Second Heart Sound Key to Auscultation Dr I








- Slides: 31
Second Heart Sound Key to Auscultation Dr. I. Sathyamurthy MD, DM, FACC FRCP (Edin), FRCP (Glas), DSc (Honoris Causa) Sr. Interventional Cardiologist Apollo Hospitals, Chennai.
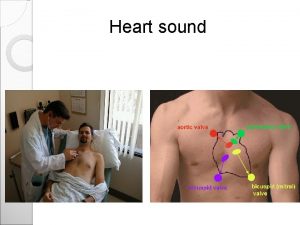
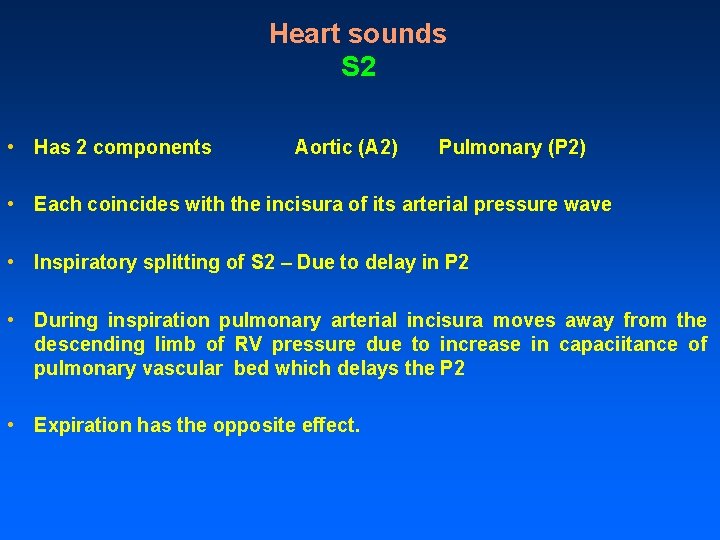
Heart sounds S 2 • Has 2 components Aortic (A 2) Pulmonary (P 2) • Each coincides with the incisura of its arterial pressure wave • Inspiratory splitting of S 2 – Due to delay in P 2 • During inspiration pulmonary arterial incisura moves away from the descending limb of RV pressure due to increase in capaciitance of pulmonary vascular bed which delays the P 2 • Expiration has the opposite effect.
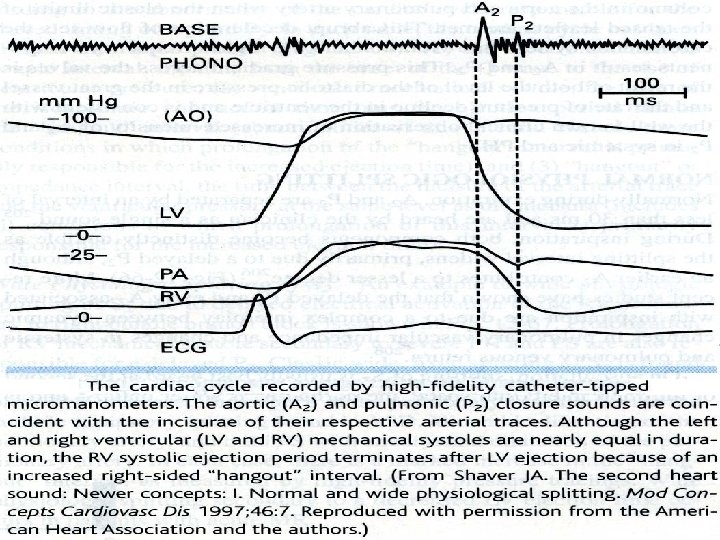
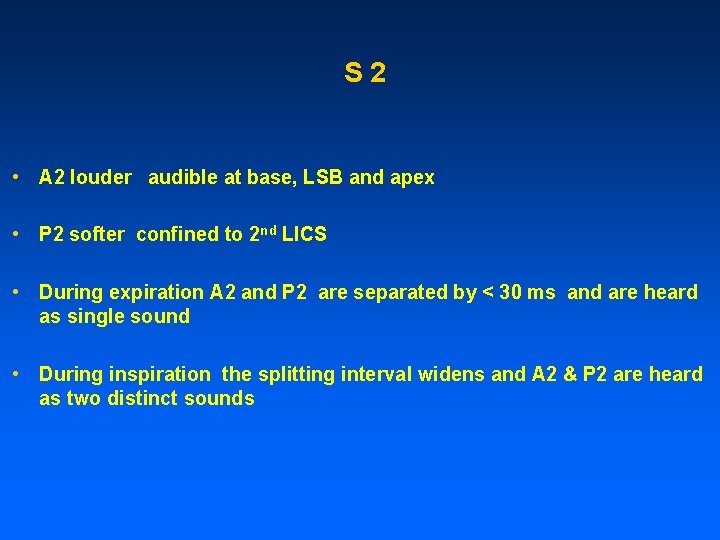
S 2 • A 2 louder audible at base, LSB and apex • P 2 softer confined to 2 nd LICS • During expiration A 2 and P 2 are separated by < 30 ms and are heard as single sound • During inspiration the splitting interval widens and A 2 & P 2 are heard as two distinct sounds
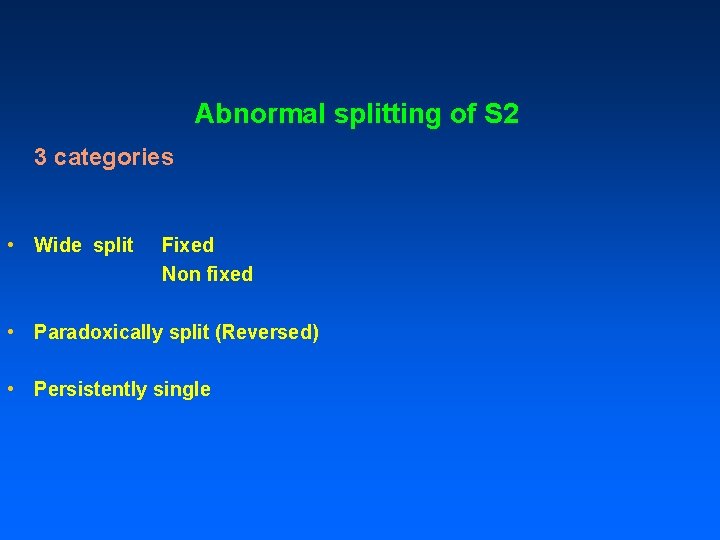
Abnormal splitting of S 2 3 categories • Wide split Fixed Non fixed • Paradoxically split (Reversed) • Persistently single

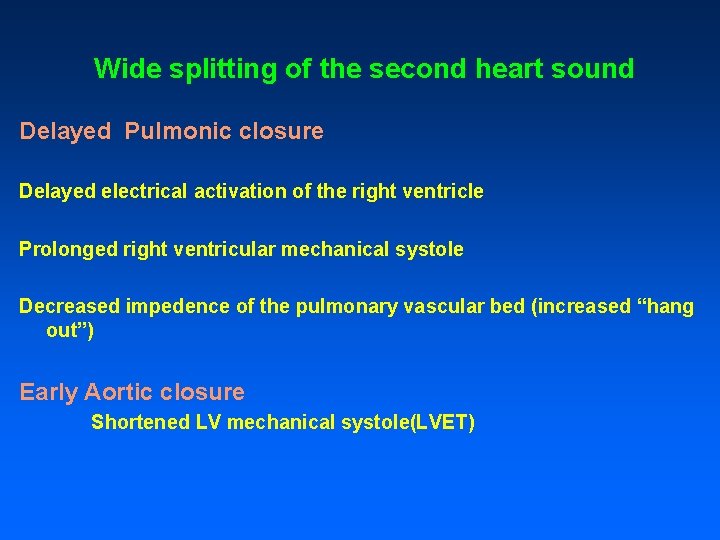
Wide splitting of the second heart sound Delayed Pulmonic closure Delayed electrical activation of the right ventricle Prolonged right ventricular mechanical systole Decreased impedence of the pulmonary vascular bed (increased “hang out”) Early Aortic closure Shortened LV mechanical systole(LVET)
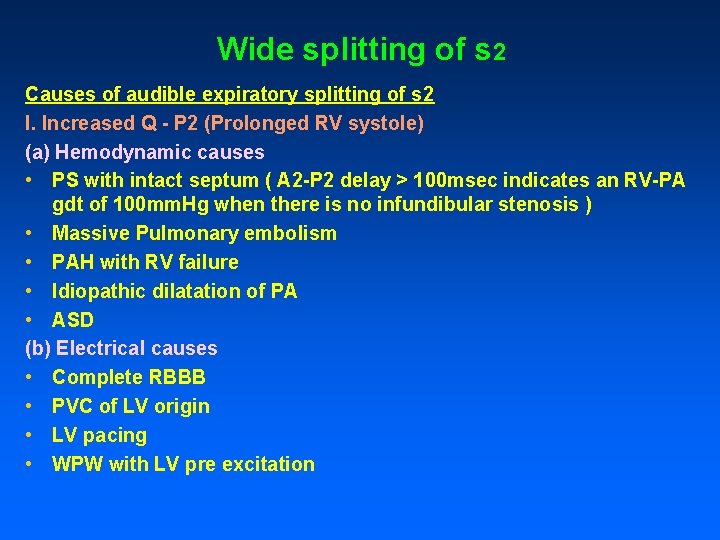
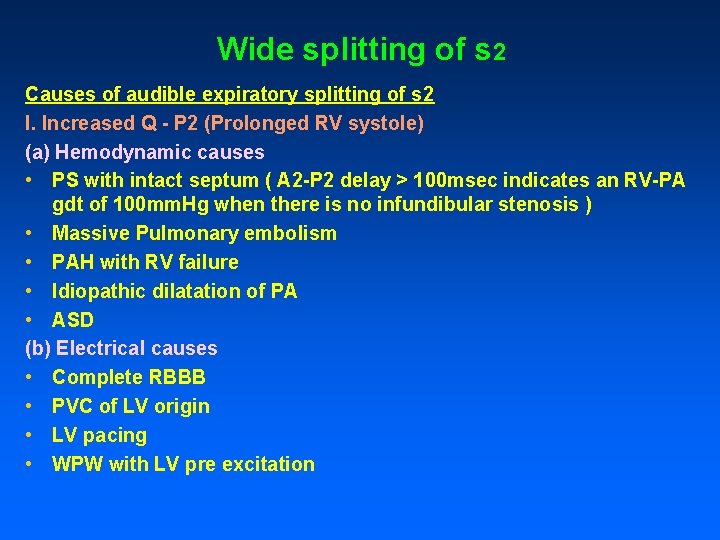
Wide splitting of s 2 Causes of audible expiratory splitting of s 2 I. Increased Q - P 2 (Prolonged RV systole) (a) Hemodynamic causes • PS with intact septum ( A 2 -P 2 delay > 100 msec indicates an RV-PA gdt of 100 mm. Hg when there is no infundibular stenosis ) • Massive Pulmonary embolism • PAH with RV failure • Idiopathic dilatation of PA • ASD (b) Electrical causes • Complete RBBB • PVC of LV origin • LV pacing • WPW with LV pre excitation
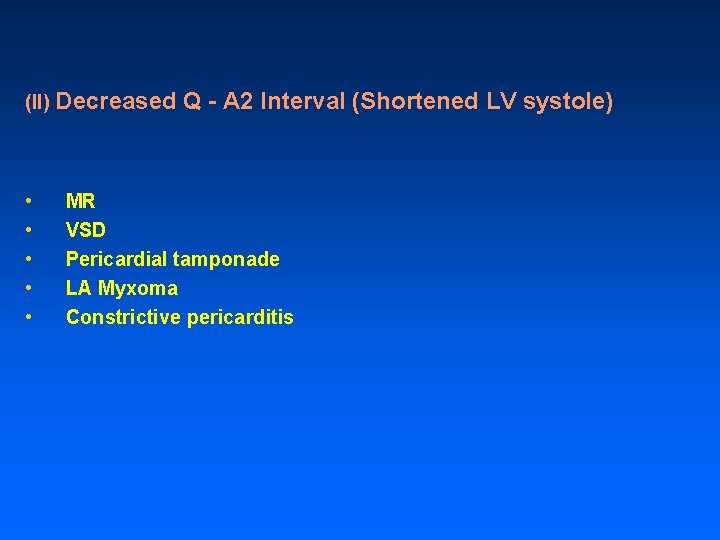
(II) Decreased • • • Q - A 2 Interval (Shortened LV systole) MR VSD Pericardial tamponade LA Myxoma Constrictive pericarditis
Wide split s 2 in Cyanotic heart disease • • • TAPVC Single atrium Ebsteins anamoly of tricuspid valve ASD Eisenmenger ASD with left to rt shunt ASD with PS and right to left shunt at atrial level • Primary Pulmonary hypertension Miscellaneous • Pectus excavatum • Occasionally normal children • Straight back syndrome
Fixed S 2 split Interval between A 2 & P 2 is wide and persistent and remains unchanged during respiratory cycle • Hallmark finding of ASD • Delay in P 2 is due to Pulmonary vascular bed capacitance – and Hangout interval ( interval between descending limbs of PA and RV pressure pulses ) – Split is wide • No significant respiratory variations in RV filling due to reciprocal changes in volume of left to right shunt – Split is fixed

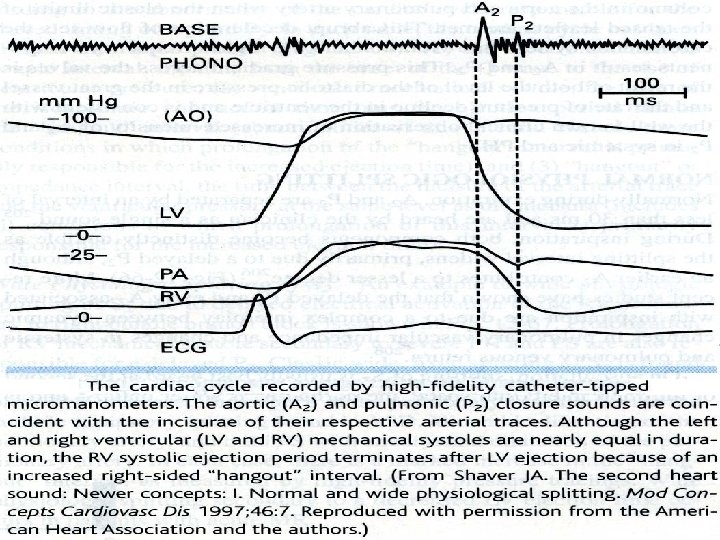
What is hangout interval? • Semilunar valve is expected to close at point of cross over of ventricular and arterial pressure. • In reality it is not so • Time interval from cross over of pressures to actual occurrence of sound is called HANGOUT interval. • Just like a rolling ball is stopped by the friction offered by the ground, the ejection of blood is stopped by the resistance offered by the pulmonary vasculature
• Since the pulmonary vascular resistance is low compared to the systemic vascular resistance, it takes some time for the blood flow from the right ventricle to stop • This corresponds to the hangout interval. • On the left side of the heart because impedance is much greater, the hangout interval between the aorta and LV pressure curves is negligible • Hang out interval may vary from 30 to 120 msec in the pulmonary vascular bed.

• Hangout interval depends on interrelated factors like : • pressure beyond the valve • dilatation of the artery • distensibility of arterial system • vascular impedance • phase of respiration.


Reverse Splitting of the second heart sound • Delayed Aortic closure Delayed electrical activation of the LV Complete LBBB (Proximal type) RV paced beat RV ectopic beats Prolonged left ventricular mechanical systole Complete LBBB LVOT obstruction Hypertensive heart disease Arteriosclerotic heart disease Chronic IHD
Contd, Decreased impedence of the systemic vascular bed (increased “hang out”) Post stenotic dilatation of the aorta secondary to AS or AR PDA Early pulmonic closure Early electrical activation of the RV WPW syndrome type B

TYPES OF REVERSE SPLIT Type 1: Classical reverse split Ø During expiration prolonged LV systole causes A 2 to follow P 2. with inspiration Q-P 2 increased normally but Q-A 2 is unchanged or shorten resulting a single second sound Type 2: S 2 reversal only in expiration(P 2 -A 2), normal in inspiration(A 2 -P 2) Ø In lesser degrees of Q-A 2 delay , inspiration may still result in normal A 2 P 2 relationship and audible splitting, although s 2 reversal occurs in expiration.
Reversed or parodoxic splitting Type 3 paradoxical split : S 2 single in both phases of respiration (reverse split not detected by human ear as interval is < 20 msec both in inspiration and expiration) • Pseudo Reverse Split Only Type I Paradoxic splitting can be detected bedside. Type III can be diagnosed only by Phonocardiography. Type II and
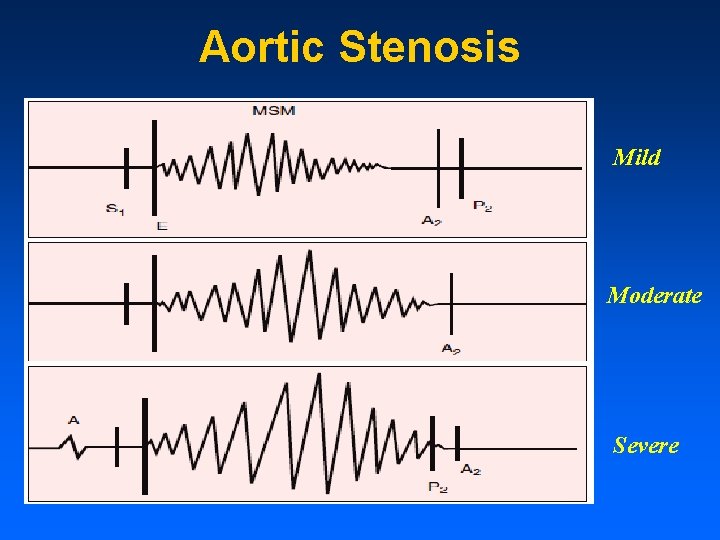
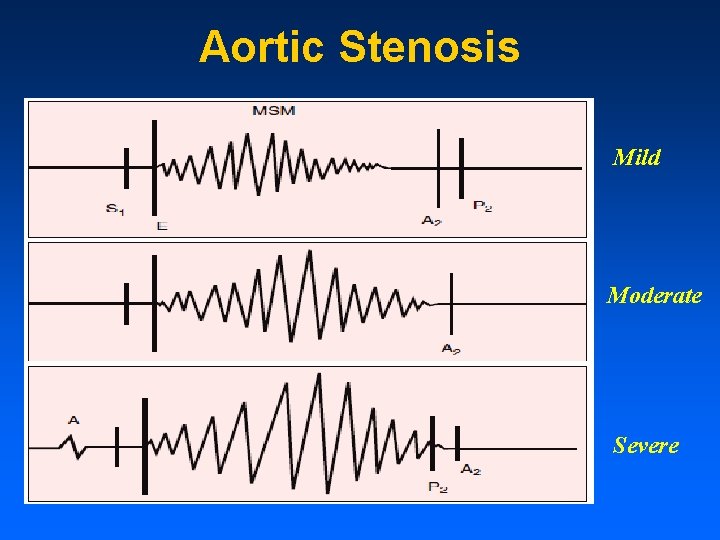
Aortic Stenosis Mild Moderate Severe
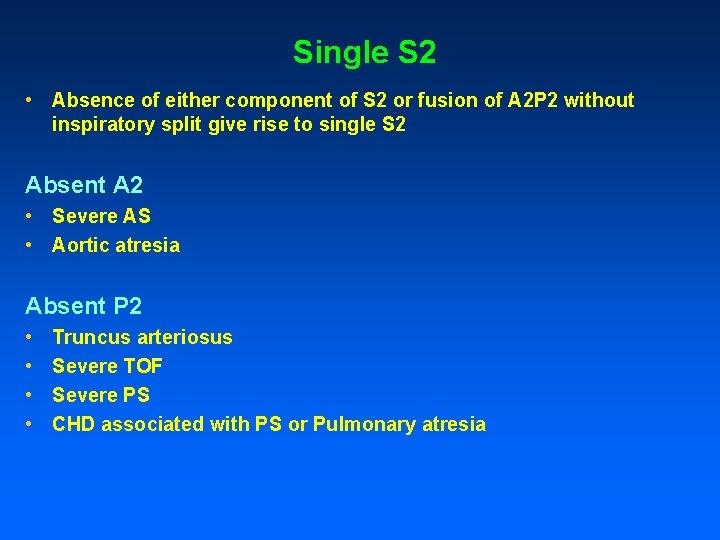
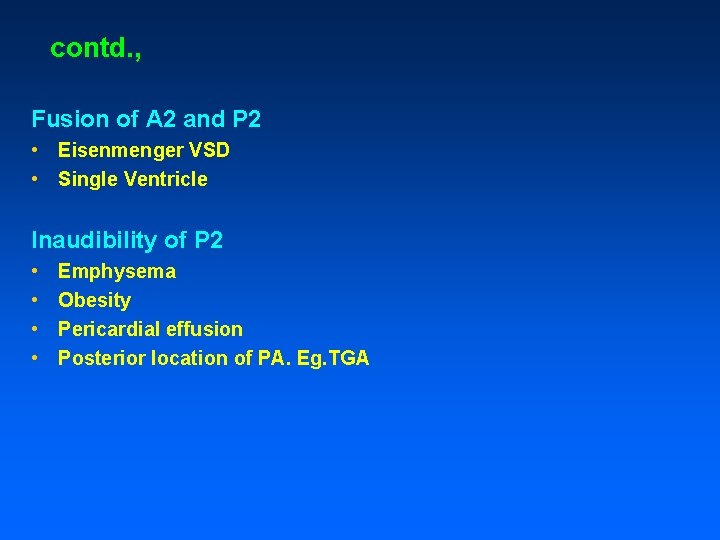
Single S 2 • Absence of either component of S 2 or fusion of A 2 P 2 without inspiratory split give rise to single S 2 Absent A 2 • Severe AS • Aortic atresia Absent P 2 • • Truncus arteriosus Severe TOF Severe PS CHD associated with PS or Pulmonary atresia
contd. , Fusion of A 2 and P 2 • Eisenmenger VSD • Single Ventricle Inaudibility of P 2 • • Emphysema Obesity Pericardial effusion Posterior location of PA. Eg. TGA
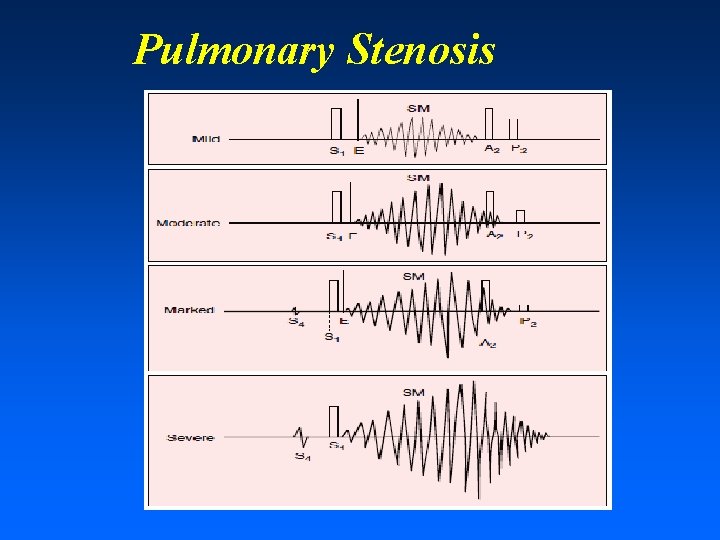
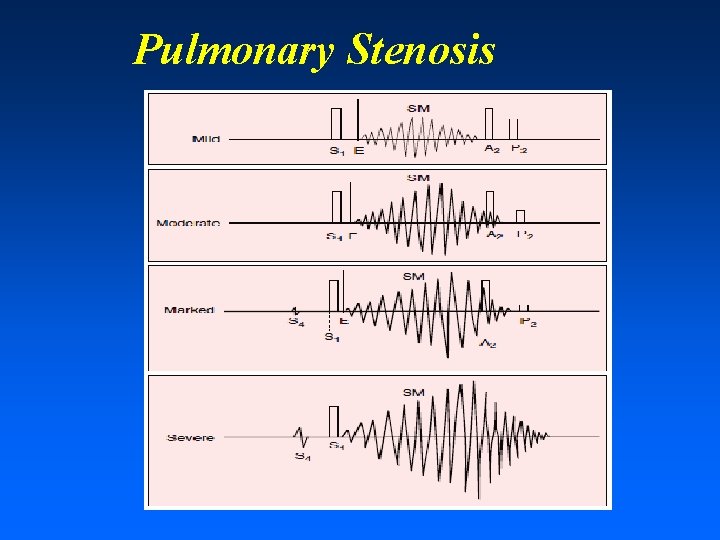
Pulmonary Stenosis
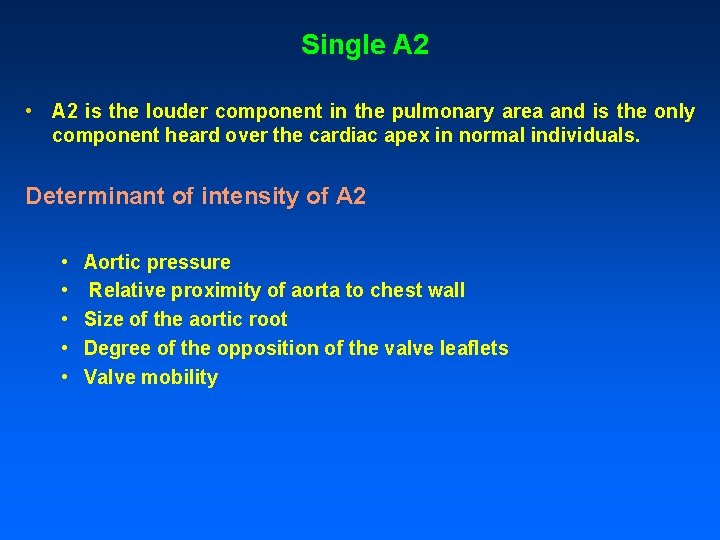
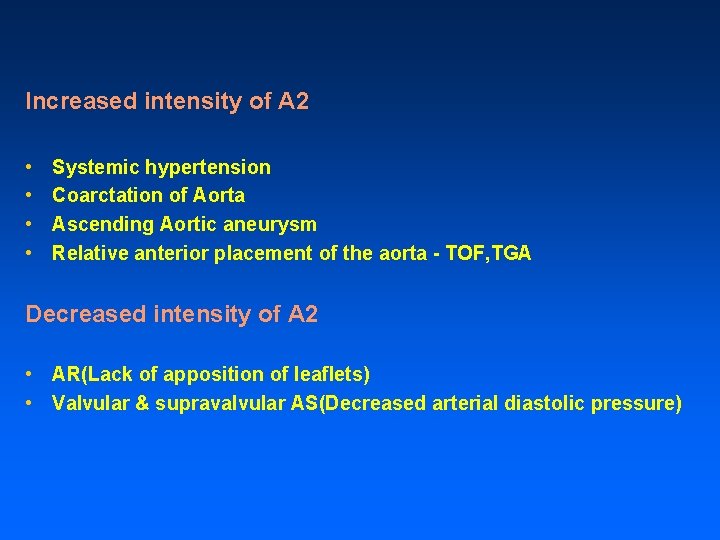
Single A 2 • A 2 is the louder component in the pulmonary area and is the only component heard over the cardiac apex in normal individuals. Determinant of intensity of A 2 • • • Aortic pressure Relative proximity of aorta to chest wall Size of the aortic root Degree of the opposition of the valve leaflets Valve mobility
Increased intensity of A 2 • • Systemic hypertension Coarctation of Aorta Ascending Aortic aneurysm Relative anterior placement of the aorta - TOF, TGA Decreased intensity of A 2 • AR(Lack of apposition of leaflets) • Valvular & supravalvular AS(Decreased arterial diastolic pressure)

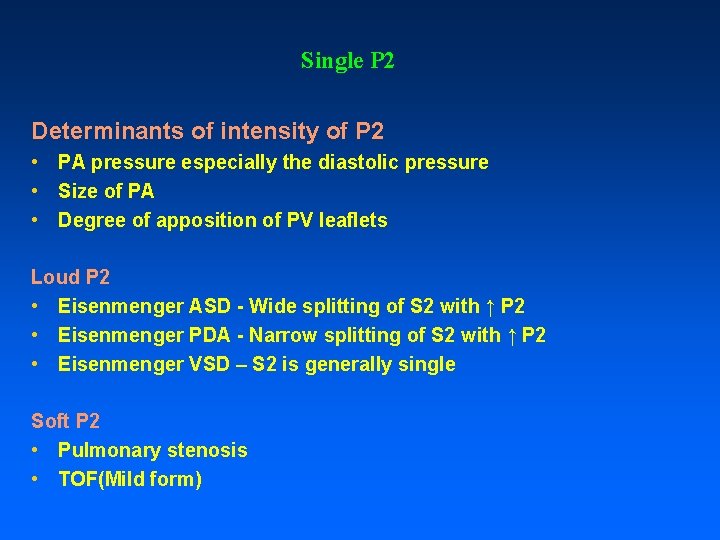
Single P 2 Increased intensity of P 2 • Normally P 2 is not audible at the apex. If P 2 is louder than A 2 in 2 nd LICS or if it is audible at the apex- It is termed loud and indicates PAH • In ASD P 2 may be audible at the apex in the absence of PAH because of RV enlargement and RV occupies the apex. • If P 2 is very loud and banging it correlates to approximate mean PA pressure of > 50 mm. Hg
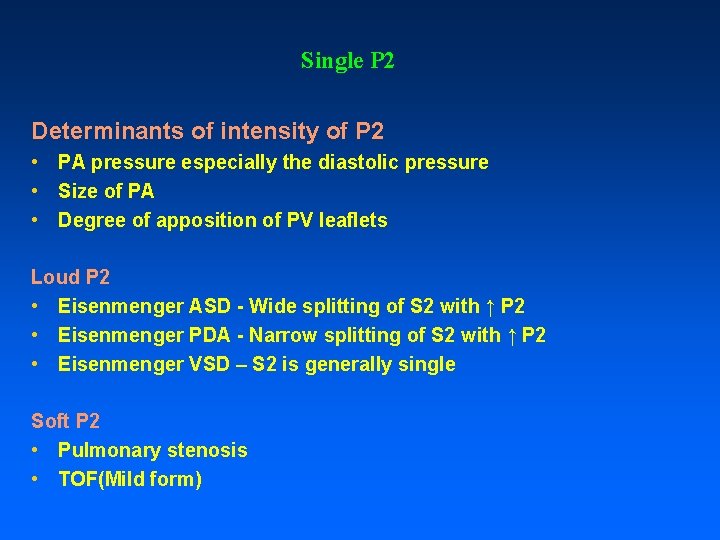
Single P 2 Determinants of intensity of P 2 • PA pressure especially the diastolic pressure • Size of PA • Degree of apposition of PV leaflets Loud P 2 • Eisenmenger ASD - Wide splitting of S 2 with ↑ P 2 • Eisenmenger PDA - Narrow splitting of S 2 with ↑ P 2 • Eisenmenger VSD – S 2 is generally single Soft P 2 • Pulmonary stenosis • TOF(Mild form)
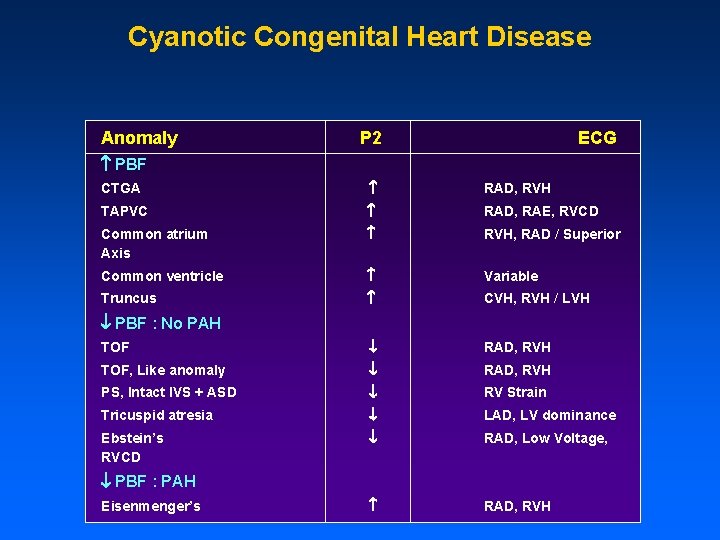
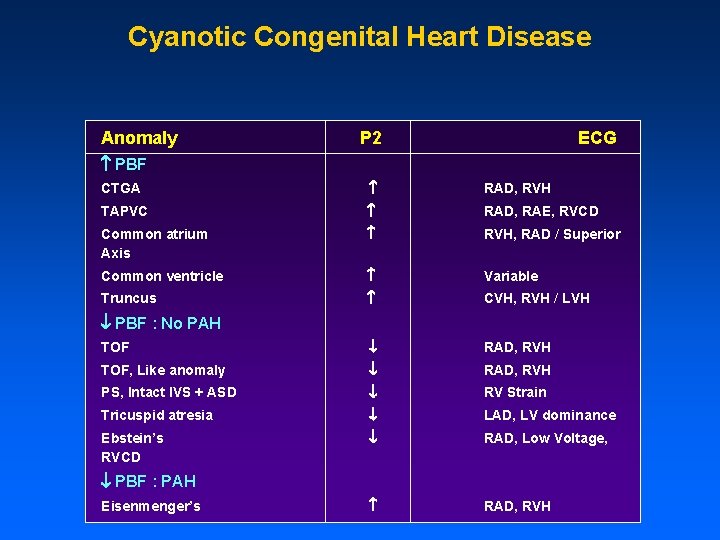
Cyanotic Congenital Heart Disease Anomaly P 2 ECG PBF CTGA RAD, RVH TAPVC RAD, RAE, RVCD Common atrium Axis RVH, RAD / Superior Common ventricle Variable Truncus CVH, RVH / LVH TOF RAD, RVH TOF, Like anomaly RAD, RVH PS, Intact IVS + ASD RV Strain Tricuspid atresia LAD, LV dominance Ebstein’s RVCD RAD, Low Voltage, RAD, RVH PBF : No PAH PBF : PAH Eisenmenger’s
Phonocardiography • • Single Vs Closed split Confirmation P 2 or A 2 Reversed Splitting For teaching purpose

Thank You
 S1 is loudest at the base of the heart
S1 is loudest at the base of the heart Splitting of second heart sound
Splitting of second heart sound Grading murmur
Grading murmur Auscultation of heart sounds
Auscultation of heart sounds Auscultation of heart sounds
Auscultation of heart sounds Left sternal border
Left sternal border 27 miles per gallon into kilometers per liter
27 miles per gallon into kilometers per liter Apical pulse location
Apical pulse location Scapula mobility
Scapula mobility Inspection auscultation percussion palpation
Inspection auscultation percussion palpation Tactical combat casualty care
Tactical combat casualty care Foyer aortique
Foyer aortique Foyer cardiaque
Foyer cardiaque Pneumothorax auscultation findings
Pneumothorax auscultation findings Bimanual palpation of spleen
Bimanual palpation of spleen Auscultation of apical pulse
Auscultation of apical pulse Tidal percussion
Tidal percussion Focused gastrointestinal assessment
Focused gastrointestinal assessment Inspection palpation percussion auscultation
Inspection palpation percussion auscultation Chapter 38 assisting with a general physical examination
Chapter 38 assisting with a general physical examination Costovertebral angle tenderness
Costovertebral angle tenderness Inspection auscultation percussion palpation
Inspection auscultation percussion palpation Left parasternal heave
Left parasternal heave Inspection auscultation percussion palpation
Inspection auscultation percussion palpation Joel niznick
Joel niznick Apical pulse auscultation location
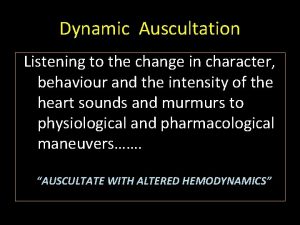
Apical pulse auscultation location Dynamic auscultation
Dynamic auscultation Site:slidetodoc.com
Site:slidetodoc.com 5 point auscultation
5 point auscultation Grey horn
Grey horn “a sound mind is in a sound body”
“a sound mind is in a sound body” Tiny astronauts
Tiny astronauts