Emergency Management of Congestive Heart Failure in Small


- Slides: 43
Emergency Management of Congestive Heart Failure in Small Animal Practice **Name**, DVM, DACVIM-Cardiology **Date**
Outline • Cardiac Auscultation and History – Useful tools for distinguishing cardiac and respiratory disease • Radiographs • Pathophysiology of Heart Failure • Treatment of Heart Failure
Cardic Auscultation: Tips • • Take your time Adequately restrain Minimize panting, growling, purring Focus on heart sounds first, breath sounds second Develop a repeatable pattern Listen for 3 rd heart sounds (clicks, gallops) Consider the signalment of the patient – Common things happen commonly – Congenital vs. Acquired – Breed-specific defects
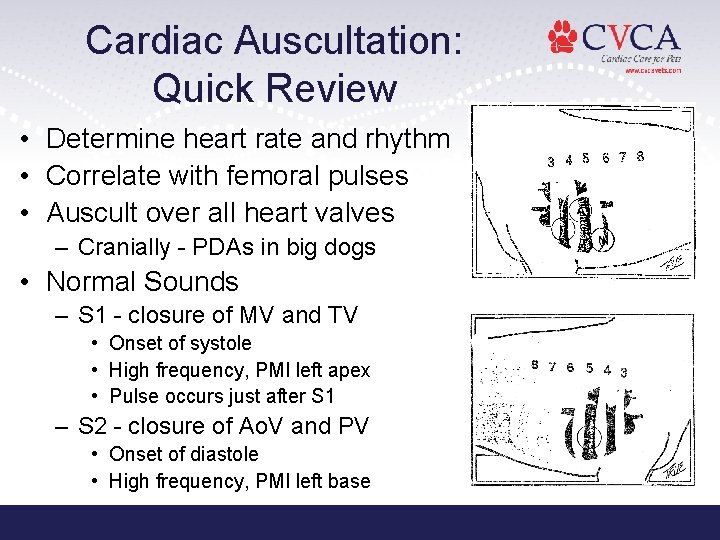
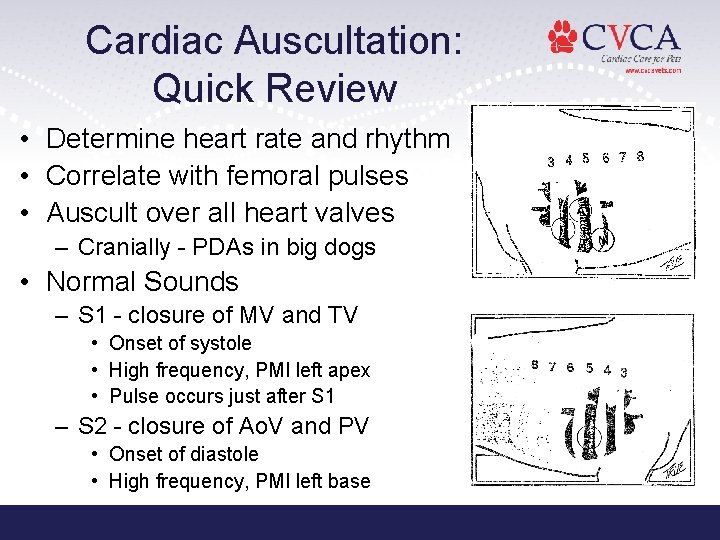
Cardiac Auscultation: Quick Review • Determine heart rate and rhythm • Correlate with femoral pulses • Auscult over all heart valves – Cranially - PDAs in big dogs • Normal Sounds – S 1 - closure of MV and TV • Onset of systole • High frequency, PMI left apex • Pulse occurs just after S 1 – S 2 - closure of Ao. V and PV • Onset of diastole • High frequency, PMI left base
Cardiac Auscultation: Quick Review • Transient Heart Sounds – Systolic Click • Dogs - usually associated with DMVD (prolapse of AMVL) • Cats - hyperdynamic function, systolic contact of LV walls – S 3 Gallop (ventricular gallop) • Low frequency • Represents ventricular stiffness (diastolic dysfunction - reduced compliance while filling) • Caused by sudden termination of expansion of LV walls during period of rapid ventricular filling • HCM, DCM, Severe DMVD – S 4 Gallop (atrial gallop) • Low frequency • Represents ventricular stiffness • Caused by atria trying to force blood into an already over-distended ventricle; atria forcing blood into stiff ventricle (atrial contraction - late ventricular diastole) • HCM • Can also hear S 4 with some 3 rd degree AVB
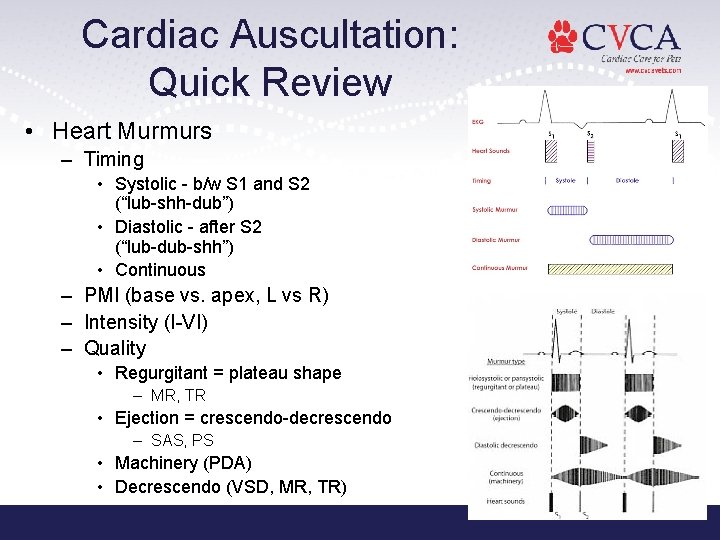
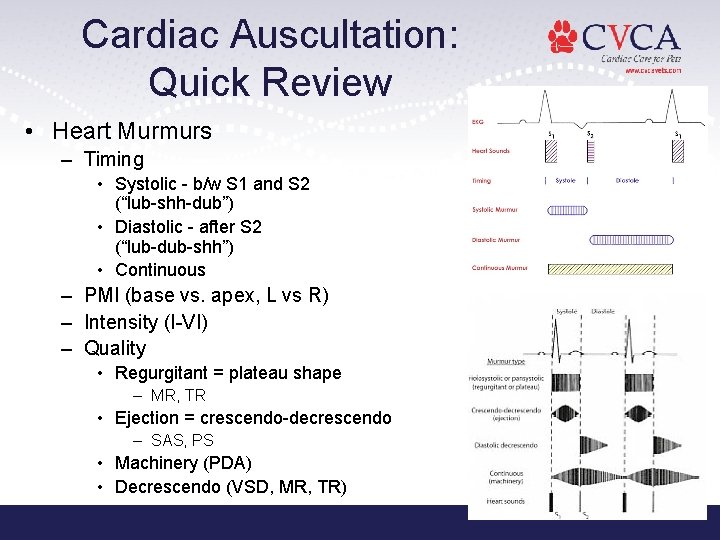
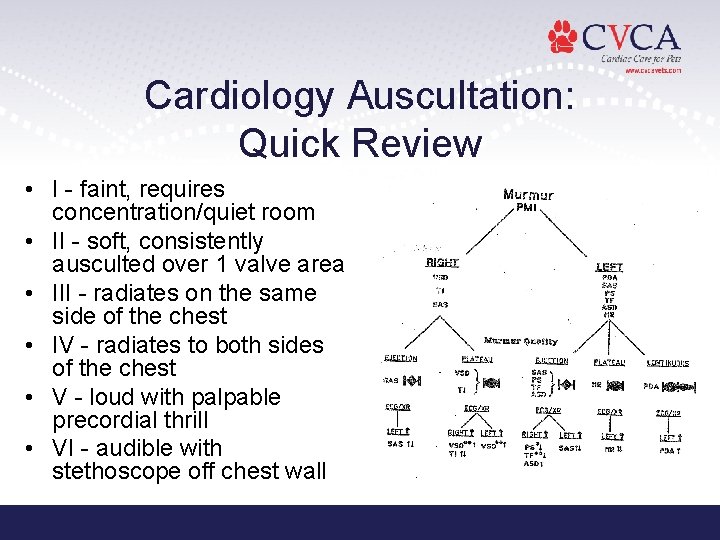
Cardiac Auscultation: Quick Review • Heart Murmurs – Timing • Systolic - b/w S 1 and S 2 (“lub-shh-dub”) • Diastolic - after S 2 (“lub-dub-shh”) • Continuous – PMI (base vs. apex, L vs R) – Intensity (I-VI) – Quality • Regurgitant = plateau shape – MR, TR • Ejection = crescendo-decrescendo – SAS, PS • Machinery (PDA) • Decrescendo (VSD, MR, TR)
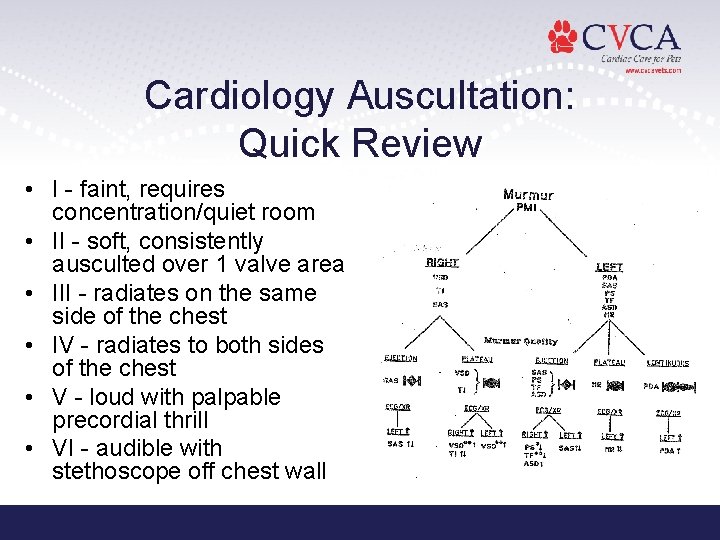
Cardiology Auscultation: Quick Review • I - faint, requires concentration/quiet room • II - soft, consistently ausculted over 1 valve area • III - radiates on the same side of the chest • IV - radiates to both sides of the chest • V - loud with palpable precordial thrill • VI - audible with stethoscope off chest wall
Cardiac Auscultation: Summary • Slow down and take your time • It matters - YOU are the gate keeper • Making the correct diagnosis makes a difference in outcome and survival • 30% of Boxers, 1 st sign to owner = SCD • Does the presence of crackles = CHF? • Document…Document – Vital signs and trends matter – Can you explain changes? • If present, when did arrhythmia start?
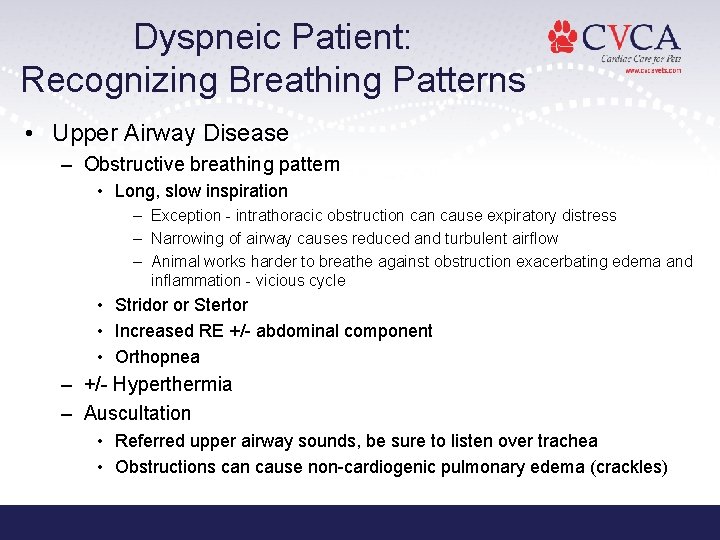
Dyspneic Patient: Recognizing Breathing Patterns • Upper Airway Disease – Obstructive breathing pattern • Long, slow inspiration – Exception - intrathoracic obstruction cause expiratory distress – Narrowing of airway causes reduced and turbulent airflow – Animal works harder to breathe against obstruction exacerbating edema and inflammation - vicious cycle • Stridor or Stertor • Increased RE +/- abdominal component • Orthopnea – +/- Hyperthermia – Auscultation • Referred upper airway sounds, be sure to listen over trachea • Obstructions can cause non-cardiogenic pulmonary edema (crackles)

Dyspneic Patient: Recognizing Breathing Patterns • Lower Airway Disease – Expiratory distress • Normal inspiration, exaggerated and prolonged expiration • Edema and cellular infiltrates of bronchiole walls lead to thickening and weakening of bronchial walls, excessive secretion, mucus plugs • Narrowing causes acute bronchospasm • As animal inhales, radial traction on the lungs pull the airways open and allows air to enter alveolus • As animal exhales, negative intrathoracic pressure causes airways to collapse, trapping air in alveolus – Alveolus full on next inspiration - reduced gas exchange – Marked expiratory abdominal “push” – Cats - cough (“coughing up hairballs”) – Auscultation • Expiratory wheezes • Loud crackles • No murmur – Exception - presence of cor pulmonale or concurrent cardiac disease
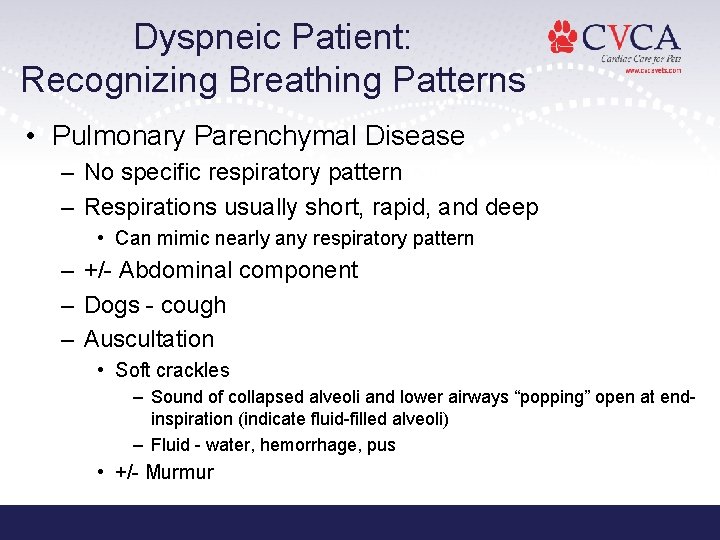
Dyspneic Patient: Recognizing Breathing Patterns • Pulmonary Parenchymal Disease – No specific respiratory pattern – Respirations usually short, rapid, and deep • Can mimic nearly any respiratory pattern – +/- Abdominal component – Dogs - cough – Auscultation • Soft crackles – Sound of collapsed alveoli and lower airways “popping” open at endinspiration (indicate fluid-filled alveoli) – Fluid - water, hemorrhage, pus • +/- Murmur
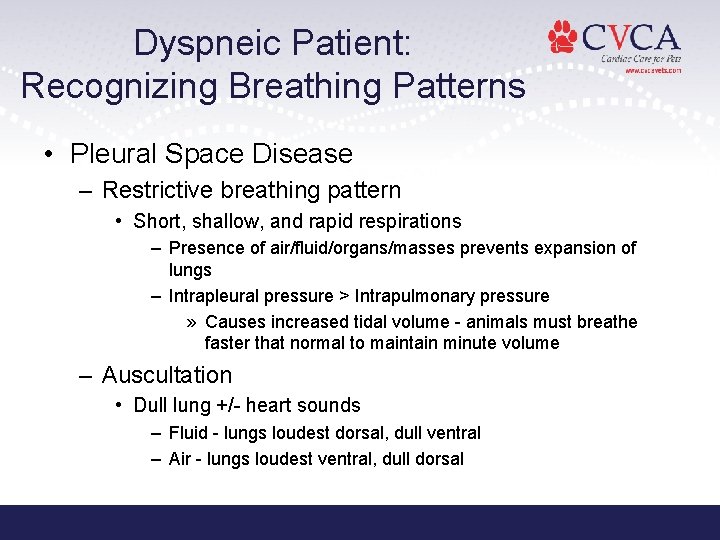
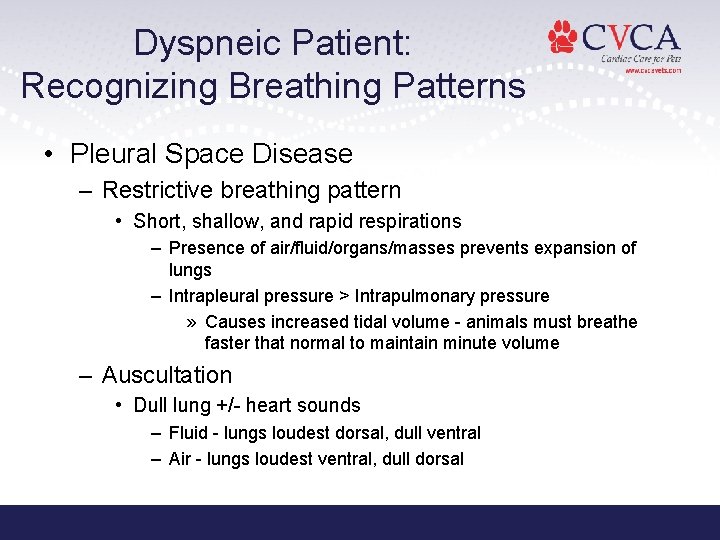
Dyspneic Patient: Recognizing Breathing Patterns • Pleural Space Disease – Restrictive breathing pattern • Short, shallow, and rapid respirations – Presence of air/fluid/organs/masses prevents expansion of lungs – Intrapleural pressure > Intrapulmonary pressure » Causes increased tidal volume - animals must breathe faster that normal to maintain minute volume – Auscultation • Dull lung +/- heart sounds – Fluid - lungs loudest dorsal, dull ventral – Air - lungs loudest ventral, dull dorsal
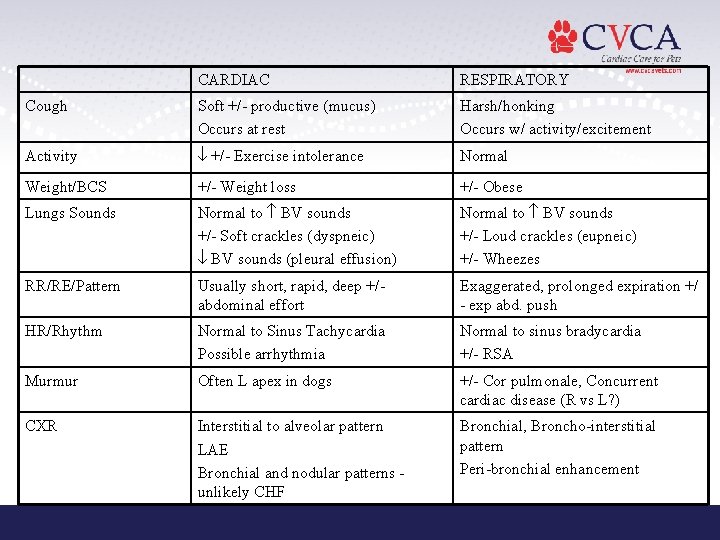
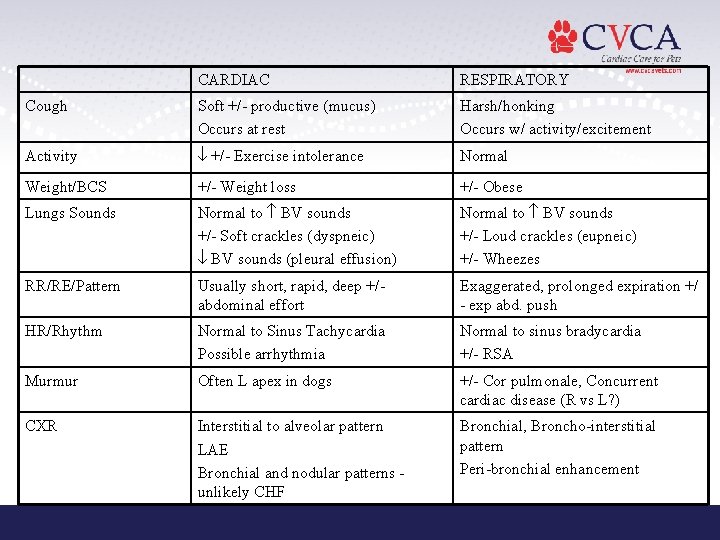
CARDIAC RESPIRATORY Cough Soft +/- productive (mucus) Occurs at rest Harsh/honking Occurs w/ activity/excitement Activity +/- Exercise intolerance Normal Weight/BCS +/- Weight loss +/- Obese Lungs Sounds Normal to BV sounds +/- Soft crackles (dyspneic) BV sounds (pleural effusion) Normal to BV sounds +/- Loud crackles (eupneic) +/- Wheezes RR/RE/Pattern Usually short, rapid, deep +/abdominal effort Exaggerated, prolonged expiration +/ - exp abd. push HR/Rhythm Normal to Sinus Tachycardia Possible arrhythmia Normal to sinus bradycardia +/- RSA Murmur Often L apex in dogs +/- Cor pulmonale, Concurrent cardiac disease (R vs L? ) CXR Interstitial to alveolar pattern LAE Bronchial and nodular patterns unlikely CHF Bronchial, Broncho-interstitial pattern Peri-bronchial enhancement
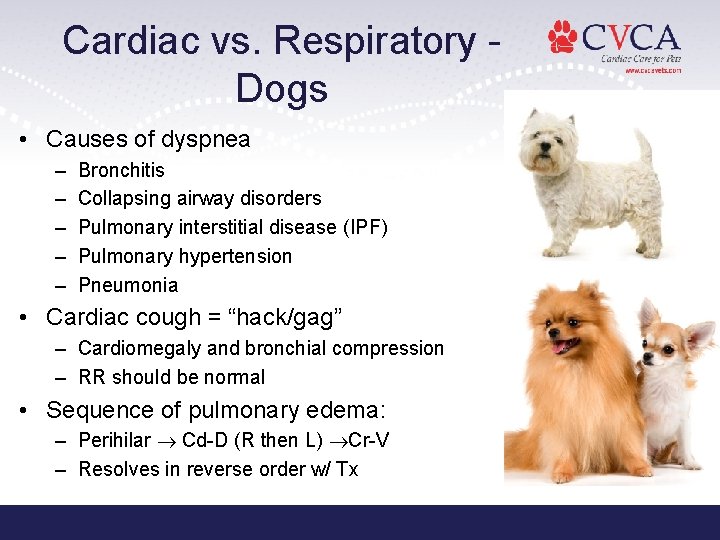
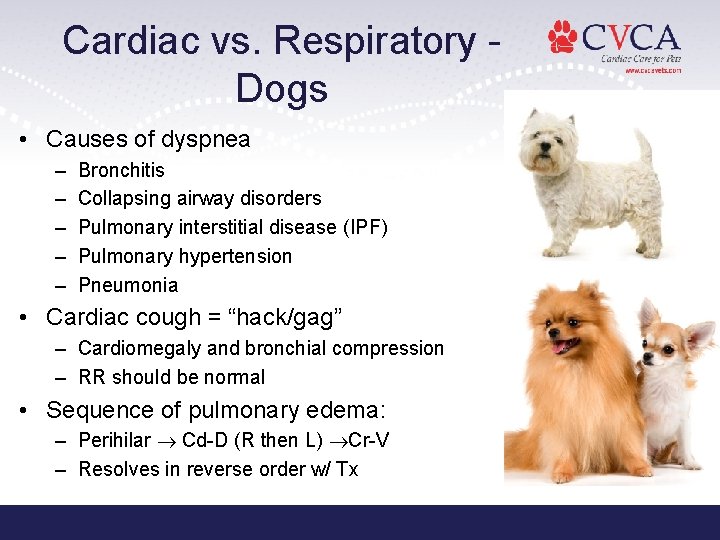
Cardiac vs. Respiratory Dogs • Causes of dyspnea – – – Bronchitis Collapsing airway disorders Pulmonary interstitial disease (IPF) Pulmonary hypertension Pneumonia • Cardiac cough = “hack/gag” – Cardiomegaly and bronchial compression – RR should be normal • Sequence of pulmonary edema: – Perihilar Cd-D (R then L) Cr-V – Resolves in reverse order w/ Tx
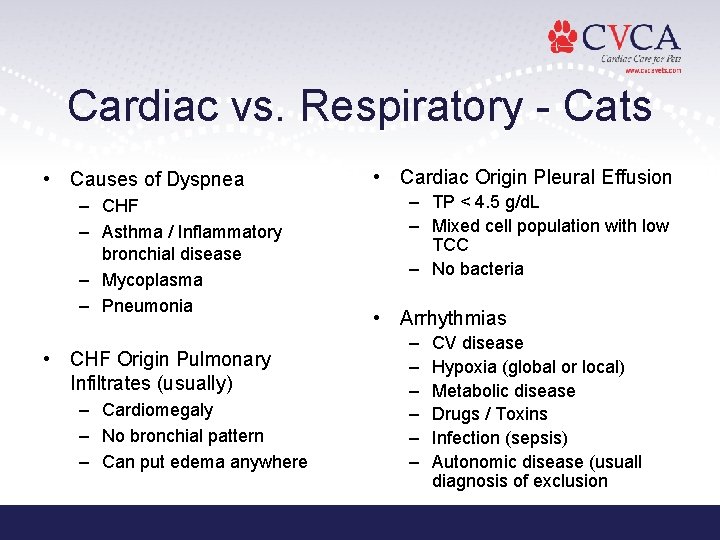
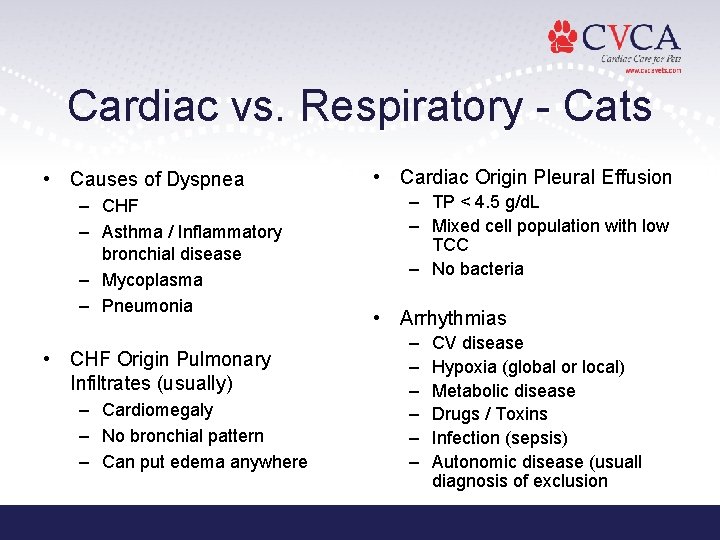
Cardiac vs. Respiratory - Cats • Causes of Dyspnea – CHF – Asthma / Inflammatory bronchial disease – Mycoplasma – Pneumonia • CHF Origin Pulmonary Infiltrates (usually) – Cardiomegaly – No bronchial pattern – Can put edema anywhere • Cardiac Origin Pleural Effusion – TP < 4. 5 g/d. L – Mixed cell population with low TCC – No bacteria • Arrhythmias – – – CV disease Hypoxia (global or local) Metabolic disease Drugs / Toxins Infection (sepsis) Autonomic disease (usuall diagnosis of exclusion
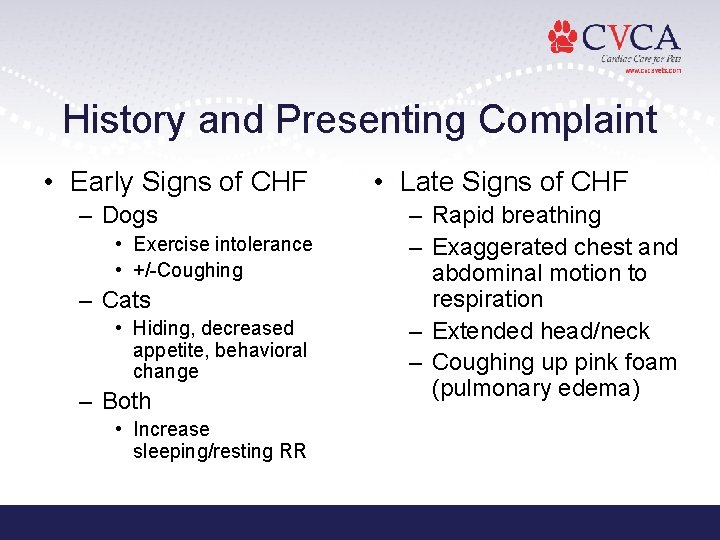
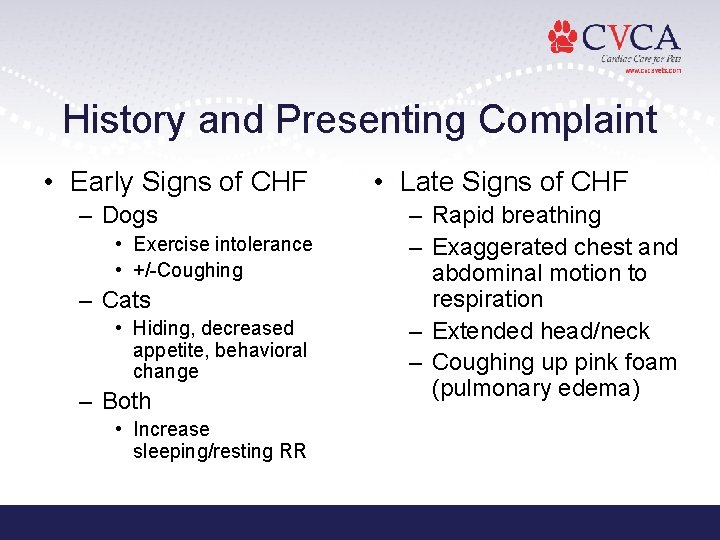
History and Presenting Complaint • Early Signs of CHF – Dogs • Exercise intolerance • +/-Coughing – Cats • Hiding, decreased appetite, behavioral change – Both • Increase sleeping/resting RR • Late Signs of CHF – Rapid breathing – Exaggerated chest and abdominal motion to respiration – Extended head/neck – Coughing up pink foam (pulmonary edema)
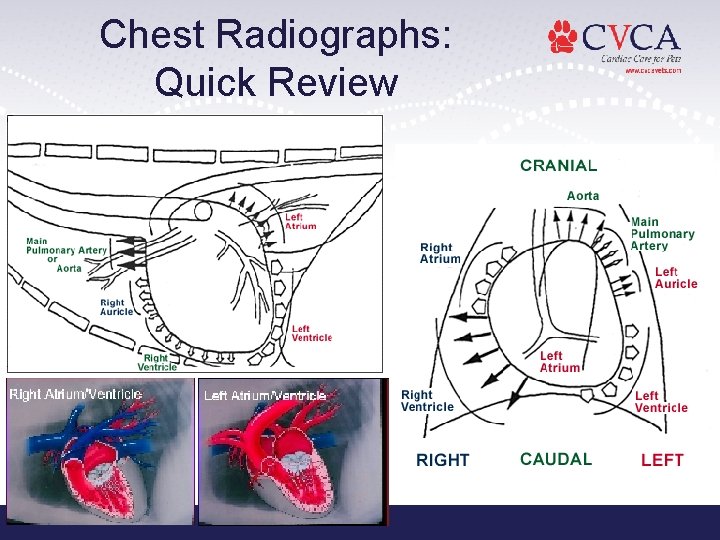
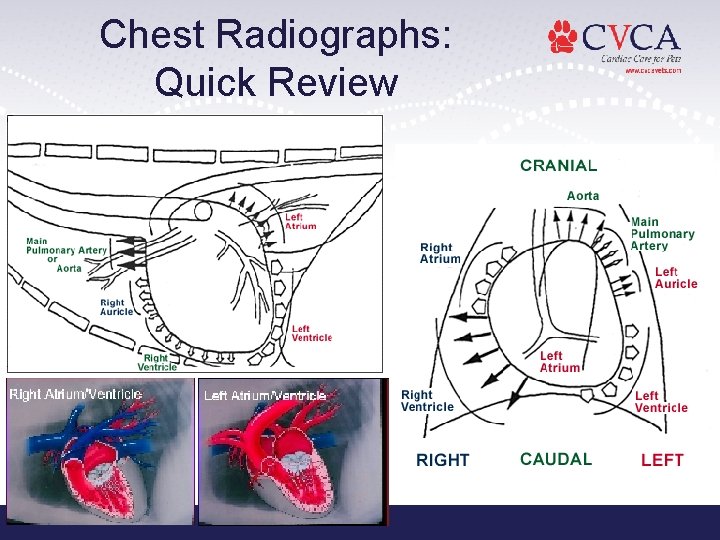
Chest Radiographs: Quick Review
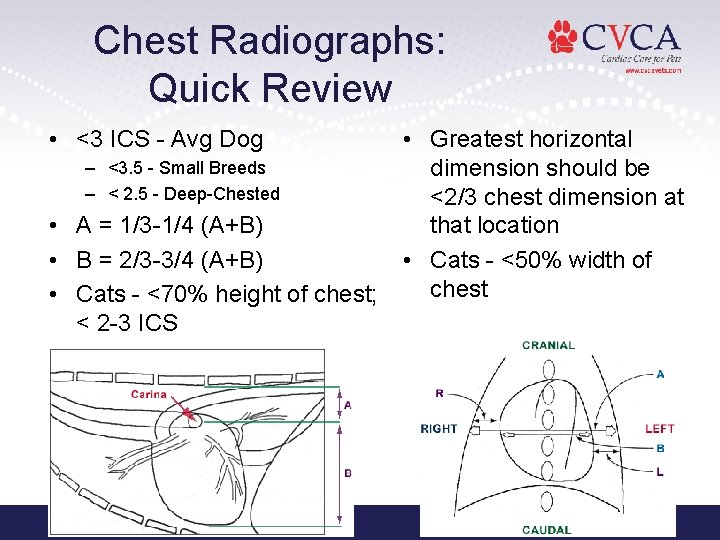
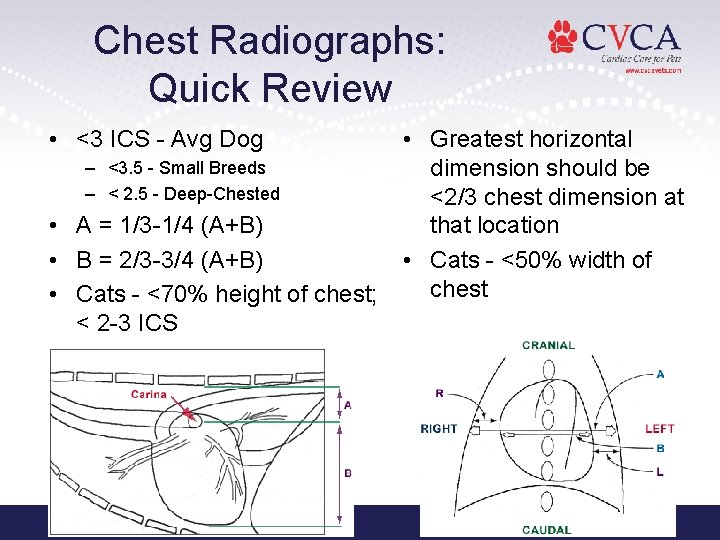
Chest Radiographs: Quick Review • <3 ICS - Avg Dog – <3. 5 - Small Breeds – < 2. 5 - Deep-Chested • A = 1/3 -1/4 (A+B) • B = 2/3 -3/4 (A+B) • Cats - <70% height of chest; < 2 -3 ICS • Greatest horizontal dimension should be <2/3 chest dimension at that location • Cats - <50% width of chest
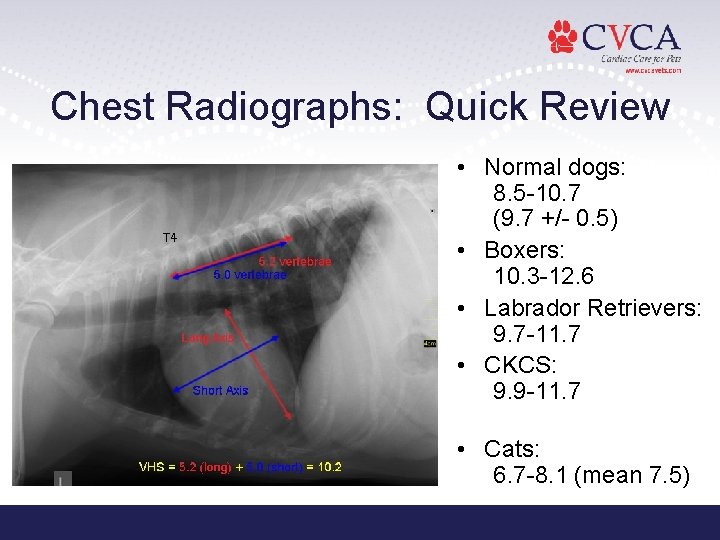
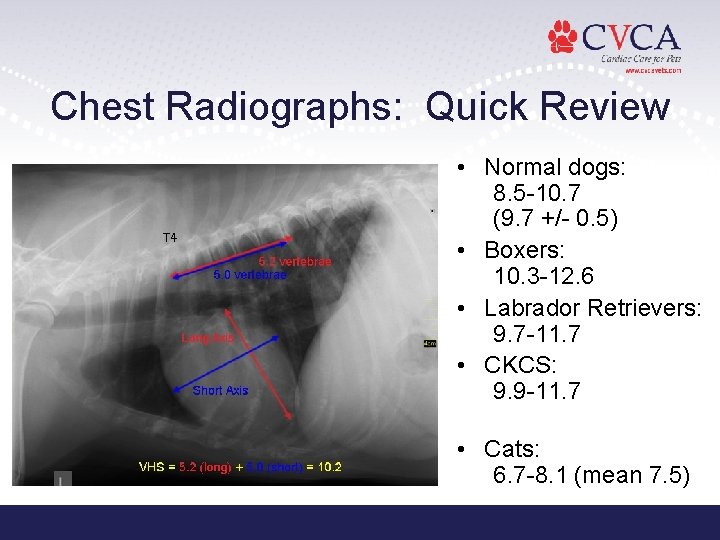
Chest Radiographs: Quick Review • Normal dogs: 8. 5 -10. 7 (9. 7 +/- 0. 5) • Boxers: 10. 3 -12. 6 • Labrador Retrievers: 9. 7 -11. 7 • CKCS: 9. 9 -11. 7 • Cats: 6. 7 -8. 1 (mean 7. 5)
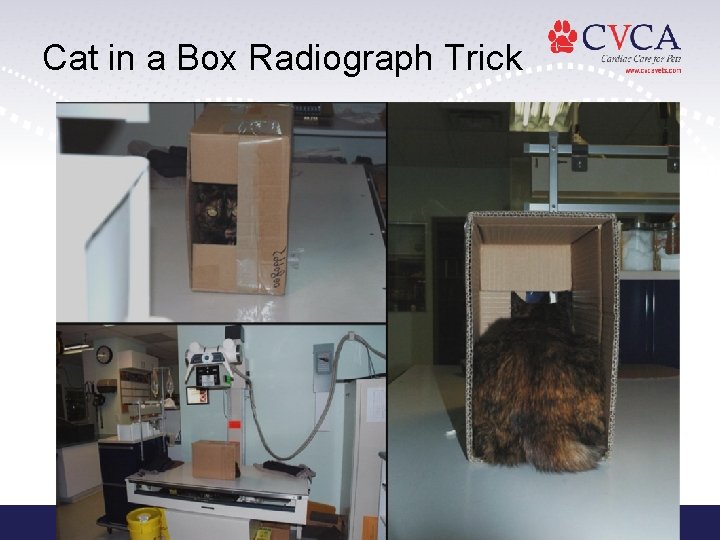
Cat in a Box Radiograph Trick
Ok…. so it’s CHF… Now what? ? ?
Congestive Heart Failure • Syndrome, not a disease – Abnormality of cardiac function that results in the failure of the heart to pump blood at a rate commensurate with requirements of metabolizing tissues
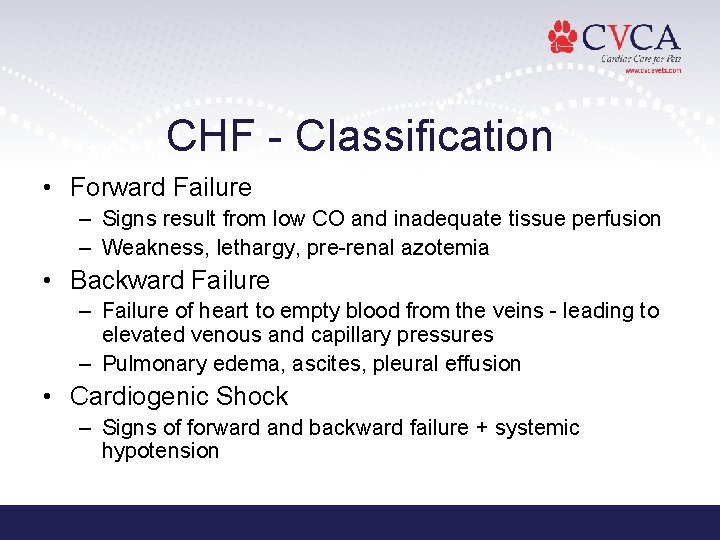
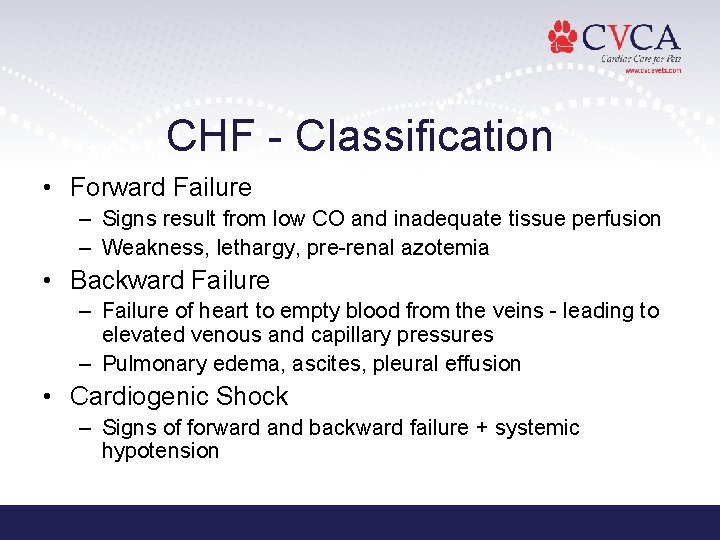
CHF - Classification • Forward Failure – Signs result from low CO and inadequate tissue perfusion – Weakness, lethargy, pre-renal azotemia • Backward Failure – Failure of heart to empty blood from the veins - leading to elevated venous and capillary pressures – Pulmonary edema, ascites, pleural effusion • Cardiogenic Shock – Signs of forward and backward failure + systemic hypotension
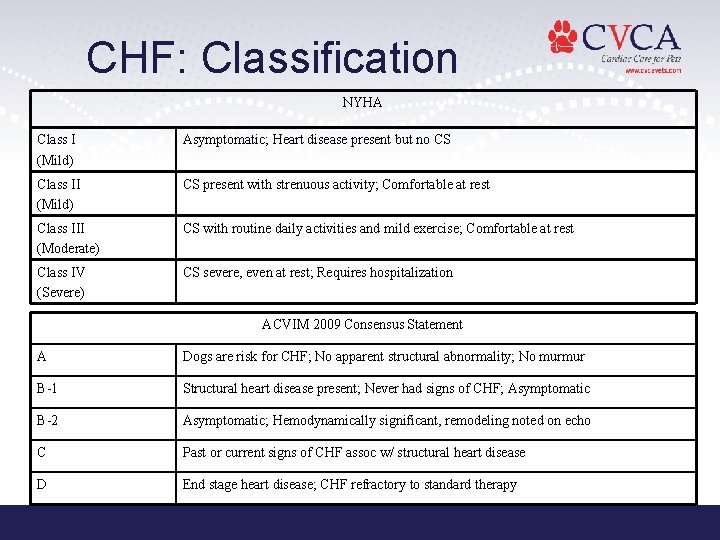
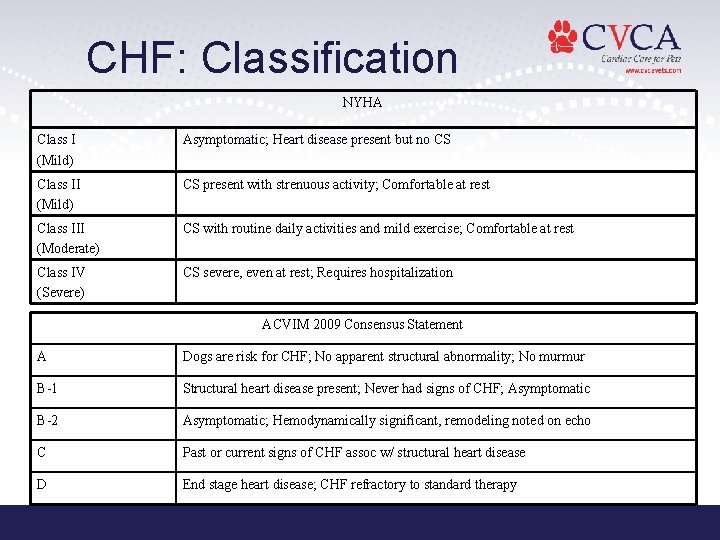
CHF: Classification NYHA Class I (Mild) Asymptomatic; Heart disease present but no CS Class II (Mild) CS present with strenuous activity; Comfortable at rest Class III (Moderate) CS with routine daily activities and mild exercise; Comfortable at rest Class IV (Severe) CS severe, even at rest; Requires hospitalization ACVIM 2009 Consensus Statement A Dogs are risk for CHF; No apparent structural abnormality; No murmur B-1 Structural heart disease present; Never had signs of CHF; Asymptomatic B-2 Asymptomatic; Hemodynamically significant, remodeling noted on echo C Past or current signs of CHF assoc w/ structural heart disease D End stage heart disease; CHF refractory to standard therapy
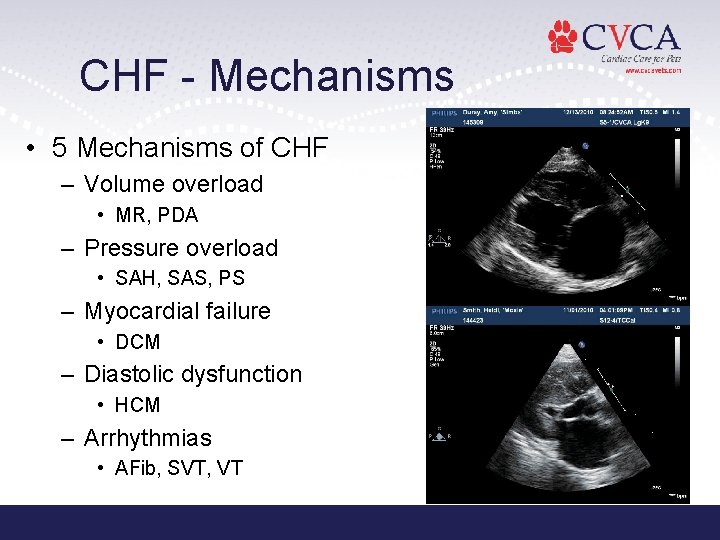
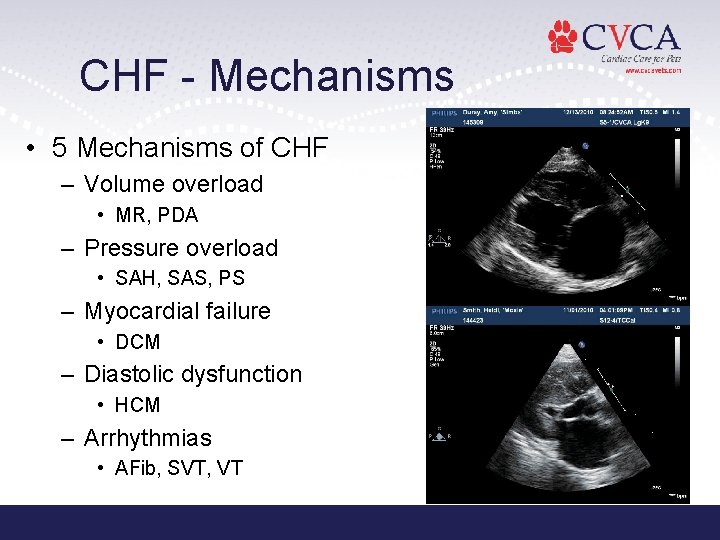
CHF - Mechanisms • 5 Mechanisms of CHF – Volume overload • MR, PDA – Pressure overload • SAH, SAS, PS – Myocardial failure • DCM – Diastolic dysfunction • HCM – Arrhythmias • AFib, SVT, VT
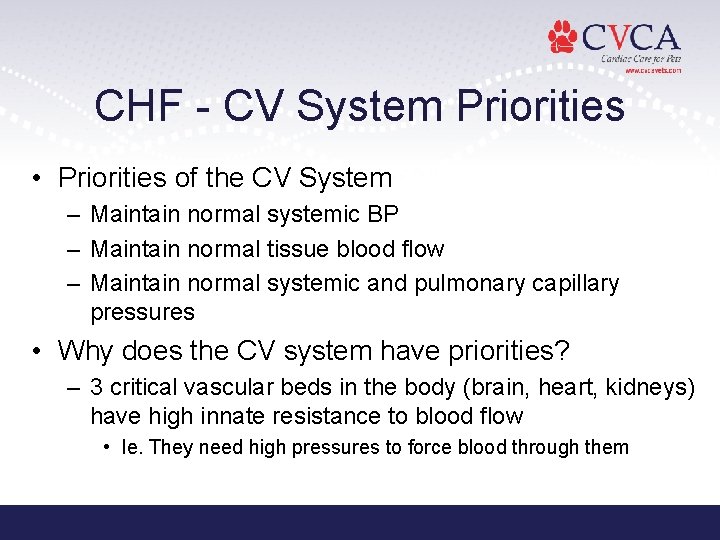
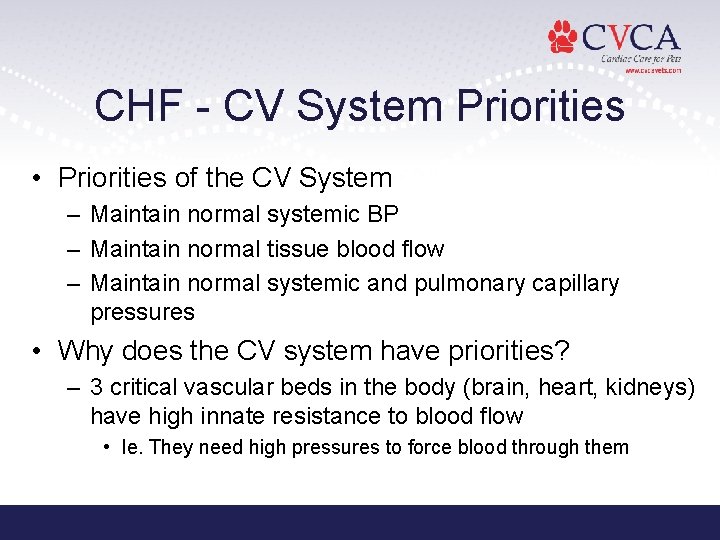
CHF - CV System Priorities • Priorities of the CV System – Maintain normal systemic BP – Maintain normal tissue blood flow – Maintain normal systemic and pulmonary capillary pressures • Why does the CV system have priorities? – 3 critical vascular beds in the body (brain, heart, kidneys) have high innate resistance to blood flow • Ie. They need high pressures to force blood through them
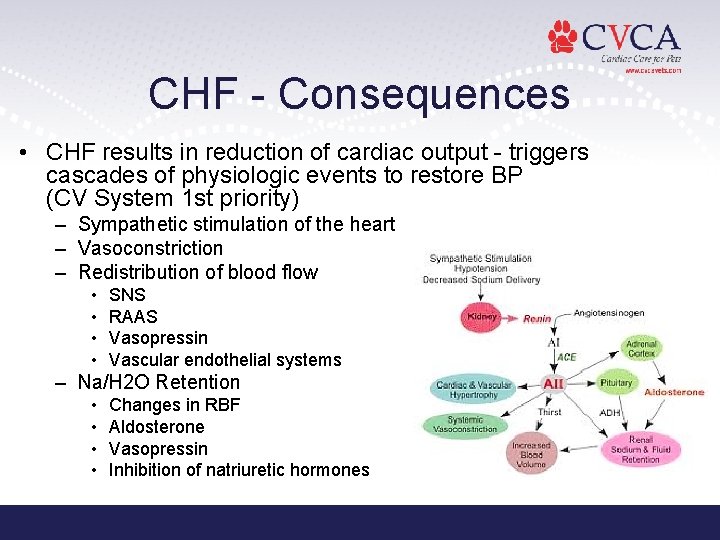
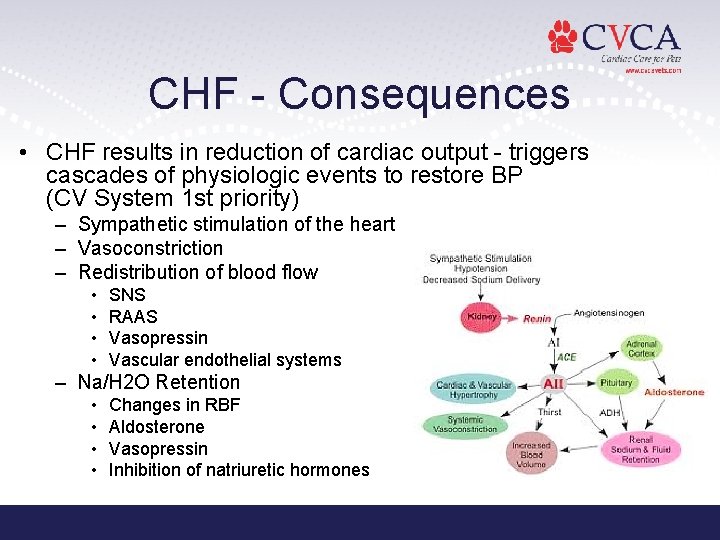
CHF - Consequences • CHF results in reduction of cardiac output - triggers cascades of physiologic events to restore BP (CV System 1 st priority) – Sympathetic stimulation of the heart – Vasoconstriction – Redistribution of blood flow • • SNS RAAS Vasopressin Vascular endothelial systems – Na/H 2 O Retention • • Changes in RBF Aldosterone Vasopressin Inhibition of natriuretic hormones
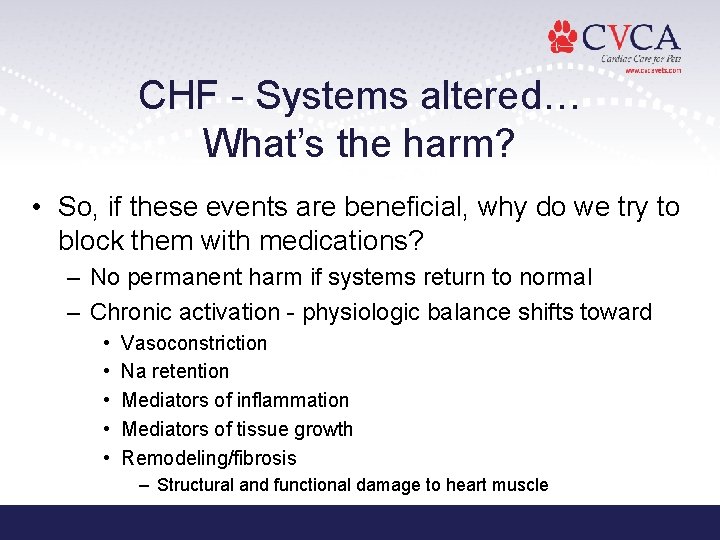
CHF - Systems altered… What’s the harm? • So, if these events are beneficial, why do we try to block them with medications? – No permanent harm if systems return to normal – Chronic activation - physiologic balance shifts toward • • • Vasoconstriction Na retention Mediators of inflammation Mediators of tissue growth Remodeling/fibrosis – Structural and functional damage to heart muscle
CHF - ER Management • Goals – Reduce venous congestion, edema, and effusion formation – Increase CO – Normalize HR and rhythm – Address forward failure signs (hypotension, hypothermia) • O 2 – Pulmonary edema can case life-threatening hypoxemia d/t decreased ability of O 2 to diffuse from alveoli into pulmonary capillaries – Increased inspired O 2 concentration increases pressure gradient of O 2 from alveoli to capillaries – Emergency - 60 -100% Fi. O 2 – Chronic O 2 therapy - 35 -40% Fi. O 2
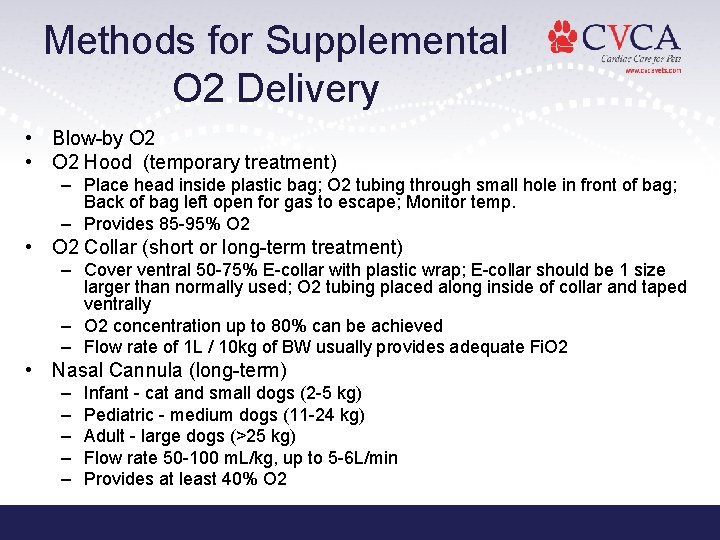
Methods for Supplemental O 2 Delivery • Blow-by O 2 • O 2 Hood (temporary treatment) – Place head inside plastic bag; O 2 tubing through small hole in front of bag; Back of bag left open for gas to escape; Monitor temp. – Provides 85 -95% O 2 • O 2 Collar (short or long-term treatment) – Cover ventral 50 -75% E-collar with plastic wrap; E-collar should be 1 size larger than normally used; O 2 tubing placed along inside of collar and taped ventrally – O 2 concentration up to 80% can be achieved – Flow rate of 1 L / 10 kg of BW usually provides adequate Fi. O 2 • Nasal Cannula (long-term) – – – Infant - cat and small dogs (2 -5 kg) Pediatric - medium dogs (11 -24 kg) Adult - large dogs (>25 kg) Flow rate 50 -100 m. L/kg, up to 5 -6 L/min Provides at least 40% O 2
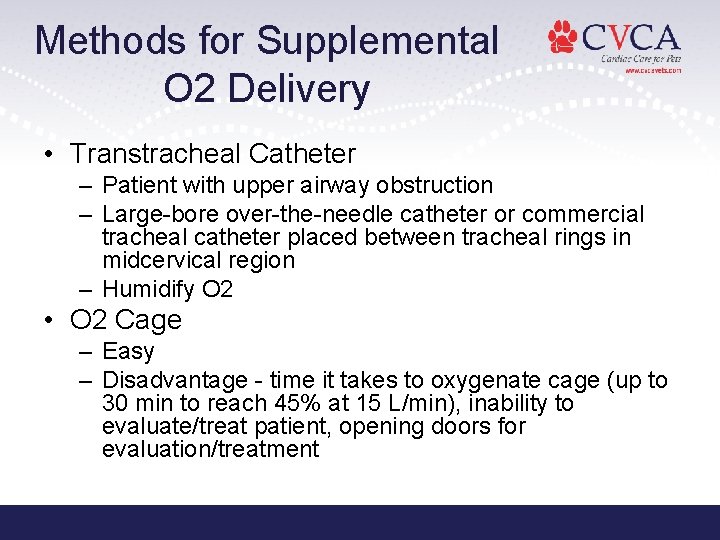
Methods for Supplemental O 2 Delivery • Transtracheal Catheter – Patient with upper airway obstruction – Large-bore over-the-needle catheter or commercial tracheal catheter placed between tracheal rings in midcervical region – Humidify O 2 • O 2 Cage – Easy – Disadvantage - time it takes to oxygenate cage (up to 30 min to reach 45% at 15 L/min), inability to evaluate/treat patient, opening doors for evaluation/treatment
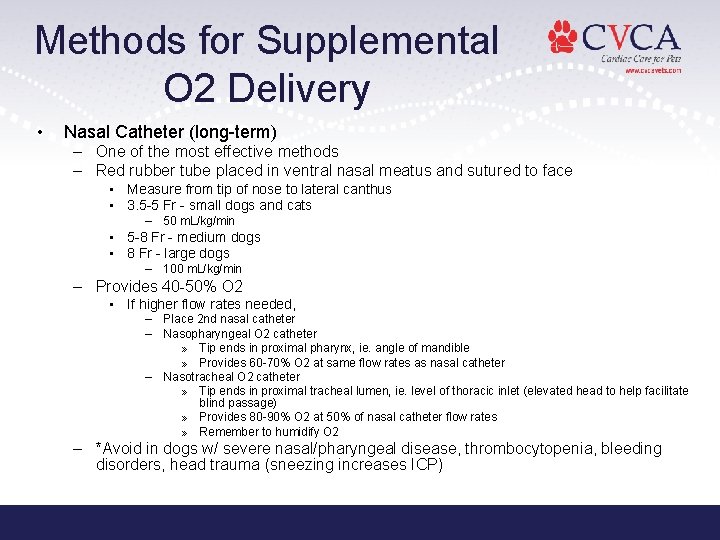
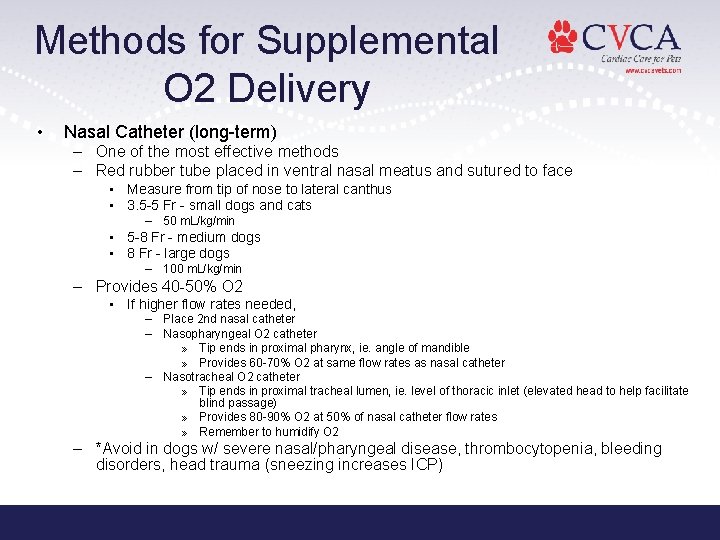
Methods for Supplemental O 2 Delivery • Nasal Catheter (long-term) – One of the most effective methods – Red rubber tube placed in ventral nasal meatus and sutured to face • Measure from tip of nose to lateral canthus • 3. 5 -5 Fr - small dogs and cats – 50 m. L/kg/min • 5 -8 Fr - medium dogs • 8 Fr - large dogs – 100 m. L/kg/min – Provides 40 -50% O 2 • If higher flow rates needed, – Place 2 nd nasal catheter – Nasopharyngeal O 2 catheter » Tip ends in proximal pharynx, ie. angle of mandible » Provides 60 -70% O 2 at same flow rates as nasal catheter – Nasotracheal O 2 catheter » Tip ends in proximal tracheal lumen, ie. level of thoracic inlet (elevated head to help facilitate blind passage) » Provides 80 -90% O 2 at 50% of nasal catheter flow rates » Remember to humidify O 2 – *Avoid in dogs w/ severe nasal/pharyngeal disease, thrombocytopenia, bleeding disorders, head trauma (sneezing increases ICP)
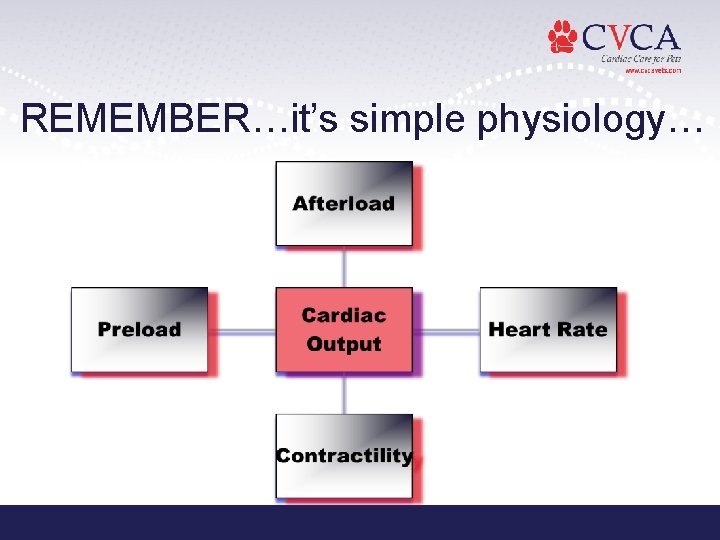
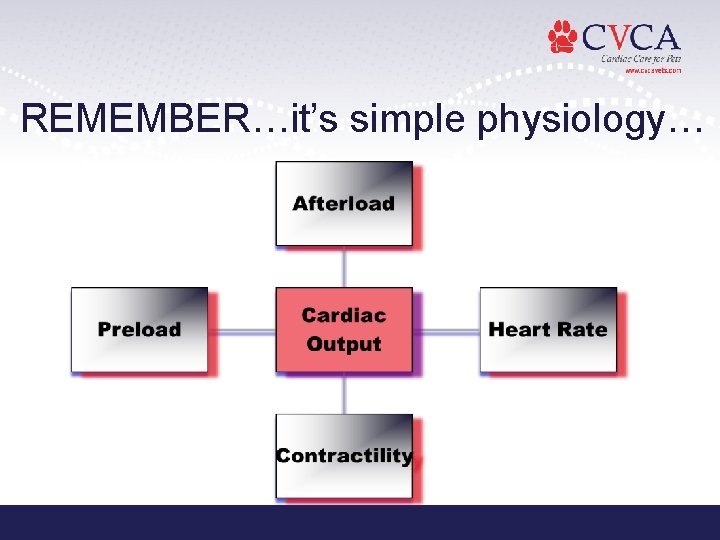
REMEMBER…it’s simple physiology…
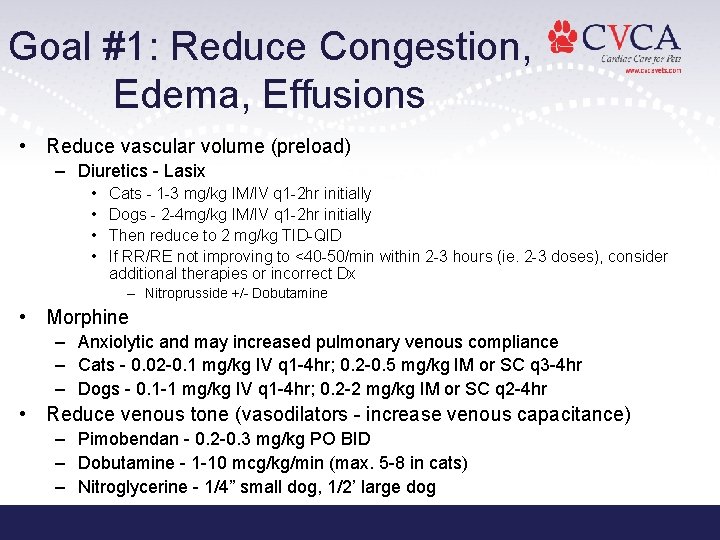
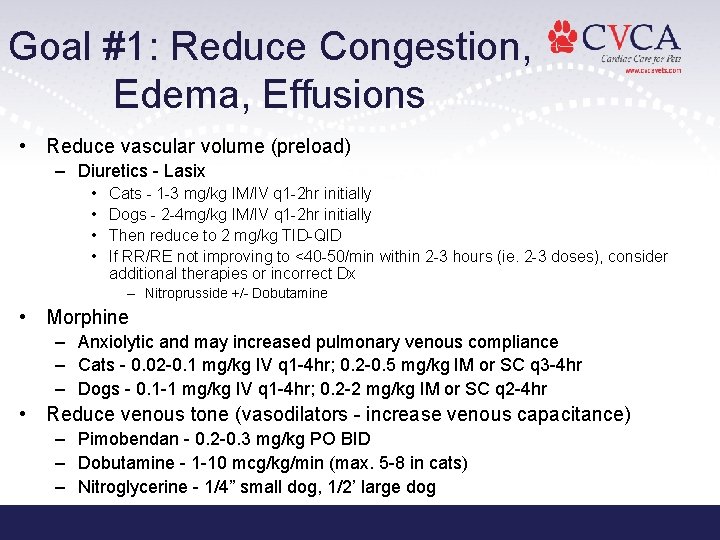
Goal #1: Reduce Congestion, Edema, Effusions • Reduce vascular volume (preload) – Diuretics - Lasix • • Cats - 1 -3 mg/kg IM/IV q 1 -2 hr initially Dogs - 2 -4 mg/kg IM/IV q 1 -2 hr initially Then reduce to 2 mg/kg TID-QID If RR/RE not improving to <40 -50/min within 2 -3 hours (ie. 2 -3 doses), consider additional therapies or incorrect Dx – Nitroprusside +/- Dobutamine • Morphine – Anxiolytic and may increased pulmonary venous compliance – Cats - 0. 02 -0. 1 mg/kg IV q 1 -4 hr; 0. 2 -0. 5 mg/kg IM or SC q 3 -4 hr – Dogs - 0. 1 -1 mg/kg IV q 1 -4 hr; 0. 2 -2 mg/kg IM or SC q 2 -4 hr • Reduce venous tone (vasodilators - increase venous capacitance) – Pimobendan - 0. 2 -0. 3 mg/kg PO BID – Dobutamine - 1 -10 mcg/kg/min (max. 5 -8 in cats) – Nitroglycerine - 1/4” small dog, 1/2’ large dog
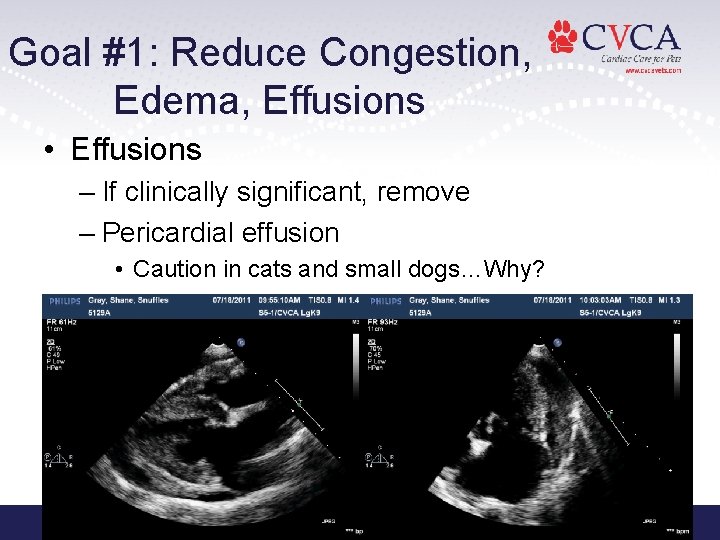
Goal #1: Reduce Congestion, Edema, Effusions • Effusions – If clinically significant, remove – Pericardial effusion • Caution in cats and small dogs…Why?
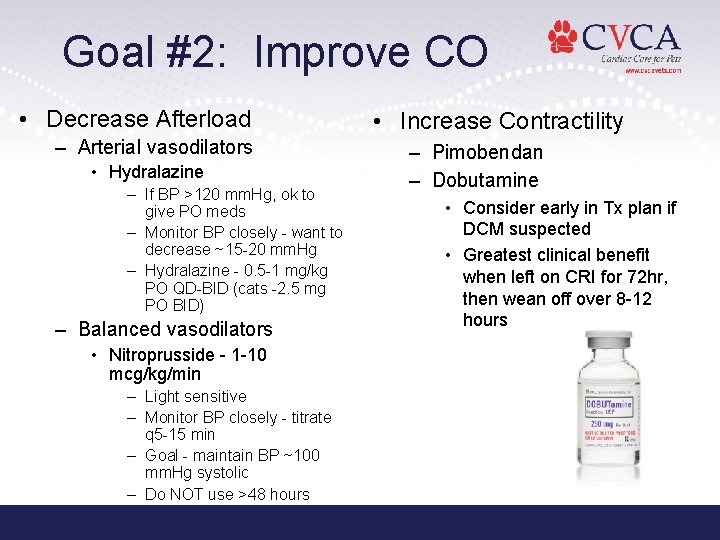
Goal #2: Improve CO • Decrease Afterload – Arterial vasodilators • Hydralazine – If BP >120 mm. Hg, ok to give PO meds – Monitor BP closely - want to decrease ~15 -20 mm. Hg – Hydralazine - 0. 5 -1 mg/kg PO QD-BID (cats -2. 5 mg PO BID) – Balanced vasodilators • Nitroprusside - 1 -10 mcg/kg/min – Light sensitive – Monitor BP closely - titrate q 5 -15 min – Goal - maintain BP ~100 mm. Hg systolic – Do NOT use >48 hours • Increase Contractility – Pimobendan – Dobutamine • Consider early in Tx plan if DCM suspected • Greatest clinical benefit when left on CRI for 72 hr, then wean off over 8 -12 hours
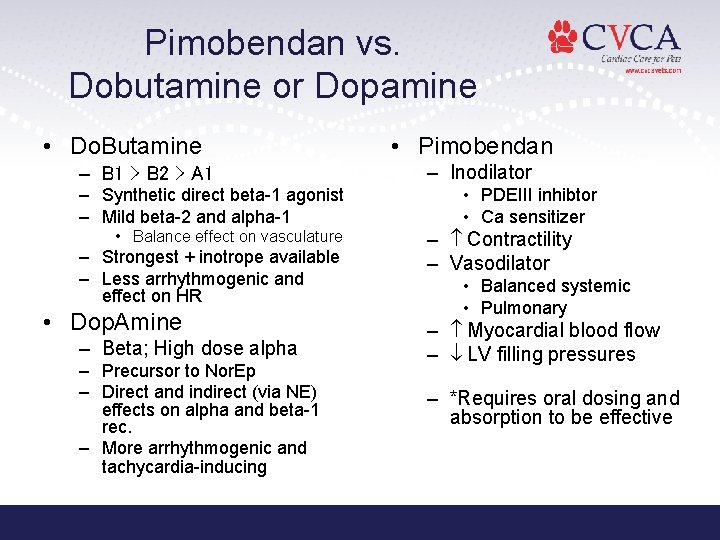
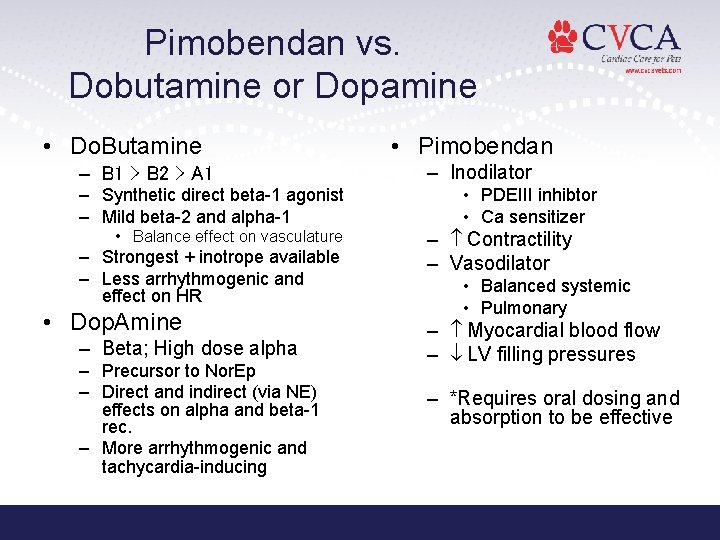
Pimobendan vs. Dobutamine or Dopamine • Do. Butamine – B 1 > B 2 > A 1 – Synthetic direct beta-1 agonist – Mild beta-2 and alpha-1 • Balance effect on vasculature – Strongest + inotrope available – Less arrhythmogenic and effect on HR • Dop. Amine – Beta; High dose alpha – Precursor to Nor. Ep – Direct and indirect (via NE) effects on alpha and beta-1 rec. – More arrhythmogenic and tachycardia-inducing • Pimobendan – Inodilator • PDEIII inhibtor • Ca sensitizer – Contractility – Vasodilator • Balanced systemic • Pulmonary – Myocardial blood flow – LV filling pressures – *Requires oral dosing and absorption to be effective
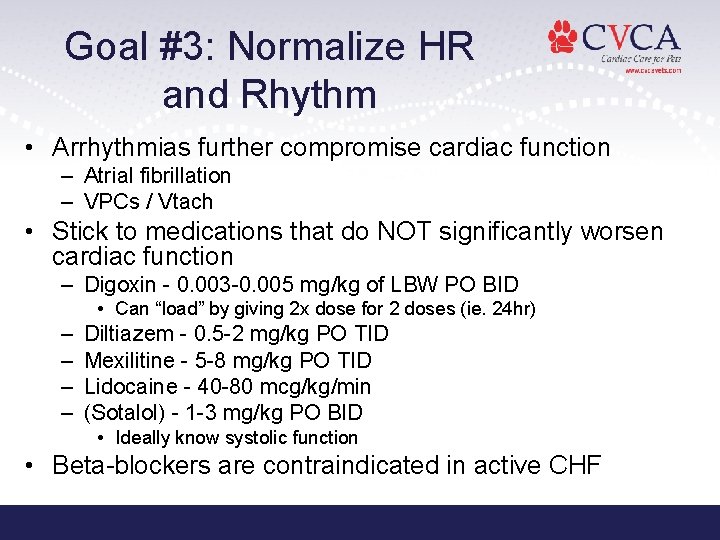
Goal #3: Normalize HR and Rhythm • Arrhythmias further compromise cardiac function – Atrial fibrillation – VPCs / Vtach • Stick to medications that do NOT significantly worsen cardiac function – Digoxin - 0. 003 -0. 005 mg/kg of LBW PO BID • Can “load” by giving 2 x dose for 2 doses (ie. 24 hr) – – Diltiazem - 0. 5 -2 mg/kg PO TID Mexilitine - 5 -8 mg/kg PO TID Lidocaine - 40 -80 mcg/kg/min (Sotalol) - 1 -3 mg/kg PO BID • Ideally know systolic function • Beta-blockers are contraindicated in active CHF
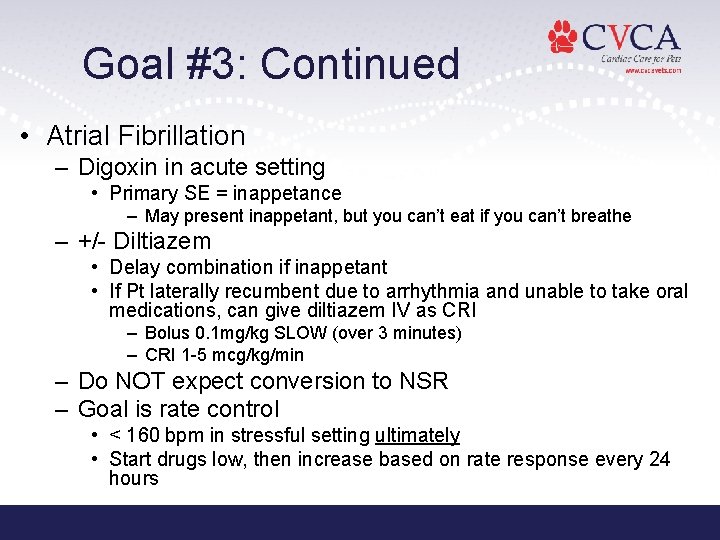
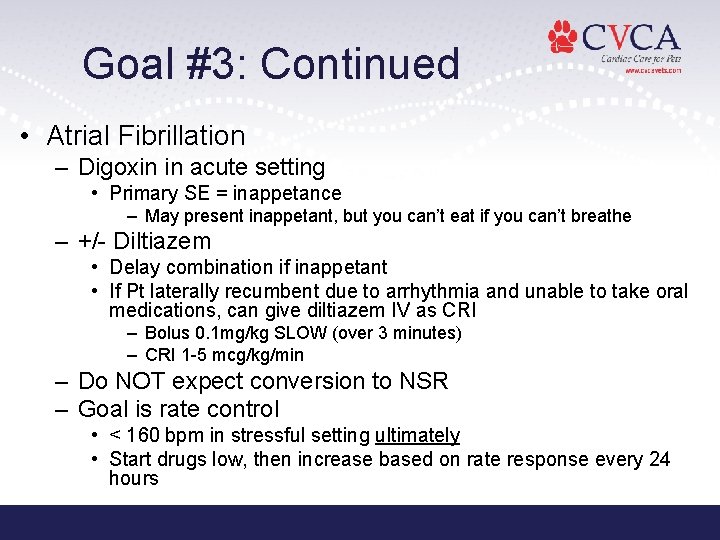
Goal #3: Continued • Atrial Fibrillation – Digoxin in acute setting • Primary SE = inappetance – May present inappetant, but you can’t eat if you can’t breathe – +/- Diltiazem • Delay combination if inappetant • If Pt laterally recumbent due to arrhythmia and unable to take oral medications, can give diltiazem IV as CRI – Bolus 0. 1 mg/kg SLOW (over 3 minutes) – CRI 1 -5 mcg/kg/min – Do NOT expect conversion to NSR – Goal is rate control • < 160 bpm in stressful setting ultimately • Start drugs low, then increase based on rate response every 24 hours
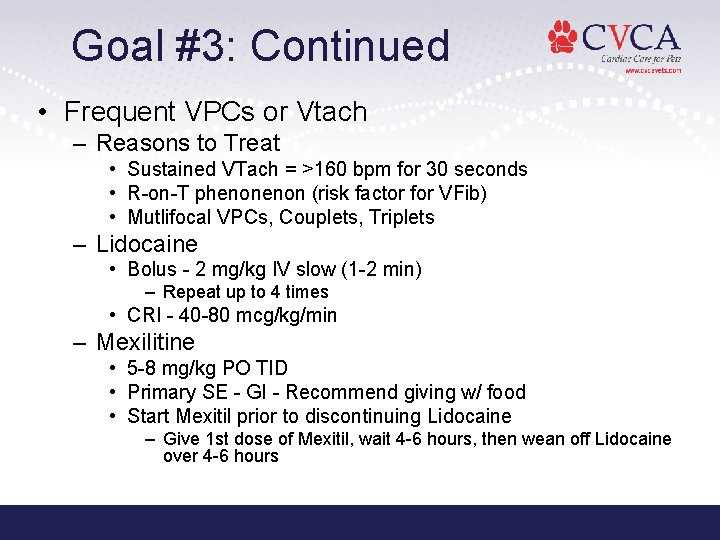
Goal #3: Continued • Frequent VPCs or Vtach – Reasons to Treat • Sustained VTach = >160 bpm for 30 seconds • R-on-T phenon (risk factor for VFib) • Mutlifocal VPCs, Couplets, Triplets – Lidocaine • Bolus - 2 mg/kg IV slow (1 -2 min) – Repeat up to 4 times • CRI - 40 -80 mcg/kg/min – Mexilitine • 5 -8 mg/kg PO TID • Primary SE - GI - Recommend giving w/ food • Start Mexitil prior to discontinuing Lidocaine – Give 1 st dose of Mexitil, wait 4 -6 hours, then wean off Lidocaine over 4 -6 hours
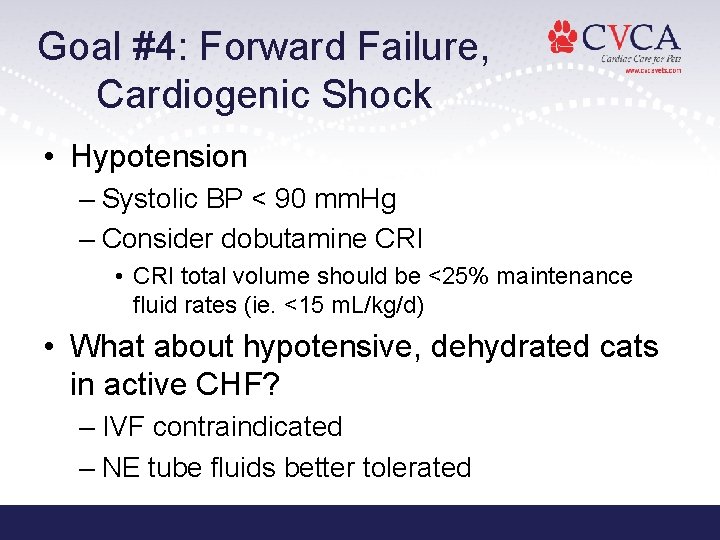
Goal #4: Forward Failure, Cardiogenic Shock • Hypotension – Systolic BP < 90 mm. Hg – Consider dobutamine CRI • CRI total volume should be <25% maintenance fluid rates (ie. <15 m. L/kg/d) • What about hypotensive, dehydrated cats in active CHF? – IVF contraindicated – NE tube fluids better tolerated
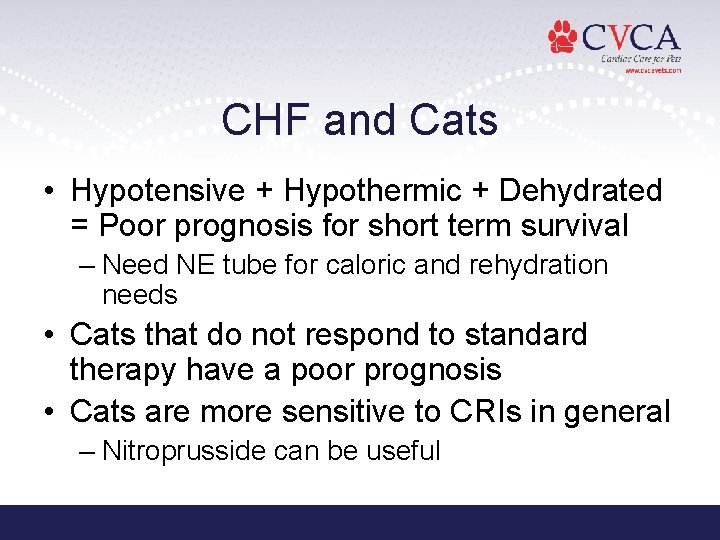
CHF and Cats • Hypotensive + Hypothermic + Dehydrated = Poor prognosis for short term survival – Need NE tube for caloric and rehydration needs • Cats that do not respond to standard therapy have a poor prognosis • Cats are more sensitive to CRIs in general – Nitroprusside can be useful

Comments / Questions Contact Information: info@cvcavets. com www. cvcavets. com
 Congestive heart failure zones for management
Congestive heart failure zones for management Nursing assessment for congestive heart failure
Nursing assessment for congestive heart failure Nursing assessment for congestive heart failure
Nursing assessment for congestive heart failure Congestive heart failure symtoms
Congestive heart failure symtoms Non conducted pac ecg
Non conducted pac ecg Failure to sense pacemaker
Failure to sense pacemaker Ductile fracture
Ductile fracture Forrester classification heart failure
Forrester classification heart failure Cardiomegay
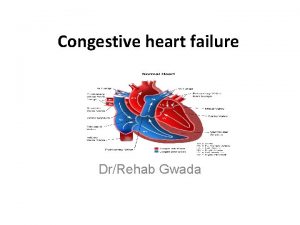
Cardiomegay Heart failure definition
Heart failure definition Causes of cardiomegaly in child
Causes of cardiomegaly in child Heart failure complications
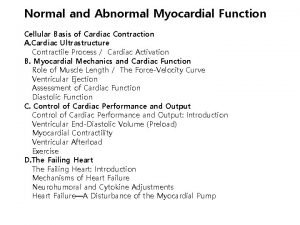
Heart failure complications Chapter 24 heart failure drugs
Chapter 24 heart failure drugs Heart failure
Heart failure Lmnop heart failure
Lmnop heart failure Keith rn heart failure case study
Keith rn heart failure case study Donkey analogy heart failure
Donkey analogy heart failure Heart failure cells are seen in lungs
Heart failure cells are seen in lungs Heart failure forward vs backward
Heart failure forward vs backward Vetsulin dosage chart for dogs
Vetsulin dosage chart for dogs Diabetes and heart failure
Diabetes and heart failure Compensatory mechanisms of heart failure
Compensatory mechanisms of heart failure Cardiac landmarks
Cardiac landmarks Acute vs chronic heart failure
Acute vs chronic heart failure Dr nienkemper
Dr nienkemper Right border of the relative cardiac dullness is formed by
Right border of the relative cardiac dullness is formed by Sheep heart diagram
Sheep heart diagram Heart 2 heart
Heart 2 heart What is sems
What is sems Emergency management of maxillofacial trauma
Emergency management of maxillofacial trauma Hennepin county emergency management
Hennepin county emergency management Emergency management
Emergency management Walmart emergency response system
Walmart emergency response system Ares clint
Ares clint Raptor reunification
Raptor reunification Emergency management institute
Emergency management institute Emergency management institute
Emergency management institute Emergency management institute
Emergency management institute Ucf public administration masters
Ucf public administration masters Tulane university emergency management
Tulane university emergency management Raptor emergency management
Raptor emergency management Emergency management
Emergency management Canadian emergency management college
Canadian emergency management college Ims incident management
Ims incident management