Pain as the th 5 Vital Sign HOSPITAL















- Slides: 90

Pain as the th 5 Vital Sign HOSPITAL TAIPING
OBJECTIVE: The purpose of module is to train doctors on pain assessment and pain management in order to implement pain as a 5 th vital sign effectively in YOUR hospital

Pain Free Hospital Pain Management & Pain Assessment Focus Day Surgery Minimal Invasive Surgery Physiotherapy Pharmacy
Definition • Pain is an unpleasant sensory & emotional experience associated with actual & potential tissue damage or described in term of such damage International Association for the Study of Pain 1996

What do you understand about pain ? What we understand … • Unpleasant • Emotions are important • The cause is not always visible
SAKIT !! Definition to the patient Pain is what the patient says
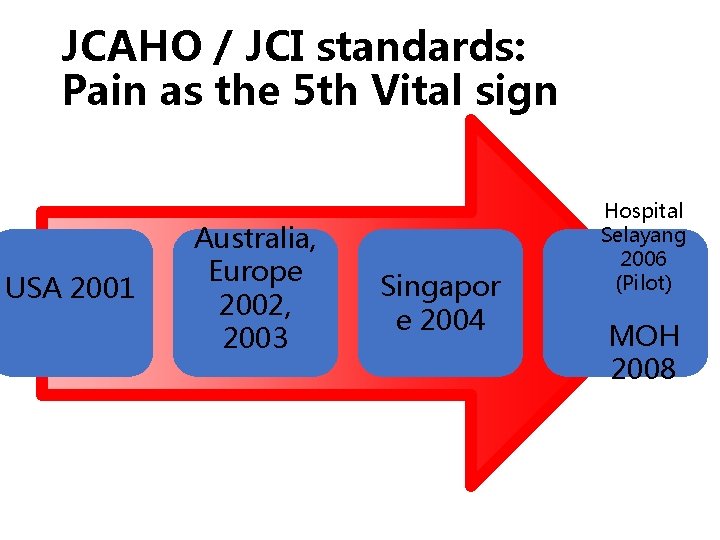
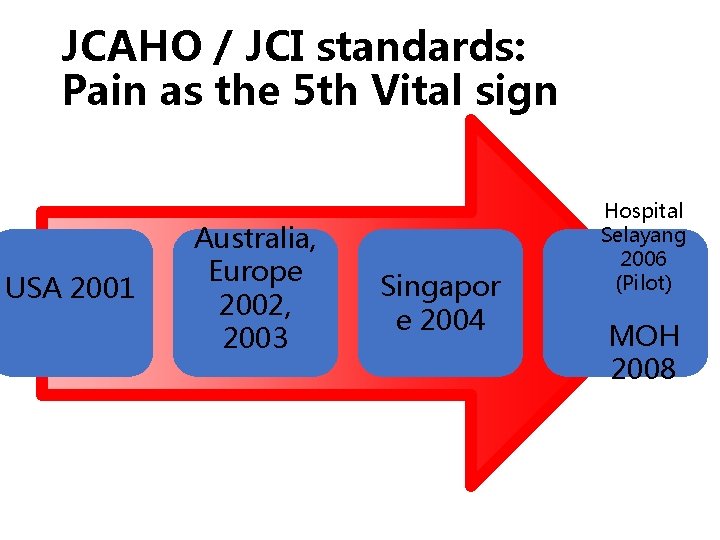
JCAHO / JCI standards: Pain as the 5 th Vital sign USA 2001 Australia, Europe 2002, 2003 Singapor e 2004 Hospital Selayang 2006 (Pilot) MOH 2008
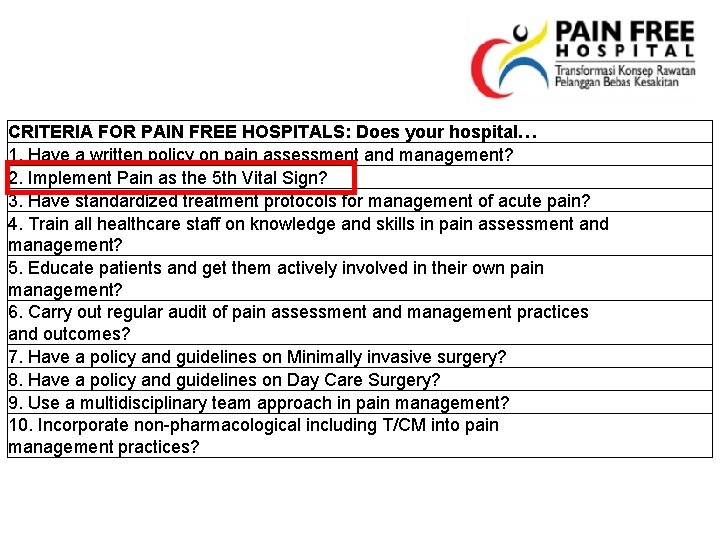
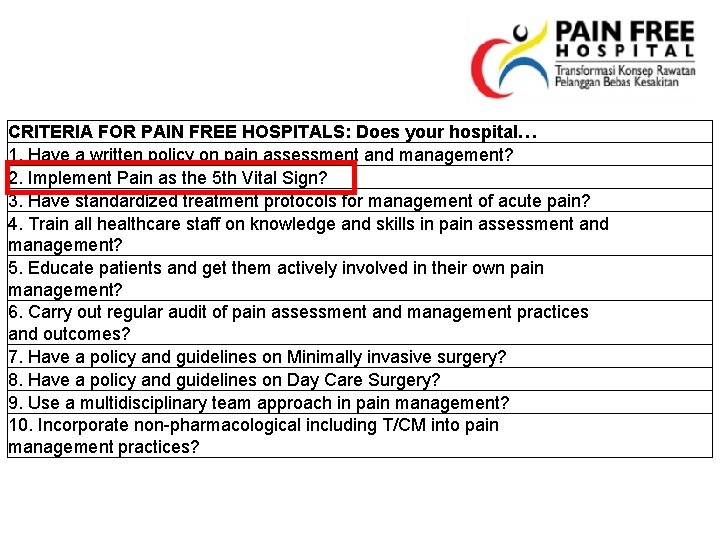
CRITERIA FOR PAIN FREE HOSPITALS: Does your hospital… 1. Have a written policy on pain assessment and management? 2. Implement Pain as the 5 th Vital Sign? 3. Have standardized treatment protocols for management of acute pain? 4. Train all healthcare staff on knowledge and skills in pain assessment and management? 5. Educate patients and get them actively involved in their own pain management? 6. Carry out regular audit of pain assessment and management practices and outcomes? 7. Have a policy and guidelines on Minimally invasive surgery? 8. Have a policy and guidelines on Day Care Surgery? 9. Use a multidisciplinary team approach in pain management? 10. Incorporate non-pharmacological including T/CM into pain management practices?
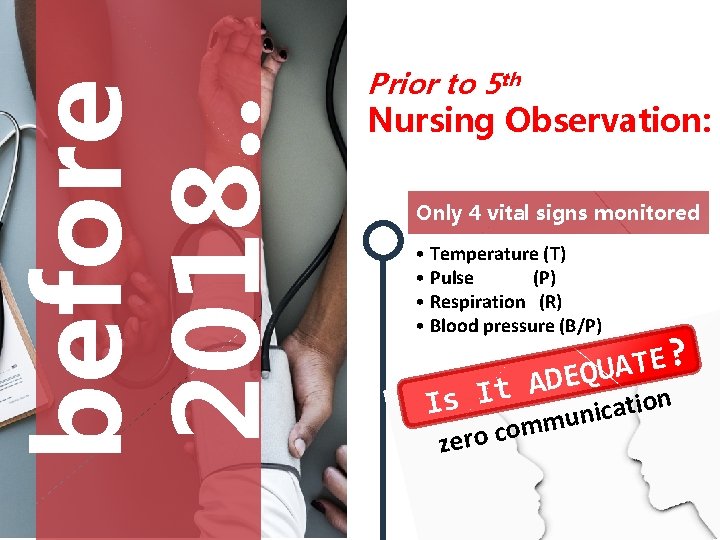
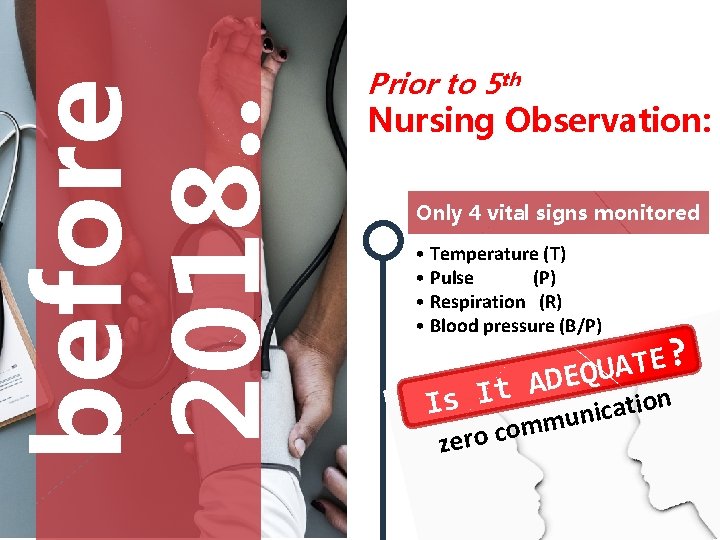
before 2018. . Prior to 5 th Nursing Observation: Only 4 vital signs monitored • Temperature (T) • Pulse (P) • Respiration (R) • Blood pressure (B/P) Is It ? E T A ADEQU ze n o i t a c i un m m o ro c

after 2018. . Pain as 5 th Vital Sign Mandatory to carry out Pain as 5 th vital sign To provide routine assessment, treatment and documentation

BENEFITS OF PAIN AS 5 TH VITAL SIGN 1 2 3 Enhance healing, reduce length of stay Reduce health care cost Promote staff- patient interaction 4 5 6 Promote client satisfaction Improve quality Of life , sleep & appetite Reduce psychological distress
How to incorporate P 5 VS effectively ? Essential Pain Management (EPM) Aims: 1. To improve understanding of pain 2. To teach a simple framework for managing pain 3. To reduce pain management barriers

Approach to pain RAT Model: • Recognize • Assess • Treat

RAT MODEL RECOGNIZE Does the patients has pain ? Do other people know patient has pain ? ASSESS How severe is the pain ? What type of pain is it ? Are there other factors ? TREAT What non-drug treatments can I use ? What drug treatments can I use
At the end of this course You will be able to: 1. Understand the importance of treating pain 2. Recognize, assess and treat different types of pain
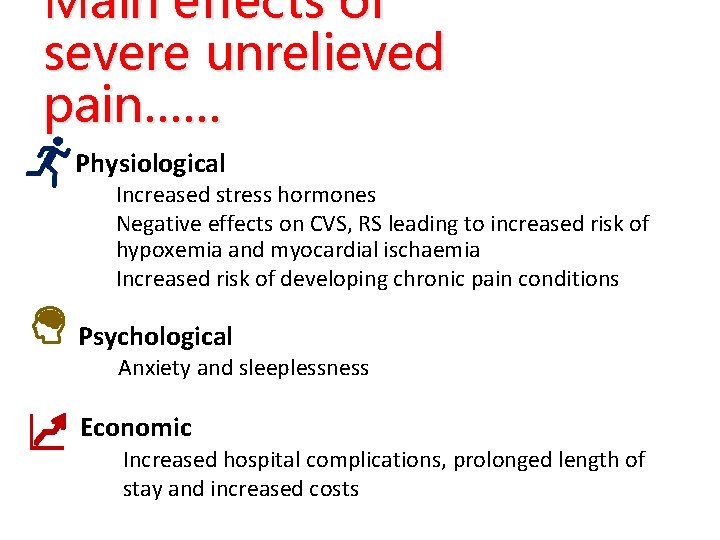
Main effects of severe unrelieved pain…… Physiological Increased stress hormones Negative effects on CVS, RS leading to increased risk of hypoxemia and myocardial ischaemia Increased risk of developing chronic pain conditions Psychological Anxiety and sleeplessness Economic Increased hospital complications, prolonged length of stay and increased costs
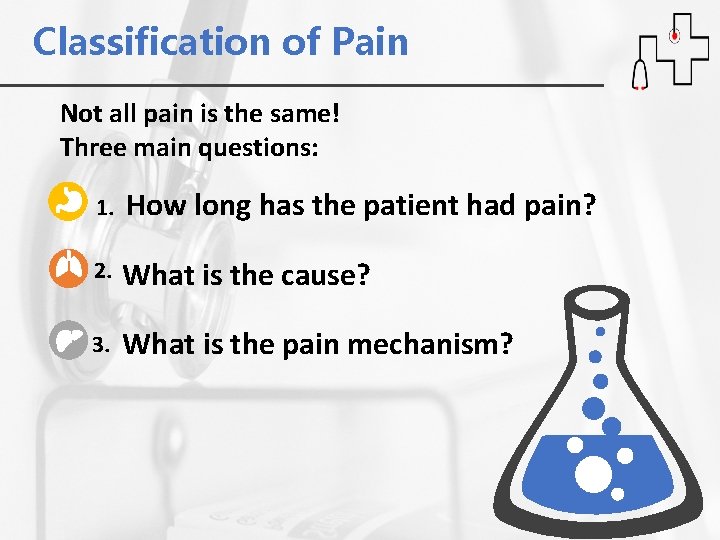
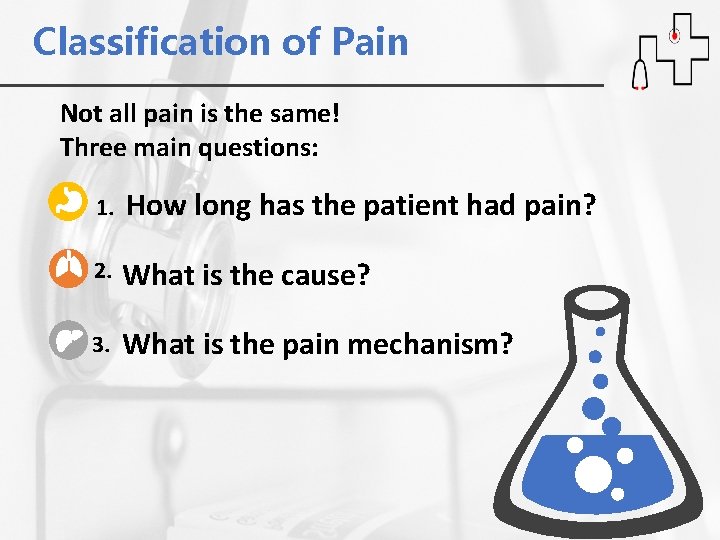
Classification of Pain Not all pain is the same! Three main questions: 1. How long has the patient had pain? 2. What is the cause? 3. What is the pain mechanism?
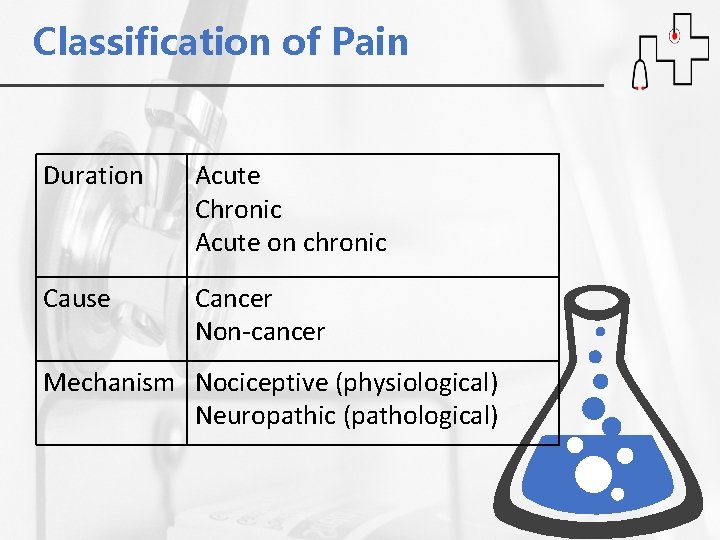
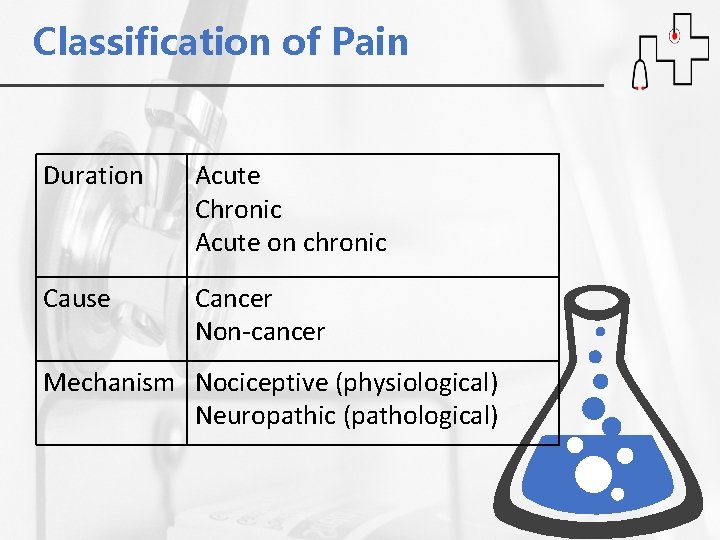
Classification of Pain Duration Acute Chronic Acute on chronic Cause Cancer Non-cancer Mechanism Nociceptive (physiological) Neuropathic (pathological)
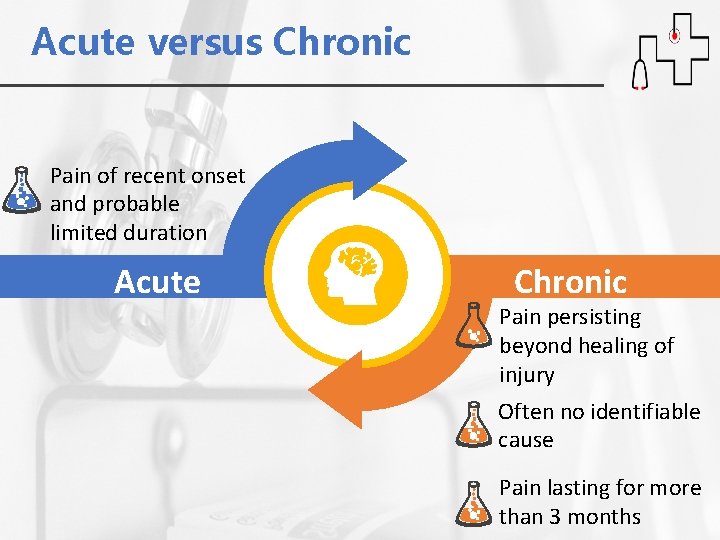
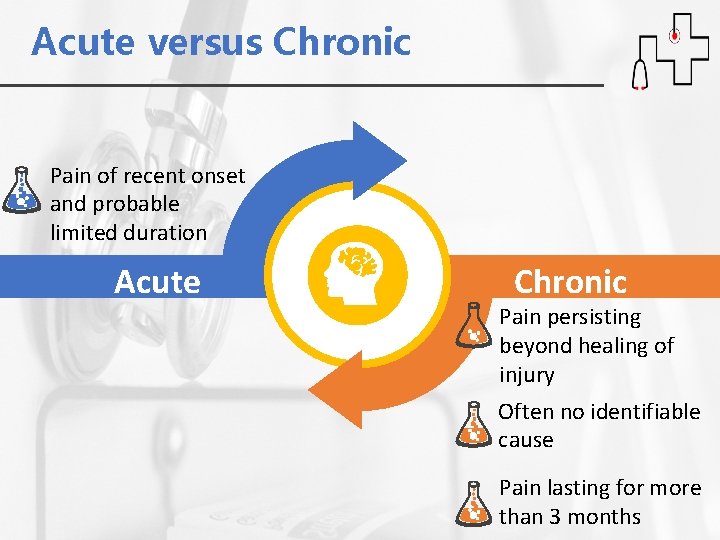
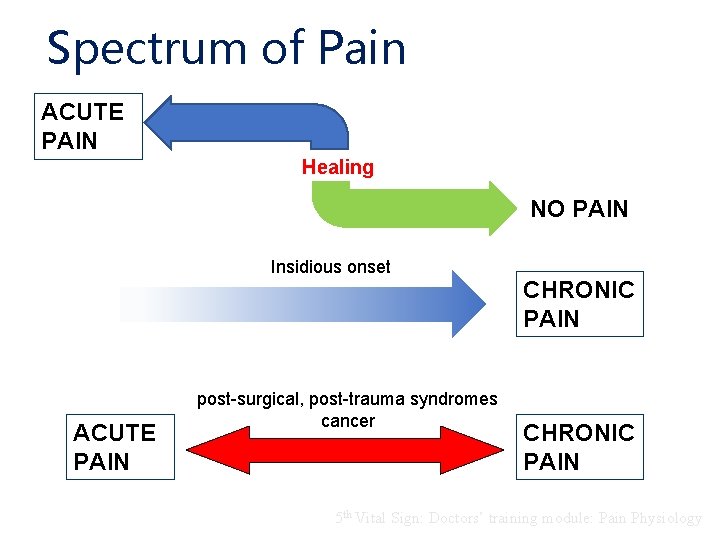
Acute versus Chronic Pain of recent onset and probable limited duration Acute Chronic Pain persisting beyond healing of injury Often no identifiable cause Pain lasting for more than 3 months
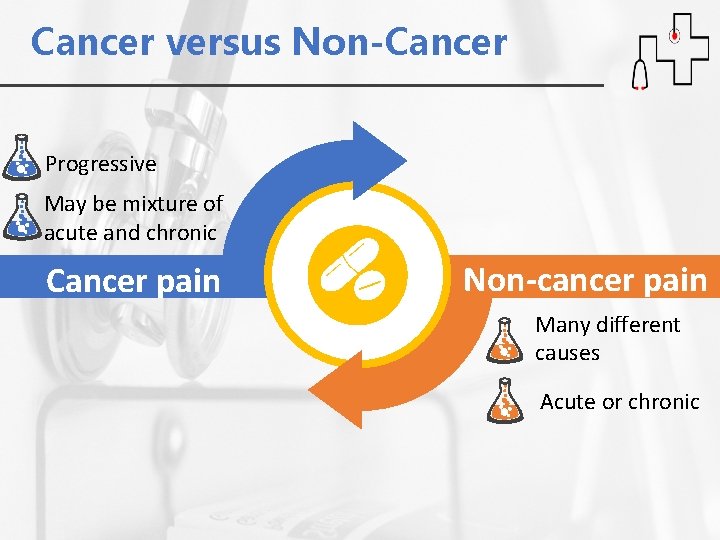
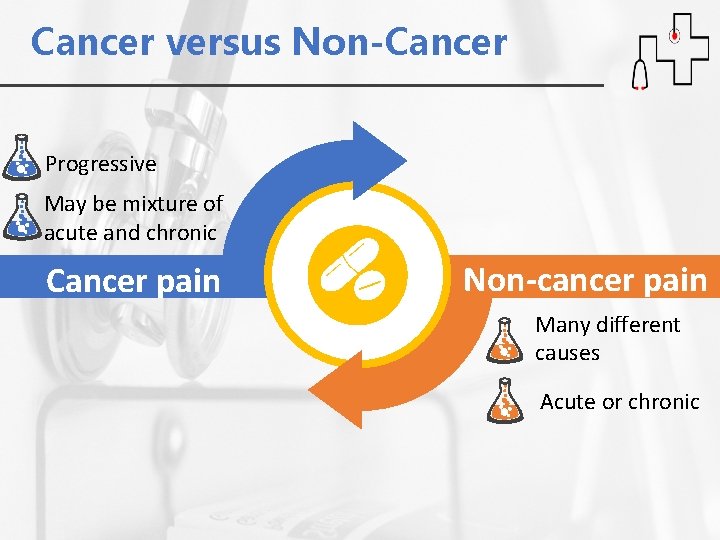
Cancer versus Non-Cancer Progressive May be mixture of acute and chronic Cancer pain Non-cancer pain Many different causes Acute or chronic
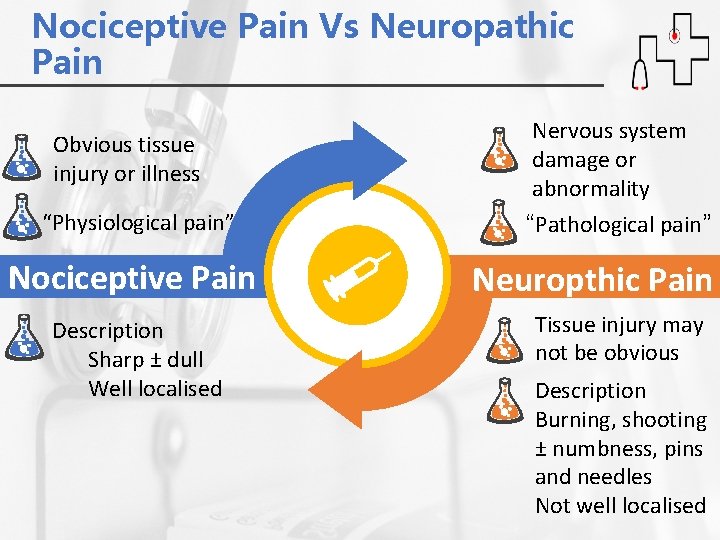
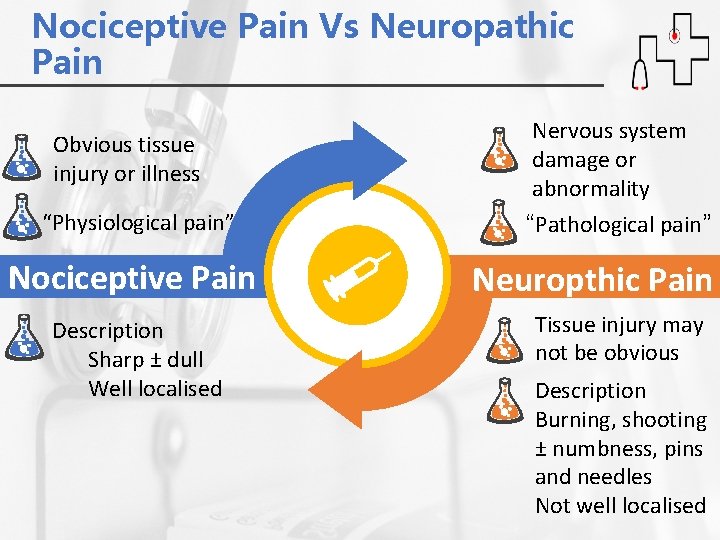
Nociceptive Pain Vs Neuropathic Pain Obvious tissue injury or illness “Physiological pain” Nociceptive Pain Description Sharp ± dull Well localised Nervous system damage or abnormality “Pathological pain” Neuropthic Pain Tissue injury may not be obvious Description Burning, shooting ± numbness, pins and needles Not well localised
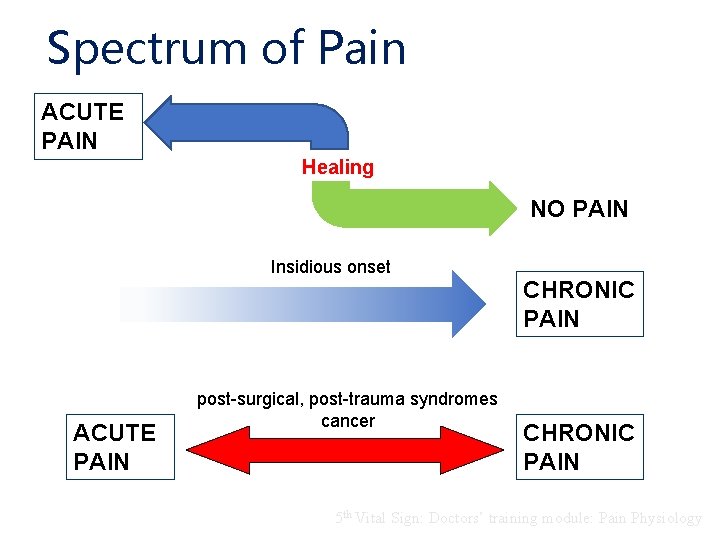
Spectrum of Pain ACUTE PAIN Healing NO PAIN Insidious onset ACUTE PAIN post-surgical, post-trauma syndromes cancer CHRONIC PAIN 5 th Vital Sign: Doctors’ training module: Pain Physiology
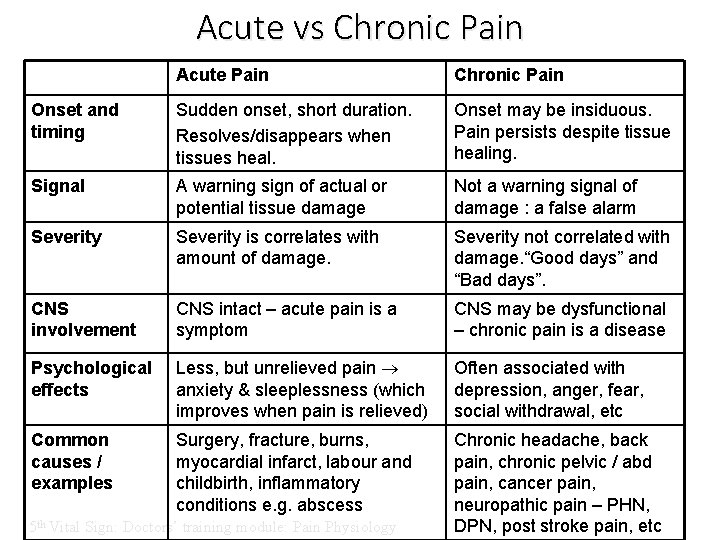
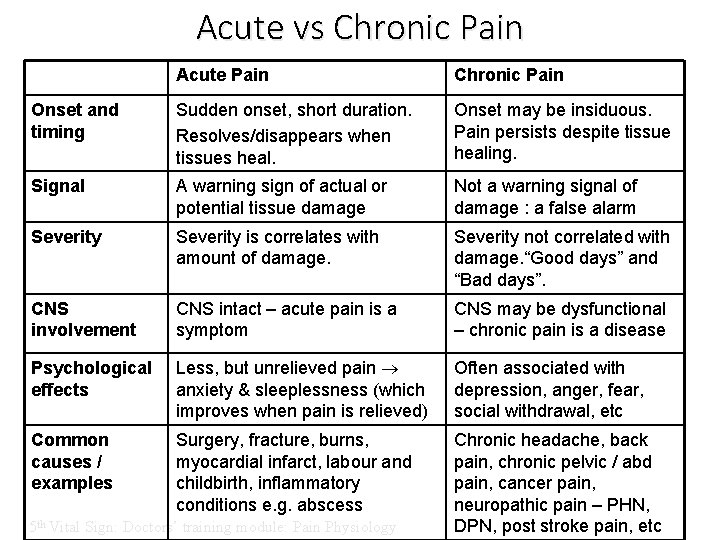
Acute vs Chronic Pain Acute Pain Chronic Pain Onset and timing Sudden onset, short duration. Resolves/disappears when tissues heal. Onset may be insiduous. Pain persists despite tissue healing. Signal A warning sign of actual or potential tissue damage Not a warning signal of damage : a false alarm Severity is correlates with amount of damage. Severity not correlated with damage. “Good days” and “Bad days”. CNS involvement CNS intact – acute pain is a symptom CNS may be dysfunctional – chronic pain is a disease Psychological effects Less, but unrelieved pain anxiety & sleeplessness (which improves when pain is relieved) Often associated with depression, anger, fear, social withdrawal, etc Common causes / examples Surgery, fracture, burns, myocardial infarct, labour and childbirth, inflammatory conditions e. g. abscess Chronic headache, back pain, chronic pelvic / abd pain, cancer pain, neuropathic pain – PHN, DPN, post stroke pain, etc 5 th Vital Sign: Doctors’ training module: Pain Physiology

Pain Pathw ay
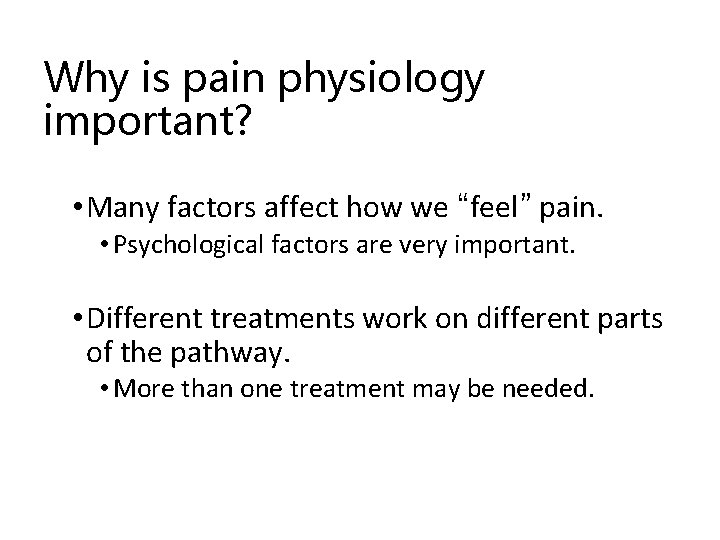
Why is pain physiology important? • Many factors affect how we “feel” pain. • Psychological factors are very important. • Different treatments work on different parts of the pathway. • More than one treatment may be needed.
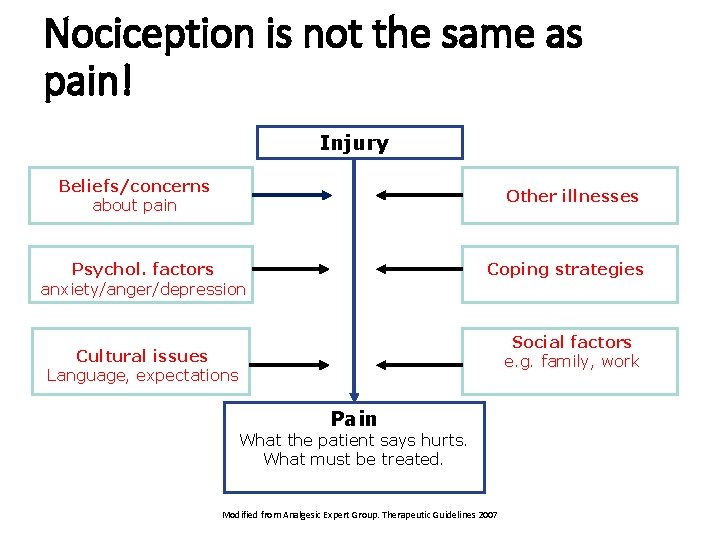
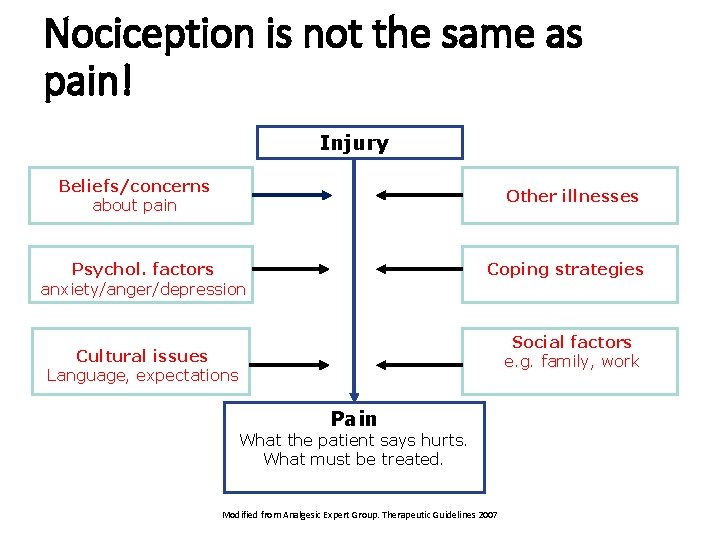
Nociception is not the same as pain! Injury Beliefs/concerns about pain Other illnesses Psychol. factors anxiety/anger/depression Coping strategies Social factors e. g. family, work Cultural issues Language, expectations Pain What the patient says hurts. What must be treated. Modified from Analgesic Expert Group. Therapeutic Guidelines 2007
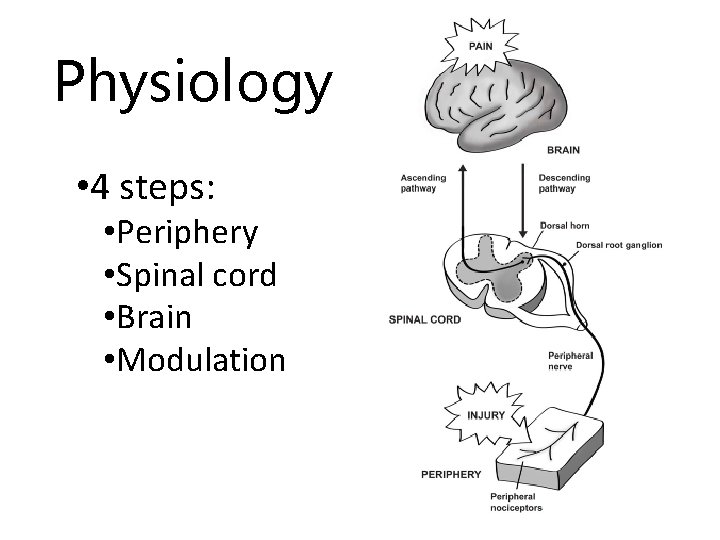
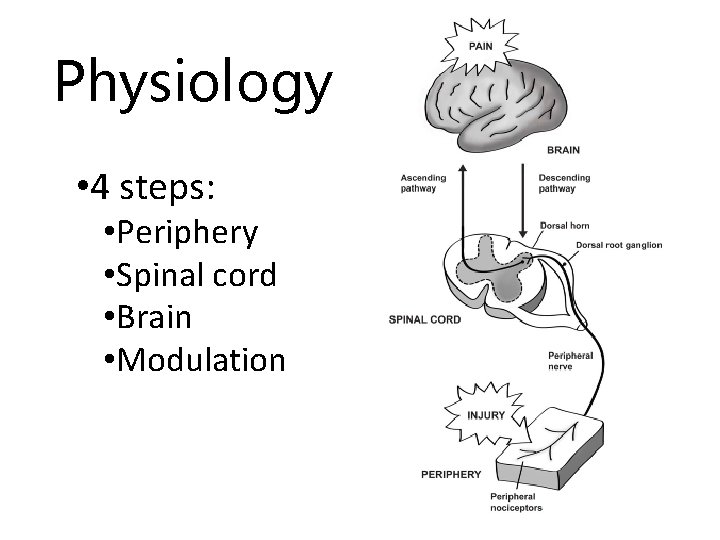
Physiology • 4 steps: • Periphery • Spinal cord • Brain • Modulation
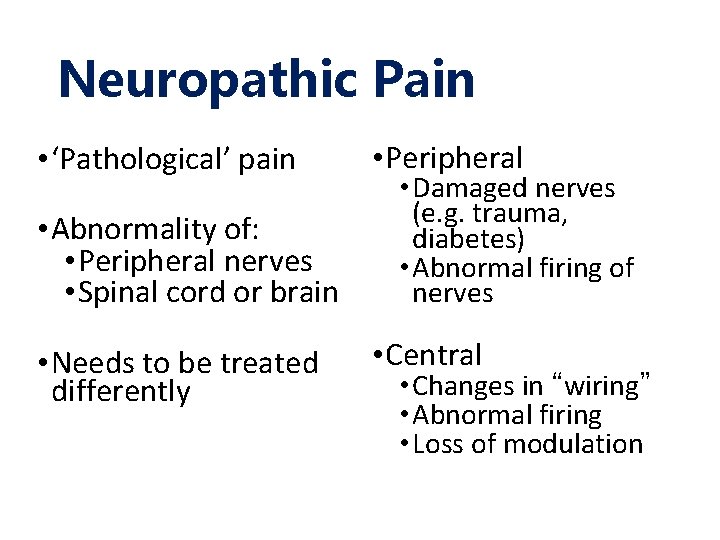
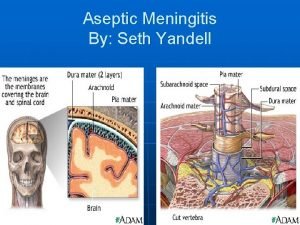
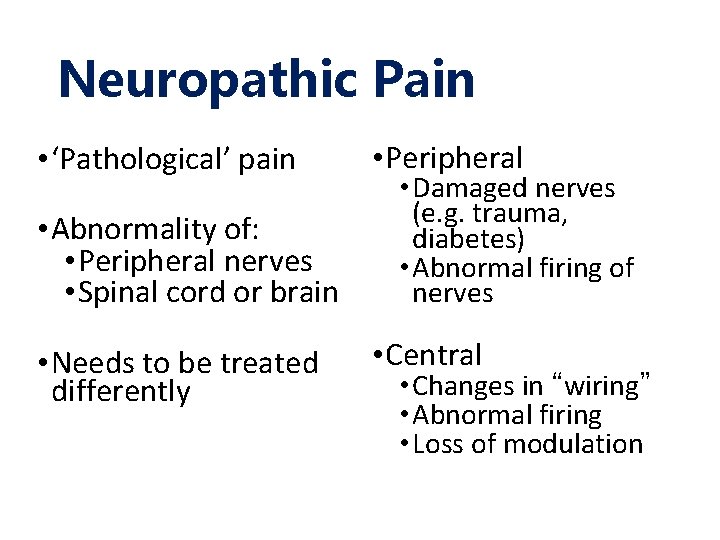
Neuropathic Pain • ‘Pathological’ pain • Abnormality of: • Peripheral nerves • Spinal cord or brain • Needs to be treated differently • Peripheral • Damaged nerves (e. g. trauma, diabetes) • Abnormal firing of nerves • Central • Changes in “wiring” • Abnormal firing • Loss of modulation
Pain Physiology and Pathology Summary (1) • Many factors affect how we “feel” pain • Different treatments work on different parts of the pain pathway • Since neuropathic and nociceptive pain are different so they must be treated differently • So are acute pain and chronic pain.
Pain Physiology and Pathology Summary (2) • It is important to differentiate between the two types of pain, remembering that : Acute pain is a symptom Chronic pain is a disease and 5 th Vital Sign: Doctors’ training module: Pain Physiology
Pain Physiology and Pathology Summary (3) • Chronic pain has to be managed using a multidisciplinary multimodal approach, which is more viable in the long term. 5 th Vital Sign: Doctors’ training module: Pain Physiology
PAIN ASSESSMENT
Why measure pain? v. Produces a baseline to assess therapeutic interventions e. g. administration of analgesic drugs v. Facilitates communication between staff looking after the patient v. For documentation 5 th Vital Sign: Doctors’ training module: Pain Assessment
Clinical techniques for measurement of pain • Self reporting by the patient (best method) • Observer assessment • Observation of behaviour and vital signs • Functional assessment 5 th Vital Sign: Doctors’ training module: Pain
How to assess pain: • Important to : • listen and believe the patient • Take a pain history : • “Tell me about your pain…” 5 th Vital Sign: Doctors’ training module: Pain
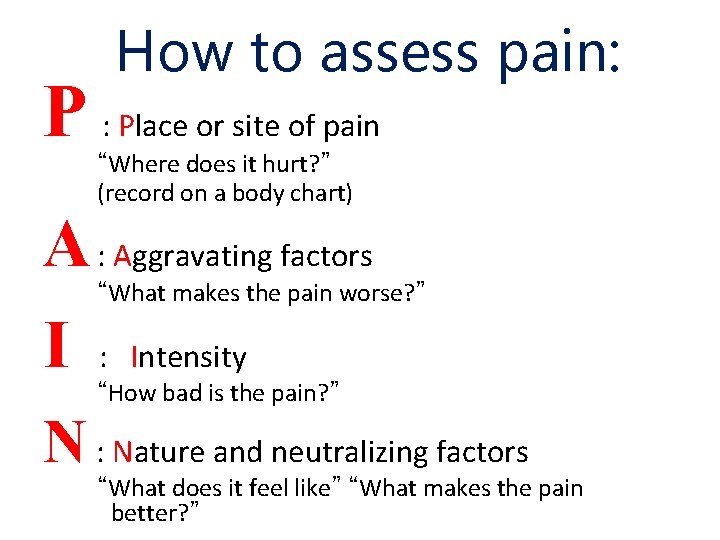
How to assess pain: P : Place or site of pain “Where does it hurt? ” (record on a body chart) A : Aggravating factors I “What makes the pain worse? ” : Intensity “How bad is the pain? ” N : Nature and neutralizing factors “What does it feel like” “What makes the pain better? ”
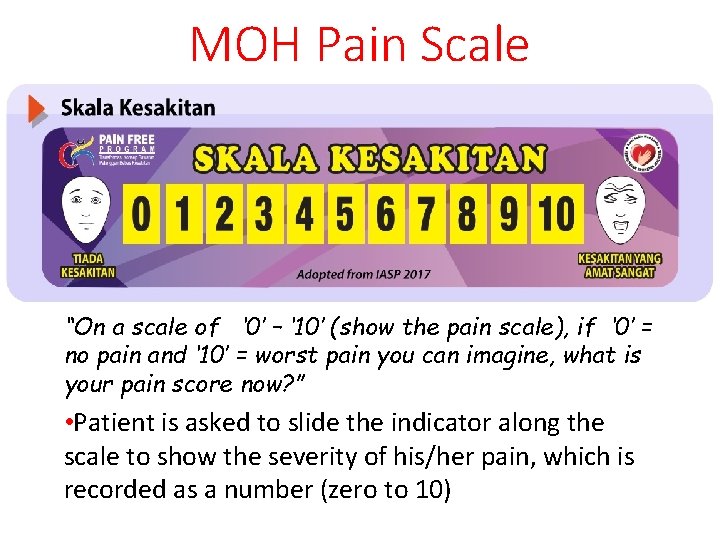
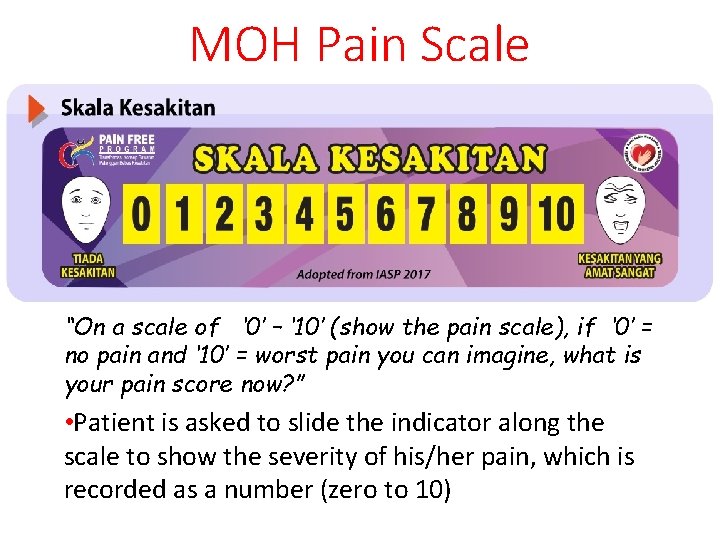
MOH Pain Scale “On a scale of ‘ 0’ – ‘ 10’ (show the pain scale), if ‘ 0’ = no pain and ‘ 10’ = worst pain you can imagine, what is your pain score now? ” • Patient is asked to slide the indicator along the scale to show the severity of his/her pain, which is recorded as a number (zero to 10)
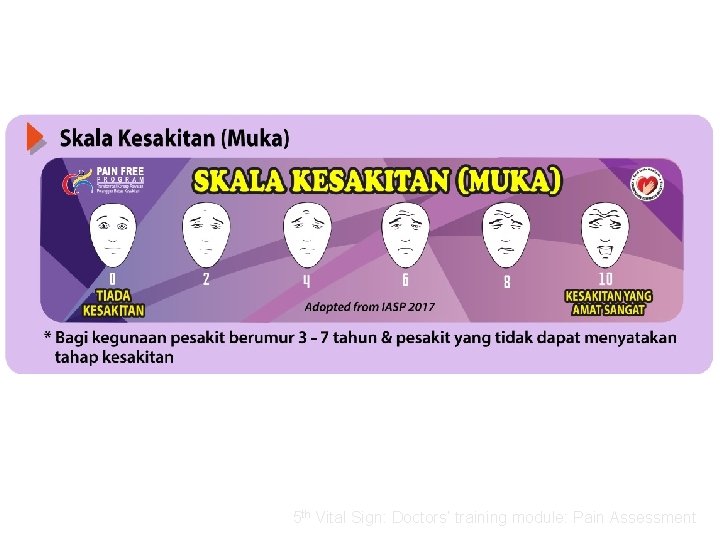
Pain measurement Scales used in children / infants and in cognitively impaired patients • Wong Baker Faces Scale • FLACC scale 5 th Vital Sign: Doctors’ training module: Pain Assessment
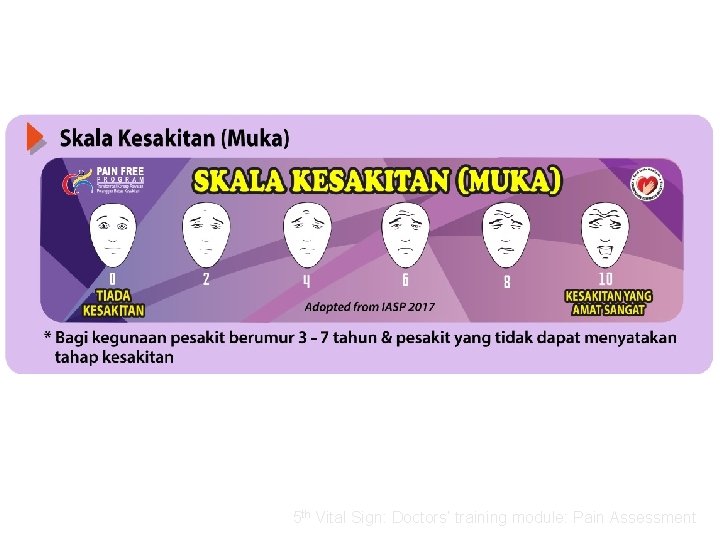
Wong-Baker Faces Pain Rating Scale 5 th Vital Sign: Doctors’ training module: Pain Assessment

FLACC SCORE Skala permarkahan Kesakitan Melalui Tingkahlaku 5 th Vital Sign: Doctors’ training module: Pain Assessment
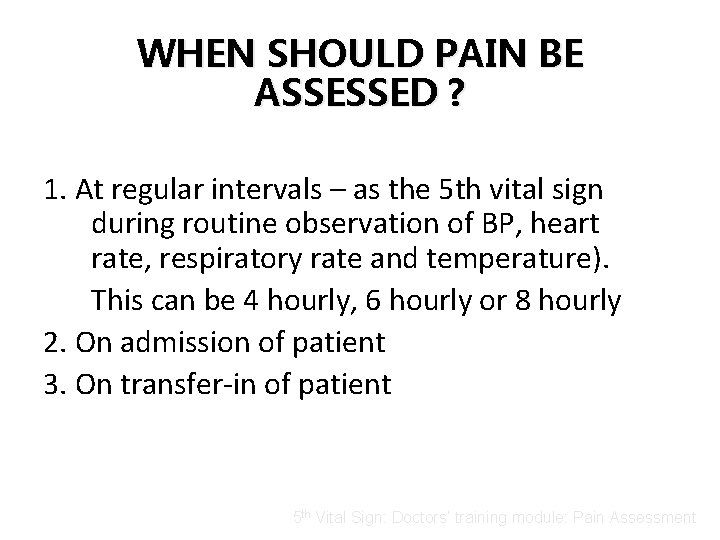
WHEN SHOULD PAIN BE ASSESSED ? 1. At regular intervals – as the 5 th vital sign during routine observation of BP, heart rate, respiratory rate and temperature). This can be 4 hourly, 6 hourly or 8 hourly 2. On admission of patient 3. On transfer-in of patient 5 th Vital Sign: Doctors’ training module: Pain Assessment
WHEN SHOULD PAIN BE ASSESSED ? . . cont 4. At other times apart from scheduled observations: - Half to one hour after administration of analgesics and nursing intervention for pain relief During and after any painful procedure in the ward e. g. wound dressing Whenever the patient complains of pain 5 th Vital Sign: Doctors’ training module: Pain Assessment
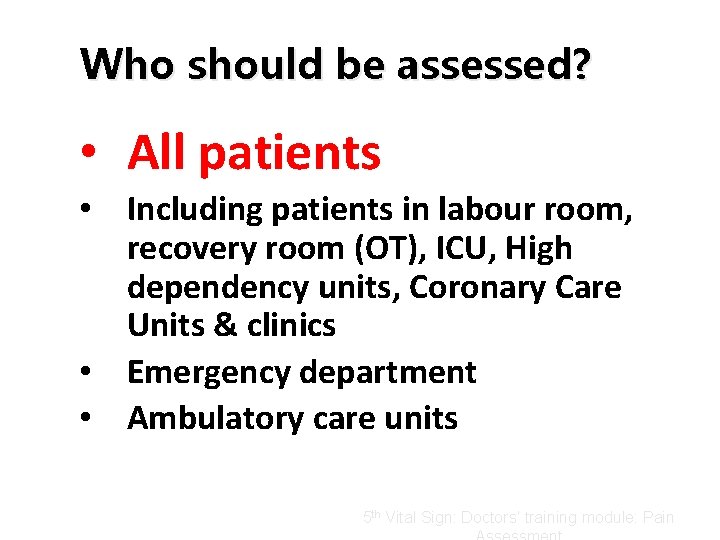
Who should be assessed? • All patients • Including patients in labour room, recovery room (OT), ICU, High dependency units, Coronary Care Units & clinics • Emergency department • Ambulatory care units 5 th Vital Sign: Doctors’ training module: Pain
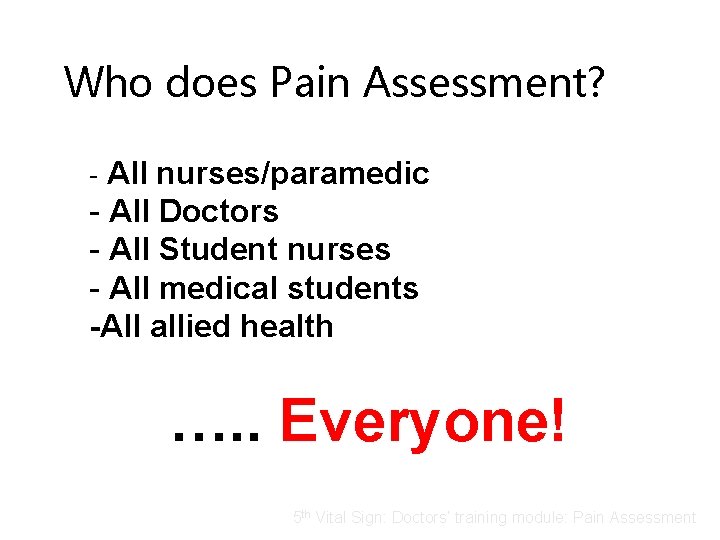
Who does Pain Assessment? - All nurses/paramedic - All Doctors - All Student nurses - All medical students -All allied health …. . Everyone! 5 th Vital Sign: Doctors’ training module: Pain Assessment
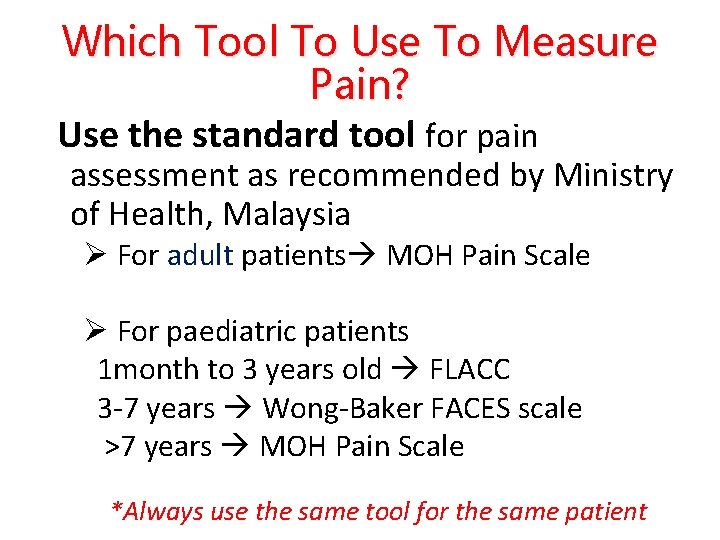
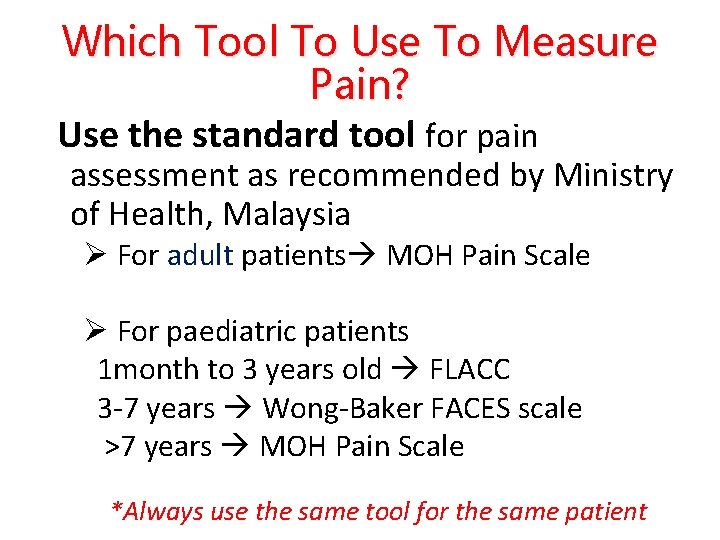
Which Tool To Use To Measure Pain? Use the standard tool for pain assessment as recommended by Ministry of Health, Malaysia Ø For adult patients MOH Pain Scale Ø For paediatric patients 1 month to 3 years old FLACC 3 -7 years Wong-Baker FACES scale >7 years MOH Pain Scale *Always use the same tool for the same patient

UNABLE TO ASSESS PAIN • Sedated • Unconscious patients • Please record ‘Unable to Score’ 5 th Vital Sign: Doctors’ training module: Pain Assessment
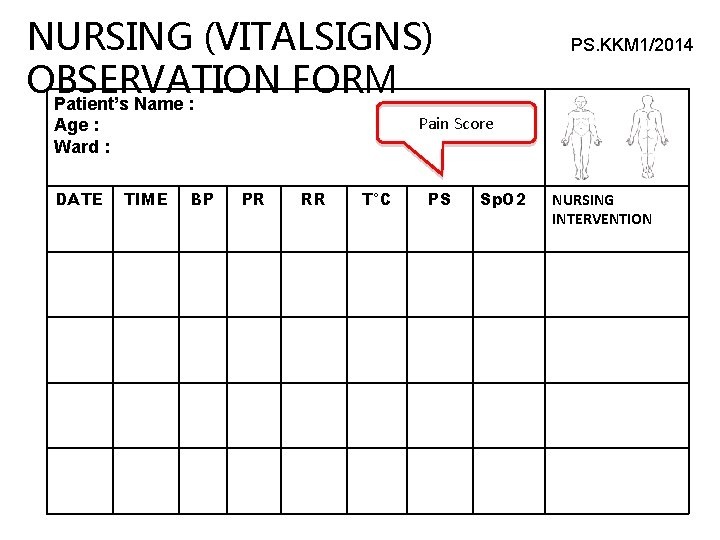
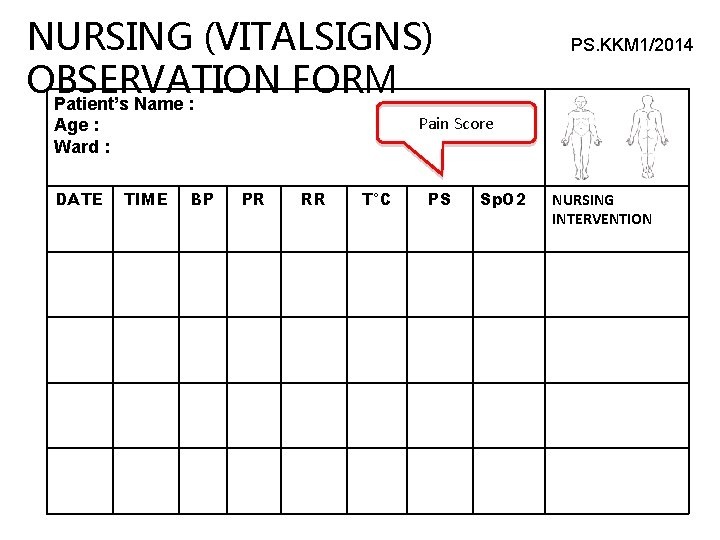
NURSING (VITALSIGNS) OBSERVATION FORM Patient’s Name : Pain Score Age : Ward : DATE PS. KKM 1/2014 TIME BP PR RR T°C PS Sp. O 2 NURSING INTERVENTION

Acute Pain Management
Pain Treatment Overview Aims � To discuss non-drug and drug treatments where you work � To classify pain treatments
Non-Drug Treatments • Physical • Rest, ice, compression, elevation • Surgery • Acupuncture, massage, physiotherapy • Psychological • Explanation • Reassurance • Counseling
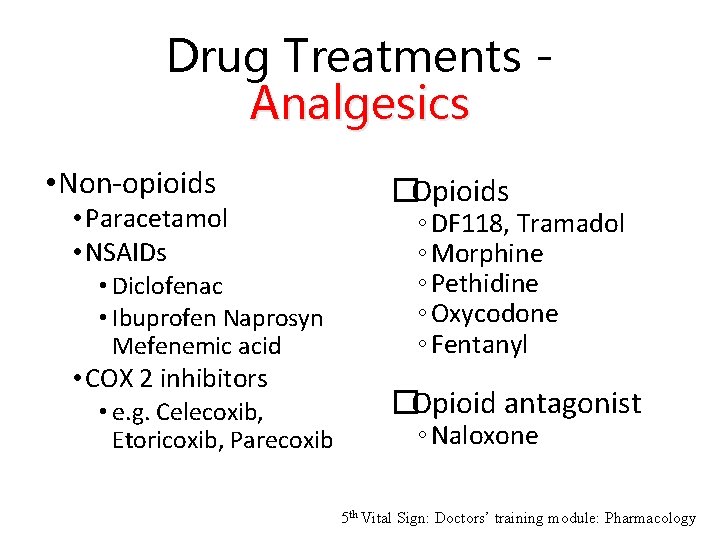
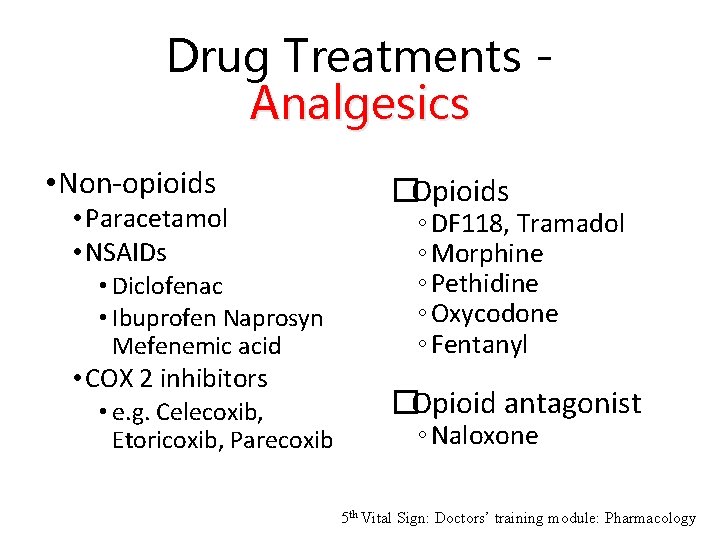
Drug Treatments Analgesics • Non-opioids • Paracetamol • NSAIDs • Diclofenac • Ibuprofen Naprosyn Mefenemic acid • COX 2 inhibitors • e. g. Celecoxib, Etoricoxib, Parecoxib �Opioids ◦ DF 118, Tramadol ◦ Morphine ◦ Pethidine ◦ Oxycodone ◦ Fentanyl �Opioid antagonist ◦ Naloxone 5 th Vital Sign: Doctors’ training module: Pharmacology
Other analgesics • Amitriptyline • Carbamazepine • Local anesthetics • Ketamine • Tramadol • Clonidine • Entonox (N 2 O/O 2)
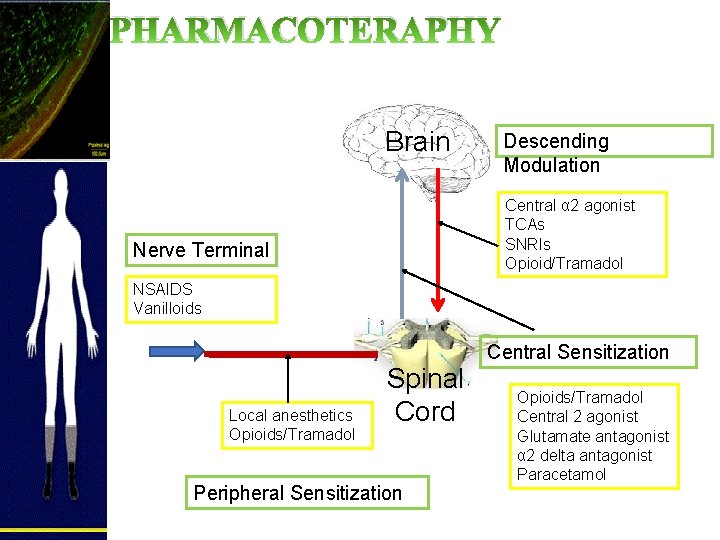
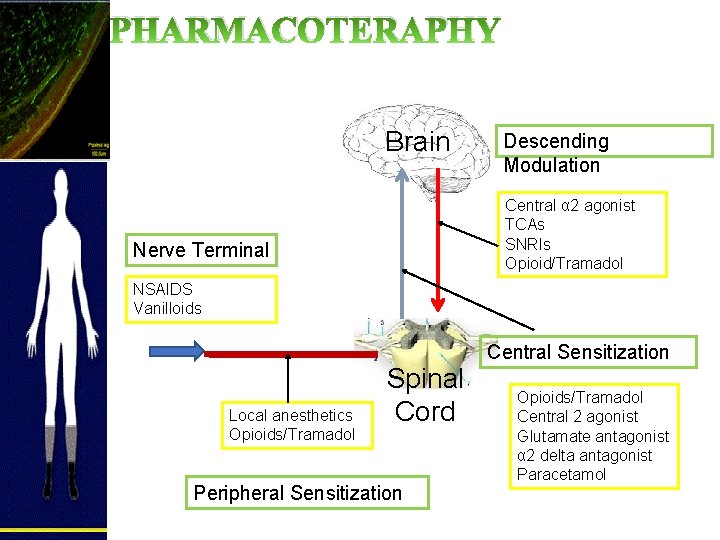
PHARMACOTERAPHY Brain Descending Modulation Central α 2 agonist TCAs SNRIs Opioid/Tramadol Nerve Terminal NSAIDS Vanilloids Local anesthetics Opioids/Tramadol Spinal Cord Peripheral Sensitization Central Sensitization Opioids/Tramadol Central 2 agonist Glutamate antagonist α 2 delta antagonist Paracetamol
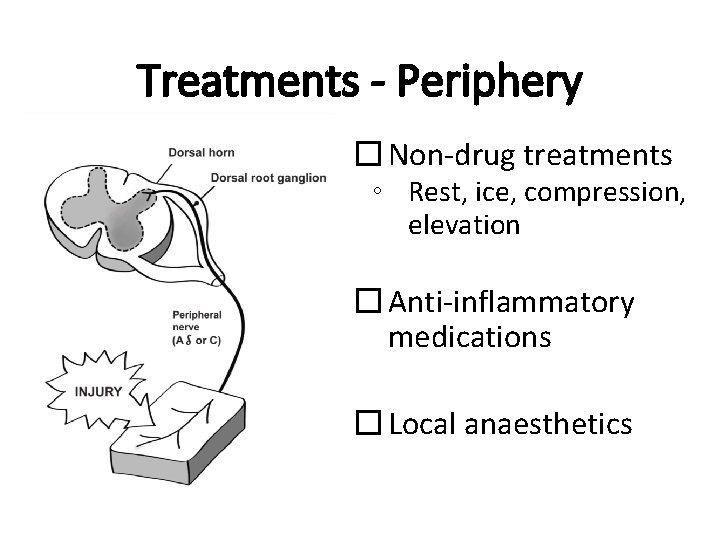
Treatments - Periphery � Non-drug treatments ◦ Rest, ice, compression, elevation � Anti-inflammatory medications � Local anaesthetics

Treatments - Spinal Cord �Non-drug treatments ◦ Acupuncture, massage �Local anaesthetics �Opioids �Ketamine
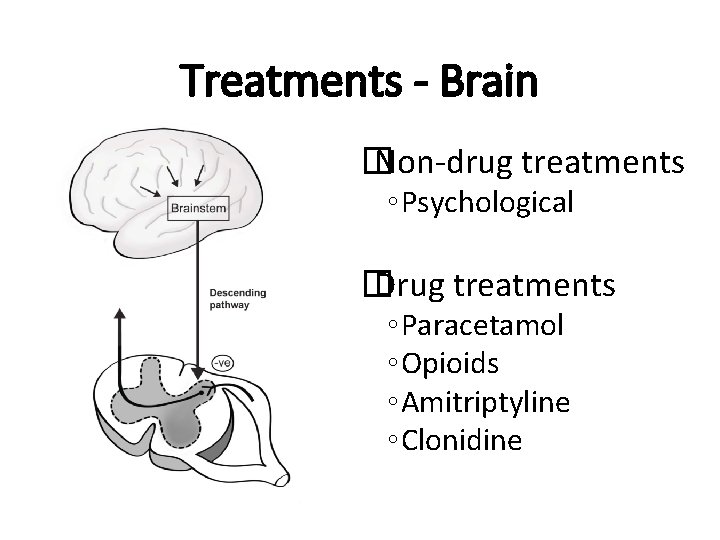
Treatments - Brain � Non-drug treatments ◦ Psychological � Drug treatments ◦ Paracetamol ◦ Opioids ◦ Amitriptyline ◦ Clonidine
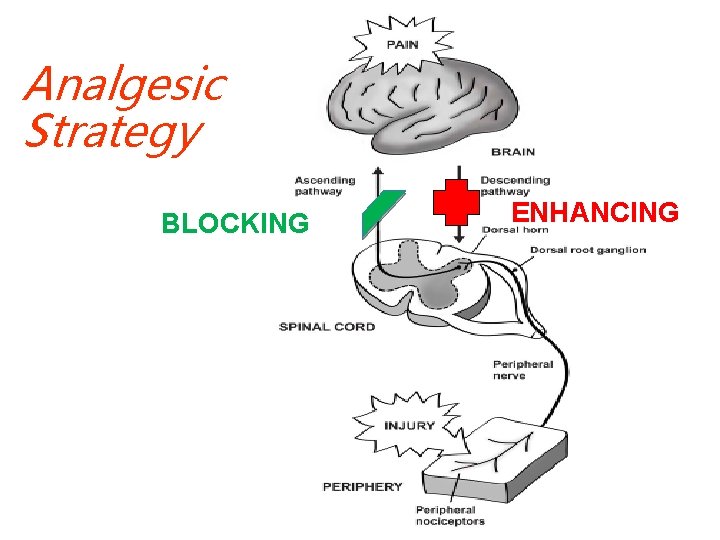
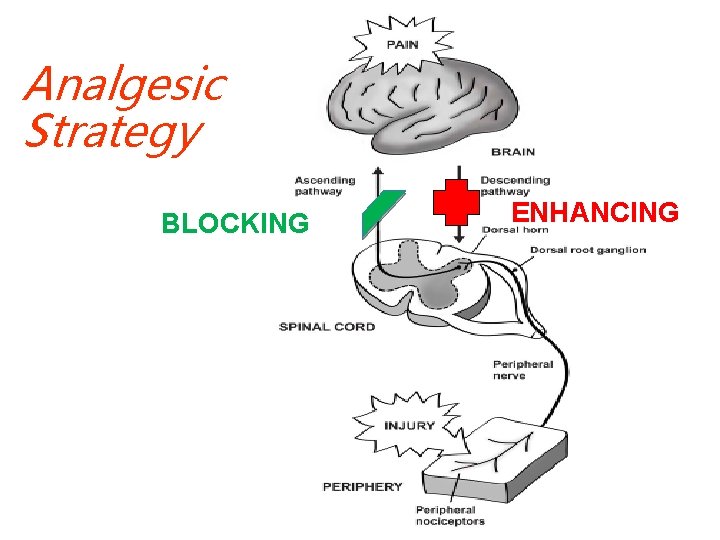
Analgesic Strategy BLOCKING ENHANCING
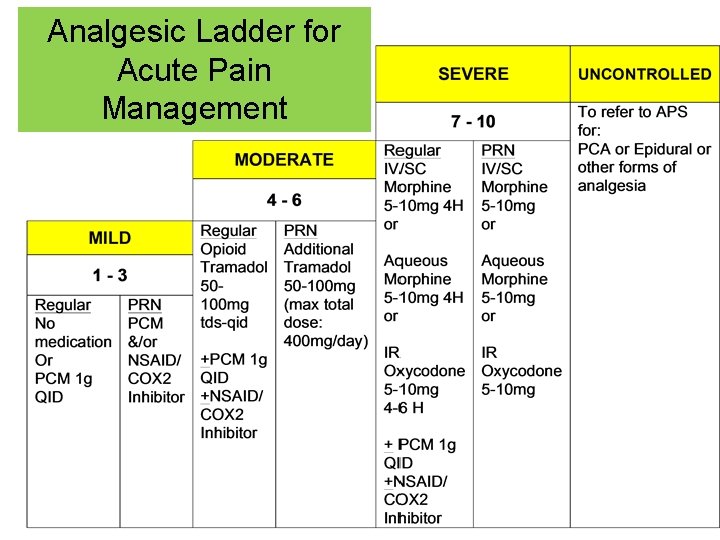
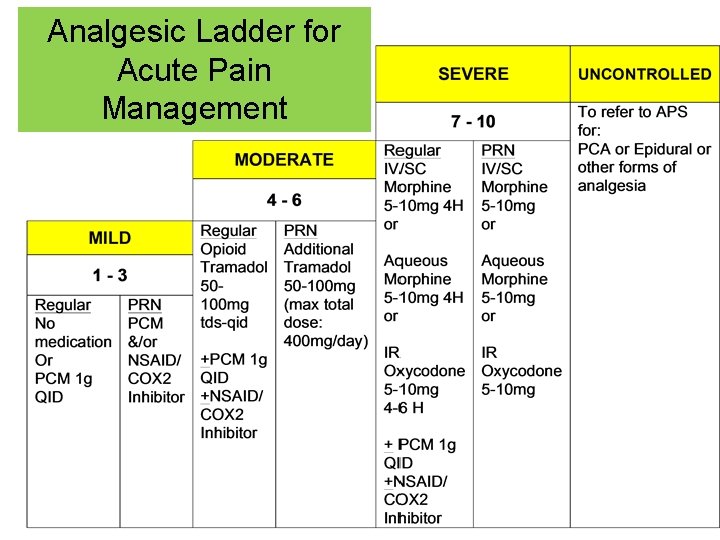
Analgesic Ladder for Acute Pain Management
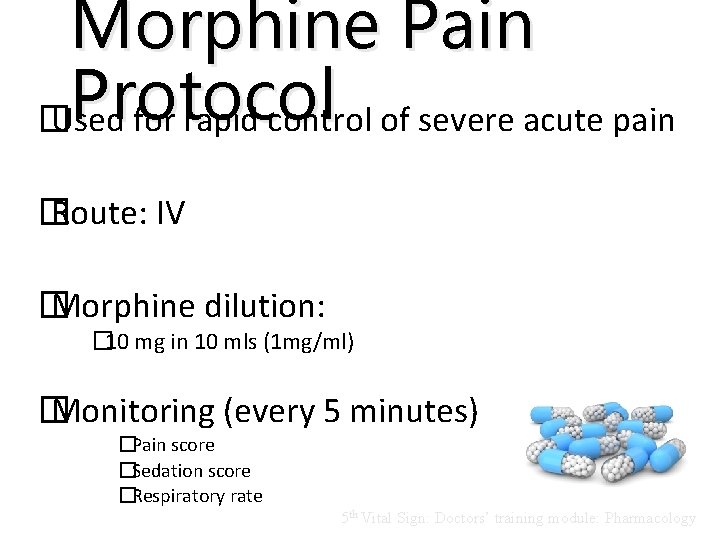
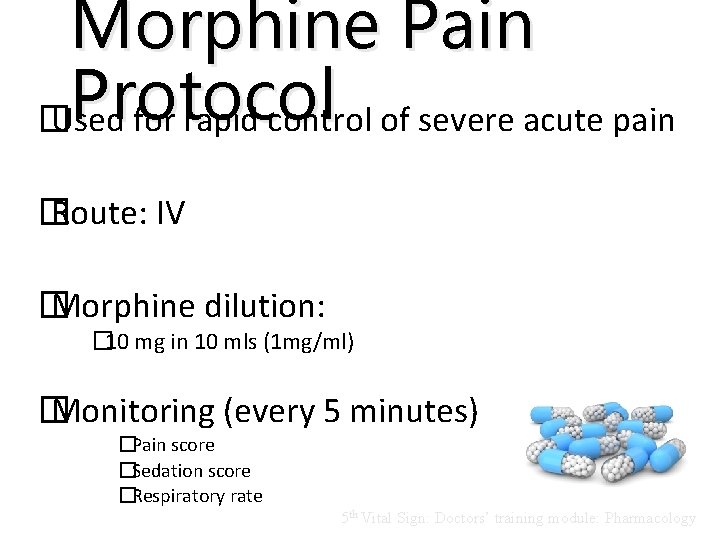
Morphine Pain Protocol � Used for rapid control of severe acute pain � Route: IV � Morphine dilution: � 10 mg in 10 mls (1 mg/ml) � Monitoring (every 5 minutes) �Pain score �Sedation score �Respiratory rate 5 th Vital Sign: Doctors’ training module: Pharmacology

PAIN AS THE 5 TH VITAL SIGN: FLOW CHART FOR DOCTORS
Flow chart for DOCTORS
MANAGEMENT OF SIDE EFFECTS
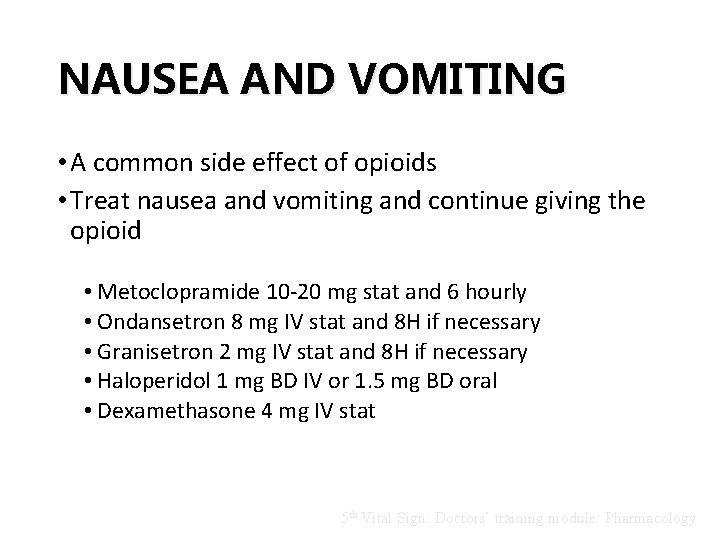
NAUSEA AND VOMITING • A common side effect of opioids • Treat nausea and vomiting and continue giving the opioid • Metoclopramide 10 -20 mg stat and 6 hourly • Ondansetron 8 mg IV stat and 8 H if necessary • Granisetron 2 mg IV stat and 8 H if necessary • Haloperidol 1 mg BD IV or 1. 5 mg BD oral • Dexamethasone 4 mg IV stat 5 th Vital Sign: Doctors’ training module: Pharmacology
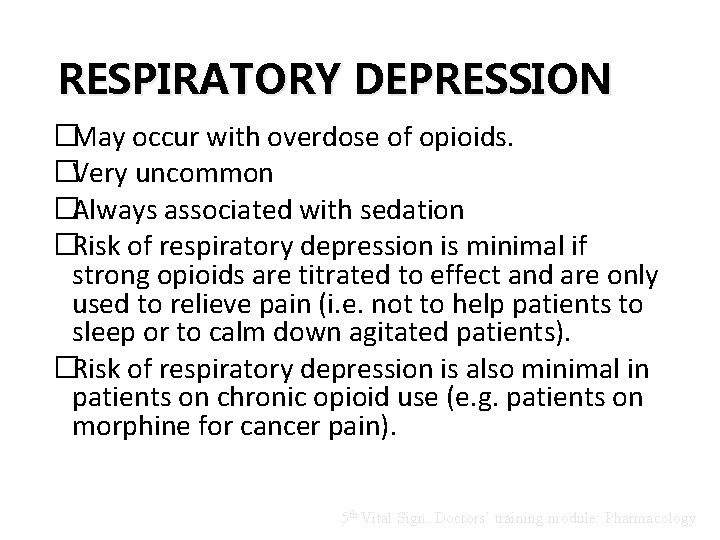
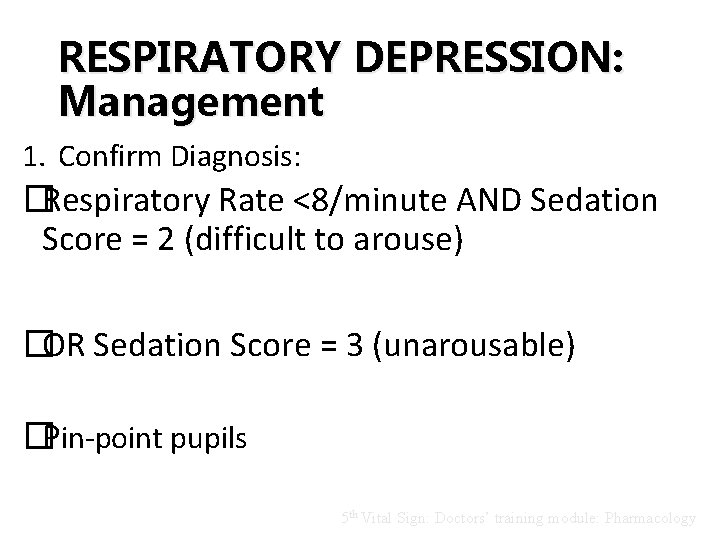
RESPIRATORY DEPRESSION �May occur with overdose of opioids. �Very uncommon �Always associated with sedation �Risk of respiratory depression is minimal if strong opioids are titrated to effect and are only used to relieve pain (i. e. not to help patients to sleep or to calm down agitated patients). �Risk of respiratory depression is also minimal in patients on chronic opioid use (e. g. patients on morphine for cancer pain). 5 th Vital Sign: Doctors’ training module: Pharmacology
RESPIRATORY DEPRESSION: Management 1. Confirm Diagnosis: �Respiratory Rate <8/minute AND Sedation Score = 2 (difficult to arouse) �OR Sedation Score = 3 (unarousable) �Pin-point pupils 5 th Vital Sign: Doctors’ training module: Pharmacology
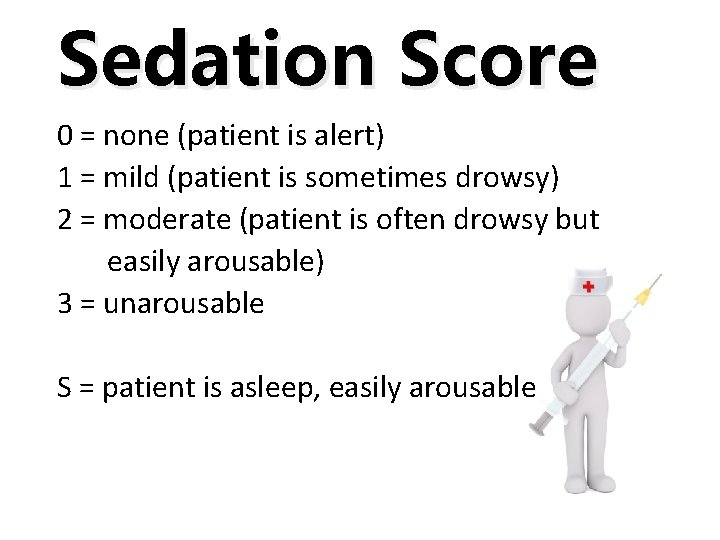
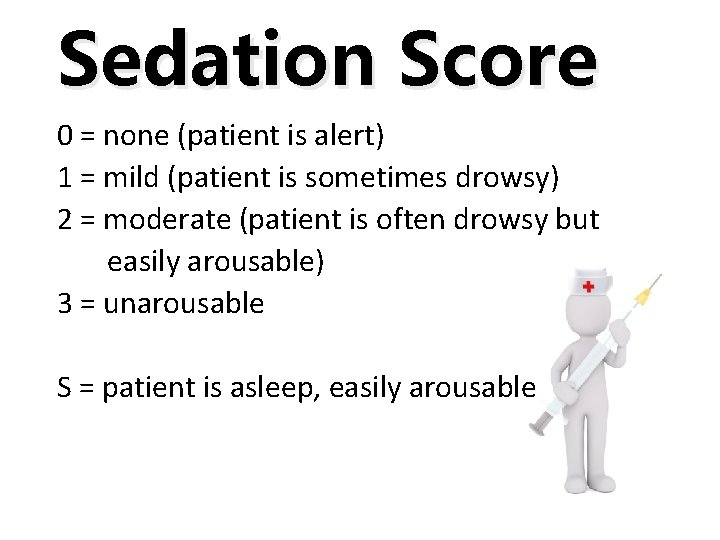
Sedation Score 0 = none (patient is alert) 1 = mild (patient is sometimes drowsy) 2 = moderate (patient is often drowsy but easily arousable) 3 = unarousable S = patient is asleep, easily arousable
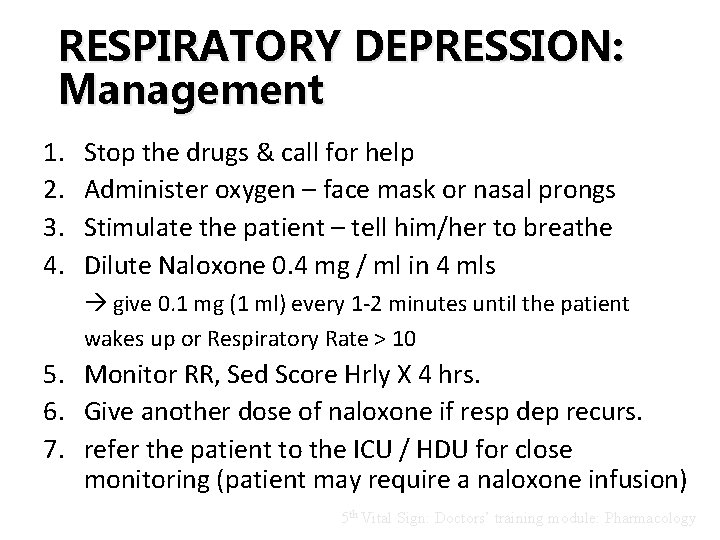
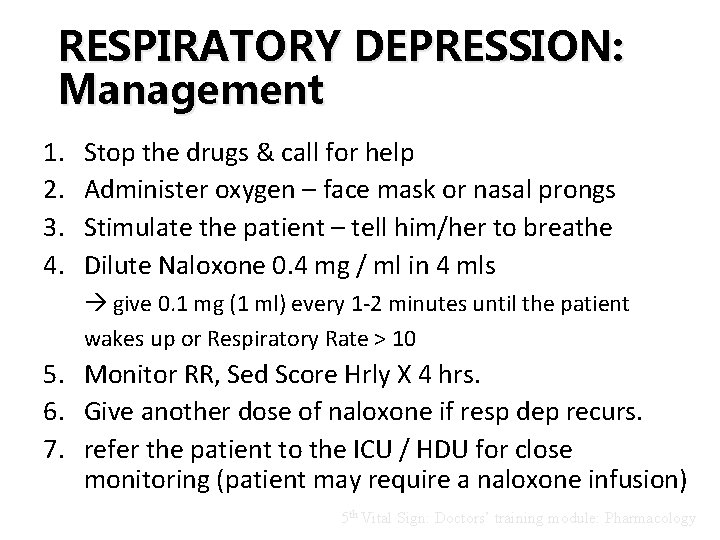
RESPIRATORY DEPRESSION: Management 1. 2. 3. 4. Stop the drugs & call for help Administer oxygen – face mask or nasal prongs Stimulate the patient – tell him/her to breathe Dilute Naloxone 0. 4 mg / ml in 4 mls give 0. 1 mg (1 ml) every 1 -2 minutes until the patient wakes up or Respiratory Rate > 10 5. Monitor RR, Sed Score Hrly X 4 hrs. 6. Give another dose of naloxone if resp dep recurs. 7. refer the patient to the ICU / HDU for close monitoring (patient may require a naloxone infusion) 5 th Vital Sign: Doctors’ training module: Pharmacology

Management of acute pain. . …Key points…. .
Key points…. . �For Pain as the 5 th Vital Sign to have an impact in improving pain management in our hospitals doctors should understand all the analgesic medications available and know how and when to use them 5 th Vital Sign: Doctors’ training module: Pharmacology
Key points…. . • Important points to note on the pharmacology of drugs are Ø Onset and duration of action (so you know how often to prescribe the drug) ØSide effects (so you can anticipate and treat side effect) 5 th Vital Sign: Doctors’ training module: Pharmacology
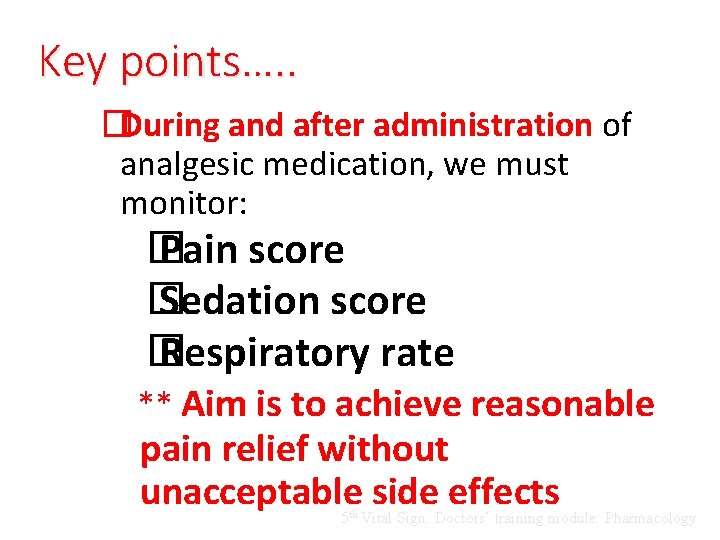
Key points…. . �During and after administration of analgesic medication, we must monitor: � Pain score � Sedation score � Respiratory rate ** Aim is to achieve reasonable pain relief without unacceptable side effects 5 th Vital Sign: Doctors’ training module: Pharmacology
PAIN in paediatric patients
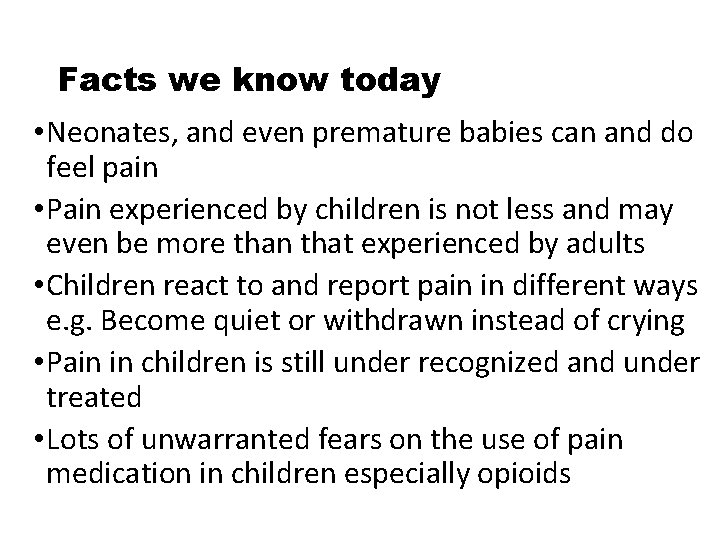
Facts we know today • Neonates, and even premature babies can and do feel pain • Pain experienced by children is not less and may even be more than that experienced by adults • Children react to and report pain in different ways e. g. Become quiet or withdrawn instead of crying • Pain in children is still under recognized and under treated • Lots of unwarranted fears on the use of pain medication in children especially opioids
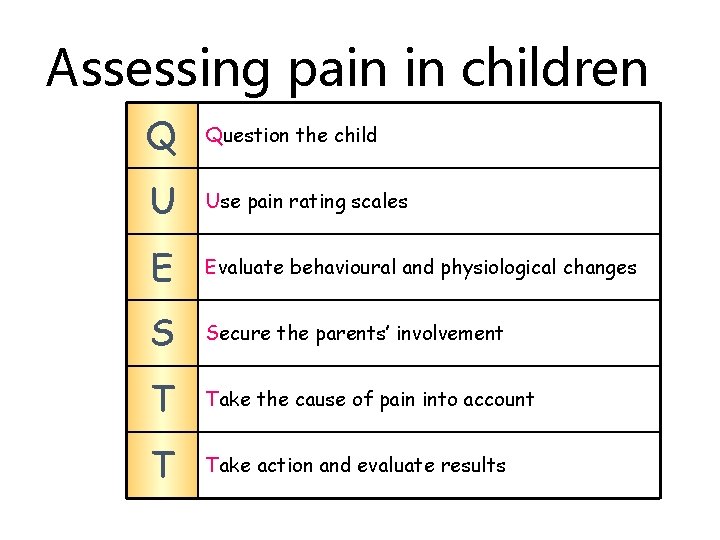
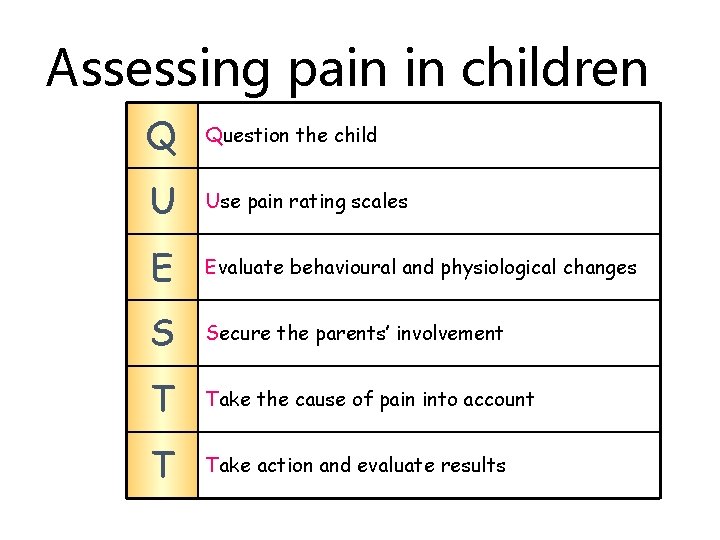
Assessing pain in children Q Question the child U Use pain rating scales E Evaluate behavioural and physiological changes S Secure the parents’ involvement T Take the cause of pain into account T Take action and evaluate results
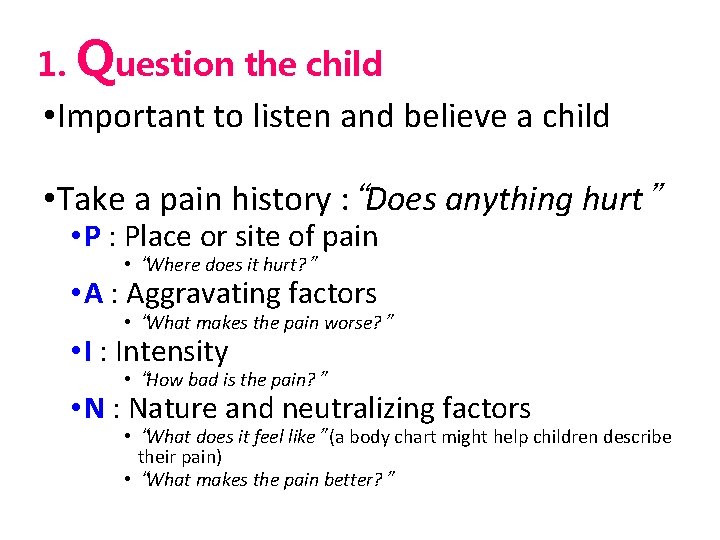
1. Question the child • Important to listen and believe a child • Take a pain history : “Does anything hurt” • P : Place or site of pain • “Where does it hurt? ” • A : Aggravating factors • “What makes the pain worse? ” • I : Intensity • “How bad is the pain? ” • N : Nature and neutralizing factors • “What does it feel like” (a body chart might help children describe their pain) • “What makes the pain better? ”
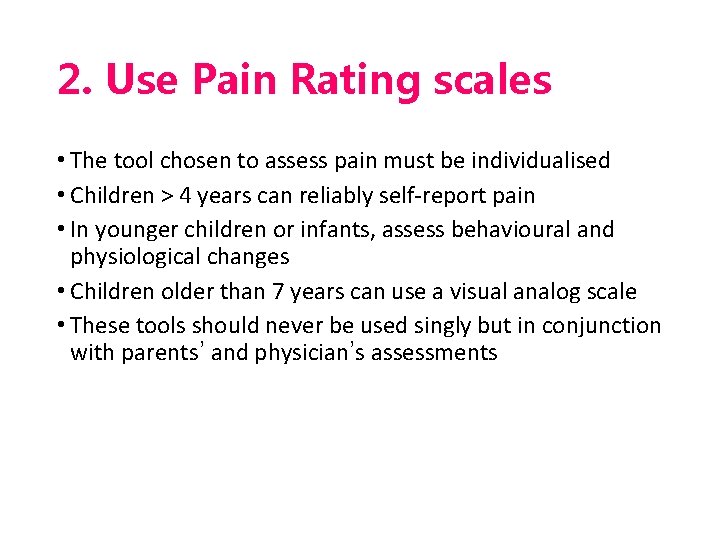
2. Use Pain Rating scales • The tool chosen to assess pain must be individualised • Children > 4 years can reliably self-report pain • In younger children or infants, assess behavioural and physiological changes • Children older than 7 years can use a visual analog scale • These tools should never be used singly but in conjunction with parents’ and physician’s assessments
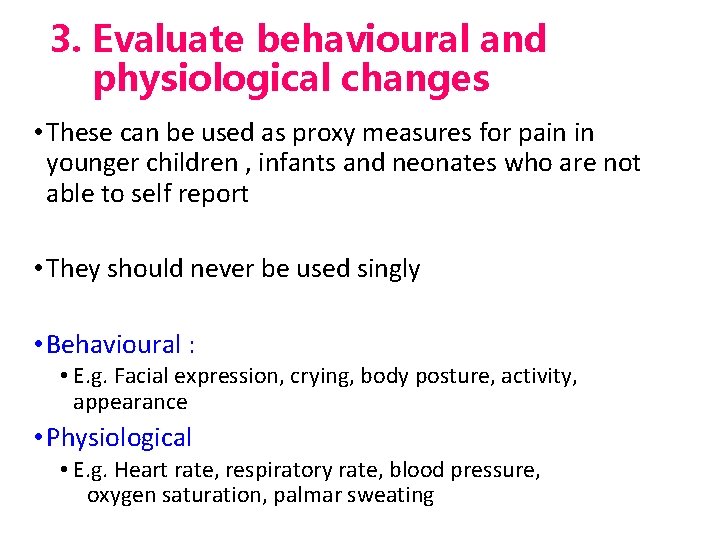
3. Evaluate behavioural and physiological changes • These can be used as proxy measures for pain in younger children , infants and neonates who are not able to self report • They should never be used singly • Behavioural : • E. g. Facial expression, crying, body posture, activity, appearance • Physiological • E. g. Heart rate, respiratory rate, blood pressure, oxygen saturation, palmar sweating
4. Secure the parents involvement • Get parents involvement in management of their child’s pain • Parents are often good judges of their child’s pain • However, if there is a discrepancy between the child and parents’ report, do not over rule a child’s response
5. Take the cause of pain into account • Search for any possible simple reversible causes of pain eg. A tissued line • Anxiety may also be a cause of pain • sometimes a child might cry due to separation anxiety and not pain.
6. Take action and evaluate the results • Do not ignore any complaints • If pain is present, check with patient/care giver is intervention required • Intervention is not necessarily a medication, it can just be touching, gentle massage or hot or cold packs • Always evaluate response after any intervention
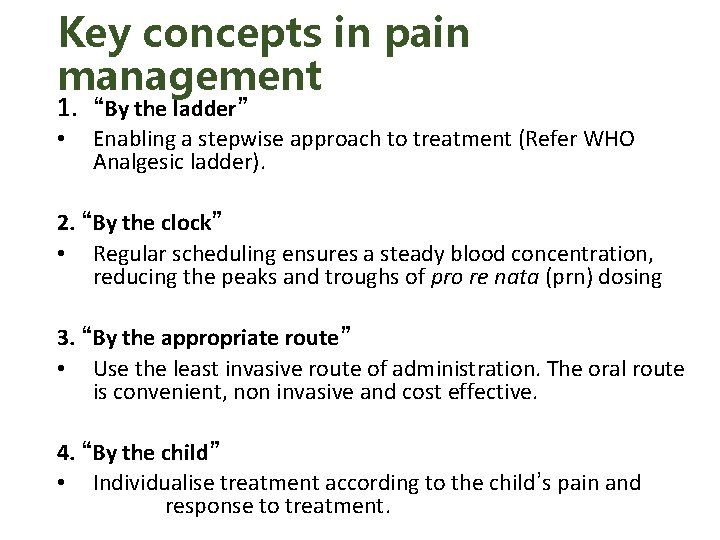
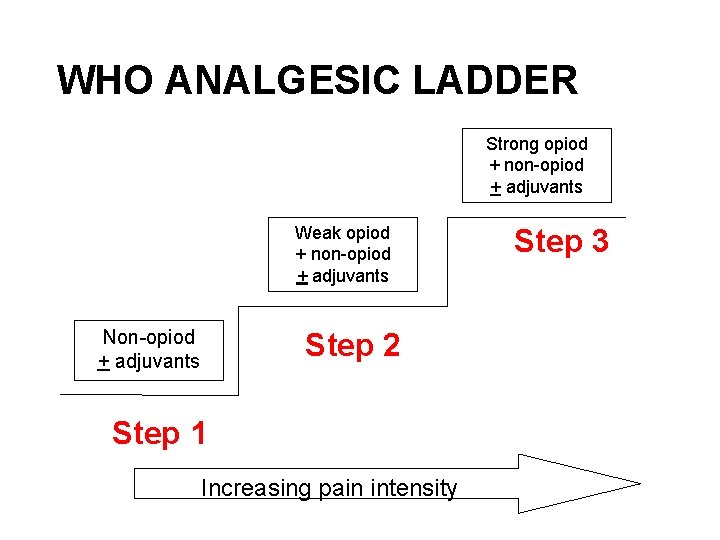
Key concepts in pain management 1. “By the ladder” • Enabling a stepwise approach to treatment (Refer WHO Analgesic ladder). 2. “By the clock” • Regular scheduling ensures a steady blood concentration, reducing the peaks and troughs of pro re nata (prn) dosing 3. “By the appropriate route” • Use the least invasive route of administration. The oral route is convenient, non invasive and cost effective. 4. “By the child” • Individualise treatment according to the child’s pain and response to treatment.
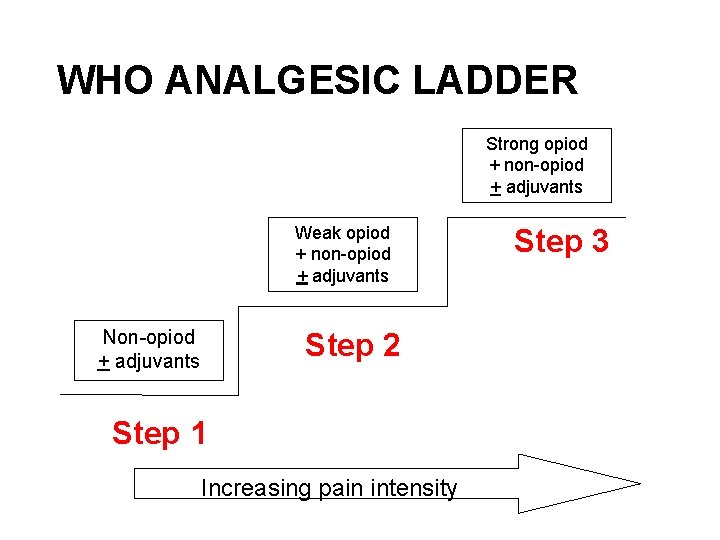
WHO ANALGESIC LADDER Strong opiod + non-opiod + adjuvants Weak opiod + non-opiod + adjuvants Non-opiod + adjuvants Step 2 Step 1 Increasing pain intensity Step 3
Methods of Pain relief 1) Pharmacological 2) Non pharmacological i. Suitable environment ii. Distraction iii. Guided imagery iv. Information before a painful procedure v. Music vi. Heat and cold packs vii. Massage and physical therapy
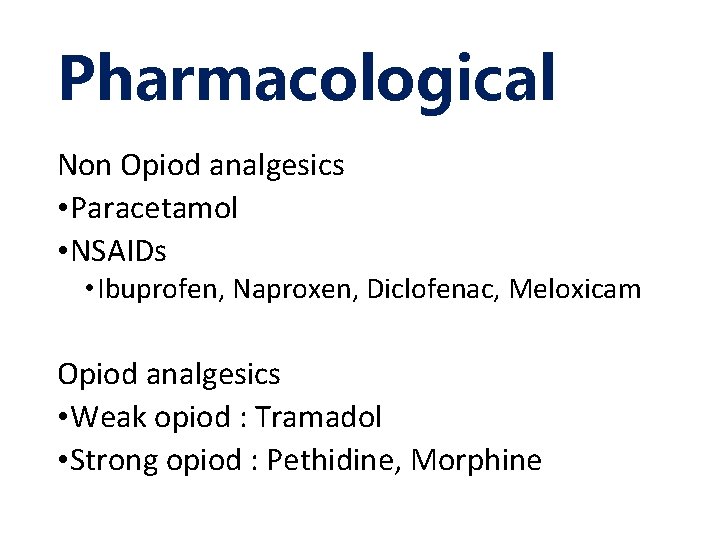
Pharmacological Non Opiod analgesics • Paracetamol • NSAIDs • Ibuprofen, Naproxen, Diclofenac, Meloxicam Opiod analgesics • Weak opiod : Tramadol • Strong opiod : Pethidine, Morphine
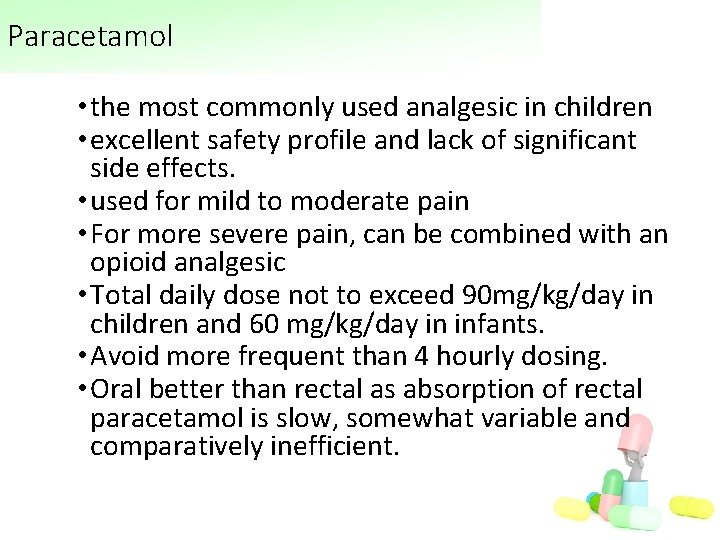
Paracetamol • the most commonly used analgesic in children • excellent safety profile and lack of significant side effects. • used for mild to moderate pain • For more severe pain, can be combined with an opioid analgesic • Total daily dose not to exceed 90 mg/kg/day in children and 60 mg/kg/day in infants. • Avoid more frequent than 4 hourly dosing. • Oral better than rectal as absorption of rectal paracetamol is slow, somewhat variable and comparatively inefficient.
NSAIDs • Ibuprofen - indicated for mild to moderate pain. • Children appear to have a lower incidence of renal and gastrointestinal side effects when compared to adults even with chronic administration.

Opioid �very useful for treatment of pain in patients of all ages �provide excellent analgesia with a wide margin of safety for a vast majority of children �routes of administration : oral, iv, rectal, transdermal or transmucosal �oral and iv route preferable �avoid intramuscular injections unless absolutely necessary as children will deny they are in pain to avoid a shot.
Conclusion • Infants and young children can and do feel pain • Untreated pain can have a negative impact and long term consequences • Pain in paediatric patients needs to be recognised and managed • Tools for assessment is dependent not only on age of the child but also other factors. • We need to treat children in a more humane manner and be responsible to eliminate or assuage pain.
Thank You
 Pain as the fifth vital sign
Pain as the fifth vital sign Pain as 5th vital sign kkm
Pain as 5th vital sign kkm Divided highway begins sign
Divided highway begins sign Capacidad vital y capacidad vital forzada
Capacidad vital y capacidad vital forzada Pregnancy or period
Pregnancy or period Symptoms before period
Symptoms before period Pain x mad
Pain x mad Hunger vital sign
Hunger vital sign Vital signs
Vital signs Respiratory rate normal range
Respiratory rate normal range Normal vital sign ranges
Normal vital sign ranges Vital signs
Vital signs Vital signs
Vital signs Vital signs normal values
Vital signs normal values Tempat pengukuran denyut nadi
Tempat pengukuran denyut nadi Pulse location in the body
Pulse location in the body What are normal vital signs
What are normal vital signs Analgesic ladder kkm
Analgesic ladder kkm Orthostatic vital sign
Orthostatic vital sign Vital signs
Vital signs Cewt chart 5-11
Cewt chart 5-11 Hospital pharmacy layout
Hospital pharmacy layout Which is the regular polygon
Which is the regular polygon Chvostek sign trousseau sign
Chvostek sign trousseau sign Hypermagnesemia causes
Hypermagnesemia causes Pleocytosis pronunciation
Pleocytosis pronunciation Chvostek sign trousseau sign
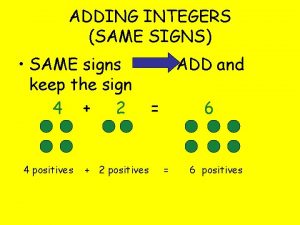
Chvostek sign trousseau sign How do you add integers with the same sign
How do you add integers with the same sign V cc cc
V cc cc Phép trừ bù
Phép trừ bù Hát lên người ơi alleluia
Hát lên người ơi alleluia Sự nuôi và dạy con của hổ
Sự nuôi và dạy con của hổ đại từ thay thế
đại từ thay thế Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Công thức tính độ biến thiên đông lượng
Công thức tính độ biến thiên đông lượng Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Dot
Dot Lời thề hippocrates
Lời thề hippocrates Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Phản ứng thế ankan
Phản ứng thế ankan Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Kể tên các môn thể thao
Kể tên các môn thể thao Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập điện thế nghỉ
điện thế nghỉ Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Lp html
Lp html Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Tia chieu sa te
Tia chieu sa te Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Một số thể thơ truyền thống
Một số thể thơ truyền thống Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Sơ đồ cơ thể người
Sơ đồ cơ thể người Tư thế ngồi viết
Tư thế ngồi viết Các số nguyên tố là gì
Các số nguyên tố là gì đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Chụp phim tư thế worms-breton
Chụp phim tư thế worms-breton ưu thế lai là gì
ưu thế lai là gì Thẻ vin
Thẻ vin Thể thơ truyền thống
Thể thơ truyền thống Bàn tay mà dây bẩn
Bàn tay mà dây bẩn Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Bổ thể
Bổ thể Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Diễn thế sinh thái là
Diễn thế sinh thái là Tư thế ngồi viết
Tư thế ngồi viết Respiratory rate chart
Respiratory rate chart Pengertian statistik vital
Pengertian statistik vital Civil registration system
Civil registration system Orthostatic vital signs positive
Orthostatic vital signs positive Normal range for vital signs
Normal range for vital signs Lungs
Lungs Artery parts of the body to locate pulse beat
Artery parts of the body to locate pulse beat Vital signs normal rate
Vital signs normal rate Iron tools and agriculture
Iron tools and agriculture 8 vital signs
8 vital signs Apical radial pulse
Apical radial pulse Chapter 16:7 reading an aneroid sphygmomanometer
Chapter 16:7 reading an aneroid sphygmomanometer Normal vital signs for all age groups
Normal vital signs for all age groups Poetry is nearer to the truth than history
Poetry is nearer to the truth than history Ciclo vital de la familia
Ciclo vital de la familia Measuring and recording vital signs
Measuring and recording vital signs Ciclo vital familiar oms
Ciclo vital familiar oms Ciclo vital familiar
Ciclo vital familiar Oms ciclo vital familiar
Oms ciclo vital familiar Mosaicos de san vital
Mosaicos de san vital Apgar familiar
Apgar familiar