Invasive Candidiasis Part 1 Aetiology Pathogenesis Clinical manifestation
- Slides: 19
Invasive Candidiasis: Part 1 Aetiology, Pathogenesis & Clinical manifestation Arnaldo Lopes Colombo, MD Federal University of São Paulo, Brazil
Intended Learning Outcomes To recognise the spectrum of diseases caused by Candida To appreciate the different forms of invasive candidiasis To be aware of the risk factors of candidaemia To understand the pathogenesis in invasive candidiasis
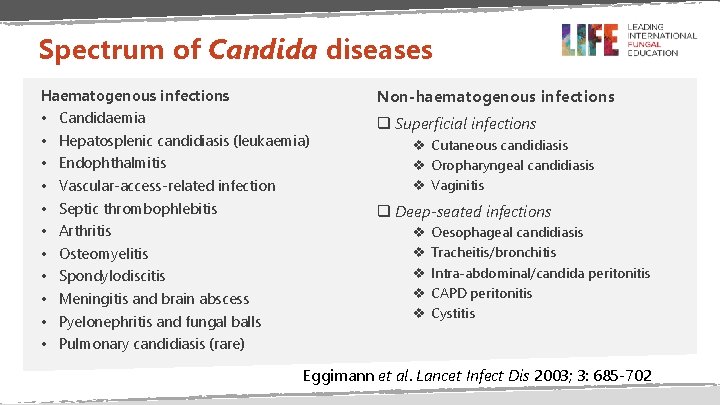
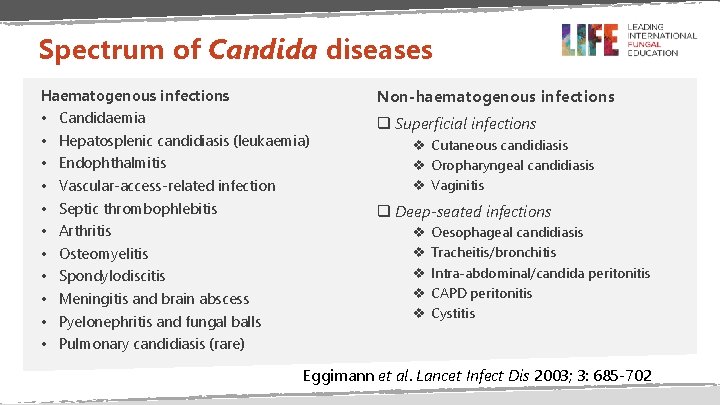
Spectrum of Candida diseases Haematogenous infections • • • Non-haematogenous infections Candidaemia Hepatosplenic candidiasis (leukaemia) Endophthalmitis Vascular-access-related infection Septic thrombophlebitis Arthritis Osteomyelitis Spondylodiscitis Meningitis and brain abscess Pyelonephritis and fungal balls q Superficial infections v Cutaneous candidiasis v Oropharyngeal candidiasis v Vaginitis q Deep-seated infections v v v Oesophageal candidiasis Tracheitis/bronchitis Intra-abdominal/candida peritonitis CAPD peritonitis Cystitis Pulmonary candidiasis (rare) Eggimann et al. Lancet Infect Dis 2003; 3: 685 -702
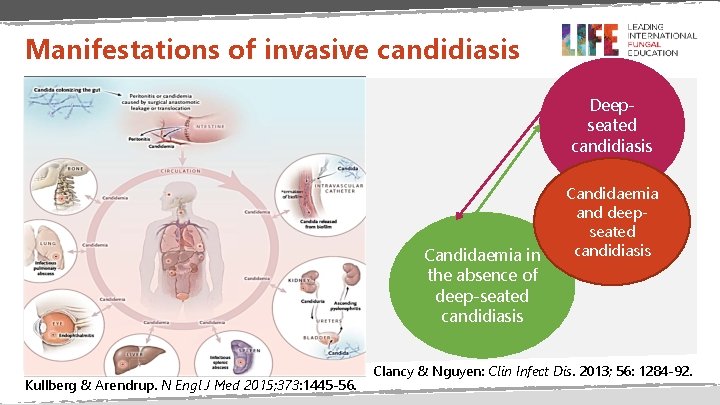
Invasive candidiasis • Invasive candidiasis = candidaemia + deep-seated tissue candidiasis • Candidaemia is the most commonly diagnosed form of invasive candidiasis • Mortality attributable to invasive candidiasis is as high as 40%, even with antifungal therapy • C. albicans is the most common Candida spp. , however, there is a global shift in favour of non-albicans species Kullberg & Arendrup. N Engl J Med 2015; 373: 1445 -56.
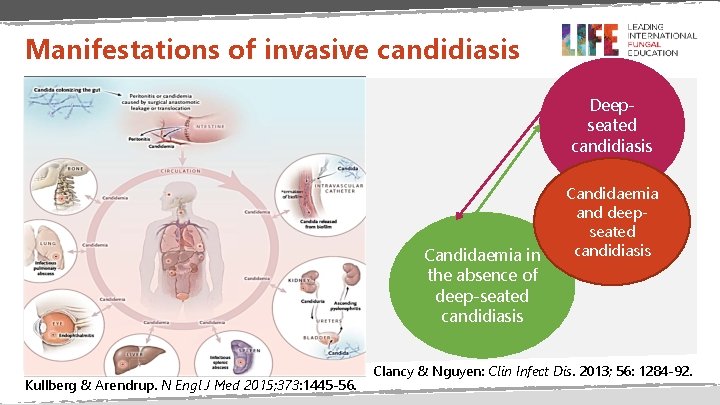
Manifestations of invasive candidiasis Deepseated candidiasis Candidaemia in the absence of deep-seated candidiasis Kullberg & Arendrup. N Engl J Med 2015; 373: 1445 -56. Candidaemia and deepseated candidiasis Clancy & Nguyen: Clin Infect Dis. 2013; 56: 1284 -92.
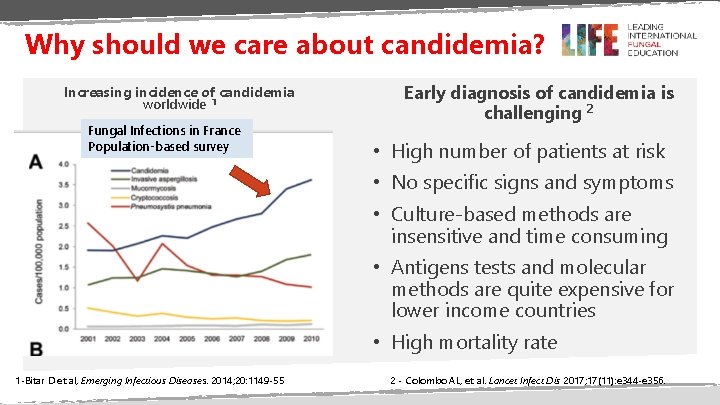
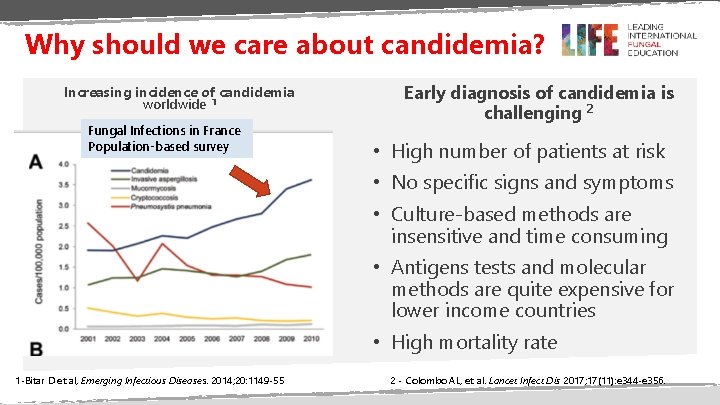
Why should we care about candidemia? Increasing incidence of candidemia worldwide 1 Fungal Infections in France Population-based survey Early diagnosis of candidemia is challenging 2 • High number of patients at risk • No specific signs and symptoms • Culture-based methods are insensitive and time consuming • Antigens tests and molecular methods are quite expensive for lower income countries • High mortality rate 1 -Bitar D et al, Emerging Infectious Diseases. 2014; 20: 1149 -55 2 - Colombo AL, et al. Lancet Infect Dis 2017; 17(11): e 344 -e 356.
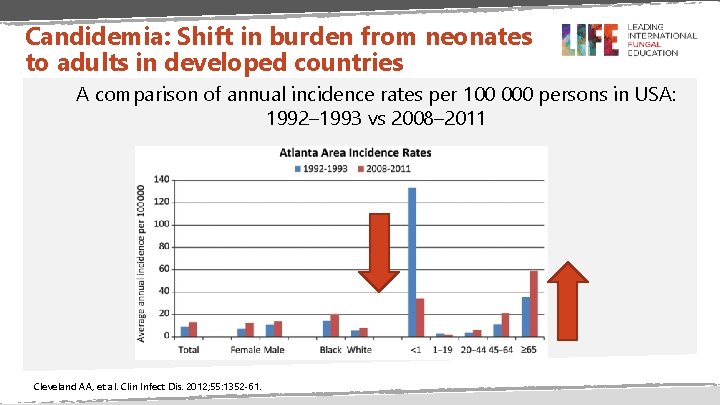
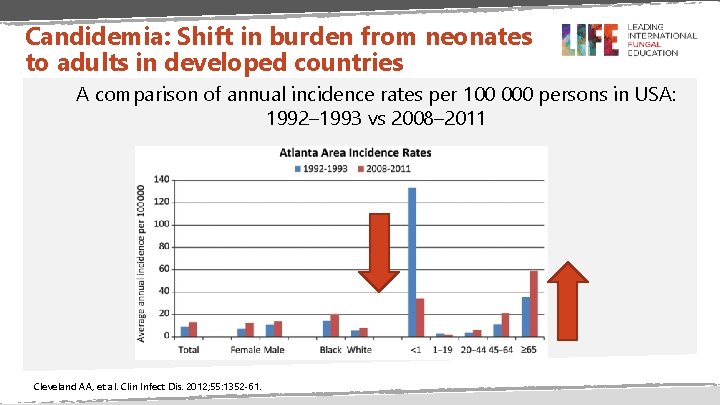
Candidemia: Shift in burden from neonates to adults in developed countries A comparison of annual incidence rates per 100 000 persons in USA: 1992– 1993 vs 2008– 2011 Cleveland AA, et al. Clin Infect Dis. 2012; 55: 1352 -61.
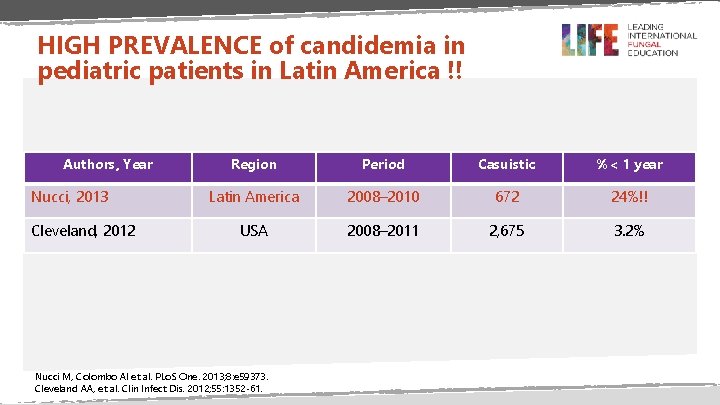
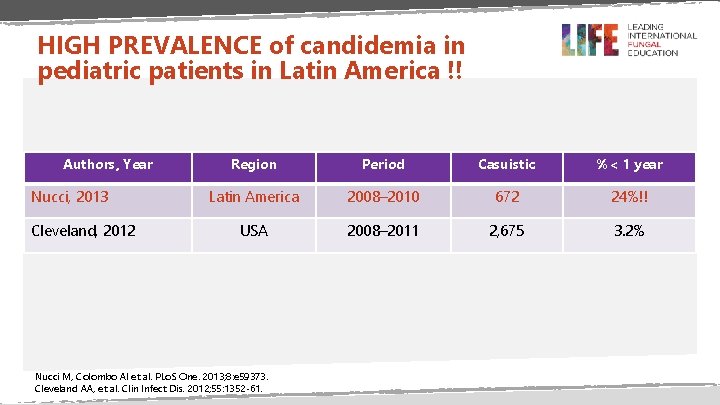
HIGH PREVALENCE of candidemia in pediatric patients in Latin America !! Authors, Year Nucci, 2013 Cleveland, 2012 Region Period Casuistic %< 1 year Latin America 2008– 2010 672 24%!! USA 2008– 2011 2, 675 3. 2% Nucci M, Colombo Al et al. PLo. S One. 2013; 8: e 59373. Cleveland AA, et al. Clin Infect Dis. 2012; 55: 1352 -61.
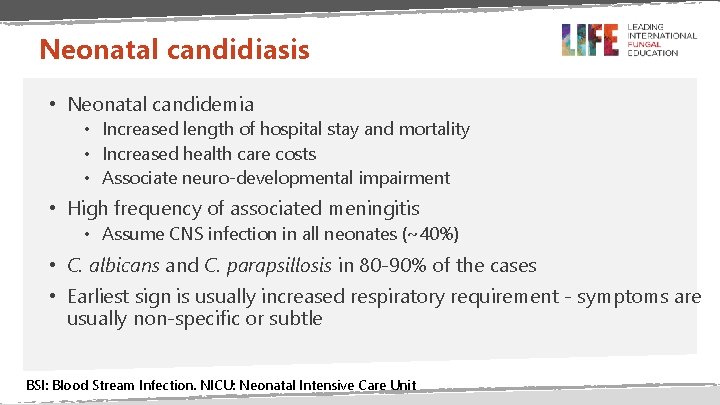
Neonatal candidiasis • Neonatal candidemia • Increased length of hospital stay and mortality • Increased health care costs • Associate neuro-developmental impairment • High frequency of associated meningitis • Assume CNS infection in all neonates (~40%) • C. albicans and C. parapsillosis in 80 -90% of the cases • Earliest sign is usually increased respiratory requirement - symptoms are usually non-specific or subtle BSI: Blood Stream Infection. NICU: Neonatal Intensive Care Unit
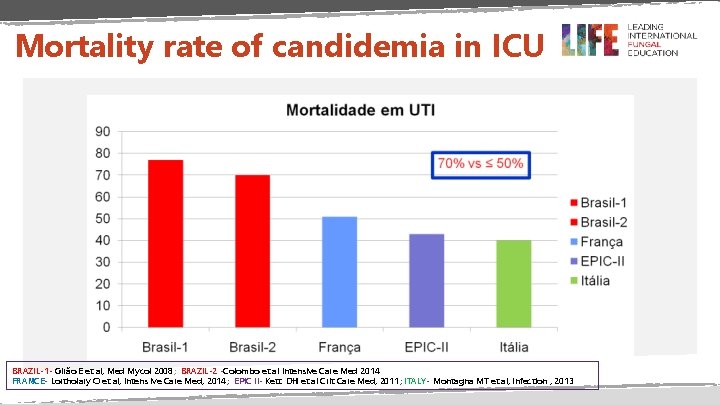
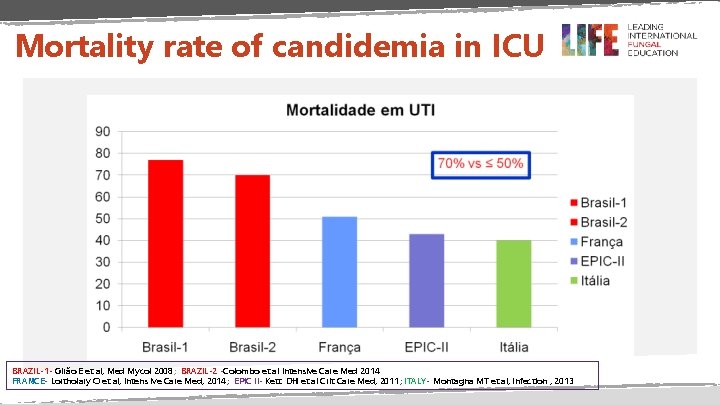
Mortality rate of candidemia in ICU BRAZIL-1 - Girão E et al, Med Mycol 2008; BRAZIL-2 -Colombo et al Intensive Care Med 2014 FRANCE- Lortholary O et al, Intens ive Care Med, 2014; EPIC II- Kett DH et al Crit Care Med, 2011; ITALY- Montagna MT et al, Infection , 2013
Candidemia: main factors associated with outcome • • • Age APACHE II score Co-morbidities Species of Candida Timing and choice of antifungal drug • Candins appears to be better choice • Management of the infectious focus • Catheter removal, drainage of abscess Morrell M, et al. Antimicrob Agents Chemother. 2005; 49: 3640 -5. Andes DR, et al. Clin Infect Dis. 2012; 54: 1110 -22. Kollef M, et al. Clin Infect Dis. 2012; 54: 1739 -46.
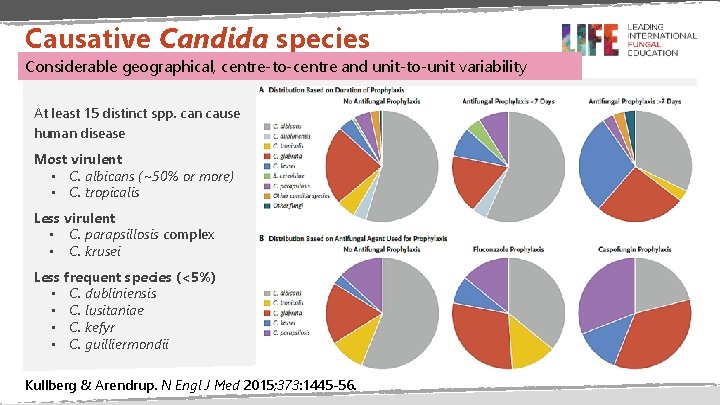
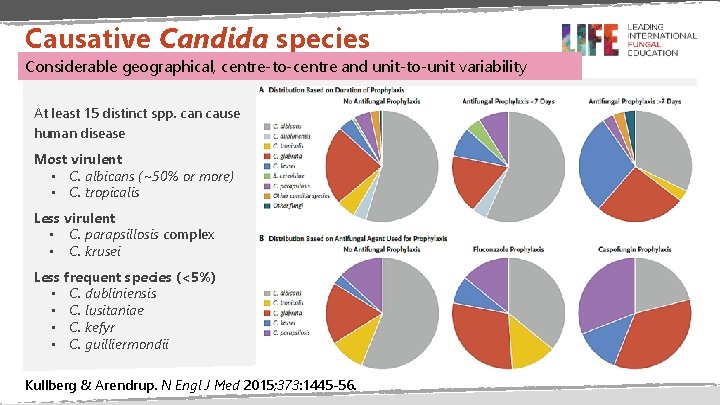
Causative Candida species Considerable geographical, centre-to-centre and unit-to-unit variability At least 15 distinct spp. can cause human disease Most virulent • C. albicans (~50% or more) • C. tropicalis Less virulent • C. parapsillosis complex • C. krusei Less frequent species (<5%) • C. dubliniensis • C. lusitaniae • C. kefyr • C. guilliermondii Kullberg & Arendrup. N Engl J Med 2015; 373: 1445 -56.
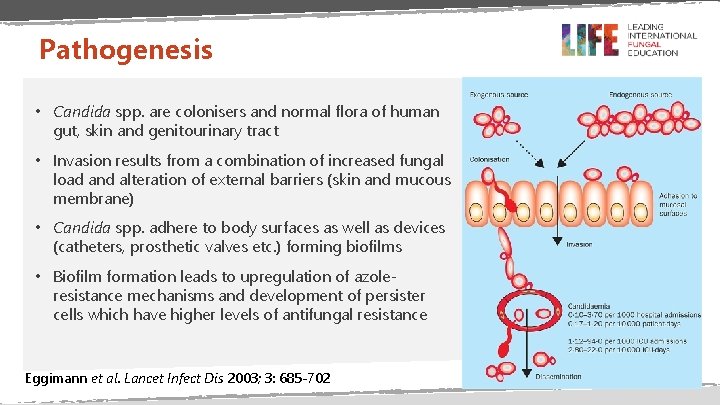
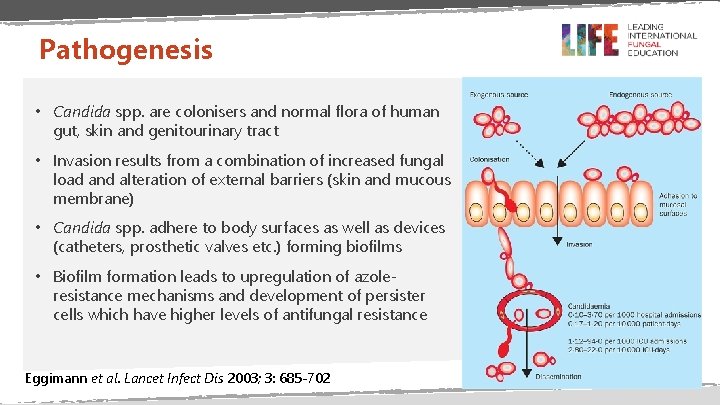
Pathogenesis • Candida spp. are colonisers and normal flora of human gut, skin and genitourinary tract • Invasion results from a combination of increased fungal load and alteration of external barriers (skin and mucous membrane) • Candida spp. adhere to body surfaces as well as devices (catheters, prosthetic valves etc. ) forming biofilms • Biofilm formation leads to upregulation of azoleresistance mechanisms and development of persister cells which have higher levels of antifungal resistance Eggimann et al. Lancet Infect Dis 2003; 3: 685 -702
Risk factors for invasive candidiasis • Critical illness: Long-term ICU stay • ~50% of episodes of candidaemia • Haemodialysis • Anti-cancer chemotherapy • Candida colonisation • Abdominal surgery: repeated laparotomies & anastomotic leakage Cleveland et al. PLo. S ONE 2015; 10: e 0120452. Colombo AL, et al. Lancet Infect Dis 2017; 17(11): e 344 -e 356;
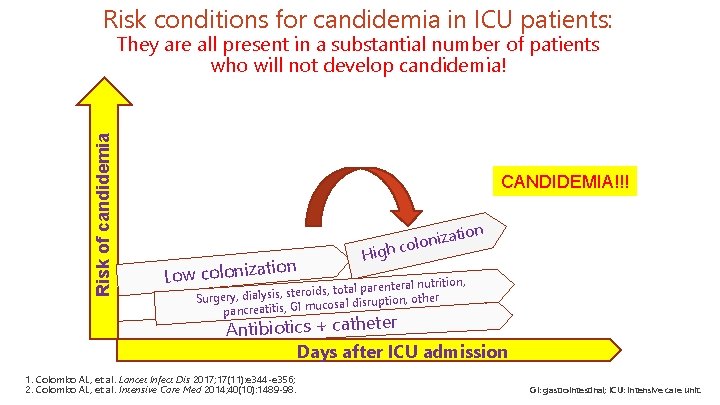
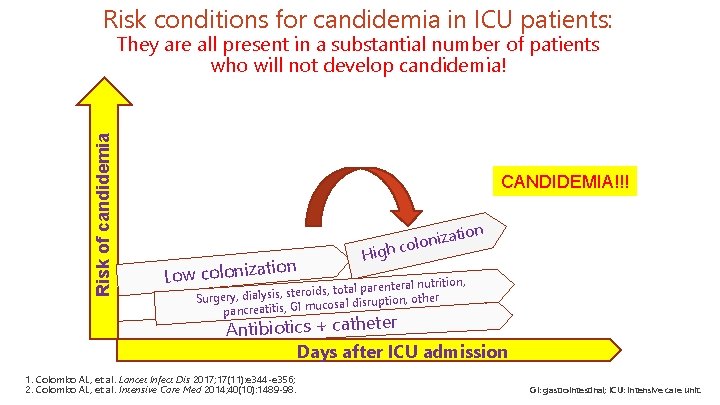
Risk conditions for candidemia in ICU patients: Risk of candidemia They are all present in a substantial number of patients who will not develop candidemia! CANDIDEMIA!!! tion Low coloniza High on izati n o l o c nutrition, , total parenteral ds oi er st , is ys al di other Surgery, ucosal disruption, pancreatitis, GI m Antibiotics + catheter Days after ICU admission 1. Colombo AL, et al. Lancet Infect Dis 2017; 17(11): e 344 -e 356; 2. Colombo AL, et al. Intensive Care Med 2014; 40(10): 1489 -98. GI: gastrointestinal; ICU: intensive care unit.
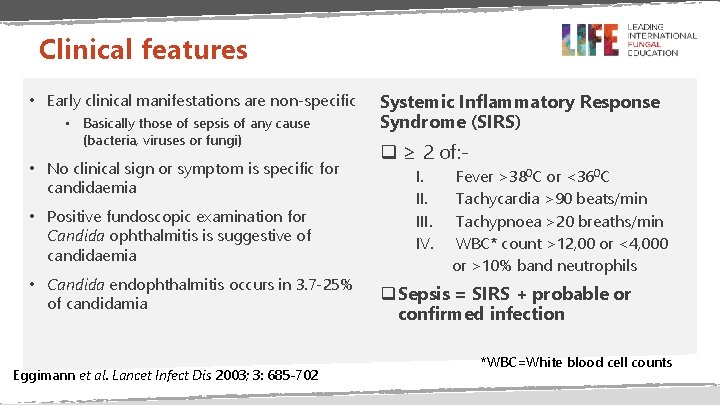
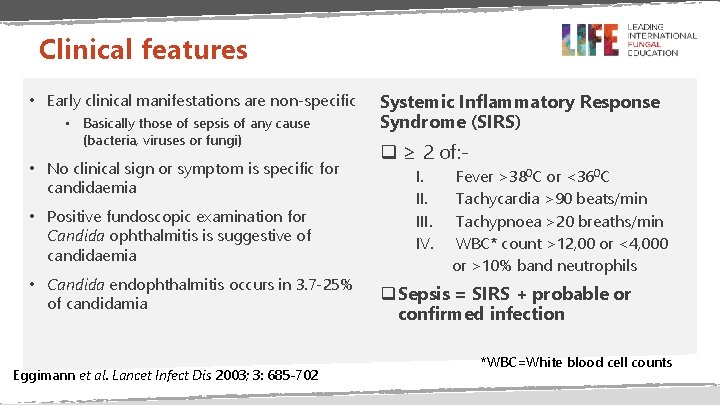
Clinical features • Early clinical manifestations are non-specific • Basically those of sepsis of any cause (bacteria, viruses or fungi) • No clinical sign or symptom is specific for candidaemia • Positive fundoscopic examination for Candida ophthalmitis is suggestive of candidaemia • Candida endophthalmitis occurs in 3. 7 -25% of candidamia Eggimann et al. Lancet Infect Dis 2003; 3: 685 -702 Systemic Inflammatory Response Syndrome (SIRS) q ≥ 2 of: I. III. IV. Fever >380 C or <360 C Tachycardia >90 beats/min Tachypnoea >20 breaths/min WBC* count >12, 00 or <4, 000 or >10% band neutrophils q Sepsis = SIRS + probable or confirmed infection *WBC=White blood cell counts
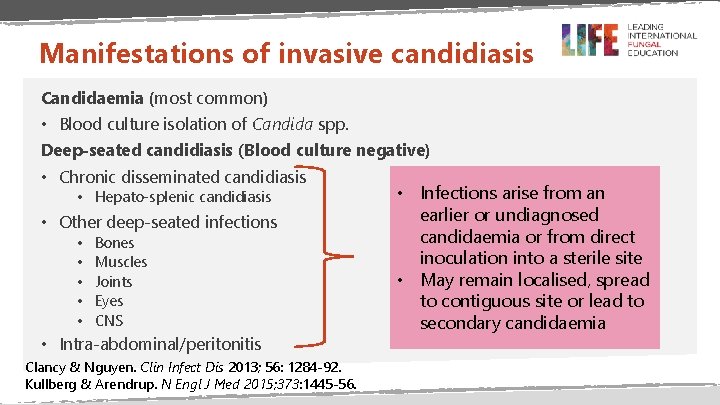
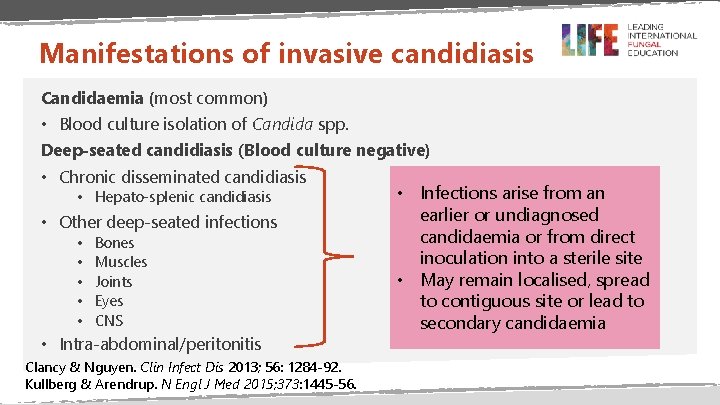
Manifestations of invasive candidiasis Candidaemia (most common) • Blood culture isolation of Candida spp. Deep-seated candidiasis (Blood culture negative) • Chronic disseminated candidiasis • Hepato-splenic candidiasis • Other deep-seated infections • • • Bones Muscles Joints Eyes CNS • Intra-abdominal/peritonitis Clancy & Nguyen. Clin Infect Dis 2013; 56: 1284 -92. Kullberg & Arendrup. N Engl J Med 2015; 373: 1445 -56. • Infections arise from an earlier or undiagnosed candidaemia or from direct inoculation into a sterile site • May remain localised, spread to contiguous site or lead to secondary candidaemia
Summary • Candidaemia, the most common form of invasive candidiasis • Increasing number of patients at risk worldwide • Invasive candidiasis results from a combination of increased fungal load and alteration of epithelial barriers • Early clinical manifestations are non-specific • Mortality rate ranges between 30 -75%, even with antifungal treatment
END