Sealants Preventive Resins and Posterior Composites Department of









- Slides: 34
Sealants, Preventive Resins and Posterior Composites Department of Pediatric Dentistry University of Isfahan medical sciences 2009
Sealants • Indications – Recently erupted teeth – Tooth can be isolated – No, or only minimal pit and fissure staining – No, or only minimal “catches” in the grooves – No evidence of radiographic caries
Sealants • Material in Y/O Clinic – Ultraseal XT ® plus™ – Manufacturer: Ultradent – Advantages • • • High strength Filled resin sealant (approximately 60% ) Low shrinkage Clinically and radiographically opaque Fluoride releasing May be used for sealants and microrestorative (PRR’s)
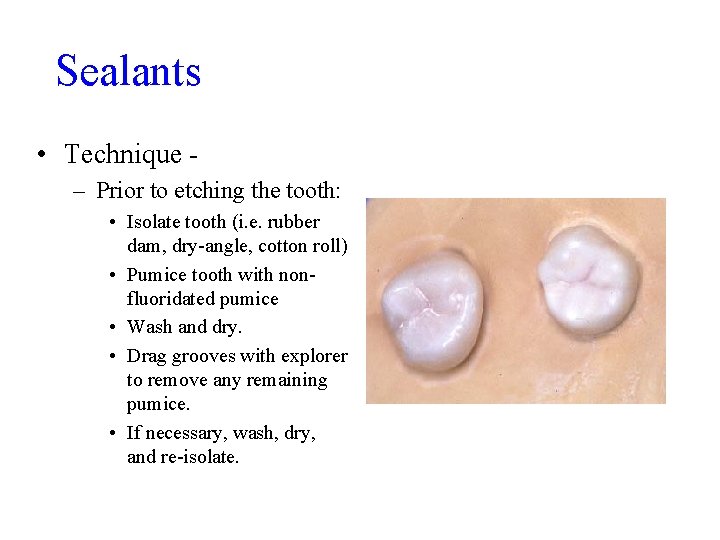
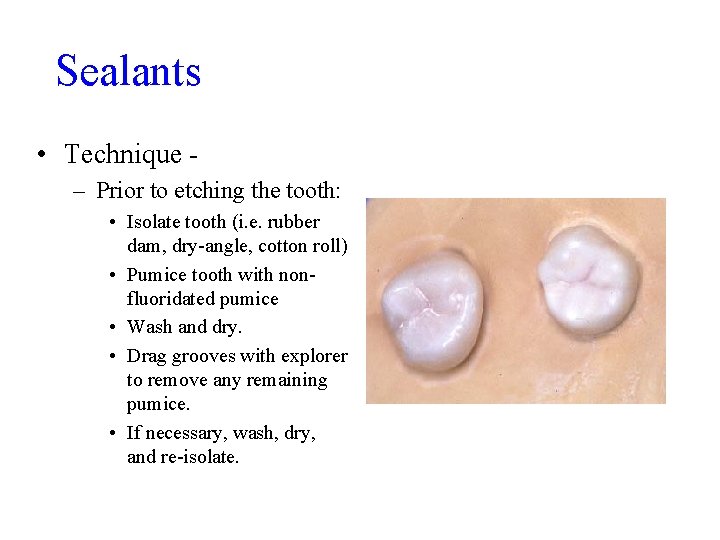
Sealants • Technique – Prior to etching the tooth: • Isolate tooth (i. e. rubber dam, dry-angle, cotton roll) • Pumice tooth with nonfluoridated pumice • Wash and dry. • Drag grooves with explorer to remove any remaining pumice. • If necessary, wash, dry, and re-isolate.

Sealants • Etching: - 35% PA – Deliver to the tooth using the blue tip, or using a microbrush – Etch the grooves and cuspal inclines – Etch for 15 seconds – Wash for 10 seconds – Evaluate “frosted” enamel
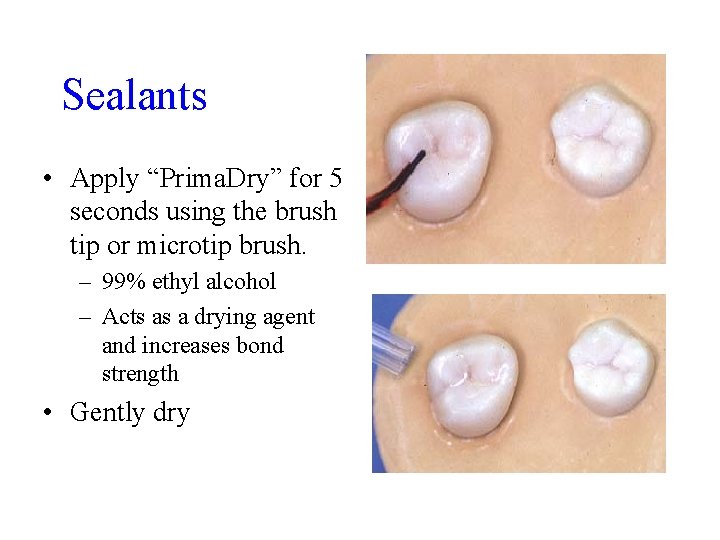
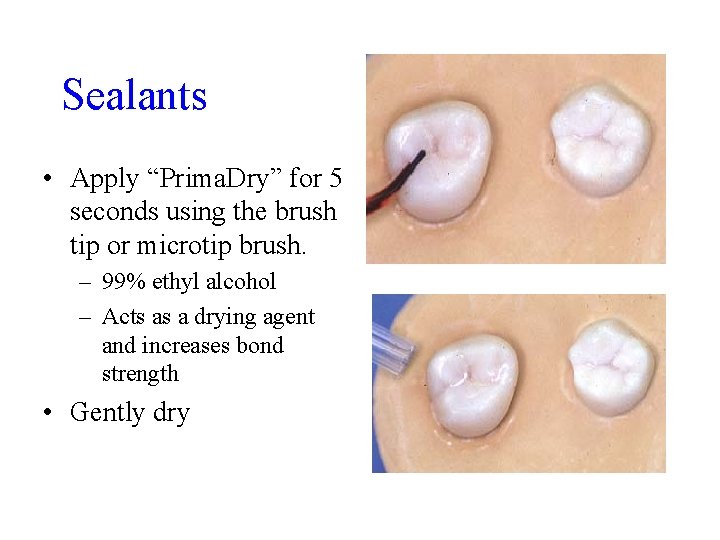
Sealants • Apply “Prima. Dry” for 5 seconds using the brush tip or microtip brush. – 99% ethyl alcohol – Acts as a drying agent and increases bond strength • Gently dry
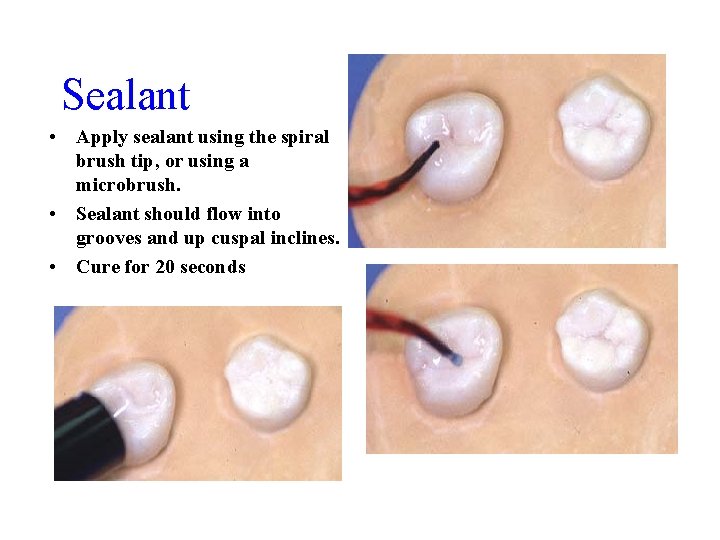
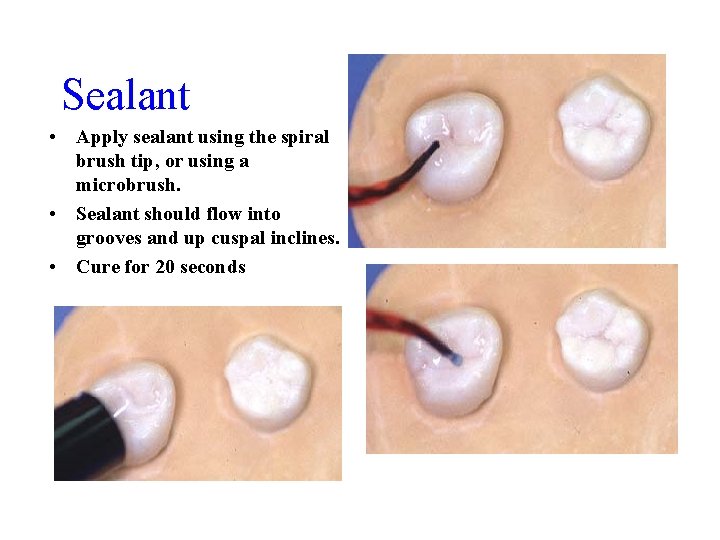
Sealant • Apply sealant using the spiral brush tip, or using a microbrush. • Sealant should flow into grooves and up cuspal inclines. • Cure for 20 seconds
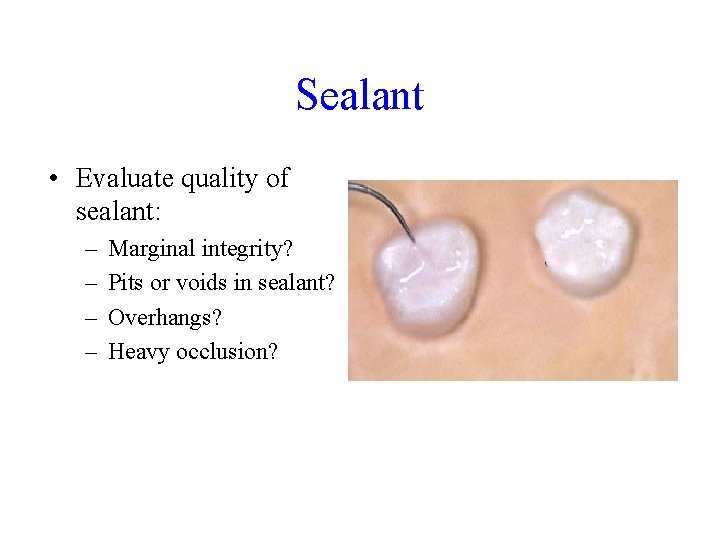
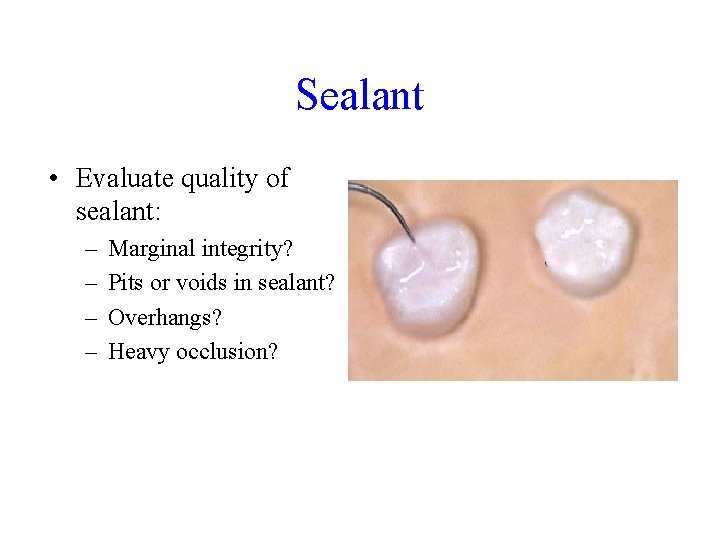
Sealant • Evaluate quality of sealant: – – Marginal integrity? Pits or voids in sealant? Overhangs? Heavy occlusion?
Sealants • Areas of concern – Retention rates on buccal pits and grooves of mandibular molars and distolinqual grooves of maxillary molars – Sealants need periodic maintenance • Moisture contamination secondary to incomplete eruption and difficulty in isolation - predicted 30% failure rate within 5 years in these areas. • Marginal integrity and wear.
Preventive Resins Restorations • Indications – Tooth can be isolated. – No, or only minimal pit and fissure staining – Minimal “catches” in the grooves, or areas with distinct incipient enamel caries. – No evidence of radiographic caries.

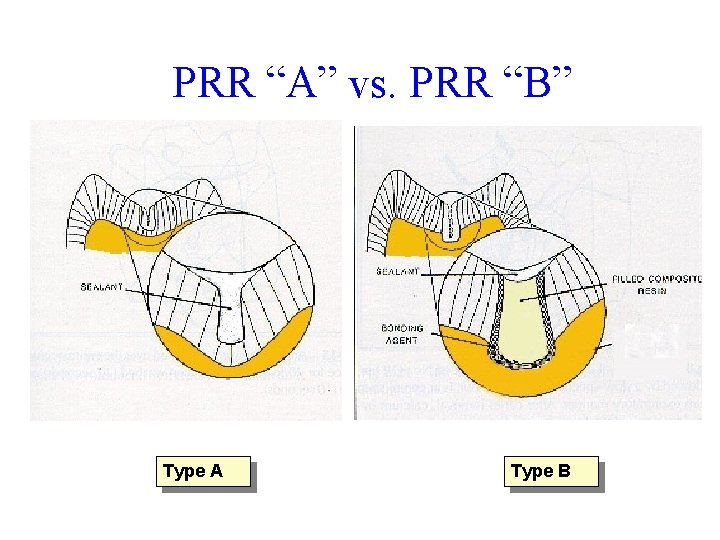
Preventive Resin Restorations • Type A – Caries is incipient and limited to enamel – No radiographic caries Many clinical situations can not be classified according to type until the operator has completed the required exploratory preparation • Type B – Caries extends minimally into dentin and is small and confined – No radiographic findings
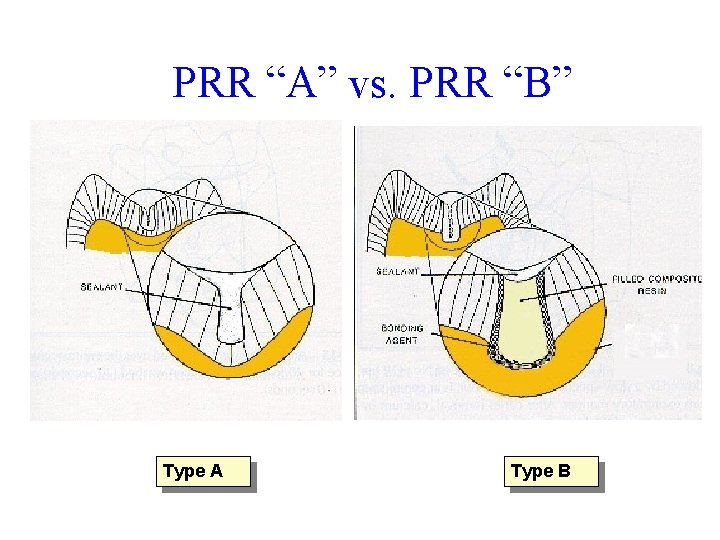
PRR “A” vs. PRR “B” Type A Type B

Preventive Resin • Isolate tooth (i. e. rubber dam, dry-angle, cotton roll) • Pumice tooth with nonfluoridated pumice • Wash and dry. • Drag grooves with explorer to remove any remaining pumice. • If necessary, wash, dry, and re -isolate.
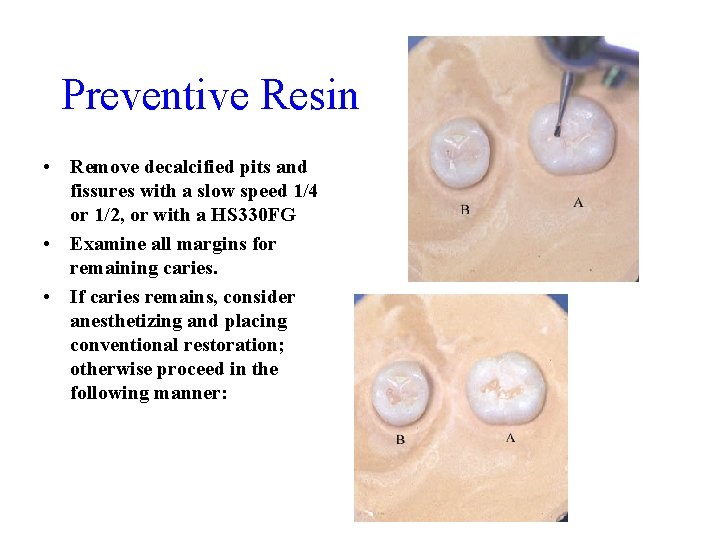
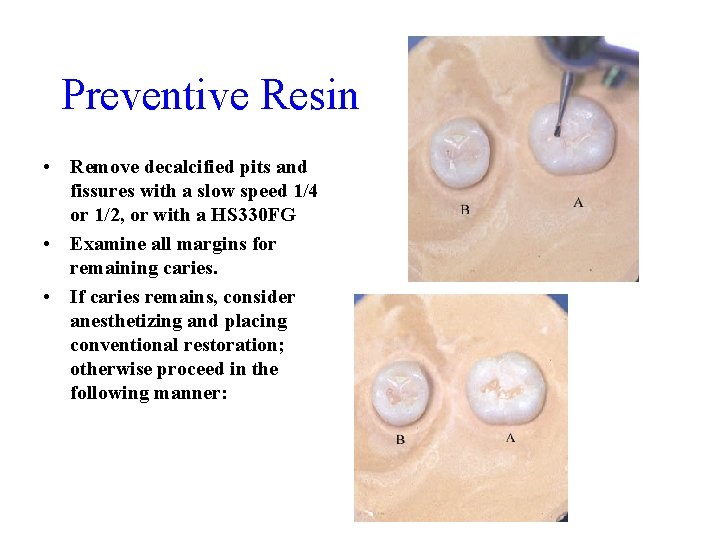
Preventive Resin • Remove decalcified pits and fissures with a slow speed 1/4 or 1/2, or with a HS 330 FG • Examine all margins for remaining caries. • If caries remains, consider anesthetizing and placing conventional restoration; otherwise proceed in the following manner:
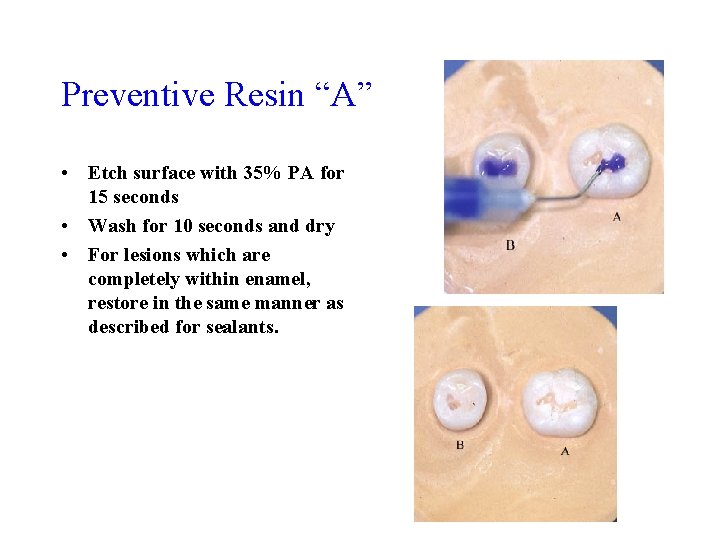
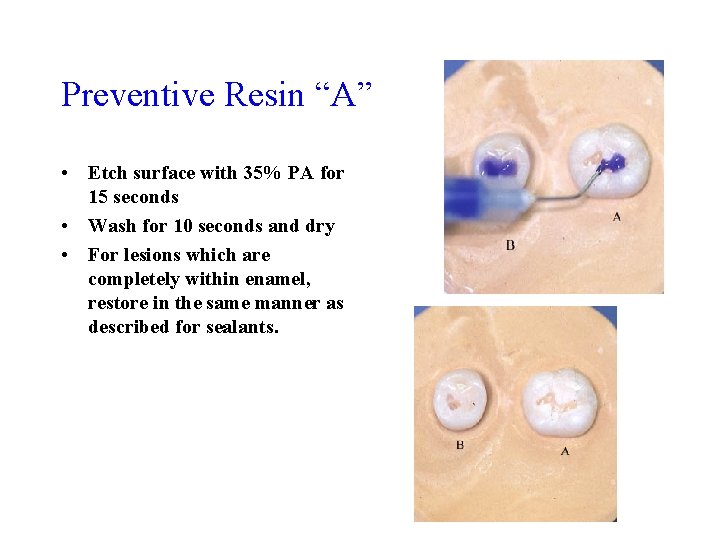
Preventive Resin “A” • Etch surface with 35% PA for 15 seconds • Wash for 10 seconds and dry • For lesions which are completely within enamel, restore in the same manner as described for sealants.
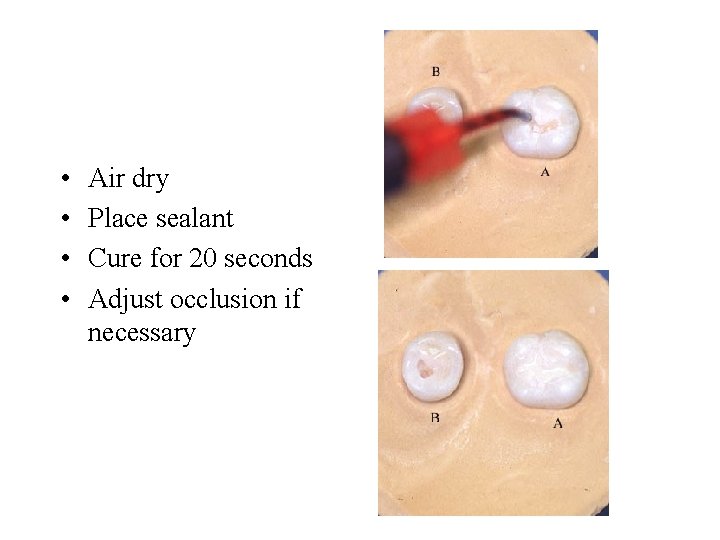
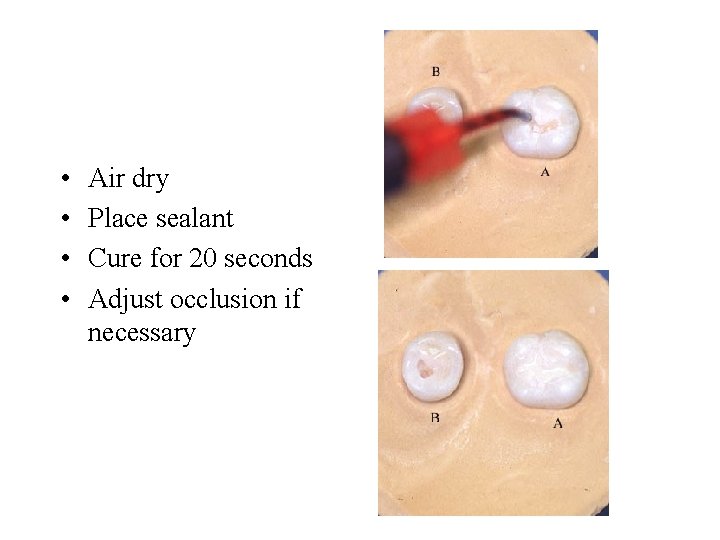
• • Air dry Place sealant Cure for 20 seconds Adjust occlusion if necessary
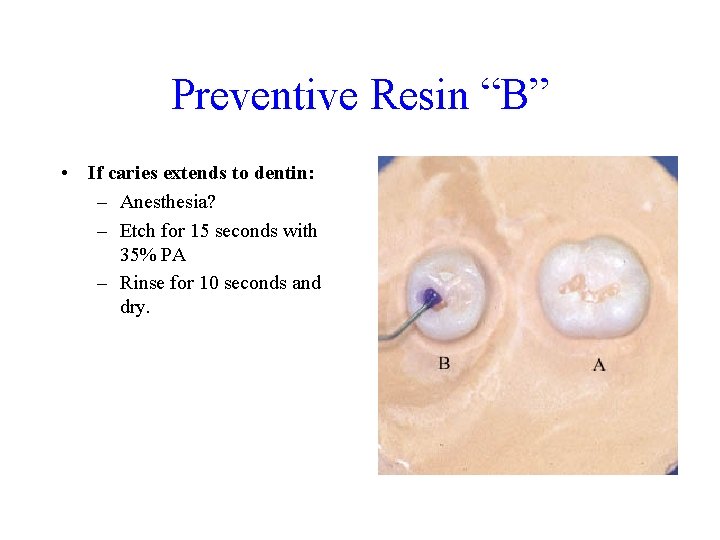
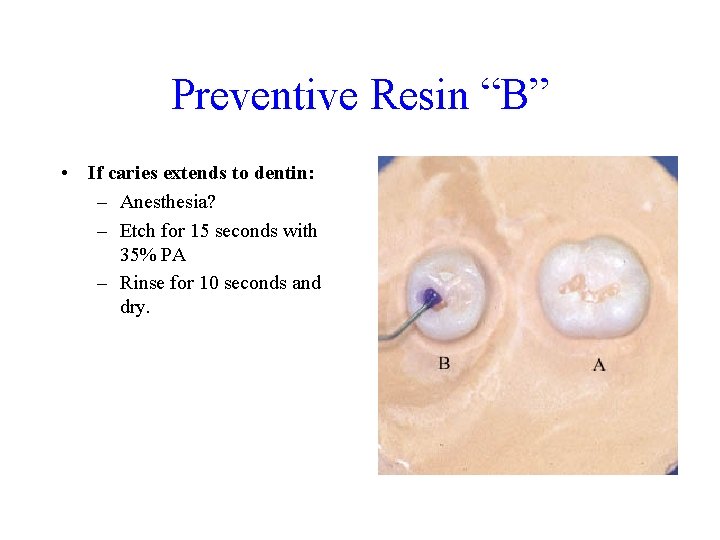
Preventive Resin “B” • If caries extends to dentin: – Anesthesia? – Etch for 15 seconds with 35% PA – Rinse for 10 seconds and dry.
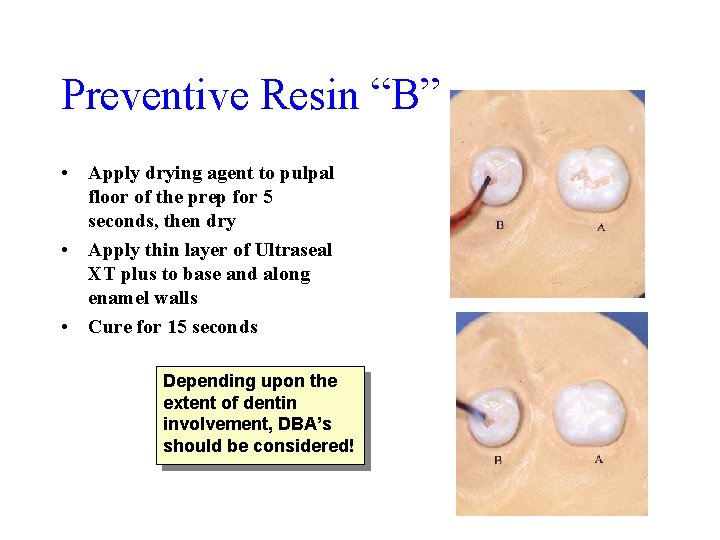
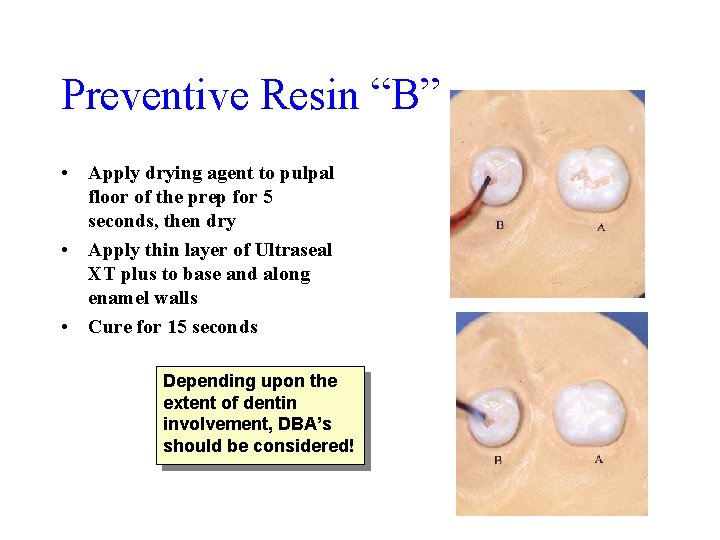
Preventive Resin “B” • Apply drying agent to pulpal floor of the prep for 5 seconds, then dry • Apply thin layer of Ultraseal XT plus to base and along enamel walls • Cure for 15 seconds Depending upon the extent of dentin involvement, DBA’s should be considered!
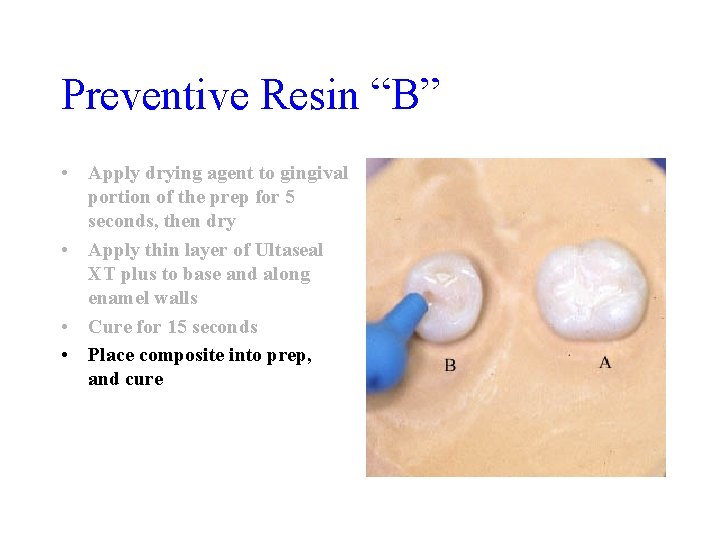
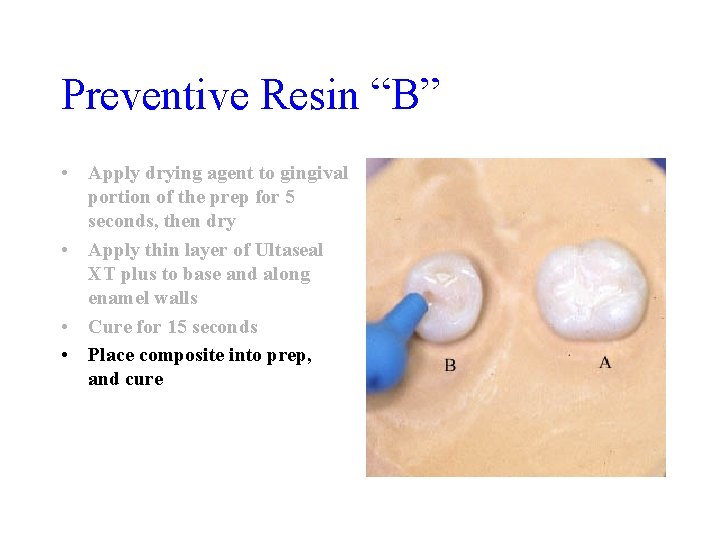
Preventive Resin “B” • Apply drying agent to gingival portion of the prep for 5 seconds, then dry • Apply thin layer of Ultaseal XT plus to base and along enamel walls • Cure for 15 seconds • Place composite into prep, and cure

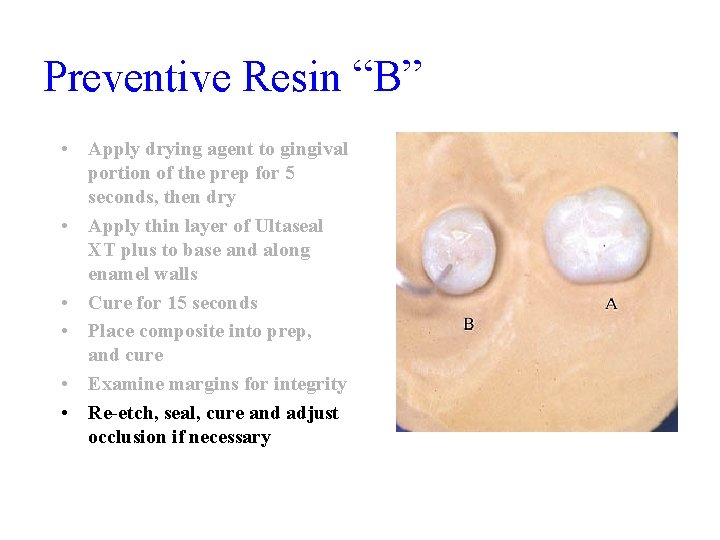
Preventive Resin “B” • Apply drying agent to gingival portion of the prep for 5 seconds, then dry • Apply thin layer of Ultaseal XT plus to base and along enamel walls • Cure for 15 seconds • Place composite into prep, and cure • Examine margins for integrity
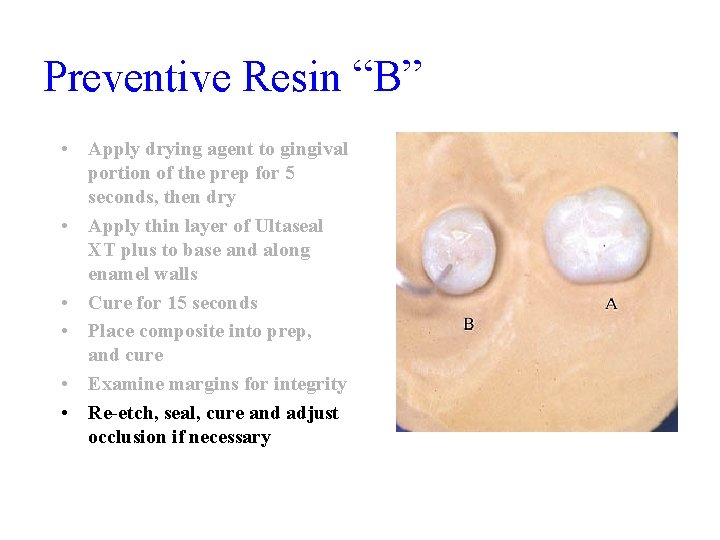
Preventive Resin “B” • Apply drying agent to gingival portion of the prep for 5 seconds, then dry • Apply thin layer of Ultaseal XT plus to base and along enamel walls • Cure for 15 seconds • Place composite into prep, and cure • Examine margins for integrity • Re-etch, seal, cure and adjust occlusion if necessary
Posterior Composite • Indications – Non-stress bearing area of the tooth - occlusal contacts in natural enamel – High esthetic demand by the patient – Conservative restoration in nature • Buccal linqual width not greater than 1/3 of occlusal table • All margins must be free of caries/decalcification • Rounded internal line angles
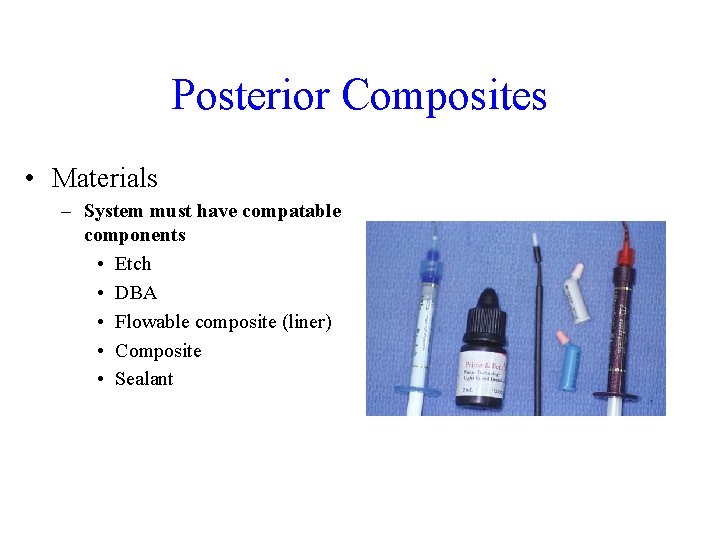
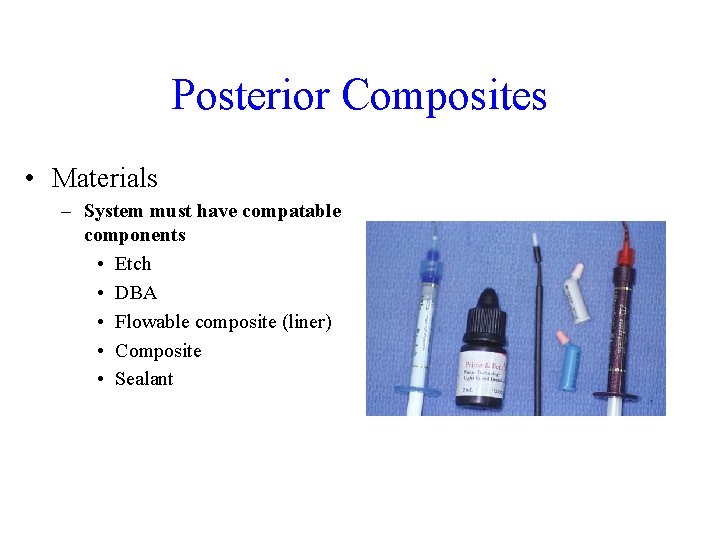
Posterior Composites • Materials – System must have compatable components • Etch • DBA • Flowable composite (liner) • Composite • Sealant

Posterior Composites • Select teeth appropriately – – Small confined lesions “chasing” grooves Decalcified grooves Minimal radiographic involvement – Outline can avoid heavy occlusal contact
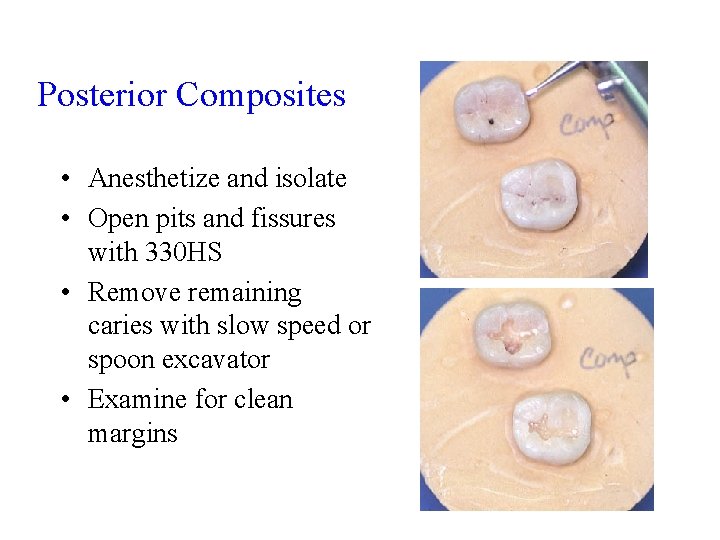
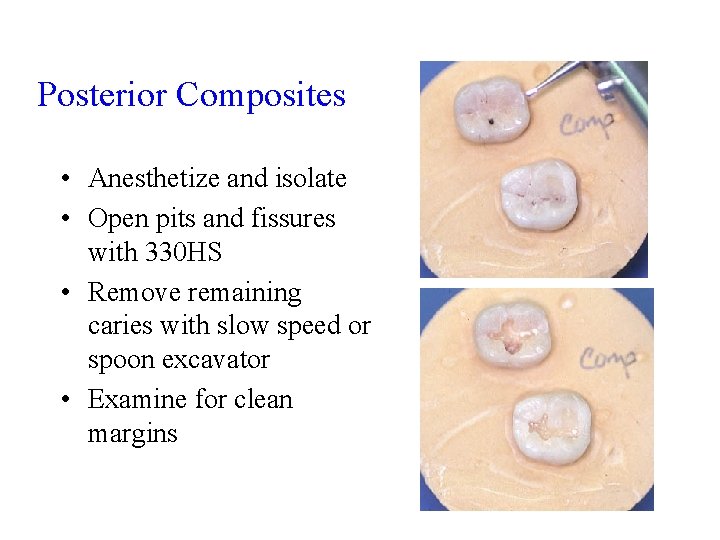
Posterior Composites • Anesthetize and isolate • Open pits and fissures with 330 HS • Remove remaining caries with slow speed or spoon excavator • Examine for clean margins

Posterior Composites • Utilize total etch technique • In cases of deep caries, it may be beneficial to place a glass ionomer liner • Etch for 20 seconds and rinse. • Dry, but DO NOT desicate the dentin
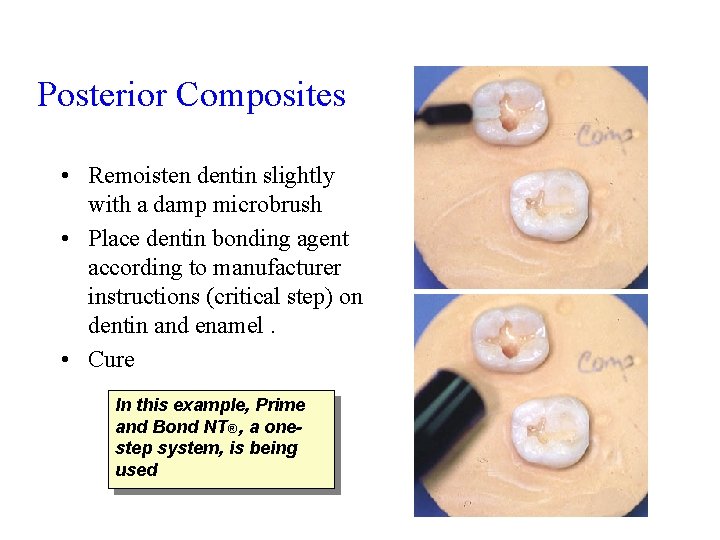
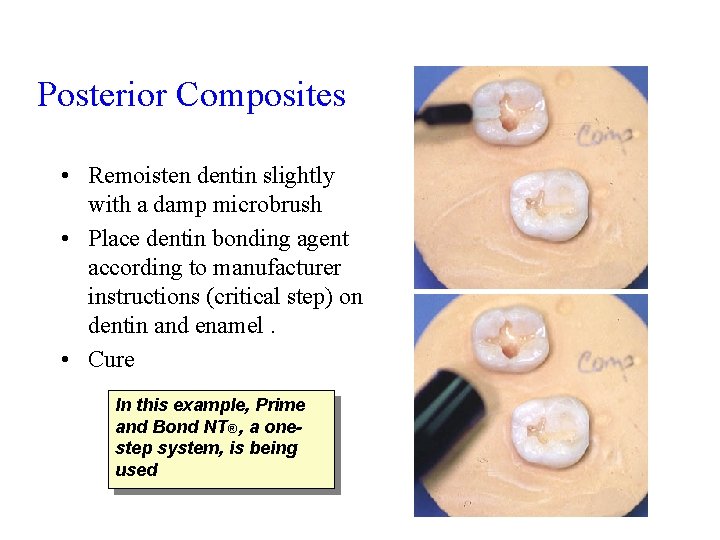
Posterior Composites • Remoisten dentin slightly with a damp microbrush • Place dentin bonding agent according to manufacturer instructions (critical step) on dentin and enamel. • Cure In this example, Prime and Bond NT® , a onestep system, is being used

Posterior Composites • Place flowable composite on pulpal floor – Acts as a stress breaker during curing – Minimizes shrinkage and gap formation • Cure

Posterior Composites • Place composite incrementally, beginning with eventual cuspal areas. • Cure between increments minimizes overall shrinkage and gap formation

Posterior Composites • Adjust occlusion if required • Finish composite in the usual manner with high speed finishing burs and polishing points
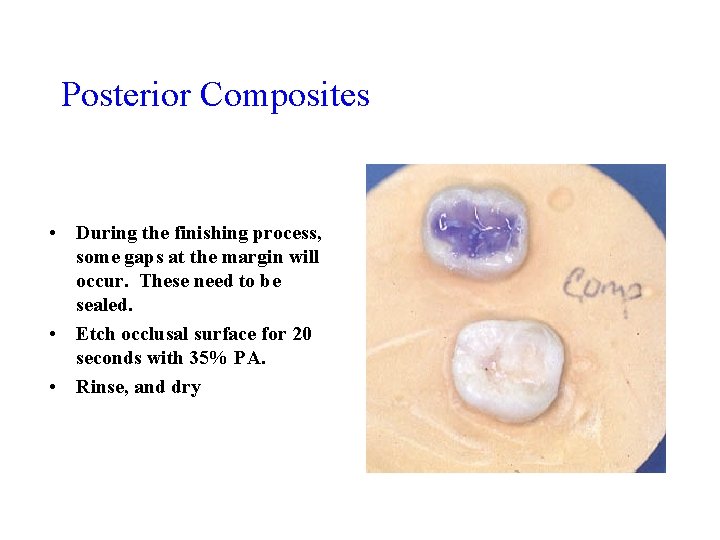
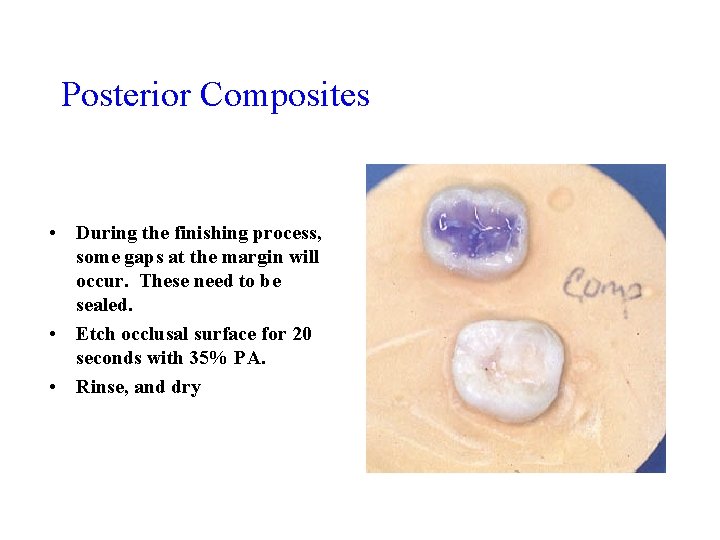
Posterior Composites • During the finishing process, some gaps at the margin will occur. These need to be sealed. • Etch occlusal surface for 20 seconds with 35% PA. • Rinse, and dry
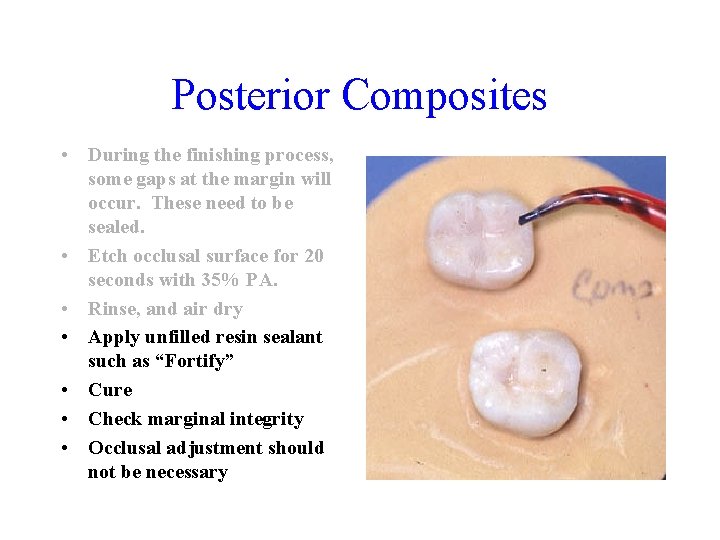
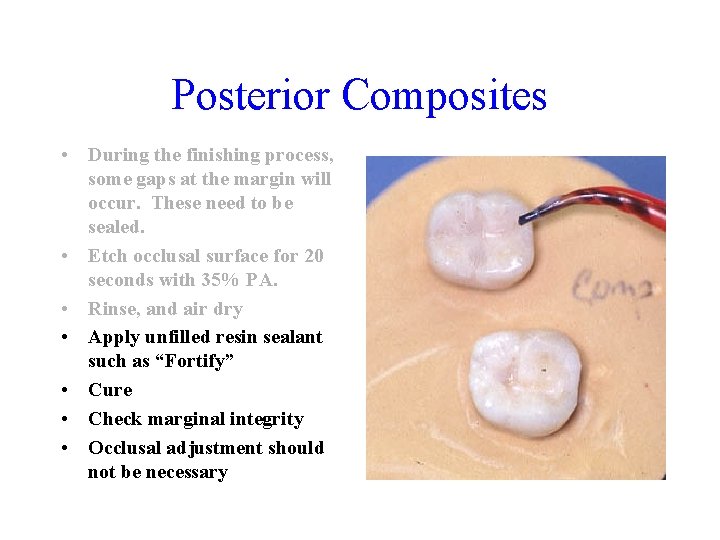
Posterior Composites • During the finishing process, some gaps at the margin will occur. These need to be sealed. • Etch occlusal surface for 20 seconds with 35% PA. • Rinse, and air dry • Apply unfilled resin sealant such as “Fortify” • Cure • Check marginal integrity • Occlusal adjustment should not be necessary
Summary • All techniques are critically dependent upon adequate isolation. If you can’t keep it dry, or keep it dry long enough, it won’t work. • Check for poor margins, overhangs, pits and voids - particulary on DLG’s and buccal grooves. • Failure to adhere to guidelines may result in a poor/failing restoration or post-op sensitivity for the patient
Summary • There is often no clear cut line between the different preventive resin restorations, and PRR’s vs. a conventional posterior composite. • When in doubt, be more aggressive. • DBA systems and composites must compliment each other. With some brands of flowable composite, you need to use a DBA first
 Dental sealant definition
Dental sealant definition Light activated denture base resins
Light activated denture base resins Feve powder coating
Feve powder coating Qenos altona
Qenos altona Acrylization definition
Acrylization definition Qenos resins
Qenos resins Cross linking in denture base resin is contributed by
Cross linking in denture base resin is contributed by Fasteners gaskets seals and sealants
Fasteners gaskets seals and sealants Automotive fasteners gaskets and sealants
Automotive fasteners gaskets and sealants Chapter 59 dental sealants
Chapter 59 dental sealants Chapter 59 dental sealants
Chapter 59 dental sealants Auto bearings and seals
Auto bearings and seals Predisation
Predisation Components and composites ofsted
Components and composites ofsted Ceramic matrix composites definition
Ceramic matrix composites definition Isotropic compliance matrix
Isotropic compliance matrix Dental composite classification
Dental composite classification Composite material definition
Composite material definition Ceramic matrix composites definition
Ceramic matrix composites definition Jeremy nedelka
Jeremy nedelka Meshlin composites zrt
Meshlin composites zrt Mechanical materials
Mechanical materials Maine marine composites
Maine marine composites Vartm process steps
Vartm process steps Composite materials classification
Composite materials classification Composites in sports
Composites in sports Warp clock composites
Warp clock composites What are composite
What are composite Structural composites industries llc
Structural composites industries llc Bts europlastics et composites option conception outillage
Bts europlastics et composites option conception outillage Software program used to create facial composites
Software program used to create facial composites Preventive and predictive maintenance of hydro power plant
Preventive and predictive maintenance of hydro power plant Monash school of public health
Monash school of public health Preventive promotive and curative aspects of health
Preventive promotive and curative aspects of health Supportive discipline
Supportive discipline