INTRAVENOUS THERAPY Indications Scope of Practice Fluid Electrolytes







- Slides: 161
INTRAVENOUS THERAPY • Indications • Scope of Practice • Fluid & Electrolytes • ABG Imbalances • IV Calculations e #1
- EXPECTATIONS IV THERAPY COURSE • To be present for all classes(40 hours/ 5 days) • To complete ALL theory and practical hours • To complete ALL assignments and submit them on time • To take all quizzes and final exam, and final practicum
- EXPECTATIONS IV THERAPY COURSE • • Sign in for class Turn Cell phones OFF (shocking, I know) Leave Computers OFF NO eating during lecture, bottled water is k • Return from break on time
- EXPECTATIONS IV THERAPY COURSE • Minimum of 36 hours of instruction - Theory - 27 hours - Skills lab experience - 9 hours No exceptions, No make-up hours • Skills Lab – 3 successful IV starts (human subject) – 3 successful venipunctures (human subject)
- EXPECTATIONS IV THERAPY COURSE • Attendance • 2 Quizzes • Final Exam Must have a 80% average test scores AND Demonstrate proficiency in IV insertion and blood withdrawal techniques … to pass the course and be eligible for certification
OBJECTIVES • Define Intravenous Therapy and the need for IV therapy • Discuss legalities, guidelines for IV therapy • Discuss the scope of practice for IV therapy • Review importance of infection control • Discuss acid-base balance • Explain equipment used for IV therapy • Explain different types of IV solutions
INTRAVENOUS DEFINITION PURPOSE and TERMINOLOGY
WHAT IS INTRAVENOUS THERAPY? • Intravenous … – “Within a vein” – (needle or catheter) inserted into a vein • Therapy… – “treatment to cure”; heal; restore to previous state
WHAT IS THE PURPOSE OF IV THERAPY? • Used to sustain patients who are unable to take substances orally • Replaces water, electrolytes, and nutrients more rapidly than oral administration • Provides immediate access to the vascular system for the rapid delivery of specific solutions without the time required for GI tract absorption • Provides a vascular route for the administration of medication or blood components
INTRAVENOUS NURSING • “IV NURSING” as defined by Infusion Nurses Society (INS): “Use of the nursing process as it relates to technology and clinical application, fluids and electrolytes, pharmacology, infection control, pediatrics, transfusion therapy, oncology, parenteral nutrition, and quality assurance”
TERMINOLOGY in INTRAVENOUS THERAPY • Cannula/catheter – Small tube for insertion into a vessel • Heparin/Saline locks – Used to clear IV lines/catheters to keep open/flowing freely. • Peripheral line – Situated away from the center, as opposed to centrally located. • Central line – An infusion tube that is situated near the heart • PICC line – Peripherally inserted central catheter • TPN – Total parenteral nutrition; method of feeding that bypasses the GI tract
TERMINOLOGY in INTRAVENOUS THERAPY • PPN – Peripheral Parenteral Nutrition • IVP – IV Push or IVPB – IV Piggy Back • Isotonic – A solution that has the same salt concentration as the body • Hypertonic – A solution that has a higher salt concentration than the body • Hypotonic – A solution that has a lower salt concentration than the body
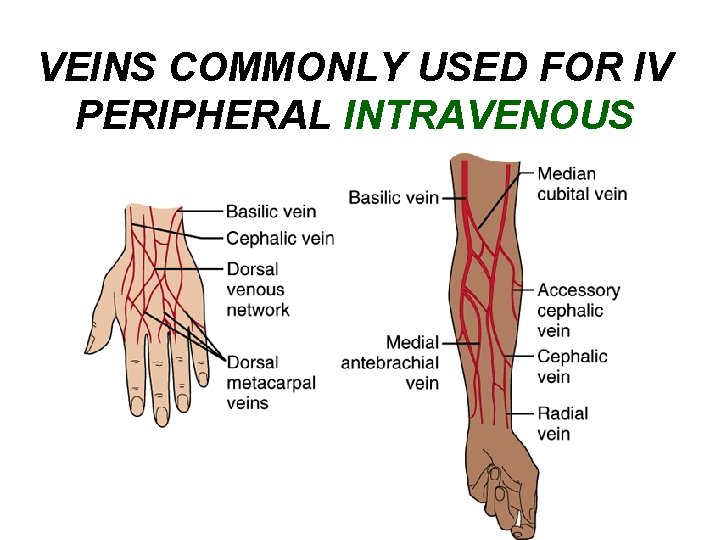
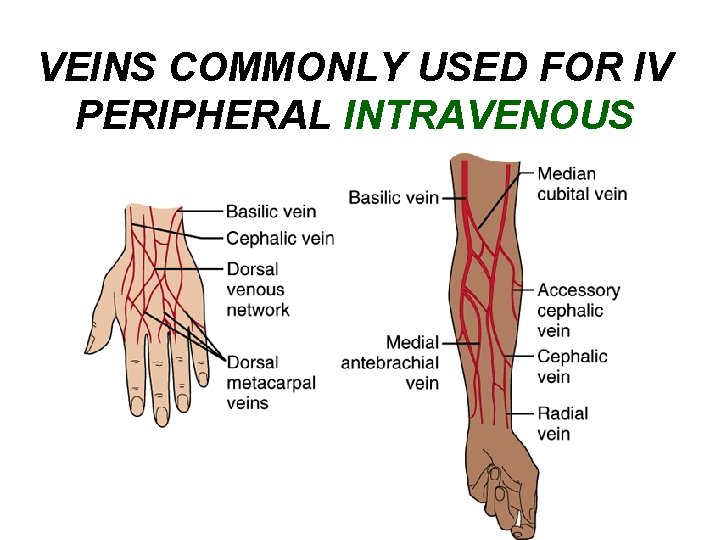
VEINS COMMONLY USED FOR IV PERIPHERAL INTRAVENOUS
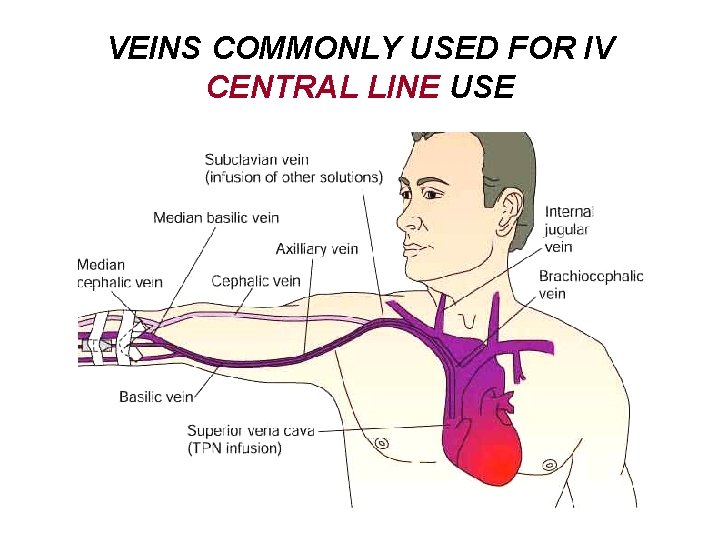
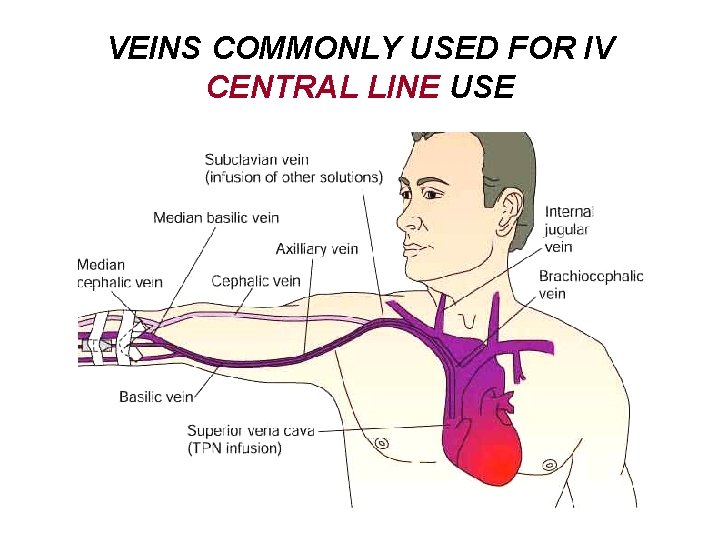
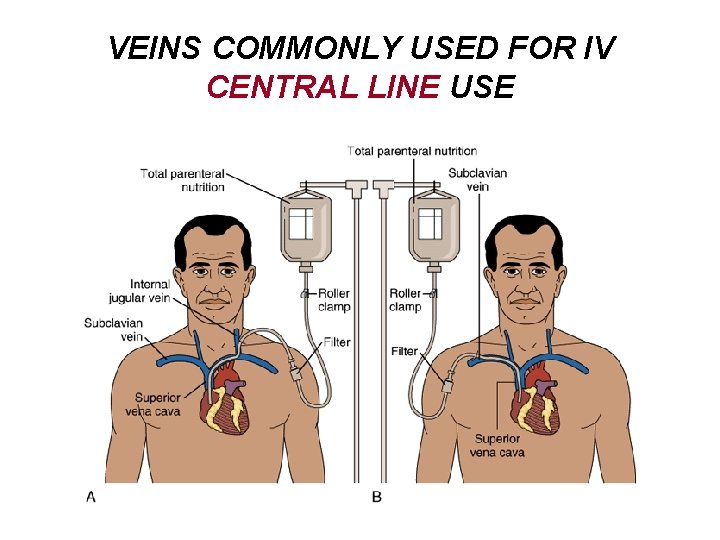
VEINS COMMONLY USED FOR IV CENTRAL LINE USE
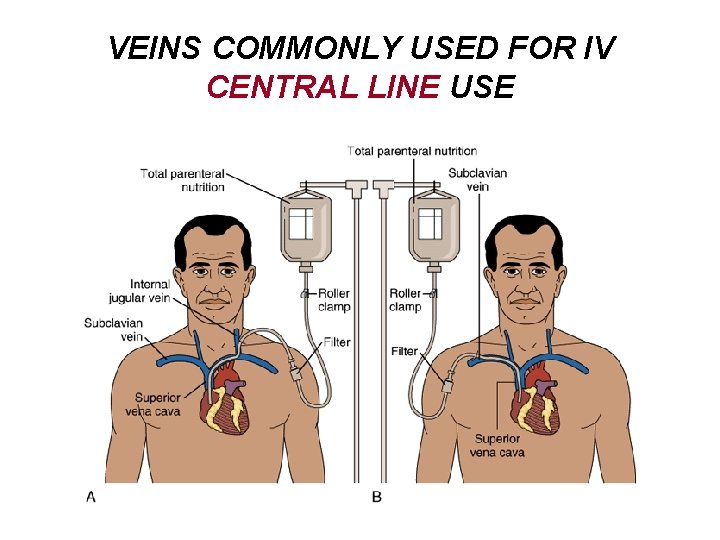
VEINS COMMONLY USED FOR IV CENTRAL LINE USE

LEGAL ASPECTS WHAT YOU NEED TO KNOW…
“THINK ABOUT THIS…” • Administering drugs and solutions to patients is one of the most legally significant tasks nurses perform – The number of lawsuits is increasing – High incidence of errors involving IV solution administration • Wrong solution used • Wrong route
LEGAL ACTION… • Many lawsuits center on – Errors in infusion pump use – Inappropriate placement of IV line – Failure to monitor
LEGAL ASPECTS State of California • California Business and Professional codes Chapter 6. 5, Article 2, Section 2859 – 2873. 6 – Vocational Nursing Practice Act 2860. 5 • California Code of Regulations Section – Health and safety codes
BUSINESS AND PROFESSIONAL CODE • “The practice of vocational nursing within the meaning of this chapter is the performance of services requiring those technical, manual skills acquired by means of a course in an accredited school of vocational nursing, or its equivalent, practiced under the direction of a licensed physician, or registered professional nurse, as defined in Section 2725 of the Business and Professional Code. ”
LEGAL TERMINOLOGY • Breach of Duty – examples of: – Delay in administration of medication – Unfamiliarity with drug – Inappropriate route of administration – Failure to qualify orders – Negligence in patient teaching
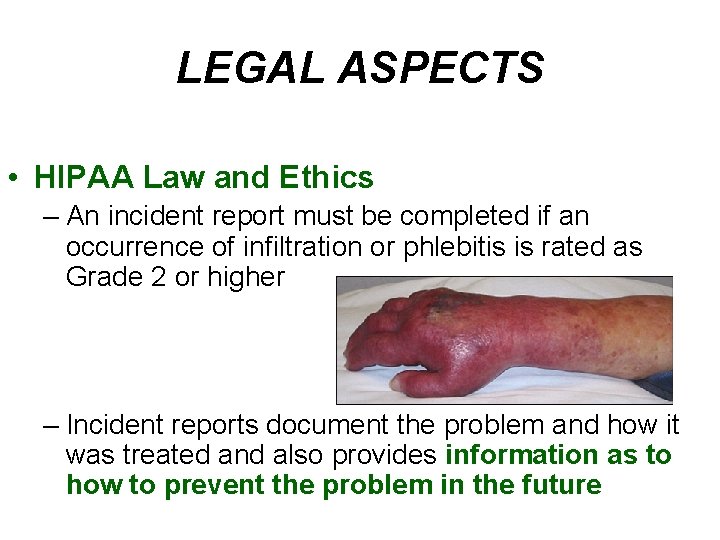
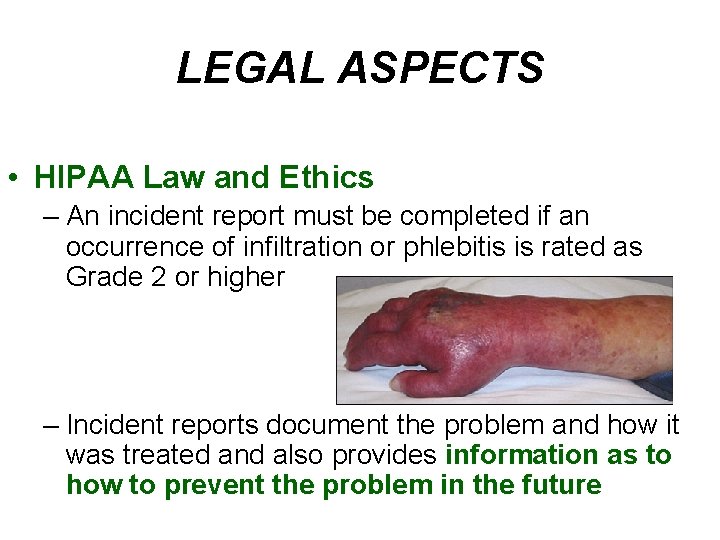
LEGAL ASPECTS • HIPAA Law and Ethics – An incident report must be completed if an occurrence of infiltration or phlebitis is rated as Grade 2 or higher – Incident reports document the problem and how it was treated and also provides information as to how to prevent the problem in the future
INCIDENT REPORTS • Incident reports for: – Med error – IV fluid error – Anaphylaxis or severe allergic reaction – Severe irritation or breakdown at site – Site infection – Phlebitis stage +2 or +3 – Needle stick to patient, family member, or health care personnel
INCIDENT REPORTS – Neurological deficit, S&S not present before IV – Patient withdraws consent for treatment or refuses treatment – Equipment failure or malfunction with impact on patient – Adverse or unexpected event – Break in policy
LEGAL ASPECTS • Facilities and Agencies will have specific policies guided by laws and organizations such as: – JCAHO – Joint Commission on Accreditation of Healthcare Organizations – HIPAA – Health Insurance Portability and Accountability Act – CDC – Centers for Disease Control and Prevention
LEGAL ASPECTSFacilities and Agency – NIOSH – National Institute of Occupational Safety and Health – OSHA – Occupational Safety and Health Administration

JOINT COMMISSION on ACCREDITATION of HEALTHCARE ORGANIZATIONS JCAHO • Organization responsible for the accreditation of healthcare facilities • Also established the National Patient Safety Standards
NATIONAL PATIENT SAFETY STANDARDS - GOALS • Before any IV procedure is performed on a patient, the patient should be identified by 2 identifiers • IV therapy orders/lab results should be read back to verify their accuracy • Use only accepted abbreviations
NATIONAL PATIENT SAFETY STANDARDS - GOALS • Report test results regarding IV therapy to Healthcare professional as soon as possible • Check concentrations of medications carefully • Check all medications at least three times to ensure correct medication used
NATIONAL PATIENT SAFETY STANDARDS - GOALS • Wash hands before and after every procedure • Ensure meds are recorded completely and accurately • Ensure that the patient supplies list of all current medications
CENTER FOR DISEASE CONTROL CDC • Agency of the Federal government – Works to prevent infectious and chronic diseases, injuries, workplace hazards, disabilities and environmental health threats – Collects information about infections that occur because of IV therapy; the information is used to track the source of infections and help prevent them
OCCUPATIONAL SAFETY and HEALTH ADMINISTRATION - OSHA • A division of the Department of Labor – Responsible for protecting the safety of employees in the workplace – They enforce standards; provide training and education – They encourage continual improvement in the workplace – They established universal and standard precautions to help prevent infections or injuries to health care workers
OSHA REGULATIONS • Washing hands • These are prohibited in work areas (includes ambulance) – Eating, drinking, smoking, applying cosmetics or lip balm, handling contact lenses • Never bend, break or recap needles • Avoid causing splashes and splatters of blood or body fluids • Properly handle contaminated items
LICENSED VOCATIONAL NURSE GUIDELINES
LEGAL GUIDELINES for the LVN • As a nurse you have a legal and ethical responsibility to your patient • By becoming aware of professional standards and related laws you can provide the best care and protect your self legally • The laws of the State and Nurse Practice Act should be your guide
VOCATIONAL NURSING PRACTICE ACT – IV Therapy • An LVN when directed by a licensed physician may start and superimpose Category II fluids (pheresis, hemodialysis and blood bank procedures) under the following circumstances – All conditions have been met – The LVN has received specialized instruction from an RN or MD – The physician’s order is specific to the patient – The order designates Category II – Intravenous (IV) to be used – An RN or MD is in the immediate area
VOCATIONAL NURSING PRACTICE ACT – IV Therapy • Guidelines for the Vocational Nurse as under the Vocational Nurse Practice Act: • Article 8, 2547 – Category I – fluids include blood, blood products, vitamins, nutrients and electrolytes – Category II – fluids used in hemodialysis, pheresis (removing blood from and individual and separating certain elements such as platelets and RBC’s) , or blood bank procedures in certain settings
VOCATIONAL NURSING PRACTICE ACT – IV Therapy • Includes – Administer medications by hypodermic injection – Withdraw blood from a patient, as ordered by a physician; having successfully completed an approved course by the Board – Start and superimpose intravenous fluids; having satisfactorily completed an approved course by the board – The procedure is performed in an approved setting
DEFINITIONS • Superimpose – Connect a container of IV fluid to tubing thru which another container of IV fluid has been administered • Primary infusion line – Line which provides a direct infusion between the container and the peripheral vein • Secondary infusion line – Line which provides infusion thru a lateral access into a primary line
LEGAL SCOPE for ARTERIAL LINE BLOOD WITHDRAWAL • The LVN can perform arterial blood withdrawal via arterial lines with instruction in proper procedure • Demonstrated requisite knowledge and skills • Performs under physician’s order • Is certified by the BVNPT in blood withdrawal
LEGAL SCOPE for CENTRAL LINES • LVN’s can not manipulate in any way central infusion lines. This includes CVP lines. • LVN’s can not access peripherally inserted central catheters (PICC lines) or midline catheters. • LVN’s can change the site dressing on central, PICC or midline catheters
LEGAL SCOPE for HEPARIN/SALINE LOCKS • LVN’s who hold an IV therapy certificate issued by the BVN/PT can instill a minute amount of heparin or normal saline into heparin locks for the sole purpose of patency • Know facility policy regarding the amount of ml’s for each solution that can be instilled
LEGAL ASPECTS for HYPERALIMENTATION • Hyperalimentation and lipids are considered nutrients. • An LVN who holds an intravenous therapy certificate issued by the BVN/PT can start and superimpose such fluid solutions in peripheral veins provided these solutions do not contain medications
LEGAL ASPECTS for LOCAL ANESTHETIC • LVN’s can administer an injection of local anesthetic via subcutaneous or intradermal routes prior insertion of an IV needle or catheter provided the LVN – Receives instruction – Demonstrates the requisite knowledge, skills and ability – Performs the procedure in accordance with a physicians order
BEST DEFENSE • Documentation – Be Accurate – Date, time of insertion – Specific vein choice and where – Gauge and length of device – Brand style of device – Solution that is infusing – Whether solution infusing by gravity or pump – How patient tolerated – Your signature

INFECTION CONTROL
INFECTIOUS DISEASE PREVENTION • Identify tasks and other activities that may involve exposure to blood or other potentially infectious materials
INFECTIOUS DISEASE FROM IV CATHETERS • Think about this… – Thousands of patients with an intravascular catheter in place die of catheter related blood stream infection (BSI) – Peripheral venous catheters are most frequently used – Infections include • Local site infection • Septic thrombophlebitis • Endocarditis • Metastatic infections
INFECTIOUS DISEASE FROM IV CATHETERS • Besides the toll in human lives, catheterrelated infections place a staggering burden on the health care system. • Care for one affected patient costs from $34, 000 to $56, 000, with annual totals in the united States from $296 million to $2. 3 billion
OSHA REQUIREMENTS • The new safety regulation affects all hospitals, physician offices, and other organizations that deliver patient care and whose healthcare workers are at risk for occupational exposure to human blood and body fluids. • The use of safety devices have been shown to be effective at reducing needle stick injuries in the clinical setting.
INFECTION CONTROL • Methods that will reduce or prevent exposure to infection – Engineering controls – Work practices – Personal protective equipment • Gloves, gowns • Face shields/masks • Lab coats • Eye protection
ENGINEERING PRACTICES • Controls That Help Prevent Contact With Blood & Body Fluids; Include: – Isolation supplies – Hand washing facilities – Waterless hand cleaners – Sharps containers – Ventilation – Medical waste containers – Self sheathing needles or needleless systems
WORK PRACTICES USING STANDARD PRECAUTIONS • Standard precautions refers to the practice in medicine of avoiding contact with patients' bodily fluids using these precautions • Hand washing • Respiratory protection (N 95 or (9508) HEPA, 99%) • Patient care equipment • Environmental control • Linen
INFECTIOUS DISEASE PREVENTION • Specific measures to take to minimize risk of contamination from IV therapy: – Monitor v/s closely – Associate elevated temp with contaminated IV fluid – Remove all IV apparatus – Do a microbiological sample – Restart IV with entirely new equipment and solutions
IF EXPOSURE HAS OCCURED • Medical follow-up and treatment – Must be reported and kept on record – Should be provided as soon after the exposure as possible (within 1 -2 hours) – Should be with the guidelines of the US Department of Health and Human Services, and Public Health service
FACT It is your responsibility to know the laws that regulate your actions. Also, consider your knowledge and experience before performing a procedure.
FLUIDS AND ELECTROLYTES In an adult weighing 155 lbs (70 kg), about 60% of the total body weight is fluid In an infant, fluids account for about 80% of total body weight
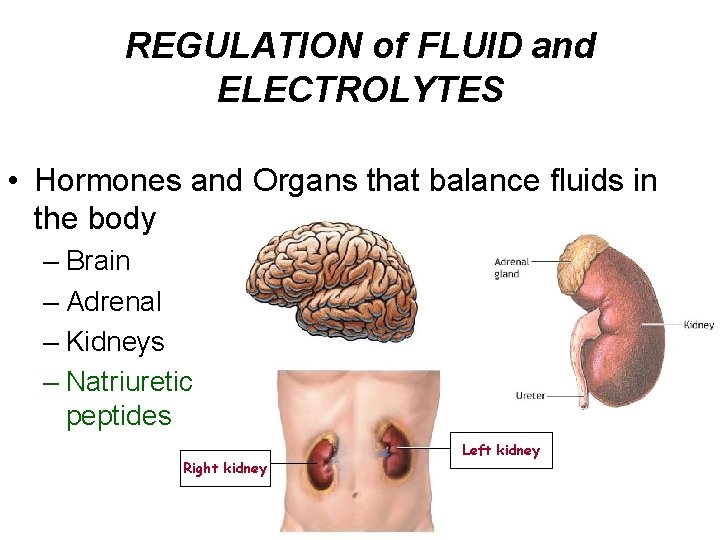
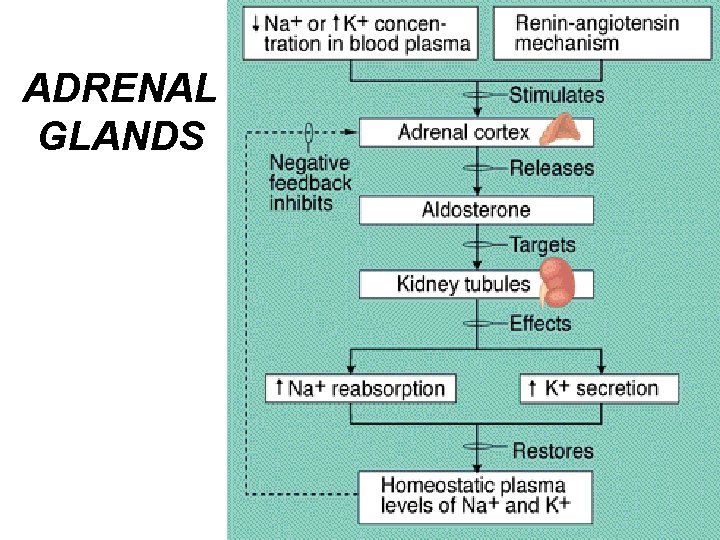
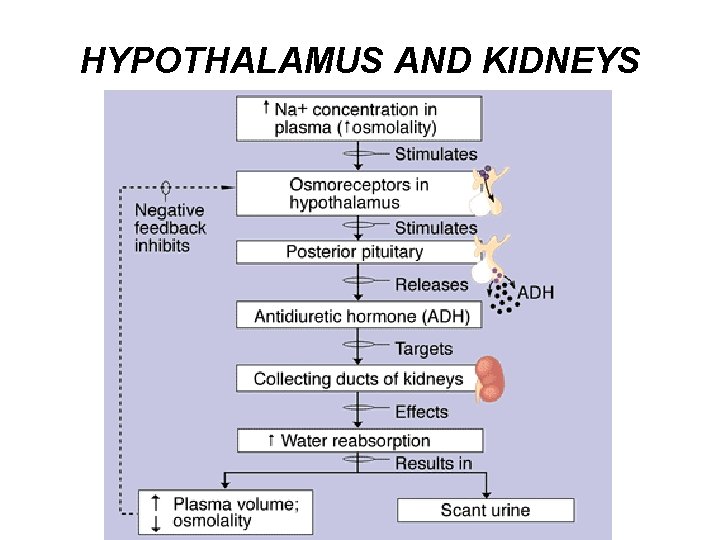
REGULATION of FLUID and ELECTROLYTES • Hormones and Organs that balance fluids in the body – Brain – Adrenal – Kidneys – Natriuretic peptides Right kidney Left kidney
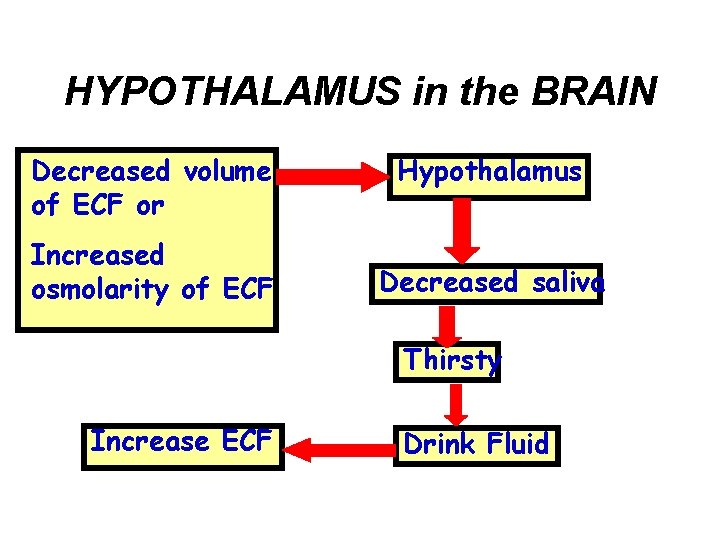
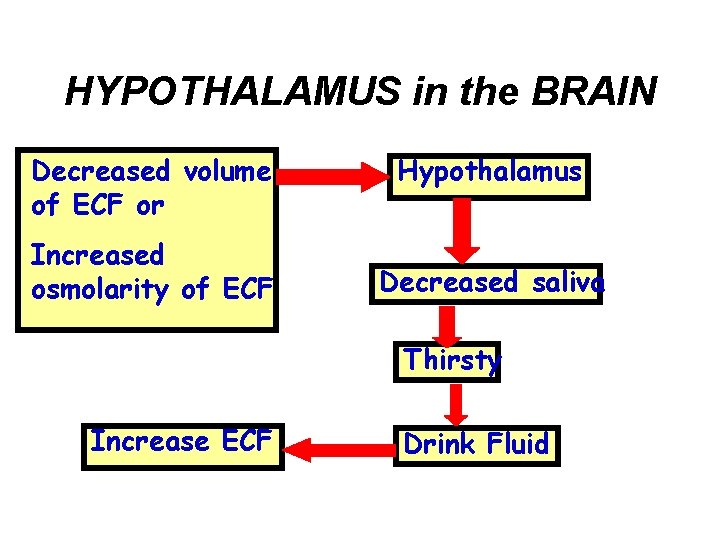
HYPOTHALAMUS in the BRAIN Decreased volume of ECF or Increased osmolarity of ECF Hypothalamus Decreased saliva Thirsty Increase ECF Drink Fluid
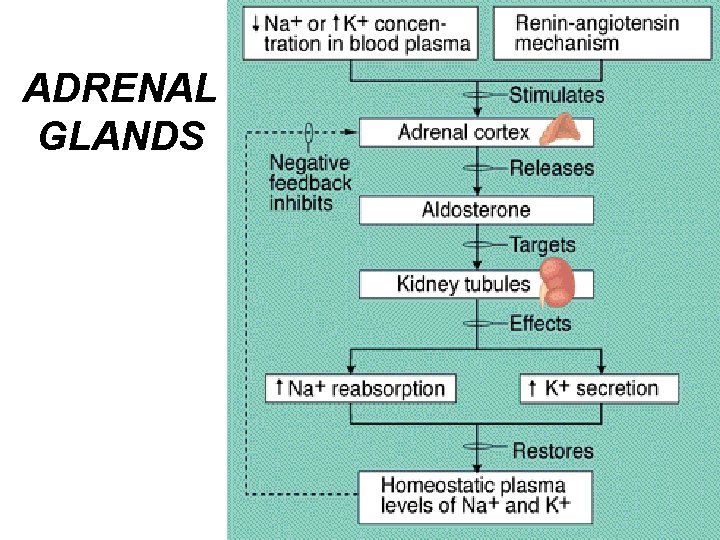
ADRENAL GLANDS
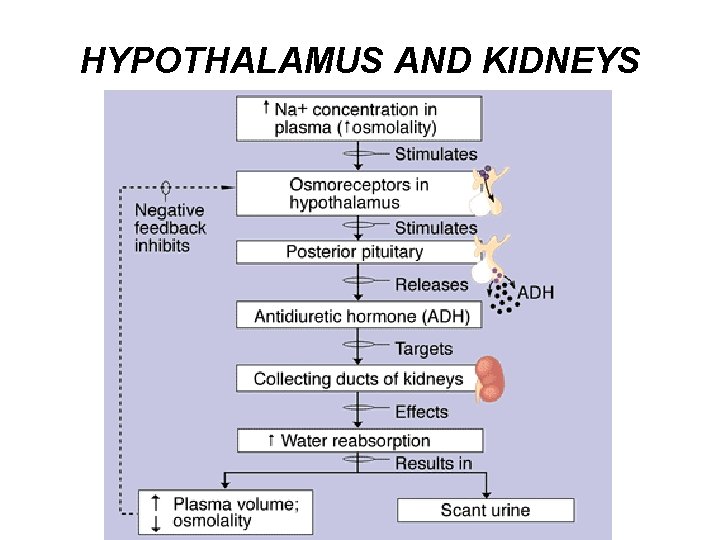
HYPOTHALAMUS AND KIDNEYS
NATRIURETIC PEPTIDES • Hormone like substances that act opposite to the kidneys role in balance of fluids – Atrial natriuretic peptide – Brain natriuretic peptide – C-type natriutetic peptide • Are released in response to overstretching of the atrial and ventricular walls – Reduces blood volume by inhibiting the release of the hormones: renin, aldosterone and ADH
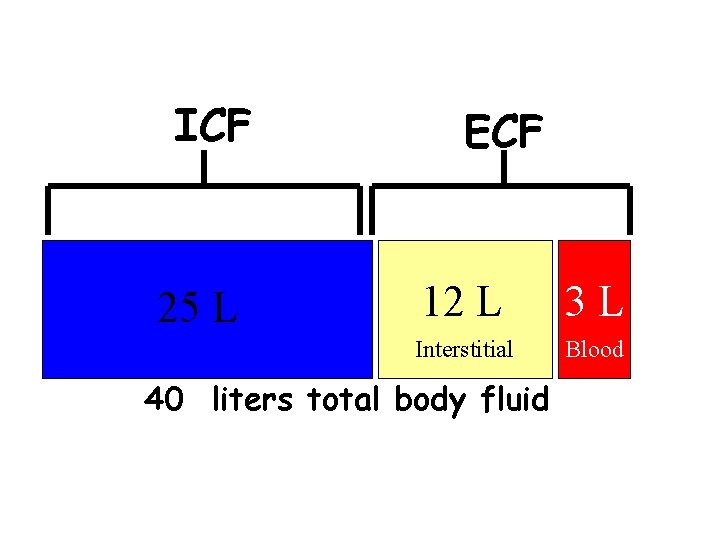
BODY FLUIDS • Body fluids are composed of water and solutes • Body fluids exist in two major compartments – Extracellular – ECF; outside the cells; in 2 forms • Interstitial (ISF) • Intravascular (Plasma) – Intracellular – ICF; inside the cells

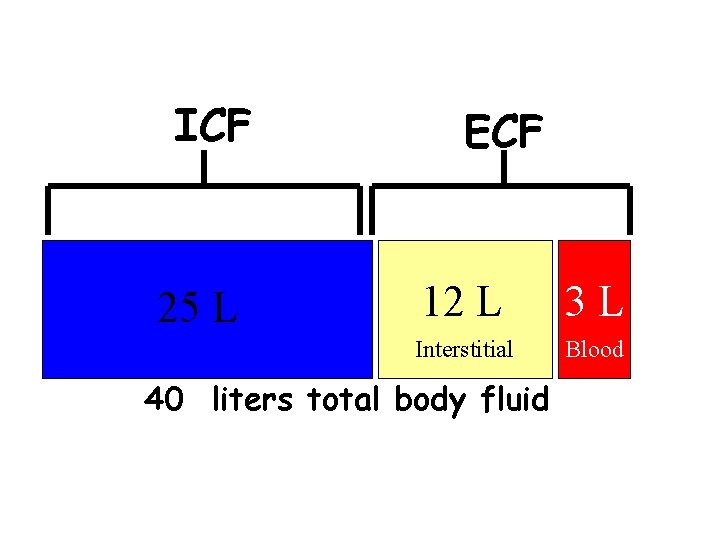
ICF 25 L ECF 12 L 3 L Interstitial Blood 40 liters total body fluid
BODY FLUIDS • INTAKE = OUTPUT • Regulation of balance of body fluids is by hormones – From Renal, Cardiovascular and Endocrine • Purpose of body fluids: – Help regulate body temperatures – Transport nutrients around the body – Transports wastes to excretion sites – Preserve cell shape

WATER • Water is important to our bodies; it makes up 60% of our bodies. What it does: – Acts as a solvent – Transportation – Heat Regulation – Chemical Reactions
ELECTROLYTES • Major component of body fluids is electrolytes • Electrolytes are associated with electricity • These substances are chemical compounds that when split in solution change into electrically charged particles called ions • There are 2 categories: – Cations – are positive – Anions – are negative
ELECTROLYTES • These are the MAJOR electrolytes – Intracellular (ICF): • Phosphorus – P • Potassium – K+ • Magnesium – Mg++ – Extracellular: • Sodium - Na+ • Chloride – Cl • Calcium – Ca++ – Bicarbonate – ICF, ECF
ELECTROLYTES • Functions - Helps regulate water and acid-base balance - Contributes to enzyme reactions - Essential to neuromuscular activity • Electrolyte imbalances occur when – There is a deficit or excess of electrolytes – Or translocation of electrolytes to another fluid compartment
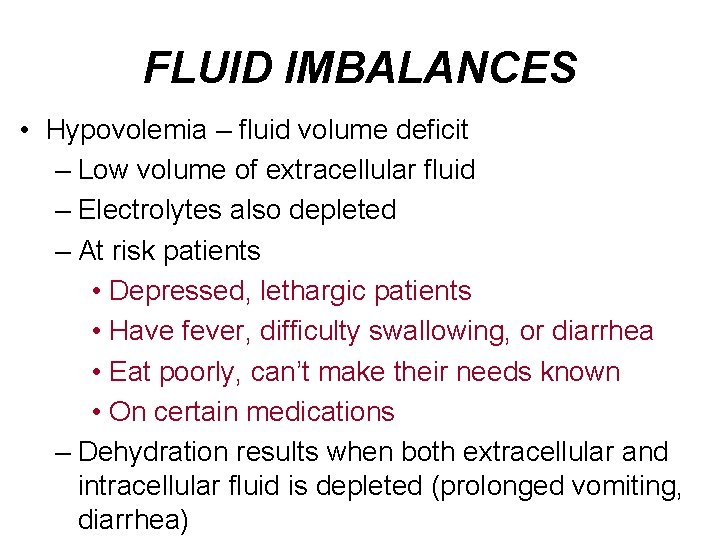
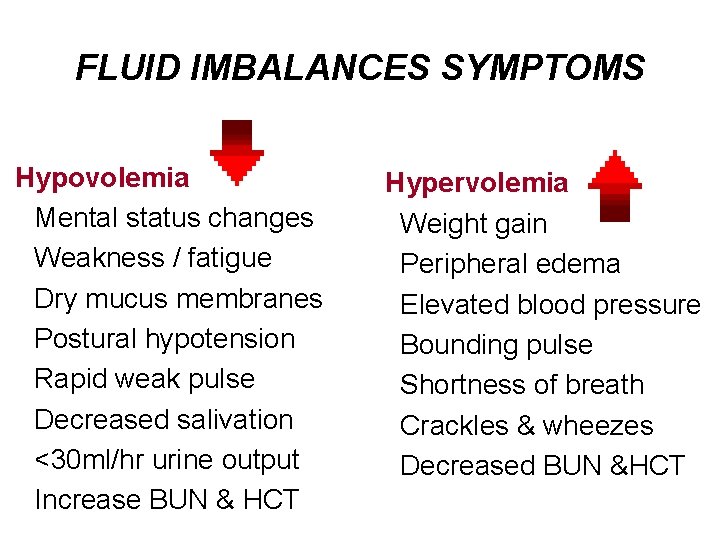
FLUID IMBALANCES • Hypovolemia – fluid volume deficit – Low volume of extracellular fluid – Electrolytes also depleted – At risk patients • Depressed, lethargic patients • Have fever, difficulty swallowing, or diarrhea • Eat poorly, can’t make their needs known • On certain medications – Dehydration results when both extracellular and intracellular fluid is depleted (prolonged vomiting, diarrhea)
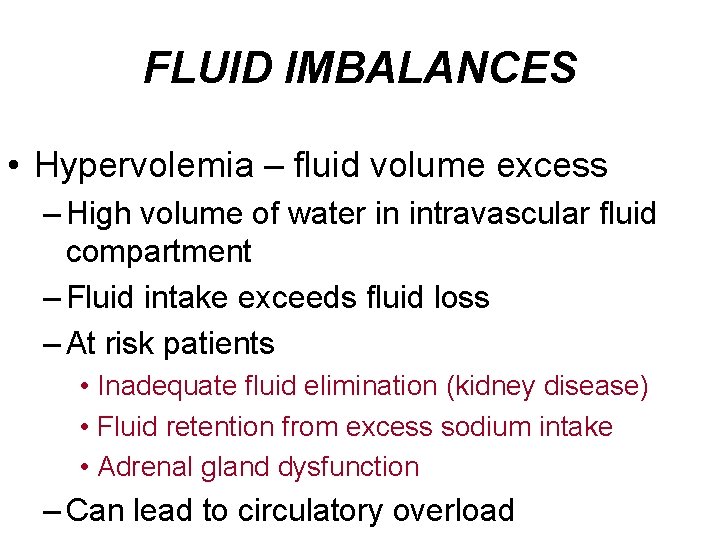
FLUID IMBALANCES • Hypervolemia – fluid volume excess – High volume of water in intravascular fluid compartment – Fluid intake exceeds fluid loss – At risk patients • Inadequate fluid elimination (kidney disease) • Fluid retention from excess sodium intake • Adrenal gland dysfunction – Can lead to circulatory overload
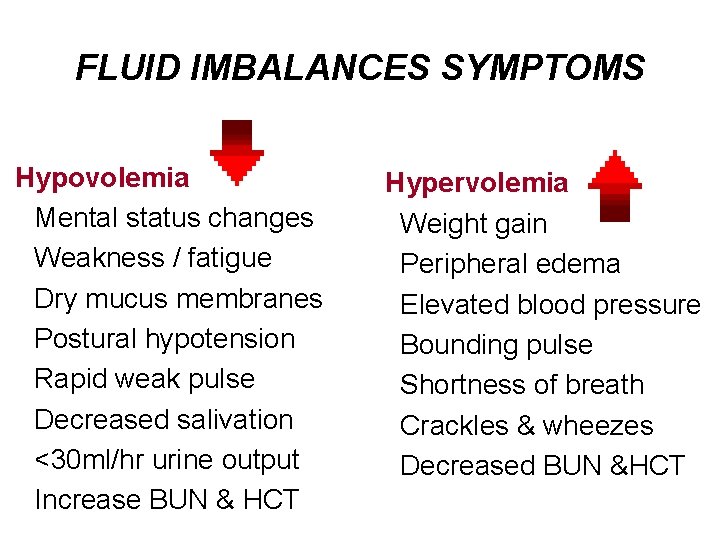
FLUID IMBALANCES SYMPTOMS Hypovolemia Mental status changes Weakness / fatigue Dry mucus membranes Postural hypotension Rapid weak pulse Decreased salivation <30 ml/hr urine output Increase BUN & HCT Hypervolemia Weight gain Peripheral edema Elevated blood pressure Bounding pulse Shortness of breath Crackles & wheezes Decreased BUN &HCT
MOVEMENT OF FLUIDS and ELECTROLYTES • Solutes and Body fluids continually move among the major fluid compartments; methods: • Solutes move by: – Diffusion (passive transport) – Active transport • Fluids move by: – Osmosis – Filtration
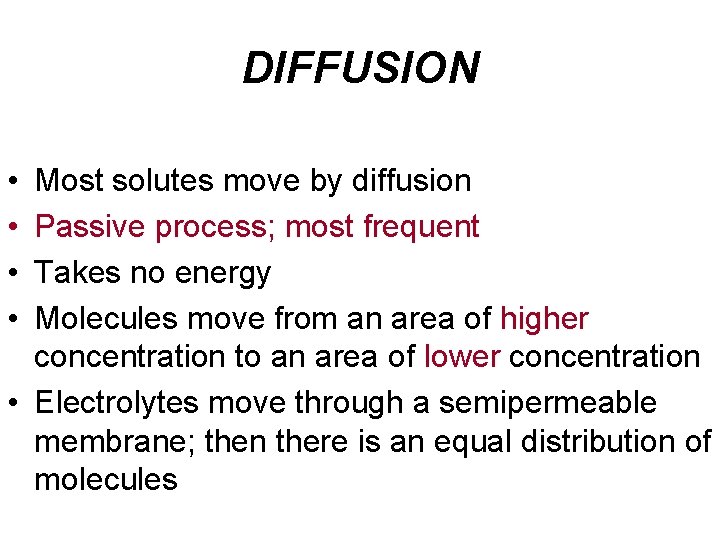
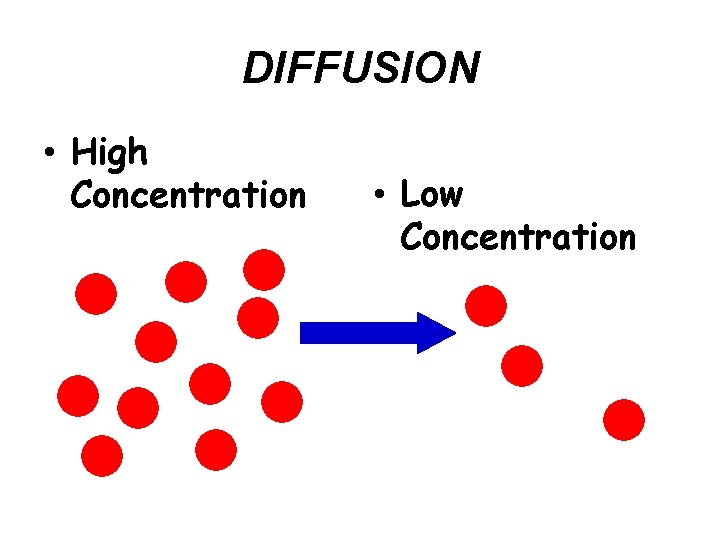
DIFFUSION • • Most solutes move by diffusion Passive process; most frequent Takes no energy Molecules move from an area of higher concentration to an area of lower concentration • Electrolytes move through a semipermeable membrane; then there is an equal distribution of molecules
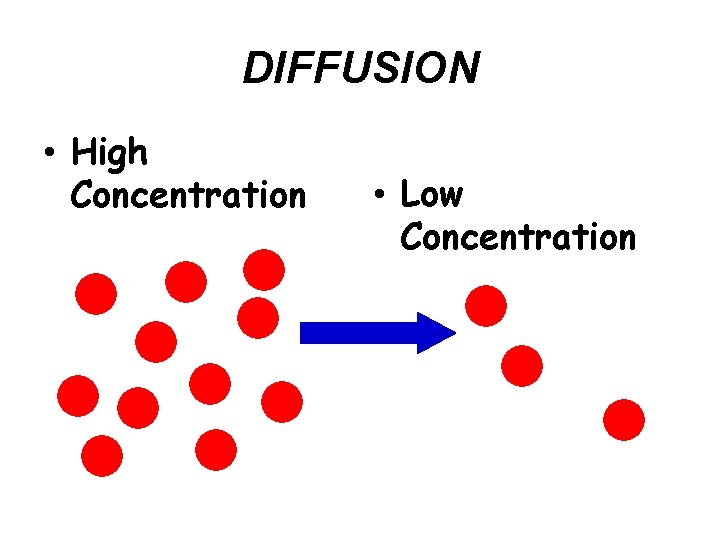
DIFFUSION • High Concentration • Low Concentration
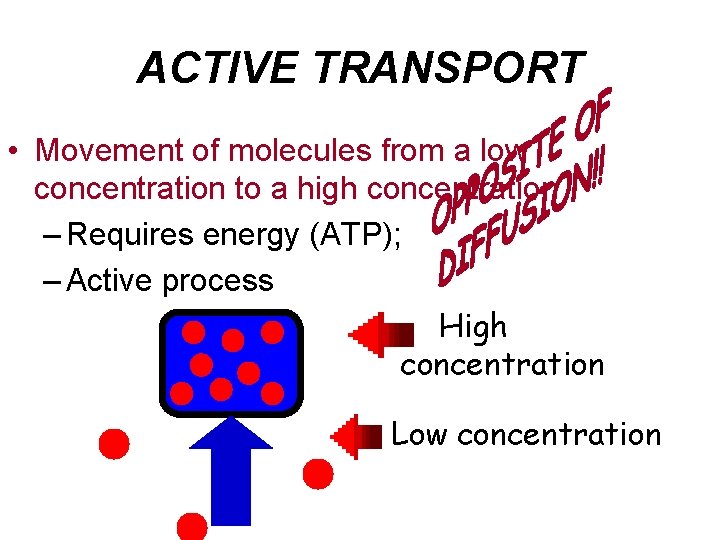
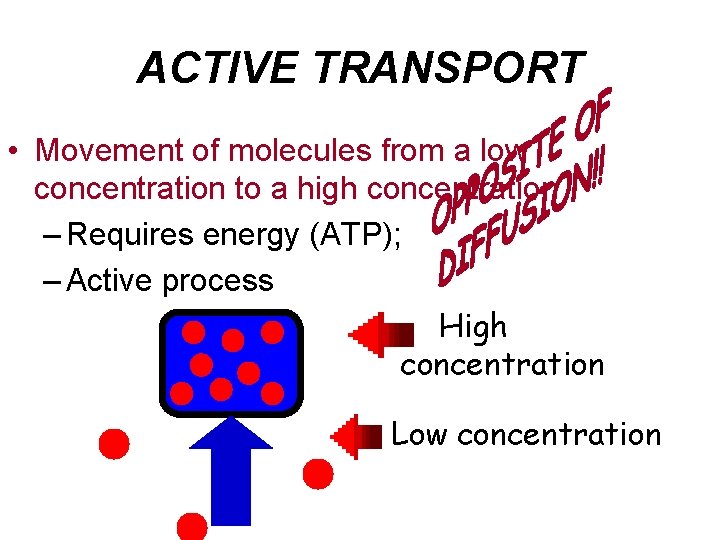
ACTIVE TRANSPORT • Movement of molecules from a low concentration to a high concentration – Requires energy (ATP); – Active process High concentration Low concentration
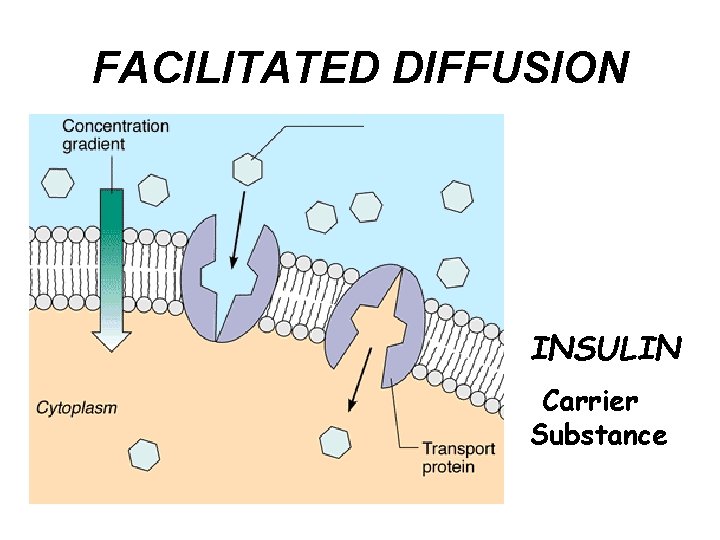
FACILITATED DIFFUSION • When certain dissolved substances require assistance from a carrier molecule to pass through a semi-permeable membrane • Example: – Insulin (carrier substance) helps distribution of glucose molecules inside cells
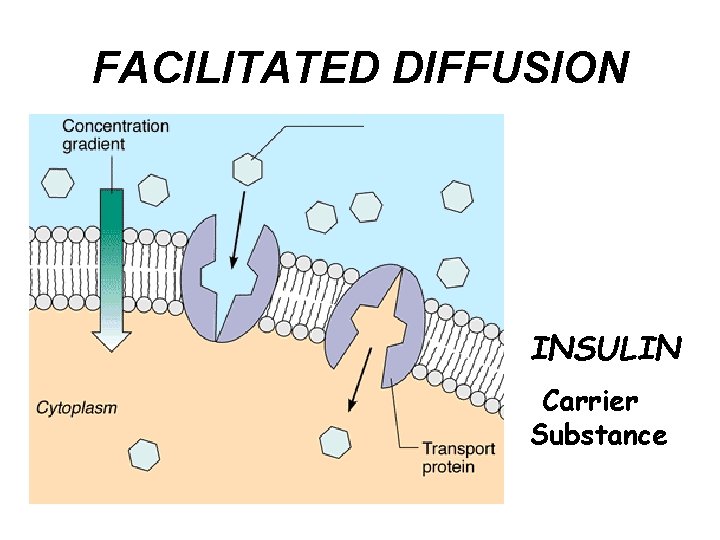
FACILITATED DIFFUSION INSULIN Carrier Substance
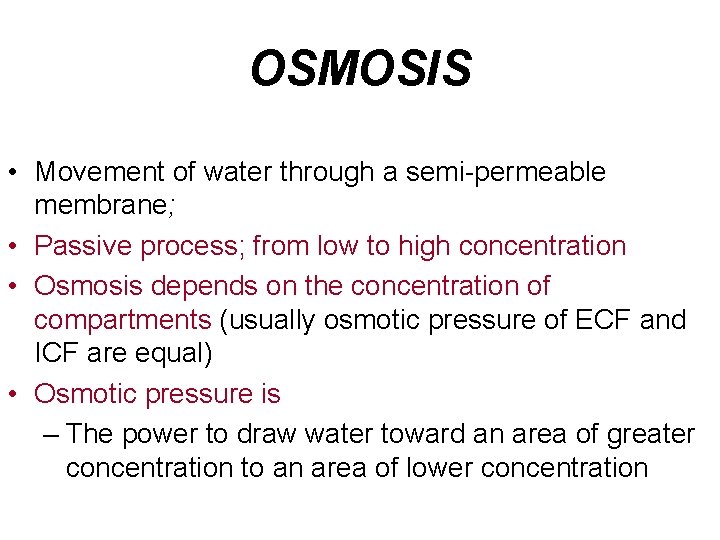
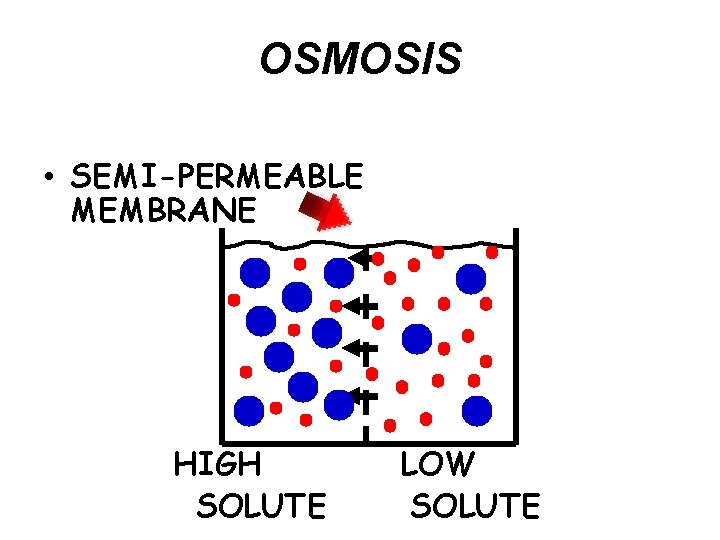
OSMOSIS • Movement of water through a semi-permeable membrane; • Passive process; from low to high concentration • Osmosis depends on the concentration of compartments (usually osmotic pressure of ECF and ICF are equal) • Osmotic pressure is – The power to draw water toward an area of greater concentration to an area of lower concentration
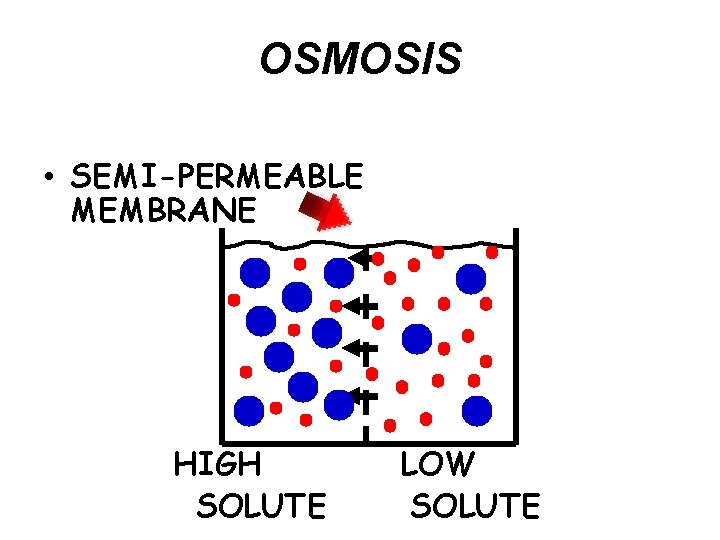
OSMOSIS • SEMI-PERMEABLE MEMBRANE HIGH SOLUTE LOW SOLUTE
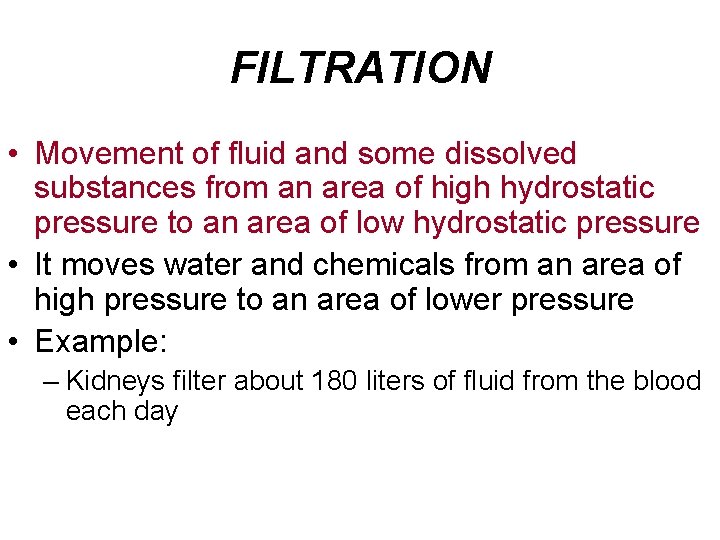
FILTRATION • Movement of fluid and some dissolved substances from an area of high hydrostatic pressure to an area of low hydrostatic pressure • It moves water and chemicals from an area of high pressure to an area of lower pressure • Example: – Kidneys filter about 180 liters of fluid from the blood each day
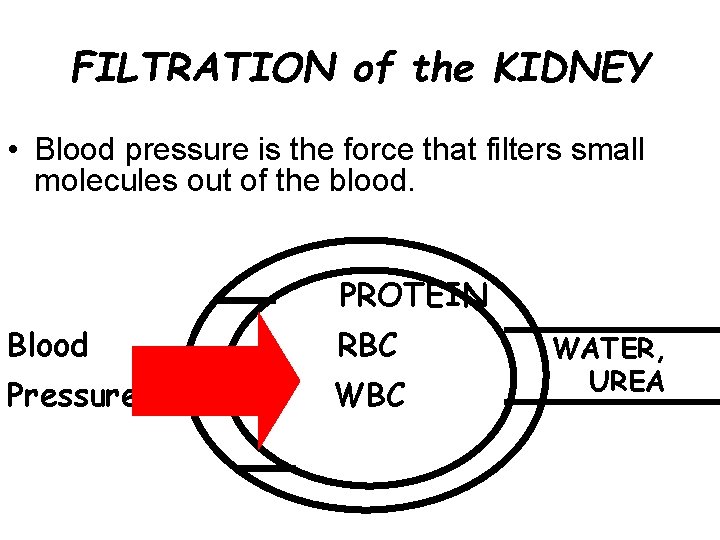
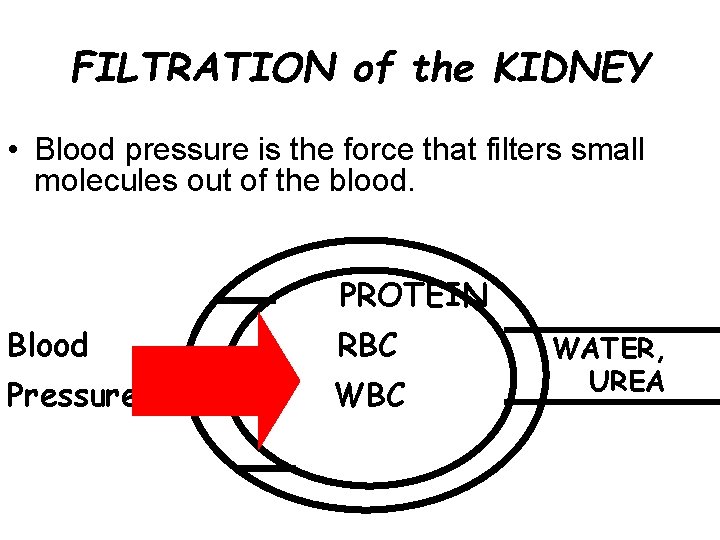
FILTRATION of the KIDNEY • Blood pressure is the force that filters small molecules out of the blood. PROTEIN Blood RBC Pressure WBC WATER, UREA
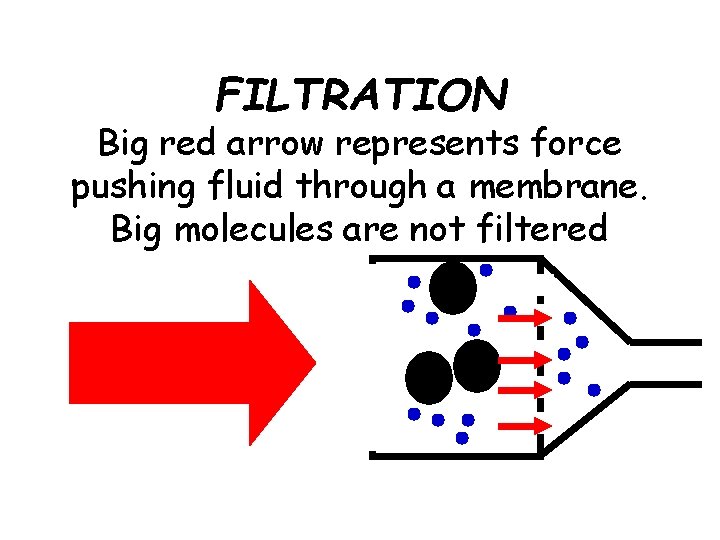
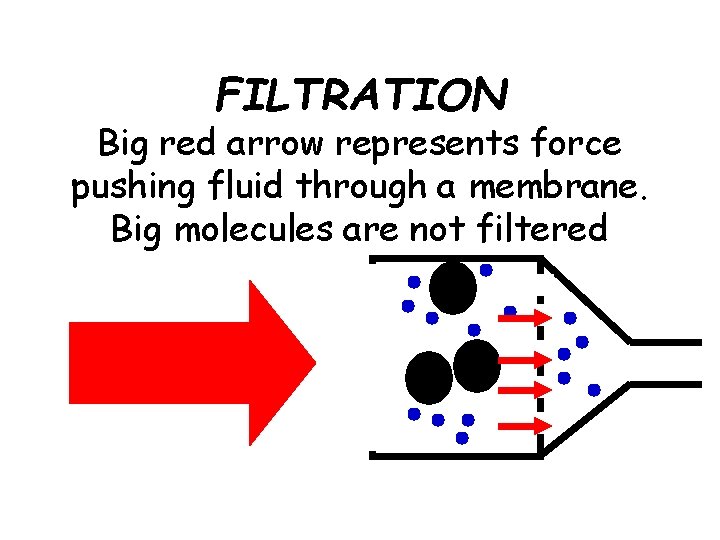
FILTRATION Big red arrow represents force pushing fluid through a membrane. Big molecules are not filtered
“THINK ABOUT THIS…” • Electrolytes attract fluids by osmosis • Loss of fluids results in a loss of electrolytes • IV Therapy is often needed to restore fluid balance, electrolyte balance or both
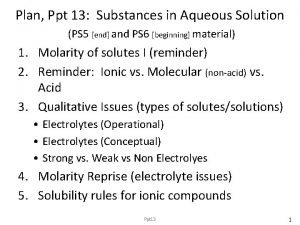
ACID/BASE BALANCE Major organs for regulating acid-base balance are the lungs, kidneys
ACID-BASE BALANCE • Body fluid contains – Water – Electrolytes – Acids are continually produced during metabolism; chief acid is carbonic acid – Bases neutralize acids; example is bicarbonate • Acid and base content influence the p. H of the body fluid • Body fluids are maintained within a narrow range that is slightly alkaline
ACID-BASE BALANCE • Buffers in the digestive tract, respiratory system and renal system work constantly to maintain a narrow p. H. – Neutralize excess acids or bases – Body’s first defense against acid-base changes – Major buffer systems in extracellular fluid are bicarbonate and carbonic acid
ACID–BASE BALANCE • The symbol p. H refers to the amount of hydrogen ions in a solution; normal p. H -7. 35 -7. 45 • If Bicarbonate is depleted while neutralizing a strong acid, ph drops – p. H Below 7. 35 – Called Acidosis • If strong base is added to extracellular fluid and depletes Carbonic acid, the p. H rises – p. H Above 7. 45 – Called Alkalosis
ASSESSING ACID-BASE BALANCE • Acid-Base balance is evaluated by measuring arterial blood gases (ABG’s) • What is measured? – p. H – measures hydrogen ion concentration p. H range 7. 35 -7. 45 – Pa. CO 2 – measures dissolved CO 2 in body – Pa. O 2 – measures amount of O 2 dissolved in body – HCO 3 (bicarbonate) – reflects the kidney regulation
RESPIRATORY SYSTEM REGULATION • Lungs help regulate acid-base balance • How? – By eliminating retained carbon dioxide which is a potential acid – In response the body will alter the rate and depth of respirations
RENAL SYSTEM REGULATION • The kidneys provide the long-term regulation of acid-base balance. • How? – They selectively retain or conserve bicarbonate and hydrogen ions • Response is slower and more permanent and selective than the other systems
ACID-BASE IMBALANCES • Two types of disturbances can alter the proper ratio of the body’s components – Metabolic disturbances affect the bicarbonate element (HCO 3) – Respiratory disturbances affect the H 2 CO 3 element (carbonic acid) • Acidosis and Alkalosis are the 2 kinds of p. H acid-base imbalance; 4 subtypes
FACT An imbalance in acids or bases is life threatening. DEATH OCCURS QUICKLY IF ph below 6. 8 or above 8. 0
ACID-BASE IMBALANCES • Respiratory Acidosis – ph HCO 3 normal initially then rises 7. 35; Pa. CO 2 45 mm; – Carbon dioxide is retained – Allows carbonic acid to build up in the blood • Cause? By slow breathing; depression of the resp center • Symptoms? – Respirations shallow, ineffective – Headache – Nausea, vomiting • Treatment? – Improve respirations; give O 2
ACID-BASE IMBALANCES • Respiratory Alkalosis – p. H-7. 45; Pa CO 2 35; HCO 3 normal – Opposite of acidosis; CO 2 blown off; breathing too rapidly • Causes? – Pain; Anxiety; fever; thyrotoxicosis • Symptoms? – Numbness, tingling of extremities • Treatment? – Rebreathe into a paper bag – If extreme - sedation
ACID-BASE IMBALANCES • Metabolic Acidosis – p. H 7. 35; normal to Pa. CO 2; HCO 3 (bicarbonate level) • When bicarbonate is lost and acid is increased • Causes? – DM, Starvation, Infection; prolonged diarrhea • Symptoms? – Rapid breathing, diminished muscle tone, n/v, changed mental status • Treatment? – Treat underlying cause – IV therapy
ACID-BASE IMBALANCES • Metabolic Alkalosis – p. H 7. 45; Pa. CO 2 normal, bicarbonate • When the plasma loses hydrogen ions (acid) and gains bicarbonate • Causes? – Diuretic therapy that doesn’t conserve K+ – Loss of gastric fluids (N/V, N/G tube suction) • Symptoms? tetany, irritability, disorientation • Treatment? – Treat underlying cause – IV therapy – Supplemental oxygen
TYPES OF INTRAVENOUS SOLUTIONS Loss of fluids results in a loss of electrolytes. IV therapy is often needed to restore fluid balance and electrolyte balance. Is used in promotion of HOMEOSTASIS
“WHAT’S THIS OSMOLARITY? ” • An IV solution is chosen for it’s osmolarity or concentration of osmoles of solutes • Osmolarity affects the body’s intracellular fluid (ICF) and extracellular fluid (ECF) – Patients who are overloaded with fluid have a lower serum osmolarity – Patients who are dehydrated have a higher serum osmolarity
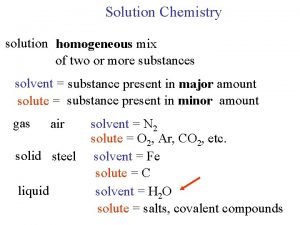
INTRAVENOUS SOLUTIONS • IV solutions consist of water containing one or more types of solutes (substance that dissolves in solution) • Solutes most commonly dissolved in IV solutions are – Sodium chloride – Dextrose – Potassium chloride REMEMBER… • Solutes that dissolve in water and dissociate into ion particles are called electrolytes
EQUILIBRIUM… or is it FUNG SHUI? • When something is in balance with it’s environment • A cell is in equilibrium if it is in a solution with the same concentration of solutes as the cell
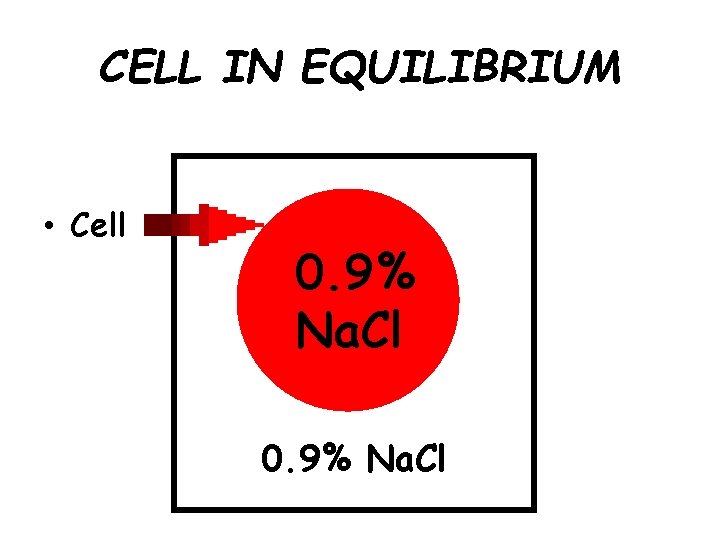
CELL IN EQUILIBRIUM • Cell 0. 9% Na. Cl
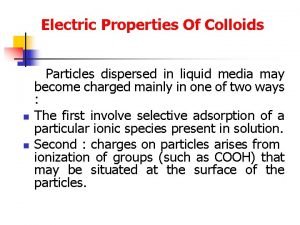
TYPES OF SOLUTIONS • There are 2 types of solution – Crystalloid solution • Consists of water and uniformly dissolved crystals like salt or sugar – Colloid solution • Consists of water and molecules of suspended substances like blood cells and blood products
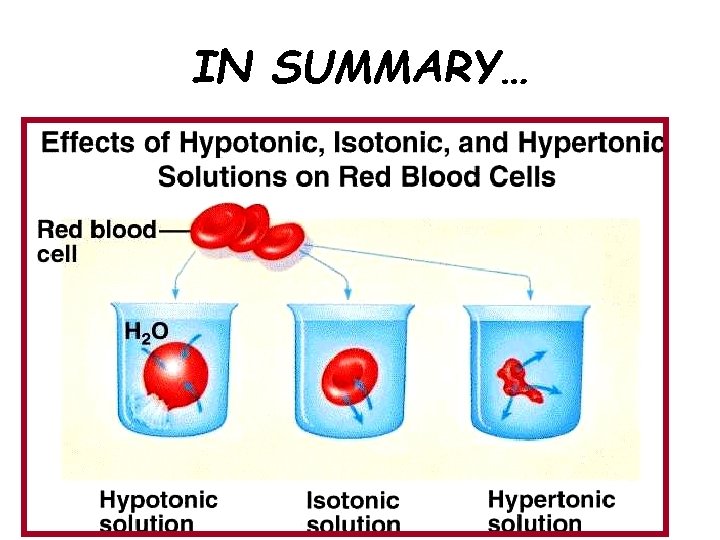
CRYSTALLOID SOLUTIONS • There are 3 categories of Crystalloid solutions: – ISOTONIC • Have the same concentration or osmolarity that serum and body fluids have – HYPOTONIC • Have an osmolarity lower than serum – HYPERTONIC • Have an osmolarity higher than serum
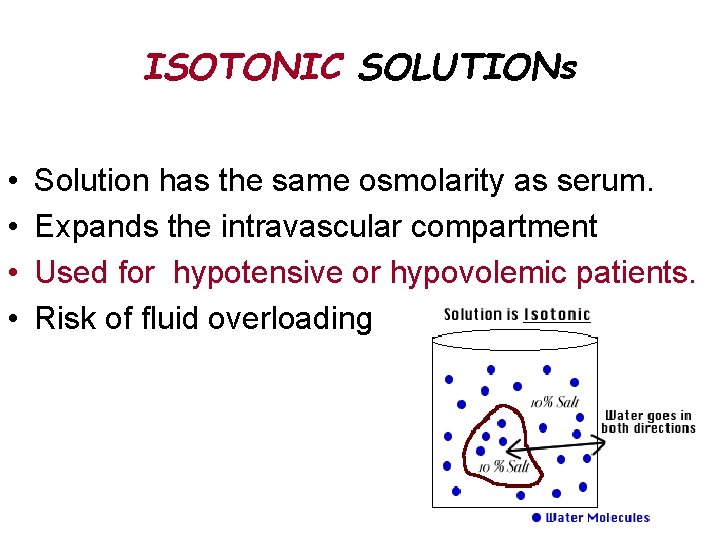
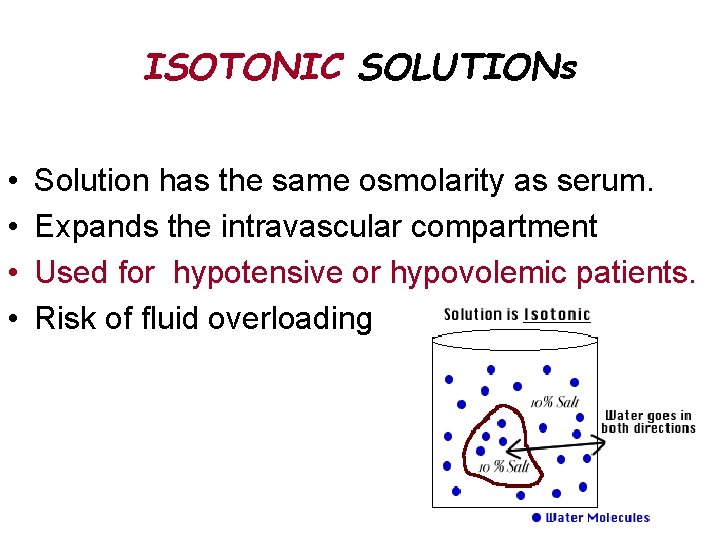
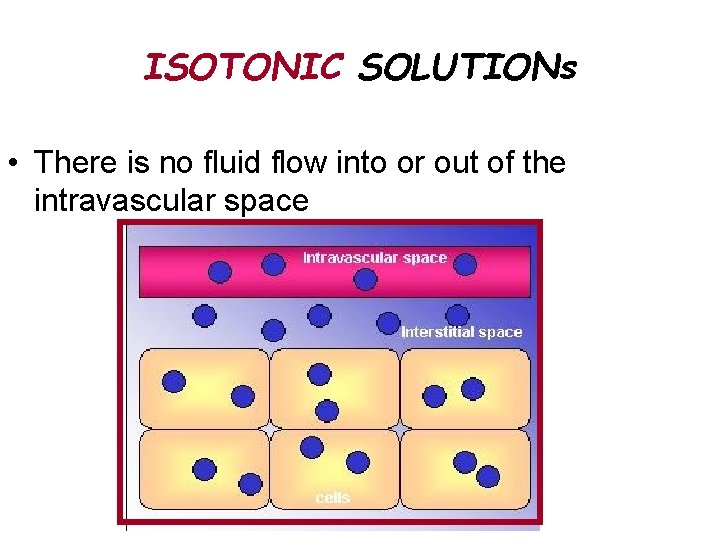
ISOTONIC SOLUTIONs • • Solution has the same osmolarity as serum. Expands the intravascular compartment Used for hypotensive or hypovolemic patients. Risk of fluid overloading
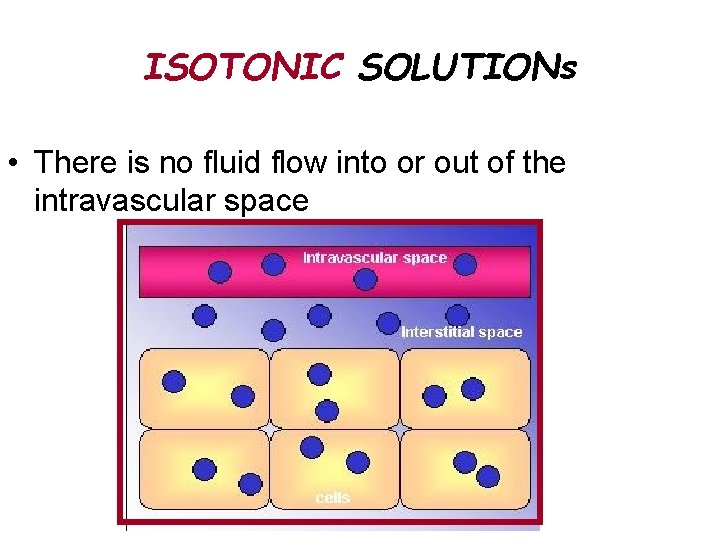
ISOTONIC SOLUTIONs • There is no fluid flow into or out of the intravascular space
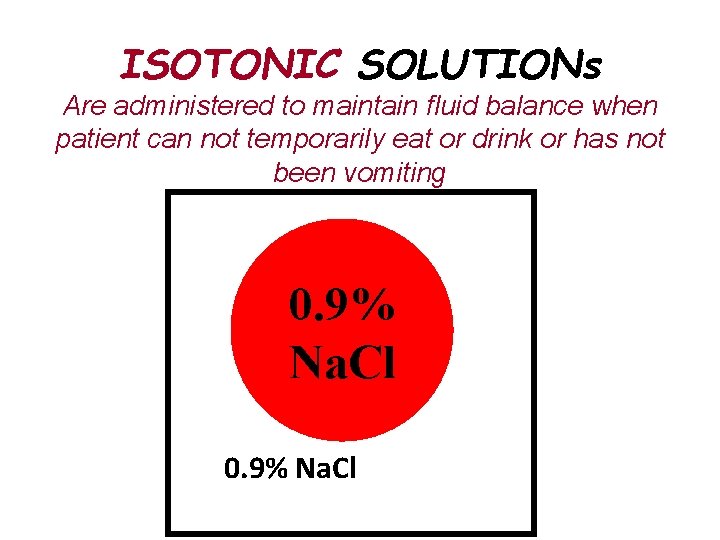
ISOTONIC SOLUTIONs Are administered to maintain fluid balance when patient can not temporarily eat or drink or has not been vomiting 0. 9% Na. Cl
ISOTONIC SOLUTIONS • Many IV solutions are isotonic • Examples: – Lactated Ringer's (LR) – NS (normal saline, or 0. 9% saline in water) – D 5% Water
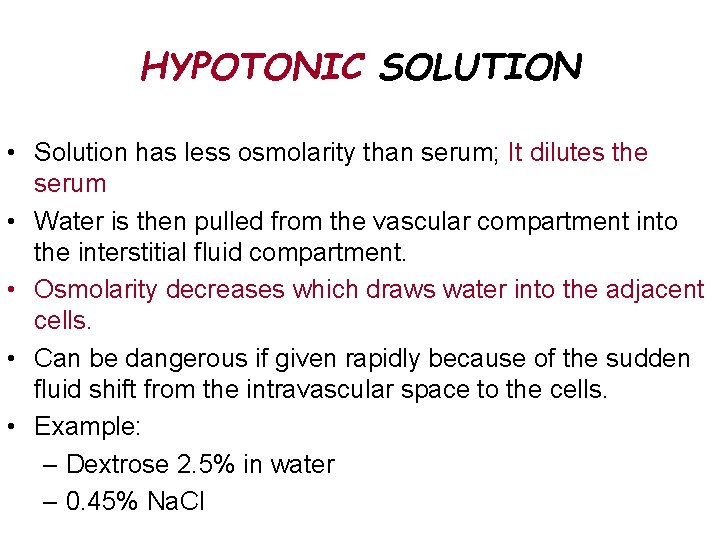
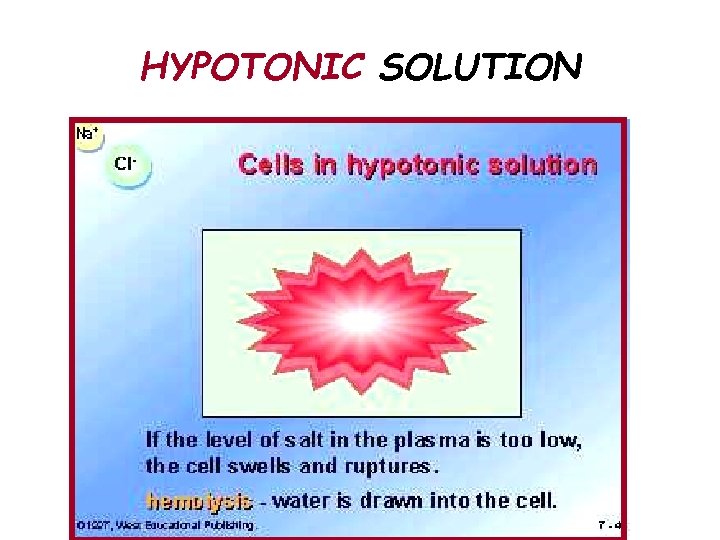
HYPOTONIC SOLUTION • Solution has less osmolarity than serum; It dilutes the serum • Water is then pulled from the vascular compartment into the interstitial fluid compartment. • Osmolarity decreases which draws water into the adjacent cells. • Can be dangerous if given rapidly because of the sudden fluid shift from the intravascular space to the cells. • Example: – Dextrose 2. 5% in water – 0. 45% Na. Cl
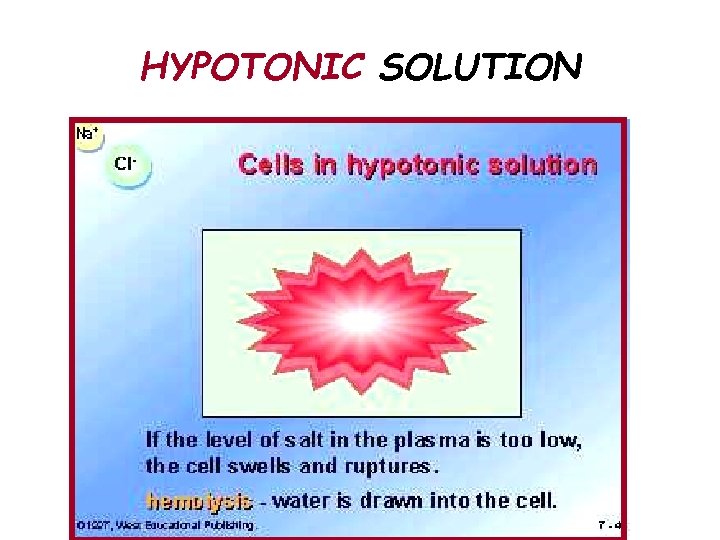
HYPOTONIC SOLUTION
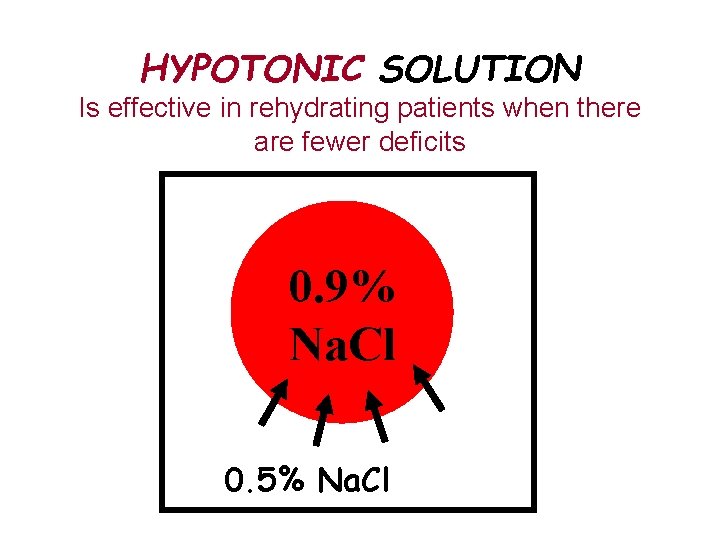
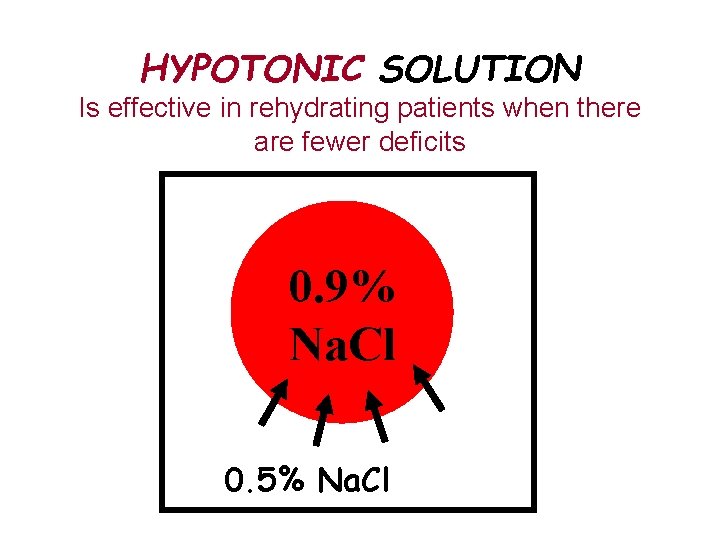
HYPOTONIC SOLUTION Is effective in rehydrating patients when there are fewer deficits 0. 9% Na. Cl 0. 5% Na. Cl
CELLS SWELL IN AN HYPOTONIC SOLUTION
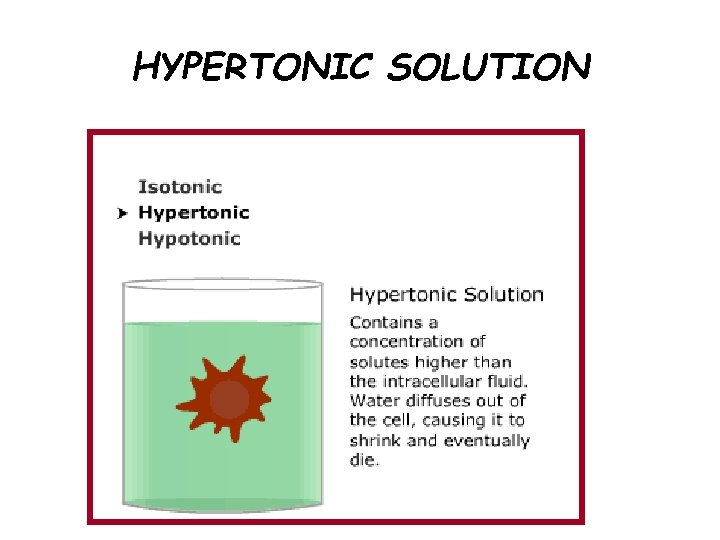
HYPERTONIC SOLUTION • Higher osmolality than serum. – Pulls fluid and electrolytes into the intravascular compartment. • Help stabilize blood pressure, increase urine output, and reduce edema. • Rarely used in the pre-hospital setting. • Examples: – D 5 ½ NS; D 5 NS
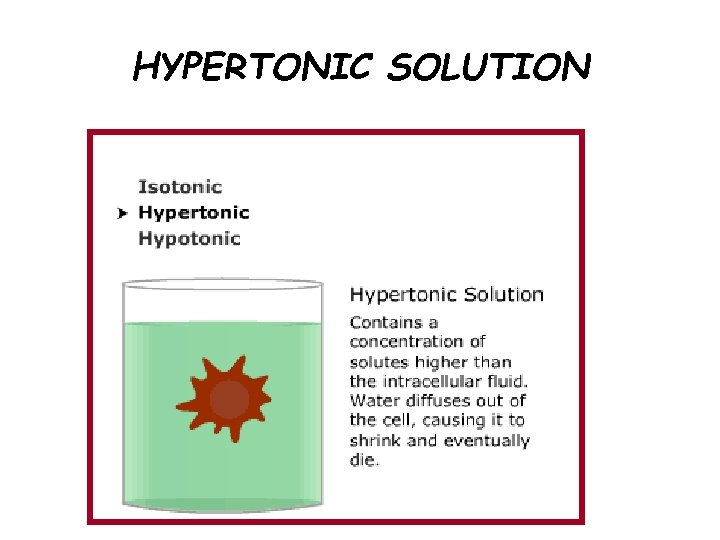
HYPERTONIC SOLUTION
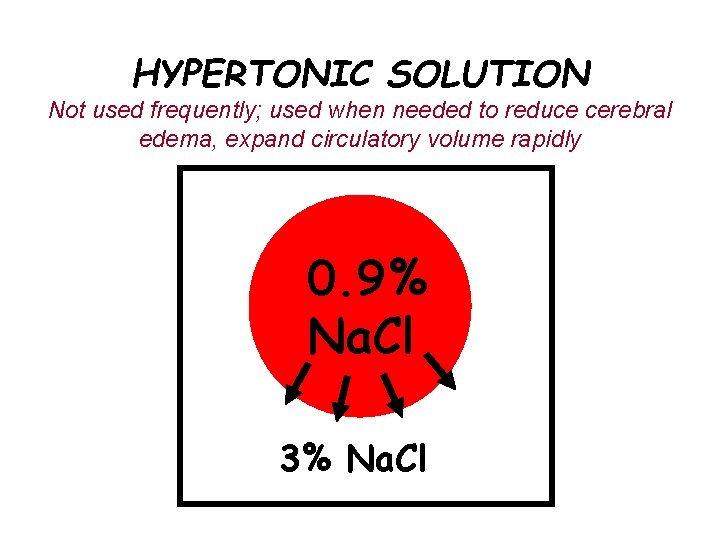
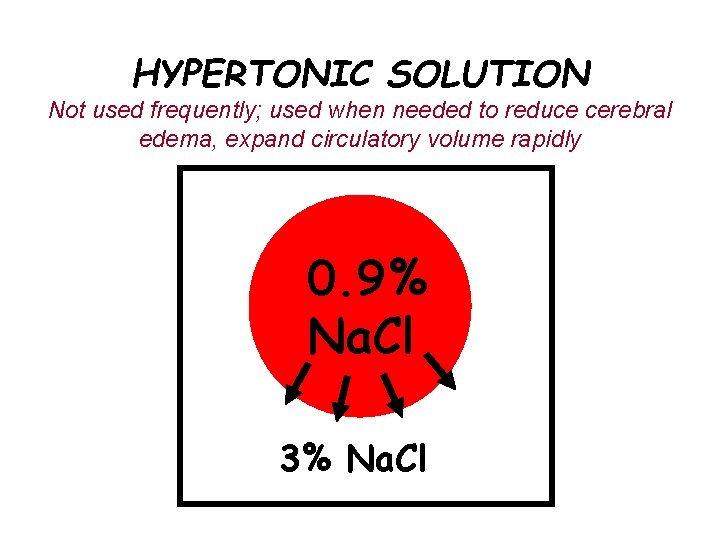
HYPERTONIC SOLUTION Not used frequently; used when needed to reduce cerebral edema, expand circulatory volume rapidly 0. 9% Na. Cl 3% Na. Cl
HYPERTONIC SOLUTIONS Nursing considerations: - Monitor for circulatory overload - Contraindicated in diabetic ketoacidosis (dehydration) - Impaired heart and kidney function
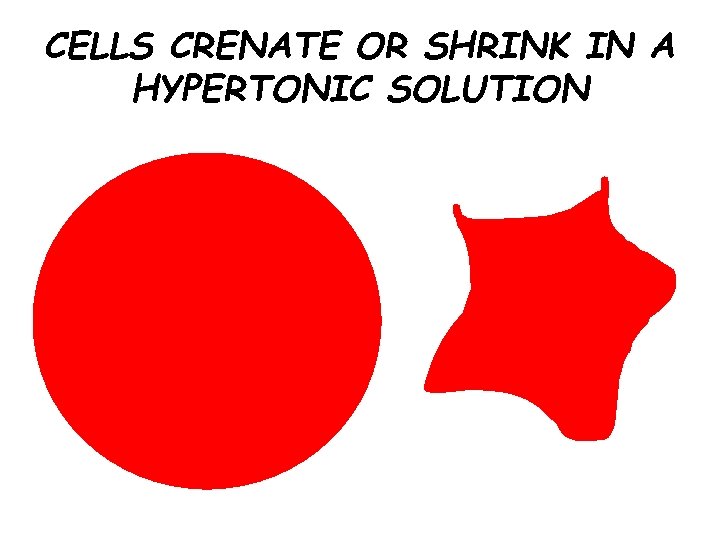
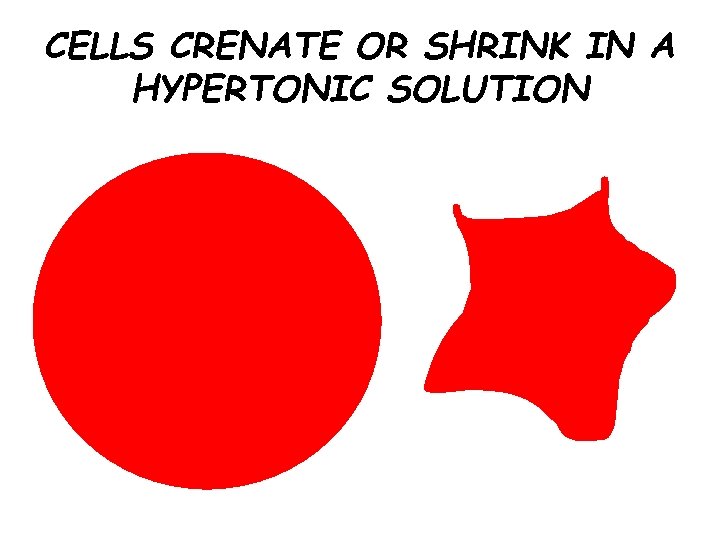
CELLS CRENATE OR SHRINK IN A HYPERTONIC SOLUTION
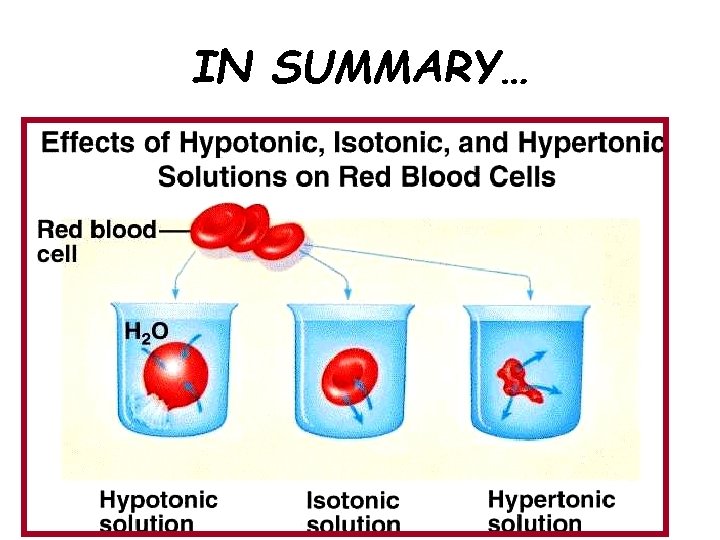
IN SUMMARY…
COLLOID SOLUTIONS • Colloid solutions are large proteins; remain in the vascular space • Used to replace circulating blood volume – Blood (whole and packed cells) – Blood products – Plasma expanders • Dextran • Hetastarch
Example of HYPERTONIC SOLUTION • Total parenteral Nutrition (TPN) – Consists of all the nutrients needed to meet the caloric and nutritional demands of the body – Used on severely malnourished patients or those who can not consume liquids or foods for a long time – Administered through an intravenous infusion, usually a central line
TOTAL PARENTERAL NUTRTION • This is a complete form of nutrition, containing protein, sugar, fat, and added vitamins and minerals as needed for each individual. • It is administered through an intravenous infusion, usually using a central line.
TOTAL PARENTERAL NUTRTION • TPN is a lifesaver for people who are unable to absorb adequate nutrition through their intestines. • Motility problems that lead to TPN usage can be very difficult to diagnose. • TPN is administered for varying hours on a daily or sometimes on a several times a week basis.
OVERVIEW OF EQUIPMENT IV administration sets are the apparatus that connects a large volume of parenteral solution with the IV access device in the patient’s vein.
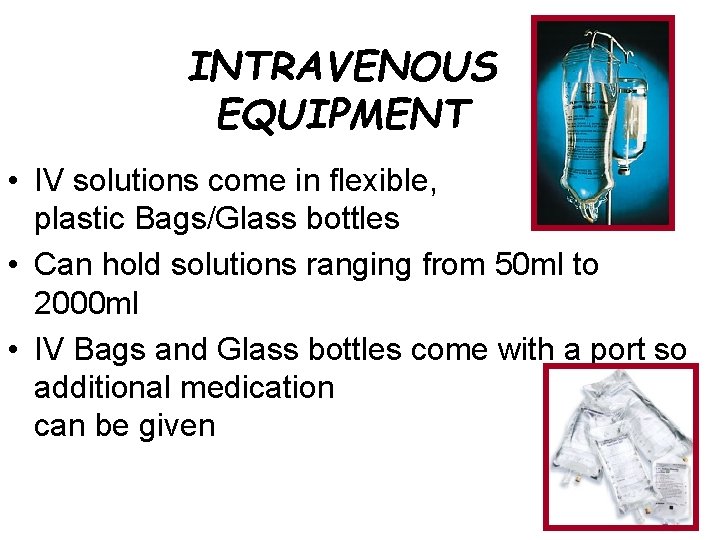
INTRAVENOUS EQUIPMENT • IV solutions come in flexible, plastic Bags/Glass bottles • Can hold solutions ranging from 50 ml to 2000 ml • IV Bags and Glass bottles come with a port so additional medication can be given
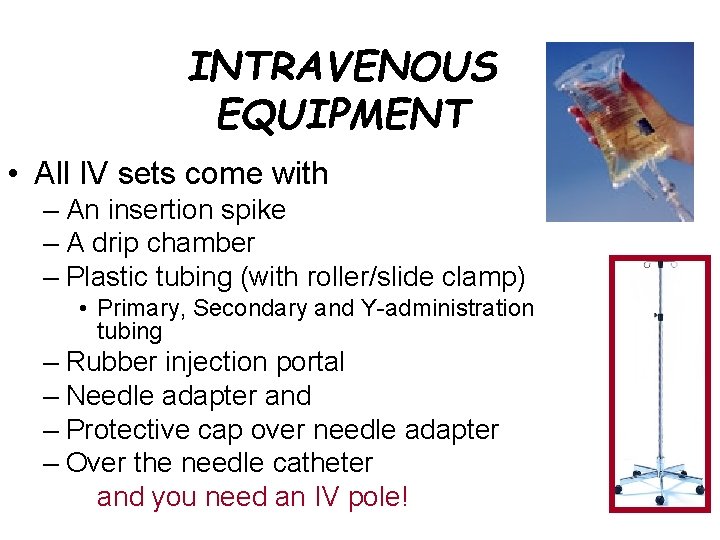
INTRAVENOUS EQUIPMENT • All IV sets come with – An insertion spike – A drip chamber – Plastic tubing (with roller/slide clamp) • Primary, Secondary and Y-administration tubing – Rubber injection portal – Needle adapter and – Protective cap over needle adapter – Over the needle catheter and you need an IV pole!
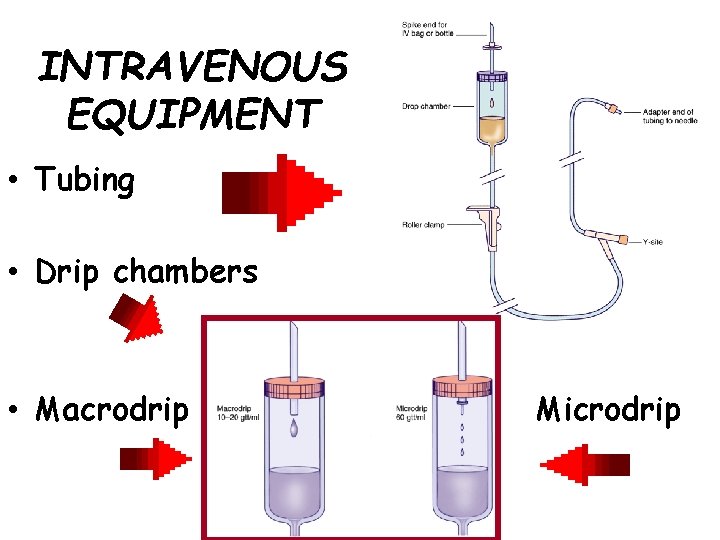
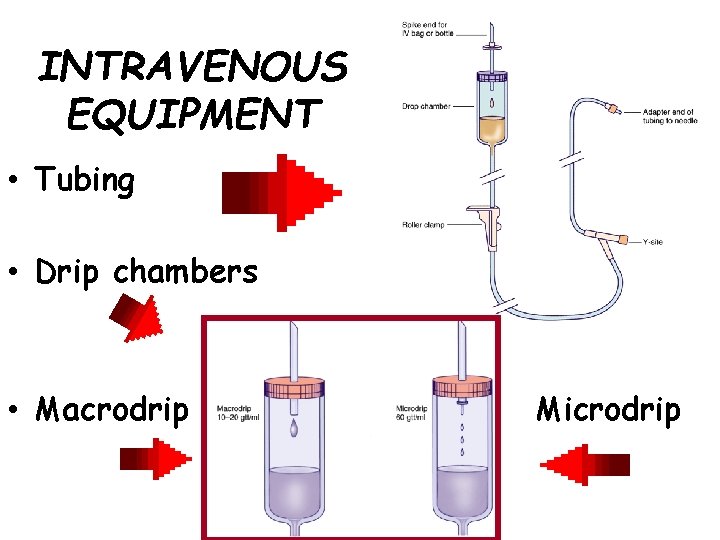
INTRAVENOUS EQUIPMENT • Tubing • Drip chambers • Macrodrip Microdrip

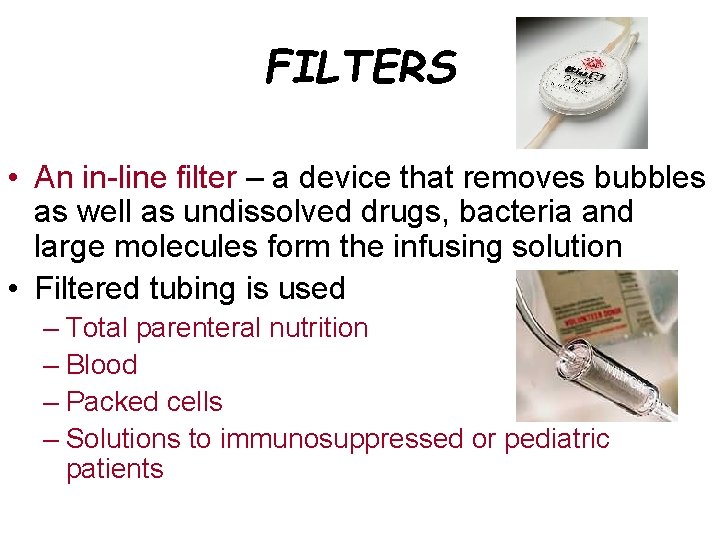
FILTERS • An in-line filter – a device that removes bubbles as well as undissolved drugs, bacteria and large molecules form the infusing solution • Filtered tubing is used – Total parenteral nutrition – Blood – Packed cells – Solutions to immunosuppressed or pediatric patients
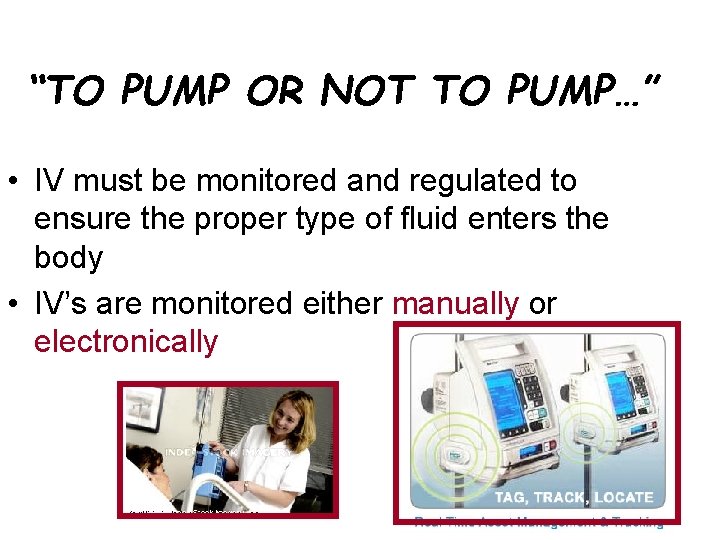
“TO PUMP OR NOT TO PUMP…” • IV must be monitored and regulated to ensure the proper type of fluid enters the body • IV’s are monitored either manually or electronically
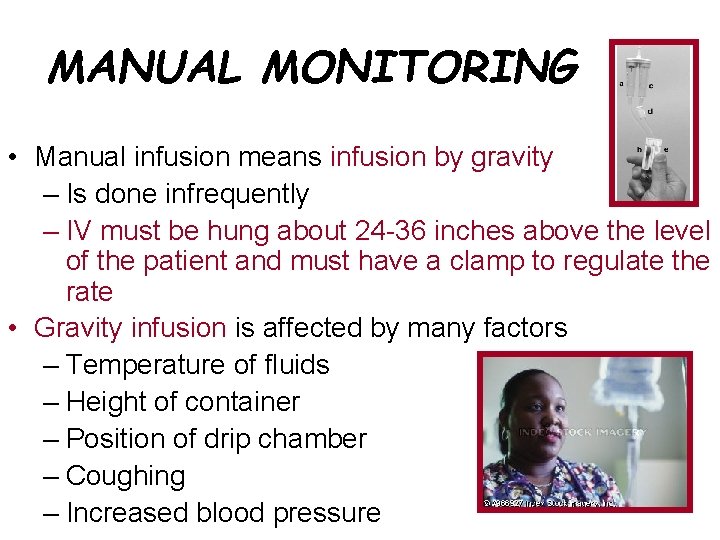
MANUAL MONITORING • Manual infusion means infusion by gravity – Is done infrequently – IV must be hung about 24 -36 inches above the level of the patient and must have a clamp to regulate the rate • Gravity infusion is affected by many factors – Temperature of fluids – Height of container – Position of drip chamber – Coughing – Increased blood pressure
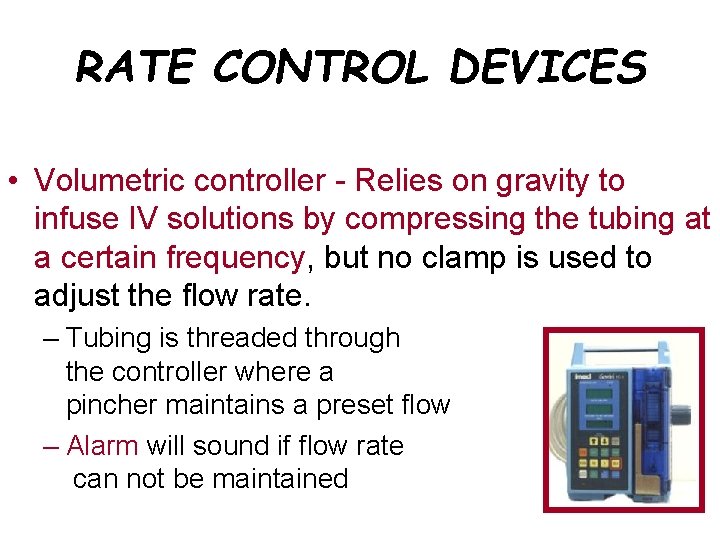
RATE CONTROL DEVICES • Volumetric controller - Relies on gravity to infuse IV solutions by compressing the tubing at a certain frequency, but no clamp is used to adjust the flow rate. – Tubing is threaded through the controller where a pincher maintains a preset flow – Alarm will sound if flow rate can not be maintained
RATE CONTROL DEVICES • Flow rates of IV’s can be tricky so they should be checked frequently • Types of IV clamps – Roller clamp – Screw clamp – Slide clamp
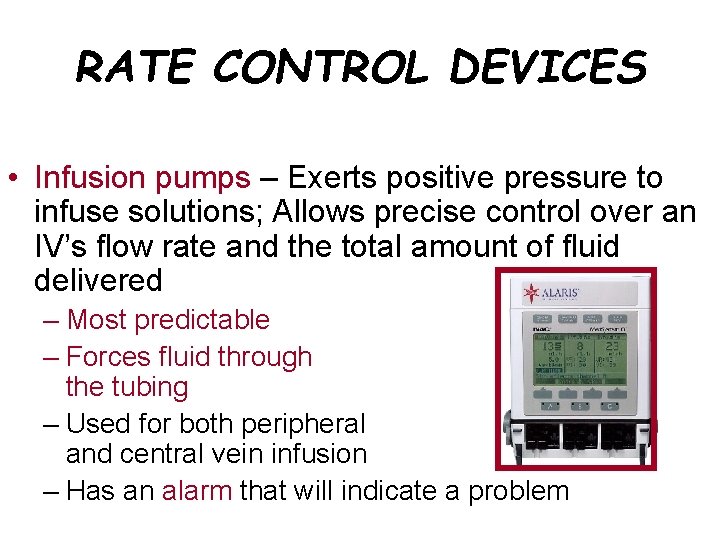
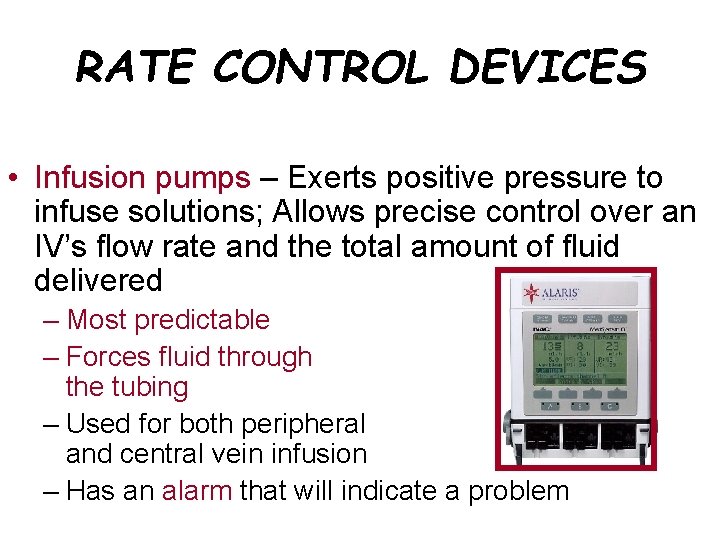
RATE CONTROL DEVICES • Infusion pumps – Exerts positive pressure to infuse solutions; Allows precise control over an IV’s flow rate and the total amount of fluid delivered – Most predictable – Forces fluid through the tubing – Used for both peripheral and central vein infusion – Has an alarm that will indicate a problem
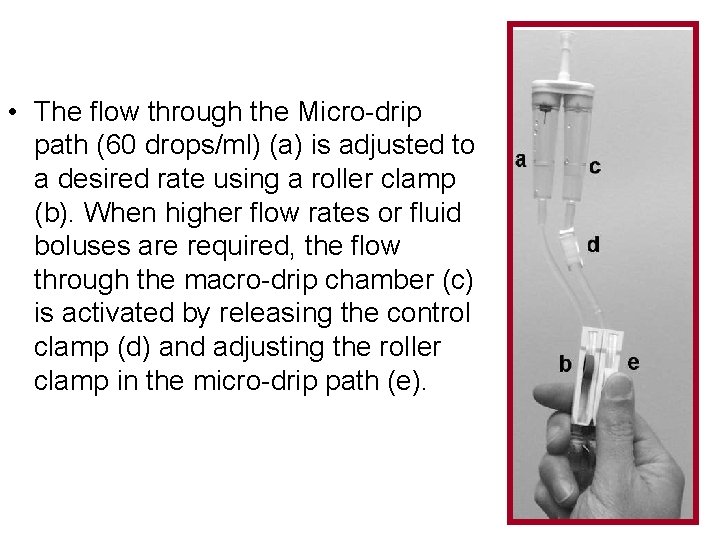
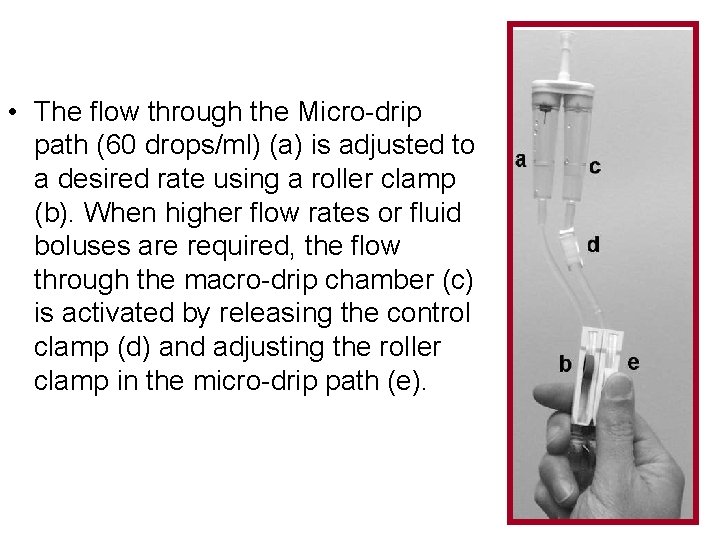
• The flow through the Micro-drip path (60 drops/ml) (a) is adjusted to a desired rate using a roller clamp (b). When higher flow rates or fluid boluses are required, the flow through the macro-drip chamber (c) is activated by releasing the control clamp (d) and adjusting the roller clamp in the micro-drip path (e).
SYRINGE PUMP • Holds a pre-filled syringe; pressure is applied to the plunger to deliver a specific volume of medicine over a set time • Examples: – Continuously infuse Insulin into subcutaneous tissue of patients with DM – Patient controlled analgesia (PCA) to administer continual or bolus pain medicine
VOLUME CONTROL DEVICE • An inline receptacle between the patient's IV catheter set and the bag of IV fluid; max capacity is 150 ml
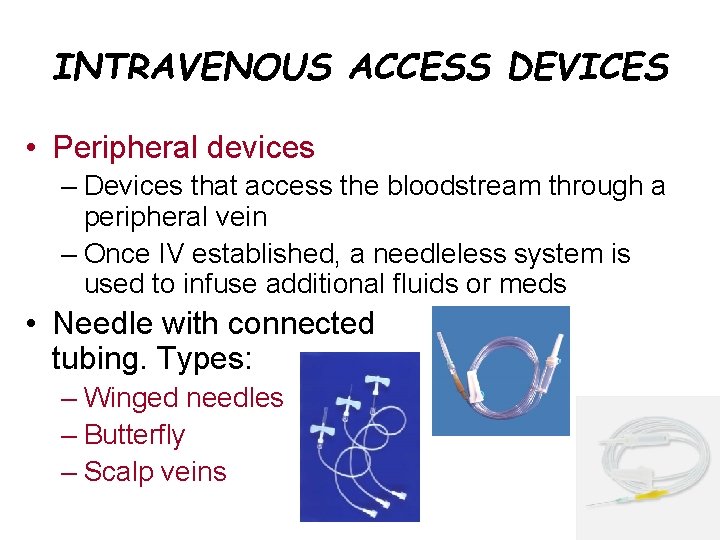
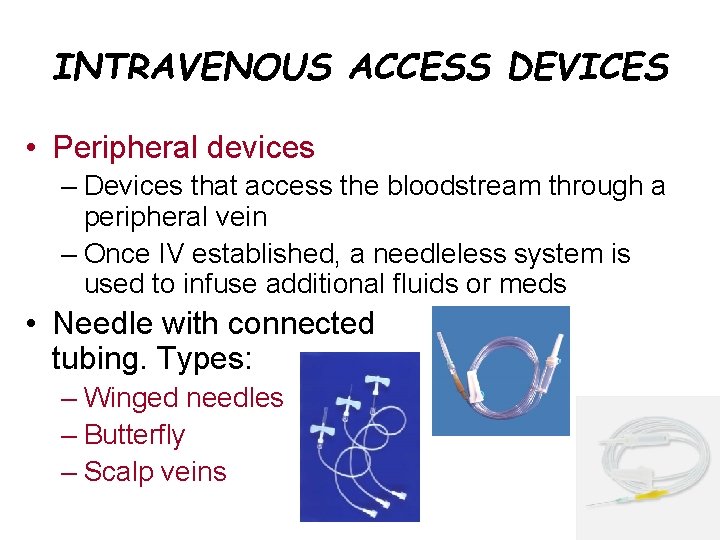
INTRAVENOUS ACCESS DEVICES • Peripheral devices – Devices that access the bloodstream through a peripheral vein – Once IV established, a needleless system is used to infuse additional fluids or meds • Needle with connected tubing. Types: – Winged needles – Butterfly – Scalp veins
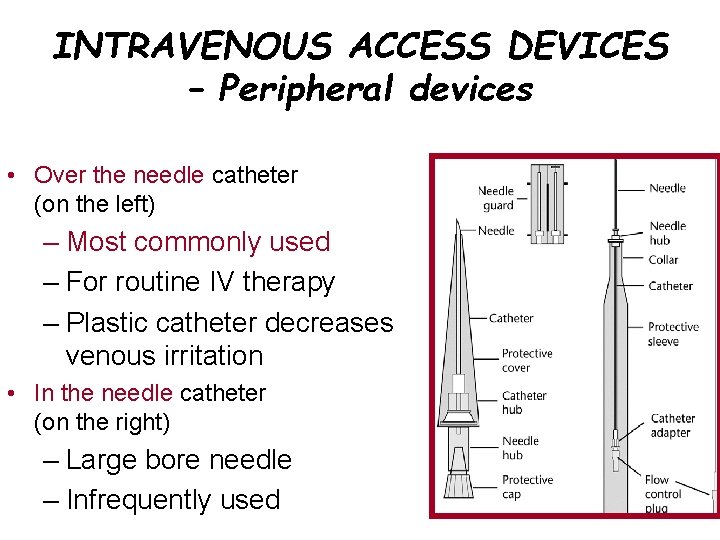
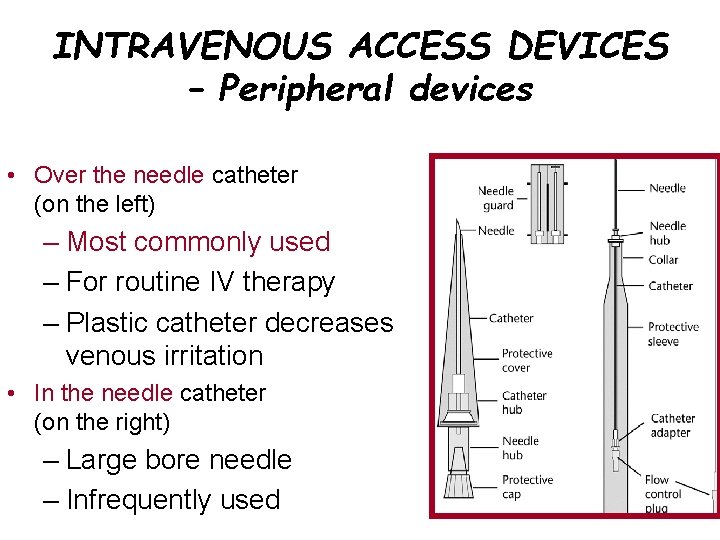
INTRAVENOUS ACCESS DEVICES – Peripheral devices • Over the needle catheter (on the left) – Most commonly used – For routine IV therapy – Plastic catheter decreases venous irritation • In the needle catheter (on the right) – Large bore needle – Infrequently used
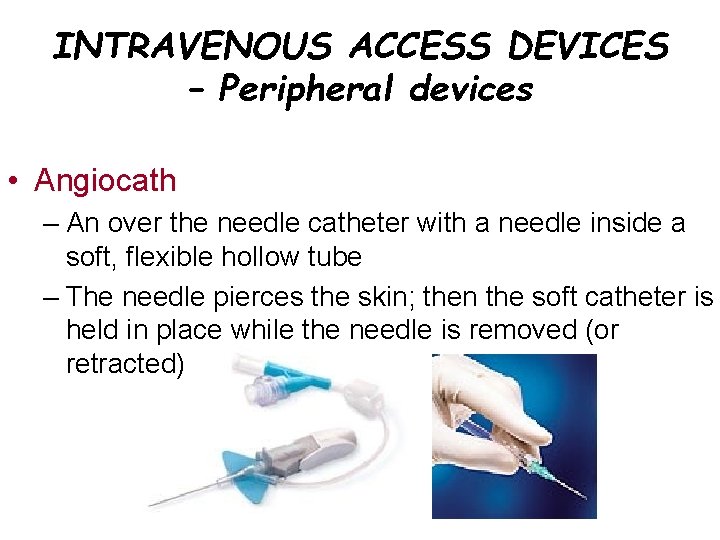
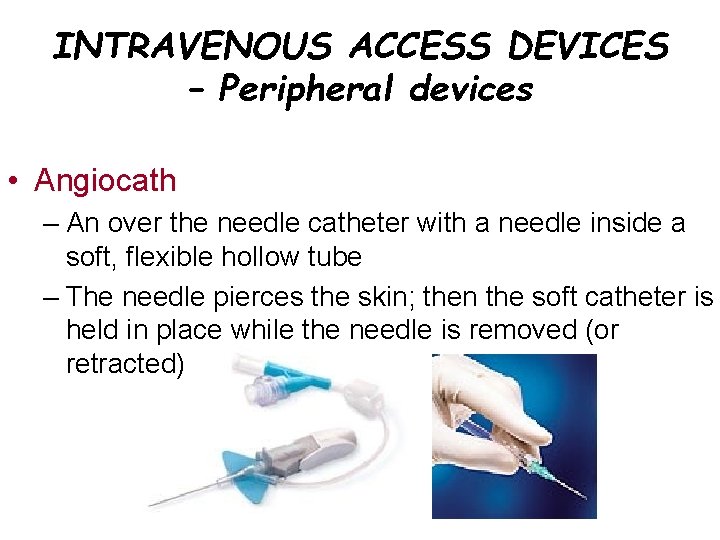
INTRAVENOUS ACCESS DEVICES – Peripheral devices • Angiocath – An over the needle catheter with a needle inside a soft, flexible hollow tube – The needle pierces the skin; then the soft catheter is held in place while the needle is removed (or retracted)

Angiocath Intravenous Catheters
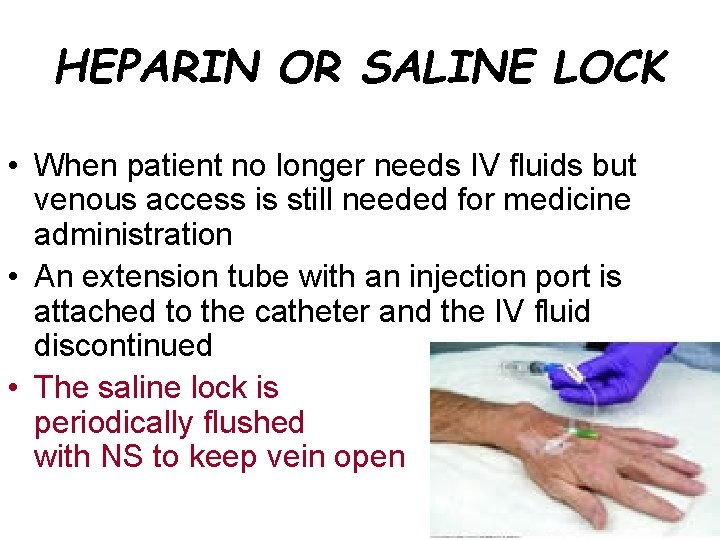
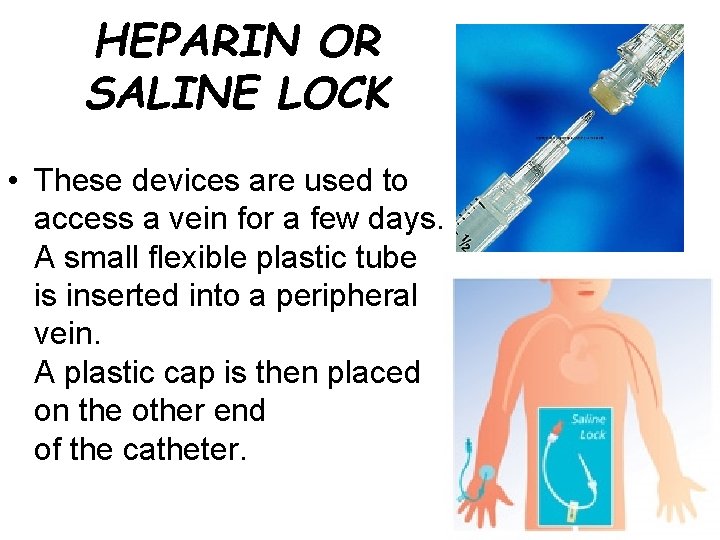
HEPARIN OR SALINE LOCK • When patient no longer needs IV fluids but venous access is still needed for medicine administration • An extension tube with an injection port is attached to the catheter and the IV fluid discontinued • The saline lock is periodically flushed with NS to keep vein open
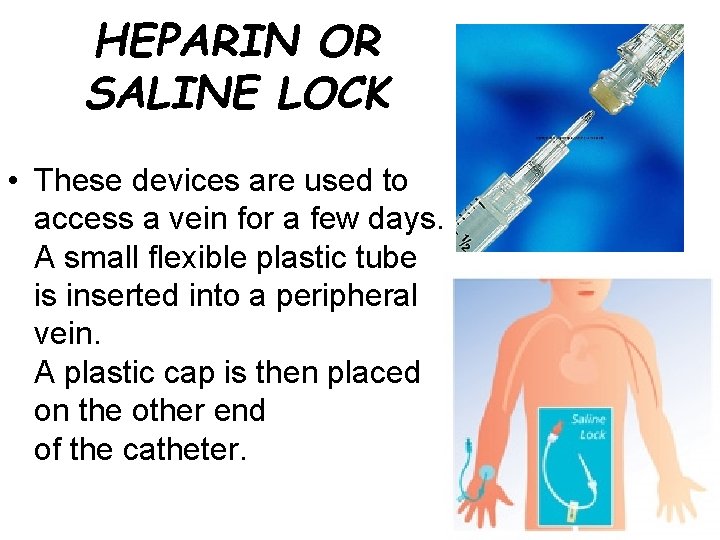
HEPARIN OR SALINE LOCK • These devices are used to access a vein for a few days. A small flexible plastic tube is inserted into a peripheral vein. A plastic cap is then placed on the other end of the catheter.
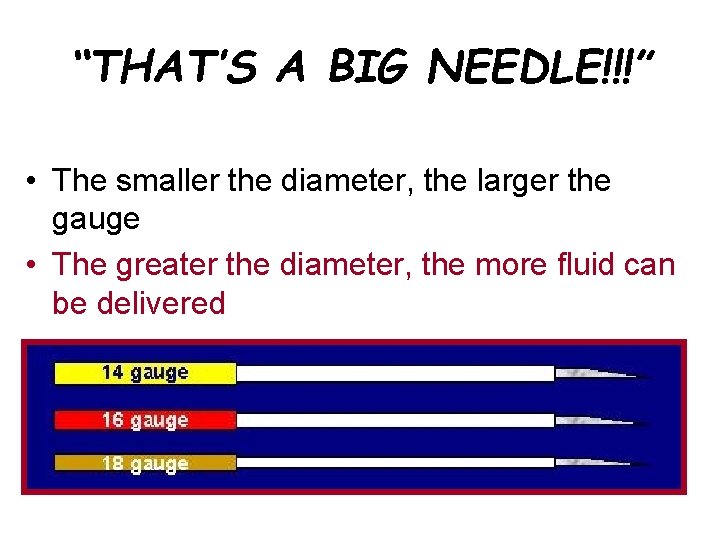
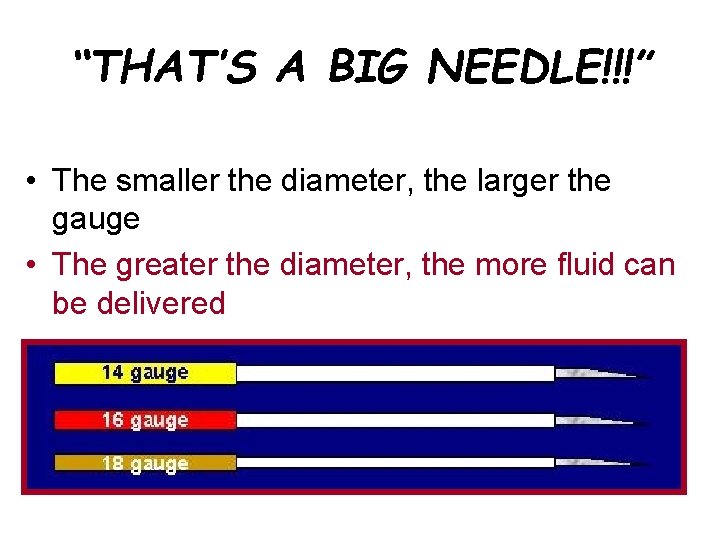
“THAT’S A BIG NEEDLE!!!” • The smaller the diameter, the larger the gauge • The greater the diameter, the more fluid can be delivered
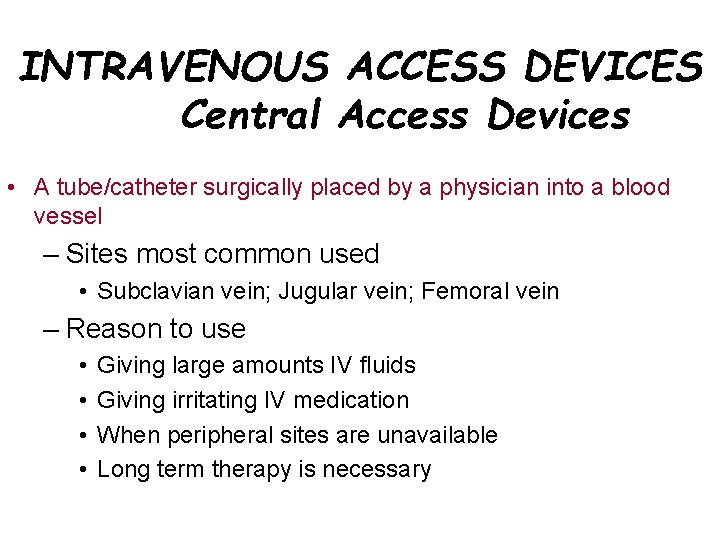
INTRAVENOUS ACCESS DEVICES Central Access Devices • A tube/catheter surgically placed by a physician into a blood vessel – Sites most common used • Subclavian vein; Jugular vein; Femoral vein – Reason to use • • Giving large amounts IV fluids Giving irritating IV medication When peripheral sites are unavailable Long term therapy is necessary
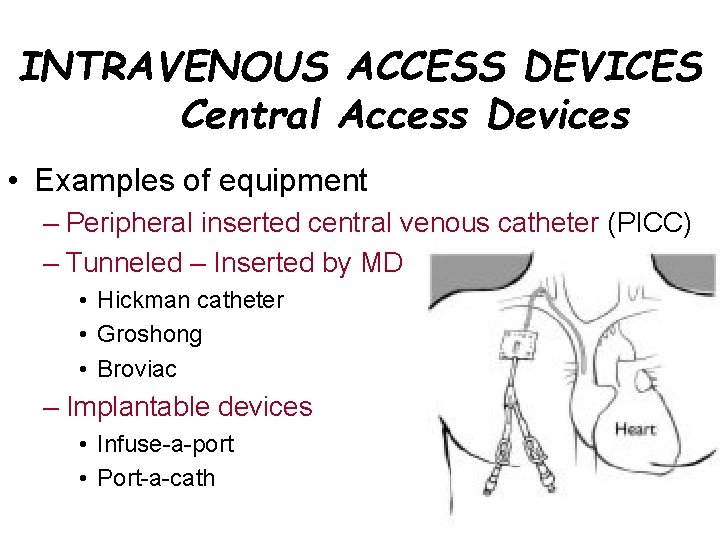
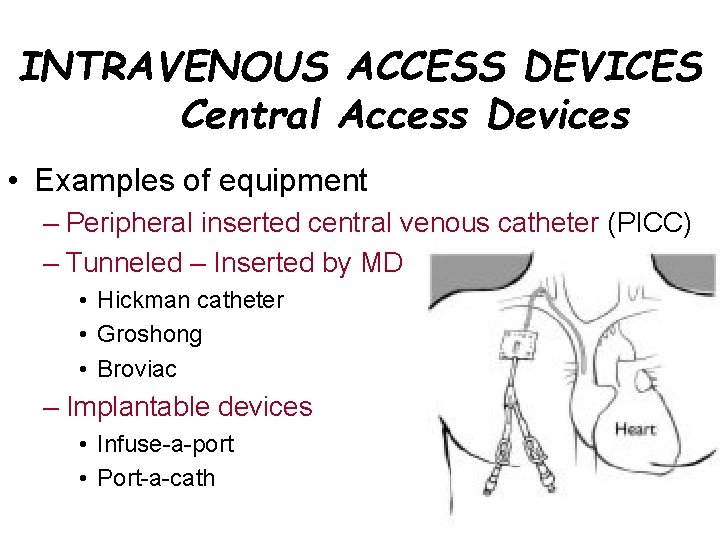
INTRAVENOUS ACCESS DEVICES Central Access Devices • Examples of equipment – Peripheral inserted central venous catheter (PICC) – Tunneled – Inserted by MD • Hickman catheter • Groshong • Broviac – Implantable devices • Infuse-a-port • Port-a-cath
CENTRAL VENOUS ACCESS • Advantages – Access to central veins – Rapid infusion – A way to draw blood without multiple sticks – Reduced risk of repeated venipunctures • Disadvantages – Pneumothorax – Sepsis – Perforation of the vessel/adjacent organs – Requires skill to insert
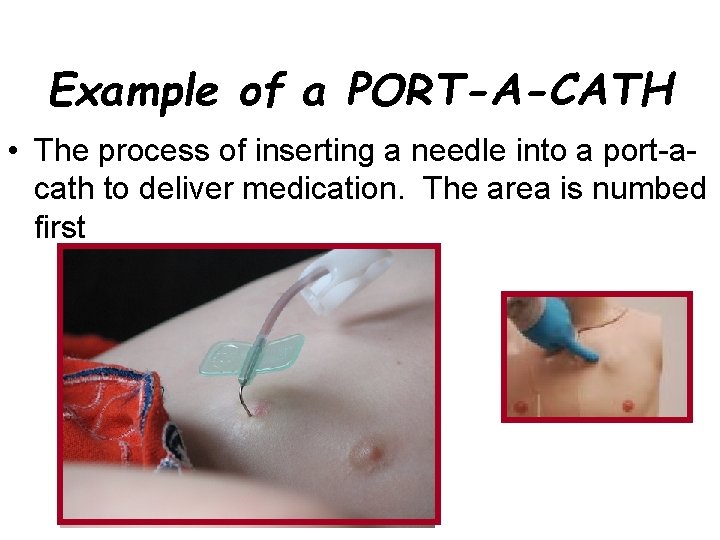
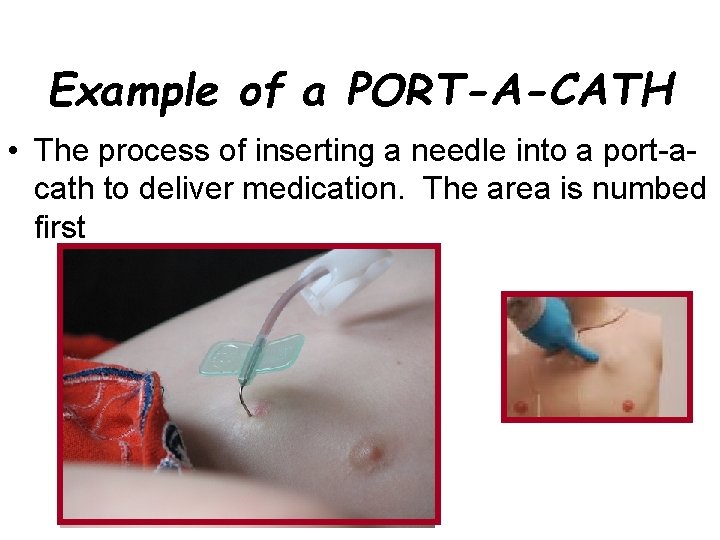
Example of a PORT-A-CATH • The process of inserting a needle into a port-acath to deliver medication. The area is numbed first
INTRAVENOUS FLOW RATES
TO BEGIN… • The physician will order the specific IV solution and amount for the patient over a specific amount of time • Before administering an IV, use these two values to calculate the flow rate for the IV solutions – For electronic pump-milliliters per hour (m. L/h) – No pump used - Drops per minute (gtt/min) –
• Unless you are using an electronic pump to deliver the fluid at precise amounts, you will need to learn how to set a flow rate yourself. • This is usually done by counting the number of drops that fall into the clear drip chamber on the IV administration set in one minute. • To do this, you must know what size administration set you are using (micro or macrodrip).
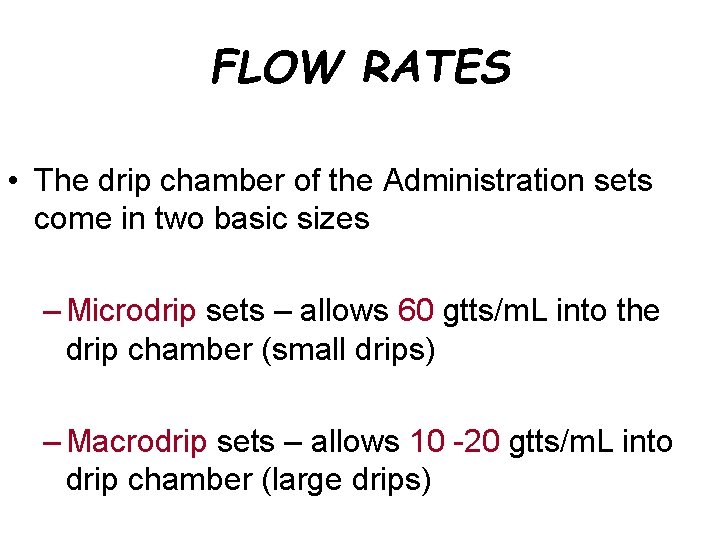
FLOW RATES • The drip chamber of the Administration sets come in two basic sizes – Microdrip sets – allows 60 gtts/m. L into the drip chamber (small drips) – Macrodrip sets – allows 10 -20 gtts/m. L into drip chamber (large drips)
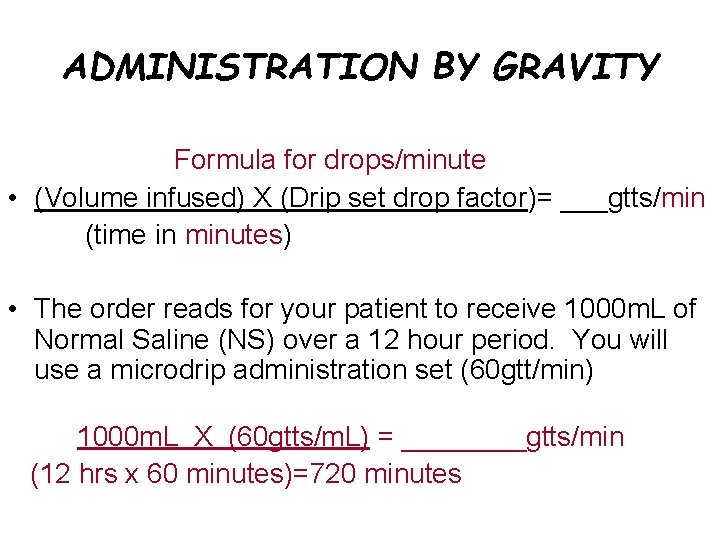
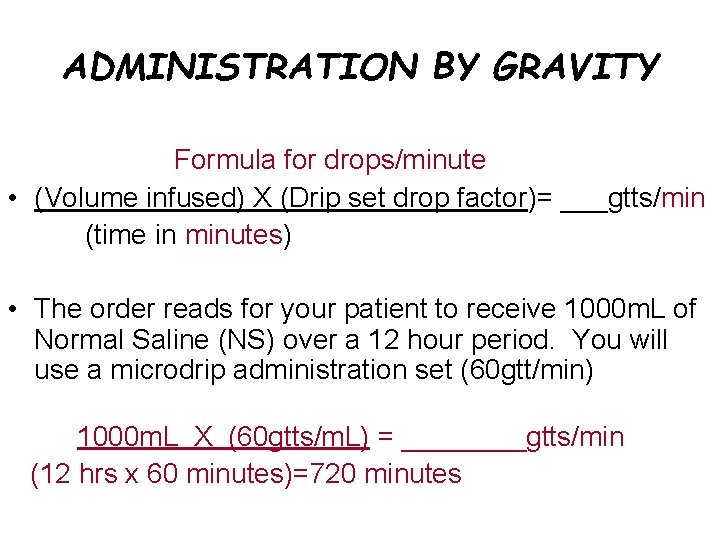
ADMINISTRATION BY GRAVITY Formula for drops/minute • (Volume infused) X (Drip set drop factor)= ___gtts/min (time in minutes) • The order reads for your patient to receive 1000 m. L of Normal Saline (NS) over a 12 hour period. You will use a microdrip administration set (60 gtt/min) 1000 m. L X (60 gtts/m. L) = ____gtts/min (12 hrs x 60 minutes)=720 minutes
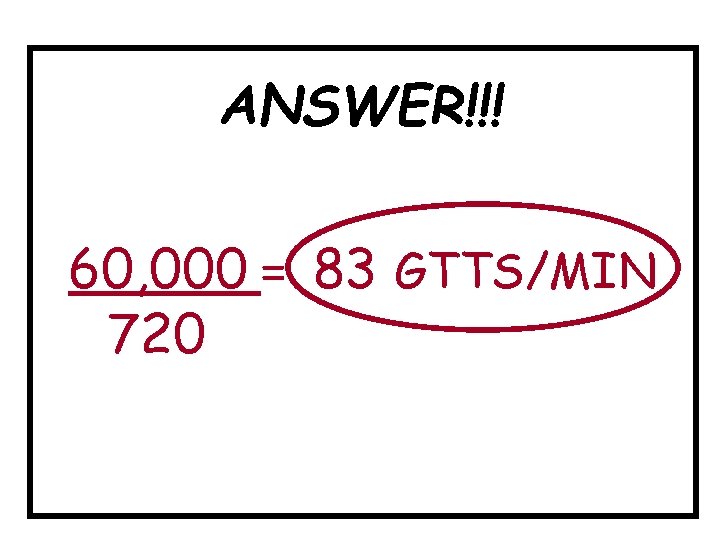
ANSWER!!! 60, 000 = 83 GTTS/MIN 720
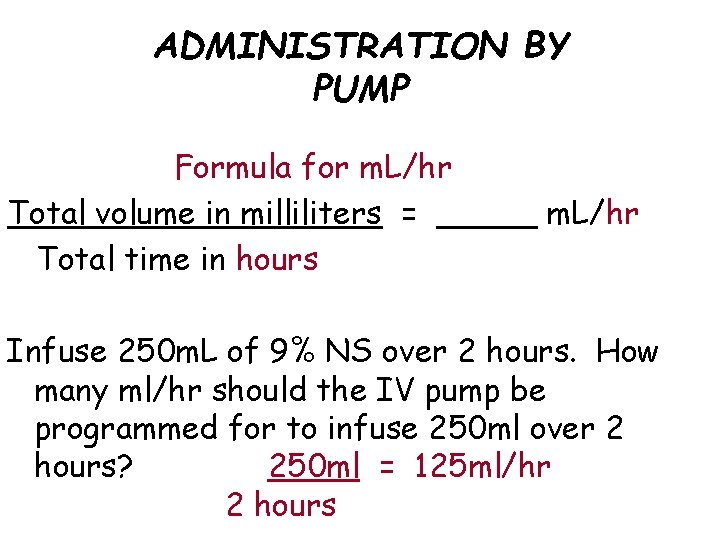
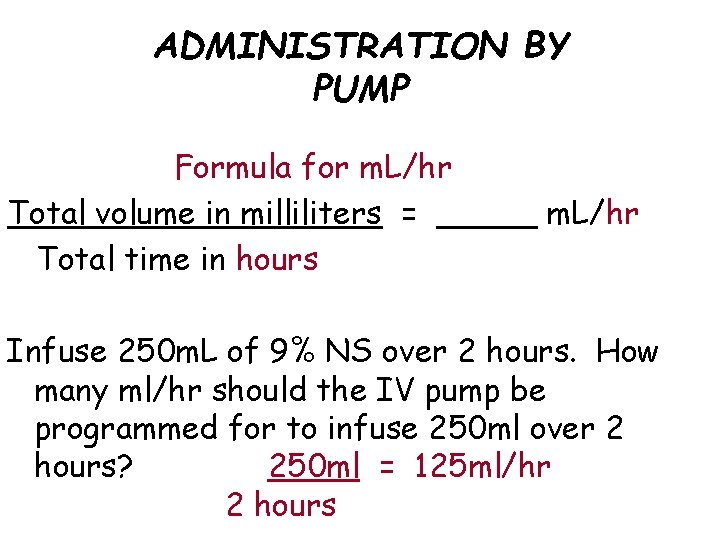
ADMINISTRATION BY PUMP Formula for m. L/hr Total volume in milliliters = _____ m. L/hr Total time in hours Infuse 250 m. L of 9% NS over 2 hours. How many ml/hr should the IV pump be programmed for to infuse 250 ml over 2 hours? 250 ml = 125 ml/hr 2 hours
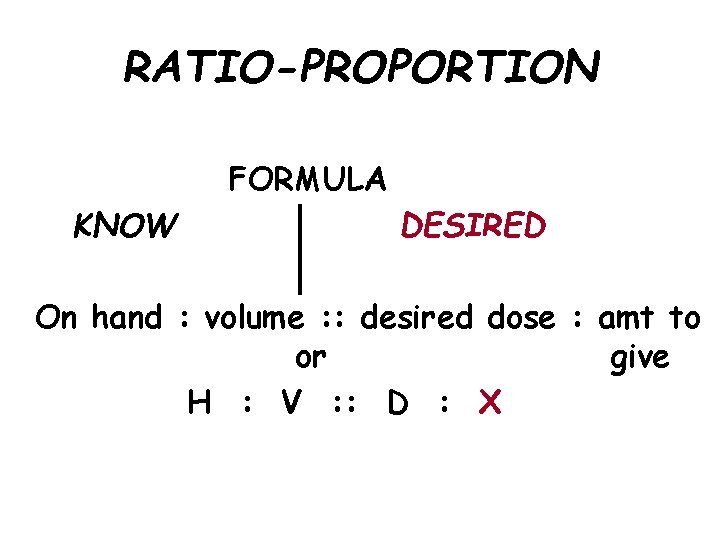
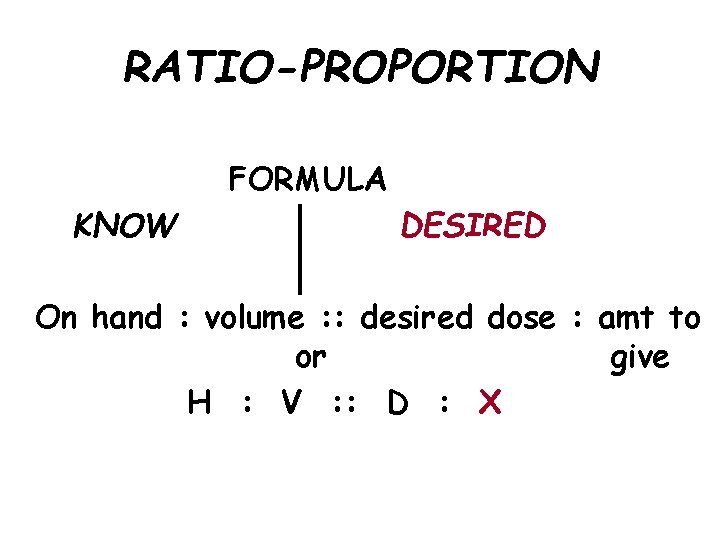
RATIO-PROPORTION FORMULA KNOW DESIRED On hand : volume : : desired dose : amt to or give H : V : : D : X
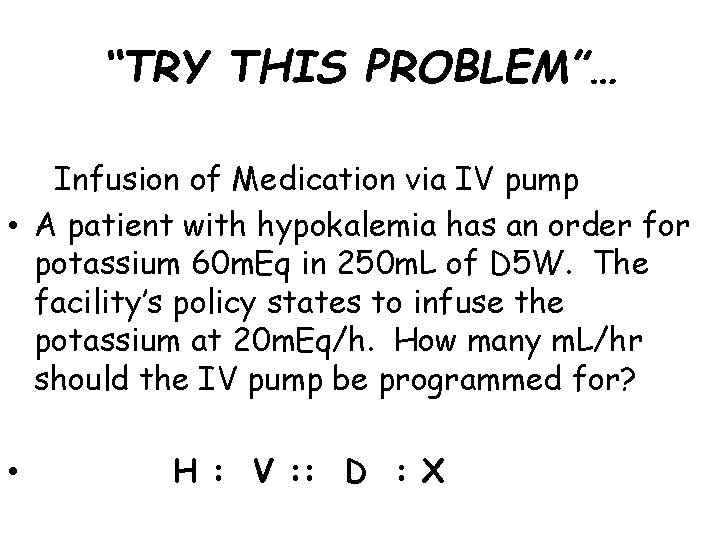
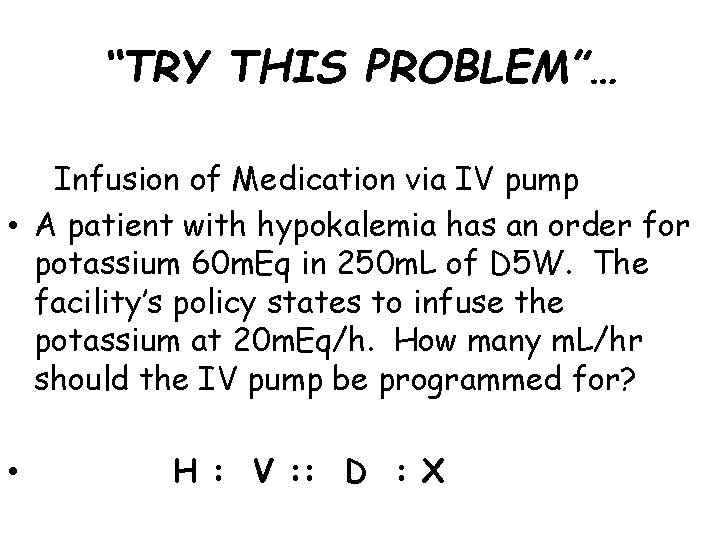
“TRY THIS PROBLEM”… Infusion of Medication via IV pump • A patient with hypokalemia has an order for potassium 60 m. Eq in 250 m. L of D 5 W. The facility’s policy states to infuse the potassium at 20 m. Eq/h. How many m. L/hr should the IV pump be programmed for? • H : V : : D : X
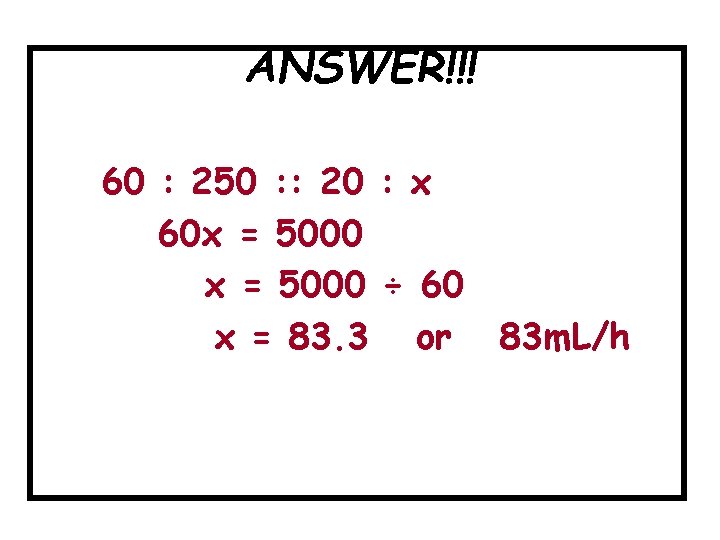
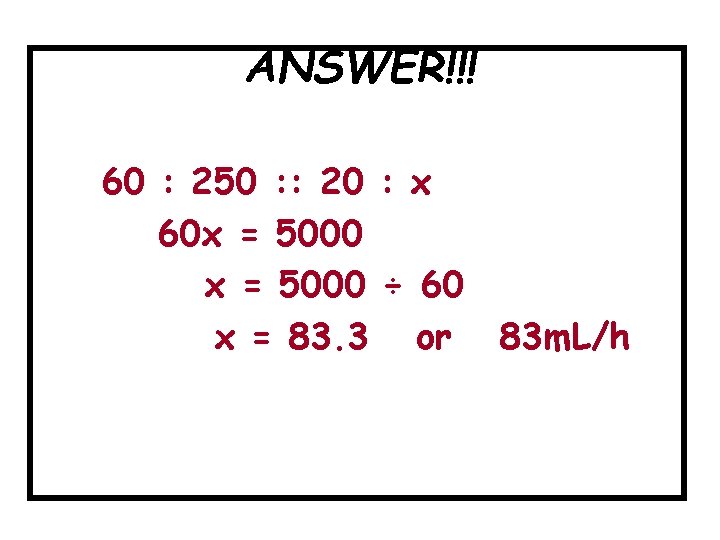
ANSWER!!! 60 : 250 : : 20 : x 60 x = 5000 ÷ 60 x = 83. 3 or 83 m. L/h
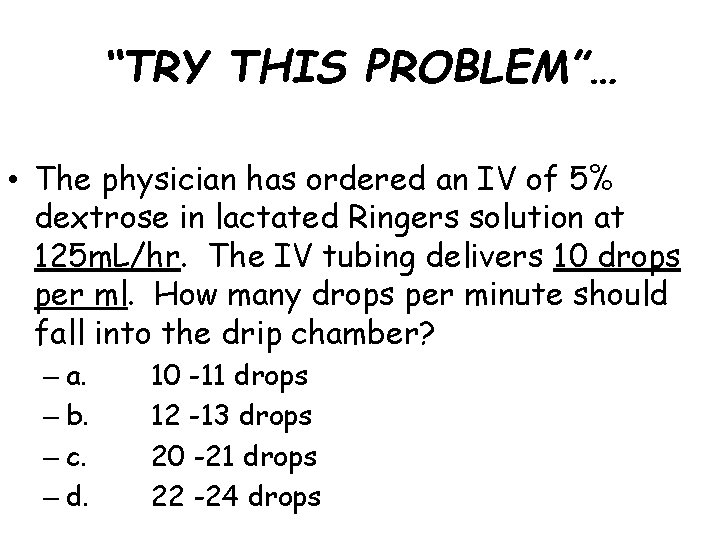
“TRY THIS PROBLEM”… • The physician has ordered an IV of 5% dextrose in lactated Ringers solution at 125 m. L/hr. The IV tubing delivers 10 drops per ml. How many drops per minute should fall into the drip chamber? – a. – b. – c. – d. 10 -11 drops 12 -13 drops 20 -21 drops 22 -24 drops
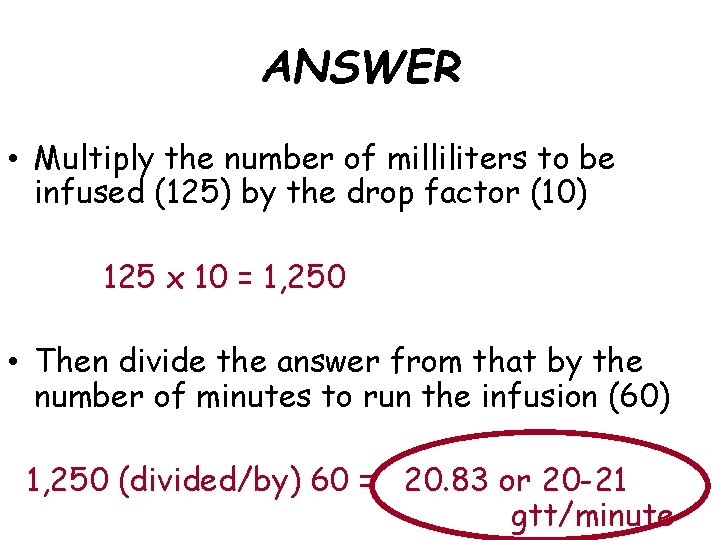
ANSWER • Multiply the number of milliliters to be infused (125) by the drop factor (10) 125 x 10 = 1, 250 • Then divide the answer from that by the number of minutes to run the infusion (60) 1, 250 (divided/by) 60 = 20. 83 or 20 -21 gtt/minute
 Iv infiltration complications
Iv infiltration complications Iv placement sites
Iv placement sites Concepts of medication administration pretest
Concepts of medication administration pretest Medication administration 3 pretest
Medication administration 3 pretest Flow rate of iv cannula
Flow rate of iv cannula Iv cannula labelling
Iv cannula labelling Iv cannula labelling
Iv cannula labelling Labelled
Labelled Three word parts
Three word parts In axial suspension which is taken as point of suspension
In axial suspension which is taken as point of suspension Bland aerosol therapy indications
Bland aerosol therapy indications Fraction of inspired oxygen
Fraction of inspired oxygen Weak electrolytes examples
Weak electrolytes examples Refeeding syndrome
Refeeding syndrome Refeeding syndrome electrolytes
Refeeding syndrome electrolytes Strong vs weak electrolytes
Strong vs weak electrolytes Congenital adrenal hyperplasia electrolytes
Congenital adrenal hyperplasia electrolytes Normal electrolytes values
Normal electrolytes values Normal electrolytes values
Normal electrolytes values Strong vs weak electrolytes
Strong vs weak electrolytes Strong vs weak electrolytes
Strong vs weak electrolytes Diabetic ketoacidosis
Diabetic ketoacidosis How does electrolytes affect the chemical equilibria?
How does electrolytes affect the chemical equilibria? Electrolytes and nonelectrolytes worksheet
Electrolytes and nonelectrolytes worksheet Weak electrolytes
Weak electrolytes Tropolar
Tropolar Protective colloids
Protective colloids Explain colloid
Explain colloid Chapter 18 fluids and electrolytes
Chapter 18 fluids and electrolytes Vapor pressure lowering
Vapor pressure lowering Major intra and extracellular electrolytes
Major intra and extracellular electrolytes Electrolytes and nonelectrolytes
Electrolytes and nonelectrolytes Herbalife hydrate 24
Herbalife hydrate 24 Fluid sf
Fluid sf Fluid statics deals with fluid at rest
Fluid statics deals with fluid at rest Fluid statics deals with
Fluid statics deals with Fluid compartments in the body
Fluid compartments in the body Ecf icf and interstitial fluid
Ecf icf and interstitial fluid Interstitial fluid vs extracellular fluid
Interstitial fluid vs extracellular fluid What is fluid kinematics
What is fluid kinematics Extracellular fluid and interstitial fluid
Extracellular fluid and interstitial fluid Tense ascites meaning
Tense ascites meaning Psychodynamic and humanistic therapies have in common
Psychodynamic and humanistic therapies have in common Bioness integrated therapy system occupational therapy
Bioness integrated therapy system occupational therapy Humanistic therapy aims to
Humanistic therapy aims to Product scope vs project scope
Product scope vs project scope Product scope vs project scope
Product scope vs project scope 8 domains of occupational therapy
8 domains of occupational therapy Contemporary occupational therapy practice
Contemporary occupational therapy practice Missouri physical therapy practice act
Missouri physical therapy practice act What is occupational health
What is occupational health Oregon state board of nursing license
Oregon state board of nursing license While a lvn has a directed scope of practice
While a lvn has a directed scope of practice Name the basic nail shapes for women.
Name the basic nail shapes for women. Oklahoma board of nursing
Oklahoma board of nursing New york state nurse practitioner scope of practice
New york state nurse practitioner scope of practice Personal trainer liability insurance ace
Personal trainer liability insurance ace Podortho nurse education
Podortho nurse education Practice assessor and practice supervisor
Practice assessor and practice supervisor Stillman vs bass technique
Stillman vs bass technique Indication of adenoidectomy
Indication of adenoidectomy Plica triangularis in tonsil
Plica triangularis in tonsil Shane barclay md
Shane barclay md Chord indications
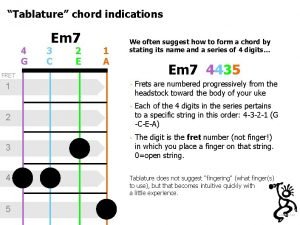
Chord indications Jewett brace icd 9
Jewett brace icd 9 Band and loop space maintainer advantages
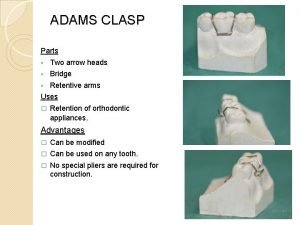
Band and loop space maintainer advantages Ryles tube contraindications
Ryles tube contraindications Single vs double lumen tracheostomy tube
Single vs double lumen tracheostomy tube What is mummy restraint
What is mummy restraint Indications for blood transfusion
Indications for blood transfusion Thoracentesis complications
Thoracentesis complications Position used in nursing
Position used in nursing Extended light's criteria for pleural effusion
Extended light's criteria for pleural effusion Thoracentesis indications
Thoracentesis indications Fissure sealant definition
Fissure sealant definition Classification of atrial fibrillation
Classification of atrial fibrillation Crown and loop space maintainer indications
Crown and loop space maintainer indications Modified three quarter crown
Modified three quarter crown Mri gp indications
Mri gp indications Throat definition
Throat definition Nasogastric tube
Nasogastric tube Lingual plate indications
Lingual plate indications Lingual plate rpd
Lingual plate rpd Major connectors
Major connectors Lumbar sympathectomy indications
Lumbar sympathectomy indications Victan supprimé
Victan supprimé Bugel prosthesis
Bugel prosthesis Indication of lma
Indication of lma Cardioversion indications
Cardioversion indications Types of hysterectomy pdf
Types of hysterectomy pdf Disadvantages
Disadvantages Periodontal healing
Periodontal healing Gravity dependent goniometer
Gravity dependent goniometer Miracle mix composition
Miracle mix composition Malek perio
Malek perio Fpd classification
Fpd classification Ecmo priming
Ecmo priming Embrasure clasps
Embrasure clasps Hanau's quint
Hanau's quint Ch 52 removable prosthodontics fill in the blank
Ch 52 removable prosthodontics fill in the blank Gtr indications
Gtr indications Indication of transfusion
Indication of transfusion Indications for blood transfusion in anemia
Indications for blood transfusion in anemia Indication of transfusion
Indication of transfusion Indications for blood transfusion in anemia
Indications for blood transfusion in anemia Cardioversion indications
Cardioversion indications Altered cast technique rpd
Altered cast technique rpd Axial wall crown prep
Axial wall crown prep Sniffing position for intubation
Sniffing position for intubation Modified arrowhead clasp
Modified arrowhead clasp Indications for abg analysis
Indications for abg analysis Doferilide
Doferilide Icd indications
Icd indications Cryoprecipetate
Cryoprecipetate Cryopercipitate
Cryopercipitate Sam pelvic sling indications
Sam pelvic sling indications Indication of serial extraction
Indication of serial extraction Subtractive osseous surgery
Subtractive osseous surgery Non anatomic teeth indications
Non anatomic teeth indications Contraindications of colostomy
Contraindications of colostomy Indications for platelet transfusion
Indications for platelet transfusion Icd indications
Icd indications Onlay indications and contraindications
Onlay indications and contraindications Contraindications of mwd
Contraindications of mwd Indication for mechanical ventilation
Indication for mechanical ventilation Mechanical ventilation indications
Mechanical ventilation indications Indications for tracheostomy
Indications for tracheostomy Indications of chemical reaction
Indications of chemical reaction Icd indications
Icd indications Contraindications of extraction
Contraindications of extraction Absolute contraindication for extraction
Absolute contraindication for extraction Indications for artificial airway
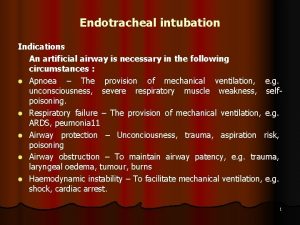
Indications for artificial airway Whats a cpm machine
Whats a cpm machine Mechanical ventilation indications
Mechanical ventilation indications Vitamin a indications
Vitamin a indications Passive movement principles
Passive movement principles Mri knee medicare
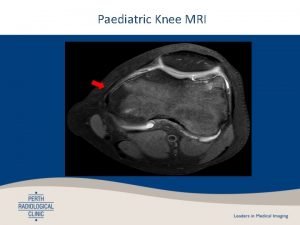
Mri knee medicare Indications of occlusal radiography
Indications of occlusal radiography Lumbar sympathectomy indications
Lumbar sympathectomy indications Composite indications
Composite indications Indications and appellations of origin
Indications and appellations of origin Thioeva indications
Thioeva indications Paladai feeding
Paladai feeding Tiva
Tiva Fluidotherapy indications
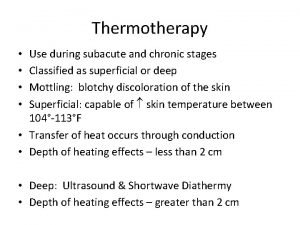
Fluidotherapy indications Resin
Resin Sunnyfield transfer belt
Sunnyfield transfer belt Indications for prostatectomy
Indications for prostatectomy Dip wrap method paraffin
Dip wrap method paraffin Lingual non occlusion
Lingual non occlusion Interim partial dentures
Interim partial dentures Best impression material for partial dentures
Best impression material for partial dentures Tooth borne passive appliance
Tooth borne passive appliance Fiksasi eksternal fraktur
Fiksasi eksternal fraktur Indications for prostatectomy
Indications for prostatectomy Aprv
Aprv Thumb spica cast indications
Thumb spica cast indications Normal range of blood sugar
Normal range of blood sugar Uvr dosage calculation
Uvr dosage calculation Platelet transfusion goals
Platelet transfusion goals Undisplaced flap
Undisplaced flap Tissue conditioner material
Tissue conditioner material