Two Types of Cardiac Defects Congenital anatomic Structural



- Slides: 164
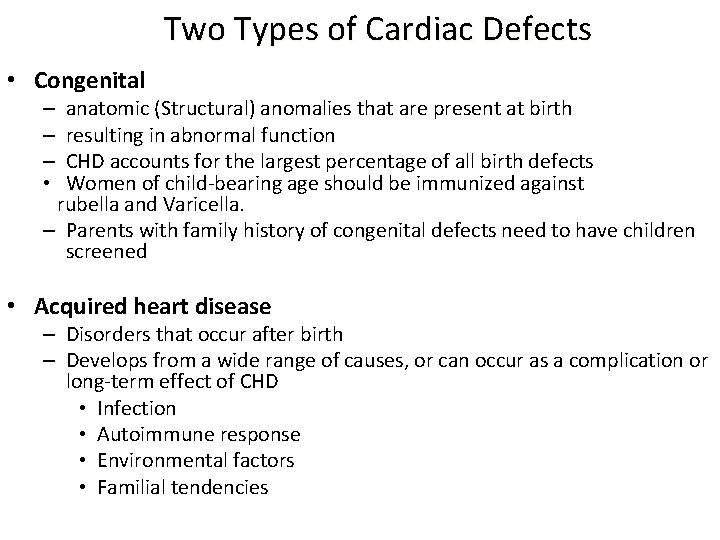
Two Types of Cardiac Defects • Congenital – anatomic (Structural) anomalies that are present at birth – resulting in abnormal function – CHD accounts for the largest percentage of all birth defects • Women of child-bearing age should be immunized against rubella and Varicella. – Parents with family history of congenital defects need to have children screened • Acquired heart disease – Disorders that occur after birth – Develops from a wide range of causes, or can occur as a complication or long-term effect of CHD • Infection • Autoimmune response • Environmental factors • Familial tendencies
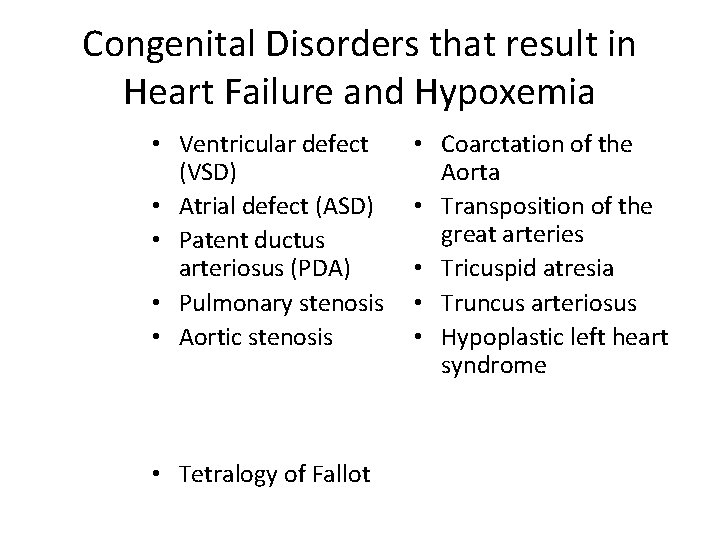
Congenital Disorders that result in Heart Failure and Hypoxemia • Ventricular defect (VSD) • Atrial defect (ASD) • Patent ductus arteriosus (PDA) • Pulmonary stenosis • Aortic stenosis • Tetralogy of Fallot • Coarctation of the Aorta • Transposition of the great arteries • Tricuspid atresia • Truncus arteriosus • Hypoplastic left heart syndrome
Health Promotion and Risk Management • Acquired - Children with hypertension, hyperlipidemia and rheumatic fever are at increased risk. – Rheumatic fever follows a group A betahemolytic streptococcus infection (otitis media, streptococcal Pharyngitis and impetigo should have antibiotic therapy) – Avoid excessive salt, lack of exercise, obesity, diets high in saturated fats (reduce to 30% of calories by school age) – Rheumatic fever – Hyperlipidema
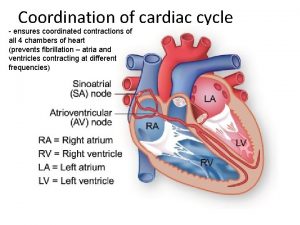
• What is Cardiac Output? – Amount of blood out of ventricle / minute • What is Stroke Volume? – Amount of blood ejected by left Ventricle at systole – Product of Preload, Afterload, and Contractility (inotropy) • Heart Sounds – These are the first heart sound (S 1) and second heart sound (S 2), produced by the closing of the AV valves and semilunar valves respectively.
Review A&P of the Heart Circulation of blood CO = SV x HR CO (squeeze power) is affected by preload, afterload and contractility • Frank-Starling law - SV can be increased by increasing the stretch of the fibers. However, excessive stretch results in a decrease in CO • •

Preload depends on… • Degree of stretch of myocardial fibers before contraction (measured by the central venous pressure (CVP) • By the volume of blood in left ventricle (LV) at end of diastole • Increased volume – increased preload- increased cardiac output (CO) • Decreased volume – decreased preload – decreased cardiac output (CO)
Factors Which Increase Preload • IV fluids • Blood • Vasoconstriction Factors Which Decrease Preload • • Diuretics Dehydration Hemorrhage Vasodilation
Afterload • Resistance or pressure the ventricles must overcome to pump blood out • Left ventricle (LV) affected by systemic vascular resistance (SVR) • Right ventricle (RV) affected by pulmonary vascular resistance (PVR) • Related to arterial pressure or diameter of arteries • As pressure increases, resistance increases, afterload increases • As pressure decreases, resistance decreases, afterload decreases
Autonomic Nervous System (ANS) Regulation of Cardiovascular System • Heart rate – chronotropic effect • Contractility – inotropic effect • Conduction velocity at AV node – dromotropic effect • Afterload - vascular resistance – arterial vasoconstriction and dilation • Preload – venous constriction and dilation
Subdivisions of ANS • Parasympathetic – acetylcholine produces inhibitory response • Sympathetic – catecholamines stimulate – Increase heart rate – Beta 1 receptors – Dilate smooth muscles – Beta 2 receptors – Vasoconstrict vessels – Alpha receptors
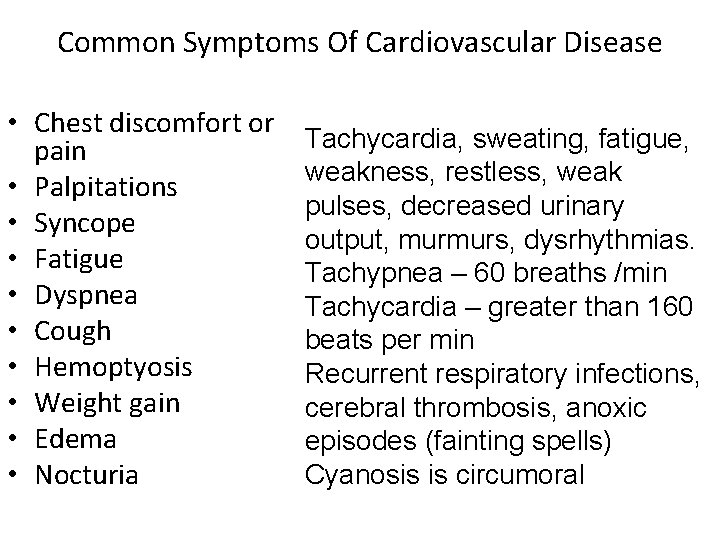
Common Symptoms Of Cardiovascular Disease • Chest discomfort or pain • Palpitations • Syncope • Fatigue • Dyspnea • Cough • Hemoptyosis • Weight gain • Edema • Nocturia Tachycardia, sweating, fatigue, weakness, restless, weak pulses, decreased urinary output, murmurs, dysrhythmias. Tachypnea – 60 breaths /min Tachycardia – greater than 160 beats per min Recurrent respiratory infections, cerebral thrombosis, anoxic episodes (fainting spells) Cyanosis is circumoral
Impaired Myocardial Function: • Pulmonary Congestion: Retractions, flaring nares, exercise intolerance, cough, cyanosis, wheezing, grunting. Orthopnea in recumbent position – increased blood flow from extremities. • Systemic Venous Congestion: Weight gain, hepatomegaly, delayed cap. refill, weak pulses, peripheral edema, ascites, polycythemia
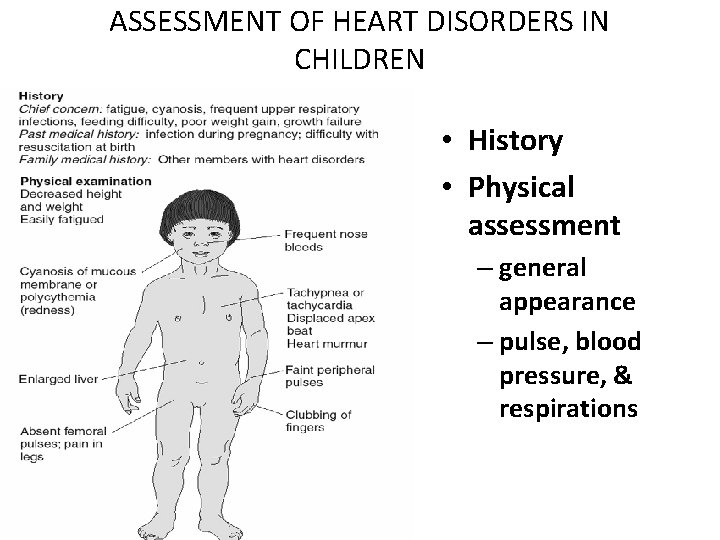
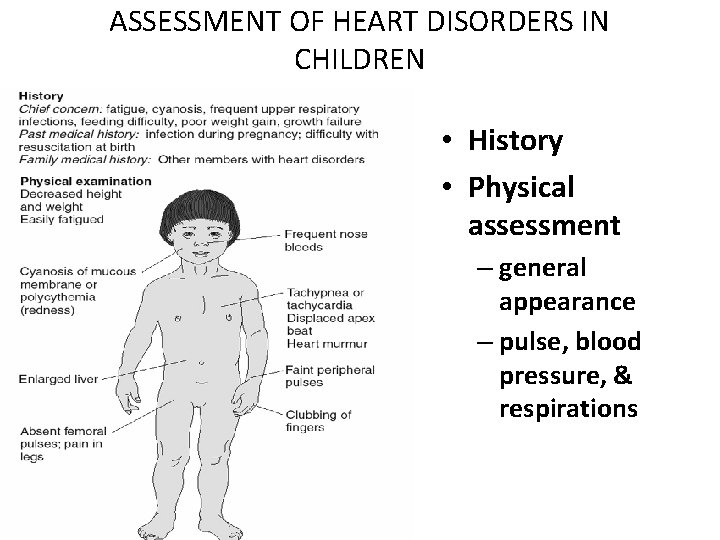
ASSESSMENT OF HEART DISORDERS IN CHILDREN • History • Physical assessment – general appearance – pulse, blood pressure, & respirations
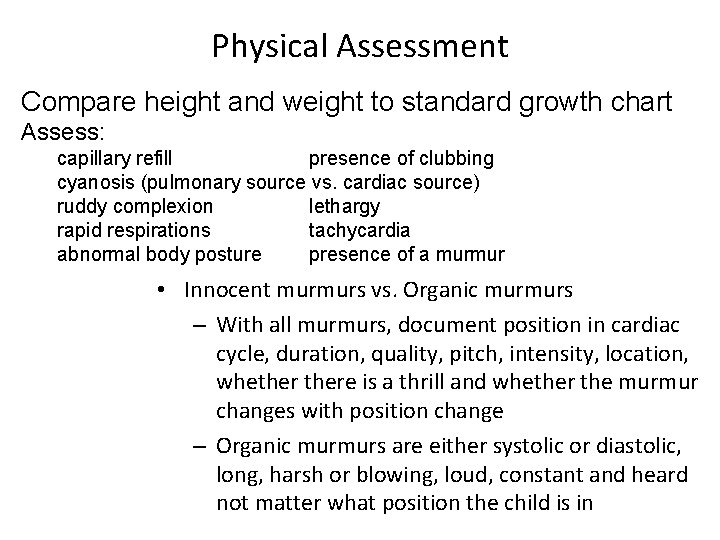
Physical Assessment Compare height and weight to standard growth chart Assess: capillary refill presence of clubbing cyanosis (pulmonary source vs. cardiac source) ruddy complexion lethargy rapid respirations tachycardia abnormal body posture presence of a murmur • Innocent murmurs vs. Organic murmurs – With all murmurs, document position in cardiac cycle, duration, quality, pitch, intensity, location, whethere is a thrill and whether the murmur changes with position change – Organic murmurs are either systolic or diastolic, long, harsh or blowing, loud, constant and heard not matter what position the child is in
Characteristics of Murmurs • Location • Relation to the heart cycle and duration • Intensity: grade I, soft and hard to hear; grade II, soft and easily heard; grade III, loud without thrill; grade IV, loud with a precordial thrill; grade IV, loud, audible with a precordial thrill; grade V, loud, audible with a stethoscope; grade VI, very loud, audible with a stethoscope or with the naked ear • Quality: harsh, musical, or rough; high, medium, or low pitch • Variation with position (sitting, lying, standing)
History Taking • Must be careful. Some of the symptoms are very subtle. • Some symptoms do not show up right after birth • Typical presentations of infants are tachycardia, tachypnea, and poor feeding • Older children may present with fatigue and frequent lower respiratory infections. Some children may perspire excessively • Edema is a late sign and usually presents first as periorbital edema. • May complain of decreased U/O • May have headaches, nose bleeds, high blood pressure in upper extremities
Past Health History • Problems occurring after birth (associated congenital malformation) • Frequent infections • Chromosomal abnormalities • Prematurity • Autoimmune disorders • Use of medications, such as corticosteroids
Health History of the Present Illness • When the symptoms started and how they progressed • Any treatments and medications used at home • History of orthopnea, dyspnea, easy fatigability, growth delays, squatting, edema, dizziness, frequent pneumonia • Poor feeding, fatigue, lethargy, vomiting, failure to thrive • Diaphoresis, delays in motor development, cyanosis, tachypnea
Additional Risk Factors for Cardiovascular Disorders • Family history of heart disease or CHD (investigate the history further if heart disease occurred in a first-degree relative) • Hyperlipidemia • Diabetes mellitus • Obesity • Inactivity • Stress • High-cholesterol diet
History Continued • Obtain a detailed prenatal history including: • exposure to infections (cytomegalovirus, toxoplasmosis, Rubella or Varicella) • medication usage • drug and alcohol use • Nutrition • exposure to radiation • Determine if there is any family history of congenital heart defects or heart disease, cognitive impairments, renal disease
Pediatric Indicators of Cardiac Dysfunction • Poor feeding, failure to thrive, poor weight gain, activity intolerance (sweating with feeds), lethargy • Tachypnea, tachycardia • Cyanosis, pallor • Developmental delays • Positive prenatal history • Positive family history of cardiac disease • Might have hypertension
Signs and Symptoms of a Cardiac Disorder Cyanosis Edema Clubbing Fever Retractions Prominence of precordial chest wall Visible, engorged, or abnormal pulsations • Abdominal distention • •
Medical Management • Lanoxin: Digoxin – Nurse alert – digitalis glycosides, improve contractility, decrease HR: same as in adults. – Don’t forget dig: slows conduction between nodes therefore heart rate and improves contractility, and b/c of all this it helps renal perfusion b/c the body is no longer panicking, and that allows us to diurese. – Infants rarely receive more than 1 ml or. 05 mg of Digoxin – higher than that = dosage error. – ALWAYS compare calculations with another nurse. Not given if pulse is below 90 to 100 in infants and below 70 in children – Compare to previous readings
Medical Management – Serum digoxin levels range from. 8 to 2 ug/L – toxicity – bradycardia and vomiting. • Diuretics [we do give Lasix] • Warning: When your K+ goes down, your dig works better. Diuretics – Lasix: furosemide, Diuril: chlorothiazide, Aldactone: spironolactone • Ace inhibitors: ACE inhibitors -Angiotensinconverting enzyme inhibitors vasodilation results in decreased pulmonary and systemic vascular resistance.
Medical Management • Beta Blockers: beta blocker decreases HR, B/P and causes vasodilation • Vaccinations – prevent infections: you don’t want these kids getting sick • Improve Tissue Oxygenation: how do we do it in babies and kids? – Give O 2 – Keep’em rested – Don’t let them cry – Small frequent feedings due to energy expense – Put them up in bed, sit them upright.
Drug Guide • • • Alprostadil Digoxin Furosemide Heparin Indomethacin Spironlactone • • Antibiotics Penicillin G Penicillin V potassium Erythromycin • • Antihypertensives ACE inhibitors B-adrenergic blockers Hydralazine
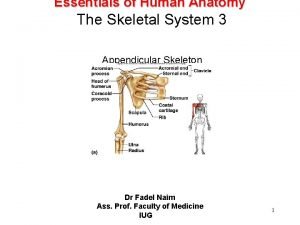
Preoperative Assessments Cardiac Surgery • Temperature and weight measurements • Examination of extremities for peripheral edema, clubbing, and evaluation of peripheral pulses • Auscultation of the heart (rate, rhythm, heart sounds, murmurs, clicks, and rubs) • Respiratory assessment, including respiratory rate, work of breathing, and auscultation of the lungs for breath sounds
Cardiac Surgery • Pre-op – baseline vital signs at rest (count a full minute) – height and weight – hold digoxin for 24 hrs – enema – patient and family teaching (surgery, equipment, what to expect after surgery, tubes, the importance of deep breathing and coughing)
Cardiac Surgery • Post-op – VS every 15 minutes progressing to q 1 hr, ventilatory support, monitoring of heart rate and rhythm, BP, heart pressures, heart sounds, UOP, fluid status, ABG’s, PT, PTT, Plt, Hgb, Hct. , K, Na, O 2 sat, lung sounds, bowel sounds, measurement of chest tube integrity and drainage
Cardiac Surgery (Cont’d) • Incentive spirometry (deep breathing) and coughing after extubated • Pain management • Explain procedures (extubation, chest tube removal, etc. ) • Administer antibiotics • Observe for signs and symptoms of infection • May need warming immediately post-op, but watch for temperature elevation • Assess for hypervolemia • Advance activities as tolerated • Avoid arm pulling and pulling with arms
Cardiac Surgery (Cont’d) • Complications – Bleeding – Shock – heart block or arrhythmias – heart failure – neuro changes – postcardiac surgery syndrome (febrile illness with pericarditis and pleurisy - one week post-op) – postperfusion syndrome (3 -12 weeks post-op - fever, splenomegaly, hepatomegaly, elevated WBC, malaise, maculopapular rash - CMV from donor blood)
Cardiac Surgery Cont’d • If valve replacement surgery - artificial valves are used more often, requires anticoagulation (Coumadin) or antiplatelet (aspirin, dipyridamole) therapy young girls should avoid accidental pregnancy, should not use an estrogen-based OCD nor an IUD – women desiring to become pregnant need to switch to Heparin therapy – prophylactic antibiotics need to be taken before dental work or oral surgery – may develop hemolytic anemia requiring blood transfusions
Cardiac Surgery Parent Teaching • Heart anatomy and its function – Activity Tolerance; • Events before surgery – No Bike Riding Until Sternotomy • Location of the child Healed after surgery – Signs & Symptoms of Wound • Appearance of the child Infection after surgery – Return to School in 2 Weeks • Location of the incision – Usually, No Further Cardiovascular and coverage with Problems dressings • ALLOW THE CHILD TO LIVE A • Postoperative activity NORMAL AND ACTIVE LIFE! level • Nutritional restrictions • Medications • Discharge Teaching:
Cardiac Surgery Cont’d • Pacemaker - if difficulty with conduction system – Consists of a battery pack and lead wires – Leads are usually epicardial as opposed to endocardial in children – Parents and patient must be taught how to take the patient’s pulse – Batteries can last up to 15 years and they lose power slowly rather than stopping abruptly – If patient has hiccuping, lead wire may need to be repositioned – Magnets should be avoided
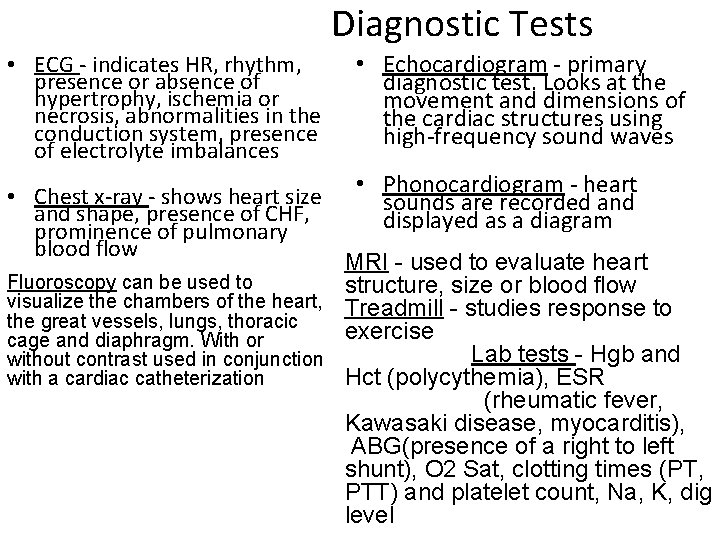
Diagnostic Tests • ECG - indicates HR, rhythm, presence or absence of hypertrophy, ischemia or necrosis, abnormalities in the conduction system, presence of electrolyte imbalances • Chest x-ray - shows heart size and shape, presence of CHF, prominence of pulmonary blood flow • Echocardiogram - primary diagnostic test. Looks at the movement and dimensions of the cardiac structures using high-frequency sound waves • Phonocardiogram - heart sounds are recorded and displayed as a diagram MRI - used to evaluate heart Fluoroscopy can be used to structure, size or blood flow visualize the chambers of the heart, Treadmill - studies response to the great vessels, lungs, thoracic exercise cage and diaphragm. With or Lab tests - Hgb and without contrast used in conjunction Hct (polycythemia), ESR with a cardiac catheterization (rheumatic fever, Kawasaki disease, myocarditis), ABG(presence of a right to left shunt), O 2 Sat, clotting times (PT, PTT) and platelet count, Na, K, dig level
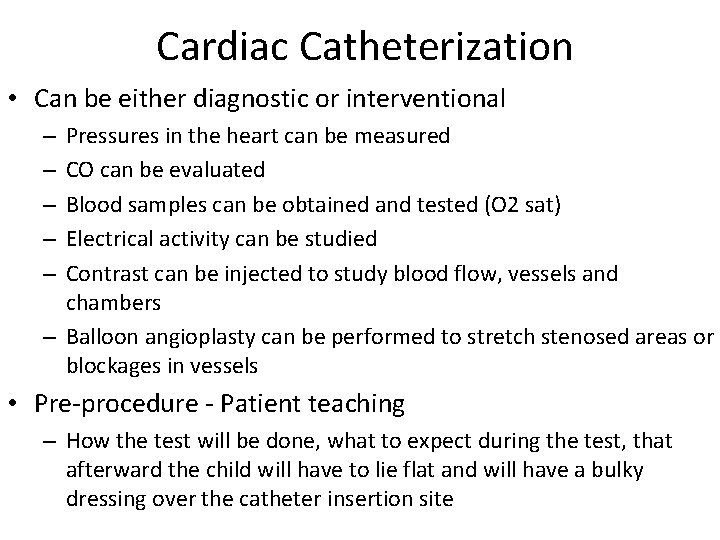
Cardiac Catheterization • Can be either diagnostic or interventional Pressures in the heart can be measured CO can be evaluated Blood samples can be obtained and tested (O 2 sat) Electrical activity can be studied Contrast can be injected to study blood flow, vessels and chambers – Balloon angioplasty can be performed to stretch stenosed areas or blockages in vessels – – – • Pre-procedure - Patient teaching – How the test will be done, what to expect during the test, that afterward the child will have to lie flat and will have a bulky dressing over the catheter insertion site
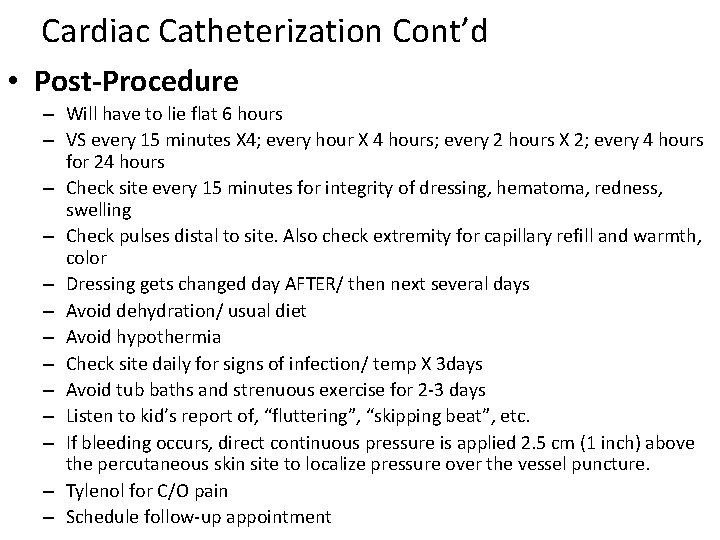
Cardiac Catheterization Cont’d • Post-Procedure – Will have to lie flat 6 hours – VS every 15 minutes X 4; every hour X 4 hours; every 2 hours X 2; every 4 hours for 24 hours – Check site every 15 minutes for integrity of dressing, hematoma, redness, swelling – Check pulses distal to site. Also check extremity for capillary refill and warmth, color – Dressing gets changed day AFTER/ then next several days – Avoid dehydration/ usual diet – Avoid hypothermia – Check site daily for signs of infection/ temp X 3 days – Avoid tub baths and strenuous exercise for 2 -3 days – Listen to kid’s report of, “fluttering”, “skipping beat”, etc. – If bleeding occurs, direct continuous pressure is applied 2. 5 cm (1 inch) above the percutaneous skin site to localize pressure over the vessel puncture. – Tylenol for C/O pain – Schedule follow-up appointment
Focus of Nursing Care for Child With a Cardiac Disorder • Improving oxygenation • Promoting adequate nutrition • Assisting the child and family with coping • Providing postoperative nursing care • Preventing infection • Providing child and family education
Focus of Nursing Care for Child With a Cardiac Disorder • Increasing cardiac output – Monitor VS closely – Monitor cardiac rhythm – Observe S/S hypoxia • Tachypnea • Cyanosis • Tachycardia • Bradycardia • Dizziness/ restlessness – Administer oxygen as needed to correct hypoxia – Knee-to-chest or squatting position to increase systemic vascular resistance
Focus of Nursing Care for Child With a Cardiac Disorder • Increasing cardiac output (cont) – Administer antiarrhythmic, vasopressors, ACE inhibitors, beta blockade, corticosteroids or diuretics to improve cardiac output • Monitor for signs of thrombosis • Redness, Hematuria • Seizure, Coma • Oliguria, anuria • Edema • Paralysis – Administer adequate hydration to decrease possibility of thrombus formation – Cluster nursing care to allow rest – Anticipate child’s needs to decrease stress, which decreases oxygen consumption requirement
Focus of Nursing Care for Child With a Cardiac Disorder • Encouraging Fluid Loss – Weigh daily – Monitor location and extent of edema Measure abdominal growth is ascites present Protect edematous areas of skin Auscultate lungs to identify any crackles Assess WOB and RR Assess heart sounds for gallop (S 3) Strict I and O Sodium-restricted diet Administer diuretics and monitor for adverse effects (lytes imbalance orthostatic hypotension) • •
Focus of Nursing Care for Child With a Cardiac Disorder • Promoting Tissue Perfusion – Assess LOC, pulse, BP, peripheral perfusion, and skin color – Administer cardiac glycosides or vasodilation – Monitor pulse oximetry and arterial blood gas – Supplement oxygen – Monitor H/H – Strictly assess I and O – Position HOB elevated – Change position every 2 hours to promote circulation and avoid sin breakdown
Focus of Nursing Care for Child With a Cardiac Disorder • Promoting adequate nutrition – Determine body weight and length/height norm for age – Assess for food preferences that fall into dietary limitations – Weigh child daily or weekly – Offer highest-calorie meals at the time of day when child’s appetite is greatest (as much as 150 calories/kg/day) – Provide increased calorie shakes or puddings within diet restrictions – Provide small frequent meals (decreases tiring)
Focus of Nursing Care for Child With a Cardiac Disorder • Promoting adequate nutrition (cont) – Feed infants with special nipple as needed to decrease amount of energy expended for sucking – Administer vitamin and mineral supplements as prescribed to attain/maintain vitamin and mineral balance Monitor Cardiac Tolerance Tachycardia Tachypnea Desaturation Gavage Feedings PRN 45
Focus of Nursing Care for Child With a Cardiac Disorder • Promoting appropriate development – Promote adequate caloric intake – Provide age-appropriate developmental activities – Consult with the physical or occupational therapist or child life specialist – Schedule daily activities to allow for essential rest periods – Encourage parents, teachers, and playmates to be sensitive to child’s self image, using positive comments – As energy allows, encourage participation in all activities as feasible
Focus of Nursing Care for Child With a Cardiac Disorder • Preventing infections – Maintain strict hand hygiene to prevent spread – Assess temperature – Avoid contact with persons with known infections – Ensure appropriate immunization, including pneumococcal and influenza vaccines – Administer prophylactic antibiotics prior to all dental procedures, surgical, or any other invasive procedures – Encourage good dental hygiene
Focus of Nursing Care for Child With a Cardiac Disorder • Promoting family processes – Provide ongoing support to the child and family – Encourage parents and family members to verbalize concerns related to child’s illness, diagnosis, and prognosis – Allow families to grieve over the loss of “normal” or “perfect” child – Explain therapies, procedures, child’s behaviors, and plan of care to parents – Encourage parents to be involved in care – Identify support system for family and child – Educate family and child on additional resources available – Encourage parents to seek genetic counseling
Important Points about Care of the Child with a Heart Defect • Parents taking a child with a heart defect home should have discharge planning which includes name/number of a primary care provider, emergency numbers, home health visits, instruction in what to do if child becomes cyanotic, CPR training, • Should not allow a child with a cyanotic heart defect or severe aortic stenosis to cry for extended periods of time • Don’t usually have to restrict sodium intake (regulates water balance)
Important Points about Care Cont’d • Need vitamin supplements and maybe an iron supplement • May need small feedings every 3 -4 hours. May require feeding tubes or high calorie formulas/supplements • Children usually limit their own activities, but parents should watch for respiratory distress when new activities are introduced • Children should receive their immunizations timely • Even minor illnesses should be treated promptly • Avoid dehydration • Receive prophylactic antibiotics prior to dental visits or oral surgery (Penicillin or Erythromycin)
Nursing Factors (cont. . ) • The newborn heart rates are too rapid to hear extra sounds of abnormal circulation. • Infants with heart disease generally have tachycardia, tachypnea, poor feeding (because of rapid breathing and the need to rest during feeding), and they also tire easily. • In children with persistent hypoxia, polycythemia develops. Dehydration must be prevented in hypoxemic children because it potentiates the risk of strokes. • Children with congenital heart disease often prefer the knee-chest position and older children prefer the squat position.
• These positions are preferred because it traps blood in lower extremities which allows the child to oxygenate the blood supply in the upper body more fully and easier. • Children with left to right shunts tend to perspire excessively because of sympathetic nerve stimulation. • Edema is a late sign with periorbital edema occurring first. • Cyanosis occurs if a shunt allows deoxygenated blood to enter the arterial system such infants generally fail to thrive and are below normal weight and height. • Children with Coarctation of the aorta have high blood pressure in the head and upper extremities. • They have a history of nose bleeds, headaches and Low blood pressure in the lower extremities and leg pain on running or exercise of lower extremities.
• Inspect toes and fingers for clubbing and for color. • Press of the finger nail, it should blanch white and then quickly pinken in the child with good oxygenation. • Blanching > 5 seconds indicates poor circulation • A ruby complexion appears in children with heart disease because of the over production of RBCs to better oxygenate body cells • Watch for signs that the heart is an ineffective pump such as – Lethargy – Rapid respiration – Abnormal body postures
• Tachycardia is a pulse rate more than 160 bpm in an infant. • Tachycardia is a pulse rate more than 100 bpm in a 3 year old. • An increase in pulse rate over these standards needs further investigation. • Tachycardia is significant if it persists during sleep or none excitement. • Because a major part of the physical assessment will include inspection, palpation, and auscultation of the chest for heart function. • It is important that the child be relaxed and not crying. • Provide a toy, age appropriate or bottle if hungry to distract the child • Playing with child before the exam may be helpful.
Nursing Factors cont. . • Inspect the child for cyanosis • Check the mouth for cyanosis which can be recognized in the newborn in the tongue and mucous membranes • After birth check for acrocyanosis. • Acrocyanosis lasting more than 20 minutes after birth suggest cardiopulmonary dysfunction. • Increase cyanosis with crying suggest cardiac dysfunction • Decreased cyanosis with crying suggest pulmonary dysfunction. • This is because crying deepens respiration. • Hgb below 4 to 6 gms/100 ml may not show cyanosis. Severe anemia masks cyanosis.
Psychosocial Interventions • Explain all that is happening with the child, using language the parents and child can understand. • Allow the parents and child to voice their feelings, concerns, or questions. • Provide ample time to address questions and concerns. • Encourage the parents and the child, as developmentally appropriate, to participate in the child’s care.
Nursing Care Teaching Guidelines • Give Meds as prescribed, exactly as prescribed • Weigh at least once a week, same scale, consistent clothes • Allow child to engage in activities as directed. Providing rest periods frequently • Provide nutritious, taking into account any • restrictions for fluids or foods • Use measures to prevent infection, such as frequent hand washing, prophylactic antibiotics, and skin care.
Nursing Care Teaching Guidelines • Adhere to schedule for follow-up diagnostic tests and procedures • Use available community resources • Notify provider if child has increasing episodes of respiratory distress, cyanosis, or difficulty breathing, fever, increased edema of hands, feet, or face. • Notify provider of decreased urinary output, weight loss or difficulty eating or drinking, increased fatigue or irritability, decreased level of alertness, or vomiting or diarrhea.
Congestive Heart Failure Nursing care depends on severity of CHF Heart no longer a good pump Blood backflow Congestion fills periphery with resultant fluid in the tissues and lungs and liver • dysrhythmias, cardiomyopathy or • Kawasaki’s disease can cause CHF • •
Congestive Heart Failure Signs and Symptoms • • Poor feeding Poor growth Irritability SOA or activity intolerance • Excessive sweating • Enlarged liver • Edema – Puffy eyes – Hands and feet – Bulging fontanelle
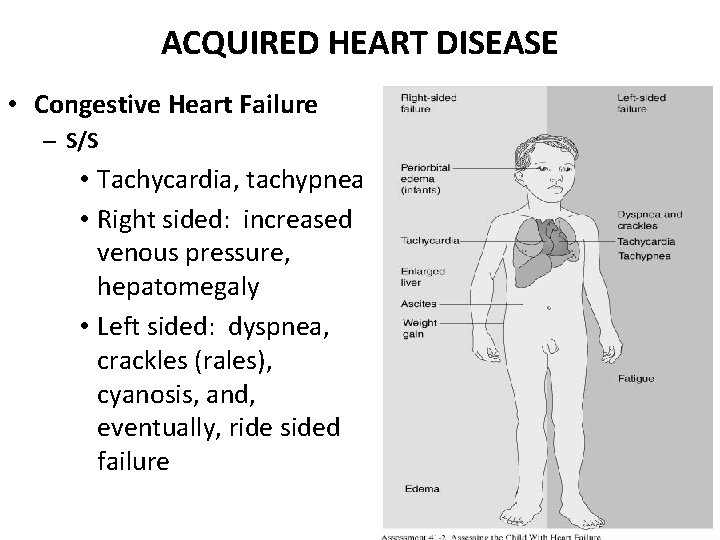
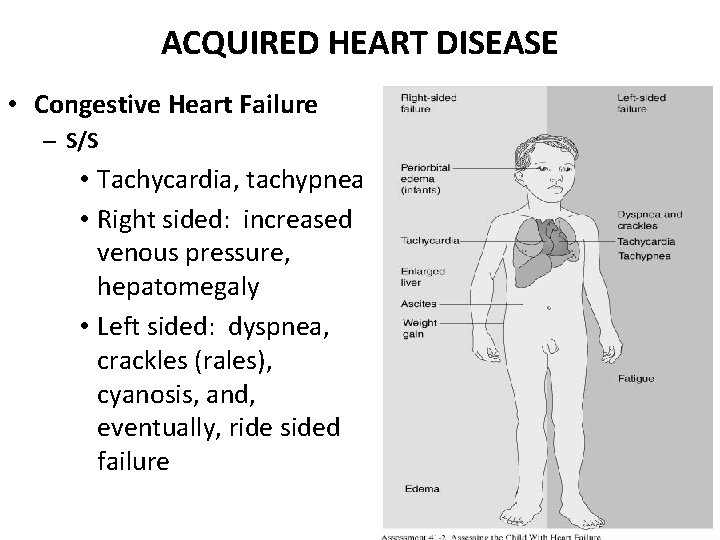
ACQUIRED HEART DISEASE • Congestive Heart Failure – S/S • Tachycardia, tachypnea • Right sided: increased venous pressure, hepatomegaly • Left sided: dyspnea, crackles (rales), cyanosis, and, eventually, ride sided failure
Congestive Heart Failure Diagnosis • Patient history and physical • Confirmed by exam echocardiogram, chest x • BP and pulses may be ray and ECG diminished • Treatment is aimed at: • Weight gain • Breath sound changes – B-type natriuretic peptide – Chest x-ray exam – Exercise test – Echocardiogram – MRI – Cardiac Catheterization – improving cardiac function – removing accumulated fluid and sodium – decrease cardiac demands – improve tissue O 2 – Therapeutic management • Reduce workload of the heart using diuretics, inotropics, and vasodilators
Congestive Heart Failure Nursing Care • Keep Kid Komfortable !!!! • Fluid restrict not usually recommended WHY? ? ? • Oxygenation • Good skin care • Careful monitoring
Heart Failure Cont’d • Diuretics (furosemide) to decrease preload – Lasix, spironalactone, thiazides (may need K replacement) • Improve contractility – Digoxin (given a loading dose and then a maintenance dose, dig level should be 0. 8 to 2. 0 u/L, toxicity includes, nausea, vomiting, anorexia, slow heart rate, family teaching required, hold dose if HR < 90 for infants and toddlers, <70 for older children or <60 for adolescents) • Decrease afterload - hydralazine (vasodilator), nifedipine (Ca channel blocker), nipride (vasodilator), or captopril (ACE inhibitor) • Dopamine used to increase contractility • Vasodilators like captopril (Capoten) or enalapril (Vasotec) to decrease afterload
Congestive Heart Failure Education/Discharge Instructions Monitoring vital signs Recognition of adverse signs and symptoms Side effects of meds Good exercise plan helps to keep heart muscle stronger and helps prevent CHF • •
How does the fetus receive sufficient oxygen from the maternal blood supply? • Fetal hemoglobin • FHR present day 17 carries 20 -30% more • Chambers and oxygen than maternal hemoglobin arteries formed during weeks 2 • Fetal hemoglobin concentration is 50% through 8. greater than mother’s • Placenta is • Fetal heart rate 120 oxygenator 160 bpm (increases cardiac output)
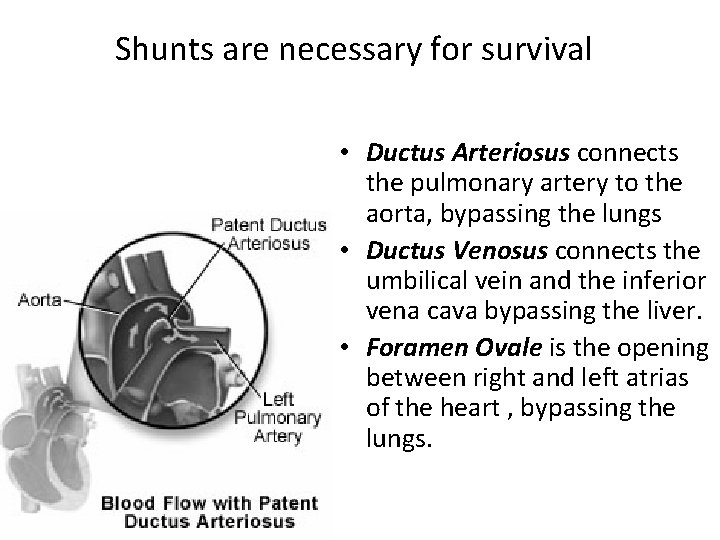
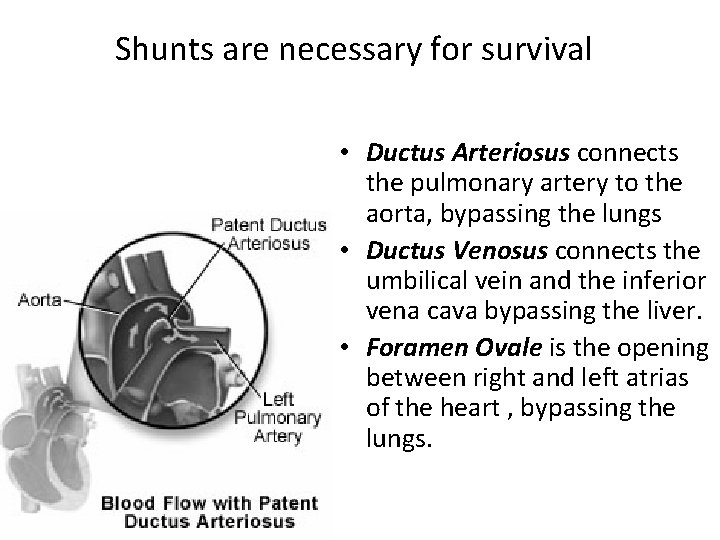
Shunts are necessary for survival • Ductus Arteriosus connects the pulmonary artery to the aorta, bypassing the lungs • Ductus Venosus connects the umbilical vein and the inferior vena cava bypassing the liver. • Foramen Ovale is the opening between right and left atrias of the heart , bypassing the lungs.
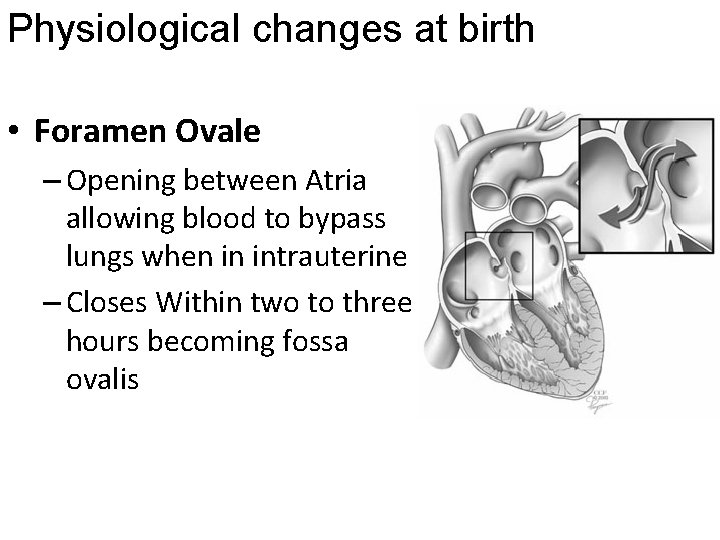
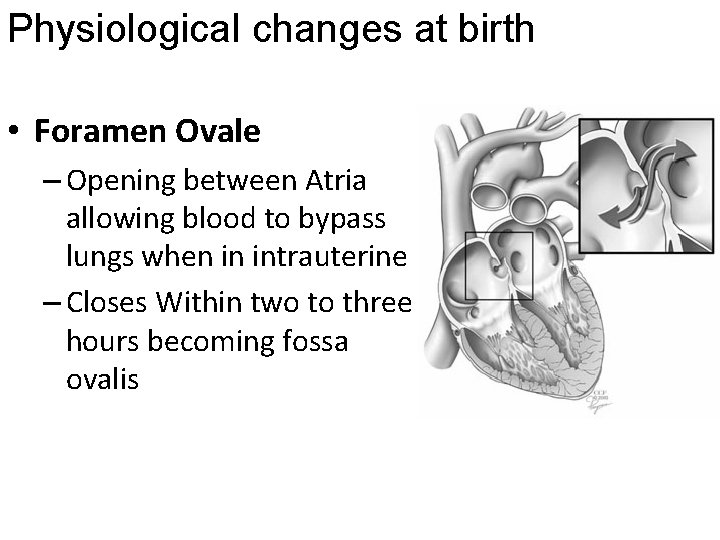
Physiological changes at birth • Foramen Ovale – Opening between Atria allowing blood to bypass lungs when in intrauterine – Closes Within two to three hours becoming fossa ovalis
Physiological changes at birth • Ductus Arteriosus: – Pathway between Pulmonary Artery & Descending giving a right-to-left direction due to high PVR and low placental resistance – Once clamped, placental resistance gone. There is an increase in SBP and vascular resistance and lungs oxygenate and blood and increased Pa. O 2 stimulates closure. – Prostaglandin E 2 (present during pregnancy) is decreased adding to closure. – Functionally closes by 72 hrs. – Becomes ligamentum arteriosum
Physiological changes at birth • Ductus Venosus: – Links inferior vena cava with umbilical vein. – Shunts a portion of the left umbilical vein blood flow directly to the inferior vena cava. Thus, it allows oxygenated blood from the placenta to bypass the liver. – Functional closure occurs within minutes of birth. Structural closure in term babies occurs within 3 to 7 days. – the remnant becomes the ligamentum venosum
Normal vital signs at birth • • • Heart rate= 120 -140 beat/min Blood pressure= 65/41 mm. Hg Respiratory rate= 30 -60 breath/min Temperature= Axillary 35. 5 -37 o. C. Oxygen saturation (Sp. O 2 )= >93% normal heart rate is higher in infancy than in adulthood, limiting the infant’s ability to increase cardiac output by increasing the heart rate.
…. . Physiological changes • Cyanosis results from 5 or more Grams of Unoxygenated Hemoglobin per 100 ml of Blood: So, If Hemoglobin is Low, You Won’t See Cyanosis In Spite of Low Pa. O 2! • Polycythemia: Increase in Production of Erythrocytes To Compensate for Chronic Hypoxemia; If Hemoglobin Greater Than 20 g/dl & Hematocrit Greater Than 55 -60%, Increased Risk for thromboembolism • Infants Respond to Severe Hypoxemia With Brady. Cardia
The Role of Pressure Gradients: Altered Hemodynamics • We know that blood flows from high pressure to low pressure. • Pressures vary in chambers • Blood flow direction from high to low: In a normal heart we’re moving from low pulmonary pressure to high systemic pressure. If we change this around, we screw up the pressure zones and resistance factors. • Resistance factors: if anything is stiff or hard or stenosed, that’s resistance and the blood won’t go in there. • Blood mixing
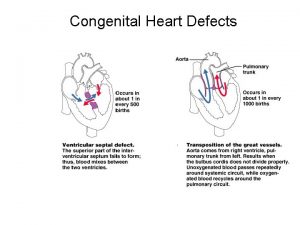
Congenital Heart Defect • Incidence: 5 -8 per 1000 live births – – About 2 -3 of these are symptomatic in first year of life Major cause of death in first year of life (after prematurity) Most common anomaly is ventricular septal defect 28% of kids with CHD have another recognized anomaly
Risk Factors • Maternal – Infection early on – ETOH and/or drugs – DM • Family hx of congenital heart disease • Syndromes like trisomy 21 • Presence of other anomalies or chromosomal abnormalities
Congenital Heart Disease • Occurs in about 8% of term newborns. Higher in pre-term infants. Can be as high as 10 -15% in infants who have a parent with aortic stenosis, ASD, VSD, or pulmonic stenosis • Females - more prone to have PDA and ASD • Males - more prone to have valvular aortic stenosis, coarctation of the aorta, TOF and transposition of the great vessels • The usual cause is failure of the heart to develop beyond an early stage of embryonic development • Maternal rubella is associated with PDA, stenosis, ASD, VSD
Etiology • Maternal Rubella • Maternal Alcoholism • Maternal DM Down Syndrome Trisomy #13 & #18 Turner’s Syndrome Marfan’s Syndrome Di George Syndrome
Congenital Heart Disease • Classification – Acyanotic vs. Cyanotic • Left-to-right shunt - oxygenated to unoxygenated blood • Right-to-left shunt - deoxygenated blood to oxygenated blood – Hemodynamic and Blood Flow Patterns - allows more predictable signs and symptoms • Increased pulmonary flow • Obstruction to blood flow (out of the heart) • Mixed blood flow (oxygenated and deoxygenated blood mixing in the heart or great vessels) • Decreased pulmonary flow

Defects with Increased Pulmonary Blood Flow LEFT-TO-RIGHT SHUNTING LESIONS • Blood flows from the left side of the heart to the right side of the heart through an abnormal opening or connection between the system or great arteries – Atrial Septal Defect (ASD) – Ventricular Septal Defect (VSD) – Patent Ductus Arteriosis (PDA) – Atrioventricular canal defect (AVC)
Atrial septal defect (ASD) • An abnormal communication between the two atria. • Blood flow is from left to right (oxygenated to deoxygenated) because of the stronger contraction of the left ventricle. • The increase volume in the right result in ventricular hypertrophy and increased pulmonary blood flow. • More frequent in girls than boys
Assessment of (ASD) • A harsh systolic murmur is heard over the second or third interspace (pulmonic area) • Radiates to apex or back • Possible thrill • Fluid overload (Hepatomegaly) • Shortness of air • Respiratory distress • Periorbital edema • FTT • Risk for stroke and infections
Assessment of (ASD) Diagnosis • Echocardiography with Doppler will reveal the enlarged right side of the heart and the increased pulmonary circulation. • Cardiac catheterization will reveal the separation in the atrial septum and the increased oxygen saturation in the right atrium.
Nursing Care of ASD • Nursing care focuses on postoperative management • Aware of signs and symptoms – Chest pain – Palpitations – Sudden hypotension – Dehydration – Anemia – Complications • Bleeding, tamponade, migration of device
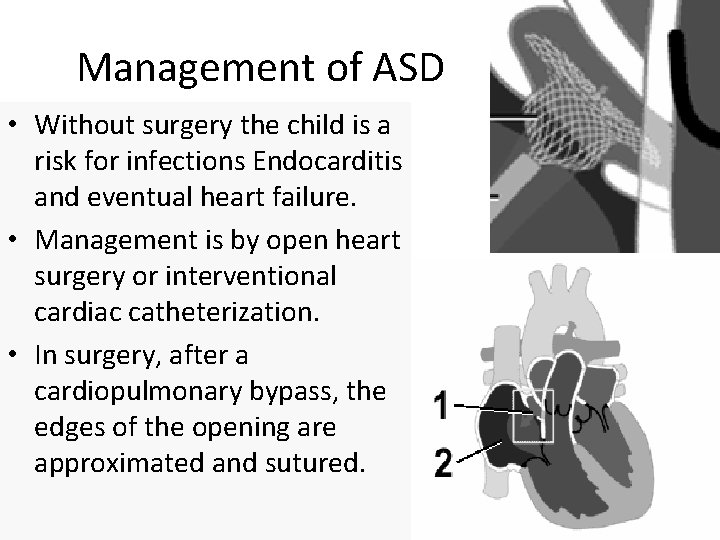
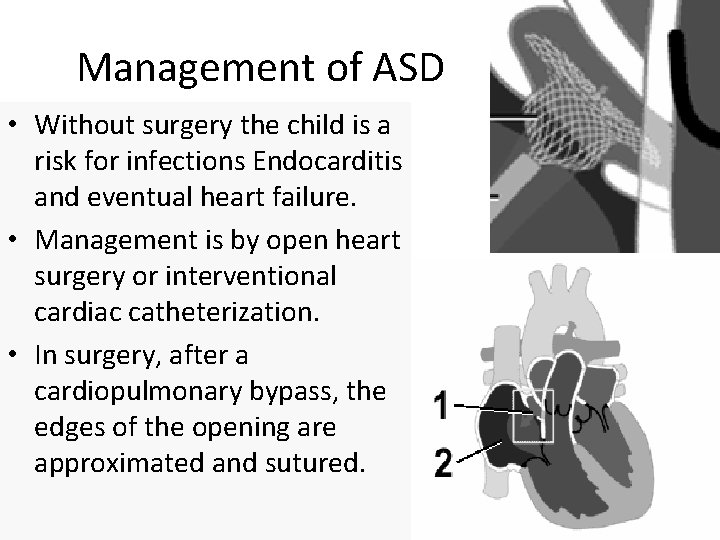
Management of ASD • Without surgery the child is a risk for infections Endocarditis and eventual heart failure. • Management is by open heart surgery or interventional cardiac catheterization. • In surgery, after a cardiopulmonary bypass, the edges of the opening are approximated and sutured.
Management of ASD cont… • If the defect is large, a silastic or dacron patch is sutured in place to occlude the space. • Post-op the child is observed for dysrhythmias. • Dysrhythmias can result from edema of the atria which can interfere with SA node function. • At risk for infectious endocarditis and heart failure • Can cause emboli in pregnant females if not corrected • May require a patch if defect not able to be closed with sutures
Ventricular septal defect (VSD) • The most common defect is ventricular septal defect (VSD). • Accounts for approximately 25% of all congenital heart disease. • Abnormal opening between the right and left ventricles. • Blood shunts from left to right. • Increase pulmonary blood involves blood flow from the left side of the heart (under greater pressure) to the right side • So remember. . . • Blood shunts into the pulmonary circulation instead of the aorta to the body. • Shunting causes right ventricular hypertrophy and increase pulmonary artery pressure.
Assessment of VSD • A ventricular septal defect may not be evident at birth. • At 4 to 8 weeks the child will have a loud systolic murmur. (Holosystolic harsh murmur along the left sternal border) – Especially at the left sternal border at the third or fourth intercostal space. – A thrill maybe palpable. • Diagnosis can be made by MRI or echocardiography. • Fetal echocardiography can reveal heart abnormalities as early as 18 weeks into pregnancy. • An echocardiography will reveal right ventricular hypertrophy and possibly pulmonary dilatation from increased blood flow. • Echocardiography is the primary diagnostic test for heart disease.
Management of VSD • 60% of the VSD close spontaneously during the first year of life. • Cardiac catheterization can be used to close the defect. • Open heart surgery is required for large defects. – A silastic or dacron patch is placed over the defect and tissue grows across the patch if edges can’t be approximated and sutured – Post-op monitor for dysrhythmias is necessary because of edema of the septum may interfere with conduction.
VSD congestive heart failure is common. – (by age 4 to 8 weeks) - develops a loud, harsh, systolic murmur along the left sternal border 3 rd or 4 th ICS, widely transmitted, usually with a thrill – Diagnosed with echocardiography or MRI – RV hypertrophy may also be seen on ECG – At risk of infectious endocarditis and cardiac failure – Arrhythmias can be a complication post-op
Patent Ductus Arteriosus • Failure of the fetal ductus arteriosus ( the artery connecting the aorta and the pulmonary artery) to close with the first weeks of life. • Failure of the ductus to close causes blood under high pressure in the aorta (oxygenated) to be shunted into the pulmonary artery (deoxygenated) • The shunted blood goes to the lungs, to the left atrium, to the left ventricle and out to the aorta, thus repeating circulation of the same blood.
Assessment of PDA • The child may be asymptomatic or shows signs of CHF • A characteristic machinery-like murmur is present in the upper left sternal border or under the left clavicle in older children. It is harsh, continuous • Widened pulse pressure (the difference between systolic and diastolic pressure) and bounding pulse are present • Fatigue, poor feeding, poor growth pattern, frequent colds, Pale, feeble appearance • Cardiac catheterization for diagnosis but may be used to rule out other abnormalities.
Management of PDA • The ductus arteriosus remains open during fetal life because of stimulation of prostaglandins (particularly PGE 1) from placenta and the low oxygen (PO 2) level of fetal blood. • After birth prostaglandin levels fall and oxygen levels increase which stimulates the ductus arteriosus to close. • May be given indomethacin or a prostaglandin inhibitor to lower PGE 1 levels and stimulate closure. Drug may be repeated as many as three times 12 to 24 hours apart
Management of PDA cont… • If medical management fails to bring about closure of the ductus arteriosus, the defect can be ligated surgically. • A thoracoscopy is performed and a clip is placed on the ductus. • Without the surgery the child is at risk from heart failure from increased amount of blood pouring back into the pulmonary artery • Also infectious Endocarditis can develop.
Treatment and Nursing Care of the Child with Patent Ductus Arteriosus • • • May close spontaneously during the first year Indomethacin Administration to inhibit prostaglandin Surgical Repair Prophylactic Antibiotics Prevent Congestive Heart Failure 95
Atrioventricular Canal (AVC) Defect • An incomplete fusion of the endocardial cushion. • May be seen as a low ASD continuous with a high VSD. Mitral and tricuspid valves are usually distorted. • Seen in 1 out of 9 children with Down syndrome • Blood flow is usually left to right, but may flow between all four chambers • Same symptoms of heart failure as ASD and VSD • Requires surgical repair and possible double valve replacement • Must be monitored post-op for jaundice from RBC destruction
Atrioventricular Canal (AVC) Defect • If medical management fails - ligation of defect – visual assisted thoracoscopy (VAT) - a clip is placed on the ductus • If not surgery, child is a risk for heart failure related to the increased shunting, infectious endocarditis from recirculating blood and potential stasis in the PA

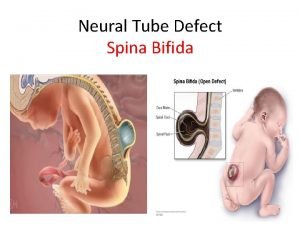
Tetralogy of Fallot (TOF) • Tetralogy of Fallot includes four defects: – Ventricular septal defects (VSD) – Pulmonic stenosis (PS) – Overriding aorta – Right ventricular hypertrophy • If pulmonary vascular resistance is higher than systemic resistance, the shunt is from right to left. • If the systemic resistance is higher than pulmonary resistance, the shunt is left to right.
Assessment Findings with Tetralogy of Fallot cont… • Severe dyspnea on exertion • Cyanosis • Tachycardia • Paroxysmal dyspnea • Blue spells • Squatting • Clubbing • Mental retardation 100
Assessment of TOF • Infants may be acutely cyanotic at birth or may have mild cyanosis that progresses over the first year of life as the Pulmonic Stenosis worsens. • Symptoms are variable depending of degree of obstruction and include: • Systolic murmur at left sternal border Retarded growth and development • A characteristic murmur is present. • Acute episodes of cyanosis and hypoxia (hypercyanotic spells) • Hyperacyanotic spells called Blue spells or “Tet spells” occur when the infant’s oxygen requirements exceed the blood supply. • This usually happens during crying or after feeding • Children with increasing cyanosis, there may be clubbing of the fingers, squatting and poor growth.
Hypercyanotic Spells/Blue Spells/Tet Spells Clinical Manifestations ٭ Most often occurs in morning after feedings, defecation, or crying v. Rapid breathing v. Acute cyanosis ٭ Hyperpenia ٭ Inconsolable crying ٭ Hypoxia which leads to acidosis 102
Place Infant in Knee-to-Chest Position Administer 100% Oxygen Administer Morphine (0. 1 mg/kg IV, IM, SQ) Use a Calm Approach IV Fluid Replacement for Blood Volume Expansion Administer Propranolol (0. 1 mg/kg IV) 103
Management of TOF • Surgical treatment for complete repair is usually performed in the first year of life. • It involves closure of the VSD and resection of the stenosis with a pericardial patch to the right ventricular outflow tract. • Surgery requires a median sternotomy and cardiopulmonary bypass.
Treatment of the Child with TOF • • Decrease cardiac workload Prevention of intercurrent infection Prevention of hemoconcentration Surgical repair 105
Nursing Care of the Child with Tetralogy of Fallot • • • Care During a Hypercyanotic Spell Decrease Cardiac Workload Maintain Nutrition Administration of Cardiac Medications Decrease Respiratory Distress 106
Truncus Arteriosus • Oxygen-poor and oxygen-rich blood mix back and forth through the ventricular septal defect. • This mixed blood then flows through the common truncal vessel. • Some of it will flow through the branch that becomes the pulmonary artery and on to the lungs, and some of the mixed blood will go into the aortic branch and continue to the body. • The mixed blood that goes to the body does not have as much oxygen as normal, and will cause varying degrees of cyanosis (blue color of the skin, lips, and nailbeds).
Transposition of Great Arteries/vessels • The aorta arises from the right ventricle instead of the left, and the pulmonary artery arises from the left instead of the right. • This condition is incompatible with life if there is no connection between right and left sides. • Emergency septostomy is performed to create a connection between the right and left sides.
Manifestations: • Blueness of the skin • Shortness of breath • Poor feeding • Clubbing of the fingers or toes Tests often include the following: • Chest x-ray • Cardiac catheterization • ECG • Echocardiogram (if done before birth, it is called a fetal echocardiogram) • Pulse oximetry (to check blood oxygen level)
Transposition of Great Arteries/vessels • Surgeries, but now they move the coronary arteries. • Severe cyanosis hours to days after birth as PDA closes • Various murmurs • Presence of ASD and VSD • CHF
Tricuspid Atresia • No communication from • RT atrium to RT ventricle • • Blood flows through atrial septal defect (ASD) or a patent foramen ovale to left • side of heart and through VSD to the RT ventricle • and out to the lungs Often associated with PS and transposition of the great vessels Complete mixing of unoxygenated and oxygenated blood in the left side Resulting in desaturation and varying amounts of pulmonary obstruction Causing decreased pulmonary blood flow
Tricuspid Atresia Manifestations • • Cyanosis seen in newborns Tachycardia Dyspnea Older children will exhibit clubbing and other signs of long standing hypoxemia
Diagnosis of Tricuspid Atresia • • Discovered during routine prenatal US Birth with signs and symptoms ECG Echocardiogram Chest X-Rays Echocardiogram Cardiac Catheterization
Tricuspid Atresia Management NEEDS IMMEDIATE SURGERY • Depends on patency of ductus arteriosis • Prostaglandin E 1 started at 0. 1 mcg/min until surgical intervention arranged (KEEP OPEN) allows blood to get to lungs • Palliative treatment – Placement of shunt (pulmonary - to – systemic artery anastomosis) to increase blood flow to lungs – If small can be accomplished during cardiac catheterization – Fenestration sometimes made in the right atrial baffle to relieve pressure
Obstructive Lesions • Pulmonic Stenosis • Aortic Stenosis • Coarctation of the Aorta
Pulmonic Stenosis • Narrowing at the entrance of the pulmonary artery • Resistance to blood flow causes RVH and decreased pulmonary blood flow • CHF prevails • Resultant Hepatomegaly
Pulmonic Stenosis Diagnosis • 25% to 35% of anomalies • May be asymptomatic or have mild heart failure, cyanotic • Usually a grade IV or V systolic murmur with a thrill. Heard loudest at the upper left sternal border. • May have a split S 2 • ECG may show right ventricular hypertrophy. • Cath can demonstrate degree of stenosis.
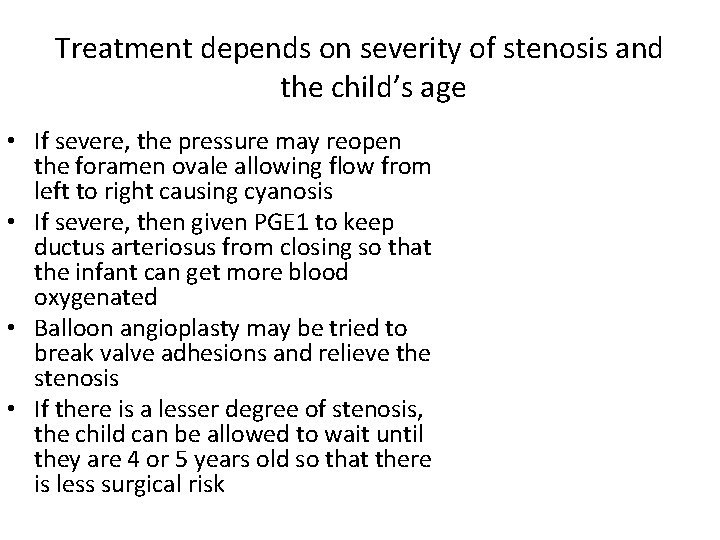
Treatment depends on severity of stenosis and the child’s age • If severe, the pressure may reopen the foramen ovale allowing flow from left to right causing cyanosis • If severe, then given PGE 1 to keep ductus arteriosus from closing so that the infant can get more blood oxygenated • Balloon angioplasty may be tried to break valve adhesions and relieve the stenosis • If there is a lesser degree of stenosis, the child can be allowed to wait until they are 4 or 5 years old so that there is less surgical risk
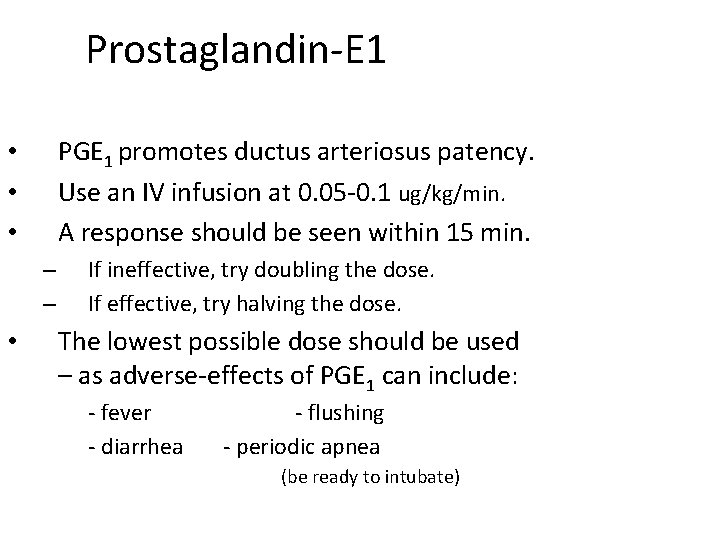
Prostaglandin-E 1 PGE 1 promotes ductus arteriosus patency. Use an IV infusion at 0. 05 -0. 1 ug/kg/min. A response should be seen within 15 min. • • • – – • If ineffective, try doubling the dose. If effective, try halving the dose. The lowest possible dose should be used – as adverse-effects of PGE 1 can include: - fever - flushing - diarrhea - periodic apnea (be ready to intubate)
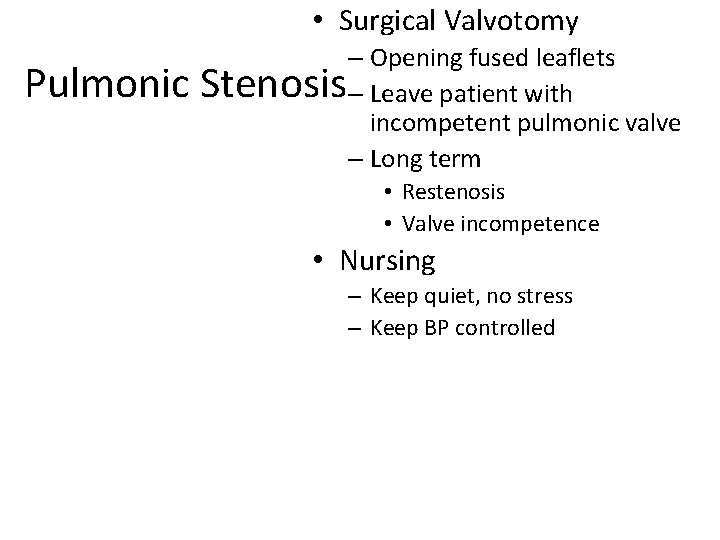
• Surgical Valvotomy Pulmonic Stenosis – Opening fused leaflets – Leave patient with incompetent pulmonic valve – Long term • Restenosis • Valve incompetence • Nursing – Keep quiet, no stress – Keep BP controlled
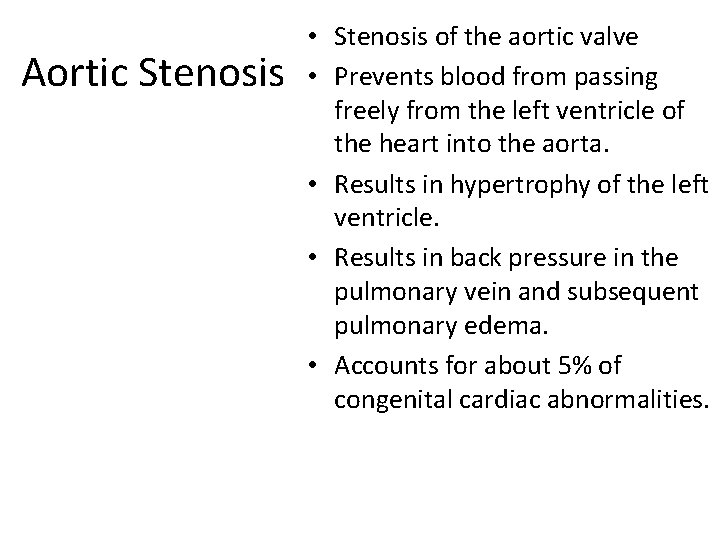
Aortic Stenosis • Stenosis of the aortic valve • Prevents blood from passing freely from the left ventricle of the heart into the aorta. • Results in hypertrophy of the left ventricle. • Results in back pressure in the pulmonary vein and subsequent pulmonary edema. • Accounts for about 5% of congenital cardiac abnormalities.
Assessment of aortic stenosis • The child may be free of symptoms • Child may exhibit a systolic ejection murmur heard best in the right 2 nd interspace (aortic space) • A thrill may be felt at the suprasternal notch. • If severe, decreased cardiac output evidenced by faint pulse, hypotension, tachycardia, and poor feeding may be present.
Assessment of aortic stenosis Diagnosis • When the child is active, he or she may develop chest pain. • Sudden death can occur when the amount of oxygen needed by the heart muscle on exertion far exceeds what is available because of the aortic stenosis. • Echocardiography will reveal left ventricular hypertrophy. • Cardiac catheterization can further reveal the degree of the stenosis
Management of aortic stenosis • Management includes balloon angioplasty or surgical repair, dividing the stenotic valve or replacing the valve with an artificial valve. • Types of valves are porcine (pig) and the prosthetic valve • If a prosthetic is used the patient will need anticoagulation or antiplatelet therapy. • Also antibody prophylaxis is necessary to prevent thrombus formation on the valve. • Preload and Afterload Reducers
Coarctation of the Aorta Narrowing of the Descending Aorta • Infants with severe Coarctation may develop severe symptoms and heart failure (CHF) including: • Poor weight gain • Poor feeding or tiring out • Rapid or labored breathing • Excessive sweating • Puffy eyes, face or extremities • Cool, pale or dusky skin
Coarctation of the Aorta • Older children and teens that have mild to moderate Coarctation may complain of: • Shortness of breath, especially when exercising • Leg cramps after exercising or at night • Fatigue • Frequent nose bleeds • Dizziness or fainting • Chest pain, especially when exercising • Very cold legs and feet • Strong, throbbing headache • High blood pressure
Assessment of coarctation of the aorta cont. . . • x-ray will reveal left ventricular enlargement. • A soft moderate load systolic murmur will be heard a the base of the heart.
Management of Coarctation of Aorta • Intervention is usually surgical removal of the narrowed portion with end to end anastomose • A graft of transplanted subclavian artery may be necessary if the narrowed section is extensive. • Medical Care: afterloading reducing agents (VASOTEC-enalapril or Capoten – captropril)
Atrioventricular Canal Defect (AVSD) • Part of the septum between the atria and the two ventricles have defects (ASD and VSD, respectively). • In addition, the heart valves separating the atria from the ventricles are defective. Instead of having two valves, the mitral and the tricuspid valves, there is one common atrioventricular valve.
Atrioventricular Canal Defect • The direction and pathway of flow determined by pulmonary and systemic resistance, LT and RT ventricular pressures, and compliance of each chamber • Moderate to severe CHF • Loud systolic murmur • Mild cyanosis increasing with crying • High risk for pulmonary vascular obstructive disease • pulmonary artery banding / complete repair in infancy
Types of Acquired Cardiovascular Disorders in Children • • Heart failure (most common) Rheumatic fever Cardiomyopathy Infective endocarditis Hyperlipidemia Hypertension Kawasaki disease
Rheumatic Fever • An autoimmune disease that is a reaction to a group-A beta -hemolytic streptococcus infection • Inflammatory Disease • Systematic inflammatory disease that affects primarily the heart, joints, brain and skin. Strep loves heart valves. The mitral valve is the most commonly affected. • Often follows an attack of Pharyngitis, tonsillitis, scarlet fever, “strep” throat, or impetigo • Children ages 6 -15 are the most susceptible
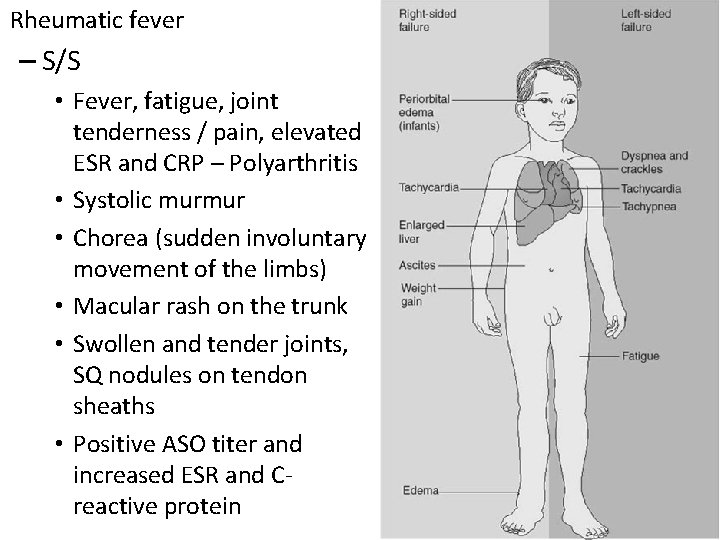
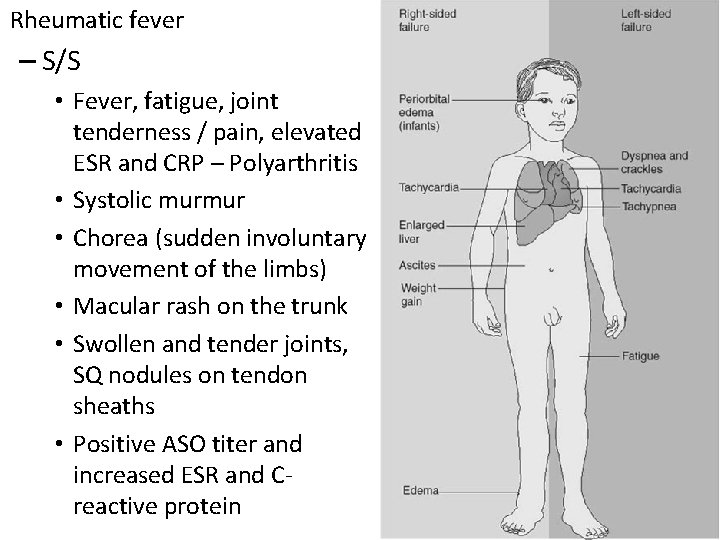
Rheumatic fever – S/S • Fever, fatigue, joint tenderness / pain, elevated ESR and CRP – Polyarthritis • Systolic murmur • Chorea (sudden involuntary movement of the limbs) • Macular rash on the trunk • Swollen and tender joints, SQ nodules on tendon sheaths • Positive ASO titer and increased ESR and Creactive protein
Rheumatic Fever Cont’d • Signs and Symptoms – Major • Aschoff bodies (hemorrhagic bullous lesions in the heart) • erythema marginatum • vegetation on valves • pericarditis • pericardial friction rub • muffled heart sounds • accentuated third heart sound • SC nodules • chorea (sudden involuntary movements of limbs)
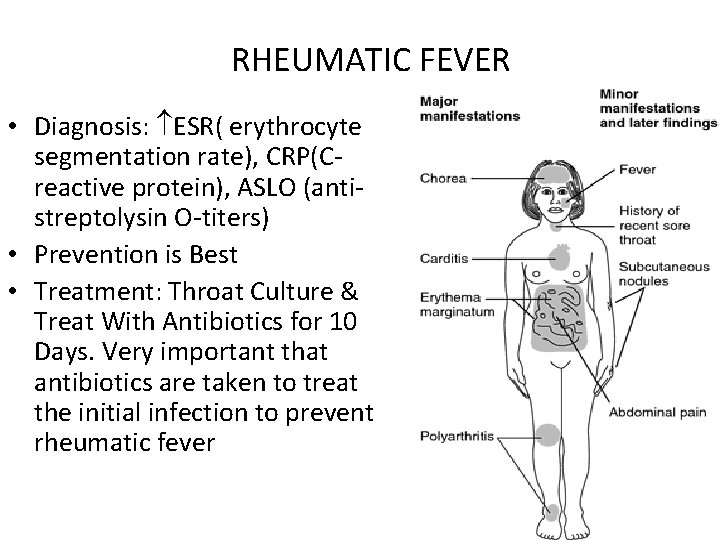
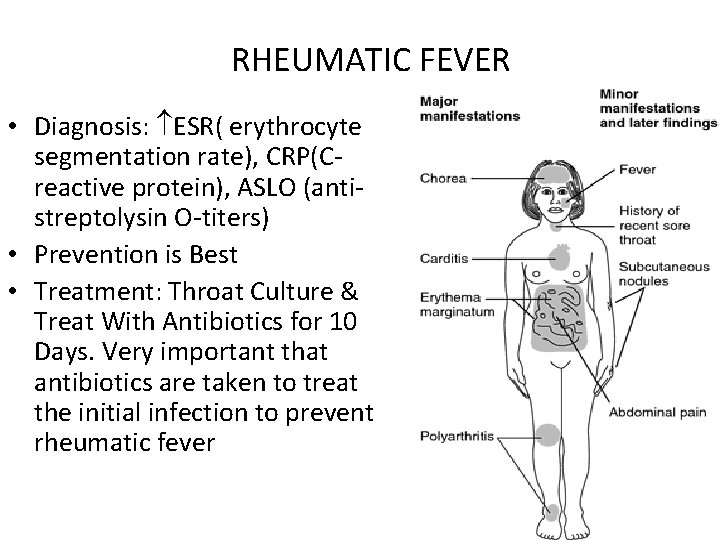
RHEUMATIC FEVER • Diagnosis: ESR( erythrocyte segmentation rate), CRP(C- reactive protein), ASLO (antistreptolysin O-titers) • Prevention is Best • Treatment: Throat Culture & Treat With Antibiotics for 10 Days. Very important that antibiotics are taken to treat the initial infection to prevent rheumatic fever
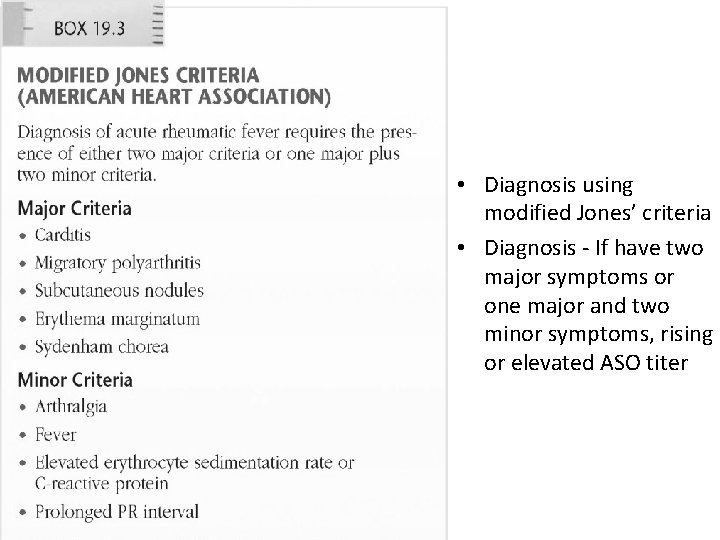
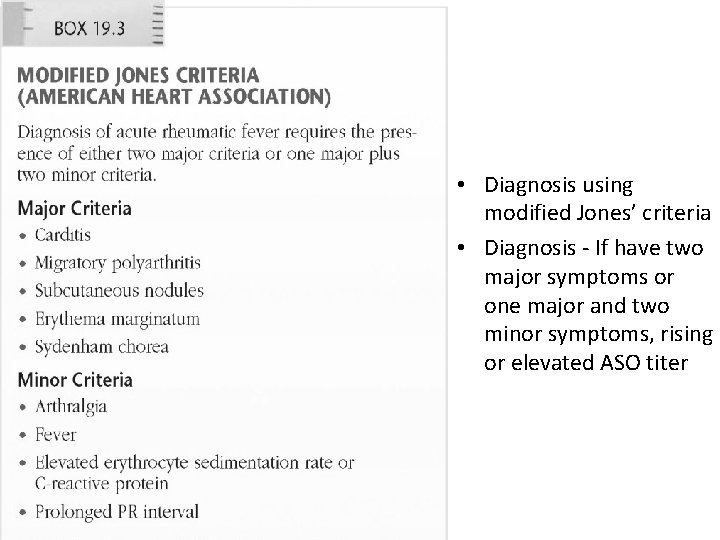
• Diagnosis using modified Jones’ criteria • Diagnosis - If have two major symptoms or one major and two minor symptoms, rising or elevated ASO titer
Rheumatic Fever Treatment (Cont’d) – Bedrest until ESR decreases (degree of bedrest is based on degree of carditis) – Antibiotics (penicillin, erythromycin) x 10 days • Tx: penicillin is #1. Otherwise we’ll go w/ 3 rd gen cephalosporin. Fever: treat it w/ Tylenol, IB, etc. • Support the kid and the family. IF the kid has ashcoff bodies, you’ll hear a murmur. – Corticosteroids if NSAIDS not working – Phenobarbital for chorea – Treatment of heart failure – Prognosis depends on the amount of cardiac involvement – Kept on prophylactic antibiotics for 5 years or until 18 to prevent recurrence
Major Problems of RD • Heart: Mitral valve Aschoff bodies [require surgical repair to valve] • Joints: edema and inflammation • Skin: erythema marginatum (round very circumscribed red things) • CNS: Sydenham chorea (St Bidus’ Dance: this guy who get a little nervous when he talked to god, so the patient gets a twitchy and dancy in their toes I guess…)
Prevention of RHD • Treatment of streptococcal tonsillitis and pharyngitis: – Penicillin G IM X 1 – Penicillin V PO q 10 days – Sulfa PO q 10 days – Erythromycin (if allergic to above) PO q 10 days • Treatment of recurrent RF: – Same as above
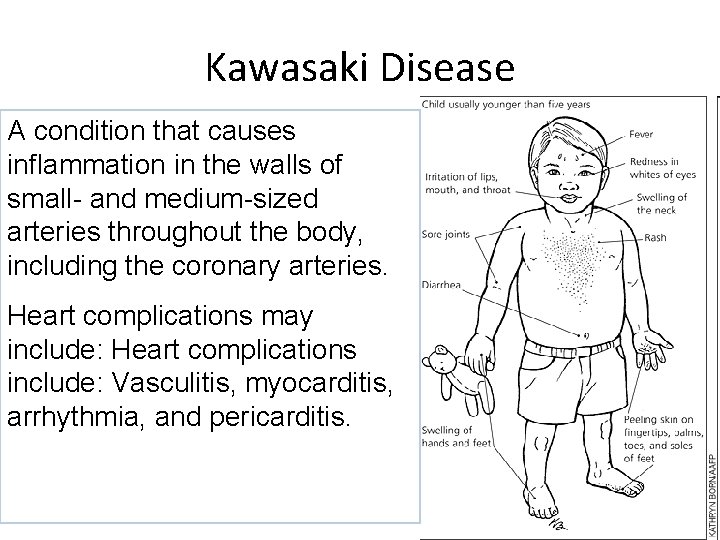
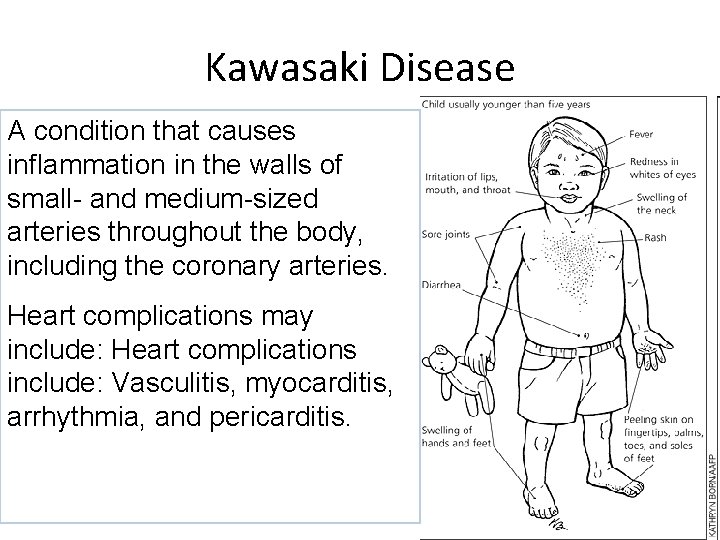
Kawasaki Disease A condition that causes inflammation in the walls of small- and medium-sized arteries throughout the body, including the coronary arteries. Heart complications may include: Heart complications include: Vasculitis, myocarditis, arrhythmia, and pericarditis.
Kawasaki Disease • Mucocutaneous Lymph Node Syndrome - an acute systemic vasculitis which leads to the formation of aneurysms and myocardial infarction • Actual cause is still unknown. Altered immune function occurs after an infection. There is an increase in antibody production. Antibody-antigen complexes apparently bind to the vascular endothelium and cause inflammation. The inflammation leads to platelet aggregation and the formation of thrombi or obstruction of heart and blood vessels
Kawasaki Disease (KD; Mucocutaneous Lymph Node Syndrome) • An acute systemic vasculitis of unknown cause • 75% of cases in children <5 years old • Three phases: – Acute: sudden high fever, unresponsive to antipyretics and antibiotics – Subacute: end of fever through end of all KD clinical signs – Convalescent: clinical signs resolved, but laboratory values not returned to normal; completed with normal values (6 -8 weeks)
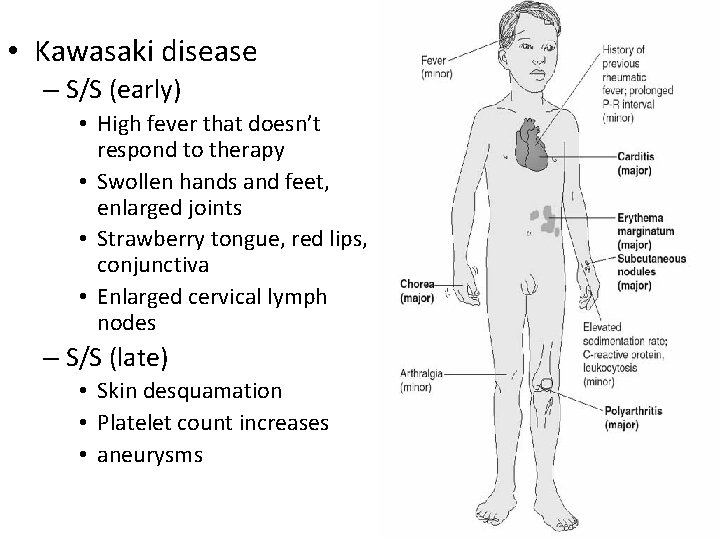
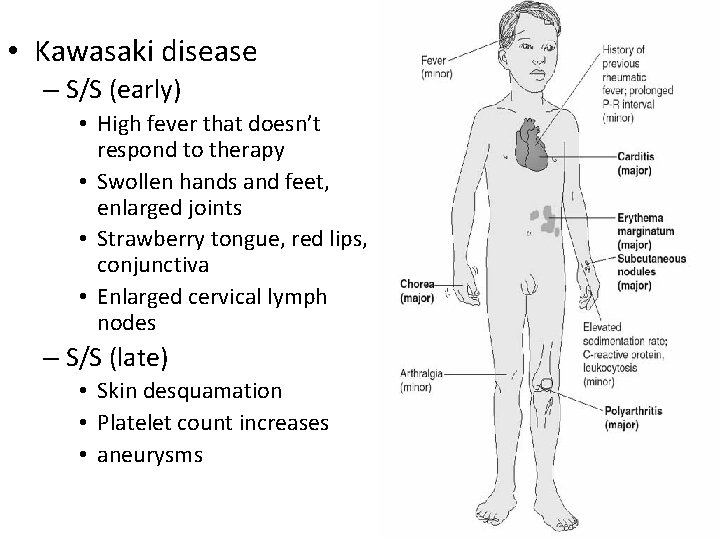
• Kawasaki disease – S/S (early) • High fever that doesn’t respond to therapy • Swollen hands and feet, enlarged joints • Strawberry tongue, red lips, conjunctiva • Enlarged cervical lymph nodes – S/S (late) • Skin desquamation • Platelet count increases • aneurysms
Signs and Symptoms of Kawasaki Disease • Fever – Note high fever for 5 days that is unresponsive to antibiotics. • Chills • Headache • Malaise • Extreme irritability • Vomiting • Diarrhea • Abdominal and joint pain
Kawasaki Disease • Acute Phase (Stage I) – High fever that doesn’t respond to antipyretics – Lethargic and irritable – May have red, swollen hands and feet, conjunctivitis, strawberry tongue and red, cracked lips, enlarged cervical lymph nodes, variety of rashes, abdominal pain as internal lymph nodes swell, anorexia, diarrhea, red and swollen joints – Elevated WBC and ESR • Subacute Phase - about 10 days after onset – Peeling of skin on palms and soles of feet – Platelet count rises (increases risk of clotting) – Aneurysms may form in coronary arteries - sudden death can occur
Kawasaki Disease • Convalescent Phase (Stage II) - begins at about the 25 th day and lasts until 40 days • Stage III lasts from 40 days until the ESR returns to normal • Diagnosis is based on criteria (Table 40. 3), blood studies and echocardiogram
Kawasaki Disease • Treatment – High dose aspirin – Dipyridamole - to increase coronary dilatation and prevent platelet accumulation – IV Gamma globulin - to reduce immune response • Observe child for signs of heart failure • Inspect and palpate extremities for warmth and capillary refill
Kawasaki Disease • Pathophysiology – Therapeutic management • Administration of Ibuprofen for inflammation and platelet aggregation is avoided while ASA is being taken • IV immunoglobulin to decrease immune response • Most children recover fully but some will need heart surgery to repair damage • Therapeutic Management • Nursing Assessment – Health History and Physical Examination – Laboratory and Diagnostic Testing
Kawasaki Disease • Nursing Management – Monitoring Cardiac Status – Promoting Comfort – Providing Patient and Family Education – Observe child for signs of heart failure Inspect and palpate extremities for warmth and capillary refill Provide comfort measures Protect edematous areas from pressure May have dry, cracked lips Monitor for dehydration, encourage fluids, but prevent fluid overload • Monitor nutritional status • • •
Pharmacology • IV Ig. G • Digoxin (Lanoxin) • ACE inhibitors ASA 80 -100 mg/kg/day—fever – ASA – Lasix –Spironolactone (Aldactone) Then 3 -5 mg/kg/day—antiplatelet
Endocarditis • Inflammation and infection of the endocardium or valves of the heart • Generally caused by streptococcal viridans. Sometimes can be staphylococcal or fungal • Strep enters the blood stream during oral procedures, impetigo, UTI’s • Vegetation of bacteria, fibrin, and blood appear on the endocardium of the valves and heart chambers - destroys the endothelial lining
Endocarditis • Signs and Symptoms - abrupt, unexplained lowgrade intermittent fever, anorexia, malaise, weight loss, change in murmur, splenomegaly • Non-specific: malaise, myalgias • Fever • Heart murmur • Nonspecific signs – petechiae, subungal or “splinter” hemorrhages, clubbing, splenomegaly, neurologic changes • More specific signs - Osler’s Nodes, Janeway lesions, and Roth Spots
Endocarditis • Vegetation of bacteria, fibrin, and blood appear on the endocardium of the valves and heart chambers - destroys the endothelial lining • Prophylaxis: 1 hour before procedures (IV) or may use PO in some cases
Endocarditis • Patients With CHD, Prosthetic Cardiac Valve, Multiple Invasive Lines, etc May Be at Increased Risk • Streptococcus viridan (most common) • Definitive Diagnosis: Blood Cultures • Intravenous Antibiotics for 2 -8 Weeks • Bedrest in Acute Phase • Prevention is Best; Inform Dentist & MD for Prophylaxis PRIOR to Procedures
Diagnostic Tests for Infective Endocarditis • ECG, elevated ESR and C-reactive protein, anemias, Leukocytosis, microscopic hematuria • Blood culture: bacteria or fungus • CBC: anemia, Leukocytosis • Urinalysis: microscopic hematuria • Echocardiogram: cardiomegaly, abnormal valve function, area of vegetation
Endocarditis • Treatment - antibiotics (PCN, Ampicillin, Gentamycin) for 2 to 8 weeks. Supportive therapy to prevent heart failure. Teach prevention with prophylactic antibiotics before procedures.
Risk Factors for Cardiomyopathy • Congenital heart defect, cardiac transplantation, or surgery • Duchenne or Becker muscular dystrophy • History of myocarditis, HIV infection, or Kawasaki disease • Hypertension • Drugs, alcohol, or radiation exposure • Connective tissue, autoimmune, or endocrine disease • Maternal diabetes • Familial history of sudden death
Cardiomyopathy • 3 types: restrictive, dilated, hypertrophic • Therapeutic Management: improvement of heart function and blood pressure (mechanical ventilation, vasoactive medications, pacemakers, or surgery) • Nursing Assessment – Health History: risk factors, signs and symptoms – Physical Examination: inspection, auscultation – Laboratory and Diagnostic Testing • Nursing Management – Monitoring for complications – Medication administration – Child and family support and education
Heart Transplantation • Indications • Candidates and Evaluation • Surgical Procedure and Postoperative Therapeutic Management • Nursing Management – Preoperative care – Postoperative care – Patient and family education
Comprehensive Assessment for Heart Transplant • Chest radiograph, electrocardiogram, echocardiogram, exercise stress test, cardiac catheterization, pulmonary function test • CBC with differential, prothrombin and partial thromboplastin time, serum chemistries and electrolytes, blood urea nitrogen, and creatinine • Urinalysis and urine creatinine clearance • Blood, throat, urine, stool, and sputum cultures for bacteria, viruses, fungi, and parasites
Comprehensive Assessment for Heart Transplant (cont. ) • Epstein-Barr virus, cytomegalovirus, varicella, herpes, hepatitis, and HIV titers • HLA typing and panel reactive antibody typing and titer • Computed tomography or MRI scan, electroencephalogram • Consults with neurology, psychology, genetics, social work, nutritionist, physical and occupational therapy, and financial coordinator or case manager
Cardiac Surgery Cont’d • Heart Transplant - for hypoplastic left ventricle or cardiomyopathy – ECG’s will show two P waves – Post-op care is the same as with other heart surgeries – Patients will be placed on immunosuppresive therapy – Rejection is the #1 cause of death • Hyperacute rejection - immediately upon restoring circulation • Acute rejection - occurs in about 7 days, fever, tachycardia, ECG changes • Chronic rejection - may begin at about a year
Systemic Hypertension • Primary: no known cause • Secondary: identifiable cause • Pediatrics: hypertension generally secondary to structural abnormality or underlying pathologic condition: – Renal disease – Cardiovascular disease – Endocrine or neurologic disorders
Hyperlipidemia • Identify kids at risk and treat early • Treatment: dietary: – Restrict intake of cholesterol and fats • If no response to diet, medications: – Colestipol (Colestid) – Cholestyramine (Questran)
 Non centric cusp
Non centric cusp Portrait teeth mould guide
Portrait teeth mould guide Minute volume
Minute volume Pleasure curve in complete denture
Pleasure curve in complete denture Objectives of final impression
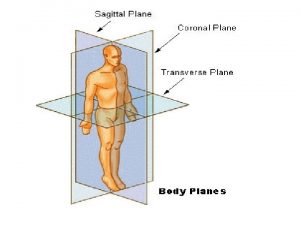
Objectives of final impression Standard anatomical position
Standard anatomical position Anatomical modifier
Anatomical modifier Non anatomic teeth indications
Non anatomic teeth indications Main arteries in the body
Main arteries in the body Anatomic end arteries
Anatomic end arteries Anatomic references
Anatomic references In anatomic lever systems the fulcrum is the
In anatomic lever systems the fulcrum is the Anatomic descriptors and fundamental body structure
Anatomic descriptors and fundamental body structure Anatomic
Anatomic Label the body regions with the proper adjective.
Label the body regions with the proper adjective. Quality management in anatomic pathology
Quality management in anatomic pathology Suflu sistolic copii
Suflu sistolic copii Aims and objectives of mudaliar commission
Aims and objectives of mudaliar commission Concrete defects honeycomb
Concrete defects honeycomb Examples of artificial defects
Examples of artificial defects Wendelin wright
Wendelin wright Delamination injection molding
Delamination injection molding Ttn vs rds cxr
Ttn vs rds cxr Congenital pneumonia
Congenital pneumonia Codivila
Codivila Congenital glaucoma classification
Congenital glaucoma classification Eisenmenger syndrome
Eisenmenger syndrome Congenital rubella syndrome
Congenital rubella syndrome Congenital malformations
Congenital malformations Congenital voice disorders
Congenital voice disorders Congenital hypothyroid
Congenital hypothyroid Tetralogy of fallot xray
Tetralogy of fallot xray Egg on a string heart
Egg on a string heart Congenital fibrosis of the extraocular muscles
Congenital fibrosis of the extraocular muscles Choanal atresia,
Choanal atresia, Larynx
Larynx Congenital adrenal hyperplasia electrolytes
Congenital adrenal hyperplasia electrolytes Congenital rubella syndrome triad
Congenital rubella syndrome triad Endocardial cushion defect
Endocardial cushion defect Congenital rubella syndrome triad
Congenital rubella syndrome triad Congenital adrenal hyperplasia characteristics
Congenital adrenal hyperplasia characteristics Potter face oligohydramnios
Potter face oligohydramnios Congenital hydronephrosis
Congenital hydronephrosis Congenital
Congenital Site:slidetodoc.com
Site:slidetodoc.com Michael addidle
Michael addidle Kode icd 10 clubfoot
Kode icd 10 clubfoot Congenital toxoplasmosis
Congenital toxoplasmosis Craneosquisis
Craneosquisis Canadian congenital heart alliance
Canadian congenital heart alliance Congenital glaucoma
Congenital glaucoma Vulvodynia
Vulvodynia Schlussel urology
Schlussel urology Farah garmany
Farah garmany Congenital diaphragmatic hernia
Congenital diaphragmatic hernia Congenital heart
Congenital heart Congenital rubella
Congenital rubella Causes of congenital anomalies
Causes of congenital anomalies Birth defects causes
Birth defects causes Congenital flat foot
Congenital flat foot Mineralocorticoid function
Mineralocorticoid function Thyroid hormone synthesis mnemonic
Thyroid hormone synthesis mnemonic Ortolani galeazzi barlow
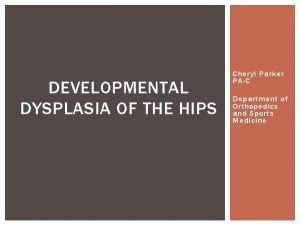
Ortolani galeazzi barlow Hip dysplasia alpha angle
Hip dysplasia alpha angle Congenital heart defect
Congenital heart defect Congenital
Congenital Congenital amusia
Congenital amusia Congenital syphilis triad
Congenital syphilis triad Stages of tb lymphadenitis
Stages of tb lymphadenitis Congenital anomalies
Congenital anomalies Congenital
Congenital Congenital glaucoma
Congenital glaucoma Molecules in two dimensions structural formulas
Molecules in two dimensions structural formulas It is a decorative design
It is a decorative design Cables in structural analysis
Cables in structural analysis What is decorative design
What is decorative design Structural adaptation for plants
Structural adaptation for plants Distortion control in welding
Distortion control in welding Execution defects
Execution defects Twinning tablet defects
Twinning tablet defects Types of moulding sand
Types of moulding sand Chain sling defects
Chain sling defects Armany classification
Armany classification Ctc en ctq
Ctc en ctq Attribute capability study excel
Attribute capability study excel Planer defect
Planer defect Physical defects in personality development
Physical defects in personality development Widows peak in periodontics
Widows peak in periodontics Defects in butter
Defects in butter Point defects in crystals
Point defects in crystals Hot spot porosity
Hot spot porosity Cuts and washes defects in casting
Cuts and washes defects in casting Birth defects causes
Birth defects causes Defects due to natural forces in timber
Defects due to natural forces in timber Radial shakes
Radial shakes Sugar coated tablet example
Sugar coated tablet example Solid solution
Solid solution Point defects in crystals
Point defects in crystals Defect amplification and removal in software engineering
Defect amplification and removal in software engineering Fault is manifestation of which defect
Fault is manifestation of which defect Learning from defects
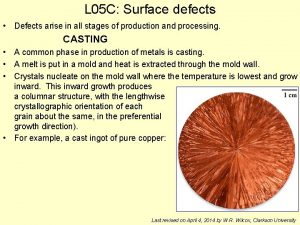
Learning from defects Surface defects examples
Surface defects examples Gravure cylinder defects
Gravure cylinder defects Apps.searo.who.int.login-database
Apps.searo.who.int.login-database Plastic extrusion defects
Plastic extrusion defects Core defects of diabetes
Core defects of diabetes Wire drawing defects
Wire drawing defects Crystal defects
Crystal defects Schottky defect and frenkel defect
Schottky defect and frenkel defect Shell cleanliness shell soundness shell
Shell cleanliness shell soundness shell Upset forging advantages and disadvantages
Upset forging advantages and disadvantages Neural tube defects
Neural tube defects Respiratory chain defects
Respiratory chain defects Neural tibe defect
Neural tibe defect Forging die terminology
Forging die terminology Neural tube defects
Neural tube defects What are the main defects in montessori method
What are the main defects in montessori method Defects in cream
Defects in cream Jaymin panchal
Jaymin panchal Homometric regulation of cardiac output
Homometric regulation of cardiac output Cardiac distension
Cardiac distension Peosinogen
Peosinogen Cardiac cycle steps
Cardiac cycle steps Mammillated areas of stomach
Mammillated areas of stomach Tubular esophagus
Tubular esophagus Function if stomach
Function if stomach Fusiform
Fusiform Mets score cardiac
Mets score cardiac Amiodarone mechanism of action
Amiodarone mechanism of action Pediatric pat
Pediatric pat Aschoff bodies diagram
Aschoff bodies diagram Comparison of skeletal cardiac and smooth muscle
Comparison of skeletal cardiac and smooth muscle Renal denervation
Renal denervation Characteristics of skeletal smooth and cardiac muscle
Characteristics of skeletal smooth and cardiac muscle Stump bed
Stump bed Gittata cardiaca
Gittata cardiaca Heart dullness
Heart dullness Air cushion comfort device
Air cushion comfort device Site:slidetodoc.com
Site:slidetodoc.com Dr johan jordaan
Dr johan jordaan Map co x tpr
Map co x tpr Cardiac orifice of stomach
Cardiac orifice of stomach Upper third esophagus
Upper third esophagus Stomach borders
Stomach borders Dobutamine vs dopamine
Dobutamine vs dopamine Wandering atrial pacemaker criteria
Wandering atrial pacemaker criteria Milrinone mechanism of action
Milrinone mechanism of action Sphincter
Sphincter Ecg phases
Ecg phases Cardiac clearance meaning
Cardiac clearance meaning Acute responses to training definition
Acute responses to training definition Cardiac output trained vs untrained
Cardiac output trained vs untrained Lesson 6: cardiac emergencies and using an aed
Lesson 6: cardiac emergencies and using an aed Cardiac output stroke volume
Cardiac output stroke volume Heart rate during exercise
Heart rate during exercise Membrane potential of cardiac muscle
Membrane potential of cardiac muscle Cardiac output trained vs untrained
Cardiac output trained vs untrained Cardiac output fick principle
Cardiac output fick principle Enlarged cardiac silhouette
Enlarged cardiac silhouette Jones and bartlett ekg strips 2012
Jones and bartlett ekg strips 2012 Phase 2 cardiac rehab exercises
Phase 2 cardiac rehab exercises Cardiac rehab phase 1
Cardiac rehab phase 1 Cardiac rehab phase 1
Cardiac rehab phase 1 Cardiac poisons example
Cardiac poisons example Refractory period heart
Refractory period heart