RESECTIVE OSSEOUS SURGERY CONTENTS l l l l



- Slides: 44
RESECTIVE OSSEOUS SURGERY
CONTENTS l l l l l INTRODUCTION HISTORY RATIONALE OBJECTIVE & GOALS TERMINOLOGIES INDICATIONS AND CONTRAINDICATIONS EXAMINATION AND TREATMENT PLANNING SURGICAL CONSIDERATIONS INSTRUMENTS USED SURGICAL TECHNIQUE
l l WOUND HEALING CROWN LENGTHENING CAUSES OF FAILURE RESECTIVE OSSEOUS SURGERY CONCLUSION.
Resective osseous surgery l Osseous surgery can be defined as the procedure by which changes in the alveolar bone can be accomplished to rid it of deformities induced by the periodontal disease process or other related factors, such as exostosis and tooth supra eruption.
Osseous surgery can be either l l Additive surgery: - Subtractive osseous surgery Including procedures directed at restoring the alveolar bone to it’s original level.
l Subtractive osseous surgery : – Designed to restore the form of preexisting alveolar bone to the level existing at the time of surgery or slightly more apical to this level. These procedures provide an alternative to additive methods and should be resorted to when the latter is not feasible.
HISTORY l The removal of superficial radicular & interproximal alveolar crestal bone has been used for over a century in conjunction with treatment of periodontal disease. l The earlier rationale for osseous surgery (as outlined by Pierre Fauchard in 1776) was that the bone surface was considered infected or necrotic & had to be removed.
Many therapist in late 1880’s & early 1900’s including Robicsek, G. V. Black et al advocated gingivectomy with denudation of radicular & interproximal crestal bone followed by some osseous removal. l Newmann, Zentler et al also removed bone as they considered it necrotic. l
Tthe classic work by R. Kronfeld published in 1935 proved that all bone is healthy & therefore need not be removed. A classic article by S. Schluger in 1949 outlined the principles of osseous surgery for recontouring of bone in elimination of periodontal pockets.
RATIONALE l The major rationale for osseous resective surgery is based on fact that this discrepancies in level & shapes of the bone & gingiva predispose patients to recurrence of pocket depth post surgically (Easley J 1967)
OBJECTIVE l Is to present a sound and solid base for the gingiva to rest upon, without generating excessive sulcular depth. ( Prichard J 1961)
l To reshape the marginal bone to resemble that of alveolar process undamaged by periodontal disease. l Is to establish a periodontium that is cleansible by the patient’s own oral hygiene procedures.
NORMAL BONY MORPHOLOGY l Interproximal bone more coronal than labial or lingual/palatal bone & pyramidal in form. The form of interdental bone is a function of the tooth form & the embrasure width. l Tapered tooth – more pyramidal bony form. Wider embrasure – flattened interdental bone. l
Position of the bony margin mimics the contours of CEJ. l The scalloping of bone on facial and lingual/palatal side is related to tooth and root form as well as tooth position, within the alveolus. l l The molars have less scalloping and more flat profile than bicuspids & incisors.
TERMINOLOGY Procedures used to correct osseous defects can be classified as – Osteoplasty & Ostectomy
l Osteoplasty This term was introduced by Friedman (1955). - Refers to reshaping the bone without removing “tooth-Supporting bone”.
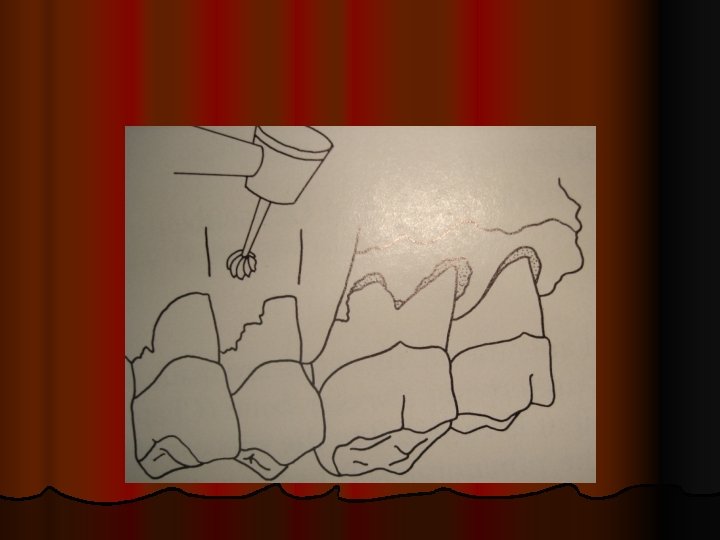
Much of osseous resection is osteoplastic. l It consists of thinning of the thick marginal ledges of bone and of establishing an undulating buccal contour by interradicular grooving. l The leveling of bony craters, the reduction of hemisepta, and the elimination of circumferential wells in bone sometimes require the cutting away of some supporting bone, but often are primarily osteoplastic procedures. l
l According to AAP’s 3 rd edition of glossary of Periodontal terms, It is reshaping of alveolar process to achieve a more physiological form without removal of supporting bone. l (Osteoplasty does not result in loss of attachment. )
Ostectomy : includes the removal of toothsupporting bone. l According to AAP’s 3 rd edition of glossary of Periodontal terms, Ostectomy is the excision of bone or portion of a bone. l

In periodontics, ostectomy is done to correct or reduce deformities caused by periodontitis in the marginal and intra-alveolar bone and includes the removal of supporting bone. Osteoplasty and ostectomy frequently are combined in practice. l Osteoplasty is usually performed with rotary instruments and the ostectomy with hand instruments. l
Supporting alveolar bone: is the bone that is directly involved in tooth support (alveolar bone proper) where the principal fibers of the periodontal ligament attach.
l Non supporting bone: is the alveolar bone not directly related to tooth support. (ie, bony exostoses, edentulous ridges, tori, flattened interdental contours and ledges)
OSTEOPLASTY INDICATIONS AND ENDPOINT l l l Buccal & lingual bony ledges. Shallow lingual or buccal intrabony defects. Thick interproximal areas. Incipient furcation involvements. Tori reduction Endpoint of osteoplasty used in conjunction with modified Widman flap or an apically positioned flap, is the enhancement of tissue placement & adaptation at the time of suturing. (Ramfjord S, Nissle R 1974)
OSTECTOMY INDICATIONS AND ENDPOINT Treat shallow (1 -2 mm deep) to medium (3 -4 mm deep) intrabony defects. l Hemiseptal osseous defects. l Correct reversals in the osseous topography. l Endpoint of ostectomy used in conjunction with apically positioned flap or a thinned palatal flap, is the elimination of an intrabony pocket. (Carranza FA 1956)
BASED ON MORPHOLOGICALLY DESCRIPTIVE TERMS: l Positive architecture: is the term used to describe the normal physiologic relationship of interdental and radicular bone heights. Radicular bone is apical to the interdental bone.
l Negative architecture: is the term used to describe any abnormal, non physiologic relationship of interdental and radicular bone heights. Interdental bone is more apical than the radicular bone.
l Flat architecture: Reduction of the interdental bone to the same height as the radicular bone. Ideal architecture: When the bone is consistently more coronal on the inter proximal surfaces than on the facial and lingual surfaces.


TERMS THAT RELATE TO THE THOROUGHNESS OF THE OSSEOUS RESHAPING TECHNIQUES l Definitive osseous reshaping: Implies that further osseous reshaping would not improve the overall results. l Compromise osseous reshaping: Indicates a bone pattern that cannot be improved without significant osseous removal that would be detrimental to the overall result.
INDICATIONS OF RESECTIVE OSSEOUS SURGERY l One walled angular defects. l Wide and shallow two wall defects. l Thick, bony margin. l Shallow crater formation.
ENDPOINTS OF OSSEOUS RESECTIVE SURGERY l Minimal probing depths and a gingival tissue morphology that enhances good self -performed oral hygiene and periodontal health
CONTRA INDICATIONS OF OSSEOUS RESECTIVE SURGERY l l l Several factors can contraindicate the use of osseous resection to eliminate periodontal pockets (Bradin, 1962) Anatomic features such as close proximity of maxillary antrum or the ramus. Impaired physical or emotional health of patient. Advanced age
l l l Inadequate oral hygiene resulting from lack of dexterity or motivation. High caries index Extreme root sensitivity Unacceptable esthetic result Advanced Periodontitis
ALTERNATIVE TREATMENTS l l l Maintenance with periodic root planing. Bone grafts. Re-attachment fill procedures. Hemisection or root amputation. Orthodontics. Extraction.
FACTORS IN SELECTION OF RESECTIVE OSSEOUS SURGERY Relationship between depth & configuration of bony lesions to root morphology & the adjacent teeth determines the extent that bone & attachment is removed during resection. l Ostectomy is best applied to patients with early to moderate bone loss (2 -3 mm) with moderate root trunk length (Ochsenbein 1964) and not for patients with advanced attachment loss. l
l Two walled defects or craters should be treated with resection of ledges and ostectomy in facial & lingual surface to obtain +ve architecture. Otherwise, presence of window’s peak causes recurrence of interproximal pockets.
l Shallow to moderate bony defects can be effectively managed by osteoplasty and ostectomy. l Patients with advanced attachment loss and deep intrabony defects are not candidates for resection to produce a positive contour.
l Patients with deep, multiwalled defects are not candidates for resective osseous surgery. They are better treated by regenerative therapies or by combining osteoplasty to reduce bony ledges and to facilitate flap closure with new attachment/ regeneration procedure.
EXAMINATION AND TREATMENT PLANNING WITH RESECTIVE SURGERY l l l Comprehensive periodontal examination. Periodontal probing and exploration are the key aspects of the examination. Careful probing reveals the presence of: Pocket depth. Location of the base of the pocket relative to the mucogingival junction & attachment level on adjacent teeth. Number of bony walls. Presence of furcation defects.
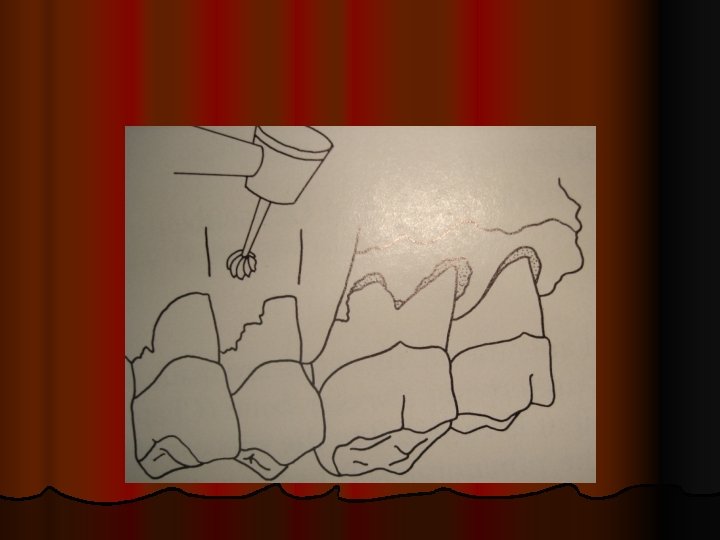
 Steps of resective osseous surgery
Steps of resective osseous surgery Bulbous bone contour
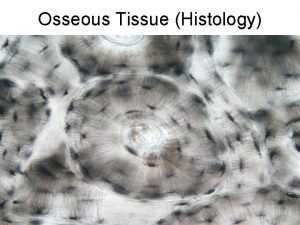
Bulbous bone contour Another name for osseous tissue
Another name for osseous tissue Osseous coagulum definition
Osseous coagulum definition Osseous meatus
Osseous meatus Synovial sheath
Synovial sheath Bone swaging
Bone swaging Mastoid antrum
Mastoid antrum Periapical
Periapical Specimen of cost audit report
Specimen of cost audit report Sds software engineering
Sds software engineering Triangular space contents
Triangular space contents Ob kit contents
Ob kit contents Health education defined
Health education defined Thoracic duck
Thoracic duck Cruropopliteal canal is formed by
Cruropopliteal canal is formed by Cause and effect contents of the dead man's pocket
Cause and effect contents of the dead man's pocket Cerebellum nuclei
Cerebellum nuclei Nature table of contents
Nature table of contents Styloid apparatus
Styloid apparatus Nutrients and their functions table
Nutrients and their functions table Continuous variable example
Continuous variable example Timeline of zheng he
Timeline of zheng he Elagse
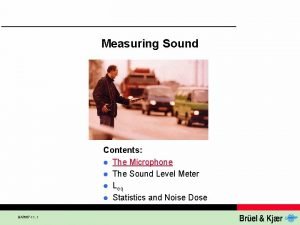
Elagse Sound contents
Sound contents Use case model
Use case model Subscapular artery anastomosis
Subscapular artery anastomosis Contents of femoral triangle
Contents of femoral triangle Prophylaxis
Prophylaxis Feedback channel definition
Feedback channel definition Table of contents background
Table of contents background Air pollution contents
Air pollution contents Ism familiarization
Ism familiarization Serratus muscle function
Serratus muscle function Table of contents science
Table of contents science Company profile table of contents
Company profile table of contents Contents of the middle mediastinum
Contents of the middle mediastinum Posterior triangle of neck contents mnemonic
Posterior triangle of neck contents mnemonic Contents
Contents Persepolis table
Persepolis table What is the perineum and where is it located
What is the perineum and where is it located Pericardium
Pericardium Ttbiz
Ttbiz Algebra 1 table of contents
Algebra 1 table of contents Nature of prospectus
Nature of prospectus