Osseous grafts Terminology l Regeneration is defined AAP














- Slides: 115
Osseous grafts
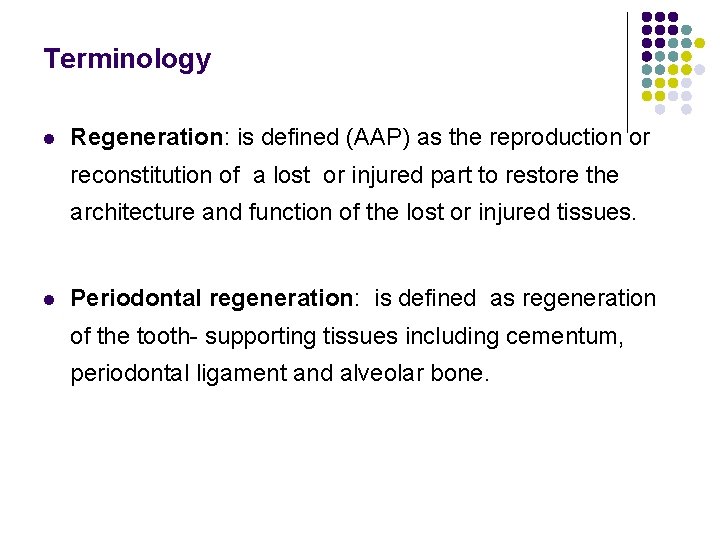
Terminology l Regeneration: is defined (AAP) as the reproduction or reconstitution of a lost or injured part to restore the architecture and function of the lost or injured tissues. l Periodontal regeneration: is defined as regeneration of the tooth- supporting tissues including cementum, periodontal ligament and alveolar bone.
l Graft: is a viable tissue that, after removal from a donor site, is implanted within a host tissue which is then restored, repaired or regenerated l Bone grafts: the donor bone is incorporated in the healing process & remains afterward as a functioning part of the periodontium
l A graft is any tissue or organ used for implantation or transplantation l Transplantation implies surgical transfer of living tissue l The transplant is the tissue used l Implantation implies the use of nonliving tissue l An implant is a material inserted or grafted into intact tissue of the recipient
l New attachment is the embedding of new periodontal ligament fibers into new cementum and the attachment of the gingival epithelium to a tooth surface previously denuded by disease l Bone fill: is defined as the clinical restoration of bone tissue in a treated periodontal defect.

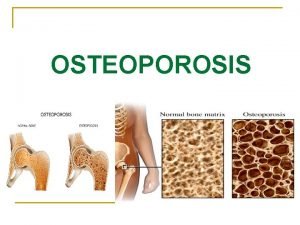
Biologic concept of using bone grafts 1. Materials may contain bone forming cells (osteogenesis) 2. Serve as a scaffold for bone formation (osteoconduction) 3. The matrix of the bone grafts contains bone inducing substances (osteoinduction) (Urist 1980, Brunsvold & Mellonig 1993)

Osteoconduction: l Occurs with the ingrowth of capillaries in new connective tissue l With bone grafts, this process is followed by simultaneous resorption of dead bone or of the synthetic trellis and the deposition of new bone lamellae
Osteoinduction: l Bone formation is induced in the surrounding soft tissue immediately adjacent to the grafted material l may induce cells in the bone to produce a new cementum layer with inserting collagen fibers on previously periodontitis-involved root surfaces
Objectives of bone grafting 1. Probing depth reduction 2. Clinical attachment gain 3. Bone fill of the osseous defect 4. Regeneration of new bone, cementum and periodontal ligament 5. Establish a healthy maintainable environment
Indications l Deep intrabony defects l Advanced periodontitis with thin gingiva where gingival recession might occur if GTR is performed l Combined with GTR for space making or facilitating membrane manipulation l Tooth retention/support for critical teeth l Furcation defects l Anatomic limitations for other procedures l Ridge augmentation
Contraindications l Considerable gingival recession in the surgical area l Extraordinary soft tissue crater in surgical area l Insufficient width of keratinized gingiva l Advanced furcation involvement
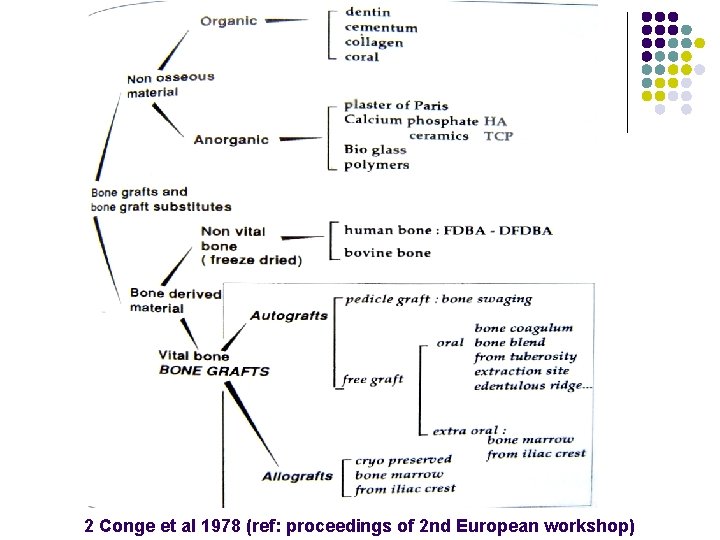
Classification 1. Autogenous grafts: grafts transferred from one position to another within the same individual 2. Allogeneic grafts: grafts transferred between genetically dissimilar members of the same species 3. Xenogeneic grafts: grafts taken from a donor of another species 4. Alloplastic materials: synthetic or inorganic implant materials which are used as substitutes for bone grafts
l Isograft: a graft between genetically identical individuals, identical twins l Homografts: a graft b/w genetically similar individuals of the same species l Heterograft: a graft taken from a donor of a different species
1 Autografts l Cortical bone chips l Osseous coagulum l Bone blend l Intraoral cancellous bone &marrow l Extraoral cancellous bone & marrow (reference: Grant)
Allografts l Frozen iliac bone & marrow l Sterilized iliac bone & marrow l Freeze-dried bone l Decalcified freeze dried bone l Merthiolated bone l Demineralized dentine l Lyophilized duramater l Sclera l cartilage (reference: Grant)
Xenografts l Boplant l Os purum l Boiled bovine bone l Anorganic bone l Kiel bone (reference: Grant)
Alloplasts l Beta tricalcium phosphate l Hydroxylapatite l Replamineform hydroxylapatite l Plaster of paris (reference: Grant)
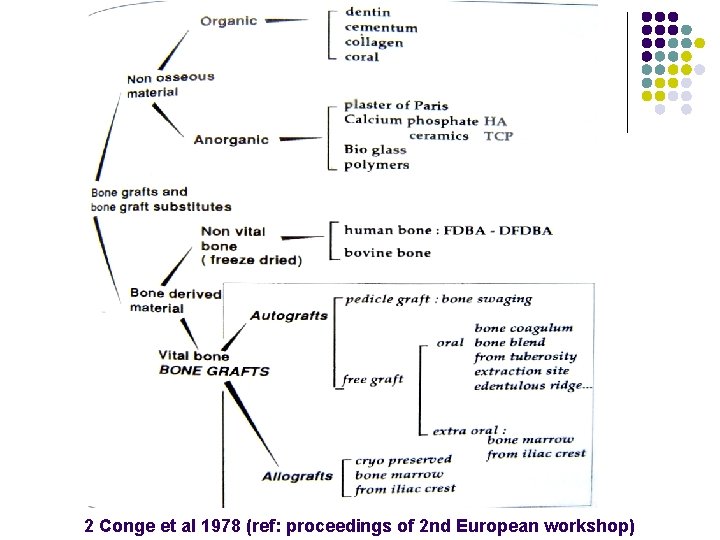
2 Conge et al 1978 (ref: proceedings of 2 nd European workshop)
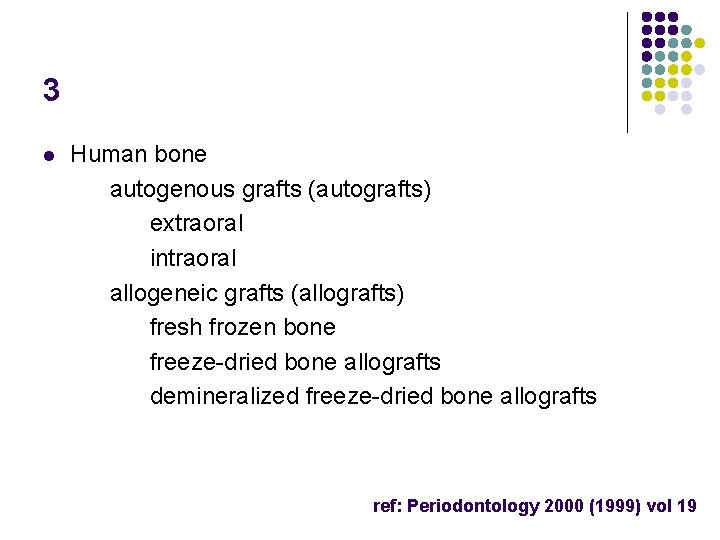
3 l Human bone autogenous grafts (autografts) extraoral intraoral allogeneic grafts (allografts) fresh frozen bone freeze-dried bone allografts demineralized freeze-dried bone allografts ref: Periodontology 2000 (1999) vol 19
l Bone substitutes Xenogeneic grafts (xenografts) bovine derived hydroxyapatite coralline calcium carbonate Alloplastic grafts (alloplasts) Polymers Bioceramics Tricalcium phosphate Hydroxyapatite dense, nonporous, nonresorbable (xenograft) resorbable HA derived at low temp Bioactive glasses ref: Periodontology 2000 (1999) vol 19
Ideal characteristics- bone graft l l l l l Nontoxic Nonantigenic Resistant to infection No root resorption or ankylosis Strong and resilient Easily adaptable Readily and sufficiently available Minimal surgical procedure Stimulates new attachment
Wound healing Three sequential phases: l Inflammation (early and late) l Granulation tissue formation l Matrix formation and remodelling
l At wound closure: clotting blood fills the space b/w the transgingivally positioned tooth and the flap l Within seconds: plasma proteins, primarily fibrinogen, precipitate onto the wound surfaces and provide an initial basis for adherence of a fibrin clot l Within 1 hour: the early inflammatory phase of healing is initiated by neutrophils infiltrating the clot from the mucogingival flap
l Within 6 hours: the root surface becomes lined by neutrophils, which decontaminate the wound by phagocytosing injured and necrotic tissue l Within 3 days: the inflammatory reaction moves into its late phase as the neutrophil infiltrate gradually decreases while the influx of macrophages increases
l The macrophage contributes to wound debridement by removing effete red blood cells, neutrophils, and residual tissue debris l release of growth factors which support fibroblast proliferation and matrix production, smooth muscle cell proliferation, and endothelial cell proliferation and angiogenesis. l plays a key role in the transition from inflammation to granulation tissue formation.
l Within seven days: the phase of granulation tissue formation gradually enters into the third phase of wound healing in which the newly formed cell- rich tissue undergoes maturation and remodeling to meet functional demands.
Autogenous grafts l l Gold standard They are gradually resorbed and replaced by new viable bone. l Osteoprogenitor cells or preosteoblasts proliferate & bridge the gap b/w the graft & the recipient bone l The preosteoblasts also form the first deposits of the bone
Source: l Bone from extraoral sites and l Bone from intraoral sites
Advantages: l Superior at retaining cell viability l Contain live osteoblasts and osteoprogenitor stem cells l Heal by osteogenesis l Avoid the potential problems of histocompatability differences and the risk of disease transfer l Decreases cost to the patient l Eliminates the possibility of graft rejection
Bone from extraoral sites Types: - fresh or preserved iliac cancellous marrow bone. Source : - anterior or posterior iliac crest. Advantages: l high potential for true osteogenesis. l can yield more marrow and cancellous bone than can the tuberosity.
l The westerman-jensen biopsy needle or of the Turkel Trephine are used for obtaining small cores l These cores are about 1 cm in length and with a diameter of 2 to 3 mm l 3 cores may be obtained from a single puncture of the posterior iliac crest and l 12 to 15 from the anterior iliac crest.

Problems l Postoperative infection, exfoliation, sequestration l Varying rates of healing l Root resorption l Rapid recurrence of the defect l Increased patient expense l Difficulty in processing the donor material (the technique is no longer in use)
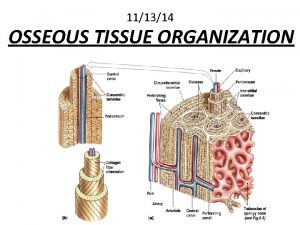
Bone graft from intraoral sites l Autogenous bone can be harvested with or without processing to yield graft materials of different forms including cortical chips, osseous coagulum and bone blend.

Advantages l Can be used immediately if donor tissue is available without fear of root resorption l Harvested by periodontist
Sources: l Maxillary tuberosity l Healing extraction sites (8 to 12 weeks to allow newly forming bone to mature) l Bone from edentulous ridges l Bone trephined from within the jaw without damaging the roots l Bone removed during osteoplasty and ostectomy l Mental and mandibular retromolar areas l Exostosis
Cortical bone chips l Nabers and O’Leary reported that shavings of cortical bone removed by hand chisels during osteoplasty/ ostectomy from sites within the surgical area could be used successfully to effect a coronal increase in bone height l Cortical chips bcoz of their large particle size and potential for sequestration were replaced by osseous coagulum and bone blend techniques
Osseous coagulum l A mixture of bone dust and blood l Technique: It is prepared by mixing particles of bone obtained using rotary instruments with the patient’s blood l Bone is removed with a carbide bur 6 or 8 at speeds between 5000 and 30, 000 rpm, placed in a sterile dappen dish or amalgam cloth, and used to fill the defect.
l Obtained from denser bone, particularly when osseous contouring procedures l This material differs from bone and marrow or bone chip grafts in that fewer cells are present in the graft l The technique uses small particles ground from cortical bone.
Advantages l ease of obtaining bone from already exposed surgical sites l Smaller particle size provides additional surface area for the interaction of cellular and vascular elements. l resorption and replacement with host bone is more certain
Disadvantages : l l relatively low predictability and inability to procure adequate material for larger defects.
Limitation: l Inability to use aspiration during accumulation of the coagulum l difficulty in controlling bone particle size and quantity, l clinical management of the graft material (materials fluidity) l Salivary contamination
Bone blend l Bone fragments harvested using a trephine, chisel or rongeur l The bone blend technique uses an autoclaved plastic capsule and pestle
l Bone is removed from a predetermined site, triturated for 10 to 30 seconds in the capsule to a workable, plastic like mass (slushy osseous mass), and packed into bony defects l yield more clinically manageable and predictable graft material of a larger particle size (100 to 200 µm)
Intraoral cancellous bone marrow transplants: Sources l Maxillary tuberosity l Edentulous areas l Healing sockets l Mandibular retromolar areas
Bone swaging l Swaging is a procedure that consists of bending and breaking the thin bony walls that form one and two walled hemisepta or craters into the defect in an effort to reduce the periodontal pocket l It involves making a greenstick fracture of bone bordering an intraosseous defect
l The bone is then displaced into the defect l This technique requires an existence of an edentulous area adjacent to the defect from which the bone is pushed into contact with the root surface without fracturing the bone at its base l Bone swaging is technically difficult and its usefulness is limited

Allogeneic grafts The need of an allogeneic source or substitute for autogenous bone arose from l the need for a supply of donor material to fill multiple or deep bone defects within the same patient and l the morbidity accompanying a second surgical site to procure donor bone.
l Allograft material is from cadaveric sources l Tissue may be either sterile or non-sterile. l A non-sterile approach requires chemical or physical sterilization, which may render the graft less desirable for human transplantation. l If bone is obtained under sterile conditions, processing is begun within 24 hours of death.
l Cortical bone is used from various sources, including ribs l it is ground into a bone powder, with particle sizes varying from 250 to 500 µm. l demineralized to expose matrix proteins for greater inductivity. l Packaging and storage is by freeze- dried technique.
l Iliac and vertebral bone and marrow are also obtained from cadaveric sources and may be stored by freezing in special media with a cryopreservative agent, or may be irradiated for sterilization.
Risk of disease transfer l fresh frozen bone allograft: approximately one in 2 million if the tissue bank uses exclusionary techniques. l freeze- dried bone: 1 in 2. 8 billion.
l Although freeze- drying destroys all cells and the graft is rendered non- viable, it has the advantage of reducing antigenicity and facilitating long- term storage. l Vacuum sealing in glass containers protects against contamination and degradation of the graft material while permitting storage at room temperature for an indefinite period of time.
The types of allogenic grafts used are l frozen iliac cancellous bone and marrow, l Cryopreserved bone from the head of a femur l mineralized freeze- dried bone grafts (FDBA) and l decalcified freeze- dried bone grafts(DFDBA).
l The need for cross- matching to decrease the likelihood of graft rejection as well as the risk of disease transmission virtually eliminated the use of frozen iliac allogenic grafts in periodontics.
Mineralized freeze- dried bone allografts l l l FDBA is a mineralized bone graft, which through the manufacturing process loses cell viability promote bone regeneration through osteoconduction FDBA is bone that has been frozen, with the water removed by sublimation in a vaccum
DFDBA l Demineralization of allografts was performed because the bone mineral blocked the effect of the factors stimulating bone growth sequestrated in bone matrix including bone morphogenetic proteins. l BMPs are a group of acidic polypeptides belonging to the transforming growth factor-ß gene super- family.

l Urist et al 1965 suggested that demineralization of a cortical bone allograft (DFDBA) enhances its osteogenic potential by exposing bone morphogenic proteins (BMPs) which presumely have the ability to induce host cells to differentiate into osteoblasts. l Controlled clinical studies documented considerable gain of attachment and bone fill in sites treated with DFDBA as compared with non- grafted sites (Pearson et al 1981, Mellonig 1984, Meadows et al 1993).
DEMBONE l Content: Demineralized Freeze-Dried Bone Allograft l Packaging: Quantity: 0. 5, 1 cc l Cost: 0. 5 cc: 2200/1 cc: 3500/-
DYNAGRAFT Content: Demineralized bone matrix in a reverse phase medium. Packaging : Gel Form - 0. 5 cc vial 1. 0 cc vial 5. 0 cc vial 10. 0 cc vial Putty Form – 1. 0 cc vial 2. 5 cc vial 5. 0 cc vial 10. 0 cc vial
GRAFTON Content: Packaging: Cost: Demineralized bone matrix Putty Quantity: 0. 5 cc and 1 cc Syringe Quantity: 0. 25 cc Flex 1. 5 X 1. 5 cm Matrix 8 X 8 X 10 mm Putty 0. 5 cc: 8950/1 cc 16725/Syringe 10900/- (pack of 2) 5850/- (pack of 1) Flex 1. 5 X 1. 5 cm 17225/Matrix 8 X 8 X 10 mm 5350/-
OSSEOGRAFT l Content: l Packaging: each l Cost: 2178/- DFDBA Quantity: 2 Vials of 0. 25 gm
Sclera: l Sclera allografts have had a brief period of popularity and utilization in inductive therapy. l Sclera meet two of the prime requirements for a graft designed to repair periodontal defects: (1) they are attained easily and (2) they are not rejected by the host.
Advantages l availability l may be preserved for long periods without deteriorating. l do not elicit an immune response, and l do not appear to be associated with root resorption or ankylosis.
Xenogeneic grafts l Sources: bovine bone and natural coral. l Both sources, through different processing techniques, provide products which are biocompatible and structurally similar to human bone. l Xenografts are osteoconductive
1. Boplant (calf bone that is detergent-extracted with chloroform-methanol, sterilized in propiolactone, and freeze dried) 2. Os porum (cow bone soaked in potassium hydroxide, acetone and salt solution) 3. Anorganic bone (cow bone extracted by means of ethylenediamine and sterilized by autoclaving) 4. Boiled bone (cow bone that is boiled and autoclaved) 5. Kiel bone (cow bone denatured with hydrogen peroxide, dried with acetone, and sterilized with ethylene oxide)
Bovine derived bone replacement grafts l Commercially available bovine bone is processed to yield natural bone mineral minus the organic component. l Anorganic bovine bone is the hydroxyapatite ‘skeleton’ that retains the macroporous and microporous structure of cortical and cancellous bone remaining after chemical or low- heat extraction of the organic component.
l Historically, bovine xenografts have failed due to rejection, probably because earlier materials used chemical detergent extraction, which left residual protein and therefore produced adverse reactions and clinically unacceptable results. l Currently available bovine- derived hydroxyapatite is deproteinated, retaining its natural microporous structure, which supports cell- mediated resorption.
l New processing and purification methods have been utilized which make it possible to remove all organic components from a bovine bone source and leave a nonorganic bone matrix in an unchanged inorganic form l Bovine derived bone xenograft is prepared from either cortical or cancellous bovine bone by chemical extraction of all organic material
BIOGEN l Content: l Quantity: l Cost: Bovine Bone Graft 0. 5 gm 2900/-
BIO-OSS l Content: l Packaging: Bovine Bone Graft 1. Spongiosa granulat Particle Size: 0. 25 – 1 mm Quantity: 0. 5, 2 gms. 2. Spongiosa granulat Particle Size: 1 – 2 mm Quantity: 0. 5, 2 gms 3. Spongiosa block Block 1 x 1 x 2 cm 4. Bio-oss collagen 100 mg Spongiosa Granulat + 10% Collagen

l Cost: spongiosa granulat: 0. 25 – 1 mm 0. 5 g: 4050/- 2 g: 13500/1 -2 mm 0. 5 g: 3555/- 2 g: 12500/ spongiosa block: 12550/bio-oss collagen: 4050/-

Alloplastic grafts l Alloplastic materials are synthetic, inorganic, biocompatible, or bioactive bone grafts substitutes. l Alloplast materials are believed to promote bone healing through osteoconduction.
Ideal properties : 1. biocompatible 2. minimal fibrotic reaction 3. the ability to undergo remodeling and support new bone formation 4. similar strength comparable to cortical /cancellous bone and 5. similar modulous of elasticity comparable to bone to prevent fatigue fracture under cyclic loading
Polymers: 1. A non-resorbable, calcium hydroxide coated copolymer of poly-methyl-methacrylate (PMMA) and polyhydroxylethyl-methacrylate (PHEMA) 2. A resorbable polylactic acid (PLA) polymer

l HTR Synthetic Bone is a biocompatible microporos composite of polymethylmethacrylate, polyhydroxylethylmethacrylate l The PMMA 550 to 880 µm diameter beads are embedded into PHEMA and coated by calcium hydroxide
l Histologically, PMMA does not promote new attachment formation l The HTR particle were most frequently encapsulated by CT with only scarce evidence of bone formation (Plotzke et al 1993)
l Its hydrophilicity enhances clotting, and its negative particle surface charge allows adherence to bone. l It appears to serve as a scaffold for bone formation when in close contact with alveolar bone. l Clinical defect fill and resolution can be achieved supporting its use as a biocompatible alloplastic bone substitute.
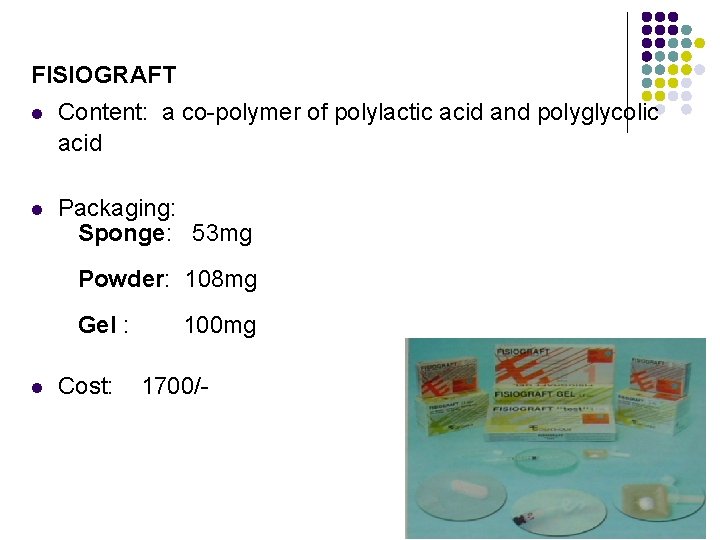
FISIOGRAFT l Content: a co-polymer of polylactic acid and polyglycolic acid l Packaging: Sponge: 53 mg Powder: 108 mg Gel : l Cost: 100 mg 1700/-
Bioceramics l Bioceramic alloplasts are comprised primariy of calcium phosphate, with the proportion of calcium and phosphate similar to bone. l The two most widely used forms are tricalcium phosphate and hydroxyapatite.
Tricalcium phosphate l Tricalcium phosphate is a porous form of calcium phosphate, the most commonly used form of which is ßtriclacium phosphate. l ß- triclacium phosphate is produced from calcium phosphate powder, mixed with naphthalene and pressed and heated at temperatures as high as 1, 000 °c to 2000°c, allowing it to fuse in a solid mass (Snyder et al 1984)
l The naphthalene evaporates, leaving spaces within the ceramic and giving rise to a porous structure l It serves as a biological filler which is partially resorbable and allows bone replacement. l The first attempt at using ß-TCP was made by Nery & Lynch in 1978
BIORESORB l Content: Pure Beta Tricalcium Phosphate Ceramic, Tertiary calcium salt of ortho-phosphoric acid l Packaging: Granule Sizes: 500 – 1000 microns Quantity : 0. 5, 1. 0 gm l Cost: 0. 5 gm: 2000/1. 0 gm: 3300/-
SYN OSS Content: Packaging: Beta Tricalcium Phosphate Particle size: 300 -600 μ 600 -1000 μ Quantity: Cost: 1100/- 0. 5 gm.
Hydroxyapatite l Hydroxyapatite is the mineral component of bone. l Are solid biomaterials obtained from powdery phosphates l A compression with slowly increasing pressure reduces the interparticle spaces, followed by a sintering process at temperatures of 1100 to 1500°C
Types: l a porous nonresorbable, l a dense or solid nonresorbable, and l a resorbable form.

DENTAOSS Content: Packaging: Cost: Hydroxyapatite Particle size: 50 -250 μ 250 -500 μ 500 -1000 μ Quantity: 1 gm 1, 500/- for 1 gm
DENTAPLUG-HA Content: Bioactive resorbable graft with bovine collagen, hydroxyapatite and chlorhexidine Packaging: Quantity: 20 plugs

OSTEOGEN l Content: l Packaging: l Cost: 4000/- Hydroxyapatite 300 to 400µm Quantity: 1. 5 gms
BIOGRAFT HT Content: Hydroxyapatite + Beta Tricalcium Phosphate Packaging: Particle size 250 microns, 500 microns Cost: Quantity 0. 5 g and 1. 0 g Block 15 X 15 X 10 mm 450/- for 0. 5 g 725/- for 1. 0 g 915/- for block
OSSIFI Content: Beta Tricalcium Phosphate + Hydroxyapatite Packaging: 1. Particle Size: 0. 25 -1 mm Quantity: 0. 5, 1, 2 cc Cost: 2. Particle Size: 1 -2 mm Quantity: 1, 2 cc 1100/- for 0. 5 g
BIOGRAFT HA Content: Hydroxyapatite Packaging: Particle size microns Cost: Quantity Block 450/- for 0. 5 g 725/- for 1. 0 g 915/- for block 250 microns, 500 0. 5 g and 1. 0 g 15 X 15 X 10 mm . .
Rajesh. K. S(1996) : histologic study l Evaluated the efficacy of Chitra HA granules & Chitra HA powder in regeneration of alveolar bone l Artificially created angular bone defect of 18 New Zealand dwarf rabbits l At 1 month: implant material surrounded by PMN cells l 3 months: multinucleate giant cells started resorbing the implant material l 6 months: small amount of newly formed alv bone l Showed that Chitra granules were superior to powder
PERIOGLASS l Content: Ceramic Glass composed of calcium, phosphorous, sodium and Silicon l Packaging: l Cost: 3600/- Particle size: 90 - 710 µm Quantity: 1 gm
Rajesh. H (2005) : clinical study l Compared bone regenerative capacity of Chitra HABG with Osteogen (HA resorb) in 16 pts l Reduction in probing depth, gain in clinical attachment at 3, 6, 9 months l Radiograph showed evidence of bone fill

Technical implications Patient selection l good physical health l acceptable level of oral hygeine l nonsmoker
Defect selection l The predictability of regeneration increase: three- wall defects>>two- wall defects> one wall defects. l Clinical and radiographic examination can aid in determining the type of lesion l Gingival coverage of the graft is important in its containment post surgery
Preoperative preparation l Plaque control l Occlusal therapy or splinting of teeth l A pre- procedural rinse 0. 12% chlorhexidine gluconate
Anesthesia l Ensures patient comfort l Good hemostasis
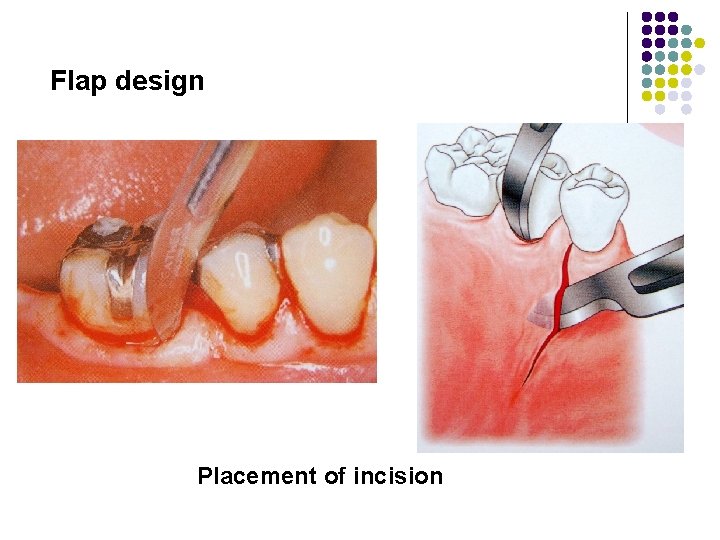
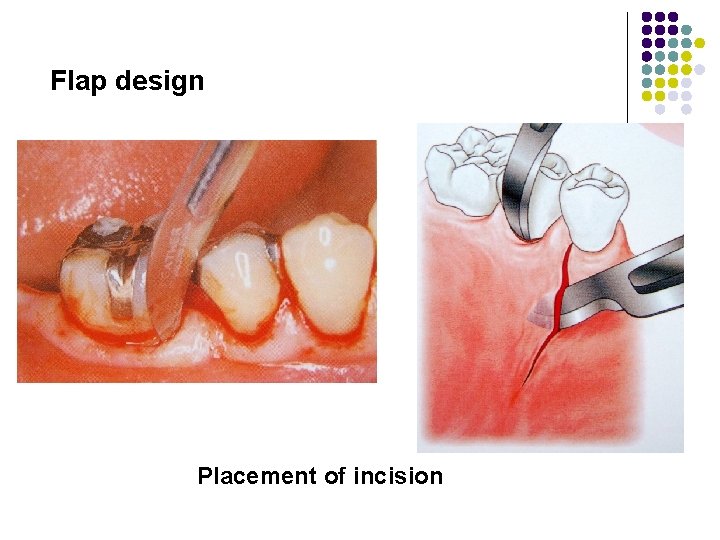
Flap design Placement of incision
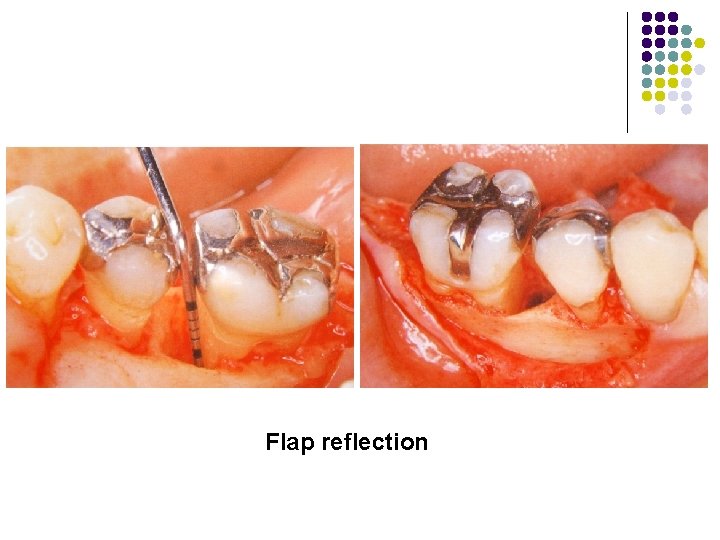
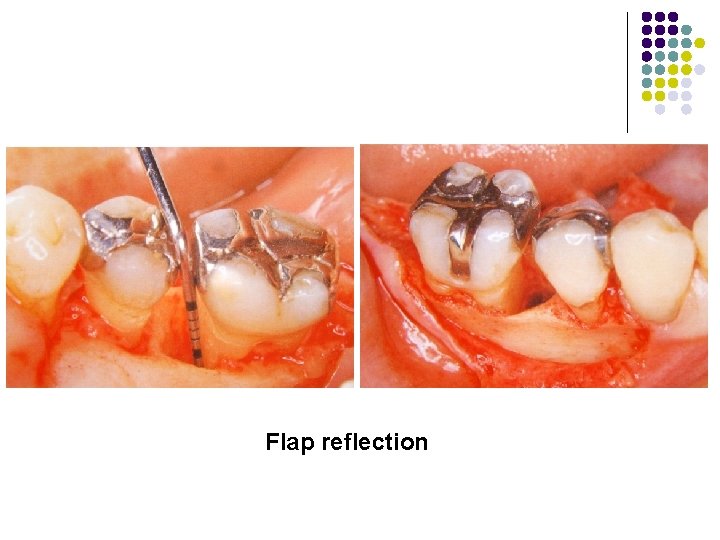
Flap reflection
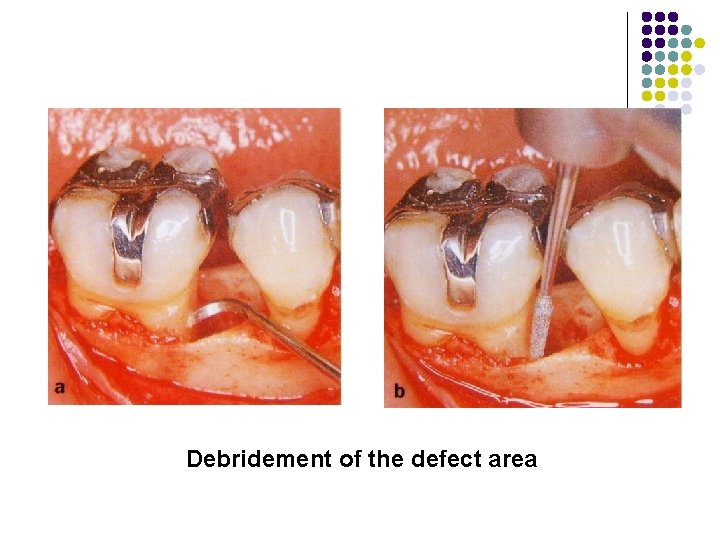
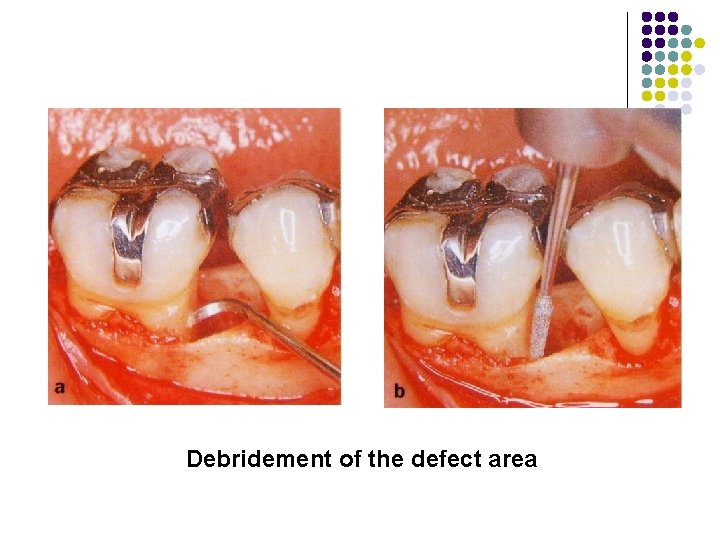
Debridement of the defect area
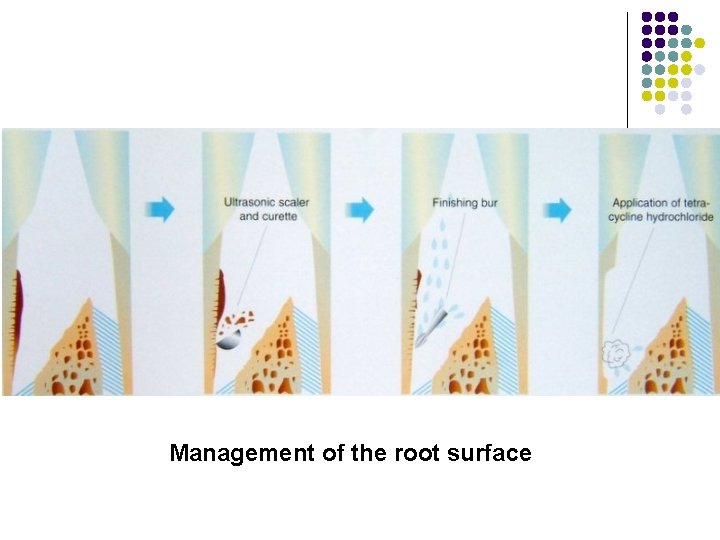
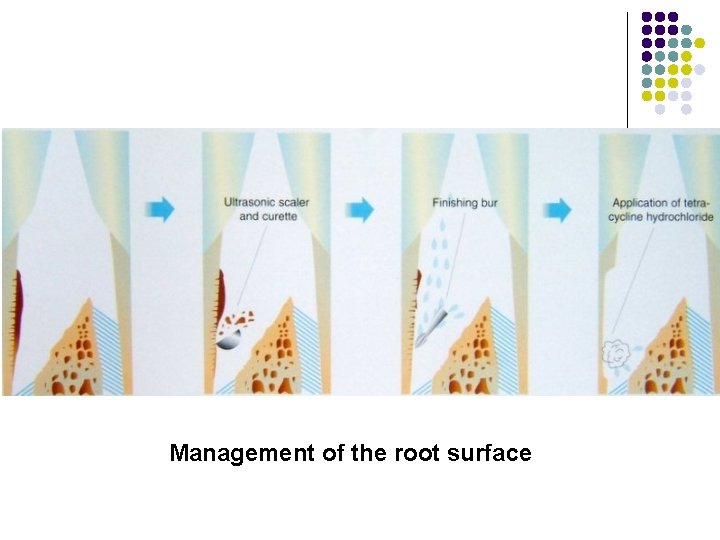
Management of the root surface
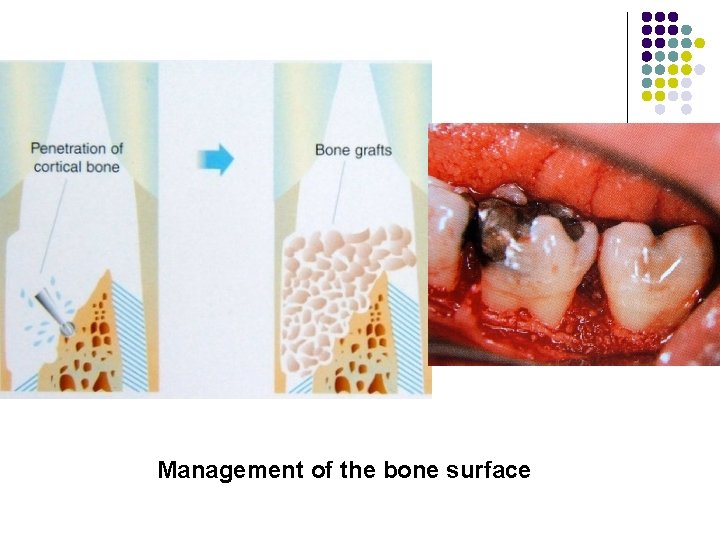
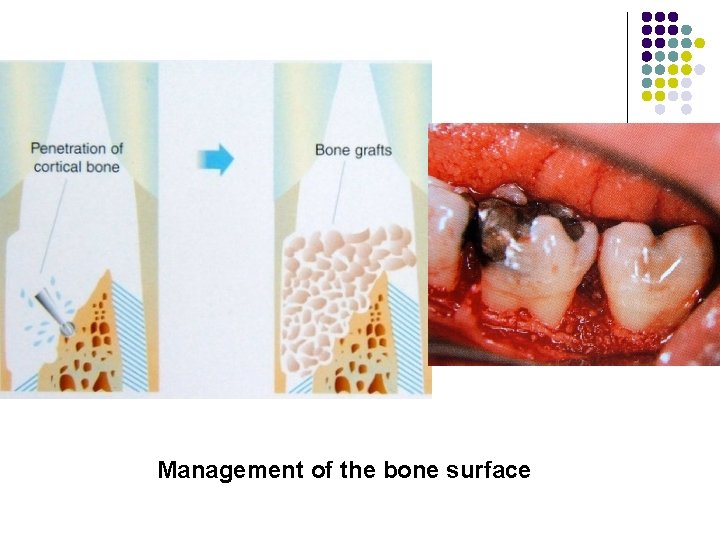
Management of the bone surface
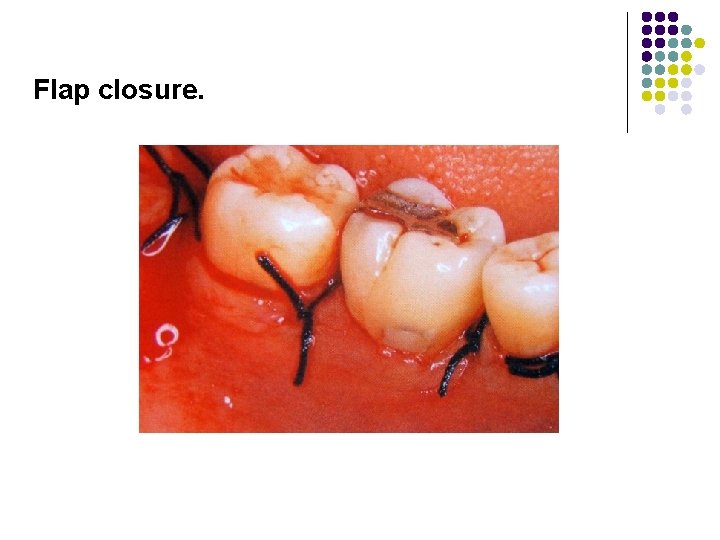
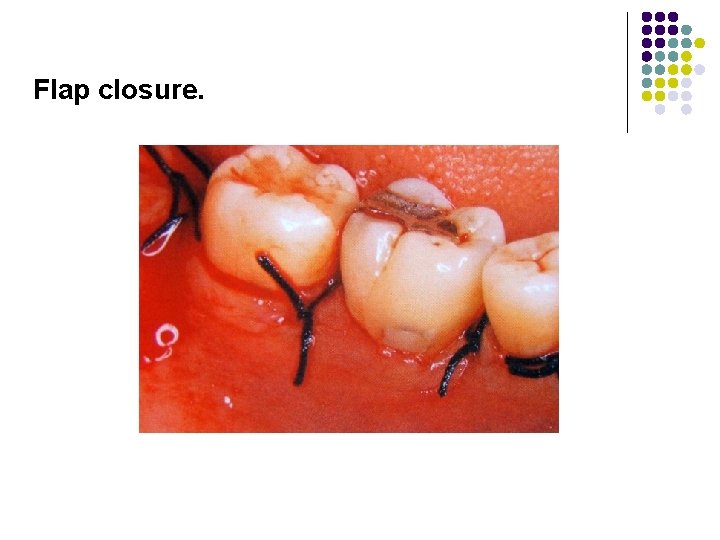
Flap closure.
Post operative management/ periodontal maintenance. l The administration of antibiotics beginning immediately post- surgery is thought to aid in plaque control. l Patients should also be placed on a topical antimicrobial rinse to further aid in this process. l For the first 4 -6 weeks, patients should refrain from brushing in the surgical area to prevent disturbance of the blood clot.
l Postoperative visits are scheduled weekly for the first month, bimonthly for the second month, and every 3 months thereafter. l Sutures are retained as long as they maintain closure and do not contribute to plaque accumulation and inflammation.
l Postoperative visits include plaque removal ( both mechanically and with topical chlorhexidine), selective stain removal and reinforcement of oral hygeine. l Periodontal probing or recording of attachment levels should not be done prior to 6 - 12 months, since probing force may damage the healing site, thereby diminishing the regenerative outcome.

Evaluation of the results l Clinical methods– Probing- soft tissue changes (bleeding on probing) pocket depth clinical attachment level Bone levels- re-entry procedures bone sounding l Radiographic bone changes l Histological methods
Re-entry surgery l performed at 6 -12 months after the initial regeneration procedure l linear measurements in mm made along the root surface with a periodontal probe. l The distance to the base of the defect is taken relative to a fixed landmark, such as CEJ
Limitations l Bone graft therapy involves additional treatment time. l Difficulty in graft procurement and/ or preparation l Unless bone can be removed from within the primary surgical site, either extraoral or intraoral, is necessary. l the quantity of intraoral bone to fill multiple or deep defects is often lacking
Conclusion l Evidence suggests that autogenous bone grafts & DFDBA allografts are effective regenerative materials l Synthetic grafts may result in improved probing depths & clinical attachment levels but have yet to demonstrate the ability to initiate or enhance the formation of a new attachment apparatus

 Tissue
Tissue Objectives of artificial regeneration
Objectives of artificial regeneration Heredity
Heredity Nottingham regeneration
Nottingham regeneration Brayton cycle with regeneration pv diagram
Brayton cycle with regeneration pv diagram Gas turbine classification
Gas turbine classification Gas turbine with regeneration
Gas turbine with regeneration Fiat doblo dpf regeneration procedure
Fiat doblo dpf regeneration procedure Cellules ciliées régénération
Cellules ciliées régénération Was the london docklands regeneration a success
Was the london docklands regeneration a success Planarian regeneration
Planarian regeneration Well-defined set example
Well-defined set example Bright futures screening guidelines
Bright futures screening guidelines Aap-6
Aap-6 Ya zahra dua
Ya zahra dua Aap soy formula
Aap soy formula Aap 2018 um professor ministra um curso especial
Aap 2018 um professor ministra um curso especial Aap cpti
Aap cpti Wat is een verkleinwoord
Wat is een verkleinwoord Aap math
Aap math Vidmid aap
Vidmid aap Aap
Aap Fcps aap level iv
Fcps aap level iv Aap
Aap Msnas
Msnas Hem katabolizması
Hem katabolizması Osseous meatus
Osseous meatus Fibro osseous tunnel
Fibro osseous tunnel Bone swaging in dentistry
Bone swaging in dentistry Fenestra vestibuli
Fenestra vestibuli Osseous surgery ppt
Osseous surgery ppt Conventional ameloblastoma
Conventional ameloblastoma Reverse architecture of bone
Reverse architecture of bone Osseous
Osseous Dfdba
Dfdba Defined planning
Defined planning Abstractions for software defined networks
Abstractions for software defined networks Foundation of army leadership definition
Foundation of army leadership definition It is defined as outsourcing process that can be enabled by
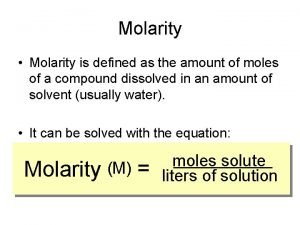
It is defined as outsourcing process that can be enabled by Molarity formula
Molarity formula Quiz 3 defined terms
Quiz 3 defined terms What is character formation
What is character formation Youtube https //www.youtube.com/watch v=vnp84pn0mjq
Youtube https //www.youtube.com/watch v=vnp84pn0mjq L7ci
L7ci Meaning and definition of cost accounting
Meaning and definition of cost accounting Is defined as the systematic inquiry aimed at the discovery
Is defined as the systematic inquiry aimed at the discovery Mandoline definition
Mandoline definition Gay tribes defined clean cut
Gay tribes defined clean cut Ansys fluent user defined function
Ansys fluent user defined function Economic growth is defined as
Economic growth is defined as During a psychiatric emergency the emt should be able to
During a psychiatric emergency the emt should be able to Is concentration and molarity the same
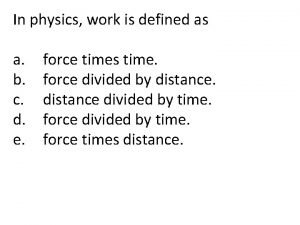
Is concentration and molarity the same In physics, work is defined as *
In physics, work is defined as * A note is generally defined as:
A note is generally defined as: Ubicom system is mythological defined as
Ubicom system is mythological defined as Diy sdr receiver
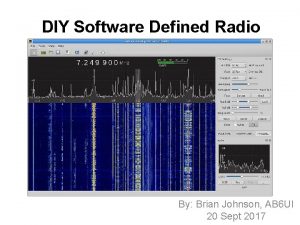
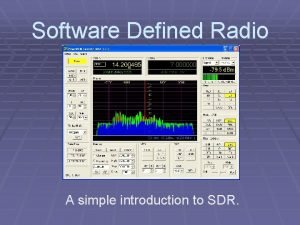
Diy sdr receiver Hdsdr setup
Hdsdr setup Websquare is not defined
Websquare is not defined Is the act of gaining unauthorized access
Is the act of gaining unauthorized access What is the objective of managing operating exposure?
What is the objective of managing operating exposure? Heart failure defined
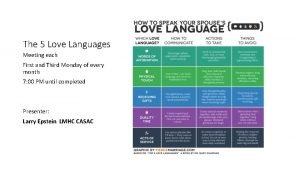
Heart failure defined Love languages defined
Love languages defined Ability to do strength work at an explosive pace
Ability to do strength work at an explosive pace The domain of discrete numeric function is
The domain of discrete numeric function is Software defined radio forum
Software defined radio forum What are biomes defined by
What are biomes defined by What is taxon
What is taxon Softrock sdr
Softrock sdr Material management is defined as: *
Material management is defined as: * Define inductively
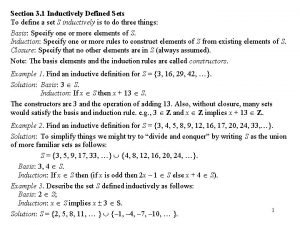
Define inductively What can be defined as the art and science of formulating
What can be defined as the art and science of formulating Elixir definition
Elixir definition A fuel's net energy yield is correctly defined as
A fuel's net energy yield is correctly defined as Learning can be defined as
Learning can be defined as Sketch the region defined by the inequalities
Sketch the region defined by the inequalities Which layer in the osi model covers http, ftp, and rdc?
Which layer in the osi model covers http, ftp, and rdc? Tipe data sederhana
Tipe data sederhana Define workdone
Define workdone An imaginary gas that conforms perfectly
An imaginary gas that conforms perfectly Epic conflict definition
Epic conflict definition Real world example of piecewise function
Real world example of piecewise function Software defined radio
Software defined radio A trait is formally defined as
A trait is formally defined as Defined
Defined Floodlight sdn controller tutorial
Floodlight sdn controller tutorial What is operations management
What is operations management Tmn functional architecture
Tmn functional architecture Volume is defined as
Volume is defined as Missy diwater the former platform diver
Missy diwater the former platform diver Carry narrow product lines with deep assorments
Carry narrow product lines with deep assorments Power is rate of
Power is rate of Pressure is defined as *
Pressure is defined as * Light may be defined as
Light may be defined as User defined functions in java
User defined functions in java Sales resistance is defined as a buyer's:
Sales resistance is defined as a buyer's: How is personality defined module 55
How is personality defined module 55 An opsec indicator is defined as
An opsec indicator is defined as Sdn vs traditional networking
Sdn vs traditional networking Define:recursively
Define:recursively Mathematical system definition
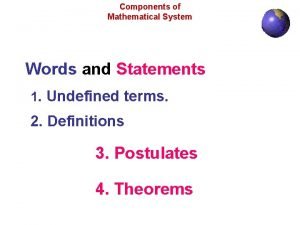
Mathematical system definition Usability definition
Usability definition Customer defined service standards
Customer defined service standards Hard standards and soft standards examples
Hard standards and soft standards examples Data plane control plane and management plane
Data plane control plane and management plane Look up table in fpga
Look up table in fpga What are the characteristics of people as media
What are the characteristics of people as media A moving freight car runs into an identical
A moving freight car runs into an identical Absolute growth rate and relative growth rate
Absolute growth rate and relative growth rate Cycle efficiency is defined as
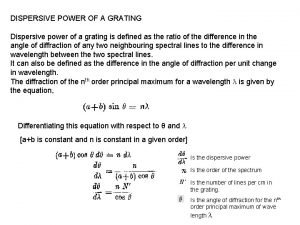
Cycle efficiency is defined as Dispersive power of grating increases with
Dispersive power of grating increases with Regex
Regex Public finance meaning
Public finance meaning The discharge through a single acting reciprocating pump is
The discharge through a single acting reciprocating pump is It is defined as an organization or enterprising entity
It is defined as an organization or enterprising entity Education definition in health
Education definition in health Defined
Defined