Respiratory Failure RF Prof Omer Alamoudi MD FRCP








- Slides: 45

Respiratory Failure (RF) Prof. Omer Alamoudi, MD, FRCP, FCCP, FACP
Respiratory Failure (RF) n Normal ABG n Definition n Classification of RF n Distinction between Acute and Chronic RF n Pathophysiologic causes of Acute RF n Diagnosis of RF n Causes n Clinical presentation n Investigations n Management of RF
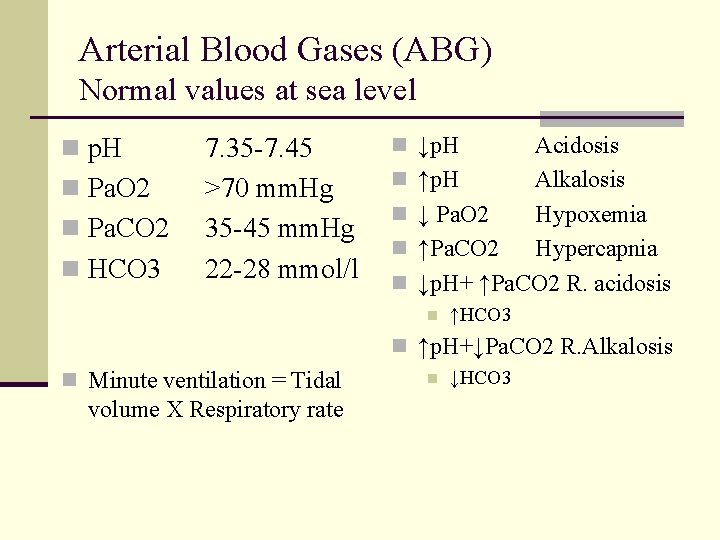
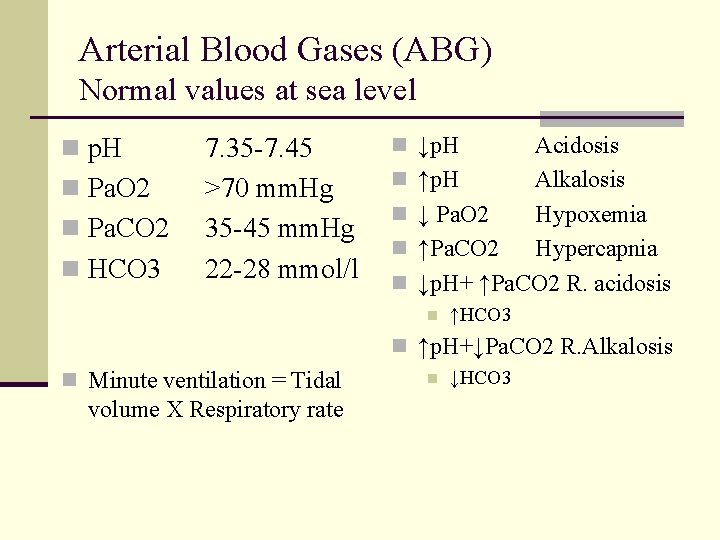
Arterial Blood Gases (ABG) Normal values at sea level n p. H n Pa. O 2 n Pa. CO 2 n HCO 3 7. 35 -7. 45 >70 mm. Hg 35 -45 mm. Hg 22 -28 mmol/l n ↓p. H n n Acidosis ↑p. H Alkalosis ↓ Pa. O 2 Hypoxemia ↑Pa. CO 2 Hypercapnia ↓p. H+ ↑Pa. CO 2 R. acidosis n ↑HCO 3 n ↑p. H+↓Pa. CO 2 R. Alkalosis n Minute ventilation = Tidal volume X Respiratory rate n ↓HCO 3
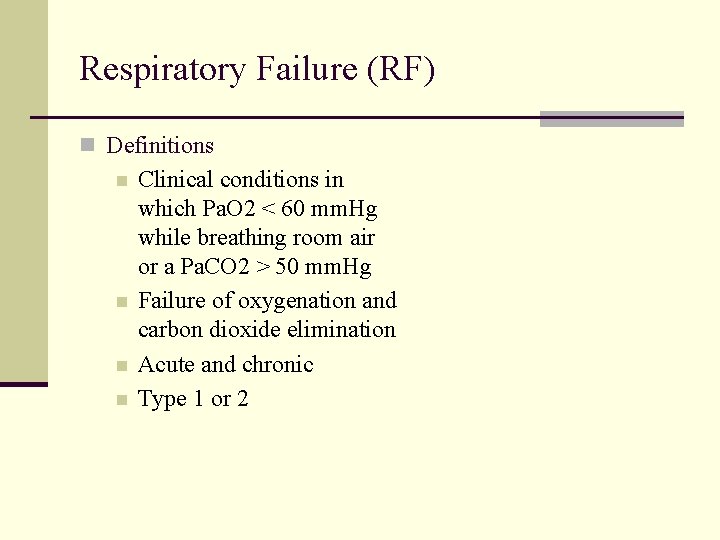
Respiratory Failure (RF) n Definitions n n Clinical conditions in which Pa. O 2 < 60 mm. Hg while breathing room air or a Pa. CO 2 > 50 mm. Hg Failure of oxygenation and carbon dioxide elimination Acute and chronic Type 1 or 2

Classification of RF n Type 1 n Hypoxemic RF ** n Pa. O 2 < 60 mm. Hg with normal or ↓ Pa. CO 2 q Associated with acute diseases of the lung q Pulmonary edema (Cardiogenic, noncardiogenic (ARDS), pneumonia, pulmonary hemorrhage, and collapse n n n Type 2 Hypercapnic RF Pa. CO 2 > 50 mm. Hg Hypoxemia is common Drug overdose, neuromuscular disease, chest wall deformity, COPD, and Bronchial asthma
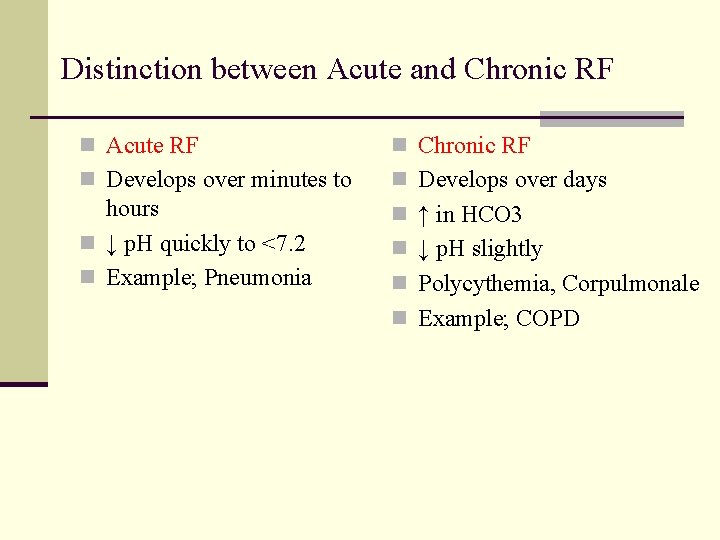
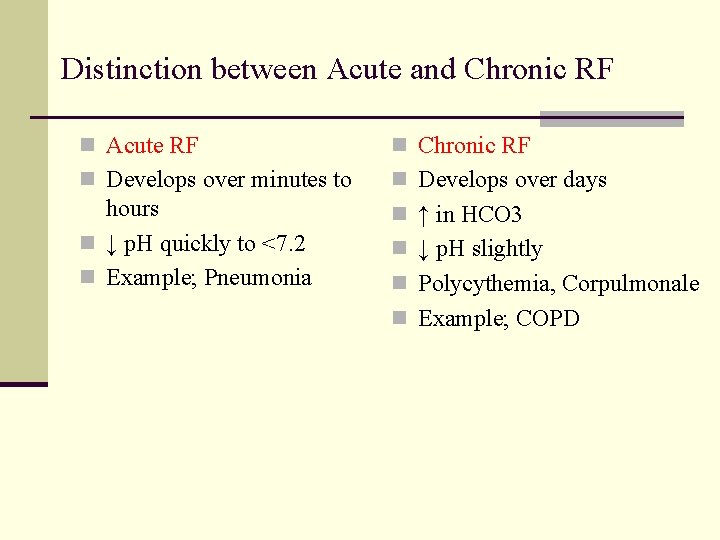
Distinction between Acute and Chronic RF n Acute RF n Chronic RF n Develops over minutes to n Develops over days hours n ↓ p. H quickly to <7. 2 n Example; Pneumonia n ↑ in HCO 3 n ↓ p. H slightly n Polycythemia, Corpulmonale n Example; COPD
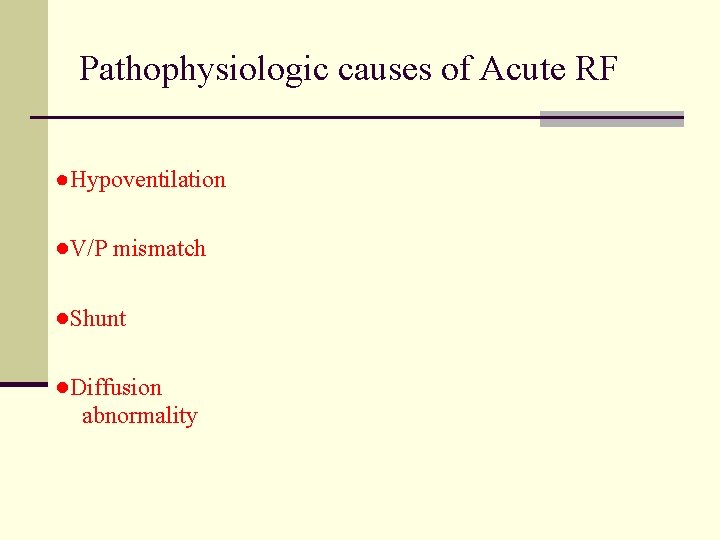
Pathophysiologic causes of Acute RF ●Hypoventilation ●V/P mismatch ●Shunt ●Diffusion abnormality

Pathophysiologic causes of Acute RF 1 - Hypoventilation n Occurs when ventilation ↓ n n 4 -6 l/min Causes n Depression of CNS from drugs n Neuromuscular disease of respiratory ms ↑Pa. CO 2 and ↓Pa. O 2 Alveolar –arterial PO 2 gradient is normal COPD
Pathophysiologic causes of Acute RF ●Hypoventilation ●V/P mismatch ●Shunt ●Diffusion abnormality
Pathophysiologic causes of Acute RF 2 -V/Q mismatch n Most common cause of hypoxemia n Low V/Q ratio, may occur either from n Decrease of ventilation 2 ry to airway or interstitial lung disease n Overperfusion in the presence of normal ventilation e. g. PE n Admin. of 100% O 2 eliminate hypoxemia
Pathophysiologic causes of Acute RF ●Hypoventilation ●V/P mismatch ●Shunt ●Diffusion abnormality
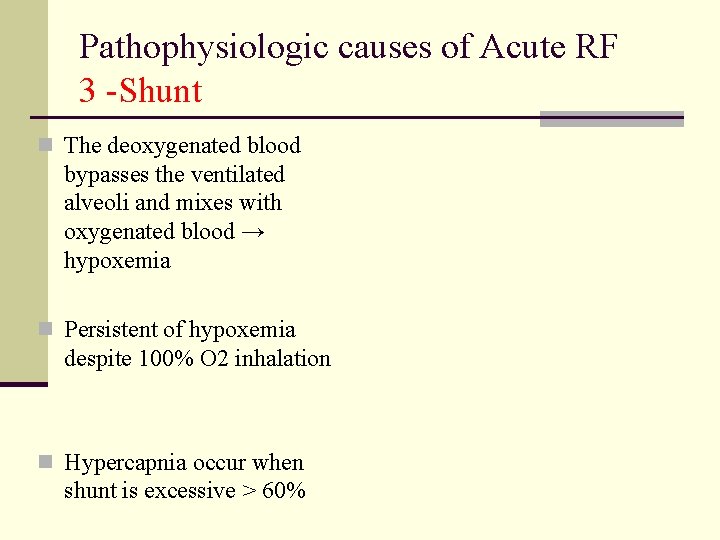
Pathophysiologic causes of Acute RF 3 -Shunt n The deoxygenated blood bypasses the ventilated alveoli and mixes with oxygenated blood → hypoxemia n Persistent of hypoxemia despite 100% O 2 inhalation n Hypercapnia occur when shunt is excessive > 60%

Pathophysiologic causes of Acute RF 3 – Causes of Shunt n Intracardiac Right to left shunt n Fallot’s tetralogy n Eisenmenger’s syndrome n Pulmonary n A/V malformation n Pneumonia n Pulmonary edema n Atelectasis/collapse n Pulmonary Hge n Pulmonary contusion n
Pathophysiologic causes of Acute RF ●Hypoventilation ●V/P mismatch ●Shunt ●Diffusion abnormality
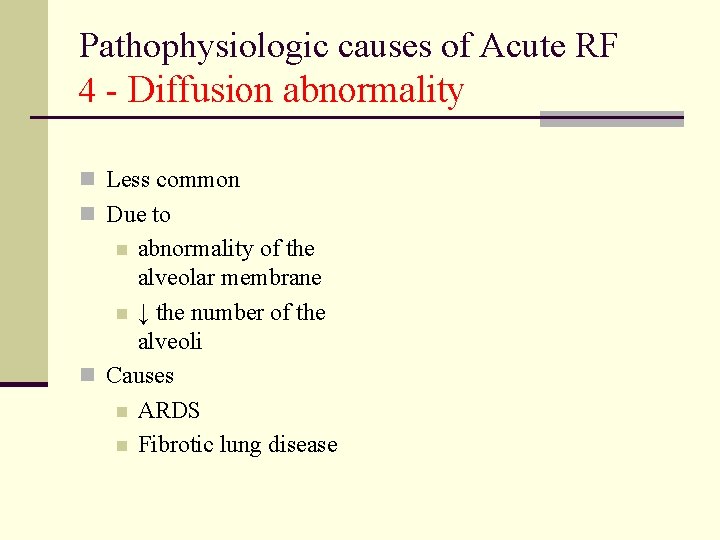
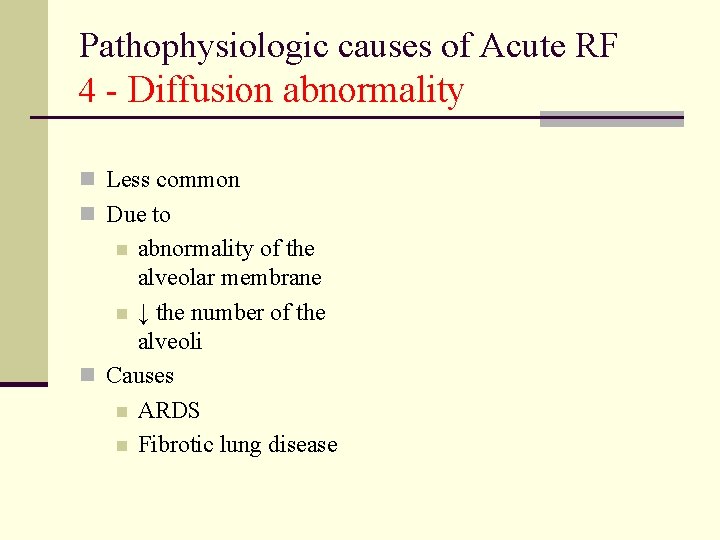
Pathophysiologic causes of Acute RF 4 - Diffusion abnormality n Less common n Due to abnormality of the alveolar membrane n ↓ the number of the alveoli n Causes n ARDS n Fibrotic lung disease n
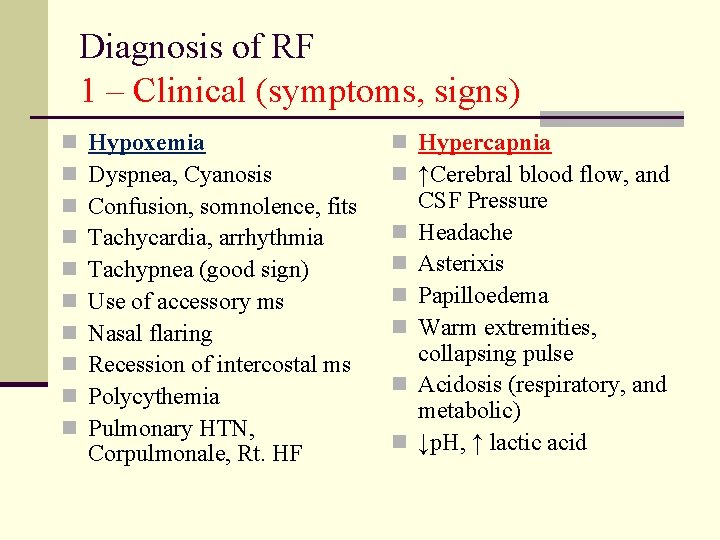
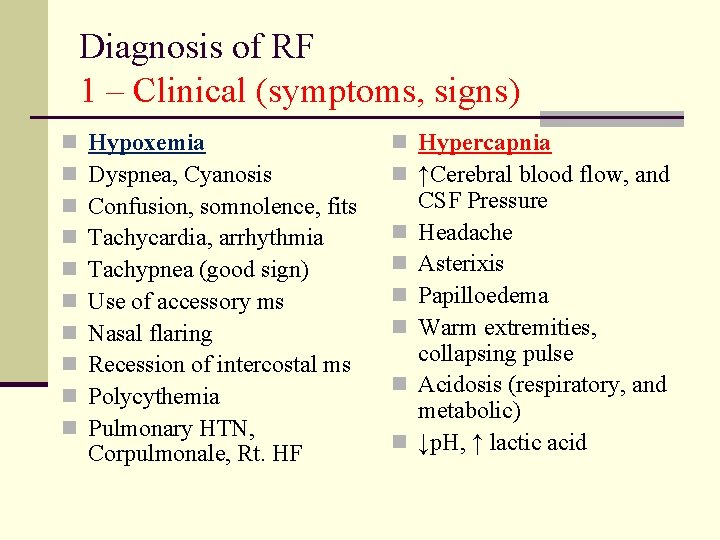
Diagnosis of RF 1 – Clinical (symptoms, signs) n n n n n Hypoxemia Dyspnea, Cyanosis Confusion, somnolence, fits Tachycardia, arrhythmia Tachypnea (good sign) Use of accessory ms Nasal flaring Recession of intercostal ms Polycythemia Pulmonary HTN, Corpulmonale, Rt. HF n Hypercapnia n ↑Cerebral blood flow, and n n n CSF Pressure Headache Asterixis Papilloedema Warm extremities, collapsing pulse Acidosis (respiratory, and metabolic) ↓p. H, ↑ lactic acid
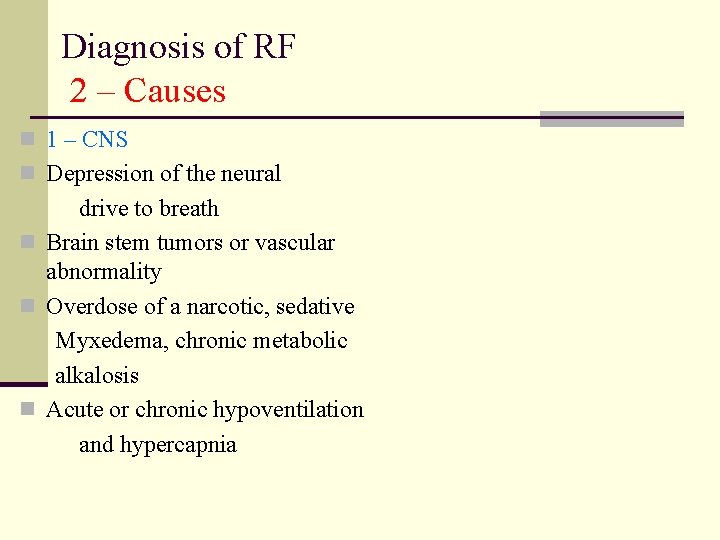
Diagnosis of RF 2 – Causes n 1 – CNS n Depression of the neural drive to breath n Brain stem tumors or vascular abnormality n Overdose of a narcotic, sedative Myxedema, chronic metabolic alkalosis n Acute or chronic hypoventilation and hypercapnia
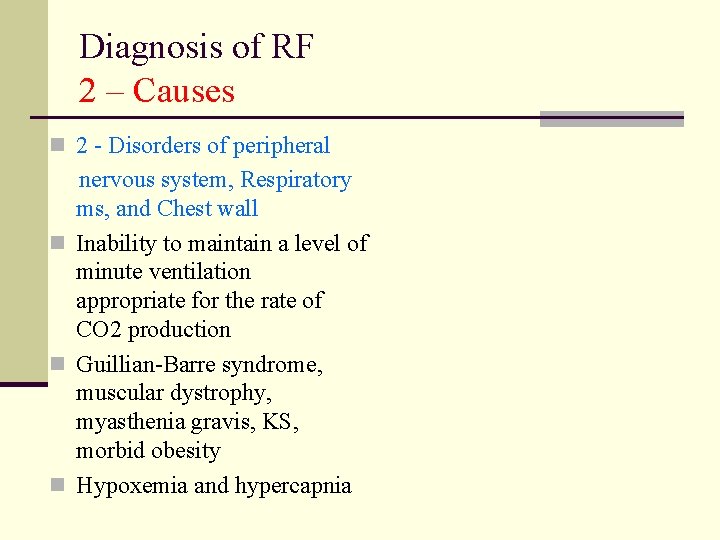
Diagnosis of RF 2 – Causes n 2 - Disorders of peripheral nervous system, Respiratory ms, and Chest wall n Inability to maintain a level of minute ventilation appropriate for the rate of CO 2 production n Guillian-Barre syndrome, muscular dystrophy, myasthenia gravis, KS, morbid obesity n Hypoxemia and hypercapnia
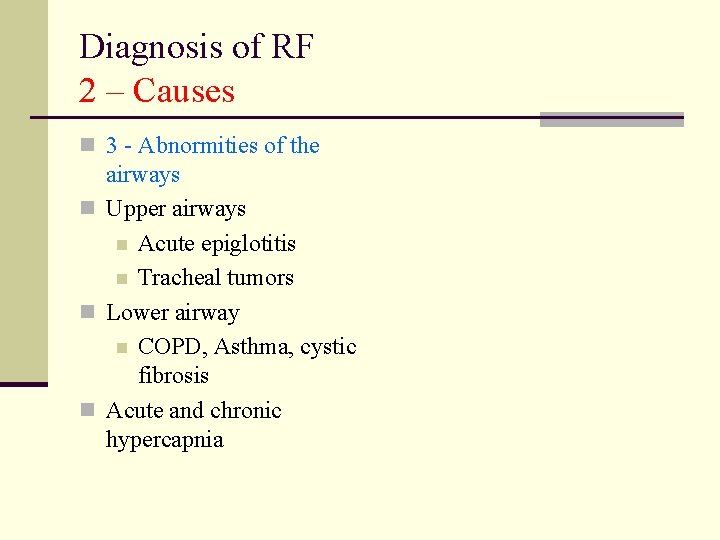
Diagnosis of RF 2 – Causes n 3 - Abnormities of the airways n Upper airways n Acute epiglotitis n Tracheal tumors n Lower airway n COPD, Asthma, cystic fibrosis n Acute and chronic hypercapnia
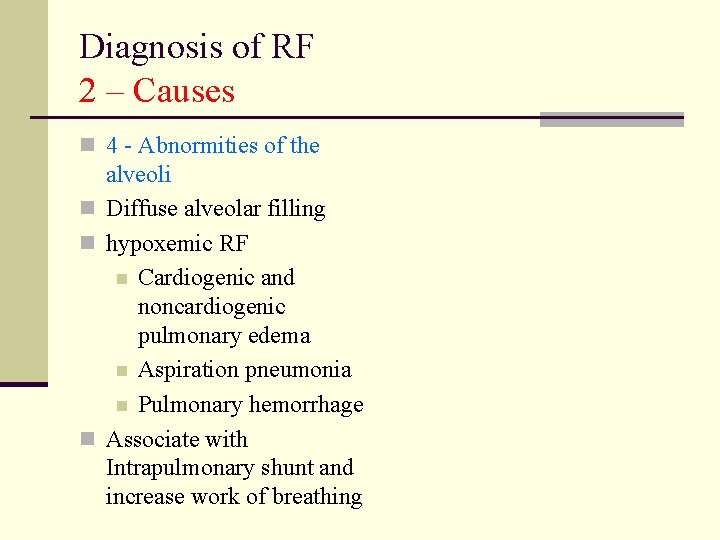
Diagnosis of RF 2 – Causes n 4 - Abnormities of the alveoli n Diffuse alveolar filling n hypoxemic RF n Cardiogenic and noncardiogenic pulmonary edema n Aspiration pneumonia n Pulmonary hemorrhage n Associate with Intrapulmonary shunt and increase work of breathing
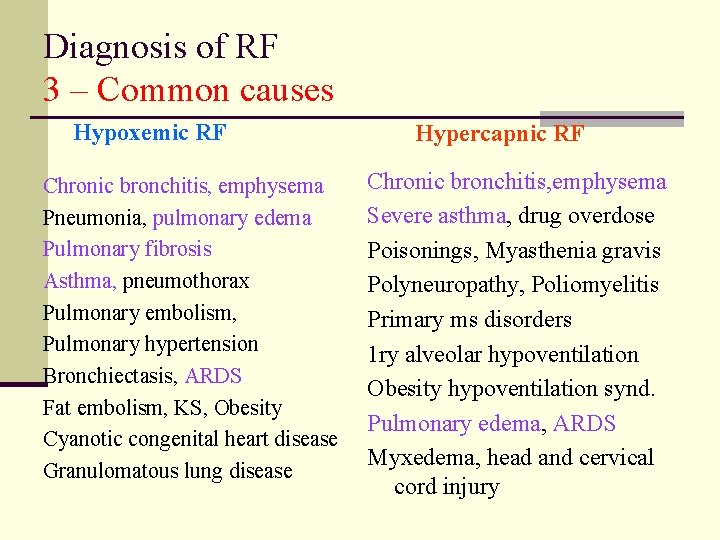
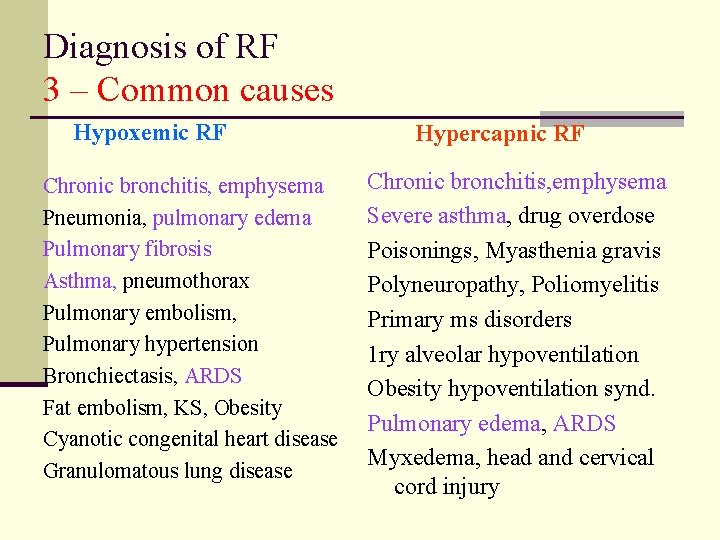
Diagnosis of RF 3 – Common causes Hypoxemic RF Chronic bronchitis, emphysema Pneumonia, pulmonary edema Pulmonary fibrosis Asthma, pneumothorax Pulmonary embolism, Pulmonary hypertension Bronchiectasis, ARDS Fat embolism, KS, Obesity Cyanotic congenital heart disease Granulomatous lung disease Hypercapnic RF Chronic bronchitis, emphysema Severe asthma, drug overdose Poisonings, Myasthenia gravis Polyneuropathy, Poliomyelitis Primary ms disorders 1 ry alveolar hypoventilation Obesity hypoventilation synd. Pulmonary edema, ARDS Myxedema, head and cervical cord injury
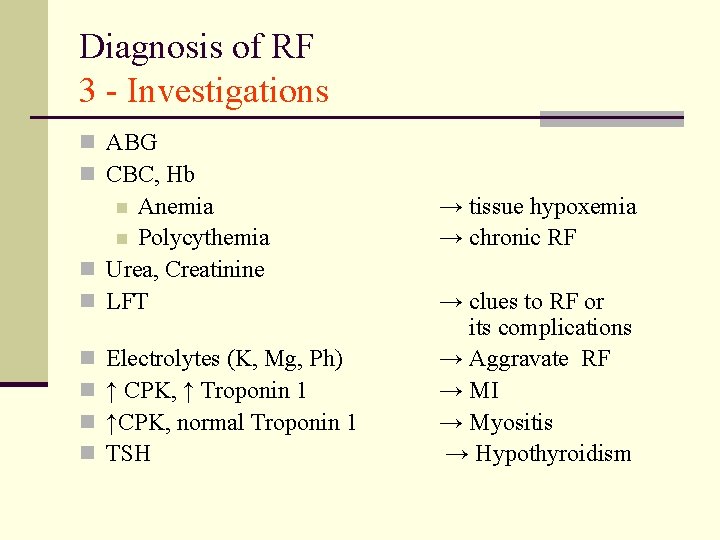
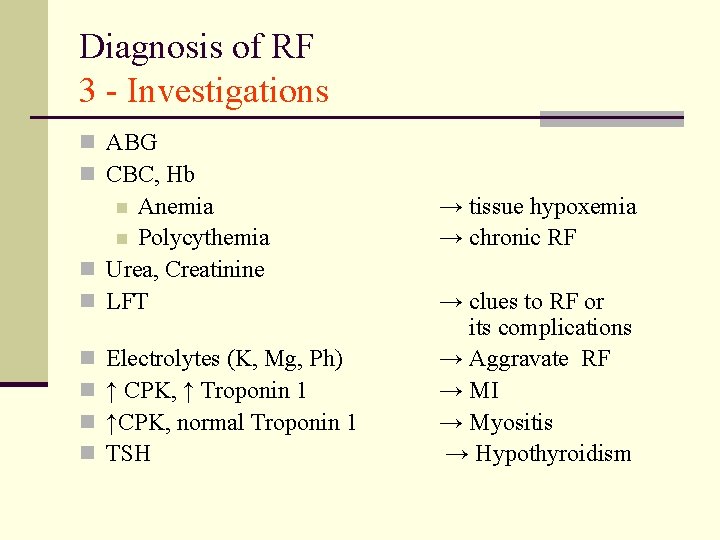
Diagnosis of RF 3 - Investigations n ABG n CBC, Hb Anemia n Polycythemia n Urea, Creatinine n LFT n n n Electrolytes (K, Mg, Ph) ↑ CPK, ↑ Troponin 1 ↑CPK, normal Troponin 1 TSH → tissue hypoxemia → chronic RF → clues to RF or its complications → Aggravate RF → MI → Myositis → Hypothyroidism
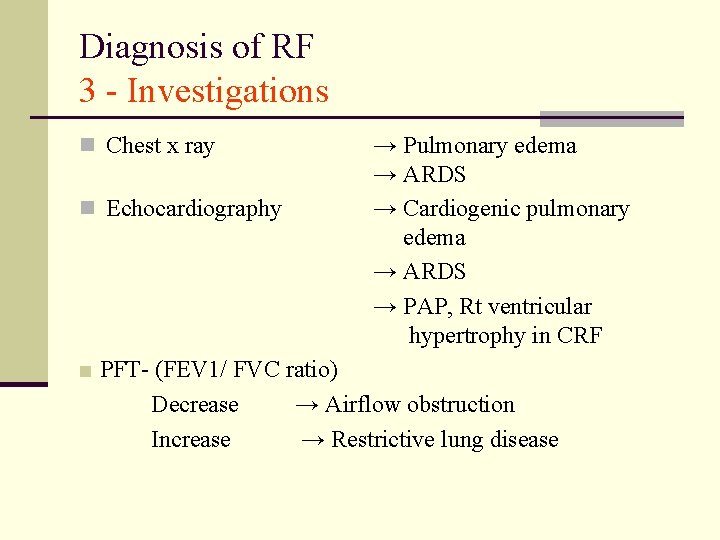
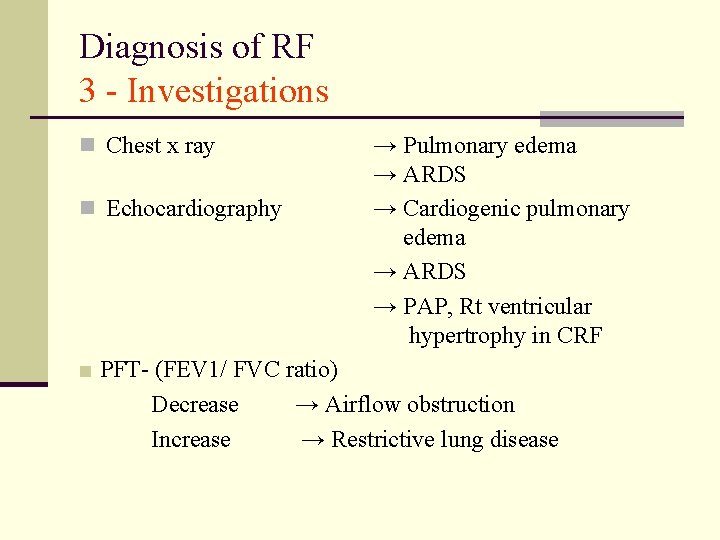
Diagnosis of RF 3 - Investigations n Chest x ray n Echocardiography → Pulmonary edema → ARDS → Cardiogenic pulmonary edema → ARDS → PAP, Rt ventricular hypertrophy in CRF ■ PFT- (FEV 1/ FVC ratio) Decrease → Airflow obstruction Increase → Restrictive lung disease
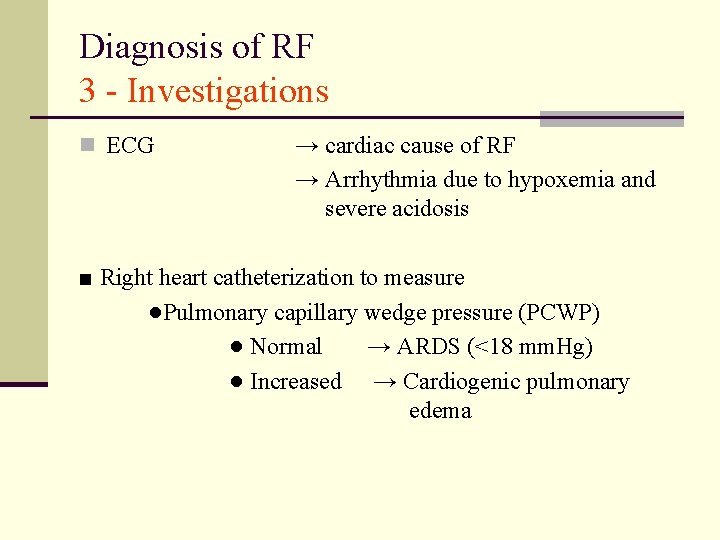
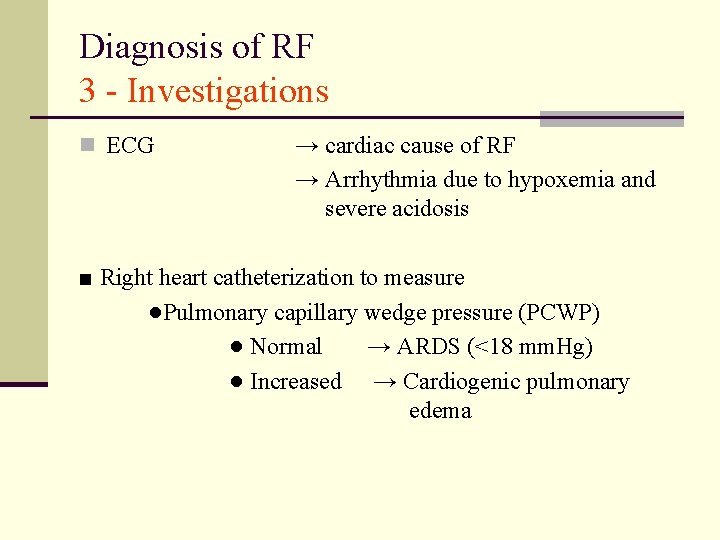
Diagnosis of RF 3 - Investigations n ECG → cardiac cause of RF → Arrhythmia due to hypoxemia and severe acidosis ■ Right heart catheterization to measure ●Pulmonary capillary wedge pressure (PCWP) ● Normal → ARDS (<18 mm. Hg) ● Increased → Cardiogenic pulmonary edema
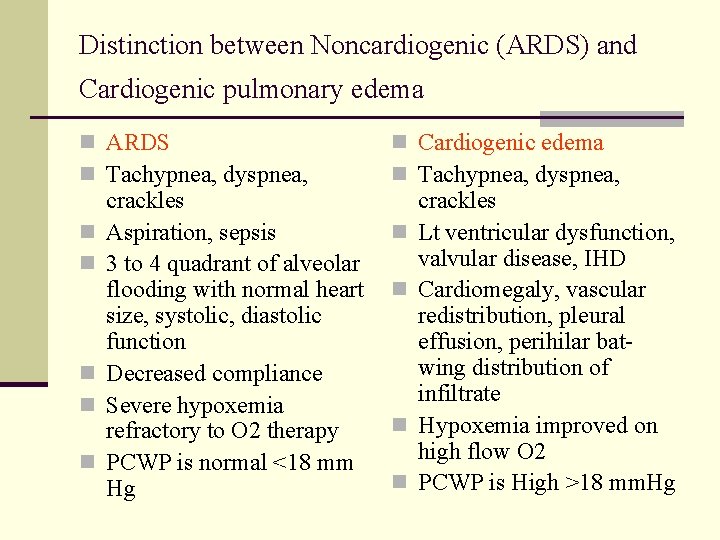
Distinction between Noncardiogenic (ARDS) and Cardiogenic pulmonary edema Pulmonary edema ARDS
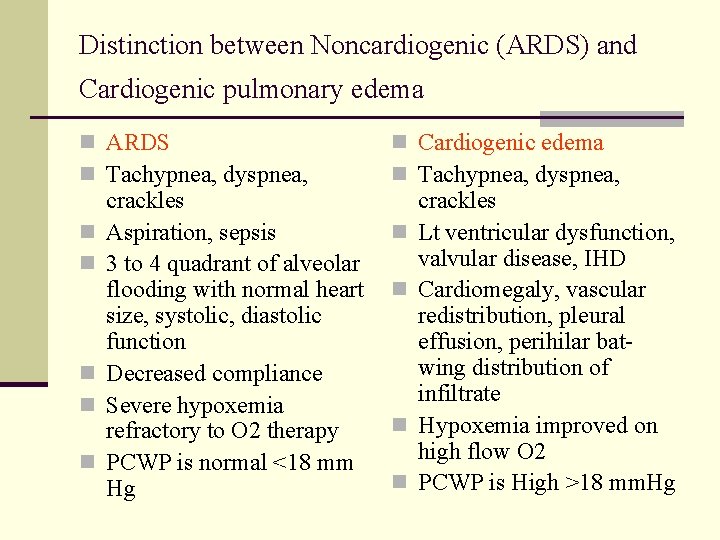
Distinction between Noncardiogenic (ARDS) and Cardiogenic pulmonary edema n ARDS n Tachypnea, dyspnea, n Cardiogenic edema n Tachypnea, dyspnea, n n n crackles Aspiration, sepsis 3 to 4 quadrant of alveolar flooding with normal heart size, systolic, diastolic function Decreased compliance Severe hypoxemia refractory to O 2 therapy PCWP is normal <18 mm Hg n n n crackles Lt ventricular dysfunction, valvular disease, IHD Cardiomegaly, vascular redistribution, pleural effusion, perihilar batwing distribution of infiltrate Hypoxemia improved on high flow O 2 PCWP is High >18 mm. Hg
Management of ARF
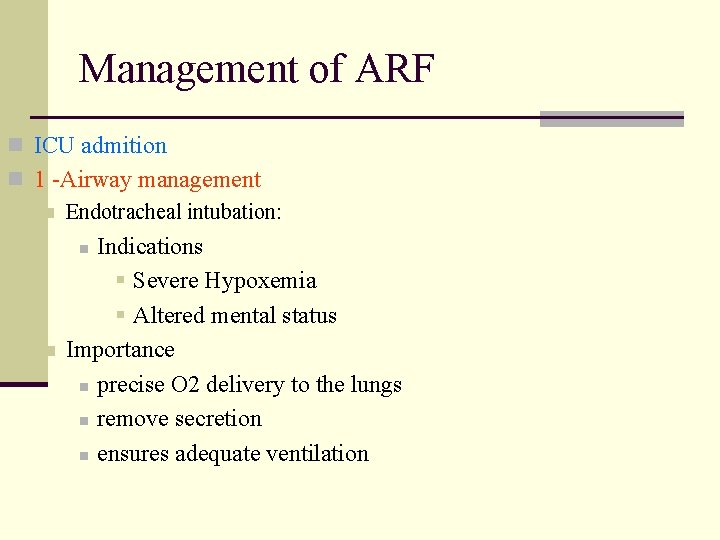
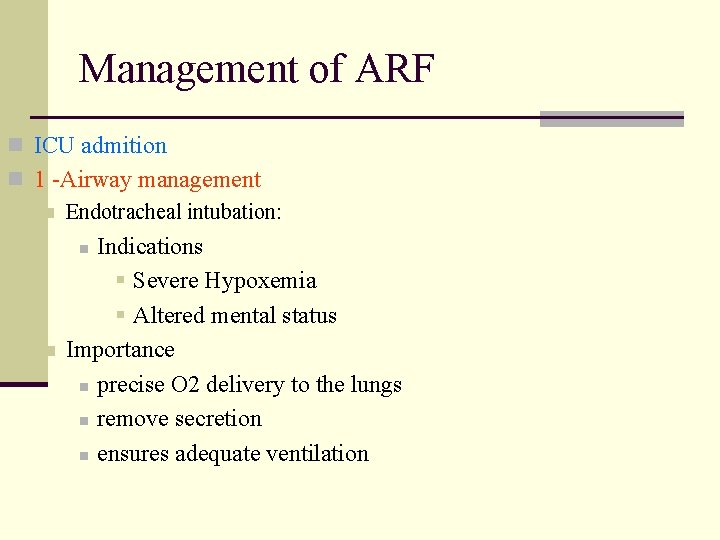
Management of ARF n ICU admition n 1 -Airway management n Endotracheal intubation: Indications § Severe Hypoxemia § Altered mental status Importance n precise O 2 delivery to the lungs n remove secretion n ensures adequate ventilation n n

Management of ARF n 2 -Correction of hypoxemia n n O 2 administration via nasal prongs, face mask, intubation and Mechanical ventilation Goal: Adequate O 2 delivery to tissues Pa. O 2 = > 60 mm. Hg Arterial O 2 saturation >90%
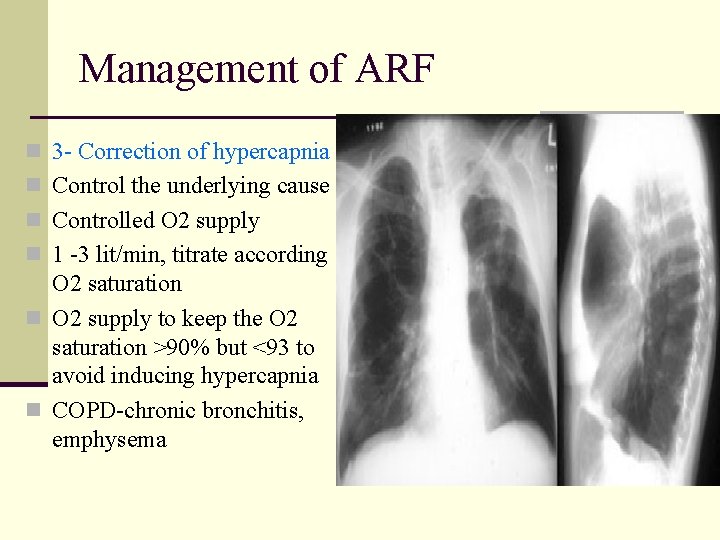
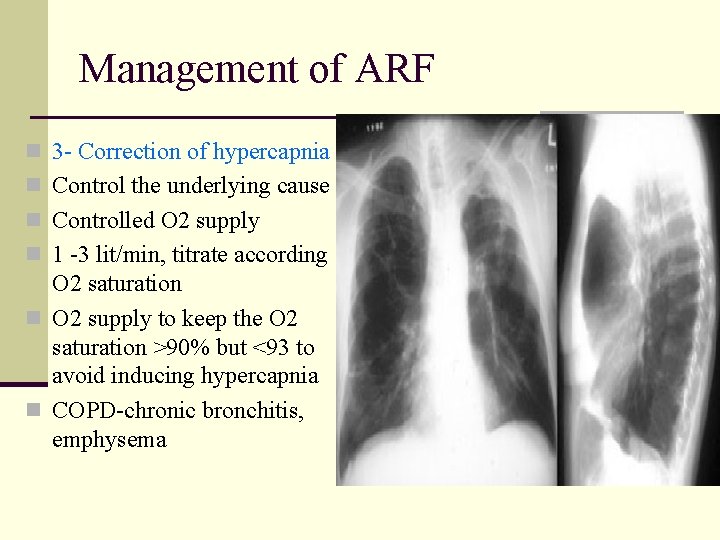
Management of ARF n 3 - Correction of hypercapnia n Control the underlying cause n Controlled O 2 supply n 1 -3 lit/min, titrate according O 2 saturation n O 2 supply to keep the O 2 saturation >90% but <93 to avoid inducing hypercapnia n COPD-chronic bronchitis, emphysema
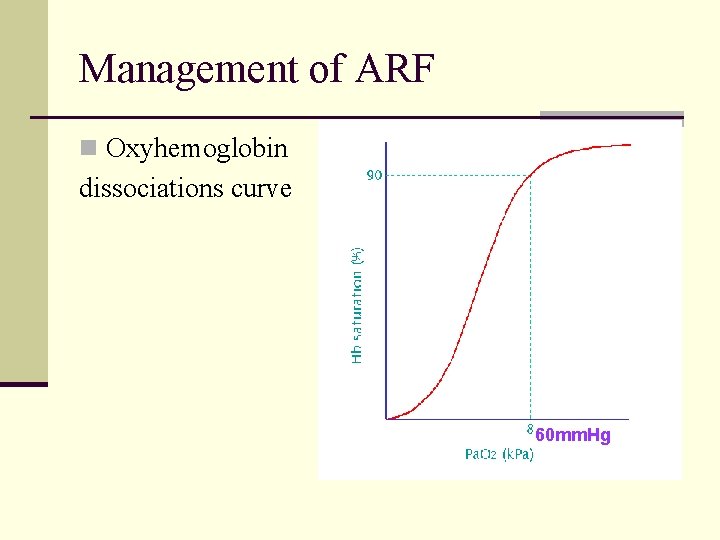
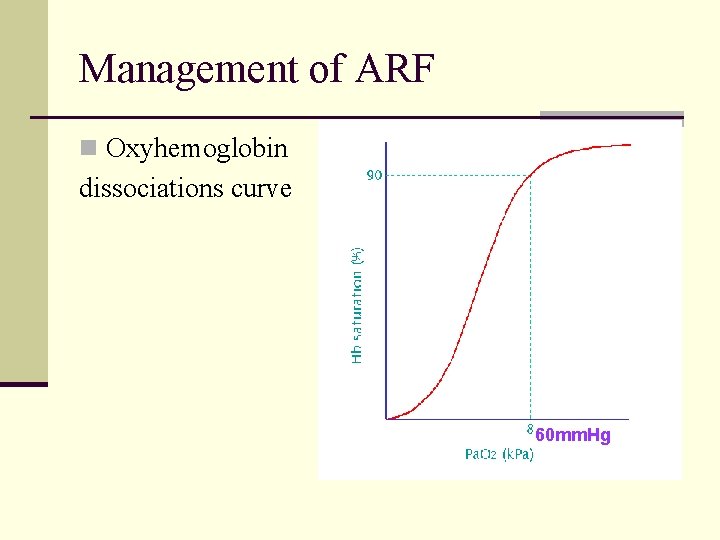
Management of ARF n Oxyhemoglobin dissociations curve 60 mm. Hg
Management of ARF n 4 – Mechanical ventilation n Indications n n n Persistence hypoxemia despite O 2 supply Decreased level of consciousness Hypercapnia with severe acidosis (p. H< 7. 2)
Management of ARF n 4 - Mechanical ventilation n Increase Pa. O 2 n Lower Pa. CO 2 n Rest respiratory ms (respiratory ms fatigue) n n Ventilator n Assists or controls the patient breathing The lowest FIO 2 that produces Sa. O 2 >90% and PO 2 >60 mm. Hg should be given to avoid O 2 toxicity
Management of ARF n 5 -PEEP (positive End- Expiratory pressure n Used with mechanical ventilation Increase intrathoracic pressure n Keeps the alveoli open n Decrease shunting n Improve gas exchange n Hypoxemic RF (type 1) n ARDS n Pneumonias n
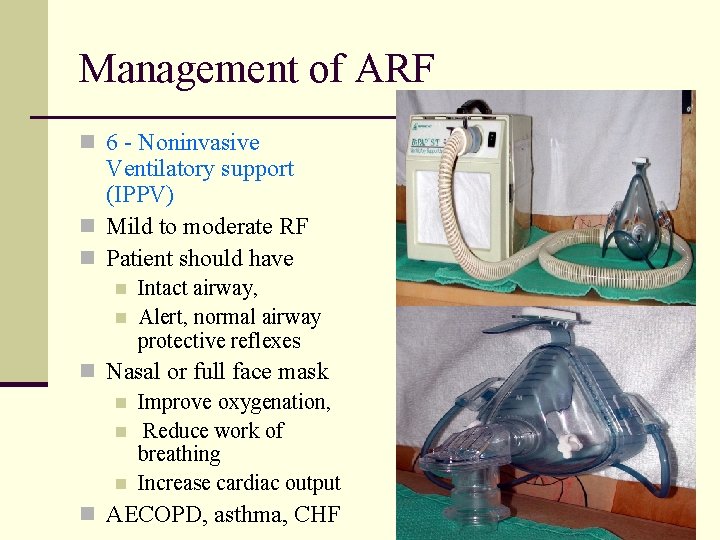
Management of ARF n 6 - Noninvasive Ventilatory support (IPPV) n Mild to moderate RF n Patient should have n n Intact airway, Alert, normal airway protective reflexes n Nasal or full face mask n Improve oxygenation, n Reduce work of breathing n Increase cardiac output n AECOPD, asthma, CHF
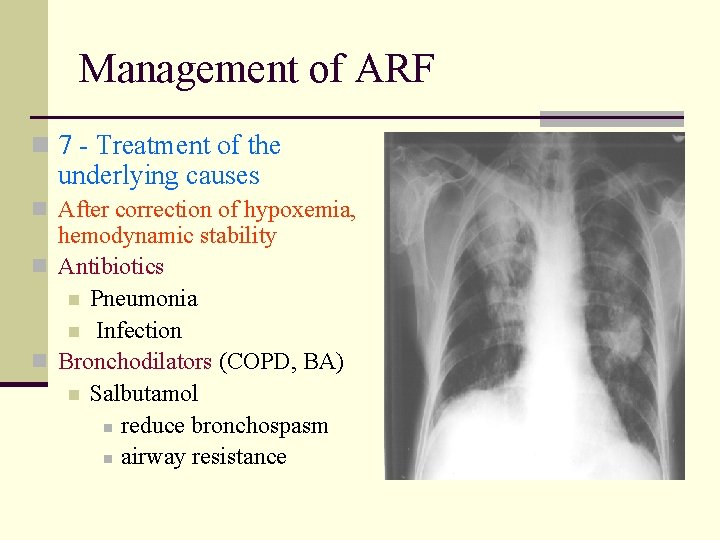
Management of ARF n 7 - Treatment of the underlying causes n After correction of hypoxemia, hemodynamic stability n Antibiotics n Pneumonia n Infection n Bronchodilators (COPD, BA) n Salbutamol n reduce bronchospasm n airway resistance
Management of ARF n 7 - Treatment of the underlying causes n Anticholinergics (COPD, BA) Ibratropium bromide n inhibit vagal tone n relax smooth ms n Theophylline (COPD, BA) n improve diaphragmatic contraction n relax smooth ms n Diuretics (pulmonary edema) n Frusemide, Metalzone n
Management of ARF n 7 - Treatment of the underlying causes n Methyl prednisone (COPD, BA, acute esinophilic pn) n Reverse bronchospasm, inflammation n Fluids and electrolytes n Maintain fluid balance and avoid fluid overload n IV nutritional support n To restore strength, loss of ms mass n Fat, carbohydrate, protein
Management of ARF n 7 - Treatment of the underlying causes n Physiotherapy n n n Chest percussion to loosen secretion Suction of airways Help to drain secretion Maintain alveolar inflation Prevent atelectasis, help lung expansion
Management of ARF n 8 - Weaning from mechanical ventilation n n Stable underlying respiratory status Adequate oxygenation Intact respiratory drive Stable cardiovascular status Patient is a wake, has good nutrition, able to cough and breath deeply

Complications of ARF n Pulmonary n Infections Pulmonary embolism n barotrauma n pulmonary fibrosis (ARDS) n Nosocomial pneumonia n Cardiovascular n Hypotension, ↓COP n Arrhythmia n MI, pericarditis n GIT n Stress ulcer, ileus, diarrhea, hemorrhage Nosocomial infection n Pneumonia, UTI, catheter related sepsis n Renal n ARF (hypoperfusion, nephrotoxic drugs) n Poor prognosis n Nutritional n Malnutrition, diarrhea hypoglycemia, electrolyte disturbances n n
Prognosis of ARF n Mortality rate for ARDS → 40% n Younger patient <60 has better survival rate n 75% of patient survive ARDS have impairment of pulmonary function one or more years after recovery n Mortality rate for COPD → 10% n Mortality rate increase in the presence of hepatic, cardiovascular, renal, and neurological disease

Quiz

Thank you
n Suggested text book to read n Davidson’s principle of internal medicine
 Non conducted pac ecg
Non conducted pac ecg Vvi pacemaker
Vvi pacemaker Brittle vs ductile fracture
Brittle vs ductile fracture Priyanka breathing
Priyanka breathing Laryngeal sarcoidosis symptoms
Laryngeal sarcoidosis symptoms Types of respiratory failure
Types of respiratory failure Blue bloaters vs pink puffers
Blue bloaters vs pink puffers Complications of respiratory failure
Complications of respiratory failure Patm syndrome
Patm syndrome Conducting zone of the respiratory system function
Conducting zone of the respiratory system function Omer reingold
Omer reingold Dr. omer
Dr. omer Jean monnet jean-gabriel monnet
Jean monnet jean-gabriel monnet Adalet evrenin ruhudur ömer hayyam
Adalet evrenin ruhudur ömer hayyam Omer boyaci
Omer boyaci Omer morshed
Omer morshed Dr shuab omer
Dr shuab omer Omer boyaci
Omer boyaci Victoria sece
Victoria sece Omer reingold
Omer reingold Omer jawed ghani
Omer jawed ghani What is this
What is this ömer hayyam ın yaptığı çalışmalar
ömer hayyam ın yaptığı çalışmalar Omer tripp
Omer tripp Omer tripp
Omer tripp Omer berkman
Omer berkman Pür matematik nedir
Pür matematik nedir Dr abdulkadir omer
Dr abdulkadir omer Gesda dans akademi
Gesda dans akademi Omer meroz
Omer meroz Omer yezdani
Omer yezdani Jae woo lee columbia
Jae woo lee columbia Aisha omer
Aisha omer şehit ömer halisdemir anadolu lisesi obp puanı
şehit ömer halisdemir anadolu lisesi obp puanı Jean monnet jean-gabriel monnet
Jean monnet jean-gabriel monnet Unss saint omer
Unss saint omer Omer angel
Omer angel ömer hayyam binom açılımı
ömer hayyam binom açılımı Ist ymm odası
Ist ymm odası Earthy look in chronic renal failure
Earthy look in chronic renal failure Selection criteria for international assignments
Selection criteria for international assignments Market failure quiz
Market failure quiz Crm failure case study
Crm failure case study Failure grade
Failure grade Transaminitis definition
Transaminitis definition Market failure examples
Market failure examples