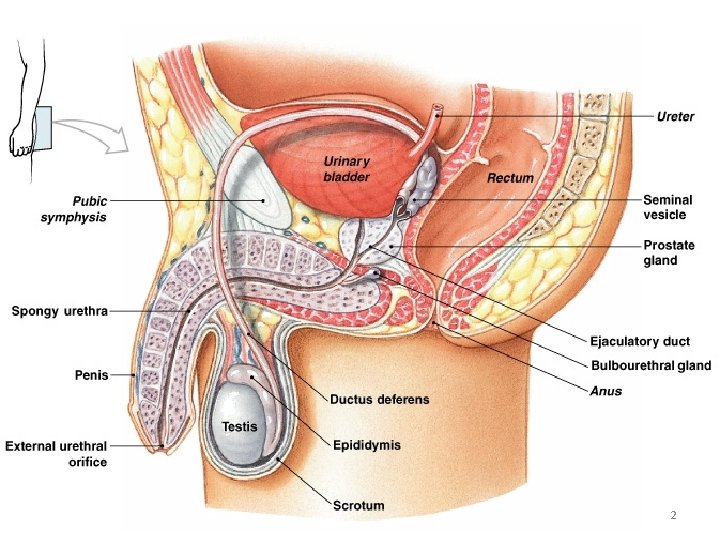
Prostate 1 2 3 4 5 Prostate Functions
- Slides: 34
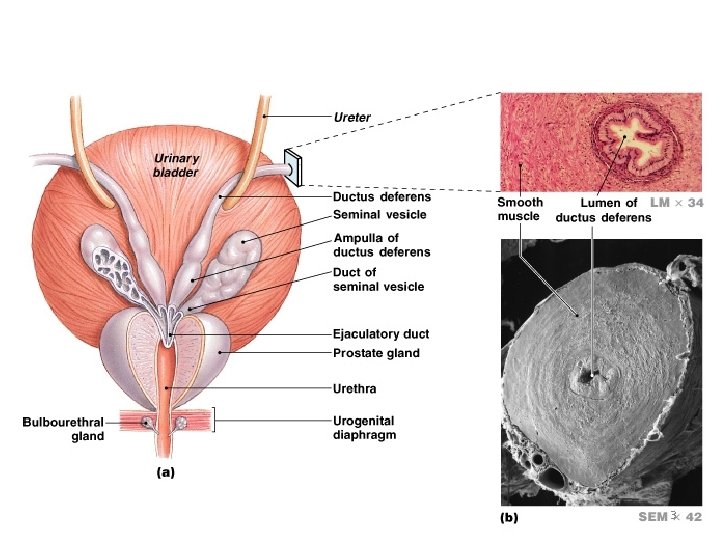
Prostate 1
2
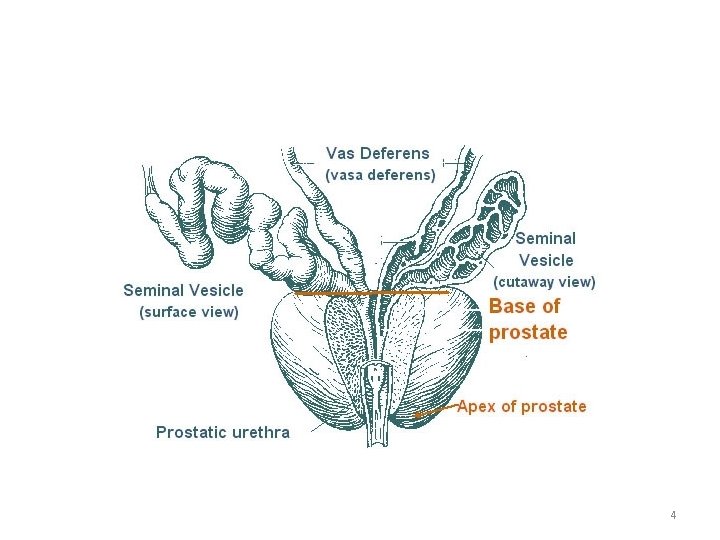
3
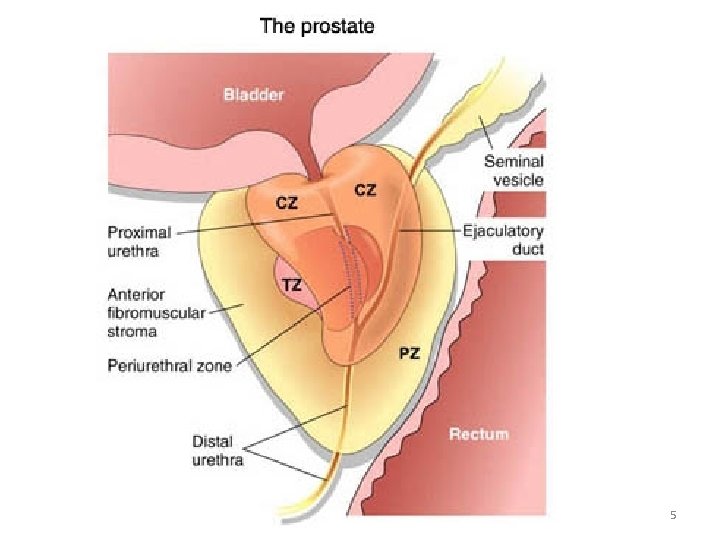
4
5
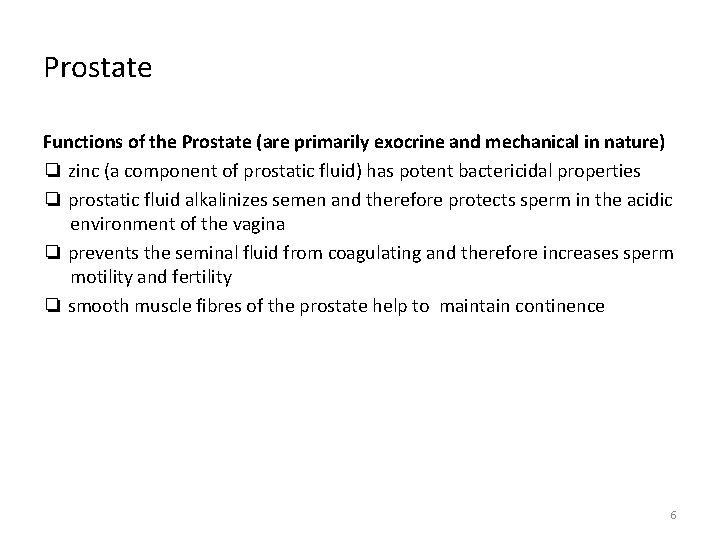
Prostate Functions of the Prostate (are primarily exocrine and mechanical in nature) ❏ zinc (a component of prostatic fluid) has potent bactericidal properties ❏ prostatic fluid alkalinizes semen and therefore protects sperm in the acidic environment of the vagina ❏ prevents the seminal fluid from coagulating and therefore increases sperm motility and fertility ❏ smooth muscle fibres of the prostate help to maintain continence 6
Benign Prostatic Hyperplasia Dr. Santosh Jha TMU
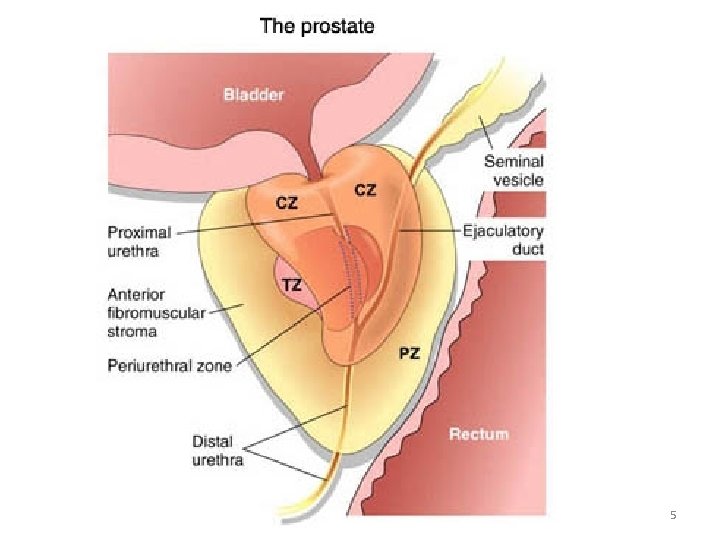
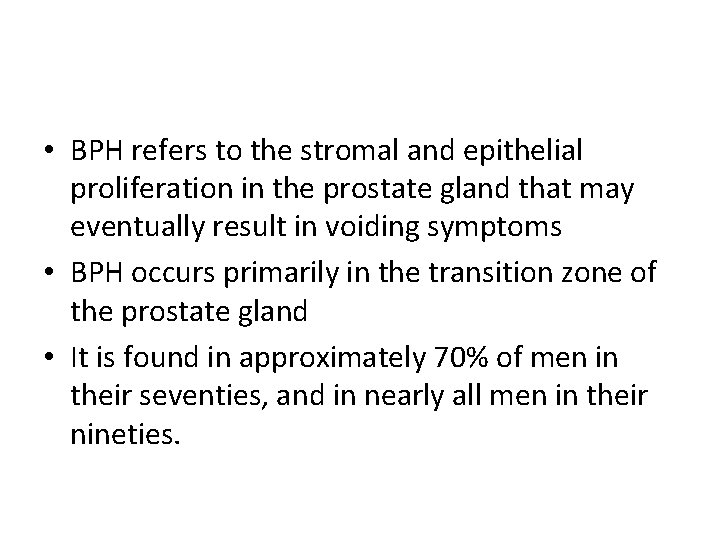
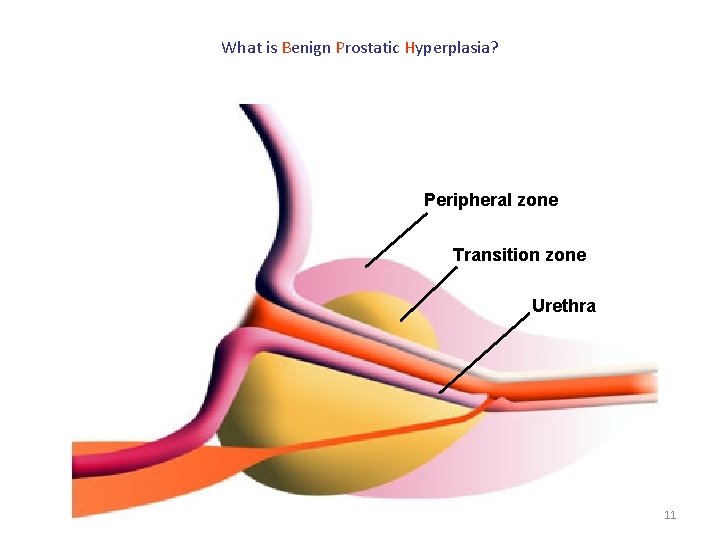
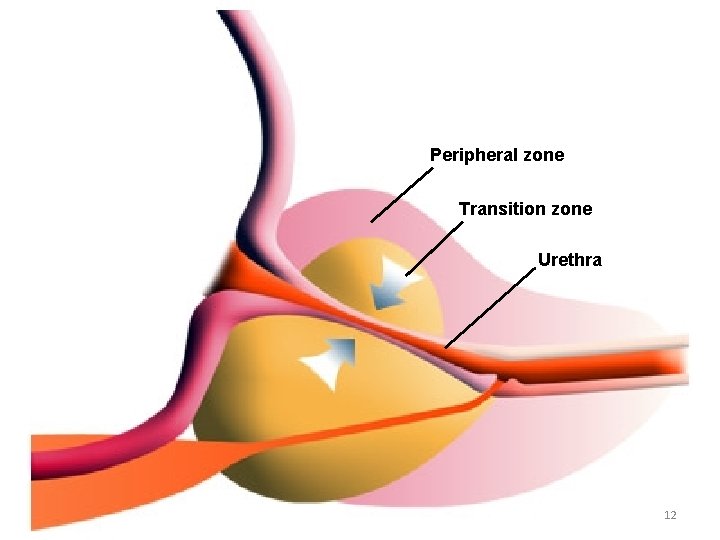
• BPH refers to the stromal and epithelial proliferation in the prostate gland that may eventually result in voiding symptoms • BPH occurs primarily in the transition zone of the prostate gland • It is found in approximately 70% of men in their seventies, and in nearly all men in their nineties.
Natural History • Patients with BPH can present with both obstructive and irritative voiding symptoms, which are often referred to collectively as lower urinary tract symptoms (LUTS). • Patients may complain of a decreased urinary stream, frequency, nocturia, urgency, hesitancy, intermittency, and a sense of incomplete emptying
n The size of prostate enlarged microscopically since the age of 40. Half of all men over the age of 60 will develop an enlarged prostate n By the time men reach their 70’s and 80’s, 80% will experience urinary symptoms But only 25% of men aged 80 will be receiving BPH treatment 10
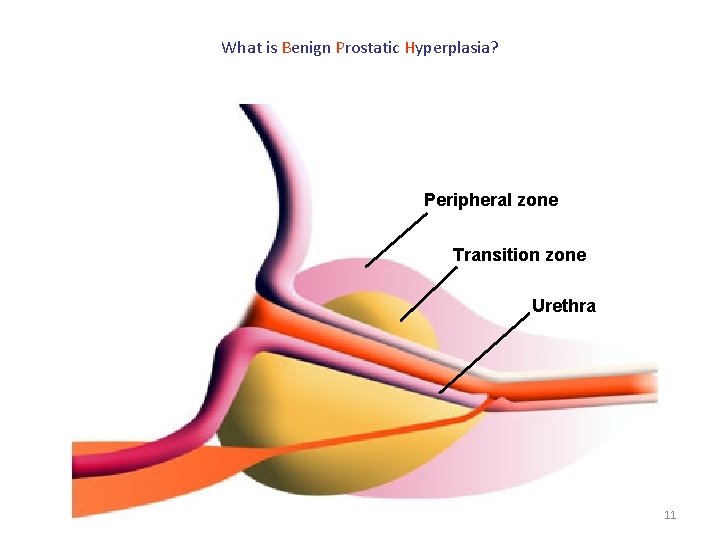
What is Benign Prostatic Hyperplasia? Peripheral zone Transition zone Urethra 11
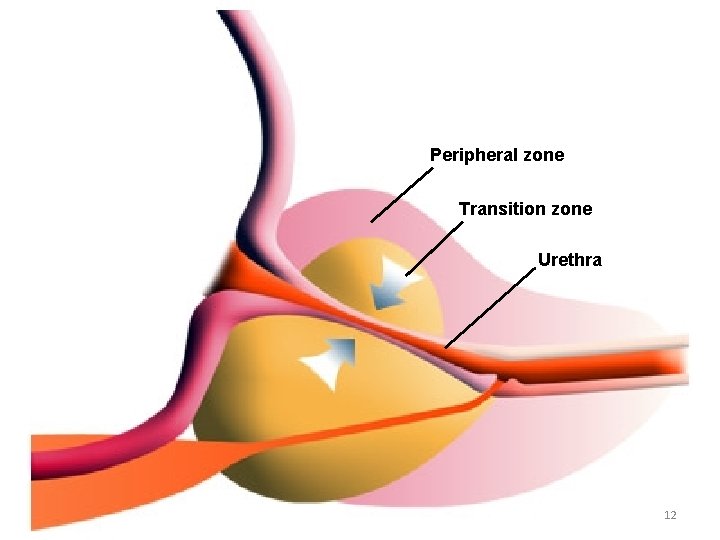
Peripheral zone Transition zone Urethra 12
BPH is part of the natural aging process, like getting gray hair or wearing glasses • BPH cannot be prevented • BPH can be treated • 13
Aetiology • Still not established properly • The hormone theory – Dihydrotestosterone – Imbalance between androgen & oestrogen 14
Pathology • Overgrowth of the glandular elements & overgrowth of connective tissue elements 15
Clinical features • • • Hesitancy Dysuria Frequency: initially mostly nocturnal Urgency Haematuria Pain: due to: – Cystitis – Acute retention – Hydronephrosis • Retention of urine: acuter or chronic • Renal failure • Prostatism: LUTS 16
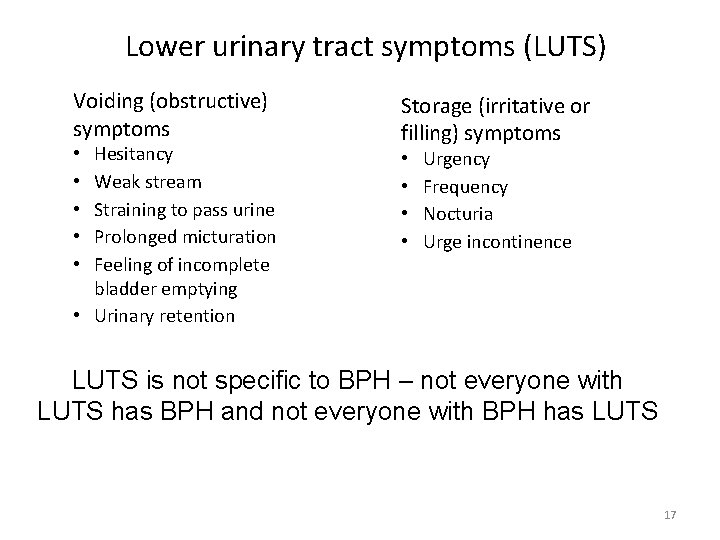
Lower urinary tract symptoms (LUTS) Voiding (obstructive) symptoms Hesitancy Weak stream Straining to pass urine Prolonged micturation Feeling of incomplete bladder emptying • Urinary retention • • • Storage (irritative or filling) symptoms • • Urgency Frequency Nocturia Urge incontinence LUTS is not specific to BPH – not everyone with LUTS has BPH and not everyone with BPH has LUTS 17
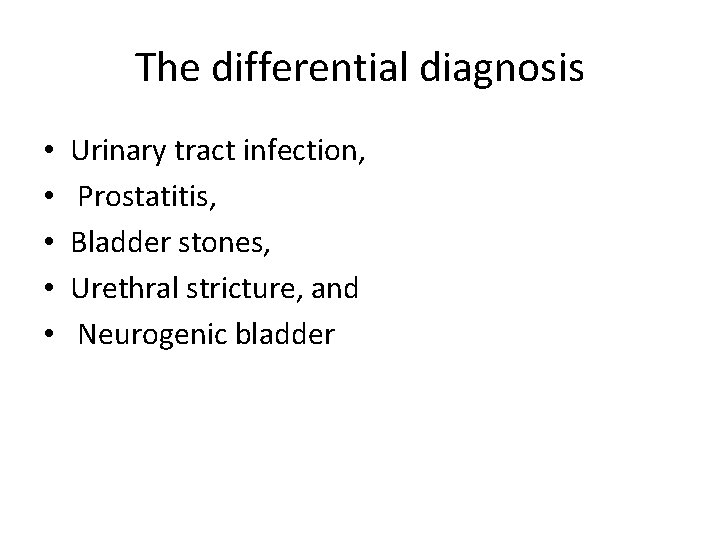
The differential diagnosis • • • Urinary tract infection, Prostatitis, Bladder stones, Urethral stricture, and Neurogenic bladder
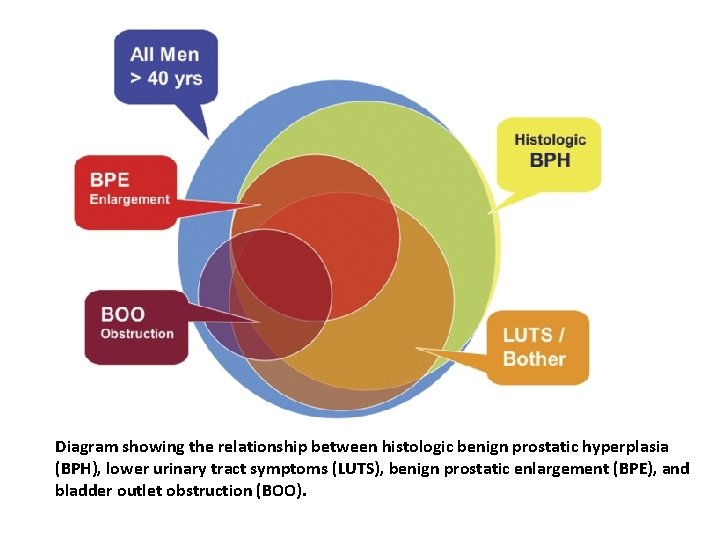
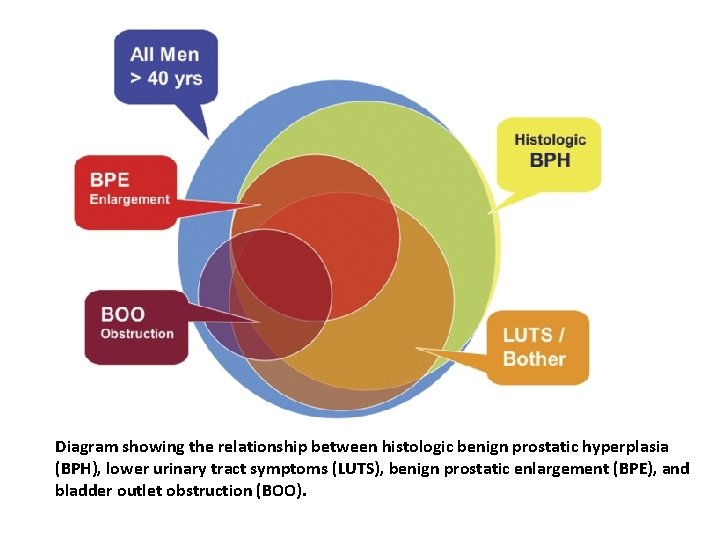
Diagram showing the relationship between histologic benign prostatic hyperplasia (BPH), lower urinary tract symptoms (LUTS), benign prostatic enlargement (BPE), and bladder outlet obstruction (BOO).
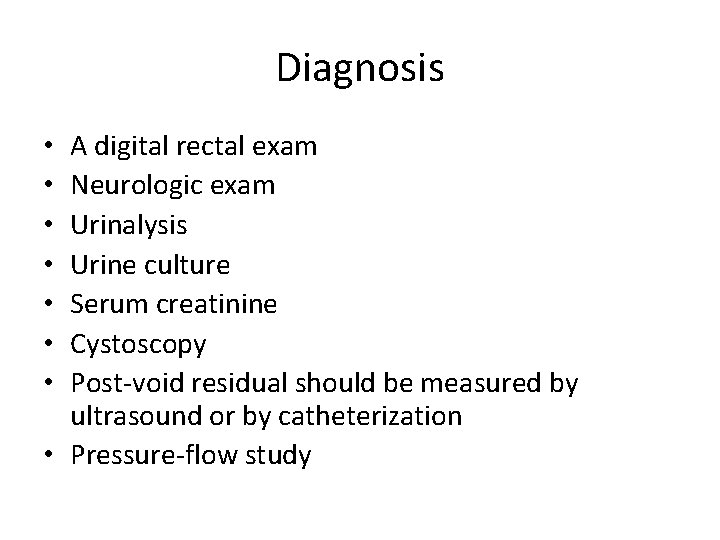
Diagnosis A digital rectal exam Neurologic exam Urinalysis Urine culture Serum creatinine Cystoscopy Post-void residual should be measured by ultrasound or by catheterization • Pressure-flow study • •
Treatment BPH needs to be treated ONLY IF: n Symptoms are severe enough to bother the patient and affect his quality of life n Complications related to BPH 22
Treatment options n Watchful waiting n Medication n Surgical approaches Minimal invasive n. TURP n. Invasive “open” procedures n 23
watchful waiting” “ n For mild symptoms. follow up 1 to 2 times yearly n Offer suggestions that help reduce symptoms n Avoid caffeine and alcohol n Avoid decongestants and antihistamines 24
Medical Therapy • Absolute indications for treatment include urinary retention, bladder stones, upper tract dilation, and renal failure. • Relative indications for treatment include large postvoid residuals, hematuria, and recurrent urinary tract infections. • The first line therapy for BPH is an alpha blocker(terazosin, doxazosin, and tamsulosin) • Patients in urinary retention require emergent catheterization and the catheter should be left in place for at least 24 hours • Other common medical therapies for BPH include saw palmetto and finasteride
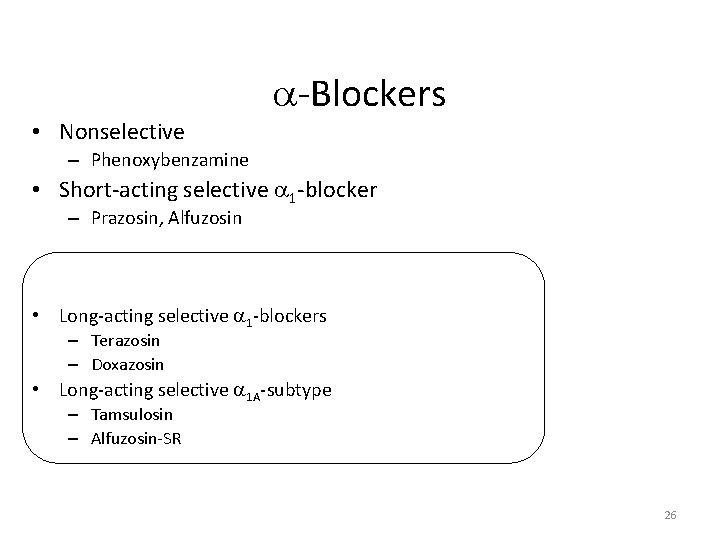
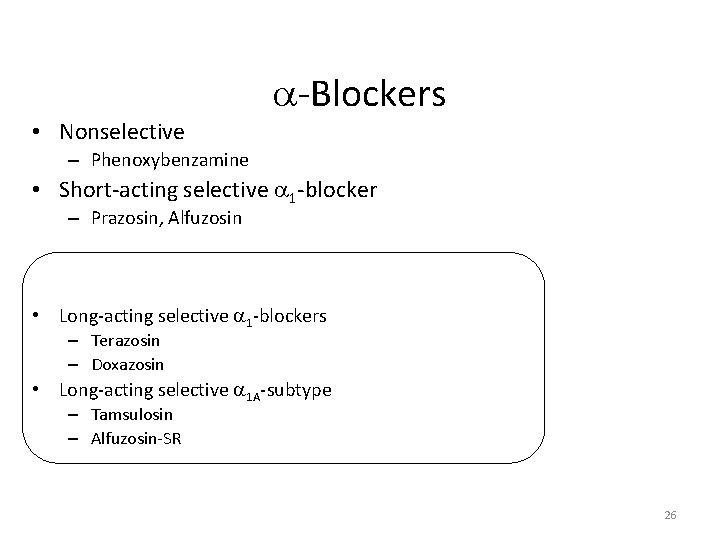
-Blockers • Nonselective – Phenoxybenzamine • Short-acting selective 1 -blocker – Prazosin, Alfuzosin • Long-acting selective 1 -blockers – Terazosin – Doxazosin • Long-acting selective 1 A-subtype – Tamsulosin – Alfuzosin-SR 26
Surgical Management Indications • upper tract dilation, • renal insufficiency secondary to BPH, or • If the prostate gland is greater than 80 to 100 g, an open prostatectomy should be performed) • The standard endoscopic procedure for BPH is a transurethral resection (TUR) of the prostate ØAcute urinary retention ØGross hematuria ØFrequent UTI ØVesical stone ØBPH related hydronephrosis or renal function deterioration
Conventional Surgical Therapy • Transurethral resection of the prostate (TURP) • Open simple prostatectomy 28
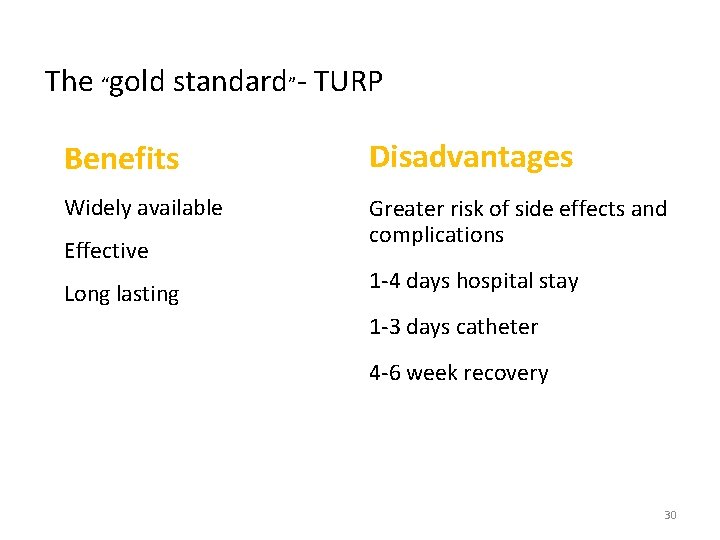
TURP • “Gold standard” of surgical treatment for BPH • 80~90% obstructive symptom improved • 30% irritative symptom improved • Low mortality rate 0. 2% 29
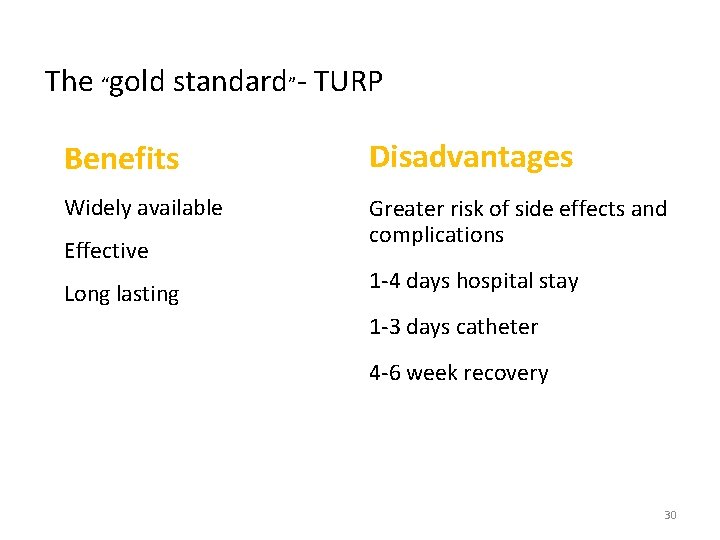
The “gold standard”- TURP Benefits Disadvantages Widely available Greater risk of side effects and complications Effective Long lasting 1 -4 days hospital stay 1 -3 days catheter 4 -6 week recovery 30
Complication of TURP • Immediate complication bleeding capsular perforation with fluid extravasation TUR syndrome • Late complication urethral stricture bladder neck contracture (BNC) retrograde ejaculation impotence (5 -10%) incontinence (0. 1%) 31
TUR syndrome • TUR is performed with a non-hemolytic fluid such as 1. 5% glycine (not Saline) • TUR syndrome may develop from the resulting hypervolemia and dilutional hyponatremia. • Patients with TUR syndrome may experience hypertension, bradycardia, nausea, vomiting, visual disturbance, mental status changes, and even seizures. • Occurs in approximately 2% of patients
Minimally invasive therapy for BPH • • • transurethral balloon dilatation of the prostate (TUBDP) transurethral incision of the prostate (TUI) intraprostatic stent transurethral microwave thermotherapy (TUMT) transurethral needle ablation of the prostate (TUNA) transurethral electrovaporization of the prostate (TUVP) photoselective vaporization of the prostate (PVP), Cryotherapy Transurethral ethanol ablation of the prostate (TEAP), 33
Minimally invasive therapy for BPH • • transurethral laser-induced prostatectomy (TULIP) visual laser ablation of the prostate (VLAP) contact laser prostatectomy (CLP) interstitial laser coagulation of the prostate (ILC) holmium: YAG laser resection of the prostate (Ho. LRP) holmium: YAG laser enucleation of the prostate (Ho. LEP) high-intensity focused ultrasound (HIFU) coagulation botulinum toxin-A injection of the prostate 34