Nutrition in Acute Stroke Andreas H Leischker M








- Slides: 56
Nutrition in Acute Stroke Andreas H. Leischker, M. D. , M. A. Head Working Group „Neurology“, German Society for Nutritional Medicine Working Group „Nutrition in Stroke“, ESPEN

Nutrition in Acute Stroke: How it started
Baseline No national and no international Guidelines on nutrition in acute stroke
Ten years ago… First meeting of a interdisciplinary working group „ Nutrition in patients with acute stroke“ August 2005 Frankfurt/Germany
Working Group Members • Rainer Wirth (Geriatrician, DGEM and DGG) • E. W. Busch (Neurologist, DGN) • Beate Schlegel ( Nutritionist, DGEM) • Kristian Hahn ( Geriatrician, DGG) • Jens Kondrup ( Nutritionist , ESPEN) • Andreas Leischker (Geriatrician, DGEM and DGG) andreas. leischker@alexianer. de
German Guideline- Societyes German Society for Geriatrics (DGG) German sociréty for Neurology(DGN) German Society for Nutritional medicine (DGEM)
Two years later. . First Milestone „DGEM-Guideline Nutrition of patients with acute stroke“ • Review by the Medical Societyes DGEM, DGN und DGG • Aktuell. Ernähr Med 2007; 32: 332 -348 andreas. leischker@alexianer. de
3 years later…. . Expiry date of guideline is exhausting. andreas. leischker@alexianer. de
DGEM Guideline Clinical Nutrition „Neurology“ • Stroke • Parkinsons Disease • Huntingtons Disease • Multiple Sclerosis andreas. leischker@alexianer. de
“Guideline Clinical Nutrition in patients with stroke” Wirth R, Smoliner C, Jäger M, Warnecke T, Leischker AH, Dziewas R and the DGEM Steering Committee, Experimental & Translational Stroke Medicine 2013, 5: 14 http: //www. etsmjournal. com/content/5/1/14 andreas. leischker@alexianer. de
Oral Nutritional Supplements (ONS)
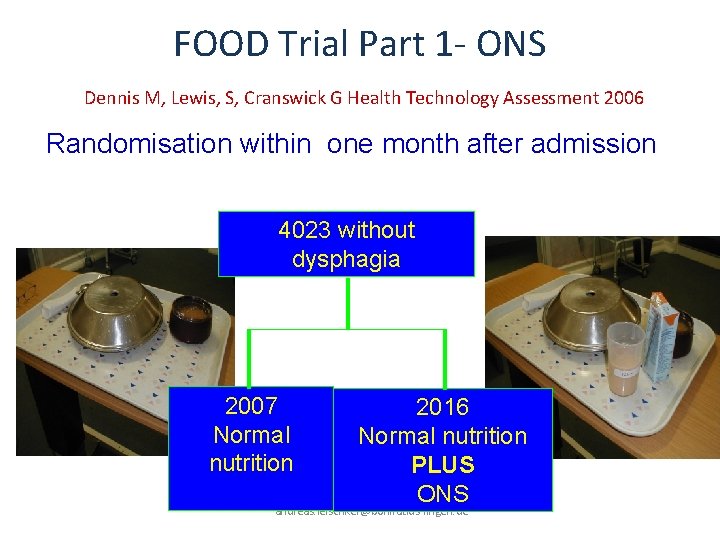
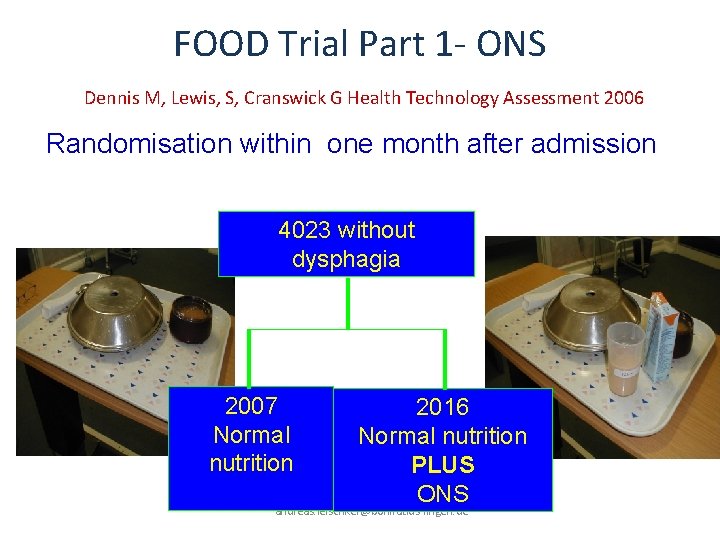
FOOD Trial Part 1 - ONS Dennis M, Lewis, S, Cranswick G Health Technology Assessment 2006 Randomisation within one month after admission 4023 without dysphagia 2007 Normal nutrition 2016 Normal nutrition PLUS ONS andreas. leischker@bonifatius-lingen. de
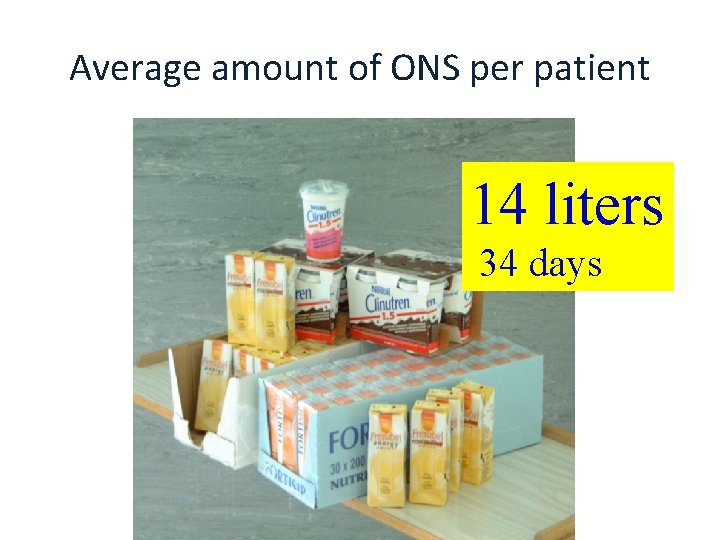
Average amount of ONS per patient 14 liters 34 days andreas. leischker@bonifatius-lingen. de
FOOD Trial Part 1 Dennis M, Lewis, S, Cranswick G: Health Technology Assessment 2006 27, 9 % of patients did not tolerate ONS
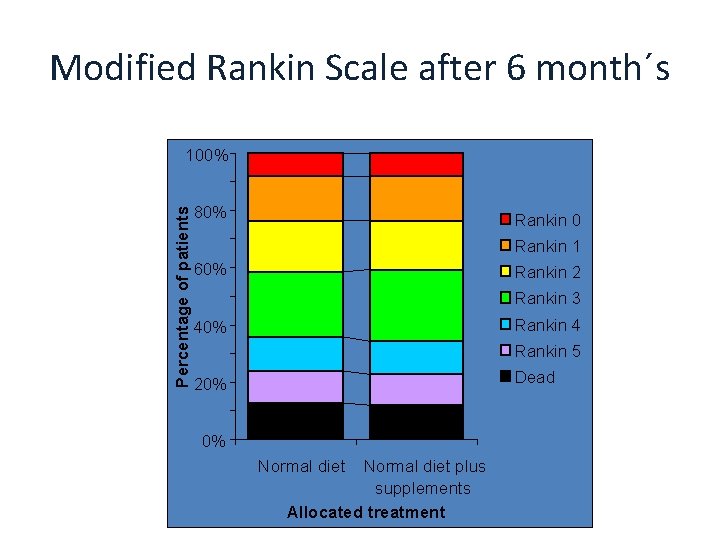
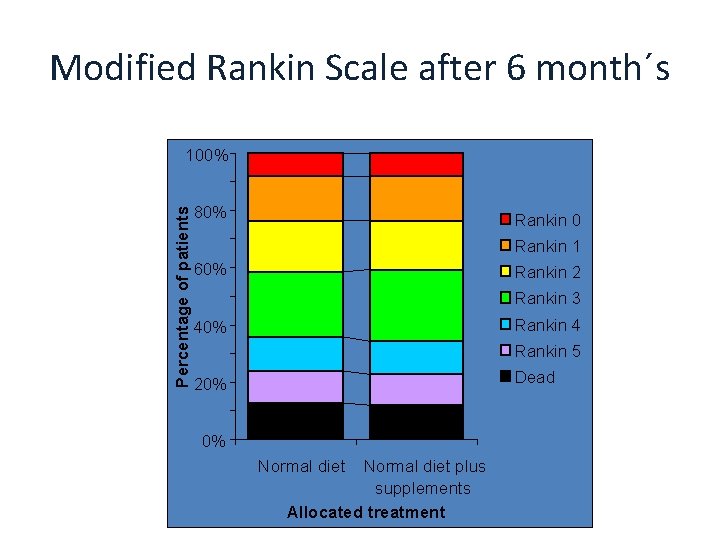
Modified Rankin Scale after 6 month´s Percentage of patients 100% 80% Rankin 0 Rankin 1 60% Rankin 2 Rankin 3 Rankin 4 40% Rankin 5 Dead 20% 0% Normal diet plus supplements Allocated treatment andreas. leischker@bonifatius-lingen. de
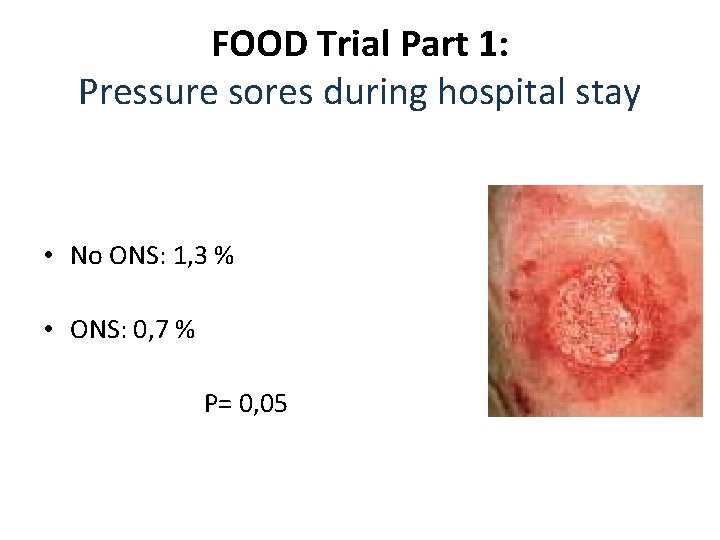
FOOD Trial Part 1: Pressure sores during hospital stay • No ONS: 1, 3 % • ONS: 0, 7 % P= 0, 05
Recommendation ONS is not recommended in general
Who should recieve ONS Patients with • malnutrition • risk for malnutrition • Risk for pressure sores AWMF Leitlinie Ernährung des Schlaganfallpatienten 2007
Enteral Nutrition: When?
„Patients with prolonged dysphagia anticipated to last for more than 7 days should receive tube feeding (within 72 hours) (C)
Dysphagia Screening • Water Swallowing Test ( WST) • Multiple Consistency Test( Gugging Swallowing Screen, GUSS) • Swallowing Provocation Test andreas. leischker@alexianer. de
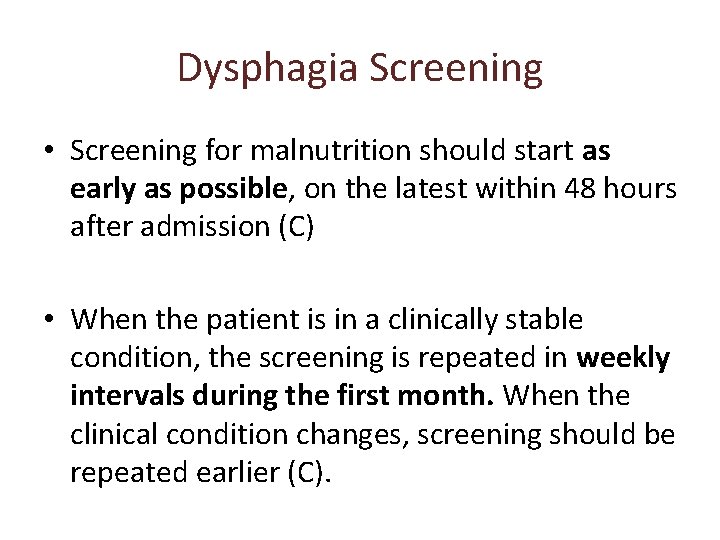
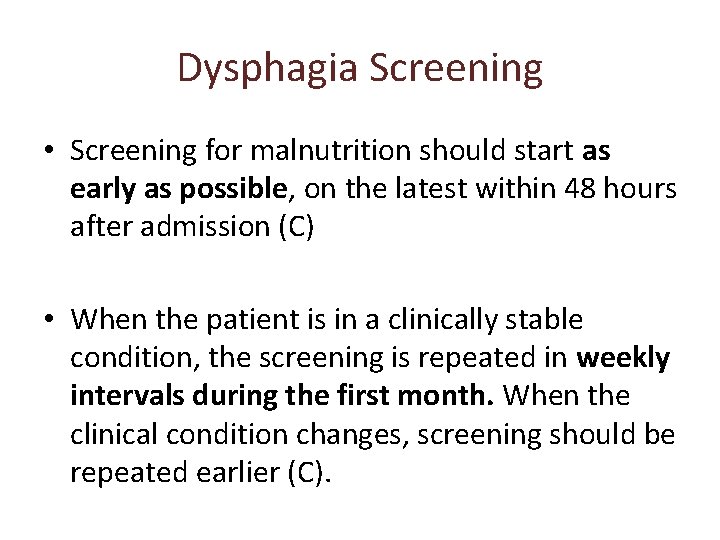
Dysphagia Screening • Screening for malnutrition should start as early as possible, on the latest within 48 hours after admission (C) • When the patient is in a clinically stable condition, the screening is repeated in weekly intervals during the first month. When the clinical condition changes, screening should be repeated earlier (C).
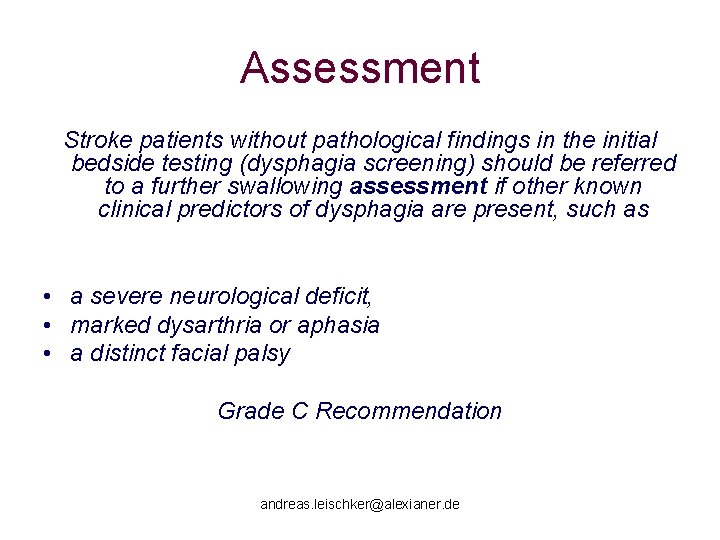
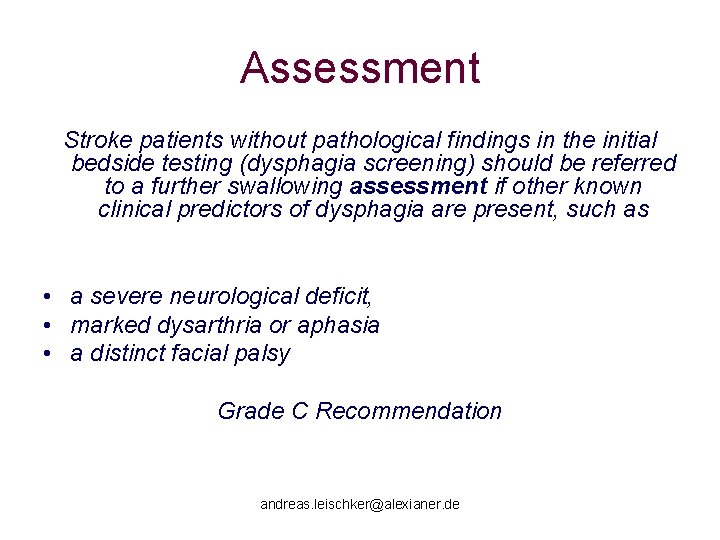
Assessment Stroke patients without pathological findings in the initial bedside testing (dysphagia screening) should be referred to a further swallowing assessment if other known clinical predictors of dysphagia are present, such as • a severe neurological deficit, • marked dysarthria or aphasia • a distinct facial palsy Grade C Recommendation andreas. leischker@alexianer. de
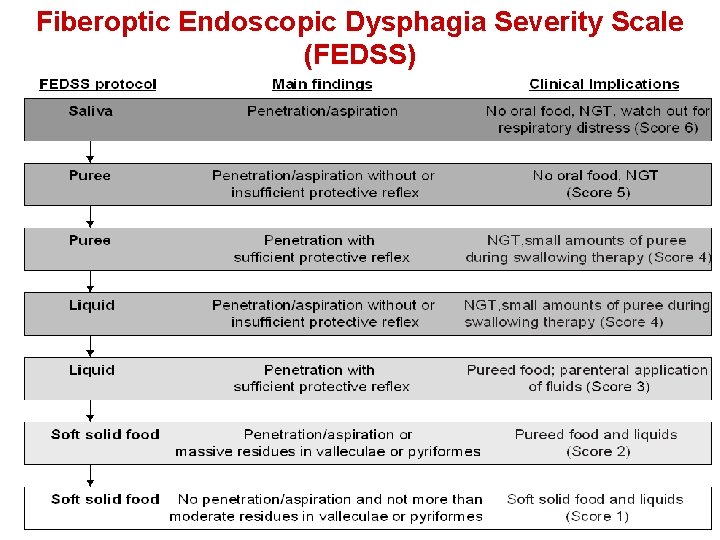
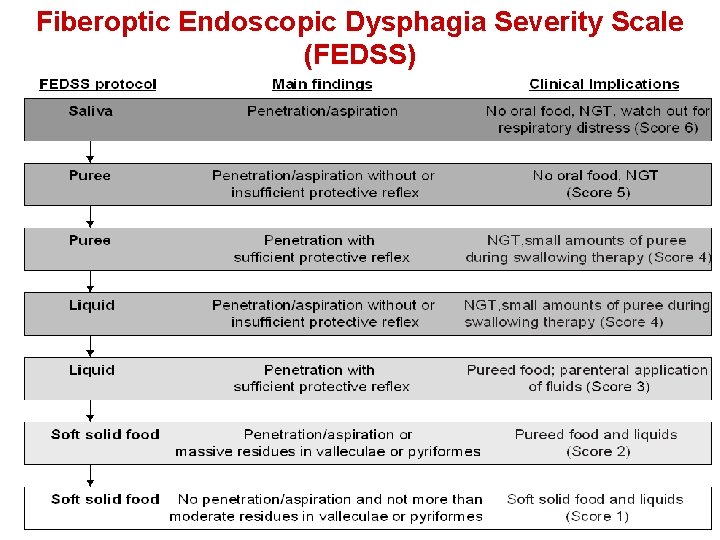
Fiberoptic Endoscopic Dysphagia Severity Scale (FEDSS) 25 andreas. leischker@alexianer. de andreas. leischker@alexianer-krefeld. de
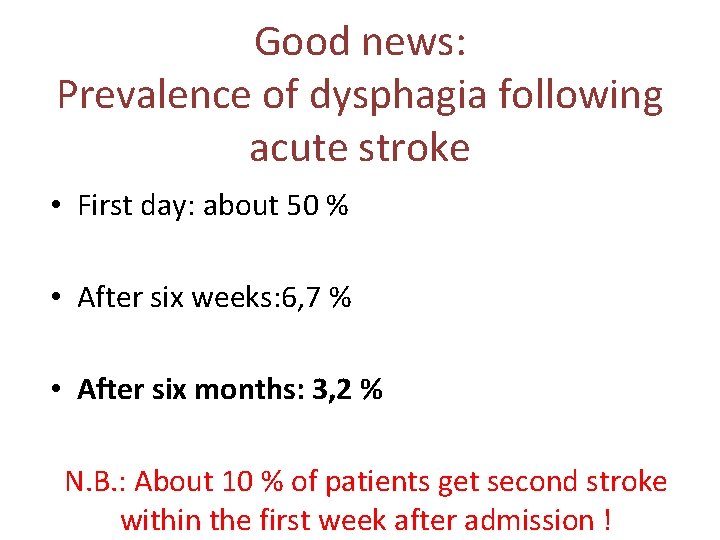
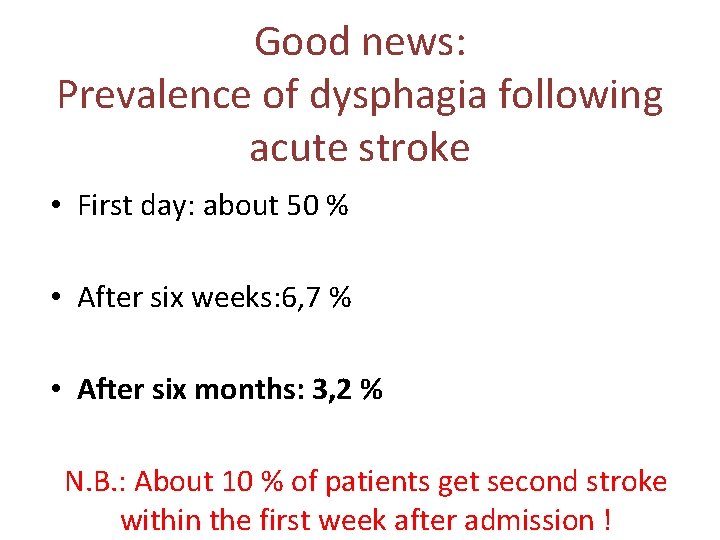
Good news: Prevalence of dysphagia following acute stroke • First day: about 50 % • After six weeks: 6, 7 % • After six months: 3, 2 % N. B. : About 10 % of patients get second stroke within the first week after admission !
Dysphagia follow up after discharge At least once per month during the first 6 months
Nasogastric or PEG ? andreas. leischker@alexianer. de
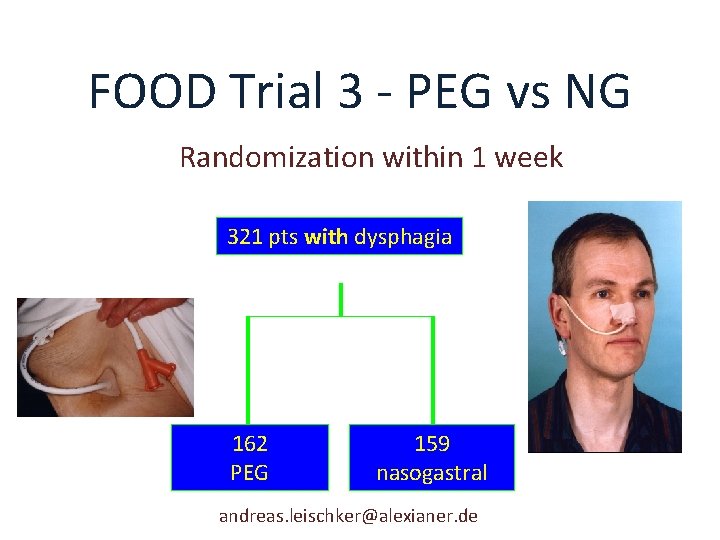
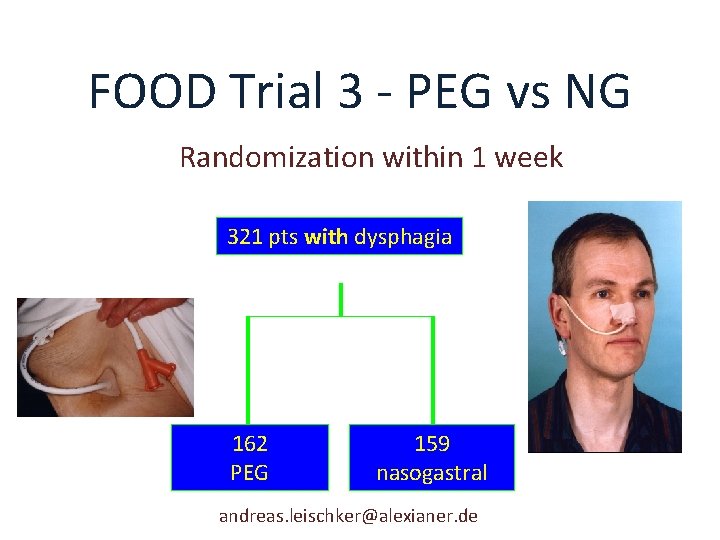
FOOD Trial 3 - PEG vs NG Randomization within 1 week 321 pts with dysphagia 162 PEG 159 nasogastral andreas. leischker@alexianer. de
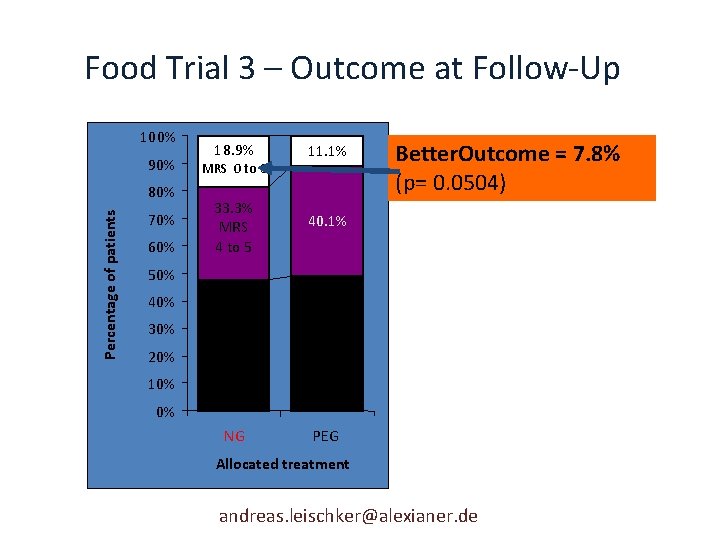
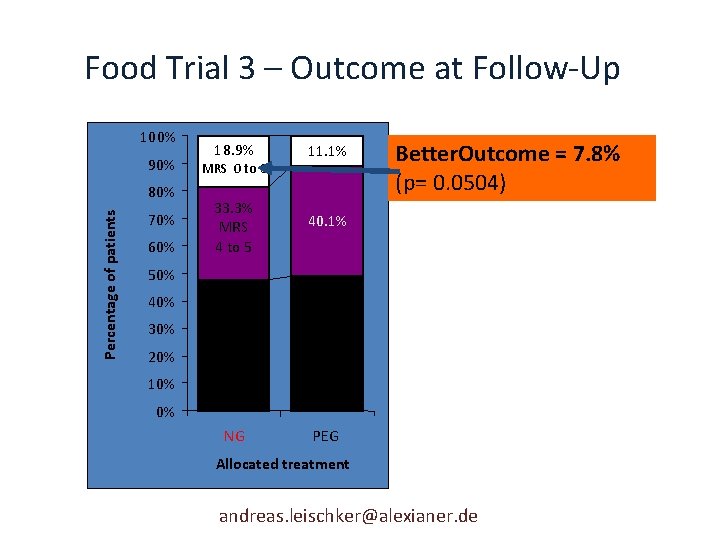
Food Trial 3 – Outcome at Follow-Up 100% 90% Percentage of patients 80% 70% 60% 18. 9% 11. 1% 33. 3% MRS 4 to 5 40. 1% 47. 8% Dead 48. 8% NG PEG MRS 0 to 3 Better. Outcome = 7. 8% (p= 0. 0504) 50% 40% 30% 20% 10% 0% Allocated treatment andreas. leischker@alexianer. de
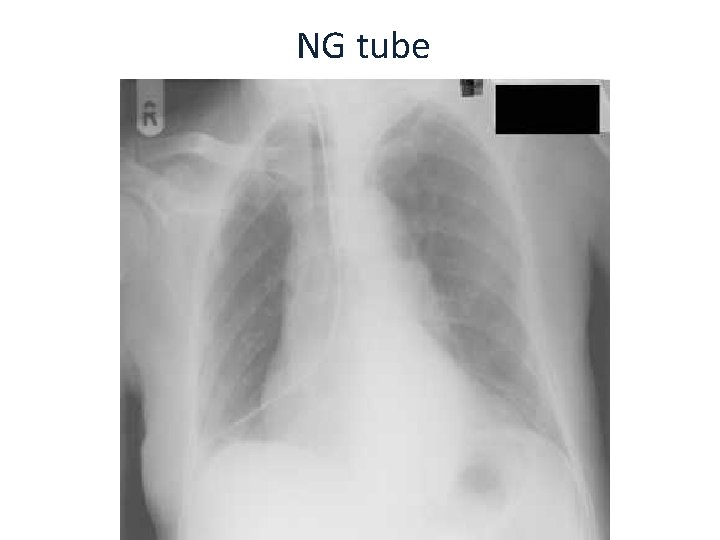
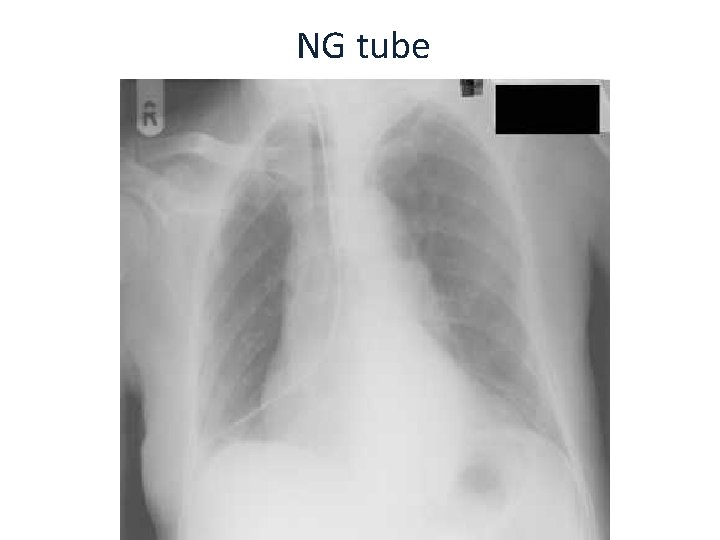
NG tube andreas. leischker@bonifatius-lingen. de
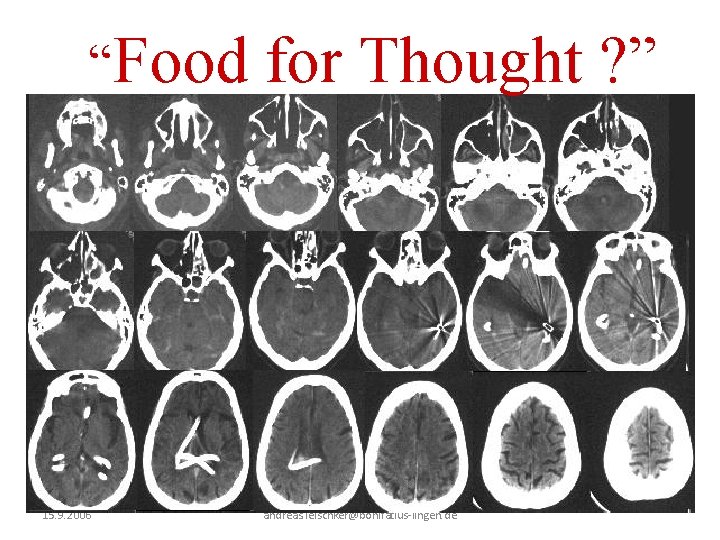
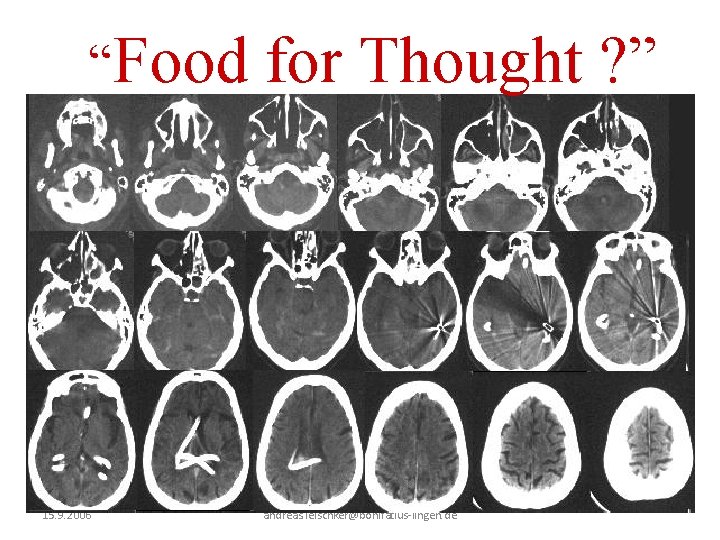
“Food 15. 9. 2006 for Thought ? ” andreas. leischker@bonifatius-lingen. de

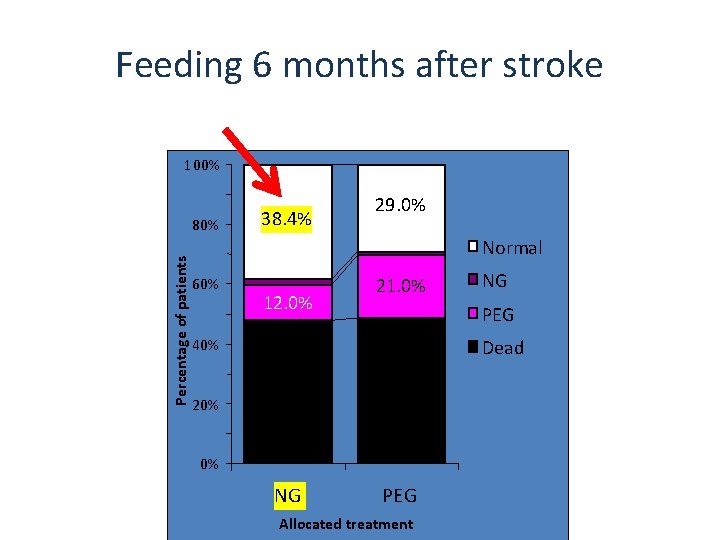
How are patients fed 6 months later ? andreas. leischker @maria-hilf. de
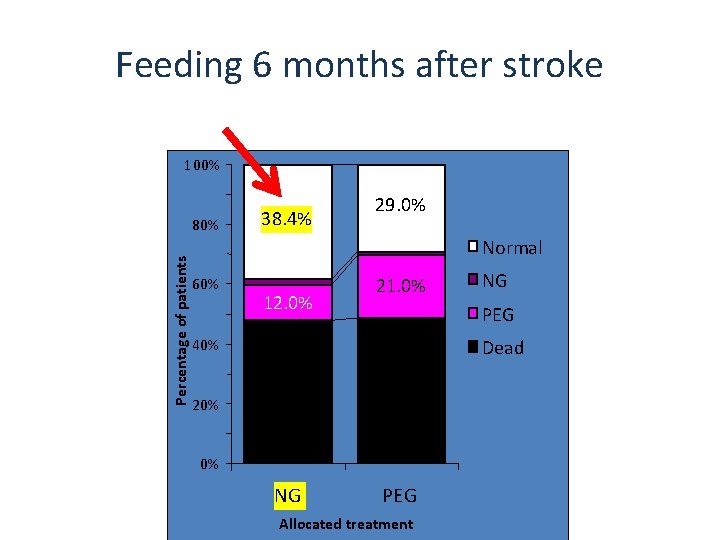
Feeding 6 months after stroke 100% Percentage of patients 80% 38. 4% 29. 0% Normal 60% 12. 0% 21. 0% PEG 40% 20% NG Dead 47. 8% 48. 8% 0% NG PEG andreas. leischker@bonifatius-lingen. de Allocated treatment
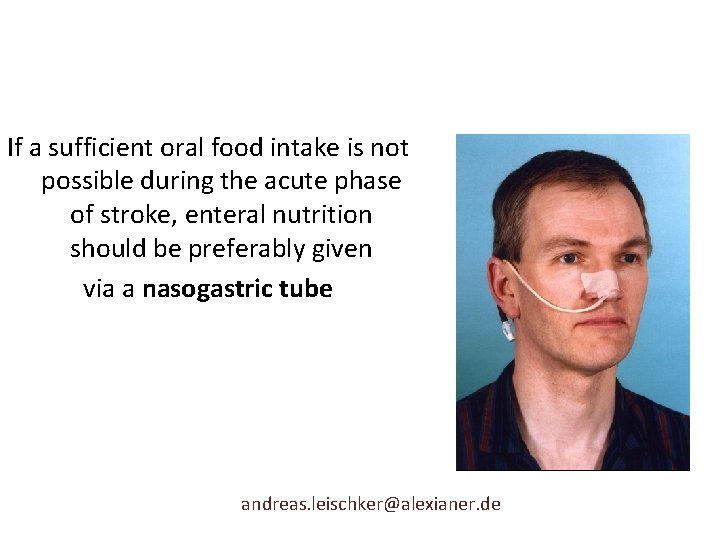
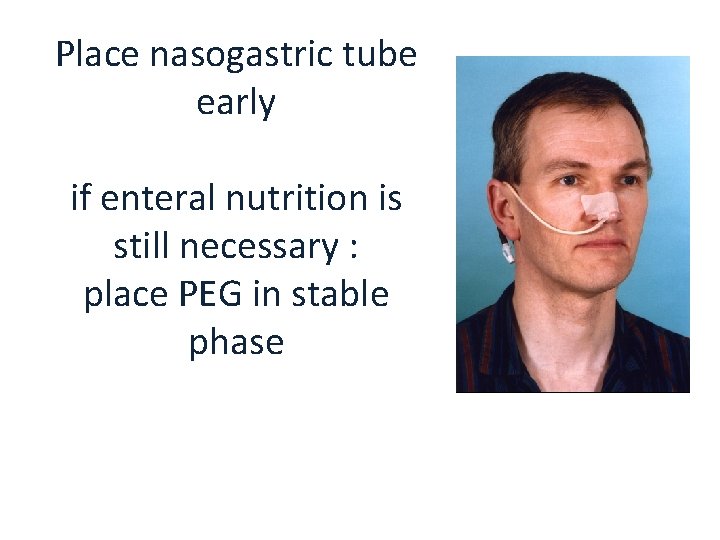
If a sufficient oral food intake is not possible during the acute phase of stroke, enteral nutrition should be preferably given via a nasogastric tube andreas. leischker@alexianer. de
“Tube feeding does not interfere with swallow training. Therefore, dysphagia therapy shall start as early as possible also in tube fed patients” Grade A andreas. leischker@alexianer. de
If enteral feeding is likely for a longer period of time (> 28 days), a PEG should be chosen and placed in a stable clinical phase (after 14 – 28 days) (A). AWMF Leitlinie Enterale Ernährung des Schlaganfallpatienten 2007 andreas. leischker@maria-hilf. de
Who should get a PEG earlyer? Mechanically ventilated stroke patients should receive a PEG at an early stage (B)
What to do if patients put out the NG tube andreas. leischker@bonifatius-lingen. de

15. 9. 2006 andreas. leischker@bonifatius-lingen. de
15. 9. 2006 andreas. leischker@bonifatius-lingen. de
If a nasogastric tube is rejected, not tolerated or repeatedly removed by the patient and if artificial nutrition will probably be necessary for more than 14 days, early feeding via PEG should be started (C). AWMF Leitlinie Enterale Ernährung des Schlaganfallpatienten 2007
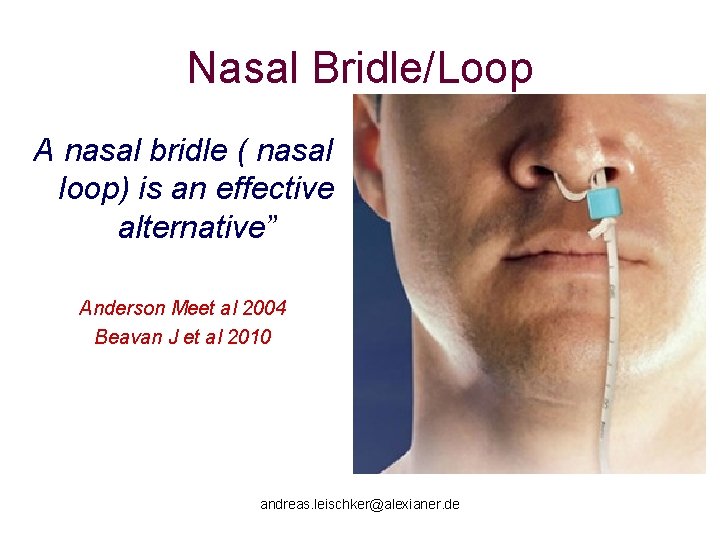
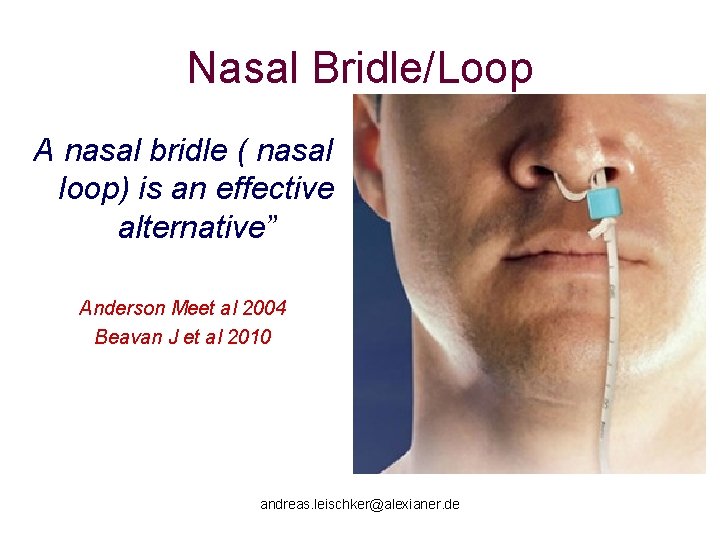
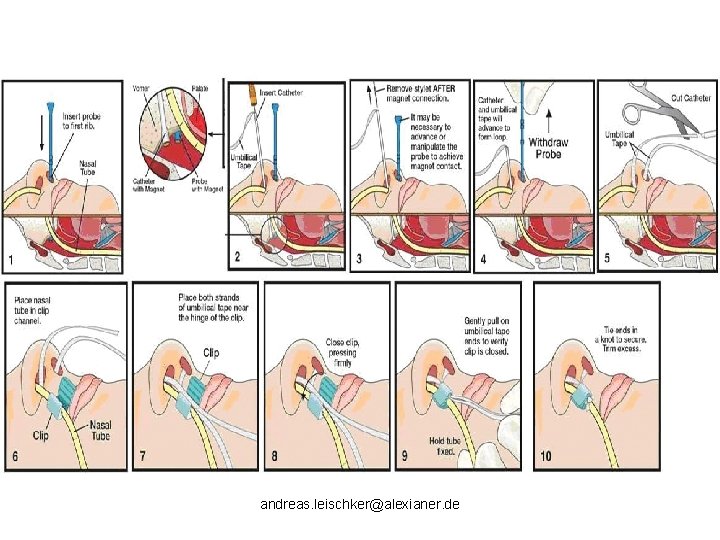
Nasal Bridle/Loop A nasal bridle ( nasal loop) is an effective alternative” Anderson Meet al 2004 Beavan J et al 2010 andreas. leischker@alexianer. de
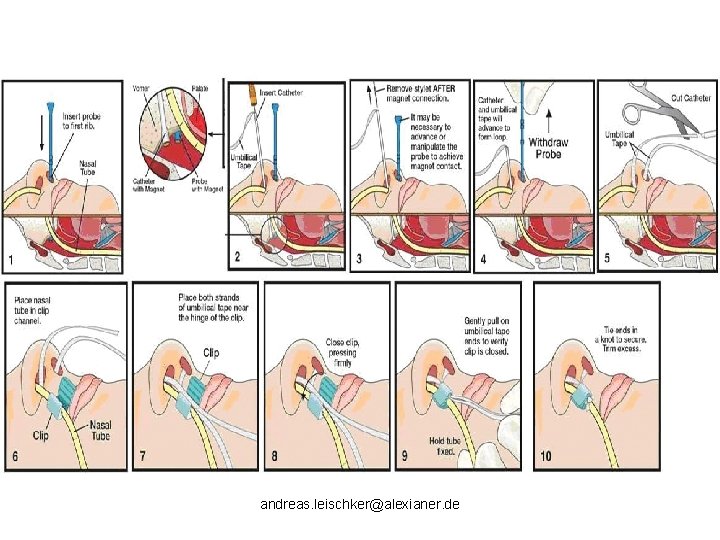
andreas. leischker@alexianer. de
With or without pump?
In stroke patients tube feed should preferably be applied with a feeding pump (C). AWMF Leitlinie Enterale Ernährung des Schlaganfallpatienten 2007
Outlook European Society for Parenteral and Enteral Nutrition ( ESPEN) European Guideline on nutrition in stroke „in progress“…

Stroke Prevention : News
The Coffee Paradox in Stroke • > 3 cups per day linked with fewer strokes (OR 0. 44, 95% CI 0. 22 -0. 87, P < 0. 02) in healthy subjects • “Heavier daily coffee consumption is associated with decreased stroke prevalence, despite smoking tendency in heavy coffee drinkers” Liebeskind DS, Sanossian N, Fu KA, Wang HJ, Arab L. The coffee paradox instroke: Increased consumption linked with fewer strokes. Nutr Neurosci. 2015 Jun 22. [Epub ahead of print]
Tea is o. k. , too “…Awaiting the results from further long-term RCTs and prospective studies, moderate consumption of filtered coffee, tea, and dark chocolate seems prudent” Larsson SC. Coffee, tea, and cocoa and risk of stroke. Review. Stroke 2014

Take Home Messages

ONS Only for patients with risk for malnutrition or risk for pressure sores
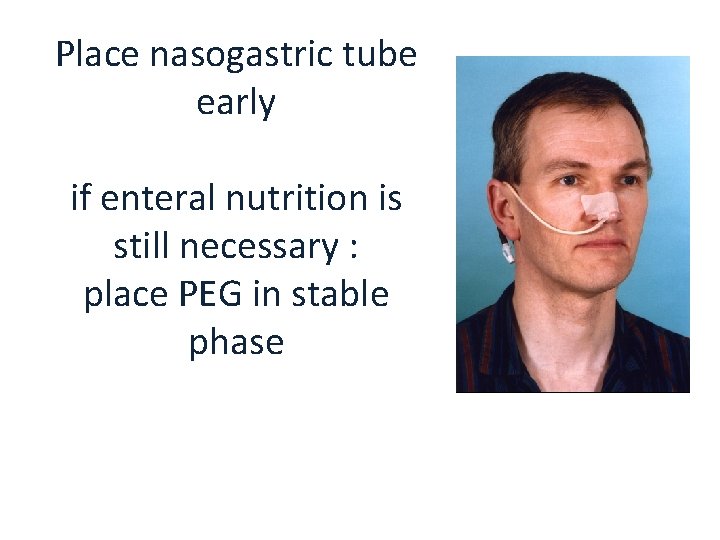
Place nasogastric tube early if enteral nutrition is still necessary : place PEG in stable phase

Repeat Dysphagia Assessment regulary for at least 6 monthsincluding time after discharge

Take coffee breaks for prevention!
 Guideline clinical nutrition in patients with stroke
Guideline clinical nutrition in patients with stroke Anterior stroke vs posterior stroke
Anterior stroke vs posterior stroke Acute ischemic stroke algorithm
Acute ischemic stroke algorithm Acute stroke ready certification
Acute stroke ready certification Medical nutrition therapy for stroke
Medical nutrition therapy for stroke Posterior cerebral artery stroke
Posterior cerebral artery stroke When does stroke volume increase
When does stroke volume increase Factors affecting cardiac output
Factors affecting cardiac output Stroke volume variation
Stroke volume variation Asuhan keperawatan eklamsia
Asuhan keperawatan eklamsia Stroke comeback center
Stroke comeback center Cincinnati stroke scale
Cincinnati stroke scale Stroke star competencies
Stroke star competencies Who stroke definition
Who stroke definition Siriraj score
Siriraj score Co = hr x sv
Co = hr x sv Tnfp
Tnfp Stroke and turn clinic
Stroke and turn clinic Nursing interventions for homonymous hemianopsia
Nursing interventions for homonymous hemianopsia Stroke
Stroke Ejection fraction vs stroke volume
Ejection fraction vs stroke volume Diagnosis topis stroke hemoragik
Diagnosis topis stroke hemoragik Stroke coordinator boot camp
Stroke coordinator boot camp Methods for isolation of pure culture
Methods for isolation of pure culture Siriraj score
Siriraj score Stroke volume ejection fraction
Stroke volume ejection fraction Lams stroke scale
Lams stroke scale Vilopositioner stroke
Vilopositioner stroke Systoms of a stroke
Systoms of a stroke Cincinnati stroke scale
Cincinnati stroke scale Pathogenesis of stroke ppt
Pathogenesis of stroke ppt Cingulate herniation
Cingulate herniation Stroke fast assessment
Stroke fast assessment Key stroke logger
Key stroke logger Key katcher
Key katcher Man behind aggressive voice
Man behind aggressive voice Preload stroke volume
Preload stroke volume Factors affecting stroke volume
Factors affecting stroke volume Uvulan
Uvulan Zoya minasyan
Zoya minasyan Stroke coordinator boot camp
Stroke coordinator boot camp Striatum részei
Striatum részei Stroke volume ejection fraction
Stroke volume ejection fraction Stroke action plan
Stroke action plan Central versus peripheral vertigo
Central versus peripheral vertigo Brake stroke indicators
Brake stroke indicators Stroke volume is calculated by
Stroke volume is calculated by Vector vs raster data
Vector vs raster data Kelly kasteel
Kelly kasteel 岁 stroke order
岁 stroke order Code fast stroke
Code fast stroke Stroke precautions nursing
Stroke precautions nursing Blood thinners names
Blood thinners names Answer of this question
Answer of this question Neurodevelopmental treatment for stroke
Neurodevelopmental treatment for stroke Brush strokes
Brush strokes Heart disease and stroke are the world's biggest killers
Heart disease and stroke are the world's biggest killers