Surgical Treatment Of Habitual Dislocation Of The Patella
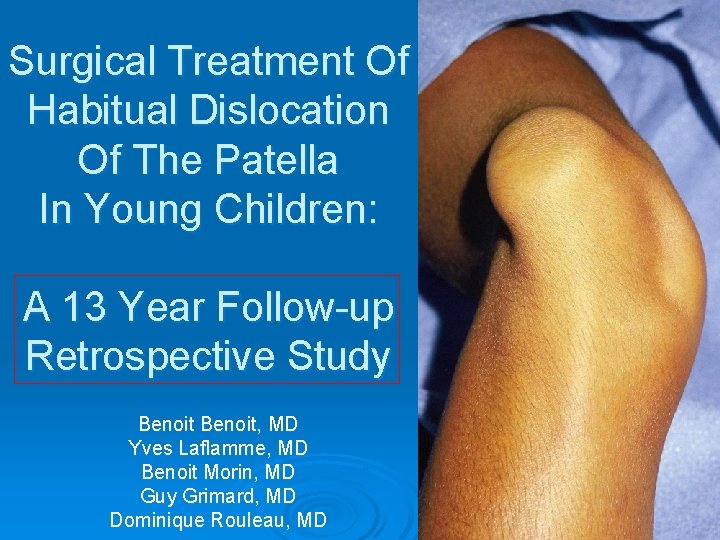
Surgical Treatment Of Habitual Dislocation Of The Patella In Young Children: A 13 Year Follow-up Retrospective Study Benoit, MD Yves Laflamme, MD Benoit Morin, MD Guy Grimard, MD Dominique Rouleau, MD
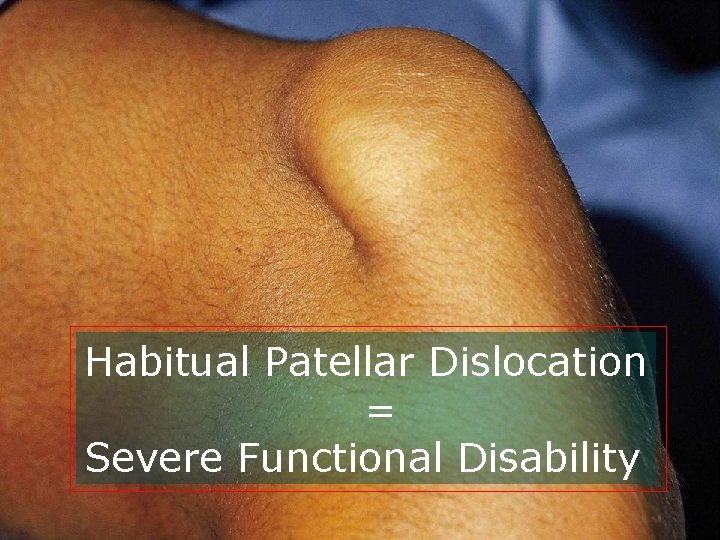
Habitual Patellar Dislocation = Severe Functional Disability
Habitual Patellar Dislocation Ø Dislocation occurs with activities of daily living Ø Sporting activities are almost impossible
Factors* Of Patellar Instability (Six) *Insall and Salvati, 2001
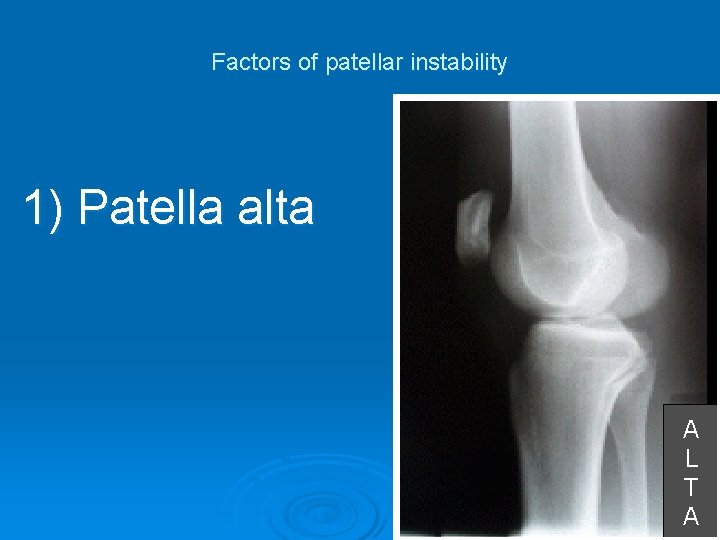
Factors of patellar instability 1) Patella alta A L T A
Radiologic Patellar Height Assessment In The Immature Patient l Koshino-Sugimoto l Caton-Deschamps
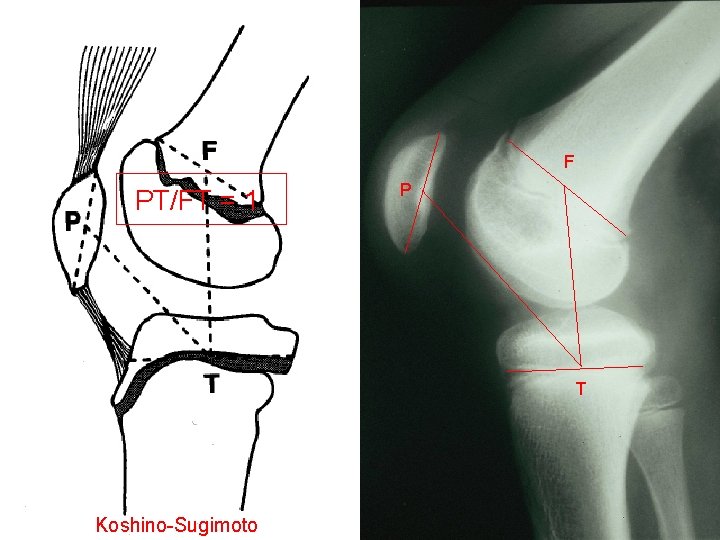
FF PT/FT = 1 P P T Koshino-Sugimoto
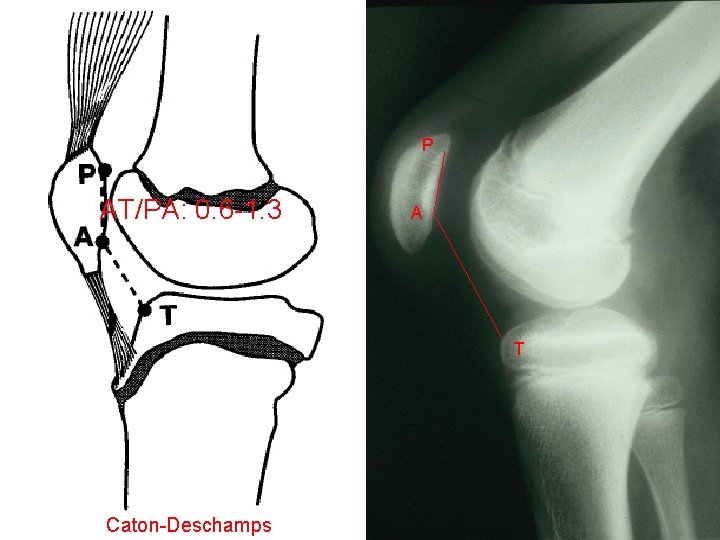
P AT/PA: 0. 6 -1. 3 P A A T T Caton-Deschamps
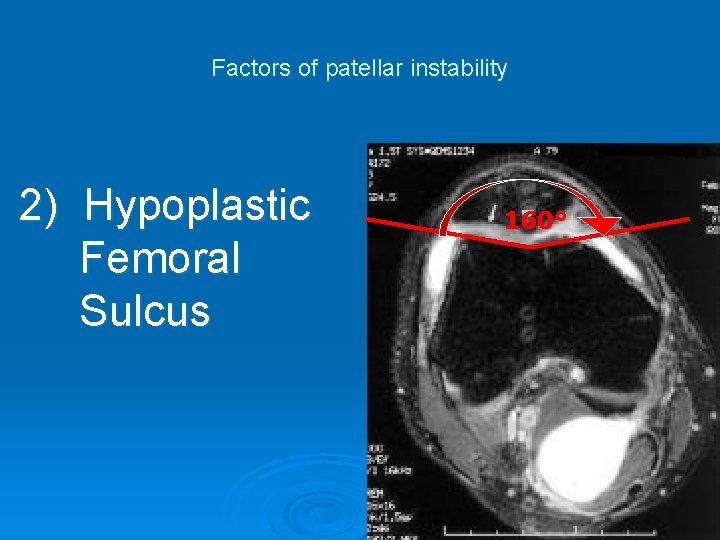
Factors of patellar instability 2) Hypoplastic Femoral Sulcus 160°
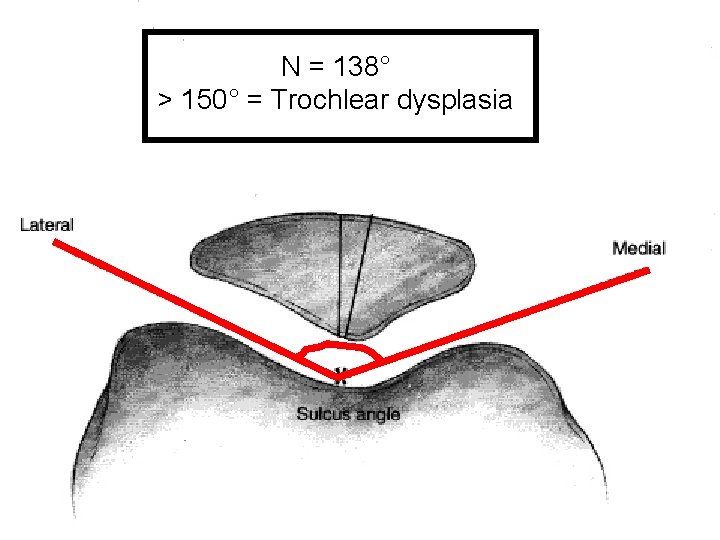
N = 138° > 150° = Trochlear dysplasia
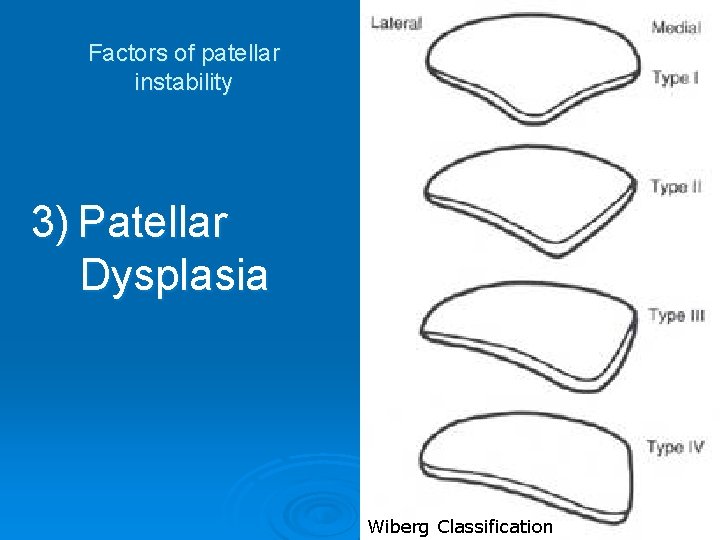
Factors of patellar instability 3) Patellar Dysplasia Wiberg Classification
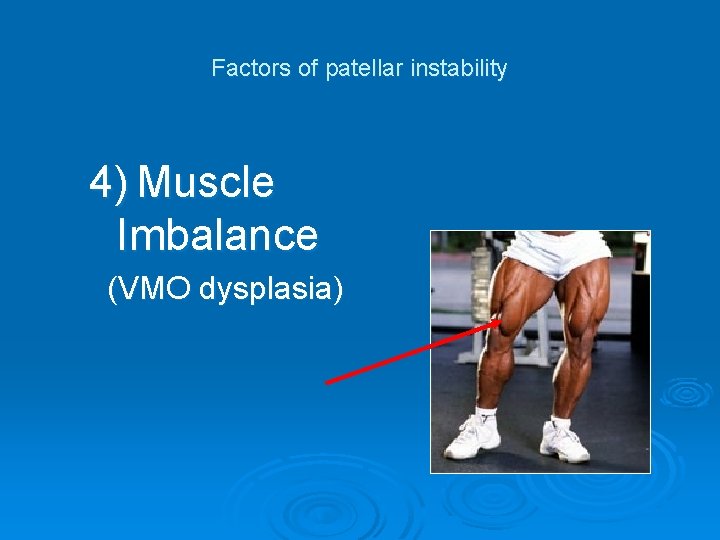
Factors of patellar instability 4) Muscle Imbalance (VMO dysplasia)
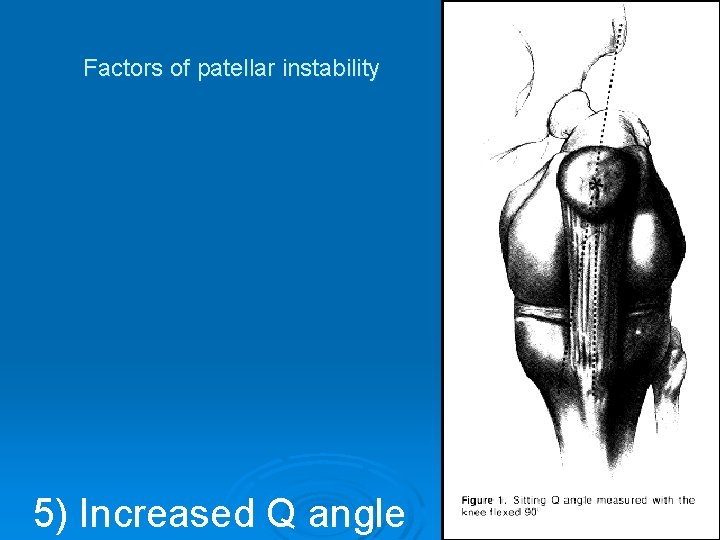
Factors of patellar instability 5) Increased Q angle
Factors of patellar instability 6) Lower Limb Malalignment

Treatment options?
Ø No study addresses specifically habitual patellar dislocation in the young child

Treatment Options Ø Conservative l Physical therapy l Knee bracing Ø Surgical

Does knee bracing prevent habitual patellar dislocation ?
Does physical therapy prevent habitual patellar dislocation ?


Recurrence rate: 40% + Garth, Am J Sports Med, 1996

Ø Surgical treatment
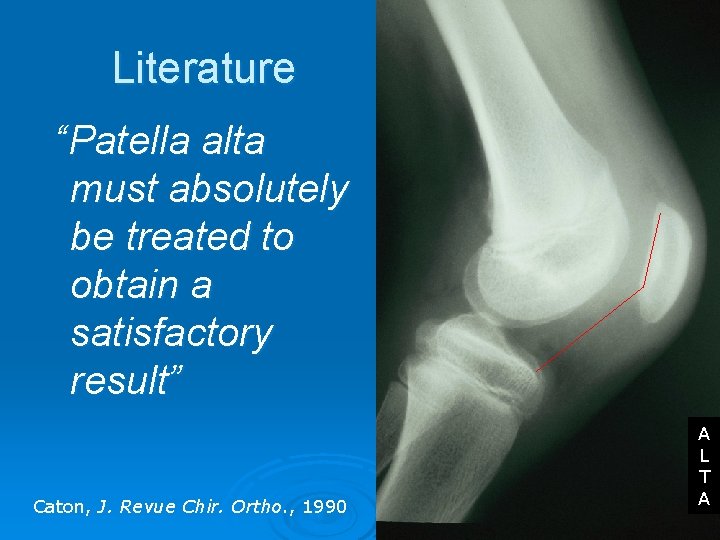
Literature “Patella alta must absolutely be treated to obtain a satisfactory result” Caton, J. Revue Chir. Ortho. , 1990 A L T A
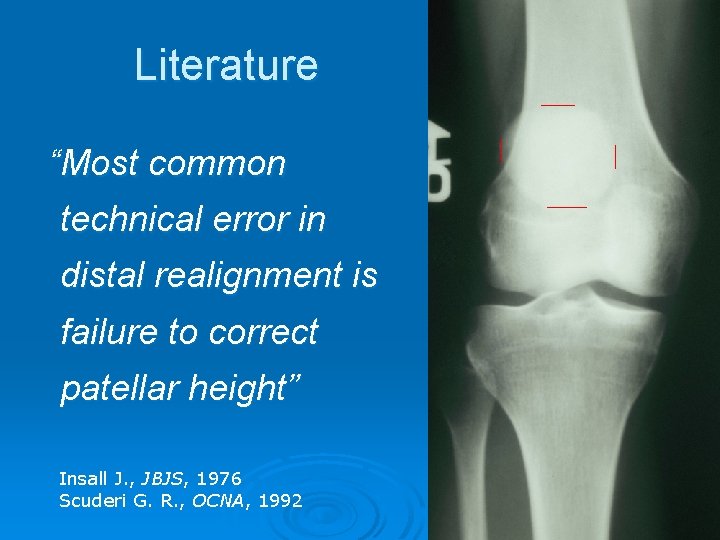
Literature “Most common technical error in distal realignment is failure to correct patellar height” Insall J. , JBJS, 1976 Scuderi G. R. , OCNA, 1992 A L T A
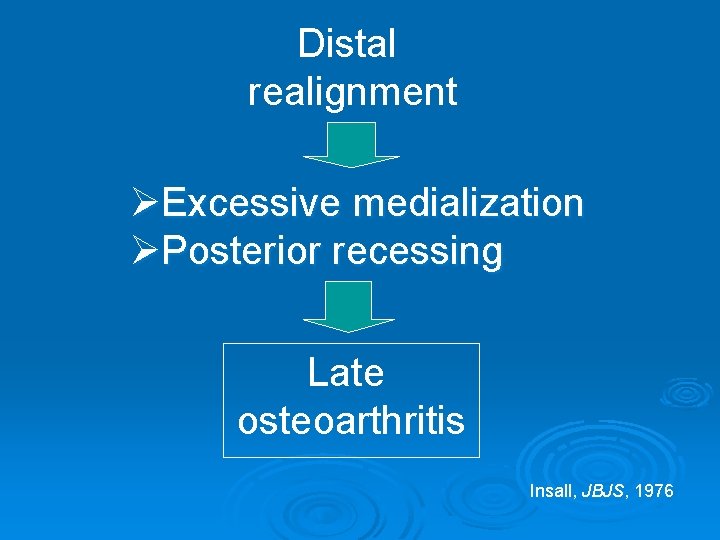
Distal realignment ØExcessive medialization ØPosterior recessing Late osteoarthritis Insall, JBJS, 1976
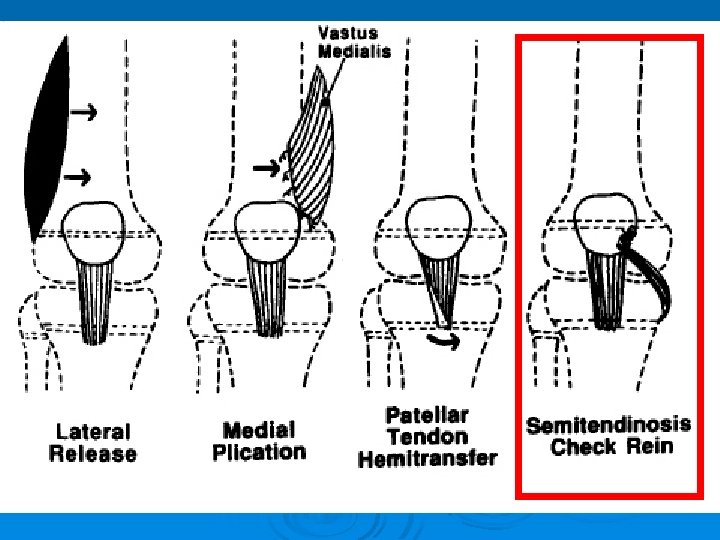
Surgical Options In The Patient With Open Physis Ø Roux-Golthwait Ø Galeazzi
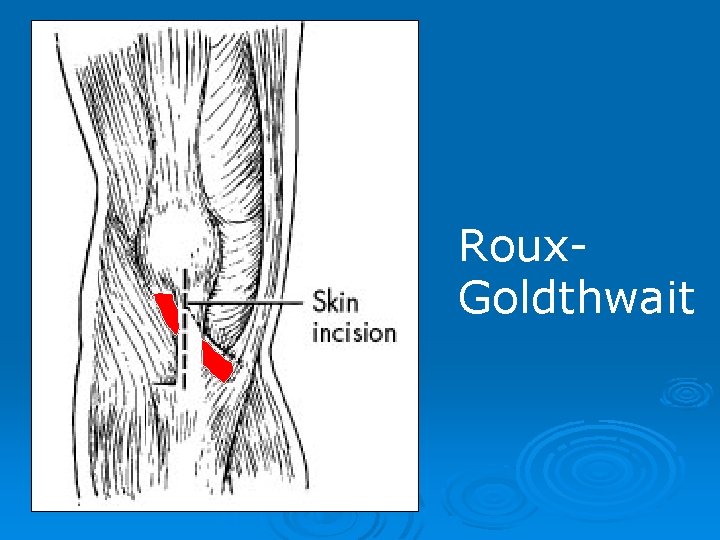
Roux. Goldthwait
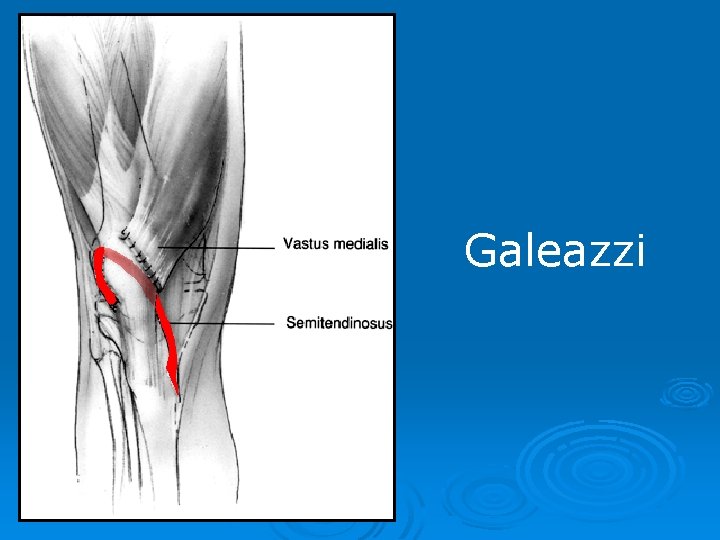
Galeazzi
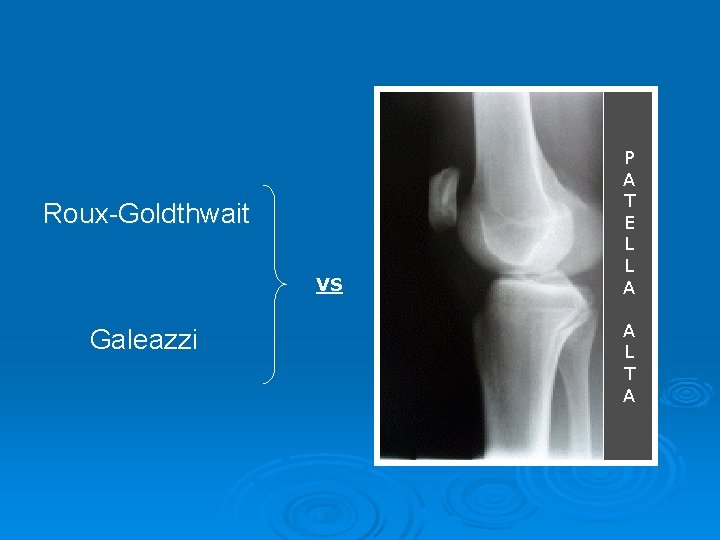
Roux-Goldthwait VS Galeazzi P A T E L L A A L T A

Roux-Goldthwait Galeazzi P A T E L L A A L T A
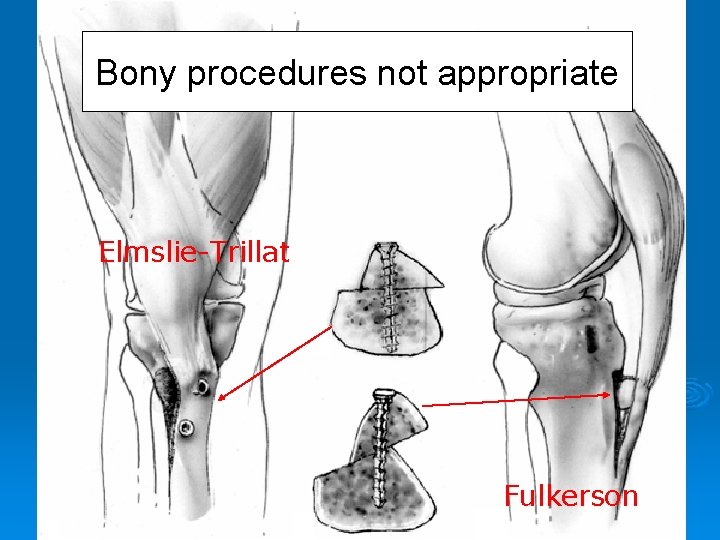
Bony procedures not appropriate Elmslie-Trillat Fulkerson

Tibial tubercule transfer on the knee with open physis Genu recurvatum
Goal of our study Clinical evaluation of a new procedure to correct patella alta in children with patellar instability Long term follow-up (13. 8 years)
Materials and methods Ø Retrospective study
Materials and methods Ø Retrospective study Ø 12 consecutive knees treated surgically in young children from 1988 to 1994
Materials and methods Ø Retrospective study Ø 12 knees in young children treated surgically Ø Follow-up: 10 -17 years (mean 13. 8 years)
Materials and methods Ø Retrospective study Ø 12 knees in young children treated surgically Ø Follow-up: 10 -17 years (mean 13. 8 years) Ø Mean age at surgery: 10 years 14 years) (6 -
Materials and methods Ø Retrospective study Ø 12 knees in young children treated surgically Ø Follow-up: 10 -17 years (mean 13. 8 years) Ø Mean age at surgery: 10 years (6 -14 years) Ø Mean age at last follow-up: 25 years

Materials and methods Ø Inclusion criterias l Habitual patellar dislocation l Functional limitations in activities of daily living l Symptoms of more than 1 year duration

l Failure of conservative treatment (bracing and physical therapy) l Growth plates opened at time of surgery
Materials and methods Preoperative clinical evaluation l High-riding patella l VMO dysplasia l Normal Q-angle l Positive apprehension test l Lateral patellar laxity IV/IV
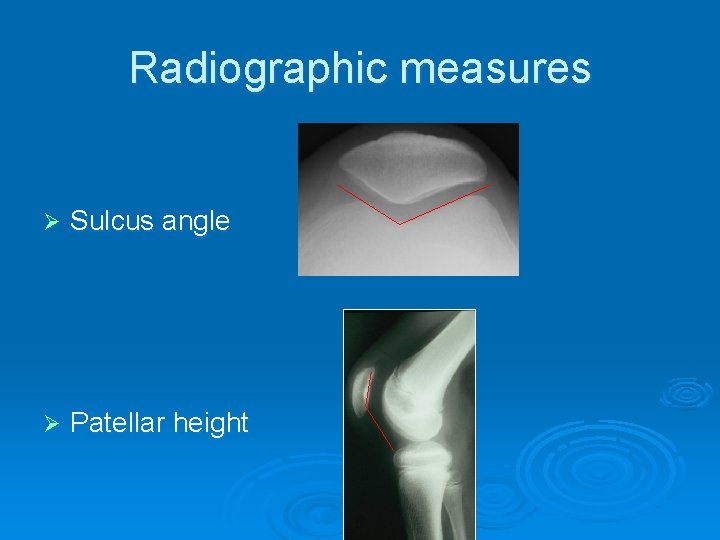
Radiographic measures Ø Sulcus angle Ø Patellar height
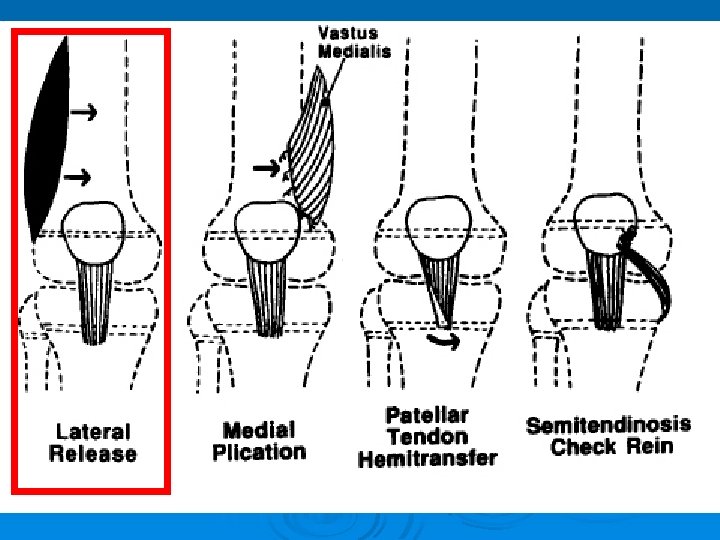
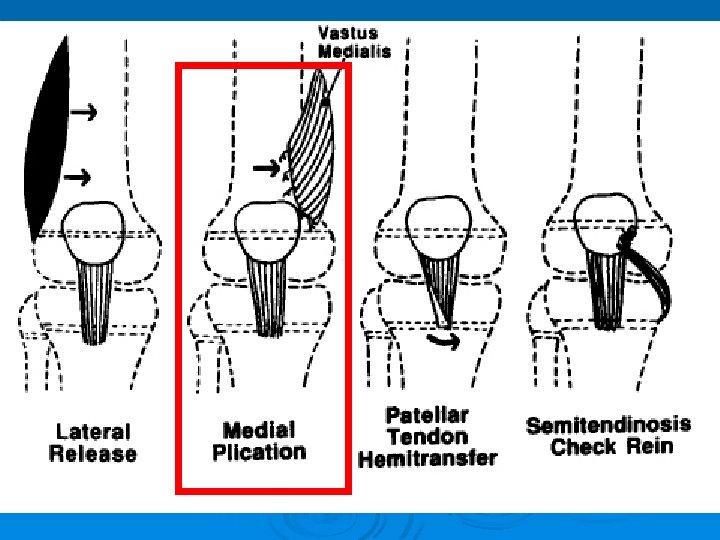
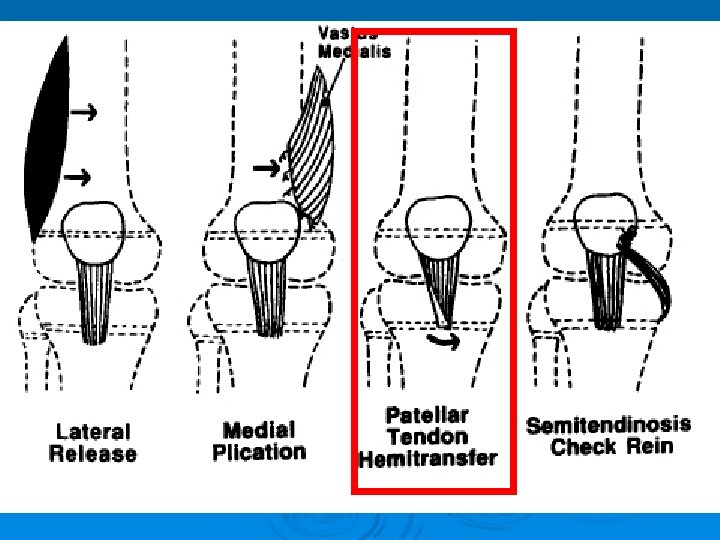
Surgical technique Proximal realignment: üLateral release Hughston technique üVMO advancement Distal realignment: üComplete patellar tendon lowering NEW!
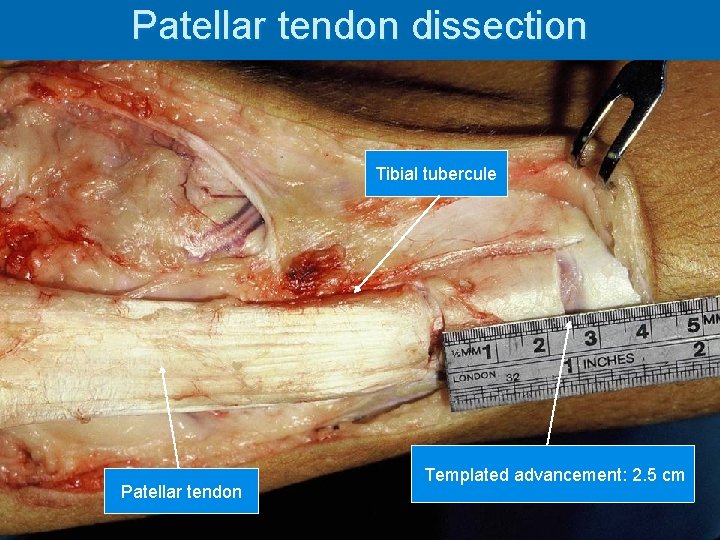
Patellar tendon dissection Tibial tubercule Patellar tendon Templated advancement: 2. 5 cm
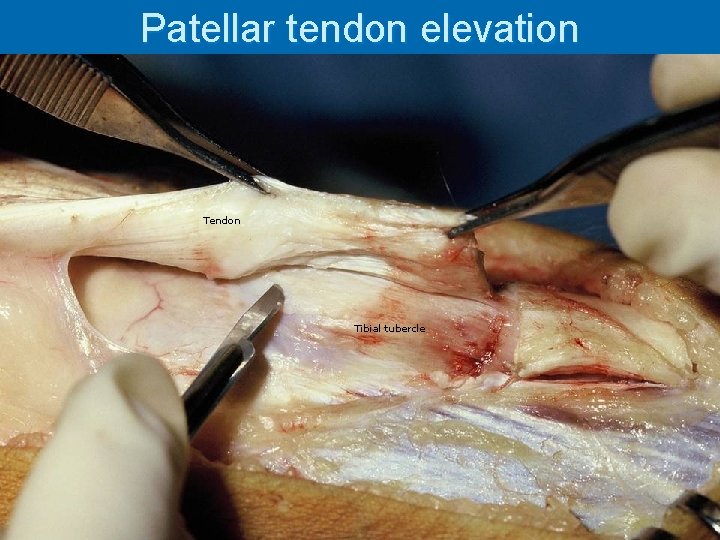
Patellar tendon elevation Tendon Tibial tubercle
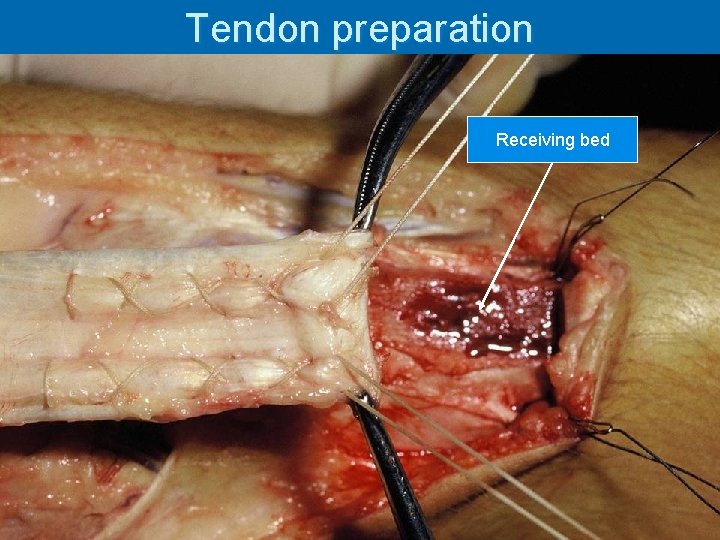
Tendon preparation Receiving bed Transosseous sutures
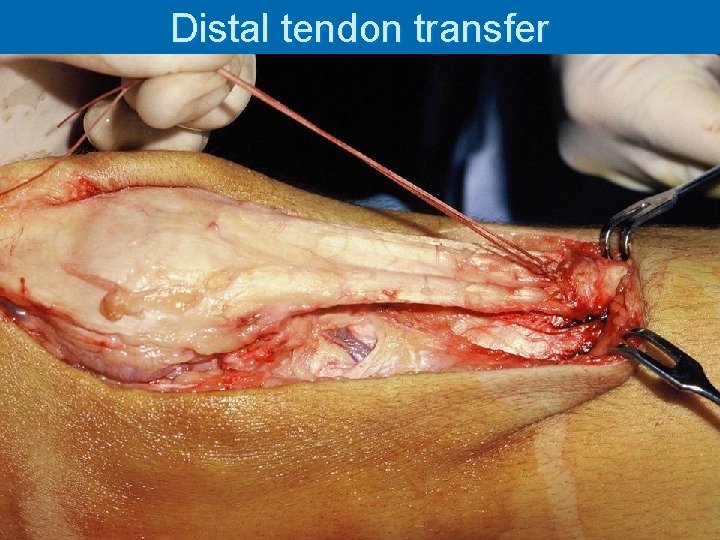
Distal tendon transfer
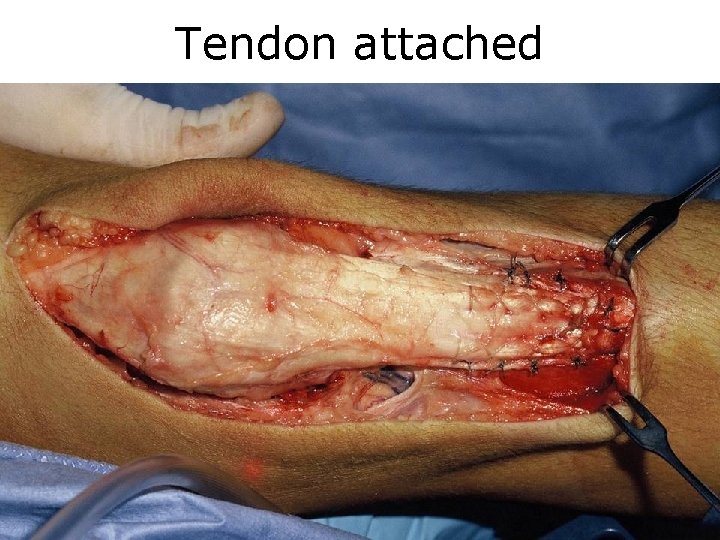
Tendon attached

Results
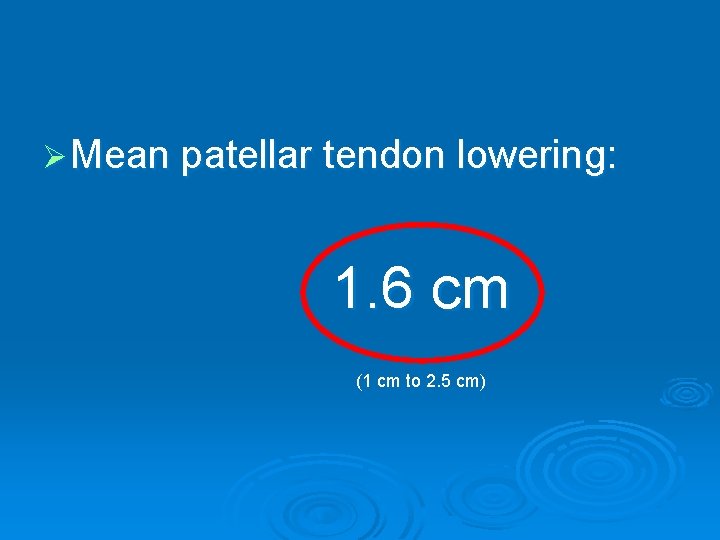
Ø Mean patellar tendon lowering: 1. 6 cm (1 cm to 2. 5 cm)
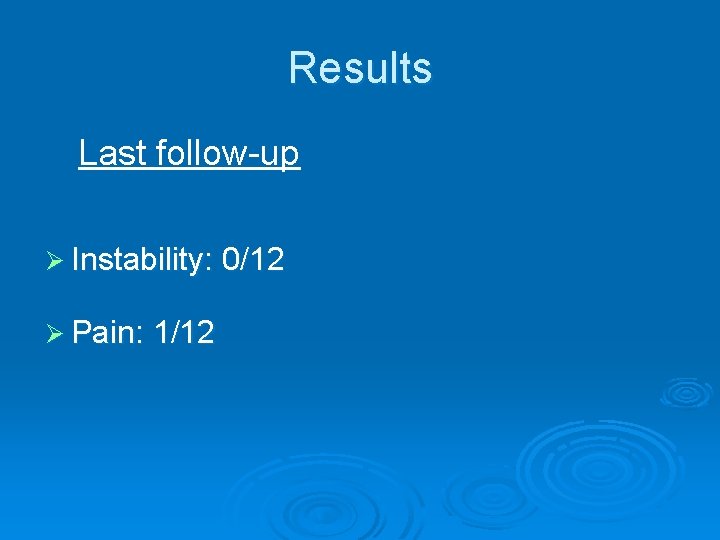
Results Last follow-up Ø Instability: 0/12 Ø Pain: 1/12
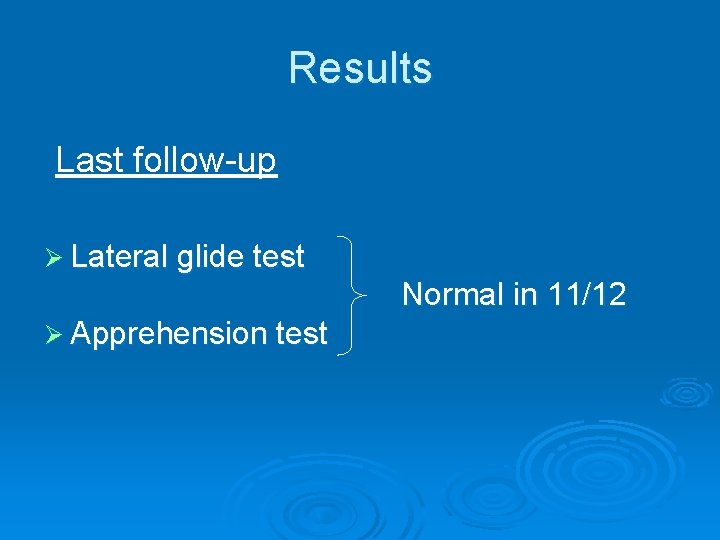
Results Last follow-up Ø Lateral glide test Normal in 11/12 Ø Apprehension test
Results Lysholm knee score at last follow-up: Ø Mean: 98/100
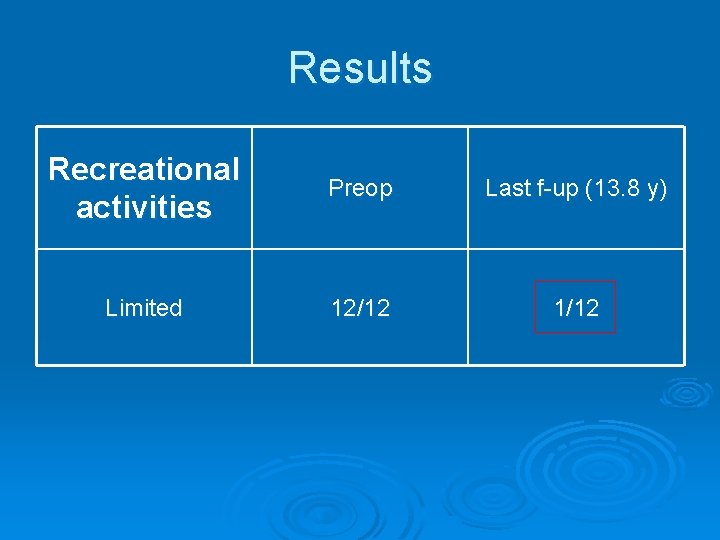
Results Recreational activities Preop Last f-up (13. 8 y) Limited 12/12 1/12
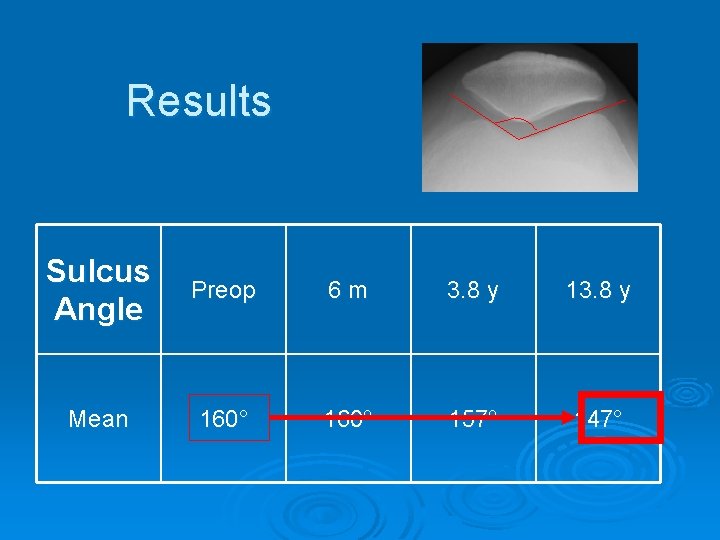
Results Sulcus Angle Preop 6 m 3. 8 y 13. 8 y Mean 160° 157° 147°
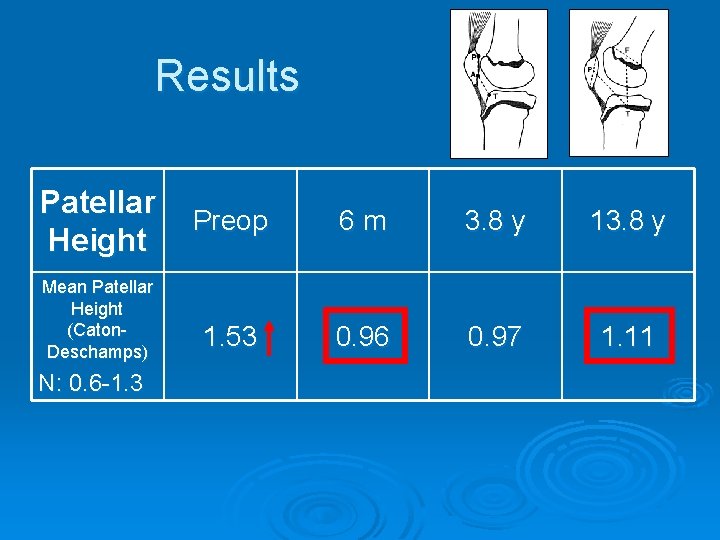
Results Patellar Height Mean Patellar Height (Caton. Deschamps) N: 0. 6 -1. 3 Preop 6 m 3. 8 y 1. 53 0. 96 0. 97 1. 11
Early postoperative complications (3) Ø 1 redislocation (undercorrection) l l Early reoperation Now stable Ø 1 wound abcess l l Surgical drainage, Antibiotics Healed Ø 1 peroneal nerve neurapraxia l l Recovered completely Cast compression?

Late postoperative complications Ø Two patella bajas (Caton ratio) in children operated at 6 and 7 years old

Discussion
Discussion Risks of osteoarthritis minimized by: Ø no unnecessary medialization Ø no posterior recessing Ø high rate of patellofemoral stability
Discussion Anatomic repositioning of the patella Ø eliminates delay of patellar engagement Ø maximizes buttressing effect of the lateral condyle, and…

…seems to remodel the shallow throchlea in the immature patient
Conclusion Ø Realistic goals were achieved: l Functional knee stability l Return to active life
Conclusion Ø Addressing patellar height is paramount in the immature patient
Conclusion Ø Patella baja occurred in two patients l No clinical or radiological consequence l Consequences in the futur? ?
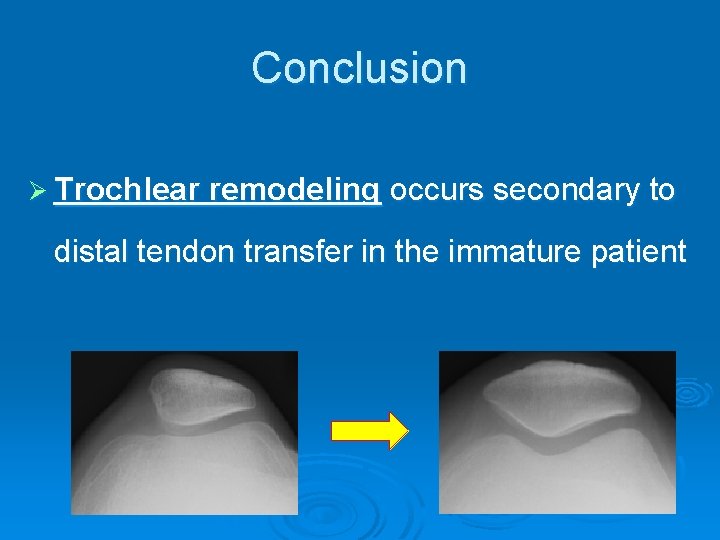
Conclusion Ø Trochlear remodeling occurs secondary to distal tendon transfer in the immature patient
Thank you

Who is right? Caton normal Insall: Patella baja
Lateral retinacular release alone in reccurent patellar dislocation Ø 21% redislocation rate (7/33 knees)¹ Ø 35% redislocation rate (7/20 knees)² 1) Dandy and Desai, JBJS Br, 1989 2) Aglietti et al, J Orthop, 1994
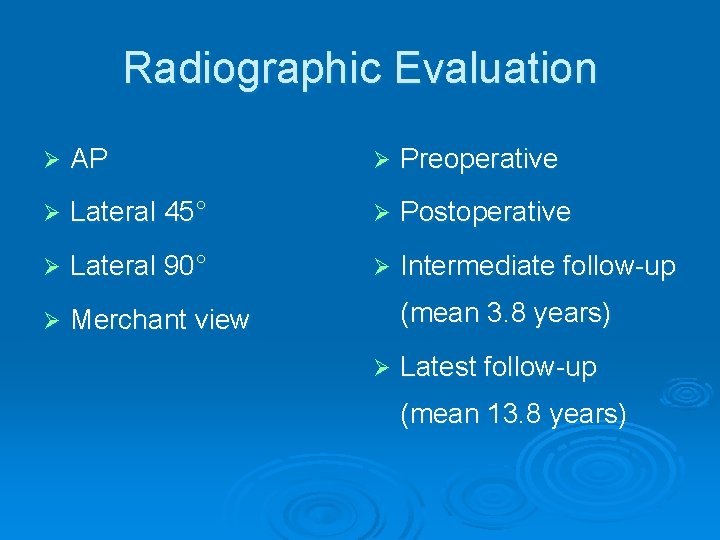
Radiographic Evaluation Ø AP Ø Preoperative Ø Lateral 45° Ø Postoperative Ø Lateral 90° Ø Intermediate follow-up Ø Merchant view (mean 3. 8 years) Ø Latest follow-up (mean 13. 8 years)
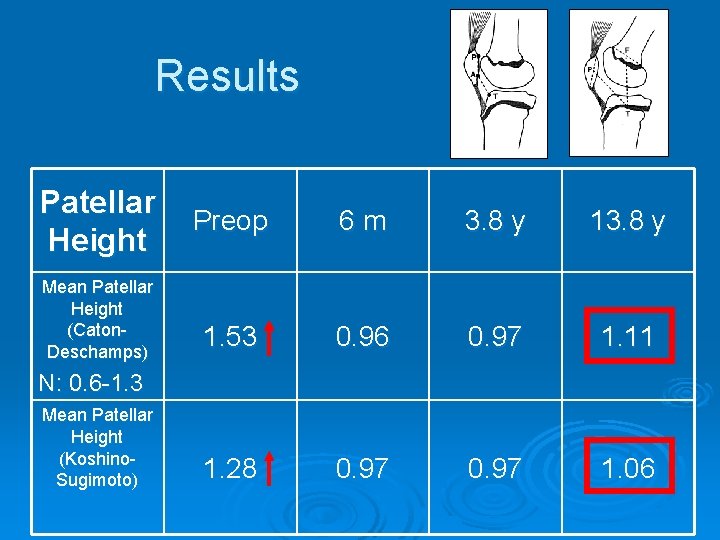
Results Patellar Height Mean Patellar Height (Caton. Deschamps) Preop 6 m 3. 8 y 1. 53 0. 96 0. 97 1. 11 1. 28 0. 97 1. 06 N: 0. 6 -1. 3 Mean Patellar Height (Koshino. Sugimoto)
Conclusion Ø The described surgical procedure is a comprehensive and effective approach to habitual patellar dislocation in young children

Lateral release
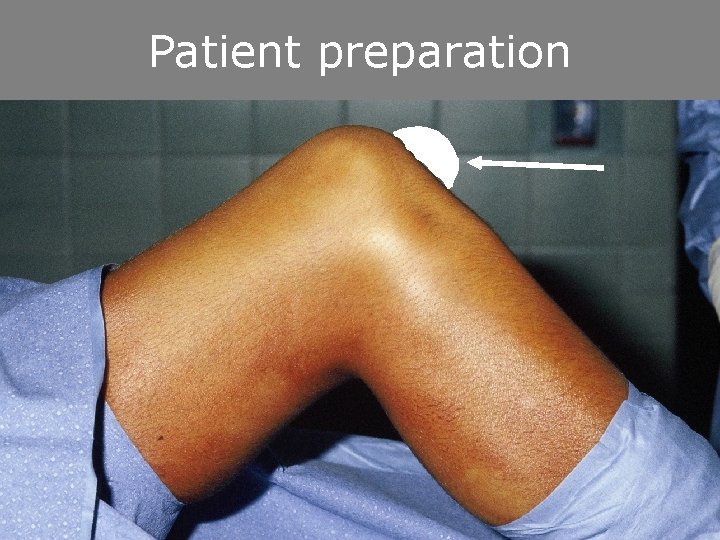
Patient preparation
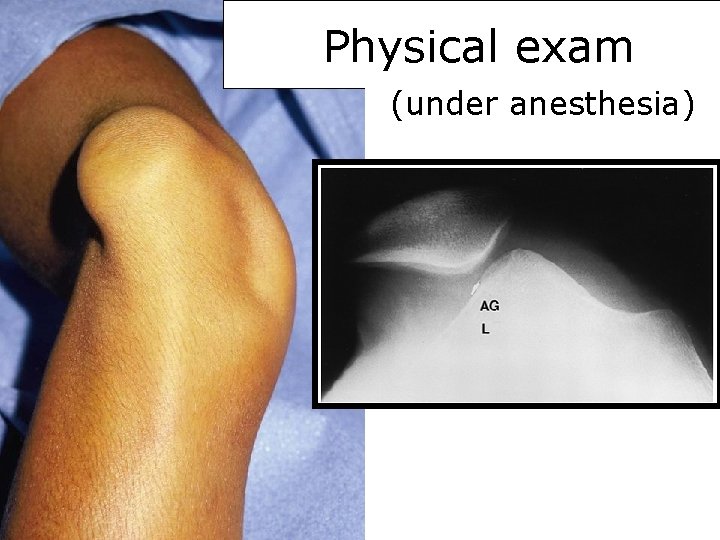
Physical exam (under anesthesia)
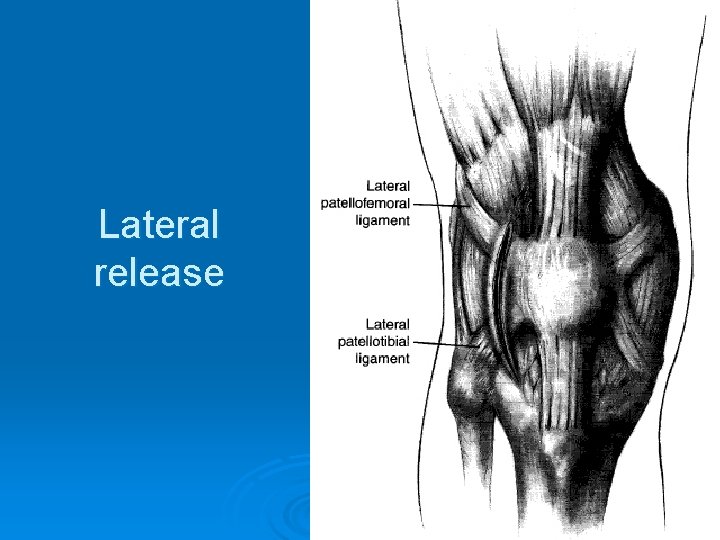
Lateral release

VMO advancement

Wound closed
- Slides: 82