Greenstick fracture Transverse fracture Fracture Epiphyseal Fracture Torus



























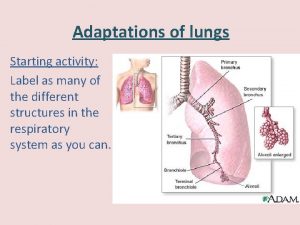
- Slides: 173
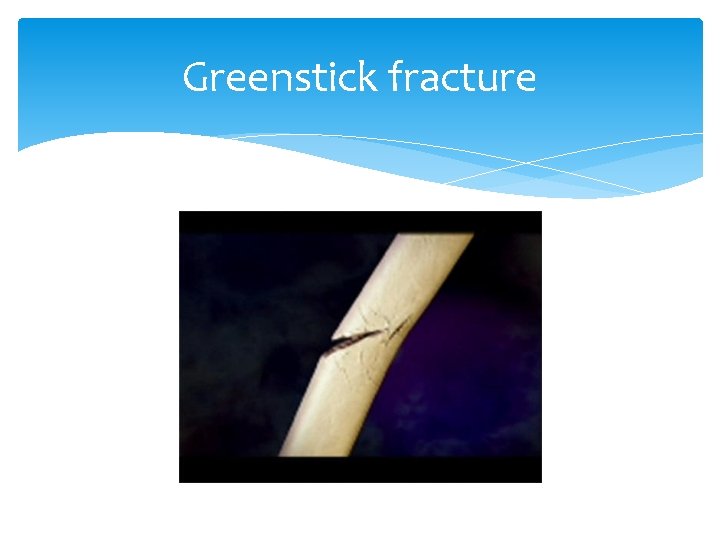
Greenstick fracture

Transverse fracture Fracture

Epiphyseal Fracture
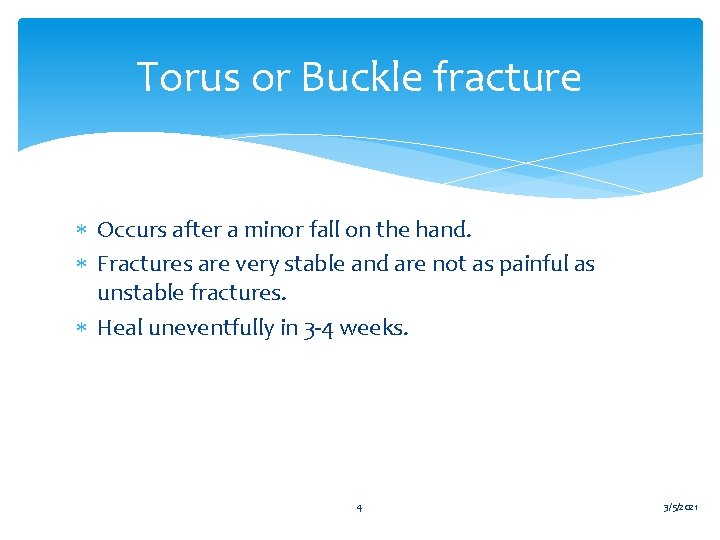
Torus or Buckle fracture Occurs after a minor fall on the hand. Fractures are very stable and are not as painful as unstable fractures. Heal uneventfully in 3 -4 weeks. 4 3/5/2021
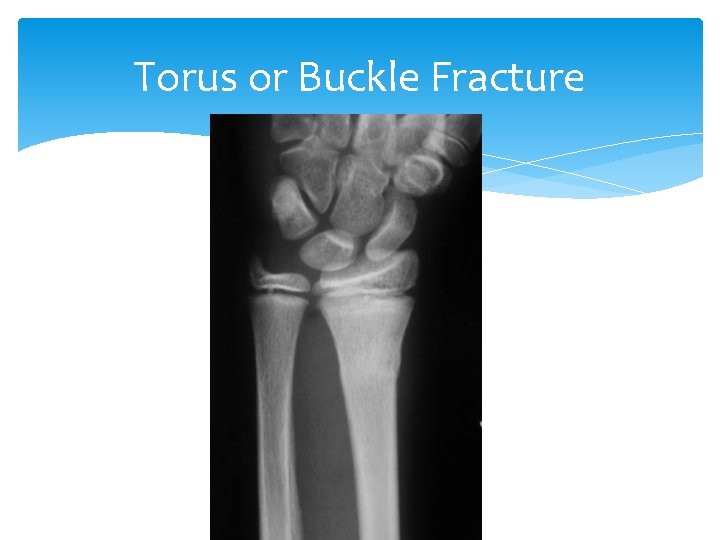
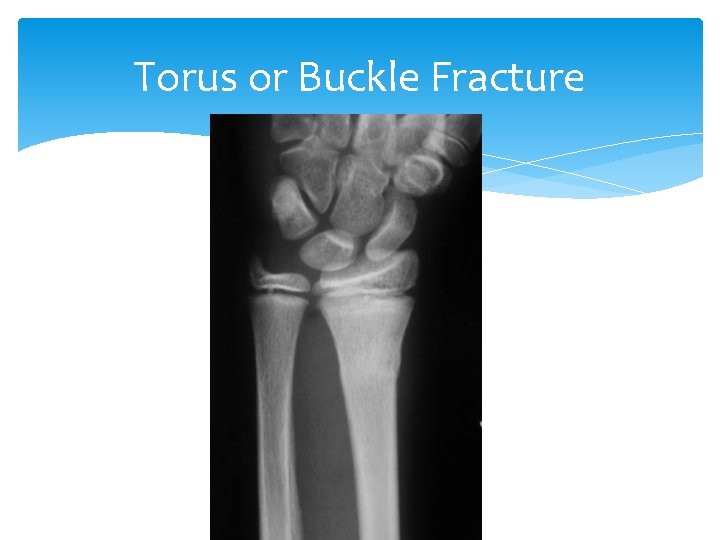
Torus or Buckle Fracture
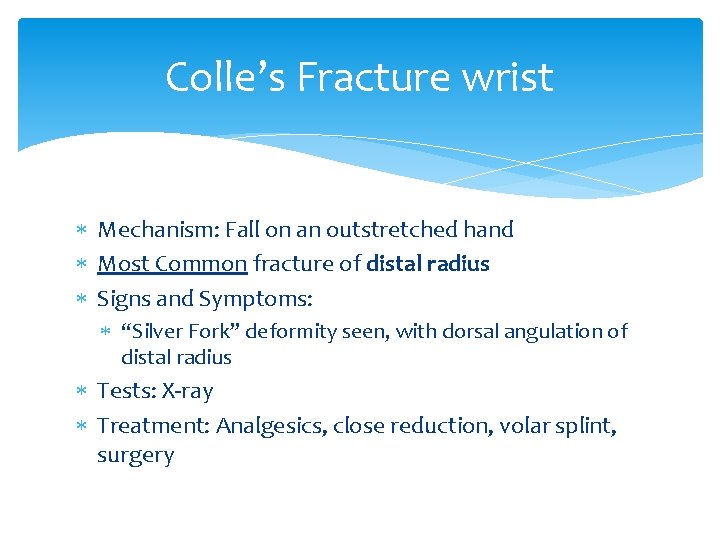
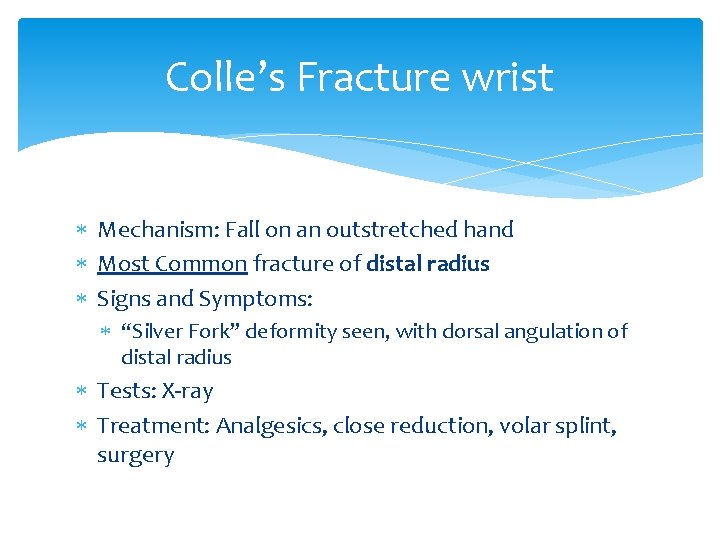
Colle’s Fracture wrist Mechanism: Fall on an outstretched hand Most Common fracture of distal radius Signs and Symptoms: “Silver Fork” deformity seen, with dorsal angulation of distal radius Tests: X-ray Treatment: Analgesics, close reduction, volar splint, surgery

Colle’s Fracture

Colle’s Fracture

Smith’s Fracture Opposite of Colle’s Fracture, “Smith Fracture” or “Reverse Colles” has volar angulation of distal radius Swelling, tenderness, deformity Volar wrist splint
DON’T CAST UNTIL SWELLING HAS SUBSIDED!! Putting on a cast while the injury is acute risks causing compromise of circulation. Leave finger tips exposed to check color, sensation, movement and cap refill! Have patient remove elastic bandages (splint) and re-apply more loosely as required
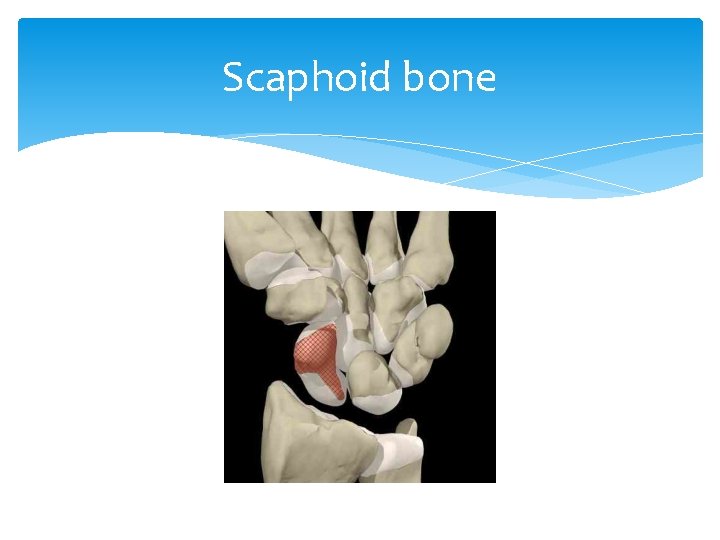
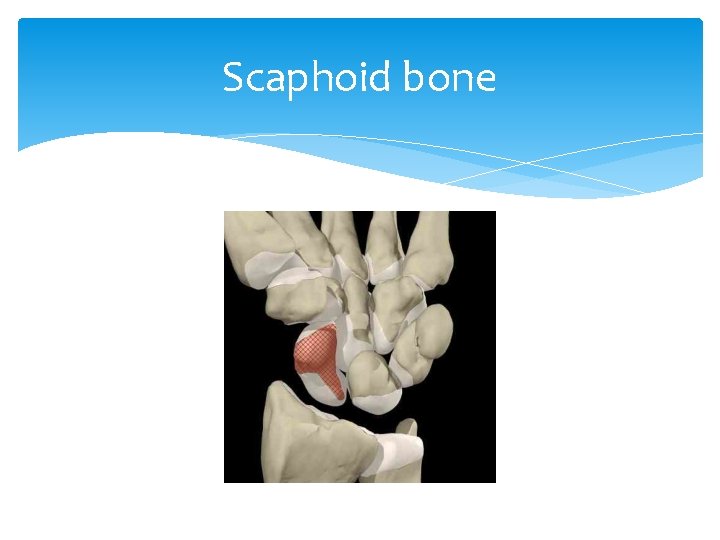
Scaphoid bone
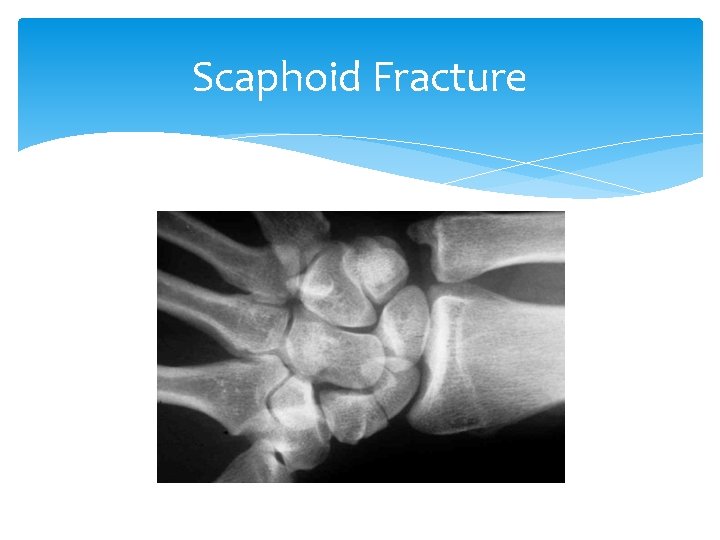
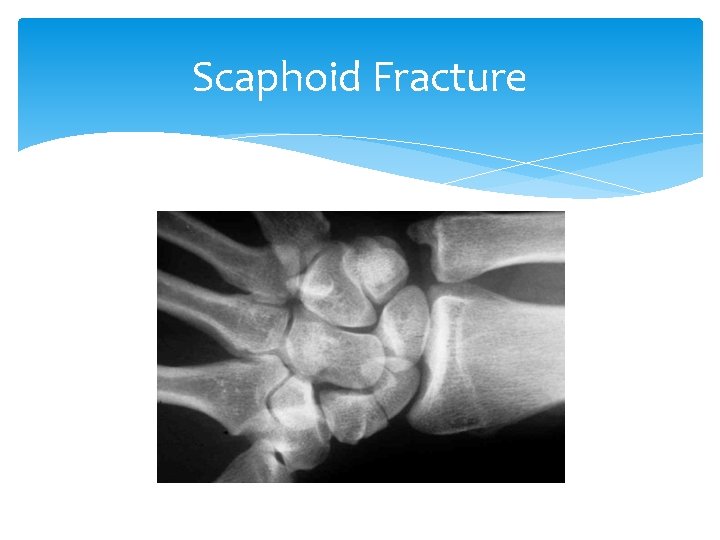
Scaphoid Fracture
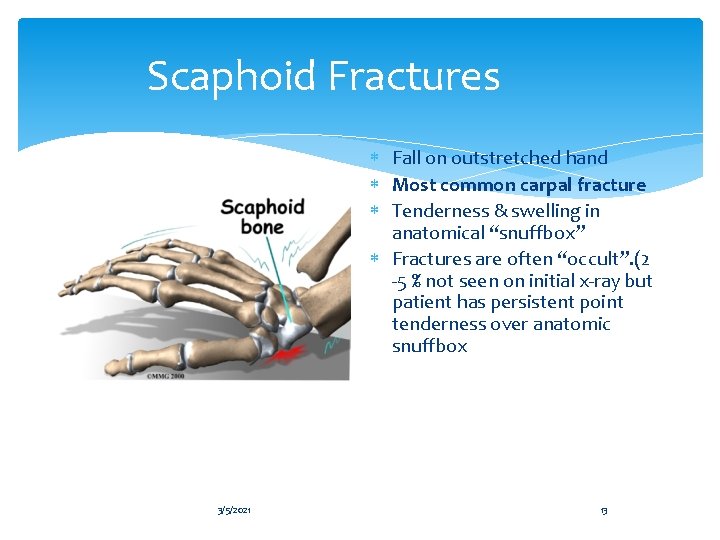
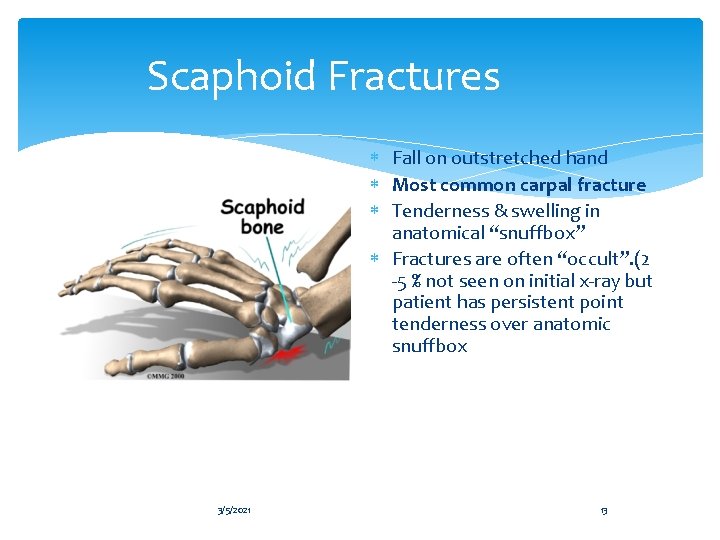
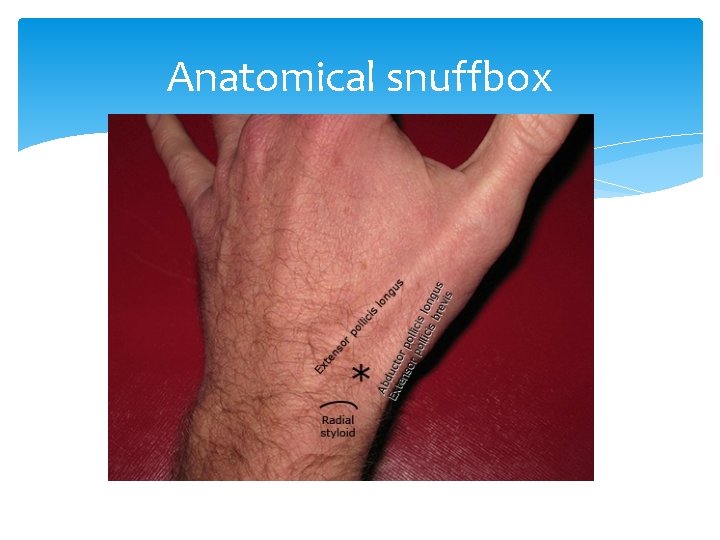
Scaphoid Fractures Fall on outstretched hand Most common carpal fracture Tenderness & swelling in anatomical “snuffbox” Fractures are often “occult”. (2 -5 % not seen on initial x-ray but patient has persistent point tenderness over anatomic snuffbox 3/5/2021 13
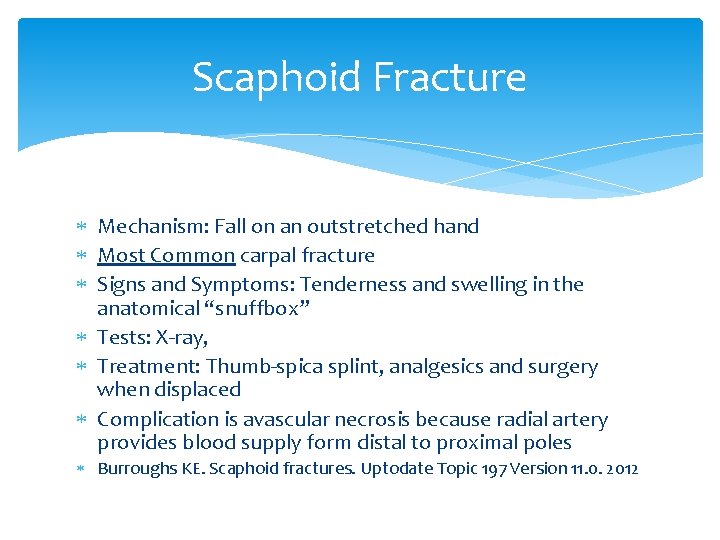
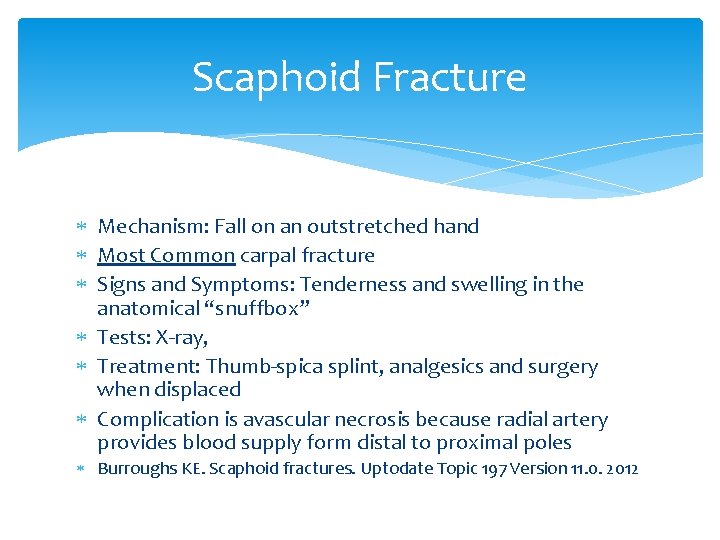
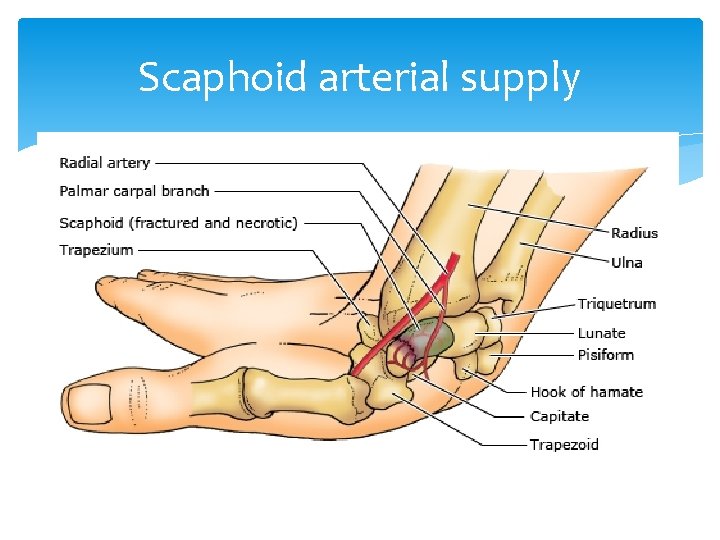
Scaphoid Fracture Mechanism: Fall on an outstretched hand Most Common carpal fracture Signs and Symptoms: Tenderness and swelling in the anatomical “snuffbox” Tests: X-ray, Treatment: Thumb-spica splint, analgesics and surgery when displaced Complication is avascular necrosis because radial artery provides blood supply form distal to proximal poles Burroughs KE. Scaphoid fractures. Uptodate Topic 197 Version 11. 0. 2012
Scaphoid arterial supply
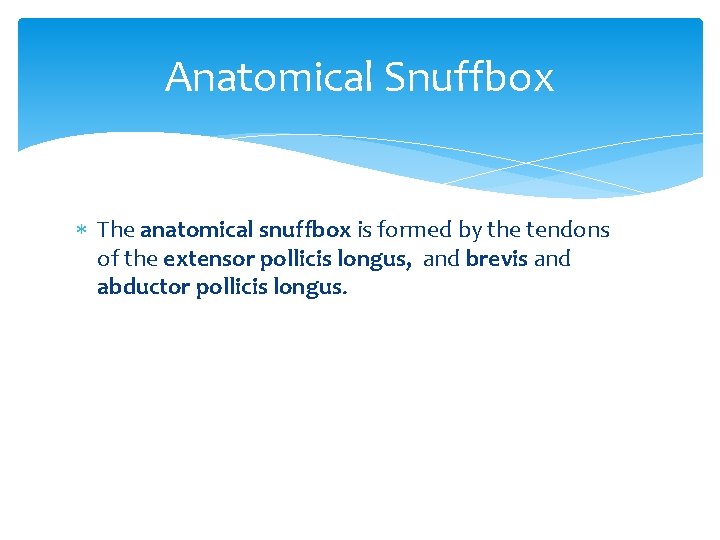
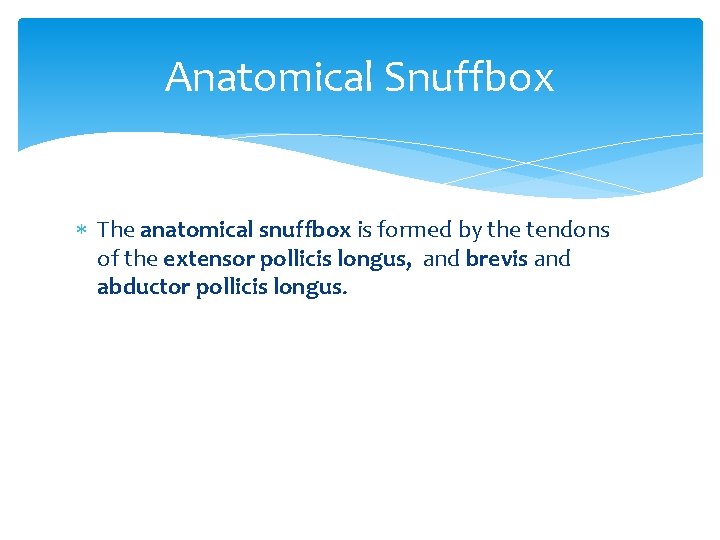
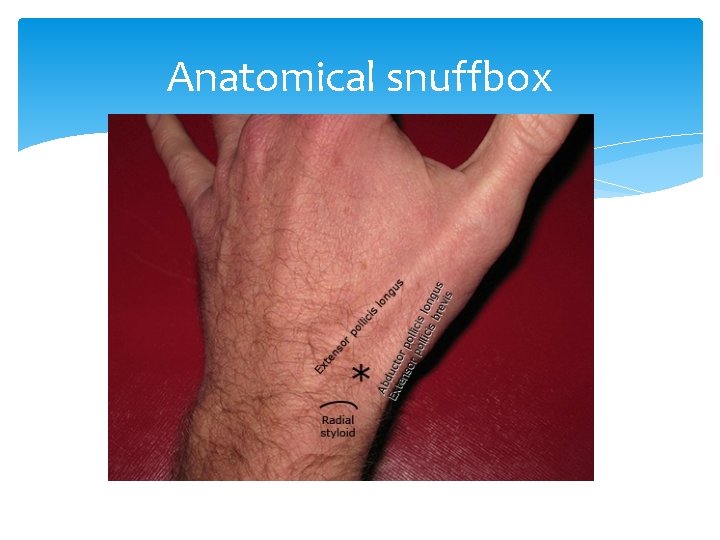
Anatomical Snuffbox The anatomical snuffbox is formed by the tendons of the extensor pollicis longus, and brevis and abductor pollicis longus.
Anatomical snuffbox
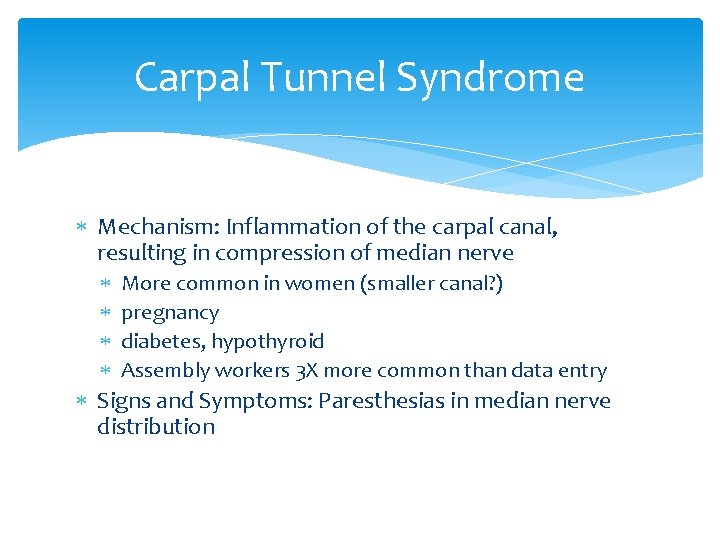
Carpal Tunnel Syndrome Mechanism: Inflammation of the carpal canal, resulting in compression of median nerve More common in women (smaller canal? ) pregnancy diabetes, hypothyroid Assembly workers 3 X more common than data entry Signs and Symptoms: Paresthesias in median nerve distribution
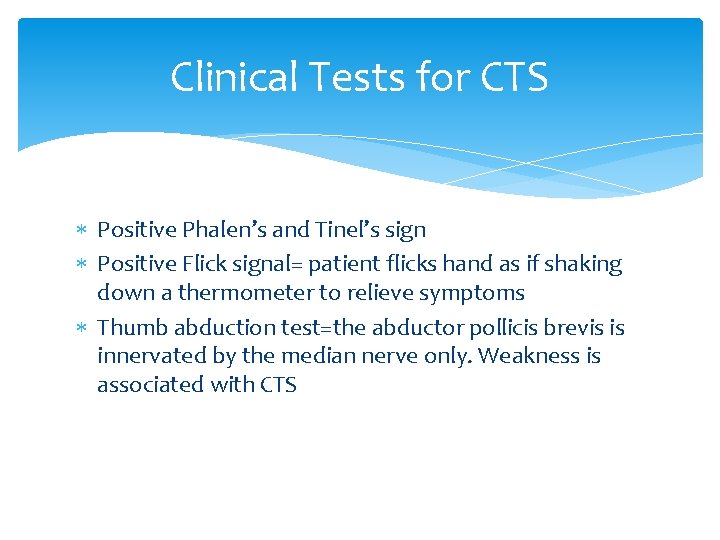
Clinical Tests for CTS Positive Phalen’s and Tinel’s sign Positive Flick signal= patient flicks hand as if shaking down a thermometer to relieve symptoms Thumb abduction test=the abductor pollicis brevis is innervated by the median nerve only. Weakness is associated with CTS
Phalen’s and Tinel’s signs Phalen’s 25% false positives Tinel’s 6 -45% false positives
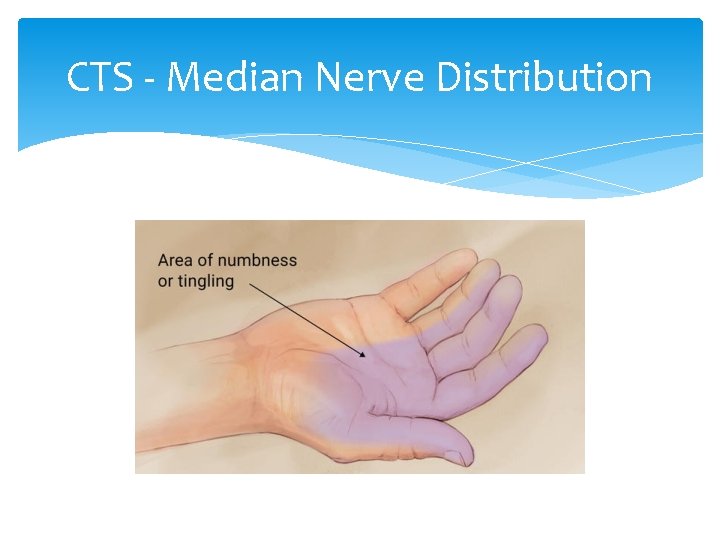
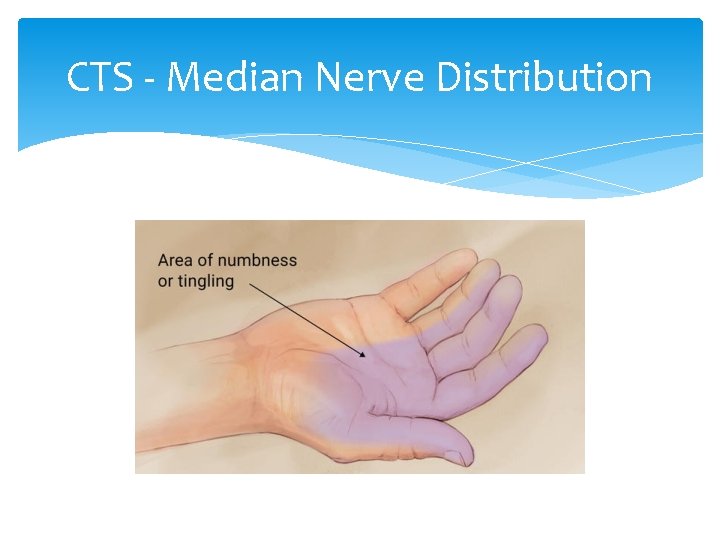
CTS - Median Nerve Distribution
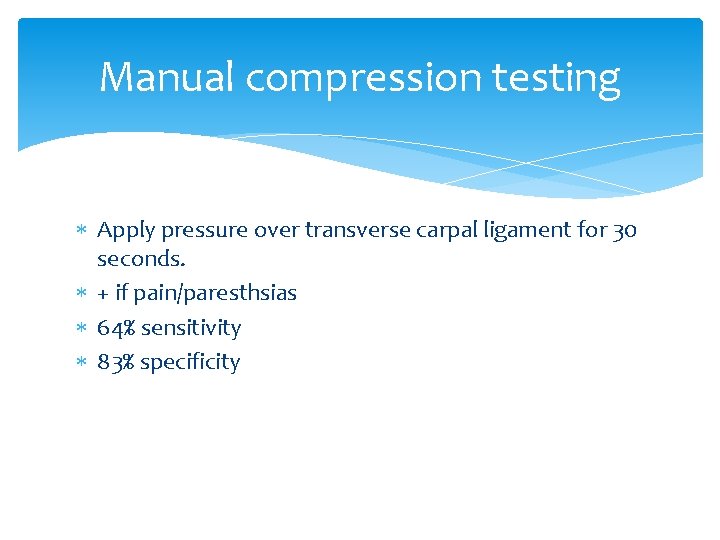
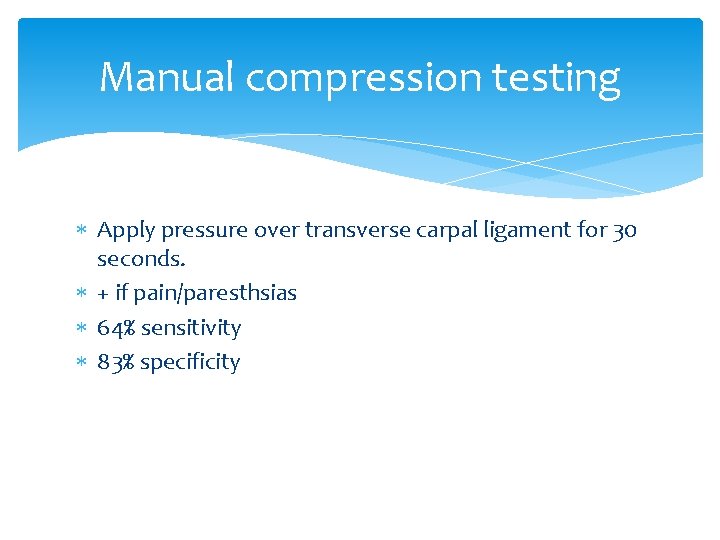
Manual compression testing Apply pressure over transverse carpal ligament for 30 seconds. + if pain/paresthsias 64% sensitivity 83% specificity
Electromyography, Nerve Conduction Study (EMG/NCS) Definitive diagnostic test Rules out other conditions
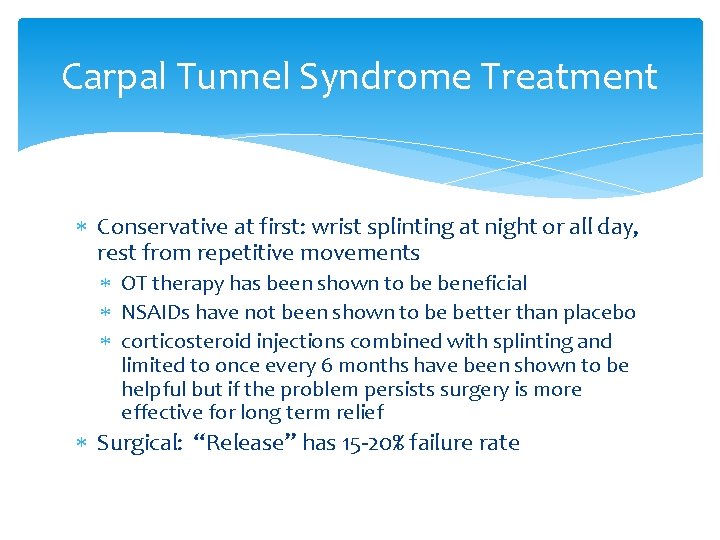
Carpal Tunnel Syndrome Treatment Conservative at first: wrist splinting at night or all day, rest from repetitive movements OT therapy has been shown to be beneficial NSAIDs have not been shown to be better than placebo corticosteroid injections combined with splinting and limited to once every 6 months have been shown to be helpful but if the problem persists surgery is more effective for long term relief Surgical: “Release” has 15 -20% failure rate
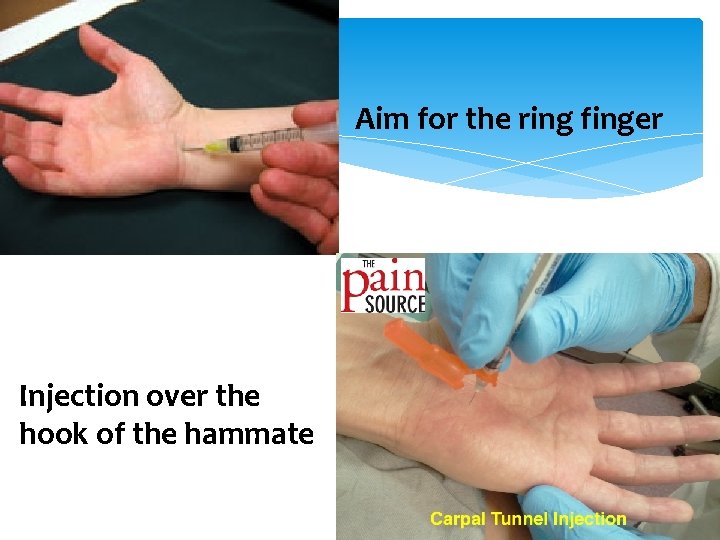
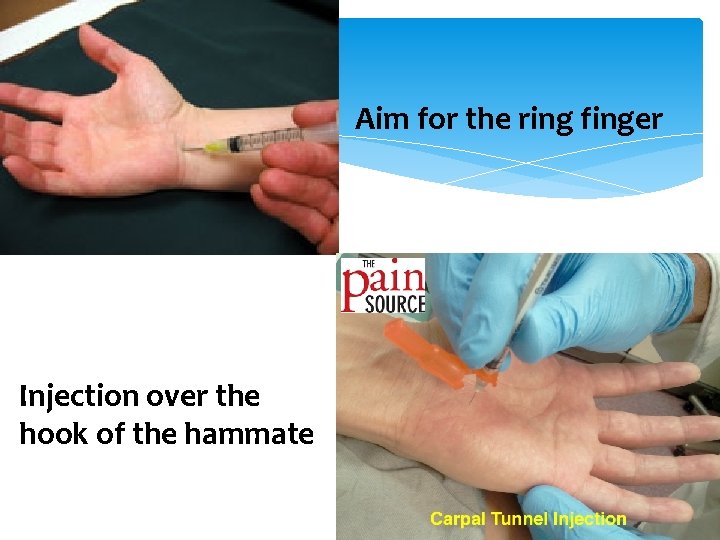
Aim for the ring finger Injection over the hook of the hammate
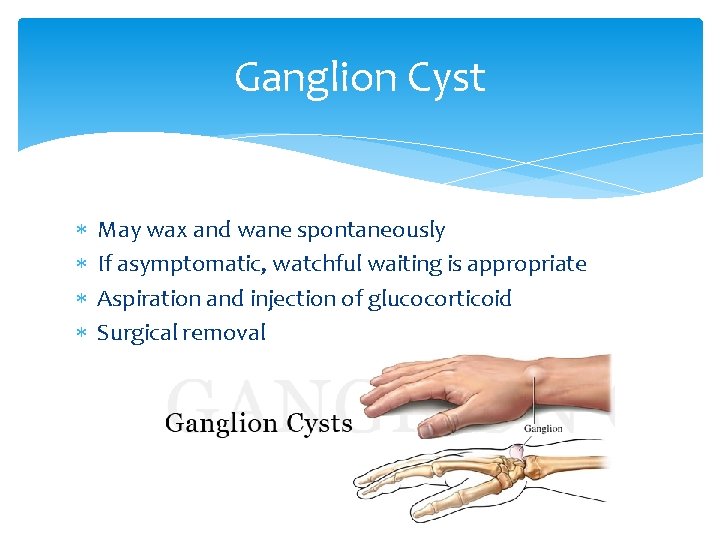
Ganglion Cyst May wax and wane spontaneously If asymptomatic, watchful waiting is appropriate Aspiration and injection of glucocorticoid Surgical removal
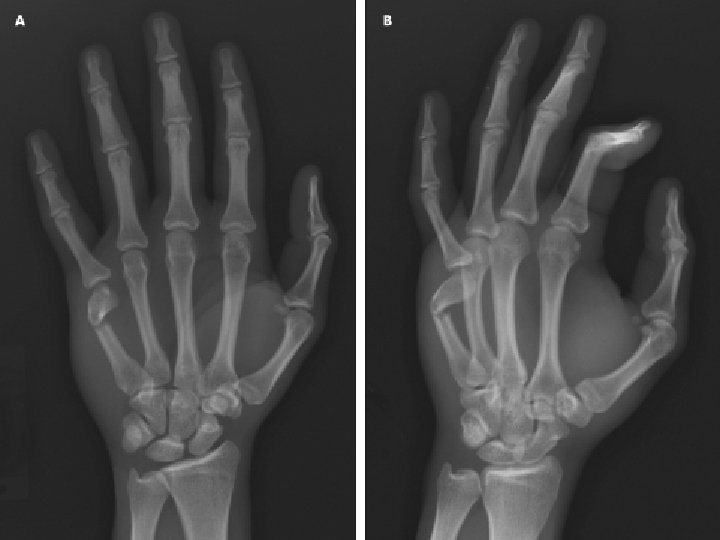
Boxer’s Fracture Mechanism: Closed-fist injury Fracture of the distal 5 th metacarpal Watch for knuckle lacerations! open fractures, tooth lac Signs and Symptoms: Pain, swelling, tenderness, and loss of prominence of knuckle at the little finger Tests: X-ray

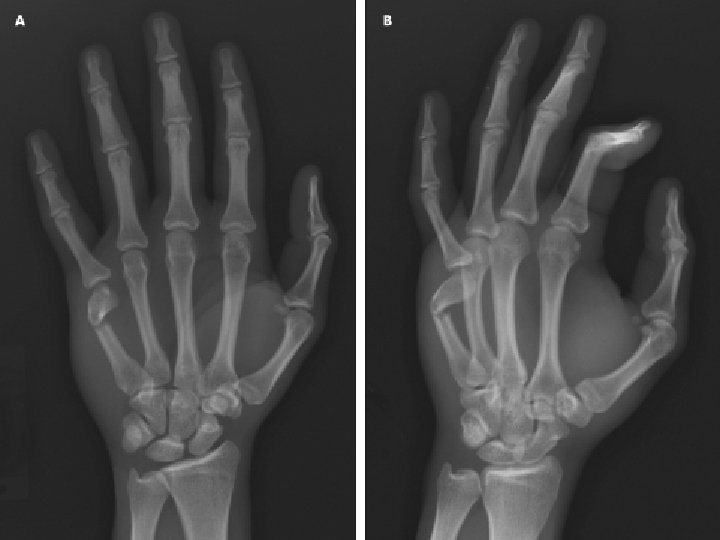
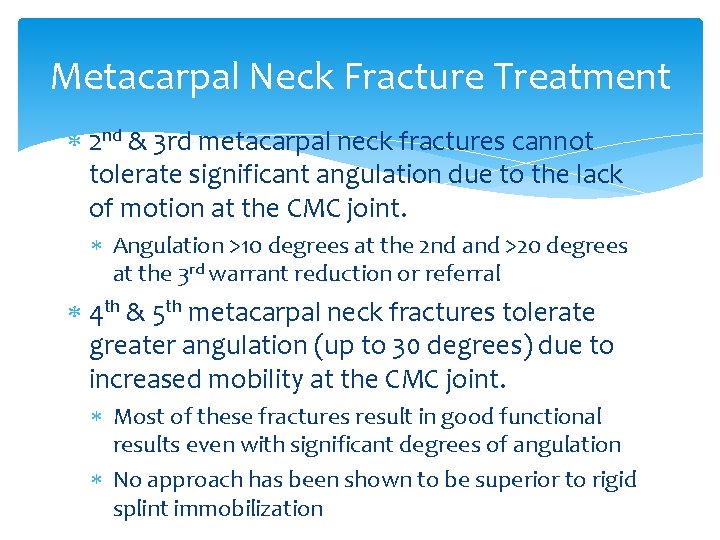
Metacarpal Neck Fracture Treatment 2 nd & 3 rd metacarpal neck fractures cannot tolerate significant angulation due to the lack of motion at the CMC joint. Angulation >10 degrees at the 2 nd and >20 degrees at the 3 rd warrant reduction or referral 4 th & 5 th metacarpal neck fractures tolerate greater angulation (up to 30 degrees) due to increased mobility at the CMC joint. Most of these fractures result in good functional results even with significant degrees of angulation No approach has been shown to be superior to rigid splint immobilization

Open Fractures Any fracture that breaks skin causes an increased risk of bacterial contamination of the wound. Osteomyelitis, gas gangrene or tetanus may occur. Treatment: IV antibiotics immediately. Admission and surgical debridement may be nesessary Ask about whether it was a punch to someone's face/teeth for HIV and Hepatitis exposure screen. 32 3/5/2021
De Quervain’s Tenosynovitis Covered by Dr. Cleveland Stenosing Tenosynovitis in which the synovial lining of the tunnel becomes inflamed and hurts with movement. Mechanism: Excessive use of the thumb Involves the tendons of 2 muscles—extensor pollicis brevis and abductor pollicis longus
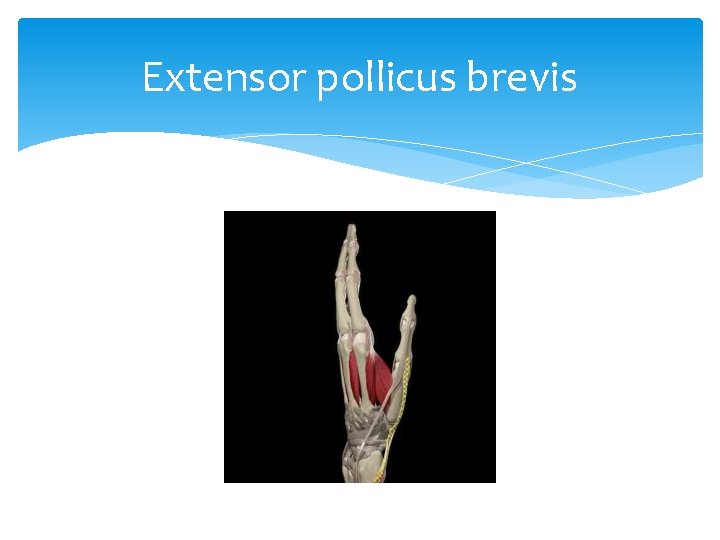
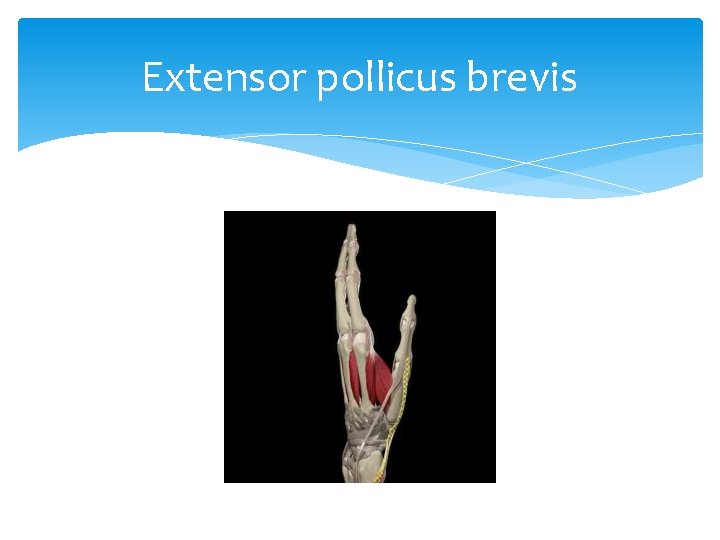
Extensor pollicus brevis
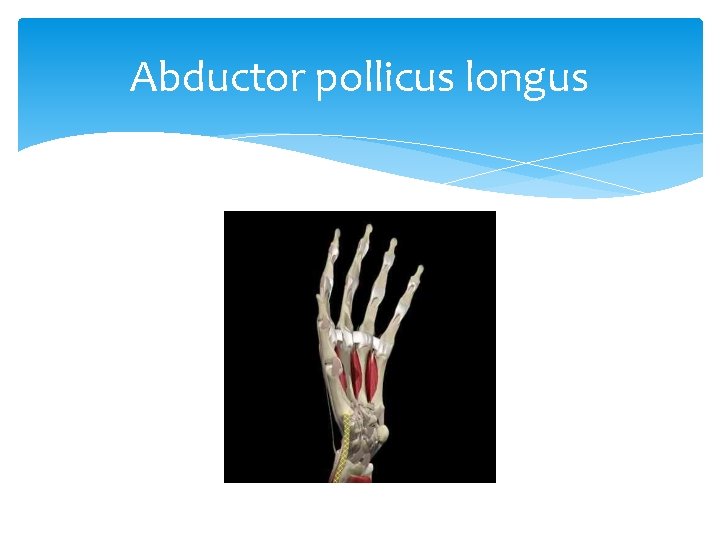
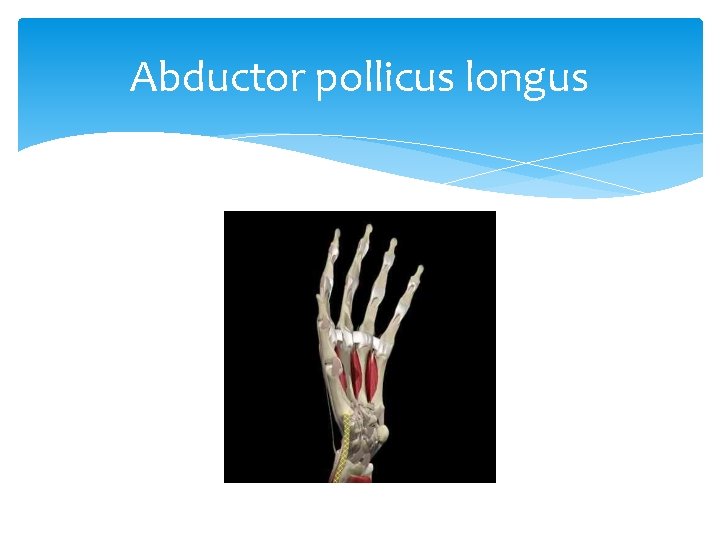
Abductor pollicus longus
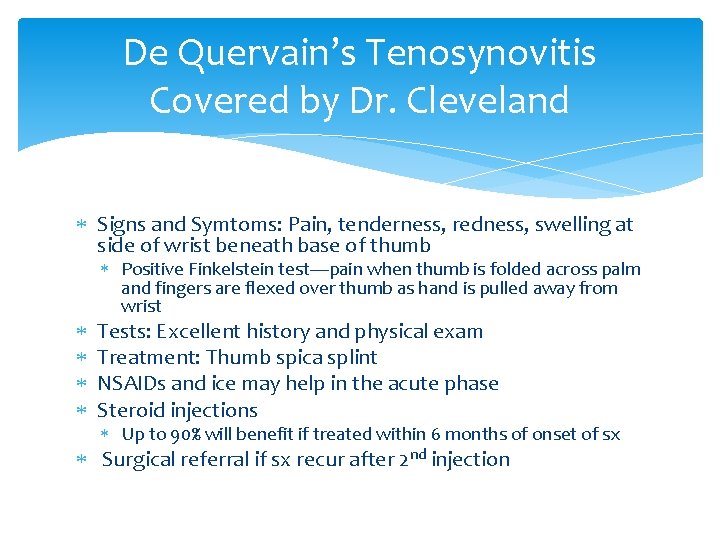
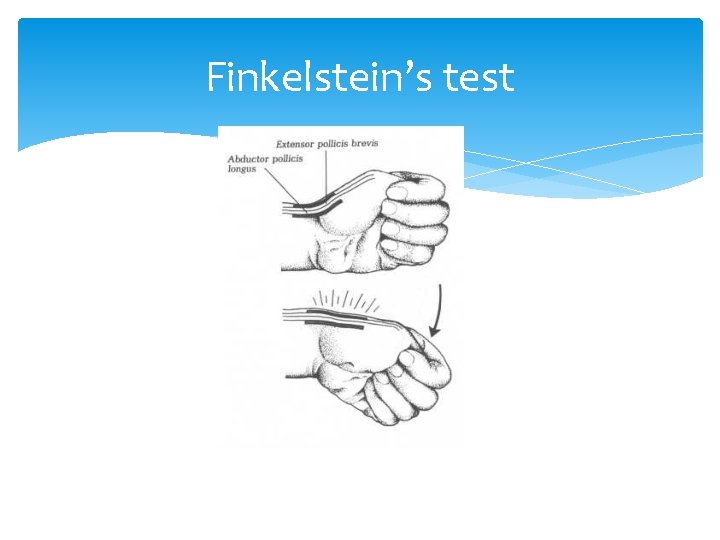
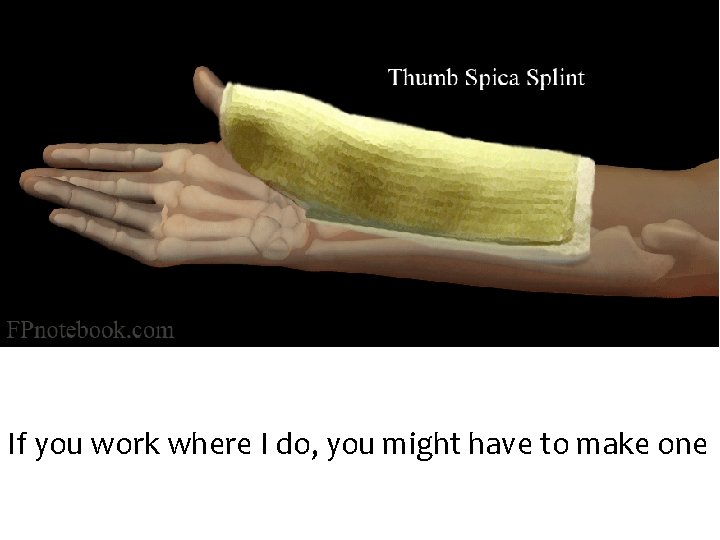
De Quervain’s Tenosynovitis Covered by Dr. Cleveland Signs and Symtoms: Pain, tenderness, redness, swelling at side of wrist beneath base of thumb Positive Finkelstein test—pain when thumb is folded across palm and fingers are flexed over thumb as hand is pulled away from wrist Tests: Excellent history and physical exam Treatment: Thumb spica splint NSAIDs and ice may help in the acute phase Steroid injections Up to 90% will benefit if treated within 6 months of onset of sx Surgical referral if sx recur after 2 nd injection
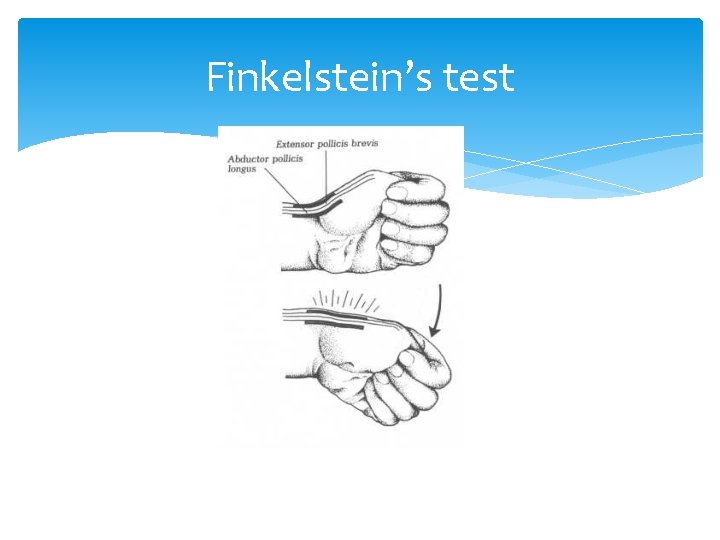
Finkelstein’s test
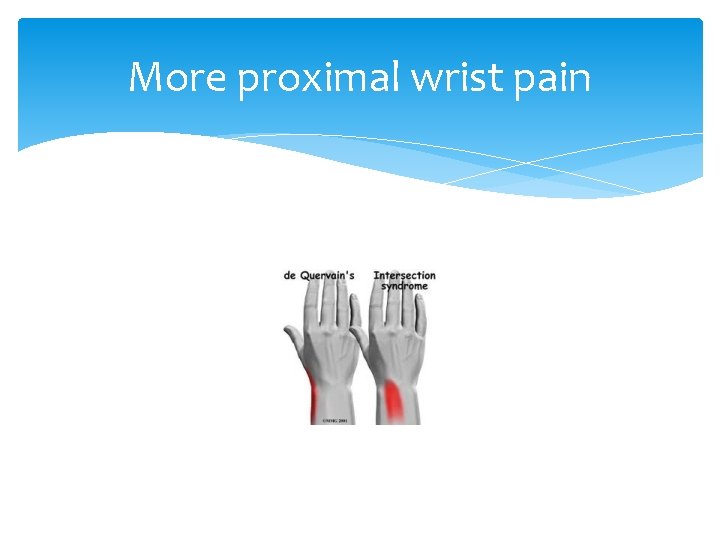
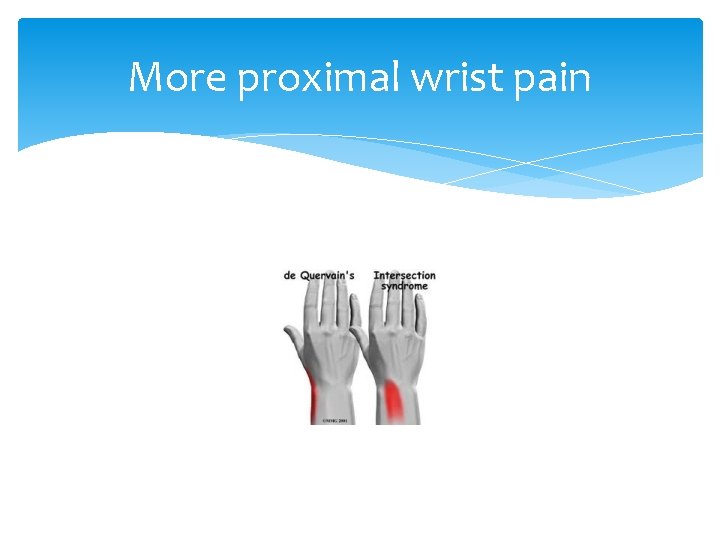
More proximal wrist pain
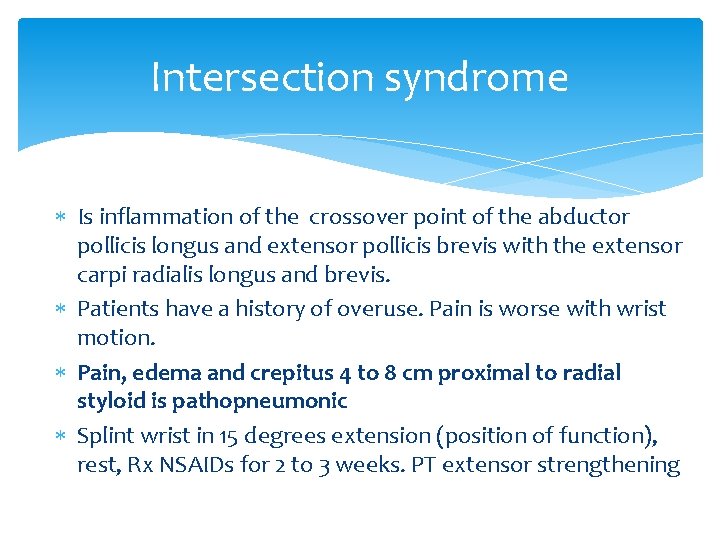
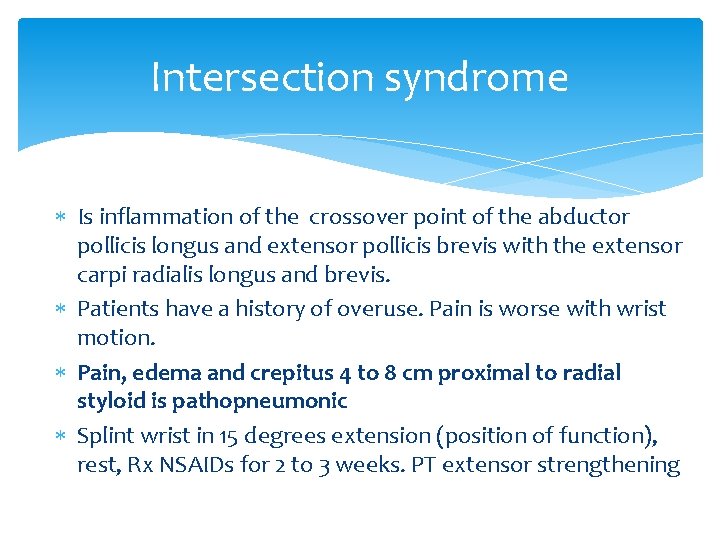
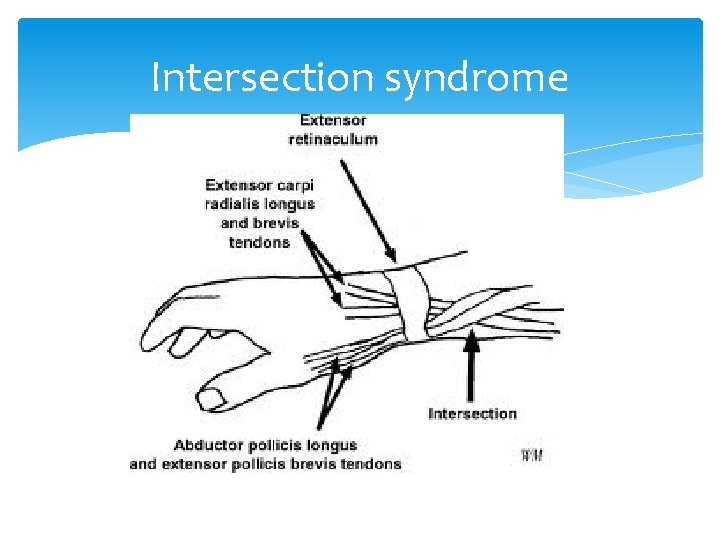
Intersection syndrome Is inflammation of the crossover point of the abductor pollicis longus and extensor pollicis brevis with the extensor carpi radialis longus and brevis. Patients have a history of overuse. Pain is worse with wrist motion. Pain, edema and crepitus 4 to 8 cm proximal to radial styloid is pathopneumonic Splint wrist in 15 degrees extension (position of function), rest, Rx NSAIDs for 2 to 3 weeks. PT extensor strengthening
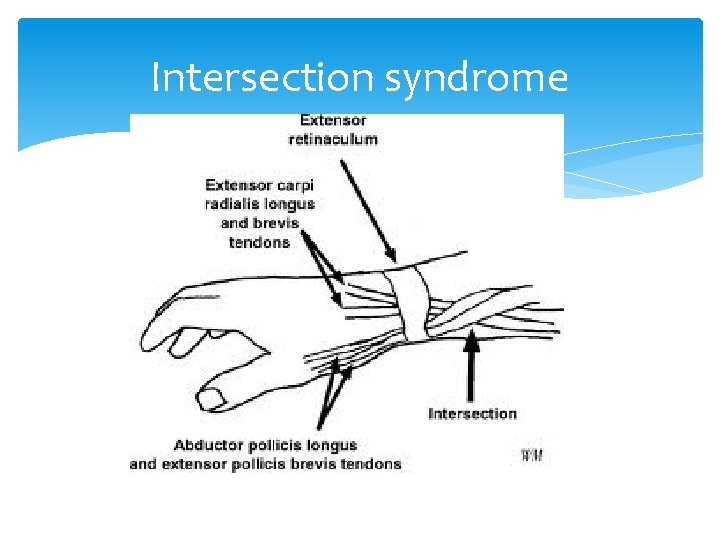
Intersection syndrome
Activity modification
Activity modification

Phalangeal Fractures/Sprains ½ of all hand injuries Nail bed injuries are common Open fractures or extensive soft tissue or boney injury, i. e. crush injury, require consultation with a hand specialist Nondisplaced fractures can be treated with immobilization splint
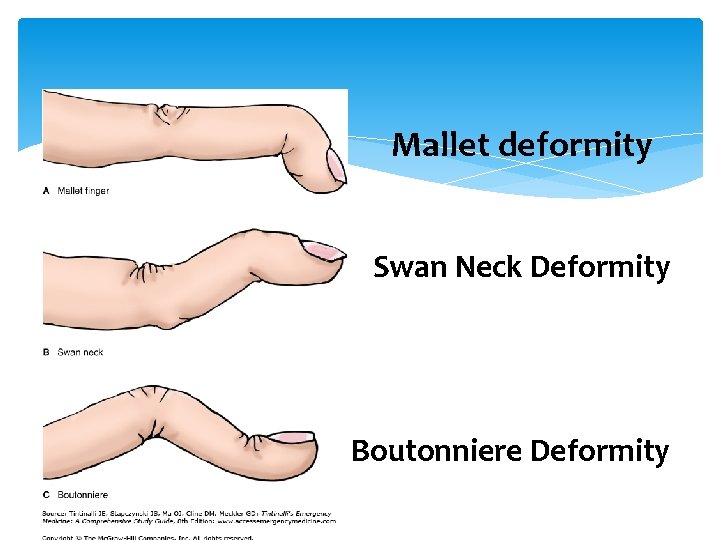
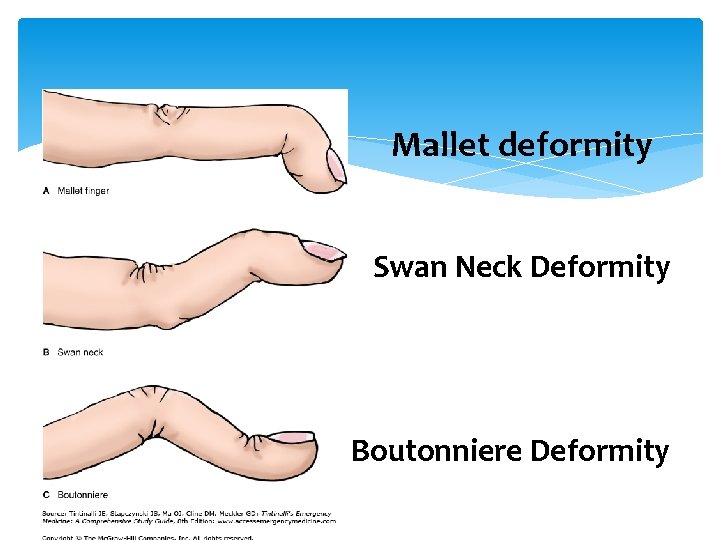
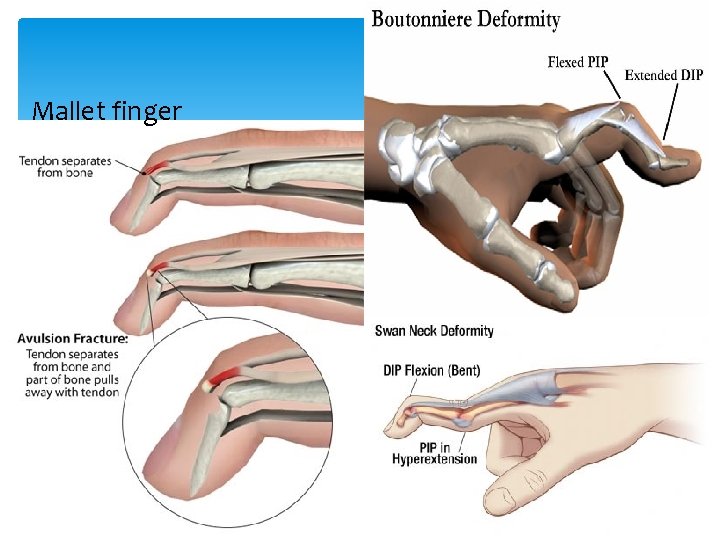
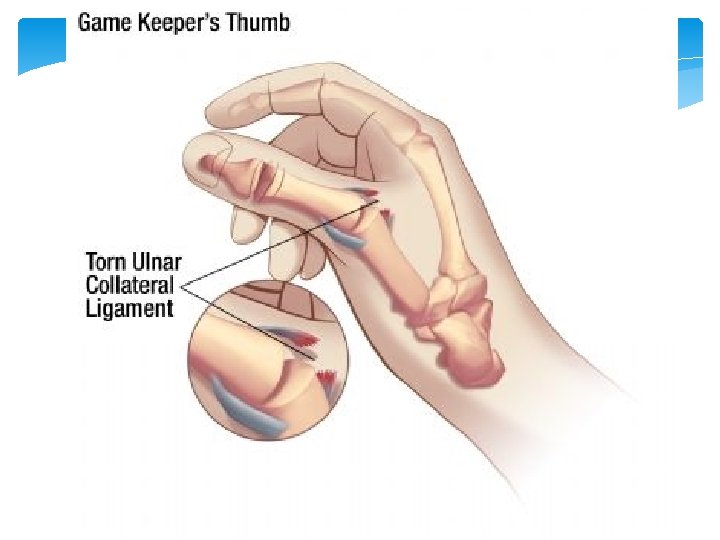
Mallet deformity Swan Neck Deformity Boutonniere Deformity
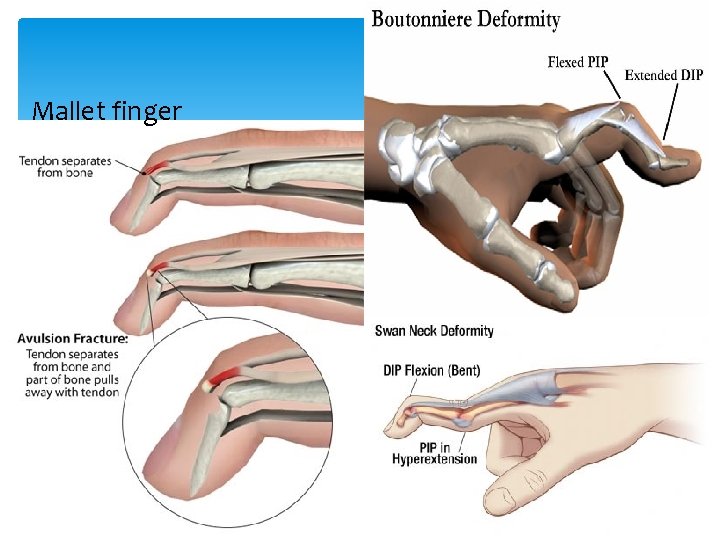
Mallet finger


Notice the padding!
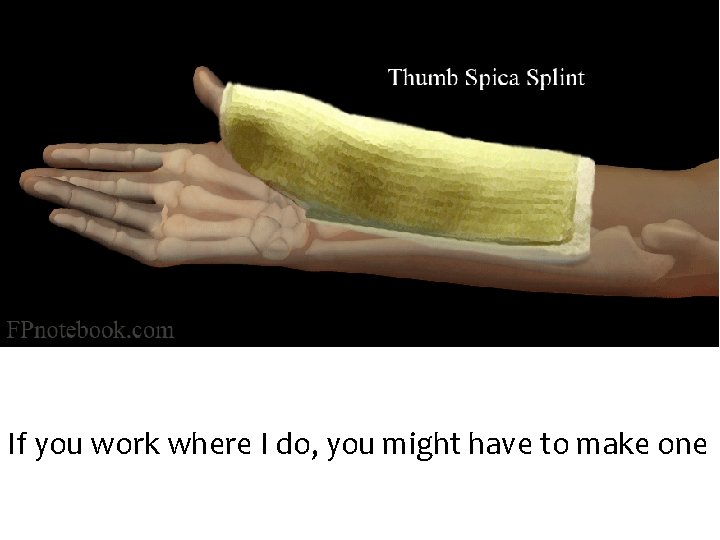
If you work where I do, you might have to make one

This one is available at most pharmacies
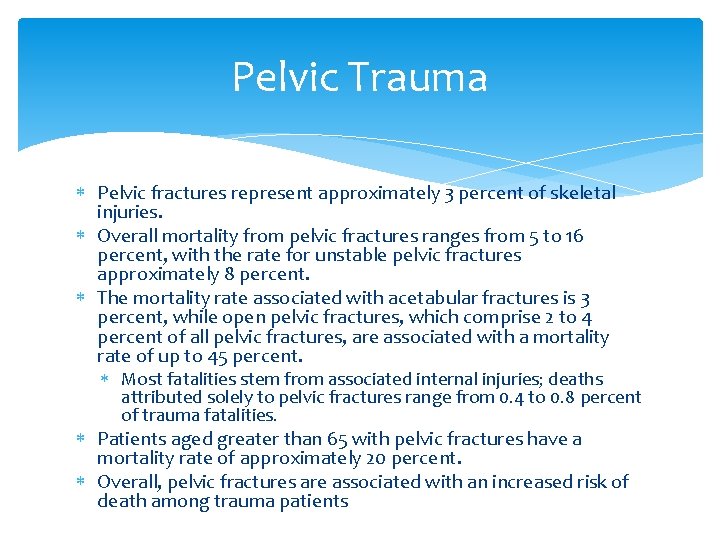
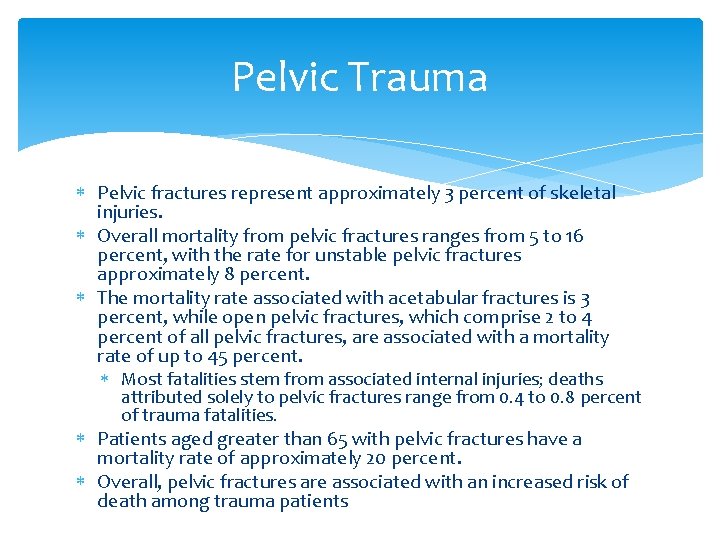
Pelvic Trauma Pelvic fractures represent approximately 3 percent of skeletal injuries. Overall mortality from pelvic fractures ranges from 5 to 16 percent, with the rate for unstable pelvic fractures approximately 8 percent. The mortality rate associated with acetabular fractures is 3 percent, while open pelvic fractures, which comprise 2 to 4 percent of all pelvic fractures, are associated with a mortality rate of up to 45 percent. Most fatalities stem from associated internal injuries; deaths attributed solely to pelvic fractures range from 0. 4 to 0. 8 percent of trauma fatalities. Patients aged greater than 65 with pelvic fractures have a mortality rate of approximately 20 percent. Overall, pelvic fractures are associated with an increased risk of death among trauma patients
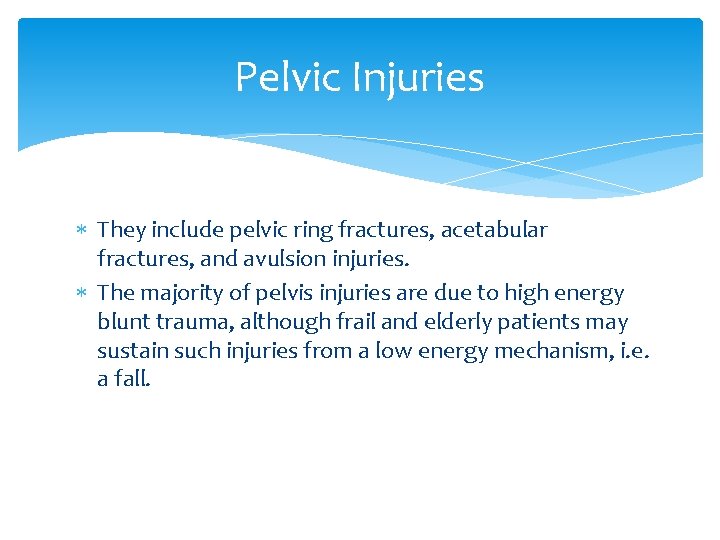
Pelvic Injuries They include pelvic ring fractures, acetabular fractures, and avulsion injuries. The majority of pelvis injuries are due to high energy blunt trauma, although frail and elderly patients may sustain such injuries from a low energy mechanism, i. e. a fall.
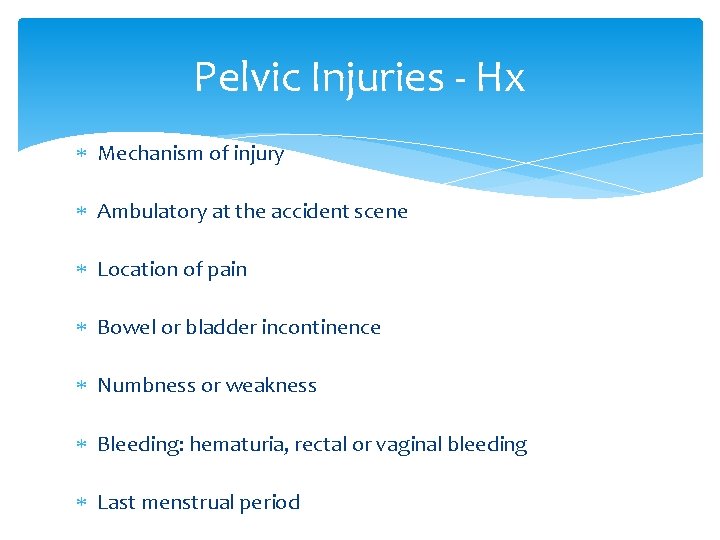
Pelvic Injuries - Hx Mechanism of injury Ambulatory at the accident scene Location of pain Bowel or bladder incontinence Numbness or weakness Bleeding: hematuria, rectal or vaginal bleeding Last menstrual period
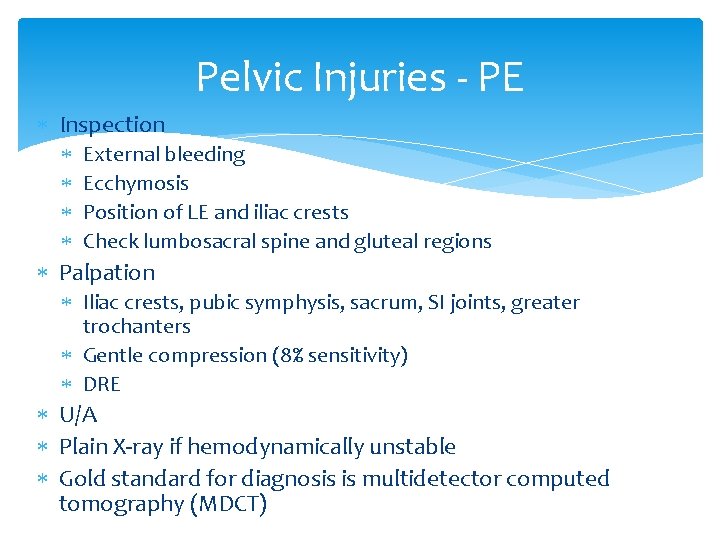
Pelvic Injuries - PE Inspection External bleeding Ecchymosis Position of LE and iliac crests Check lumbosacral spine and gluteal regions Palpation Iliac crests, pubic symphysis, sacrum, SI joints, greater trochanters Gentle compression (8% sensitivity) DRE U/A Plain X-ray if hemodynamically unstable Gold standard for diagnosis is multidetector computed tomography (MDCT)

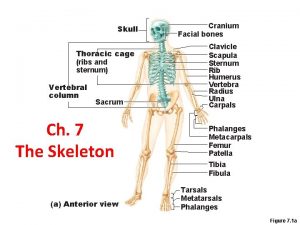
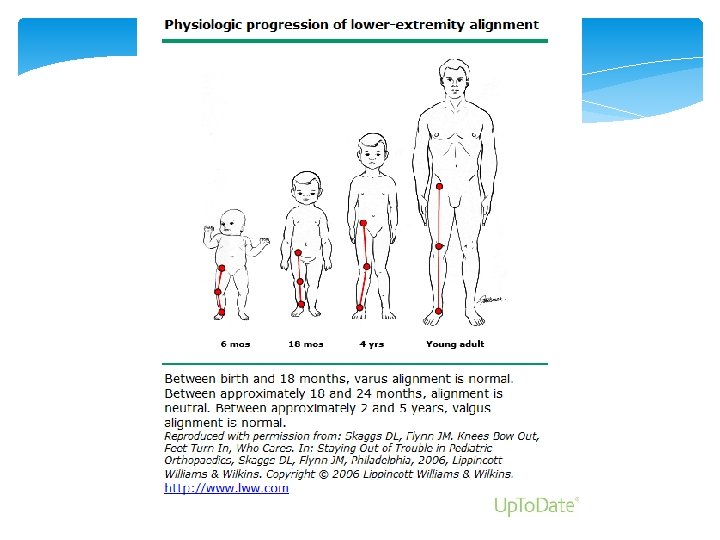
Disorders of the Lower Extremity Hips Knees Ankles Feet
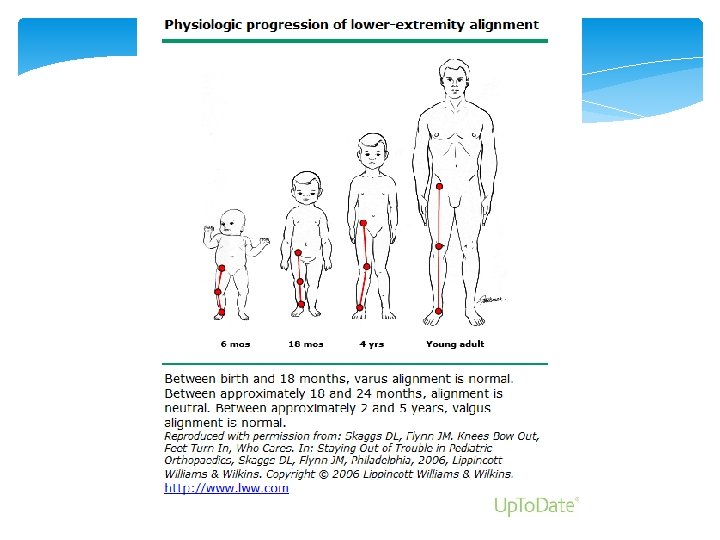
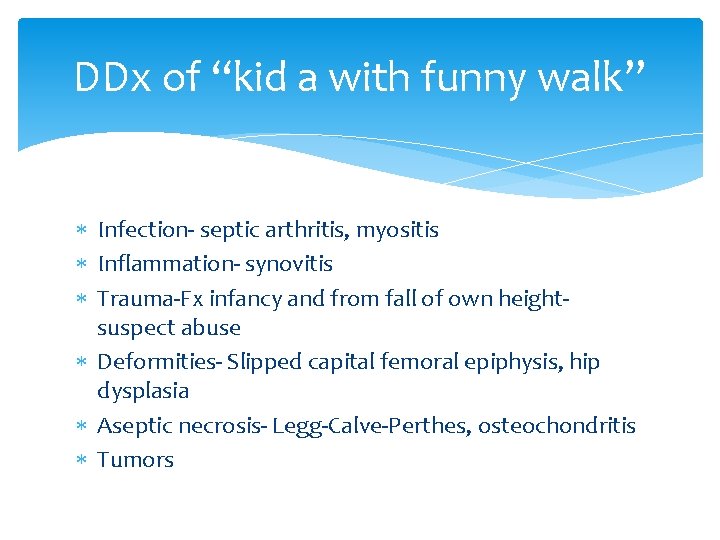
DDx of “kid a with funny walk” Infection- septic arthritis, myositis Inflammation- synovitis Trauma-Fx infancy and from fall of own height- suspect abuse Deformities- Slipped capital femoral epiphysis, hip dysplasia Aseptic necrosis- Legg-Calve-Perthes, osteochondritis Tumors
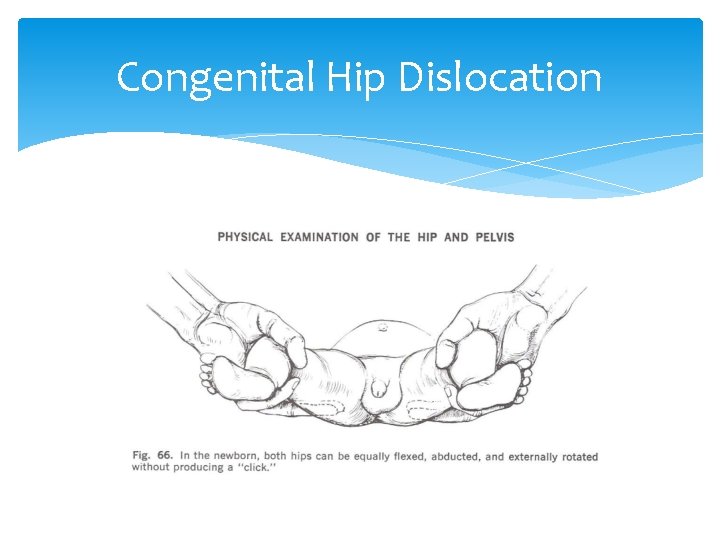
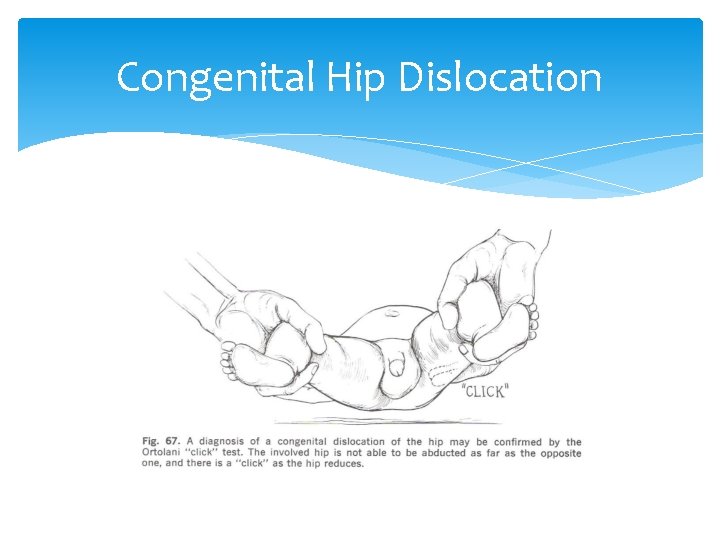
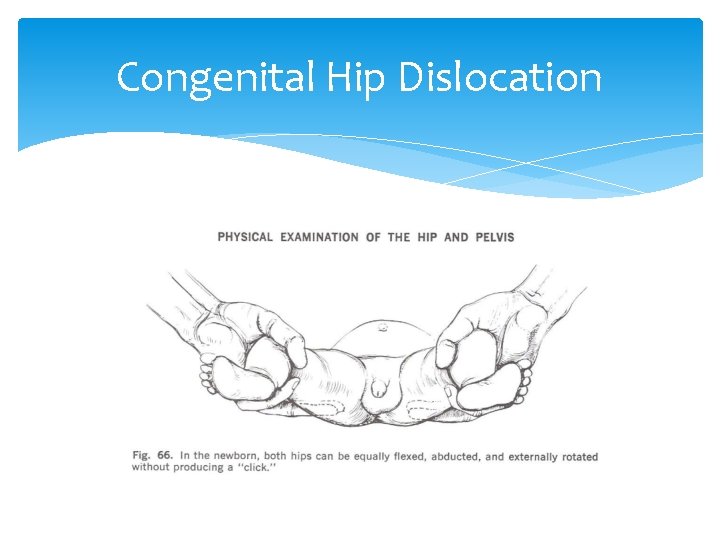
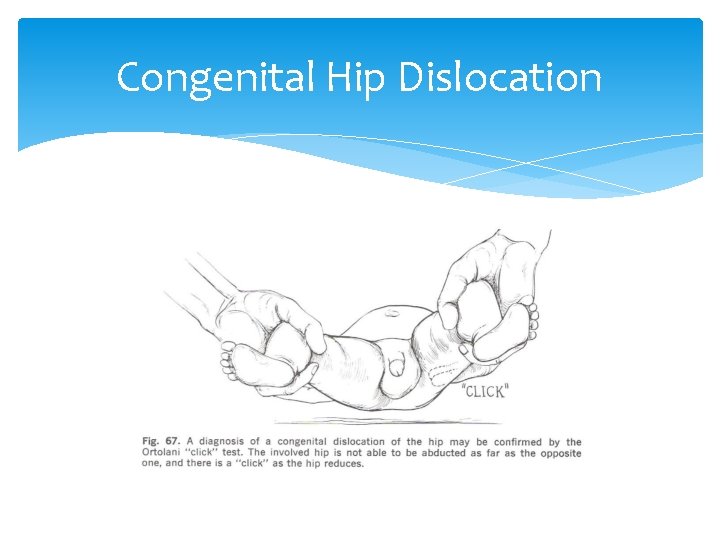
Congenital Hip Dislocation If a congenitally dislocated hip is flexed and abducted and externally rotated, the femoral head slips over the acetabular rim, reducing the dislocation and producing a palpable and/or audible click or jerk. This is called the Ortolani click.
Barlow maneuver Posterior pressure is applied to the greater trochanters to cause posterior subluxation/dislocation Determines if the hip is dislocatable
Ortolani Anterior pressure is applied to greater trochanters to reduce the posterior dislocation Determines if the hip is reducible
Congenital Hip Dislocation
Congenital Hip Dislocation
Congenital Hip Dislocation X-rays cannot diagnose this until 3 months of age Ortalani and Barlow maneuvers must be done on all infants and documented as + or If it is not diagnosed and corrected by conservative means before the child begins to walk it may result in permanent disability
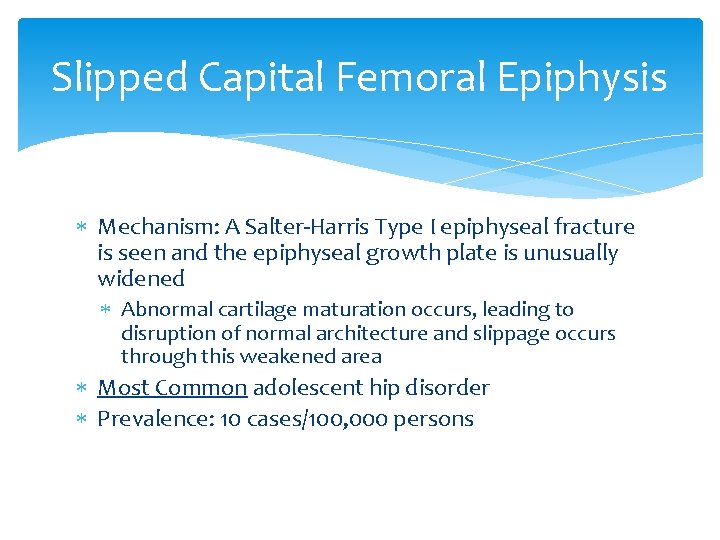
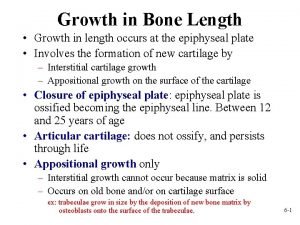
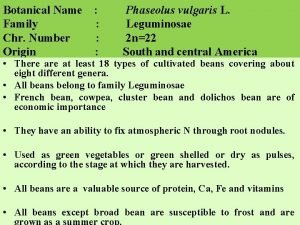
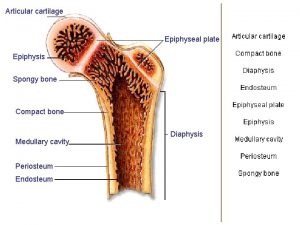
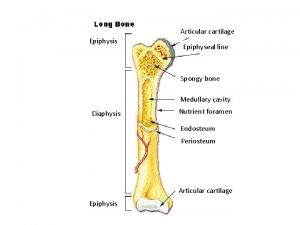
Slipped Capital Femoral Epiphysis Mechanism: A Salter-Harris Type I epiphyseal fracture is seen and the epiphyseal growth plate is unusually widened Abnormal cartilage maturation occurs, leading to disruption of normal architecture and slippage occurs through this weakened area Most Common adolescent hip disorder Prevalence: 10 cases/100, 000 persons
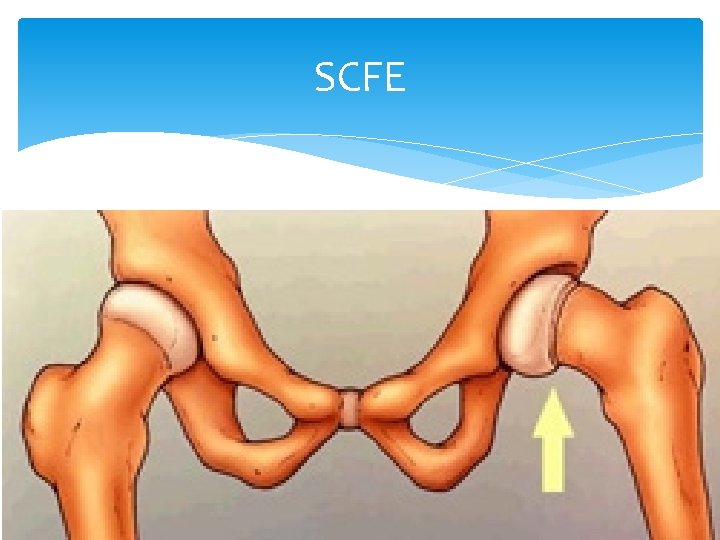
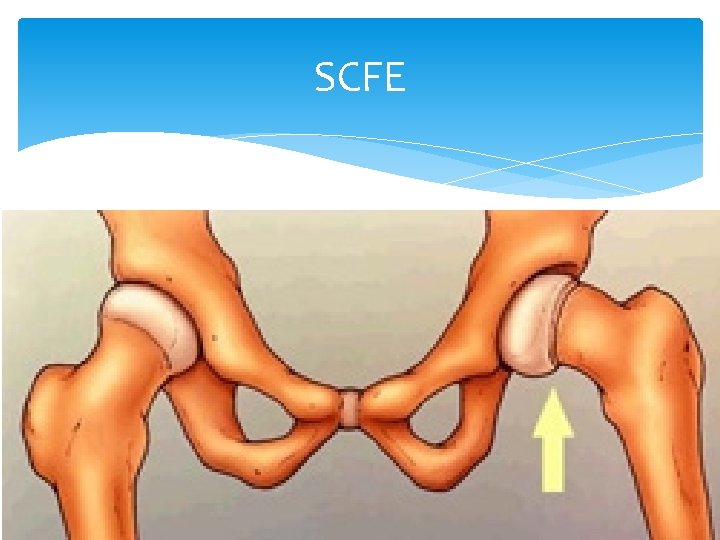
SCFE Adolescent, ball of femur slips backwards, weakness of growth plate
Slipped Capital Femoral Epiphysis The child with SCFE usually presents with pain and a limp. Since the pain is often located only in the thigh or knee, the diagnosis is often missed. It is important to remember that knee pain in the child can be secondary to hip disease.
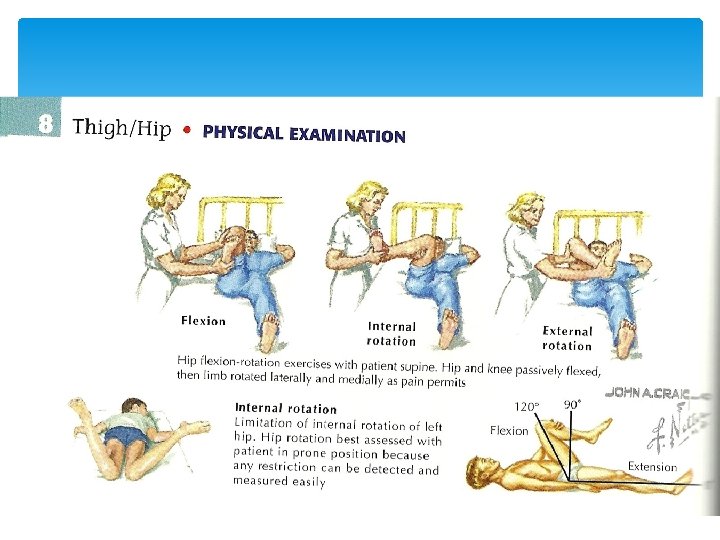
Slipped Capital Femoral Epiphysis On physical examination, there is frequently limitation of motion, especially internal rotation and abduction. As the examiner flexes the hip, it moves into external rotation and the patient often holds the leg externally rotated when standing.
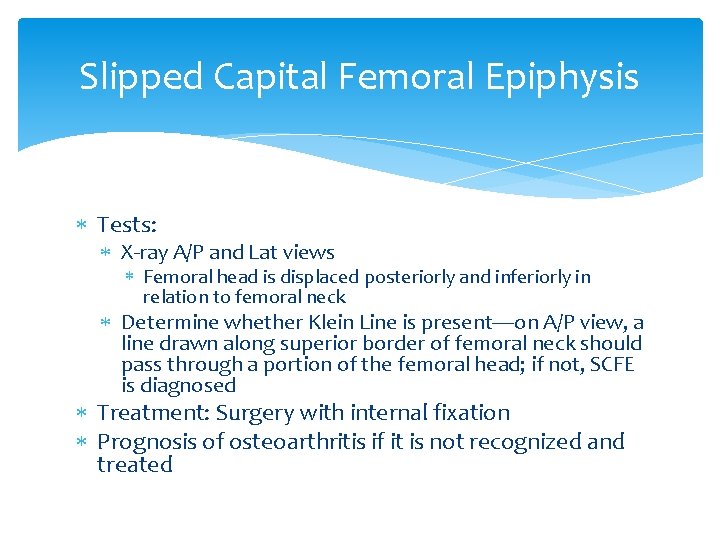
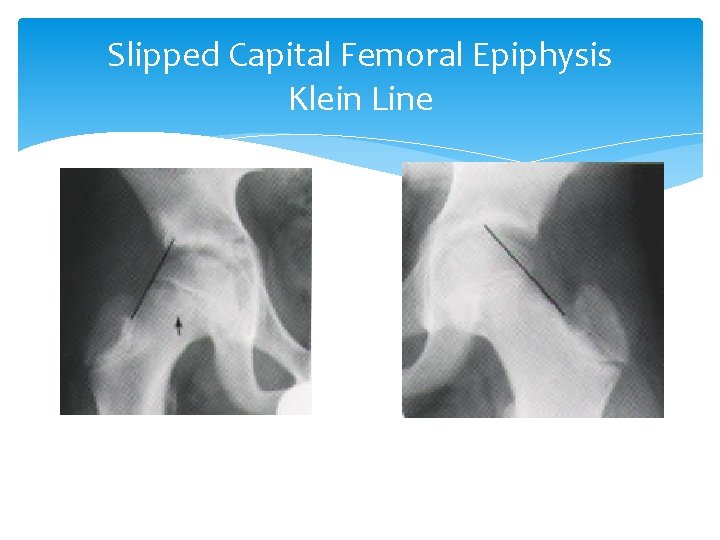
Slipped Capital Femoral Epiphysis Tests: X-ray A/P and Lat views Femoral head is displaced posteriorly and inferiorly in relation to femoral neck Determine whether Klein Line is present—on A/P view, a line drawn along superior border of femoral neck should pass through a portion of the femoral head; if not, SCFE is diagnosed Treatment: Surgery with internal fixation Prognosis of osteoarthritis if it is not recognized and treated
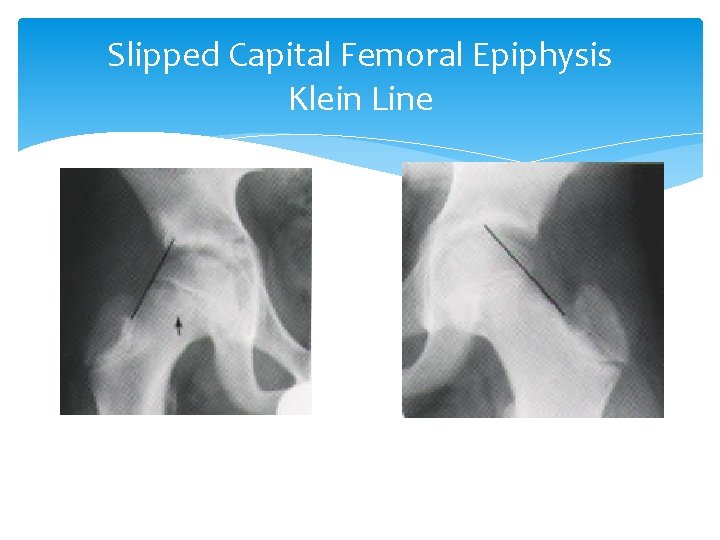
Slipped Capital Femoral Epiphysis Klein Line
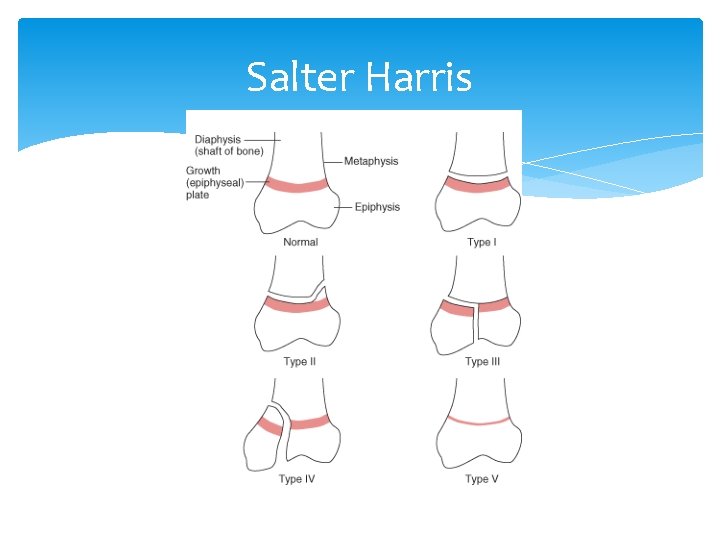
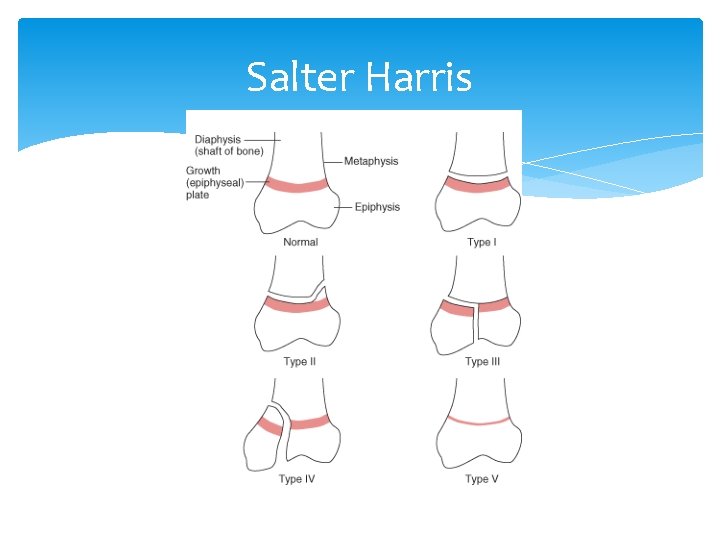
Salter Harris
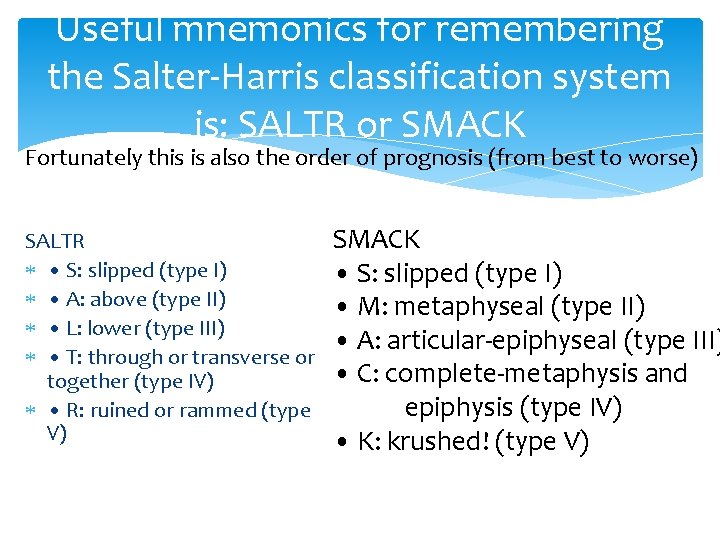
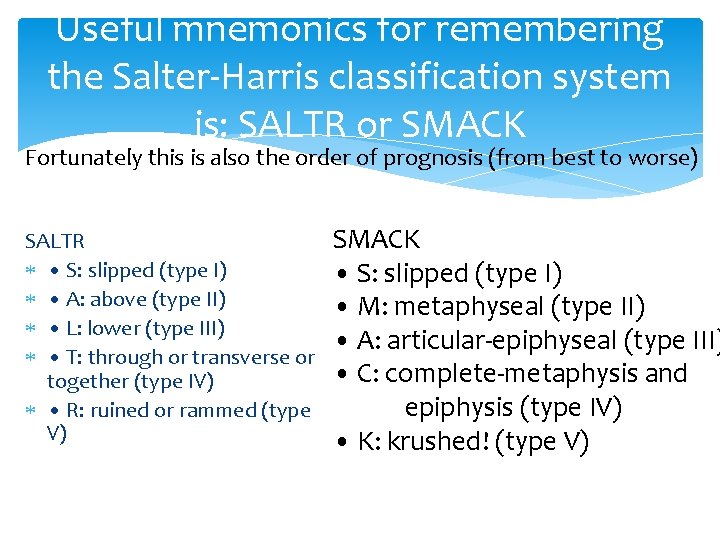
Useful mnemonics for remembering the Salter-Harris classification system is: SALTR or SMACK Fortunately this is also the order of prognosis (from best to worse) SALTR • S: slipped (type I) • A: above (type II) • L: lower (type III) • T: through or transverse or together (type IV) • R: ruined or rammed (type V) SMACK • S: slipped (type I) • M: metaphyseal (type II) • A: articular-epiphyseal (type III) • C: complete-metaphysis and epiphysis (type IV) • K: krushed! (type V)
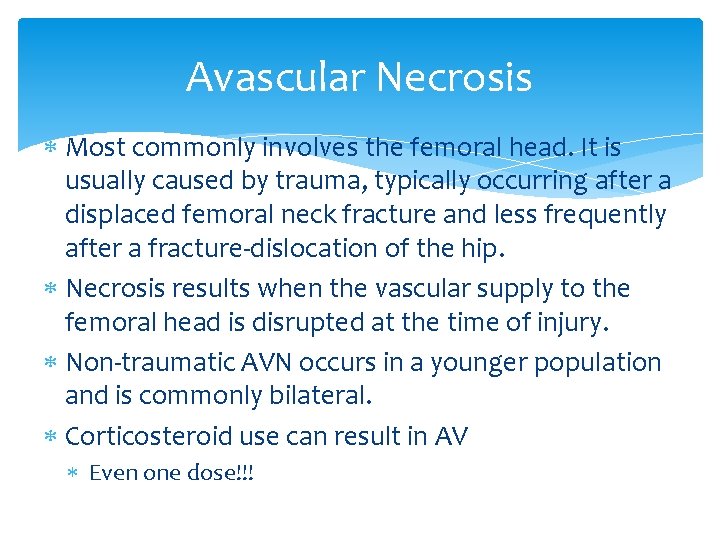
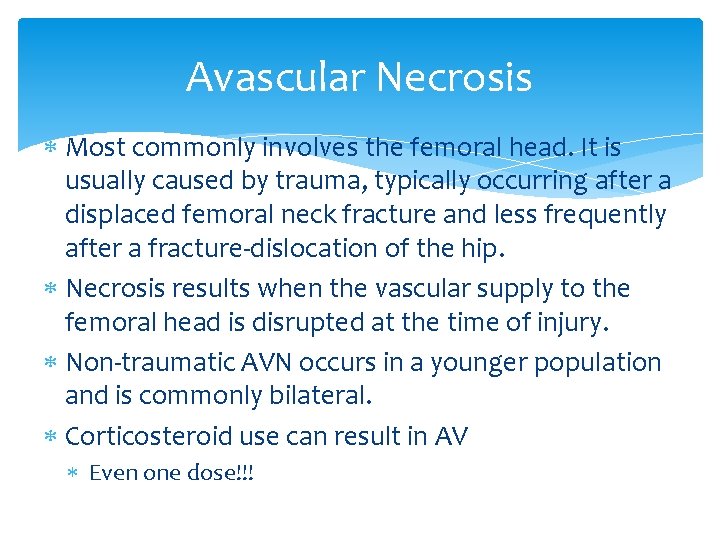
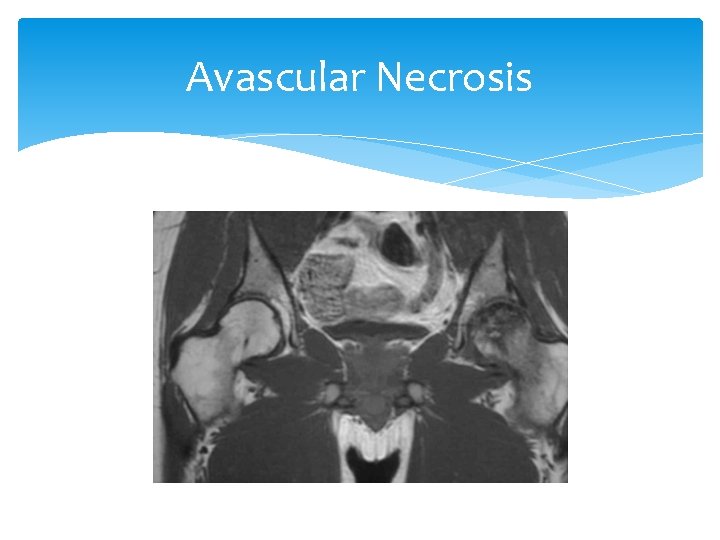
Avascular Necrosis Most commonly involves the femoral head. It is usually caused by trauma, typically occurring after a displaced femoral neck fracture and less frequently after a fracture-dislocation of the hip. Necrosis results when the vascular supply to the femoral head is disrupted at the time of injury. Non-traumatic AVN occurs in a younger population and is commonly bilateral. Corticosteroid use can result in AV Even one dose!!!
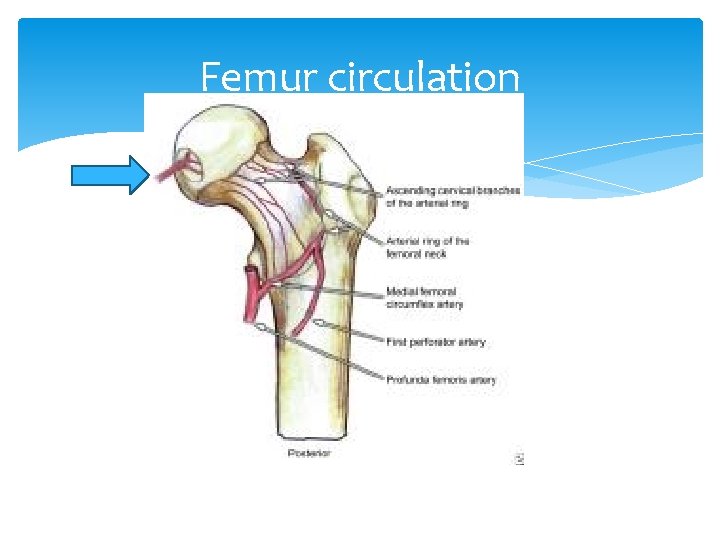
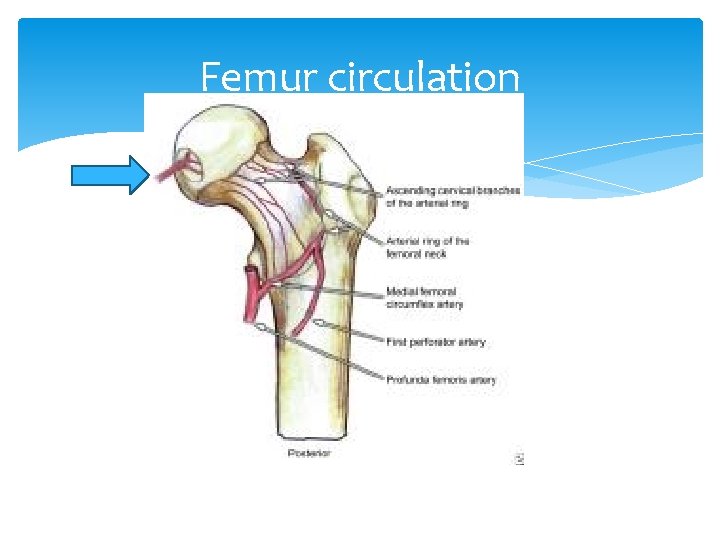
Femur circulation
Avascular Necrosis Signs and Symptoms Gradual onset pain that progresses and worsens to severe pain Decreased range of motion Arthritis May take months to a year for sx’s to progress
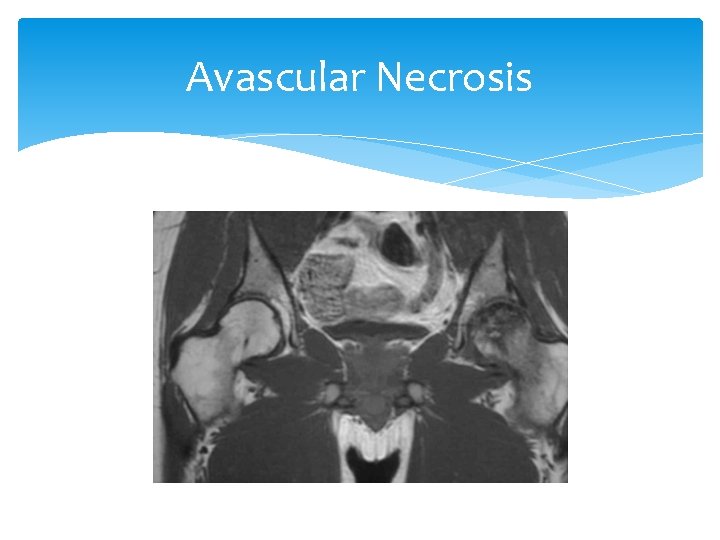
Avascular Necrosis Tests The Gold Standard is MRI, bone scan. The X-ray in early stage is normal, late stage may show changes.
Avascular Necrosis
Avascular Necrosis Treatment: Two approaches Conservative Medications NSAIDS Meds to reduce fatty substances (lipids) that increase with steroid use (statins) Meds to decrease coagulation in clotting disorders Vasodilators bisphonates Decrease weight bearing and exercises Nonoperative management has generally been ineffective at halting the progression of disease Surgical Bone graft Total hip arthroplasty (THA)
Hip fracture 310, 000 individuals were hospitalized with hip fractures in the United States alone in 2003 30 percent of all hospitalized patients Hip fractures substantially increase the risk of death and major morbidity in the elderly Femoral neck and intertrochanteric fractures occur with approximately the same frequency in patients between the ages of 65 and 99 years Isolated trochanteric fractures occur more often in young, active adults between the ages of 14 and 25
Hip Fractures Major risk factors for hip fractures among elderly patients include osteoporosis and falls Mechanism of injury: A fall directly onto the lateral hip A twisting mechanism in which the patient's foot is planted and the body rotates A sudden spontaneous completion of a fatigue (or insufficiency) fracture, which then causes a fall Did they fall and break their hip or did they break their hip and fall?
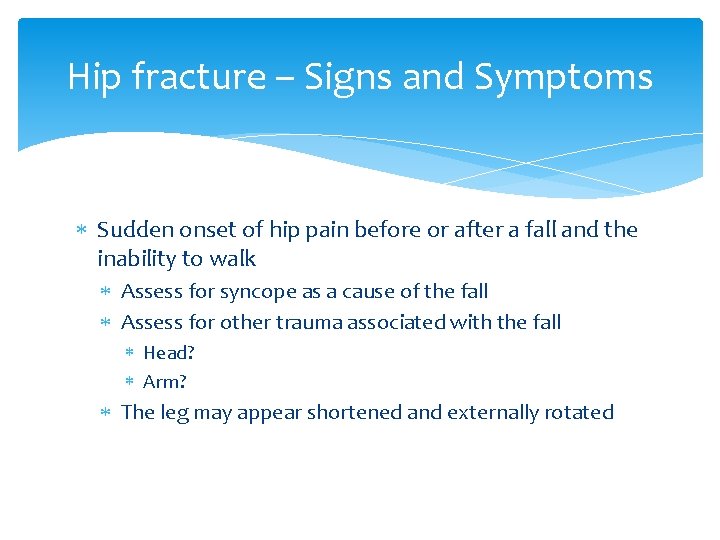
Hip fracture – Signs and Symptoms Sudden onset of hip pain before or after a fall and the inability to walk Assess for syncope as a cause of the fall Assess for other trauma associated with the fall Head? Arm? The leg may appear shortened and externally rotated

Hip Fracture - Treatment Depending on overall functional status Nonoperative management Nonambulatory Demented Unstable with major, uncorrectable comorbid disease Patients at the end stage of a terminal disease Surgical Open reduction with internal fixation (ORIF)

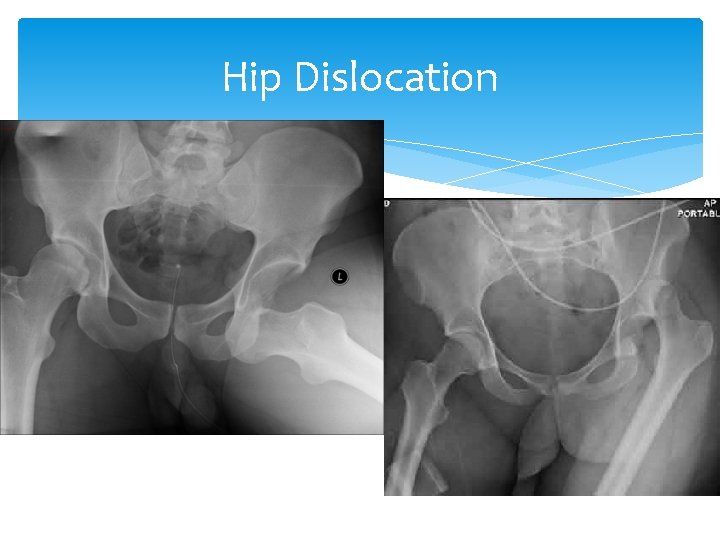
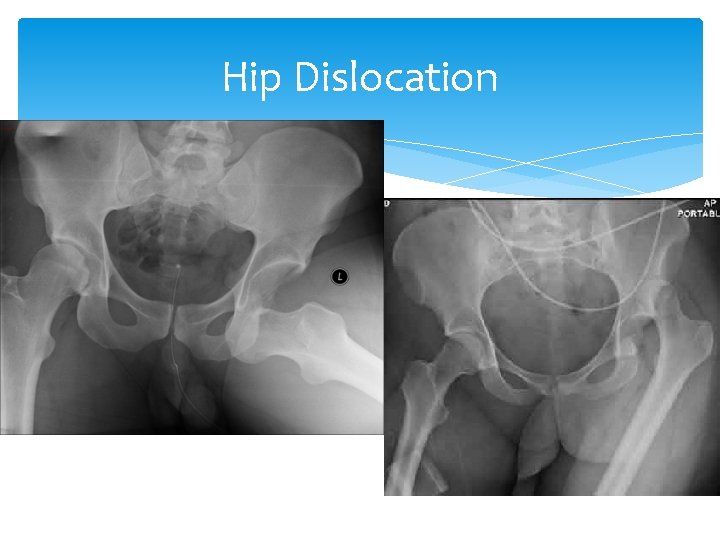
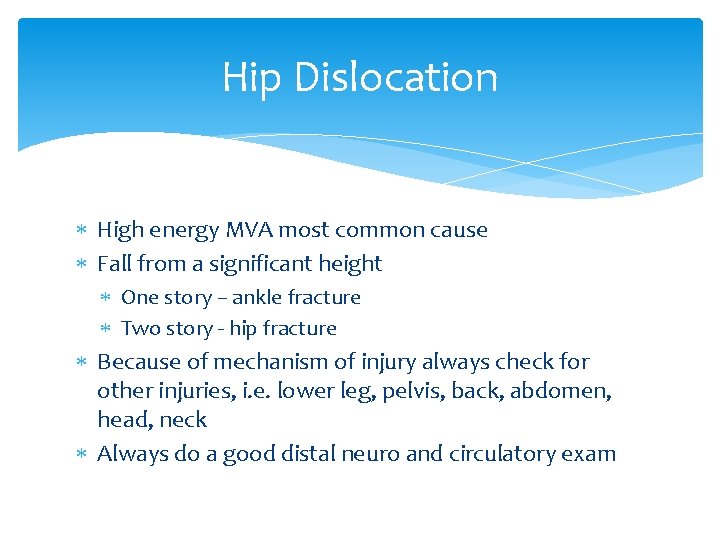
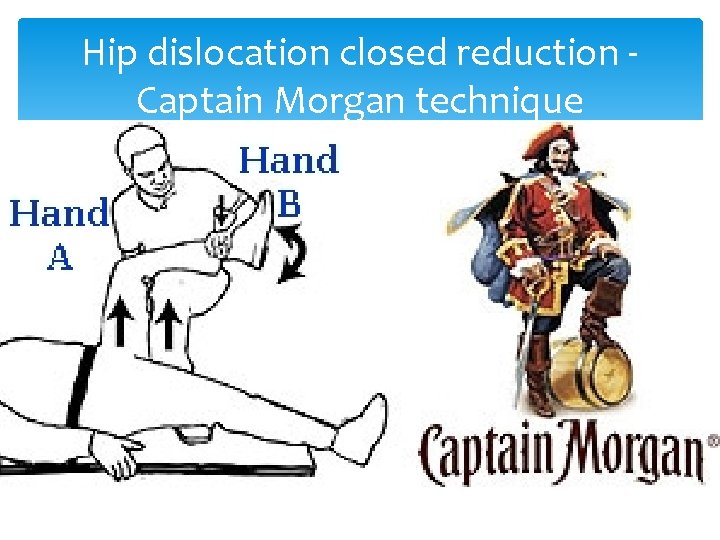
Hip Dislocation
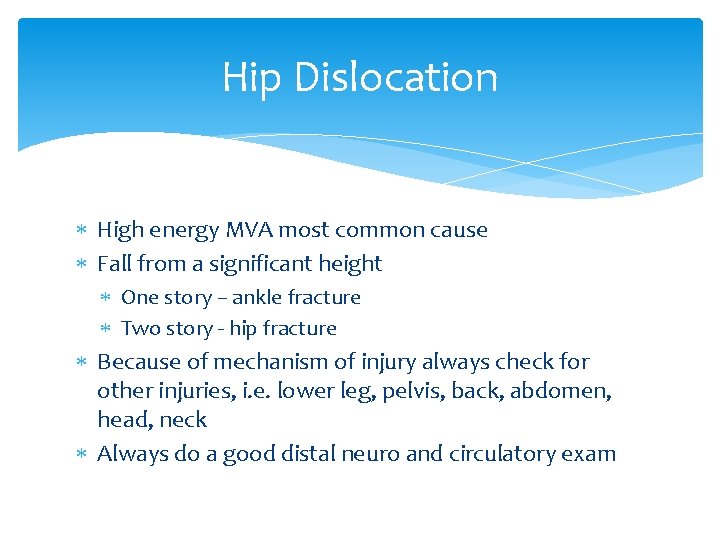
Hip Dislocation High energy MVA most common cause Fall from a significant height One story – ankle fracture Two story - hip fracture Because of mechanism of injury always check for other injuries, i. e. lower leg, pelvis, back, abdomen, head, neck Always do a good distal neuro and circulatory exam
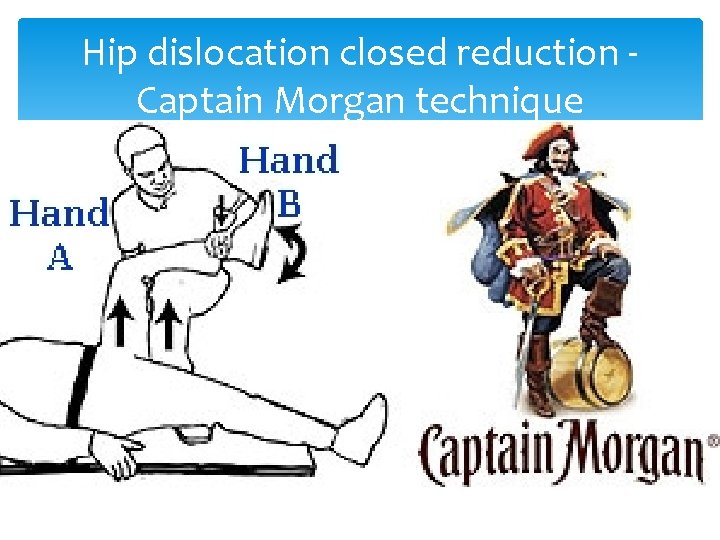
Hip dislocation closed reduction - Captain Morgan technique
DDx of “hip Pain” Lateral hip pain aggravated by pressure Trochanteric bursitis Rest, ice, NSAIDs Glucocorticoid + local anesthetic injection Lateral hip pain associated with paresthesias and hypesthesias Meralgia paresthetica Anterior hip or groin pain Primary involvement of the hip joint OA, osteonecrosis, occult fracture, acute synovitis, septic arthritis (uncommon)
DDx of “hip Pain” Posterior hip pain Least common SI joint dis Lumbar radiculopathy HZV Unusual hip joint Lower anterior thigh pain Clinically challenging Primary hip joint dis Lesions of the upper femur Stress fracture of femoral neck Upper lumbar radiculopathy
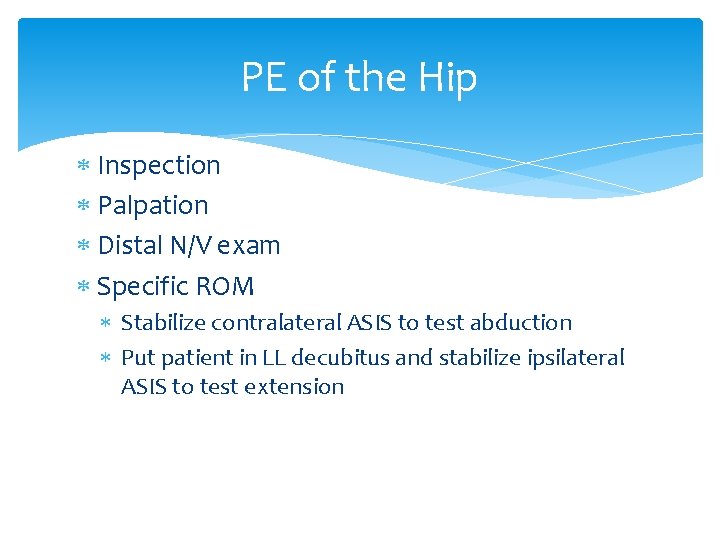
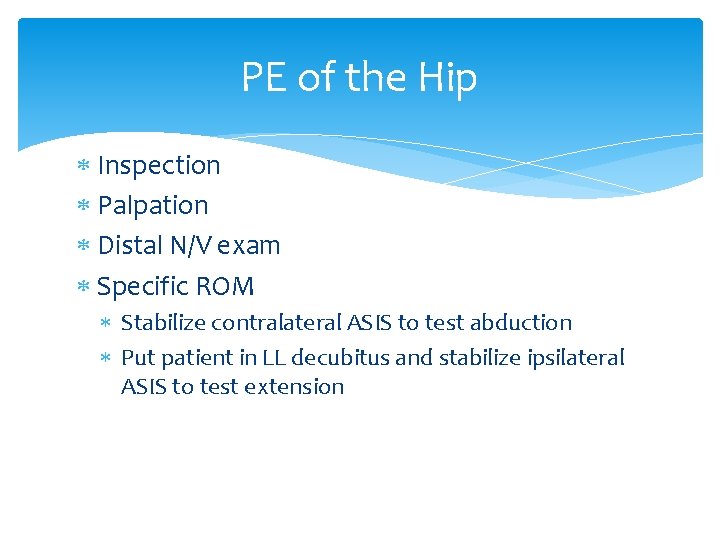
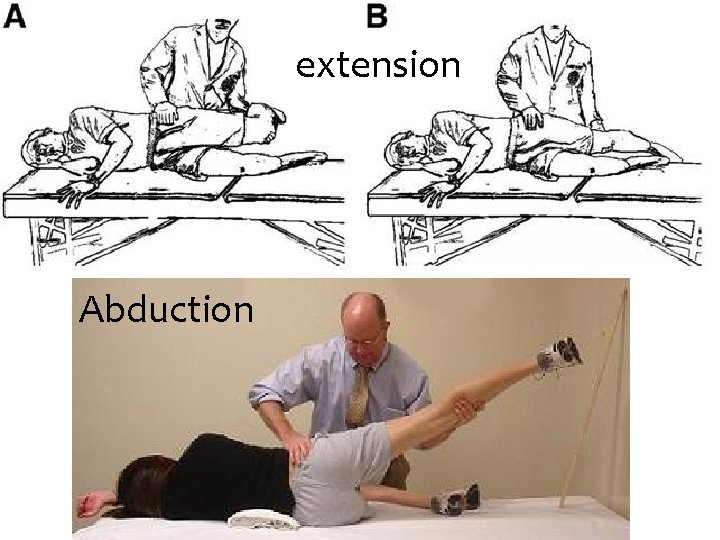
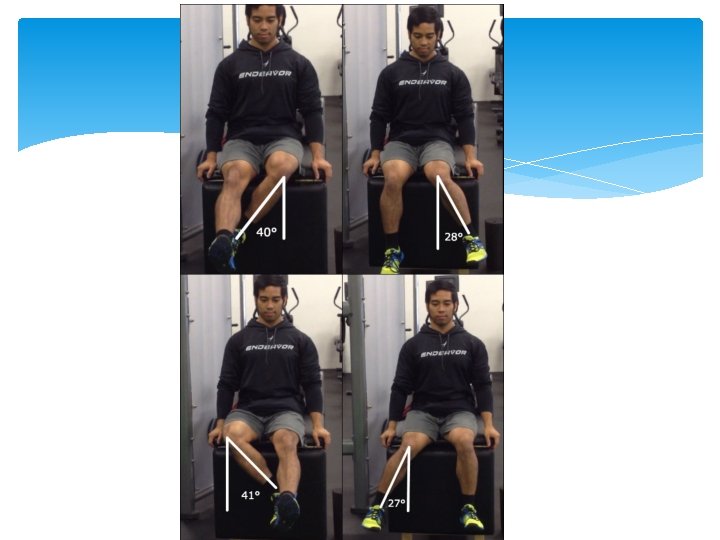
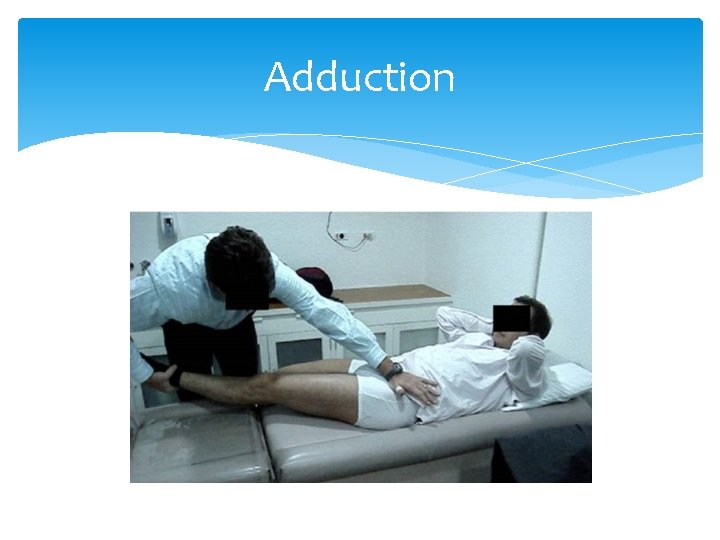
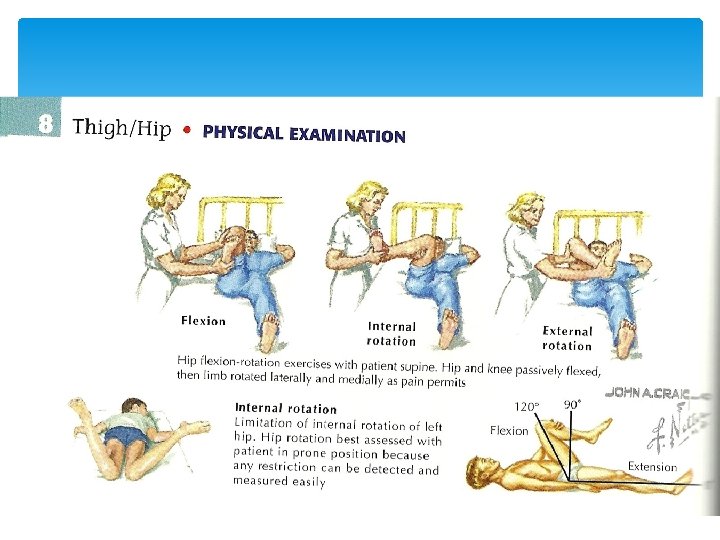
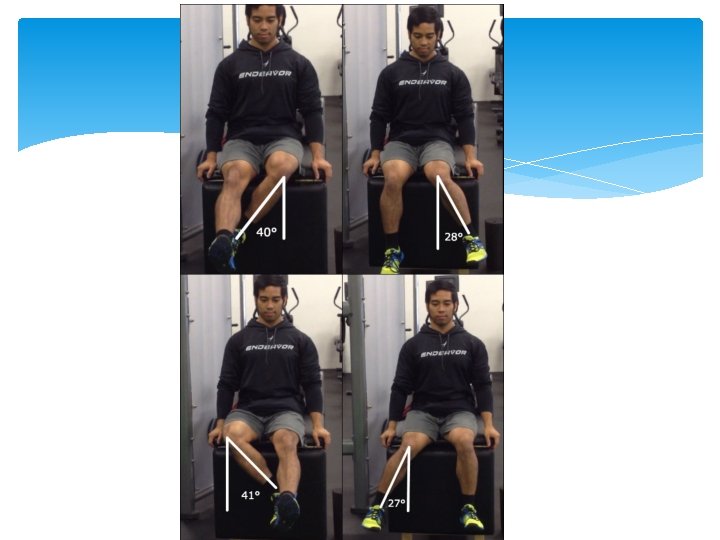
PE of the Hip Inspection Palpation Distal N/V exam Specific ROM Stabilize contralateral ASIS to test abduction Put patient in LL decubitus and stabilize ipsilateral ASIS to test extension
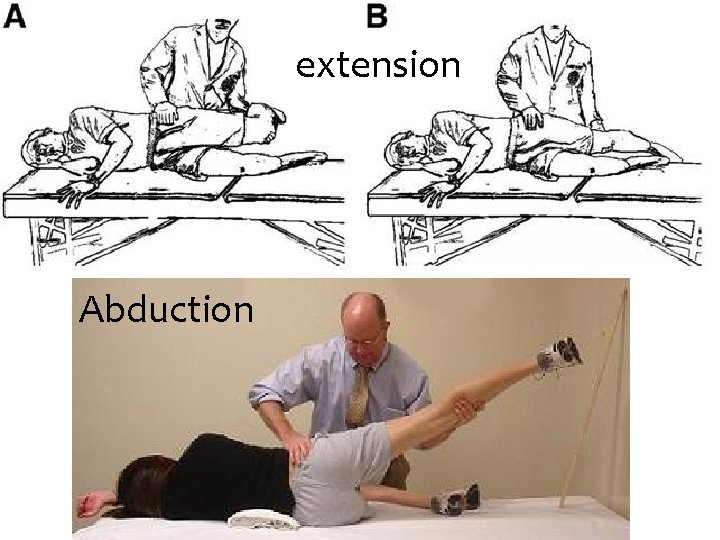
extension Abduction
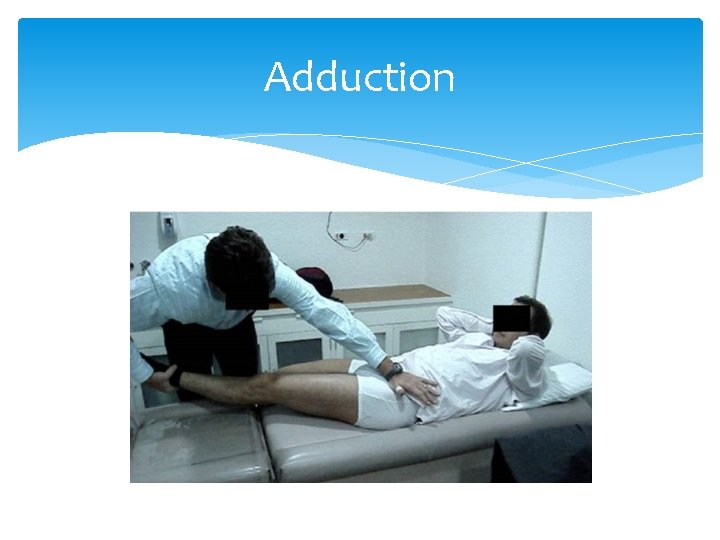
Adduction
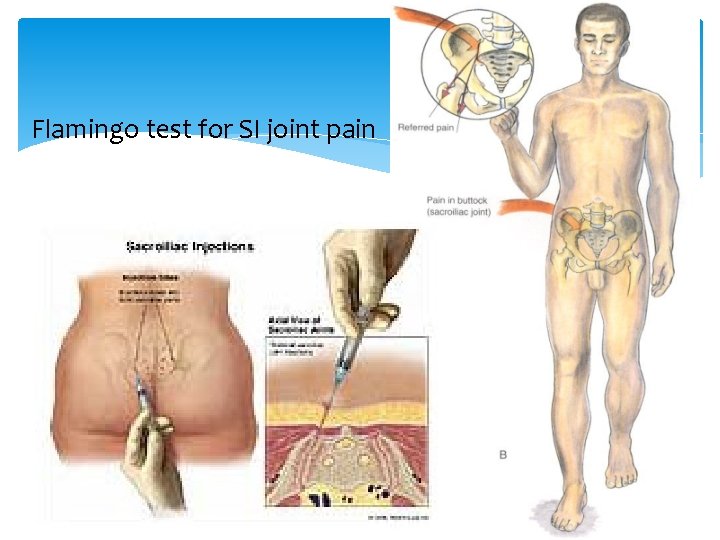
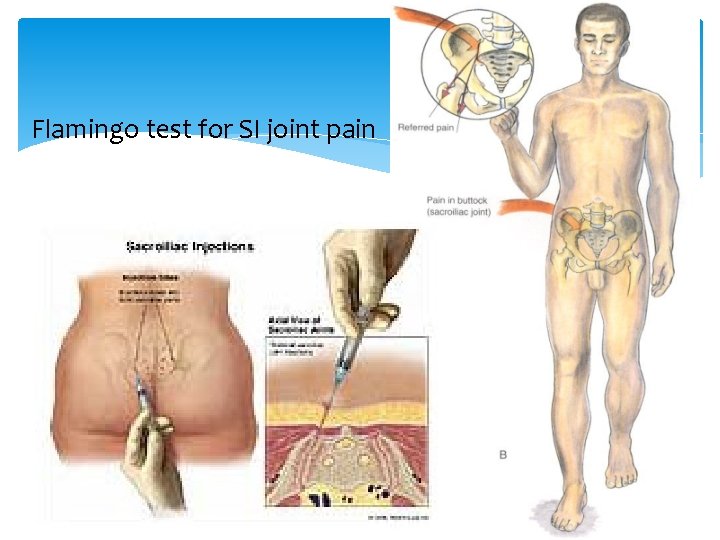
Flamingo test for SI joint pain

Knee Effusions Internal derangements: Meniscal tears Cruciate ligament tears Dislocations Infection Inflammation
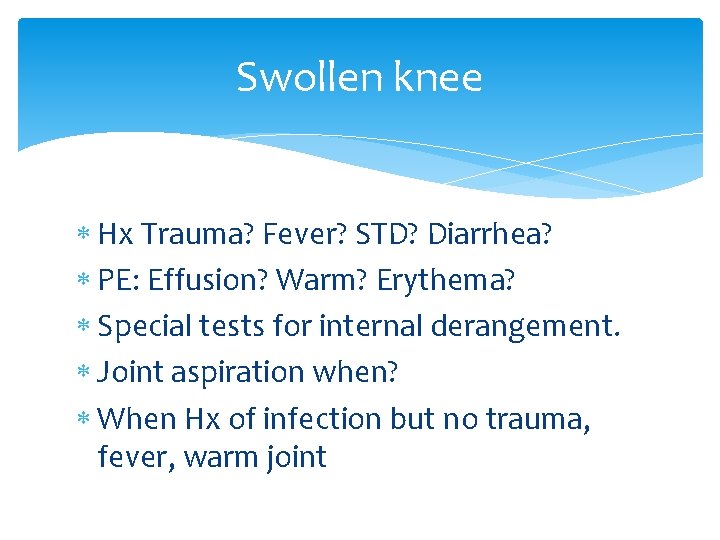
Swollen knee Hx Trauma? Fever? STD? Diarrhea? PE: Effusion? Warm? Erythema? Special tests for internal derangement. Joint aspiration when? When Hx of infection but no trauma, fever, warm joint
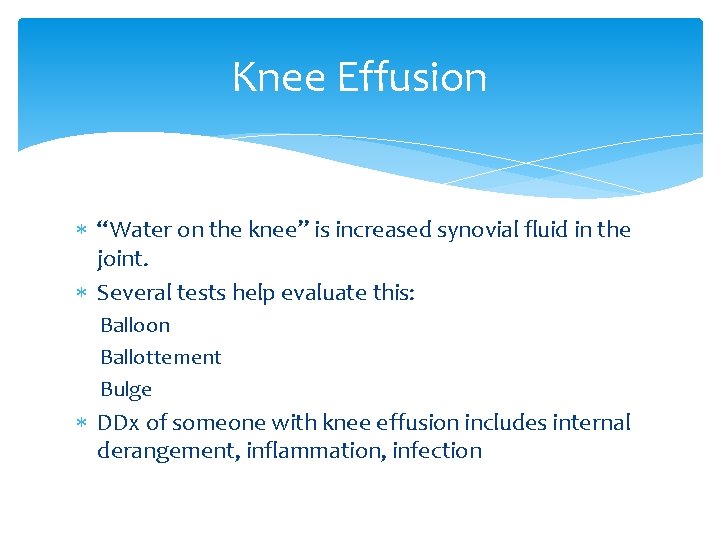
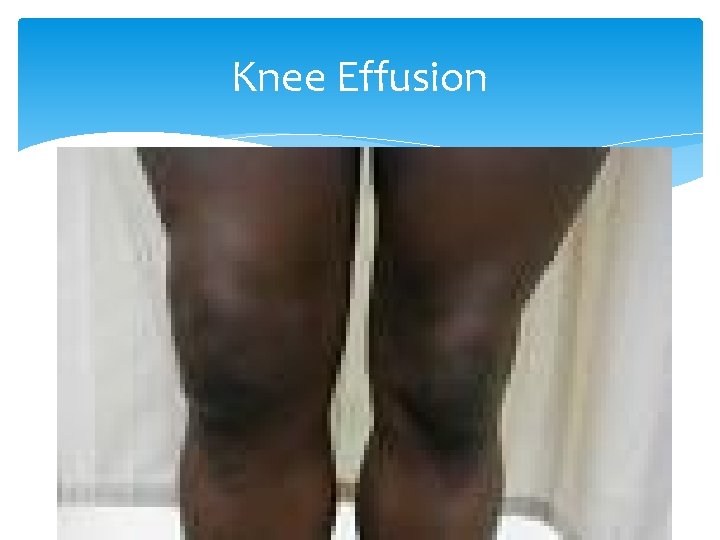
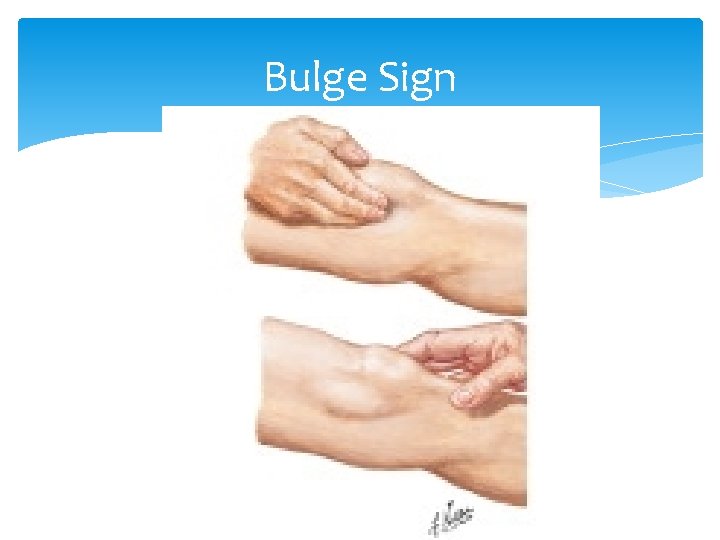
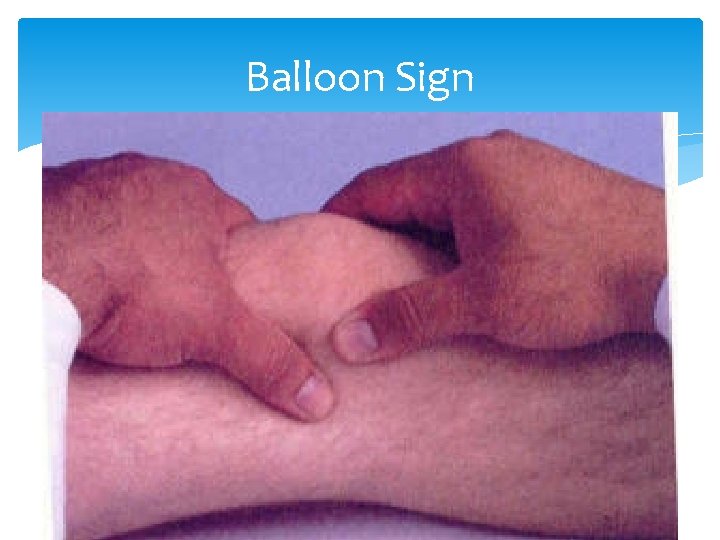
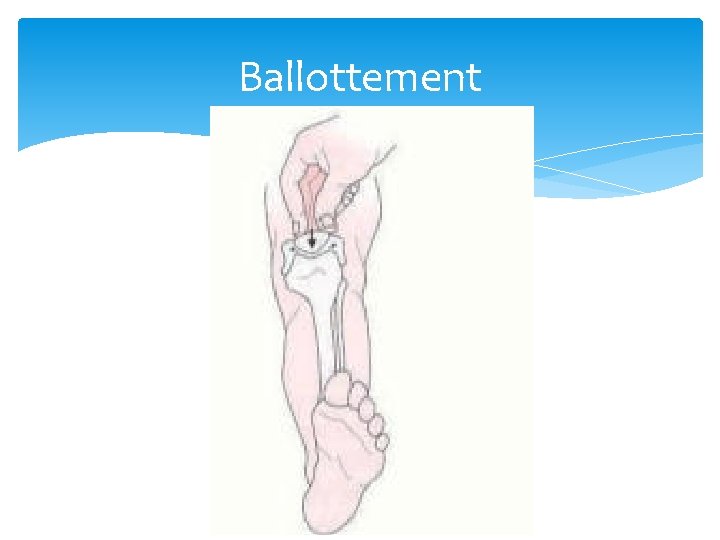
Knee Effusion “Water on the knee” is increased synovial fluid in the joint. Several tests help evaluate this: Balloon Ballottement Bulge DDx of someone with knee effusion includes internal derangement, inflammation, infection
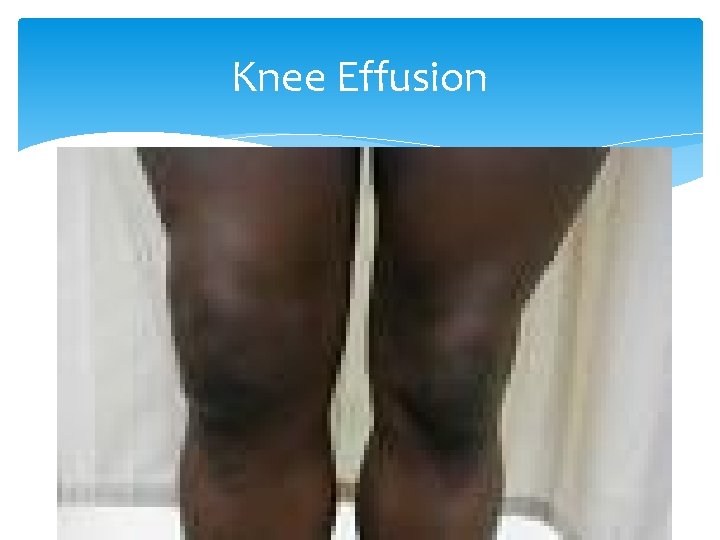
Knee Effusion
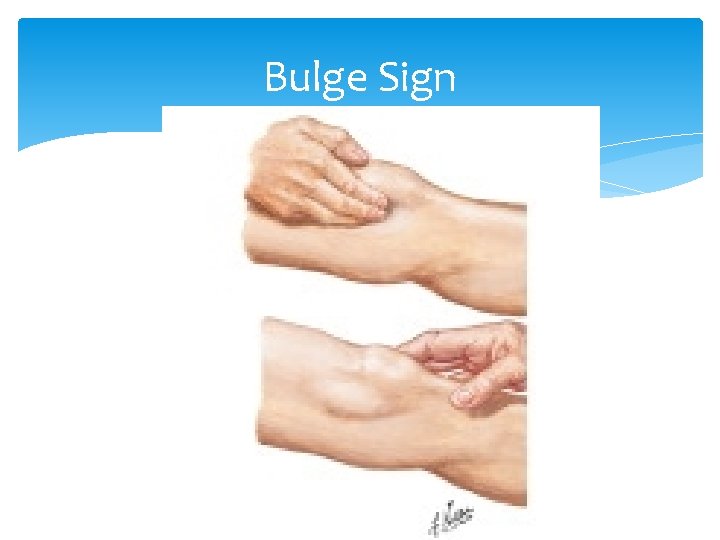
Bulge Sign
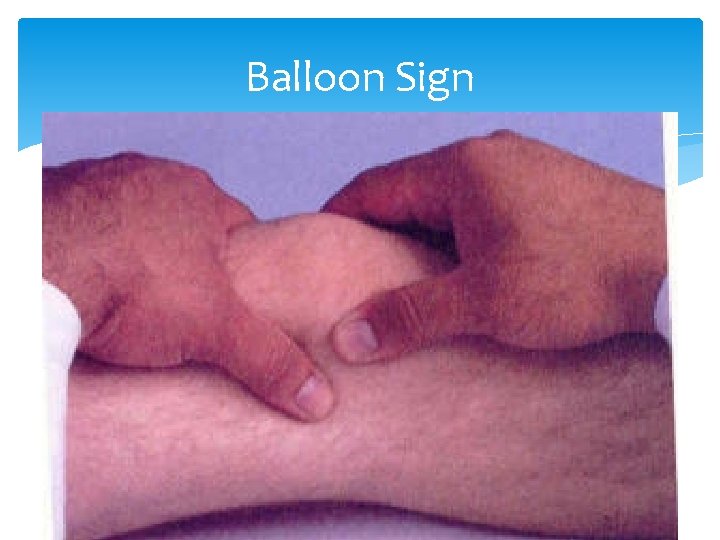
Balloon Sign
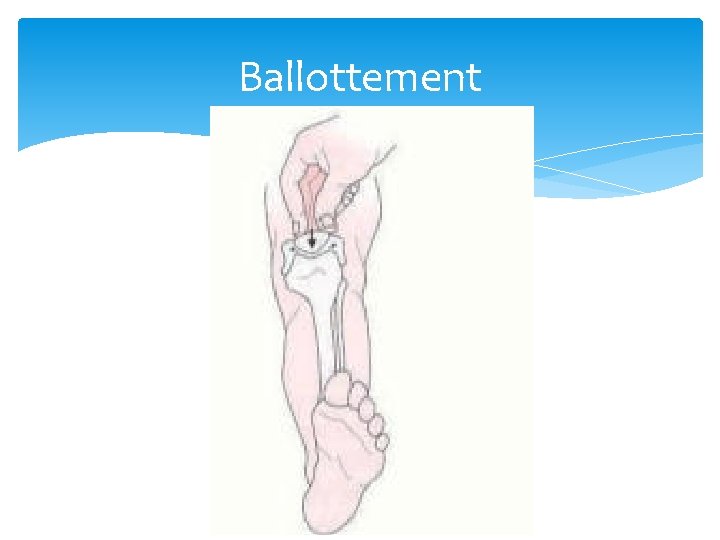
Ballottement
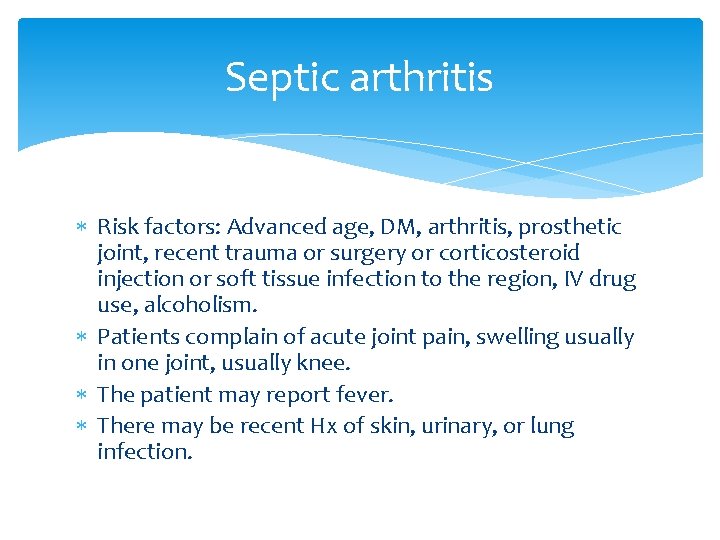
Septic arthritis Risk factors: Advanced age, DM, arthritis, prosthetic joint, recent trauma or surgery or corticosteroid injection or soft tissue infection to the region, IV drug use, alcoholism. Patients complain of acute joint pain, swelling usually in one joint, usually knee. The patient may report fever. There may be recent Hx of skin, urinary, or lung infection.
Septic arthritis PE: Patient may be febrile. Joint is warm, swollen, with restricted ROM. Diagnosis is by synovial fluid aspiration and analysis with gram stain, leukocyte count, and culture. Culture is considered definitive. Synovial fluid will have leukocytosis 50 -150, 000 cells/mm 3 Blood culture may be positive, ESR and CRP are usually elevated. Radiographs should also be taken to assess for osteomyelitis.
Septic arthritis If gram stain is positive, vancomycin should be initiated IV. If gram stain is negative, a third generation cephalosporin should be used. IV antibiotics are used for 14 days followed by 14 days of oral medication. Some orthos drain the joint. Osteoarthritis sometimes follows DDx includes reactive arthritis, rheumatoid arthritis, Lyme disease, gout and psuedogout
(Arthritis) Osteoarthritis is very common Anyone over 35 YOA Progressive loss of cartilage (wear and tear) Loose weight NSAIDS Activity Knee replacement

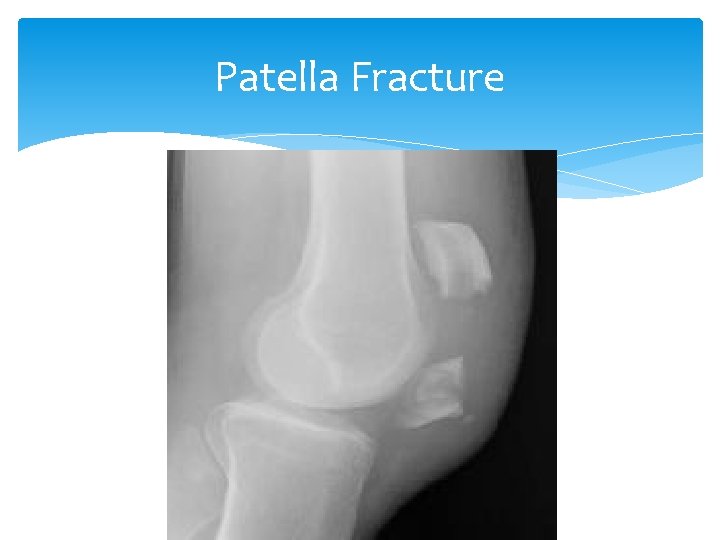
Patella Fracture Signs and Symptoms are swelling, tenderness, hemarthrosis Proximal displacement of patella Difficulty with weight bearing Inability to actively extend knee Sometimes a palpable gap
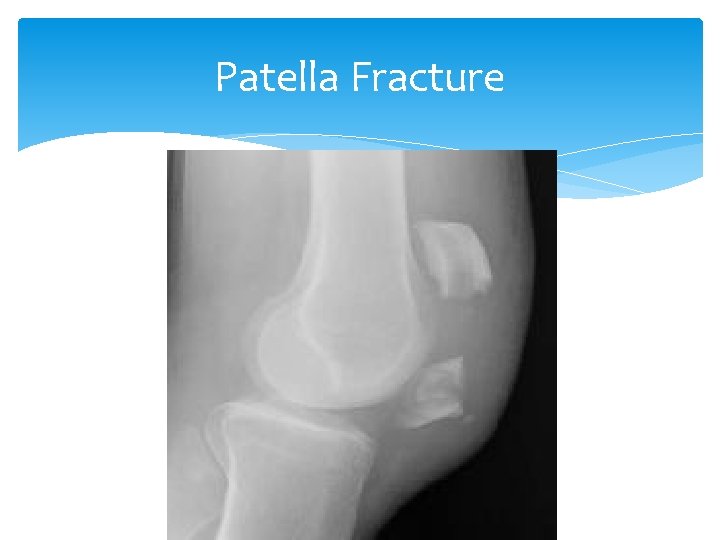
Patella Fracture
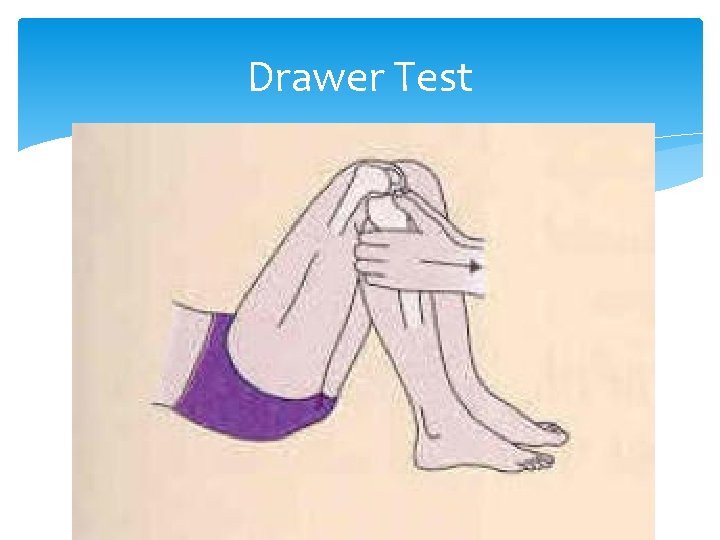
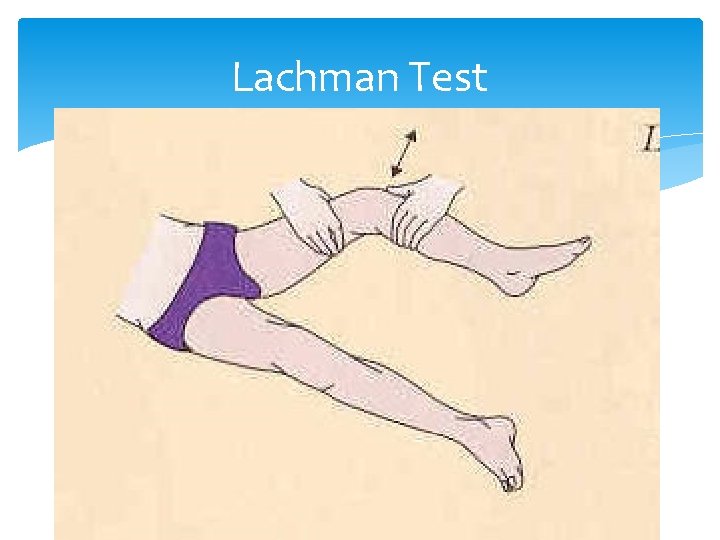
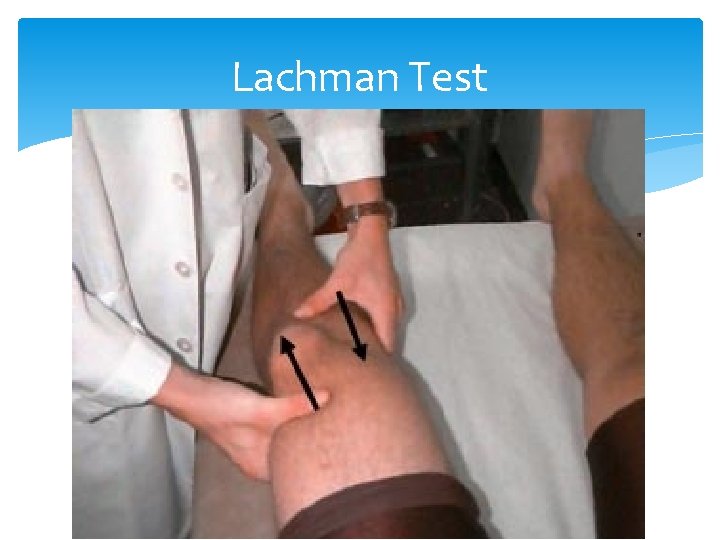
Anterior-posterior instability of the knee Tests for Anterior-posterior instability, or injury to the cruciate ligaments include the Lachman and Drawer tests. Anterior displacement of the tibia implies anterior cruciate ligament tear. Posterior displacement of the tibia implies posterior cruciate ligament tear.
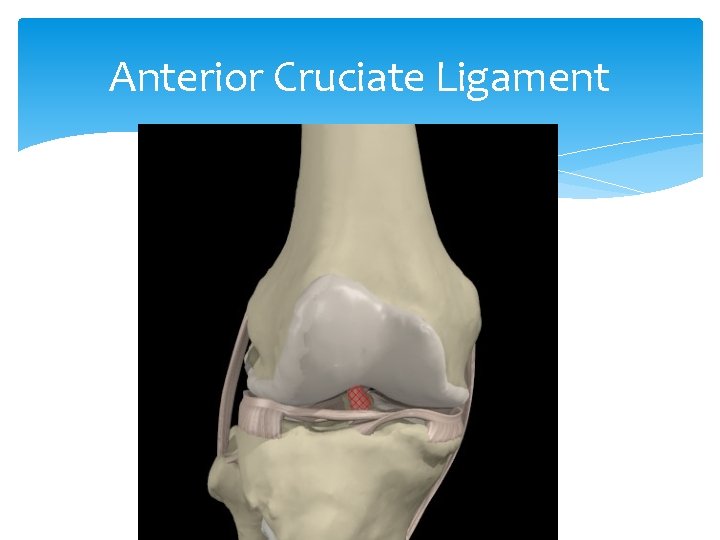
Cruciate Ligament Tear Provides anterior/posterior stability May see partial or complete tear Mechanism: Twisting injury with usual contact (athletes) Signs and Symptoms include pain, swelling, hemarthrosis and instability Tests: MRI, Drawer test, Lachman test Treatment: RICE, knee immobilizer, analgesics, surgery
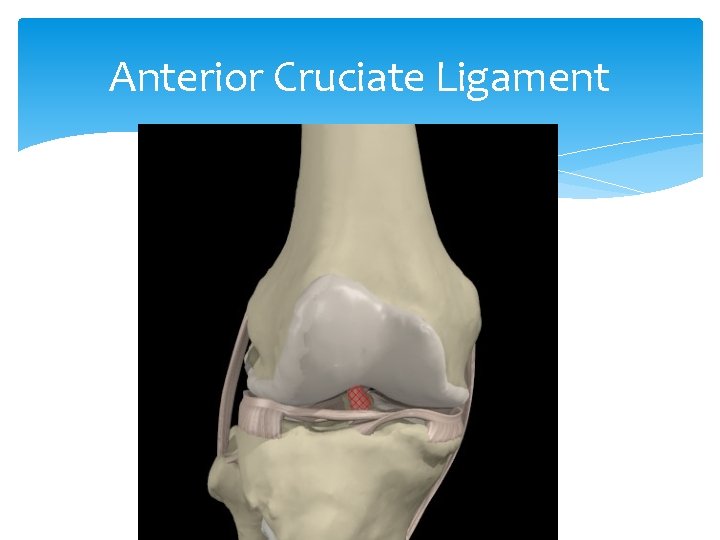
Anterior Cruciate Ligament
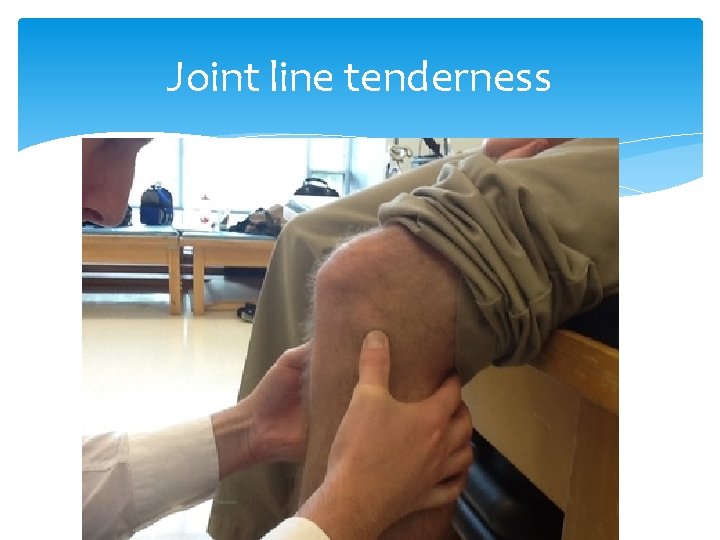
Joint line tenderness
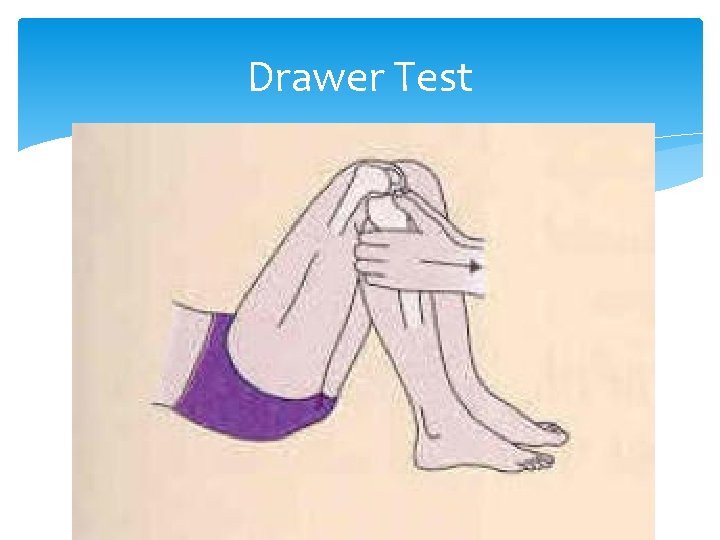
Drawer Test
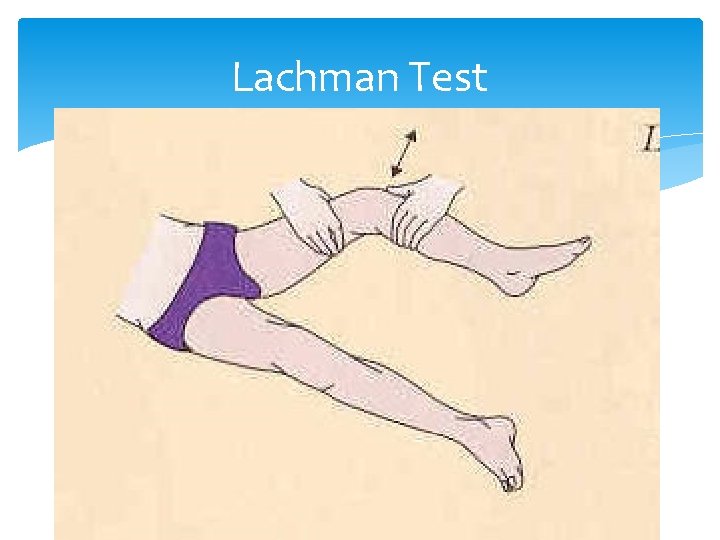
Lachman Test
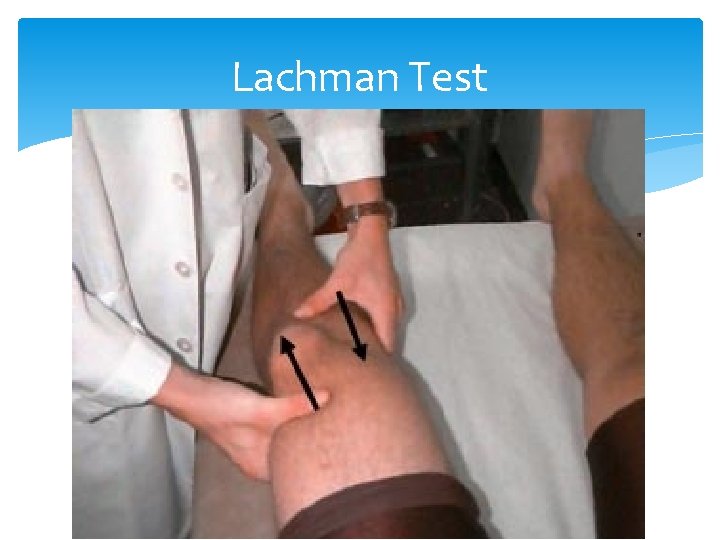
Lachman Test
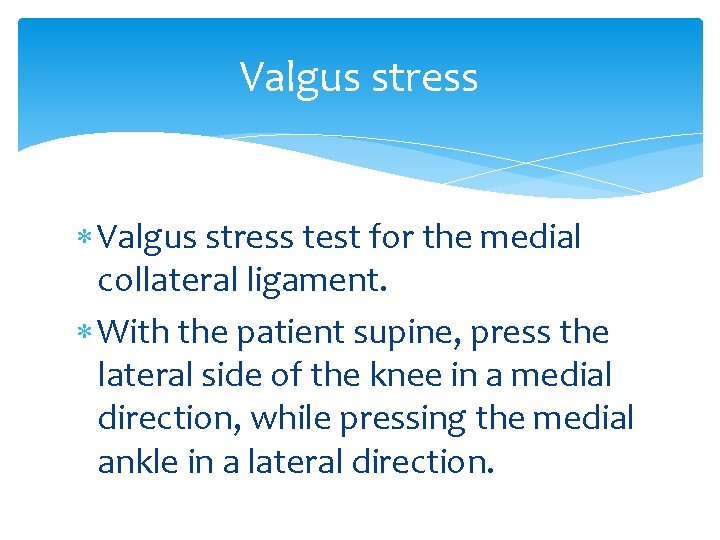
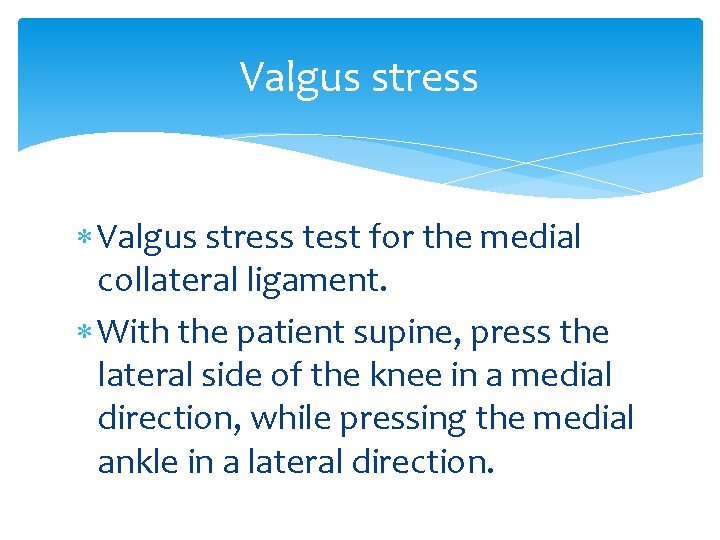
Valgus stress test for the medial collateral ligament. With the patient supine, press the lateral side of the knee in a medial direction, while pressing the medial ankle in a lateral direction.
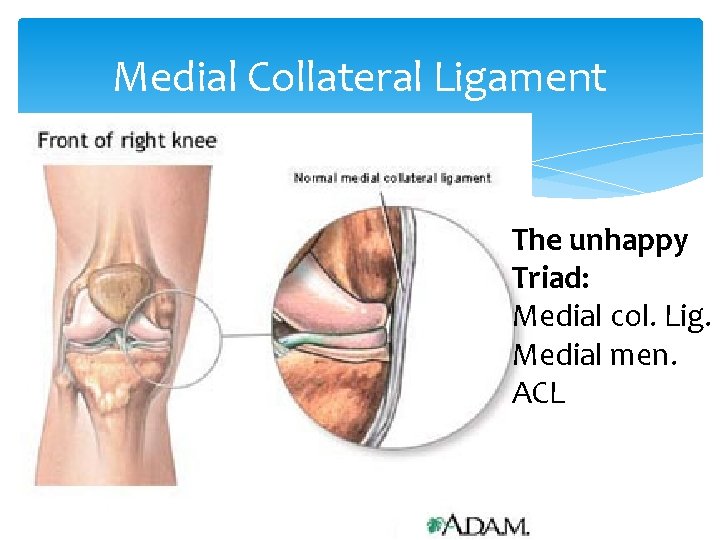
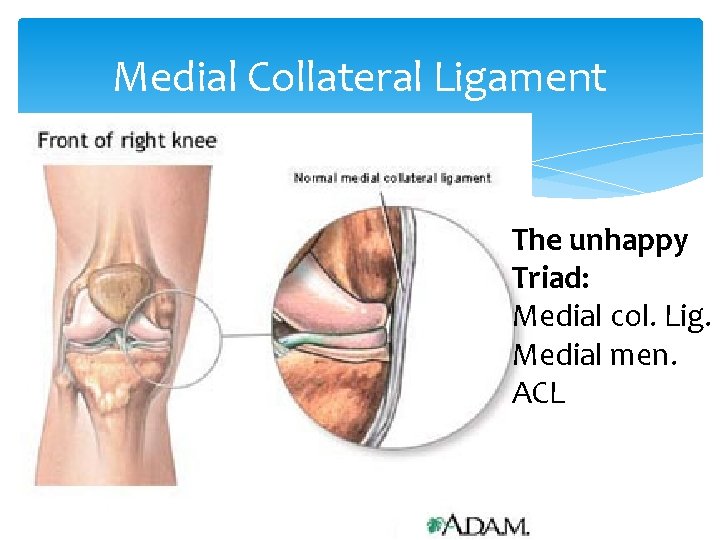
Medial Collateral Ligament The unhappy Triad: Medial col. Lig. Medial men. ACL
Varus Stress Checks stability of Lateral Collateral Ligament With the patient supine, press the medial side of the knee in a lateral direction, while pressing the lateral ankle in a medial direction.

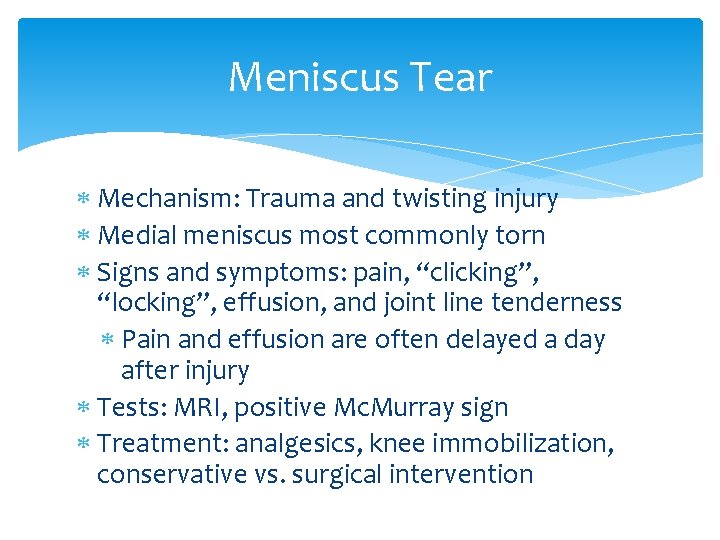
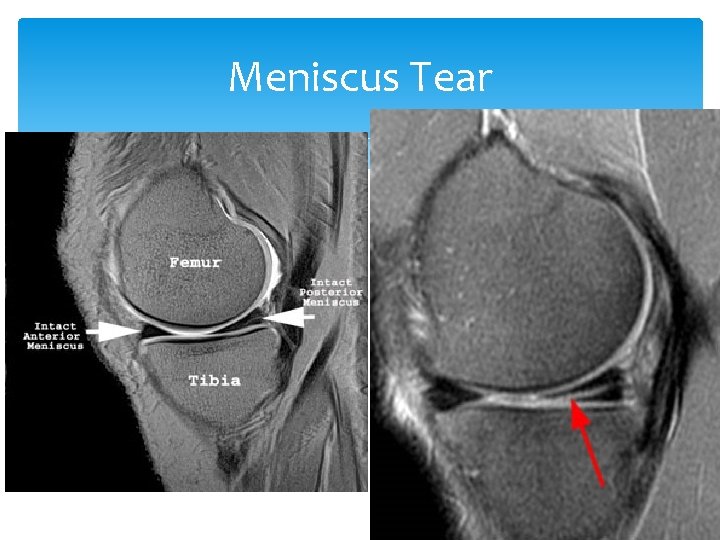
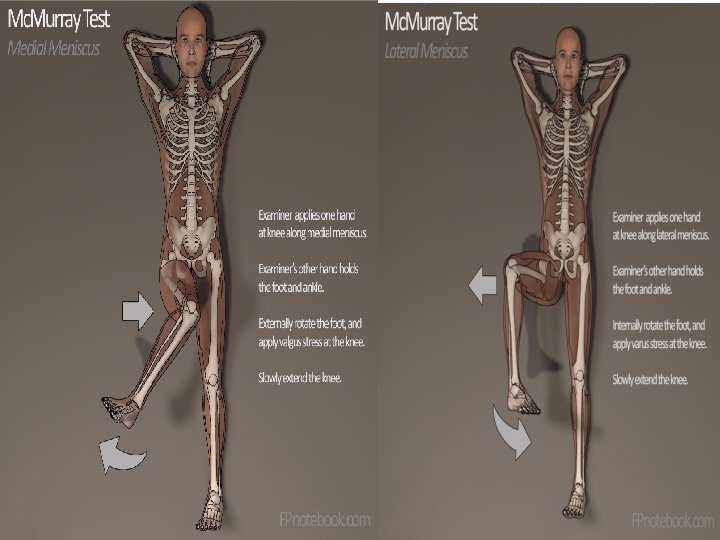
Meniscus Tear Mechanism: Trauma and twisting injury Medial meniscus most commonly torn Signs and symptoms: pain, “clicking”, “locking”, effusion, and joint line tenderness Pain and effusion are often delayed a day after injury Tests: MRI, positive Mc. Murray sign Treatment: analgesics, knee immobilization, conservative vs. surgical intervention
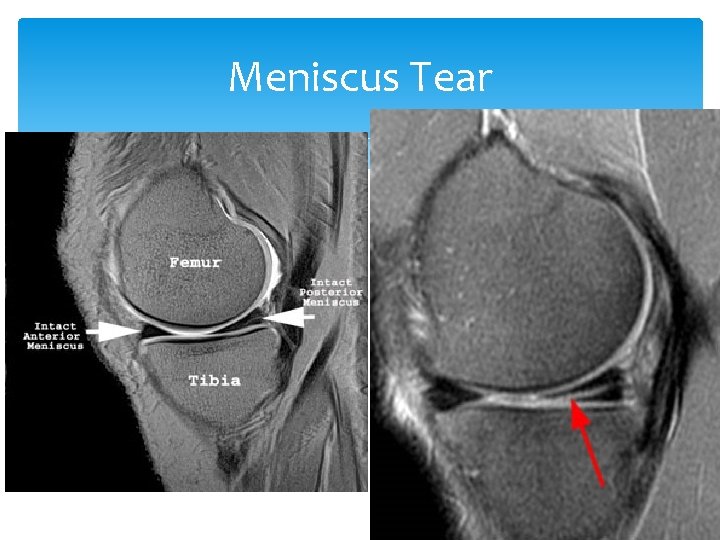
Meniscus Tear
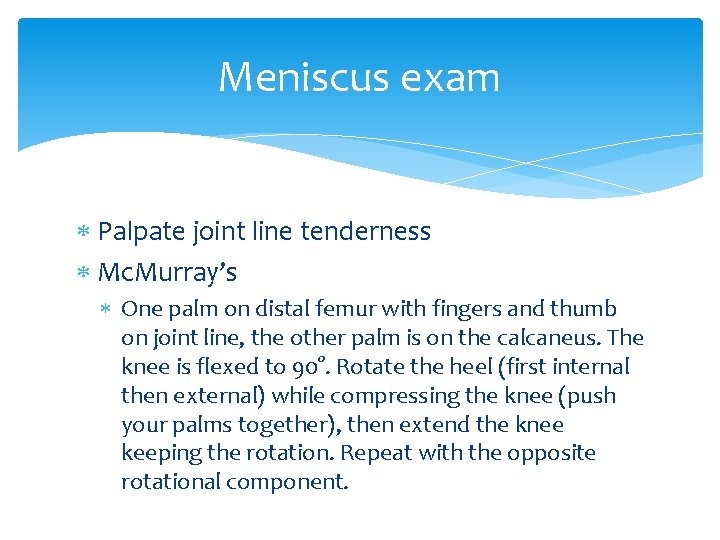
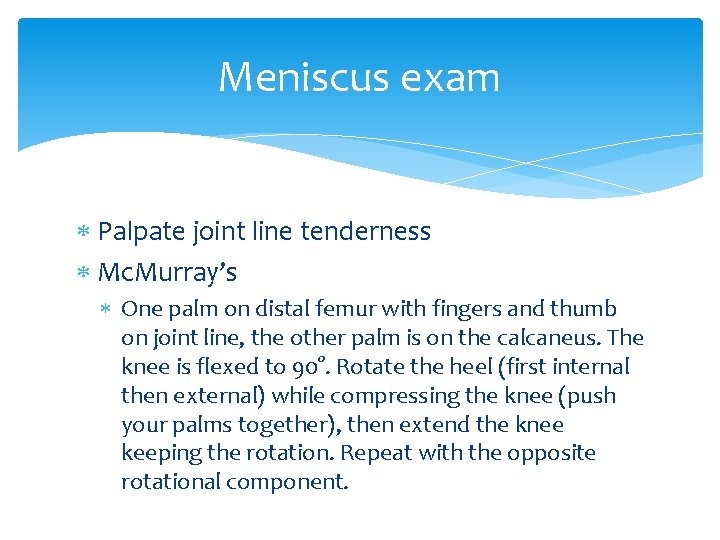
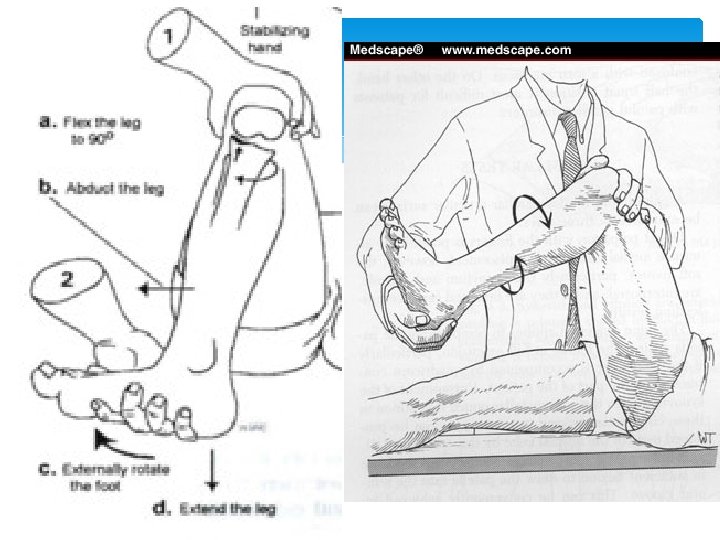
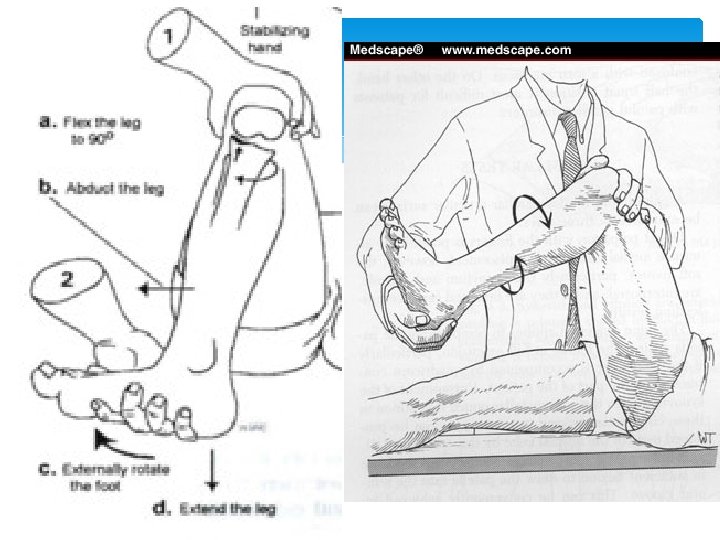
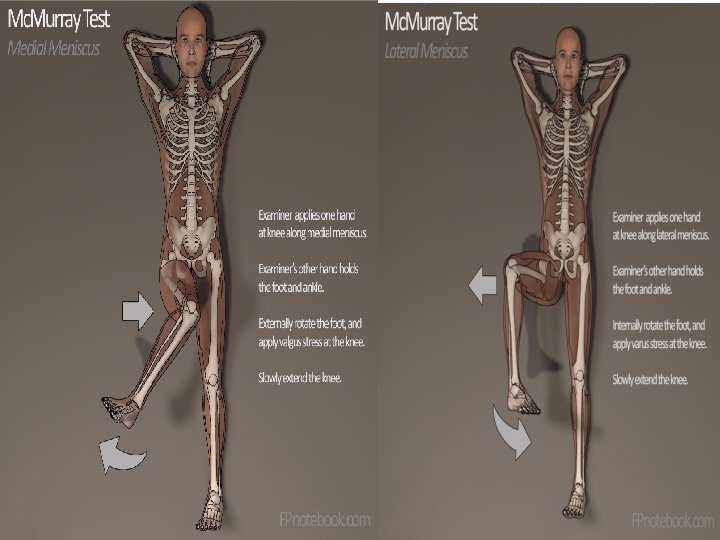
Meniscus exam Palpate joint line tenderness Mc. Murray’s One palm on distal femur with fingers and thumb on joint line, the other palm is on the calcaneus. The knee is flexed to 90°. Rotate the heel (first internal then external) while compressing the knee (push your palms together), then extend the knee keeping the rotation. Repeat with the opposite rotational component.
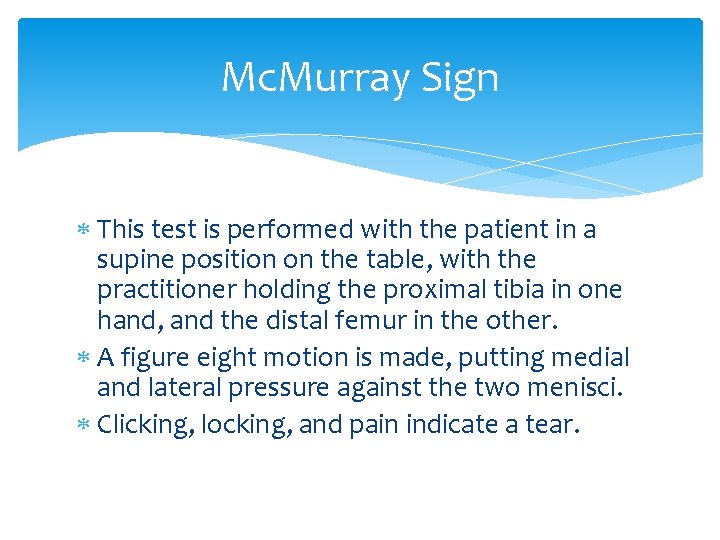
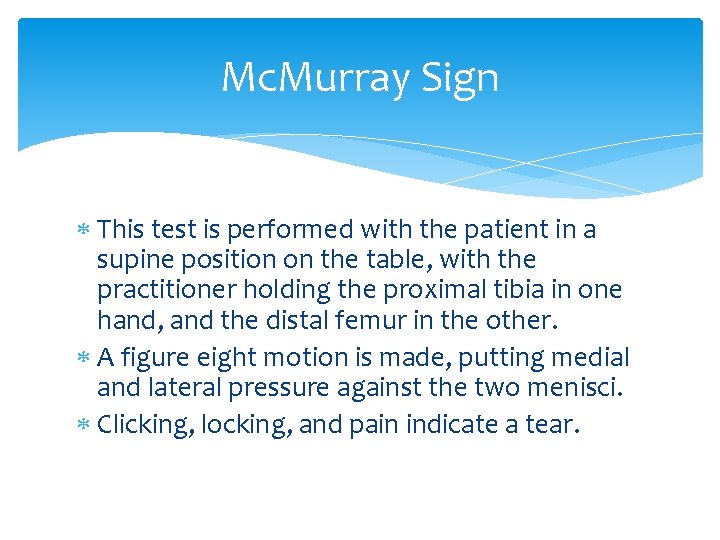
Mc. Murray Sign This test is performed with the patient in a supine position on the table, with the practitioner holding the proximal tibia in one hand, and the distal femur in the other. A figure eight motion is made, putting medial and lateral pressure against the two menisci. Clicking, locking, and pain indicate a tear.
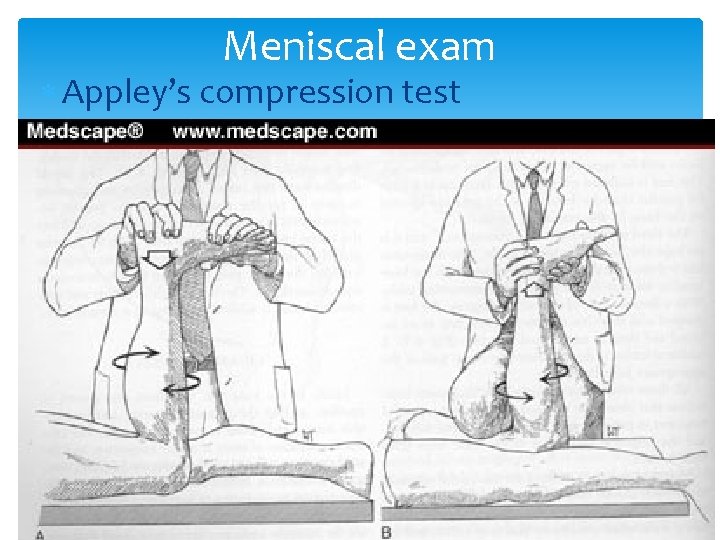
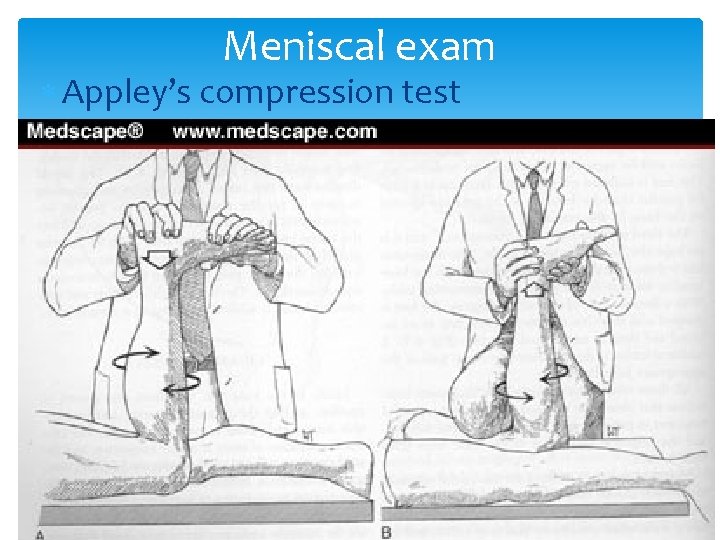
Meniscal exam Appley’s compression test
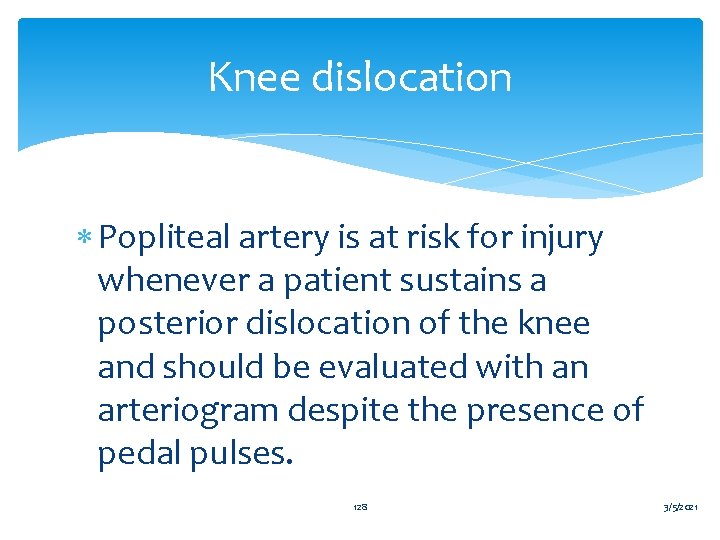
Knee dislocation Popliteal artery is at risk for injury whenever a patient sustains a posterior dislocation of the knee and should be evaluated with an arteriogram despite the presence of pedal pulses. 128 3/5/2021
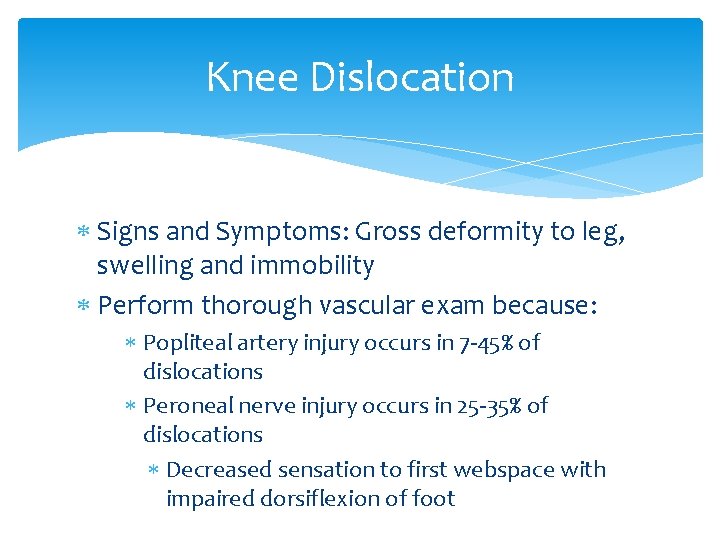
Knee Dislocation Signs and Symptoms: Gross deformity to leg, swelling and immobility Perform thorough vascular exam because: Popliteal artery injury occurs in 7 -45% of dislocations Peroneal nerve injury occurs in 25 -35% of dislocations Decreased sensation to first webspace with impaired dorsiflexion of foot

Knee Injury Treatment Rest (immobilization) Ice Compression Elevation Analgesia

Knee Aspiration
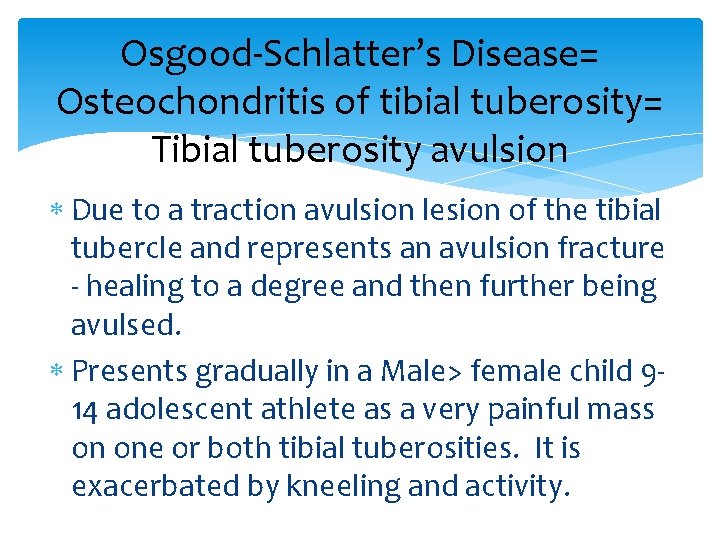
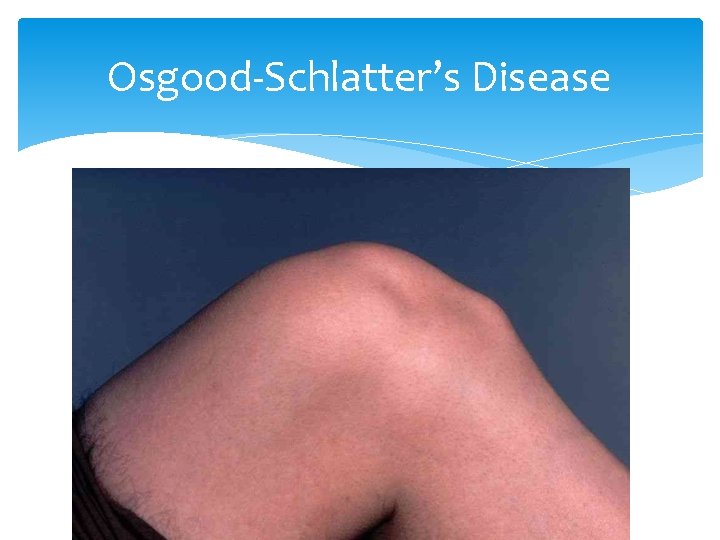
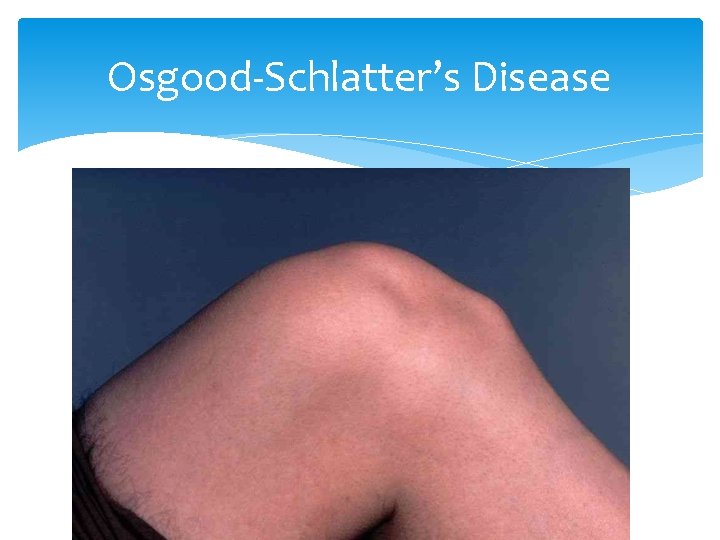
Osgood-Schlatter’s Disease= Osteochondritis of tibial tuberosity= Tibial tuberosity avulsion Due to a traction avulsion lesion of the tibial tubercle and represents an avulsion fracture - healing to a degree and then further being avulsed. Presents gradually in a Male> female child 914 adolescent athlete as a very painful mass on one or both tibial tuberosities. It is exacerbated by kneeling and activity.
Osgood-Schlatter’s Disease
Osgood-Schlatter’s Disease Dx On PE, the pain and tenderness is directly over the tibial tuberosity. Pain is exacerbated by knee extension and squatting. X-ray is not necessary to make the Dx, which is clinical. If done to differentiate, X-ray will show DDx includes slipped capfem epishesis and Legg-Calve-Perth’s, tumor
Osgood-Schlatter’s Disease Rx Continue sports activity Pain control with Acetaminophen, NSAIDs Wrapping Ice PT to strengthen quads, ROM quads and Hams Prognosis is great and resolves when epiphyseal plates close.
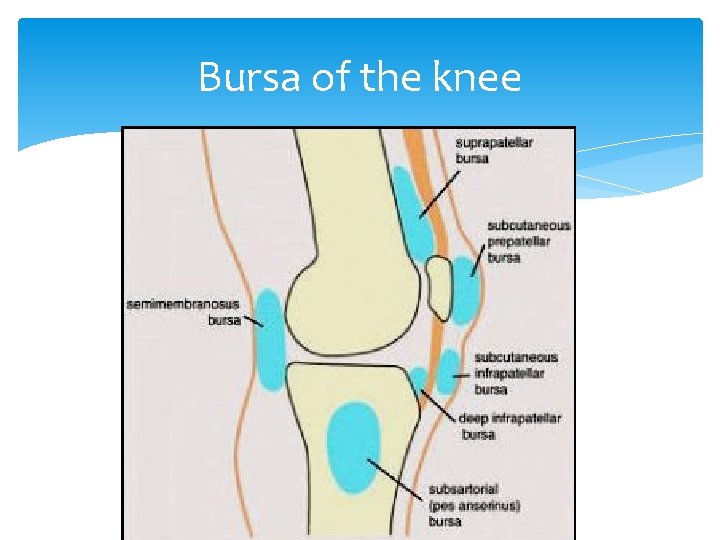
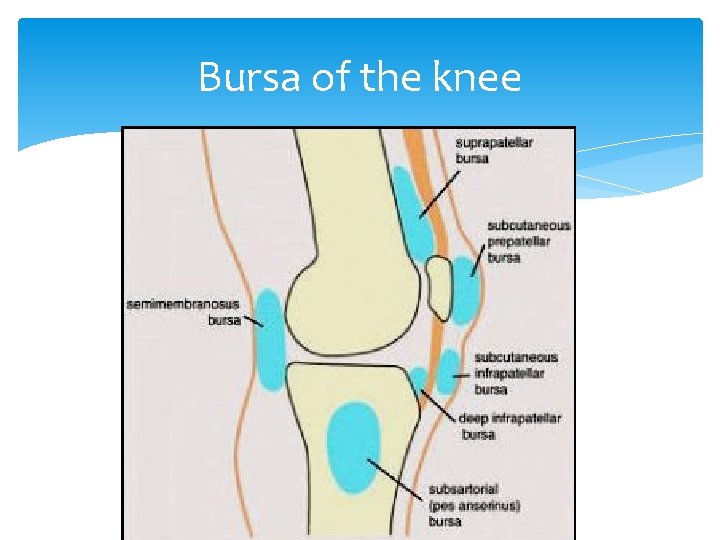
Bursa of the knee
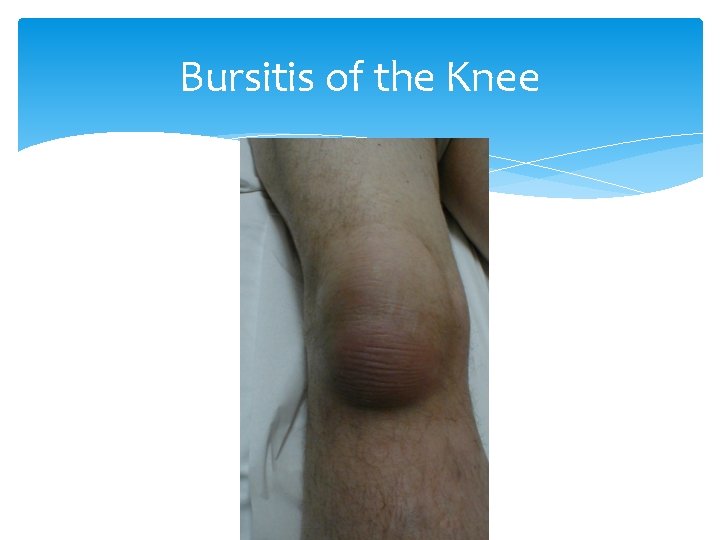
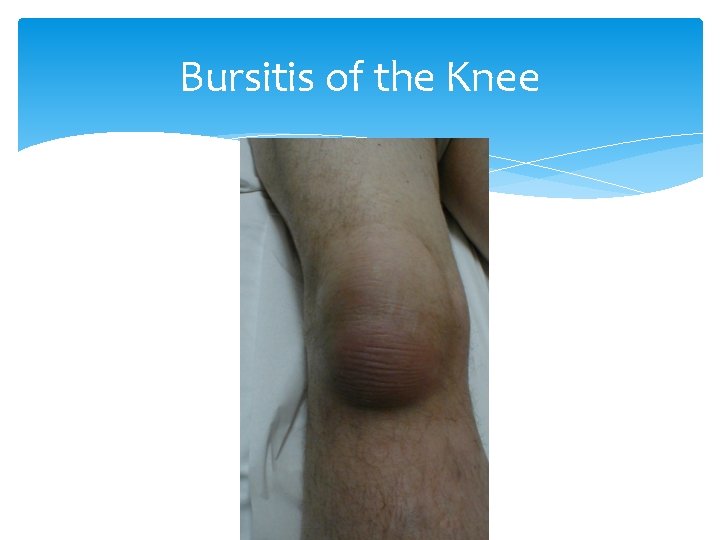
Bursitis of the Knee

Bursitis of the Knee
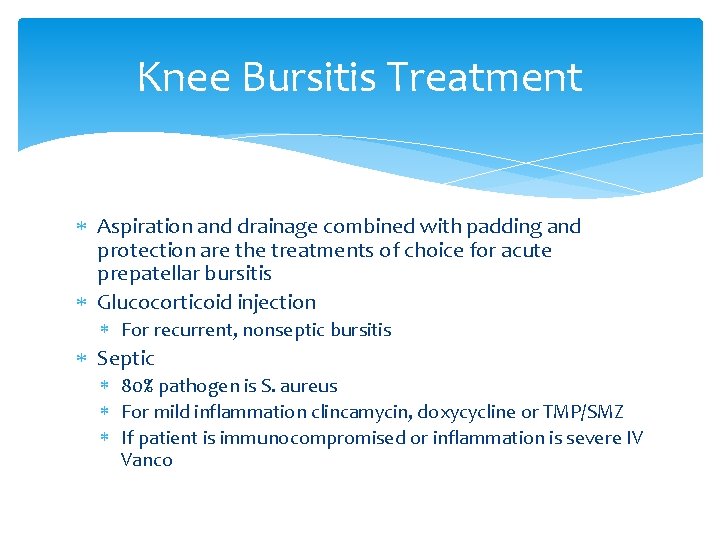
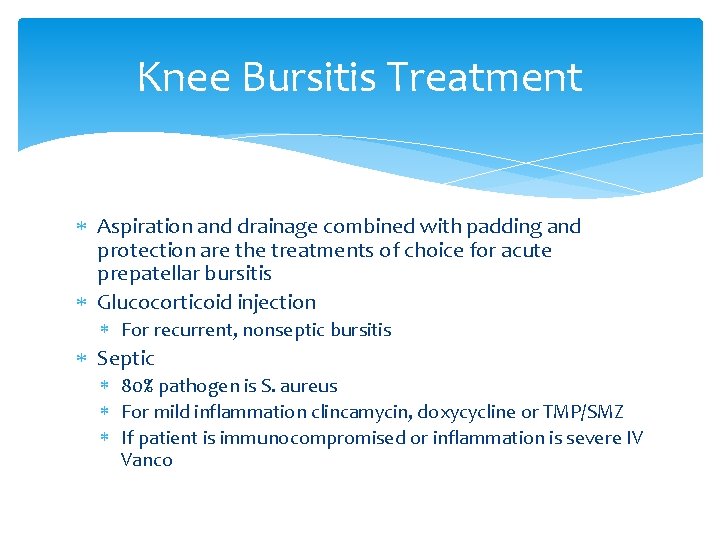
Knee Bursitis Treatment Aspiration and drainage combined with padding and protection are the treatments of choice for acute prepatellar bursitis Glucocorticoid injection For recurrent, nonseptic bursitis Septic 80% pathogen is S. aureus For mild inflammation clincamycin, doxycycline or TMP/SMZ If patient is immunocompromised or inflammation is severe IV Vanco

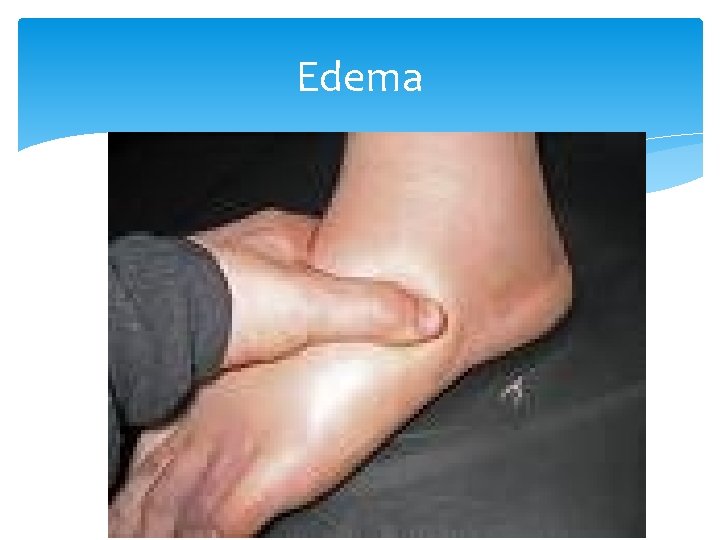
Edema History Ask a patient if his legs are swollen, or if rings are tight. Be sure to determine onset, duration, aggravating factors.
Pitting edema If the pressing causes an indentation that persists for some time after the release of the pressure, the edema is referred to as pitting edema. It is measured, and therefore documented as 1+, 2+, 3+ and 4+.
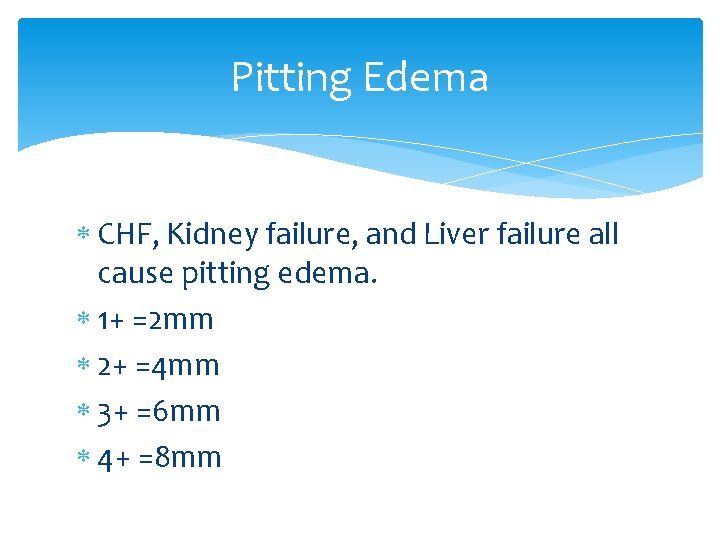
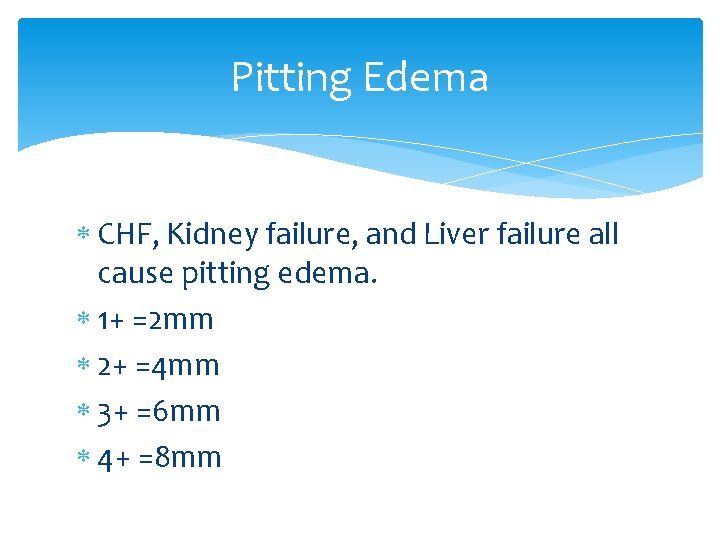
Pitting Edema CHF, Kidney failure, and Liver failure all cause pitting edema. 1+ =2 mm 2+ =4 mm 3+ =6 mm 4+ =8 mm
Pitting edema The most common local conditions that cause edema are varicose veins and thrombophlebitis of the deep veins of the legs.
Nonpitting edema The skin does not result in a persistent indentation. Non-pitting edema can occur in certain disorders of the lymphatic system such as lymphedema, that may occur after a mastectomy, lymph node surgery, or congenitally. Pretibial myxedema is a swelling over the shin that occurs in some patients with hyperthyroidism.
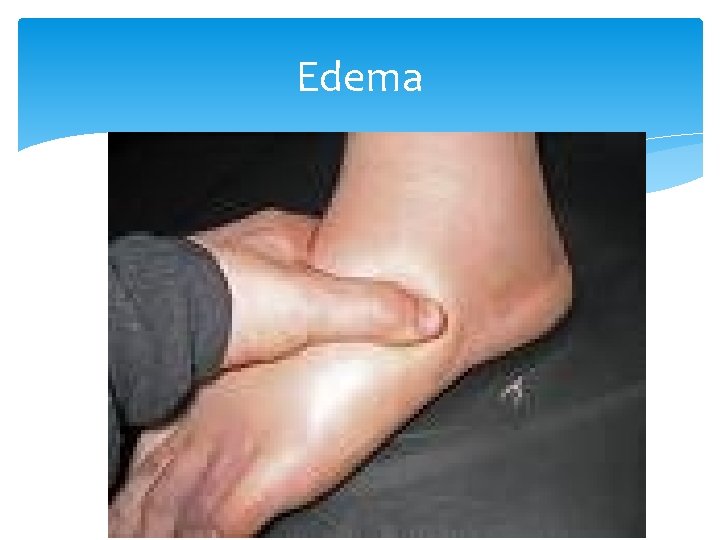
Edema
Unilateral pedal edema For Unilateral pedal edema, DVT should be at the top of your DDx
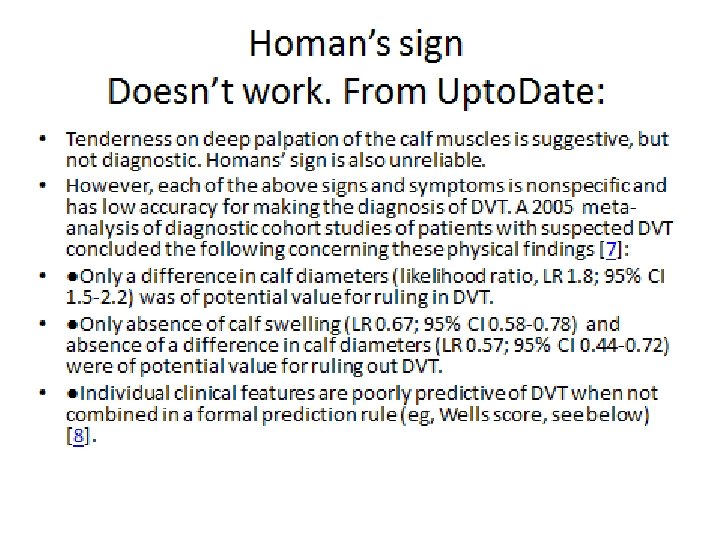
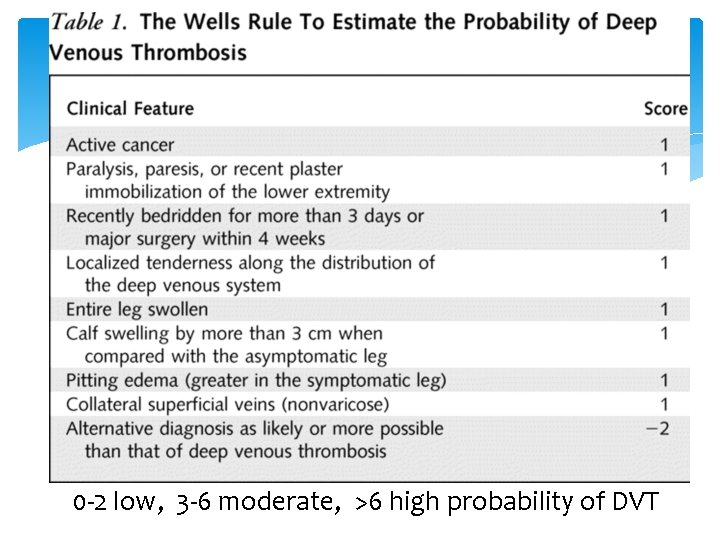
0 -2 low, 3 -6 moderate, >6 high probability of DVT
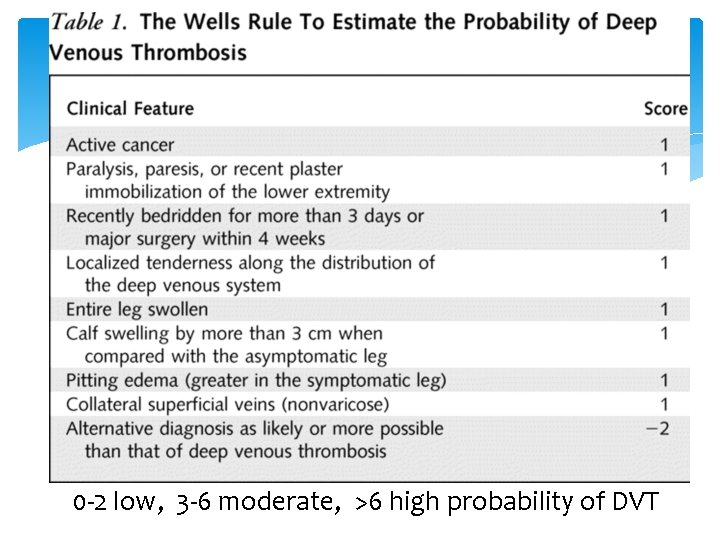
Ankle Fractures Signs an Symptoms: inability to bear weight Can’t walk more than 4 steps Pain and swelling Point tenderness Obvious deformity

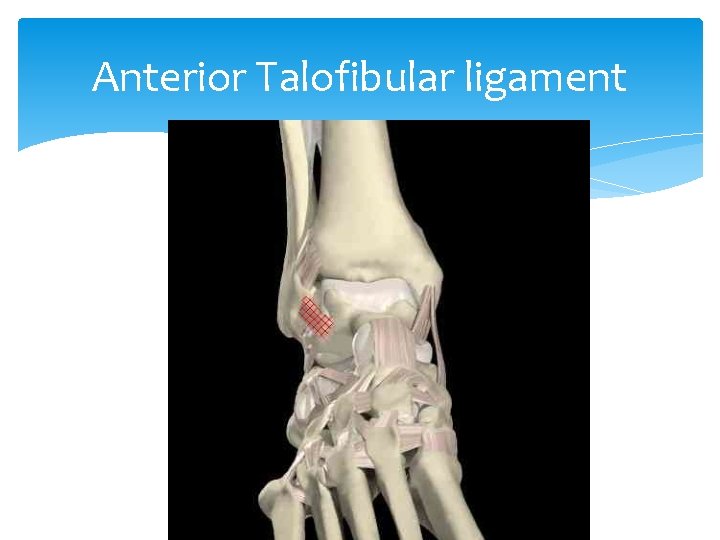
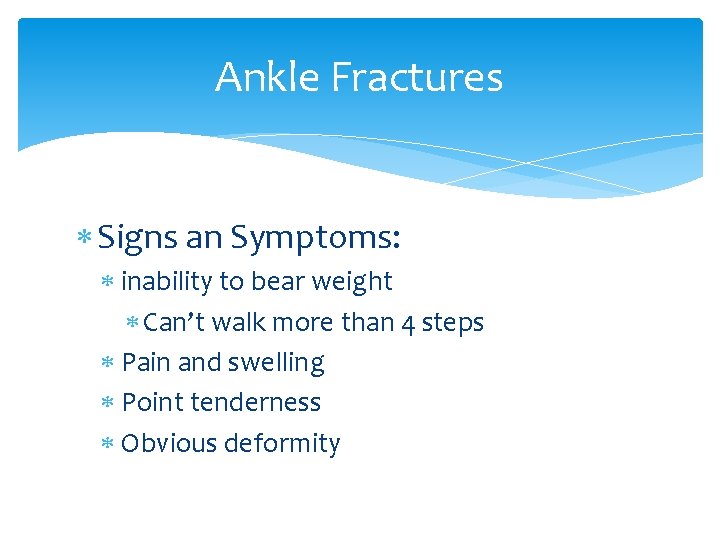
Ankle Sprain Mechanism: Inversion forces Most common injury of the ankle Most common ligament injured— anterior talo-fibular ligament
Anterior Talofibular ligament
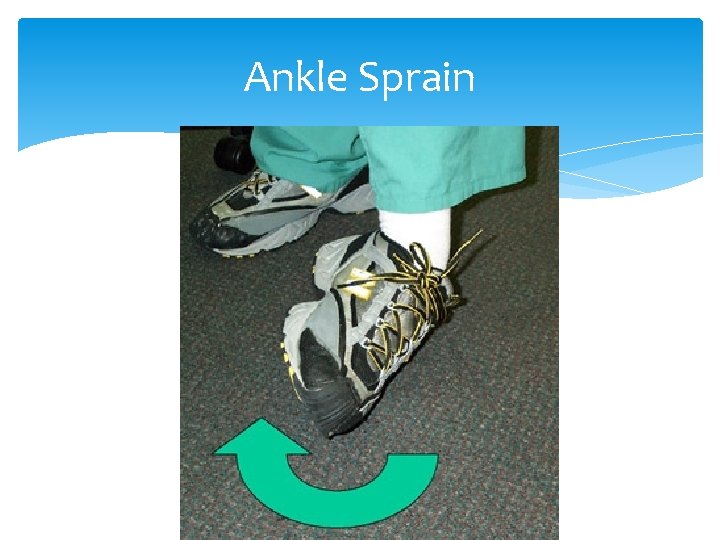
Ankle Sprain
Sprain versus Strain Sprain: involves collagenous tissue such as ligaments and tendons Mechanism by twist or stretch Strain: injury to the bone-tendon unit at the myotendinous junction or the muscle itself Mechanism by muscle contraction
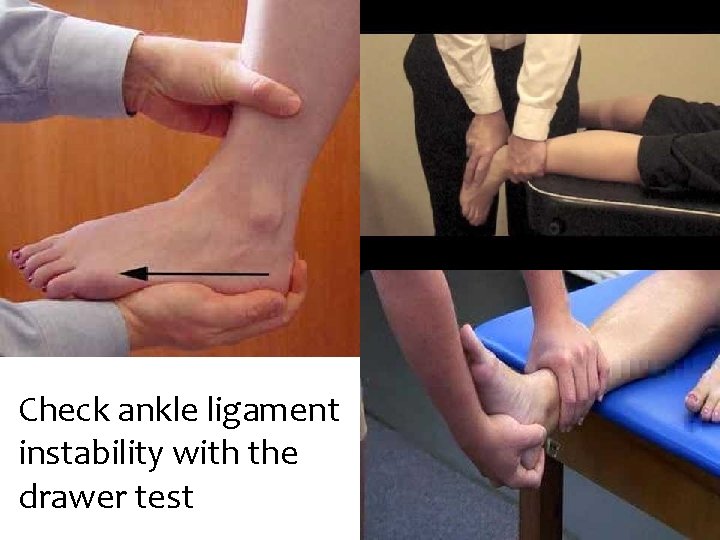
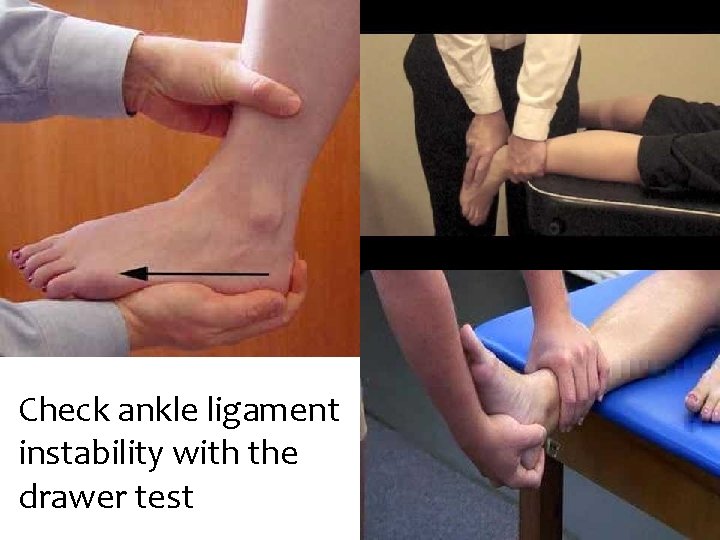
Check ankle ligament instability with the drawer test
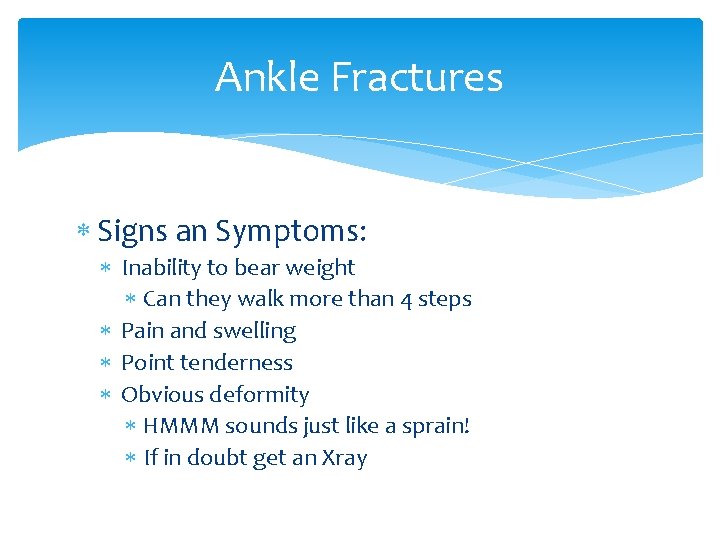
Ankle Fractures Signs an Symptoms: Inability to bear weight Can they walk more than 4 steps Pain and swelling Point tenderness Obvious deformity HMMM sounds just like a sprain! If in doubt get an Xray
Ankle Fractures are commonly either medial or lateral, but may be complex: Bimalleolar fracture—Pott’s fx or Dupuytren fx Trimalleolar fracture—Henderson fx (involves medial, lateral, and posterior malleoli of tibia)

Ankle Fractures
Ankle Fracture treatment Stable fracture (fibula) Boot Unstable (tibia or both) Splint and refer to ortho depending on the Mof. I, N/V status
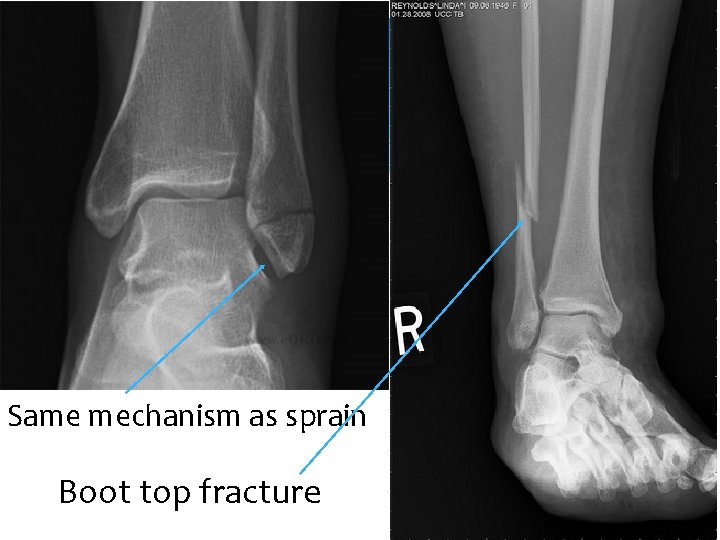
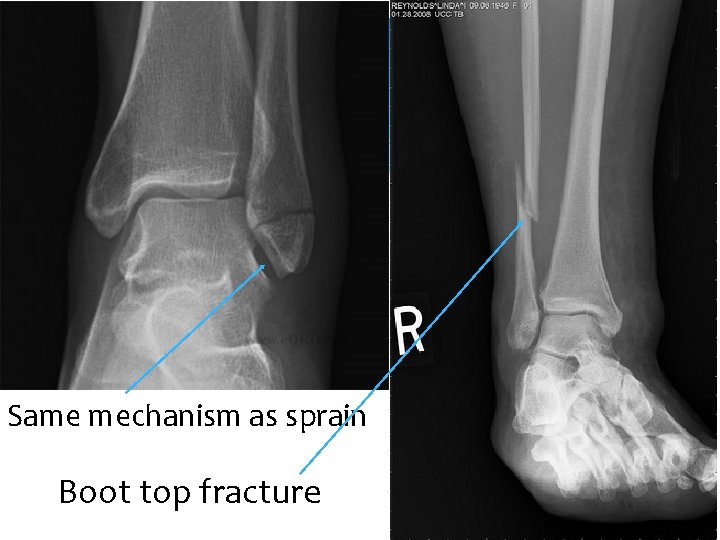
Same mechanism as sprain Boot top fracture
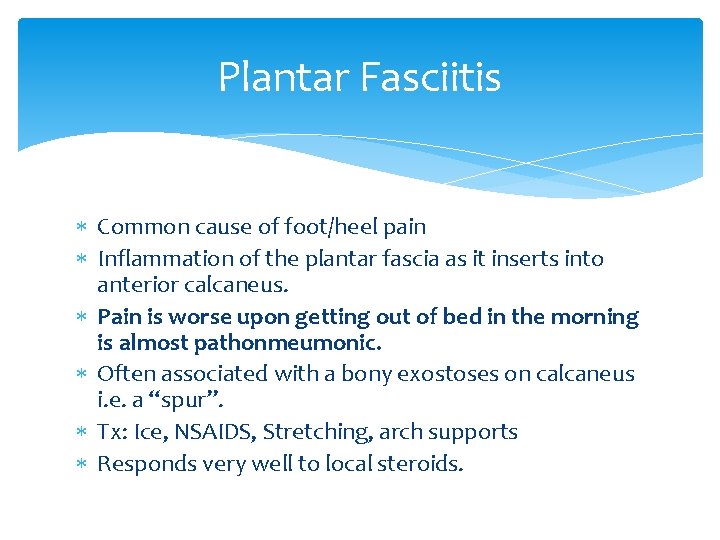
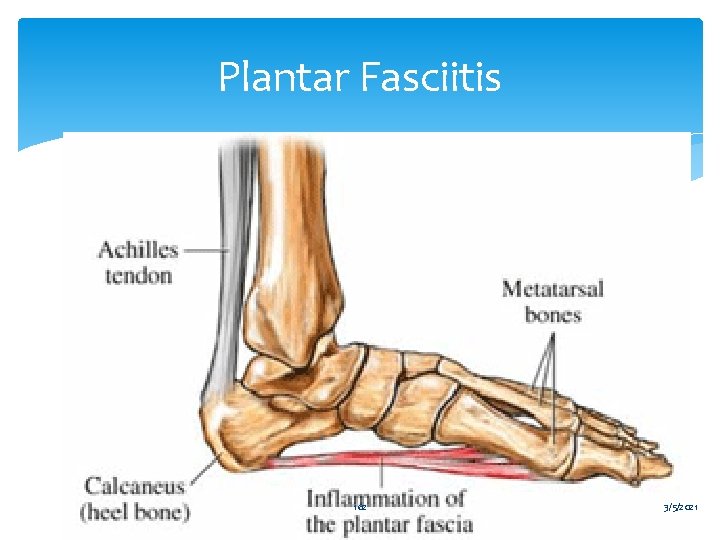
Plantar Fasciitis Common cause of foot/heel pain Inflammation of the plantar fascia as it inserts into anterior calcaneus. Pain is worse upon getting out of bed in the morning is almost pathonmeumonic. Often associated with a bony exostoses on calcaneus i. e. a “spur”. Tx: Ice, NSAIDS, Stretching, arch supports Responds very well to local steroids.
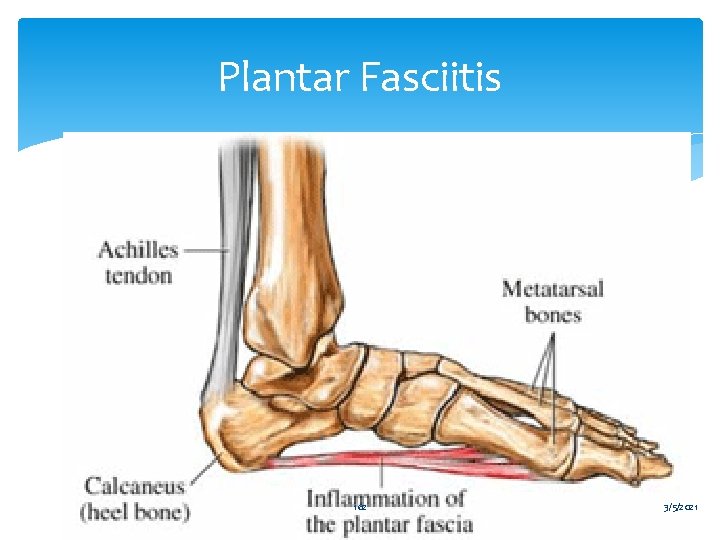
Plantar Fasciitis 162 3/5/2021

Plantar Fasciitis – Treatment Stretching exercises Prefabricated, OTC, shoe heel inserts Rest Short course (2 – 3 weeks) NSAID If the above fail (3 -4 weeks no improvement) try glucocorticoid + anesthetic injection
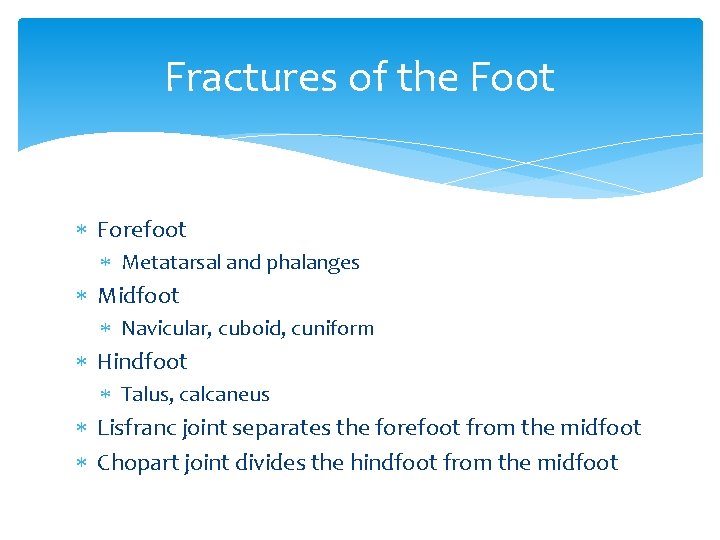
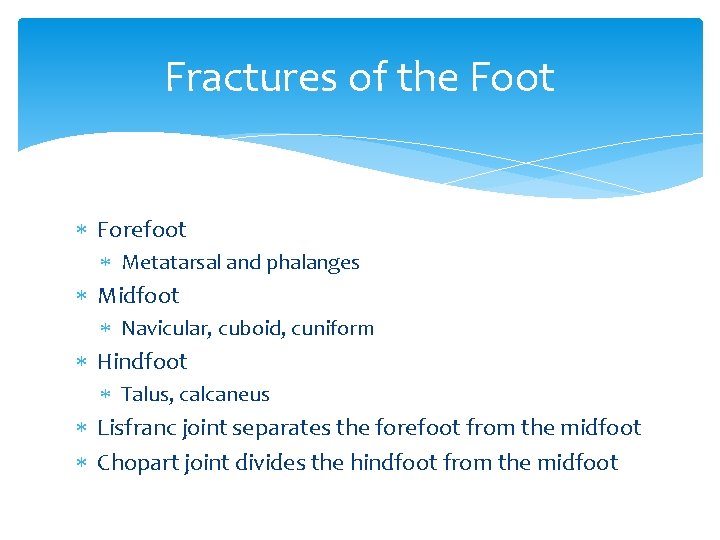
Fractures of the Foot Forefoot Metatarsal and phalanges Midfoot Navicular, cuboid, cuniform Hindfoot Talus, calcaneus Lisfranc joint separates the forefoot from the midfoot Chopart joint divides the hindfoot from the midfoot
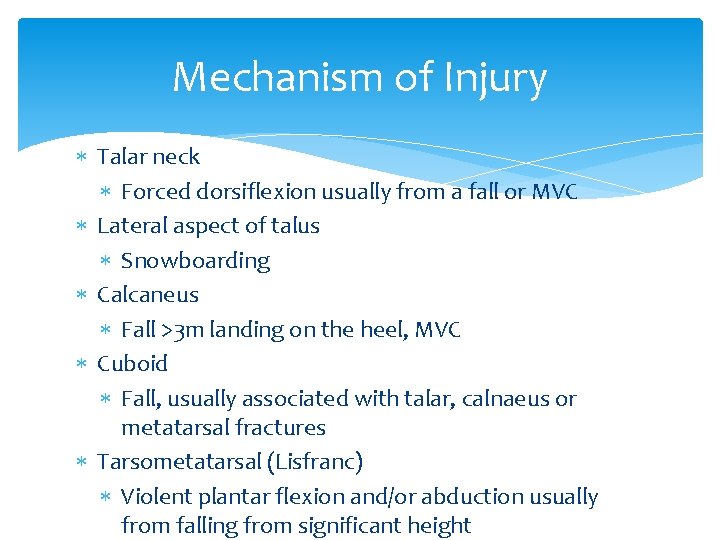
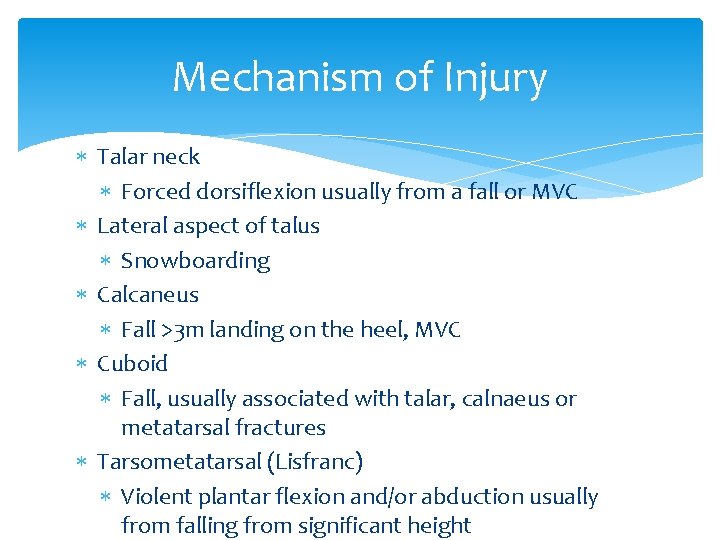
Mechanism of Injury Talar neck Forced dorsiflexion usually from a fall or MVC Lateral aspect of talus Snowboarding Calcaneus Fall >3 m landing on the heel, MVC Cuboid Fall, usually associated with talar, calnaeus or metatarsal fractures Tarsometatarsal (Lisfranc) Violent plantar flexion and/or abduction usually from falling from significant height

Treatment Emergent ortho consult with Open fracture Compartment syndrome Vascular compromise Urgent ortho consult Talar nec fracture Intrarticular calneus fracture Lisfranc fracture Generally RICE, analgesia
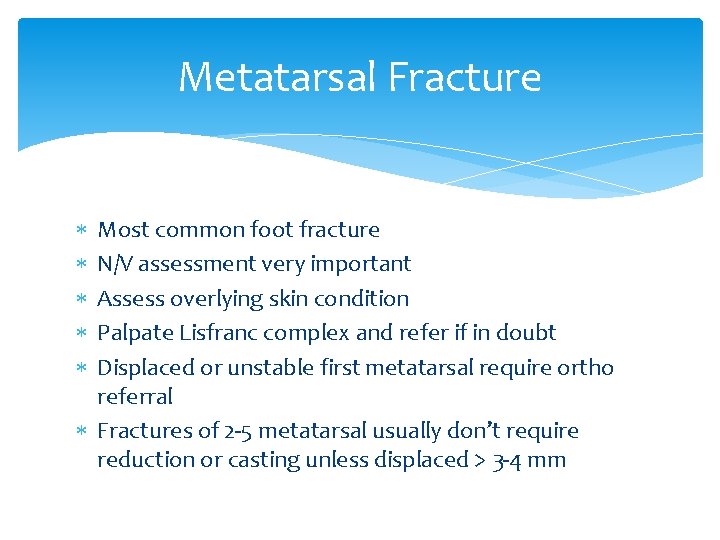
Metatarsal Fracture Most common foot fracture N/V assessment very important Assess overlying skin condition Palpate Lisfranc complex and refer if in doubt Displaced or unstable first metatarsal require ortho referral Fractures of 2 -5 metatarsal usually don’t require reduction or casting unless displaced > 3 -4 mm


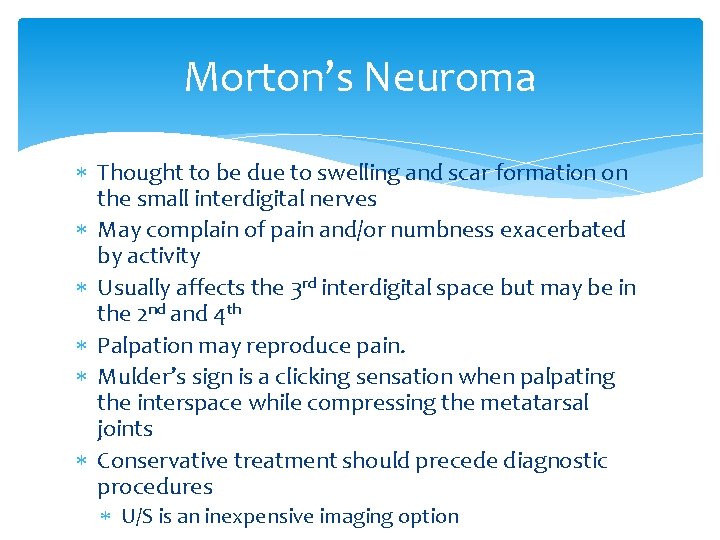
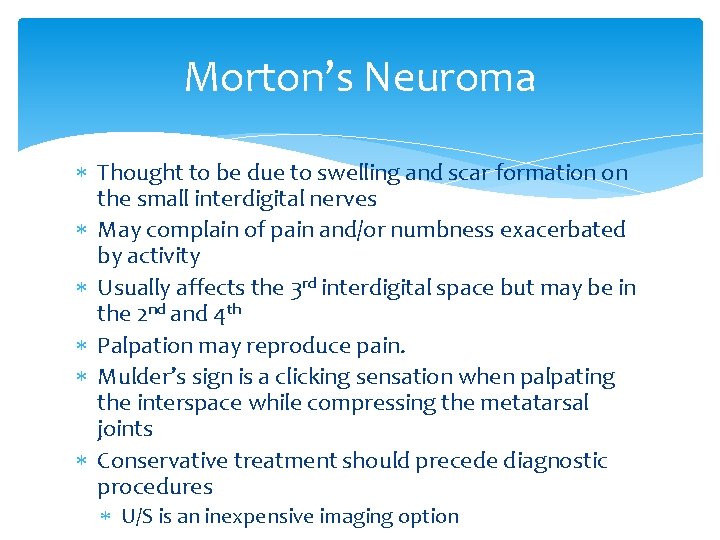
Morton’s Neuroma Thought to be due to swelling and scar formation on the small interdigital nerves May complain of pain and/or numbness exacerbated by activity Usually affects the 3 rd interdigital space but may be in the 2 nd and 4 th Palpation may reproduce pain. Mulder’s sign is a clicking sensation when palpating the interspace while compressing the metatarsal joints Conservative treatment should precede diagnostic procedures U/S is an inexpensive imaging option
Musculoskeletal Exam Summary Good Hx: Trauma, Constitutional Sx, Red flags, restrained in MVC? Good PE: Inspect Palpate what hurts gently! ROM active and passive Neurovascular exam Good workup: radiography if indicated
References Patel, Nina H. , Holman and John R. Overuse or injury: is it Tendonitis or Bursitis? Consultant April 1, 2008 Bol. 48 No. 4, pages 314 to 320. Provenzano, David A. and Levin, Morris. Chronic Pain Syndromes: How to break the cycle, Part 1, Consultant April 1, 2008 Bol. 48 No. 4, pages 297 to 304. Seidel, Ball, Davis and Benedict. Mosby’s Guide to Physical Examination Fourth Edition. Benson, Leon S. Orthopedic Pearls. Hoppenfeld, Stanley. Physical Exam of the Spine and Extremities. Appleton-Century. Crofts 1976. Bickley, Lynn S. and Szilagyi, Peter G. Bates’ Guide to Physical Examination and History Taking Ninth Edition Lippencott Williams & Wilkins 2007. Dr. Samuel Cleveland, Barry University PA Program Medical Director Tintinalli, Ruiz, and Krome. EM 4 th edition. Tierney, Mc. Phee, Papadakis. Current Medical Dx&Tx 2002.
References • • Larson, Betty and Kuntz, Susan. Dx and Pharm management of Back Pain. JAAPA, 25(3) March 2012. Koehler SM, Fields KB, Grayzel J. AC joint injuries in Upto. Date 2012 Hsu PS, Armon C, Levin K. Lumbosacral radiculopathy in Upto. Date 2012. Topic 5262 Version 9. 0 Maughan KL, Upto. Date 2012 Topic 189 Version 9. 0 Schiff D. Upto. Date 2012. Topic 2819 Version 4. 0 Sherman. Shraider. Shoulder dislocation and reduction Uptodate 2012. Topic 258 Version 8. 0 Burroughs KE. Scaphoid fractures. Uptodate Topic 197 Version 11. 0. 2012 Dr. Armstrong, lecture slides Kienstra AJ, Macias CG. Ossgood Shlatter Disease. Up to date Topic 6289 Version 7. 0 2012 Isolated clavicle fracture with secondary pneumothorax, Hong Kong Journal of EM Upto. Date. Topic Causes of limp in children 6460 Version 11. 0 Upto. Date Approach to child with bow-legs Topic 6285 Version 11. 0 Up. To. Date Pelvic trauma: Initial evaluation and management Wendy Langen, lecture content Albert Armstrong- shoulder X rays SA Landaw, KA Bauer. Uptodate, 2015 Topic 1322 Version 33. 0
 Incomplete fracture radiology
Incomplete fracture radiology Greenstick fracture definition
Greenstick fracture definition Visceral peritoneum
Visceral peritoneum Epiphyseal growth plates
Epiphyseal growth plates Epiphyseal line
Epiphyseal line Epiphyseal plate vs line
Epiphyseal plate vs line Epiphyseal plate
Epiphyseal plate Epiphyseal fusion
Epiphyseal fusion Nasal silling/guttering skull
Nasal silling/guttering skull What is epiphyseal plate
What is epiphyseal plate Epiphyseal plate vs line
Epiphyseal plate vs line Epiphyseal plate
Epiphyseal plate Epiphyseal fusion
Epiphyseal fusion Appendicular
Appendicular Glutwire
Glutwire Dreieck parametrisieren
Dreieck parametrisieren Torus palatino definicion
Torus palatino definicion Sagittal keel
Sagittal keel Torus eversion
Torus eversion Glut solid cone
Glut solid cone Torus intervenosus
Torus intervenosus Torus topology network
Torus topology network Io plasma torus
Io plasma torus Cupula pericardii
Cupula pericardii Hexagonal torus
Hexagonal torus Dusty torus
Dusty torus Glut torus
Glut torus Fundamental group torus
Fundamental group torus Natalie enright jerger
Natalie enright jerger Torus eversion
Torus eversion Stanford torus space station
Stanford torus space station Jo van den brand
Jo van den brand Torus
Torus Glut solid torus
Glut solid torus Torus tubarius
Torus tubarius Torus palatin prise en charge
Torus palatin prise en charge Dusty torus
Dusty torus Ostium venarum pulmonalium
Ostium venarum pulmonalium Ductile fracture vs brittle fracture
Ductile fracture vs brittle fracture Anteversion of uterus
Anteversion of uterus Types of half turn staircase
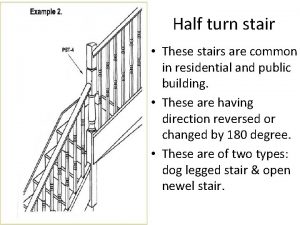
Types of half turn staircase Version in obstetrics
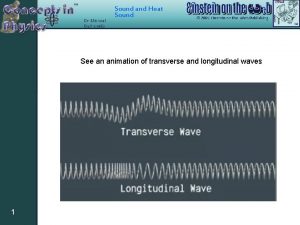
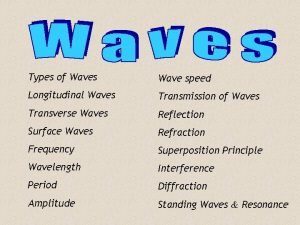
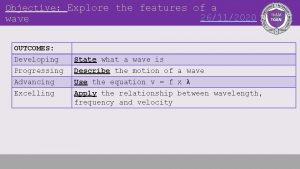
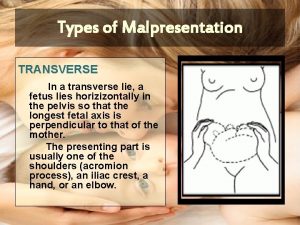
Version in obstetrics Transverse wave
Transverse wave Functions of temporal lobe
Functions of temporal lobe Occlusion rim dimensions
Occlusion rim dimensions A physics teacher attaches a slinky to the wall
A physics teacher attaches a slinky to the wall Buccal triangular ridge
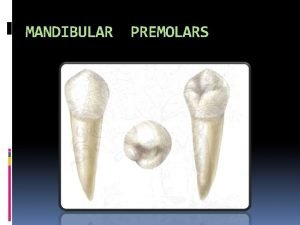
Buccal triangular ridge Transverse shear example
Transverse shear example Perineum
Perineum Shapiro
Shapiro L
L Bicep femoris
Bicep femoris Horizontal anatomical plane
Horizontal anatomical plane Right temporal bone
Right temporal bone Transverse vs longitudinal waves
Transverse vs longitudinal waves Rhinitis medicamentosa
Rhinitis medicamentosa Transverse wve
Transverse wve Tone twitch
Tone twitch Transverse colon
Transverse colon Transverse septa fungi
Transverse septa fungi Transverse binary fission
Transverse binary fission Paroi abdominale antero laterale
Paroi abdominale antero laterale Fibrous and serous pericardium
Fibrous and serous pericardium Longitudinal framing and transverse framing
Longitudinal framing and transverse framing Smooth muscle
Smooth muscle Proscenium diagram
Proscenium diagram Maxillary first molar oblique ridge
Maxillary first molar oblique ridge Double kocher's incision
Double kocher's incision Wave speed examples
Wave speed examples Ventral plane
Ventral plane Horizontal
Horizontal Efface
Efface Dry docking calculations
Dry docking calculations Transverse wave ex
Transverse wave ex Transverse cotyledon cracking in french bean
Transverse cotyledon cracking in french bean Vertical
Vertical Transverse fissure
Transverse fissure Sigmoidectomy
Sigmoidectomy Offset surveys
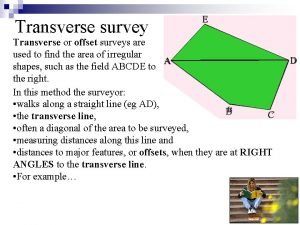
Offset surveys Example of mechanical wave
Example of mechanical wave Transverse deflection of beam
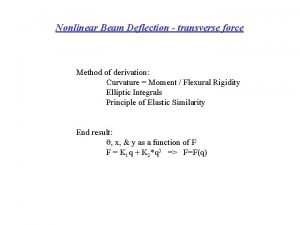
Transverse deflection of beam Transverse abdominal incision
Transverse abdominal incision Transverse colon
Transverse colon Ml cusp
Ml cusp Median sacral crest
Median sacral crest Identify the parts of the wave
Identify the parts of the wave Thigh cross section
Thigh cross section Transverse flux motor wiki
Transverse flux motor wiki Dorsal view of sheep brain
Dorsal view of sheep brain Stealer plate in ship construction
Stealer plate in ship construction Tibial tuberosity
Tibial tuberosity Transverse waves for kids
Transverse waves for kids Leopold's maneuver
Leopold's maneuver Wave list
Wave list Prevertebral muscles
Prevertebral muscles Velocity frequency wavelength triangle
Velocity frequency wavelength triangle Transverse statical stability
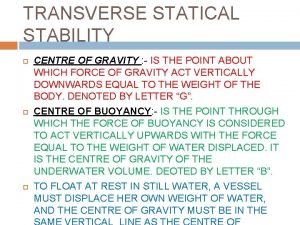
Transverse statical stability Transverse em wave
Transverse em wave Label the parts of transverse wave
Label the parts of transverse wave Transverse
Transverse Zone of decomposed dentin
Zone of decomposed dentin Transverse ridge mandibular first molar
Transverse ridge mandibular first molar Spatial reference framework
Spatial reference framework What is a mechanical wave? *
What is a mechanical wave? * Transverse myelitis physiotherapy
Transverse myelitis physiotherapy Wavelength constructive interference
Wavelength constructive interference External forces on the transverse statical stability
External forces on the transverse statical stability Conjugate and transverse axis
Conjugate and transverse axis Transverse axis gymnastics
Transverse axis gymnastics Sound waves longitudinal waves
Sound waves longitudinal waves Transverse waves def
Transverse waves def In running nip points
In running nip points Denominator in brow presentation
Denominator in brow presentation Waves energy transfer
Waves energy transfer Slings in arches of foot
Slings in arches of foot Transverse statical stability
Transverse statical stability Whats a transverse wave
Whats a transverse wave Transverse impedance of a string
Transverse impedance of a string Transverse axis of elbow joint
Transverse axis of elbow joint Vitellointestinal duct
Vitellointestinal duct The lens equation
The lens equation Muscle root word
Muscle root word Transverse tubule
Transverse tubule Dorso superior transverse lie
Dorso superior transverse lie Banana autopsy
Banana autopsy Rotator interval contents
Rotator interval contents Seesile
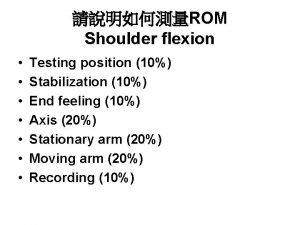
Seesile Shoulder extension rom
Shoulder extension rom Garber
Garber Double white cross aerodrome
Double white cross aerodrome Single riveted double strap butt joint
Single riveted double strap butt joint Elevated ridges “winding” around the brain
Elevated ridges “winding” around the brain Locking and unlocking of knee joint
Locking and unlocking of knee joint Muscle infra hyoïdien
Muscle infra hyoïdien Fascia of parotid gland
Fascia of parotid gland Module transverse
Module transverse Oblique plane
Oblique plane Colles fascia continuous with
Colles fascia continuous with Hyperbola equation formula
Hyperbola equation formula Wax rim measurements
Wax rim measurements Transverse waves
Transverse waves Dextrorotation uterus
Dextrorotation uterus Coronal axial sagittal
Coronal axial sagittal Goblet cell secretes
Goblet cell secretes Pneumonia and tactile fremitus
Pneumonia and tactile fremitus Accessory digestive organs
Accessory digestive organs Intersegmental ties
Intersegmental ties Interlocking cement concrete pavement
Interlocking cement concrete pavement Axial magnification
Axial magnification Cadre duodeno pancreatique
Cadre duodeno pancreatique Conic sections table
Conic sections table Light is electromagnetic wave true or false
Light is electromagnetic wave true or false Webphysics.davidson.edu physlet_resources
Webphysics.davidson.edu physlet_resources Infection du colon
Infection du colon Length of transverse axis of hyperbola
Length of transverse axis of hyperbola Transverse incision c section
Transverse incision c section Ligaments of stomach
Ligaments of stomach Smooth mucle
Smooth mucle Transverse velocity
Transverse velocity Transverse ridge mandibular first molar
Transverse ridge mandibular first molar Transverse myelitis
Transverse myelitis Longitudinal plane definition anatomy
Longitudinal plane definition anatomy Transverse jugular vein cat
Transverse jugular vein cat Transverse and longitudnal waves
Transverse and longitudnal waves Transverse wave ex
Transverse wave ex Palatine raphe
Palatine raphe Transverse tubule
Transverse tubule Lefort classification
Lefort classification Fracture en.bois vert
Fracture en.bois vert Grosse tuberosite calcaneum
Grosse tuberosite calcaneum Jungbluth clamp
Jungbluth clamp Manoeuvre arrache botte
Manoeuvre arrache botte Spino tubérositaire
Spino tubérositaire Moderately ductile fracture
Moderately ductile fracture