OSTEOPOROSIS Definition n Osteoporosis is defined as a

- Slides: 35
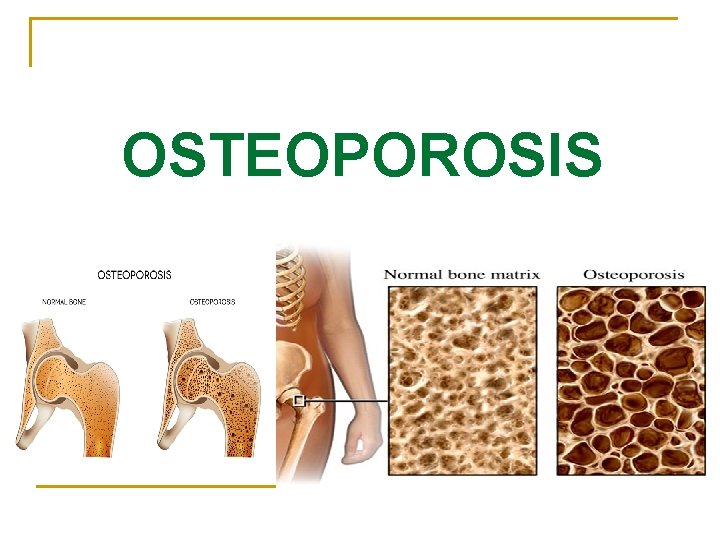
OSTEOPOROSIS
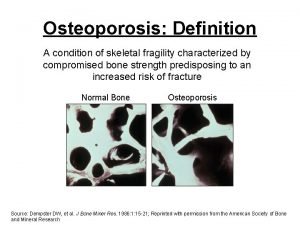
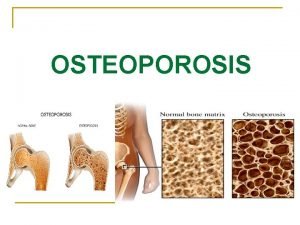
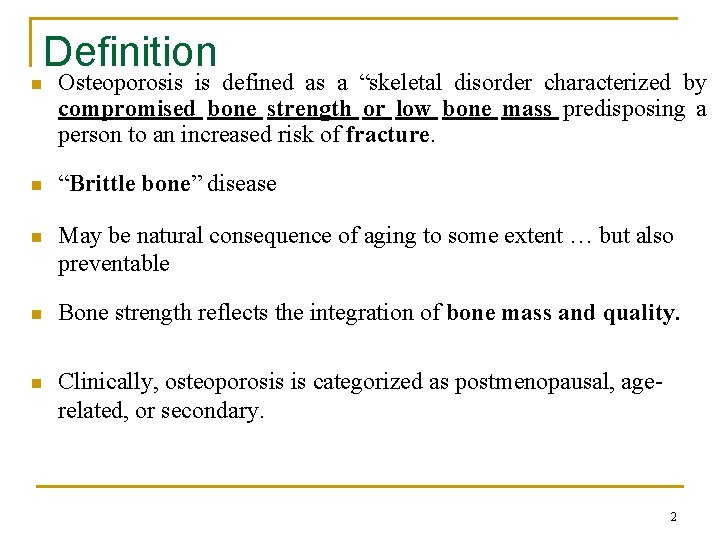
Definition n Osteoporosis is defined as a “skeletal disorder characterized by compromised bone strength or low bone mass predisposing a person to an increased risk of fracture. n “Brittle bone” disease n May be natural consequence of aging to some extent … but also preventable n Bone strength reflects the integration of bone mass and quality. n Clinically, osteoporosis is categorized as postmenopausal, agerelated, or secondary. 2
Epidemiology n In the United States, 8 million women and 2 million men are estimated to have osteoporosis. n Men experience fewer osteoporosis-related fractures (only approximately 20%) than women. n Men's bones also have a mechanical advantage because the larger bone diameter makes them more fractureresistant. n The etiology of male osteoporosis tends to be multifactorial. But in female is due to estrogen defieicncy. 3
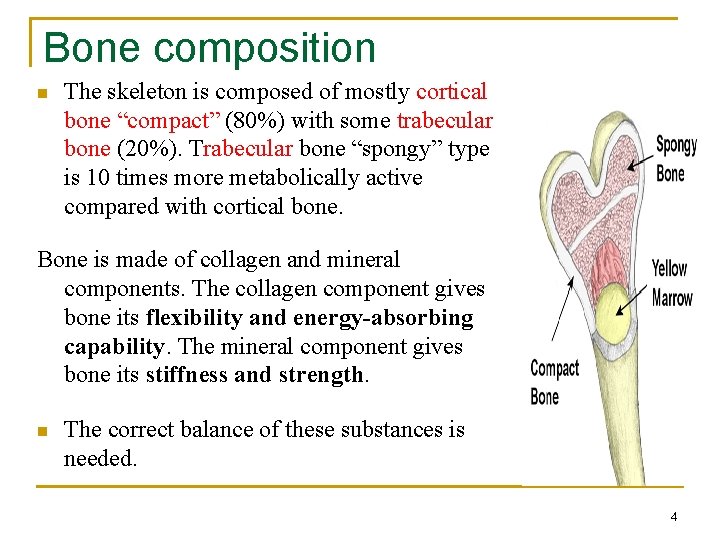
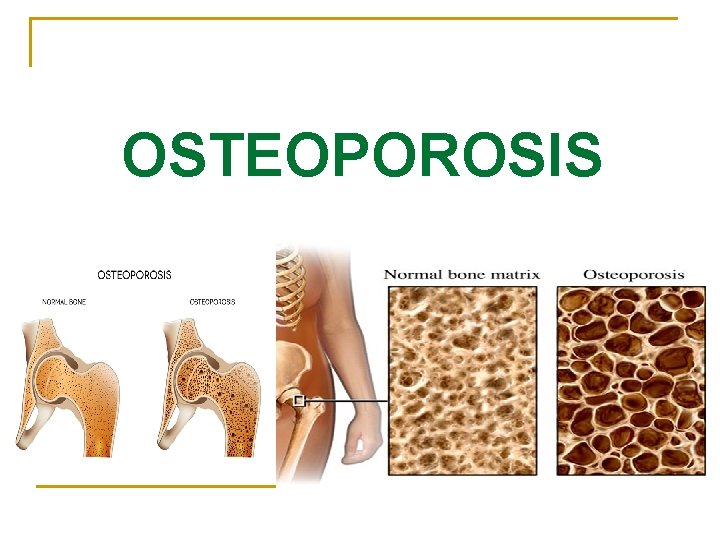
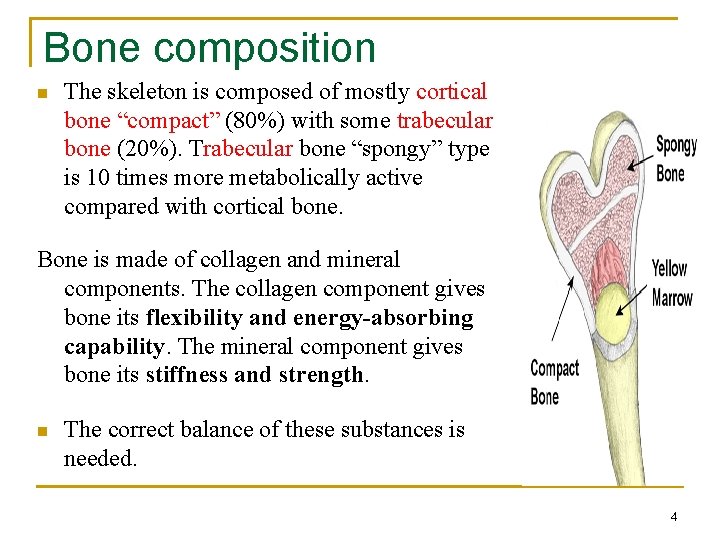
Bone composition n The skeleton is composed of mostly cortical bone “compact” (80%) with some trabecular bone (20%). Trabecular bone “spongy” type is 10 times more metabolically active compared with cortical bone. Bone is made of collagen and mineral components. The collagen component gives bone its flexibility and energy-absorbing capability. The mineral component gives bone its stiffness and strength. n The correct balance of these substances is needed. 4
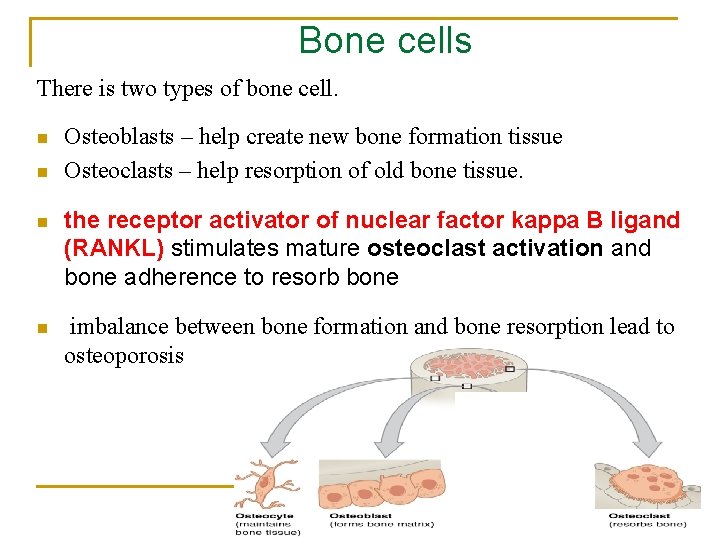
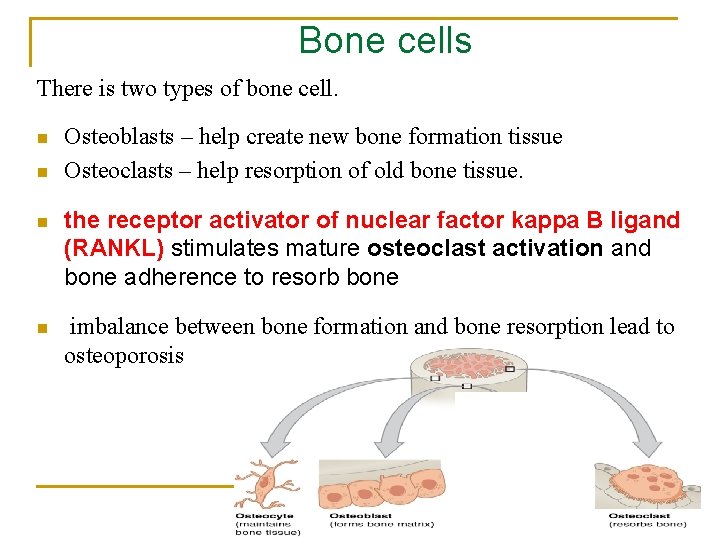
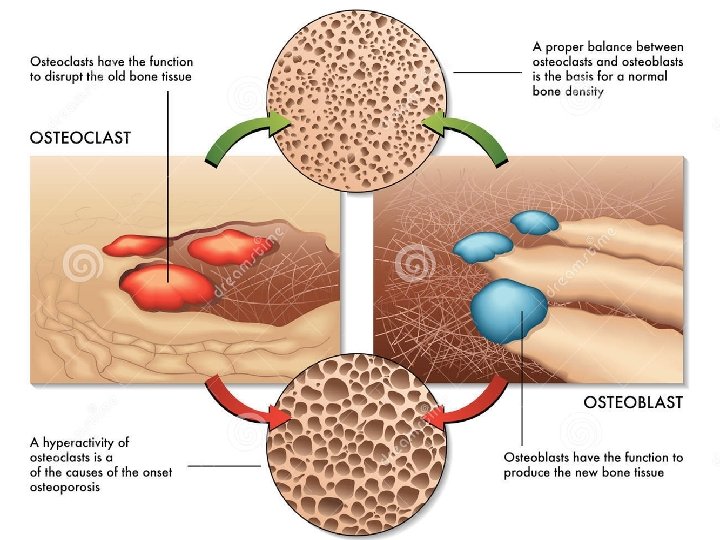
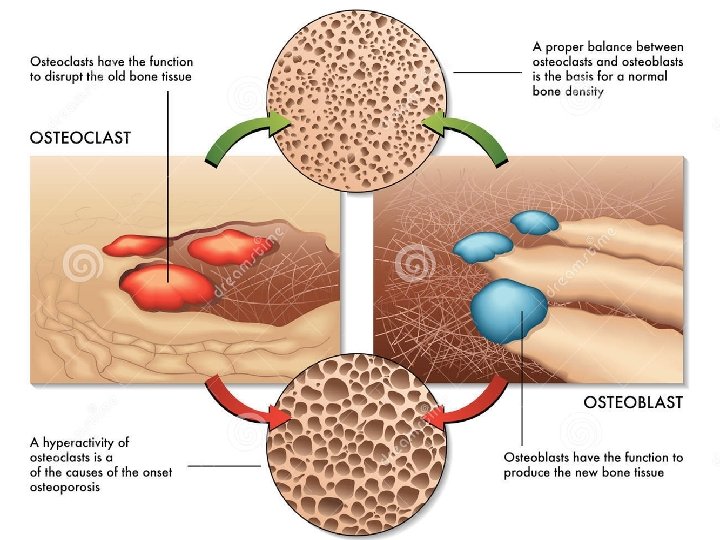
Bone cells There is two types of bone cell. n n Osteoblasts – help create new bone formation tissue Osteoclasts – help resorption of old bone tissue. n the receptor activator of nuclear factor kappa B ligand (RANKL) stimulates mature osteoclast activation and bone adherence to resorb bone n imbalance between bone formation and bone resorption lead to osteoporosis
Bone cells
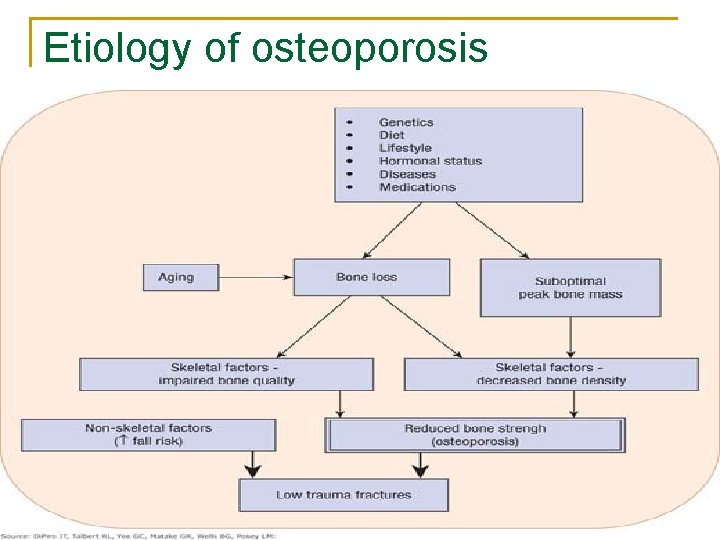
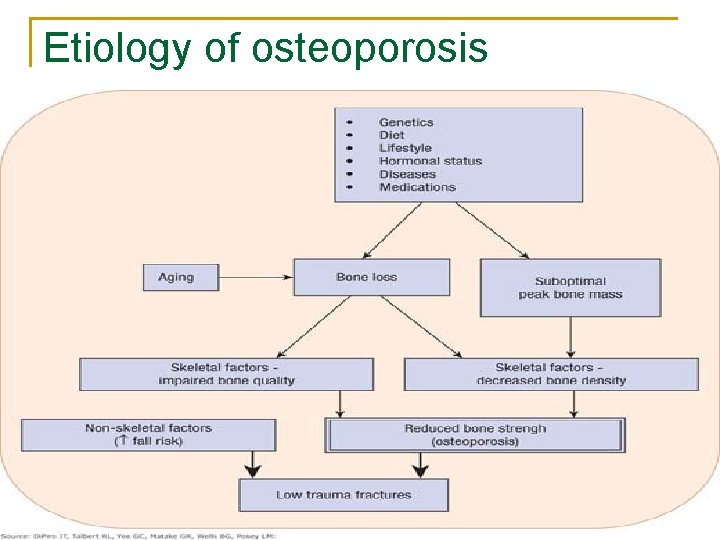
Etiology of osteoporosis 7
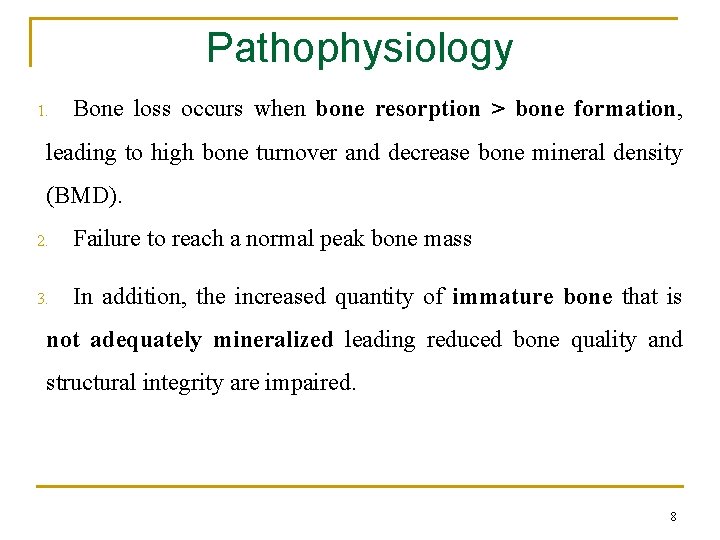
Pathophysiology 1. Bone loss occurs when bone resorption > bone formation, leading to high bone turnover and decrease bone mineral density (BMD). 2. Failure to reach a normal peak bone mass 3. In addition, the increased quantity of immature bone that is not adequately mineralized leading reduced bone quality and structural integrity are impaired. 8
POSTMENOPAUSAL n Postmenopausal osteoporosis affects primarily trabecular bone (vertebral bone) with fractures occurring predominantly at vertebral and distal forearm sites. n The rate of bone loss commonly accelerates at menopause due to a decline in estrogen hormone production. Estrogen deficiency increases bone resorption more than formation. Estrogen deficiency during menopause increases proliferation, differentiation, and activation of new osteoclasts and prolongs survival of mature osteoclasts 9
Age-related osteoporosis n that affects both cortical and trabecular bone and leads to vertebral, hip, and wrist fractures. n n Age birth – 30 years q osteoblasts > osteoclasts Age > 30 years q osteoblasts = osteoclasts, then osteoblasts < osteoclasts after 50 years n Bone resorption increases with age. Age-related osteoporosis occurs mainly because of calcium, and vitamin D deficiencies due to change in their absorption and metabolism leading to accelerated bone turnover and reduced osteoblast formation. 10
DRUG-INDUCED n Secondary osteoporosis is caused by either diseases or medications on both bone types. n Disease include hyperparathyroidism, arthritis, hypogonadism n Systemic glucocorticoids, thyroid hormone replacement, some antiepileptic drugs, depot medroxyprogesterone acetate and heparin use. n Some anticonvulsants, like phenobarbital and phenytoin, hasten vitamin D metabolism and the resultant effects can lead to osteoprosis. n Heparin stimulate osteoclast activity (exact mech not known) Low-molecular-weight heparins such as enoxaparin may pose less risk of bone loss. rheumatoid 11
Risk factors n Current Smoker n Heavy alcohol intake n n low body mass index (<19 kg/m 2), Family history: history of osteoporotic fracture in a first-degree relative n personal history of low-trauma fracture as an adult n Old age n rheumatoid arthritis, hypogonadism, hypeparathyroidism 12
Diagnosis n Osteoporosis is diagnosed by BMD (bone mineral density) measurement or presence of a fragility fracture. General: Many patients are unaware they have osteoporosis until testing for a fracture. Fractures occur after bending, lifting, or independent of any activity. Signs &Symptoms : n Vertebra: mainly asymptomatic or sever lower back pain, decrease height and sometimes curve the spine (kyphosis). n Non vertebra: Pain, Immobility, swelling at fracture site. 13
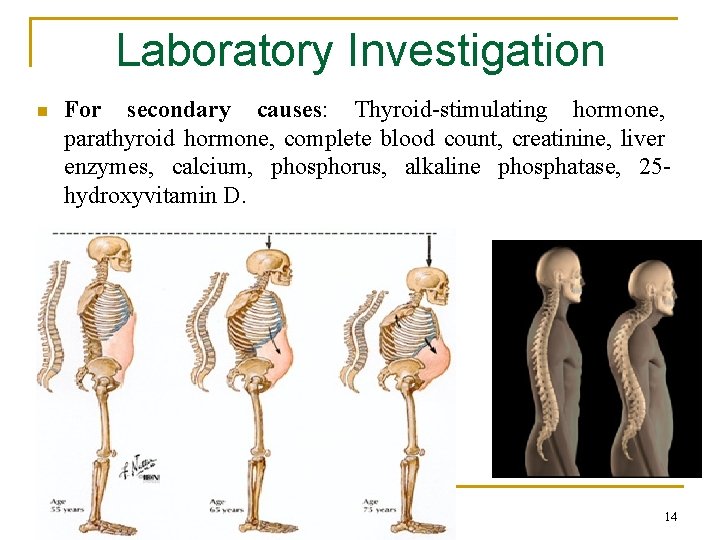
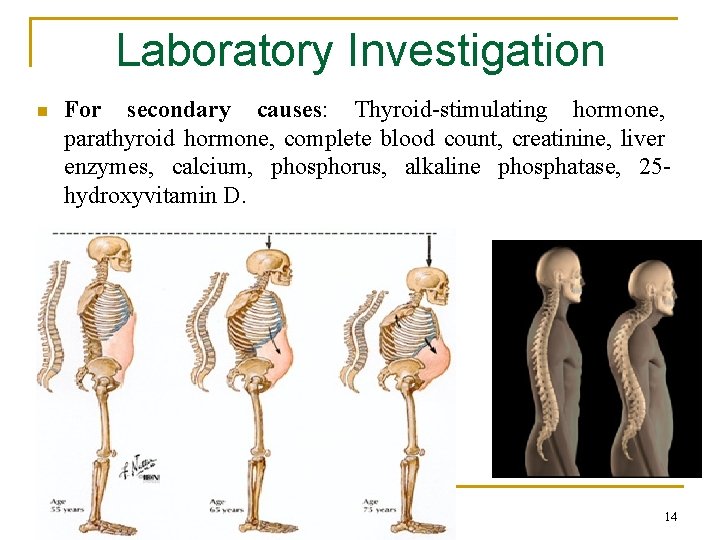
Laboratory Investigation n For secondary causes: Thyroid-stimulating hormone, parathyroid hormone, complete blood count, creatinine, liver enzymes, calcium, phosphorus, alkaline phosphatase, 25 hydroxyvitamin D. 14
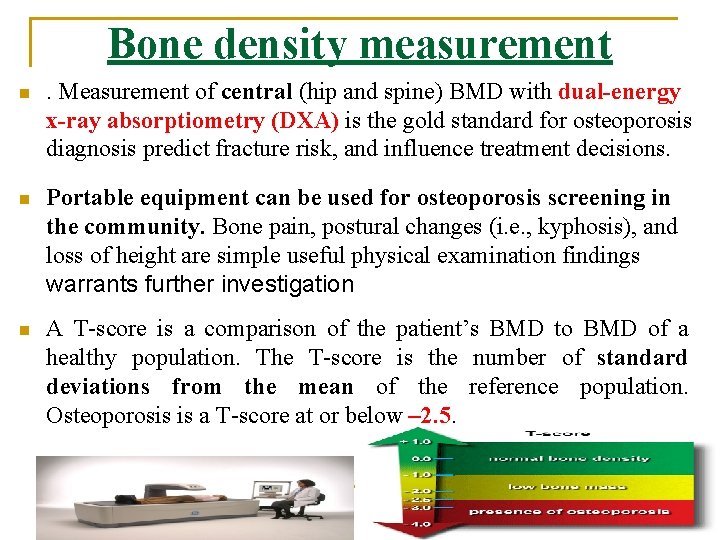
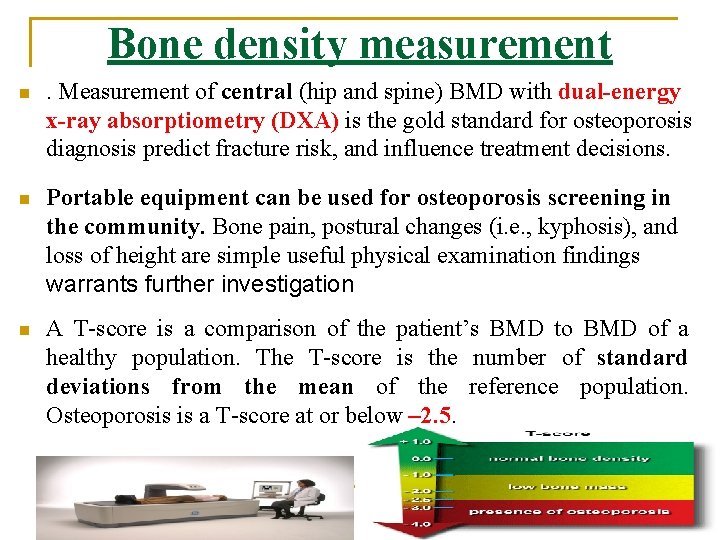
Bone density measurement n . Measurement of central (hip and spine) BMD with dual-energy x-ray absorptiometry (DXA) is the gold standard for osteoporosis diagnosis predict fracture risk, and influence treatment decisions. n Portable equipment can be used for osteoporosis screening in the community. Bone pain, postural changes (i. e. , kyphosis), and loss of height are simple useful physical examination findings warrants further investigation n A T-score is a comparison of the patient’s BMD to BMD of a healthy population. The T-score is the number of standard deviations from the mean of the reference population. Osteoporosis is a T-score at or below – 2. 5. 15
Treatment Desired Outcome n n n reducing pain and deformity, and improving quality of life Optimize and stabilize bone mass reduce the future incidence of osteoporosis improving functional capacity and mobility identify risk factors for developing osteoporosis and resolve reversible risks. This require both pharmacologic and non-pharmacologic treatment 16
NON PHARMACOLOGIC TREATMENT n Because excessive caffeine consumption increases calcium excretion, caffeine intake should ideally be limited. n Smoking cessation: Cigarette smoking is associated with up to an 80% increased relative risk for hip fracture. n Alcohol increased risk for osteoporosis. Alcohol increases bone resorption by increasing RANKL and decreases bone formation by increasing oxidative stress n Physical activity or exercise prevents osteoporotic fractures. It decrease the risk of falls and fractures by improving muscle strength, coordination, balance, and mobility. 17
Diet n A well-balanced diet with adequate calcium and vitamin D is essential for healthy bones mainly Dairy products (milk and cheese). Vitamin K is a cofactor for carboxylation (activation) of proteins, such as osteocalcin, involved in bone formation. Vitamin K deficiency can contribute to bone loss and increase fracture risk. (vit K supply is questionable) n n Isoflavones: phytoestrogens are plant-derived compounds that possess weak estrogenic agonist and antagonist effects throughout the body EX: Genistein is isoflavone in soybeans available as a supplement or part of a calcium combination product. 18
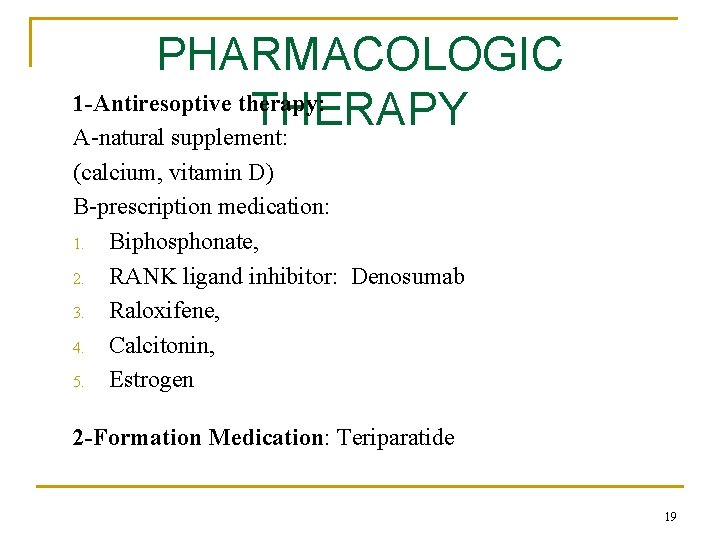
PHARMACOLOGIC 1 -Antiresoptive therapy: THERAPY A-natural supplement: (calcium, vitamin D) B-prescription medication: 1. Biphosphonate, 2. RANK ligand inhibitor: Denosumab 3. Raloxifene, 4. Calcitonin, 5. Estrogen 2 -Formation Medication: Teriparatide 19
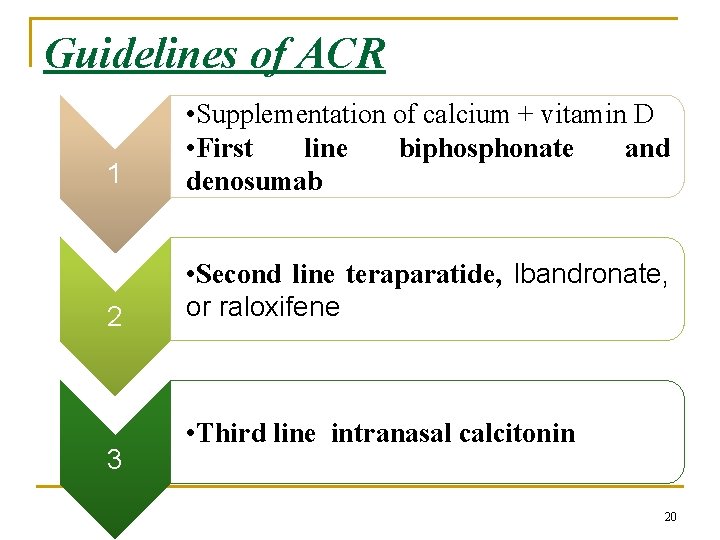
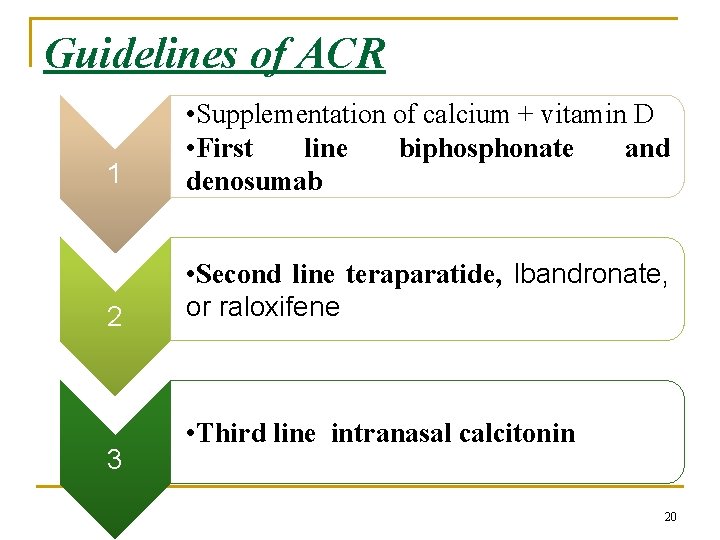
Guidelines of ACR 1 • Supplementation of calcium + vitamin D • First line biphosphonate and denosumab 2 • Second line teraparatide, Ibandronate, or raloxifene 3 • Third line intranasal calcitonin 20
Calcium n taken in adequate amounts to prevent bone destruction. Usually combined with vitamin D and osteoporosis medications n Calcium carbonate (Calcimate®) is the salt of choice because it contains the highest concentration of elemental calcium (40%) and is the least expensive. It should be ingested with meals to enhance absorption from increased acid secretion. Calcium citrate or acetate: absorption is acid independent and need not be taken with meals. maximum single doses of 600 mg or less of elemental calcium are recommended n n n SE: Constipation treated with increased water intake, and dietary fiber
Vitamin D 3 Vitamin D deficiency results from insufficient intake, decreased sun exposure, decreased skin production, decreased liver and renal metabolism n Vitamin D and PTH work together to maintain calcium homeostasis. Supplemental vitamin D maximizes intestinal calcium absorption and has been shown to increase BMD n Dose: 200– 1000 units/day. n Usually found as alone or combination with calcium or as alfacalcidol “Bone one®”(vitamin D precursor) 22
Bisphonates (eg. Alendronate (Fosamax), risedronate (Actonel), ibandronate (bonaprove), zoledronic acid) -Binds to bone, inhibits osteoclast activity bisphonates provide the greatest BMD increases and fracture risk reductions. Fracture reductions are demonstrated as early as 6 months. BMD increases are dose dependent. After discontinuation, the increased BMD is sustained for a prolonged period for years Taken once daily, once weekly, once monthly. Most patients prefer once-weekly or once-monthly bisphonate administration over daily therapy
Bisphonates -Available in tablet mainly or may injectable forms (IV) -Tablets are poorly absorbed (bioavailability 1% to 5%) but work well if taken correctly. Take on empty stomach in the morning with at least 200 ml of plain tap water (not coffee, juice, mineral water, or milk) Remain upright and do not eat for ½-1 hour after taking Duration of bisphonate therapy has not been defined, but safety data exist for periods of 10 to 13 years adverse effects are Esophageal, gastric, or duodenal irritation, perforation, ulceration, or bleeding. Also, nausea, abdominal pain, and dyspepsia.

Bisphonates
Denosumab (Prolia) n Denosumab is FDA approved for treatment of osteoporosis in women and men at high risk for fracture. Also, to prevent osteoprosis for men receiving androgen-deprivation therapy for nonmetastatic prostate cancer and in women receiving adjuvant aromatase inhibitor therapy for breast cancer. n Denosumab is a fully human monoclonal antibody that binds to RANKL, blocking its activity on receptor n No dosage adjustment is necessary in renal impairment 26
Denosumab n The BMD effects are similar to weekly alendronate. n Activity appears to dissipate upon medication discontinuation n The product is available as a refrigerated prefilled pen or single -use vial administered subcutaneously n Denosumab was generally well tolerated. Dermatologic reactions not specific to the injection site such as dermatitis, eczema, and rash. Serious infections including skin infections. If any signs of skin infection such as cellulitis. 27
q Parathyroid Hormone (eg. The first 34 amino acids in human parathyroid hormone, Stimulates teriparatide) more bone formation than resorption q q (second line): Used for those who cannot tolerate bisphonates or who continue to have fractures on bisphonates Discontinuation of therapy results in a decrease in BMD, but some antifracture efficacy appears to be maintained. Provided as a daily SC injection or as pen. The initial dose should be given lying or sitting to avoid orthostatic hypotension Transient hypercalcemia may occur (calcium monitoring)
Estrogen Agonist/Antagonist (eg. Raloxifene) n estrogen agonists antagonists (known previously as selective estrogen receptor modulators or SERMs). Raloxifene (Evista®) is an estrogen agonist on bone but an antagonist on the breast and uterus. is approved for prevention and treatment of postmenopausal osteoporosis. Less effective than bisphonates, After discontinuation, the beneficial effect is lost and bone loss returns SE: DVT and stroke risk. Endometrial bleeding.
Estrogen therapy (ET) q q q Protective anti-resorptive effect for post menopausal osteoprosis For short term treatment to avoid SE: Increases the incidence of breast cancer, coronary heart disease, stroke, and venous thromboembolism. less than those from bisphonates or teriparatide but greater than those from raloxifene or calcitonin. Effect on BMD is dose dependent When ET is discontinued, fracture protection is lost. Available as oral and transdermal preparation
Calcitonin Hormone released from the thyroid gland Binds to osteoclasts, inhibits resorption Salmon-derived because more potent and longer lasting Less effective than other treatments (third line) Helpful in reducing pain from fractures of spine mainly. it should be prescribed for short-term treatment (4 weeks) Nasal spray is most popular preparation > SC route. The intranasal dose is 200 units daily, alternating nares every other day. Subcutaneous administration of 100 units daily is available but rarely used because of adverse effects (allergic reaction, rhinitis and epistaxis) and high cost
Testosterone n Although it is not FDA indicated for osteoporosis, the male osteoporosis guideline recommends testosterone alone for men with testosterone concentrations <200 ng/d. L if low fracture risk and in combination with an osteoporosis medication if fracture risk is High n Testosterone is converted to estradiol, which decreases bone resorption in men and women. n Testosterone has increased BMD in men with low testosterone concentrations, but has no effect if testosterone concentrations are normal n Preparation: capsule or injection, gels 32
EVALUATION OF THERAPEUTIC OUTCOMES q BMD measurements can be obtained every 1 to 2 years for monitoring bone loss and treatment response. n Patients should be asked about possible fracture symptoms (e. g. , bone pain, disability) at each visit. n Medication adherence and tolerance and side effects should be evaluated at each visit.
GLUCOCORTICOID-INDUCED OSTEOPOROSIS n The most commonly drug-induced osteoporosis. It Decrease osteoblast activity, increase resorption, decrease calcium absorption, increase renal calcium excretion n Oral daily doses greater than 7. 5 mg of prednisone or equivalent show significant risk. n Bone losses are rapid, with the greatest decrease occurring during the first 6 to 12 months of therapy. n inhaled glucocorticoids have no effect on BMD or fracture risk unless high doses is used (greater than 800 to 1200 mcg for beclomethasone (clenil) 800 to 1000 mcg for budesonide(miflonide), 750 mcg for fluticasone (flixotide) 34
TREATMENT n According to the American College of Rheumatology (ACR) guidelines. All patients starting or receiving long-term systemic glucocorticoid therapy should: n 1 -receive at least 1, 500 mg elemental calcium and 800 to 1, 200 units of vitamin D daily and practice a bone-healthy lifestyle. n 2 - measuring BMD at the beginning of chronic therapy and follow up monitoring with DXA in 6 to 12 months. n 3 -receive preventive bisphonate therapy if GC will be used for more than 3 months. n 4 -Bisphonates are the best therapeutic choice for patients with teriparatide is the second choice. 35
 Collection of well defined objects is called
Collection of well defined objects is called Alendronate brand name
Alendronate brand name Osteoporosis
Osteoporosis Pes statement for osteoporosis
Pes statement for osteoporosis Osteoporosis t score
Osteoporosis t score Is osteoporosis hypokinetic or hyperkinetic
Is osteoporosis hypokinetic or hyperkinetic Defination of osteoporosis
Defination of osteoporosis Osteoporosis subjective data
Osteoporosis subjective data Pathway hiperkalemia
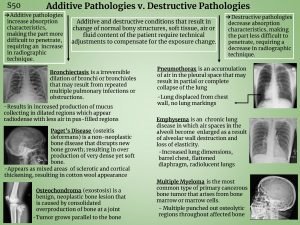
Pathway hiperkalemia Additive pathology in radiography
Additive pathology in radiography Royal osteoporosis society leaflets
Royal osteoporosis society leaflets Osteoporosis
Osteoporosis Osteoporosis
Osteoporosis Tbs osteoporosis
Tbs osteoporosis International osteoporosis foundation
International osteoporosis foundation Osteoporosis
Osteoporosis Define piecewise function
Define piecewise function Real life situation using piecewise function
Real life situation using piecewise function Work physics definition
Work physics definition Finance can be defined as
Finance can be defined as Slurry definition cooking
Slurry definition cooking Usability quality attribute that assesses
Usability quality attribute that assesses What is conflick
What is conflick Ambiguously defined triangle
Ambiguously defined triangle Concept of learning ppt
Concept of learning ppt Cognitive affective personality system
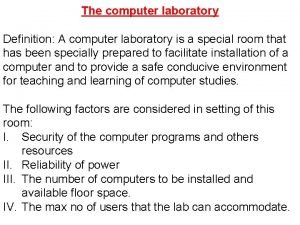
Cognitive affective personality system Definition of computer laboratory
Definition of computer laboratory What can be defined as the art and science of formulating
What can be defined as the art and science of formulating Quantitative study of reactants and products
Quantitative study of reactants and products Stoichiometry is defined as the quantitative study of
Stoichiometry is defined as the quantitative study of 7 ci
7 ci Sdn architecture vs traditional network
Sdn architecture vs traditional network Which greek philosopher defined the art of persuasion
Which greek philosopher defined the art of persuasion Sql user defined table
Sql user defined table Terrestrial biomes definition
Terrestrial biomes definition Onomatopoeia definition and examples
Onomatopoeia definition and examples