Overview of Malaysian Patient Safety Goals Orientation Program


- Slides: 24
Overview of Malaysian Patient Safety Goals Orientation Program Duchess of Kent Hospital Dr Paul Chan Deputy Director HDOK Adv Dip (Med Sci), MBBS, MBA (Healthcare Management)
Introduction • The Malaysian Patient Safety Goals are designed : • To stimulate health care organizations in improving patient safety. • To outline important patient safety areas that need to be improved • To act as a “Performance Measurement” in areas that are critical to a safe health care system. • For Patient Safety Council to monitor and evaluate the status of patient safety in the country. TH August 2012 9 th 30 December 2013 2
Introduction • Philosophy of Patient Safety Goals • “Patient safety shall be given prime importance in health care and preventable adverse events should be avoided at all costs”. • Scope: • Applicable to all public and private health care facilities • Hospitals, medical clinics, dental clinics TH August 2012 9 th 30 December 2013 3
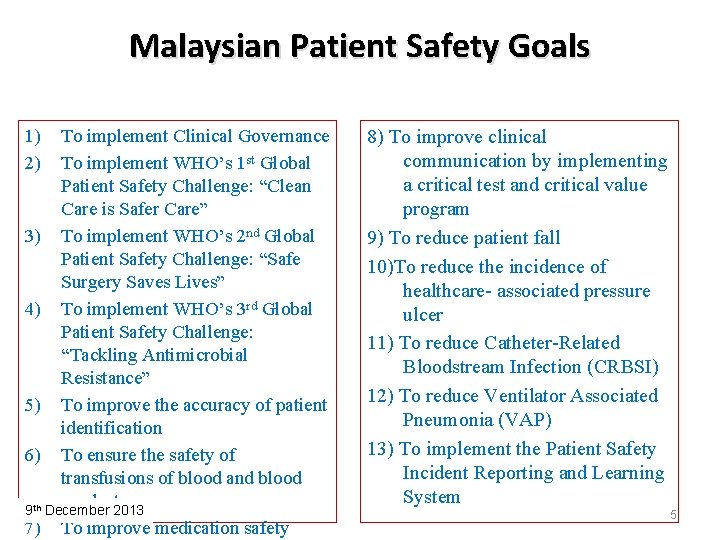
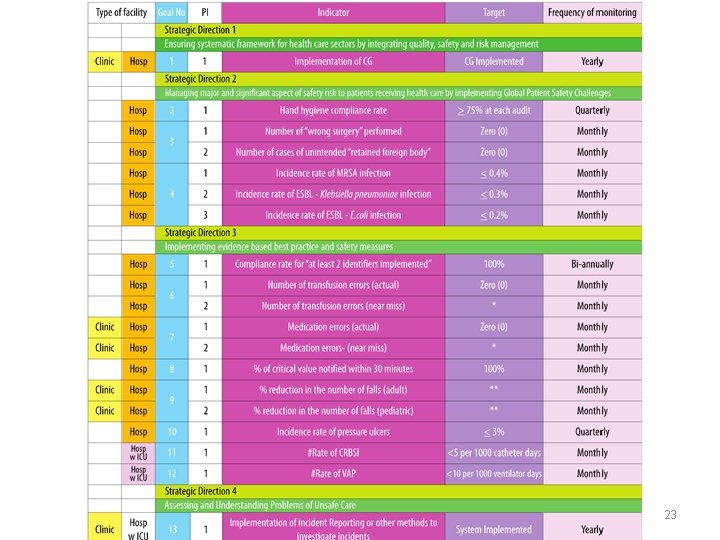
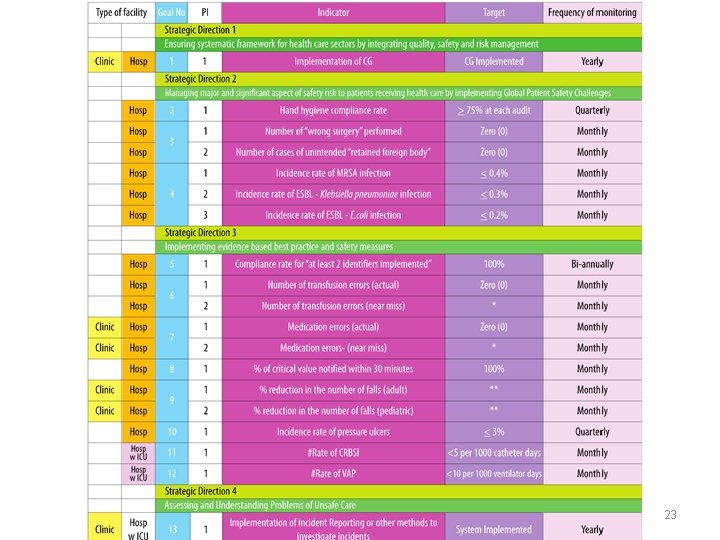
Derivation of Goals, Indicators & Targets �Goals originally based on WHO Patient Safety Program Areas and JCI Patient Safety Goals �PIs and targets are based on: � Philosophy of goals, current MOH standards, statistics on previous performance of Malaysian health care facilities and consensus decision of Patient Safety Council Members, Officers from State Health Departments, Hospital Directors, Clinicians and discussion with Sir Liam Donaldson (Patient Safety Advisor to WHO Director General) �Initially there were 15 goals, 59 PIs which were reduced to 29 PIs after first meeting and further reduced to: � 13 goals and 19 PIs – for hospitals � 4 goals and 6 PIs – for clinics TH August 2012 9 th 30 December 2013
Malaysian Patient Safety Goals 1) 2) To implement Clinical Governance To implement WHO’s 1 st Global Patient Safety Challenge: “Clean Care is Safer Care” 3) To implement WHO’s 2 nd Global Patient Safety Challenge: “Safe Surgery Saves Lives” 4) To implement WHO’s 3 rd Global Patient Safety Challenge: “Tackling Antimicrobial Resistance” 5) To improve the accuracy of patient identification 6) To ensure the safety of transfusions of blood and blood products 9 th December 2013 7) To improve medication safety 8) To improve clinical communication by implementing a critical test and critical value program 9) To reduce patient fall 10)To reduce the incidence of healthcare- associated pressure ulcer 11) To reduce Catheter-Related Bloodstream Infection (CRBSI) 12) To reduce Ventilator Associated Pneumonia (VAP) 13) To implement the Patient Safety Incident Reporting and Learning System 5
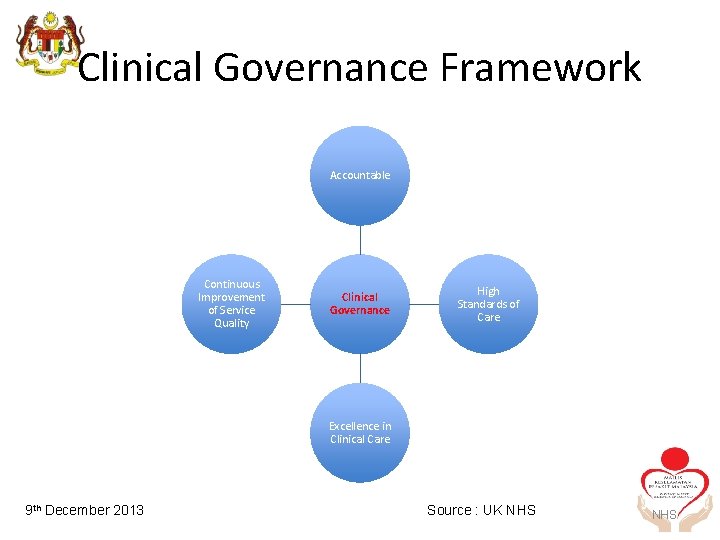
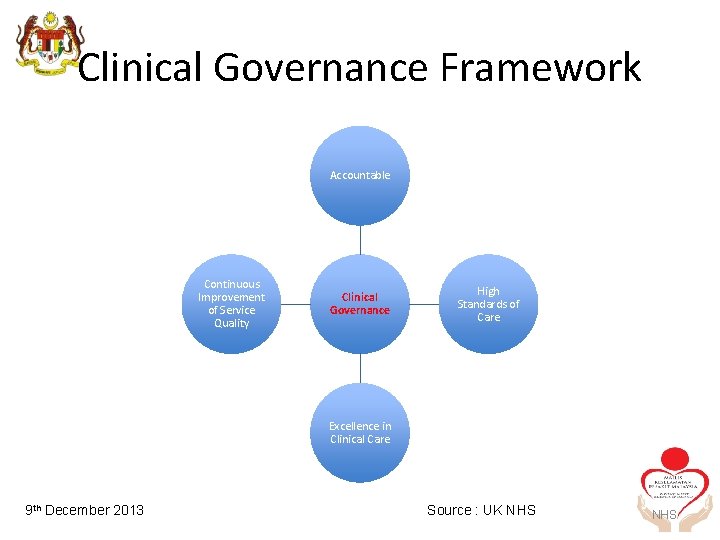
Clinical Governance Framework Accountable Continuous Improvement of Service Quality Clinical Governance High Standards of Care Excellence in Clinical Care TH August 2012 9 th 30 December 2013 Source : UK NHS
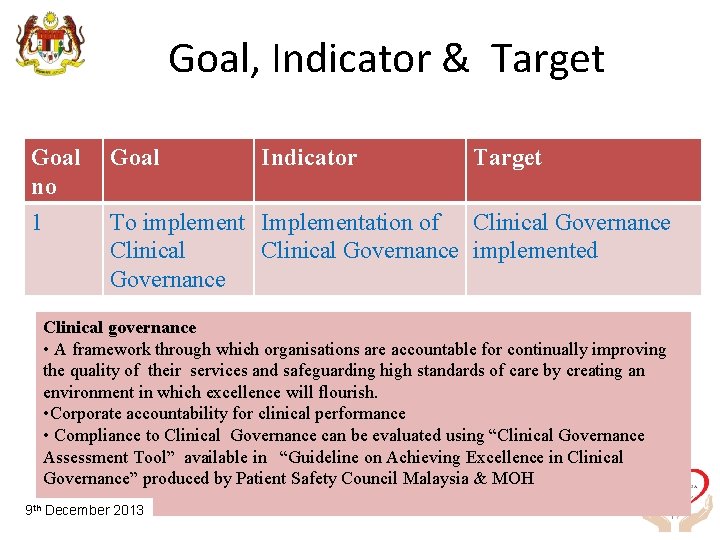
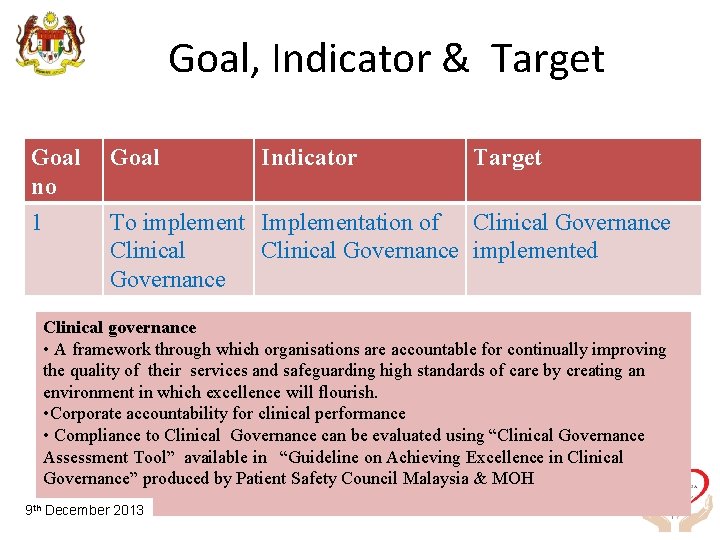
Goal, Indicator & Target Goal no Goal Indicator Target 1 To implement Implementation of Clinical Governance implemented Governance Clinical governance • A framework through which organisations are accountable for continually improving the quality of their services and safeguarding high standards of care by creating an environment in which excellence will flourish. • Corporate accountability for clinical performance • Compliance to Clinical Governance can be evaluated using “Clinical Governance Assessment Tool” available in “Guideline on Achieving Excellence in Clinical Governance” produced by Patient Safety Council Malaysia & MOH TH August 2012 9 th 30 December 2013 7
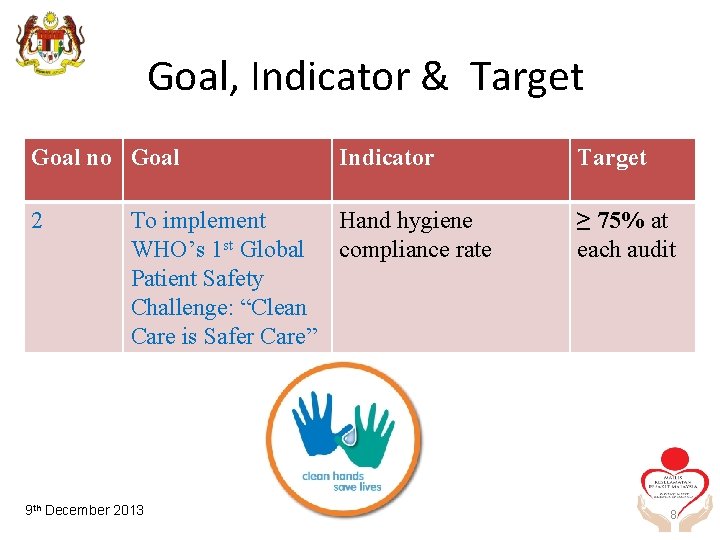
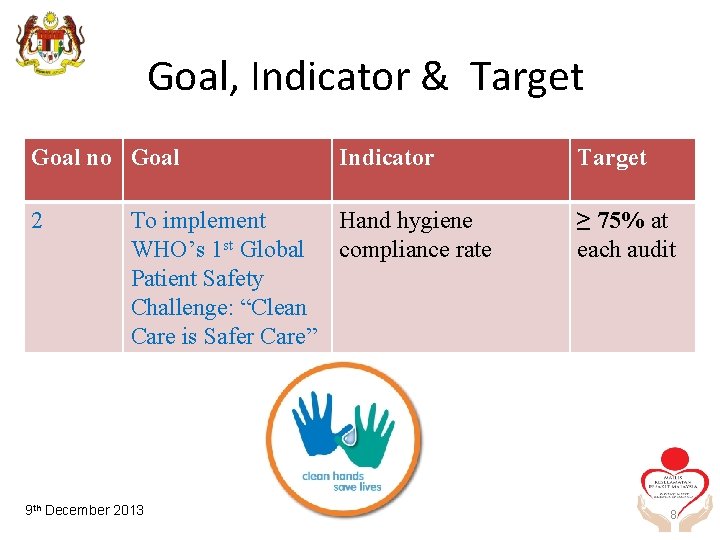
Goal, Indicator & Target Goal no Goal 2 Indicator To implement Hand hygiene WHO’s 1 st Global compliance rate Patient Safety Challenge: “Clean Care is Safer Care” TH August 2012 9 th 30 December 2013 Target ≥ 75% at each audit 8
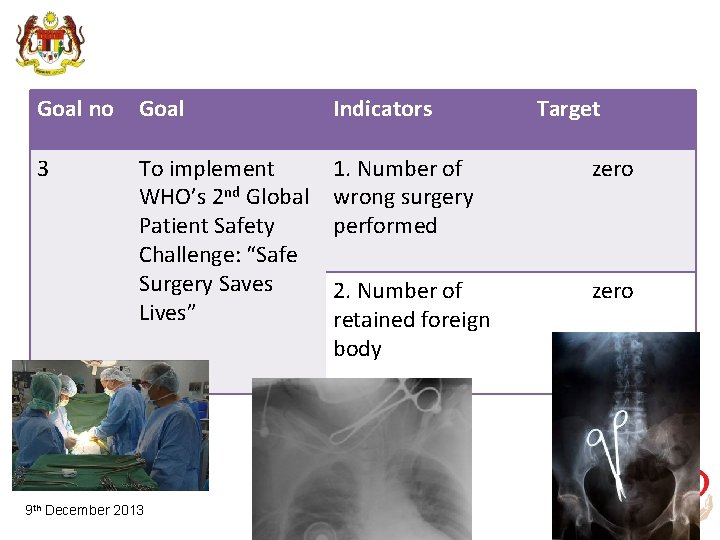
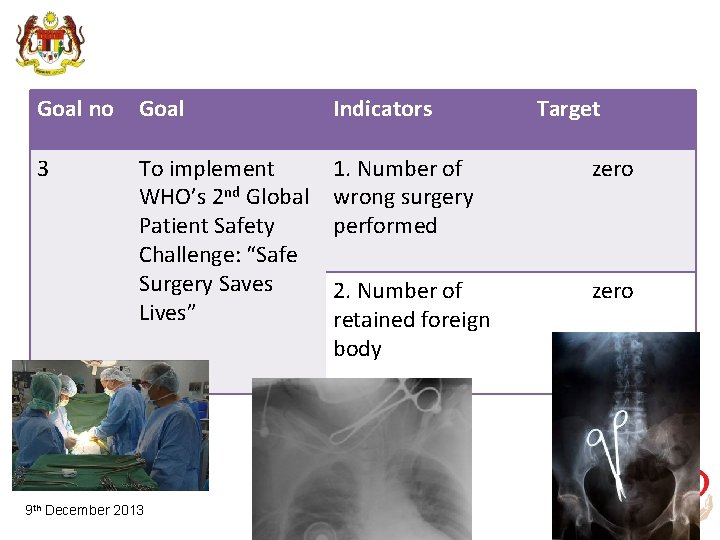
Goal no Goal Indicators 3 To implement WHO’s 2 nd Global Patient Safety Challenge: “Safe Surgery Saves Lives” 1. Number of wrong surgery performed zero 2. Number of retained foreign body zero TH August 2012 9 th 30 December 2013 Target 9
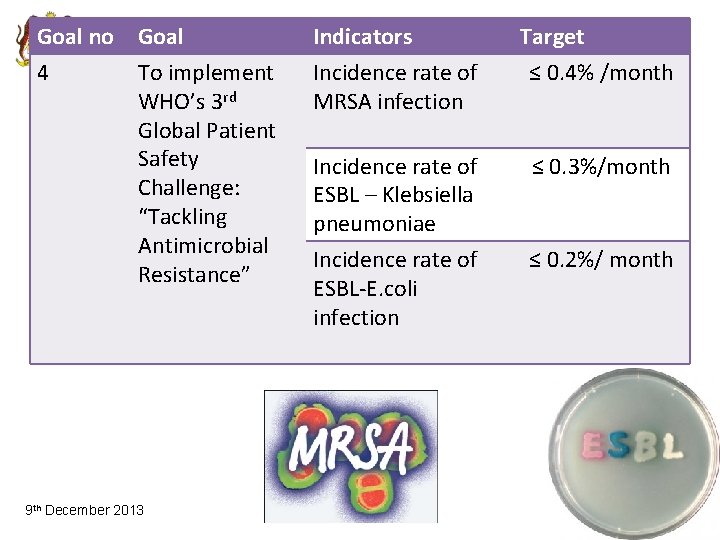
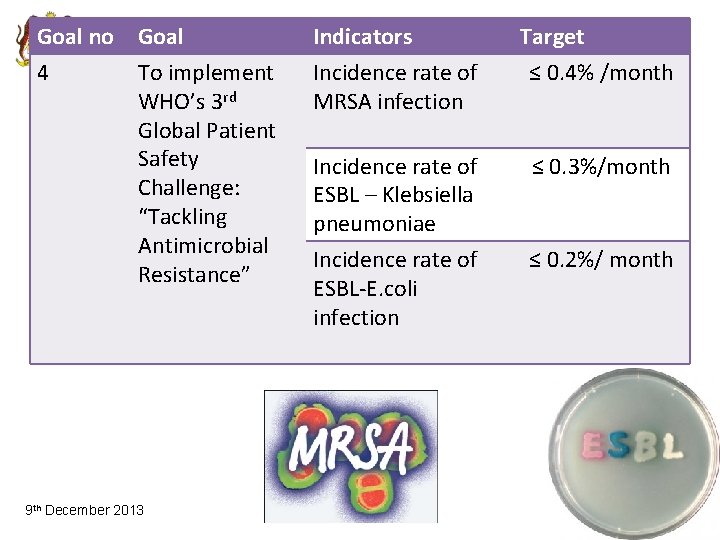
Goal no Goal 4 To implement WHO’s 3 rd Global Patient Safety Challenge: “Tackling Antimicrobial Resistance” TH August 2012 9 th 30 December 2013 Indicators Incidence rate of MRSA infection Target ≤ 0. 4% /month Incidence rate of ESBL – Klebsiella pneumoniae Incidence rate of ESBL-E. coli infection ≤ 0. 3%/month ≤ 0. 2%/ month 10

Goal no Goal Indicator 5 To improve the accuracy of patient identification Compliance rate of 100% at least 2 identifiers implemented TH August 2012 9 th 30 December 2013 Target 11
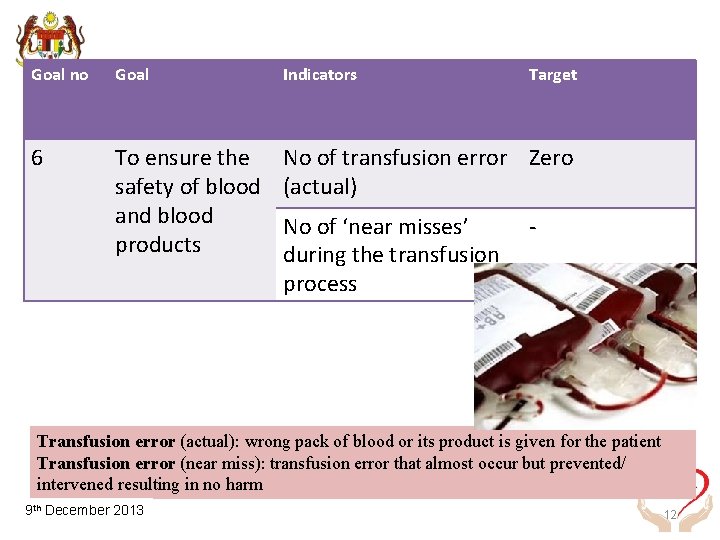
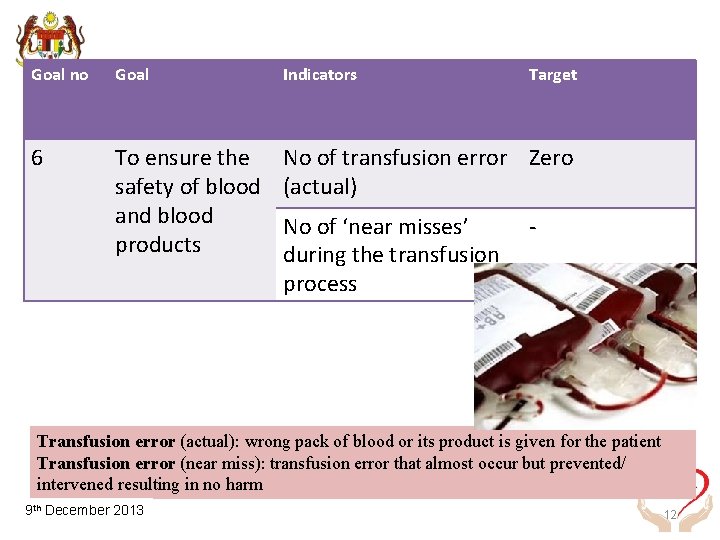
Goal no Goal Indicators 6 To ensure the safety of blood and blood products No of transfusion error Zero (actual) No of ‘near misses’ during the transfusion process Target - Transfusion error (actual): wrong pack of blood or its product is given for the patient Transfusion error (near miss): transfusion error that almost occur but prevented/ intervened resulting in no harm TH August 2012 9 th 30 December 2013 12

30 TH August 2012 13
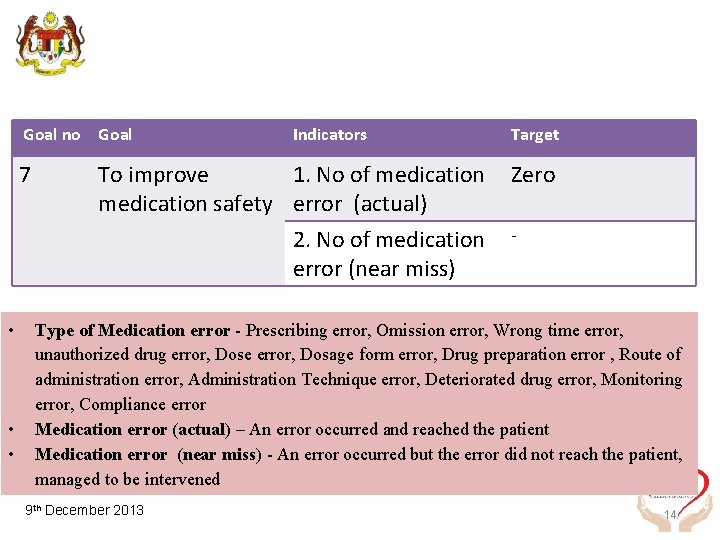
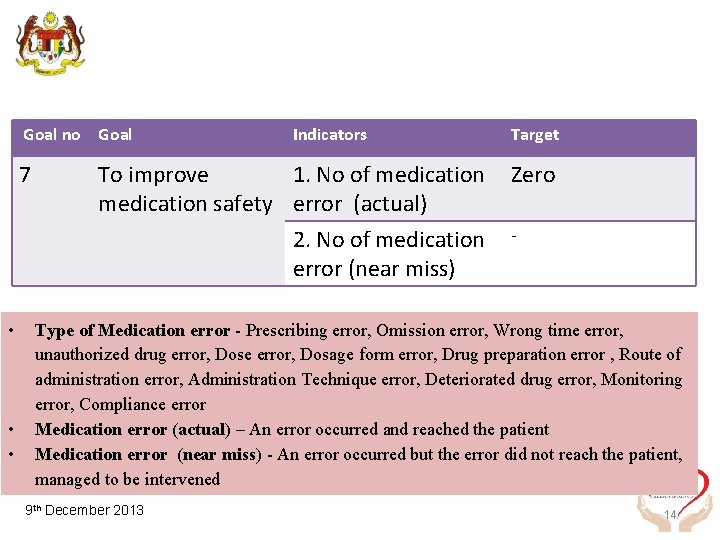
Goal no Goal 7 • • • Indicators To improve 1. No of medication safety error (actual) 2. No of medication error (near miss) Target Zero - Type of Medication error - Prescribing error, Omission error, Wrong time error, unauthorized drug error, Dose error, Dosage form error, Drug preparation error , Route of administration error, Administration Technique error, Deteriorated drug error, Monitoring error, Compliance error Medication error (actual) – An error occurred and reached the patient Medication error (near miss) - An error occurred but the error did not reach the patient, managed to be intervened TH August 2012 9 th 30 December 2013 14
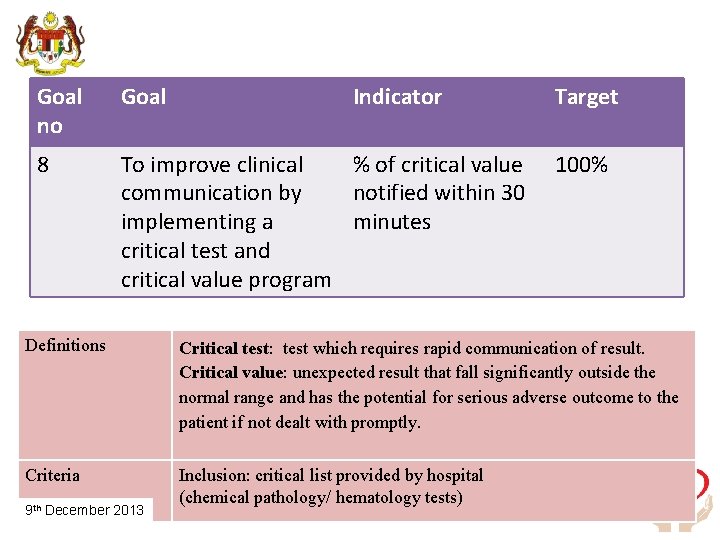
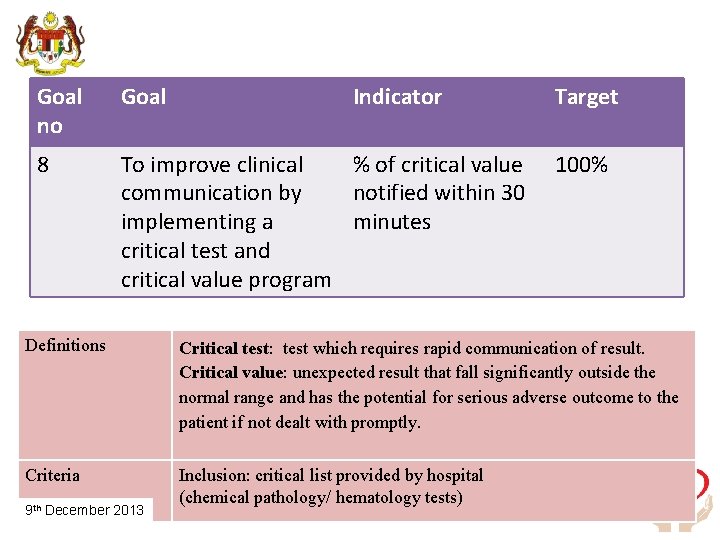
Goal no Goal Indicator 8 To improve clinical % of critical value communication by notified within 30 implementing a minutes critical test and critical value program Target 100% Definitions Critical test: test which requires rapid communication of result. Critical value: unexpected result that fall significantly outside the normal range and has the potential for serious adverse outcome to the patient if not dealt with promptly. Criteria Inclusion: critical list provided by hospital (chemical pathology/ hematology tests) TH August 2012 9 th 30 December 2013 15
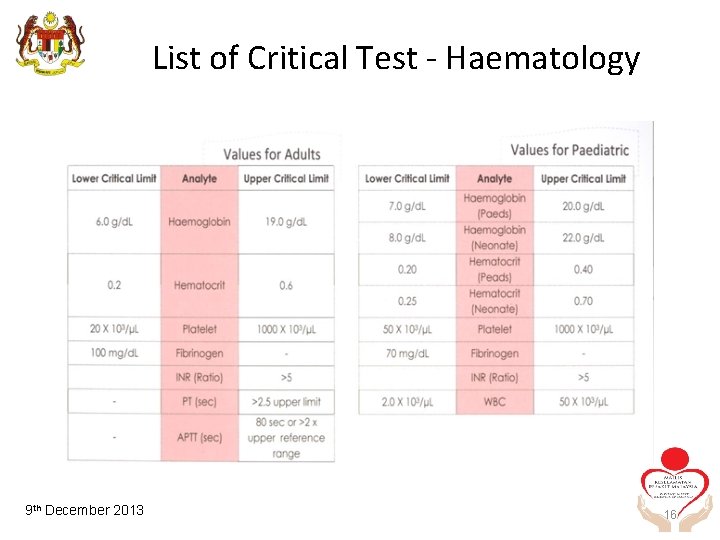
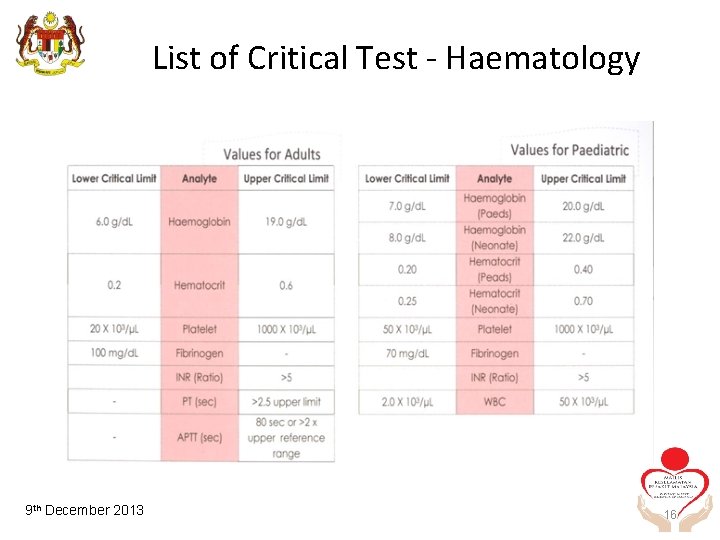
List of Critical Test - Haematology TH August 2012 9 th 30 December 2013 16
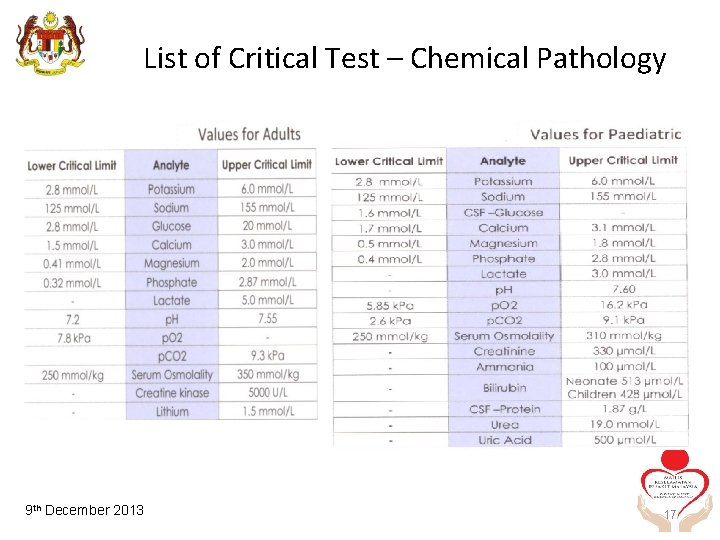
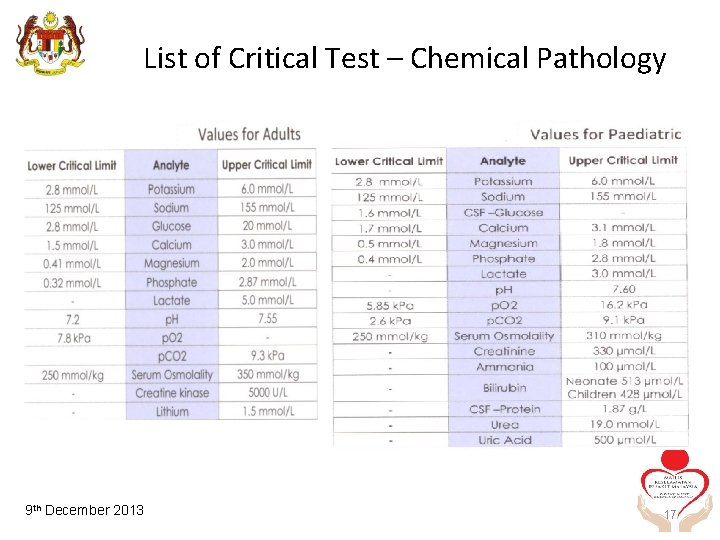
List of Critical Test – Chemical Pathology TH August 2012 9 th 30 December 2013 17
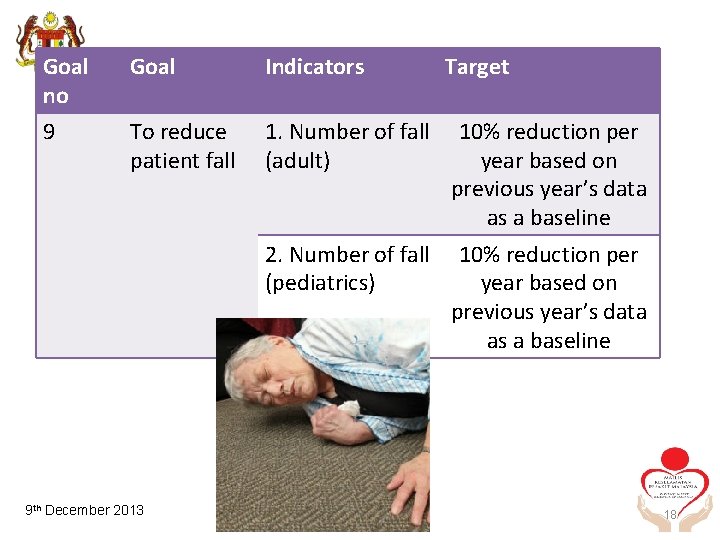
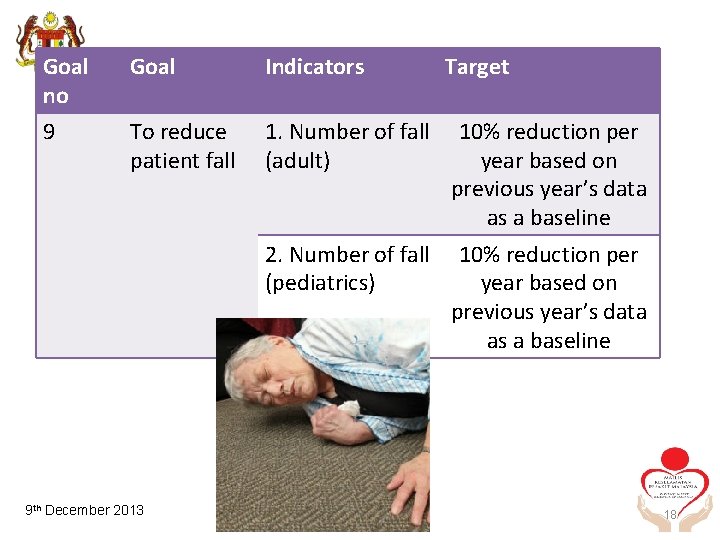
Goal no 9 Goal Indicators Target To reduce patient fall 1. Number of fall (adult) 10% reduction per year based on previous year’s data as a baseline 2. Number of fall (pediatrics) 10% reduction per year based on previous year’s data as a baseline TH August 2012 9 th 30 December 2013 18
Goal no Goal 10 Indicator To reduce the Incidence rate incidence of of pressure healthcareulcer associated pressure ulcer TH August 2012 9 th 30 December 2013 Target ≤ 3% 19
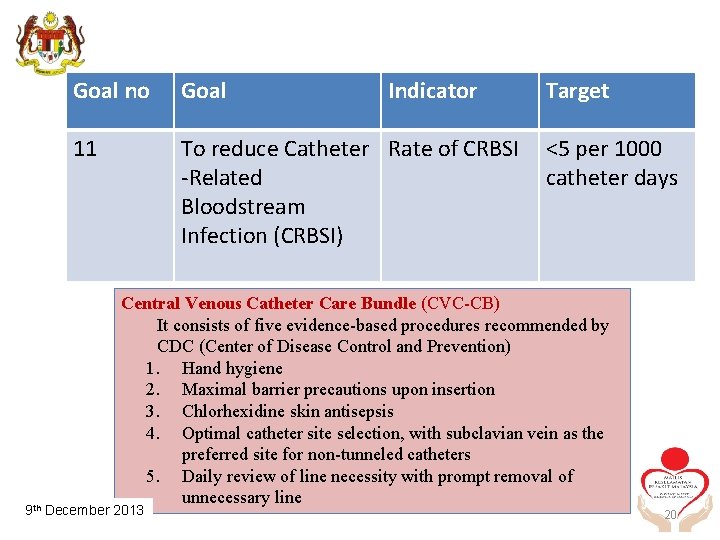
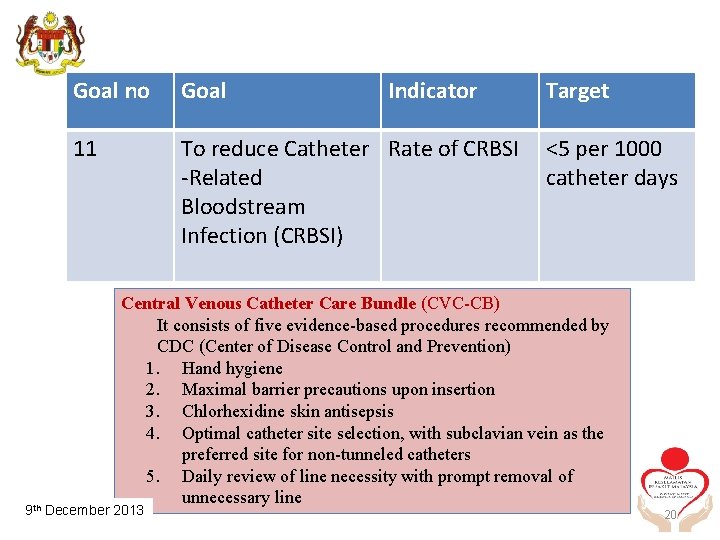
Goal no Goal Indicator 11 To reduce Catheter Rate of CRBSI -Related Bloodstream Infection (CRBSI) Target <5 per 1000 catheter days Central Venous Catheter Care Bundle (CVC-CB) It consists of five evidence-based procedures recommended by CDC (Center of Disease Control and Prevention) 1. Hand hygiene 2. Maximal barrier precautions upon insertion 3. Chlorhexidine skin antisepsis 4. Optimal catheter site selection, with subclavian vein as the preferred site for non-tunneled catheters 5. Daily review of line necessity with prompt removal of unnecessary line TH August 2012 9 th 30 December 2013 20
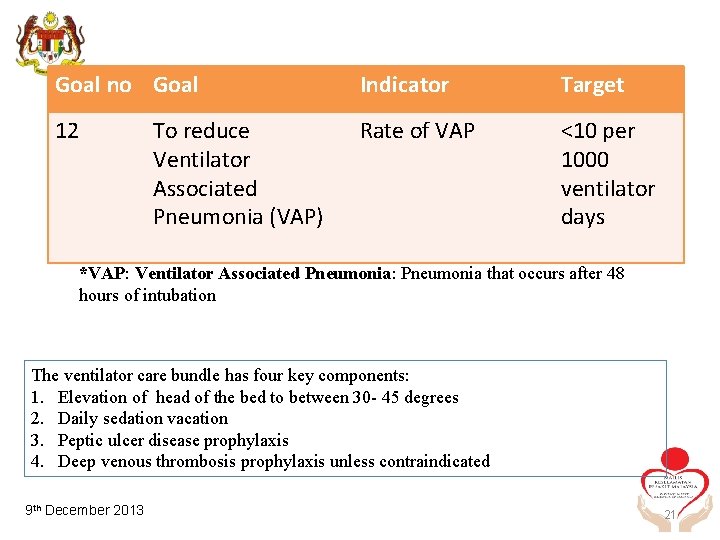
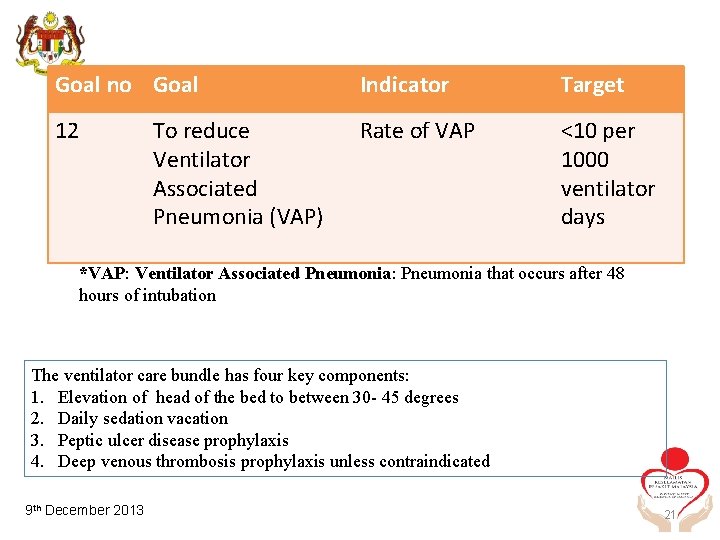
Goal no Goal Indicator Target 12 Rate of VAP <10 per 1000 ventilator days To reduce Ventilator Associated Pneumonia (VAP) *VAP: Ventilator Associated Pneumonia: Pneumonia that occurs after 48 hours of intubation The ventilator care bundle has four key components: 1. Elevation of head of the bed to between 30 - 45 degrees 2. Daily sedation vacation 3. Peptic ulcer disease prophylaxis 4. Deep venous thrombosis prophylaxis unless contraindicated TH August 2012 9 th 30 December 2013 21
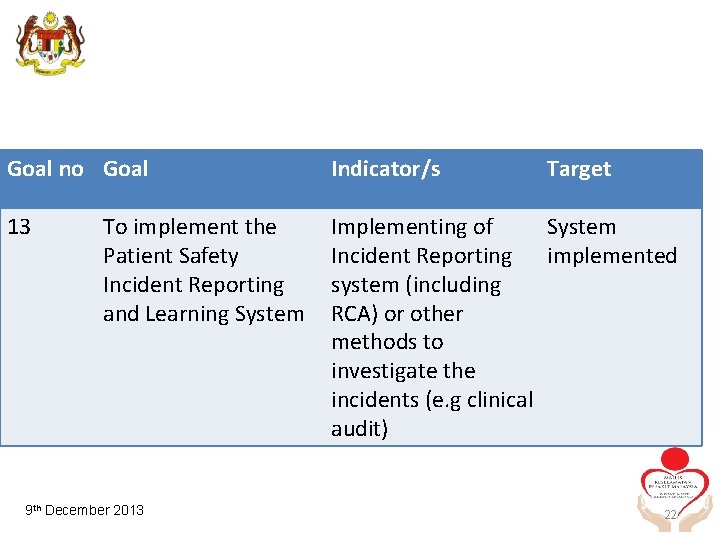
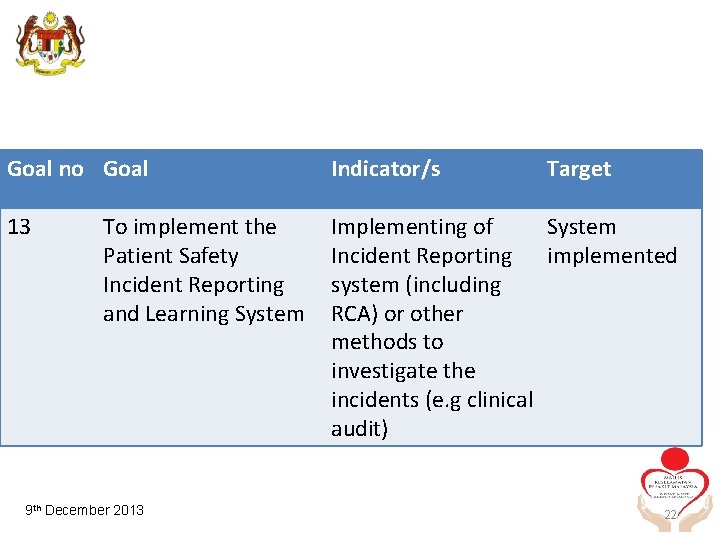
Goal no Goal Indicator/s 13 Implementing of System Incident Reporting implemented system (including RCA) or other methods to investigate the incidents (e. g clinical audit) To implement the Patient Safety Incident Reporting and Learning System TH August 2012 9 th 30 December 2013 Target 22
drpaul. chk@moh. gov. my 23
SUMMARY • Malaysian Patient Safety Goals is ready for implementation nation wide this year June 2013 • Need to know what to do to ensure patients safety • Prevent litigation 24