IRRITABLE BOWEL SYNDROME Kimberly M Persley MD IBS
IRRITABLE BOWEL SYNDROME Kimberly M. Persley, MD
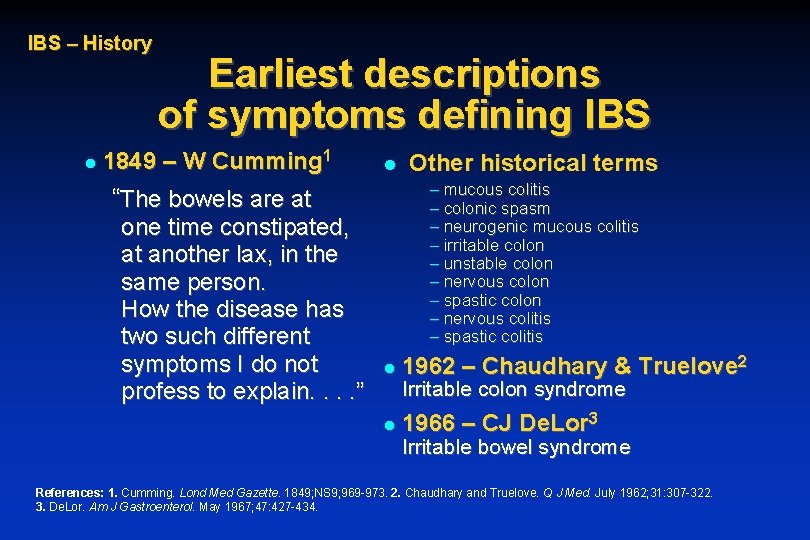
IBS – History l Earliest descriptions of symptoms defining IBS 1849 – W Cumming 1 l – mucous colitis – colonic spasm – neurogenic mucous colitis – irritable colon – unstable colon – nervous colon – spastic colon – nervous colitis – spastic colitis “The bowels are at one time constipated, at another lax, in the same person. How the disease has two such different symptoms I do not profess to explain. . ” Other historical terms l 1962 – Chaudhary & Truelove 2 l 1966 – CJ De. Lor 3 Irritable colon syndrome Irritable bowel syndrome References: 1. Cumming. Lond Med Gazette. 1849; NS 9; 969 -973. 2. Chaudhary and Truelove. Q J Med. July 1962; 31: 307 -322. 3. De. Lor. Am J Gastroenterol. May 1967; 47: 427 -434.
IBS – History Historical perspective l Long dismissed as a psychosomatic condition 1 – no clear etiology – affects predominantly women (~70% of sufferers are women)2 – condition not fatal l Attitudes now changing l Incidence and prevalence not extensively monitored in past References: 1. Maxwell et al. Lancet. December 1997; 350: 1691 -1695. 2. Sandler. Gastroenterology. August 1990; 99: 409 -415.
IBS – Signs and symptoms Hallmark symptoms of IBS l Chronic or recurrent GI symptoms – lower abdominal pain/discomfort – altered bowel function (urgency, altered stool consistency, altered stool frequency, incomplete evacuation) – bloating l Not explained by identifiable structural or biochemical abnormalities Reference: Thompson et al. Gut. 1999; 45(suppl 2): 1143 -1147.
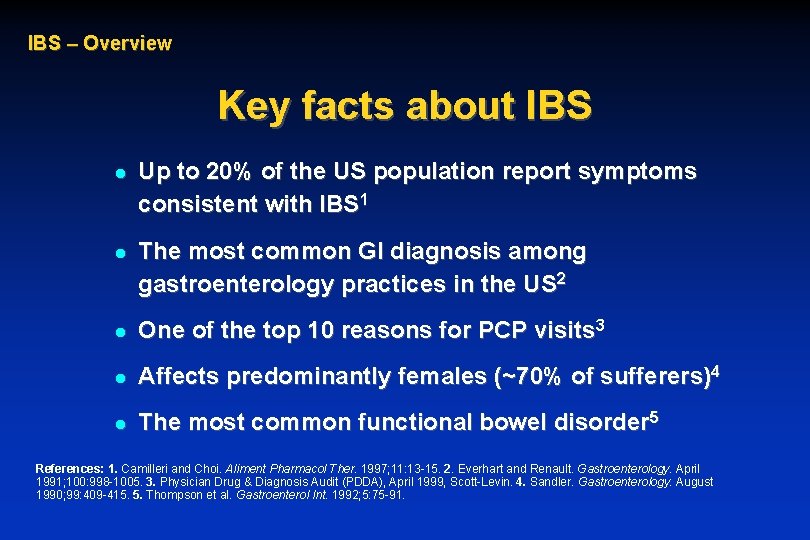
IBS – Overview Key facts about IBS l Up to 20% of the US population report symptoms consistent with IBS 1 l The most common GI diagnosis among gastroenterology practices in the US 2 l One of the top 10 reasons for PCP visits 3 l Affects predominantly females (~70% of sufferers)4 l The most common functional bowel disorder 5 References: 1. Camilleri and Choi. Aliment Pharmacol Ther. 1997; 11: 13 -15. 2. Everhart and Renault. Gastroenterology. April 1991; 100: 998 -1005. 3. Physician Drug & Diagnosis Audit (PDDA), April 1999, Scott-Levin. 4. Sandler. Gastroenterology. August 1990; 99: 409 -415. 5. Thompson et al. Gastroenterol Int. 1992; 5: 75 -91.
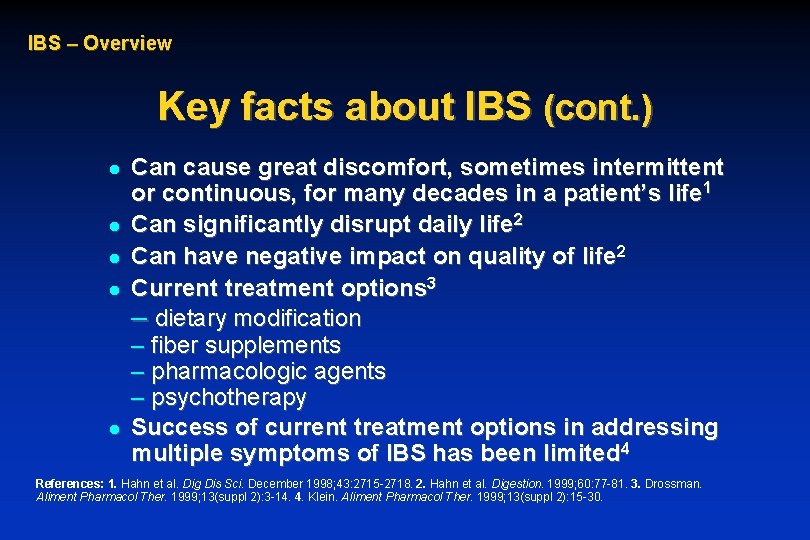
IBS – Overview Key facts about IBS (cont. ) l l l Can cause great discomfort, sometimes intermittent or continuous, for many decades in a patient’s life 1 Can significantly disrupt daily life 2 Can have negative impact on quality of life 2 Current treatment options 3 – dietary modification – fiber supplements – pharmacologic agents – psychotherapy Success of current treatment options in addressing multiple symptoms of IBS has been limited 4 References: 1. Hahn et al. Dig Dis Sci. December 1998; 43: 2715 -2718. 2. Hahn et al. Digestion. 1999; 60: 77 -81. 3. Drossman. Aliment Pharmacol Ther. 1999; 13(suppl 2): 3 -14. 4. Klein. Aliment Pharmacol Ther. 1999; 13(suppl 2): 15 -30.
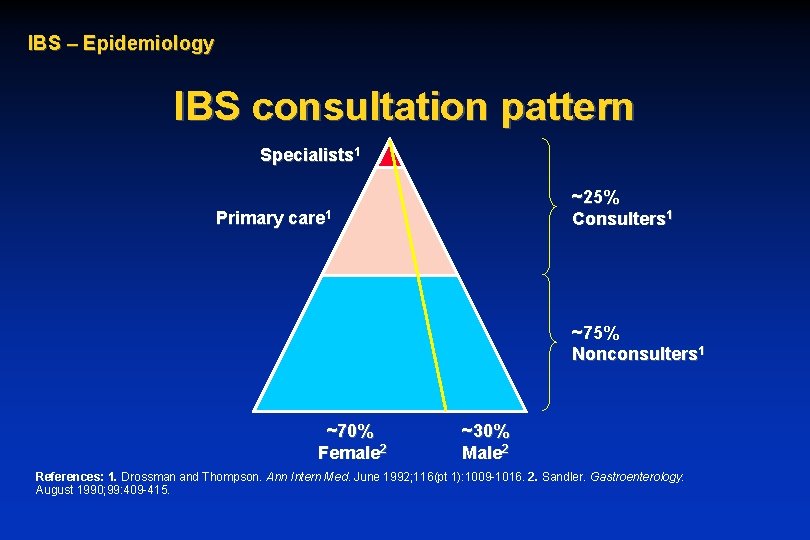
IBS – Epidemiology IBS consultation pattern Specialists 1 ~25% Consulters 1 Primary care 1 ~75% Nonconsulters 1 ~70% Female 2 ~30% Male 2 References: 1. Drossman and Thompson. Ann Intern Med. June 1992; 116(pt 1): 1009 -1016. 2. Sandler. Gastroenterology. August 1990; 99: 409 -415.
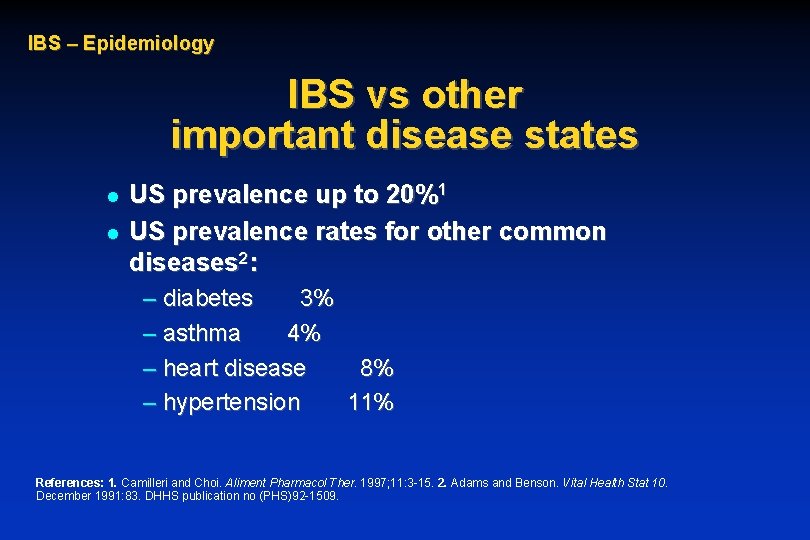
IBS – Epidemiology IBS vs other important disease states l l US prevalence up to 20%1 US prevalence rates for other common diseases 2: – diabetes 3% – asthma 4% – heart disease 8% – hypertension 11% References: 1. Camilleri and Choi. Aliment Pharmacol Ther. 1997; 11: 3 -15. 2. Adams and Benson. Vital Health Stat 10. December 1991: 83. DHHS publication no (PHS)92 -1509.
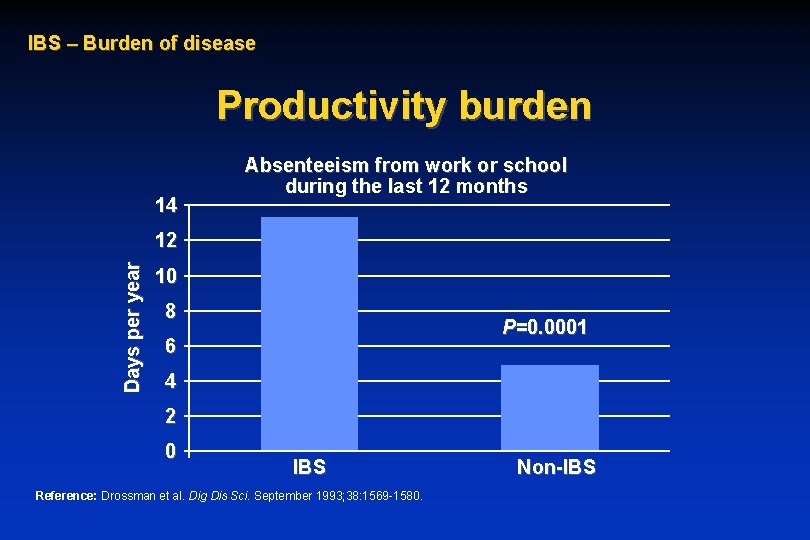
IBS – Burden of disease Productivity burden 14 Absenteeism from work or school during the last 12 months Days per year 12 10 8 P=0. 0001 6 4 2 0 IBS Reference: Drossman et al. Dig Dis Sci. September 1993; 38: 1569 -1580. Non-IBS
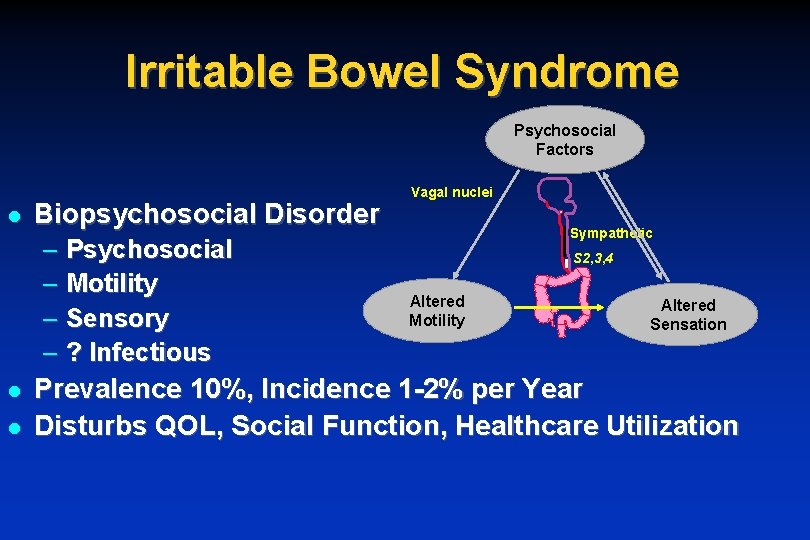
Irritable Bowel Syndrome Psychosocial Factors l Biopsychosocial Disorder – – l l Psychosocial Motility Sensory ? Infectious Vagal nuclei Sympathetic S 2, 3, 4 Altered Motility Altered Sensation Prevalence 10%, Incidence 1 -2% per Year Disturbs QOL, Social Function, Healthcare Utilization
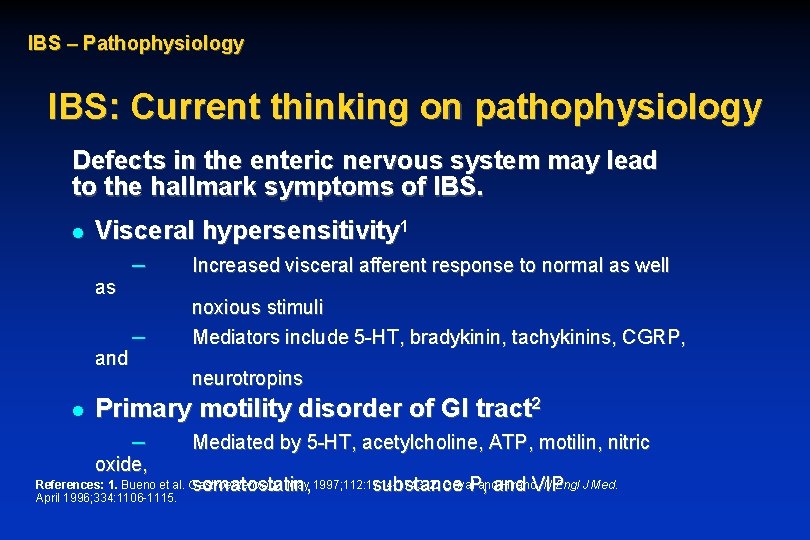
IBS – Pathophysiology IBS: Current thinking on pathophysiology Defects in the enteric nervous system may lead to the hallmark symptoms of IBS. l Visceral hypersensitivity 1 as and l – Increased visceral afferent response to normal as well – noxious stimuli Mediators include 5 -HT, bradykinin, tachykinins, CGRP, neurotropins Primary motility disorder of GI tract 2 – oxide, Mediated by 5 -HT, acetylcholine, ATP, motilin, nitric somatostatin, substance P, and VIP References: 1. Bueno et al. Gastroenterology. May 1997; 112: 1714 -1743. 2. Goyal and Hirano. N Engl J Med. April 1996; 334: 1106 -1115.
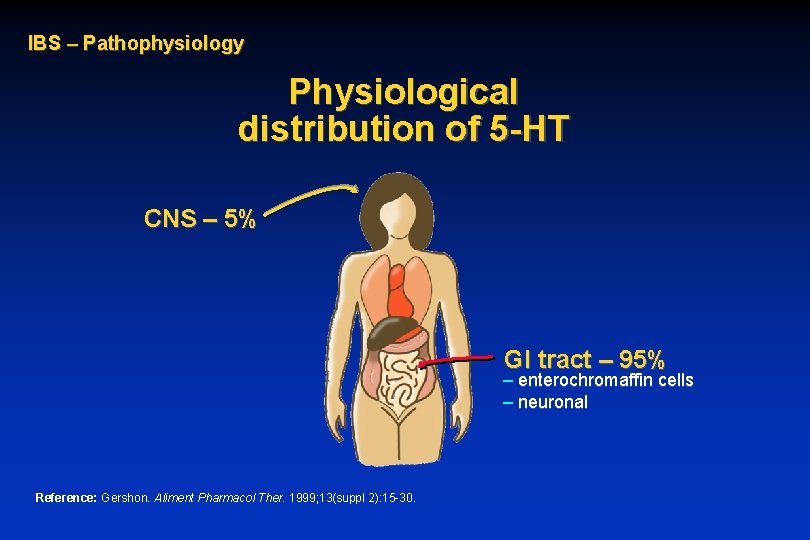
IBS – Pathophysiology Physiological distribution of 5 -HT CNS – 5% GI tract – 95% – enterochromaffin cells – neuronal Reference: Gershon. Aliment Pharmacol Ther. 1999; 13(suppl 2): 15 -30.
IBS – Pathophysiology 5 -HT receptor effects l Mediate reflexes controlling gastrointestinal motility and secretion l Mediate perception of visceral pain Reference: Gershon. Aliment Pharmacol Ther. 1999; 13(suppl 2): 15 -30.
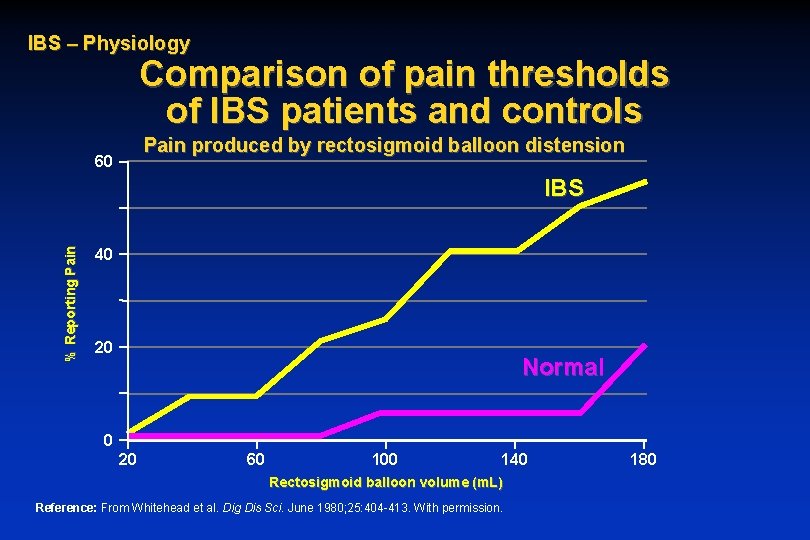
IBS – Physiology Comparison of pain thresholds of IBS patients and controls Pain produced by rectosigmoid balloon distension 60 % Reporting Pain IBS 40 20 Normal 0 20 60 100 140 Rectosigmoid balloon volume (m. L) Reference: From Whitehead et al. Dig Dis Sci. June 1980; 25: 404 -413. With permission. 180
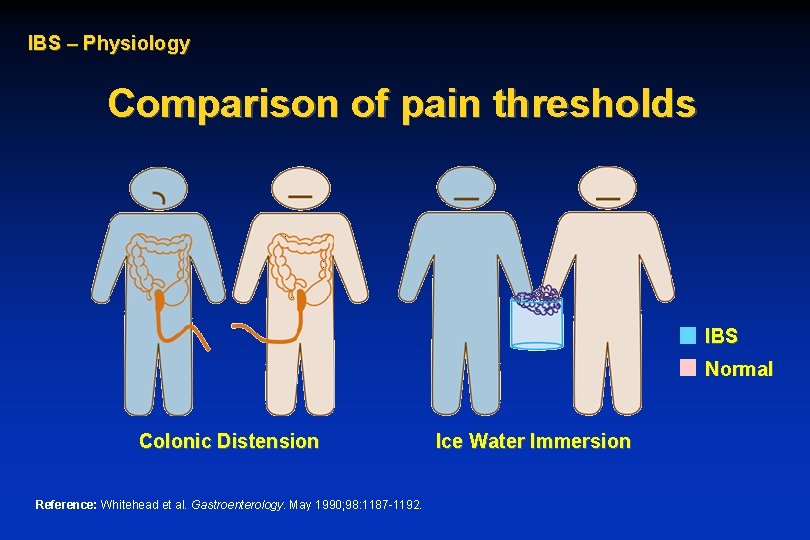
IBS – Physiology Comparison of pain thresholds IBS Normal Colonic Distension Reference: Whitehead et al. Gastroenterology. May 1990; 98: 1187 -1192. Ice Water Immersion
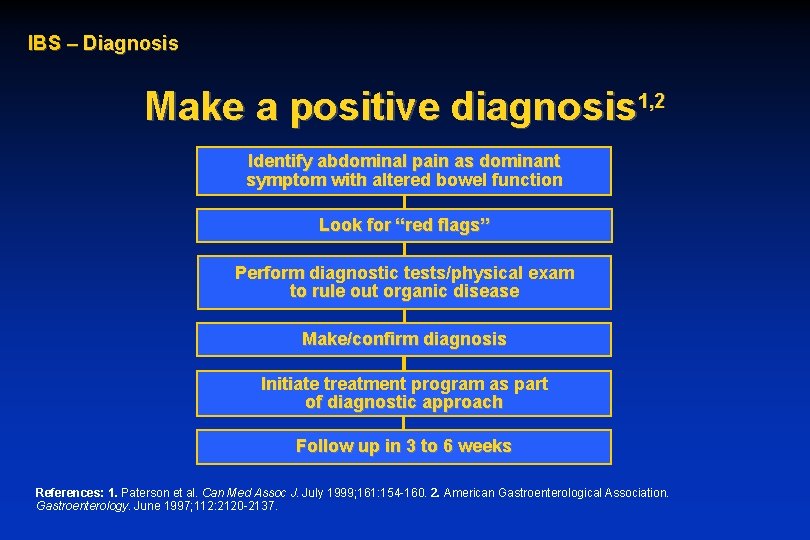
IBS – Diagnosis Make a positive diagnosis 1, 2 Identify abdominal pain as dominant symptom with altered bowel function Look for “red flags” Perform diagnostic tests/physical exam to rule out organic disease Make/confirm diagnosis Initiate treatment program as part of diagnostic approach Follow up in 3 to 6 weeks References: 1. Paterson et al. Can Med Assoc J. July 1999; 161: 154 -160. 2. American Gastroenterological Association. Gastroenterology. June 1997; 112: 2120 -2137.
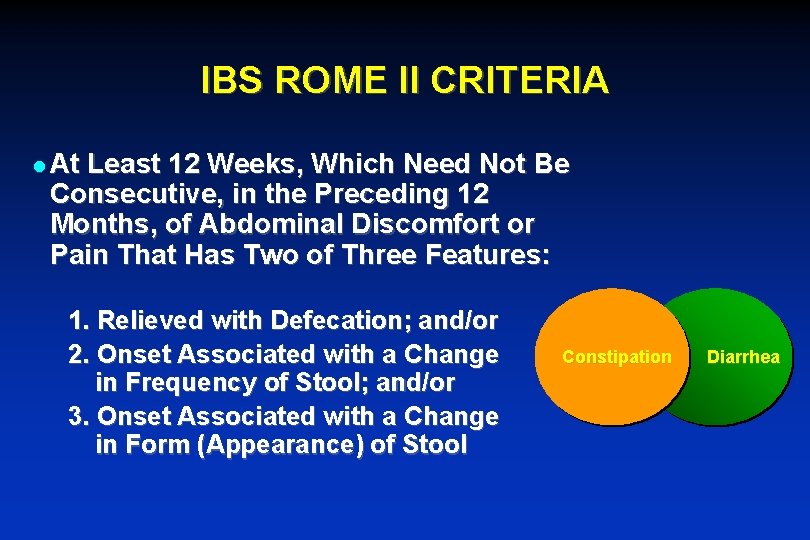
IBS ROME II CRITERIA l At Least 12 Weeks, Which Need Not Be Consecutive, in the Preceding 12 Months, of Abdominal Discomfort or Pain That Has Two of Three Features: 1. Relieved with Defecation; and/or 2. Onset Associated with a Change in Frequency of Stool; and/or 3. Onset Associated with a Change in Form (Appearance) of Stool Constipation Diarrhea
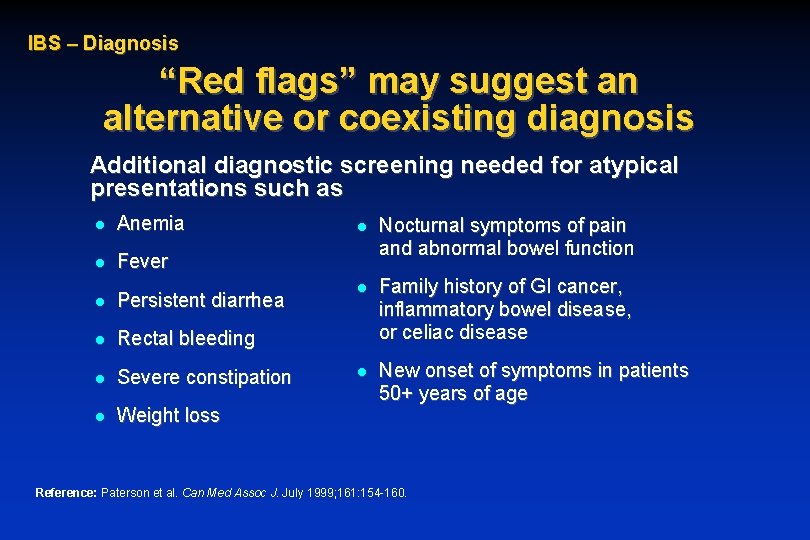
IBS – Diagnosis “Red flags” may suggest an alternative or coexisting diagnosis Additional diagnostic screening needed for atypical presentations such as l Anemia l Fever l Persistent diarrhea l Rectal bleeding l Severe constipation l Weight loss l Nocturnal symptoms of pain and abnormal bowel function l Family history of GI cancer, inflammatory bowel disease, or celiac disease l New onset of symptoms in patients 50+ years of age Reference: Paterson et al. Can Med Assoc J. July 1999; 161: 154 -160.
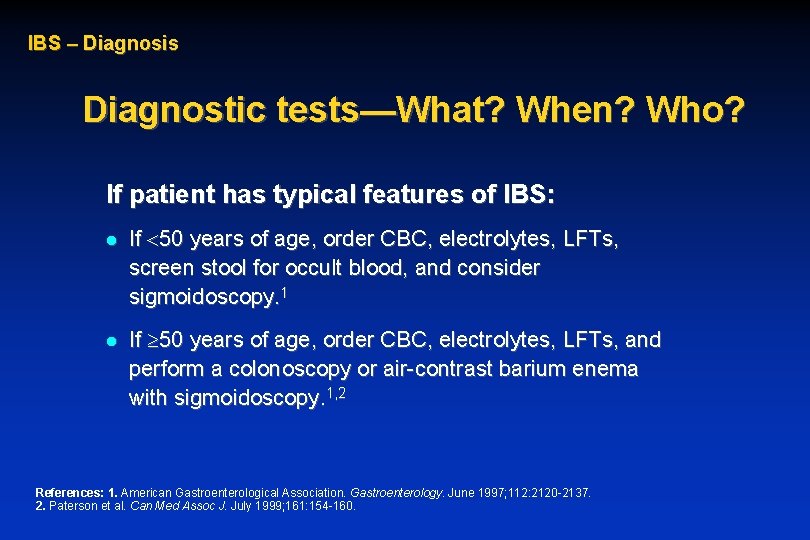
IBS – Diagnosis Diagnostic tests—What? When? Who? If patient has typical features of IBS: l l If 50 years of age, order CBC, electrolytes, LFTs, screen stool for occult blood, and consider sigmoidoscopy. 1 If 50 years of age, order CBC, electrolytes, LFTs, and perform a colonoscopy or air-contrast barium enema with sigmoidoscopy. 1, 2 References: 1. American Gastroenterological Association. Gastroenterology. June 1997; 112: 2120 -2137. 2. Paterson et al. Can Med Assoc J. July 1999; 161: 154 -160.
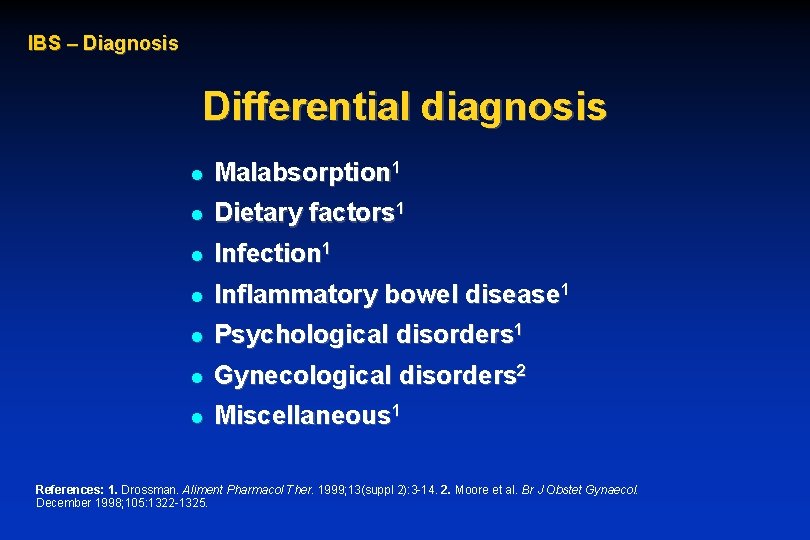
IBS – Diagnosis Differential diagnosis l Malabsorption 1 l Dietary factors 1 l Infection 1 l Inflammatory bowel disease 1 l Psychological disorders 1 l Gynecological disorders 2 l Miscellaneous 1 References: 1. Drossman. Aliment Pharmacol Ther. 1999; 13(suppl 2): 3 -14. 2. Moore et al. Br J Obstet Gynaecol. December 1998; 105: 1322 -1325.
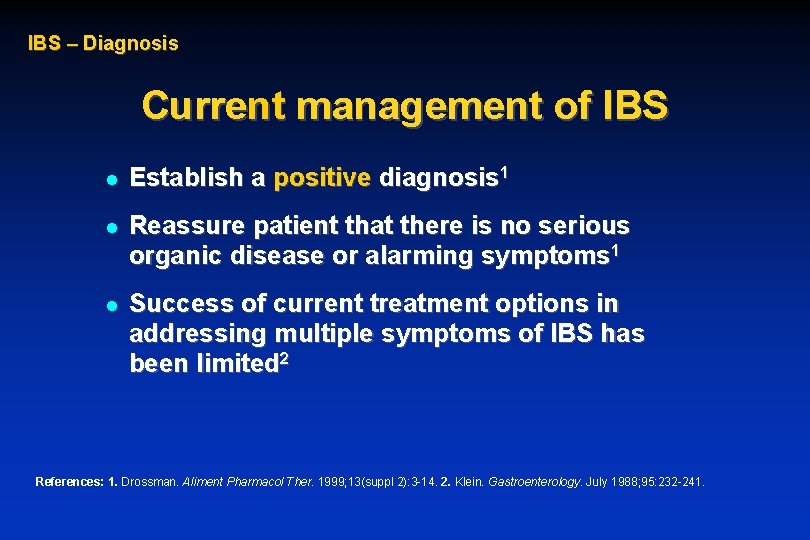
IBS – Diagnosis Current management of IBS l Establish a positive diagnosis 1 l Reassure patient that there is no serious organic disease or alarming symptoms 1 l Success of current treatment options in addressing multiple symptoms of IBS has been limited 2 References: 1. Drossman. Aliment Pharmacol Ther. 1999; 13(suppl 2): 3 -14. 2. Klein. Gastroenterology. July 1988; 95: 232 -241.
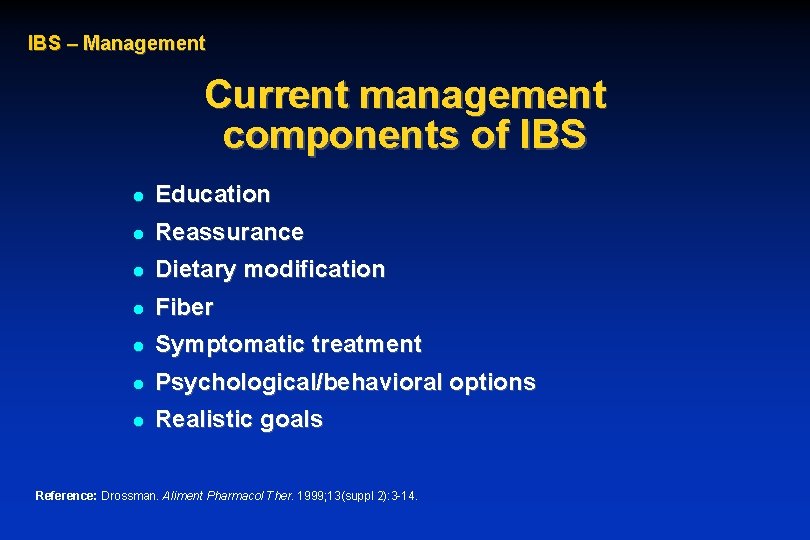
IBS – Management Current management components of IBS l Education l Reassurance l Dietary modification l Fiber l Symptomatic treatment l Psychological/behavioral options l Realistic goals Reference: Drossman. Aliment Pharmacol Ther. 1999; 13(suppl 2): 3 -14.
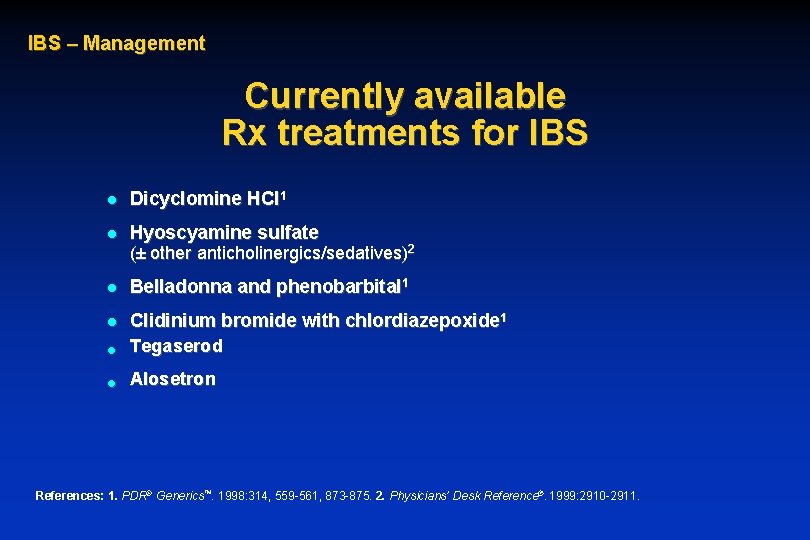
IBS – Management Currently available Rx treatments for IBS l Dicyclomine HCl 1 l Hyoscyamine sulfate (± other anticholinergics/sedatives)2 l Belladonna and phenobarbital 1 l l Clidinium bromide with chlordiazepoxide 1 Tegaserod l Alosetron References: 1. PDR® Generics™. 1998: 314, 559 -561, 873 -875. 2. Physicians’ Desk Reference®. 1999: 2910 -2911.
IBS – Management Antispasmodics/anticholinergics Symptomatic treatment—pain 1 l Smooth muscle relaxants via anticholinergic effects and/or direct action on smooth muscle 2 References: 1. Drossman. Aliment Pharmacol Ther. 1999; 13(suppl 2): 3 -14. 2. Drug Facts and Comparisons®. 1999: 298 -298 c.
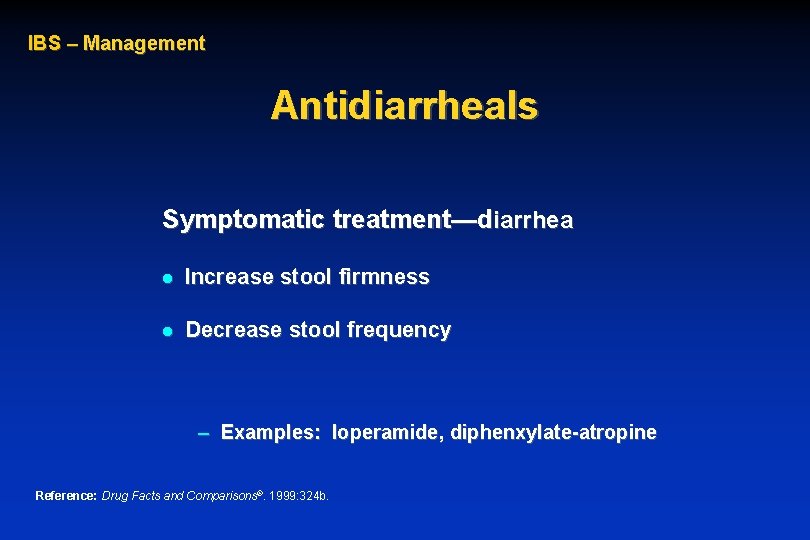
IBS – Management Antidiarrheals Symptomatic treatment—diarrhea l Increase stool firmness l Decrease stool frequency – Examples: loperamide, diphenxylate-atropine Reference: Drug Facts and Comparisons®. 1999: 324 b.
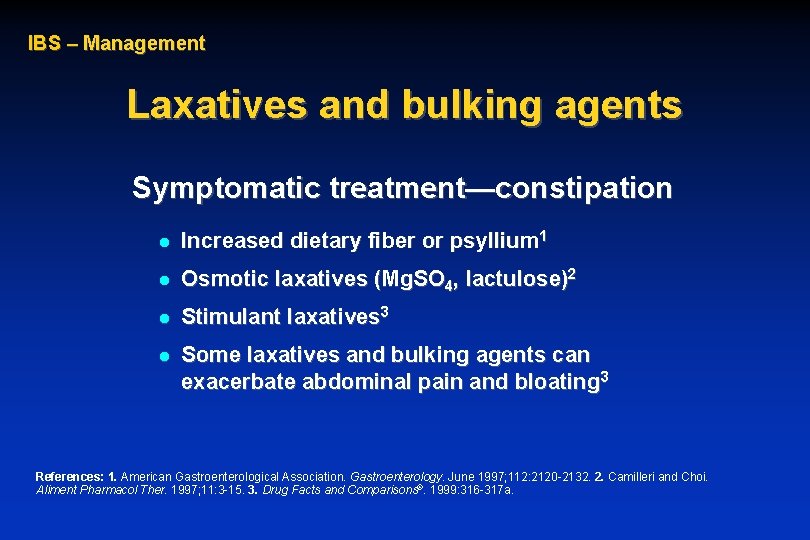
IBS – Management Laxatives and bulking agents Symptomatic treatment—constipation l Increased dietary fiber or psyllium 1 l Osmotic laxatives (Mg. SO 4, lactulose)2 l Stimulant laxatives 3 l Some laxatives and bulking agents can exacerbate abdominal pain and bloating 3 References: 1. American Gastroenterological Association. Gastroenterology. June 1997; 112: 2120 -2132. 2. Camilleri and Choi. Aliment Pharmacol Ther. 1997; 11: 3 -15. 3. Drug Facts and Comparisons®. 1999: 316 -317 a.

IBS – Management Tricyclic antidepressants and SSRIs Symptomatic treatment—pain l Reserved for patients with severe or refractory pain Reference: Drossman and Thompson. Ann Intern Med. 1992; 116(pt 1): 1009 -1016.
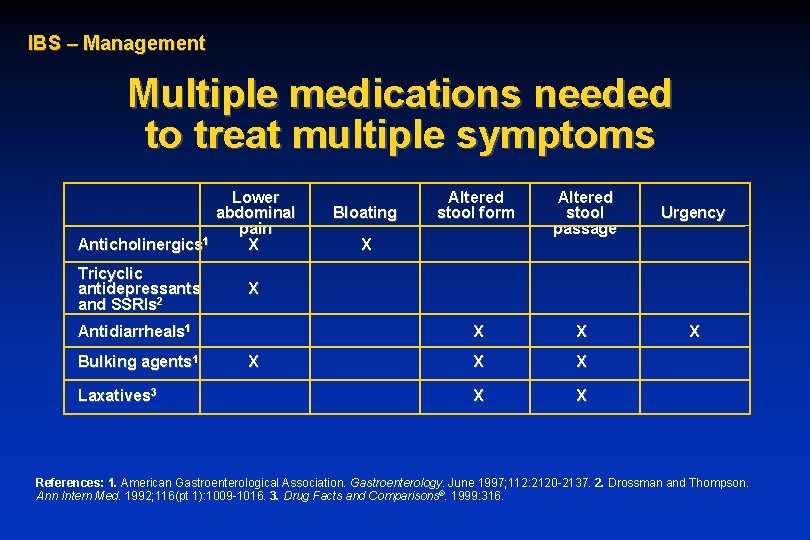
IBS – Management Multiple medications needed to treat multiple symptoms Lower abdominal pain 1 Anticholinergics X Tricyclic antidepressants and SSRIs 2 Laxatives 3 Altered stool passage Urgency X X X X X Antidiarrheals 1 Bulking agents 1 Bloating Altered stool form X References: 1. American Gastroenterological Association. Gastroenterology. June 1997; 112: 2120 -2137. 2. Drossman and Thompson. Ann Intern Med. 1992; 116(pt 1): 1009 -1016. 3. Drug Facts and Comparisons®. 1999: 316.
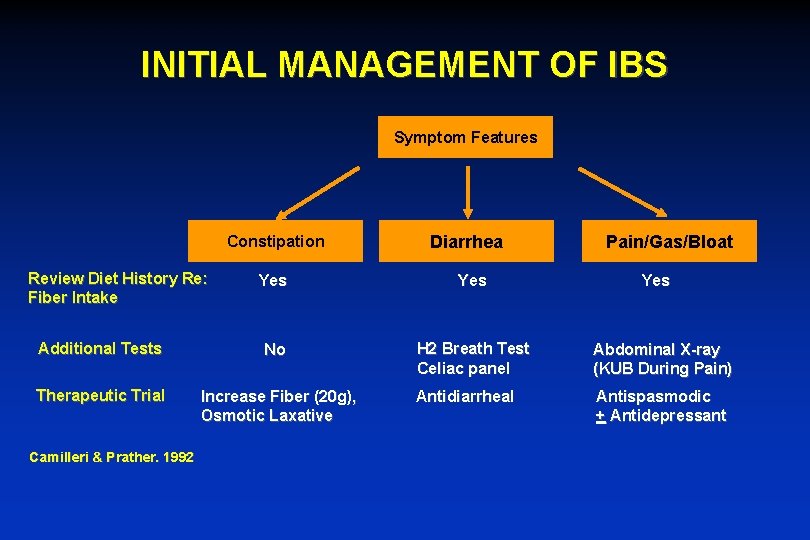
INITIAL MANAGEMENT OF IBS Symptom Features Constipation Review Diet History Re: Fiber Intake Diarrhea Pain/Gas/Bloat Yes Additional Tests No H 2 Breath Test Celiac panel Abdominal X-ray (KUB During Pain) Therapeutic Trial Increase Fiber (20 g), Osmotic Laxative Antidiarrheal Antispasmodic + Antidepressant Camilleri & Prather. 1992 Yes
Tegaserod (Zelnorm) (serotinin 4 receptor agonist) Approved for constipation predominant IBS l 1 pill given twice daily l Improvement of symptoms in women but not men l Use up to 12 weeks l Mild side effects: diarrhea the most prominent side effect l
Non-Traditional Remedies l Chinese Herbal Medicine – 116 pts randomized to CHM did better than pts receiving placebo l Peppermint Oil – Relaxation of GI smooth muscle – Meta-analysis showed significant improvement of IBS symptoms l l l Acupunture Probiotics Antibiotics Benoussan A. JAMA 1998 Pittler M. AJG 1998
Surgical Therapy for IBS l IBS symptoms may be attributed to: – Non-functioning gallbladder disease, chronic appendicitis, uterine fibroids, tortuous colon IBS symptoms rarely improve after surgery l IBS patients 2 to 3 times more likely to undergo unnecessary surgery l
Take Home Points IBS is a chronic medical condition characterized by abdominal pain, diarrhea or constipation, bloating, passage of mucus and feelings of incomplete evacuation l Precise etiology of IBS is unknown and therefore treatment is focused on relieving symptoms rather that “curing disease” l
Take Home Points Although many IBS patients complain of symptoms after eating, true food allergies are uncommon l Specific therapies are determined by individual patient symptoms l Life-style modifications and possible alternative therapies may relieve symptoms l Surgery has NO Role in treatment of IBS l
- Slides: 34