Allergic Rhinitis Dr Vishal Sharma Introduction Commonest chronic















- Slides: 61

Allergic Rhinitis Dr. Vishal Sharma
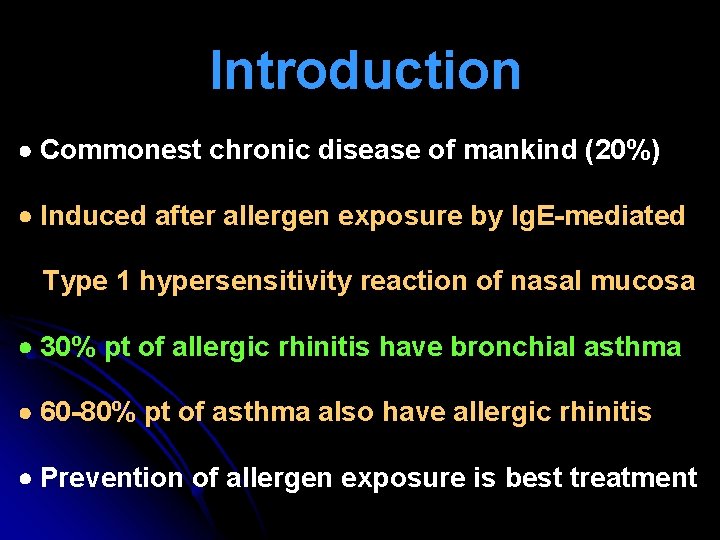
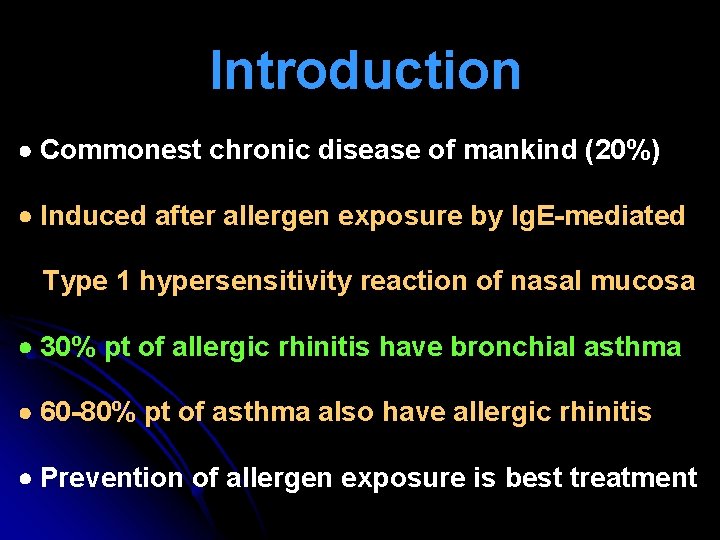
Introduction Commonest chronic disease of mankind (20%) Induced after allergen exposure by Ig. E-mediated Type 1 hypersensitivity reaction of nasal mucosa 30% pt of allergic rhinitis have bronchial asthma 60 -80% pt of asthma also have allergic rhinitis Prevention of allergen exposure is best treatment
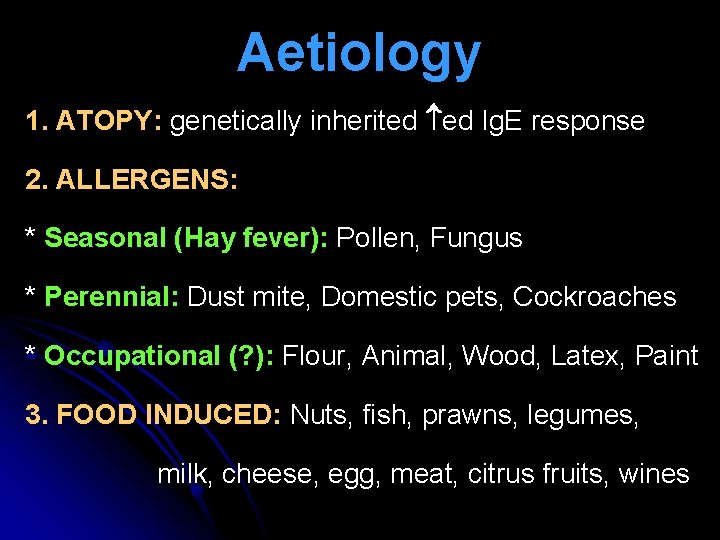
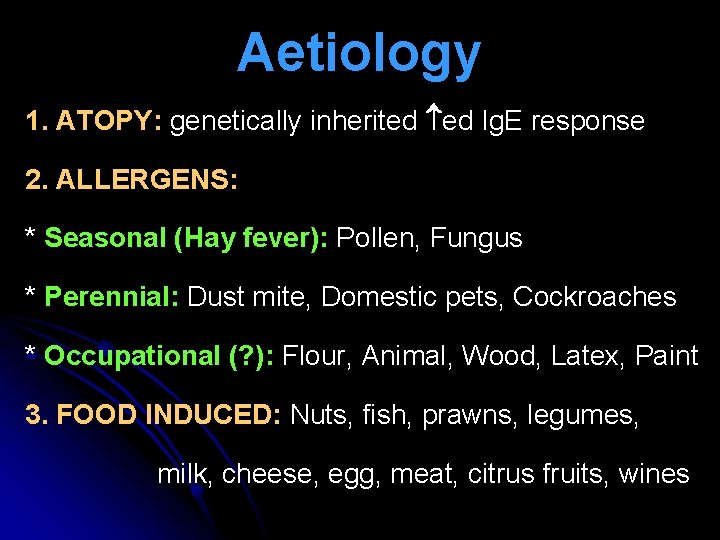
Aetiology 1. ATOPY: genetically inherited ed Ig. E response 2. ALLERGENS: * Seasonal (Hay fever): Pollen, Fungus * Perennial: Dust mite, Domestic pets, Cockroaches * Occupational (? ): Flour, Animal, Wood, Latex, Paint 3. FOOD INDUCED: Nuts, fish, prawns, legumes, milk, cheese, egg, meat, citrus fruits, wines
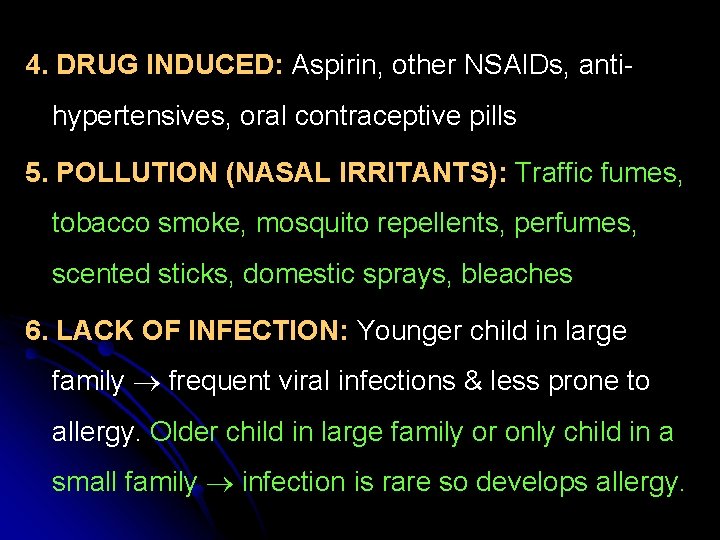
4. DRUG INDUCED: Aspirin, other NSAIDs, antihypertensives, oral contraceptive pills 5. POLLUTION (NASAL IRRITANTS): Traffic fumes, tobacco smoke, mosquito repellents, perfumes, scented sticks, domestic sprays, bleaches 6. LACK OF INFECTION: Younger child in large family frequent viral infections & less prone to allergy. Older child in large family or only child in a small family infection is rare so develops allergy.

Grass pollen & dust mite
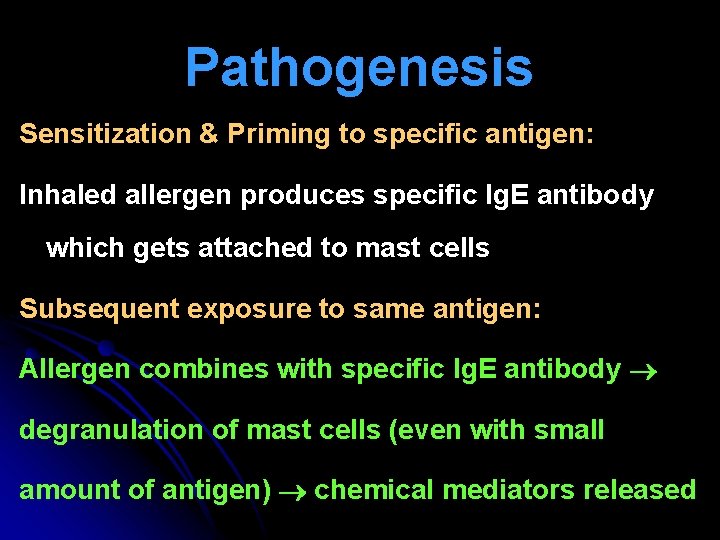
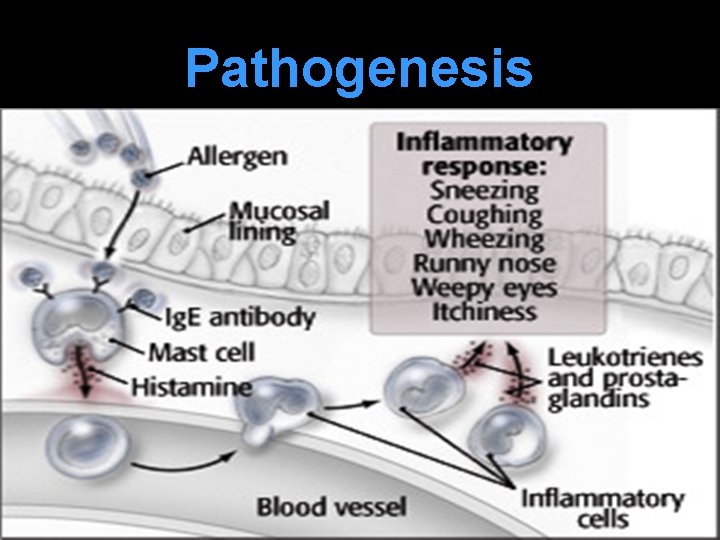
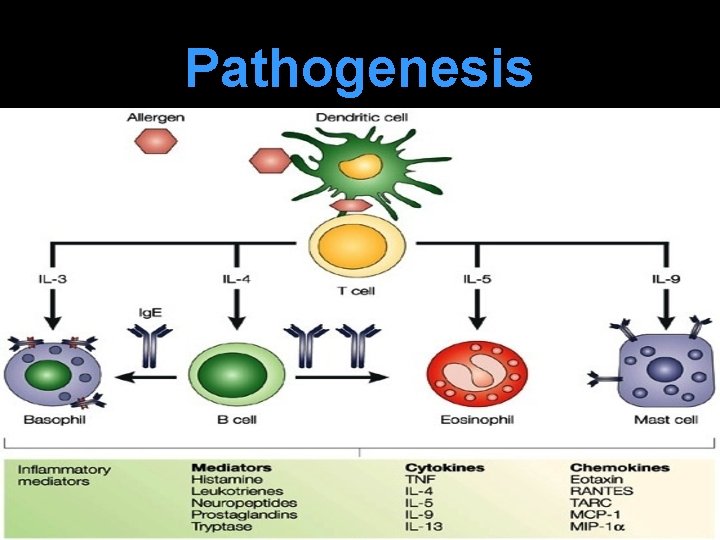
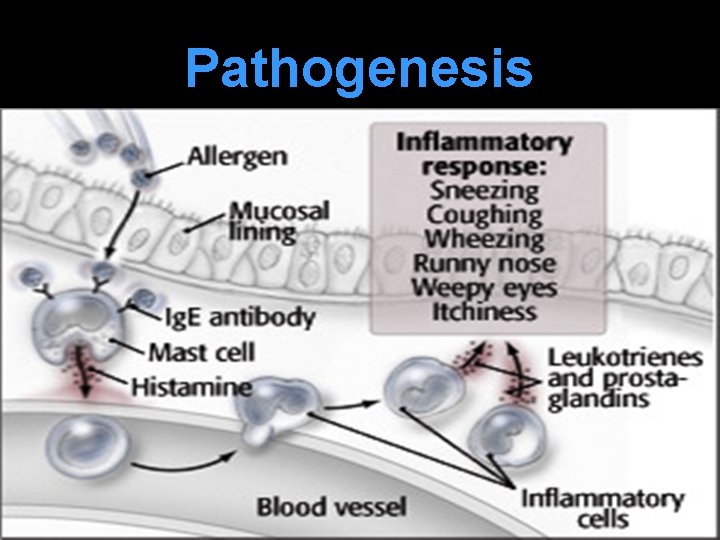
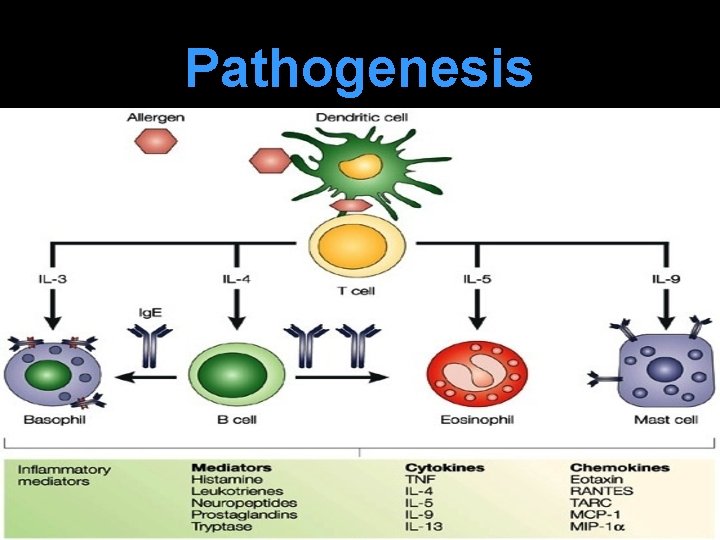
Pathogenesis Sensitization & Priming to specific antigen: Inhaled allergen produces specific Ig. E antibody which gets attached to mast cells Subsequent exposure to same antigen: Allergen combines with specific Ig. E antibody degranulation of mast cells (even with small amount of antigen) chemical mediators released
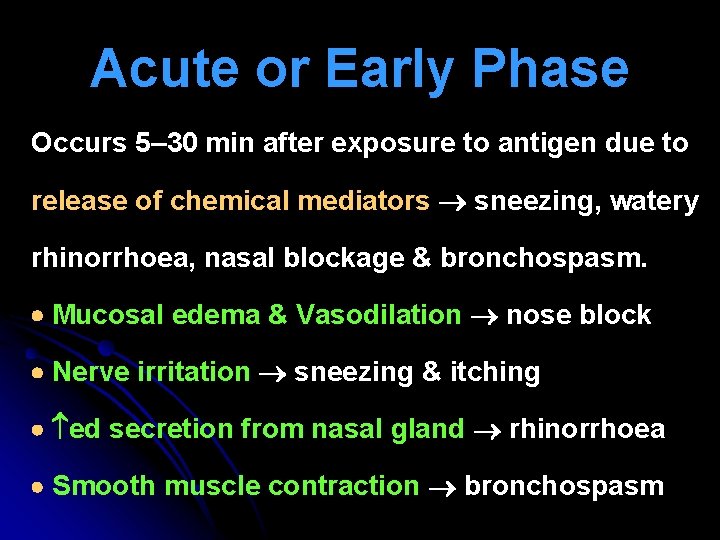
Acute or Early Phase Occurs 5– 30 min after exposure to antigen due to release of chemical mediators sneezing, watery rhinorrhoea, nasal blockage & bronchospasm. Mucosal edema & Vasodilation nose block Nerve irritation sneezing & itching ed secretion from nasal gland rhinorrhoea Smooth muscle contraction bronchospasm
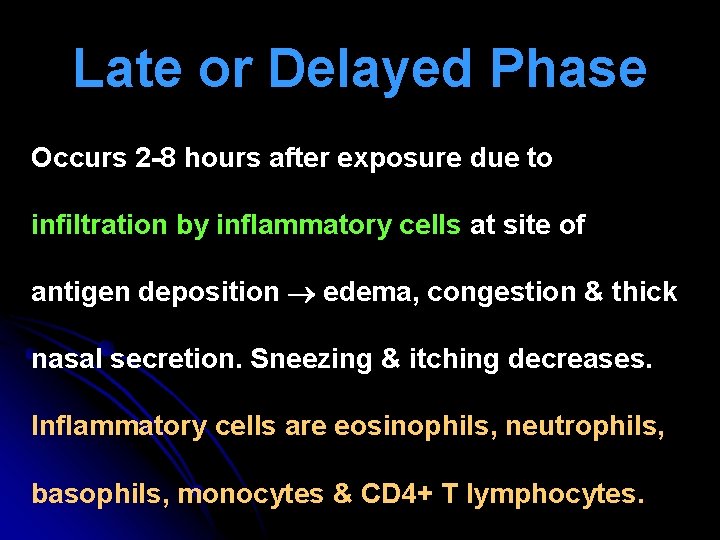
Late or Delayed Phase Occurs 2 -8 hours after exposure due to infiltration by inflammatory cells at site of antigen deposition edema, congestion & thick nasal secretion. Sneezing & itching decreases. Inflammatory cells are eosinophils, neutrophils, basophils, monocytes & CD 4+ T lymphocytes.
Pathogenesis
Pathogenesis
Cardinal Symptoms 1. Watery rhinorrhoea 2. Nasal obstruction: bilateral 3. Paroxysmal sneezing: 10 -20 at a time 4. Itching in nose, eyes, palate, pharynx Presence of 2 or more symptoms for > 1 hour on most days indicates allergic rhinitis.
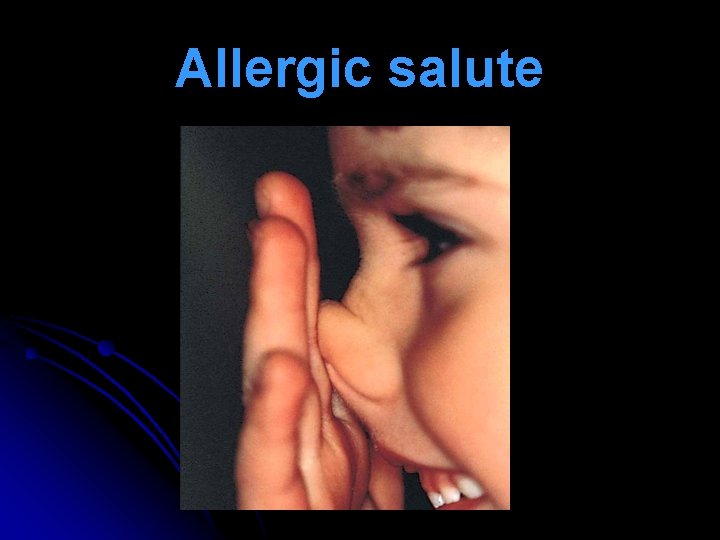
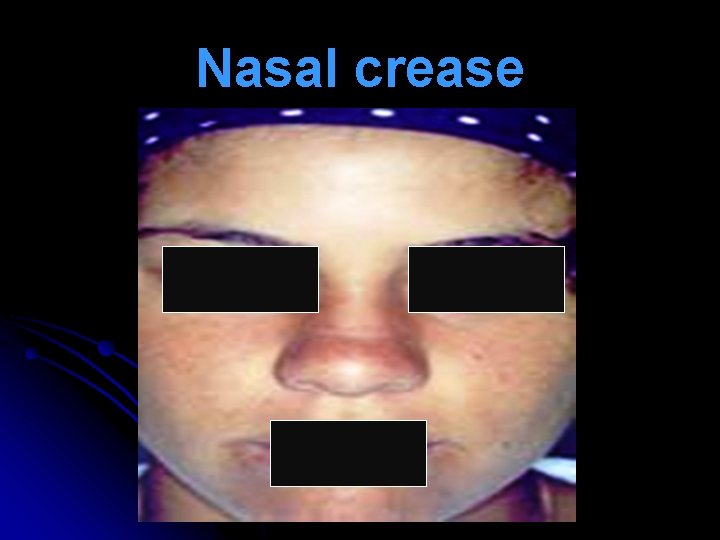
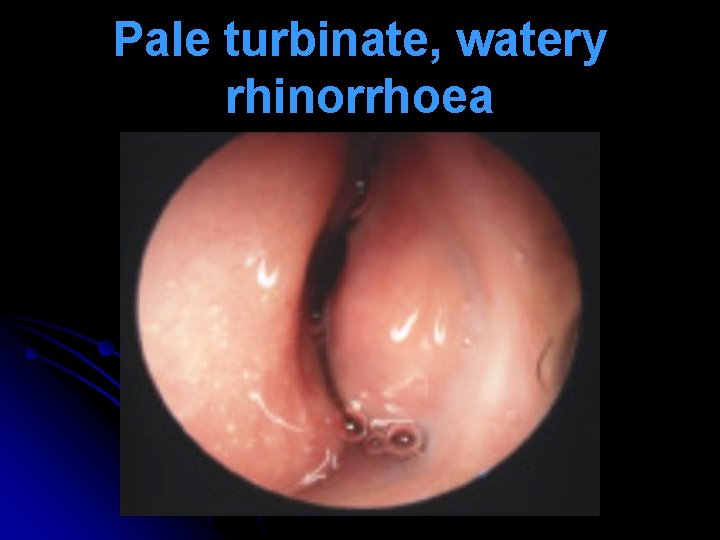
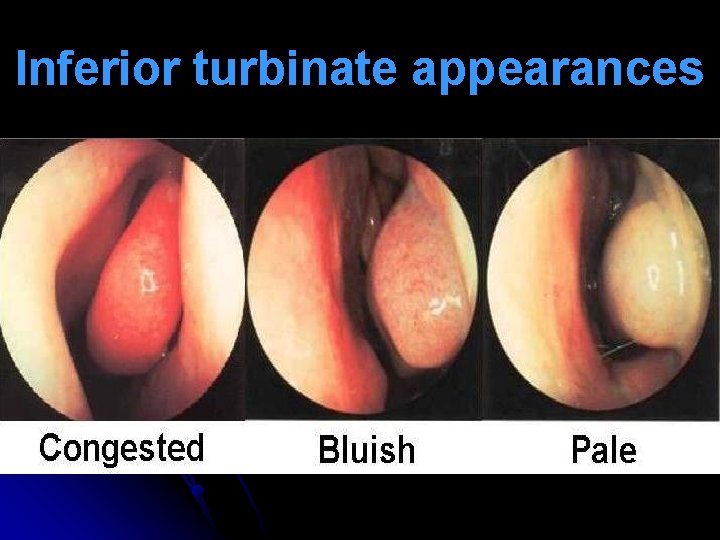
Nasal Signs l Repeated lifting of nasal tip (allergic salute) to relieve itching & open nasal airway transverse nasal crease (Darrier’s crease, Hilton’s line). l Hypertrophied turbinates are covered with pale or blue, boggy mucosa. Pitting edema seen on probing (mulberry turbinates). l Nasal secretions are watery mucoid. l Nasal polyps with hyposmia / anosmia.
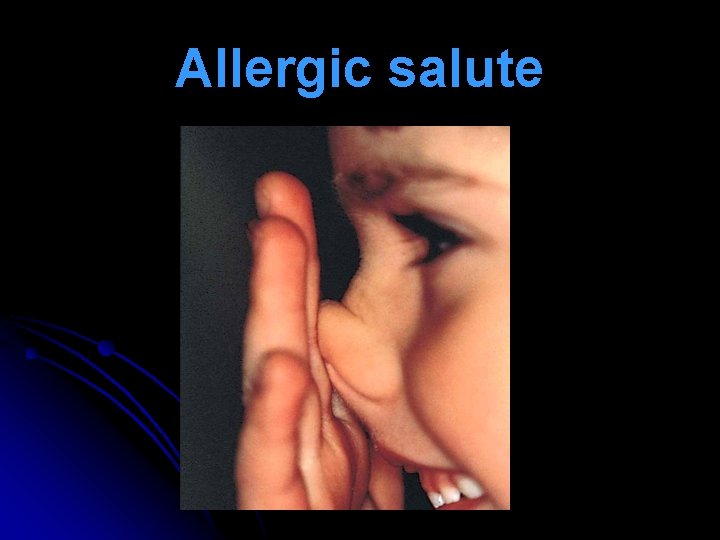
Allergic salute
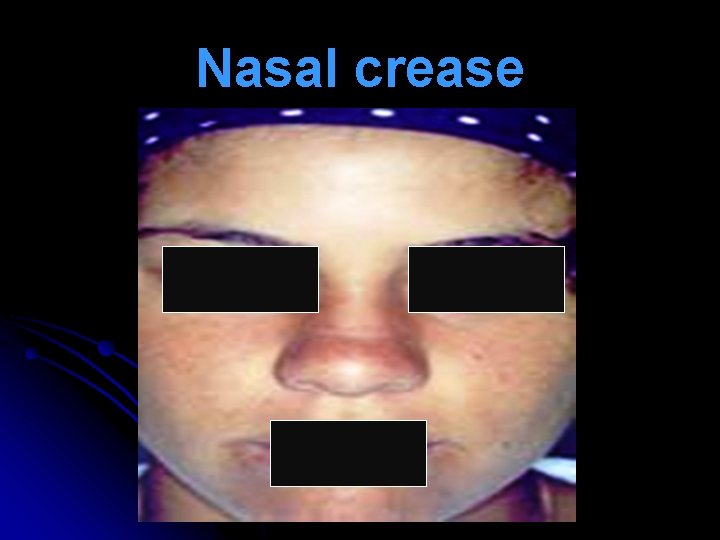
Nasal crease
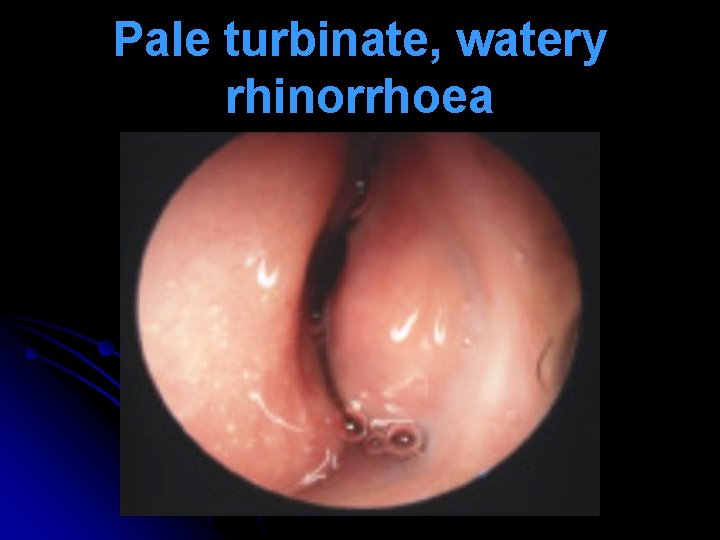
Pale turbinate, watery rhinorrhoea

Blue, boggy turbinate
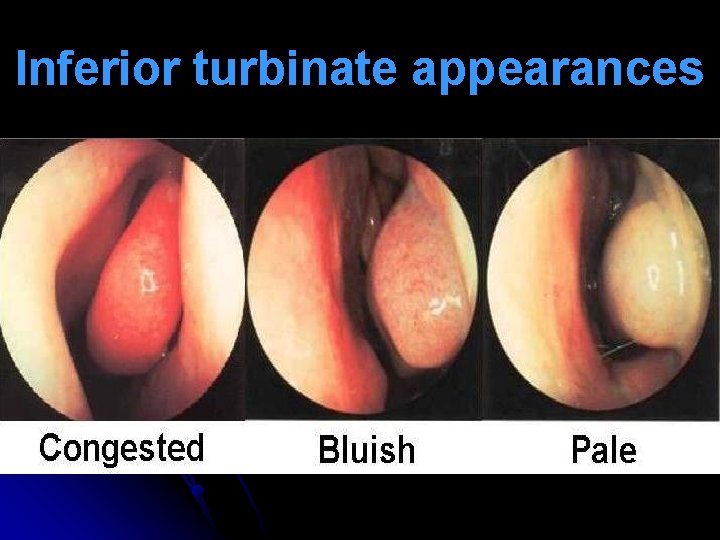
Inferior turbinate appearances
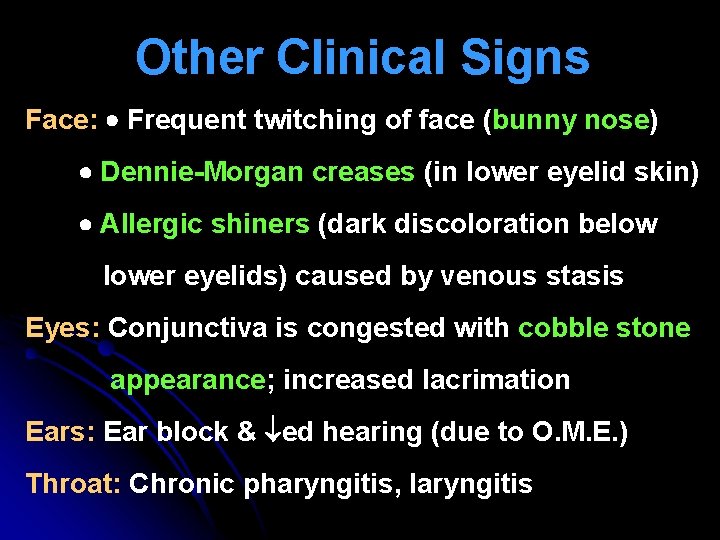
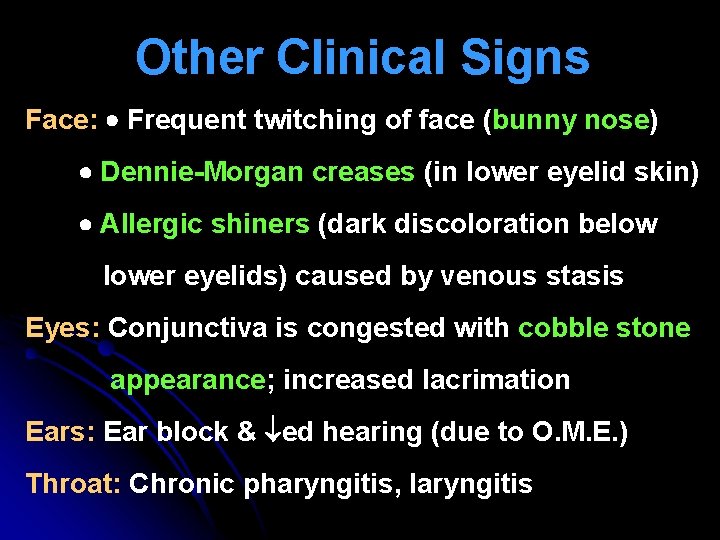
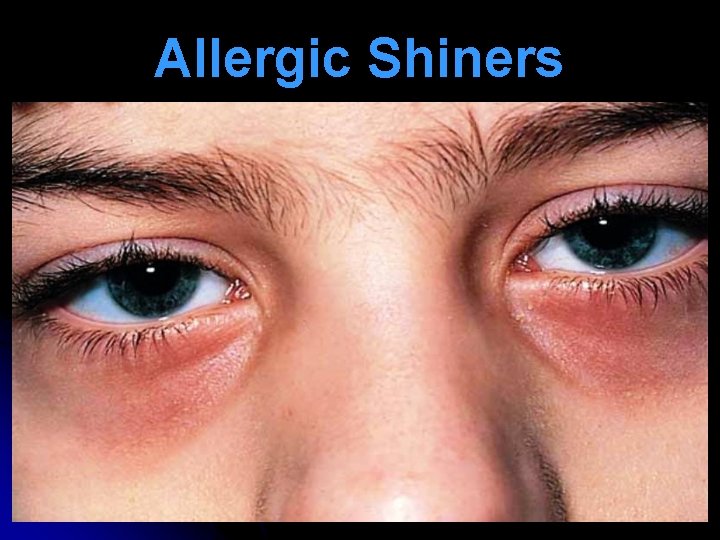
Other Clinical Signs Face: Frequent twitching of face (bunny nose) Dennie-Morgan creases (in lower eyelid skin) Allergic shiners (dark discoloration below lower eyelids) caused by venous stasis Eyes: Conjunctiva is congested with cobble stone appearance; increased lacrimation Ears: Ear block & ed hearing (due to O. M. E. ) Throat: Chronic pharyngitis, laryngitis

Dennie-Morgan Creases
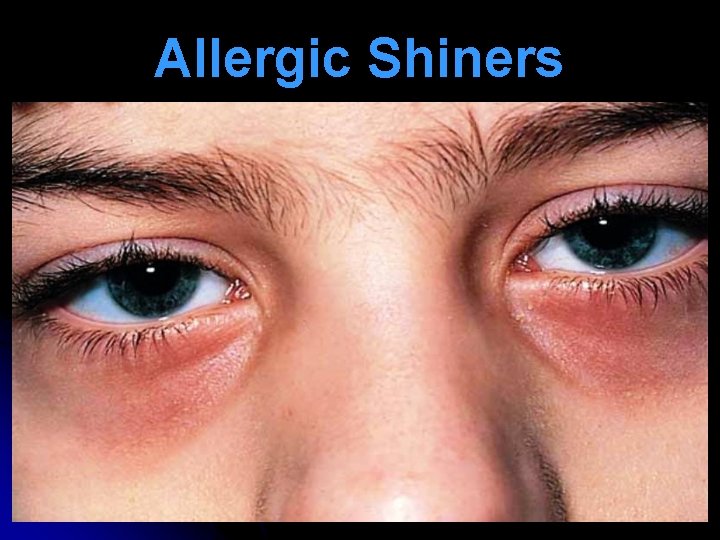
Allergic Shiners

Allergic conjunctivitis
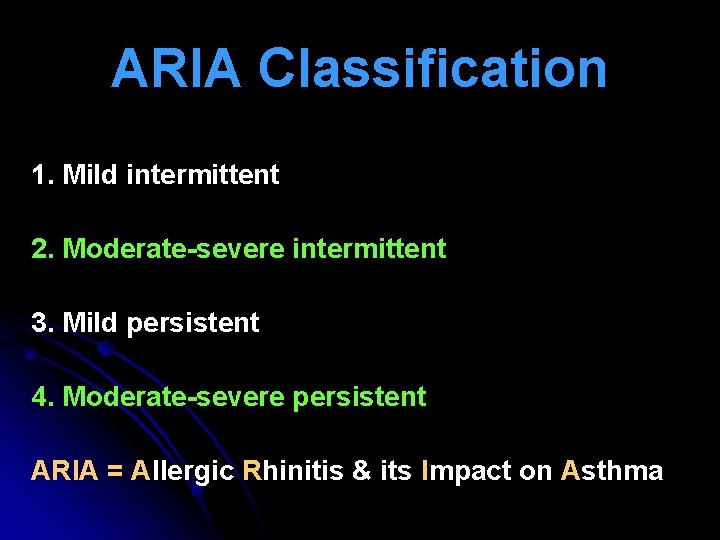
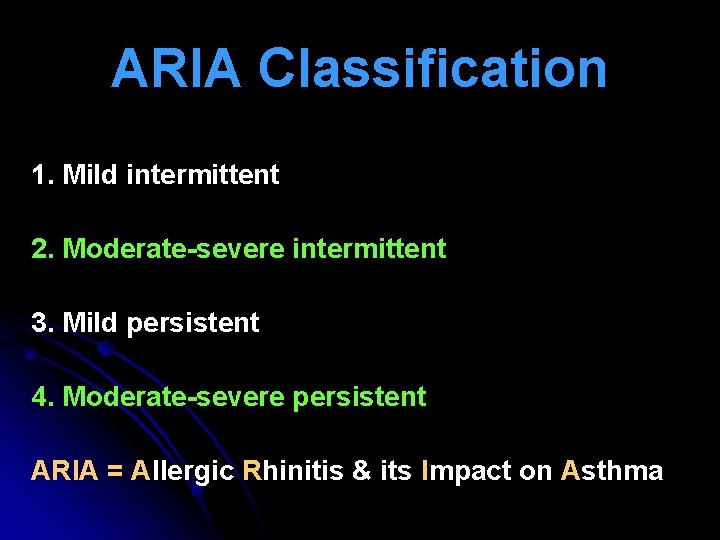
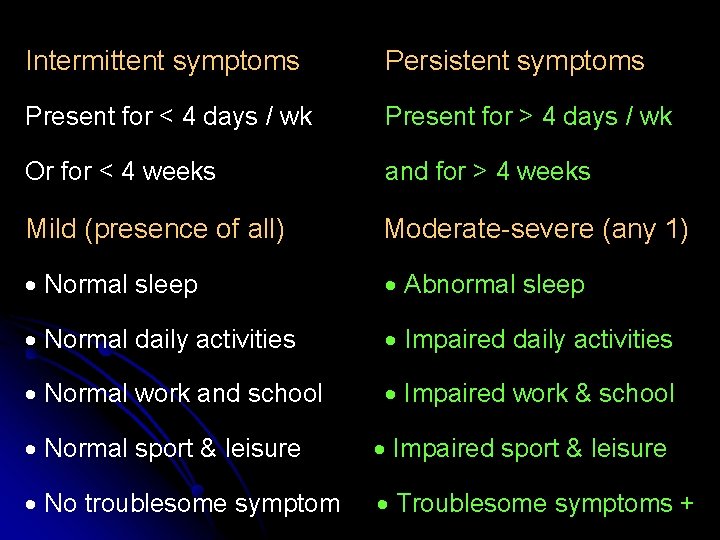
ARIA Classification 1. Mild intermittent 2. Moderate-severe intermittent 3. Mild persistent 4. Moderate-severe persistent ARIA = Allergic Rhinitis & its Impact on Asthma
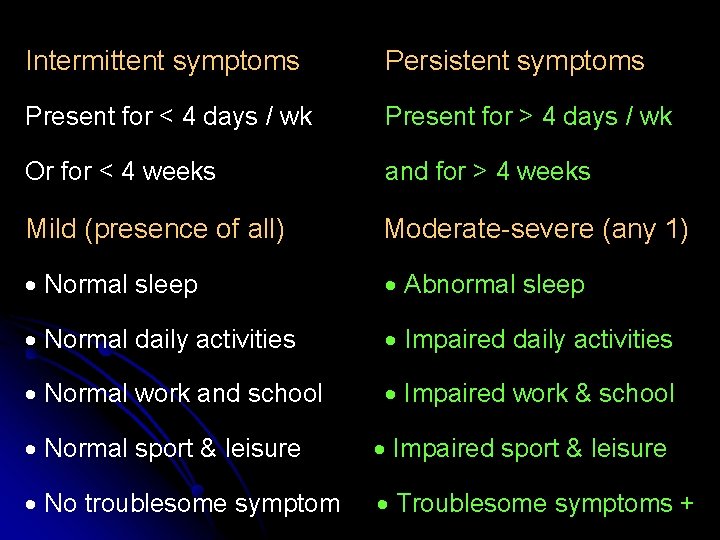
Intermittent symptoms Persistent symptoms Present for < 4 days / wk Present for > 4 days / wk Or for < 4 weeks and for > 4 weeks Mild (presence of all) Moderate-severe (any 1) Normal sleep Abnormal sleep Normal daily activities Impaired daily activities Normal work and school Impaired work & school Normal sport & leisure Impaired sport & leisure No troublesome symptom Troublesome symptoms +
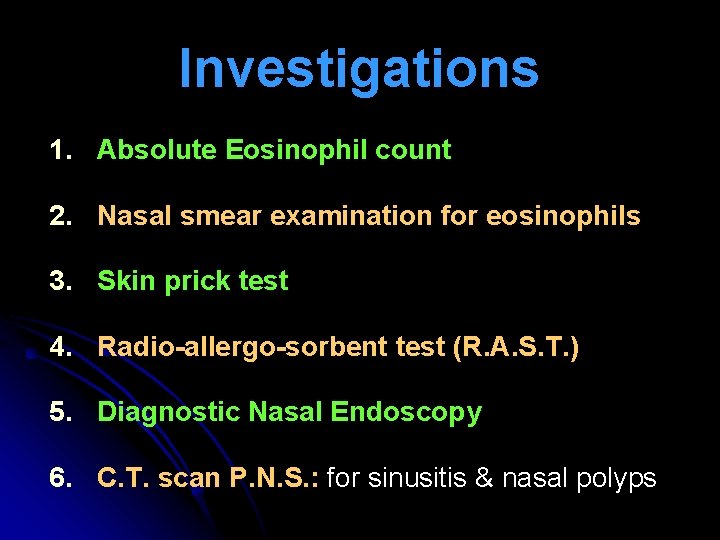
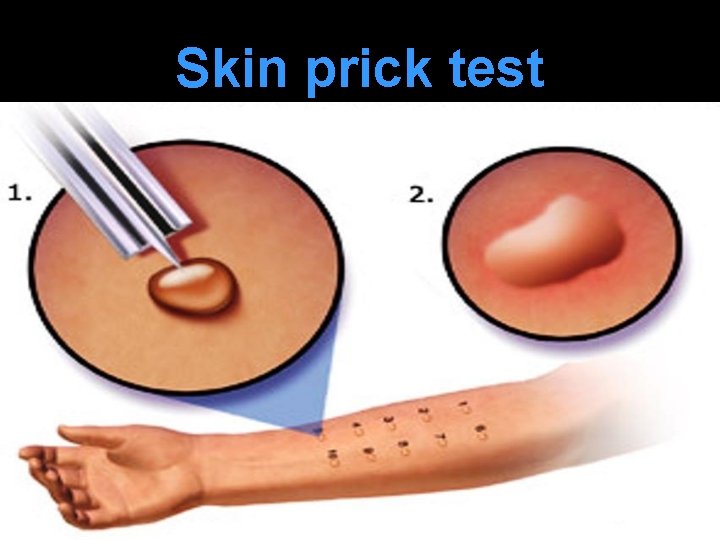
Investigations 1. Absolute Eosinophil count 2. Nasal smear examination for eosinophils 3. Skin prick test 4. Radio-allergo-sorbent test (R. A. S. T. ) 5. Diagnostic Nasal Endoscopy 6. C. T. scan P. N. S. : for sinusitis & nasal polyps
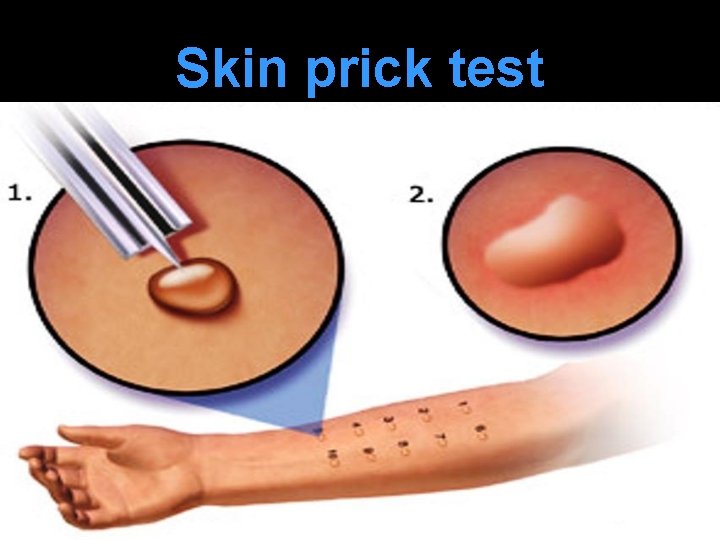
Skin prick test

Skin prick test

Skin prick test
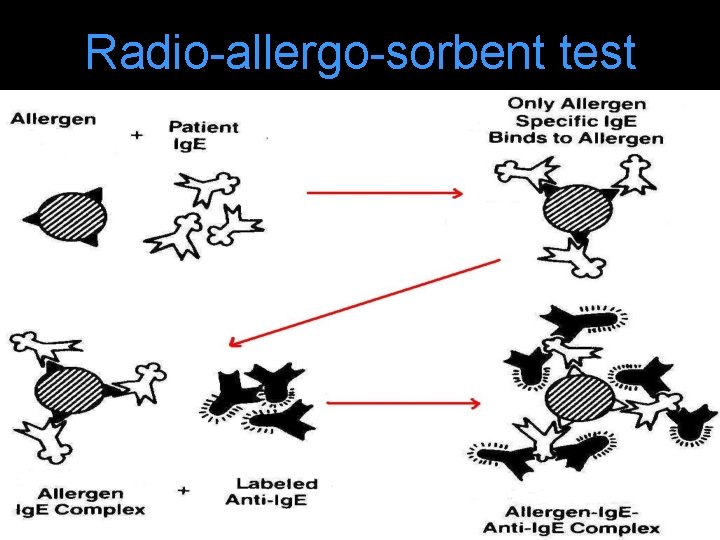
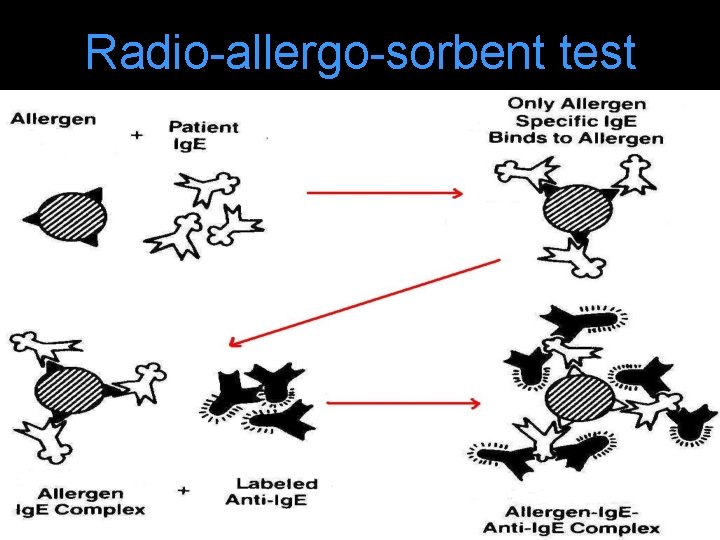
Radio-allergo-sorbent test
l Pt serum is incubated with allergen disc. Only specific Ig. E binds with allergen. Rest is washed away with a buffer. l Disc is incubated with radio-labeled anti - Ig. E antibody. Anti-Ig. E antibody binds with allergen. Ig. E complex. l Amount of radio-labelled anti-Ig. E antibody on disc amount of Ig. E & is quantified by counting radioactivity from the disc.
Complications 1. Recurrent sinusitis 2. Nasal polyp 3. Serous otitis media 4. Prolonged mouth breathing 5. Bronchial asthma 6. Atopic dermatitis 7. Conjunctivitis
Differential diagnosis l Vasomotor rhinitis l Rhinitis medicamentosa l Hormonal rhinitis (pregnancy, hypothyroidism, oral contraceptive use) l Cerebrospinal fluid leak l Ethmoid polyps
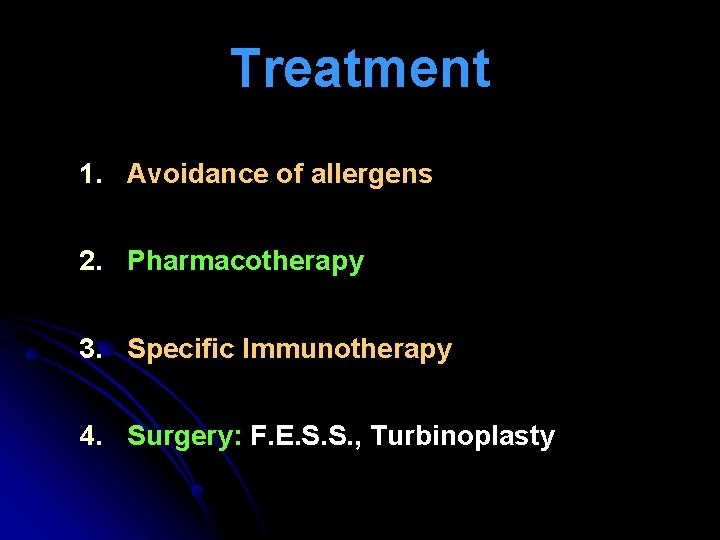
Treatment 1. Avoidance of allergens 2. Pharmacotherapy 3. Specific Immunotherapy 4. Surgery: F. E. S. S. , Turbinoplasty
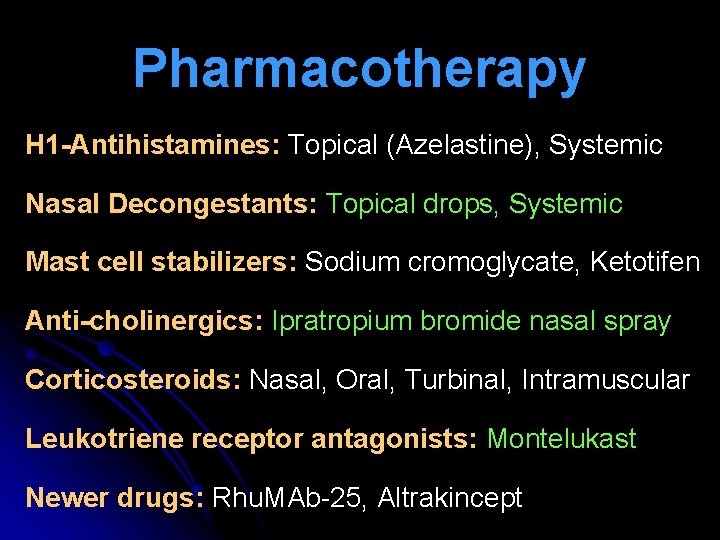
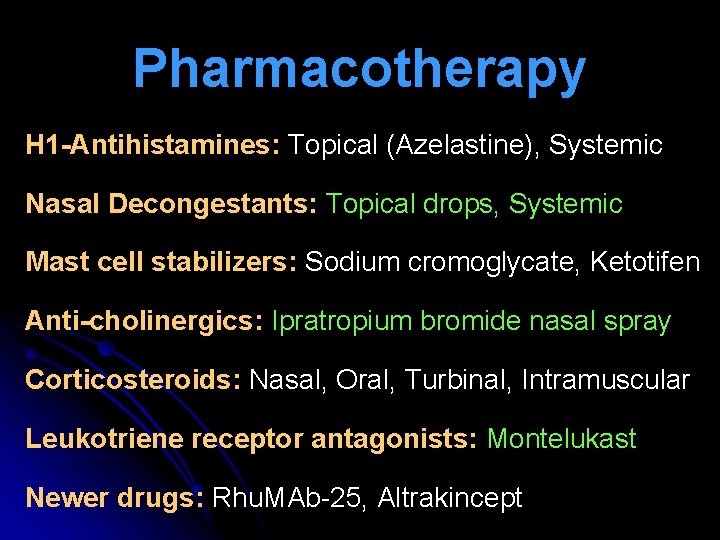
Pharmacotherapy H 1 -Antihistamines: Topical (Azelastine), Systemic Nasal Decongestants: Topical drops, Systemic Mast cell stabilizers: Sodium cromoglycate, Ketotifen Anti-cholinergics: Ipratropium bromide nasal spray Corticosteroids: Nasal, Oral, Turbinal, Intramuscular Leukotriene receptor antagonists: Montelukast Newer drugs: Rhu. MAb-25, Altrakincept
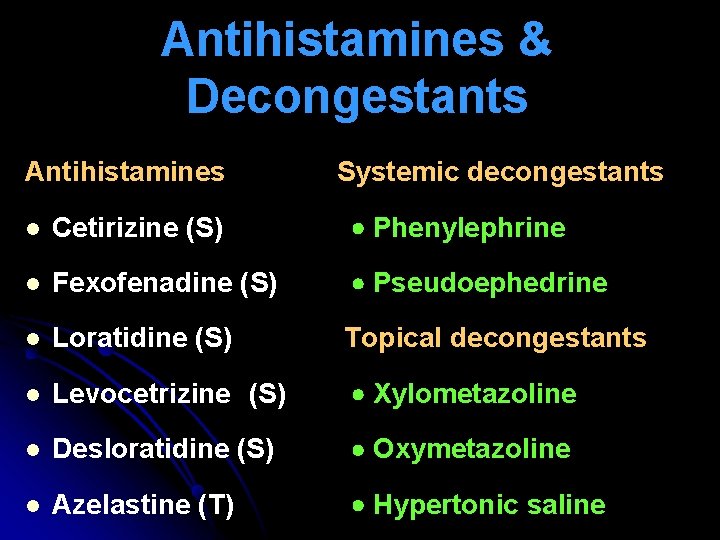
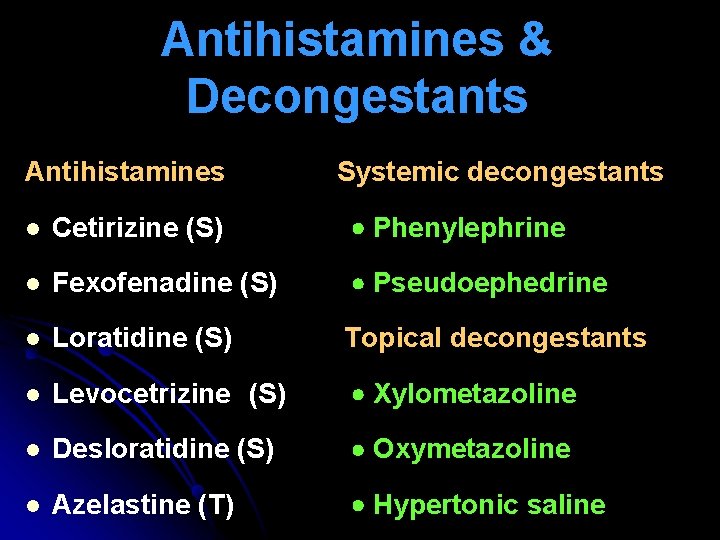
Antihistamines & Decongestants Antihistamines Systemic decongestants l Cetirizine (S) Phenylephrine l Fexofenadine (S) Pseudoephedrine l Loratidine (S) Topical decongestants l Levocetrizine (S) Xylometazoline l Desloratidine (S) Oxymetazoline l Azelastine (T) Hypertonic saline
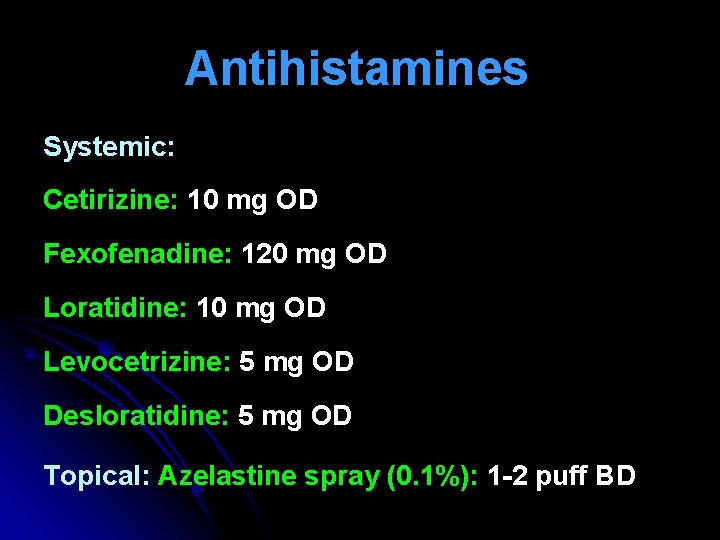
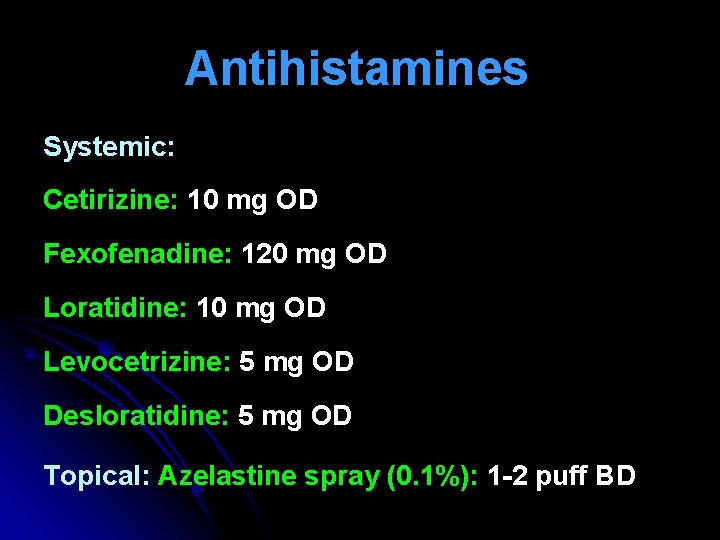
Antihistamines Systemic: Cetirizine: 10 mg OD Fexofenadine: 120 mg OD Loratidine: 10 mg OD Levocetrizine: 5 mg OD Desloratidine: 5 mg OD Topical: Azelastine spray (0. 1%): 1 -2 puff BD

Nasal Decongestants Systemic decongestants Phenylephrine Pseudoephedrine Topical decongestants Xylometazoline Oxymetazoline Saline
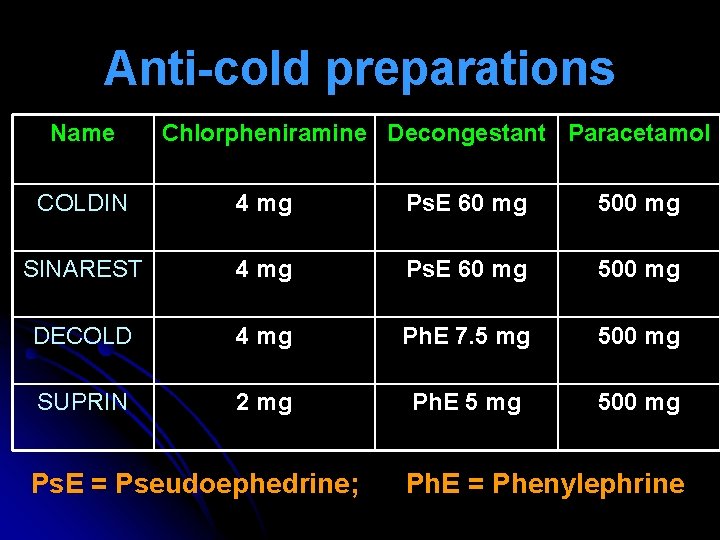
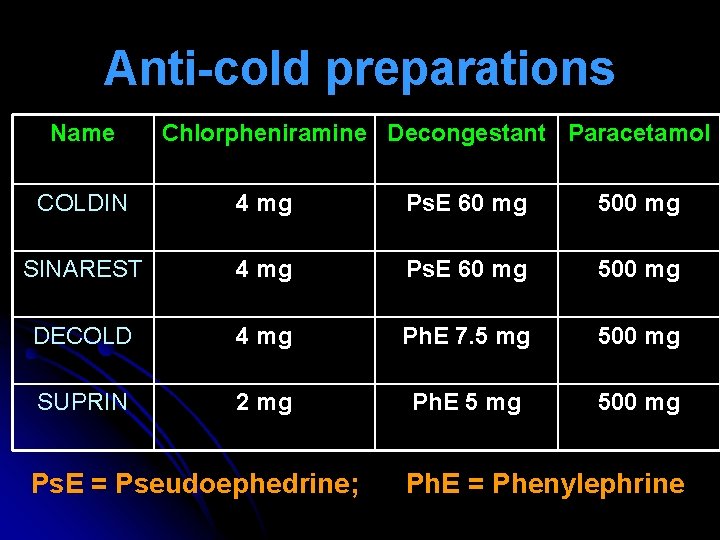
Anti-cold preparations Name Chlorpheniramine Decongestant Paracetamol COLDIN 4 mg Ps. E 60 mg 500 mg SINAREST 4 mg Ps. E 60 mg 500 mg DECOLD 4 mg Ph. E 7. 5 mg 500 mg SUPRIN 2 mg Ph. E 5 mg 500 mg Ps. E = Pseudoephedrine; Ph. E = Phenylephrine
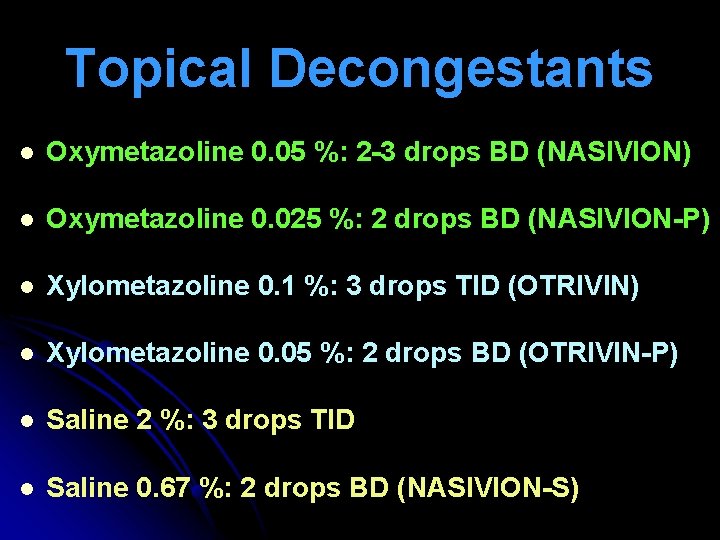
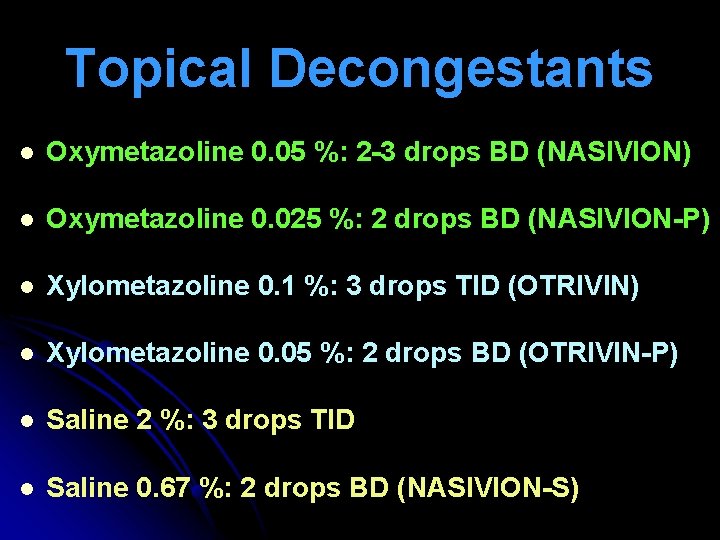
Topical Decongestants l Oxymetazoline 0. 05 %: 2 -3 drops BD (NASIVION) l Oxymetazoline 0. 025 %: 2 drops BD (NASIVION-P) l Xylometazoline 0. 1 %: 3 drops TID (OTRIVIN) l Xylometazoline 0. 05 %: 2 drops BD (OTRIVIN-P) l Saline 2 %: 3 drops TID l Saline 0. 67 %: 2 drops BD (NASIVION-S)

Systemic Antihistamines

Topical Antihistamine spray
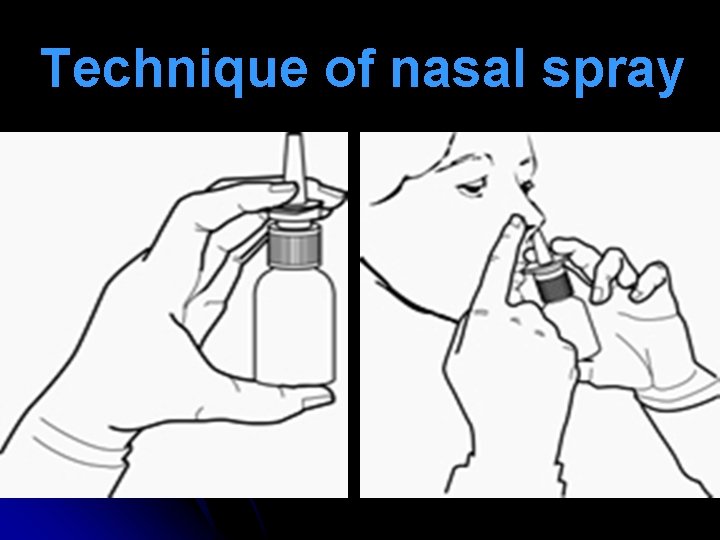
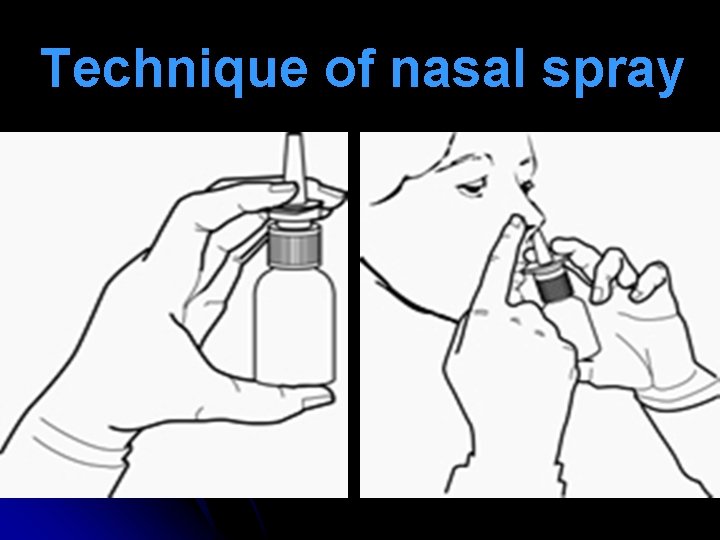
Technique of nasal spray

Nasal Decongestants
Sodium Cromoglycate

Ipratropium nasal spray
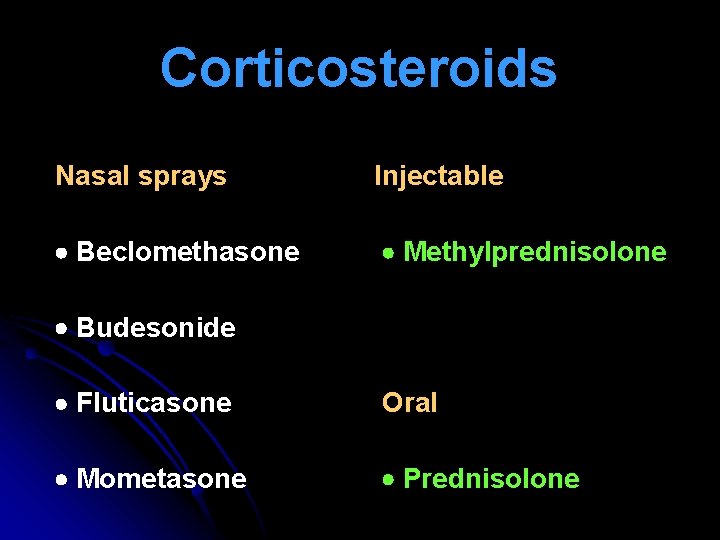
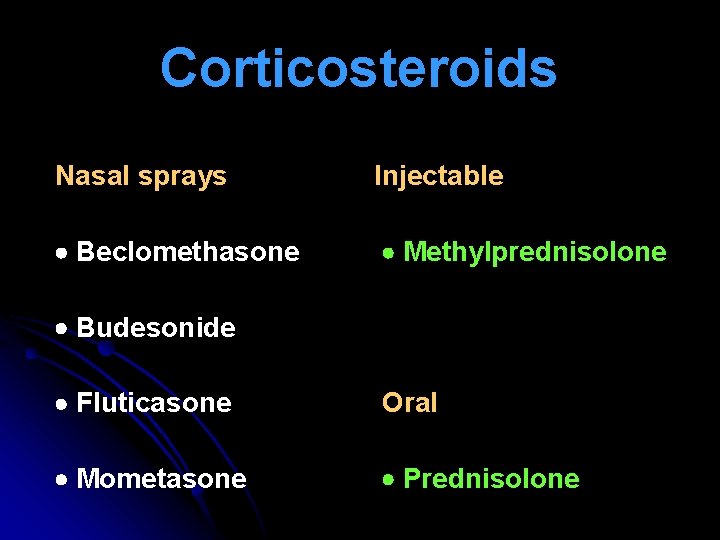
Corticosteroids Nasal sprays Injectable Beclomethasone Methylprednisolone Budesonide Fluticasone Oral Mometasone Prednisolone

Corticosteroid nasal spray
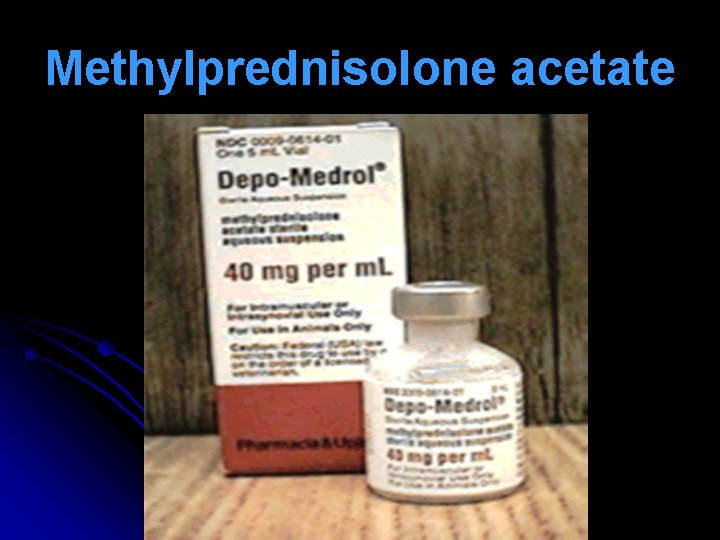
Methylprednisolone acetate
Montelukast
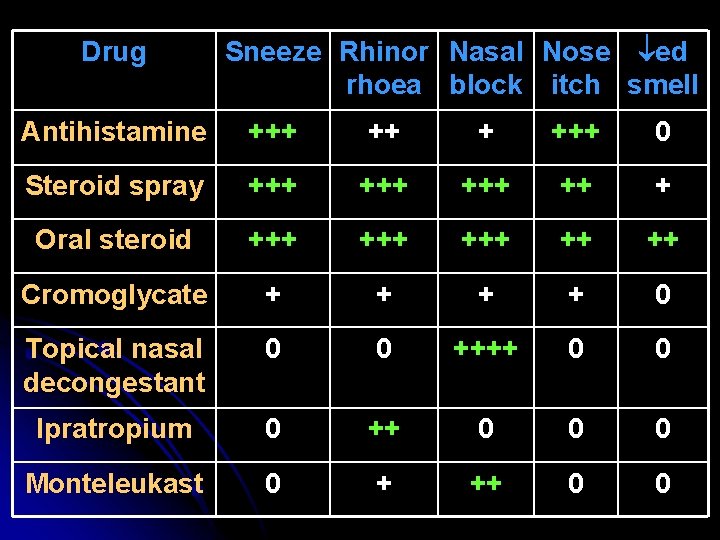
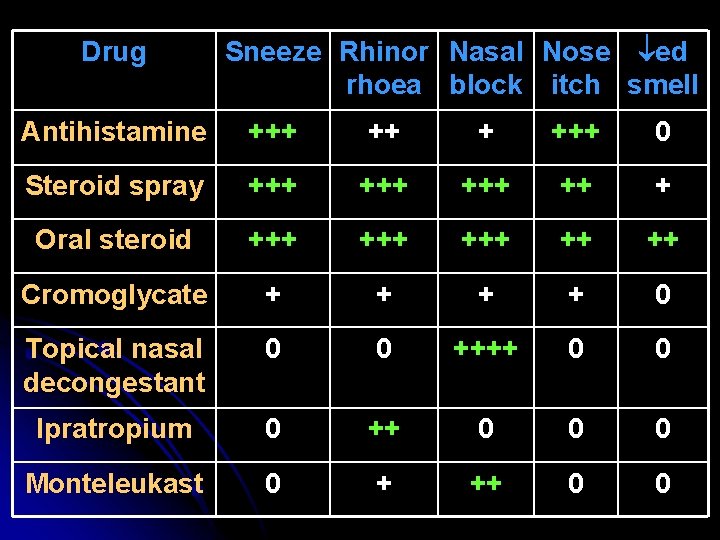
Drug Sneeze Rhinor Nasal Nose ed rhoea block itch smell Antihistamine +++ +++ 0 Steroid spray +++ +++ ++ + Oral steroid +++ +++ ++ ++ Cromoglycate + + 0 Topical nasal decongestant 0 0 ++++ 0 0 Ipratropium 0 ++ 0 0 0 Monteleukast 0 + ++ 0 0
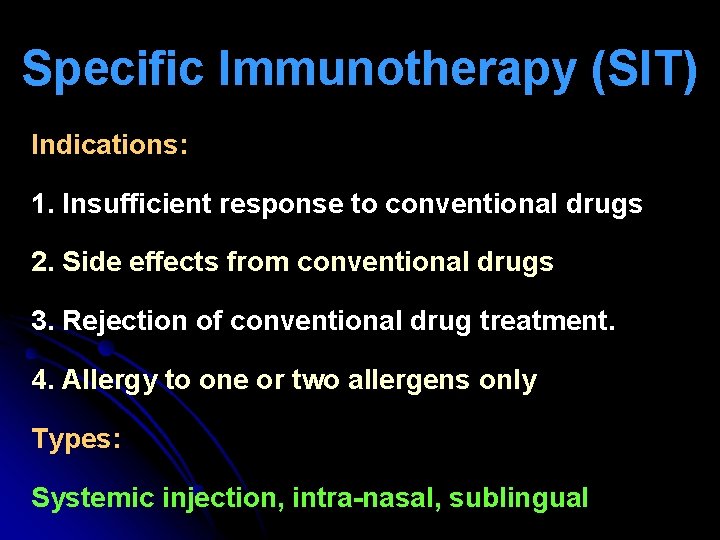
Specific Immunotherapy (SIT) Indications: 1. Insufficient response to conventional drugs 2. Side effects from conventional drugs 3. Rejection of conventional drug treatment. 4. Allergy to one or two allergens only Types: Systemic injection, intra-nasal, sublingual
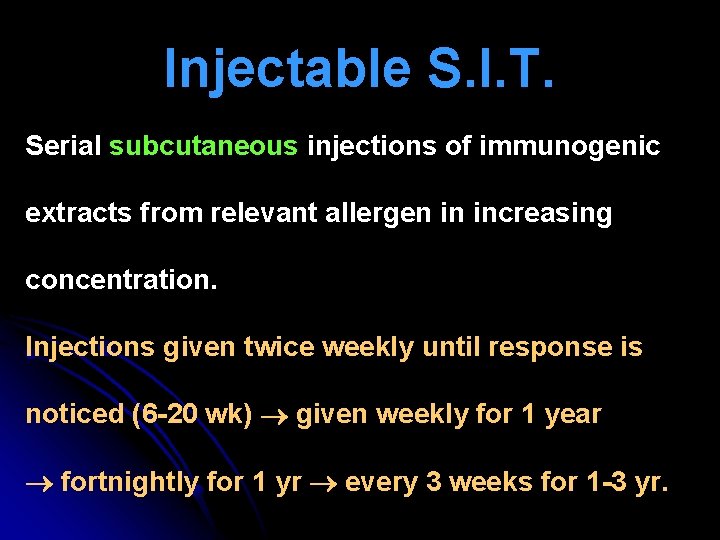
Injectable S. I. T. Serial subcutaneous injections of immunogenic extracts from relevant allergen in increasing concentration. Injections given twice weekly until response is noticed (6 -20 wk) given weekly for 1 year fortnightly for 1 yr every 3 weeks for 1 -3 yr.

Injectable S. I. T.
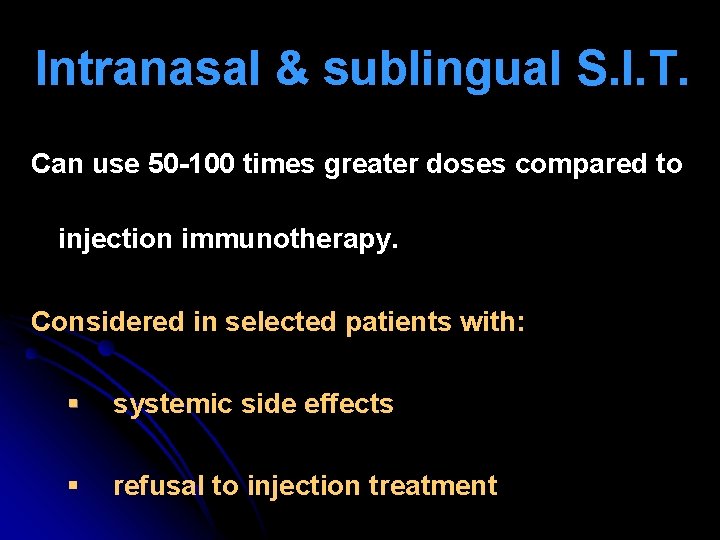
Intranasal & sublingual S. I. T. Can use 50 -100 times greater doses compared to injection immunotherapy. Considered in selected patients with: § systemic side effects § refusal to injection treatment
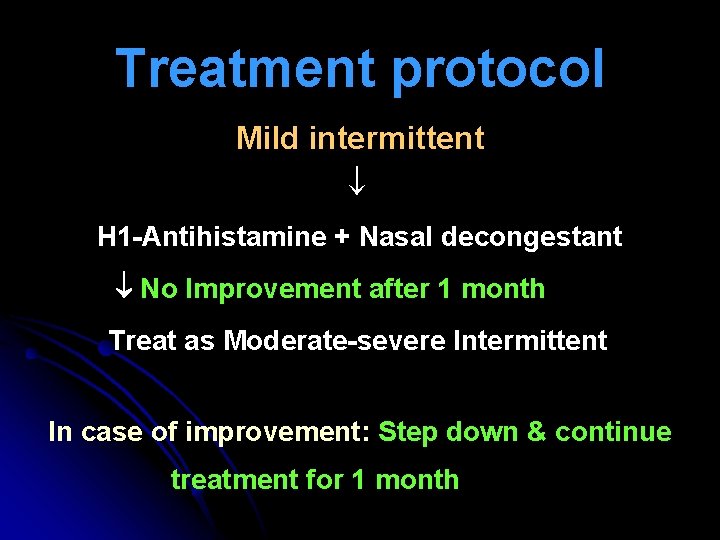
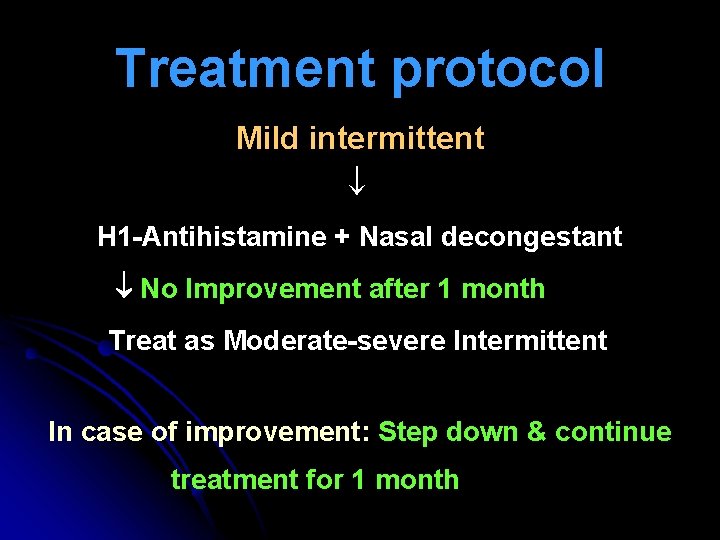
Treatment protocol Mild intermittent H 1 -Antihistamine + Nasal decongestant No Improvement after 1 month Treat as Moderate-severe Intermittent In case of improvement: Step down & continue treatment for 1 month
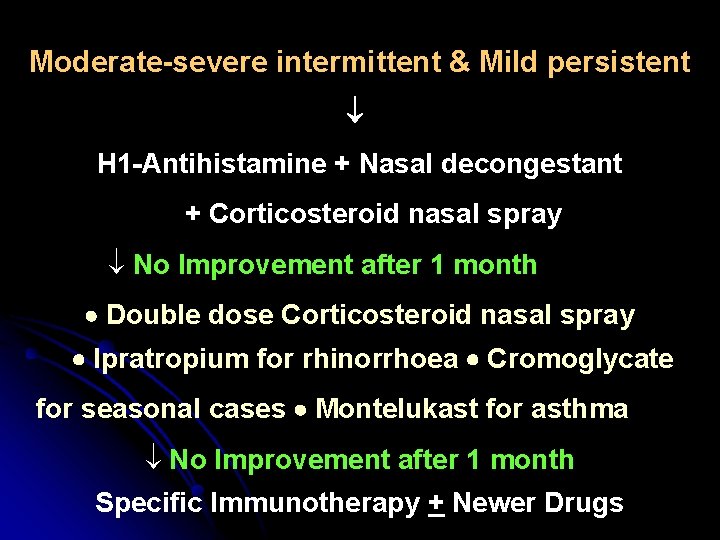
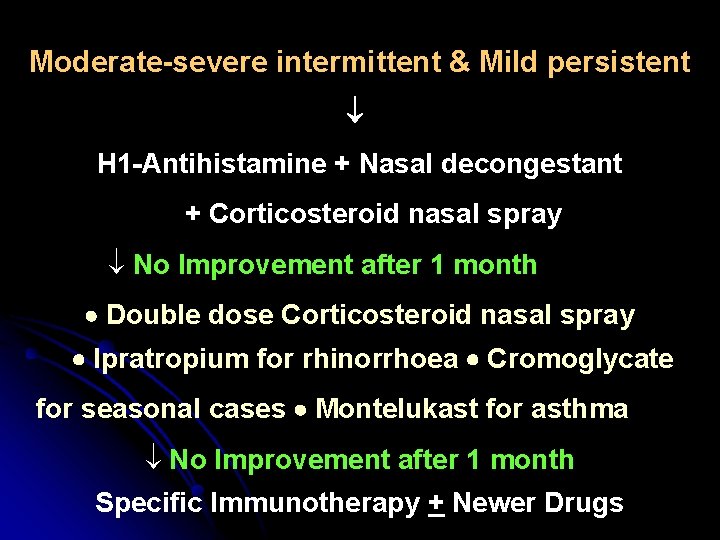
Moderate-severe intermittent & Mild persistent H 1 -Antihistamine + Nasal decongestant + Corticosteroid nasal spray No Improvement after 1 month Double dose Corticosteroid nasal spray Ipratropium for rhinorrhoea Cromoglycate for seasonal cases Montelukast for asthma No Improvement after 1 month Specific Immunotherapy + Newer Drugs
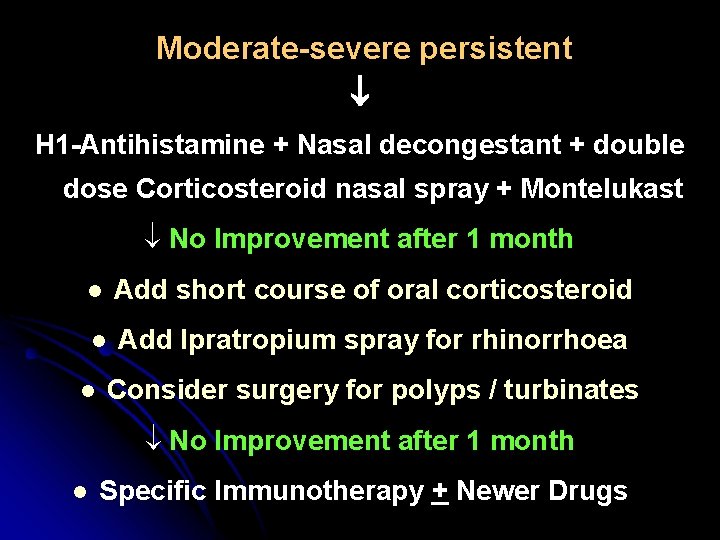
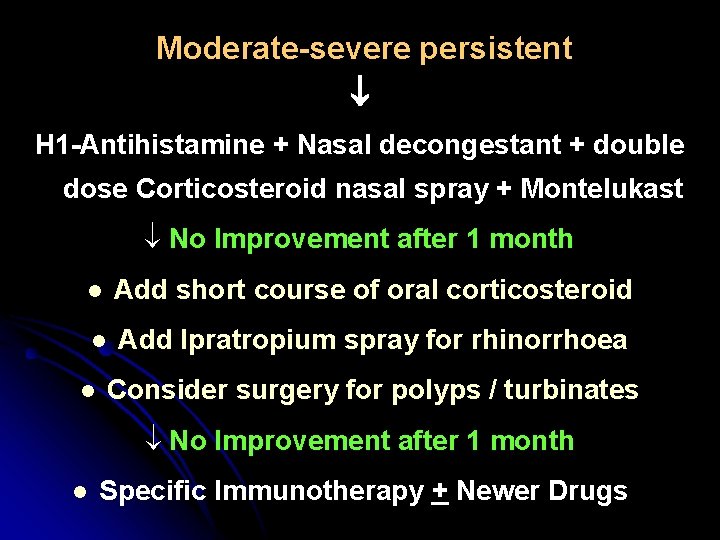
Moderate-severe persistent H 1 -Antihistamine + Nasal decongestant + double dose Corticosteroid nasal spray + Montelukast No Improvement after 1 month l Add short course of oral corticosteroid l Add Ipratropium spray for rhinorrhoea l Consider surgery for polyps / turbinates No Improvement after 1 month l Specific Immunotherapy + Newer Drugs
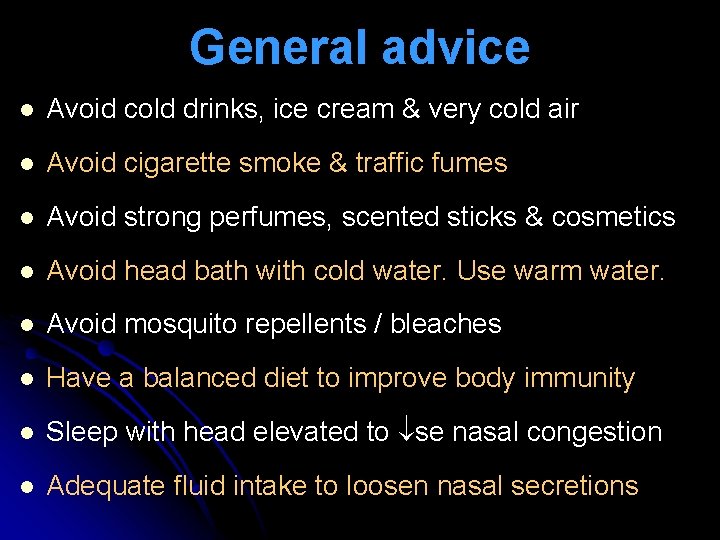
General advice l Avoid cold drinks, ice cream & very cold air l Avoid cigarette smoke & traffic fumes l Avoid strong perfumes, scented sticks & cosmetics l Avoid head bath with cold water. Use warm water. l Avoid mosquito repellents / bleaches l Have a balanced diet to improve body immunity l Sleep with head elevated to se nasal congestion l Adequate fluid intake to loosen nasal secretions
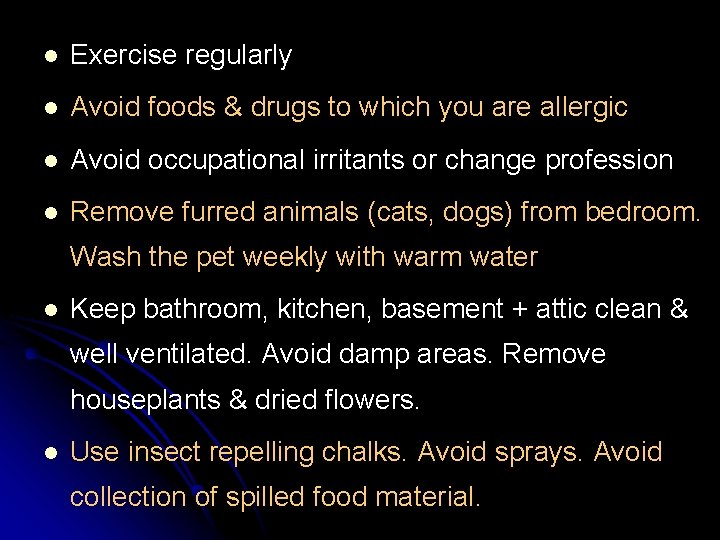
l Exercise regularly l Avoid foods & drugs to which you are allergic l Avoid occupational irritants or change profession l Remove furred animals (cats, dogs) from bedroom. Wash the pet weekly with warm water l Keep bathroom, kitchen, basement + attic clean & well ventilated. Avoid damp areas. Remove houseplants & dried flowers. l Use insect repelling chalks. Avoid sprays. Avoid collection of spilled food material.
Pollen advice l Avoid walking in open grassy spaces during hot, dry days. Move outdoors only on damp days. l Keep windows closed. Move flowering plants away from doors & windows. l Wear facemask & sunglasses when moving out. l Keep grass & plants trimmed. Get rid of weeds & leaves. l Plant less allergenic flowers & trees.
House dust mite advice l Use foam pillows & mattresses with dust-proof cover. l Remove carpets, upholstered furniture, stuffed toys, old newspapers & magazines. l Wash bedcovers & clothes in warm water. l Damp-wipe house regularly wearing a facemask. l Use vacuum cleaners with high-efficiency particle arresting (HEPA) filters weekly. l Use air-conditioning (with pollen filters) to maintain the humidity less than 50 %.

Thank You