SOFT LINERS AND DENTURE ADHESIVES SOFT LINERS INTRODUCTION




- Slides: 85
SOFT LINERS AND DENTURE ADHESIVES
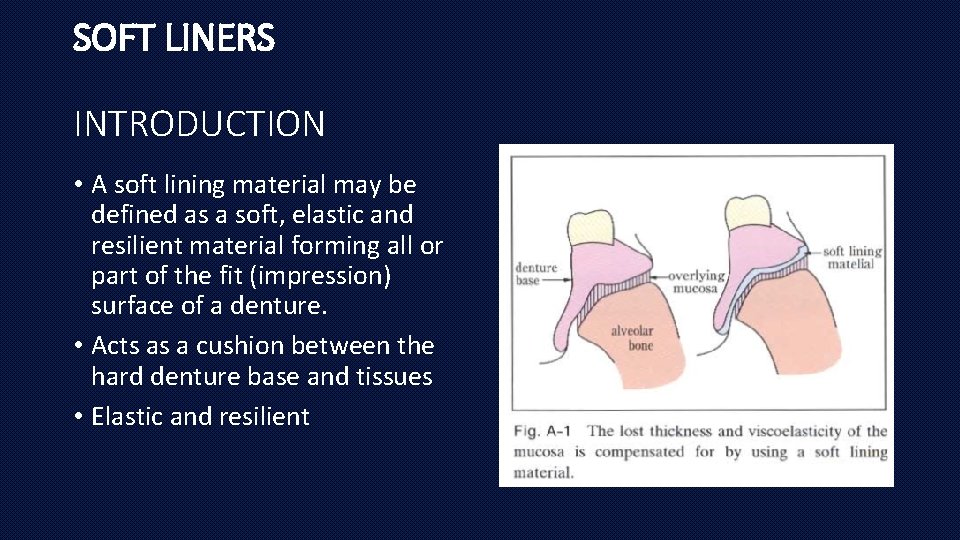
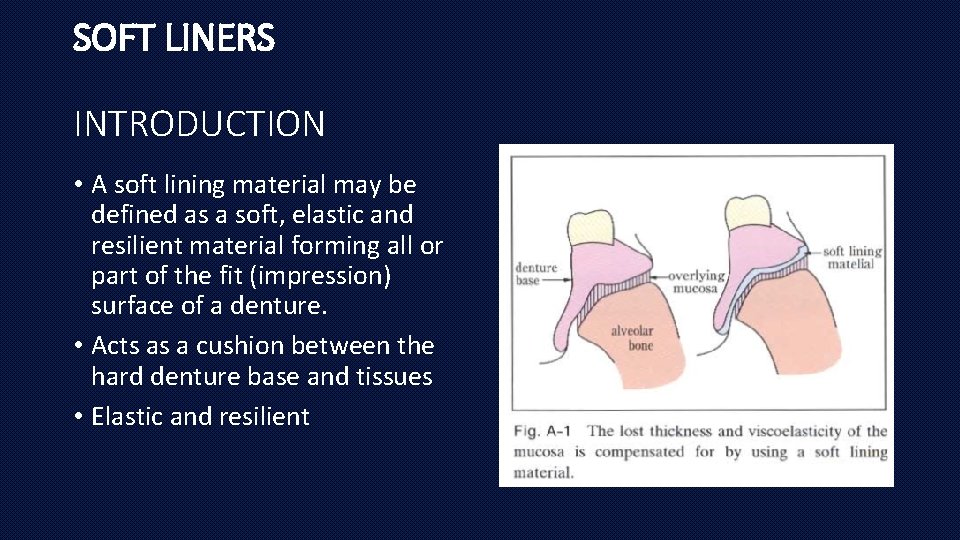
SOFT LINERS INTRODUCTION • A soft lining material may be defined as a soft, elastic and resilient material forming all or part of the fit (impression) surface of a denture. • Acts as a cushion between the hard denture base and tissues • Elastic and resilient
CLASSIFICATION • International Organization for Standardization (ISO) has issued two international standards related to soft liner materials: 1. Resilient lining materials for removable dentures–Part 1: short-term materials and soft lining materials and 2. Resilient lining materials for removable dentures–Part 2: materials for long-term use.
• Based on duration of use 1. Short term liners : Upto 1 month 2. Intermediate liners : 1 -6 months 3. Long term liners : 1 year or longer
• Based on composition: (1) Heat-polymerised acrylic resin (2) auto polymerized acrylic resin (3) heat polymerised silicone, (4) auto polymerized silicone (5) treatment liners (tissue conditioners).
Available Materials • The commercially available soft lining materials generally fall into two basic groups: 1. Silicone type and 2. Acrylic type materials
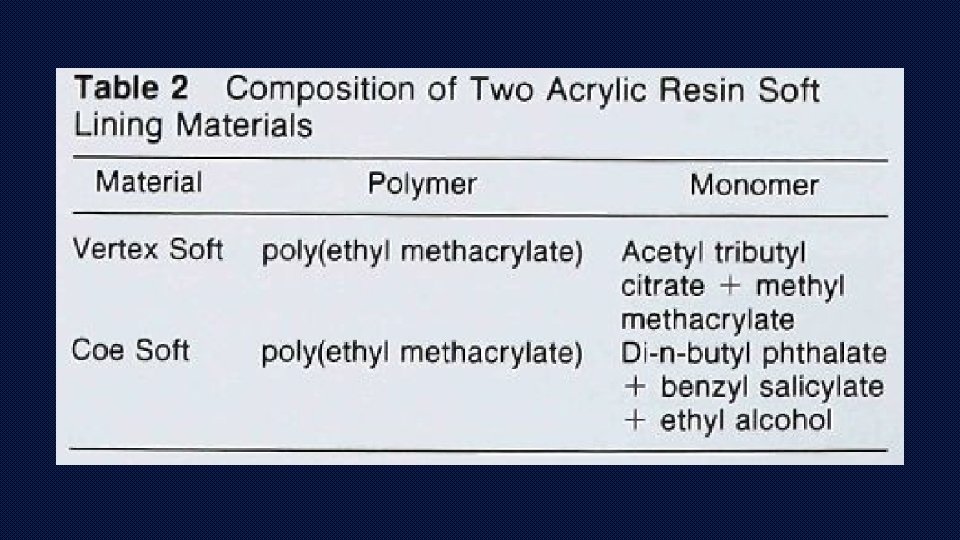
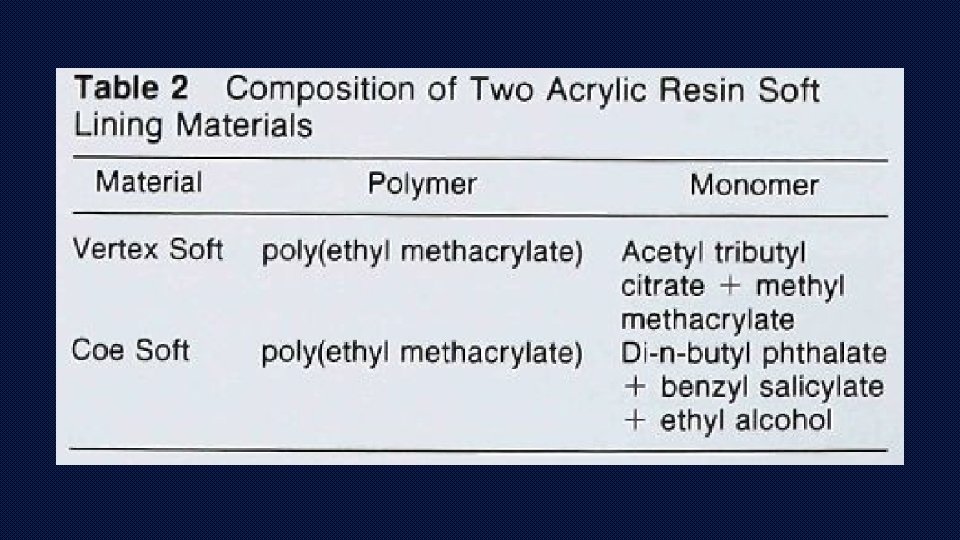
Acrylic resin soft liners Both heat processed and auto-polymerizing types have powder and liquid components • Powder : acrylic polymers and copolymers; benzoyl peroxide- initiator • Liquid : methyl methacrylate monomer and a plasticizer. • Purpose of the plasticizer : usually di-n-butyl phthalate, is to reduce the transition of the polymer from liquid to solid below mouth temperature. • No adhesive is required
Silicone rubber materials • Composed of polymers of dimethyl siloxane—a viscous liquid that can be crosslinked to give good elastic properties. • The crosslinking agent: alkyl-silane • Catalyst: an organometal salt or benzoyl peroxide • E. g. : molloplast b, flexibase.
IDEAL PROPERTIES 1. Ease of processing 2. Minimal dimensional change during processing 3. Water absorption should be minimal 4. Minimal solubility in saliva 5. Resilience 6. Bonding to poly(methyl methacrylate) 7. Adequate tear resistance 8. Easily cleansability and maintenance 9. Nontoxic, odourless, and tasteless 10. Aesthetically acceptable
TREATMENT LINERS / TEMPORARY SOFT LINERS/ TISSUE CONDITIONERS
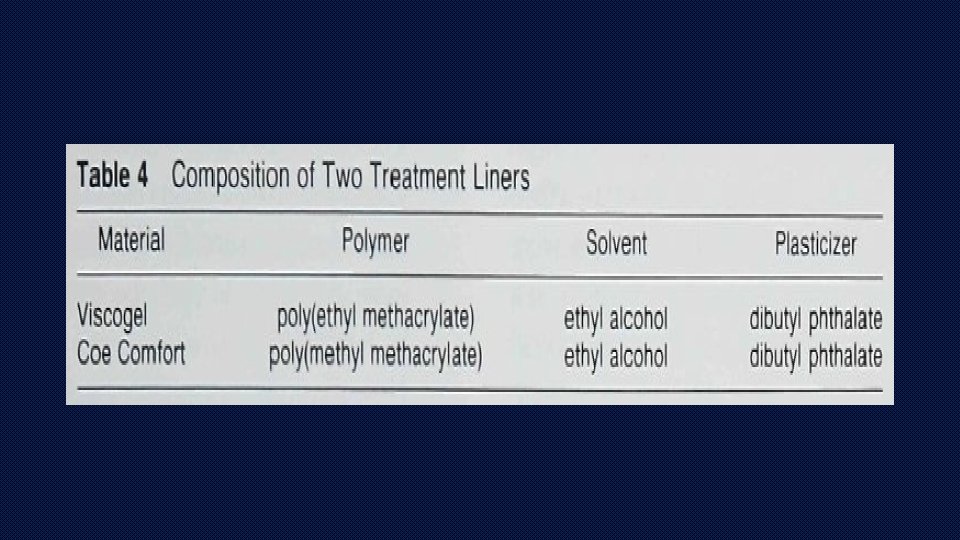
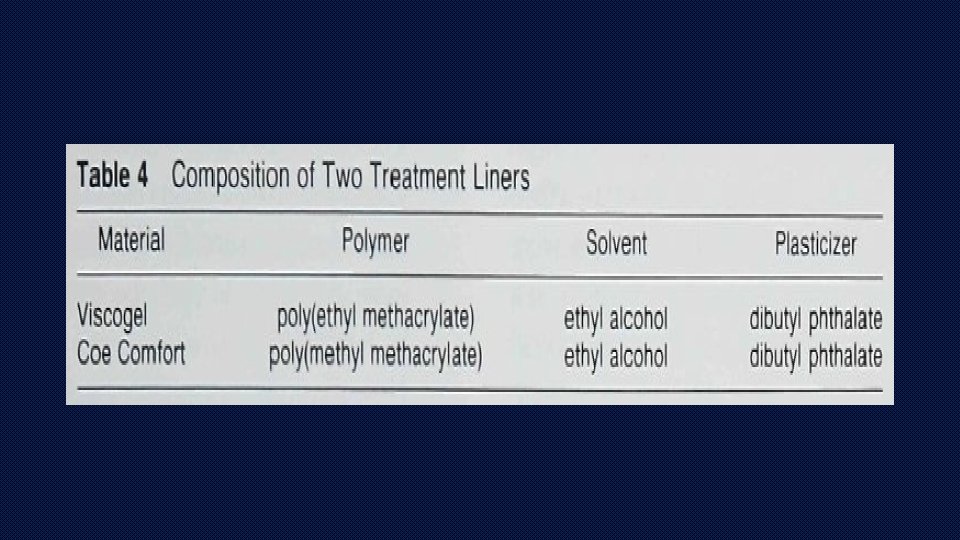
COMPOSITION • Consist of a two-component powder and liquid system • Powder : higher methacrylate, e. g. poly(ethyl methacrylate) and copolymers • Liquid : mixture of ethyl alcohol as solvent and dibutyl phthalate as plasticizer • Leaching and evaporation of these components leads to rapid hardening of the material in the mouth. • Tissue conditioners need to be replaced every 2 -3 days in the mouth
INDICATIONS FOR SHORT TERM SOFT LINERS/ TISSUE CONDITIONERS 1. Treatment and conditioning of abused/ irritated denture supporting tissues prior to impression making for new dentures 2. For provisional adjunctive/ diagnostic purposes such as recovery of vertical dimension of occlusion and correcting occlusion of old prosthesis 3. Temporary relining of immediate dentures/ immediate surgical splints
4. Relining cleft palate speech aids 5. Tissue- conditioning during implant healing 6. Functional impression materials
MECHANISM OF GELATION • Gelation of tissue conditioners is a physical process ( devoid of any chemical reaction or any monomeric substances that could cause tissue irritation). • Upon mixing the powder and liquid, the alcohol and plasticizer mix diffuses into the swellable acrylic beads. • Gelation involves the entanglement of outer polymer chains of swollen beads, resulting in a tacky set gel with high cohesive properties.
MECHANISM OF ACTION • Tissue conditioners show combination of both viscous fluid and elastic solid behaviour • Viscous behaviour allows adaptation gel to inflamed/ irritated mucosa, improving the fit of denture • During chewing, the material demonstrates a time dependent elastic behaviour that allows it to recover initial deformation, absorbing impact forces and cushioning the underlying tissues. • Short-term soft liners used for functional impressions differ from those used for tissue conditioning • Functional impression material should display good flow but with minimal elastic recovery, and exhibit adequate dimensional stability in terms of weight change , water sorption and solubility
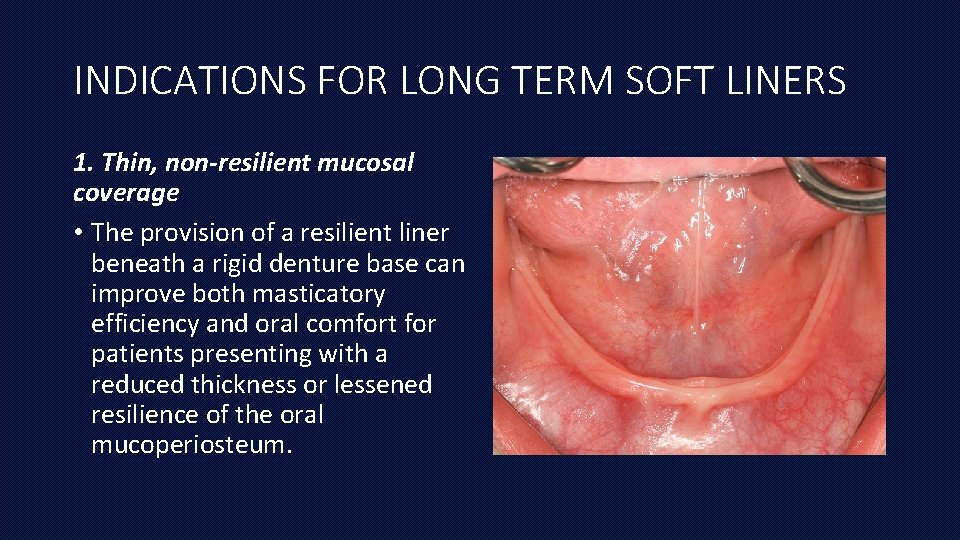
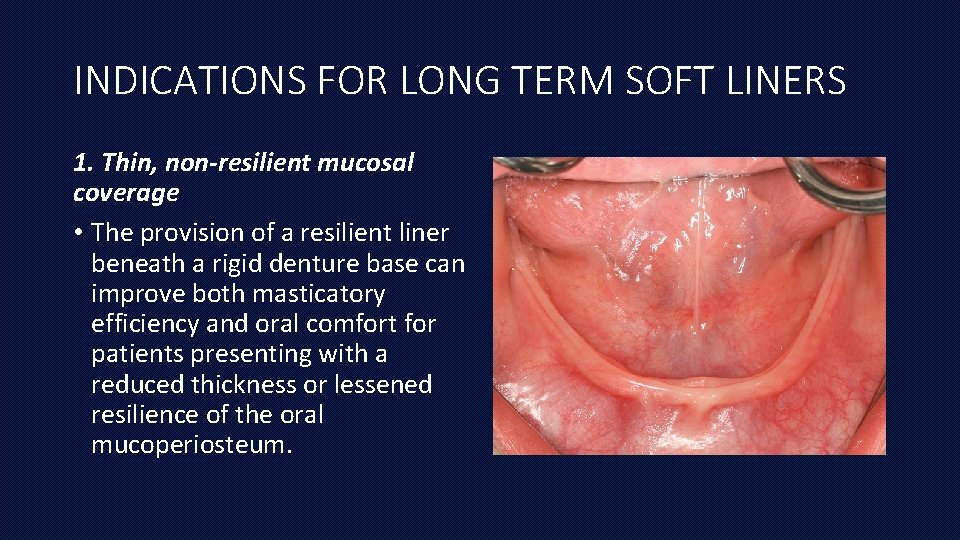
INDICATIONS FOR LONG TERM SOFT LINERS 1. Thin, non-resilient mucosal coverage • The provision of a resilient liner beneath a rigid denture base can improve both masticatory efficiency and oral comfort for patients presenting with a reduced thickness or lessened resilience of the oral mucoperiosteum.
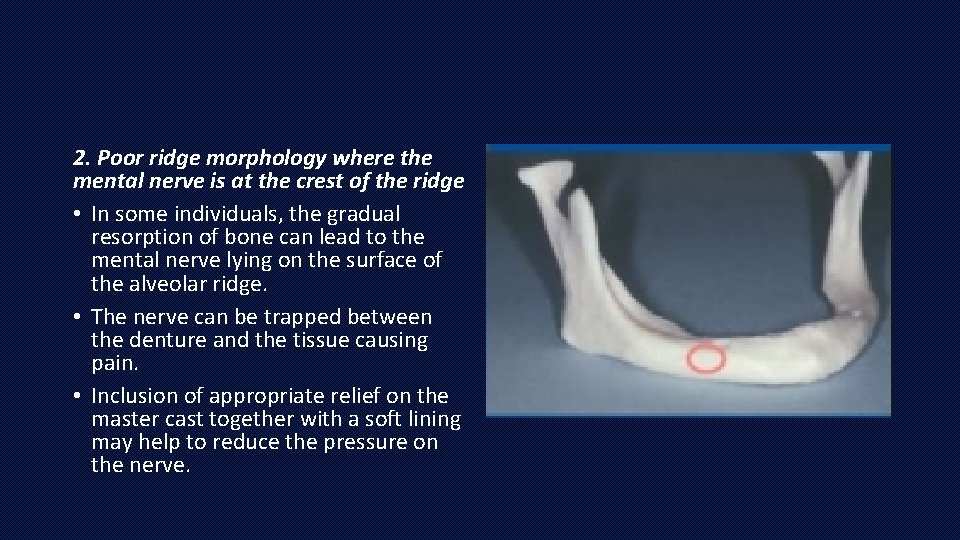
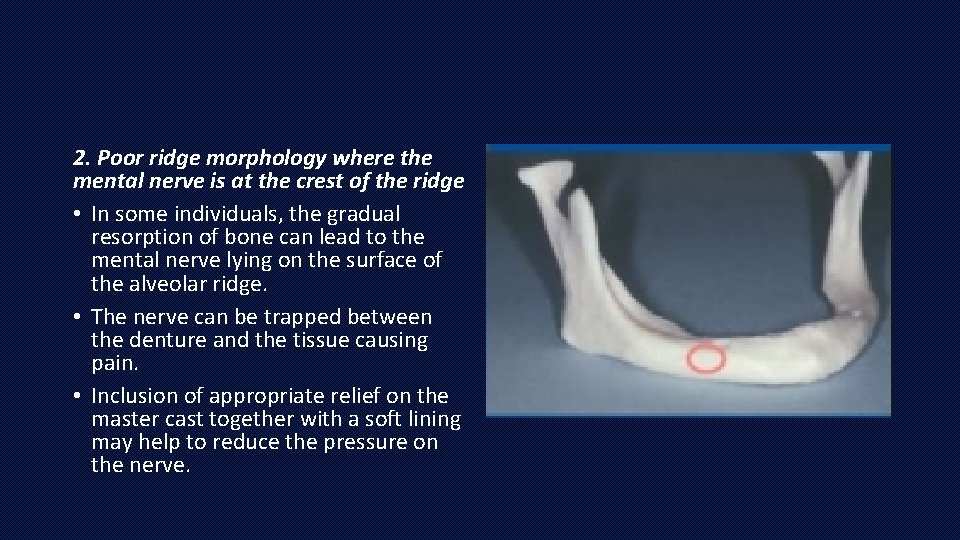
2. Poor ridge morphology where the mental nerve is at the crest of the ridge • In some individuals, the gradual resorption of bone can lead to the mental nerve lying on the surface of the alveolar ridge. • The nerve can be trapped between the denture and the tissue causing pain. • Inclusion of appropriate relief on the master cast together with a soft lining may help to reduce the pressure on the nerve.
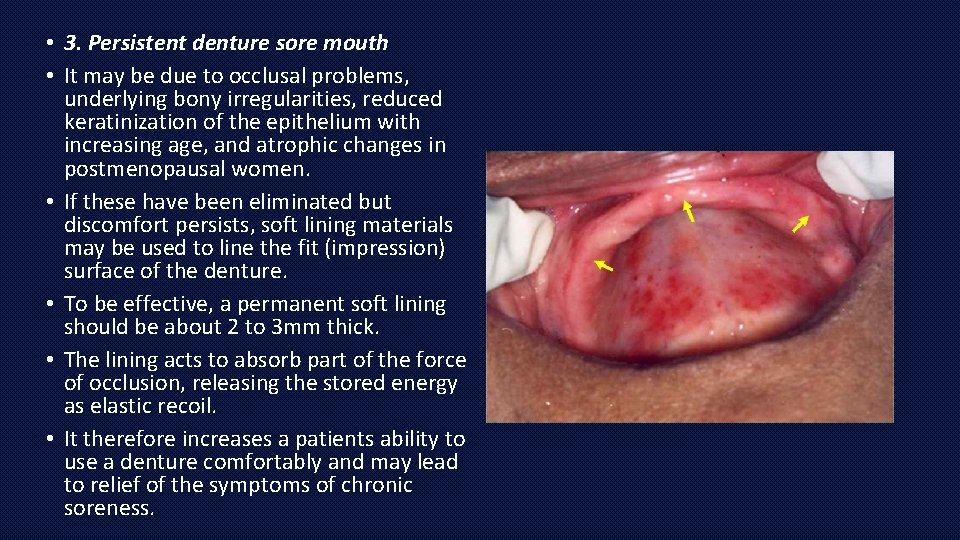
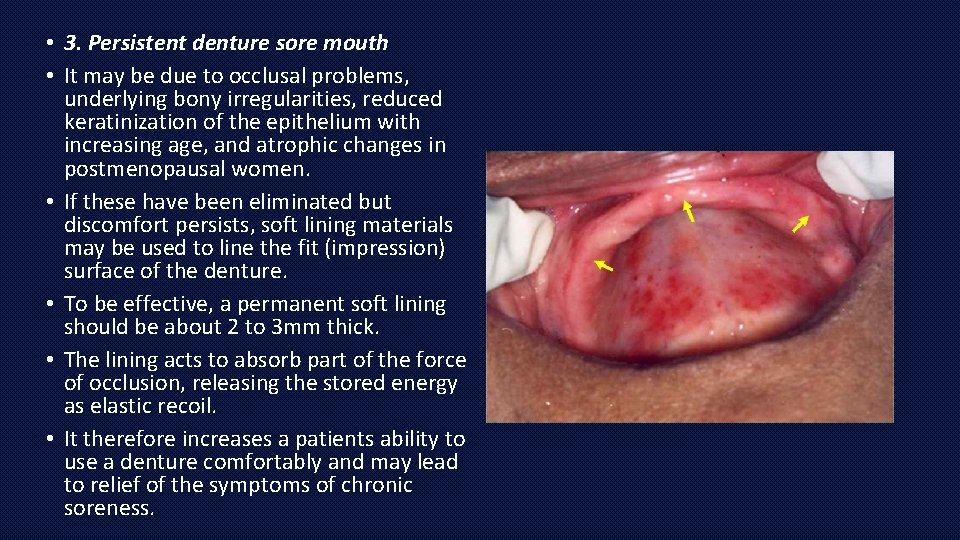
• 3. Persistent denture sore mouth • It may be due to occlusal problems, underlying bony irregularities, reduced keratinization of the epithelium with increasing age, and atrophic changes in postmenopausal women. • If these have been eliminated but discomfort persists, soft lining materials may be used to line the fit (impression) surface of the denture. • To be effective, a permanent soft lining should be about 2 to 3 mm thick. • The lining acts to absorb part of the force of occlusion, releasing the stored energy as elastic recoil. • It therefore increases a patients ability to use a denture comfortably and may lead to relief of the symptoms of chronic soreness.
4. Acquired or congenital oral defects • Soft lining material could be used for the cleft palate patient, or an acquired oral defect related to trauma, to improve retention of the denture by engaging undercuts. • Soft lining materials are also used for obturators after maxillofacial surgery.
5. Xerostomia • A soft lining may be indicated in those with a reduced saliva flow, possibly as a result of degenerative changes in the salivary glands, radiotherapy or drug therapy. • However, the use of silicone resilient liners which lack wettability may result in trauma to the mucosa due to friction if the denture is loose and is dragged across the tissues. • Candidal colonization of permanent resilient linings is a common feature in the edentulous patient with a dry mouth.
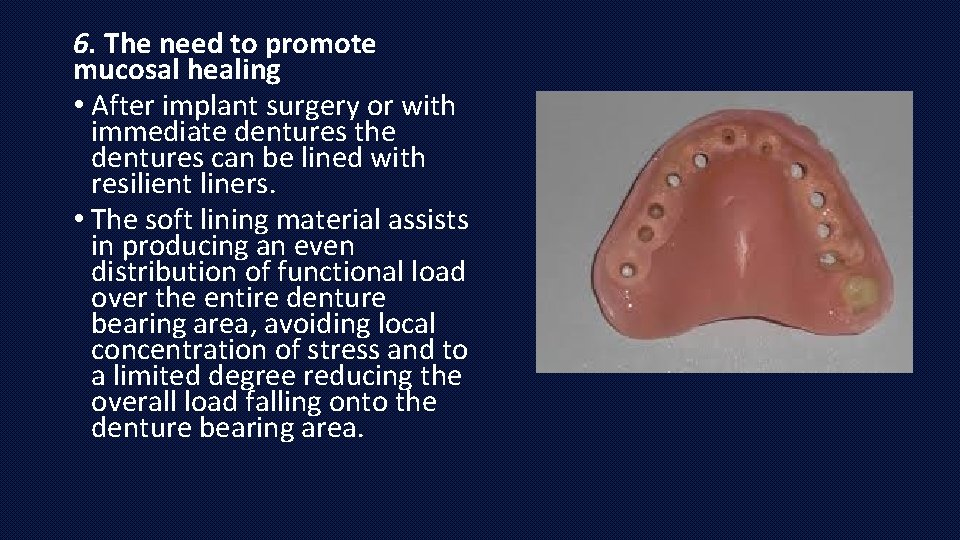
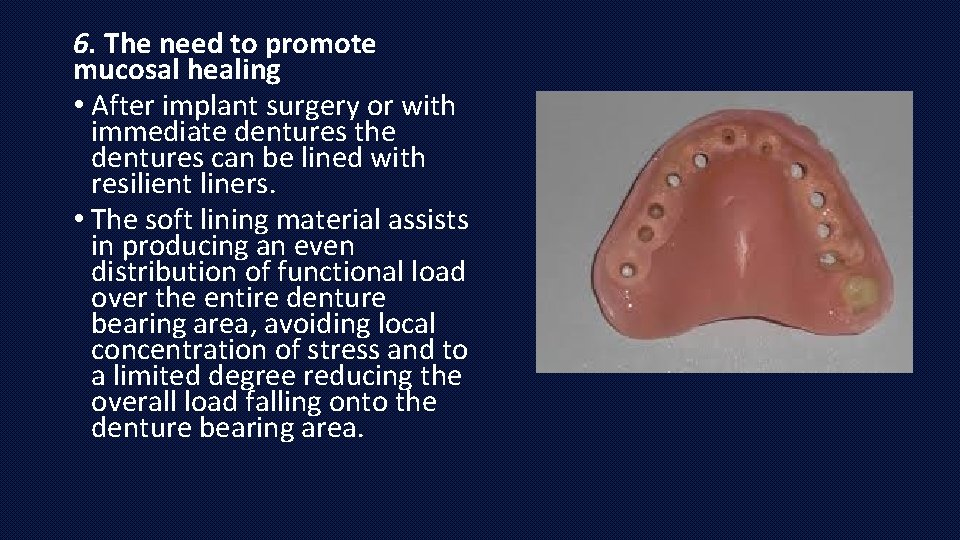
6. The need to promote mucosal healing • After implant surgery or with immediate dentures the dentures can be lined with resilient liners. • The soft lining material assists in producing an even distribution of functional load over the entire denture bearing area, avoiding local concentration of stress and to a limited degree reducing the overall load falling onto the denture bearing area.
7. In cases of bilateral undercuts • Placing a rigid acrylic resin denture is difficult and there is a problem of retention. • Its use in this situation allows the denture to be placed over the prominence and since the soft material is elastic, it will spring back into close contact with the undercut area.
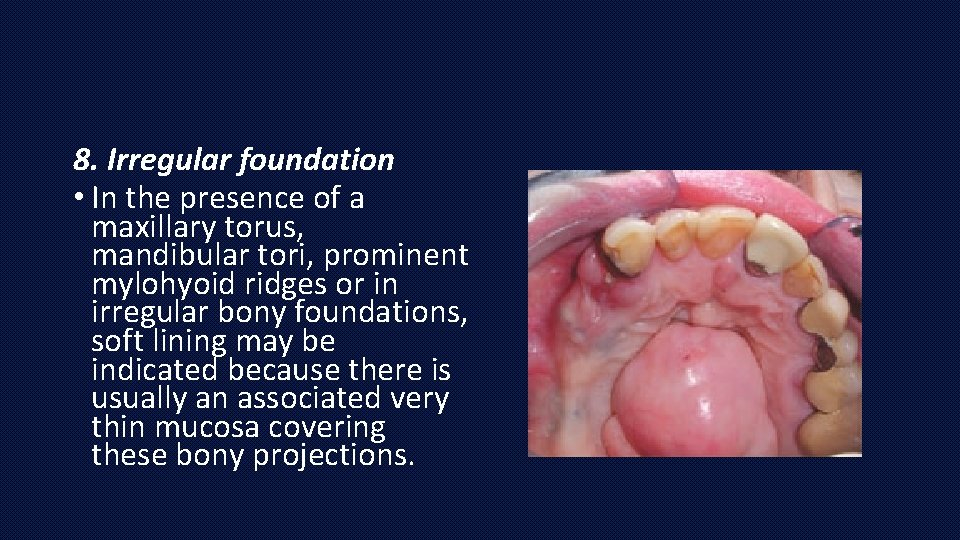
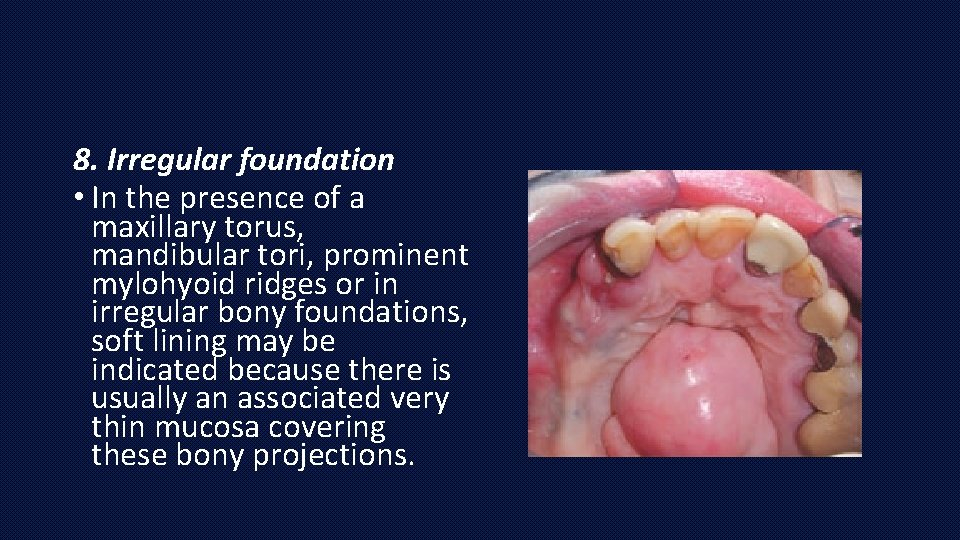
8. Irregular foundation • In the presence of a maxillary torus, mandibular tori, prominent mylohyoid ridges or in irregular bony foundations, soft lining may be indicated because there is usually an associated very thin mucosa covering these bony projections.
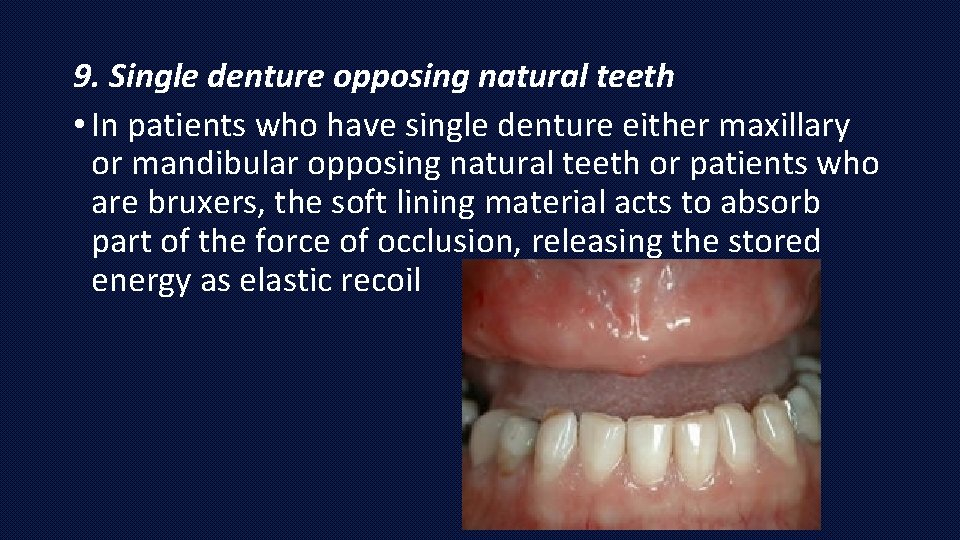
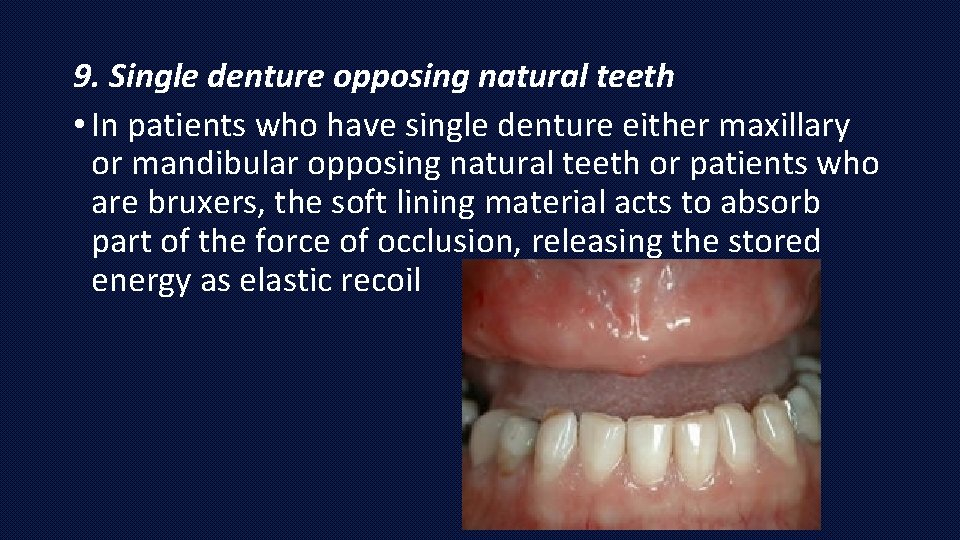
9. Single denture opposing natural teeth • In patients who have single denture either maxillary or mandibular opposing natural teeth or patients who are bruxers, the soft lining material acts to absorb part of the force of occlusion, releasing the stored energy as elastic recoil
10. Mandibular distal extension base partial dentures • For improving retention in mandibular distal extension base partial dentures where there is retromylohyoid undercut and the presence of teeth limits the available paths of placement, resulting in an absence of valuable retentive and stabilizing areas of the denture extensions. • To overcome this problem, acrylic resin material in undercut region of the retromylohyoid fossa is replaced with soft lining material.
CONTRAINDICATIONS • Contraindications for use of soft liners are: 1. drastic loss of vertical dimension, 2. altered plane of occlusion, 3. short denture borders, 4. dramatically changed tissues, 5. dissatisfying original esthetics. “ Liners are not a panacea for the correction of all denture base problems and the patient should understand that eventually a reline, rebase, or remake of the prosthesis will be necessary. ”

TECHNIQUES FOR USING SOFT LINERS
As a tissue conditioner 1. Pre-requisites: • Dentures should have adequate coverage of the bearing areas • Adequate OVD • No occlusal interferences
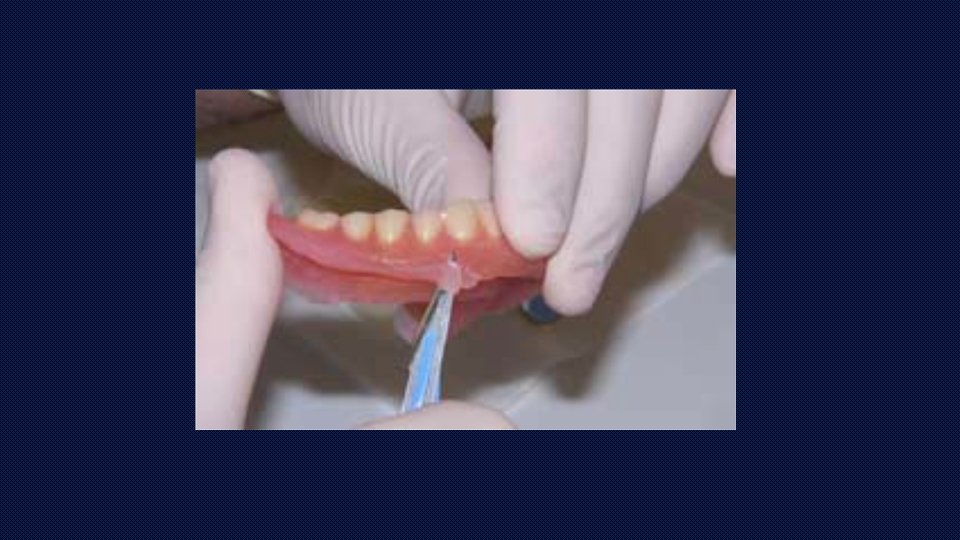
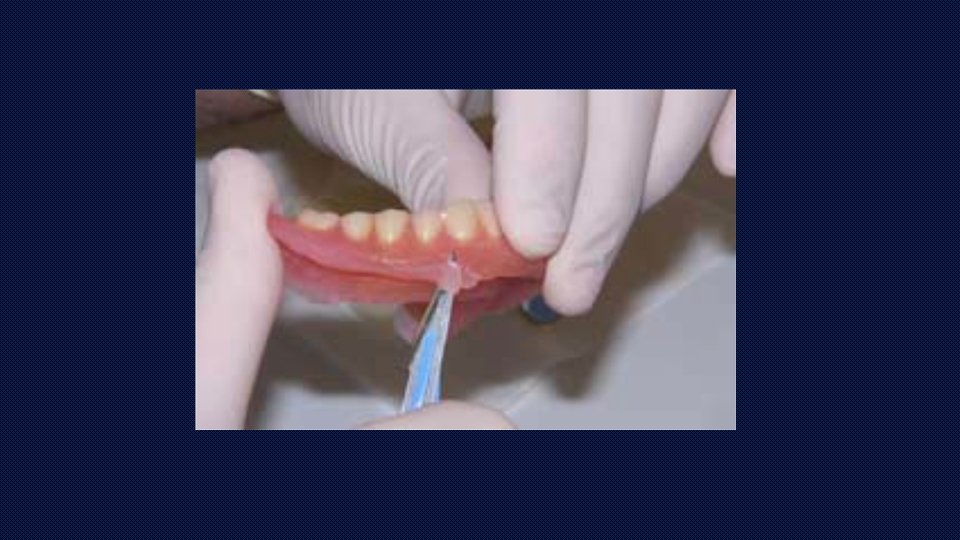
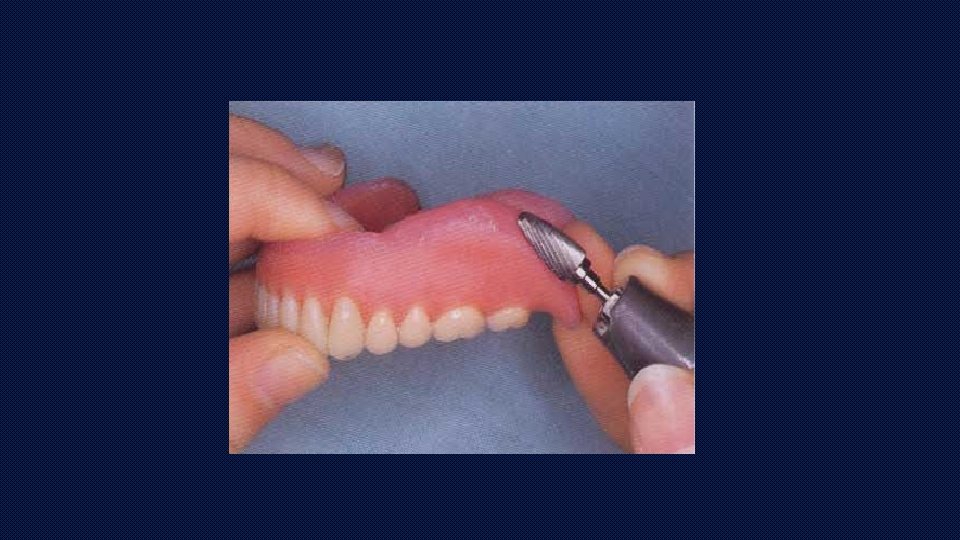
2. Preparation of the denture. • From the denture base all undercuts and some area immediately on the ridge to a depth of 1 mm or more is removed. • Borders and flanges maintained as vertical stops • If the denture base is short, it should be extended using self cure acrylic resin to provide support for the soft material • Dentures should be provided with room for the conditioning material that is sufficient to allow the displaced and traumatized tissue over to a normal state.
PREPARATION AND PLACEMENT OF THE TISSUE CONDITIONER IN THE MOUTH • Material used is a three component system; the polymer (powder), the monomer (liquid) and a liquid plasticizer (“Flow Control”). • For conditioning tissues, a ratio of 1 ¼ parts of polymer to 1 part of monomer is recommended with the addition of approximately ½ cc of the plasticizer (flow control).


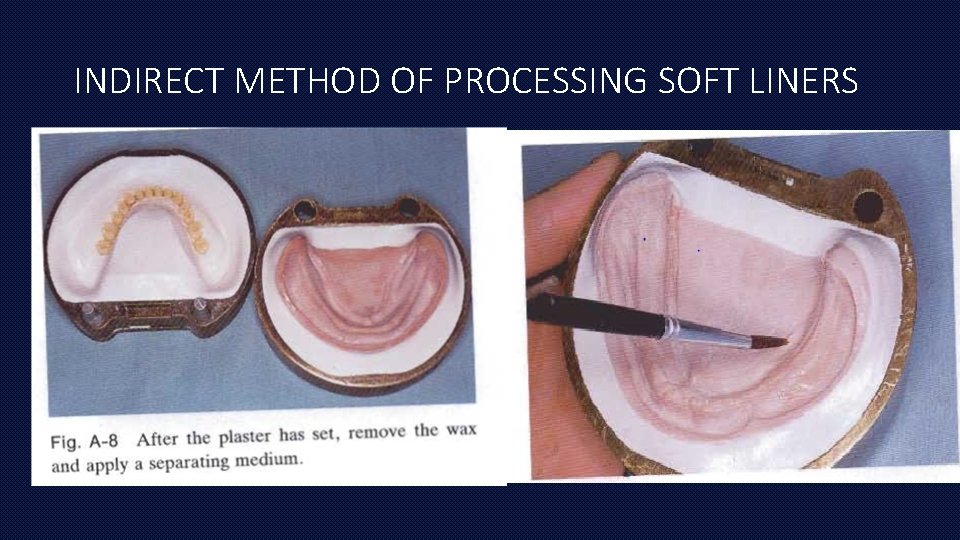
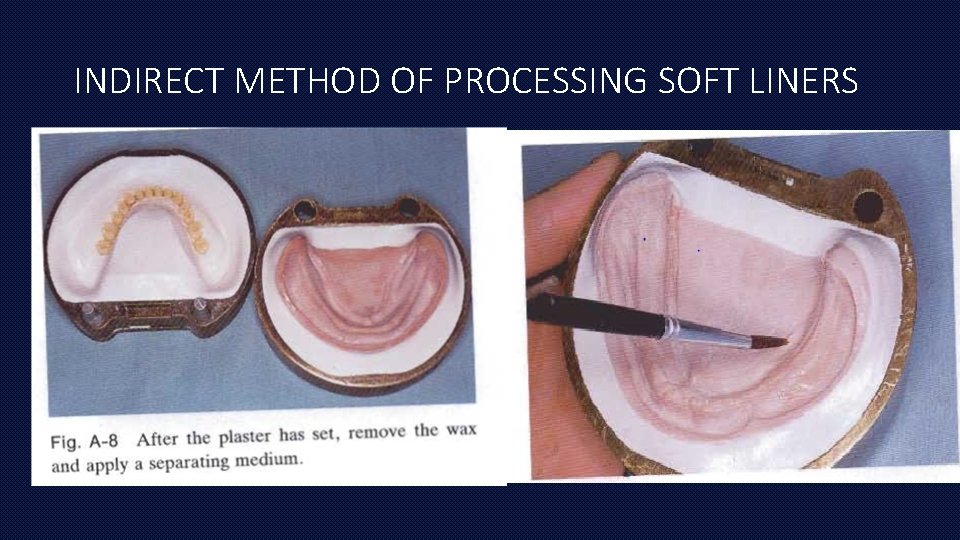
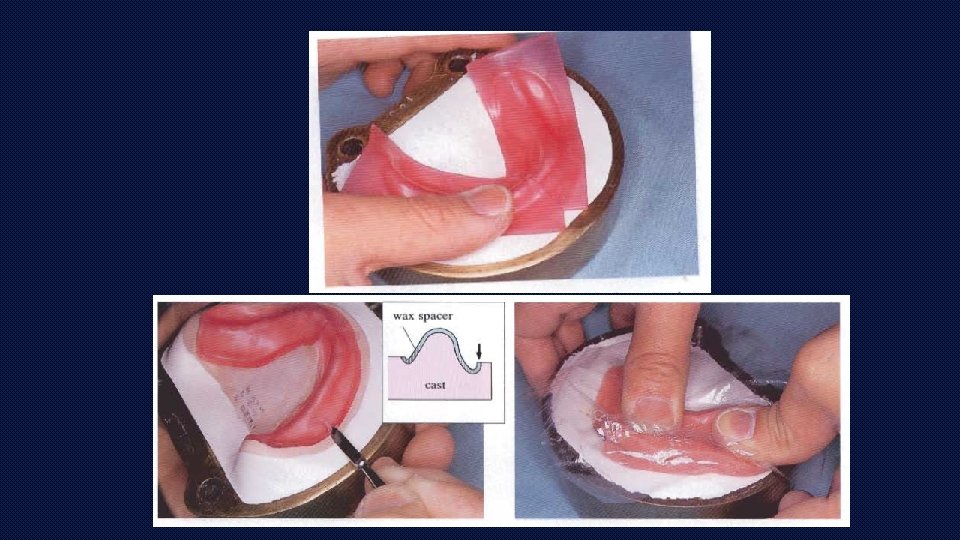
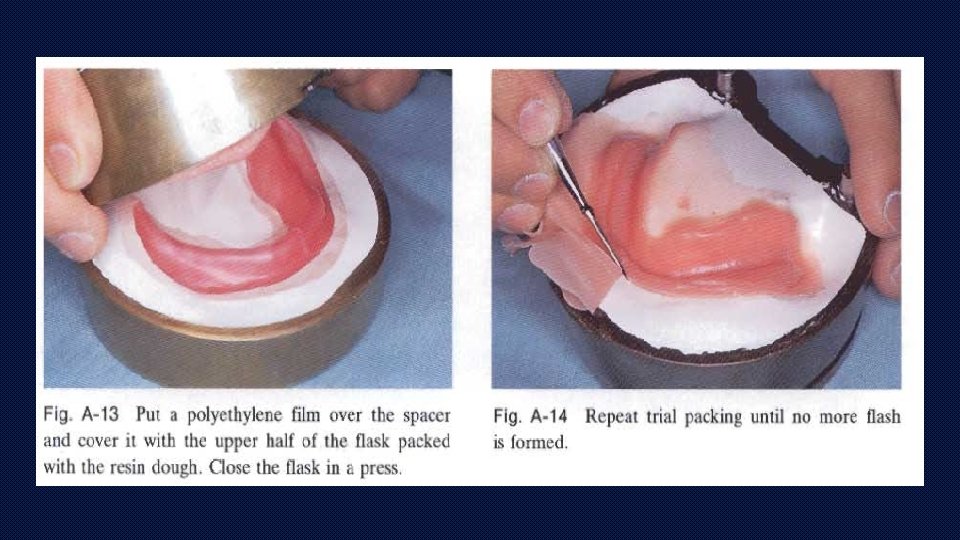
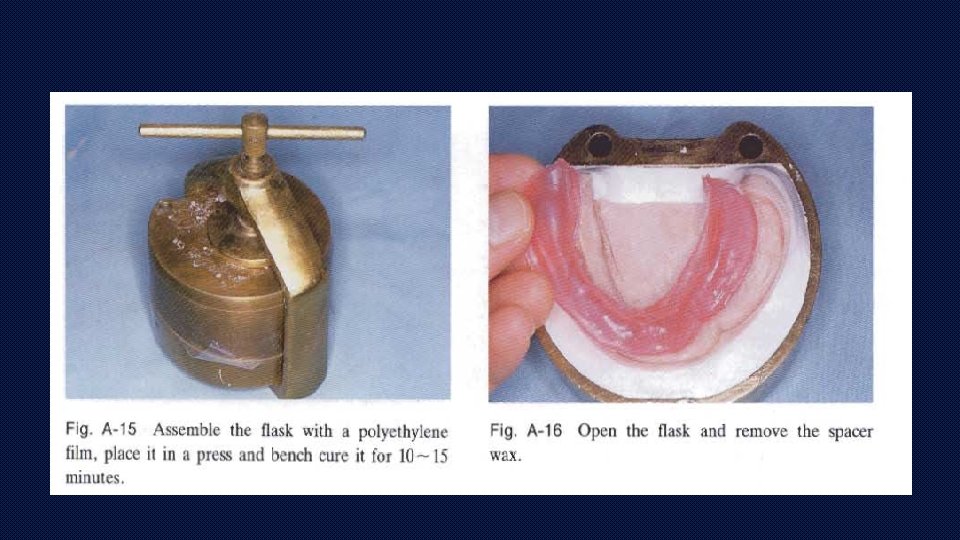
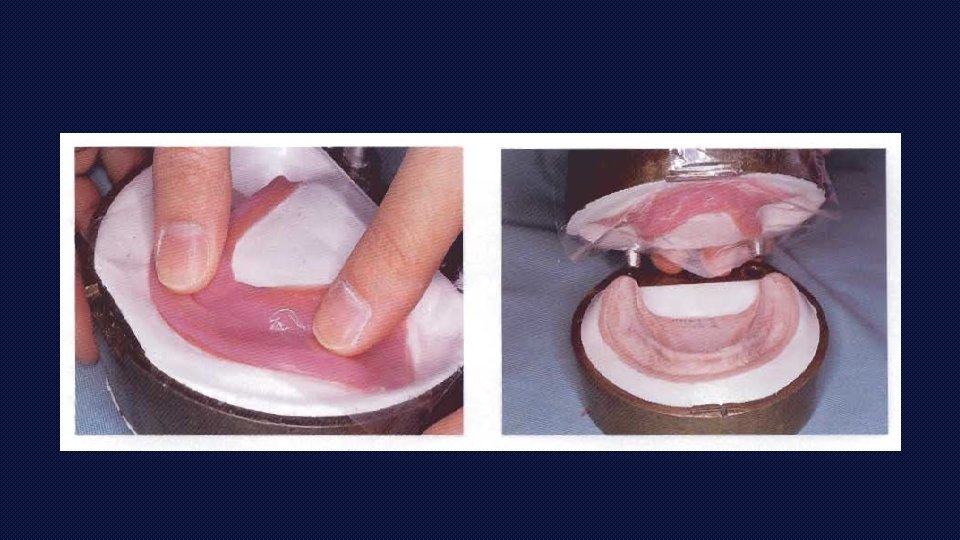
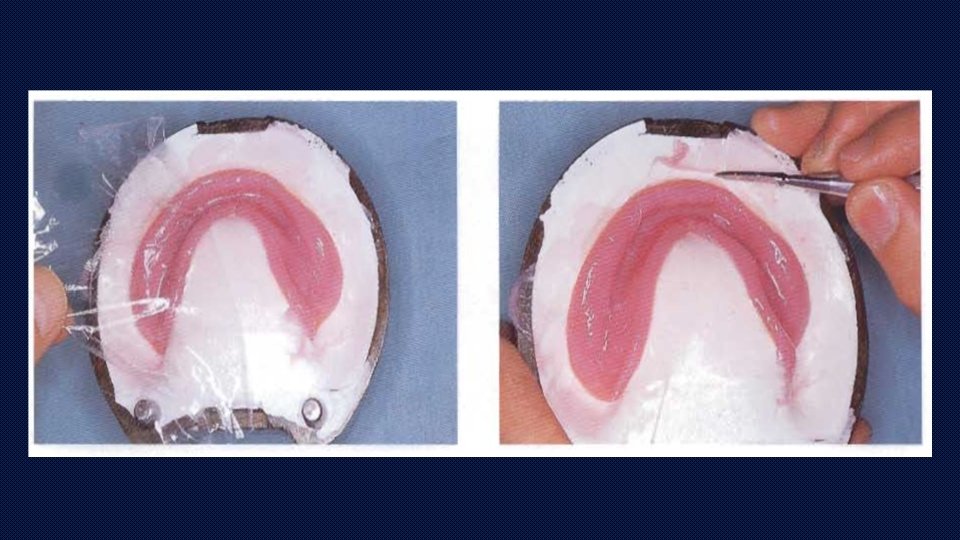
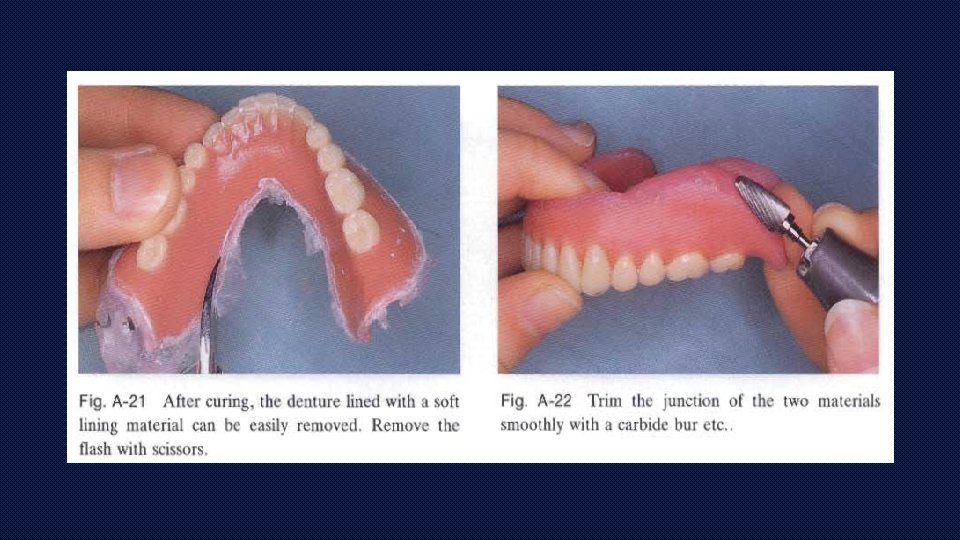
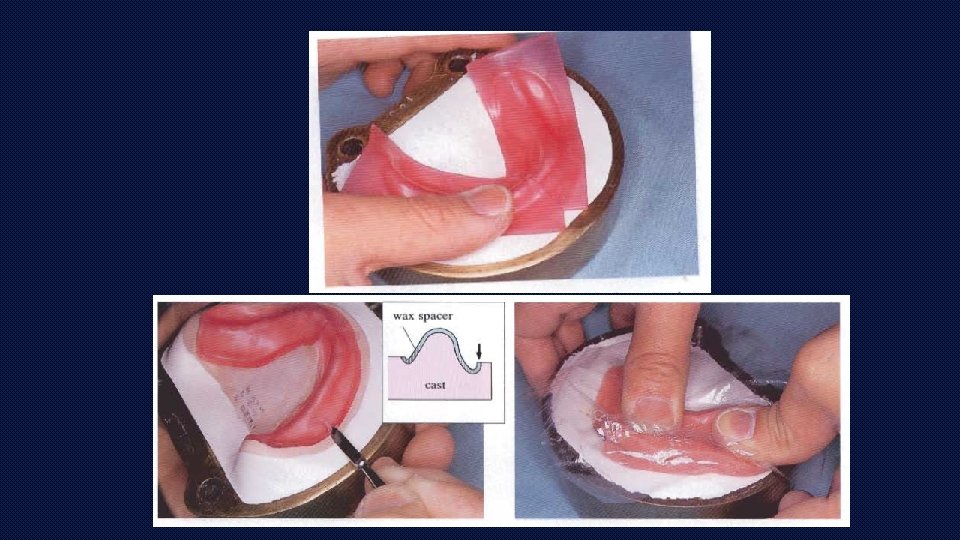
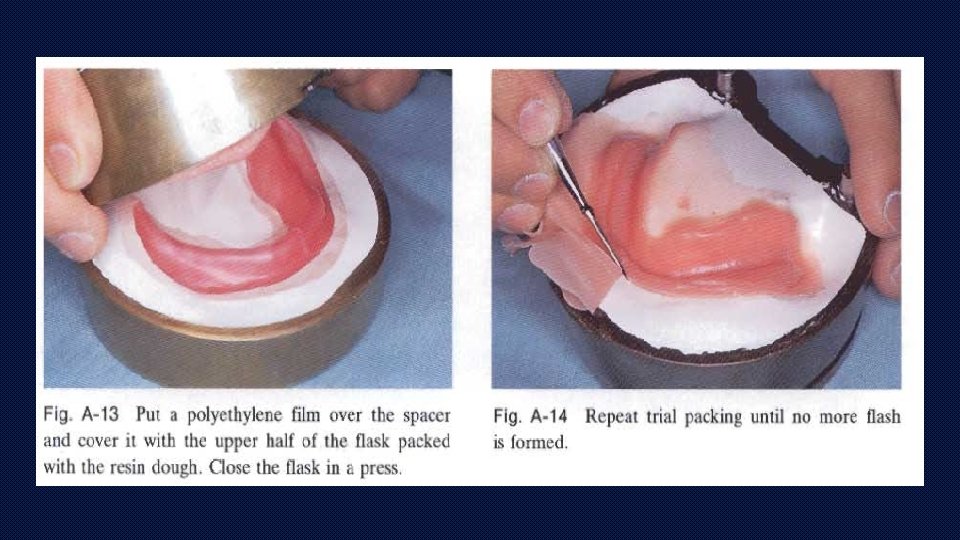
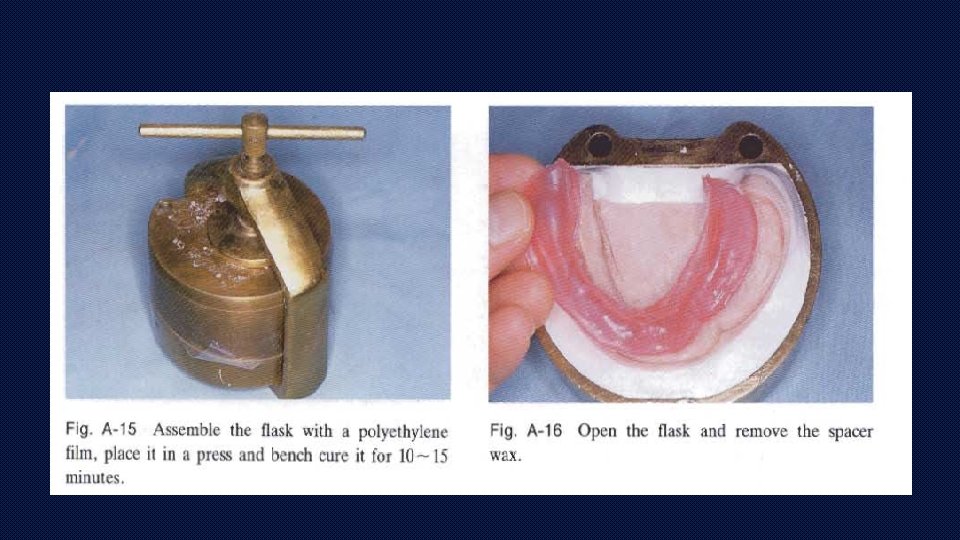
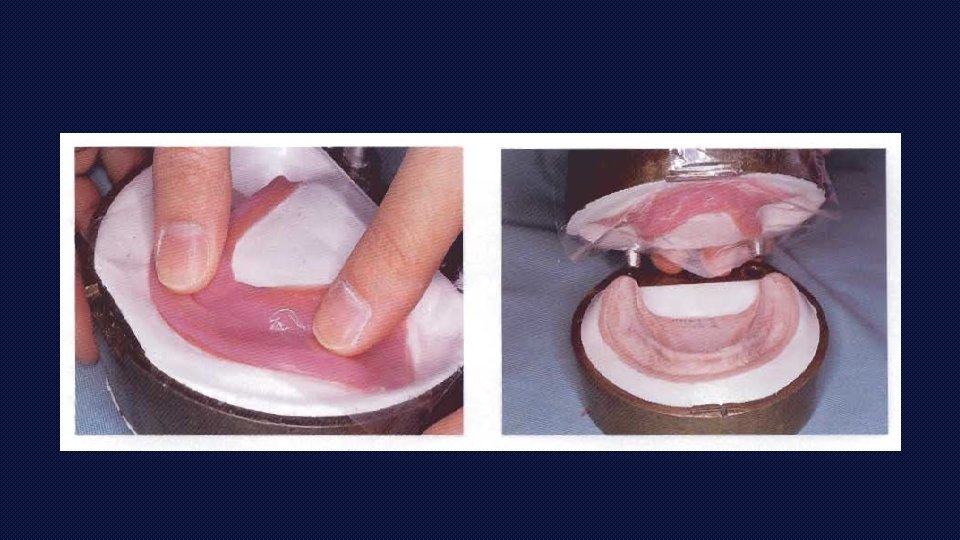
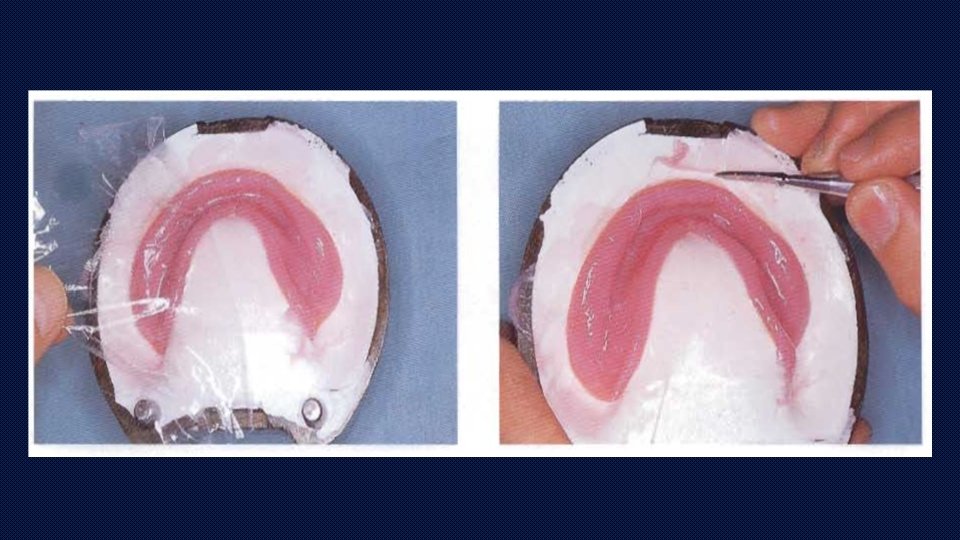
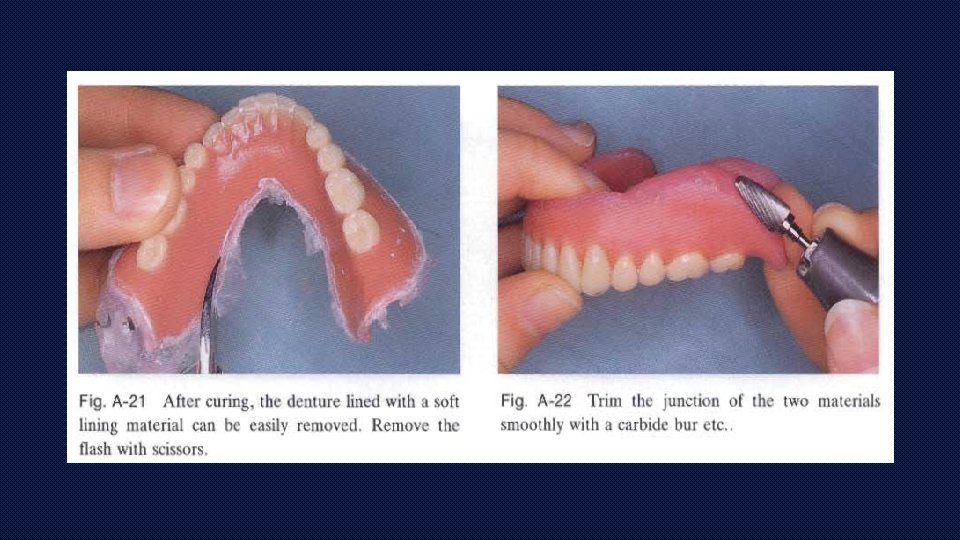
INDIRECT METHOD OF PROCESSING SOFT LINERS
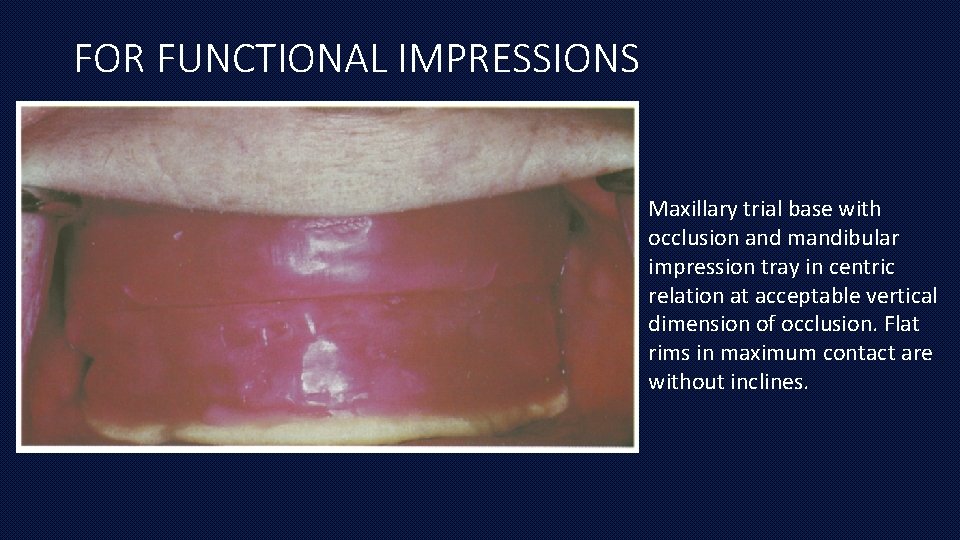
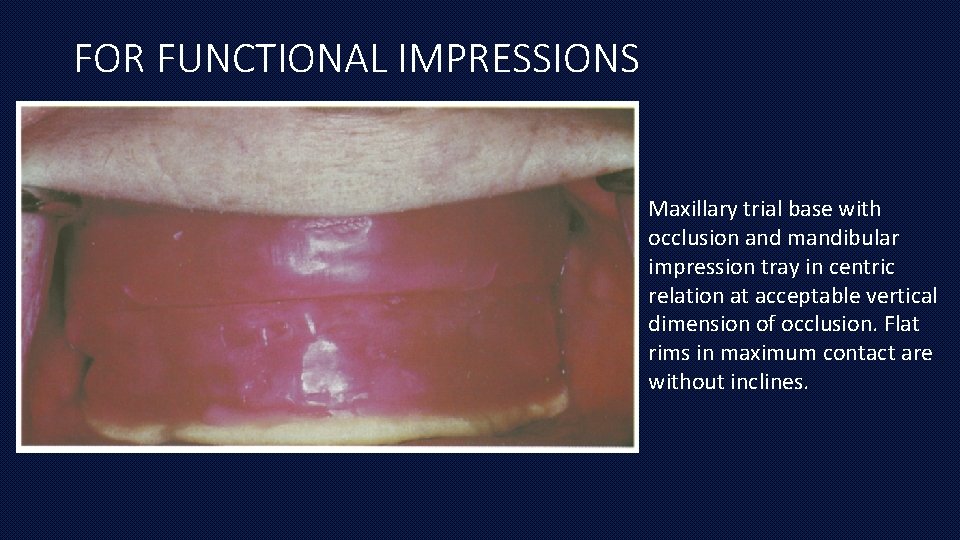
FOR FUNCTIONAL IMPRESSIONS Maxillary trial base with occlusion and mandibular impression tray in centric relation at acceptable vertical dimension of occlusion. Flat rims in maximum contact are without inclines.
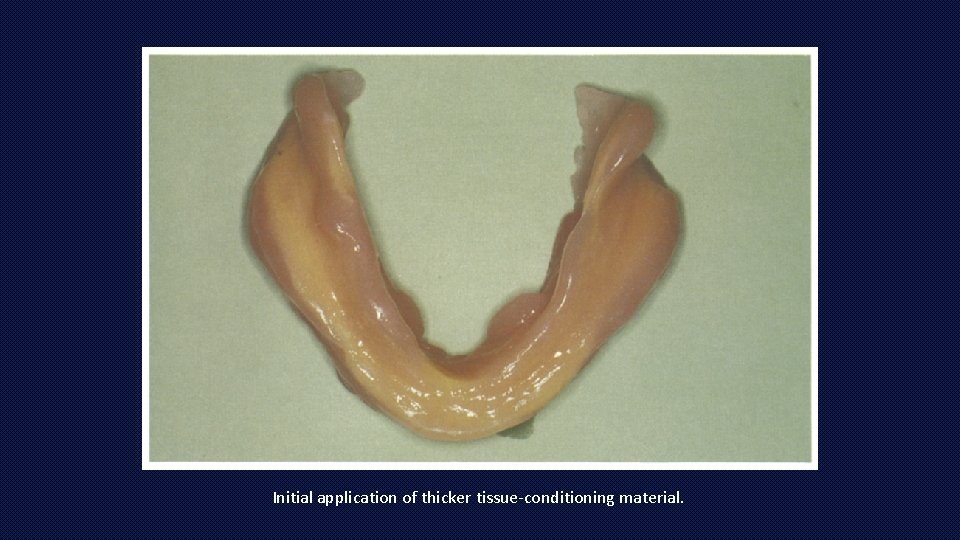
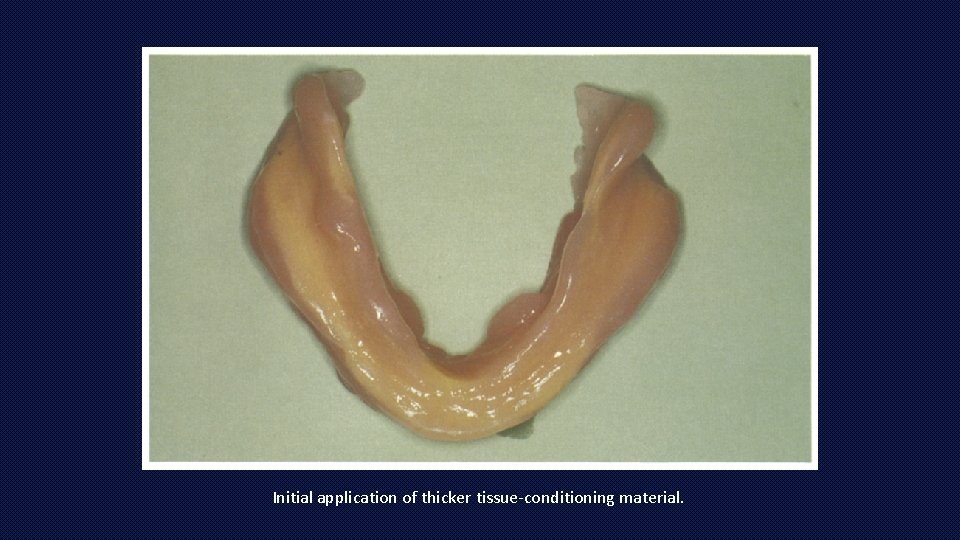
Initial application of thicker tissue-conditioning material.
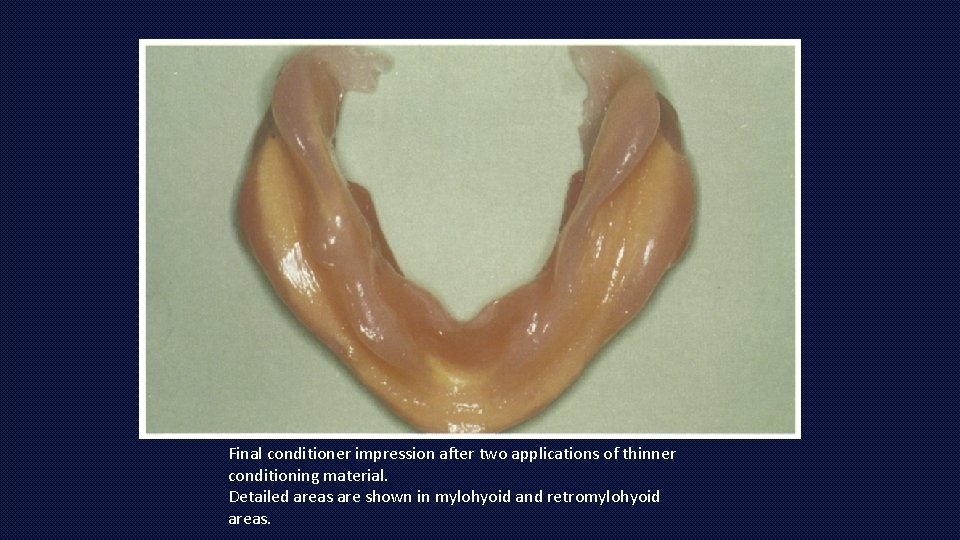
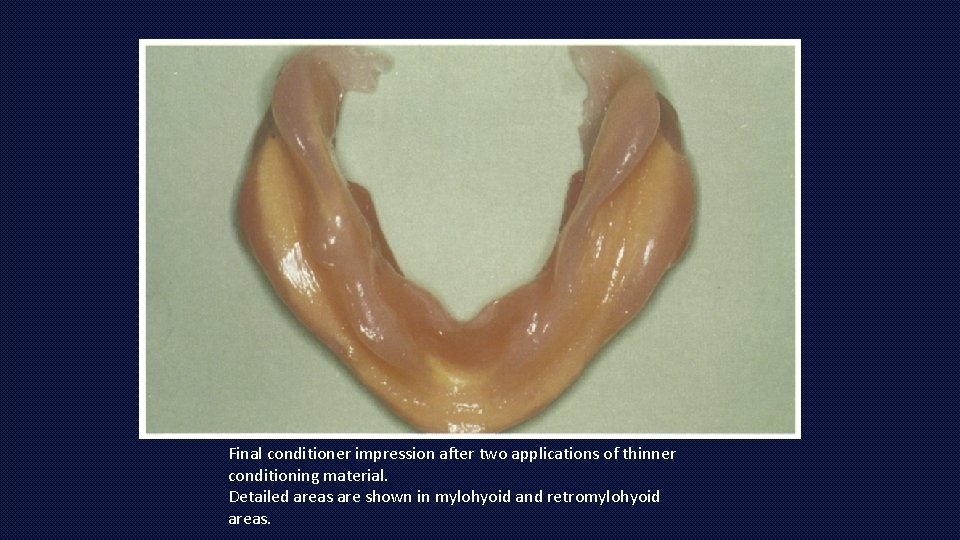
Final conditioner impression after two applications of thinner conditioning material. Detailed areas are shown in mylohyoid and retromylohyoid areas.
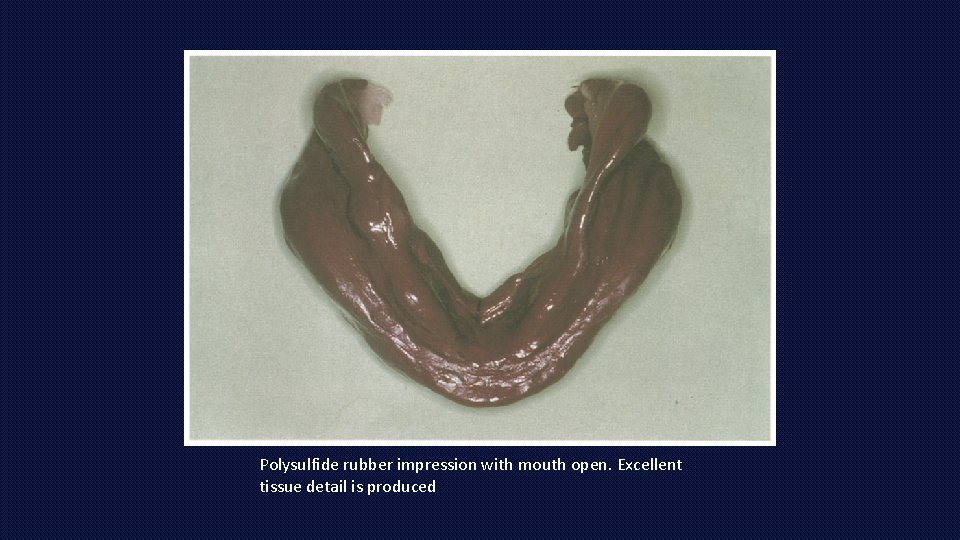
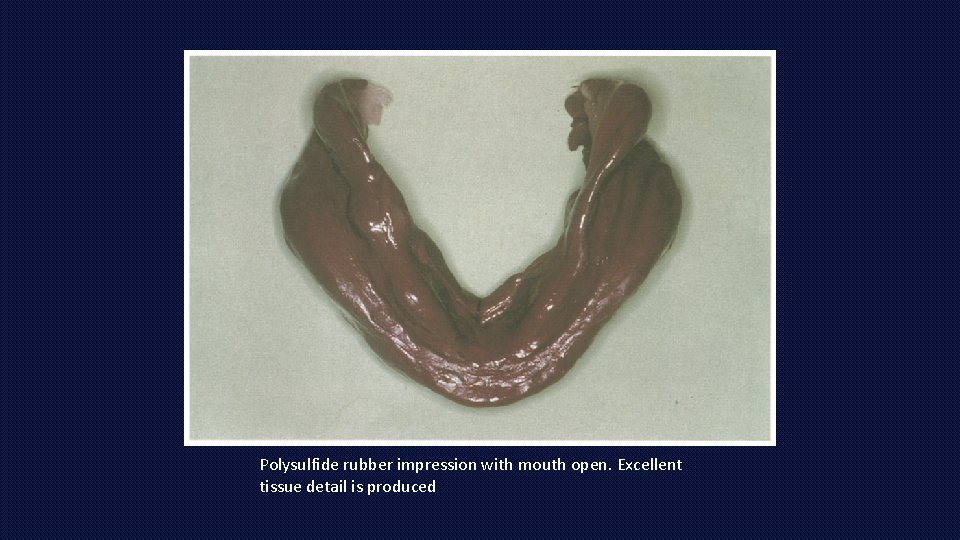
Polysulfide rubber impression with mouth open. Excellent tissue detail is produced
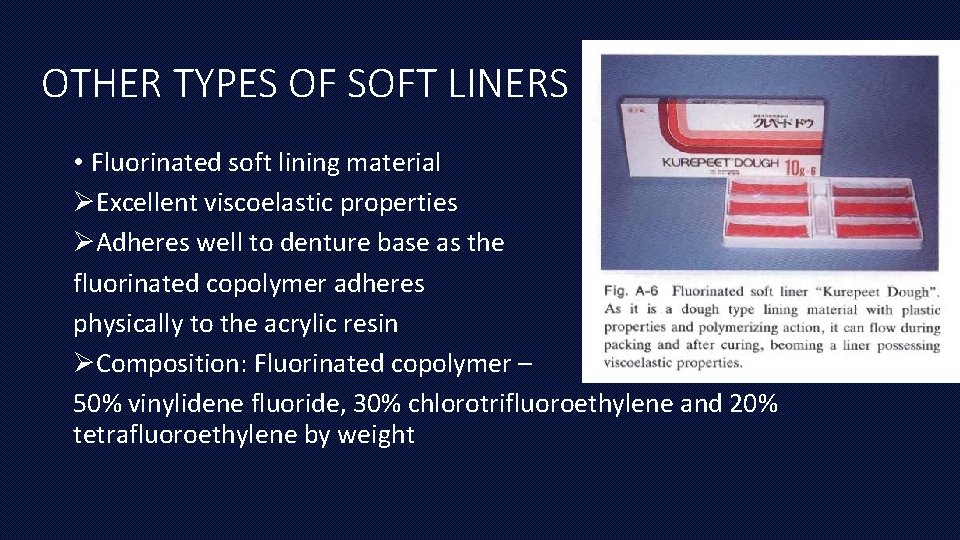
OTHER TYPES OF SOFT LINERS • Fluorinated soft lining material ØExcellent viscoelastic properties ØAdheres well to denture base as the fluorinated copolymer adheres physically to the acrylic resin ØComposition: Fluorinated copolymer – 50% vinylidene fluoride, 30% chlorotrifluoroethylene and 20% tetrafluoroethylene by weight
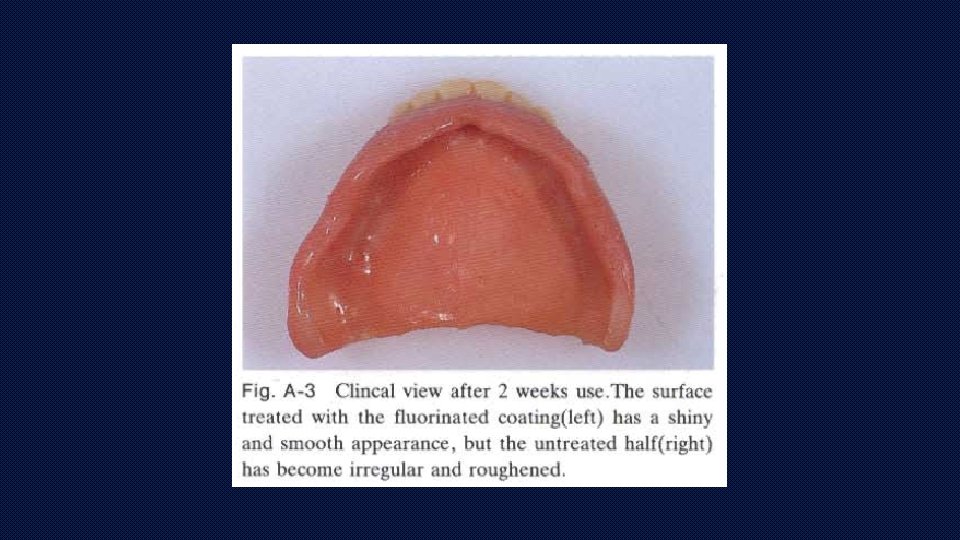
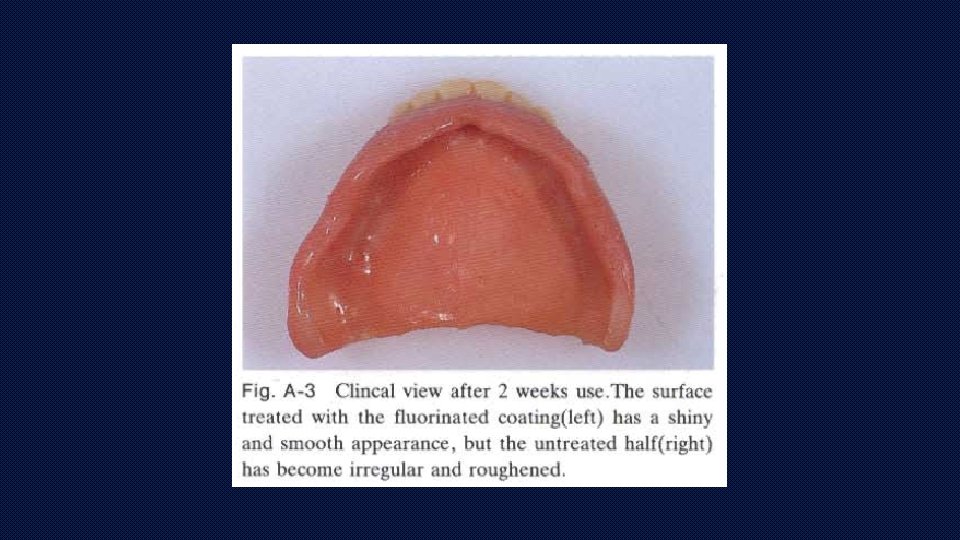
• Kregard ØEthyl acetate solution containing a fluorinated soft resin. ØApplied to the surface of the tissue conditioner leaving the surface coated by a thin film of the resin after the solvent evaporates. ØHence, components of tissue conditioner will not leach out leading to: 1. Increased duration of viscoelasticity of the conditioner 2. More smoother and abrasion resistant 3. Decreased contamination
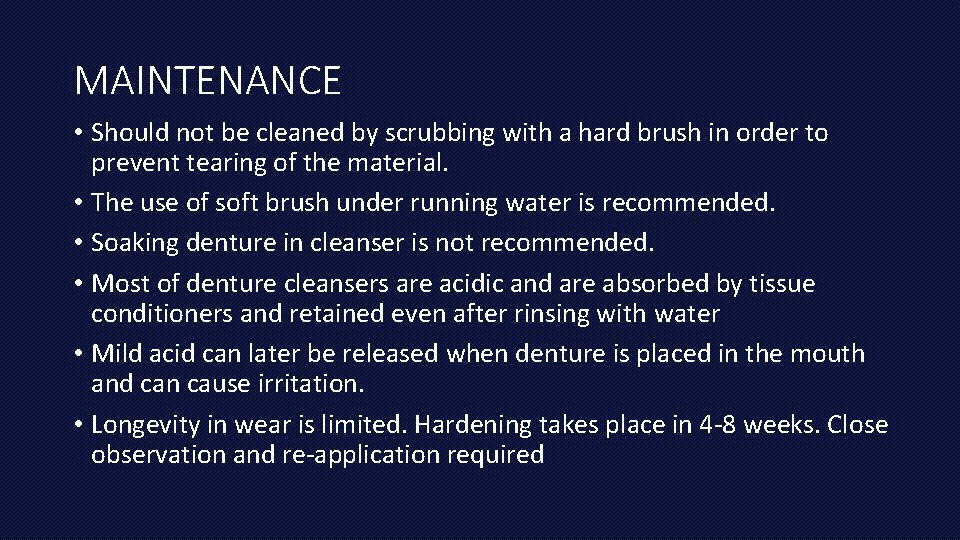
MAINTENANCE • Should not be cleaned by scrubbing with a hard brush in order to prevent tearing of the material. • The use of soft brush under running water is recommended. • Soaking denture in cleanser is not recommended. • Most of denture cleansers are acidic and are absorbed by tissue conditioners and retained even after rinsing with water • Mild acid can later be released when denture is placed in the mouth and can cause irritation. • Longevity in wear is limited. Hardening takes place in 4 -8 weeks. Close observation and re-application required
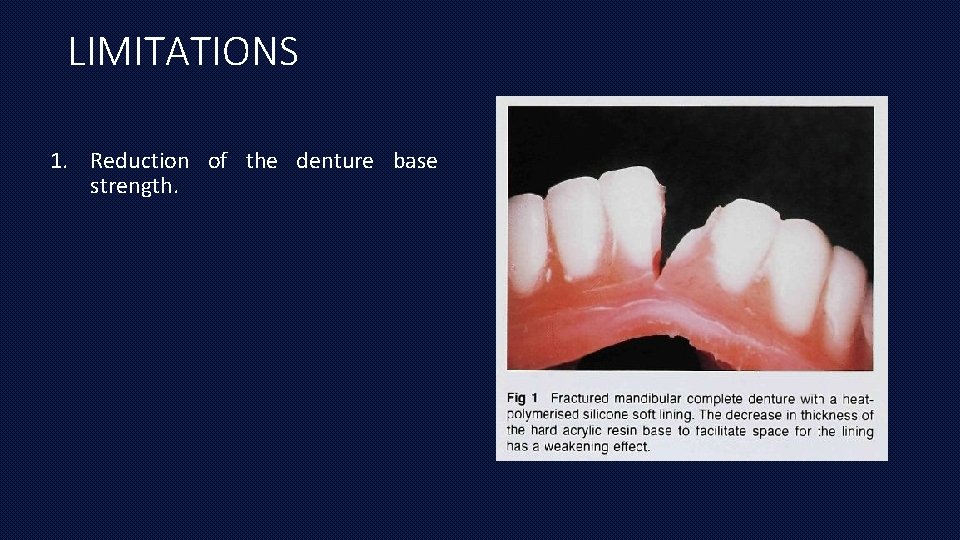
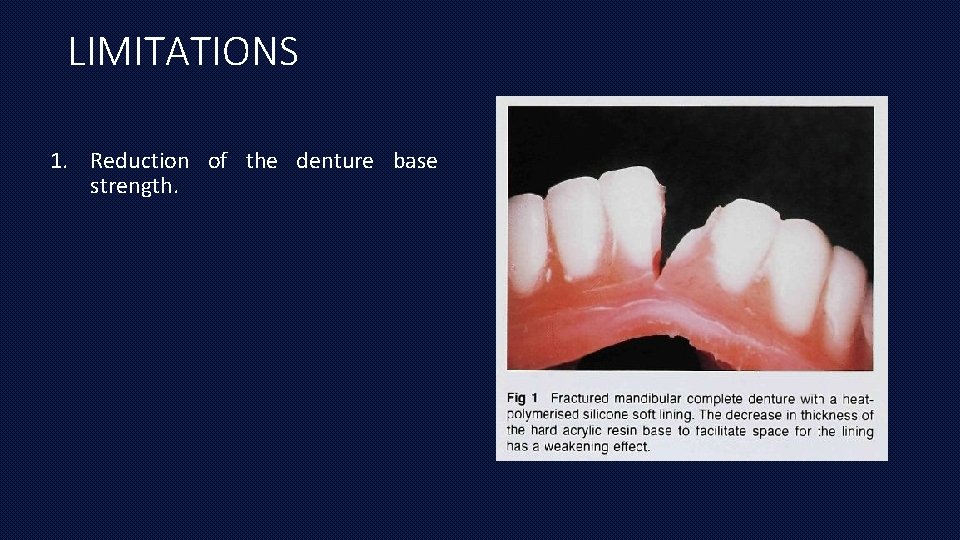
LIMITATIONS 1. Reduction of the denture base strength.
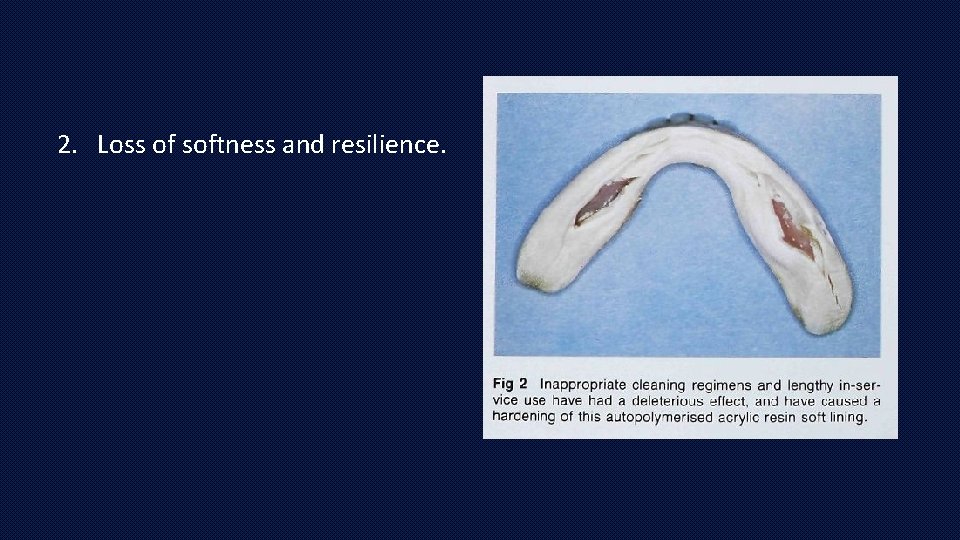
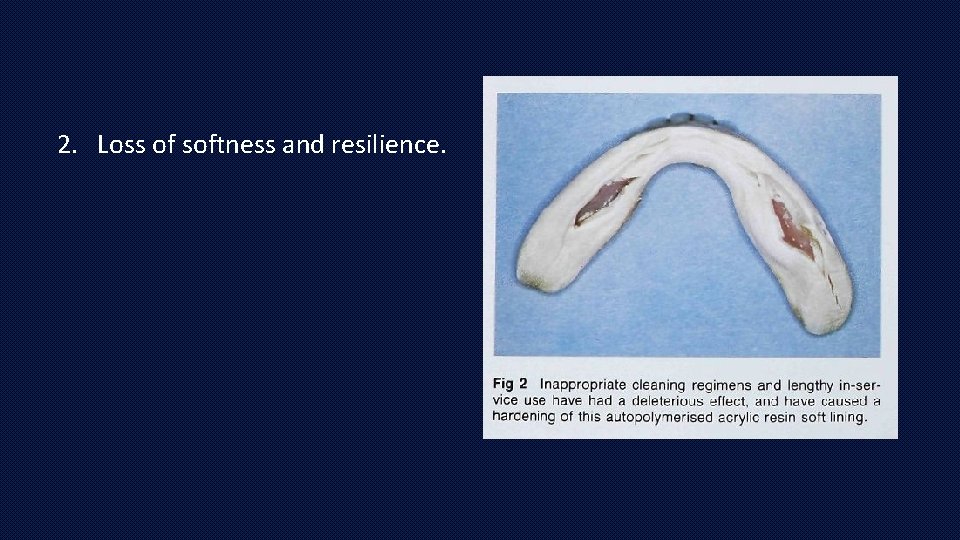
2. Loss of softness and resilience.
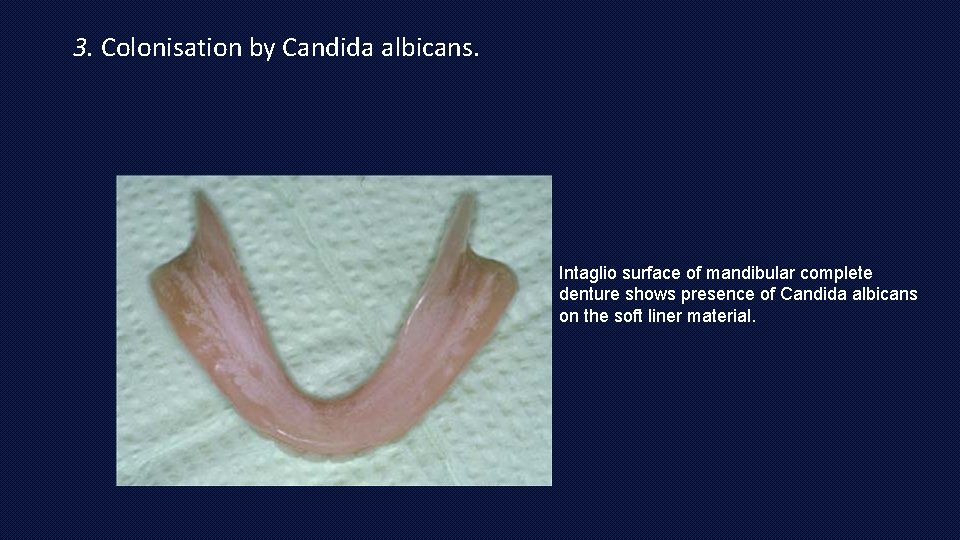
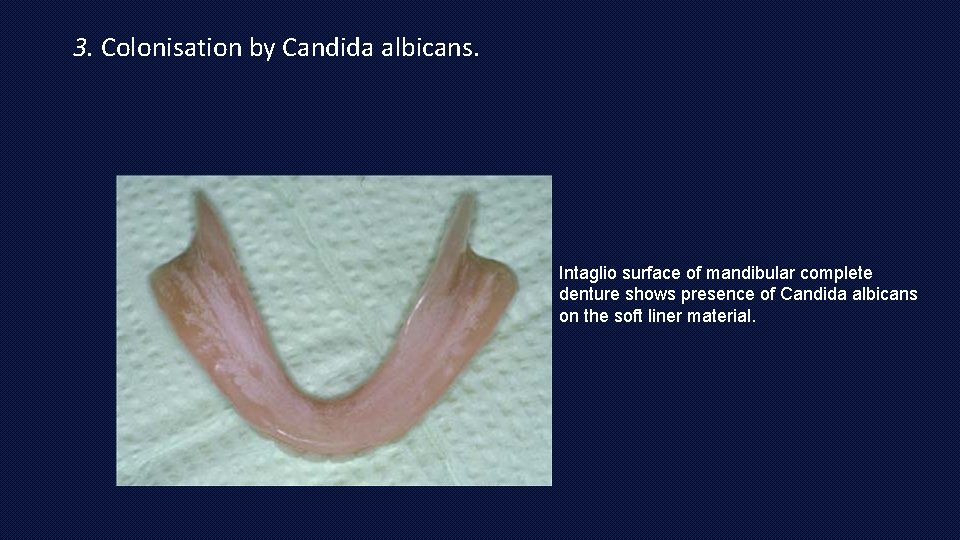
3. Colonisation by Candida albicans. Intaglio surface of mandibular complete denture shows presence of Candida albicans on the soft liner material.
4. Difficulty in keeping soft linings clean using normal denture cleaning methods. 5. Dimensional instability. • Some soft linings lose their plasticizer with time, and most of them absorb water. • These factors may cause dimensional changes.
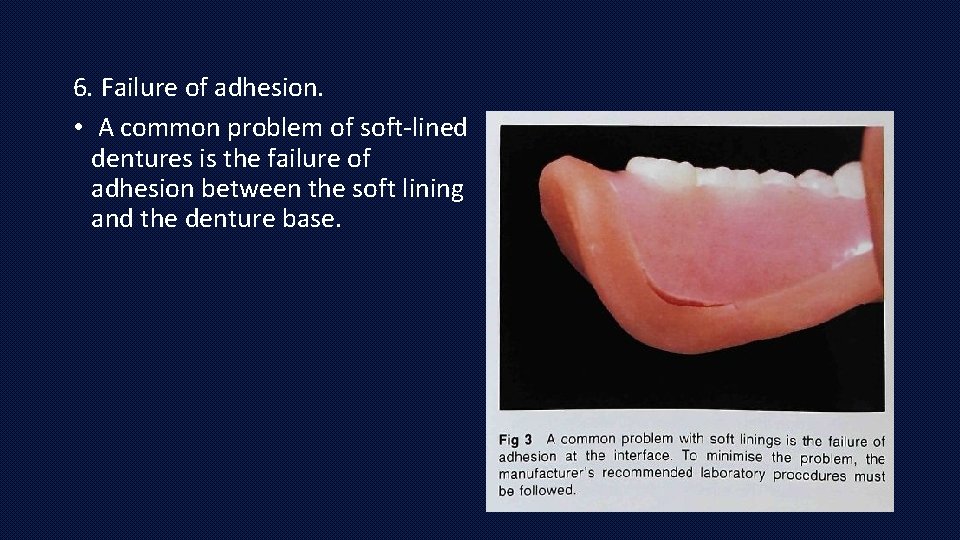
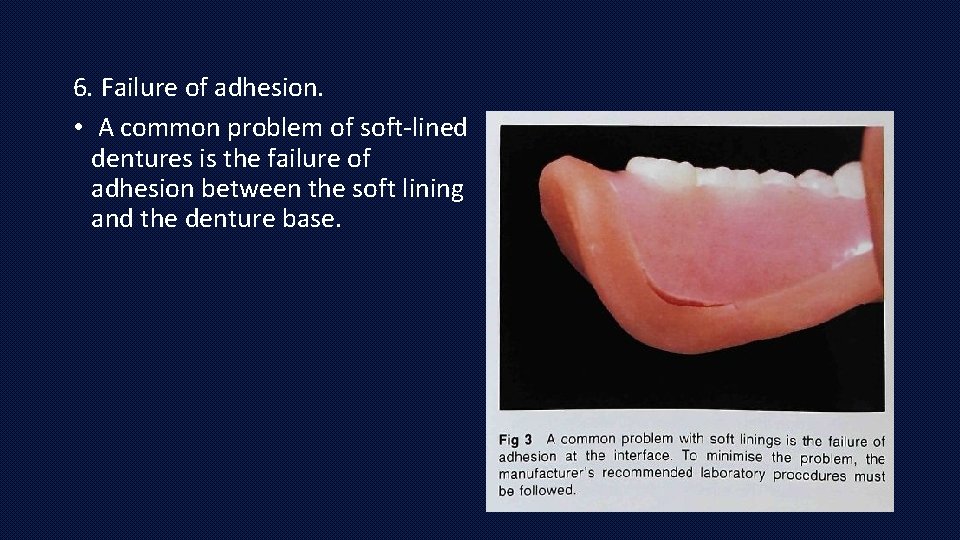
6. Failure of adhesion. • A common problem of soft-lined dentures is the failure of adhesion between the soft lining and the denture base.
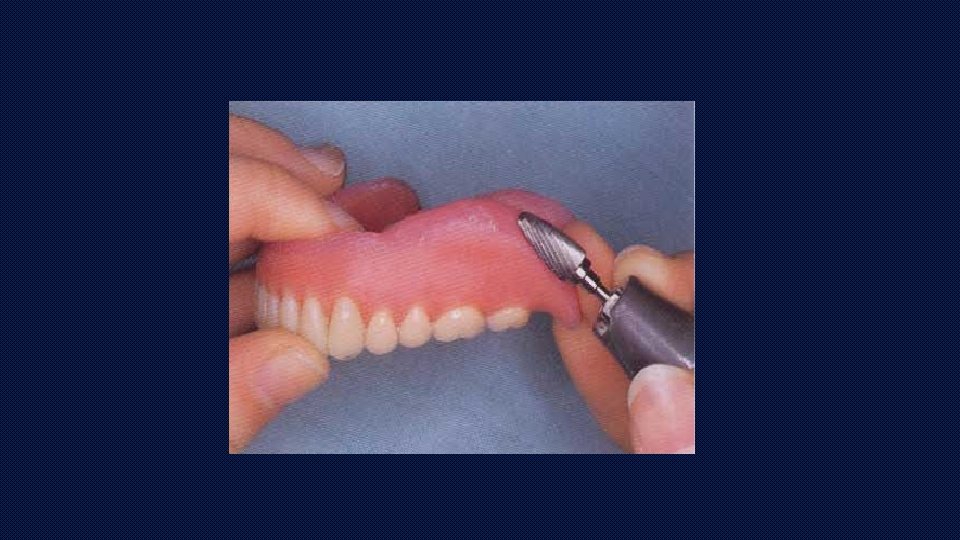
• Methods used to increase bonding between liner and denture base resin: 1. Surface roughening using lasers and alumina abrasion 2. Chemical etching with acetone, methylene chloride 3. Oxygen plasma treatment
DENTURE ADHESIVES
INTRODUCTION DEFINITION “As a material used to adhere a denture to oral mucosa” (GPT 8)
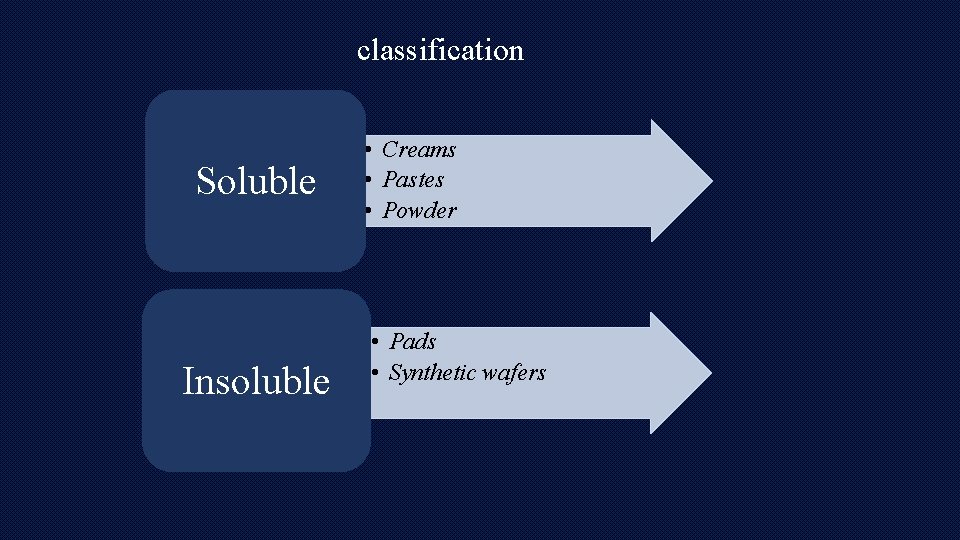
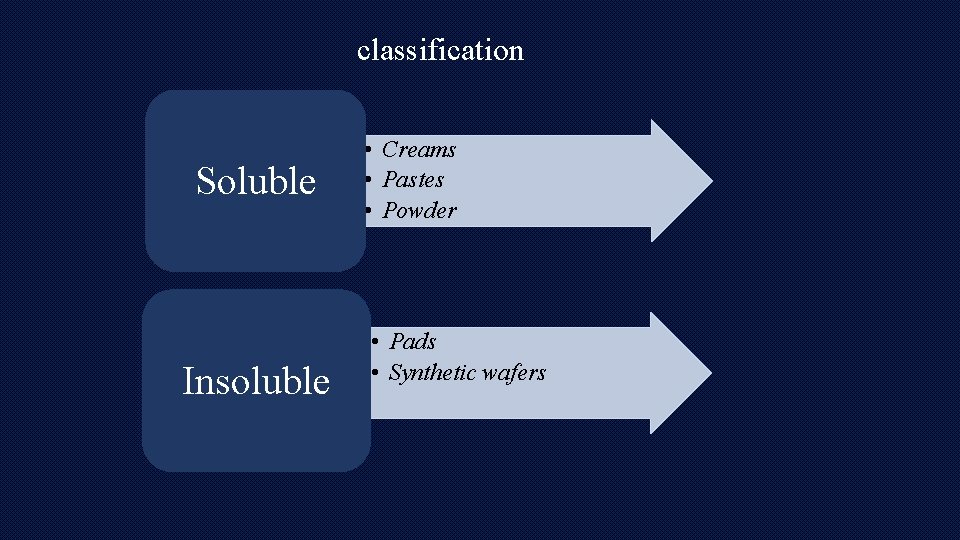
classification Soluble Insoluble • Creams • Pastes • Powder • Pads • Synthetic wafers
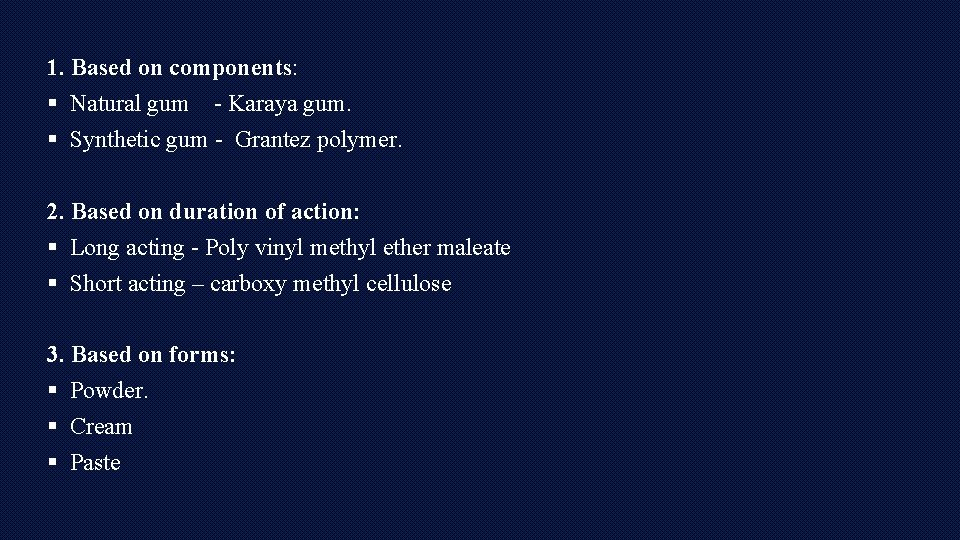
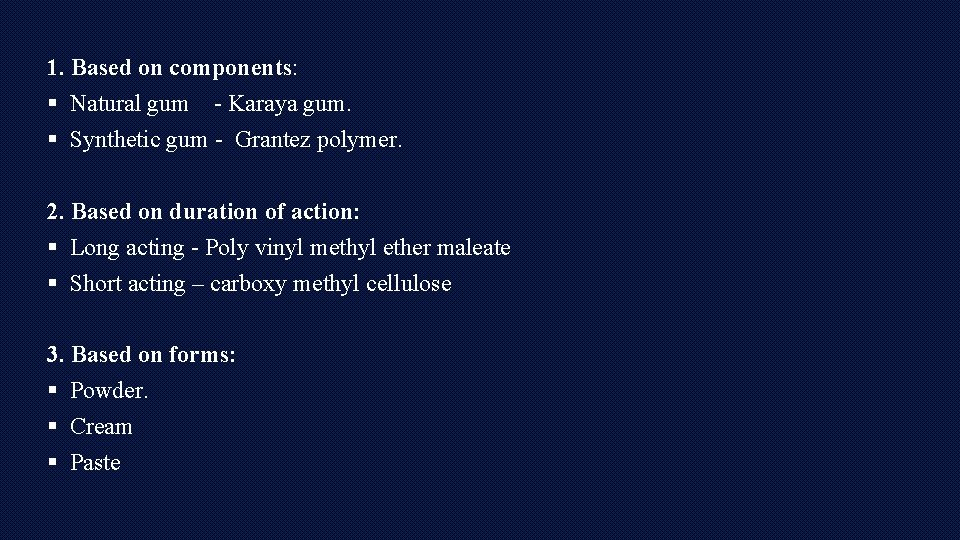
1. Based on components: § Natural gum - Karaya gum. § Synthetic gum - Grantez polymer. 2. Based on duration of action: § Long acting - Poly vinyl methyl ether maleate § Short acting – carboxy methyl cellulose 3. Based on forms: § Powder. § Cream § Paste
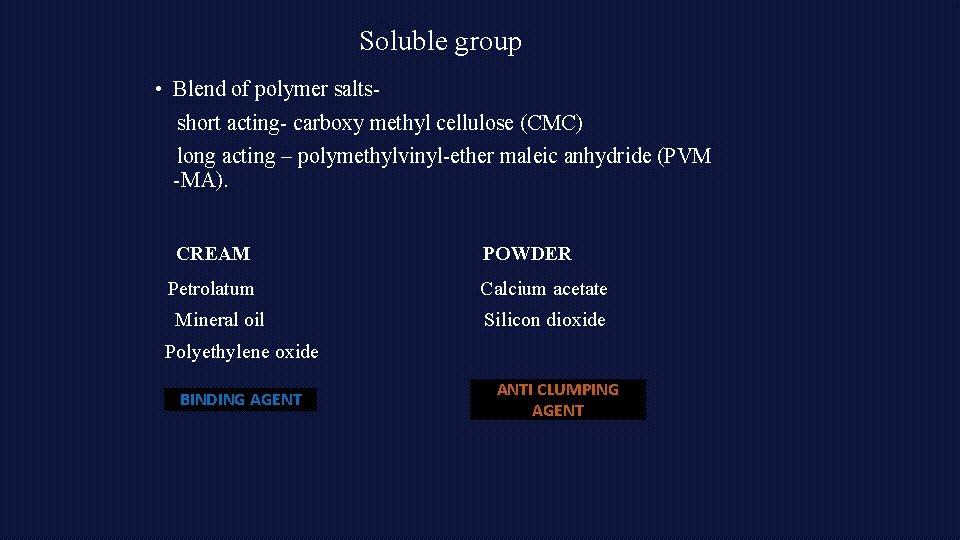
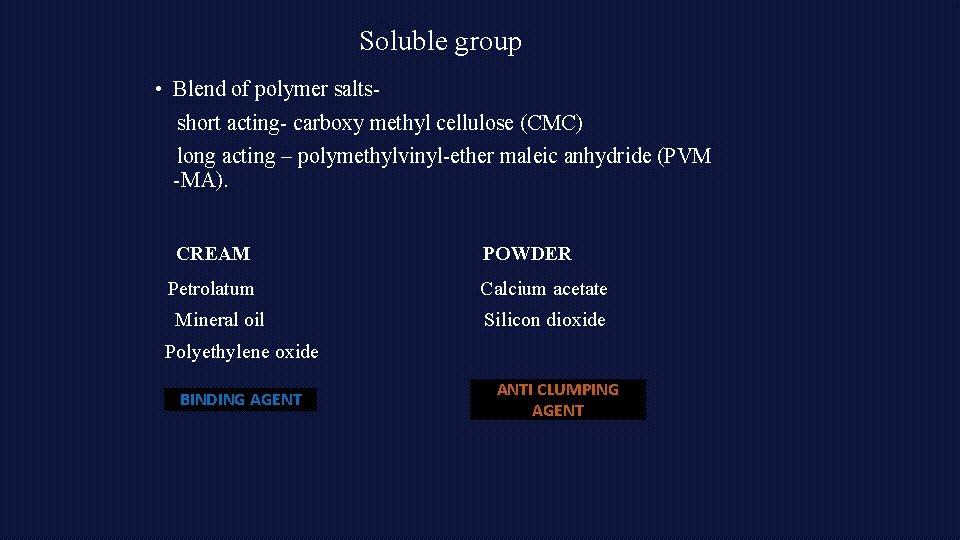
Soluble group • Blend of polymer saltsshort acting- carboxy methyl cellulose (CMC) long acting – polymethylvinyl-ether maleic anhydride (PVM -MA). CREAM Petrolatum Mineral oil POWDER Calcium acetate Silicon dioxide Polyethylene oxide BINDING AGENT ANTI CLUMPING AGENT
• FLAVORING -Menthol and peppermint oil • COLOR - dye • PRESERVATIVES-Sodium borate and methylparaben or polyparaben
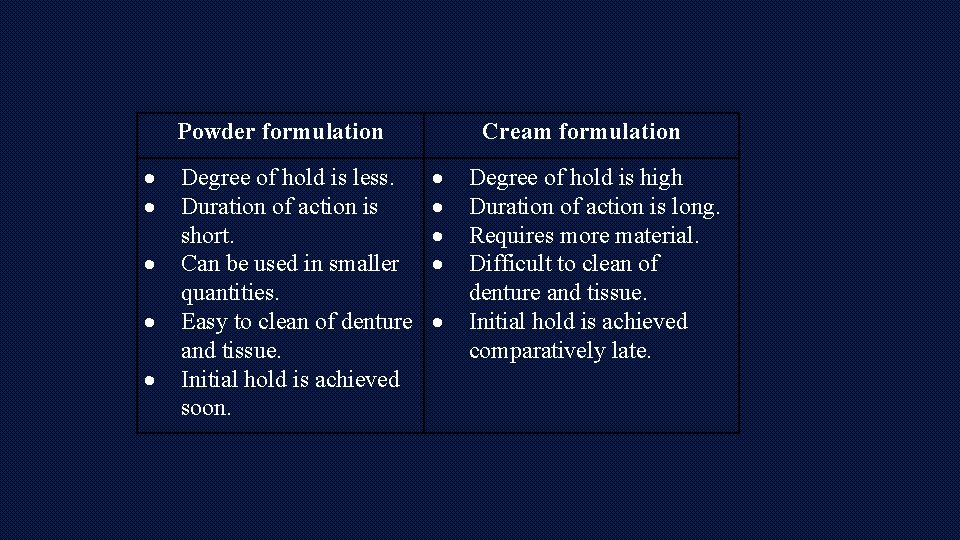
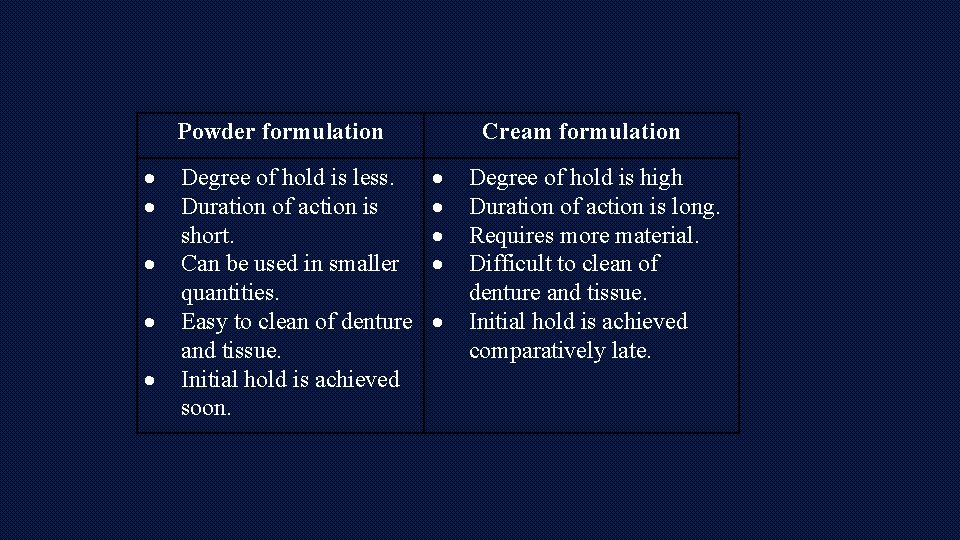
Powder formulation Degree of hold is less. Duration of action is short. Can be used in smaller quantities. Easy to clean of denture and tissue. Initial hold is achieved soon. Cream formulation Degree of hold is high Duration of action is long. Requires more material. Difficult to clean of denture and tissue. Initial hold is achieved comparatively late.
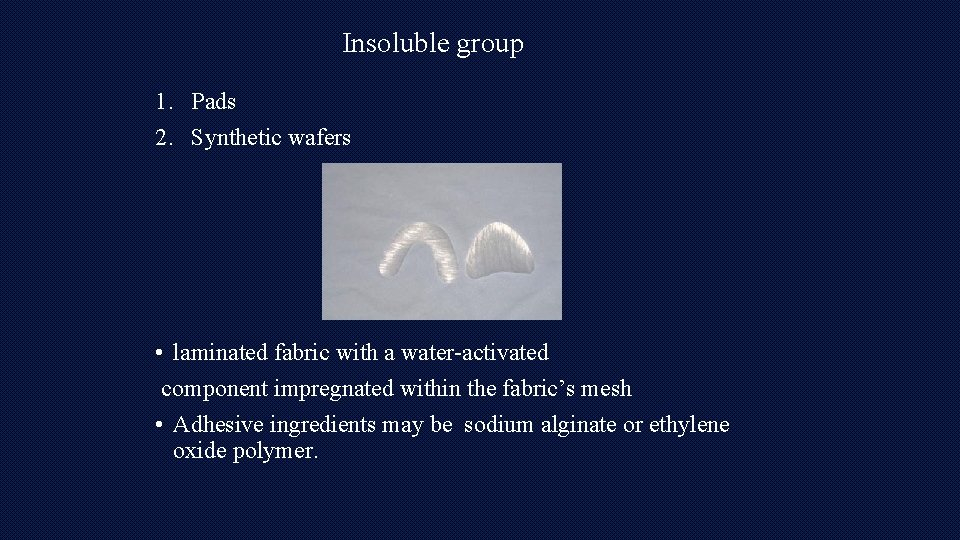
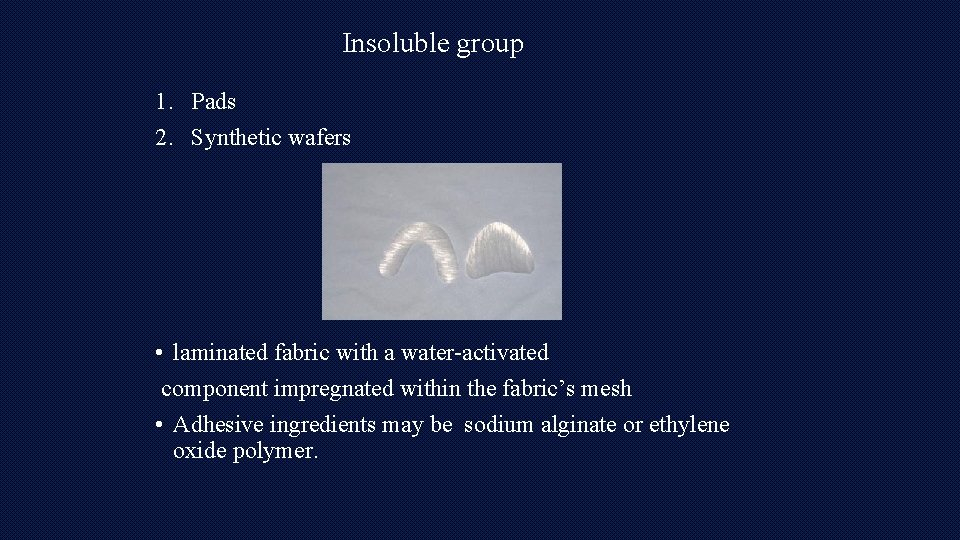
Insoluble group 1. Pads 2. Synthetic wafers • laminated fabric with a water-activated component impregnated within the fabric’s mesh • Adhesive ingredients may be sodium alginate or ethylene oxide polymer.
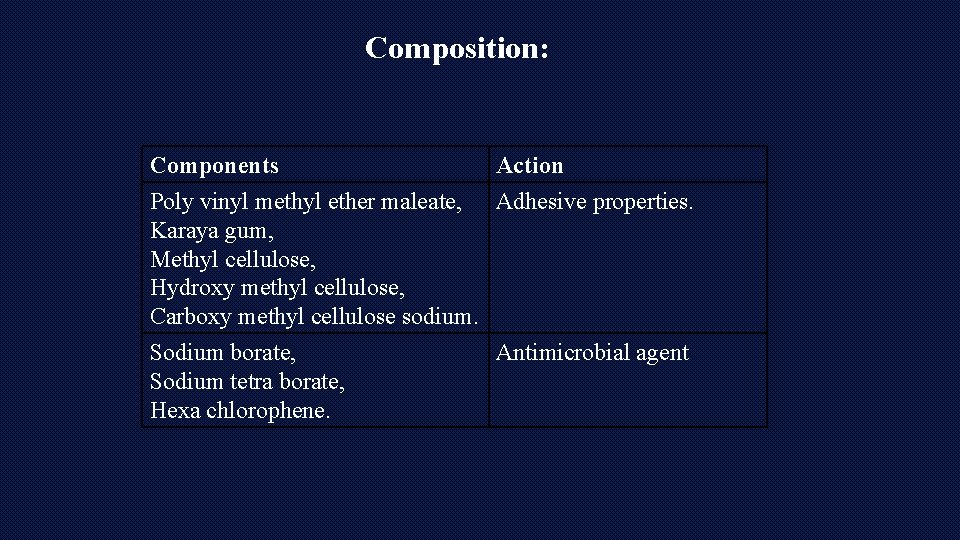
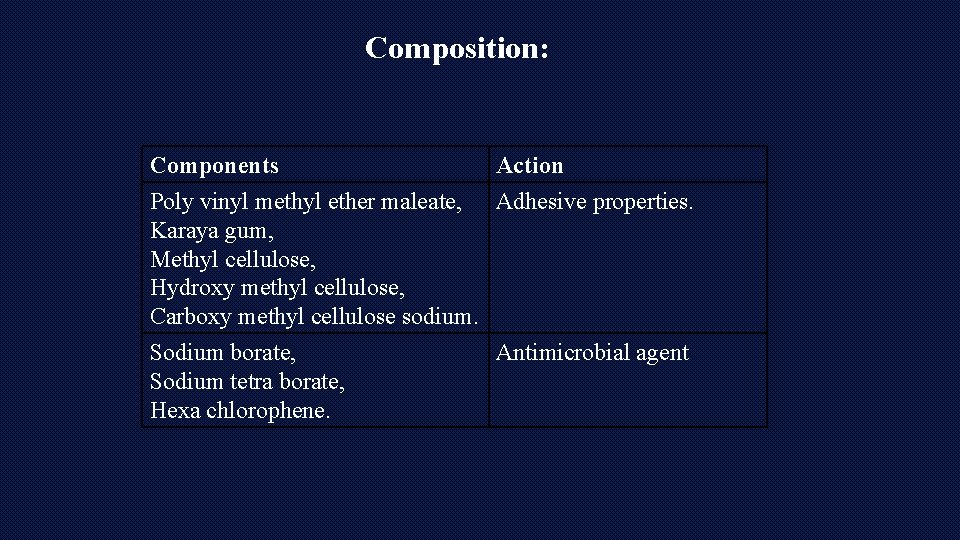
Composition: Components Action Poly vinyl methyl ether maleate, Adhesive properties. Karaya gum, Methyl cellulose, Hydroxy methyl cellulose, Carboxy methyl cellulose sodium. Sodium borate, Antimicrobial agent Sodium tetra borate, Hexa chlorophene.
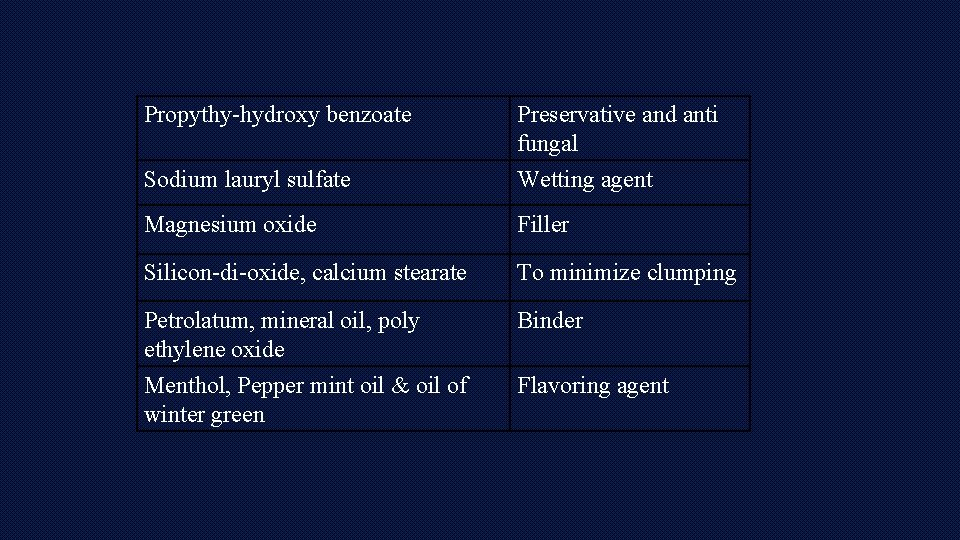
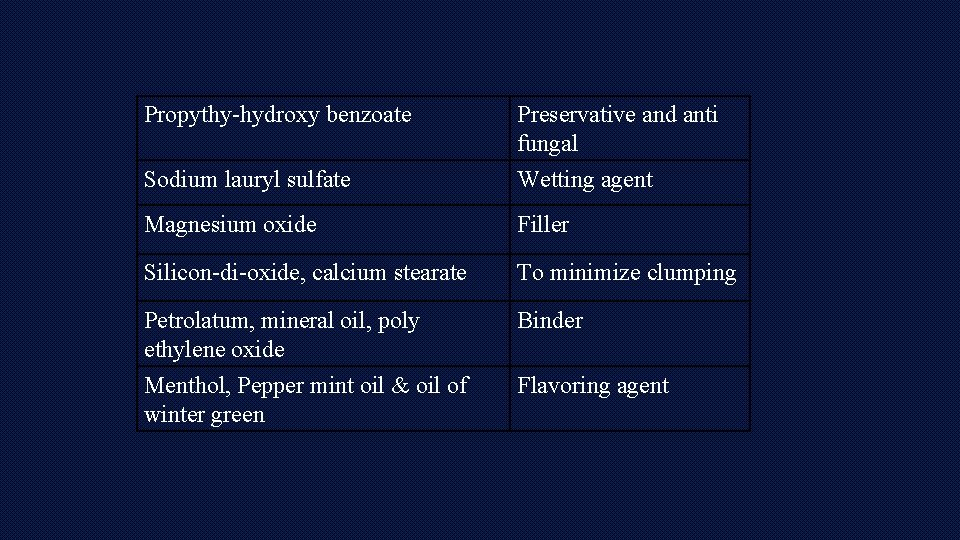
Propythy-hydroxy benzoate Sodium lauryl sulfate Preservative and anti fungal Wetting agent Magnesium oxide Filler Silicon-di-oxide, calcium stearate To minimize clumping Petrolatum, mineral oil, poly ethylene oxide Binder Menthol, Pepper mint oil & oil of winter green Flavoring agent
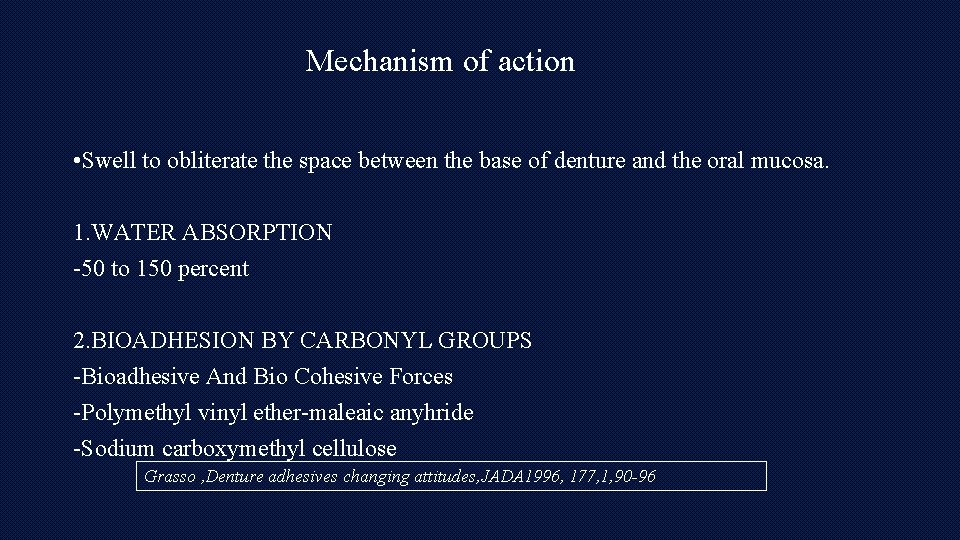
Mechanism of action • Swell to obliterate the space between the base of denture and the oral mucosa. 1. WATER ABSORPTION -50 to 150 percent 2. BIOADHESION BY CARBONYL GROUPS -Bioadhesive And Bio Cohesive Forces -Polymethyl vinyl ether-maleaic anyhride -Sodium carboxymethyl cellulose Grasso , Denture adhesives changing attitudes, JADA 1996, 177, 1, 90 -96
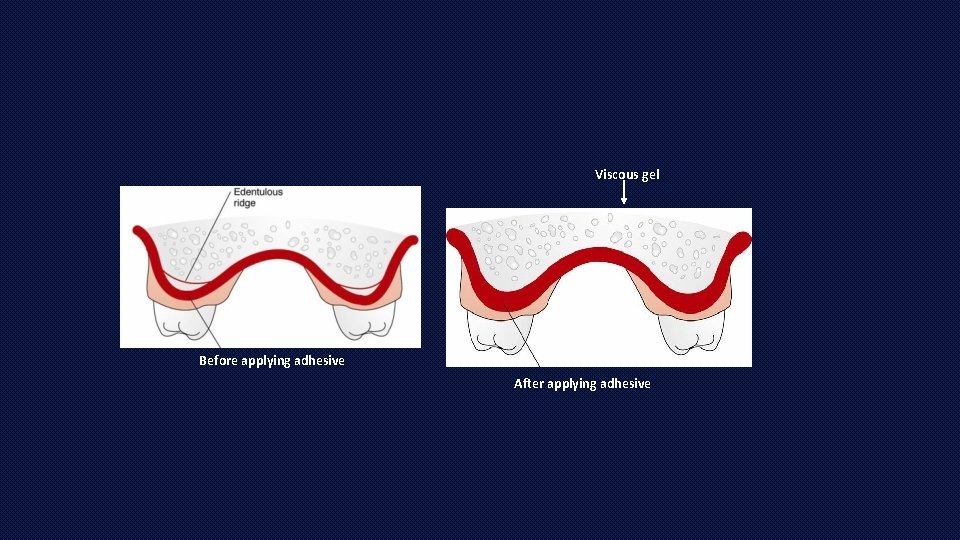
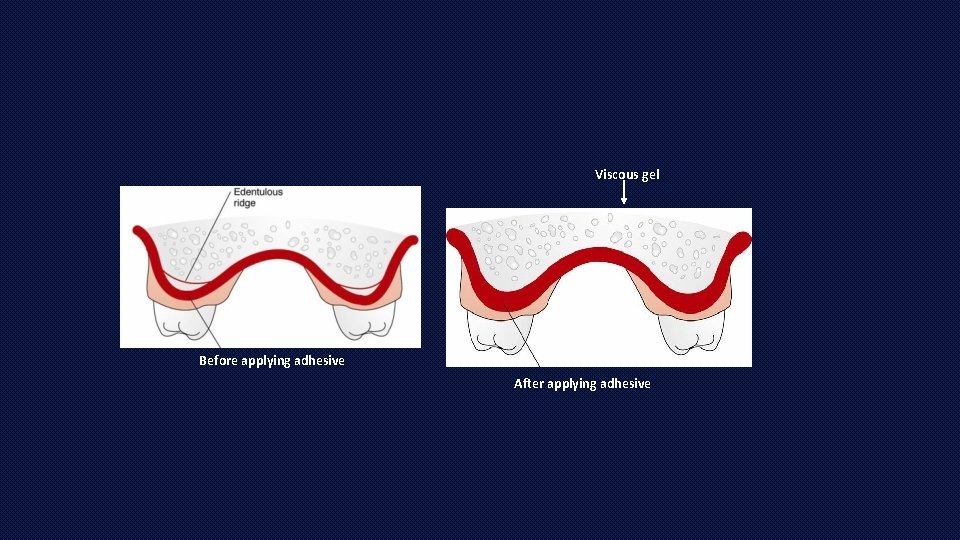
Viscous gel Before applying adhesive After applying adhesive
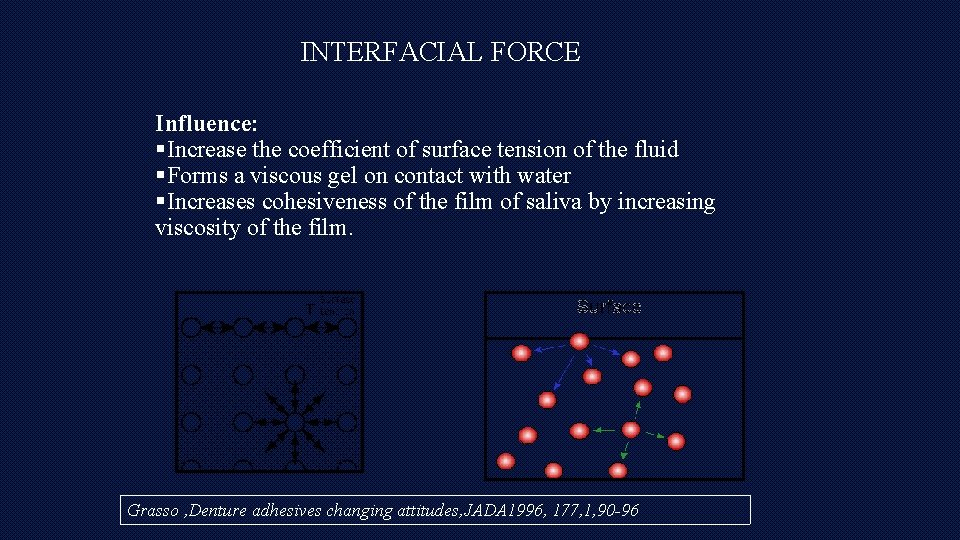
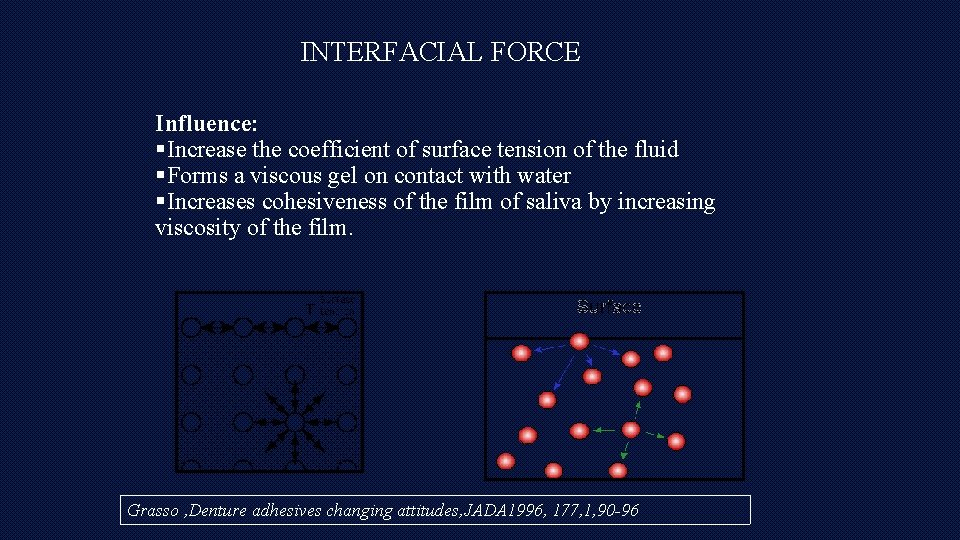
INTERFACIAL FORCE Influence: §Increase the coefficient of surface tension of the fluid §Forms a viscous gel on contact with water §Increases cohesiveness of the film of saliva by increasing viscosity of the film. Grasso , Denture adhesives changing attitudes, JADA 1996, 177, 1, 90 -96
Ideal requirements • • Physically it should be in a powder, cream, or a gel form. nontoxic, non-irritant, and biocompatible with the oral mucosa. odorless and tasteless. easy to apply and to remove from the tissue surface of the denture. • Should not promote microbial growth. • Should retain its adhesive properties for 12– 16 h. • Provide comfort, retention and stability to the denture,
INDICATIONS 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. Jaw relation records Try in Insertion of denture Immediate dentures Reduction of tissue irritation Systematic diseases Maxillofacial surgery patients Administration of drug therapy For extra severity of stable denture Osseointegrated implants Removable partial dentures
Contraindications 1. 2. 3. 4. 5. Allergy Inadequate ill fitting and function dentures Excessive loss of vertical dimension Broken dentures Improperly using denture adhesive
ADVANTAGES • Reduces irritation • Increases masticatory efficacy • Psycological benefit • Retention • Stability DISADVANTAGES • Poor oral hygiene • Tissue destruction-insoluble adhesives
Can Denture Adhesives Contribute To Oral Pathoses? Growth of microorganisms in denture adhesives • Denture adhesives often include antimicrobial agents such as hexachlorophene, sodium tetra borate, methyl salicylate, sodium borate and amphotericin (Kim 2003, Okzan 2012). • Adhesives do not have an inhibitory effect upon the oral flora, whereas others were claimed to promote Streptococcus mitis and C. albicans growth (Stafford, 1971). • Adisman (1989) denture adhesives have a cushion effect and thereby prevent the food bolus going underneath the denture and eventually inhibit C. albicans growth.
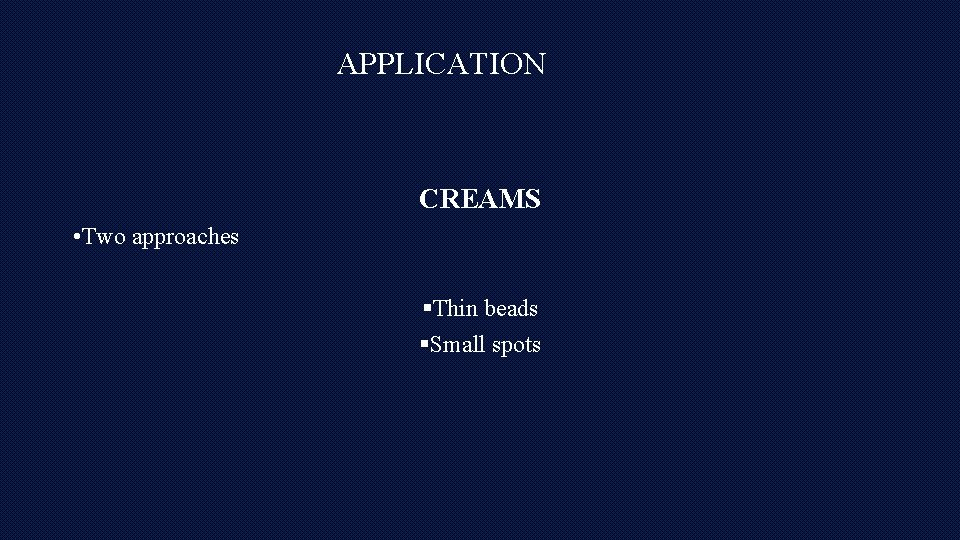
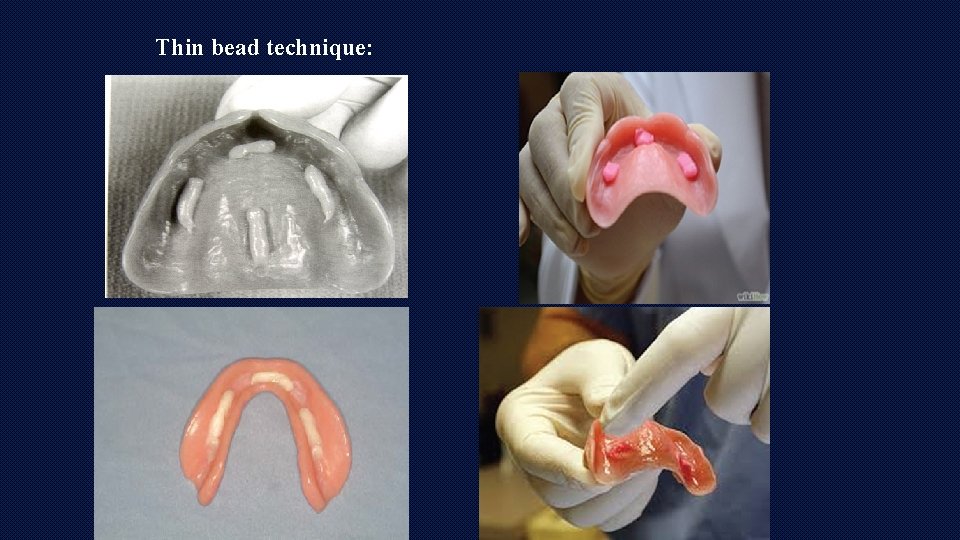
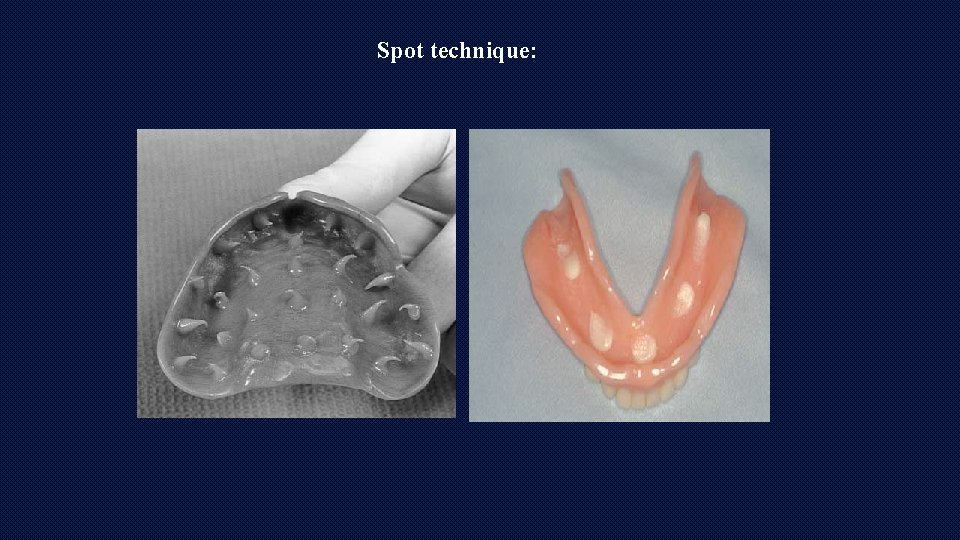
APPLICATION CREAMS • Two approaches §Thin beads §Small spots
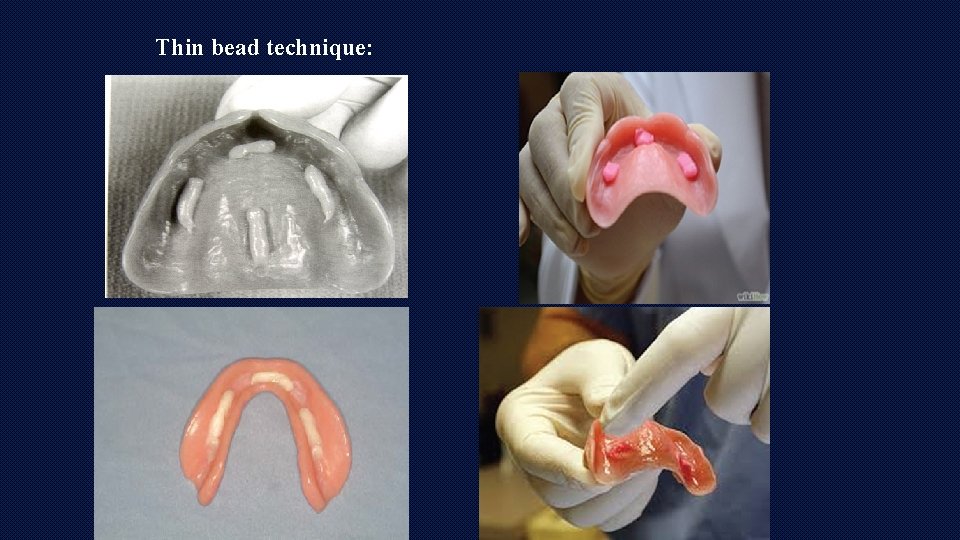
Thin bead technique:
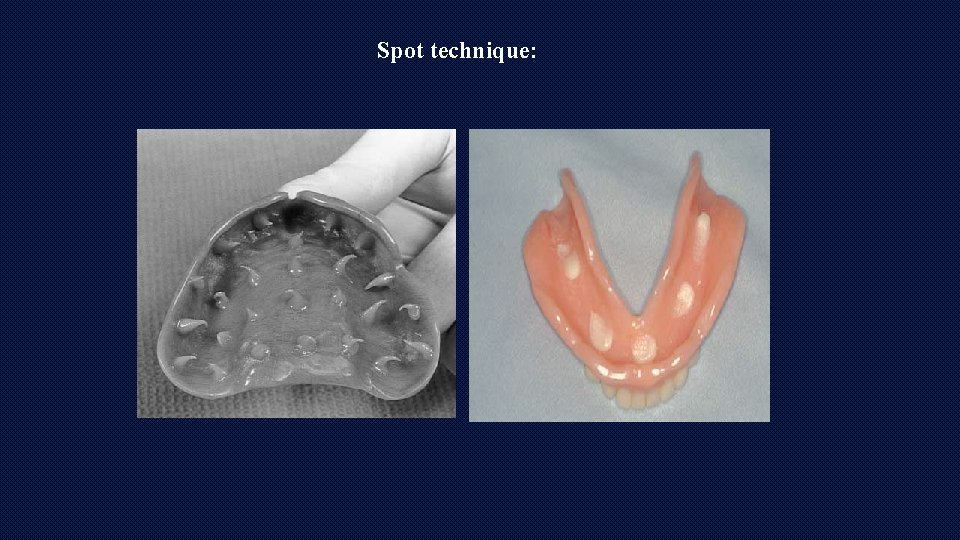
Spot technique:
advantages • • • A more controlled application Less likelihood of applying an excessive amount Elimination of ooze Easier to achieve a more even distribution Helps impress upon the patient that he/she has control of the amount used
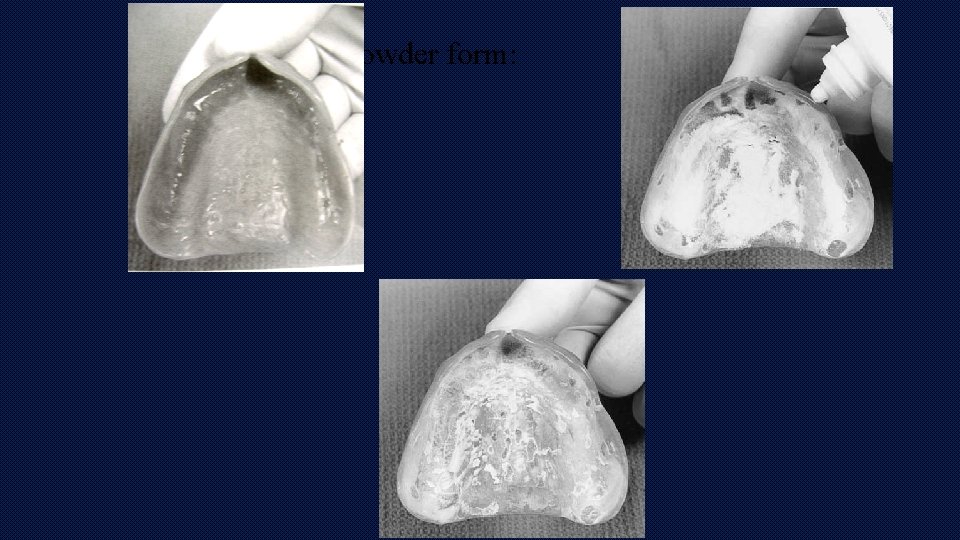
Powder form:
Pads and synthetic wafers • fabric carrier impregnated with an adhesive.
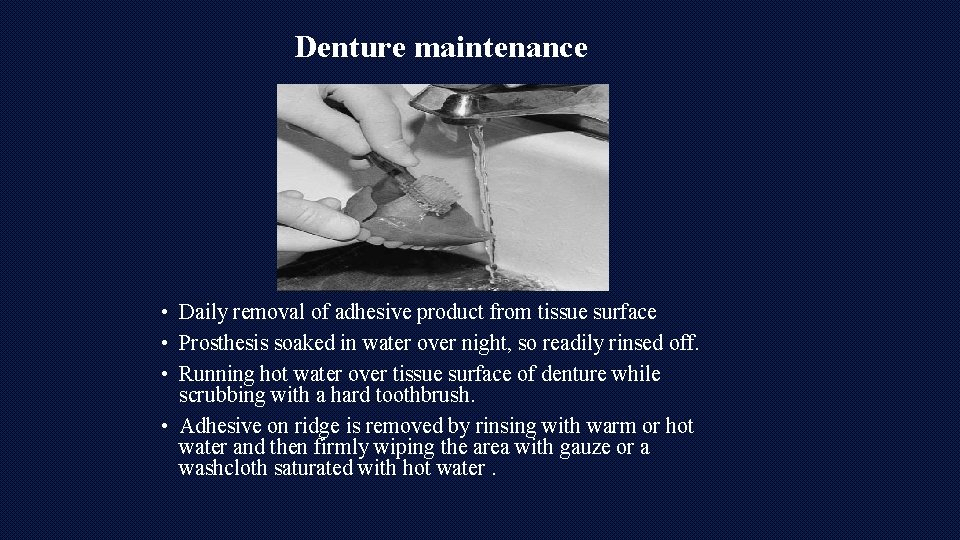
Denture maintenance • Daily removal of adhesive product from tissue surface • Prosthesis soaked in water over night, so readily rinsed off. • Running hot water over tissue surface of denture while scrubbing with a hard toothbrush. • Adhesive on ridge is removed by rinsing with warm or hot water and then firmly wiping the area with gauze or a washcloth saturated with hot water.
Ada REQUIREMENTS • • Product composition should be supplied Should not affect the integrity of denture Biologically acceptable Effective function as adherant
1. 2. 3. 4. Polygrip Fixodent Fitty dent Fixon

4. Cushion grip 5. Sea bond 6. End slip