PH Pulmonary Hypertension PH Pulmonary hypertension is an



- Slides: 22
PH Pulmonary Hypertension
PH • Pulmonary hypertension is an abnormal elevation of the pulmonary artery pressure (PAP and the pulmonary vascular resistance (PVR) resulting in right ventricular (RV) failure and premature death.
PH • PH used to be recognized as a disease with a grim prognosis. • Over the last decade, new medications have been developed to treat PH. These medications have improved both the quantity and quality of life for patients with PH. • Since we can now treat PH, we need to be more aware of pursuing it as a diagnosis.
PH What is PH? m. PAP > 25 mm. Hg at rest m. PAP > 30 mm. Hg with activity What are the most common symptoms? Worsening SOB Chest pain Fatigue Palpitations Lower extremity edema Syncope
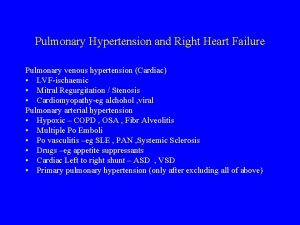
PH • WHO classification ▫ Group I- PAH ▫ Group II- PVH, PH secondary to LV failure ▫ Group III- PH associated with lung disease or hypoxia ▫ Group IV- PH secondary to chronic thromboembolic disease ▫ Group V- miscellaneous - HIV infection, drug exposure
PH • Group I - PAH ▫ ▫ ▫ Replaces primary pulmonary hypertension No known underlying risk factors Usually seen in women of childbearing age Rare - 2 to 3 per million per year Genetic predisposition

PH • Facts: ▫ Group II – PVH – most common, >15 mm. Hg ▫ Group III - lung disease PCWP COPD – mild PH seen in up to 50% of pts OSA – usually associated with mild PH OHS – more commonly seen with cor pulmonale ▫ Group IV - chronic PTED – up to 4%
PH • Pathophysiology ▫ Pulmonary endothelial cell dysfunction or injury causing vascular changes Intimal proliferation Hypertrophy Proliferation of smooth muscle cells Vasoconstriction In situ thrombosis
PH • Making the diagnosis ▫ High index of suspicion ▫ PE – early, Nl; increased P 2, TR, heptojugular reflux ▫ CXR, CT chest – enlarged PA’s ▫ EKG – V 1, tall R wave and short S wave (RV hypertrophy); II, p-pulmonale (RAE) ▫ Transthoracic ECHO – evaluate LV function, estimate RVSP and PAP’S ▫ Right heart catheterization – measure PAP’s and PCWP
PH • Further Evaluation ▫ Lab – ANA, RF, HIV, CBC, LFT’s, TFT’s ▫ PFT’s – OLD or ILD; decrease in DLCO ▫ Overnight oximetry – desaturation is seen in 70% of pts ▫ PSG ▫ V/Q scan, CT chest, pulmonary angiography
PH • Treatment – General measures ▫ O 2 – keep sats > 90% ▫ Avoid vasoconstricting decongestants, B blockers, stimulants and anorexigens ▫ Do low level aerobic exercise ▫ Follow a low sodium (<2400 mg) diet ▫ Avoid pregnancy ▫ Anticoagulation ▫ Diuretics ▫ Digoxin?

PH • Treatment – Medications ▫ Prostanoids – epoprostenol, treprostinil, and iloprost ▫ ERA’s (endothelin receptor antagonists) – bosentan and ambrisentan ▫ Phosphodiesterase-5 (PDE-5) inhibitors sildenafil
PH • Prostanoids – prostacyclin analogues ▫ Prostacyclin is a potent vasodilator and antiplatelet agent ▫ Deficient in pts with PH ▫ Improve symptoms ▫ Improve hemodynamics ▫ Overdosage causes hypotension and hyperdynamic state with high-output cardiac failure
PH • Prostanoids cont. ▫ Epoprostenol – only drug with proven survival benefit; 6 minute half-life Must be kept cold during storage and administration Continuous IV infusion thru tunneled catheter ▫ Treprostinil – not shown to improve survival; 3 hour half life Continuous SQ infusion ▫ Iloprost – inhaled route of administration; 6 -9 times a day (Q 2 hours while awake)
PH • ERA’s – improve sx and functional class; antagonizes vasoconstriction and smooth muscle proliferation ▫ Bosentan (Tracleer) – oral, BID LFT’s Anemia Fluid retention HA’s ▫ Ambrisentan (Letairis) – oral, QD Fluid retention
PH • PDE-5’s – improve sx and functional class; augments vasodilatory effects of nitric oxide ▫ Sildenafil (Revatio) – oral, TID HA’s Flu-like sx Flushing Epistaxis
PH • NYHA classification of functional status of pts with PH ▫ I – no limitations in nl physical activity ▫ II – mild limitation, no sx at rest, worsening sx with exertion ▫ III – marked limitation, no sx at rest, worsening sx with light activity ▫ IV – sx at rest, unable to do any activity, signs of RV failure at rest
PH • Treatment by Classification ▫ I – monitor ▫ II – oral sildenafil (Revatio) ▫ III – oral sildenafil or bosentan (Tracleer) and inhaled or intravenous prostanoids ▫ IV – intravenous prostanoids
PH • Goals of Treatment ▫ ▫ Improvement to class I or II Improvement in the 6 MWDT to 380 m or better Max SBP with exercise of 120 mm Hg or greater Decrease in BNP to < 180 pg/ml

PH • Other treatments ▫ Surgery Atrial septostomy – decrease right-sided pressures, may worsen hypoxia Lung transplant – curative, post op median survival 5 years Pulmonary thromboendarterectomy – curative for PH from chronic PTED, tx of choice in appropriate candidates
PH • Upcoming therapies ▫ Treprostinil – infusion and inhaled available now, working on oral formulation ▫ Sitaxsentan – approved in Europe, application is pending with FDA ▫ Tadalafil (Cialis) – longer half-life and greater selectivity and potency than sildenafil; in trials now
PH • Prognosis ▫ 1980 s – grim, medial survival of 2. 8 years from time of diagnosis in untreated pts ▫ Current – newer medications have greatly improved the outlook for pts with PH ▫ Poor prognostic indicators – low 6 MWDT; pericardial effusion, RV dysfunction, and RAE on ECHO; increased m. RAP (the most powerful hemodynamic predictor) and decreased cardiac index on RHC; and elevated BNP
 Pulmonary hypertension
Pulmonary hypertension Paedp echo
Paedp echo Mitral stenosis pulmonary hypertension
Mitral stenosis pulmonary hypertension Stages of pulmonary hypertension
Stages of pulmonary hypertension Nt pro brain natriuretic peptide
Nt pro brain natriuretic peptide Dianne zwicke
Dianne zwicke Pulmonary hypertension
Pulmonary hypertension Pulmonary hypertension definition
Pulmonary hypertension definition Chd pulmonary hypertension
Chd pulmonary hypertension Pah vs pulmonary hypertension
Pah vs pulmonary hypertension Pathophysiology of pulmonary hypertension
Pathophysiology of pulmonary hypertension Bmpr gene
Bmpr gene Intracranial hypertension
Intracranial hypertension Hypokalemia
Hypokalemia Esterman efficiency score 92
Esterman efficiency score 92 Gestational hypertension symptoms
Gestational hypertension symptoms Cld chronic liver disease
Cld chronic liver disease Essential hypertension
Essential hypertension Circulation veineuse collatérale porto cave
Circulation veineuse collatérale porto cave Health coaches for hypertension control
Health coaches for hypertension control Hypertension artérielle
Hypertension artérielle Jnc 7 hypertension
Jnc 7 hypertension Medical nutrition therapy for hypertension
Medical nutrition therapy for hypertension