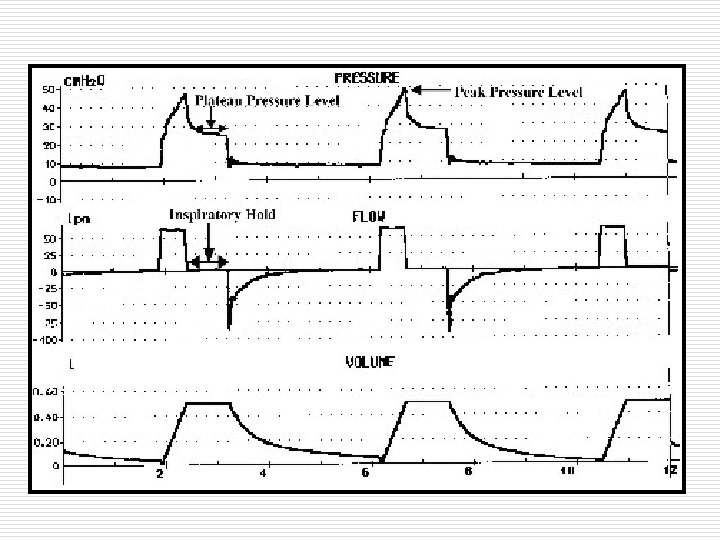
What are Peak and Plateau Pressures?
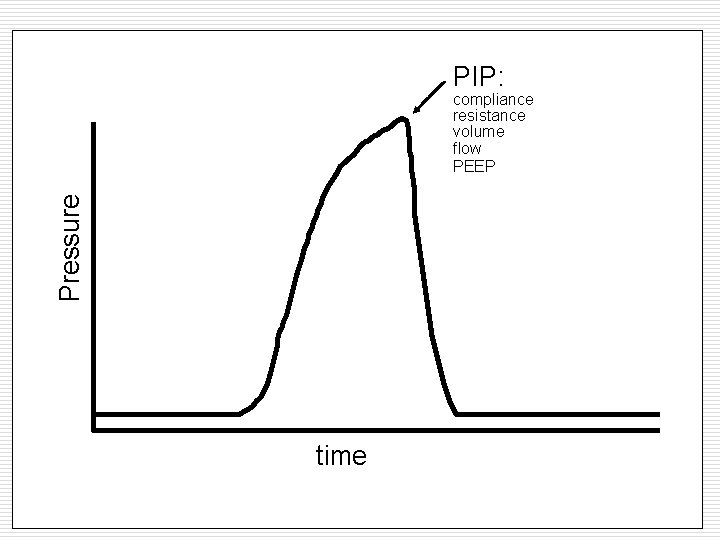
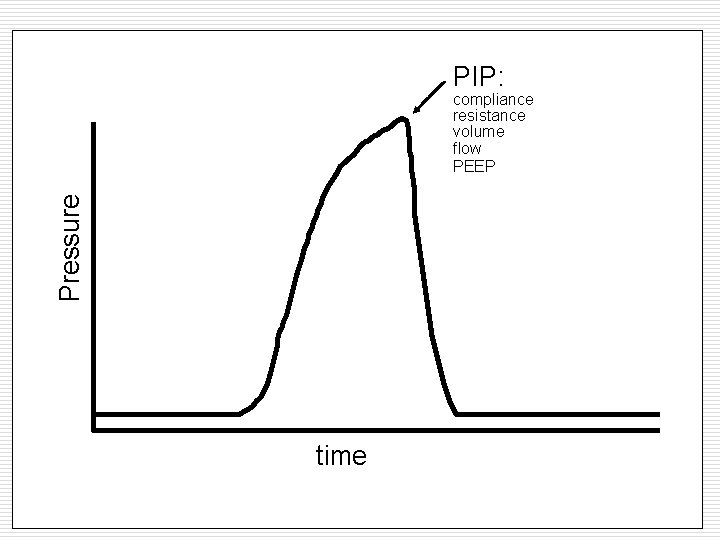
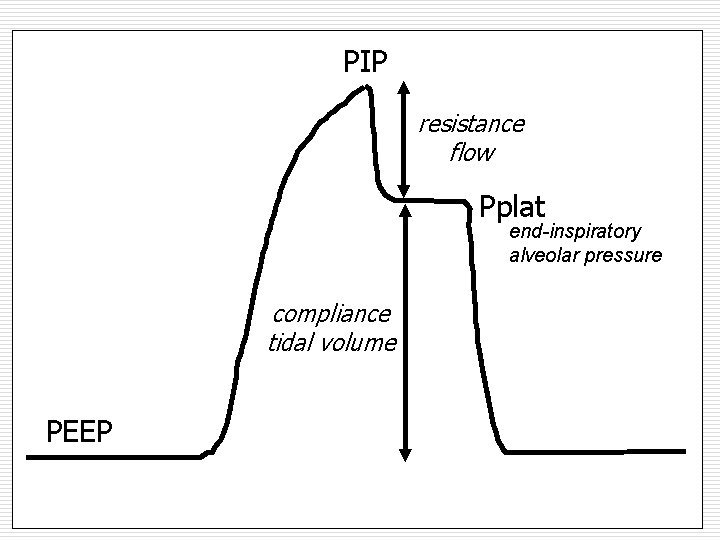
PIP: Pressure compliance resistance volume flow PEEP time
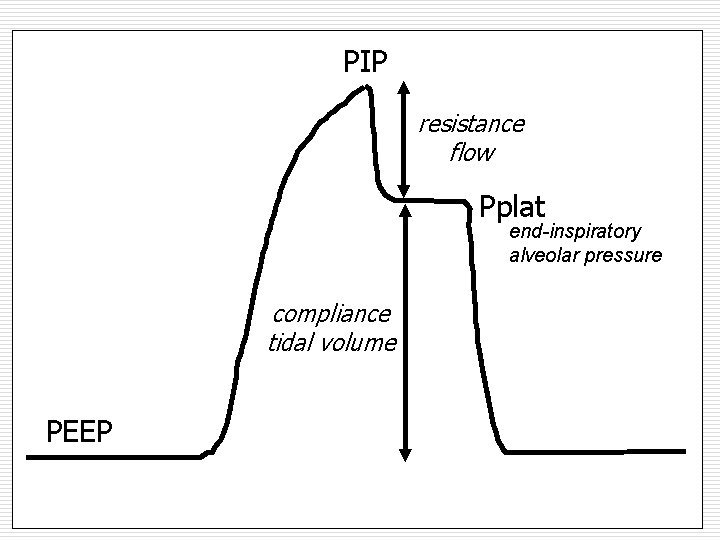
No active breathing Treats lung as single unit PIP resistance flow Pplat end-inspiratory alveolar pressure compliance tidal volume PEEP
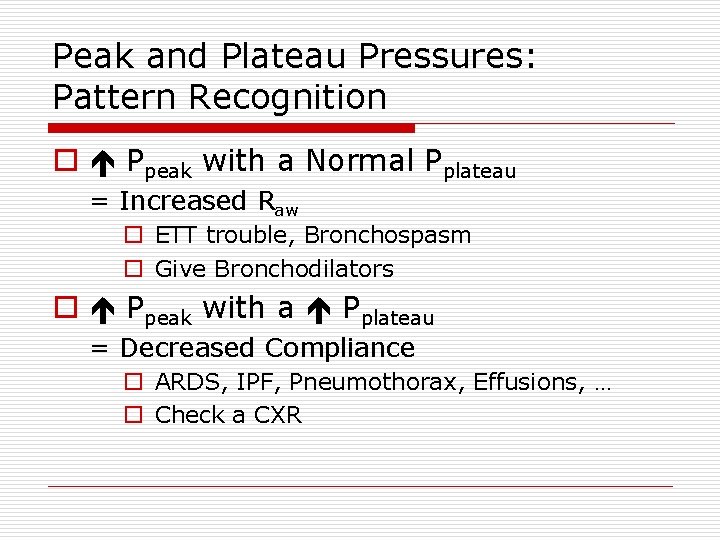
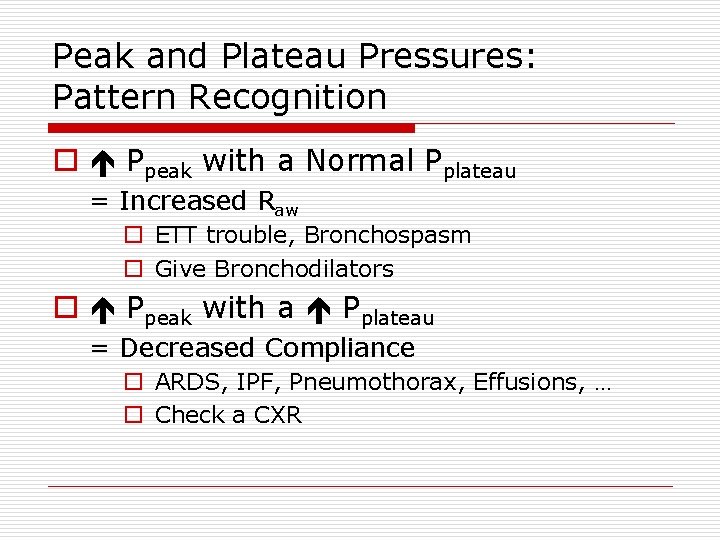
Peak and Plateau Pressures: Pattern Recognition o Ppeak with a Normal Pplateau = Increased Raw o ETT trouble, Bronchospasm o Give Bronchodilators o Ppeak with a Pplateau = Decreased Compliance o ARDS, IPF, Pneumothorax, Effusions, … o Check a CXR
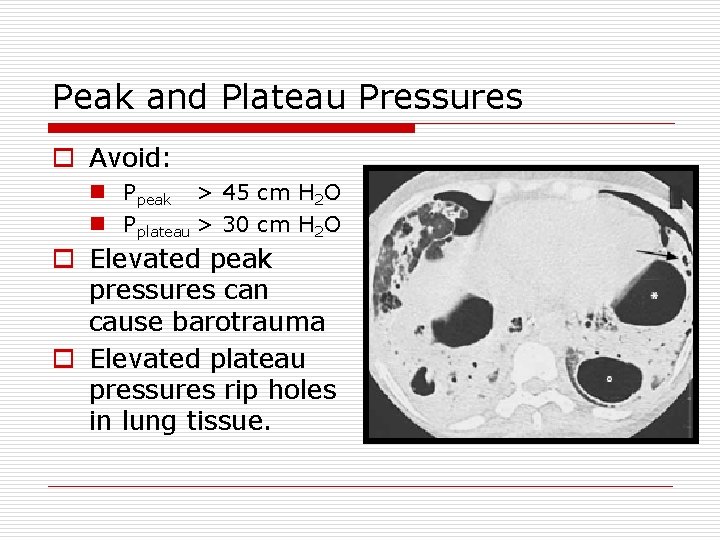
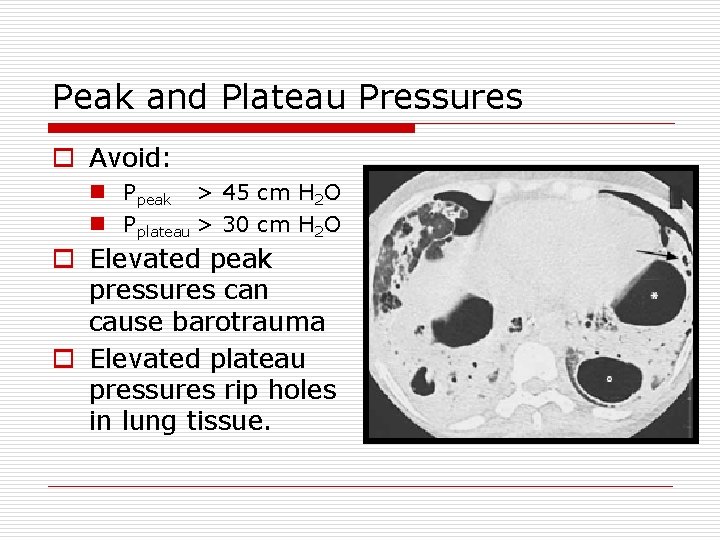
Peak and Plateau Pressures o Avoid: n Ppeak > 45 cm H 2 O n Pplateau > 30 cm H 2 O o Elevated peak pressures can cause barotrauma o Elevated plateau pressures rip holes in lung tissue.

Patient Ventilator Dyssynchrony Nilsestuen, Respir Care 2005; 50: 202 -232
Measuring Auto-PEEP o Retained air at end of breath o Another name for breath stacking o Apply an “expiratory hold” o Assess pressure rise
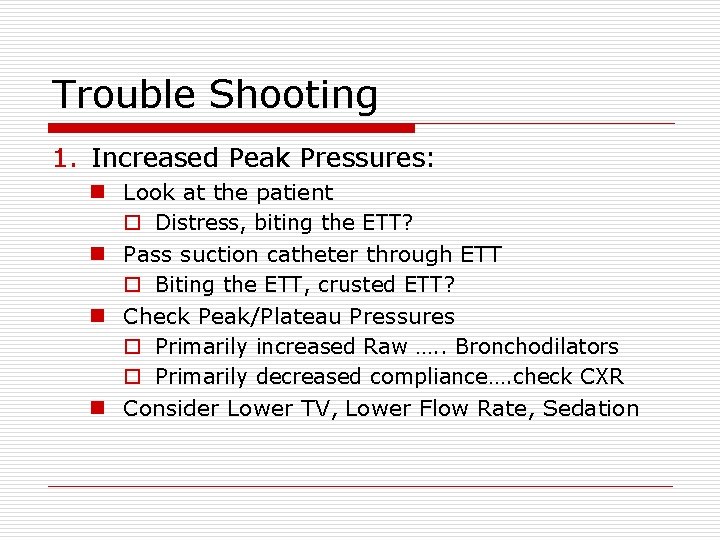
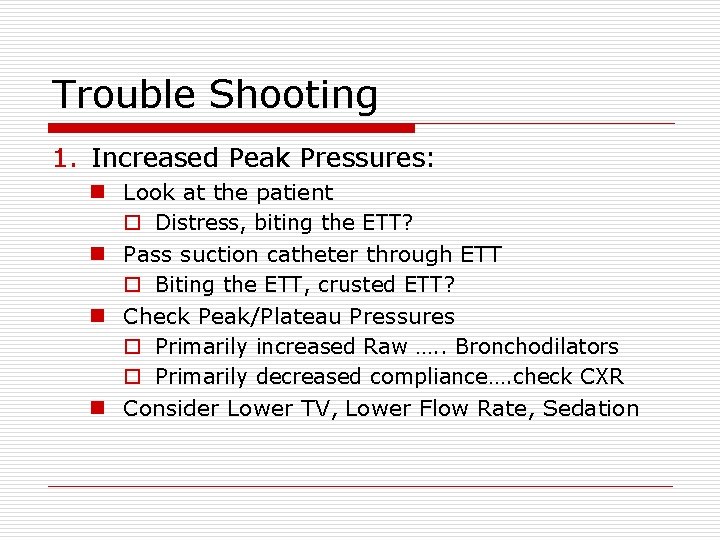
Trouble Shooting 1. Increased Peak Pressures: n Look at the patient o Distress, biting the ETT? n Pass suction catheter through ETT o Biting the ETT, crusted ETT? n Check Peak/Plateau Pressures o Primarily increased Raw …. . Bronchodilators o Primarily decreased compliance…. check CXR n Consider Lower TV, Lower Flow Rate, Sedation
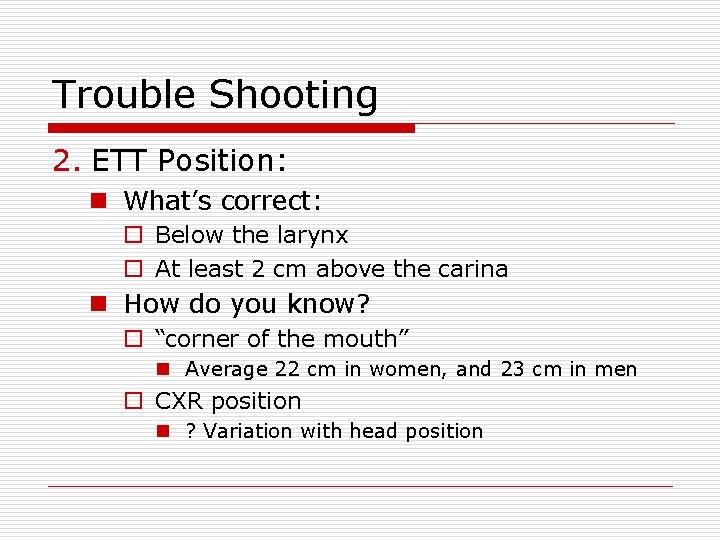
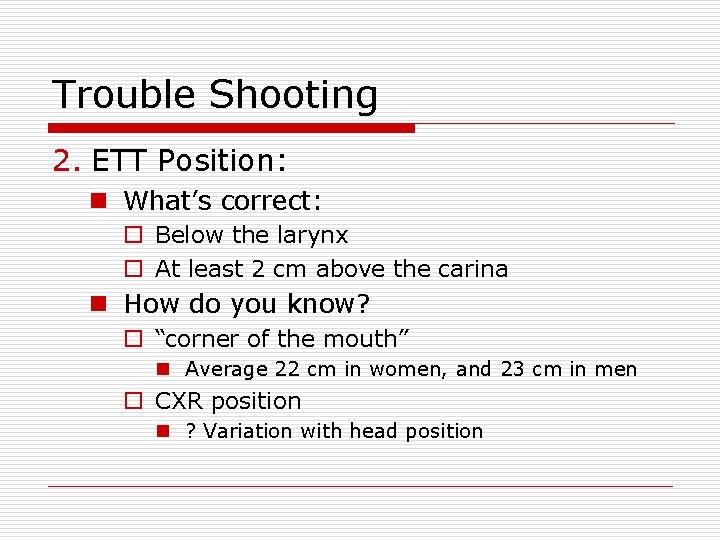
Trouble Shooting 2. ETT Position: n What’s correct: o Below the larynx o At least 2 cm above the carina n How do you know? o “corner of the mouth” n Average 22 cm in women, and 23 cm in men o CXR position n ? Variation with head position
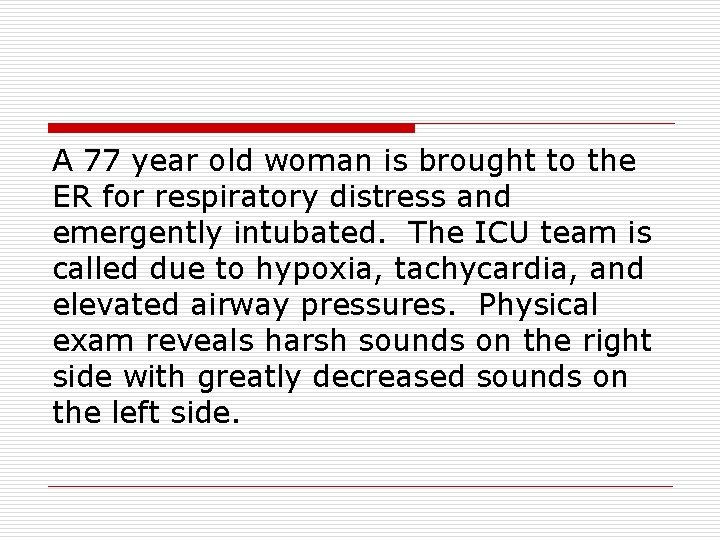
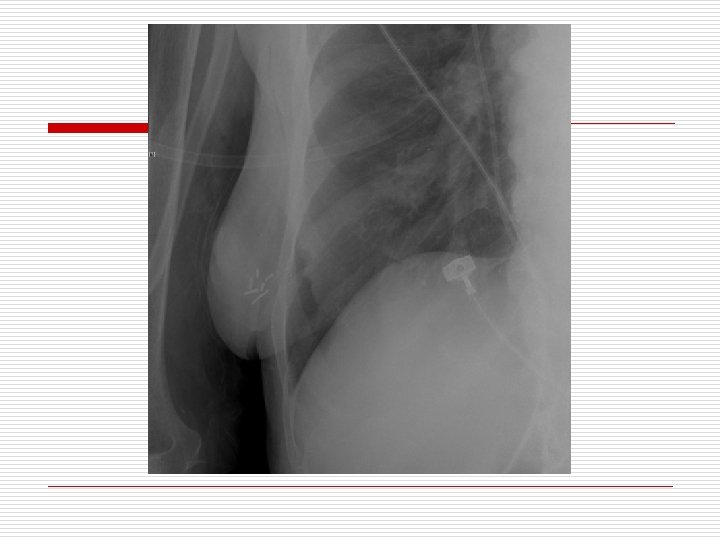
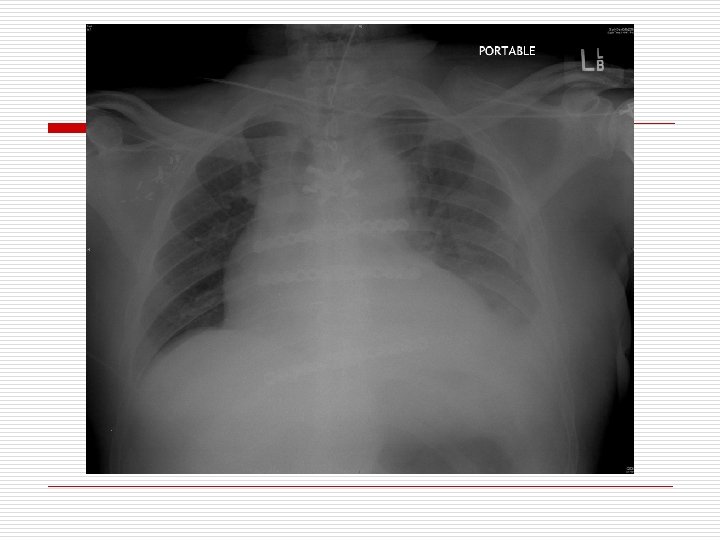
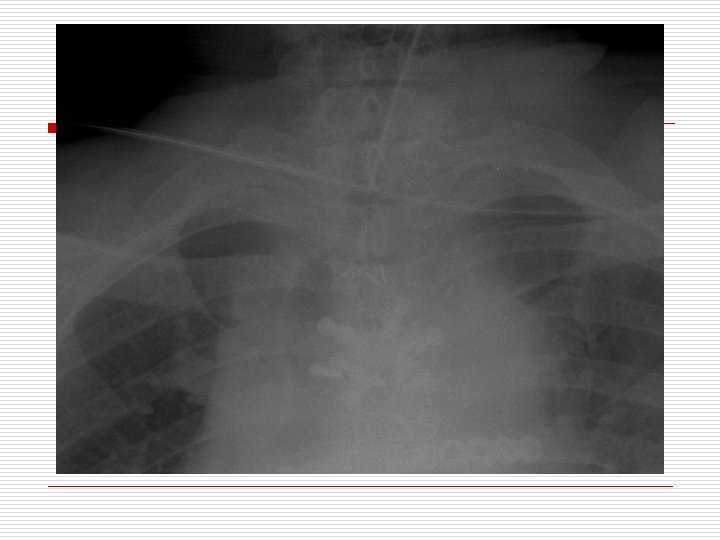
A 77 year old woman is brought to the ER for respiratory distress and emergently intubated. The ICU team is called due to hypoxia, tachycardia, and elevated airway pressures. Physical exam reveals harsh sounds on the right side with greatly decreased sounds on the left side.
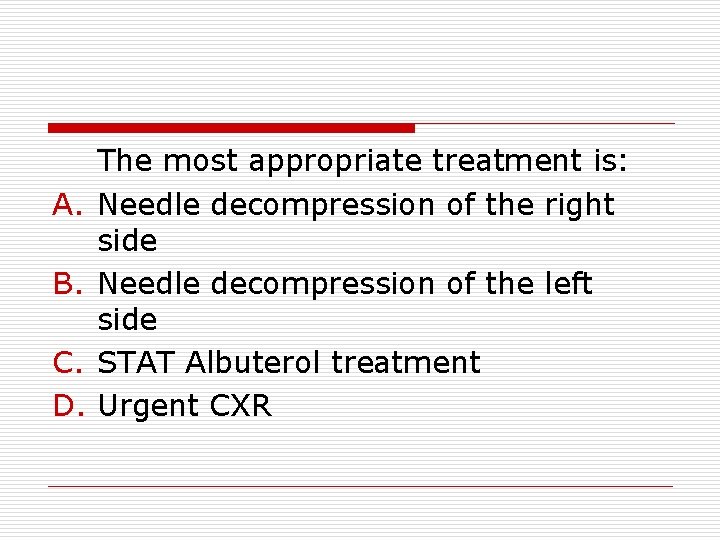
A. B. C. D. The most appropriate treatment is: Needle decompression of the right side Needle decompression of the left side STAT Albuterol treatment Urgent CXR
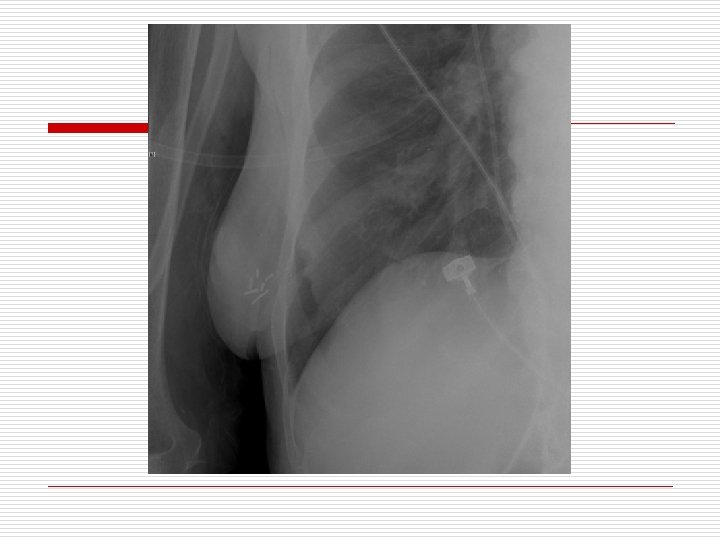
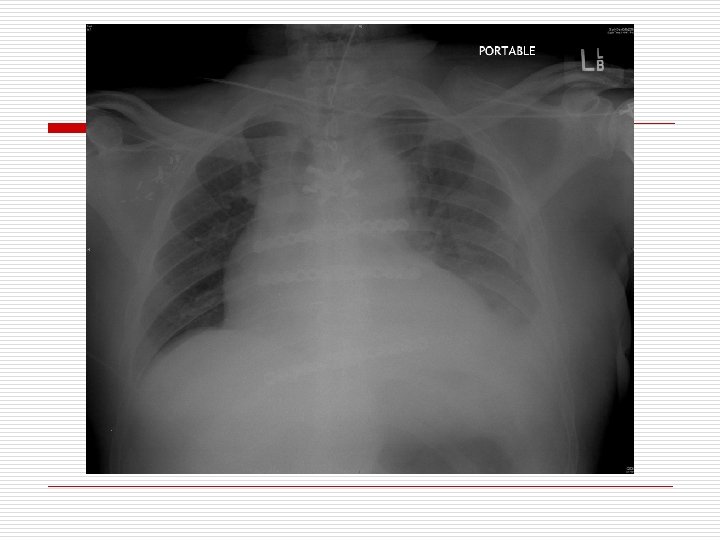
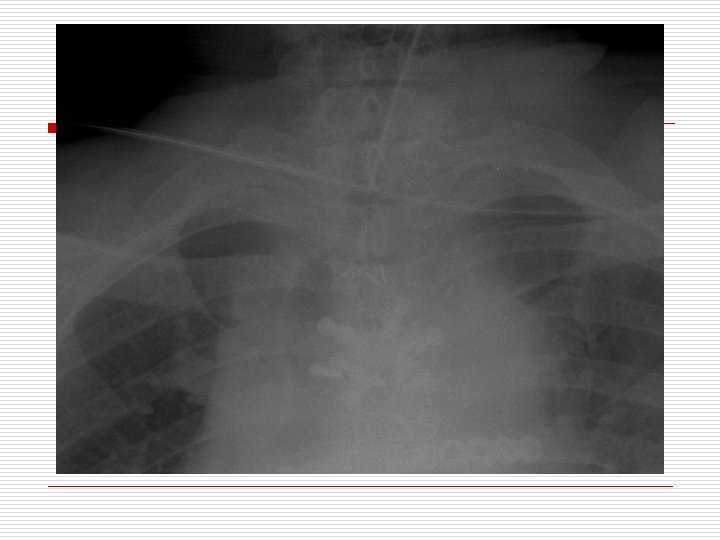
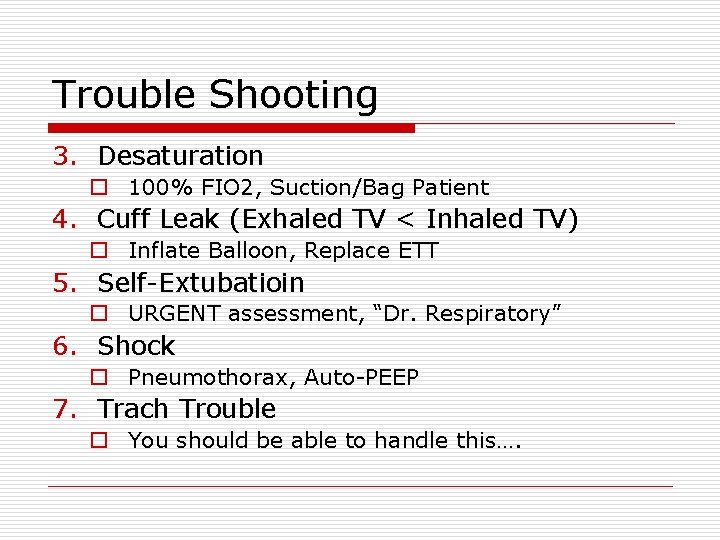
Trouble Shooting 3. Desaturation o 100% FIO 2, Suction/Bag Patient 4. Cuff Leak (Exhaled TV < Inhaled TV) o Inflate Balloon, Replace ETT 5. Self-Extubatioin o URGENT assessment, “Dr. Respiratory” 6. Shock o Pneumothorax, Auto-PEEP 7. Trach Trouble o You should be able to handle this….
Weaning - Daily Assessment Did we fix the initial problem? ? ? Is the patient hypoxic – Pa. O 2/FIO 2 > 200 Is the patient hemodynamically stable? Does the patient have a moderate to severe metabolic or respiratory abnormality? n Are we planning any major procedures today outside of Tracheotomy? n What is the RASS? n n
Modes of Weaning o o Pressure Support SIMV T – Piece Further Questions n Has the patient failed multiple weaning attempts before n Does the patient have a tracheotomy?
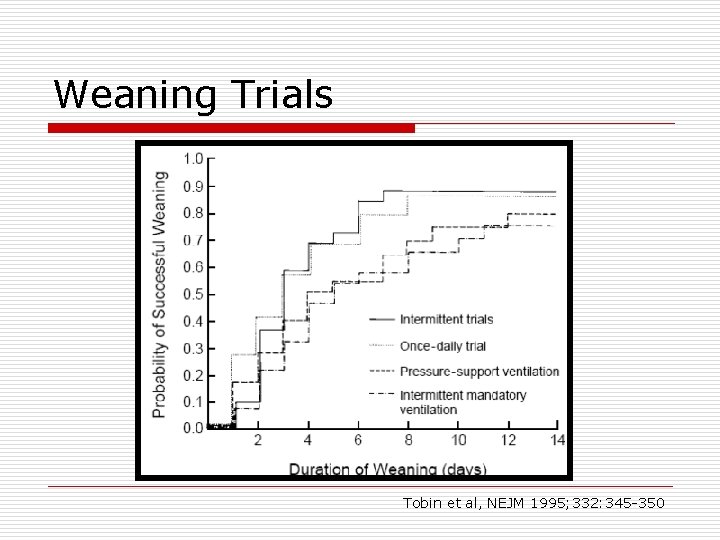
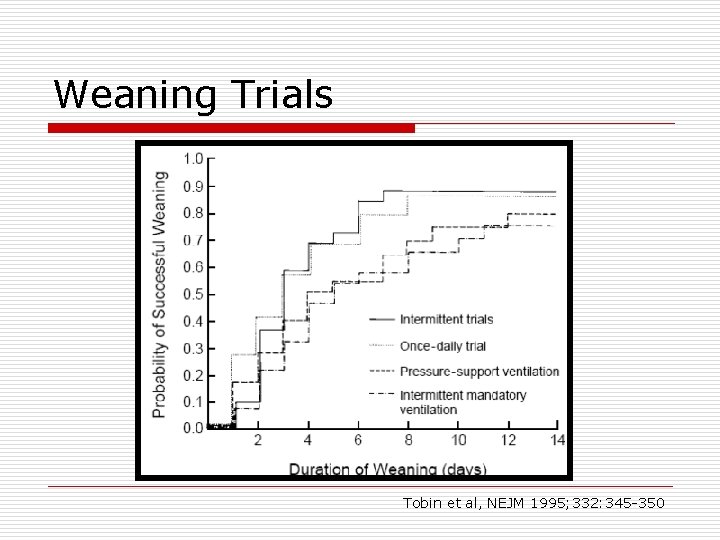
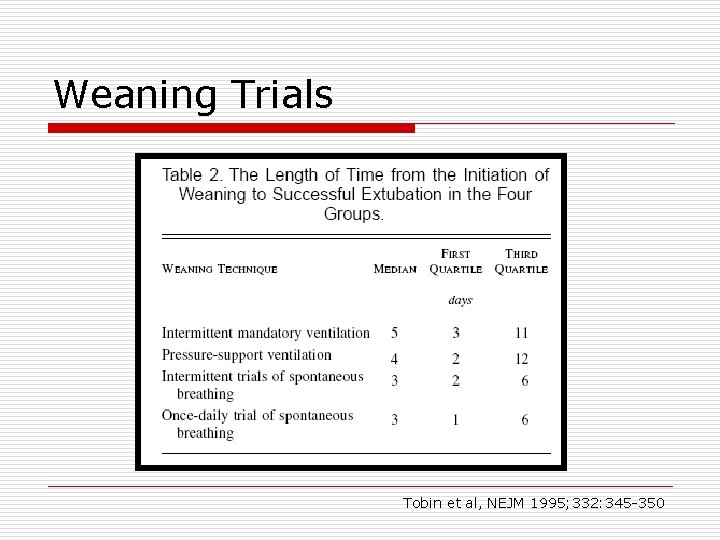
Weaning Trials Tobin et al, NEJM 1995; 332: 345 -350
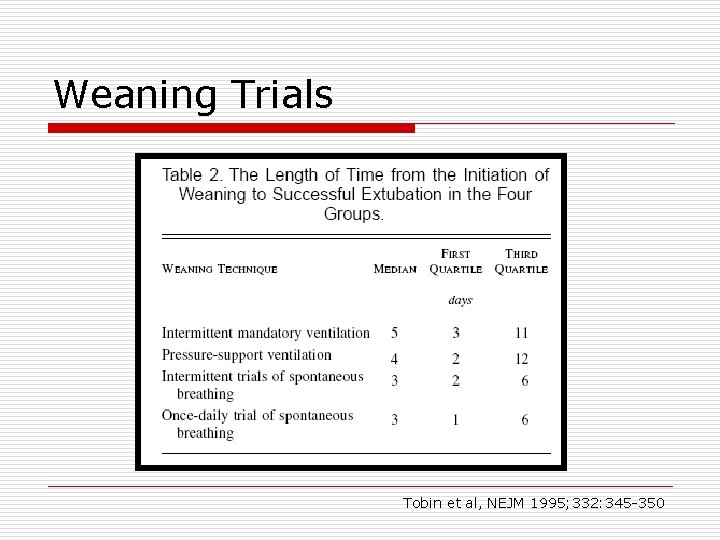
Weaning Trials Tobin et al, NEJM 1995; 332: 345 -350
Trials of trials… o Multiple studies have shown that PS trials with low pressure (5 -8) performed once daily are equally effective as T – piece studies. o Some trials have shown SIMV weans take longer to get there - additional ventilator days. o The jury is still very much out.
What do We Do? o Daily assessment to hold sedation (Sedation Vacation). o Daily assessment by respiratory therapy to evaluate for weaning. o If minute ventilation is < 13, patient is HD stable and neurologically able to cough, we try. n IF ETT ≤ 7. 5, PS 8 for 40 minutes n IF ETT ≥ 8, PS 5 for 40 minutes o Patient is watched at bedside for first 10 minutes for signs of distress. o ABG at 40 minutes.
Weaning Trial o Is RSBI (Rapid Shalow Breathing Index) - RR/TV is < 110 at end of 40 minutes? o Does the ABG shows no acute acidosis? o If yes to both, can extubate.
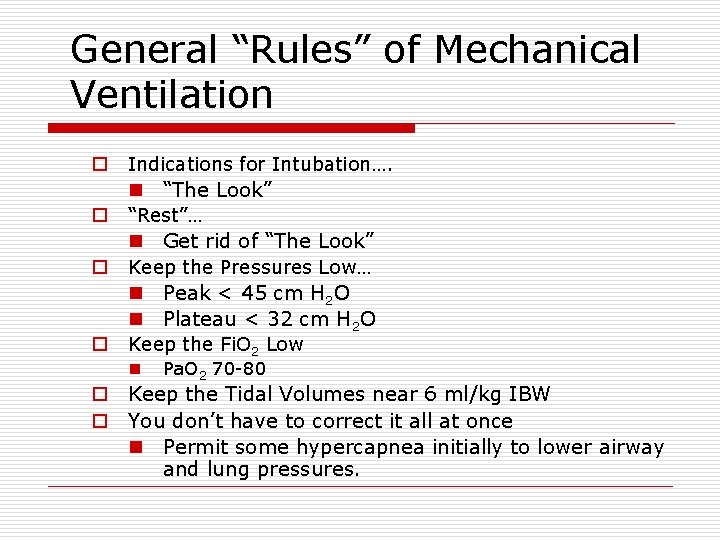
General “Rules” of Mechanical Ventilation o Indications for Intubation…. n “The Look” o “Rest”… n Get rid of “The Look” o o Keep the Pressures Low… n Peak < 45 cm H 2 O n Plateau < 32 cm H 2 O Keep the Fi. O 2 Low n Pa. O 2 70 -80 o Keep the Tidal Volumes near 6 ml/kg IBW o You don’t have to correct it all at once n Permit some hypercapnea initially to lower airway and lung pressures.
Who’s Watching the Patient? Pierson, IN: Tobin, Principles and Practice of Critical Care Monitoring
Thank You Feel free to pop by the ICU anytime!
 Mode of ventilation
Mode of ventilation Positive end expiratory pressure
Positive end expiratory pressure Indication for mechanical ventilation
Indication for mechanical ventilation Dr paul healey
Dr paul healey Mechanical ventilation indications
Mechanical ventilation indications Mechanical ventilation learning package
Mechanical ventilation learning package Peep in ventilator
Peep in ventilator Pinsp ventilation definition
Pinsp ventilation definition Types of ventilation fire fighting
Types of ventilation fire fighting Ventilators 101
Ventilators 101 Transpulmonary pressure formula
Transpulmonary pressure formula Adult bible study guide
Adult bible study guide Actual mechanical advantage vs ideal mechanical advantage
Actual mechanical advantage vs ideal mechanical advantage Sources nso july frenchhowell neill technology...
Sources nso july frenchhowell neill technology... Leaf yeast experiment
Leaf yeast experiment Harris burdick oscar and alphonse
Harris burdick oscar and alphonse June 22 to july 22
June 22 to july 22 Poppies in july
Poppies in july 2001 july 15
2001 july 15 March april may june july
March april may june july Slidetodoc.com
Slidetodoc.com July 4 sermon
July 4 sermon May 1775
May 1775 July 1-4 1863
July 1-4 1863 July 26 1953
July 26 1953 July 12 1776
July 12 1776 Archie smith boy wonder picture
Archie smith boy wonder picture Gdje se rodio nikola tesla
Gdje se rodio nikola tesla 2003 july 17
2003 july 17 July 14 1789
July 14 1789 June too soon july stand by
June too soon july stand by Sylvia plath poppies in july
Sylvia plath poppies in july Tender definition
Tender definition July 16 1776
July 16 1776 The hot july sun beat relentlessly down
The hot july sun beat relentlessly down Monday 13th july
Monday 13th july Ctdssmap payment schedule july 2021
Ctdssmap payment schedule july 2021 July 30 2009 nasa
July 30 2009 nasa Malaga in july
Malaga in july July 2 1937 amelia earhart
July 2 1937 amelia earhart Miss cuba receives an invitation
Miss cuba receives an invitation Astronomy picture of the day 11 july 2001
Astronomy picture of the day 11 july 2001 Super saturday tribal bingo july 4
Super saturday tribal bingo july 4 Sergei korolev
Sergei korolev On july 18 2001 a train carrying hazardous chemicals
On july 18 2001 a train carrying hazardous chemicals How does nurse ratched manipulate the patients
How does nurse ratched manipulate the patients Moving and handling dementia patients
Moving and handling dementia patients Nursing management for ocd
Nursing management for ocd Life expectancy of sickle cell patients
Life expectancy of sickle cell patients Self rostering system
Self rostering system Rocking chair therapy for dementia patients
Rocking chair therapy for dementia patients Andreas leischker
Andreas leischker Prevention of vte in nonorthopedic surgical patients
Prevention of vte in nonorthopedic surgical patients Lippincott williams
Lippincott williams Chapter 58 care of patients with liver problems
Chapter 58 care of patients with liver problems Backboard strapping techniques
Backboard strapping techniques Patients rights charter
Patients rights charter Circumcised vs uncircumcised cartoon
Circumcised vs uncircumcised cartoon Nursing diagnosis for undescended testis
Nursing diagnosis for undescended testis Leader rounding
Leader rounding Studer rounding tool
Studer rounding tool Genupectoral position
Genupectoral position Tena cap
Tena cap Banshee psychiatrist
Banshee psychiatrist Correction factor insulin
Correction factor insulin Rapid extrication technique emt
Rapid extrication technique emt Management of patients with neurologic trauma
Management of patients with neurologic trauma Introduction of admission
Introduction of admission Patient safety goals
Patient safety goals Chapter 55 care of patients with stomach disorders
Chapter 55 care of patients with stomach disorders Cingulate herniation
Cingulate herniation Diet chart for icu patients
Diet chart for icu patients