Kidney By Dr Abdel Aziz M Hussein Lecturer
Kidney By Dr. Abdel Aziz M. Hussein Lecturer of Medical Physiology

• • • Given these structures: 1. basement membrane 2. fenestra 3. filtration slit Choose the arrangement that lists the structures in the order a molecule of glucose encounters them as the glucose passes through the filtration membrane to enter Bowman’s capsule. a. 1, 2, 3 b. 2, 1, 3 c. 2, 3, 1 d. 3, 1, 2 e. 3, 2, 1

Urine Formation

Glomerular Filtration Def. , • Means the bulk flow of a solvent through a filter carrying with it the solutes that are small enough to pass through the filter.

Glomerular Filtration Blood Capillary endothelium Basement Membrane Podocytes slits Bowman Capsule

Glomerular Filtration Def. , • It is an ultrafiltration since it is plasma minus plasma protein and cellular elements while simple filtration excludes only cellular elements.
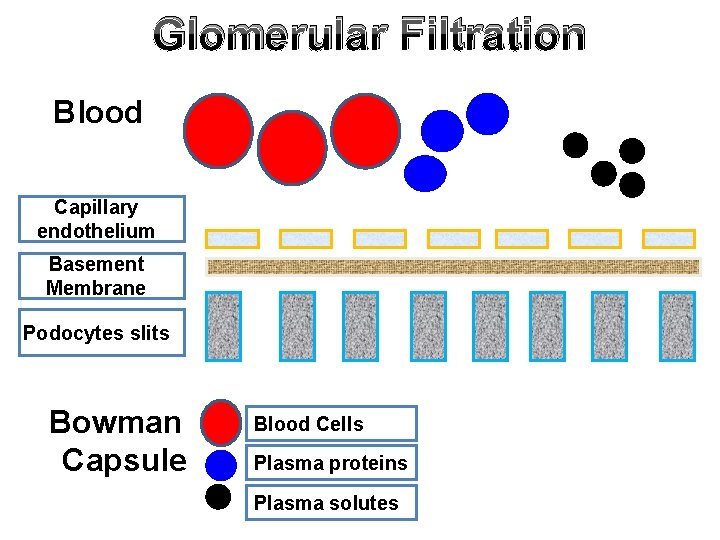
Glomerular Filtration Blood Capillary endothelium Basement Membrane Podocytes slits Bowman Capsule Blood Cells Plasma proteins Plasma solutes

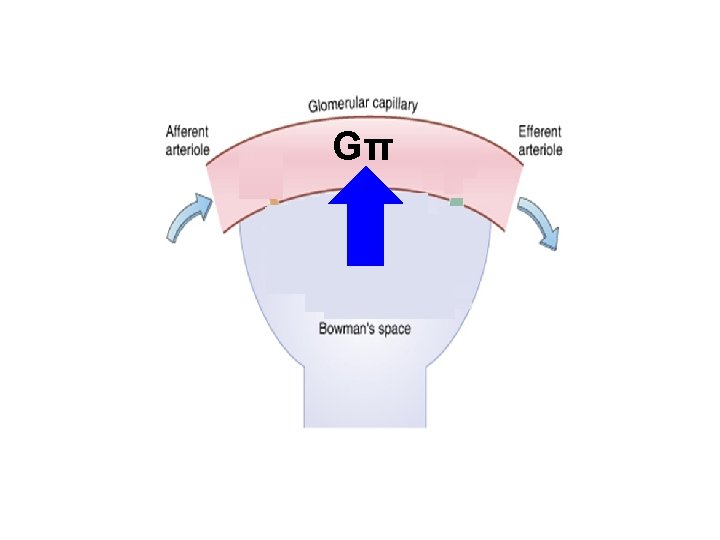
Glomerular Filtration Dynamics: • Glomerular Filtration is formed by the forces of filtration as many capillary filtrate in the body (Starling's forces of filtration). • They are 4 forces; v 2 Hydrostatic pressures v 2 Oncotic pressures

Glomerular Filtration Glomerular capillary Glomerular Hydrostatic Pressure (Gp) Glomerular Oncotic Pressure (Gπ) Capillary endothelium Basement Membrane Podocytes slits Bowman Capsule Bowman oncotic Pressure (B π) Bowman Hydrostatic Pressure (Bp)

Glomerular Filtration Gp = 60 mm. Hg Gπ = 32 mm. Hg Bπ = 0 mm. Hg Gp = 18 mm. Hg

Glomerular Filtration • GFR is determined by Starling's principle; ″The rate & direction of fluid movement is proportional to the algebraic sum of hydrostatic & oncotic pressures″ • So, GFR α (hydrostatic pressure – oncotic pressure) GFR α { (Gp- Bp) – (Gπ – Bπ)} • KF = filtration coefficient

Glomerular Filtration • Net filtering force {60 -(32+18)} = 10 mm. Hg and GFR = 120 m. L/ min
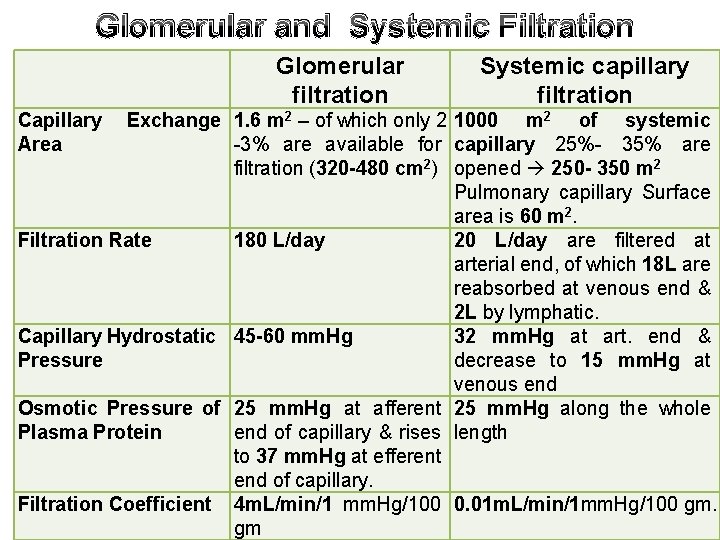
Glomerular and Systemic Filtration Glomerular filtration Capillary Area Systemic capillary filtration Exchange 1. 6 m 2 – of which only 2 1000 m 2 of systemic -3% are available for capillary 25%- 35% are filtration (320 -480 cm 2) opened 250 - 350 m 2 Pulmonary capillary Surface area is 60 m 2. Filtration Rate 180 L/day 20 L/day are filtered at arterial end, of which 18 L are reabsorbed at venous end & 2 L by lymphatic. Capillary Hydrostatic 45 -60 mm. Hg 32 mm. Hg at art. end & Pressure decrease to 15 mm. Hg at venous end Osmotic Pressure of 25 mm. Hg at afferent 25 mm. Hg along the whole Plasma Protein end of capillary & rises length to 37 mm. Hg at efferent end of capillary. Filtration Coefficient 4 m. L/min/1 mm. Hg/100 0. 01 m. L/min/1 mm. Hg/100 gm. gm
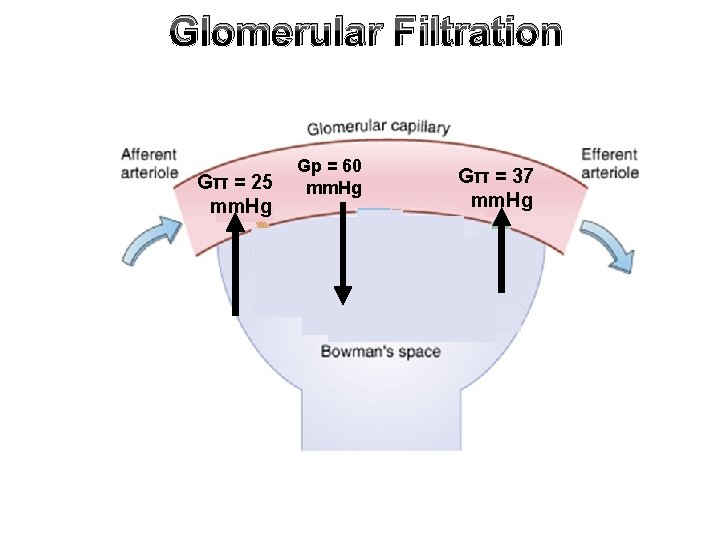
Glomerular Filtration Gπ = 25 mm. Hg Gp = 60 mm. Hg Gπ = 37 mm. Hg
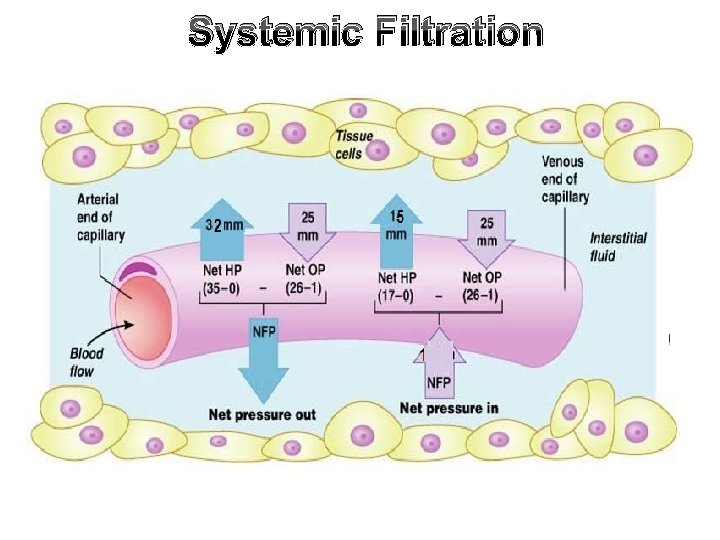
Systemic Filtration

Glomerular Filtration Rate (GFR)

Glomerular Filtration Rate Def. , • Volume of plasma filtered by both kidney per unit time Value: – 125 ml/min – 180 L/day or – 60 nl/min for single nephron (SNGFR). Filtration fraction: is part of RPF filtered in Glomeruli GFR = 125 ml/min = RPF = 1/5 or 20% 650 ml/min

RPF 650 ml/min FF= 120/ 650 = 20% GFR 120 ml/min RPF 649 ml/min Urine flow rate 1 ml/min

Glomerular Filtration Rate Significance of High GFR: • To ensure processing of plasma (3 L) about 60 times/day (since daily GFR = 180 L/day prevents accumulation of metabolites. Causes of high GFR: 1) High filtration coefficient: • KF is volume of fluid filtered /min/ mm. Hg pressure difference across the membrane
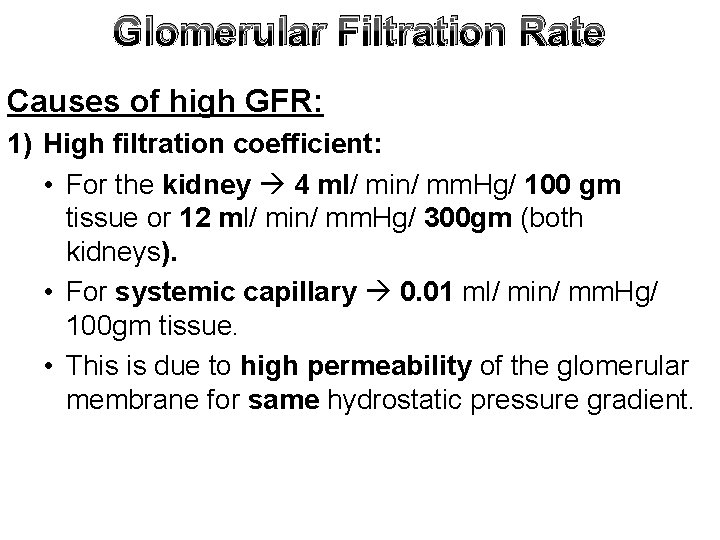
Glomerular Filtration Rate Causes of high GFR: 1) High filtration coefficient: • For the kidney 4 ml/ min/ mm. Hg/ 100 gm tissue or 12 ml/ min/ mm. Hg/ 300 gm (both kidneys). • For systemic capillary 0. 01 ml/ min/ mm. Hg/ 100 gm tissue. • This is due to high permeability of the glomerular membrane for same hydrostatic pressure gradient.
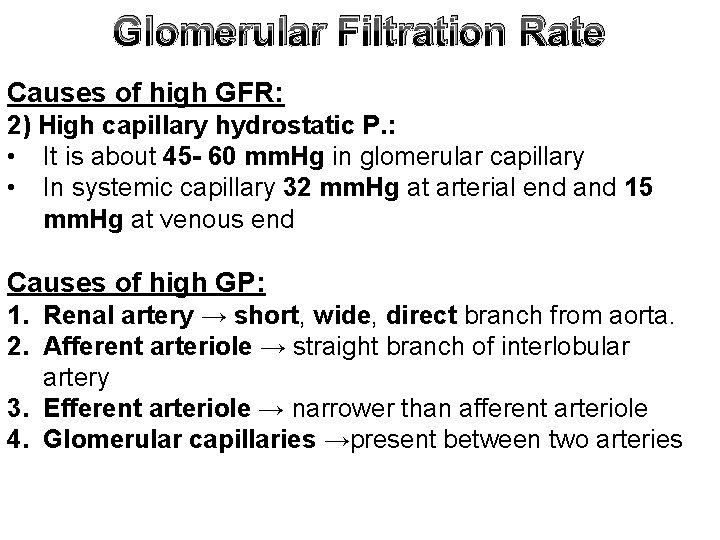
Glomerular Filtration Rate Causes of high GFR: 2) High capillary hydrostatic P. : • It is about 45 - 60 mm. Hg in glomerular capillary • In systemic capillary 32 mm. Hg at arterial end and 15 mm. Hg at venous end Causes of high GP: 1. Renal artery → short, wide, direct branch from aorta. 2. Afferent arteriole → straight branch of interlobular artery 3. Efferent arteriole → narrower than afferent arteriole 4. Glomerular capillaries →present between two arteries

Causes of High Gp

Causes of High Gp
Glomerular Filtration Rate Causes of high GFR: 3) High RPF. : • It is about 600 ml/ min. • This high RBF eventually leads to high GFR. RBF
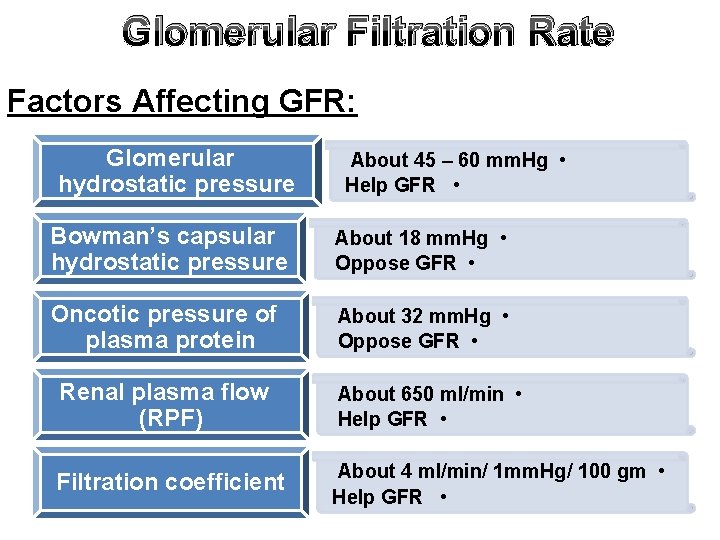
Glomerular Filtration Rate Factors Affecting GFR: Glomerular hydrostatic pressure About 45 – 60 mm. Hg • Help GFR • Bowman’s capsular hydrostatic pressure About 18 mm. Hg • Oppose GFR • Oncotic pressure of plasma protein About 32 mm. Hg • Oppose GFR • Renal plasma flow (RPF) About 650 ml/min • Help GFR • Filtration coefficient About 4 ml/min/ 1 mm. Hg/ 100 gm • Help GFR •
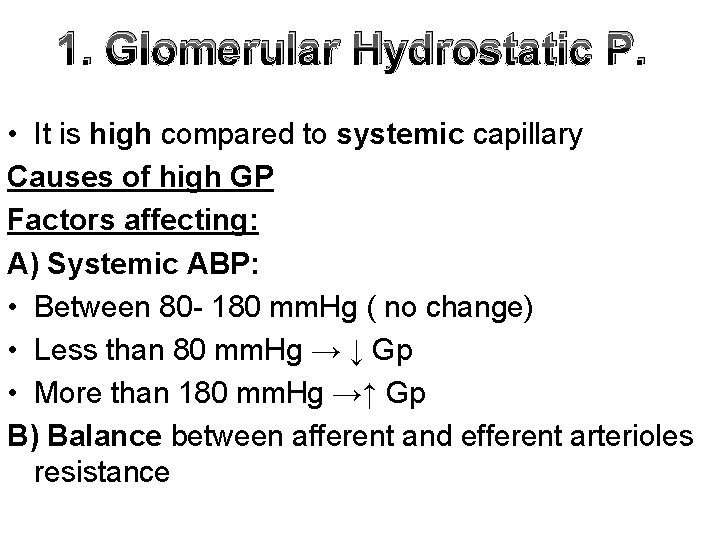
1. Glomerular Hydrostatic P. • It is high compared to systemic capillary Causes of high GP Factors affecting: A) Systemic ABP: • Between 80 - 180 mm. Hg ( no change) • Less than 80 mm. Hg → ↓ Gp • More than 180 mm. Hg →↑ Gp B) Balance between afferent and efferent arterioles resistance

2. Bowman Hydrostatic P. • It is about 18 mm. Hg helps to maintain renal tubules patent. • Acts as a driving force to propel glomerular filtrate along whole length of renal tubules. • If increased e. g. in ureteric obstruction decrease GFR.

Bp Increased Bp
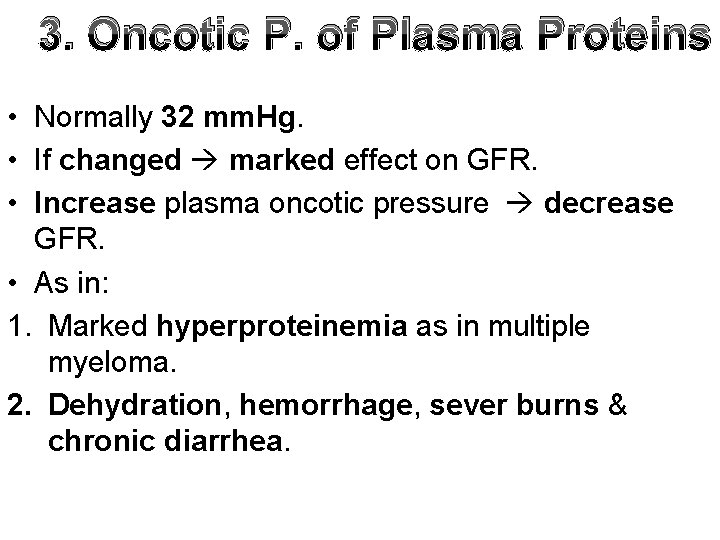
3. Oncotic P. of Plasma Proteins • Normally 32 mm. Hg. • If changed marked effect on GFR. • Increase plasma oncotic pressure decrease GFR. • As in: 1. Marked hyperproteinemia as in multiple myeloma. 2. Dehydration, hemorrhage, sever burns & chronic diarrhea.

3. Oncotic P. of Plasma Proteins • Leakage of plasma albumin from glomerular membrane in some pathological conditions decrease plasma oncotic pressure & increase Bowman’s oncotic pressure increase GFR.

4. Renal Plasma Flow • RPF affect indirectly the plasma oncotic pressure • Increase RPF maintain normal plasma oncotic pressure and filtration equilibrium is achieved too late helps GFR. • Decrease RPF elevates plasma oncotic pressure decrease GFR.

High RPF
5. Filtration Coefficient • It is the effectiveness of the permeability of the barrier. • It depends on: 1. Hydraulic conductivity (water permeability of the barrier). 2. Effective filtration surface area

5. Filtration Coefficient 2. Effective filtration surface area is affected by: a. Total number of functioning glomeruli. b. State of intraglomerular mesangium. • Their contraction (e. g. by AII) decrease effective filtration area & their relaxation (e. g. by dopamine) increase effective surface area.

Effect of Afferent and Efferent Arteriolar Resistance on: RPF, GFR, and Filtration Fraction (FF)

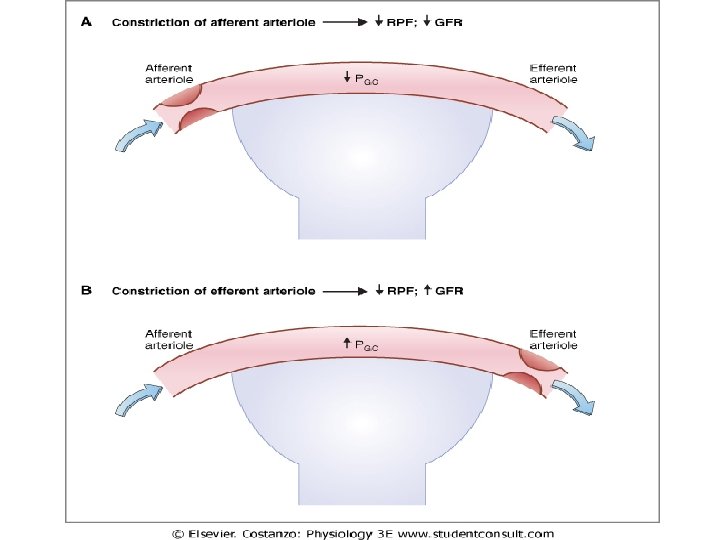
Change in Preglomerular Resistance Or (afferent arteriole diameter) V. D. of afferent arterioles ↑ Gp ↑ RPF FF = no change ↑ GFR

Change in Preglomerular Resistance Or (afferent arteriole diameter) V. C. of afferent arterioles ↓ Gp ↓ RPF FF = no change ↓ GFR
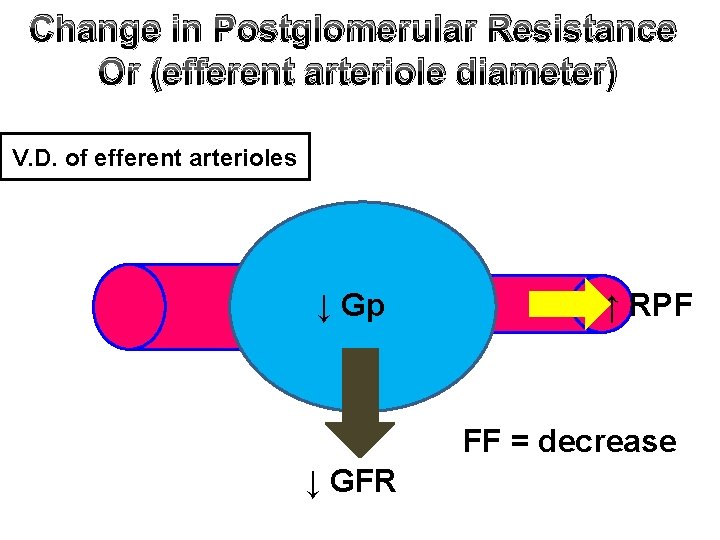
Change in Postglomerular Resistance Or (efferent arteriole diameter) V. D. of efferent arterioles ↓ Gp ↑ RPF FF = decrease ↓ GFR

Change in Postglomerular Resistance Or (efferent arteriole diameter) V. C. of efferent arterioles ↑ Gp ↓ RPF FF = Increase ↑ GFR
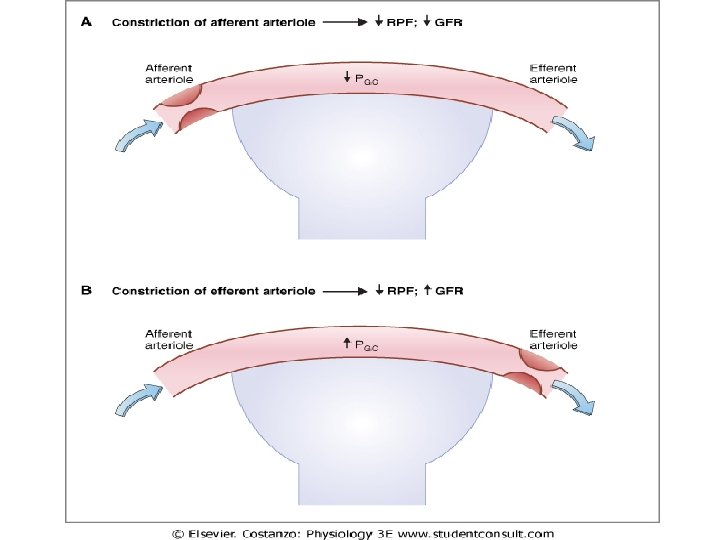

Afferent Efferent RPF GFR (Preglomerular (Postglomerular resistance) resistance VC VD --- --VC VD FF (GFR / RBF) constant

THANKS
- Slides: 48