Electrolytes Hyponatremia What is the serum osmolarity 2Na


- Slides: 36
Electrolytes
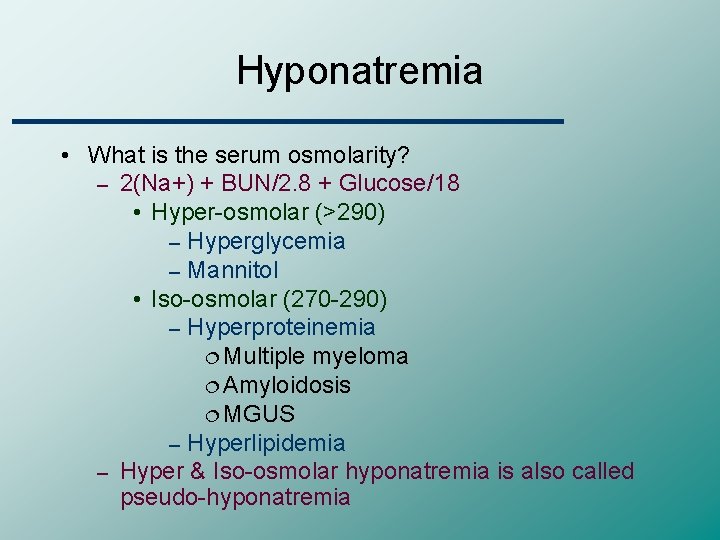
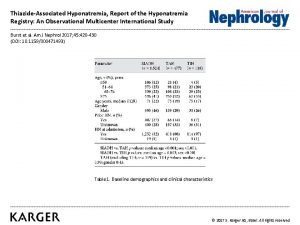
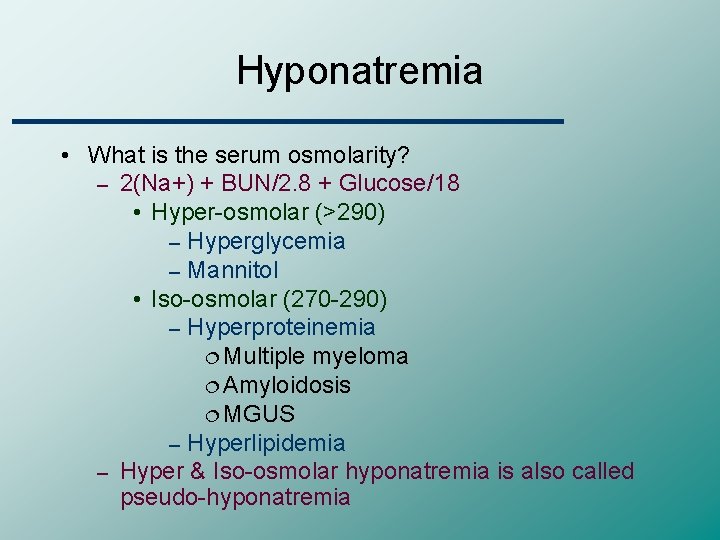
Hyponatremia • What is the serum osmolarity? – 2(Na+) + BUN/2. 8 + Glucose/18 • Hyper-osmolar (>290) – Hyperglycemia – Mannitol • Iso-osmolar (270 -290) – Hyperproteinemia ¦ Multiple myeloma ¦ Amyloidosis ¦ MGUS – Hyperlipidemia – Hyper & Iso-osmolar hyponatremia is also called pseudo-hyponatremia
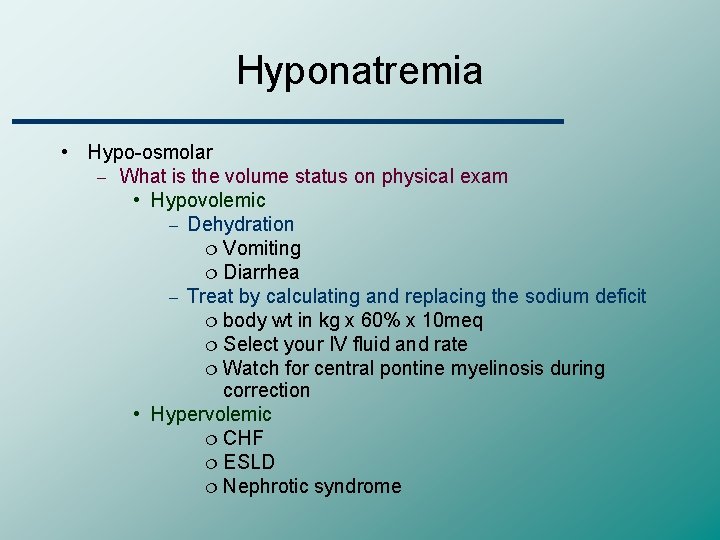
Hyponatremia • Hypo-osmolar – What is the volume status on physical exam • Hypovolemic – Dehydration ¦ Vomiting ¦ Diarrhea – Treat by calculating and replacing the sodium deficit ¦ body wt in kg x 60% x 10 meq ¦ Select your IV fluid and rate ¦ Watch for central pontine myelinosis during correction • Hypervolemic ¦ CHF ¦ ESLD ¦ Nephrotic syndrome
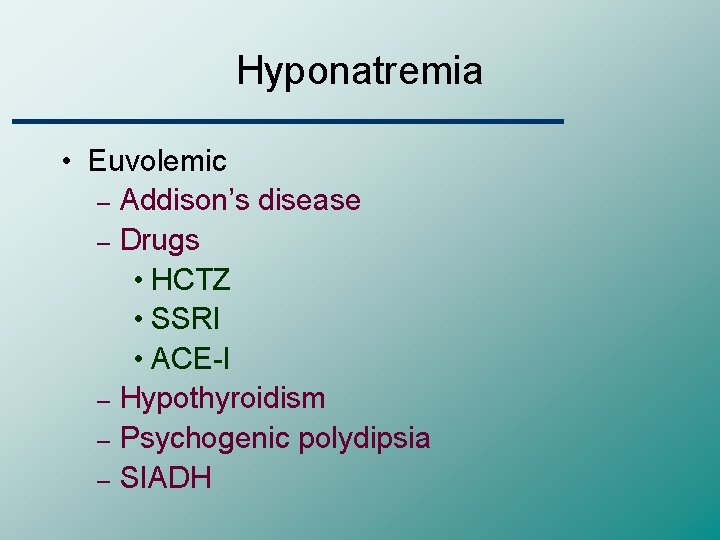
Hyponatremia • Euvolemic – Addison’s disease – Drugs • HCTZ • SSRI • ACE-I – Hypothyroidism – Psychogenic polydipsia – SIADH
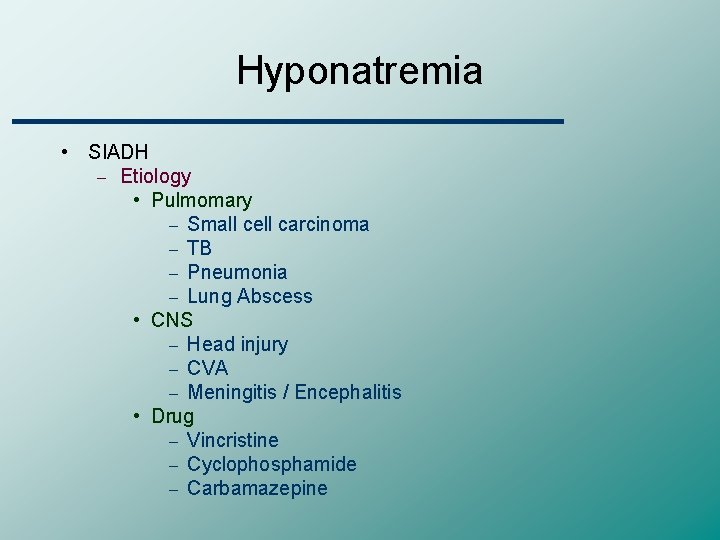
Hyponatremia • SIADH – Etiology • Pulmomary – Small cell carcinoma – TB – Pneumonia – Lung Abscess • CNS – Head injury – CVA – Meningitis / Encephalitis • Drug – Vincristine – Cyclophosphamide – Carbamazepine
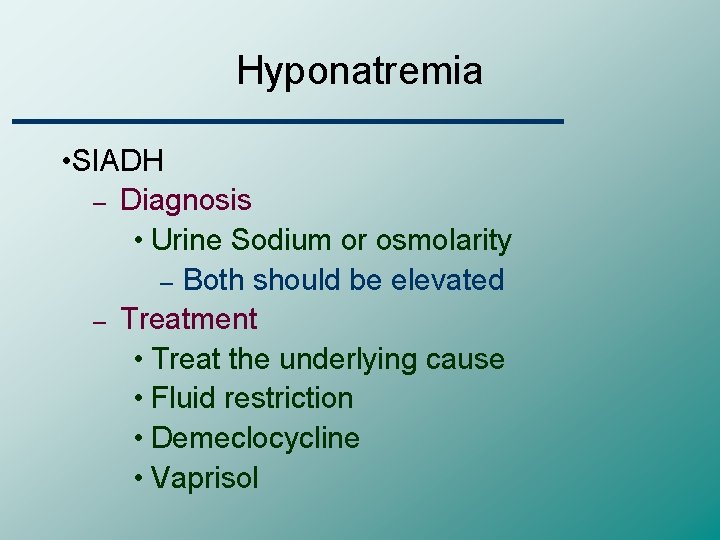
Hyponatremia • SIADH – Diagnosis • Urine Sodium or osmolarity – Both should be elevated – Treatment • Treat the underlying cause • Fluid restriction • Demeclocycline • Vaprisol

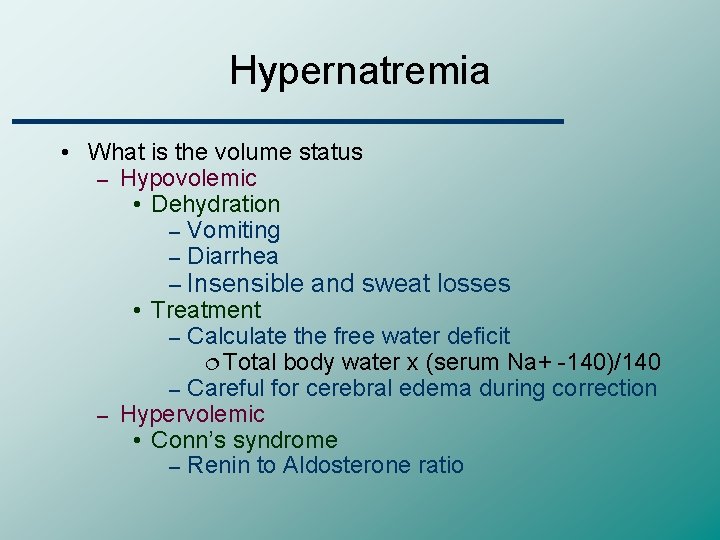
Hypernatremia • What is the volume status – Hypovolemic • Dehydration – Vomiting – Diarrhea – Insensible and sweat losses • Treatment – Calculate the free water deficit ¦ Total body water x (serum Na+ -140)/140 – Careful for cerebral edema during correction – Hypervolemic • Conn’s syndrome – Renin to Aldosterone ratio
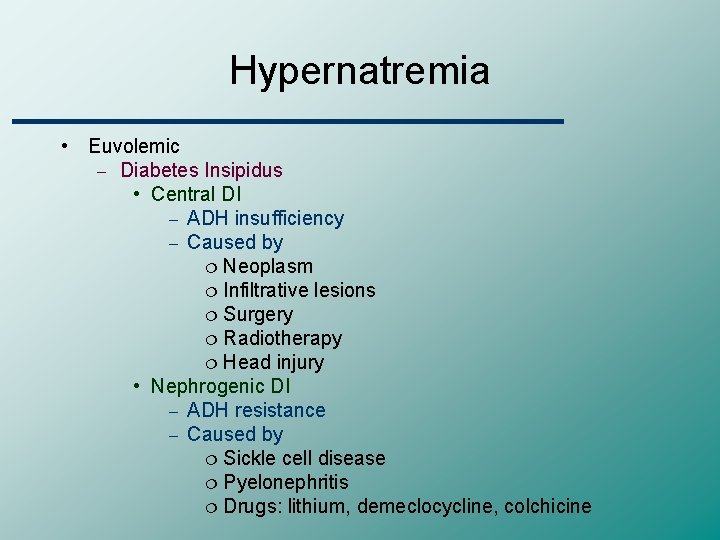
Hypernatremia • Euvolemic – Diabetes Insipidus • Central DI – ADH insufficiency – Caused by ¦ Neoplasm ¦ Infiltrative lesions ¦ Surgery ¦ Radiotherapy ¦ Head injury • Nephrogenic DI – ADH resistance – Caused by ¦ Sickle cell disease ¦ Pyelonephritis ¦ Drugs: lithium, demeclocycline, colchicine
Hypernatremia • Diabetes Insipidus – Diagnosis • Compare plasma and urine osmolarity after dehydration (water deprivation test) and after vasopressin – Treatment • Central DI – Hormone replacement with vasopressin • Nephrogenic DI – HCTZ or amiloride enhances the reabsorption of fluid from the proximal tubule

Hyperkalemia • INCREASED POTASSIUM RELEASE FROM CELLS • Pseudohyperkalemia – Mechanical trauma during venipuncture – Cooling of the sample and specimen deterioration because of increased length of storage – May also represent severe intravascular hemolysis rather than a hemolyzed specimen – Marked leukocytosis or thrombocytosis (white cell or platelet count greater than 100, 000 per mm 3 or 400, 000 mm 3, respectively), as may occur with leukemia or a myeloproliferative disease
Hyperkalemia • INCREASED POTASSIUM RELEASE FROM CELLS • Metabolic acidosis • Insulin deficiency • Increased tissue catabolism – Any cause of increase tissue breakdown result in the release of potassium into the extracellular fluid – hyperkalemia may occur in this setting, particularly if renal failure is also present – Clinical examples include trauma
Hyperkalemia • INCREASED POTASSIUM RELEASE FROM CELLS • Beta-adrenergic blockade • Exercise • Hyperkalemic periodic paralysis • Digitialis • Succinylcholine
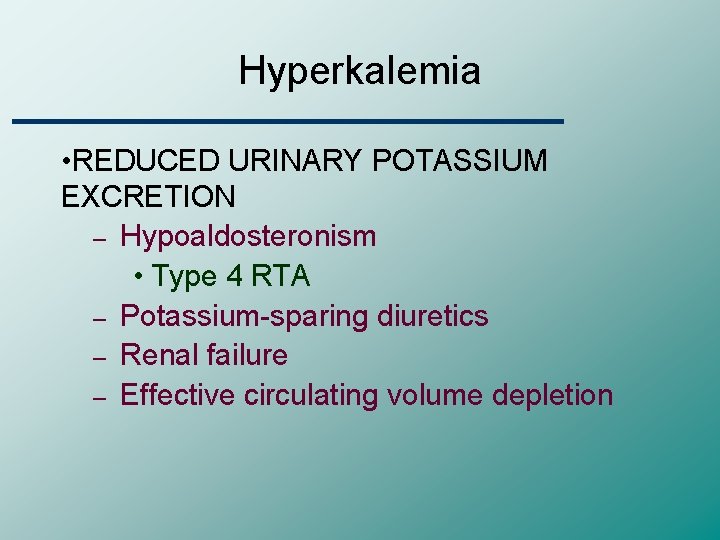
Hyperkalemia • REDUCED URINARY POTASSIUM EXCRETION – Hypoaldosteronism • Type 4 RTA – Potassium-sparing diuretics – Renal failure – Effective circulating volume depletion
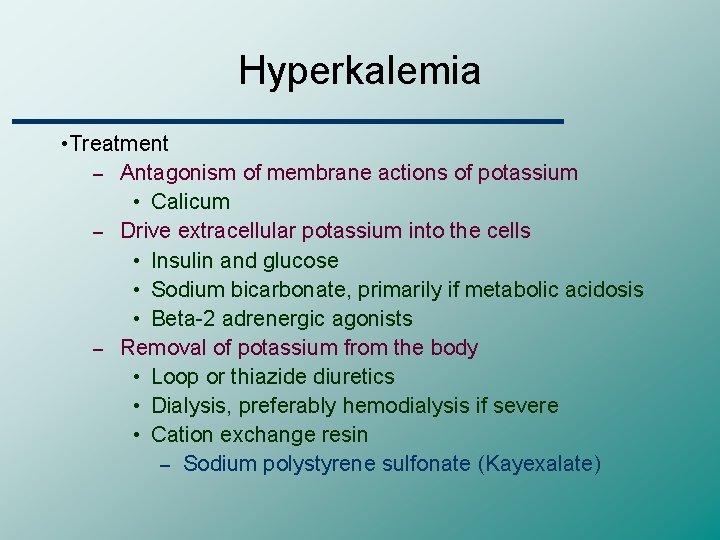
Hyperkalemia • Treatment – Antagonism of membrane actions of potassium • Calicum – Drive extracellular potassium into the cells • Insulin and glucose • Sodium bicarbonate, primarily if metabolic acidosis • Beta-2 adrenergic agonists – Removal of potassium from the body • Loop or thiazide diuretics • Dialysis, preferably hemodialysis if severe • Cation exchange resin – Sodium polystyrene sulfonate (Kayexalate)
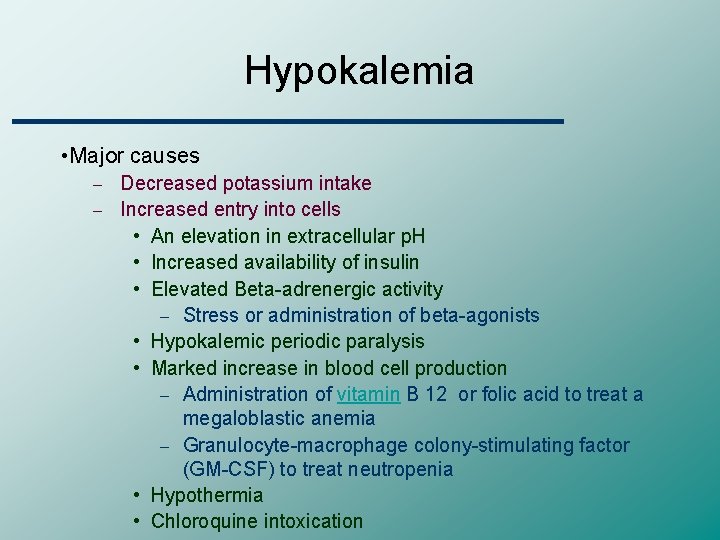
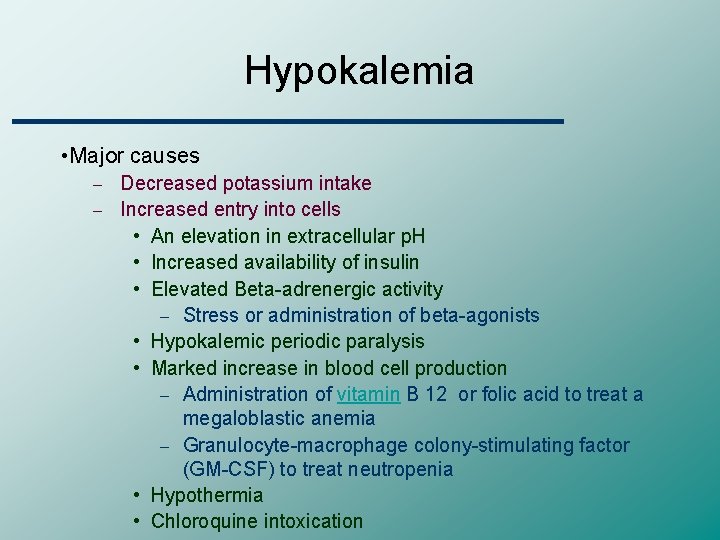
Hypokalemia • Major causes Decreased potassium intake – Increased entry into cells • An elevation in extracellular p. H • Increased availability of insulin • Elevated Beta-adrenergic activity – Stress or administration of beta-agonists • Hypokalemic periodic paralysis • Marked increase in blood cell production – Administration of vitamin B 12 or folic acid to treat a megaloblastic anemia – Granulocyte-macrophage colony-stimulating factor (GM-CSF) to treat neutropenia • Hypothermia • Chloroquine intoxication –
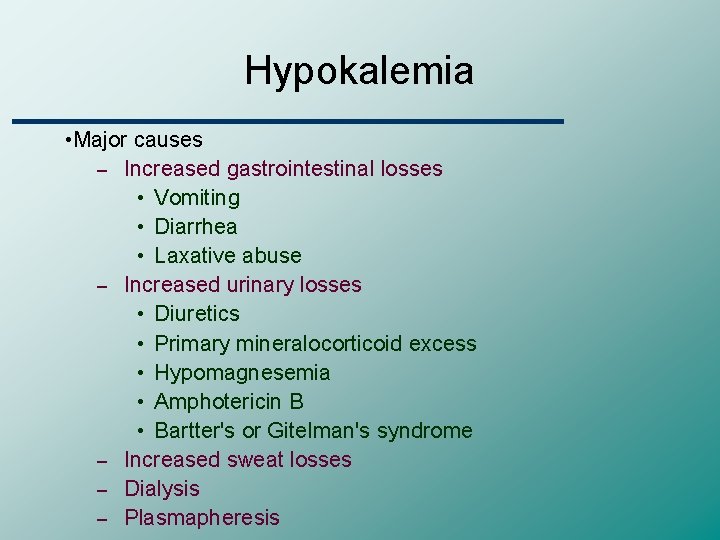
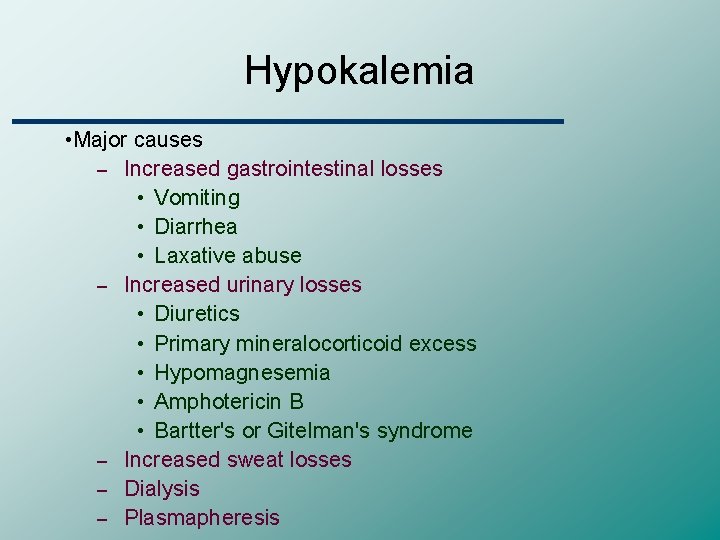
Hypokalemia • Major causes – Increased gastrointestinal losses • Vomiting • Diarrhea • Laxative abuse – Increased urinary losses • Diuretics • Primary mineralocorticoid excess • Hypomagnesemia • Amphotericin B • Bartter's or Gitelman's syndrome – Increased sweat losses – Dialysis – Plasmapheresis
Hypokalemia • Treatment – 10 meq KCl will raise serum K+ by 0. 1 • Be careful in renal failure
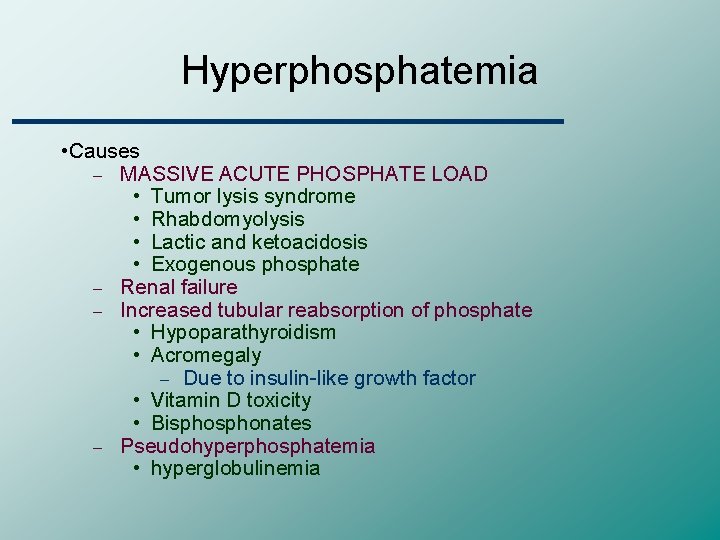
Hyperphosphatemia • Causes – MASSIVE ACUTE PHOSPHATE LOAD • Tumor lysis syndrome • Rhabdomyolysis • Lactic and ketoacidosis • Exogenous phosphate – Renal failure – Increased tubular reabsorption of phosphate • Hypoparathyroidism • Acromegaly – Due to insulin-like growth factor • Vitamin D toxicity • Bisphonates – Pseudohyperphosphatemia • hyperglobulinemia
Hypophosphatemia • Major causes – Internal redistribution • Increased insulin secretion • Refeeding syndrome • Hungry bone syndrome – Decreased intestinal absorption • Inadequate intake • Antacids containing aluminum or magnesium • Steatorrhea and chronic diarrhea • Vitamin D deficiency or resistance – Increased urinary excretion • Hyperparathyroidism • Vitamin D deficiency or resistance
Hypophosphatemia • Signs and symptoms – Mineral metabolism • Release of bone calcium contributes to the hypercalciuria • More prolonged hypophosphatemia leads to rickets and osteomalacia due to decreased bone mineralization – CNS • Metabolic encephalopathy • Confusion, seizures, delirium, and coma – CVS • Myocardial contractility may be impaired with ATP depletion • The reduction in cardiac output may become clinically significant, leading to congestive heart failure, when the plasma phosphate concentration falls to 1. 0 mg/d. L
Hypophosphatemia • Signs and symptoms – Skeletal and smooth muscle • Proximal myopathy, dysphagia and ileus – Hematologic dysfunction • Hypophosphatemia can also affect each of the components of the hematopoietic system • Treatment – Oral (Neutra-Phos) – IV (K-Phos)
Hypermagnesemia • Causes – Renal failure – Magnesium infusion • Severe preeclampsia or eclampsia – Oral ingestion – Magnesium enemas • Substantial quantities of magnesium can be absorbed from the large bowel • Among patients with renal failure, the administration of a magnesium enema can be fatal
Hypermagnesemia • Treatment – Most cases of symptomatic hypermagnesemia can be prevented by anticipation – Dialysis – When the toxic effects of magnesium must be reversed more quickly in a patient with severe symptoms, intravenous calcium can be given as a magnesium antagonist
Hypomagnesemia • Causes – GI losses – Renal losses • Both loop and thiazide diuretic can inhibit net magnesium reabsorption • Alcohol – Appears to reflect alcohol-induced tubular dysfunction that is reversible within four weeks of abstinence • Hypercalcemia – Calcium and magnesium seem to compete for transport in the thick ascending limb of the loop of Henle • Nephrotoxins – Aminoglycoside – Amphotericin B – Pentamidine – Cyclosporine • Loop of Henle or distal tubule dysfunction – Bartter’s syndrome
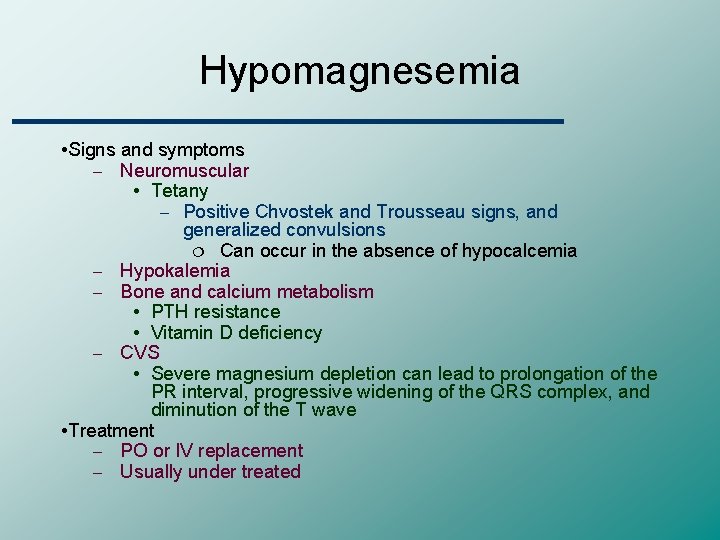
Hypomagnesemia • Signs and symptoms – Neuromuscular • Tetany – Positive Chvostek and Trousseau signs, and generalized convulsions ¦ Can occur in the absence of hypocalcemia – Hypokalemia – Bone and calcium metabolism • PTH resistance • Vitamin D deficiency – CVS • Severe magnesium depletion can lead to prolongation of the PR interval, progressive widening of the QRS complex, and diminution of the T wave • Treatment – PO or IV replacement – Usually under treated
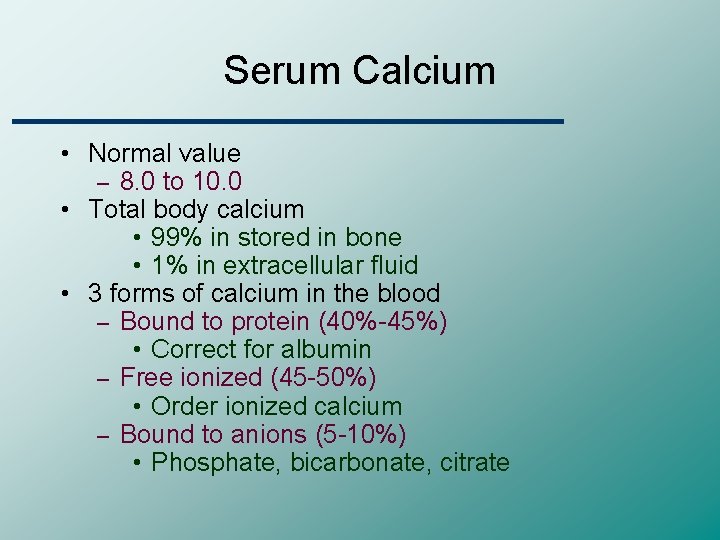
Serum Calcium • Normal value – 8. 0 to 10. 0 • Total body calcium • 99% in stored in bone • 1% in extracellular fluid • 3 forms of calcium in the blood – Bound to protein (40%-45%) • Correct for albumin – Free ionized (45 -50%) • Order ionized calcium – Bound to anions (5 -10%) • Phosphate, bicarbonate, citrate
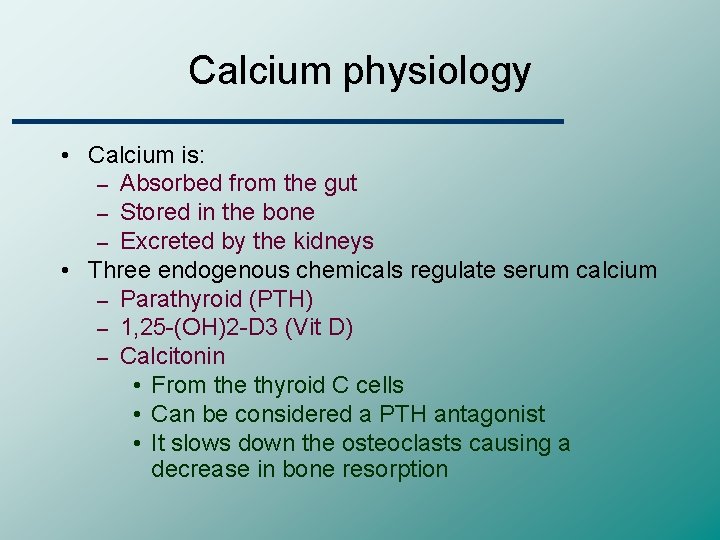
Calcium physiology • Calcium is: – Absorbed from the gut – Stored in the bone – Excreted by the kidneys • Three endogenous chemicals regulate serum calcium – Parathyroid (PTH) – 1, 25 -(OH)2 -D 3 (Vit D) – Calcitonin • From the thyroid C cells • Can be considered a PTH antagonist • It slows down the osteoclasts causing a decrease in bone resorption
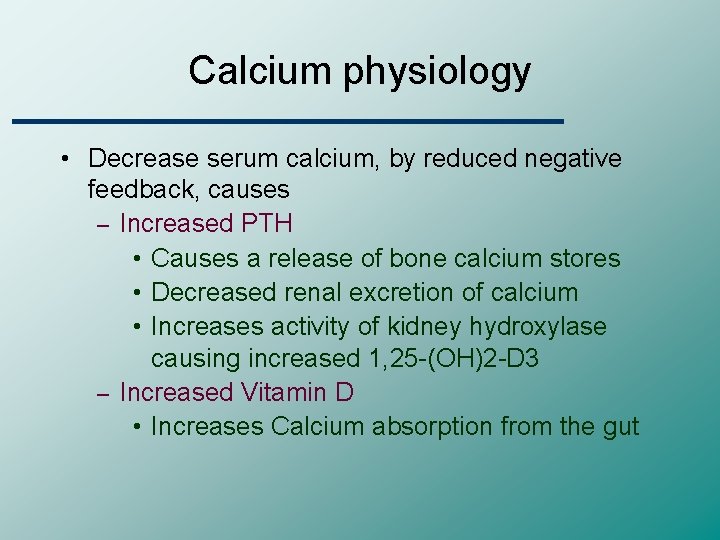
Calcium physiology • Decrease serum calcium, by reduced negative feedback, causes – Increased PTH • Causes a release of bone calcium stores • Decreased renal excretion of calcium • Increases activity of kidney hydroxylase causing increased 1, 25 -(OH)2 -D 3 – Increased Vitamin D • Increases Calcium absorption from the gut
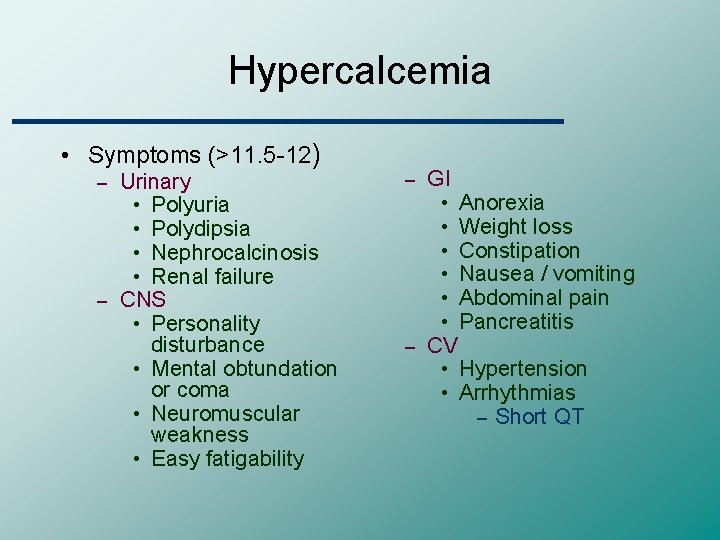
Hypercalcemia • Symptoms (>11. 5 -12) Urinary • Polyuria • Polydipsia • Nephrocalcinosis • Renal failure – CNS • Personality disturbance • Mental obtundation or coma • Neuromuscular weakness • Easy fatigability – GI • Anorexia • Weight loss • Constipation • Nausea / vomiting • Abdominal pain • Pancreatitis – CV • Hypertension • Arrhythmias – Short QT –
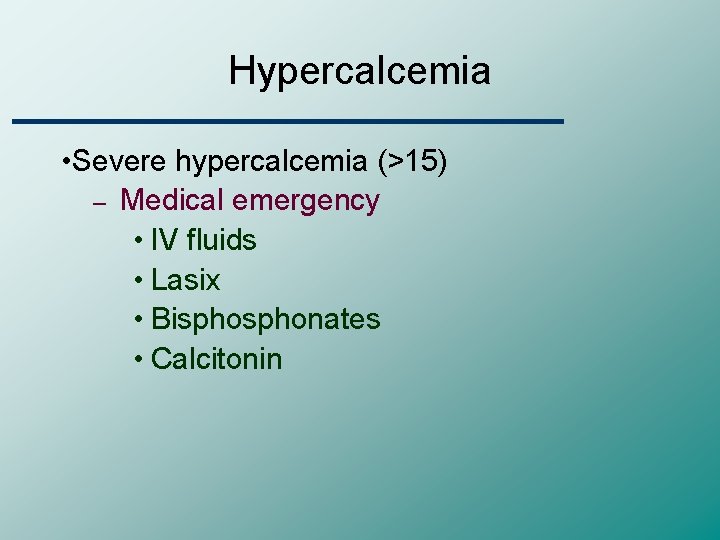
Hypercalcemia • Severe hypercalcemia (>15) – Medical emergency • IV fluids • Lasix • Bisphonates • Calcitonin
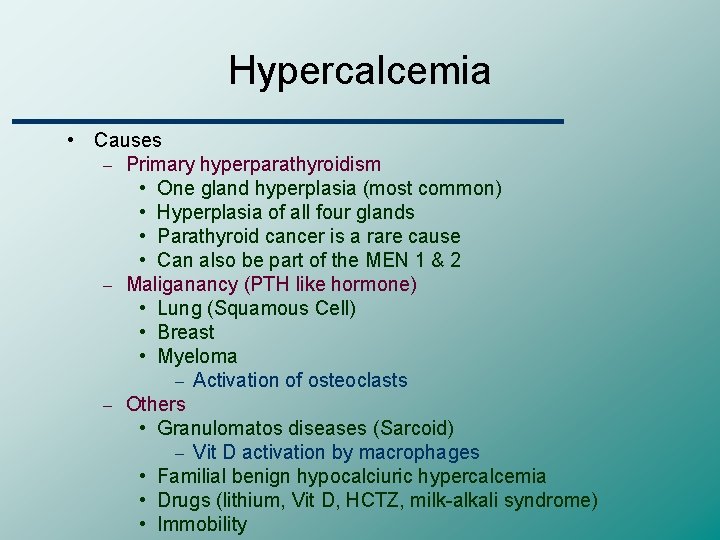
Hypercalcemia • Causes – Primary hyperparathyroidism • One gland hyperplasia (most common) • Hyperplasia of all four glands • Parathyroid cancer is a rare cause • Can also be part of the MEN 1 & 2 – Maliganancy (PTH like hormone) • Lung (Squamous Cell) • Breast • Myeloma – Activation of osteoclasts – Others • Granulomatos diseases (Sarcoid) – Vit D activation by macrophages • Familial benign hypocalciuric hypercalcemia • Drugs (lithium, Vit D, HCTZ, milk-alkali syndrome) • Immobility
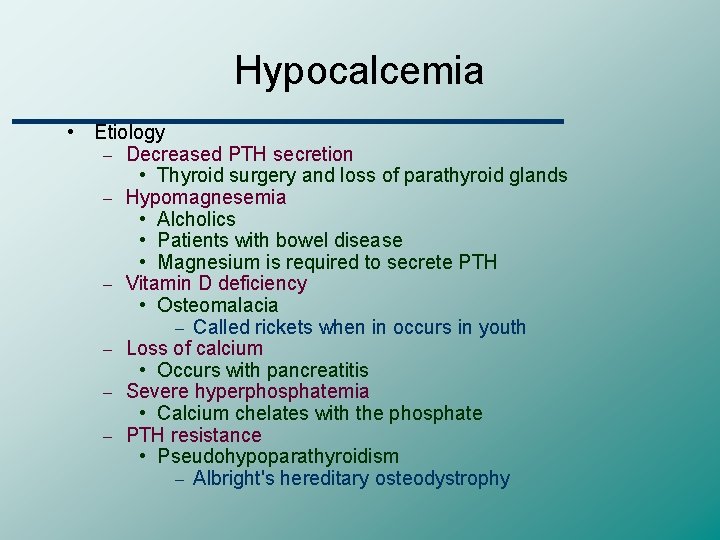
Hypocalcemia • Etiology – Decreased PTH secretion • Thyroid surgery and loss of parathyroid glands – Hypomagnesemia • Alcholics • Patients with bowel disease • Magnesium is required to secrete PTH – Vitamin D deficiency • Osteomalacia – Called rickets when in occurs in youth – Loss of calcium • Occurs with pancreatitis – Severe hyperphosphatemia • Calcium chelates with the phosphate – PTH resistance • Pseudohypoparathyroidism – Albright's hereditary osteodystrophy
Hypocalcemia • Clinical findings – Neuromuscular • Tetany – Chvostek sign (percussion of CN VII) – Trousseau sign • Laryngospasm • Cramping • Seizures – CV • QT prolongation • Refractory CHF • hypotension
Hypocalcemia • Diagnosis – Suggested when the serum calcium is low • Check albumin • Check ionized calcium • PTH may be low or high depending on the etiology • Check serum magnesium • Management – In the acute stages IV calcium can be given – Maintenance therapy includes oral calcium
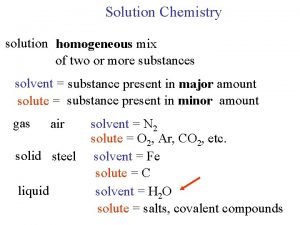
 Serum osmolarity formula
Serum osmolarity formula Serum osmolarity formula
Serum osmolarity formula Serum osmolarity formula
Serum osmolarity formula Serum osmolarity equation
Serum osmolarity equation Hypokalemia harrison
Hypokalemia harrison Chvostek sign trousseau sign
Chvostek sign trousseau sign Ba+2na
Ba+2na Correct na
Correct na Hypochloremia nursing interventions
Hypochloremia nursing interventions Serum osmolality formula
Serum osmolality formula Mehdi mojtabavi
Mehdi mojtabavi Na deficit formula
Na deficit formula Hdl level
Hdl level Management of hyponatremia
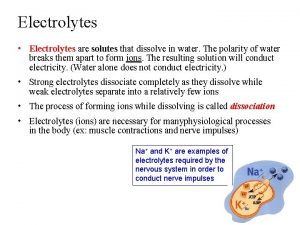
Management of hyponatremia Weak electrolytes examples
Weak electrolytes examples Lyophobic and lyophilic difference
Lyophobic and lyophilic difference Major intra and extracellular electrolytes
Major intra and extracellular electrolytes Is sucrose soluble in water
Is sucrose soluble in water Whats refeeding syndrome
Whats refeeding syndrome Weak electrolytes
Weak electrolytes Rome mnemonic for acid base balance
Rome mnemonic for acid base balance Electrolytes and nonelectrolytes
Electrolytes and nonelectrolytes Dka and electrolytes
Dka and electrolytes Pn
Pn Tropolar
Tropolar Chapter 18 fluids and electrolytes
Chapter 18 fluids and electrolytes Normal values of potassium
Normal values of potassium Herbalife hydrate
Herbalife hydrate Effect of electrolytes on chemical equilibria
Effect of electrolytes on chemical equilibria Strong vs weak electrolytes
Strong vs weak electrolytes Effect of electrolytes on colloidal dispersion
Effect of electrolytes on colloidal dispersion Electrolytes and nonelectrolytes
Electrolytes and nonelectrolytes Strong vs weak electrolytes
Strong vs weak electrolytes Vacid definition
Vacid definition Dr dawn lim
Dr dawn lim Difference between osmolarity and tonicity
Difference between osmolarity and tonicity Macula densa
Macula densa