Drugs affecting haemostasis Antianemic drugs A Koht Drugs
- Slides: 37
Drugs affecting haemostasis, Antianemic drugs A. Kohút
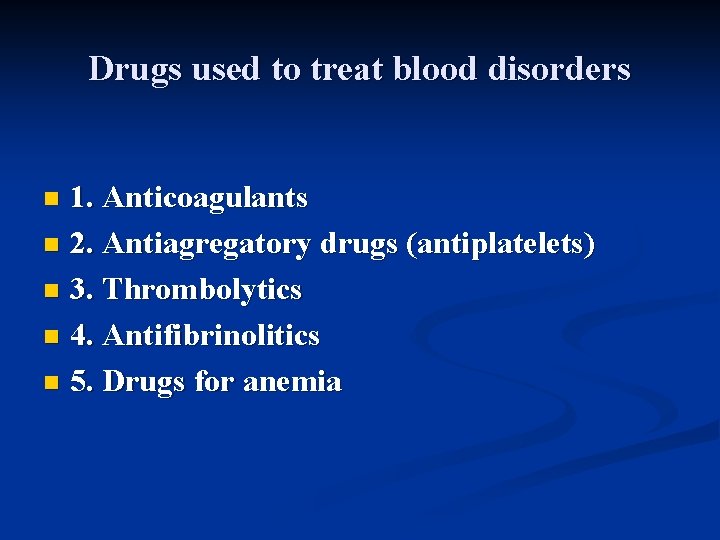
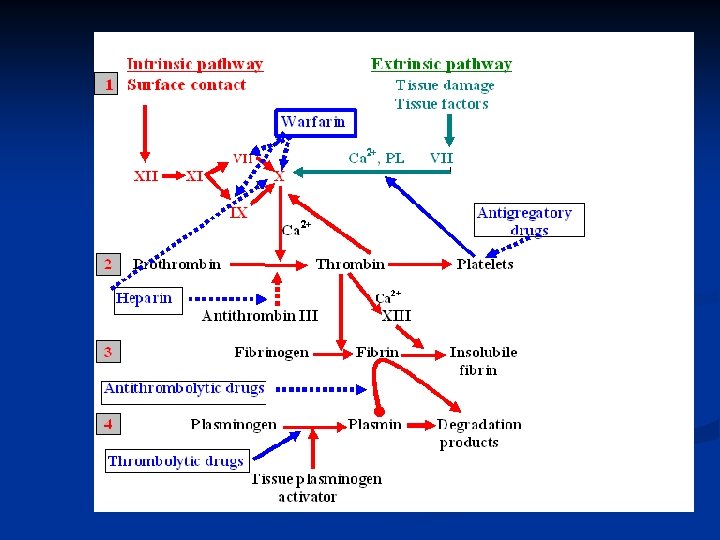
Drugs used to treat blood disorders 1. Anticoagulants n 2. Antiagregatory drugs (antiplatelets) n 3. Thrombolytics n 4. Antifibrinolitics n 5. Drugs for anemia n
Anticoagulants
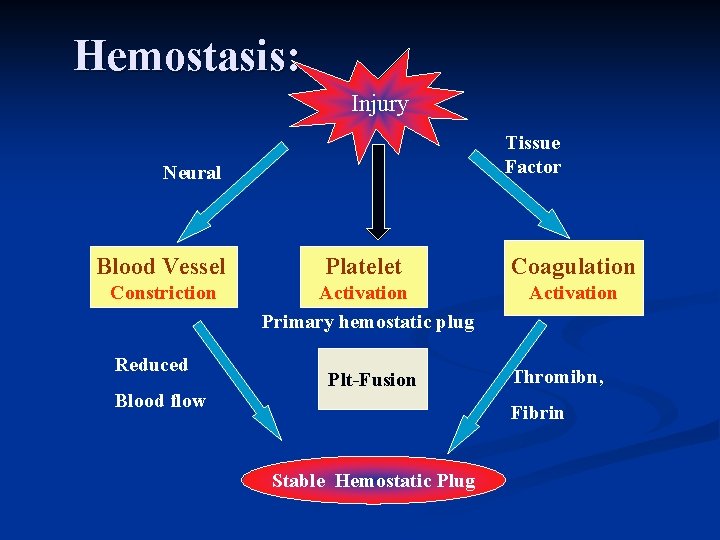
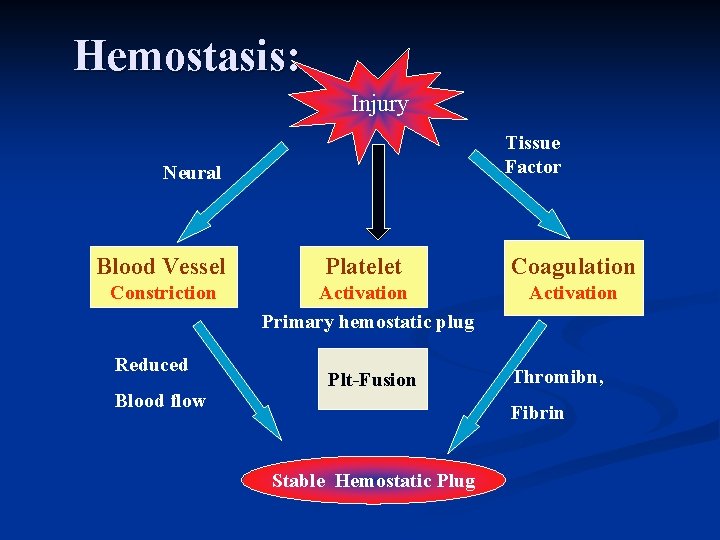
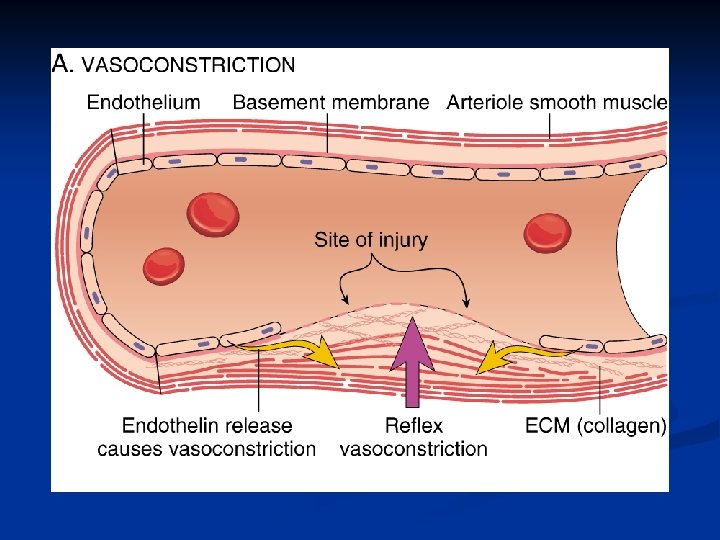
Hemostasis: Injury Tissue Factor Neural Blood Vessel Platelet Coagulation Constriction Activation Primary hemostatic plug Activation Reduced Blood flow Plt-Fusion Thromibn, Fibrin Stable Hemostatic Plug
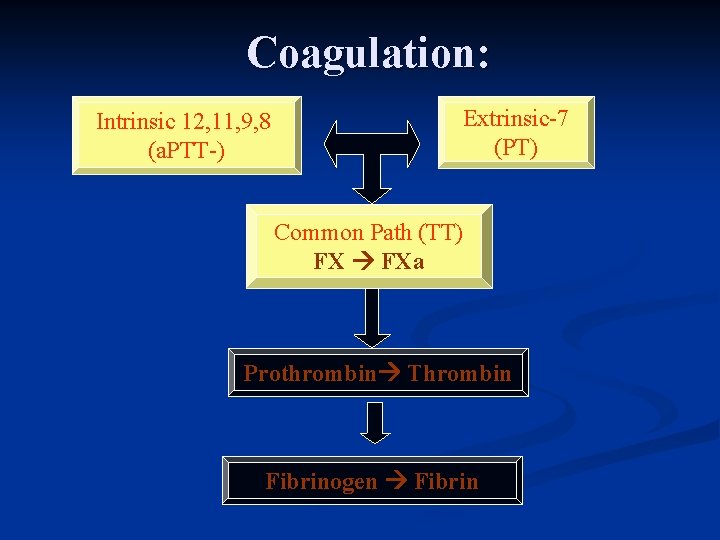
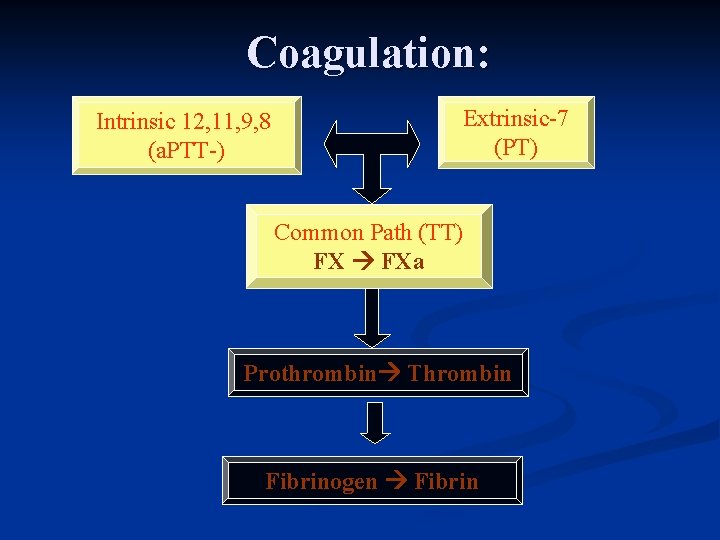
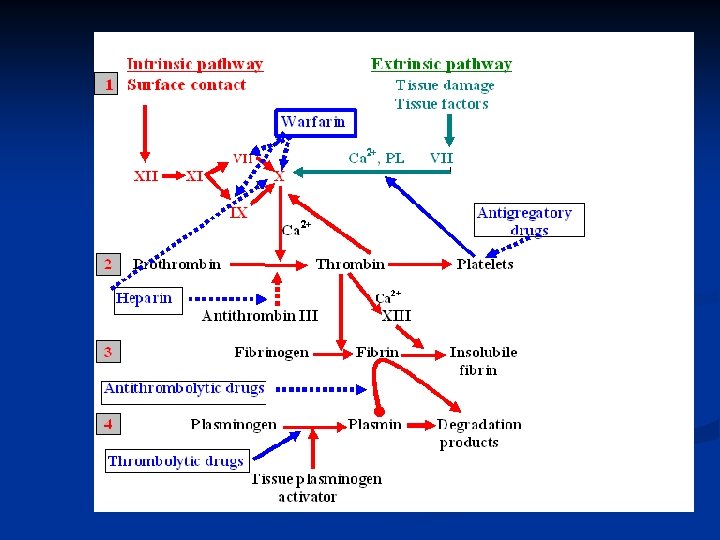
Coagulation: Intrinsic 12, 11, 9, 8 (a. PTT-) Extrinsic-7 (PT) Common Path (TT) FX FXa Prothrombin Thrombin Fibrinogen Fibrin
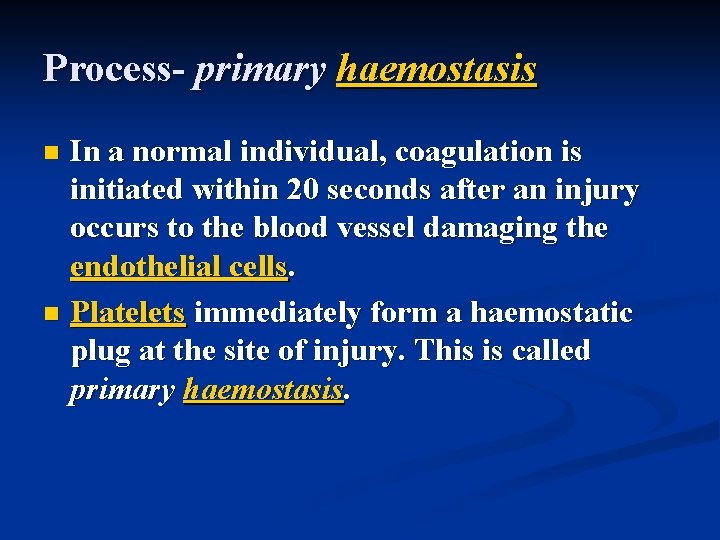
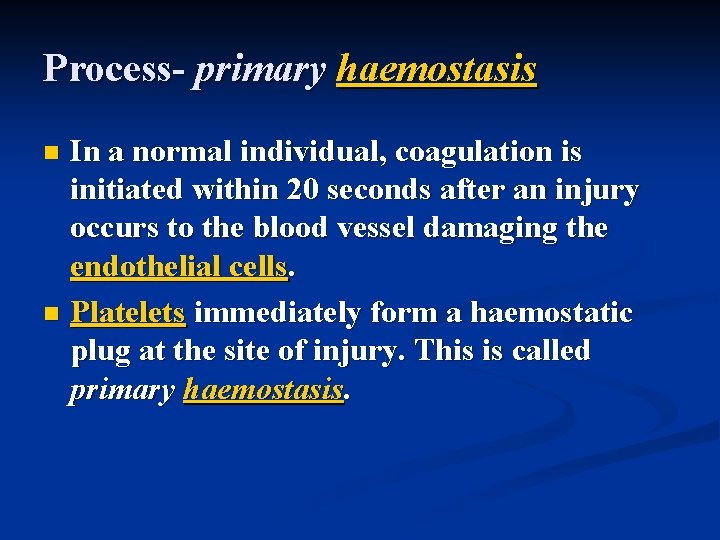
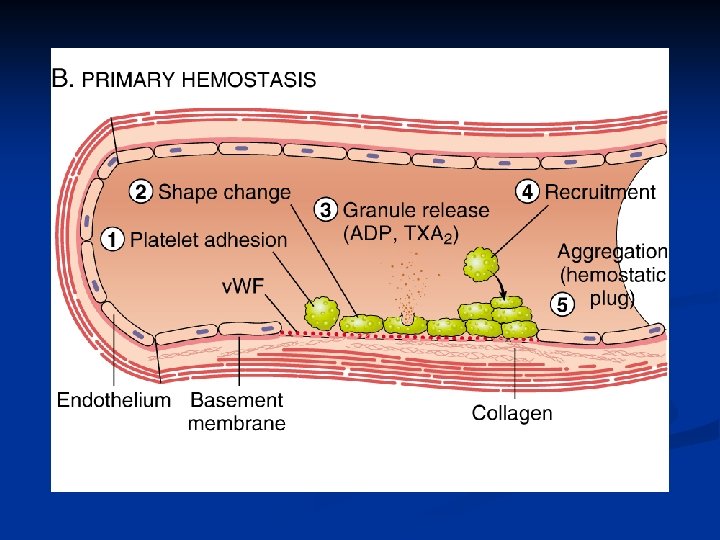
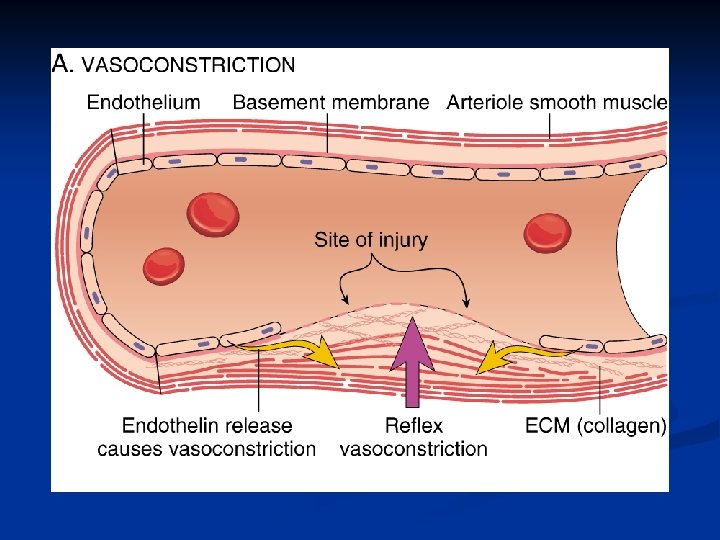
Process- primary haemostasis In a normal individual, coagulation is initiated within 20 seconds after an injury occurs to the blood vessel damaging the endothelial cells. n Platelets immediately form a haemostatic plug at the site of injury. This is called primary haemostasis. n
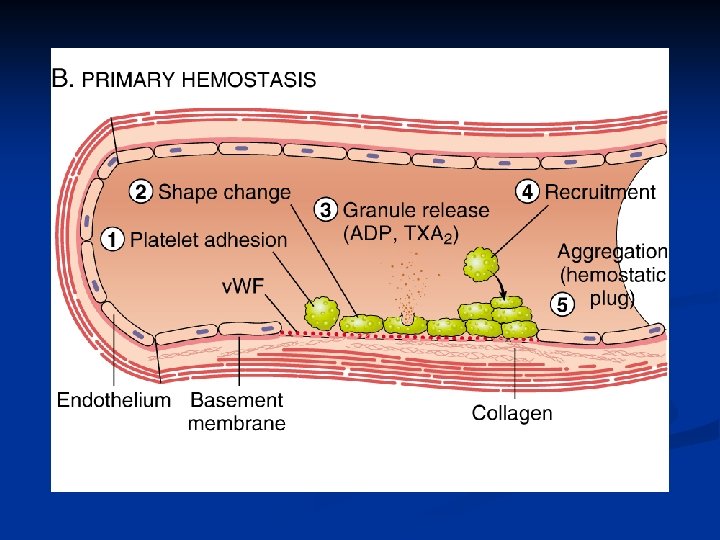
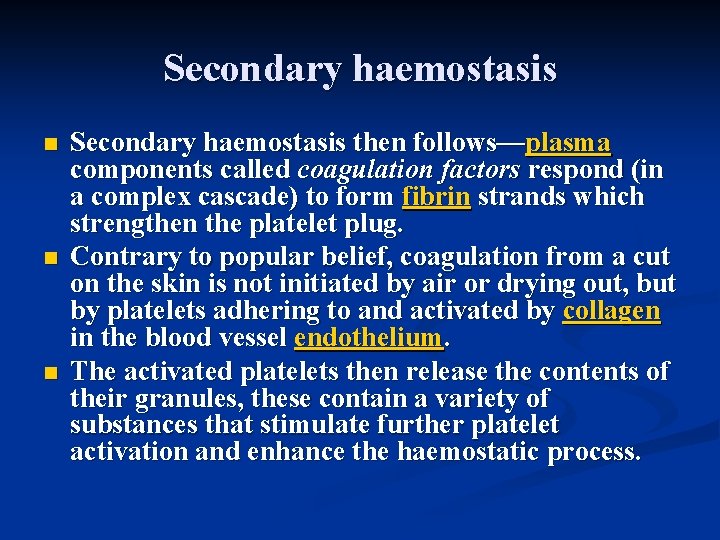
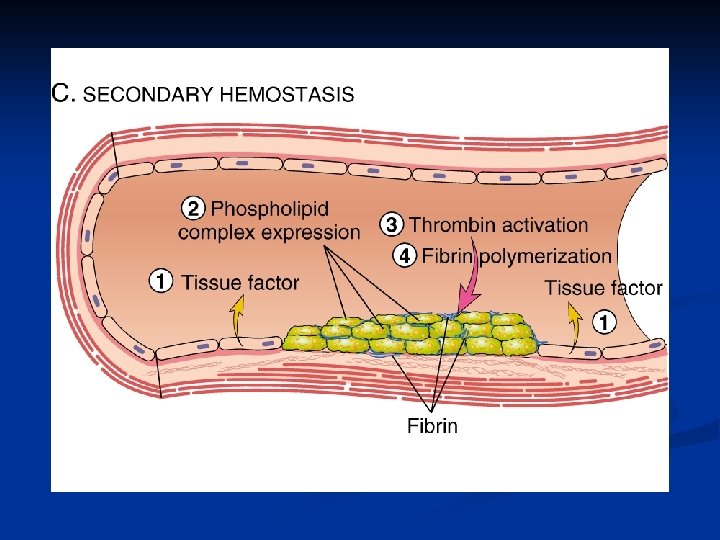
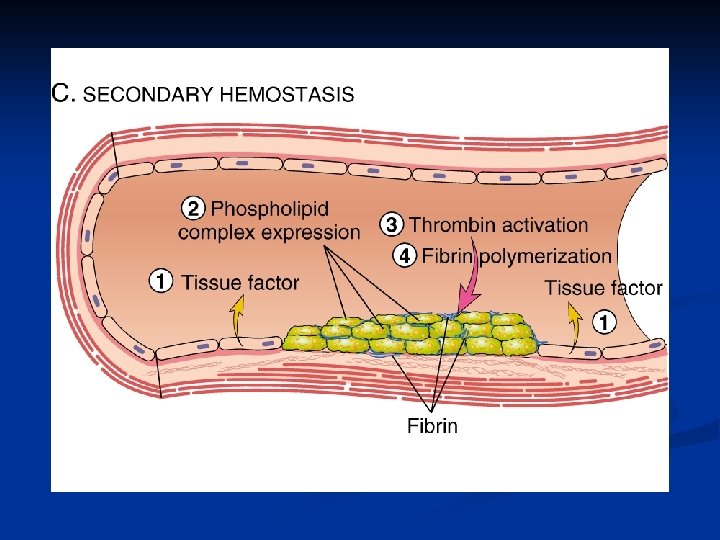
Secondary haemostasis n n n Secondary haemostasis then follows—plasma components called coagulation factors respond (in a complex cascade) to form fibrin strands which strengthen the platelet plug. Contrary to popular belief, coagulation from a cut on the skin is not initiated by air or drying out, but by platelets adhering to and activated by collagen in the blood vessel endothelium. The activated platelets then release the contents of their granules, these contain a variety of substances that stimulate further platelet activation and enhance the haemostatic process.
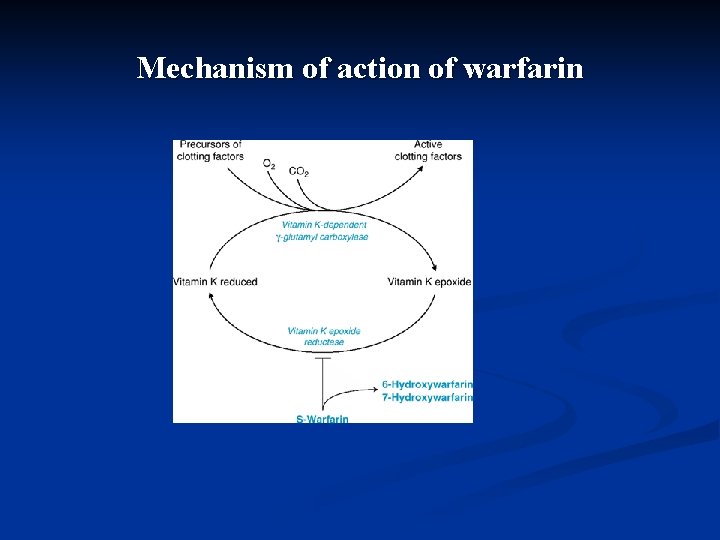
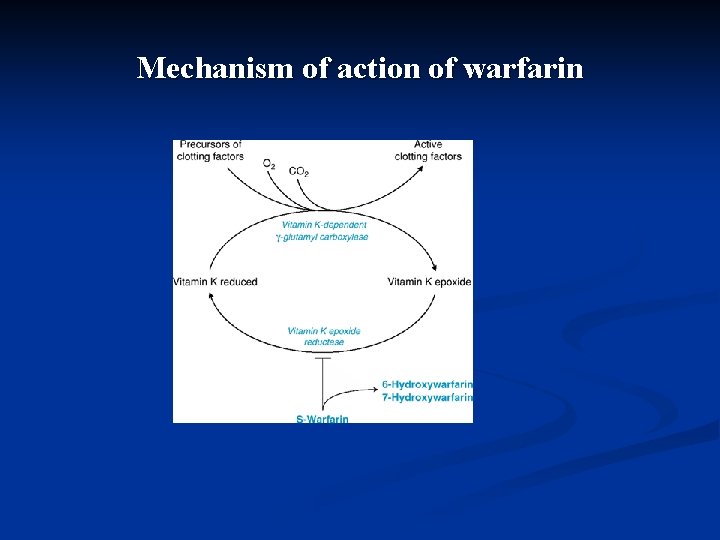
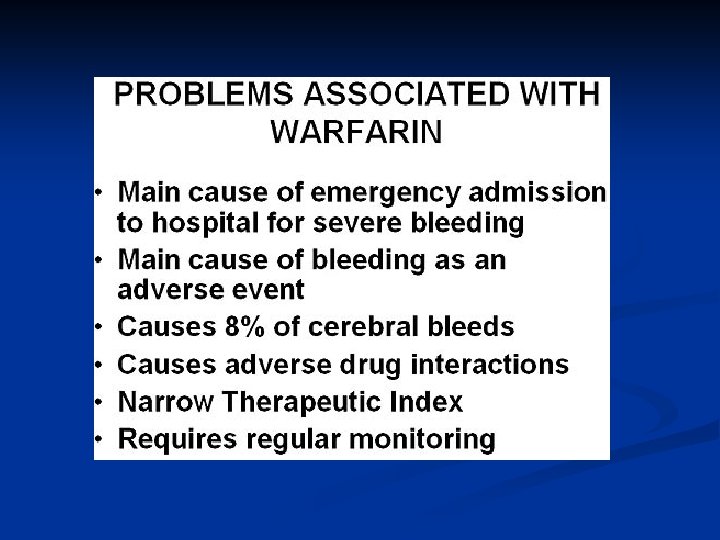
Mechanism of action of warfarin
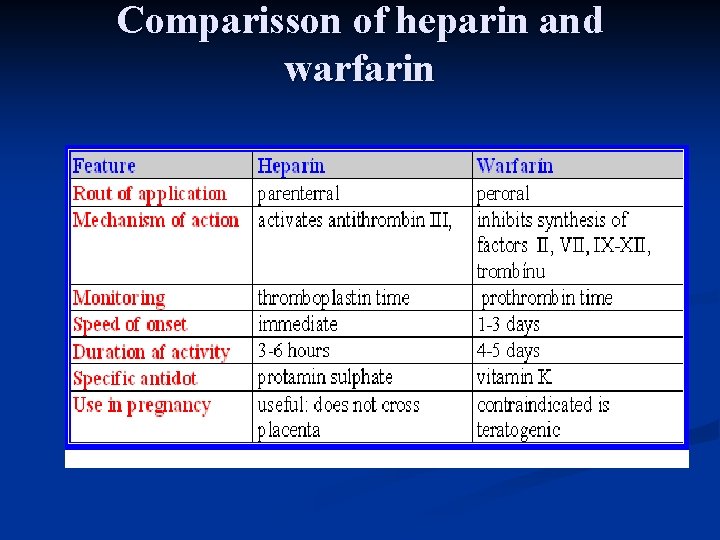
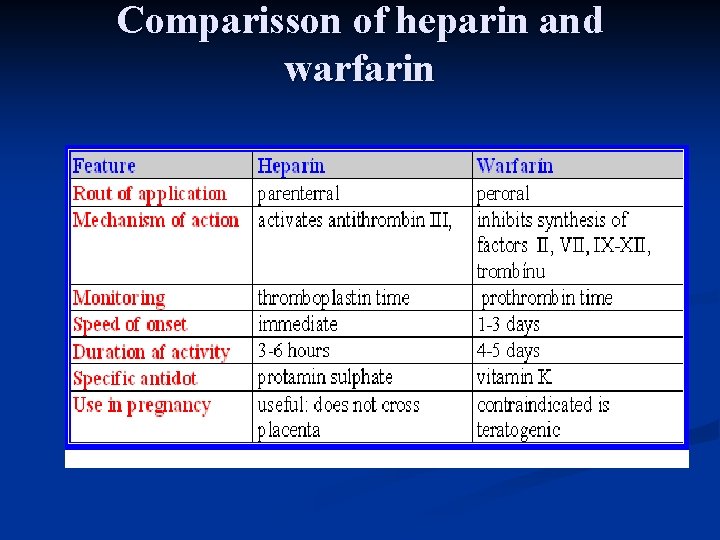
Comparisson of heparin and warfarin
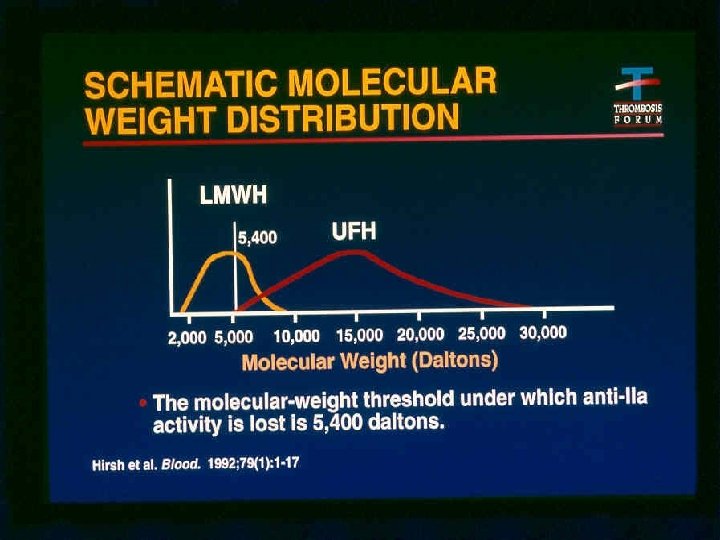
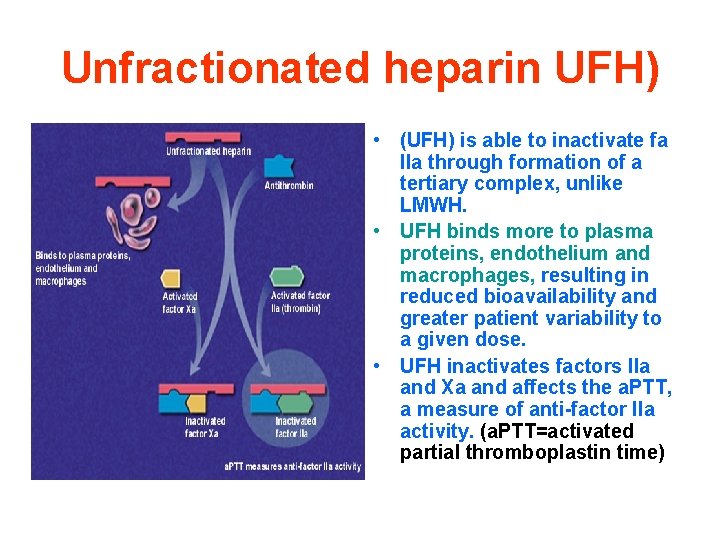
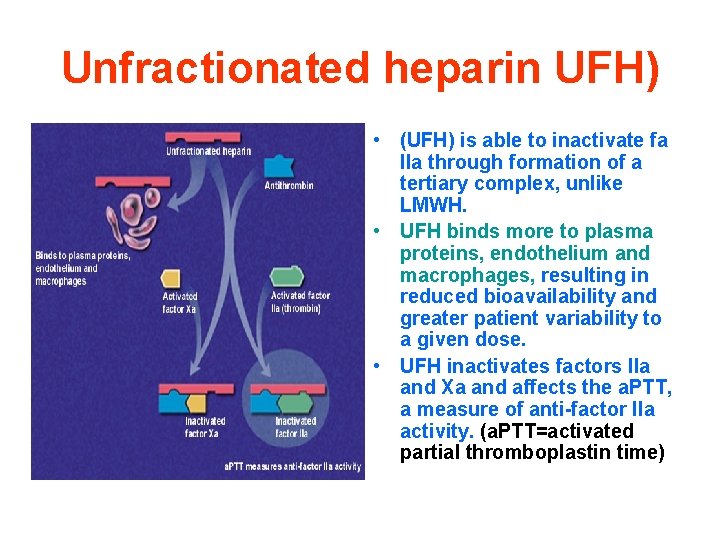
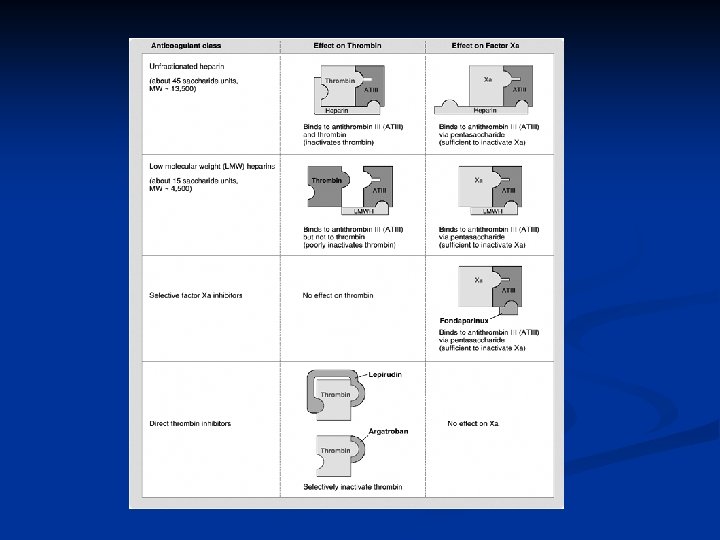
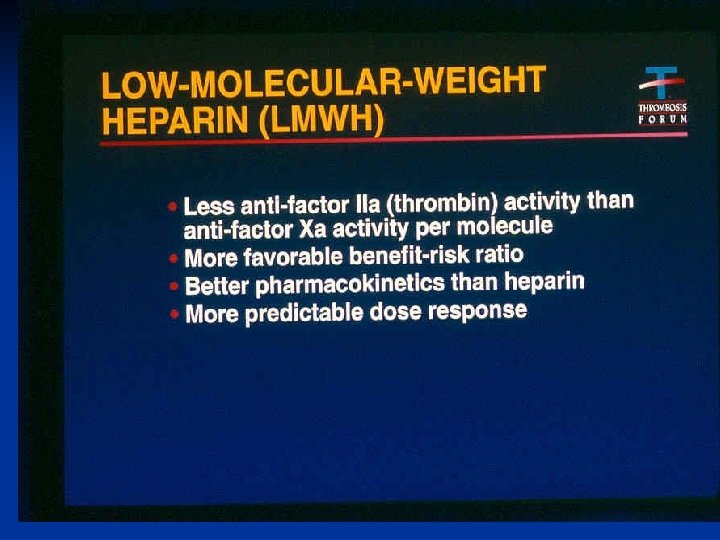
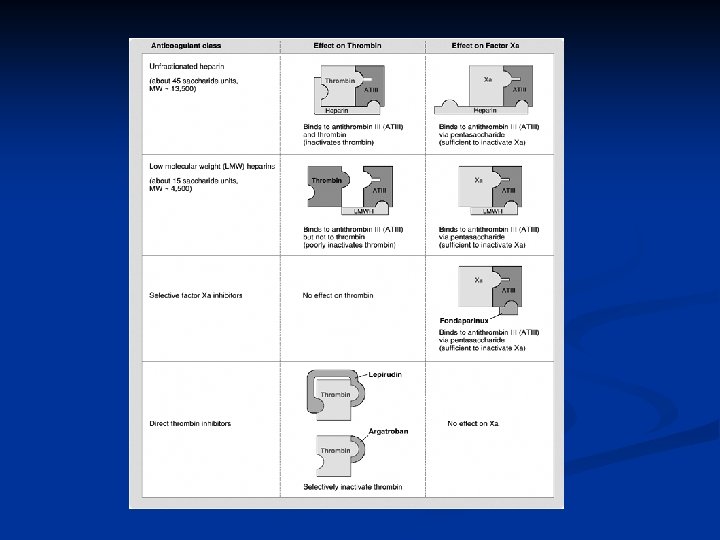
Unfractionated heparin UFH) • (UFH) is able to inactivate fa IIa through formation of a tertiary complex, unlike LMWH. • UFH binds more to plasma proteins, endothelium and macrophages, resulting in reduced bioavailability and greater patient variability to a given dose. • UFH inactivates factors IIa and Xa and affects the a. PTT, a measure of anti-factor IIa activity. (a. PTT=activated partial thromboplastin time)
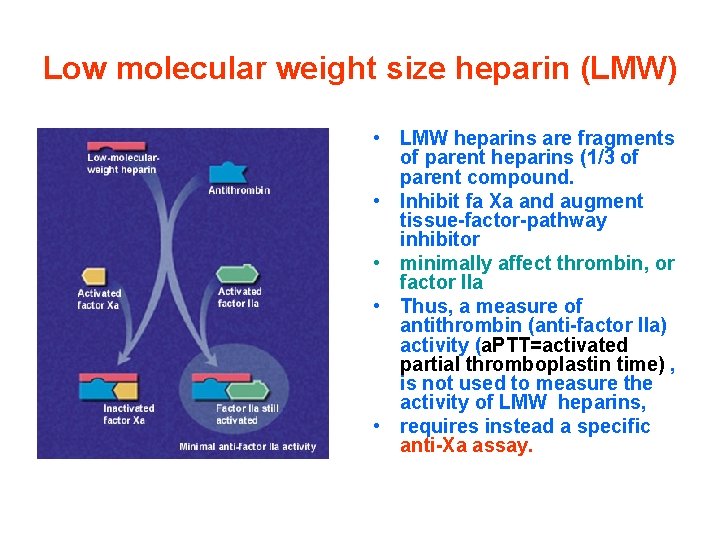
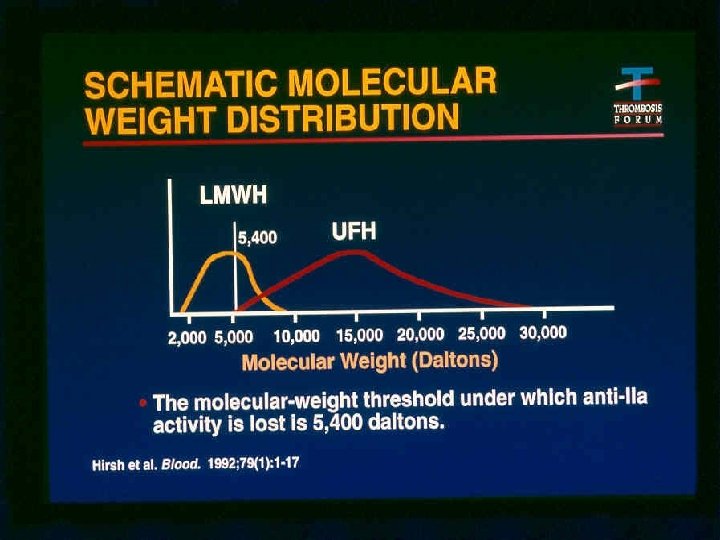
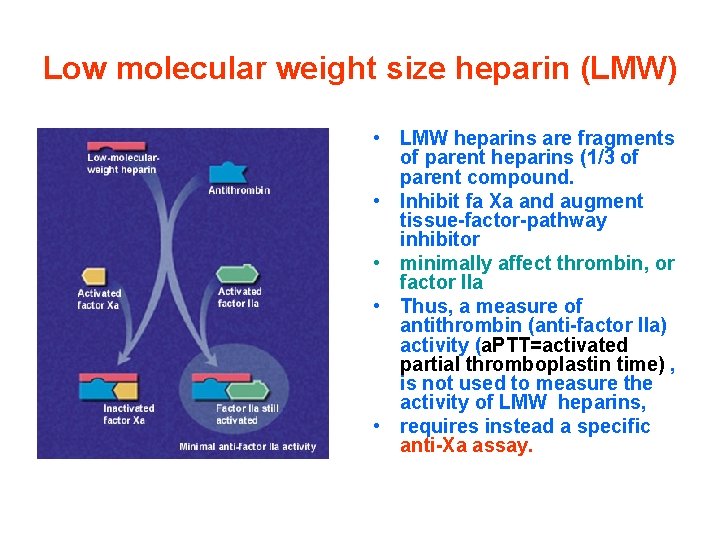
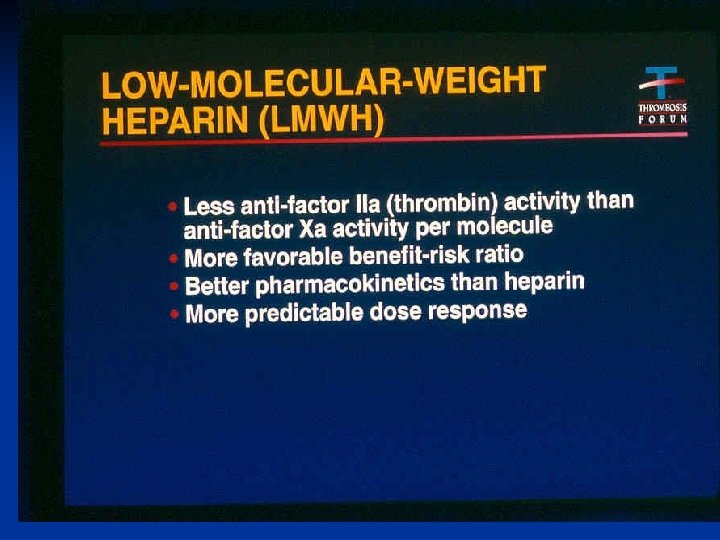
Low molecular weight size heparin (LMW) • LMW heparins are fragments of parent heparins (1/3 of parent compound. • Inhibit fa Xa and augment tissue-factor-pathway inhibitor • minimally affect thrombin, or factor IIa • Thus, a measure of antithrombin (anti-factor IIa) activity (a. PTT=activated partial thromboplastin time) , is not used to measure the activity of LMW heparins, • requires instead a specific anti-Xa assay.
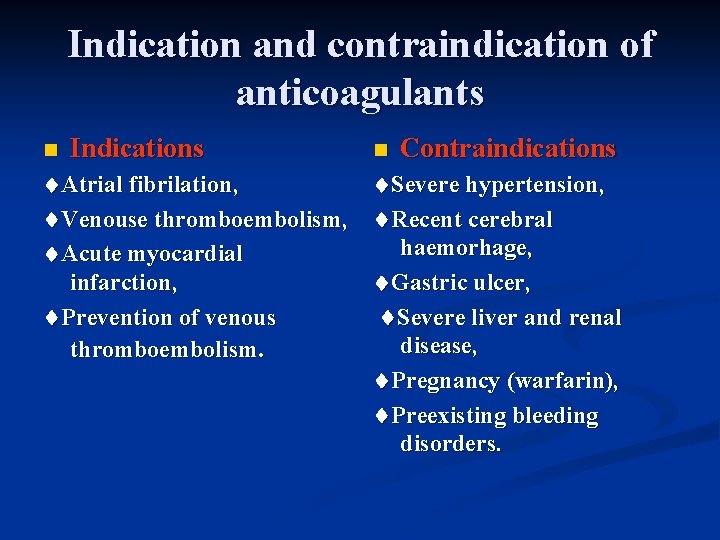
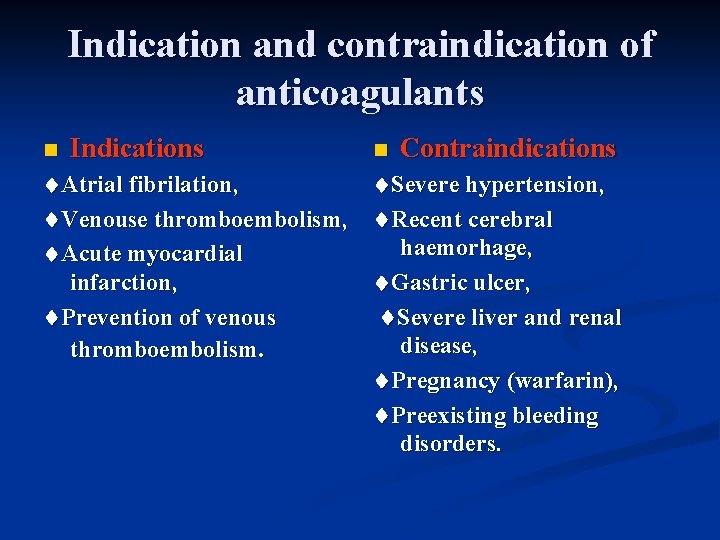
Indication and contraindication of anticoagulants n Indications Atrial fibrilation, Venouse thromboembolism, Acute myocardial infarction, Prevention of venous thromboembolism. n Contraindications Severe hypertension, Recent cerebral haemorhage, Gastric ulcer, Severe liver and renal disease, Pregnancy (warfarin), Preexisting bleeding disorders.
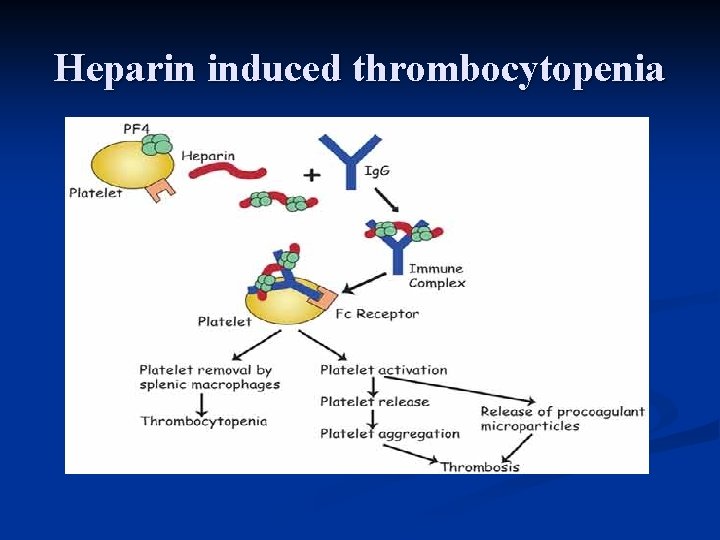
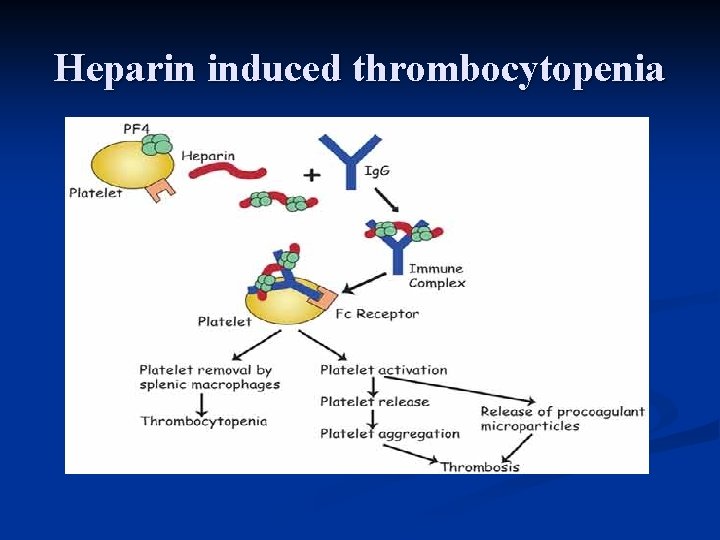
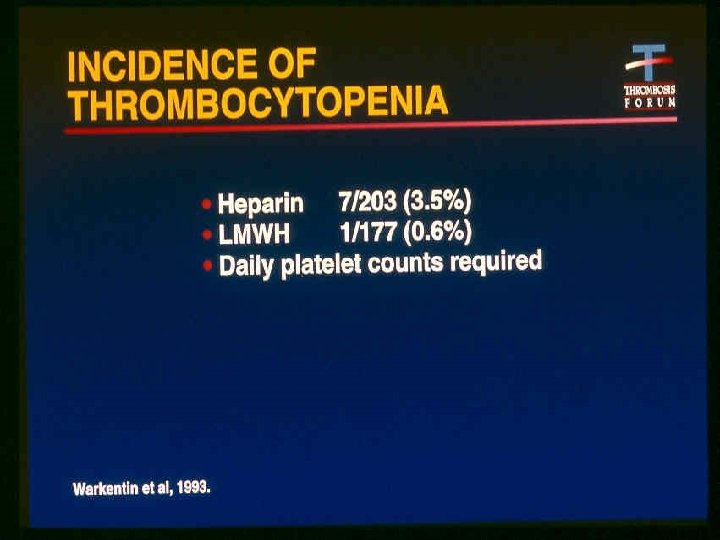
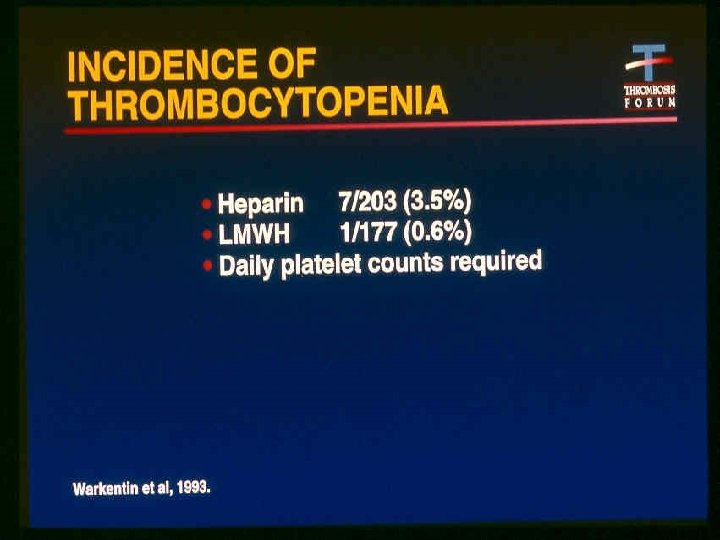
Heparin induced thrombocytopenia
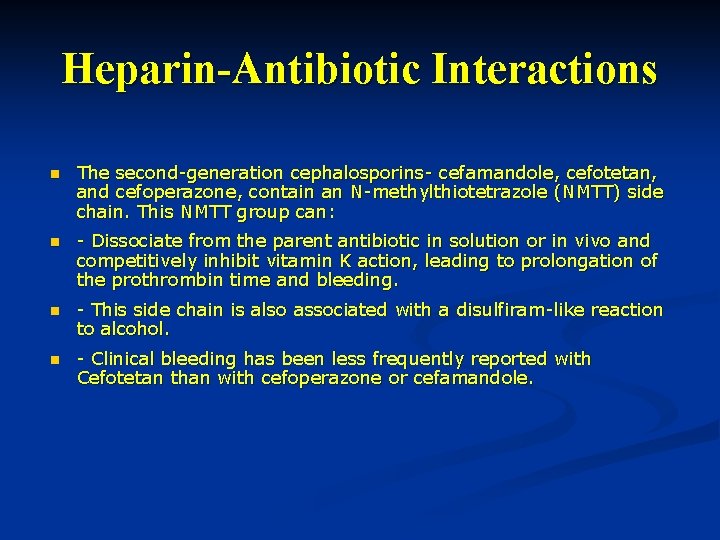
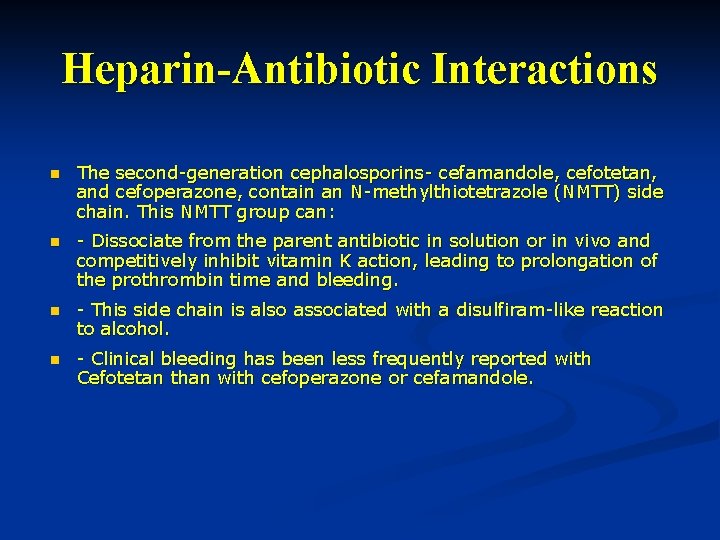
Heparin-Antibiotic Interactions n The second-generation cephalosporins- cefamandole, cefotetan, and cefoperazone, contain an N-methylthiotetrazole (NMTT) side chain. This NMTT group can: n - Dissociate from the parent antibiotic in solution or in vivo and competitively inhibit vitamin K action, leading to prolongation of the prothrombin time and bleeding. n - This side chain is also associated with a disulfiram-like reaction to alcohol. n - Clinical bleeding has been less frequently reported with Cefotetan than with cefoperazone or cefamandole.
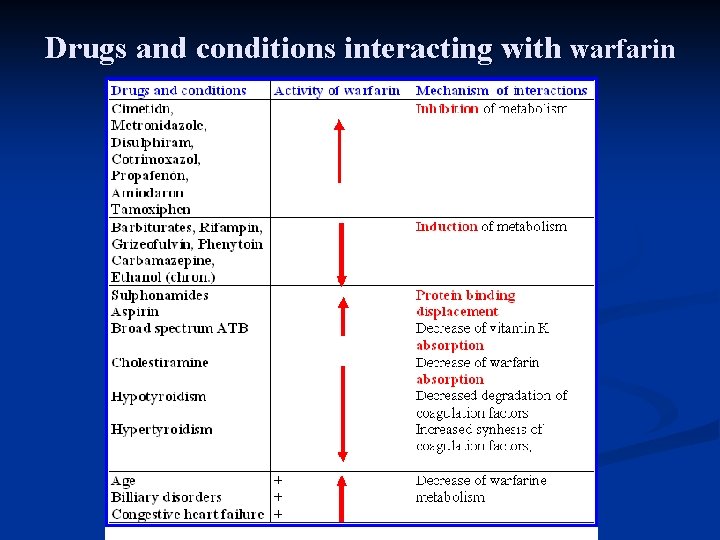
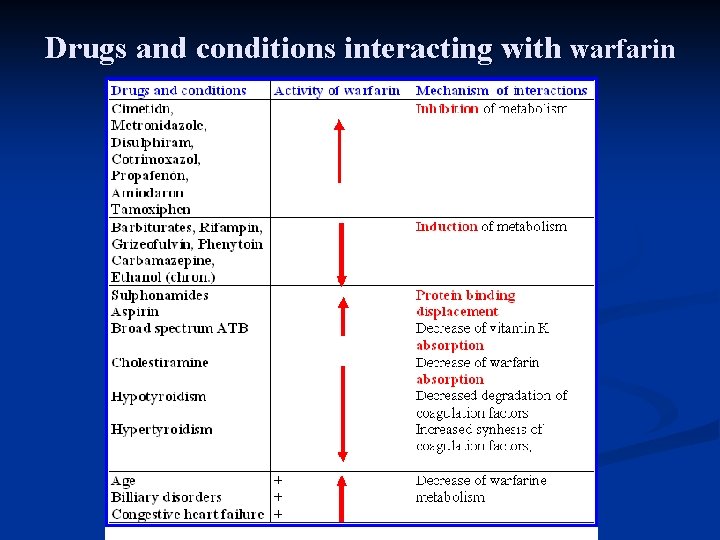
Drugs and conditions interacting with warfarin
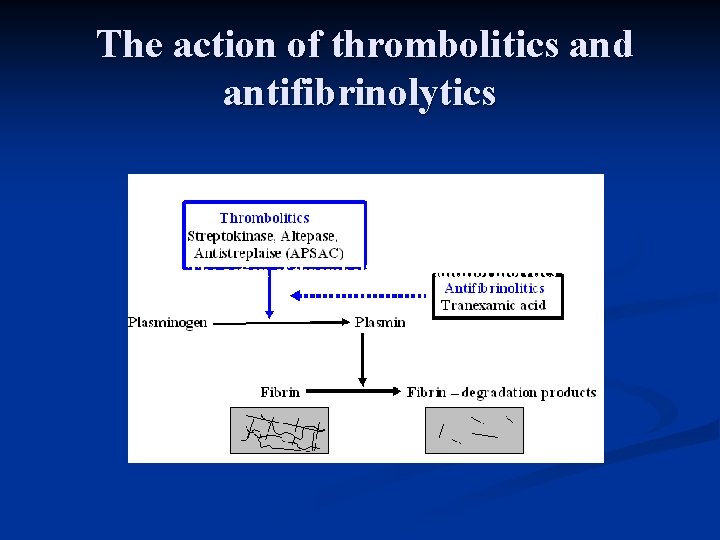
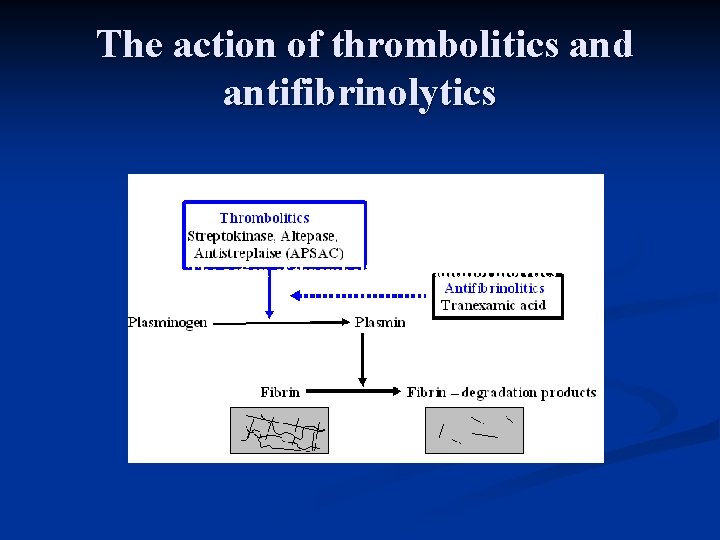
The action of thrombolitics and antifibrinolytics
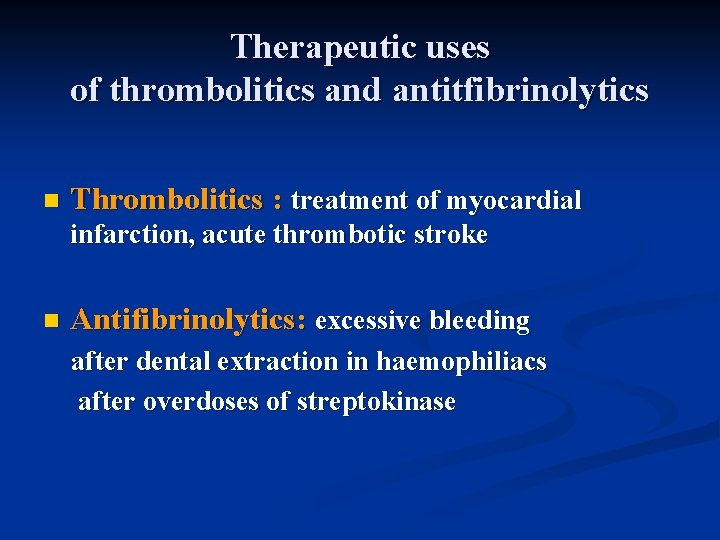
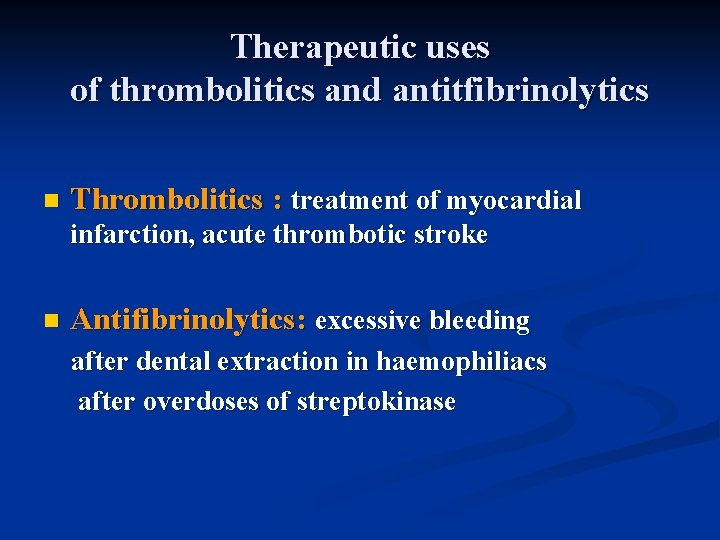
Therapeutic uses of thrombolitics and antitfibrinolytics n Thrombolitics : treatment of myocardial infarction, acute thrombotic stroke n Antifibrinolytics: excessive bleeding after dental extraction in haemophiliacs after overdoses of streptokinase
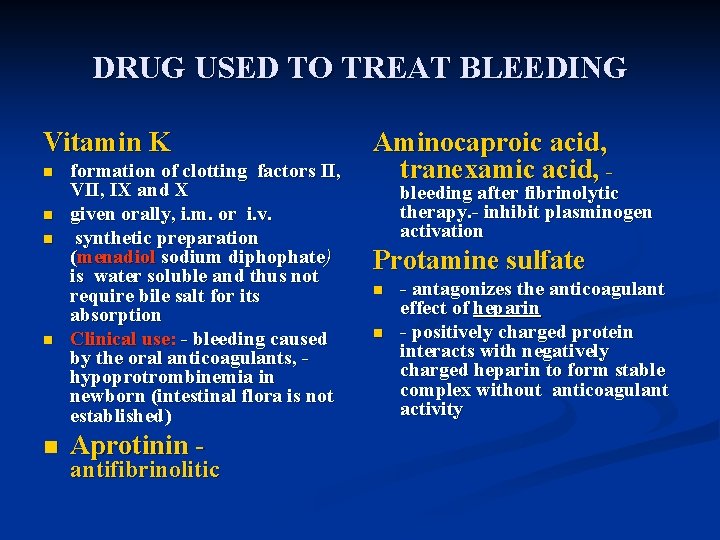
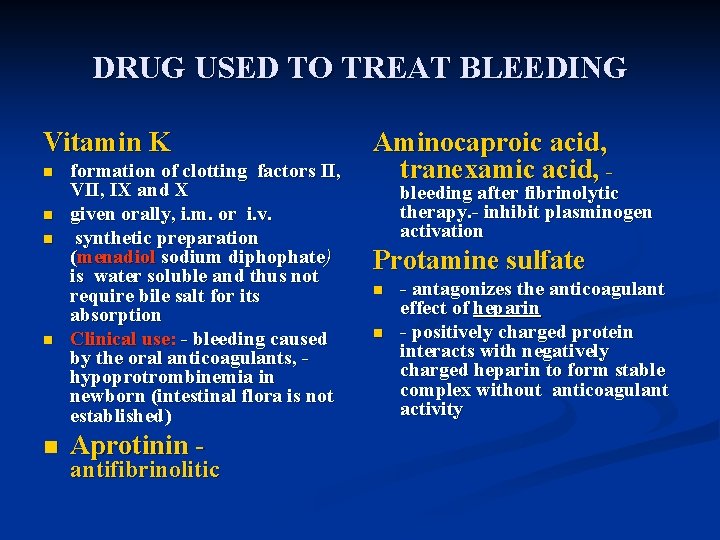
DRUG USED TO TREAT BLEEDING Vitamin K n n n formation of clotting factors II, VII, IX and X given orally, i. m. or i. v. synthetic preparation (menadiol sodium diphophate) is water soluble and thus not require bile salt for its absorption Clinical use: - bleeding caused by the oral anticoagulants, hypoprotrombinemia in newborn (intestinal flora is not established) Aprotinin - antifibrinolitic Aminocaproic acid, tranexamic acid, - bleeding after fibrinolytic therapy. - inhibit plasminogen activation Protamine sulfate n n - antagonizes the anticoagulant effect of heparin - positively charged protein interacts with negatively charged heparin to form stable complex without anticoagulant activity
Antiagregatory drugs (Antiplatelet drugs)
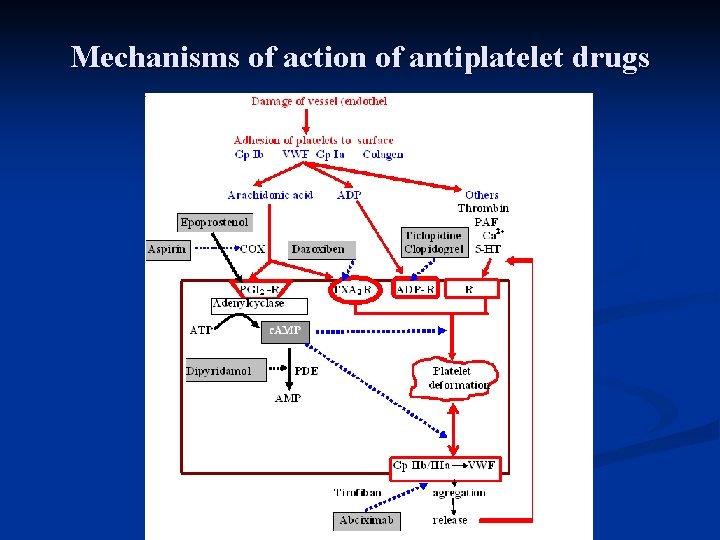
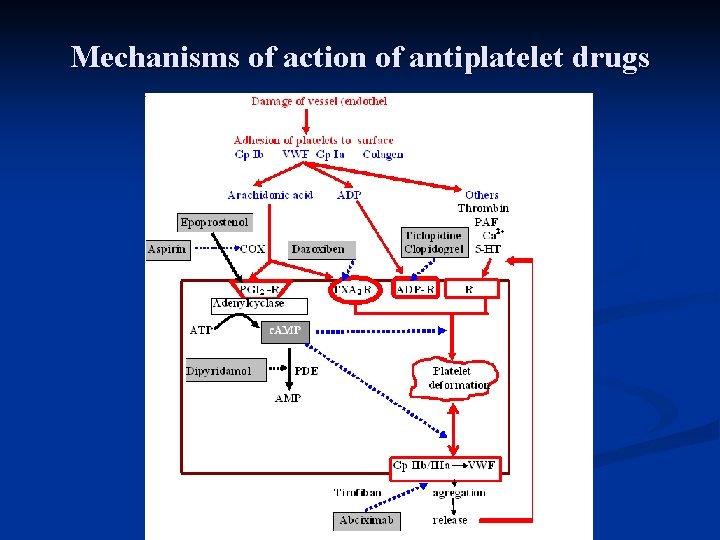
Mechanisms of action of antiplatelet drugs
Antianemic drugs
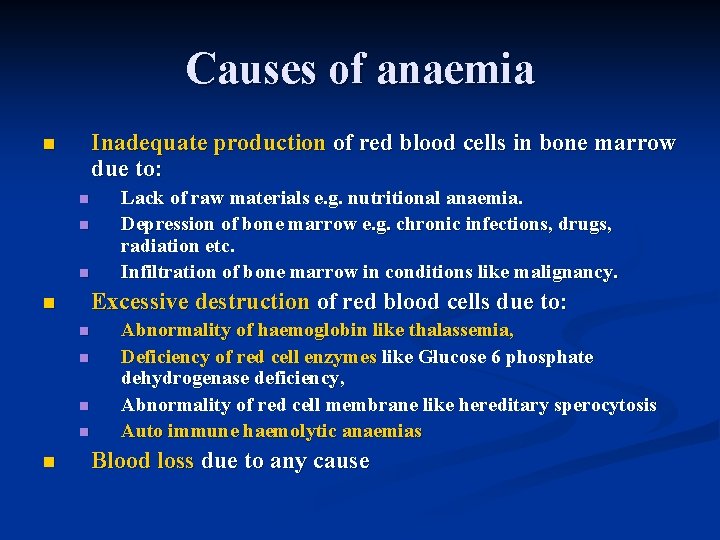
Causes of anaemia Inadequate production of red blood cells in bone marrow due to: n n Excessive destruction of red blood cells due to: n n n Lack of raw materials e. g. nutritional anaemia. Depression of bone marrow e. g. chronic infections, drugs, radiation etc. Infiltration of bone marrow in conditions like malignancy. Abnormality of haemoglobin like thalassemia, Deficiency of red cell enzymes like Glucose 6 phosphate dehydrogenase deficiency, Abnormality of red cell membrane like hereditary sperocytosis Auto immune haemolytic anaemias Blood loss due to any cause
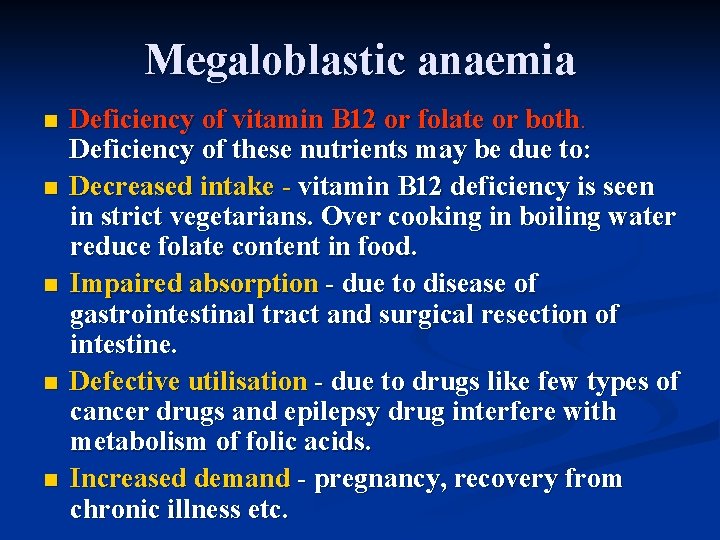
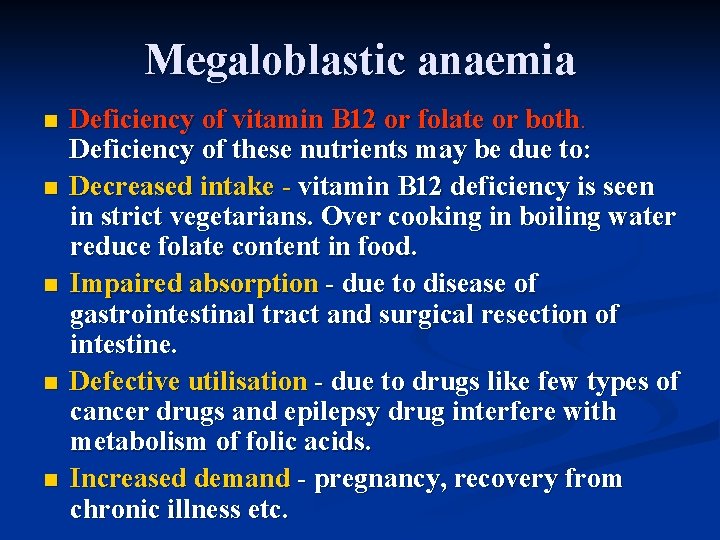
Megaloblastic anaemia n n n Deficiency of vitamin B 12 or folate or both. Deficiency of these nutrients may be due to: Decreased intake - vitamin B 12 deficiency is seen in strict vegetarians. Over cooking in boiling water reduce folate content in food. Impaired absorption - due to disease of gastrointestinal tract and surgical resection of intestine. Defective utilisation - due to drugs like few types of cancer drugs and epilepsy drug interfere with metabolism of folic acids. Increased demand - pregnancy, recovery from chronic illness etc.
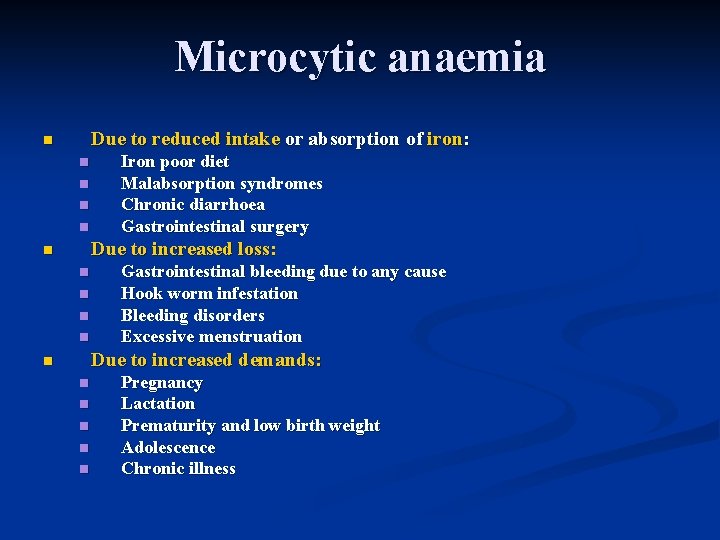
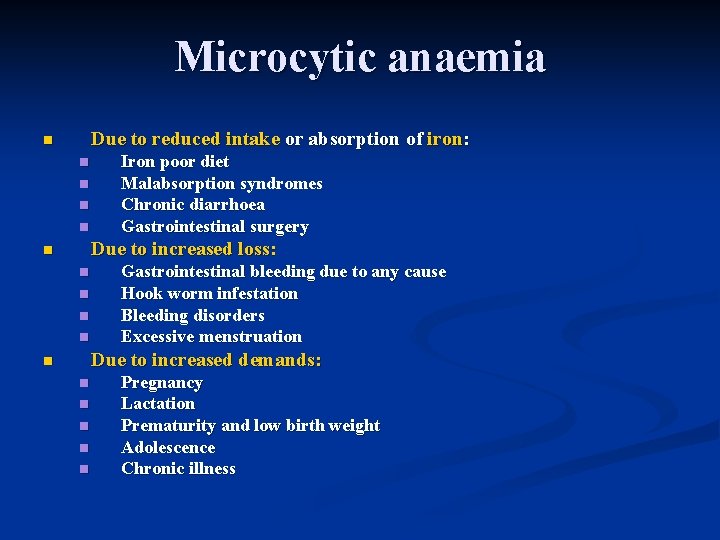
Microcytic anaemia Due to reduced intake or absorption of iron: n n n Iron poor diet Malabsorption syndromes Chronic diarrhoea Gastrointestinal surgery Due to increased loss: n n n Gastrointestinal bleeding due to any cause Hook worm infestation Bleeding disorders Excessive menstruation Due to increased demands: n n n Pregnancy Lactation Prematurity and low birth weight Adolescence Chronic illness
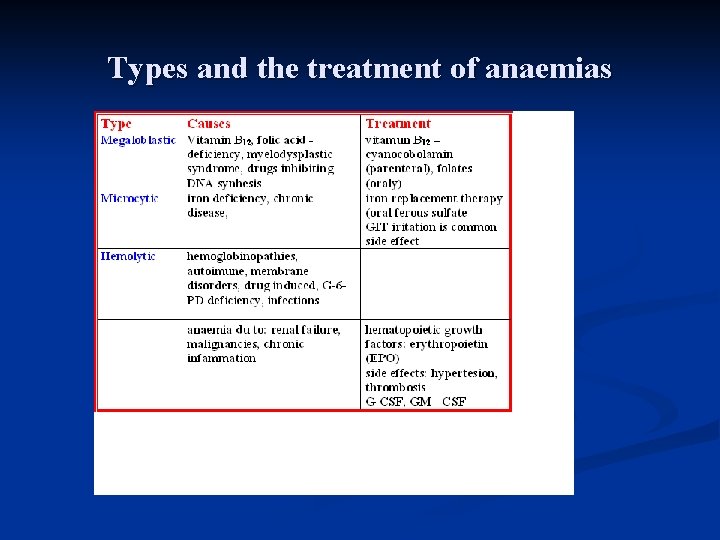
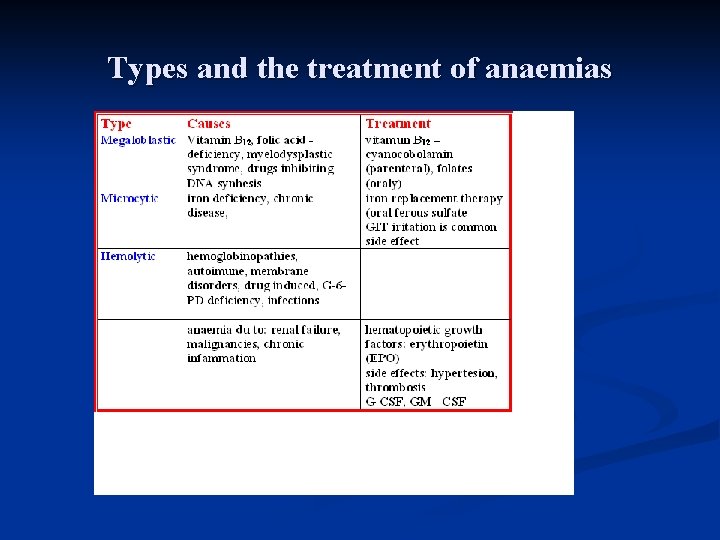
Types and the treatment of anaemias
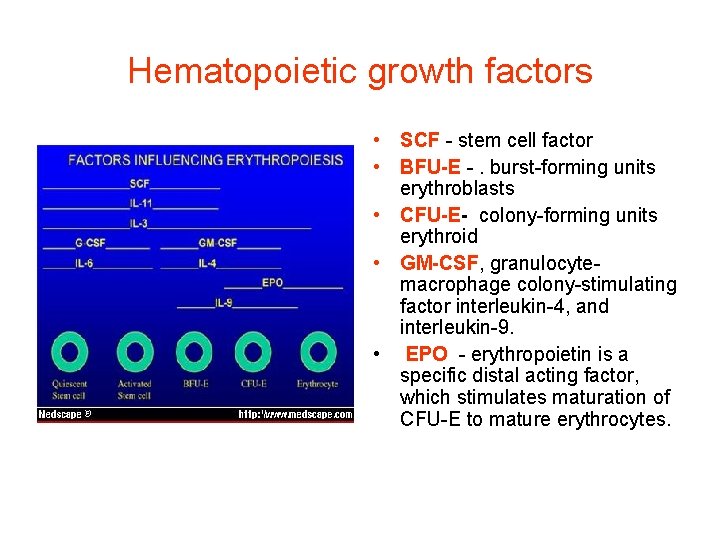
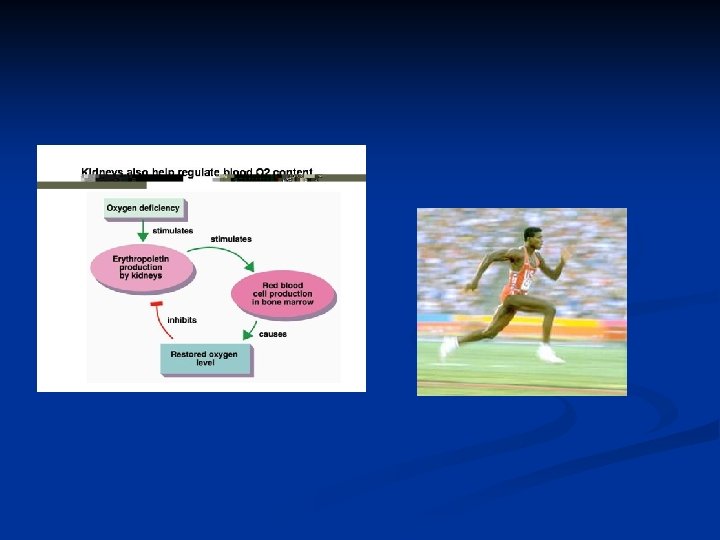
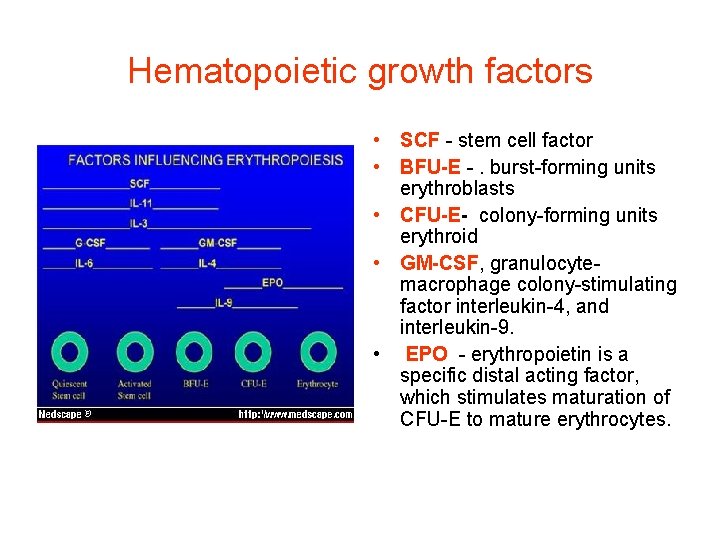
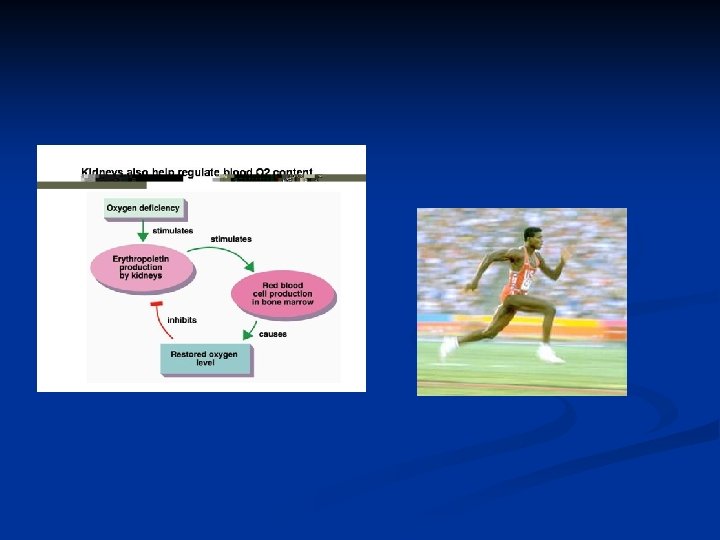
Hematopoietic growth factors • SCF - stem cell factor • BFU-E -. burst-forming units erythroblasts • CFU-E- colony-forming units erythroid • GM-CSF, granulocytemacrophage colony-stimulating factor interleukin-4, and interleukin-9. • EPO - erythropoietin is a specific distal acting factor, which stimulates maturation of CFU-E to mature erythrocytes.
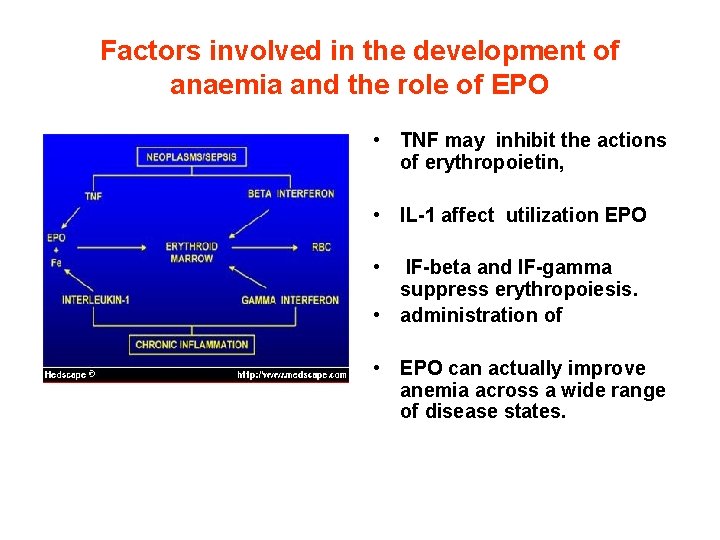
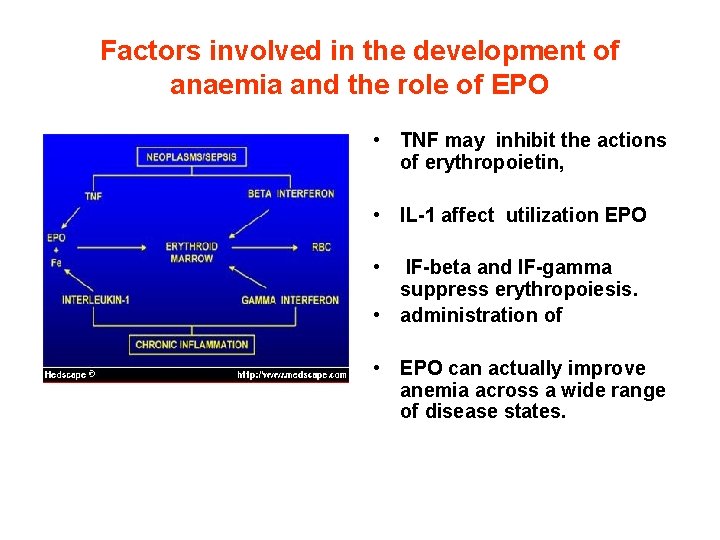
Factors involved in the development of anaemia and the role of EPO • TNF may inhibit the actions of erythropoietin, • IL-1 affect utilization EPO • IF-beta and IF-gamma suppress erythropoiesis. • administration of • EPO can actually improve anemia across a wide range of disease states.