Vitamins Deficiencies Toxicities Vitamins Organic molecules needed in
- Slides: 76
Vitamins Deficiencies & Toxicities
Vitamins Organic molecules needed in small quantities for normal metabolism and other biochemical functions, such as growth or repair of tissue n Attach to enzymes or coenzymes and help them activate anabolic (tissuebuilding) processes n
Vitamins Essential part of enzymatic reactions n Natural sources from both plants and animals n Insufficient amounts result in various deficiencies n
Vitamins (cont'd) Vitamin K and vitamin B complex vitamins obtained by synthesis in the small intestine n Vitamin D can be synthesized by the skin when exposed to sunlight n
Water-Soluble Vitamins B-complex group and vitamin C n Can be dissolved in water n Cannot be stored by the body in large amounts n Daily intake required to prevent deficiencies n
Fat-Soluble Vitamins A, D, E, K n Present in both plant and animal foods n Stored in the liver and fatty tissues n Daily intake not required n
Fat-Soluble Vitamins (cont'd) Deficiency occurs only after prolonged deprivation n Can become toxic if excessive amounts are consumed n
Vitamins: Other Issues Nutrient mega dosing n Toxic hypervitaminosis n
Vitamin A Fat soluble n Vitamin A (retinol) derived from animal fats (butter and milk), eggs, meat, liver, fish liver oils n The vitamin A in animal tissues is derived from carotenes, which are found in plants (green and yellow vegetables and yellow fruits) n
Vitamin A Required for growth and development of bones and teeth n Necessary for other processes n – Reproduction – Integrity of mucosal and epithelial surfaces – Cholesterol and steroid synthesis – Essential for night vision
Vitamin A: Deficiency states Hyperkeratosis of the skin n Night blindness n Skin conditions n – Acne, psoriasis, keratosis follicularis
Vitamin A: Toxicity n Ingestion of excessive amounts causes toxicity – Irritability, drowsiness, vertigo, delirium, other symptoms – Increased intracranial pressure in infants – Generalized peeling of the skin and erythema over several weeks
DIAGNOSIS n Abnormalities of dark adaptation are strongly suggestive of vitamin deficiency. Serum level below the normal range of 30 -65 mg/dl are commonly seen in advance deficiency.
TREATMENT Orally: DOSE 30, 000 iu of vit A daily for 1 week. n Advance deficiency with corneal damage -20, 000 ius/kg orally for 5 days. n
Vitamin D Fat soluble n “Sunshine vitamin” n Responsible for proper utilization of calcium and phosphorus n Actually a group of analog steroid chemicals n
Vitamin D (Fat Soluble) Different chemicals, produce same effect n Vitamin D 2 (ergocalciferol) n – Plant vitamin D – Obtained through dietary sources n Vitamin D 3 (cholecalciferol) – Produced in the skin by ultraviolet irradiation (sunshine)
Vitamin D (cont'd) n Vitamin D 2 -containing foods – Fish oils, salmon, sardines, herring – Fortified milk, breads, cereals – Animal livers, tuna fish, eggs, butter n Endogenous synthesis in the skin
Vitamin D: Function Regulates absorption of and use of calcium and phosphorus n Necessary for normal calcification of bone and teeth n
Vitamin D: Indications Dietary supplement n Treatment of vitamin D deficiency n Treatment and correction of conditions related to long-term deficiency: rickets, tetany, osteomalacia n Prevention of osteoporosis n
Vitamin D: Deficiency States n n n Vitamin D deficiency generally results from an inadequate dietary intake of vitamin D, or too little exposure to sunlight. The vitamin D deficiency has also been found to occur in overcrowded urban areas. The absence of sunlight or smog limitations inhibit the absorption of the D vitamin.
Vitamin D: Toxicity n Long-term ingestion of excessive amounts causes toxicity – Hypertension, weakness, fatigue, headache, many others – GI tract effects – CNS effects
Forms of Vitamin D calcifediol n calcitriol n dihydrotachysterol n ergocalciferol n
DIAGNOSIS Serum 25(OH)D and PTH level. n Alkaline phosphatase level elevated. n Serum calcium and phosphate low. n Treatment n 250 -1000 microgram daily for 3 -4 month, than decrease the dose 10 -20 microgram or stop therapy. n
Vitamin E Fat soluble n Tocopherols n Dietary plant sources n – Fruits, grains, cereals, vegetables, oils, wheat germ n Animal sources – Eggs, chicken, meats, fish
Vitamin E: Function Exact biologic function of vitamin E is unknown n Believed to act as an antioxidant n
Vitamin E: Deficiencies n n The Vitamin E deficiency is commonly found in infants and usually results from them having consumed formulas high in polyunsaturated fatty acids that are fortified with iron but not vitamin E. Also, because vitamin E is a fat-soluble vitamin, a deficiency also develops in conditions associated with fat malabsorption, such as cystic fibrosis.
Vitamin E: Indications Dietary supplement n Antioxidant n Treatment of deficiency n – Highest risk of deficiency in premature infants
Diagnosis n Plasma vitamin E levels can be measured; normal levels are 0. 5– 0. 7 mg/d. L or higher. Since vitamin E is normally transported in lipoproteins, the serum level should be interpreted in relation to circulating lipids.
Treatment n The potential antioxidant benefits of vitamin E can be achieved with supplements of 100– 400 IU/d.
Vitamin K Fat soluble n Three types: K 1, K 2, K 3 n Dietary sources of K 1 n – Green leafy vegetables (cabbage, spinach), meats, milk n Vitamin K 2 synthesized by intestinal flora
Vitamin K: Functions Essential for synthesis of blood coagulation factors in the liver n Vitamin K–dependent clotting factors n – II – VII – IX –X
Vitamin K: Indications Dietary supplementation n Treatment of deficiency states (rare) n – Antibiotic therapy – Newborn infants – Malabsorption n Reverse the effects of certain anticoagulants (warfarin)
Vitamin K: Deficiencies n n The Vitamin K deficiency is commonly found among newborns within the first few days postpartum. Poor placental transfer of vitamin K to the infant and also inadequate production of vitamin K-producing intestinal flora is the main culprit. The deficiency can also be caused by a prolonged use of drugs, such as antibiotics that destroy normal intestinal bacteria. Additionally, other causes are a decreased bile flow to the small intestine from bile duct obstruction, a malabsorption of vitamin K due to bowel resection, ulcerative colitis, or chronic hepatic disease. The vitamin K deficiency seldom results from an insufficient dietary intake of it.
Laboratory Findings n The prothrombin time (PT) is prolonged to a greater extent than the PTT, and with mild vitamin K deficiency only the PT is defective. Fibrinogen level, thrombin time, and platelet count are not affected.
Treatment n Vitamin K deficiency responds rapidly to subcutaneous vitamin K, and a single dose of 15 mg will completely correct laboratory abnormalities in 12– 24 hours.
Water-Soluble Vitamins n Vitamin B complex – thiamine (B 1) – pyridoxine (B 6) – riboflavin (B 2) – folic acid (B 9) – niacin (B 3) – cyanocobalamin (B 12) – pantothenic acid (B 5) n Vitamin C – ascorbic acid
Water-Soluble Vitamins (cont'd) Can dissolve in water n Excessive amounts excreted in the urine, not stored in the body n Toxic reactions are very rare n
Vitamin B 1 (Thiamine) Water soluble n Food sources n – Whole grains, liver, beans n Deficiencies – Beriberi – Wernicke’s encephalopathy
Vitamin B 1 (Thiamine) Deficiencies n Beriberi – Brain lesions, polyneuropathy of peripheral nerves, serous effusions, cardiac anatomic changes n Wernicke’s encephalopathy – Cerebral beri
Vitamin B 1 (Thiamine): Causes of Deficiencies Poor diet n Extended fever n Hyperthyroidism n Liver disease n Alcoholism n Malabsorption n Pregnancy and breast-feeding n
Vitamin B 1 (Thiamine) Functions n Essential for: – Carbohydrate metabolism – Many metabolic pathways, including Krebs’ cycle n Maintains integrity of: – Peripheral nervous system – Cardiovascular system – GI tract
Diagnosis Erythrocyte transketolase activity. Coefficient greater than 15 -20% suggest thiamine deficiency. n Urinary thiamine excretion. n
Vitamin B 1 (Thiamine): Indications n Treatment of thiamine deficiency – Beriberi – Wernicke’s encephalopathy – Peripheral neuritis associated with pellagra n Metabolic disorders
Vitamin B 1 (Thiamine): Indications (cont'd) n Dietary supplement – Malabsorption induced by alcoholism, cirrhosis, GI disease n Thiamine deficiency is treated with large parental doses of thiamine. 50100 mg/d. All patients should simultaneously receive therapeutic doses of other water soluble vitamins Other uses
Vitamin B 2 (Riboflavin) Water soluble n Food sources n – Leafy green vegetables – Eggs – Nuts – Meats – Yeast
Vitamin B 2 (Riboflavin) Causes of Deficiency Alcoholism is a major cause n Deficiency also caused by: n – Intestinal malabsorption – Long-term infections – Liver disease – Malignancy – Probenecid therapy
Vitamin B 2 (Riboflavin) Functions Converted into enzymes essential for tissue respiration n Required to activate vitamin B 6 (pyridoxine) n Converts tryptophan into niacin n Maintains erythrocyte integrity n
Vitamin B 2 (Riboflavin) Deficiency n Deficiency results in: – Cutaneous, oral, and corneal changes – Cheilosis – Seborrheic dermatitis – Keratitis
Vitamin B 2 (Riboflavin): Indications Dietary supplement n Treatment of deficiency n Microcytic anemia n Acne n Migraine headaches n Many other uses n
Vitamin B 2 (Riboflavin): Side Effects No side effects or toxic effects n Large doses will discolor urine to a yellow-orange n
Vitamin B 3 (Niacin) Water soluble n Food sources n – Meats, beans, liver, yeast, wheat n Also synthesized from tryptophan (an essential amino acid obtained from protein digestion)
Vitamin B 3 (Niacin): Functions Once ingested, converted to nicotinamide n Nicotinamide is converted to two coenzymes n These enzymes are required for: n – Glycogenolysis, tissue respiration – Lipid, protein, and purine metabolism
Vitamin B 3 (Niacin): Indications n Antihyperlipidemic agent – Lowers serum cholesterol and triglyceride levels by reducing VLDL synthesis – Doses required for this effect are higher than those required for its nutritional and metabolic effects
Vitamin B 3 (Niacin): Deficiency n Pellagra: niacin deficiency – Mental: various psychotic symptoms – Neurologic: neurasthenic syndrome – Cutaneous: crusting, erythema – Mucous membrane: oral, vaginal, and urethral lesions – GI: diarrhea or bloody diarrhea
Vitamin B 3 (Niacin): Side Effects n Side effects seen when higher doses are used in the treatment of hyperlipidemia – Flushing – Pruritus – GI distress
Vitamin B 6 (Pyridoxine) Water soluble n Sources n – Whole grains, wheat germ, nuts, yeast – Fish and organ meats
Vitamin B 6 (Pyridoxine) (cont'd) n Composed of three compounds – Pyridoxine – Pyridoxal – Pyridoxamine
Vitamin B 6 (Pyridoxine): Function n Necessary for many metabolic functions – Protein, lipid, and carbohydrate utilization – Conversion of tryptophan to niacin n Necessary for integrity of peripheral nerves, skin, mucous membranes, hematopoietic system
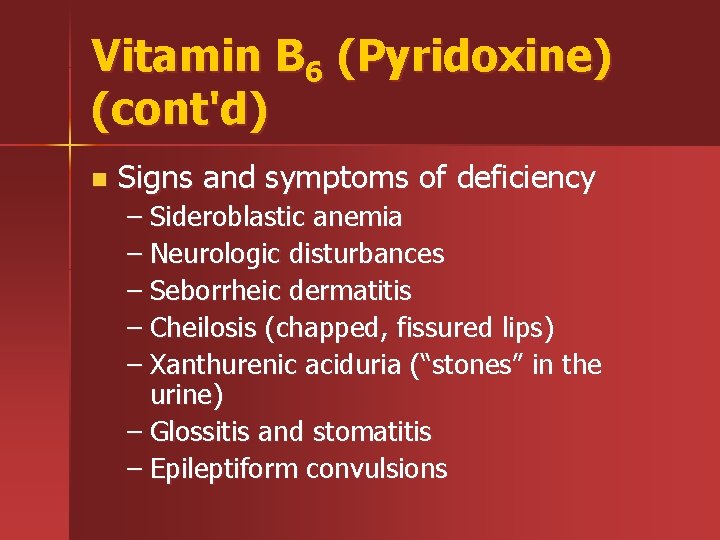
Vitamin B 6 (Pyridoxine) (cont'd) n Signs and symptoms of deficiency – Sideroblastic anemia – Neurologic disturbances – Seborrheic dermatitis – Cheilosis (chapped, fissured lips) – Xanthurenic aciduria (“stones” in the urine) – Glossitis and stomatitis – Epileptiform convulsions
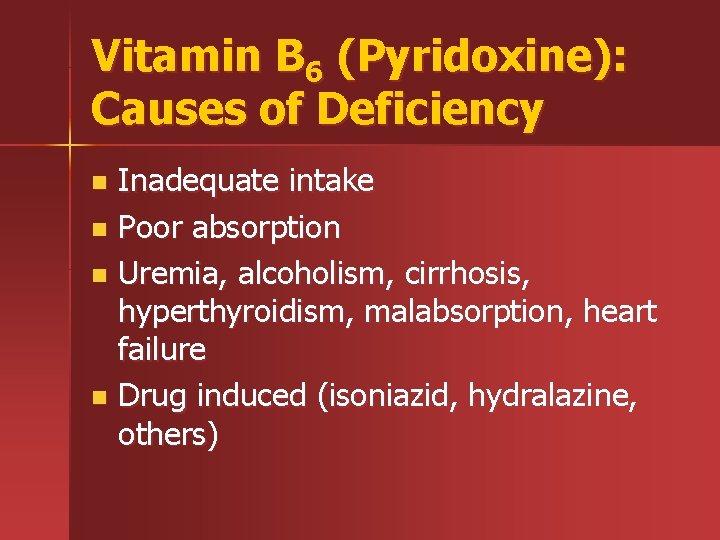
Vitamin B 6 (Pyridoxine): Causes of Deficiency Inadequate intake n Poor absorption n Uremia, alcoholism, cirrhosis, hyperthyroidism, malabsorption, heart failure n Drug induced (isoniazid, hydralazine, others) n
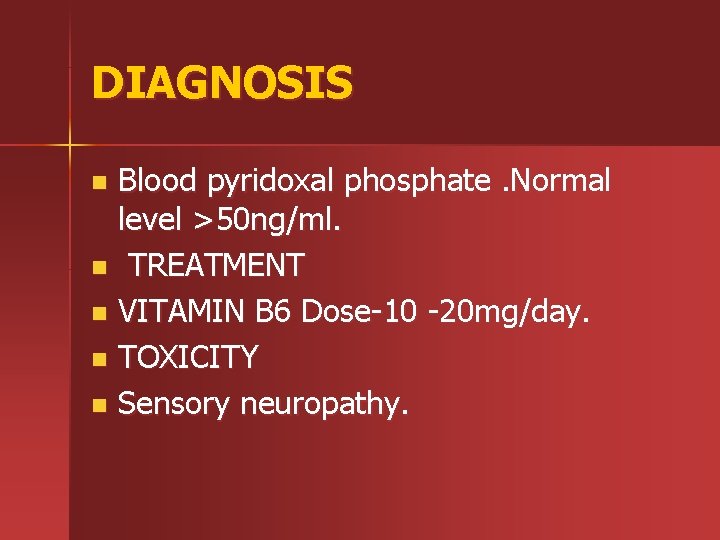
DIAGNOSIS Blood pyridoxal phosphate. Normal level >50 ng/ml. n TREATMENT n VITAMIN B 6 Dose-10 -20 mg/day. n TOXICITY n Sensory neuropathy. n
Vitamin B 6 (Pyridoxine) Toxicity Toxic effects occur with large doses, especially neurotoxicity
Vitamin B 12 (Cyanocobalamin) Water soluble n Synthesized by microorganisms present in the body n Food sources n – Liver, kidney, fish, shellfish, meat, dairy foods n Contained in minimal amounts in plants
General Considerations n Vitamin B 12 belongs to the family of cobalamins and serves as a cofactor for two important reactions in humans. As methylcobalamin, it is a cofactor for methionine synthetase in the conversion of homocysteine to methionine, and as adenosylcobalamin for the conversion of methylmalonyl-coenzyme A (Co. A) to succinyl. Co. A. All vitamin B 12 comes from the diet and is present in all foods of animal origin. The daily absorption of vitamin B 12 is 5 mcg.
Vitamin B 12 (Cyanocobalamin): Function n Required for many metabolic pathways – Fat and carbohydrate metabolism – Protein synthesis – Growth, cell replication – Hematopoiesis – Nucleoprotein and myelin synthesis
Vitamin B 12 (Cyanocobalamin): Deficiency n Deficiency leads to: – Neurologic damage – Pernicious anemia n Deficiency states caused by: – Malabsorption – Poor dietary intake (vegetarians)
Vitamin B 12 (Cyanocobalamin): Oral Absorption Oral absorption of vitamin B 12 (extrinsic factor) required presence of the intrinsic factor n The intrinsic factor is a glycoprotein secreted from the gastric parietal cells n
Vitamin B 12 (Cyanocobalamin): Oral Absorption (cont'd) The extrinsic and intrinsic factors form a complex that is then absorbed by the intestines
Treatment n n Intramuscular injections of 100 mcg of vitamin B 12 are adequate for each dose. Replacement is usually given daily for the first week, weekly for the first month, and then monthly for life. It is a lifelong disorder, and if patients discontinue their monthly therapy the vitamin deficiency will recur. Oral cobalamin The dose is 1000 mcg/d and must be continued indefinitely. Patients respond to therapy with an immediate improvement in their sense of well-being. A brisk reticulocytosis occurs in 5– 7 days, and the hematologic picture normalizes in 2 months. Central nervous system symptoms and signs are reversible if they are of relatively short duration (less than 6 months) but become permanent if treatment is not initiated promptly.
Vitamin C (Ascorbic Acid) Water soluble n Natural sources n – Citrus fruits and juices – Tomatoes – Cabbage – Cherries – Liver n Can also be synthesized
Vitamin C (Ascorbic Acid): Functions Acts in oxidation-reduction reactions n Required for several metabolic activities n – Collagen synthesis – Maintenance of connective tissue – Tissue repair – Maintenance of bone, teeth, and capillaries – Folic acid metabolism – Erythropoiesis
Vitamin C (Ascorbic Acid): Functions (cont'd) Enhances absorption of iron n Required for the synthesis of: n – Lipids – Proteins – Steroids Aids in cellular respiration n Aids in resistance to infections n
Vitamin C (Ascorbic Acid): Deficiency n Prolonged deficiency results in scurvy – Gingivitis and bleeding gums – Loss of teeth – Anemia – Subcutaneous hemorrhage – Bone lesions – Delayed healing of soft tissues and bones
DIAGNOSIS Diagnose on clinical ground. n Ascorbic acid level below 0. 1 mg/dl. n
TREATMENT n n 300 -1000 mg/d of ascorbic acid. Response occurs within days. High intake decrease the risk of cancer, also protect from against coronary heart disease. TOXICITY High doses cause gastric irritation, flatulence, or diarrhea. it may also causes false negative test for faecal occult blood and false positive and false negative test for urine glucose.
Vitamin C (Ascorbic Acid): Megadoses n Megadoses may cause: – Nausea, vomiting, headache, abdominal cramps – Acidified urine, with possible stone formation n Discontinuing megadoses may result in scurvy-like symptoms
 Organic molecules vs inorganic molecules
Organic molecules vs inorganic molecules Water soluble vitamins vs fat soluble vitamins
Water soluble vitamins vs fat soluble vitamins What is individual psychology
What is individual psychology Safeguarding tendencies withdrawal
Safeguarding tendencies withdrawal Celiac beri beri
Celiac beri beri Where are vitamins absorbed
Where are vitamins absorbed Vitamins classification chart
Vitamins classification chart Hemoragea
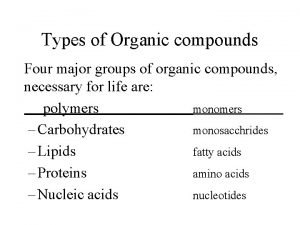
Hemoragea The four types of organic molecules
The four types of organic molecules Ch4o organic or inorganic
Ch4o organic or inorganic Biochemistry
Biochemistry Water soluble vitamins characteristics
Water soluble vitamins characteristics Objectives of vitamins
Objectives of vitamins Water soluble vitamins
Water soluble vitamins Biochemical function of vitamin a
Biochemical function of vitamin a Vital amine
Vital amine Vitamins part1
Vitamins part1 Characteristics of vitamins
Characteristics of vitamins Different forms of vitamin a
Different forms of vitamin a Digestion vitamins
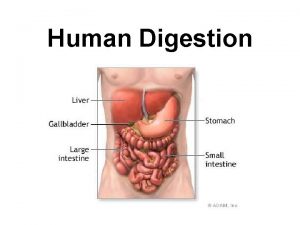
Digestion vitamins Vitamin deficiency diseases chart
Vitamin deficiency diseases chart Primitiv vitamins
Primitiv vitamins Types of vitamins
Types of vitamins Water soluble vitamins characteristics
Water soluble vitamins characteristics Adek vitamins water soluble
Adek vitamins water soluble The chef does everything but cook that's what wives are for
The chef does everything but cook that's what wives are for Prepare chart for vitamins and minerals
Prepare chart for vitamins and minerals When to take vitamins chart
When to take vitamins chart Vitamin classification
Vitamin classification Asea via
Asea via Chapter 8 vitamins and minerals
Chapter 8 vitamins and minerals Excess b vitamins urine
Excess b vitamins urine Vitamin examples
Vitamin examples Vitamins definition and classification
Vitamins definition and classification Prepare chart for vitamins and minerals
Prepare chart for vitamins and minerals Dairy produts
Dairy produts What are vitamins functions
What are vitamins functions Importance of vitamins
Importance of vitamins Echymosis
Echymosis Xerophthalmia stages
Xerophthalmia stages Categories of vitamins
Categories of vitamins Vitamins conclusion
Vitamins conclusion Do vitamins yield energy
Do vitamins yield energy Which statement concerning vitamins is incorrect
Which statement concerning vitamins is incorrect Vitamins definition
Vitamins definition List of macronutrients and micronutrients
List of macronutrients and micronutrients Site:slidetodoc.com
Site:slidetodoc.com Vitamins type
Vitamins type Water soluble vitamins
Water soluble vitamins Objectives of vitamins
Objectives of vitamins Keratomalacia
Keratomalacia Digestion refers to
Digestion refers to Characteristics of vitamins
Characteristics of vitamins Water soluble vitamins chart
Water soluble vitamins chart Categories of vitamins
Categories of vitamins Objectives of vitamins
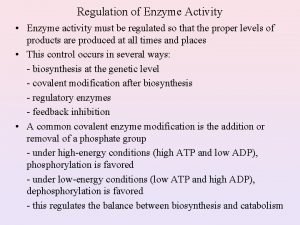
Objectives of vitamins Enzyme regulation
Enzyme regulation Carrotenosis
Carrotenosis Quasi vitamin b
Quasi vitamin b Fat soluble vitamins excretion
Fat soluble vitamins excretion When did nicholas novikov write the telegram
When did nicholas novikov write the telegram Number needed to harm
Number needed to harm Nnt calculation
Nnt calculation To clarify any discrepancies in the plans use a
To clarify any discrepancies in the plans use a A friend is never known till needed
A friend is never known till needed Magnetic disk
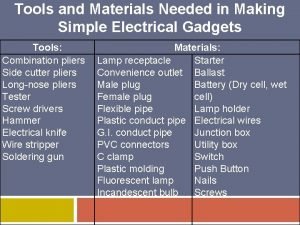
Magnetic disk Tools and materials needed in making electrical gadgets
Tools and materials needed in making electrical gadgets Assumptions of confidence interval
Assumptions of confidence interval Sources of waste
Sources of waste Number needed to harm
Number needed to harm Number need to treat
Number need to treat Needed complement
Needed complement Is atp needed for muscle contraction
Is atp needed for muscle contraction Purpose of business activity
Purpose of business activity My dentist says i need a crown i know right
My dentist says i need a crown i know right Tools utensils and equipment needed in egg preparation
Tools utensils and equipment needed in egg preparation Krebs cycle outputs
Krebs cycle outputs