PULMONARY HYPERTENSION INVASIVE MONITORING By Kimberly Napper Pulmonary
PULMONARY HYPERTENSION INVASIVE MONITORING By Kimberly Napper
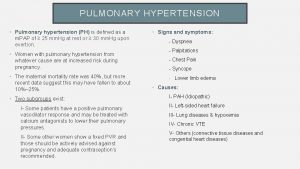
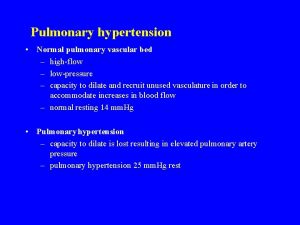
Pulmonary Hypertension p. 579 Brunner 12 th edition Abnormally high blood pressure in the arteries of the lungs. Makes the right side of the heart work harder than normal. http: //www. ncbi. nlm. nih. gov/pubmedhealth/PMH 0001171/
Pulmonary Hypertension Right side of the heart pumps blood to lungs, where it picks up oxygen. Blood returns to the left side of the heart, where it is pumped to the whole body. When the small arteries of the lung become narrowed, they cannot carry as much blood, & pressure builds up.
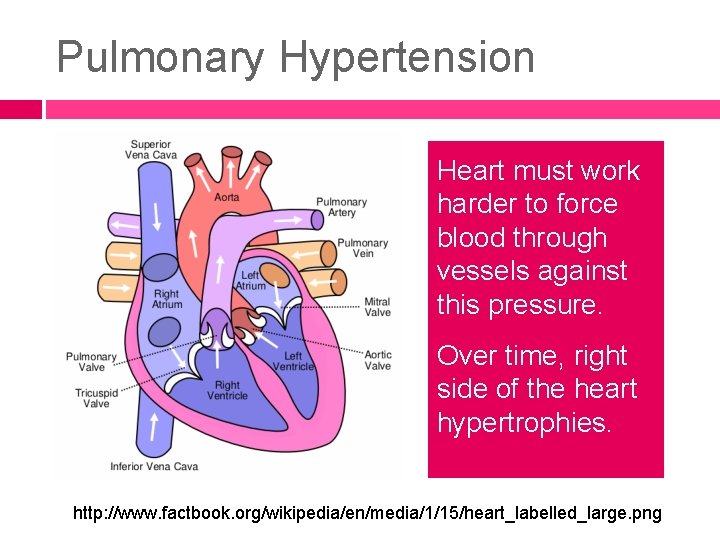
Pulmonary Hypertension Heart must work harder to force blood through vessels against this pressure. Over time, right side of the heart hypertrophies. http: //www. factbook. org/wikipedia/en/media/1/15/heart_labelled_large. png
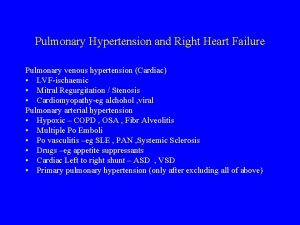
Pulmonary hypertension may be caused by: see also Chart 23 -7 Brunner 12 th ed. p. 579 Autoimmune diseases that damage the lungs � Ex. Scleroderma, rheumatoid arthritis Birth defects of the heart Pulmonary embolism Congestive heart failure Heart valve disease HIV infection Chronic Hypoxemia Lung disease, such as COPD or pulmonary fibrosis Medicines (for example, certain diet drugs) Obstructive sleep apnea
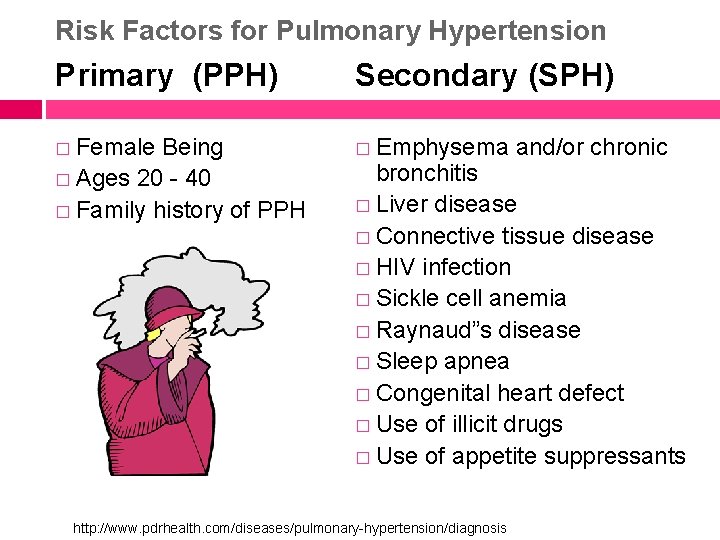
Risk Factors for Pulmonary Hypertension Primary (PPH) Secondary (SPH) � Female � Emphysema Being � Ages 20 - 40 � Family history of PPH and/or chronic bronchitis � Liver disease � Connective tissue disease � HIV infection � Sickle cell anemia � Raynaud”s disease � Sleep apnea � Congenital heart defect � Use of illicit drugs � Use of appetite suppressants http: //www. pdrhealth. com/diseases/pulmonary-hypertension/diagnosis
Pulmonary Hypertension Types Idiopathic � Cause unknown (IPAH) � Formerly called primary pulmonary hypertension (PPH). � IPAH is rare � Affects more women than men. Secondary � Caused by a known medicine or medical condition http: //www. ncbi. nlm. nih. gov/pubmedhealth/PMH 0001171/
Pulmonary Hypertension S/S Shortness of breath or light-headedness during activity is often the first symptom Ankle and leg swelling Bluish color of the lips or skin (cyanosis) Chest pain or pressure, usually in the front of the chest Dizziness or fainting spells Fatigue Increased abdomen size Weakness
Pulmonary Hypertension S/S Murmur on right side of heart Distended neck veins Leg swelling Hepatosplenomegaly (liver & spleen swelling) Normal breath sounds (Sounds like right-sided CHF? ? ? )
“Cor Pulmonale” see p. 581 Brunner 12 th Latin: cor = heart + New Latin: pulmōnāle = of the lungs Pulmonary heart disease: enlargement of the right ventricle of the heart due to increased resistance or high blood pressure in the lungs To be classified as cor pulmonale, the cause must originate in the pulmonary circulation system. http: //en. wikipedia. org/wiki/Cor_pulmonale
“Cor Pulmonale” Acute usually results in dilatation Chronic usually results in right ventricular hypertrophy (RVH)
Acute Cor Pulmonale Dilatation is a stretching (in length) of the ventricle in response to acute increased pressure, such as when caused by a pulmonary embolism.
Chronic Cor Pulmonale Hypertrophy is an adaptive response to a longterm increase in pressure. Individual muscle cells grow larger/thicker and change to drive the increased contractile force required to move the blood against greater resistance. http: //en. wikipedia. org/wiki/Cor_pulmonale
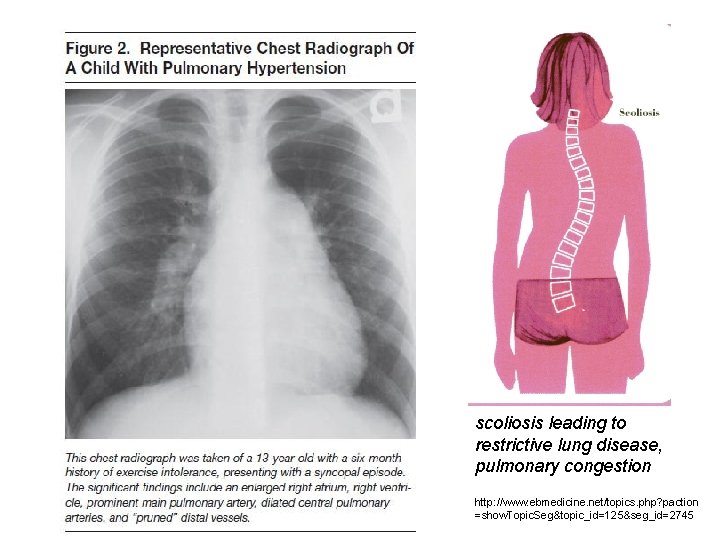
scoliosis leading to restrictive lung disease, pulmonary congestion http: //www. ebmedicine. net/topics. php? paction =show. Topic. Seg&topic_id=125&seg_id=2745
Pulmonary Hypertension No known cure Goal of treatment is to control symptoms and prevent more lung damage Important to treat medical disorders that cause pulmonary hypertension � Ex. obstructive sleep apnea, lung conditions, and heart valve disorders. http: //www. ncbi. nlm. nih. gov/pubmedhealth/PMH 0001171/
Tests R/T Pulmonary Hypertension Chest x-ray Lung function tests ECG Echocardiogram Nuclear lung scan CT scan of the chest Cardiac catheterization Pulmonary arteriogram
Tests R/T Pulmonary Hypertension Sleep study HIV test Blood tests for autoantibodies � ANA (antinuclear antibody) � ANCA (anti-neutrophilic cytoplasmic antibodies) � RF (rheumatoid factor ) � CRP (C-reactive protein )
Goals of treatment Dilate pulmonary vessels Decrease thickening of blood Decrease preload on heart Increase oxygen supply to lungs Prevention and treatment of respiratory infection Increase cardiac output Treat cause of secondary Pulmonary hypertension. http: //www. highbloodpressuremed. com/role-of-viagra-sildenafil-in-pulmonary-hypertension. html
Medications for Pulmonary Hypertension Anticoagulants Oxygen Calcium channel blockers � Cardizem (diltiazem), Procardia (nifedipine) � Avoid grapefruit or grapefruit juice Diuretics
Medications for Pulmonary Hypertension Endothelin Receptor Antagonists � Letairis (ambrisentan) � Tracleer (bosentan) May damage the liver; may cause birth defects Prostaglandin (prostacyclin) � potent vasodilator � inhibits platelet aggregation � can be given orally, subcutaneously, intravenously or inhaled via a nebulizer
Medications for Pulmonary Hypertension PDE 5 -inhibitor � Viagra (sildenafil citrate) Pfizer repackaged Viagra's key ingredient (sildenafil) and markets it as Revatio. � Do not take with nitrates!! � Most common side effects: headache, indigestion, flushing, insomnia, and nosebleeds.
Pulmonary Hypertension Dx Right-side heart catheterization to diagnose elevated pulmonary arterial pressure � Catheter passed into heart by way of antecubital or femerol vein → right atrium→ right ventricle → pulmonary artery (PA) →pulmonary arterioles (different from left-side cath, which is entered through right brachial artery or femoral artery) � p. 716 Brunner 12 th ed
Persistant Pulmonary Hypertension of the Newborn (PPHN) failure of the normal circulatory transition that occurs after birth a syndrome characterized by marked pulmonary hypertension that causes hypoxemia and right-to-left extrapulmonary shunting of blood. http: //emedicine. medscape. com/article/898437 -overview
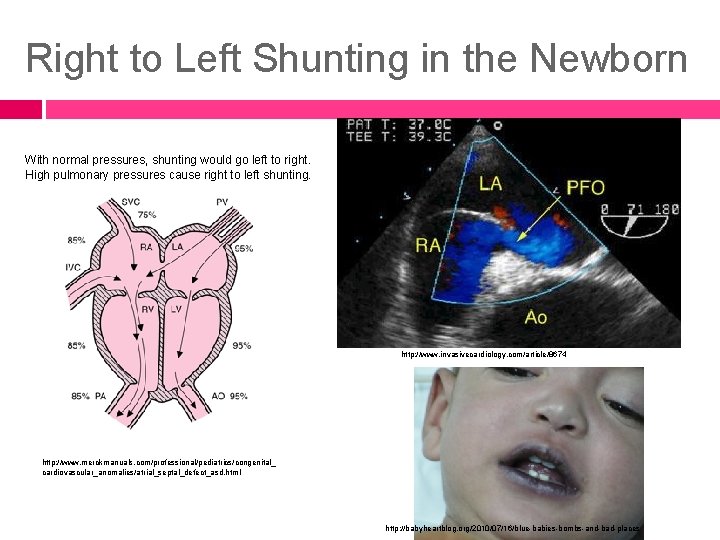
Right to Left Shunting in the Newborn With normal pressures, shunting would go left to right. High pulmonary pressures cause right to left shunting. http: //www. invasivecardiology. com/article/8674 http: //www. merckmanuals. com/professional/pediatrics/congenital_ cardiovascular_anomalies/atrial_septal_defect_asd. html http: //babyheartblog. org/2010/07/16/blue-babies-bombs-and-bad-places
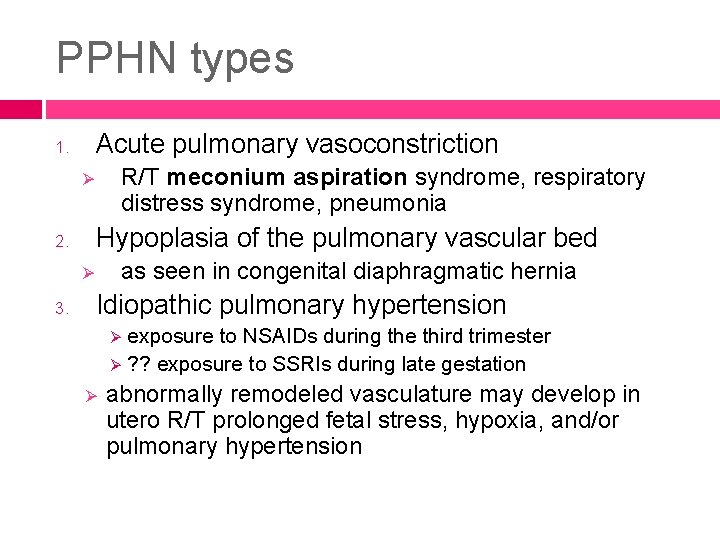
PPHN types Acute pulmonary vasoconstriction 1. R/T meconium aspiration syndrome, respiratory distress syndrome, pneumonia Ø Hypoplasia of the pulmonary vascular bed 2. as seen in congenital diaphragmatic hernia Ø 3. Idiopathic pulmonary hypertension exposure to NSAIDs during the third trimester Ø ? ? exposure to SSRIs during late gestation Ø Ø abnormally remodeled vasculature may develop in utero R/T prolonged fetal stress, hypoxia, and/or pulmonary hypertension
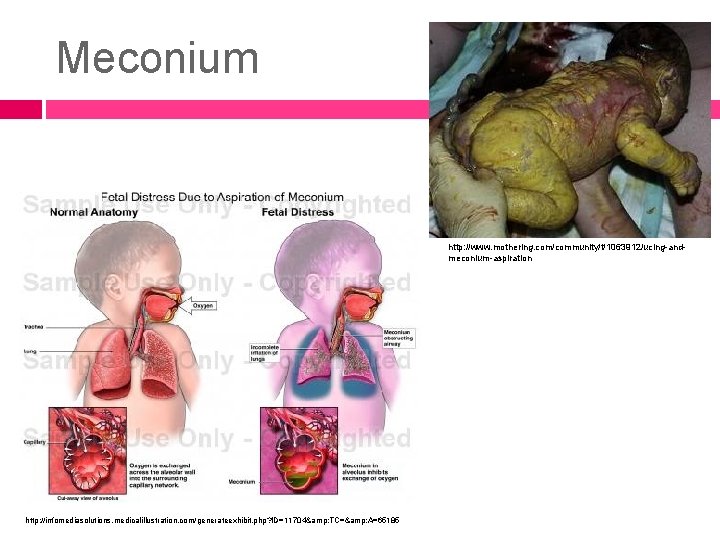
Meconium http: //www. mothering. com/community/t/1063912/ucing-andmeconium-aspiration http: //infomediasolutions. medicalillustration. com/generateexhibit. php? ID=11704& TC=& A=65185
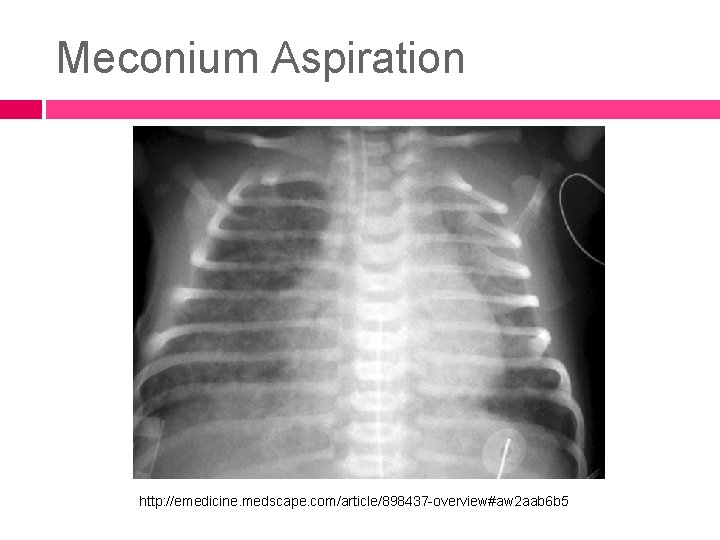
Meconium Aspiration http: //emedicine. medscape. com/article/898437 -overview#aw 2 aab 6 b 5
Care of Infant with PPHN Use a minimal stimulation protocol to minimize the need to handle the patient and to perform invasive procedures, such as suctioning.
Care of Infant with PPHN Endotracheal intubation and mechanical ventilation are almost always necessary for the newborn with persistent pulmonary hypertension of the newborn (PPHN).
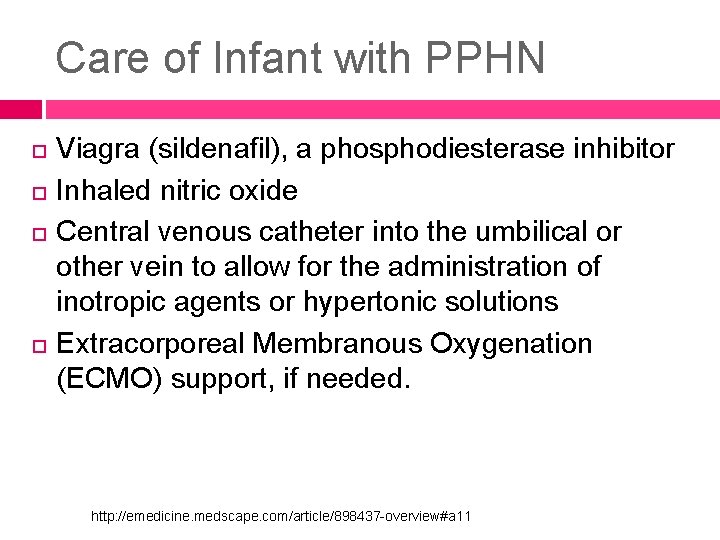
Care of Infant with PPHN Viagra (sildenafil), a phosphodiesterase inhibitor Inhaled nitric oxide Central venous catheter into the umbilical or other vein to allow for the administration of inotropic agents or hypertonic solutions Extracorporeal Membranous Oxygenation (ECMO) support, if needed. http: //emedicine. medscape. com/article/898437 -overview#a 11
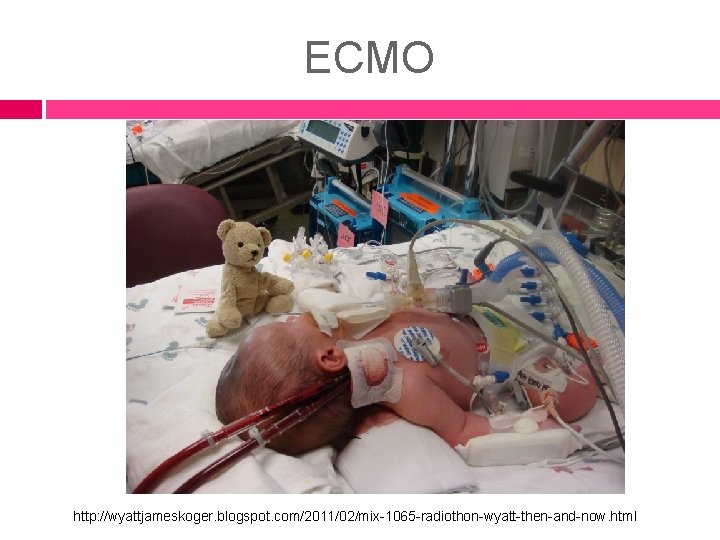
ECMO http: //wyattjameskoger. blogspot. com/2011/02/mix-1065 -radiothon-wyatt-then-and-now. html
How to Give Oral Medication to an Infant � Aim the medicine toward the back near the gums or cheeks, but not at the back of the tongue. � Squirt medicine into the mouth in small amounts. or � Place a clean nipple into the baby's mouth and then put the medicine into the nipple and let the baby suck the medicine through the nipple. http: //www. ehow. com/how_2068060_give-baby-medicine. html Also, look in Wong p. 718 -719 re: oral medication administration for infants.

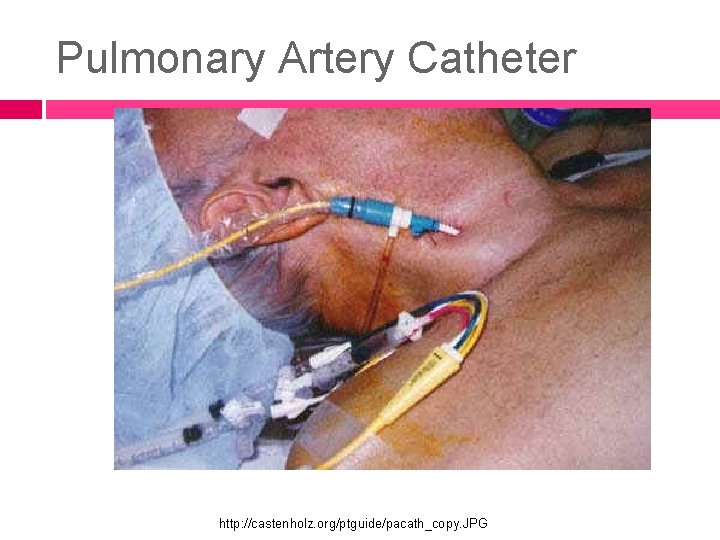
Pulmonary Artery Catheter http: //castenholz. org/ptguide/pacath_copy. JPG
Central Venous Catheters Usually inserted into the subclavian or jugular vein with the distal tip just above the right atrium May be inserted at the bedside May be surgically inserted for longer term access A “PA” catheter is a special type needed to measure pulmonary artery “wedge” pressures & cardiac output � “Swan-Ganz” catheter used as “central line”
Indications for a PA line (pulmonary artery catheter) Diagnostic Diagnosis of shock states � Differentiation of high- versus low-pressure pulmonary edema � Diagnosis of idiopathic pulmonary hypertension � Diagnosis of valvular disease, intracardiac shunts, cardiac tamponade, and pulmonary embolus (PE) � Monitoring and management of complicated AMI � Assessing hemodynamic response to therapies � Management of multiorgan system failure and/or severe burns � Management of hemodynamic instability after cardiac surgery � Assessment of response to treatment in patients with idiopathic pulmonary hypertension � Therapeutic � Aspiration of air emboli http: //emedicine. medscape. com/article/1824547 -overview#a 03
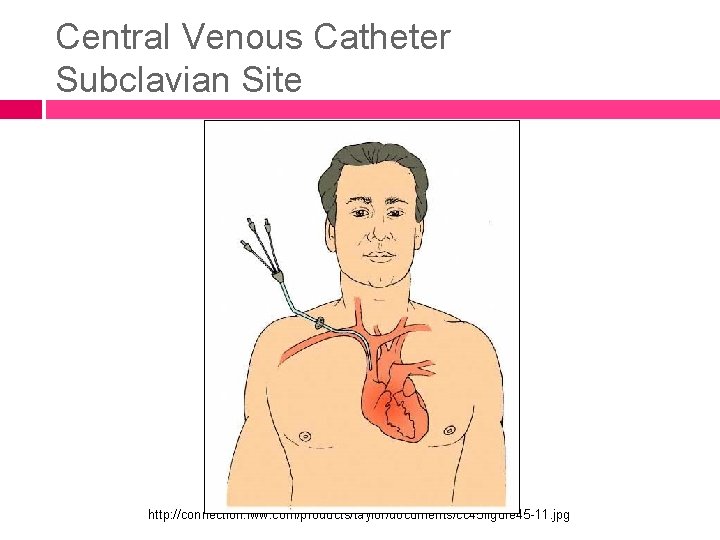
Central Venous Catheter Subclavian Site http: //connection. lww. com/products/taylor/documents/cc 45 figure 45 -11. jpg
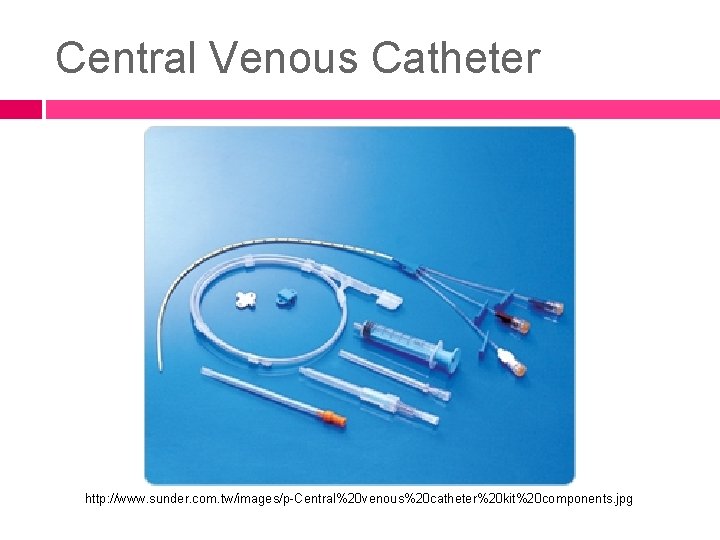
Central Venous Catheter http: //www. sunder. com. tw/images/p-Central%20 venous%20 catheter%20 kit%20 components. jpg

Jugular Site Insertion http: //www. visualsunlimited. com/images/watermarked/1002. jpg

Jugular Site with Transparent Dressing http: //www. visualsunlimited. com/images/watermarked/1000. jpg
Subclavian Site http: //www. icu-usa. com/tour/images/equipment/CVP 1. jpg
Possible Complications of CVC Pneumothorax � With insertion of line Infection at site Sepsis Bleeding Blockage of the catheter Shifting of the catheter
Pneumothorax A collection of air inside the chest, between the lung and inner chest wall, which causes the lung to collapse Diagnosed by chest x-ray Treated with chest tube S/S: � Chest pain � Shortness of breath � Rapid breathing � Chest tightness � Hypoxemia (low oxygen level in blood)
Nursing Responsibilities Assess for S/S of pneumothorax � Shortness of breath � Chest pain � Cough � Hypotension � Tachycardia � Anxiety
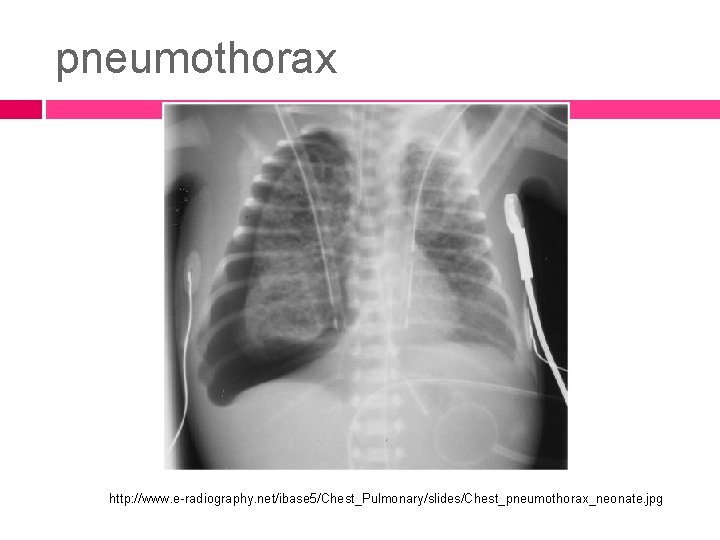
pneumothorax http: //www. e-radiography. net/ibase 5/Chest_Pulmonary/slides/Chest_pneumothorax_neonate. jpg
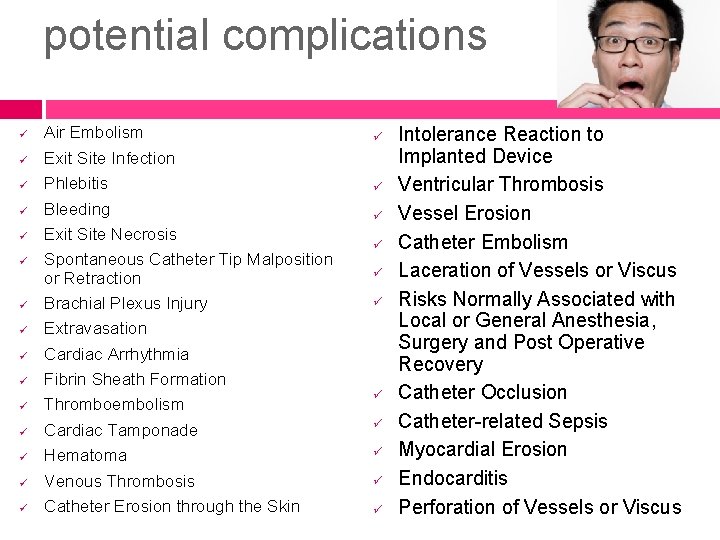
potential complications ü ü ü ü Air Embolism Exit Site Infection Phlebitis Bleeding Exit Site Necrosis Spontaneous Catheter Tip Malposition or Retraction Brachial Plexus Injury Extravasation Cardiac Arrhythmia Fibrin Sheath Formation Thromboembolism Cardiac Tamponade Hematoma Venous Thrombosis Catheter Erosion through the Skin ü ü ü Intolerance Reaction to Implanted Device Ventricular Thrombosis Vessel Erosion Catheter Embolism Laceration of Vessels or Viscus Risks Normally Associated with Local or General Anesthesia, Surgery and Post Operative Recovery Catheter Occlusion Catheter-related Sepsis Myocardial Erosion Endocarditis Perforation of Vessels or Viscus
Dressing Changes for CVC Sterile procedure is necessary!! Cleanse insertion site with appropriate agent, using a circular motion moving from center to the outside. Allow site to air dry. Cleanse catheter from site to cap. Apply appropriate dressing. Label with time, date, & initials.
Prevention of Infection Appropriate catheter and IV site care Strict sterile technique for dressing changes Wear mask when changing the dressing. Assess insertion site. Assess for indicators of infection. Proper IV and tubing care
Pulmonary Artery Catheters � Usually heparin bonded � Have similar rates of bloodstream infection as central venous catheters (CVCs) � Subclavian site preferred to reduce infection risk � Inserted through a Teflon® introducer in a central vein (subclavian, internal jugular, or femoral) � See p. 716 -718 Brunner 12 th edition PA pressure monitoring Nursing Alert box p. 717
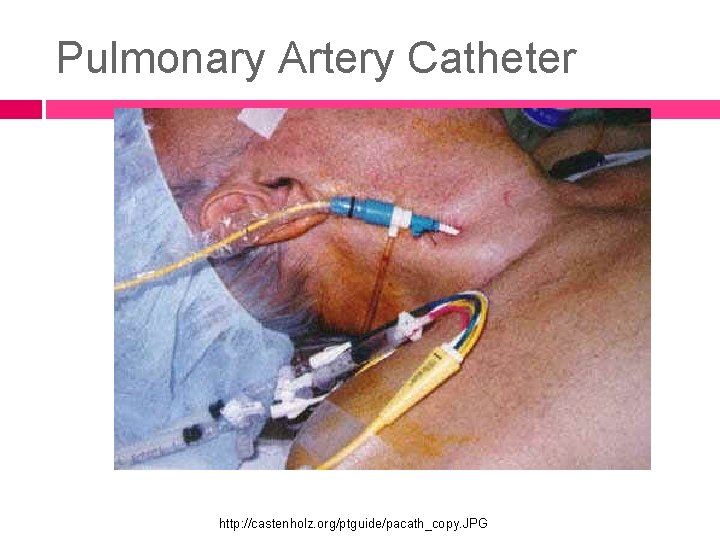
Pulmonary Artery Catheter http: //castenholz. org/ptguide/pacath_copy. JPG
Pulmonary Artery Catheter (PA) line is the most appropriate hemodynamic monitoring procedure to assess the left ventricular function of a patient �A normal PA systolic pressure ranges from 20 to 30 mm Hg and is equal to the RV systolic pressure. elevated in some high-flow states (eg, hypervolemia), left ventricular failure, and high-resistance states (eg, pulmonary hypertension, mitral valve disease) http: //emedicine. medscape. com/article/1824547 -overview#a 15
Pulmonary Artery Catheter Pulmonary Capillary Wedge Pressure (PCWP) is the measurement by which changes in lung water can be assessed. Pressures are normally 8 -10 mm. Hg. When above 20 mm. Hg, pulmonary edema is likely to be present, which is a life-threatening condition.
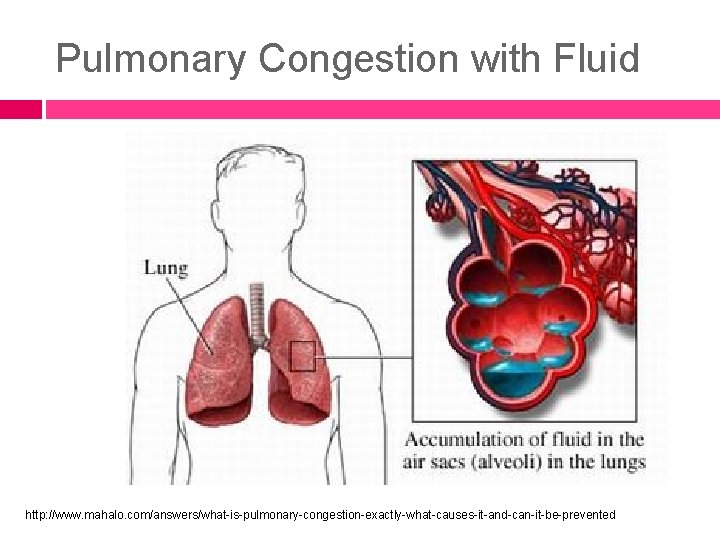
Pulmonary Congestion with Fluid http: //www. mahalo. com/answers/what-is-pulmonary-congestion-exactly-what-causes-it-and-can-it-be-prevented

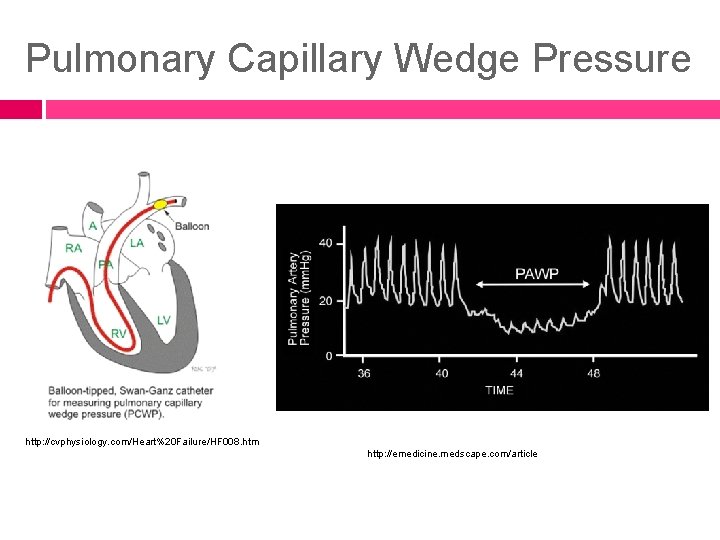
Pulmonary Capillary Wedge Pressure http: //cvphysiology. com/Heart%20 Failure/HF 008. htm http: //emedicine. medscape. com/article
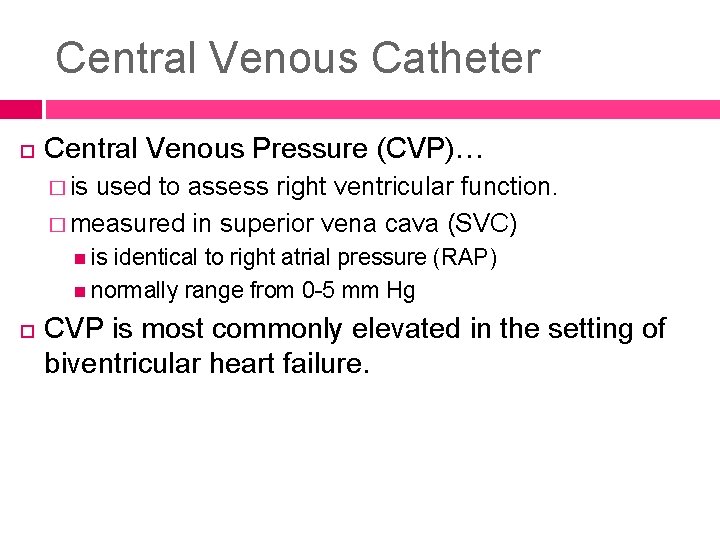
Central Venous Catheter Central Venous Pressure (CVP)… � is used to assess right ventricular function. � measured in superior vena cava (SVC) is identical to right atrial pressure (RAP) normally range from 0 -5 mm Hg CVP is most commonly elevated in the setting of biventricular heart failure.
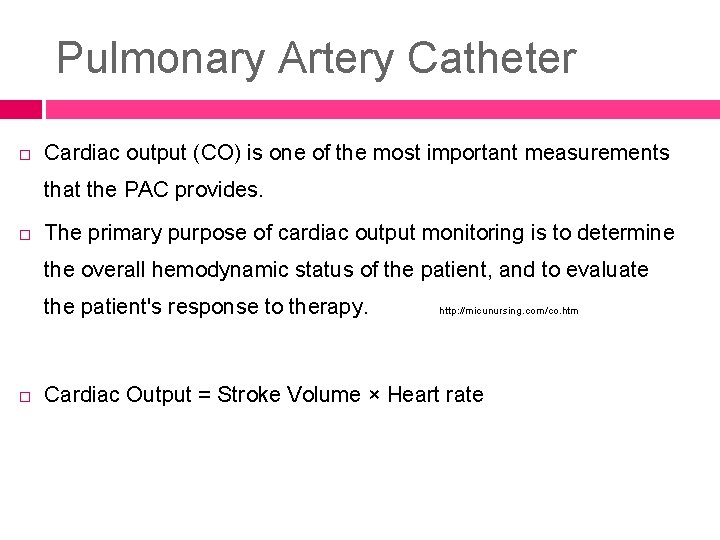
Pulmonary Artery Catheter Cardiac output (CO) is one of the most important measurements that the PAC provides. The primary purpose of cardiac output monitoring is to determine the overall hemodynamic status of the patient, and to evaluate the patient's response to therapy. http: //micunursing. com/co. htm Cardiac Output = Stroke Volume × Heart rate
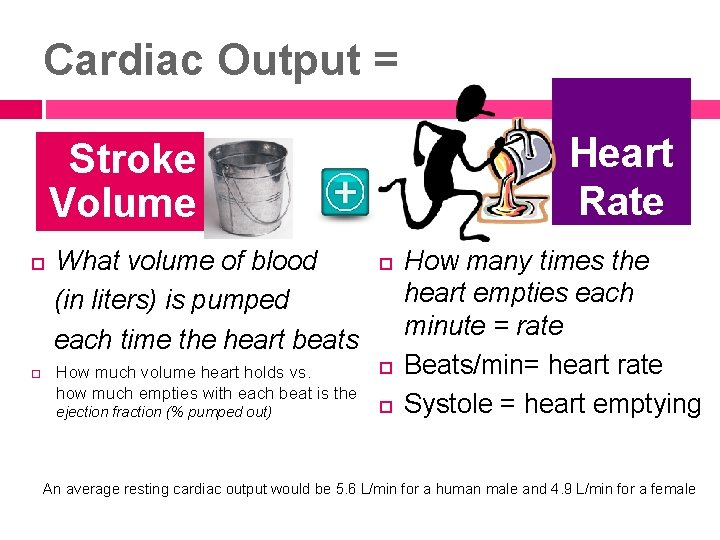
Cardiac Output = Heart Rate Stroke Volume What volume of blood (in liters) is pumped each time the heart beats How much volume heart holds vs. how much empties with each beat is the ejection fraction (% pumped out) How many times the heart empties each minute = rate Beats/min= heart rate Systole = heart emptying An average resting cardiac output would be 5. 6 L/min for a human male and 4. 9 L/min for a female
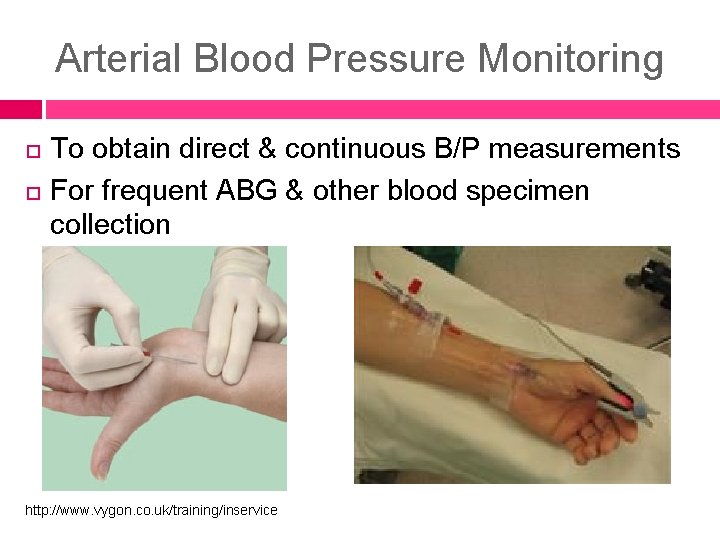
Arterial Blood Pressure Monitoring To obtain direct & continuous B/P measurements For frequent ABG & other blood specimen collection http: //www. vygon. co. uk/training/inservice

Radial Artery Line in Infant http: //www. flickr. com/photos/zippyandbaker/2763547254/
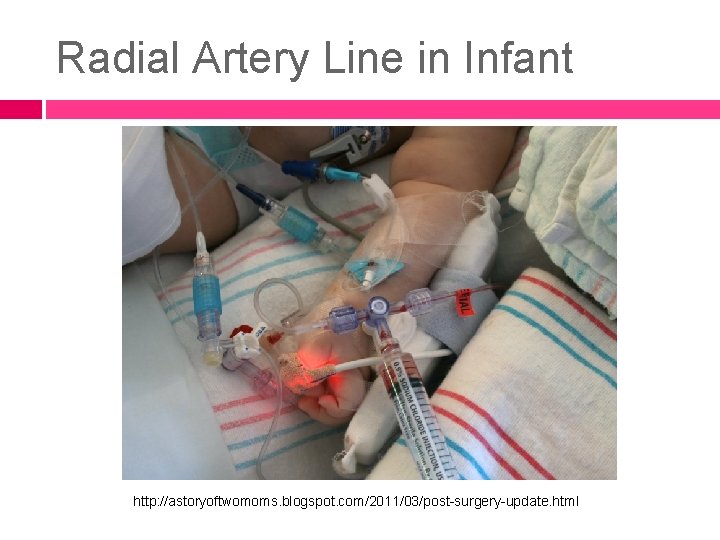
Radial Artery Line in Infant http: //astoryoftwomoms. blogspot. com/2011/03/post-surgery-update. html
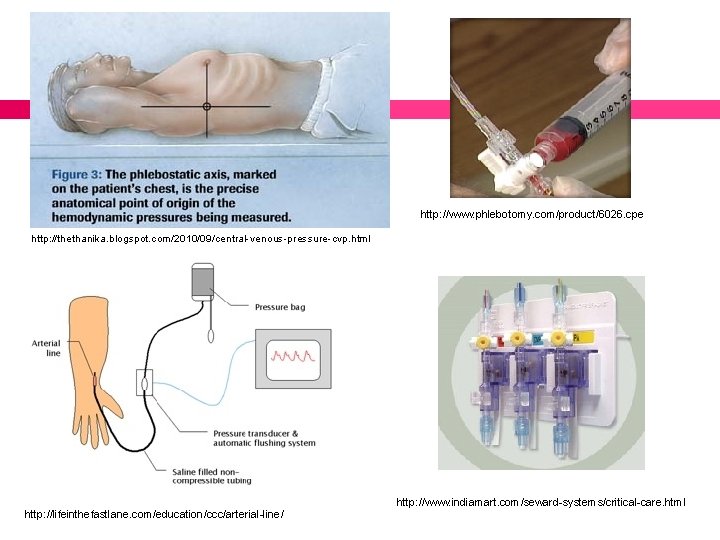
http: //www. phlebotomy. com/product/6026. cpe http: //thethanika. blogspot. com/2010/09/central-venous-pressure-cvp. html http: //lifeinthefastlane. com/education/ccc/arterial-line/ http: //www. indiamart. com/seward-systems/critical-care. html
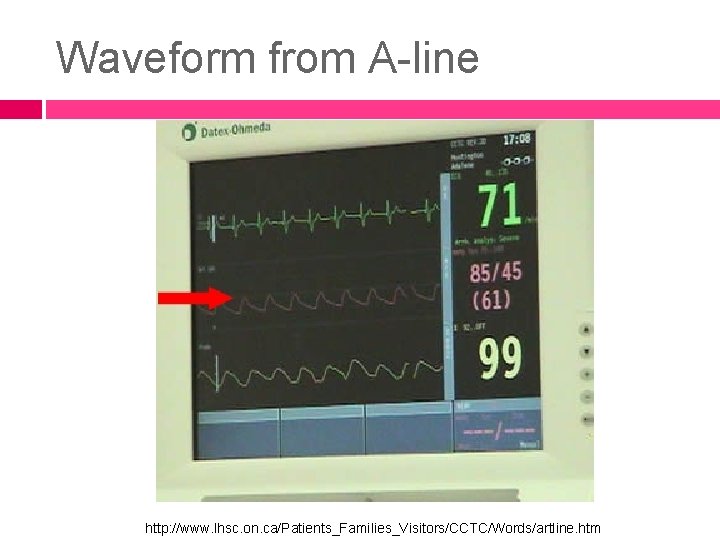
Waveform from A-line http: //www. lhsc. on. ca/Patients_Families_Visitors/CCTC/Words/artline. htm
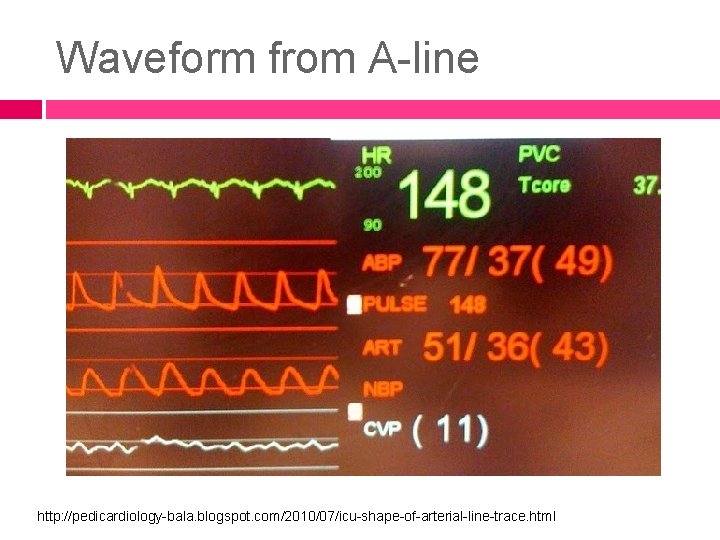
Waveform from A-line http: //pedicardiology-bala. blogspot. com/2010/07/icu-shape-of-arterial-line-trace. html
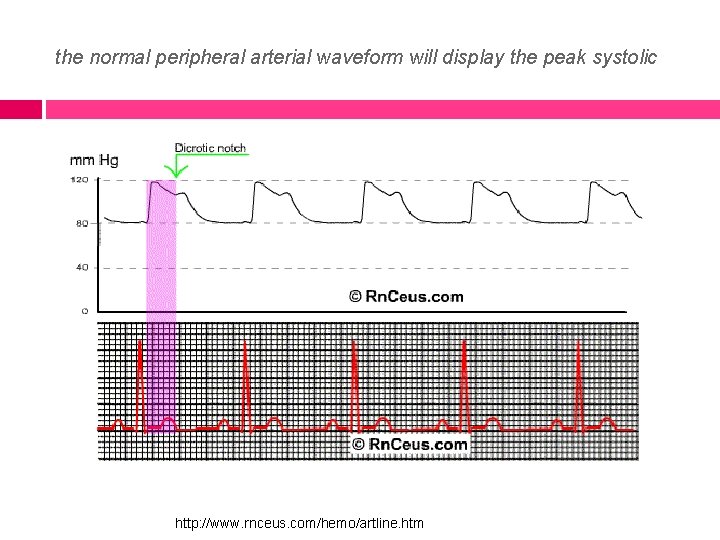
the normal peripheral arterial waveform will display the peak systolic http: //www. rnceus. com/hemo/artline. htm
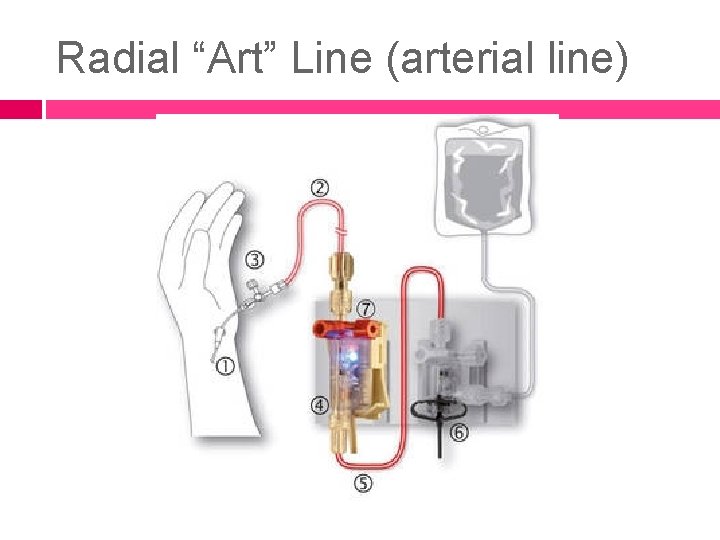
Radial “Art” Line (arterial line)
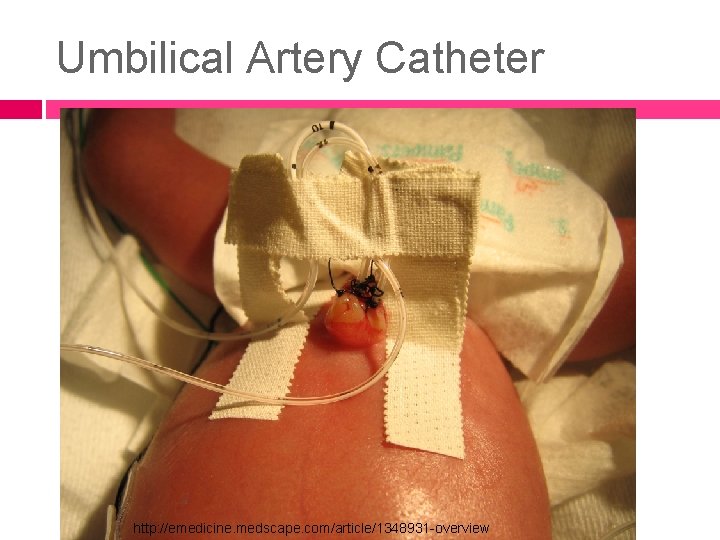
Umbilical Artery Catheter http: //emedicine. medscape. com/article/1348931 -overview
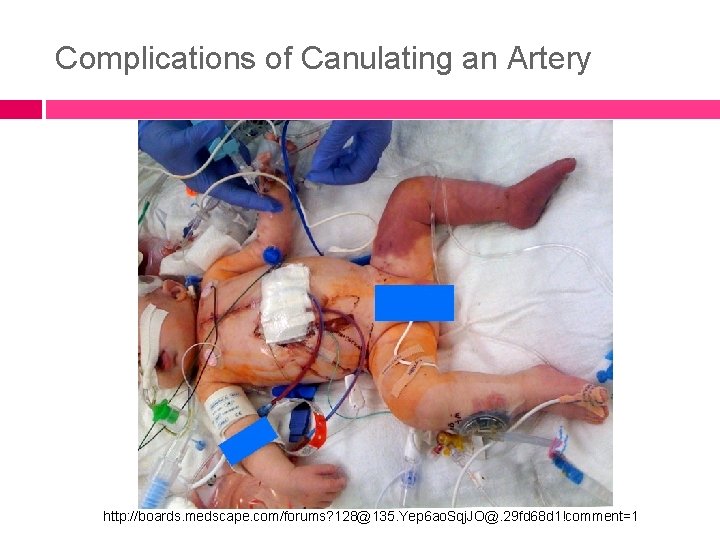
Complications of Canulating an Artery http: //boards. medscape. com/forums? 128@135. Yep 6 ao. Sqj. JO@. 29 fd 68 d 1!comment=1
A client is being assessed for his semiannual examination and you hear crackles bilaterally in his lungs. Which of the following could be a cause of crackles in the bases of his lungs? a) Pulmonary congestion b) Pulmonary hypertension c) Heart palpitations d) Mitral valve stenosis
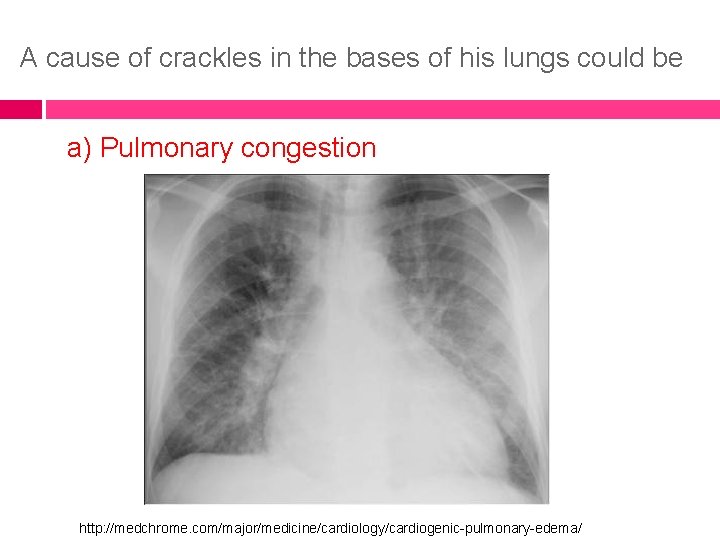
A cause of crackles in the bases of his lungs could be a) Pulmonary congestion http: //medchrome. com/major/medicine/cardiology/cardiogenic-pulmonary-edema/
The critical care nurse is caring for a patient with a central venous pressure (CVP) monitoring system. The nurse notes that the patient's CVP is increasing. What may this be indicative of? a) Hypovolemia b) Hypervolemia c) Hypermagnesemia d) Hypomagnesemia
A patient's CVP increasing may be indicative of… b) Hypervolemia CVP is a useful hemodynamic parameter to observe when managing an unstable patient's fluid volume status. An increasing pressure may be caused by hypervolemia or by a condition, such as heart failure, that results in decreased myocardial contractility. Smeltzer, S. C. , and Bare, B. Brunner & Suddarth's Textbook of Medical-Surgical Nursing, 12 th ed. Philadelphia: Lippincott Williams & Wilkins, 2010, Chapter 26: Assessment of Cardiovascular Function, p. 716.
How is hemodynamic monitoring achieved? a. Noninvasive monitoring systems b. Extracorporeal monitoring systems c. Direct pressure monitoring systems d. Partial pressure monitoring systems
hemodynamic monitoring is achieved by c. Direct pressure monitoring systems Critically ill patients require continuous assessment of their cardiovascular system to diagnose and manage their complex medical conditions. This type of assessment is achieved by the use of direct pressure monitoring systems, referred to as hemodynamic monitoring. Options A, B, and D do not describe hemodynamic monitoring systems.
A critically ill patient is admitted to the ICU. The physician decides to use intra-arterial pressure monitoring. What is the purpose of this? a) To assess left ventricular function b) To assess the pressure of the vena cava c) To assess the pressure in the right atrium d) To measure the patient's BP continually
the purpose of intra-arterial pressure monitoring is d) To measure the patient's BP continually Intra-arterial pressure monitoring is used to continually monitor a patient's blood pressure. It does not assess left ventricular function, pressure of the vena cava, or pressure of the right atrium.
You are a critical care nurse caring for a patient who has suffered an MI. You know that the most appropriate hemodynamic monitoring procedure to assess the left ventricular function of a patient who has suffered an MI would be what? a) CVP monitoring b) Pulmonary artery pressure monitoring c) Systemic arterial pressure monitoring d) Arterial blood gases (ABG)
hemodynamic monitoring procedure to assess the left ventricular function b) Pulmonary artery pressure monitoring CVP is used to assess right ventricular function c) Systemic arterial pressure monitoring is used to continually assess BP. ABGs are used to assess for acidic and alkalotic levels in the blood.
- Slides: 78