Chapter 17 19 20 9 Drugs for Degenerative










- Slides: 99

Chapter 17, 19, 20, & 9 Drugs for Degenerative Diseases and Muscles Drugs for Pain
Chapter 17 Antiparkinson Drugs

Degenerative Diseases • Medication is unable to cure degenerative diseases of the CNS • Cause is usually unknown • Includes: • Parkinson’s disease • Alzheimer’s disease • Multiple sclerosis (MS) • Huntington’s disease • Amyotrophic lateral sclerosis (ALS)
Neurotransmitters of the Basal Ganglia • Acetylcholine (ACH) & Dopamine (DA): • DA is an inhibitory neurotransmitter. • DA inhibits muscle tone and activity. • Parkinson’s disease is caused by the destruction of the DA neurons: • Deficiency of dopamine disturbs the balance between ACH and DA. • Increased activity of ACH produces excessive motor nerve stimulation. 17 -4
Symptoms • Classic Triad • Tremors • Muscle rigidity • Bradykinesia • Postural instability

Parkinson’s • Symptoms develop due to destruction of dopamine producing neurons in brain • Brain depends on proper balance of dopamine (inhibitory) and acetylcholine (stimulatory) neurotransmitters • If dopamine is absent, acetylcholine is able to stimulate brain more
Pharmacotherapy • Drug therapy for Parkinson’s focuses on: • 1. restoring dopamine function • Dopaminergic Agents • Enzyme Inhibitors • Dopamine Receptor Agonists • 2. blocking effect of acetylcholine • Anticholinergics
Dopaminergic Agents • Used to increase dopamine levels in brain • Drug of choice for Parkinson’s is levodopa • MOA: Precursor of (an agent that stimulates) dopamine synthesis • Levodopa can cross blood-brain barrier; dopamine cannot • Effectiveness of levodopa can be boosted by combining it with carbidopa (marketed as Sinemet) • Carbidopa prevents metabolism of levodopa, making it more available to enter CNS (MOA) • Amino acids in food can interfere with levodopa transport across the barrier
Side Effects • Involuntary movements • Loss of appetite • N&V • Orthostatic hypotension • On-off phenomenon • Nursing Considerations: • Several drug interactions • **D/C gradually…abrupt withdrawal can produce acute Parkinsonism
Common Dopaminergic Agents • levodopa (Larodopa) • carbidopa-levodopa (Sinemet) • amantadine hydrochloride (Symmetrel) • Useful only in early stages • Believed to increase neuronal release of DA and decrease reuptake of DA • Adverse effects—dry mouth, dizziness, and confusion
Anticholinergics • How do they work (MOA)? • What about side effects? • NC: Not as effective as levodopa • Used early when symptoms not severe, in pts who cannot tolerate levodopa, and in combo therapy
Common Anticholinergics • benztropine mesylate (Cogentin) • MOA: Block ACH and decrease cholinergic activity • Adverse effects —dry mouth, constipation, and urinary retention
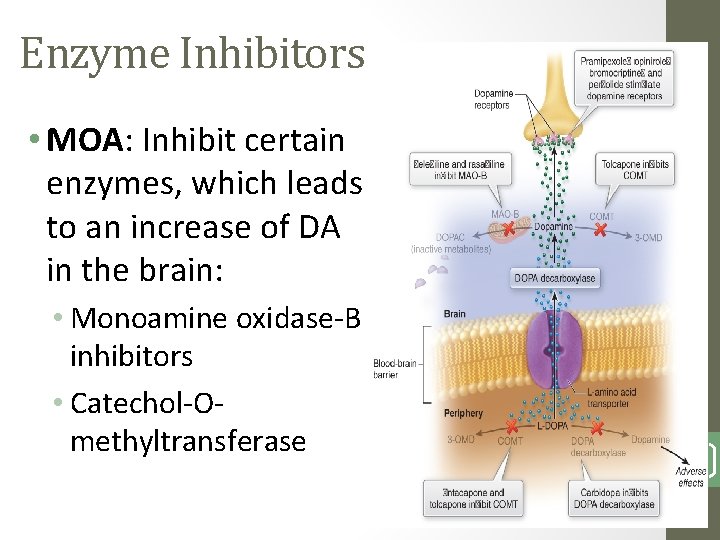
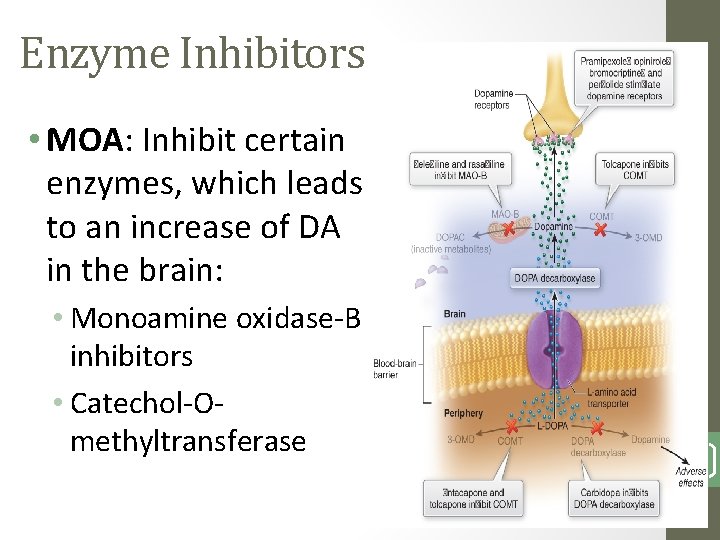
Enzyme Inhibitors • MOA: Inhibit certain enzymes, which leads to an increase of DA in the brain: • Monoamine oxidase-B inhibitors • Catechol-Omethyltransferase 1714
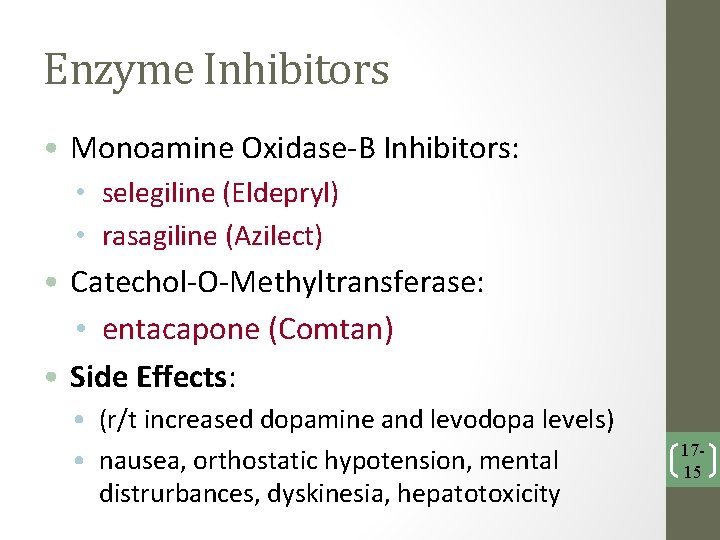
Enzyme Inhibitors • Monoamine Oxidase-B Inhibitors: • selegiline (Eldepryl) • rasagiline (Azilect) • Catechol-O-Methyltransferase: • entacapone (Comtan) • Side Effects: • (r/t increased dopamine and levodopa levels) • nausea, orthostatic hypotension, mental distrurbances, dyskinesia, hepatotoxicity 1715
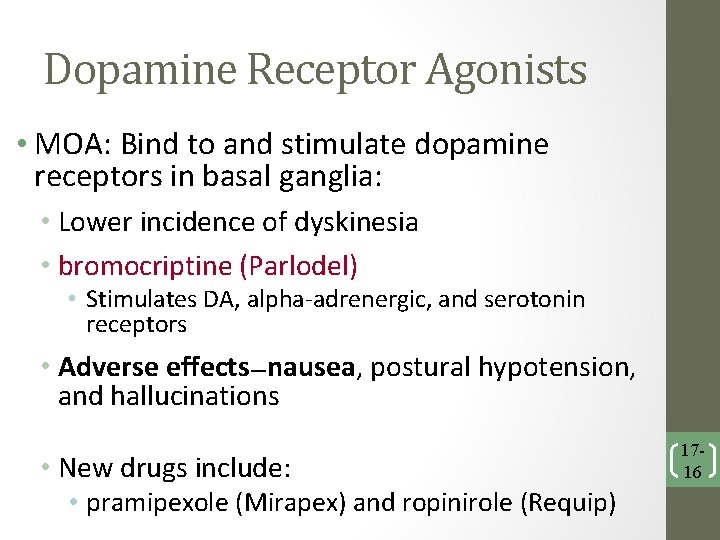
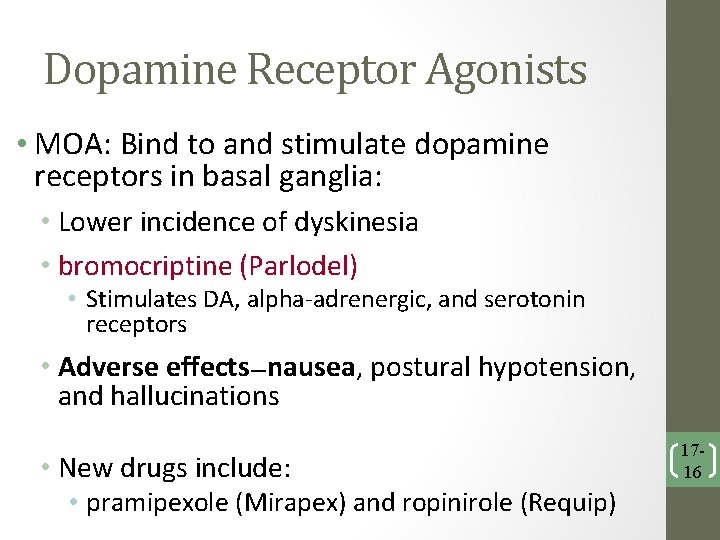
Dopamine Receptor Agonists • MOA: Bind to and stimulate dopamine receptors in basal ganglia: • Lower incidence of dyskinesia • bromocriptine (Parlodel) • Stimulates DA, alpha-adrenergic, and serotonin receptors • Adverse effects—nausea, postural hypotension, and hallucinations • New drugs include: • pramipexole (Mirapex) and ropinirole (Requip) 1716

Preferred Therapy for Parkinson’s • Treatment of Tremors: • Amantadine or anticholinergic drugs • Treatment of Mild-Moderate Disease: • Dopamine receptor agonist • Levodopa/carbidopa • Enzyme inhibitors • Treatment of Advanced Disease: • Levodopa/carbidopa • Enzyme inhibitors • Dopamine receptor agonist 1717
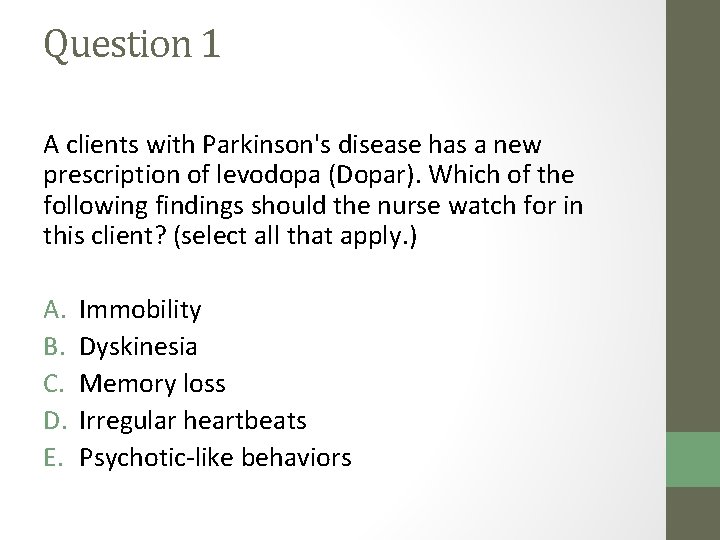
Question 1 A clients with Parkinson's disease has a new prescription of levodopa (Dopar). Which of the following findings should the nurse watch for in this client? (select all that apply. ) A. B. C. D. E. Immobility Dyskinesia Memory loss Irregular heartbeats Psychotic-like behaviors
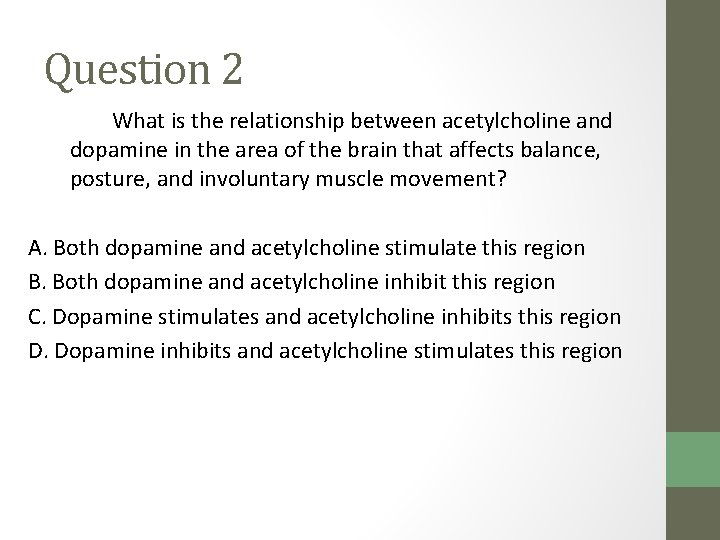
Question 2 What is the relationship between acetylcholine and dopamine in the area of the brain that affects balance, posture, and involuntary muscle movement? A. Both dopamine and acetylcholine stimulate this region B. Both dopamine and acetylcholine inhibit this region C. Dopamine stimulates and acetylcholine inhibits this region D. Dopamine inhibits and acetylcholine stimulates this region
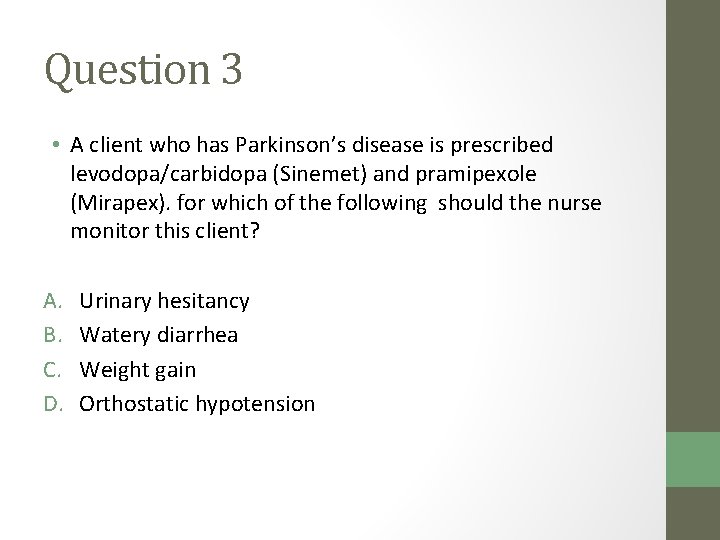
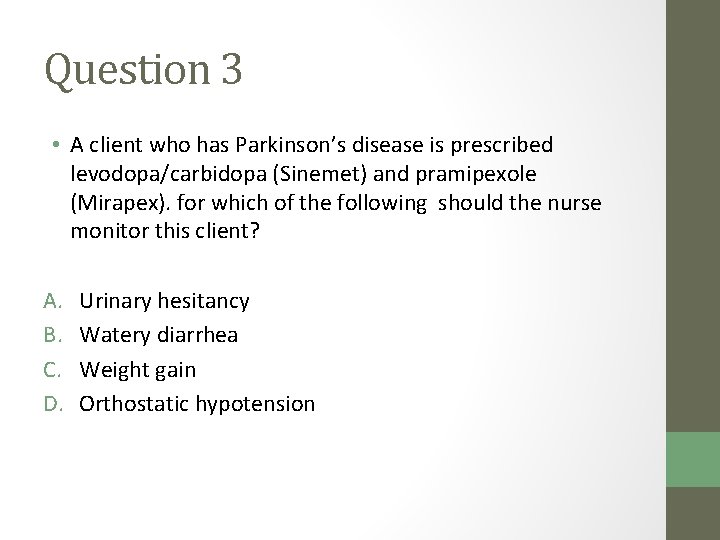
Question 3 • A client who has Parkinson’s disease is prescribed levodopa/carbidopa (Sinemet) and pramipexole (Mirapex). for which of the following should the nurse monitor this client? A. B. C. D. Urinary hesitancy Watery diarrhea Weight gain Orthostatic hypotension
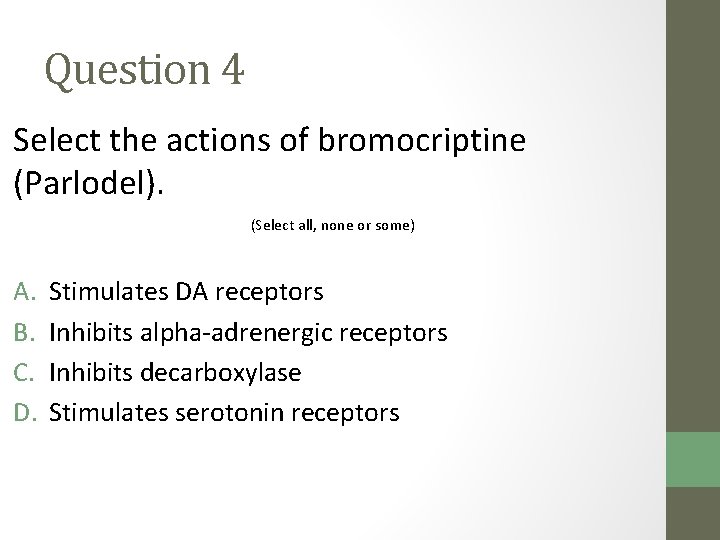
Question 4 Select the actions of bromocriptine (Parlodel). (Select all, none or some) A. B. C. D. Stimulates DA receptors Inhibits alpha-adrenergic receptors Inhibits decarboxylase Stimulates serotonin receptors
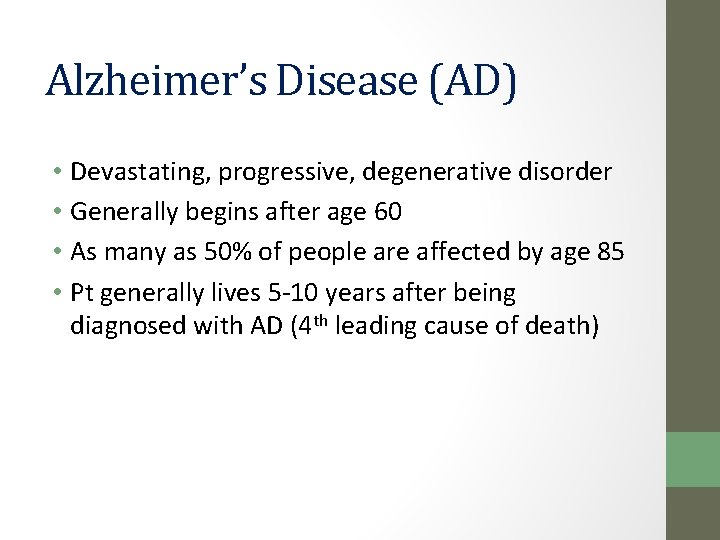
Alzheimer’s Disease (AD) • Devastating, progressive, degenerative disorder • Generally begins after age 60 • As many as 50% of people are affected by age 85 • Pt generally lives 5 -10 years after being diagnosed with AD (4 th leading cause of death)
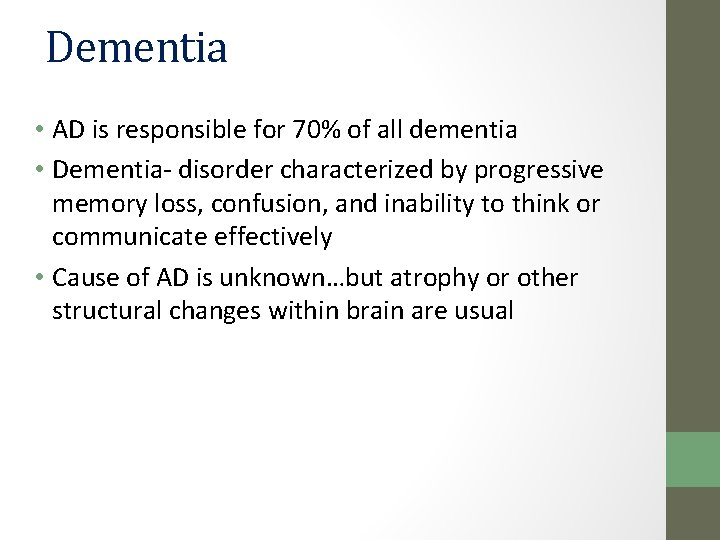
Dementia • AD is responsible for 70% of all dementia • Dementia- disorder characterized by progressive memory loss, confusion, and inability to think or communicate effectively • Cause of AD is unknown…but atrophy or other structural changes within brain are usual
Alzheimer’s and Acetylcholine � Acetylcholine is major neurotransmitter within hippocampus (area of brain responsible for learning and memory) and other parts of cerebral cortex � AD pts experience a dramatic loss of ability to perform tasks that require acetylcholine › Impaired memory and judgment › Confusion or disorientation › Inability to recognize family and friends › Aggressive behavior › Depression › Psychoses › Anxiety
Pharmacotherapy Continued • Most widely treated with acetylcholineresterase inhibitors • What is acetylcholineresterase? • What happens when acetylcholineresterase is inhibited?
Acetylcholineresterase inhibitors • Acetylcholine is naturally degraded in the synapse by the enzyme acetylcholineresterase • MOA: When acetylcholineresterase is inhibited, acetylcholine levels increase and affect receptors –which brings about more rest and digest. • They are indirect acting cholinergic agents!
Side Effects • Those expected of drugs that enhance the parasympathetic NS • N, V, D • Fatigue • Increased libido • Urinary incontinence • Bradycardia
Common Acetylcholineresterase Inhibitors • Donepexil hydrochloride (Aricept) • Tacrine (Cognex) • Nursing Condsiderations: • D/C as disease progresses
Multiple Sclerosis (MS) � Autoimmune disorder of CNS � Antibodies target and slowly destroy tissues in brain and spinal cord � As tissues are damaged, inflammation of nervous tissue causes demyelination (loss of myelin) � Loss of myelin leaves multiple areas of hard scarred tissue called plaques along the covering of nerve cells � Axons are gradually destroyed, disrupting the ability of the nerves to conduct electrical impulses to and from brain
Pharmacotherapy • 2 basic strategies: • 1. attempt to reduce inflammation and prevent attacks on the nervous system • Immuno-modulators • Myelin Protein Builders • 2. relieve symptoms • Muscle Relaxants
Immunomodulators • Interferon beta- 1 a (Avonex, Rebif) • Interferon beta- 1 b (Betaseron) • MOA: Changes immunity (MS is autoimmune, so we want to stop the body from attacking itself) • Use: • Only clinically proven drugs for treating underlying causes of MS • SE • Flu-like symptoms • Pain at injection site • hepatotoxicity
Myelin protein builder • Glatiramer acetate (Copaxone) • MOA: • Synthetic protein that simulates myelin basic protein, as essential part of the nerve’s myelin coating • Since glatiramer acetate resembles myelin, it is thought to curb the body’s attack on the myelin covering and reduce the creation of new lesions • SE: discomfort at inj site; NC: monitor site
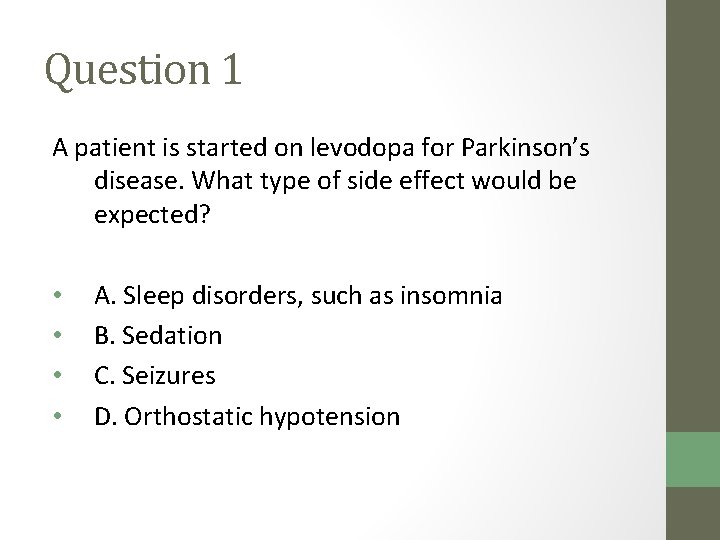
Question 1 A patient is started on levodopa for Parkinson’s disease. What type of side effect would be expected? • • A. Sleep disorders, such as insomnia B. Sedation C. Seizures D. Orthostatic hypotension
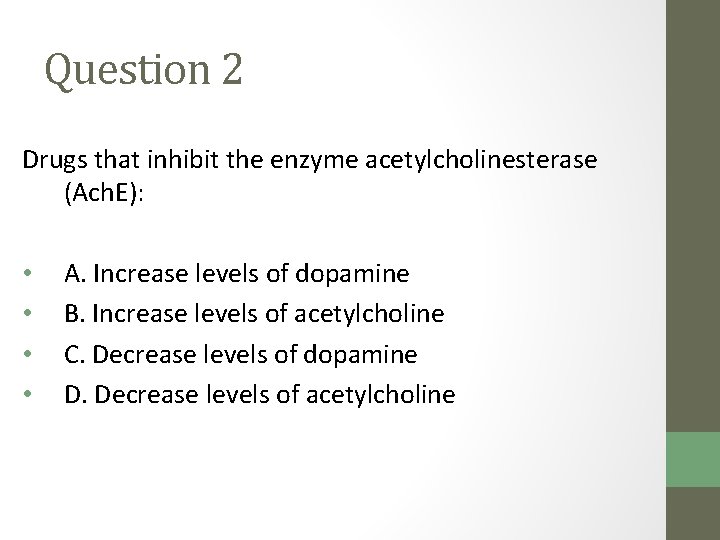
Question 2 Drugs that inhibit the enzyme acetylcholinesterase (Ach. E): • • A. Increase levels of dopamine B. Increase levels of acetylcholine C. Decrease levels of dopamine D. Decrease levels of acetylcholine
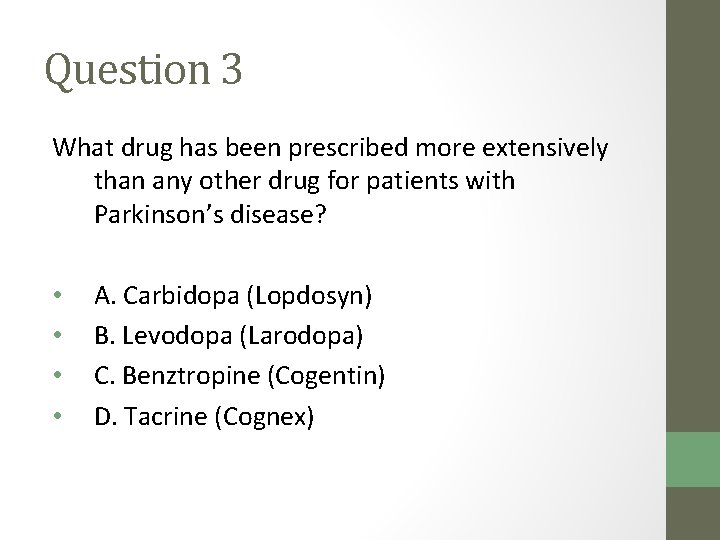
Question 3 What drug has been prescribed more extensively than any other drug for patients with Parkinson’s disease? • • A. Carbidopa (Lopdosyn) B. Levodopa (Larodopa) C. Benztropine (Cogentin) D. Tacrine (Cognex)
Chapter 20 Nonopioid Analgesics
Pain • Physiological and emotional experience characterized by unpleasant feelings • Usually associated with trauma or disease • The same degree and type of pain can be described differently by different peoplereaction to pain is a subjective experience • Numerical scales or survey instruments can be used to: ▫ Assess pain ▫ Measure progress of pain therapy

Pain 1938
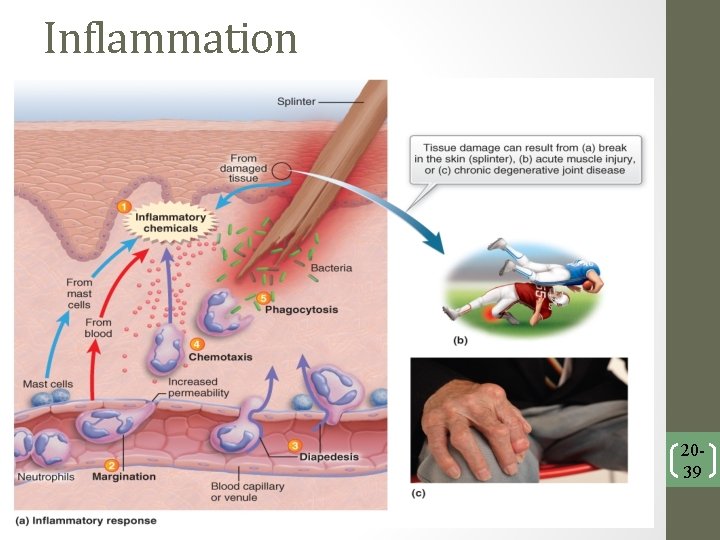
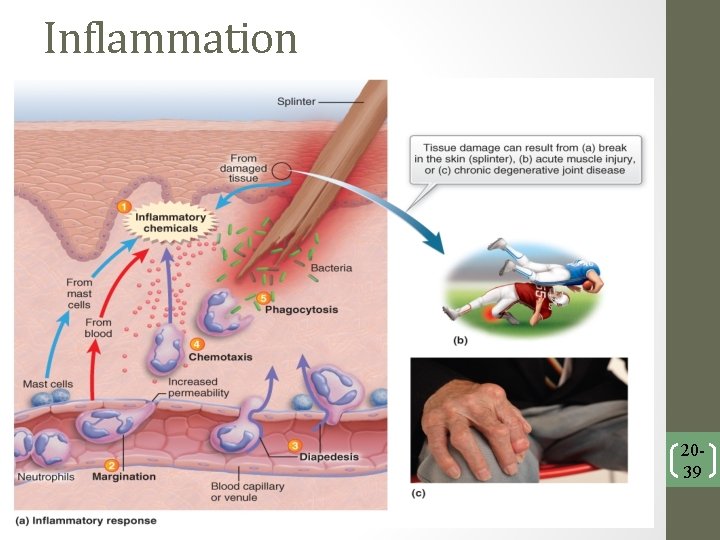
Inflammation 2039
Nonpharmacological Techniques �When used with pharmacotherapy can allow: ◦ Lower doses of the drug �Examples ◦ Acupuncture ◦ Biofeedback therapy ◦ Massage ◦ Heat/cold packs ◦ Meditation ◦ Relaxation therapy ◦ Art or music therapy ◦ Imagery ◦ Chiropractic manipulations ◦ Hypnosis ◦ Therapeutic touch ◦ Transcutaneous electric nerve stimulation (TENS) ◦ Energy therapies
Analgesics • Medications used to relieve pain • 2 basic categories 1. Opioids • natural or synthetic morphine-like substance responsible for reducing severe pain • Narcotic substances-they produce analgesia and CNS depression 2. Non-opioids NSAIDS –ASA, COX-2 Inhibitors, Traditional NSAIDs Acetaminophen
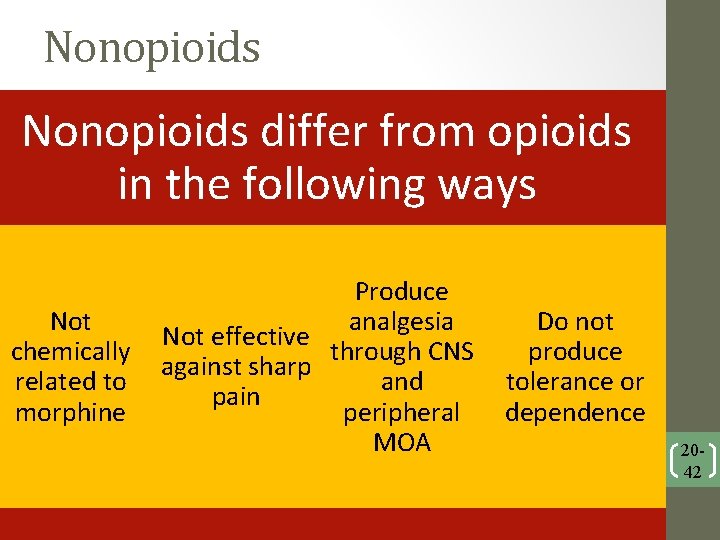
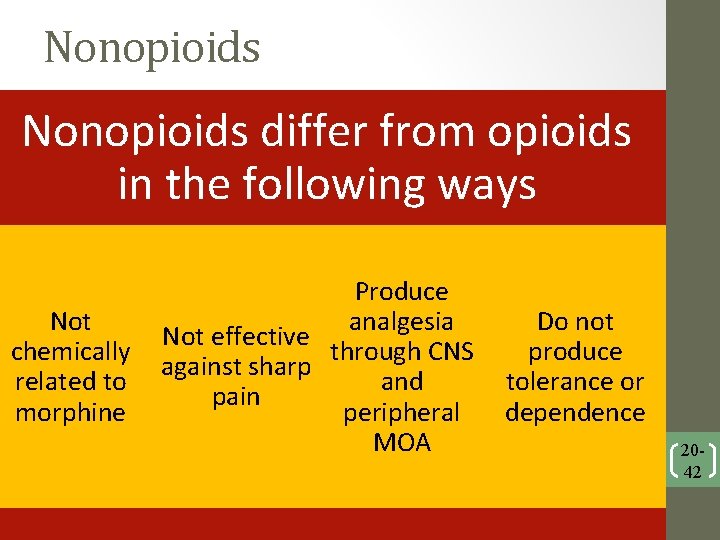
Nonopioids differ from opioids in the following ways Not chemically related to morphine Produce analgesia Not effective through CNS against sharp and pain peripheral MOA Do not produce tolerance or dependence 2042
Nonsteroidal anti-inflammatory drugs (NSAIDS) • Inhibit cyclooxygenase type one and/or two, an enzyme responsible for the formation prostaglandins • When cyclooxygenase is inhibited, inflammation and pain are reduced • Drugs of choice for mild to moderate pain, especially associated with inflammation • Have anti-inflammatory, analgesic, and anti-pyretic properties (the 3 A’s) • Many are OTC and inexpensive
Nonopioids (NSAIDs) • There are two groups within this class distinguished by their pharmacologic action: • Salicylates –Aspirin (ASA) • Nonsteroidal anti-inflammatory drugs -Traditional NSAIDs 2044
NSAIDs: Salicylates • Aspirin and salicylic acid are the main salicylates: • Oldest and most frequently used nonopioid analgesics, for mild to moderate pain • Used as analgesics, antipyretics, and antiinflammatories • Also used for inhibit platelet aggregation • Discovered from Native Americans’ use of willow tree bark 2045
NSAIDs: Salicylates • Salicylates produce analgesia and antipyresis by affecting the hypothalamic centers in the brain. • Aspirin is a potent inhibitor of prostaglandin synthesis, which decreases inflammation (MOA) • Salicylates block COX-1: • Protective environment in stomach is altered • Gastric ulcers can result • SE: Bleeding, esp GI Bleeding • frank bleeding or black tarry stools, ecchymosis, petechia • NC: Monitor for GI Bleeding, • take Enteric Coated(EC) for long term use and/or take with milk 2046
NSAIDs: Salicylates • Aspirin (prophylactic use): • Helps reduce risk of reinfarction • Prevents cardiovascular issues (MI and CVA) • (Used) for mild to moderate pain, osteoarthritis, and rheumatoid arthritis • Reduces inflammation • (SE) Salicylate intoxication: • Nausea, vomiting, salicylism; GI Bleeding • Nursing Consideration: • Aspirin should not be given to children with chickenpox or flu symptoms: • Reye’s syndrome 2047
Traditional NSAIDS • Ibuprofen and Ibuprofen-like (Nonsalicylates) • MOA: Are nonselective- inhibit both COX 1&2 • USE: anti-pyretic, anti-inflammatory, and analgesic • Profile Drugs: • Ibuprofen (Advil, Motrin) • Naproxen sodium (Aleve)
Traditional NSAIDs • All anti-inflammatory drugs may produce (SE): • Nausea, GI distress, and ulceration (GI bleeding) • Vertigo, vomiting, mental confusion, and headaches • Overdose of NSAIDs is similar to salicylate overdose. • No specific antidote for NSAID poisoning • NSAID use is discouraged in elderly patients. 2049
Acetaminophen (Tylenol) • Class: Synthetic non-opiate analgesic • MOA: Inhibits prostaglandin synthesis, but the exact site and mechanism of action are unknown! • Use: Anti-pyretic effectiveness and analgesic potency are similar to aspirin • No anti-inflammatory activity- not effective in the relief of symptoms of inflammation
Nonopioid Anaglgesic: Acetaminophen • Acetaminophen is effective in treating headaches, fever, and minor musculoskeletal pain. • Inhibits prostaglandin synthetase • Considered an aspirin substitute • Does not have anti-inflammatory properties • Not useful in the treatment of arthritis 2051
acetaminophin (Tylenol) • Side Effects: Hepatotoxicity • Nursing Considerations: • Maximum Tylenol dosage is 4 grams daily • Be careful of combination meds • Reversal agent is acetylcysteine (Mucomyst)

Preferred Therapy • Aspirin: • Fever, headaches, inflammation including arthritis, prophylaxis of heart attack or stroke • Ibuprofen: • Aches, pains, inflammation • Acetaminophen: • Fever and headache, aspirin substitute 2053
Tension Headache • HA is one of the most common complaints of patients • Tension HAs are most common kind • Occurs when muscles of head and neck tighten in response to stress • Tightness causes steady and lingering pain • Usually end when stress is resolved • Treated with OTC analgesics like ASA, acetaminophen, or ibuprofen
Migraines �Most painful type of HA �Characterized by throbbing or pulsating pain, sometimes proceeded by an aura (similar to those that warn of a seizure) �Most patients also experience N and V � 2 primary goals for pharmacology therapy 1. Stop migraines in progress 2. Prevent migraines from occurring �Drug therapy is more effective if begun before migraine has reached severe level
Triptans • MOA: Constrict certain vessels within the brain in order to stop migraine • Vasoconstricts the cranial arteries • Example: • Sumatriptan (Imitrex) • Side Effects: • Dizziness, drowsiness • Nursing Considerations: • Due to vasoconstriction, use cautiously in pts with recent MI, HTN, DM, or CVA

Ergot Alkaloids • Use: for patients who are unresponsive to triptans to stop migraines • Example: Ergotamine (Ergostat) • MOA: interacts with dopaminergic, adrenergic, and serotonin receptors • SE: Dizziness, N/V • NC: may cause physical dependence, monitor for withdrawal symptoms • Pregnancy Category X
Other drugs for migraine prevention • Examples • beta-adrenergic blockers • calcium channel blockers • antidepressants • antiseizure drugs
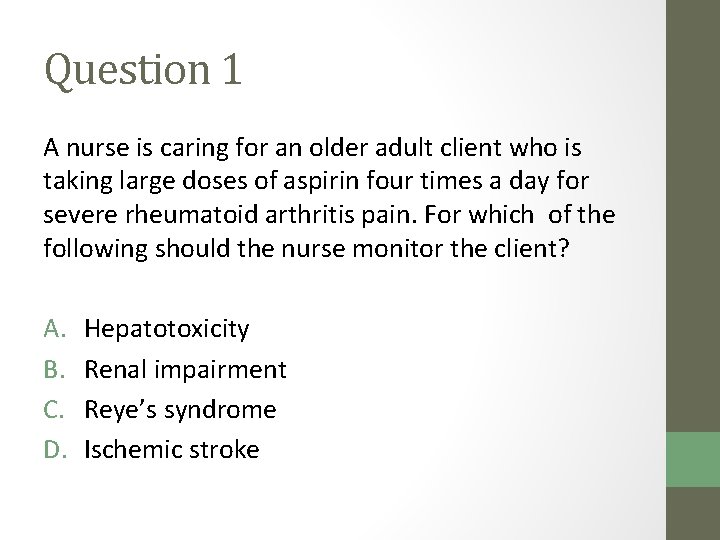
Question 1 A nurse is caring for an older adult client who is taking large doses of aspirin four times a day for severe rheumatoid arthritis pain. For which of the following should the nurse monitor the client? A. B. C. D. Hepatotoxicity Renal impairment Reye’s syndrome Ischemic stroke
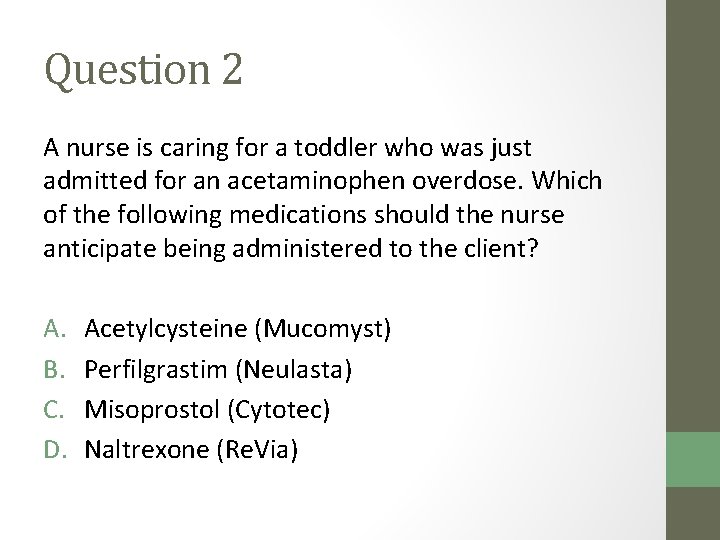
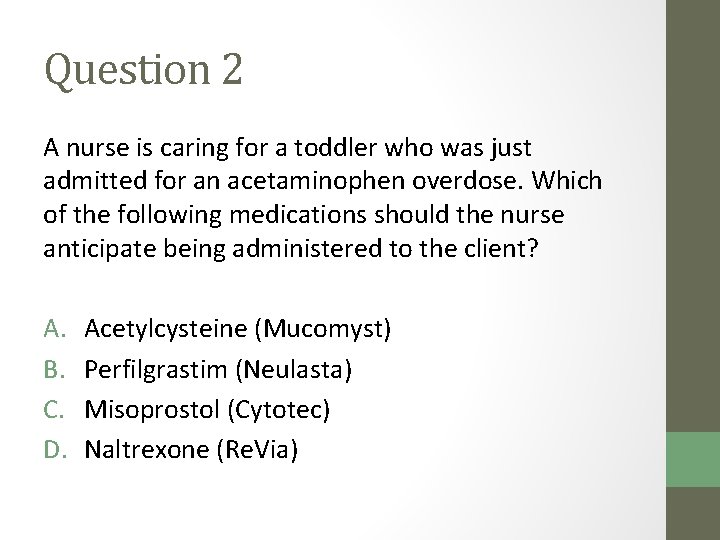
Question 2 A nurse is caring for a toddler who was just admitted for an acetaminophen overdose. Which of the following medications should the nurse anticipate being administered to the client? A. B. C. D. Acetylcysteine (Mucomyst) Perfilgrastim (Neulasta) Misoprostol (Cytotec) Naltrexone (Re. Via)
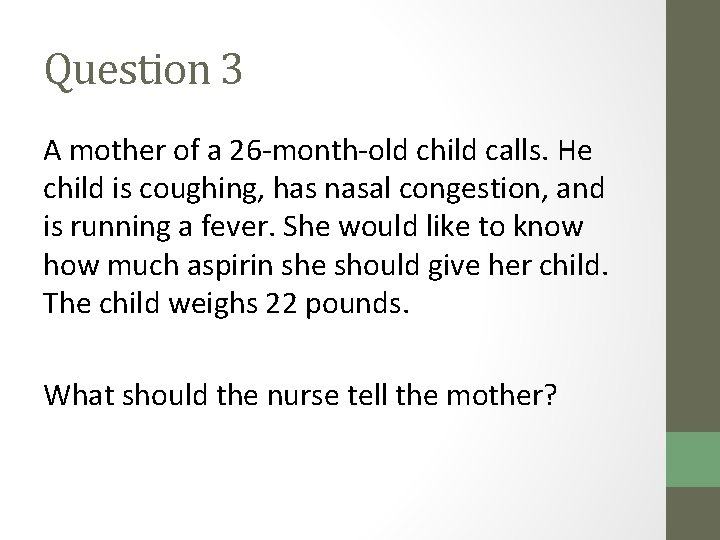
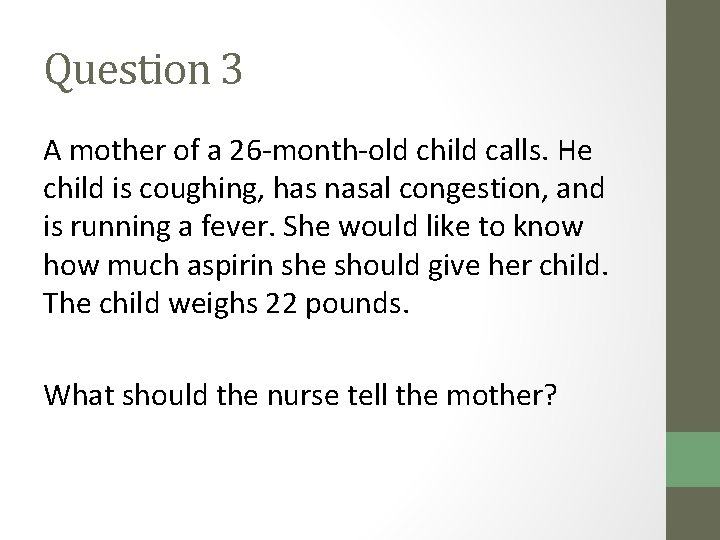
Question 3 A mother of a 26 -month-old child calls. He child is coughing, has nasal congestion, and is running a fever. She would like to know how much aspirin she should give her child. The child weighs 22 pounds. What should the nurse tell the mother?
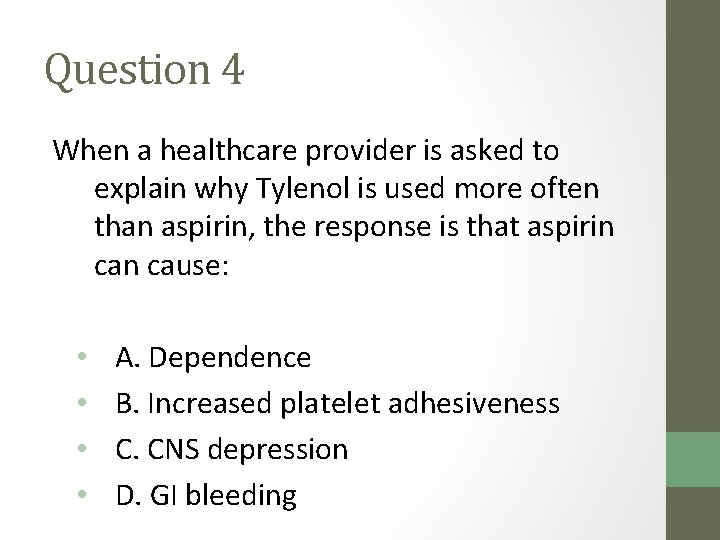
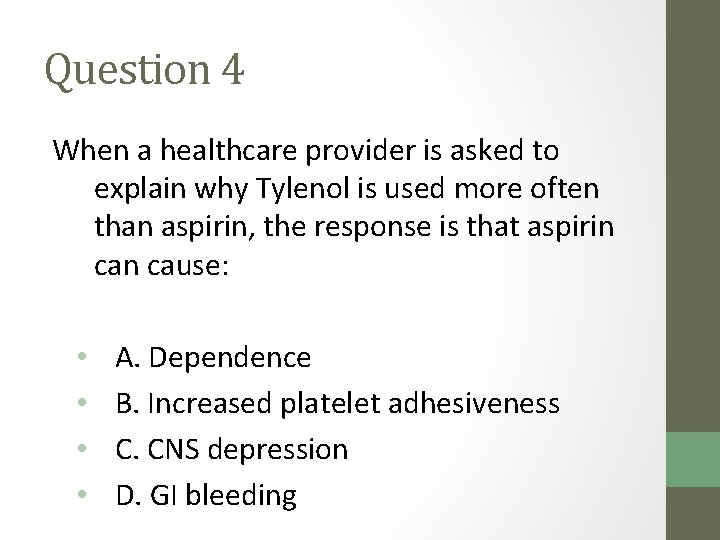
Question 4 When a healthcare provider is asked to explain why Tylenol is used more often than aspirin, the response is that aspirin cause: • • A. Dependence B. Increased platelet adhesiveness C. CNS depression D. GI bleeding
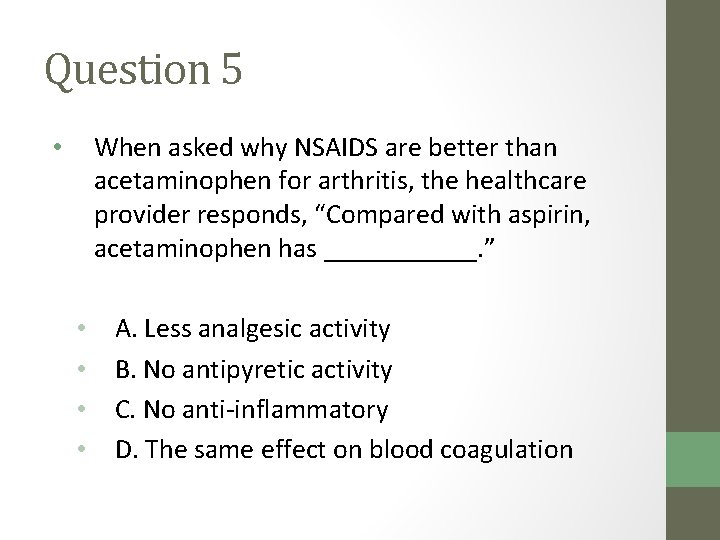
Question 5 When asked why NSAIDS are better than acetaminophen for arthritis, the healthcare provider responds, “Compared with aspirin, acetaminophen has ______. ” • • • A. Less analgesic activity B. No antipyretic activity C. No anti-inflammatory D. The same effect on blood coagulation
Chapter 19 Opioid Analgesics
Opioid Analgesics (Uses): • Opioids are considered first-line therapy for: • Pain associated with procedures • Pain due to trauma or cancer • Visceral pain (appendicitis) • Used to relieve acute or chronic pain • analgesic • Suppress cough • Treat diarrhea (slow GI motility) 1965
Opioid Analgesics: • (MOA) Opioid analgesics act by binding to opioid receptors and mimicking the effects of the analgesic peptides. • (SE) Opioids influence CNS activity: • Decrease mental alertness • Euphoria • Dysphoria • Respiratory depression 1966
Opioid Analgesics (SE): • Opioids have direct action on smooth muscle in the GI tract, which can lead to constipation. • Nausea, vomiting • Constipation • They can also cause: • Bronchoconstriction • Decreased urination 1967
Drug Administration • Because opioid analgesics are CNS depressants at any dose, patients should be closely monitored for overdose. • NC: Monitor for Respiratory Depression • Opioid analgesics are metabolized by the liver and then excreted by the kidneys. • Anything that causes alkaline urine increases the concentration of opioids in the blood. 1968
Opioid Agonists • Bind to opioid receptors and produce multiple responses • Morphine is the representative drug used to treat severe pain- the standard against which the effectiveness of every other opioid is compared
Opioids • Drugs of choice for moderate to severe pain that cannot be controlled with other classes of analgesics • More than 20 different opioids are available as medications • Most commonly classified by effectiveness, which places opiates into categories of strong or moderate narcotic activity
Common Opioid Agonists with High Effectiveness • Hydromorphone hydrochloride (Dilaudid) • Meperidine hydrochloride (Demerol) • Morphine sulfate (Duramorph) • Hydrocodone • oxycodone hydrochloride (Oxy. Contin) • Codiene
Combinations • It is common practice to combine opioids and nonnarcotic analgesics • Two classes work synergistically to relieve pain • What is the benefit to this?
Common Combinations • Vicodin (hydrocodone 5 mg; acetaminophen 500 mg) • Percocet (oxycodone HCl 5 mg; acetaminophen 325 mg)
Tolerance and Physical Dependence • Methadone is used in the treatment of opioid addiction: • Satisfies opioid hunger • Does not produce severe withdrawal symptoms • Buprenorphine: • Pushes opioids out of receptors • Blocks attachment of opioids to receptors 1974
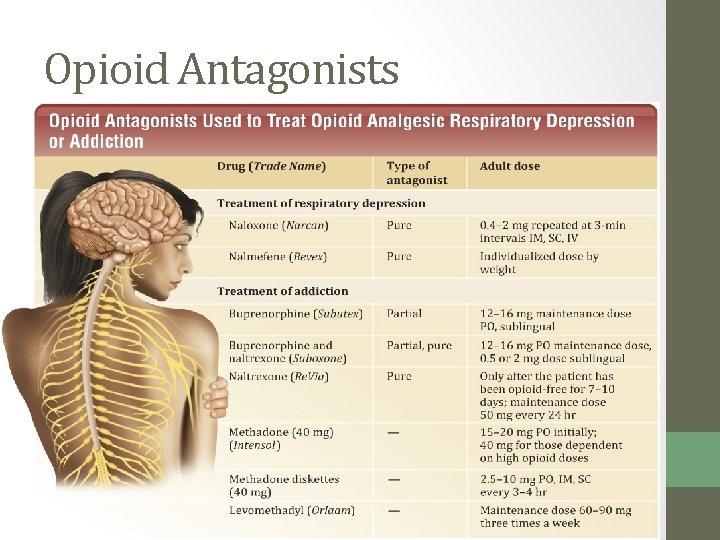
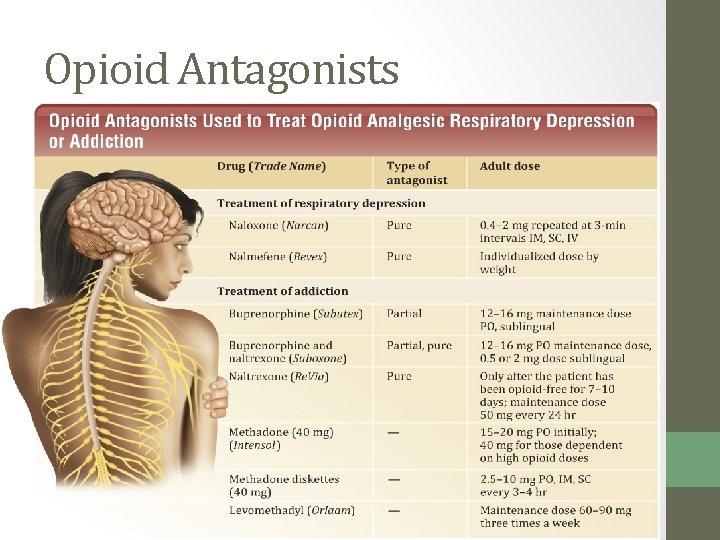
Opioid Antagonists • Opioid poisoning presents with coma, depressed respiration, cyanosis, and hypotension. • MOA: Antagonists are drugs that attach to opioid receptors and displace the analgesic, rapidly reversing poisoning. • Pure • Partial 1975
Opioid Antagonists
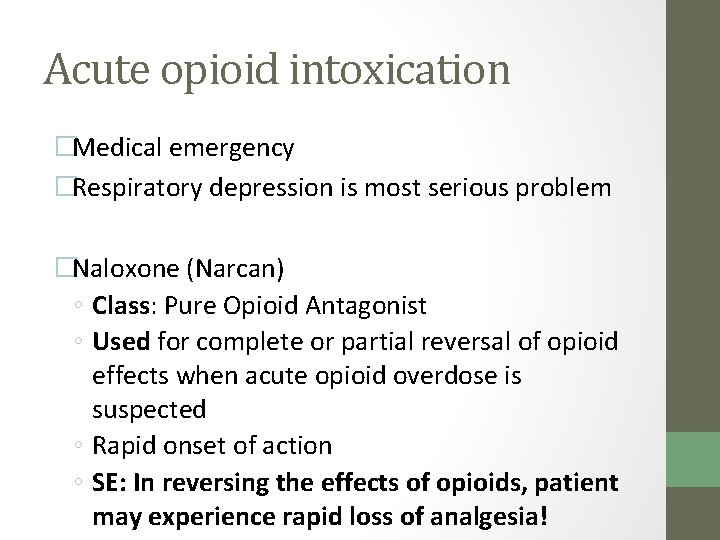
Acute opioid intoxication �Medical emergency �Respiratory depression is most serious problem �Naloxone (Narcan) ◦ Class: Pure Opioid Antagonist ◦ Used for complete or partial reversal of opioid effects when acute opioid overdose is suspected ◦ Rapid onset of action ◦ SE: In reversing the effects of opioids, patient may experience rapid loss of analgesia!
Opioid Antitussives • Antitussives are drugs that suppress the cough reflex: • Codeine • Hydrocodone • Dextromethorphan • Expectorants are commonly combined with antitussives to aid in the removal of mucus. 1978

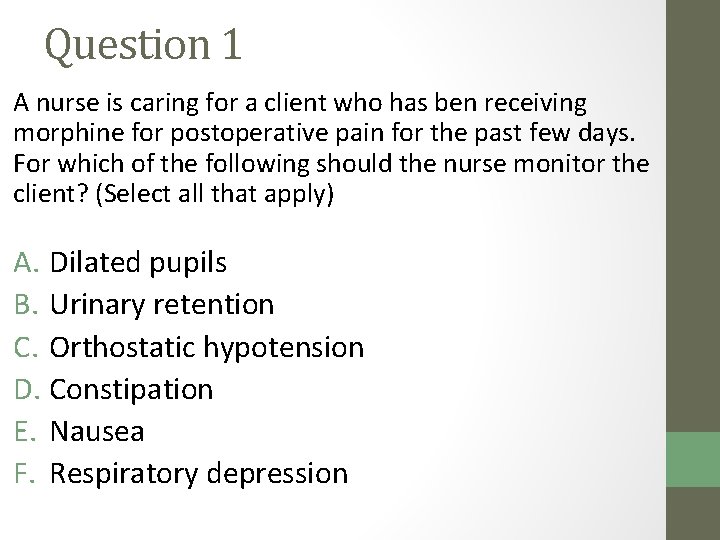
Question 1 A nurse is caring for a client who has ben receiving morphine for postoperative pain for the past few days. For which of the following should the nurse monitor the client? (Select all that apply) A. Dilated pupils B. Urinary retention C. Orthostatic hypotension D. Constipation E. Nausea F. Respiratory depression
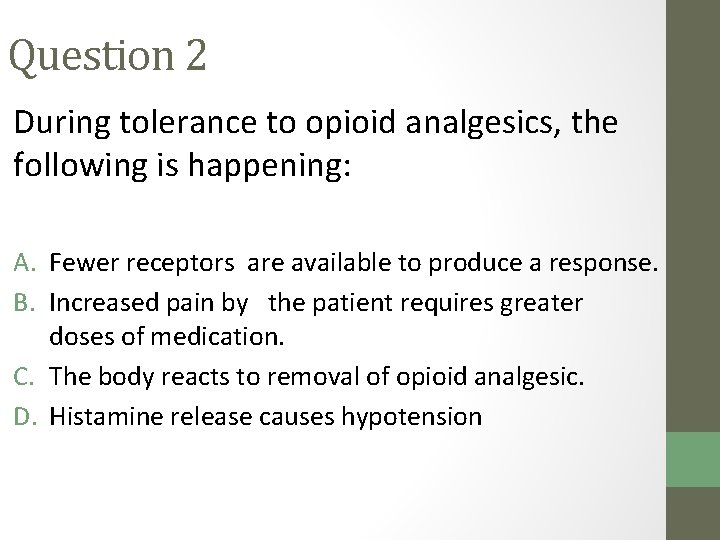
Question 2 During tolerance to opioid analgesics, the following is happening: A. Fewer receptors are available to produce a response. B. Increased pain by the patient requires greater doses of medication. C. The body reacts to removal of opioid analgesic. D. Histamine release causes hypotension
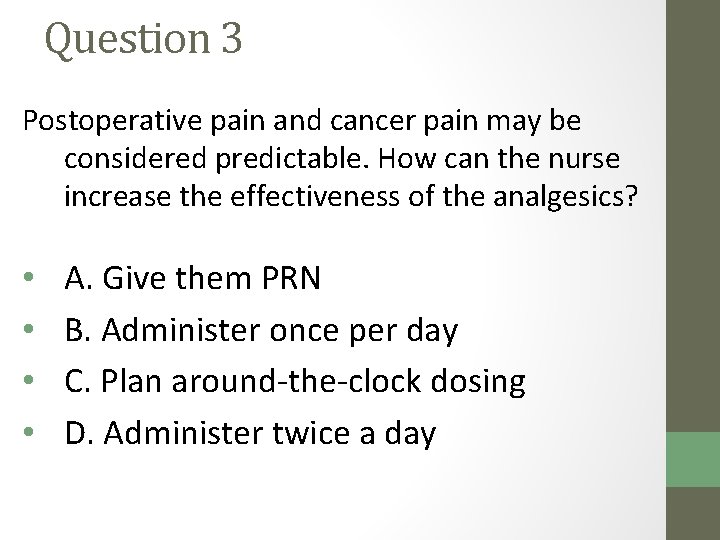
Question 3 Postoperative pain and cancer pain may be considered predictable. How can the nurse increase the effectiveness of the analgesics? • • A. Give them PRN B. Administer once per day C. Plan around-the-clock dosing D. Administer twice a day
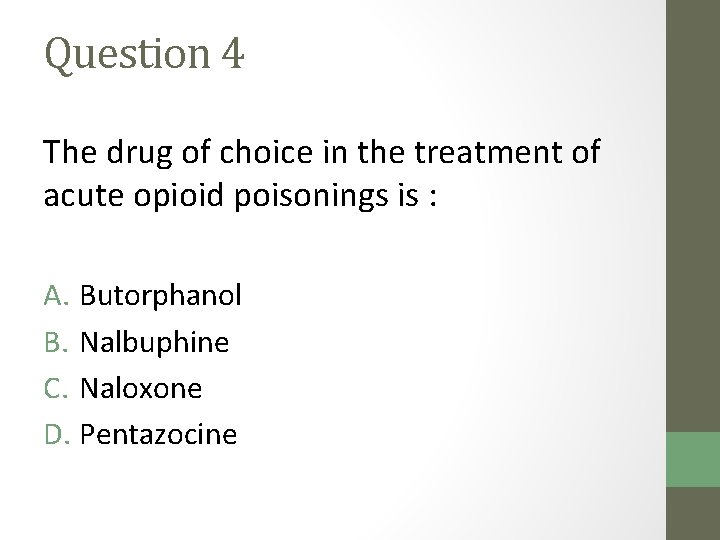
Question 4 The drug of choice in the treatment of acute opioid poisonings is : A. Butorphanol B. Nalbuphine C. Naloxone D. Pentazocine
Question 5 Postoperative pain and cancer pain may be considered predictable. How can the nurse increase the effectiveness of the analgesics? • • A. Give them PRN B. Administer once per day C. Plan around-the-clock dosing D. Administer twice a day
Question 6 The following preoperative medications have been ordered: morphine 5 mg with atropine 0. 4 mg IM on call to the OR. The nurse would explain to the client that the purpose of these medications is to: • • A. Assist the client to sleep and not be aware of his surroundings during transport to the OR B. Reduce client anxiety and cause amnesia during the preoperative period C. Reduce the client’s oral and respiratory secretions, and promote induction of anesthesia in surgery D. Reduce the possibility of the client being nauseated and vomiting during and after surgery
Question 7 A client goes to the ER with an overdose of morphine. What would the priority nursing assessment be? • • A. Dilated pupils B. Depressed respiration C. Hypertension D. Diarrhea
Chapter 9 Skeletal Muscle Relaxants
Skeletal Muscle Relaxants • There are two ways skeletal muscle can be relaxed: • By blocking conduction to the spinal cord • By inhibiting contraction of the neuromuscular junction 9 -88
Peripherally/Direct Acting Relaxants • Neuromuscular blockers inhibit skeletal muscle contraction. • There are two types of neuromuscular blockers: • Nondepolarizing • Depolarizing 9 -89

Direct-Acting Relaxants • dantrolene (Dantium) interferes with calcium ion release in the muscle fibers, which inhibits muscle contraction. (MOA) • dantrolene is used in the treatment of malignant hyperthermia and spastic conditions • To relieve muscle spasms and pain associated with injuries • MS, Huntington’s, Cerebral Palsy, stroke 9 -91

Direct-Acting Relaxants • The adverse effects seen from dantrolene include: • • • Dizziness Vomiting Fatigue Weakness Hepatotoxicity Respiratory muscle paralysis 9 -92
Centrally Acting Relaxants • Drugs that relax skeletal muscle by a central mechanism depress reflex impulse conduction within the spinal cord. • This change in conduction reduces the number of impulses available to produce muscle contraction. 9 -93
Centrally Acting Relaxants • Used to treat spastic contraction from: • Overexertion • Trauma • Nervous tension • Adverse effects include: • Blurred vision • Lethargy • Decreased mental alertness • Respiratory muscle paralysis 9 -94
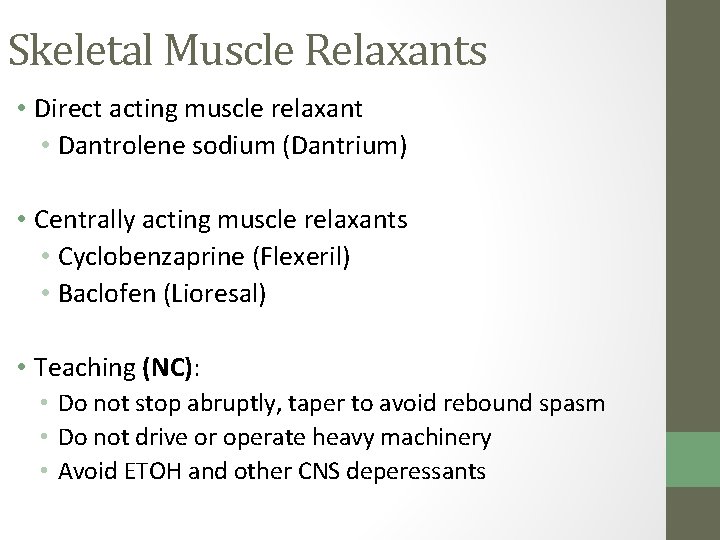
Skeletal Muscle Relaxants • Direct acting muscle relaxant • Dantrolene sodium (Dantrium) • Centrally acting muscle relaxants • Cyclobenzaprine (Flexeril) • Baclofen (Lioresal) • Teaching (NC): • Do not stop abruptly, taper to avoid rebound spasm • Do not drive or operate heavy machinery • Avoid ETOH and other CNS deperessants
Adverse and Toxic Effects • The major toxicity of neuromuscular blockers is respiratory muscle paralysis. • Additional adverse effects include: • Malignant hyperthermia • Increased neuromuscular blockade with drugs that inhibit skeletal muscle function 9 -96
Question 1 A nurse is caring for a client who has a prescription for tizanidine (Zanaflex) for relief of muscle spasm following a back injury. Which of the following lab values should the nurse expect to monitor while the patient is taking this medicaiton? A. Serum creatinine B. Liver enzymes C. WBC count D. RBC count
Question 2 A nurse is caring for a client who has been taking oral baclofen (Lioresal) three times daily for the past 8 months. The client says to the nurse, “I’ve been having problems with constipation, so I'm just going to stop taking this medicaiton. ” What should the be the nurse’s response? Why?
Question 3 Skeletal muscle relaxants may alter control of respirations because: A. The diaphragm is a skeletal muscle. B. Succinylcholine stimulates the respiratory centers of the brain. C. Like dantrolene, all muscle relaxants inhibit the action of norepinephrine at the neuromuscular junction. D. Relaxation of the muscles in the lower extremities pulls blood away form the lungs.