Congenital Heart Defects MODULE F Chapter Eleven Cardiac




- Slides: 48
Congenital Heart Defects MODULE F Chapter Eleven Cardiac System Pages 348 - 359
Objectives • Differentiate between the different congenital heart diseases and state whether they are cyanotic and acyanotic. • Describe the defect present with each congenital heart disease. • Describe the surgical repair (if any) for each congenital heart disease.
Cardiac Defects • • • Patent Ductus Arteriosus Atrial Septal Defect Ventricular Septal Defect Tetralogy of Fallot Transposition of the Great Arteries Coarctation of the Aorta Anomalous Venous Return Truncus Arteriosus Hypoplastic Left-Heart Syndrome

Web Sites • http: //www. childrensheartinstitute. org/edu cate/defects. htm
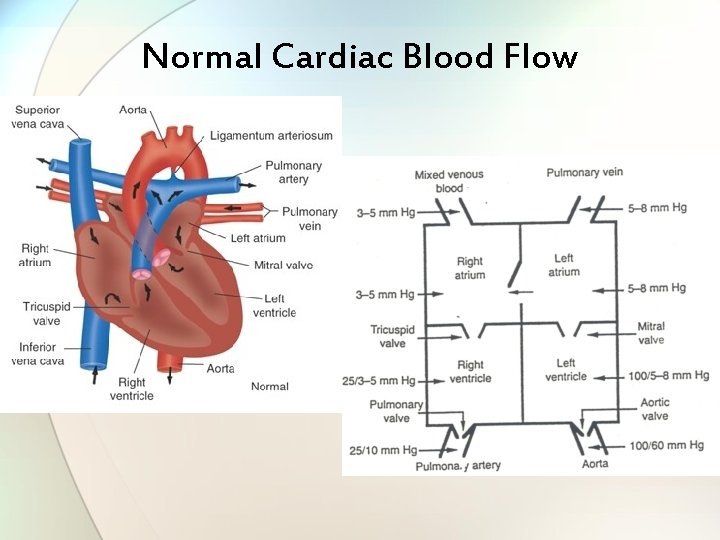
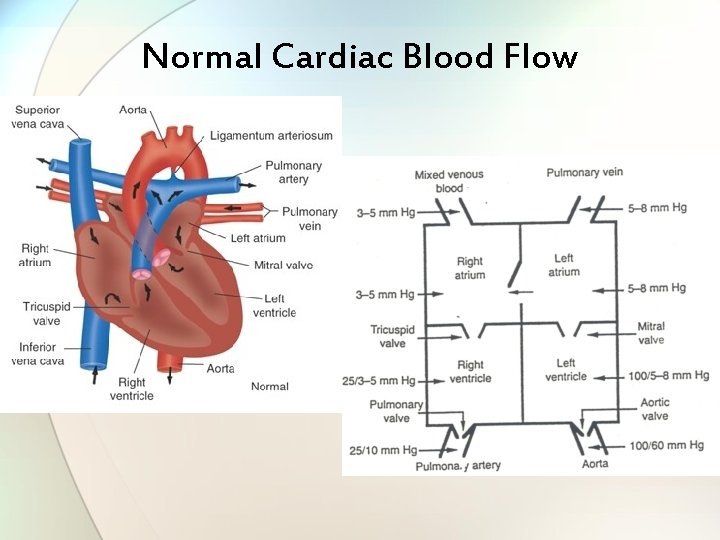
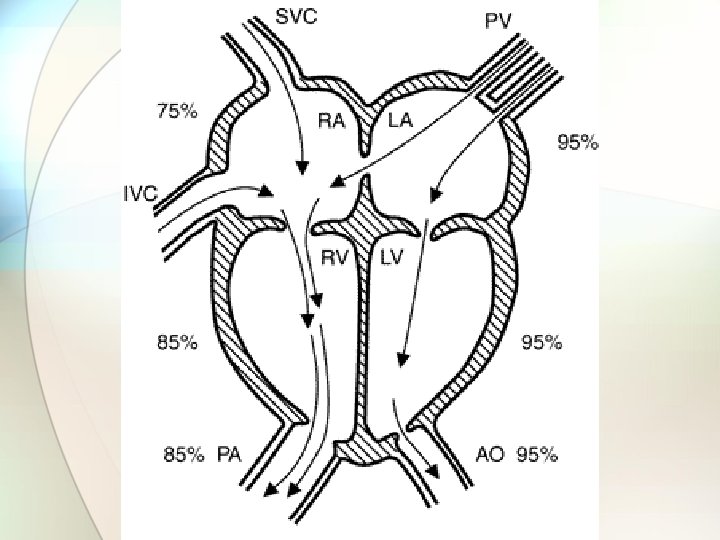
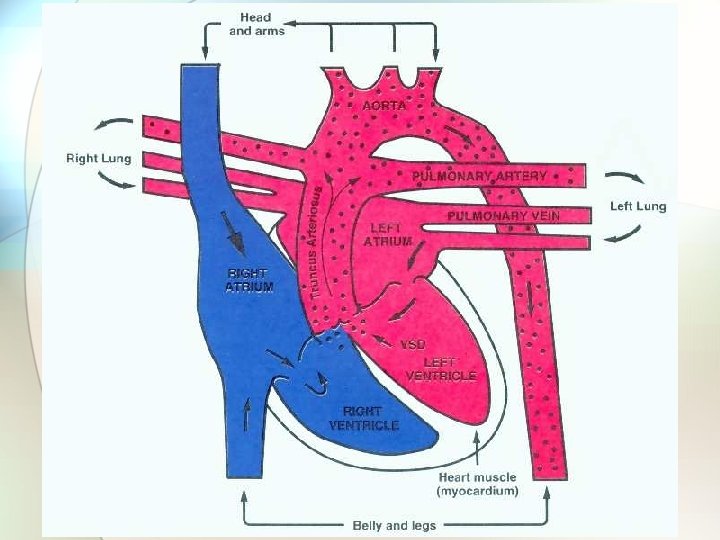
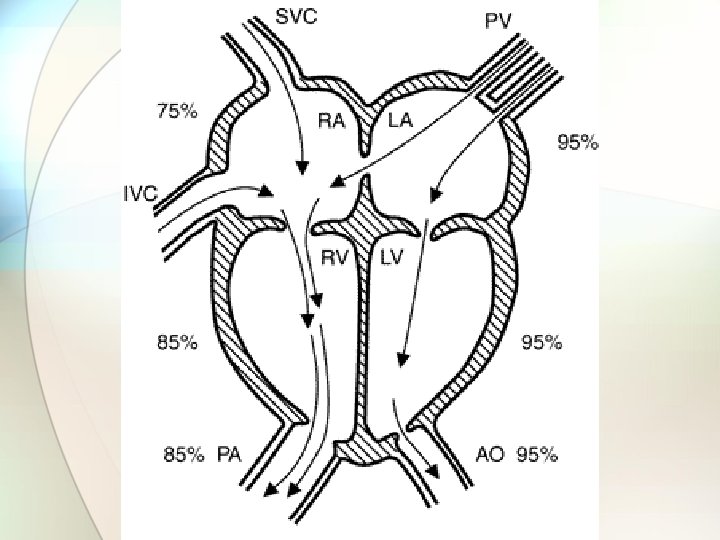
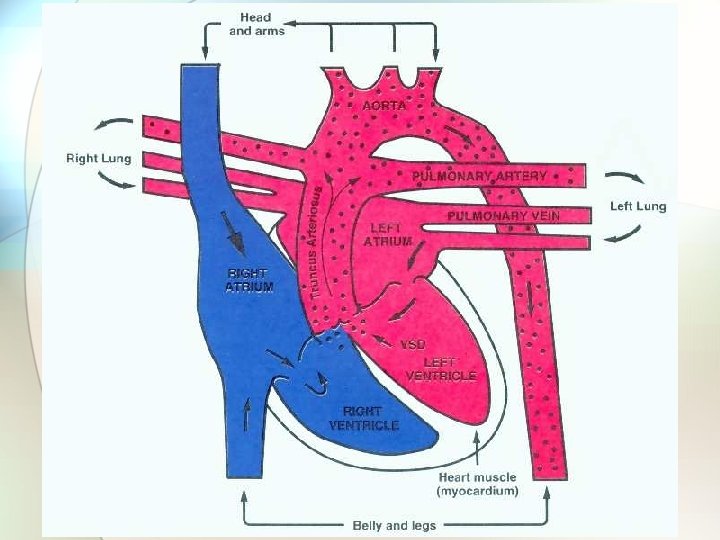
Normal Cardiac Blood Flow
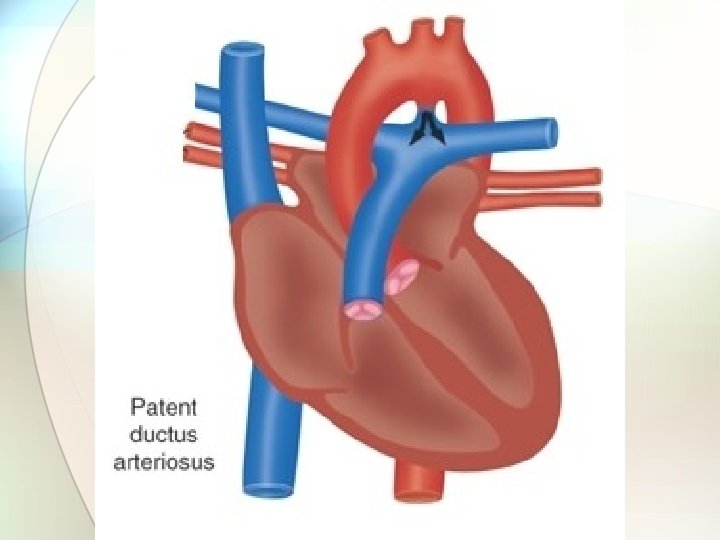
Ductus Arteriosus • Fetal Circulation Component • Connects Pulmonary Artery to Aorta • Shunts blood away from lungs • Maintained patent by presence of prostaglandins • Closure secondary to: • Increase in Pa. O 2_ • Decrease in level of prostaglandins
Patent Ductus Arteriosus • 5 -10% of all births (1 of 2000 live births) • 80% of premature babies • 2 -3 times more common in females than males. • 5 th or 6 th most common congenital cardiac defect. • Often associated with other defects. • May be desirable with some defects. • Morbidity/Mortality related to degree of blood flow through PDA.
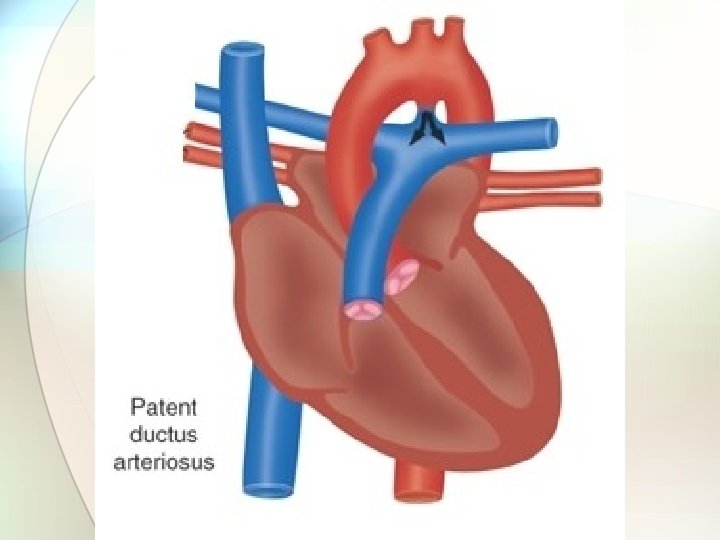
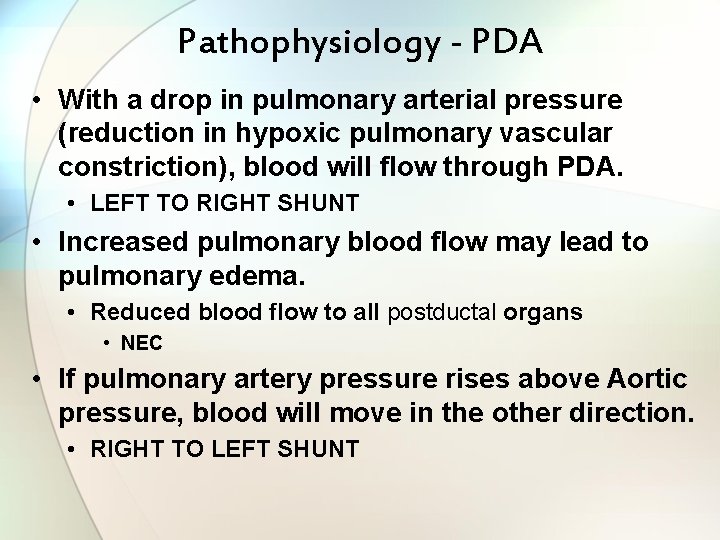
Pathophysiology - PDA • With a drop in pulmonary arterial pressure (reduction in hypoxic pulmonary vascular constriction), blood will flow through PDA. • LEFT TO RIGHT SHUNT • Increased pulmonary blood flow may lead to pulmonary edema. • Reduced blood flow to all postductal organs • NEC • If pulmonary artery pressure rises above Aortic pressure, blood will move in the other direction. • RIGHT TO LEFT SHUNT
Diagnosis - PDA • Loud grade I to grade III systolic murmur at left sternal border. • Washing machine • Echocardiography
Treatment - PDA • • Restrict fluids. Diuretics Prostaglandin Inhibitors - Indomethacin Surgical closure (ligation).
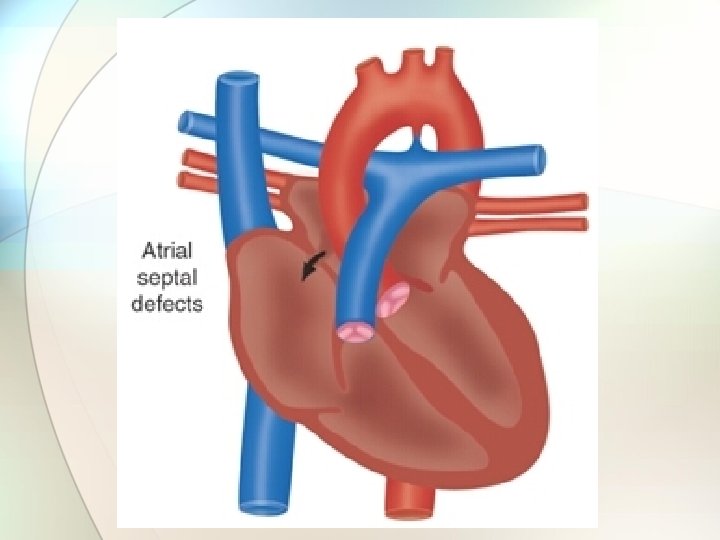
Atrial Septal Defect • 6 -10% of all births (1 of 1500 live births) • 2 times more common in females than males. • Types: • Ostium Secundum (at or about the Foramen Ovale) • Sinus Venous (at about the point where SVC and IVC attach to Right Atrium) • In 1950 most children with ASD did not reach the first grade. Today, first year surgery facilitates normal growth and development.
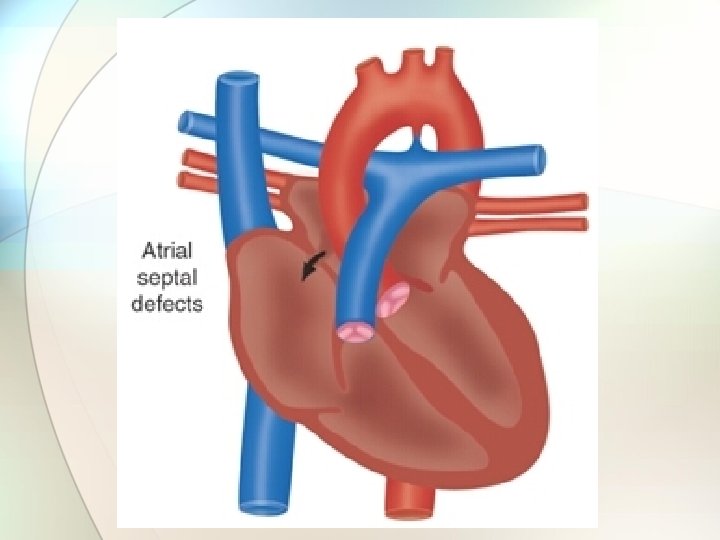
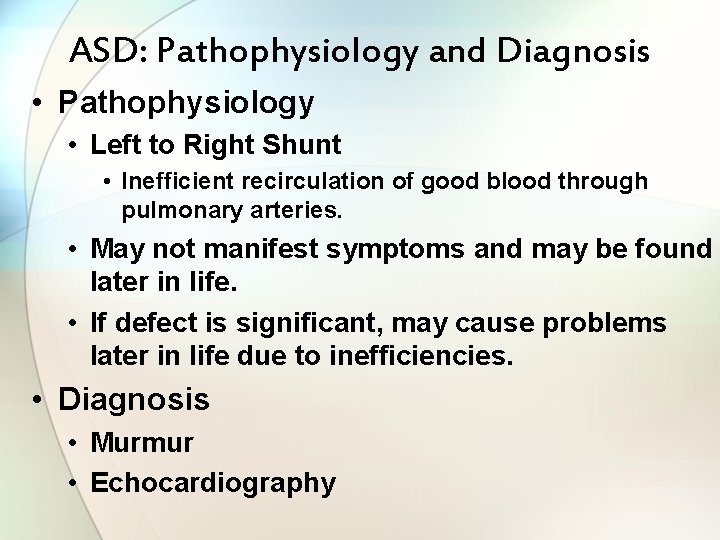
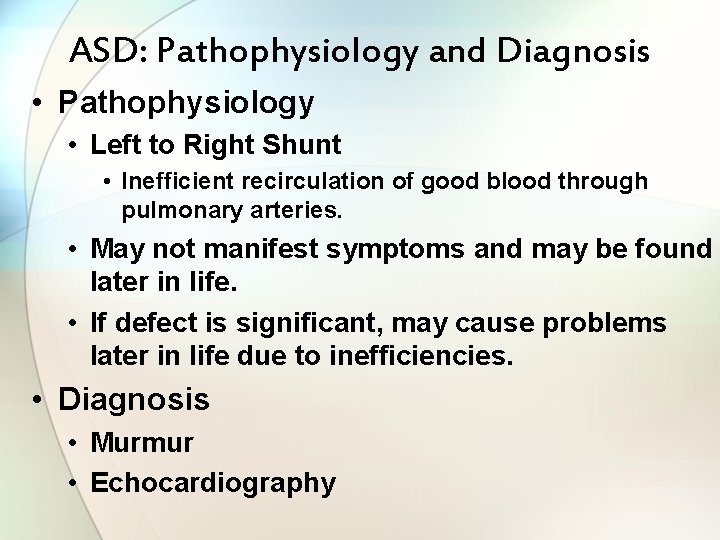
ASD: Pathophysiology and Diagnosis • Pathophysiology • Left to Right Shunt • Inefficient recirculation of good blood through pulmonary arteries. • May not manifest symptoms and may be found later in life. • If defect is significant, may cause problems later in life due to inefficiencies. • Diagnosis • Murmur • Echocardiography
Treatment - ASD • Surgical closure. • Non-Surgical closure via cardiac catheterization.
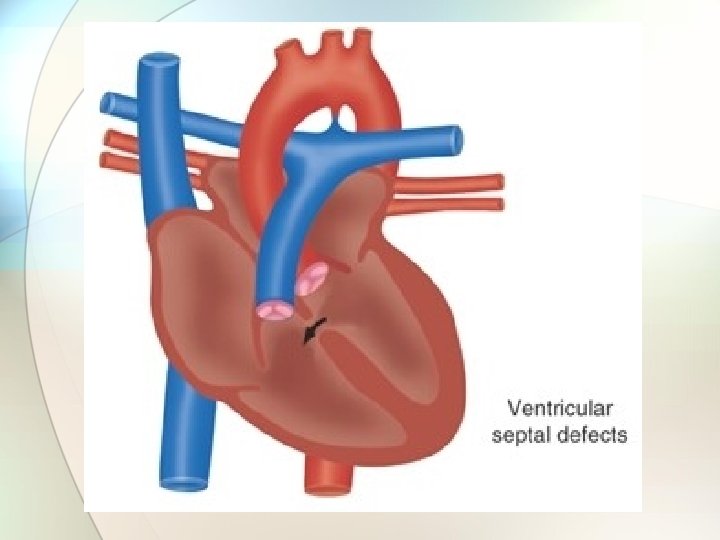
Ventricular Septal Defect • 1% of all births (2 to 4 of 1000 live births) • Vast majority the hole is small. • In 1950, fatal. Today almost all VSD can be closed successfully, even in small babies. Lillehei was the first person in history to correct both ASD and VSD on 8/31/54.
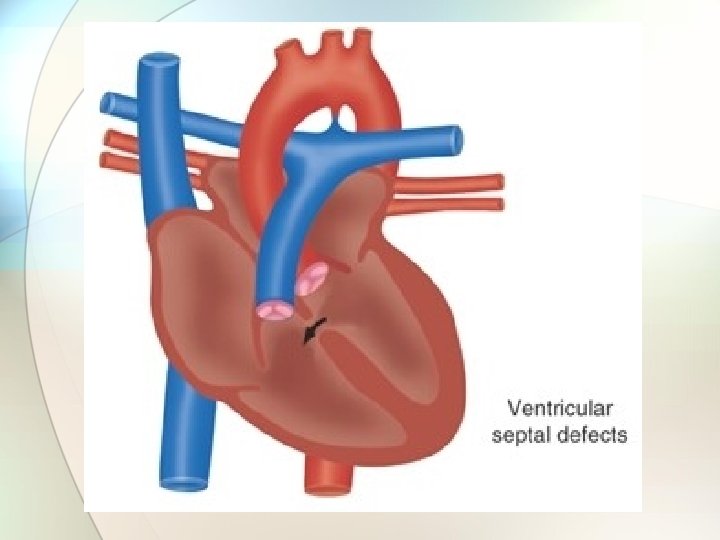

VSD: Pathophysiology & Diagnosis • Pathophysiology • May be isolated or associated with other congenital cardiac defects. • With normal PVR: • LEFT TO RIGHT SHUNT • With elevated PVR (RDS): • RIGHT TO LEFT SHUNT • Diagnosis • Echocardiography
Treatment - VSD • Nothing if VSD is small. • With CHF or Failure to Thrive: Surgical closure. http: //64. 143. 41. 32/news. html
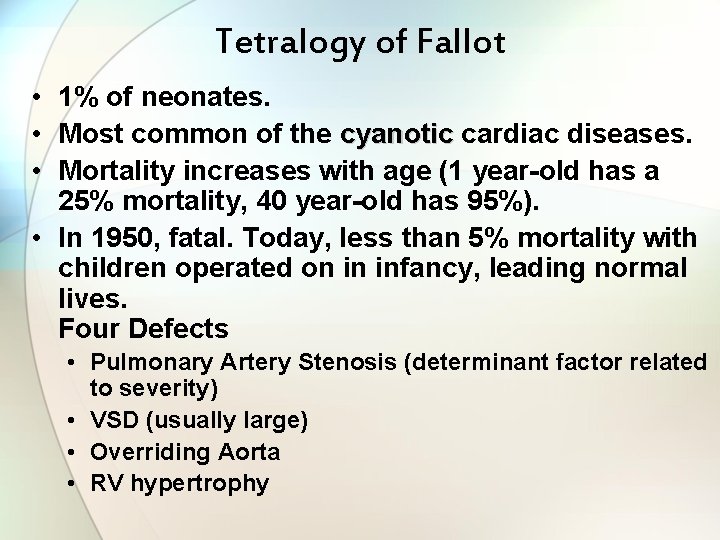
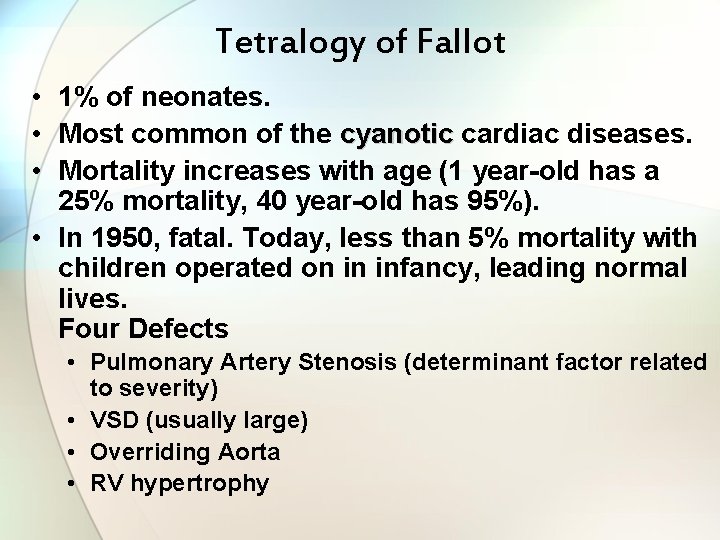
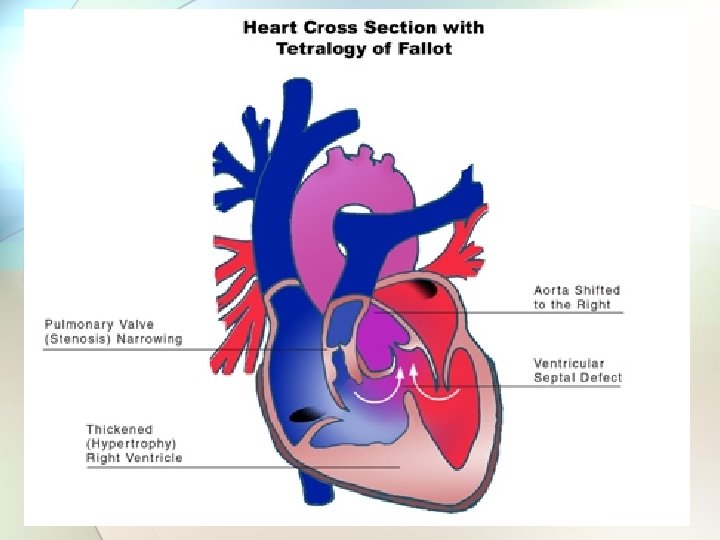
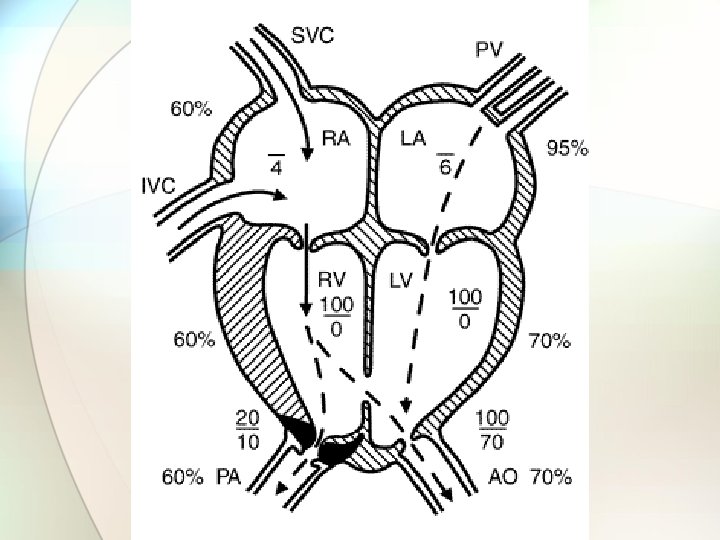
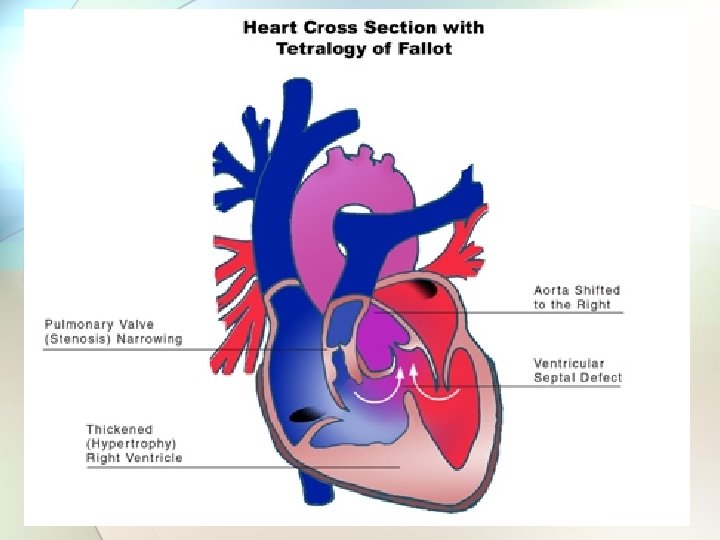
Tetralogy of Fallot • 1% of neonates. • Most common of the cyanotic cardiac diseases. • Mortality increases with age (1 year-old has a 25% mortality, 40 year-old has 95%). • In 1950, fatal. Today, less than 5% mortality with children operated on in infancy, leading normal lives. Four Defects • Pulmonary Artery Stenosis (determinant factor related to severity) • VSD (usually large) • Overriding Aorta • RV hypertrophy
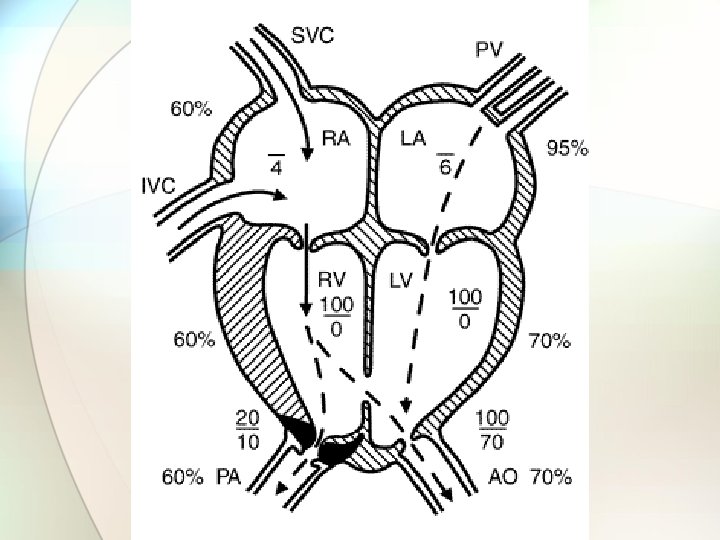
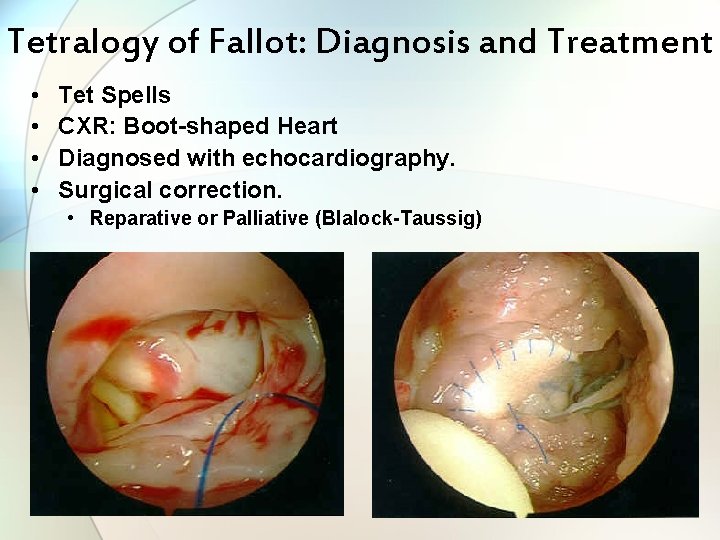
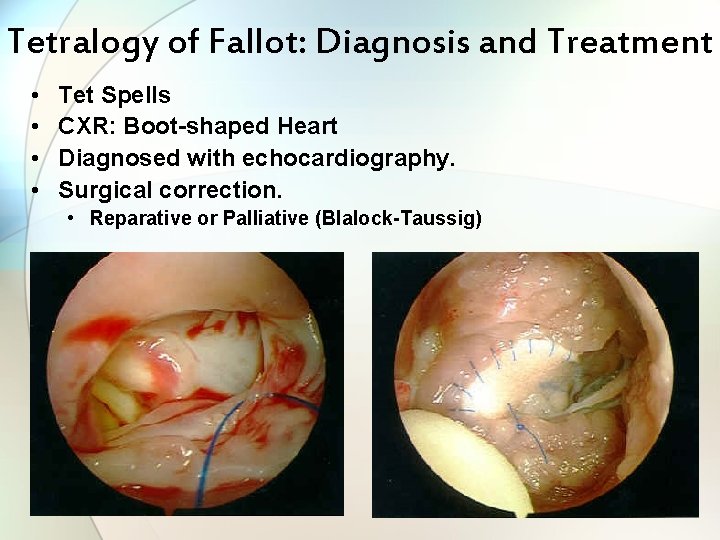
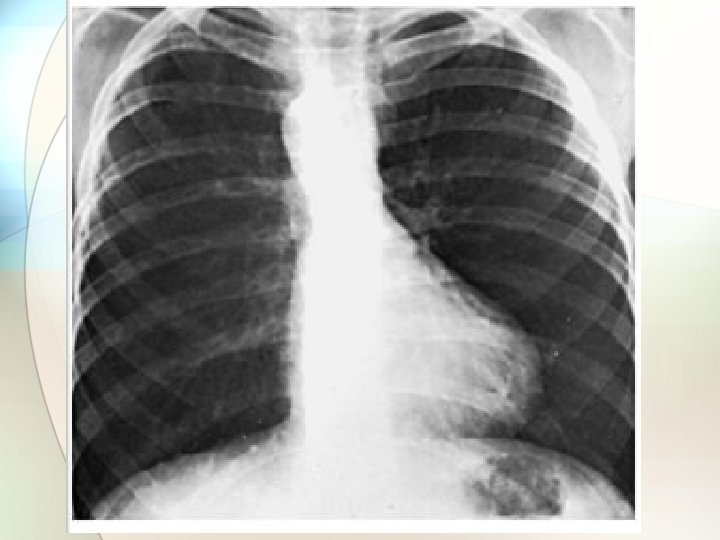
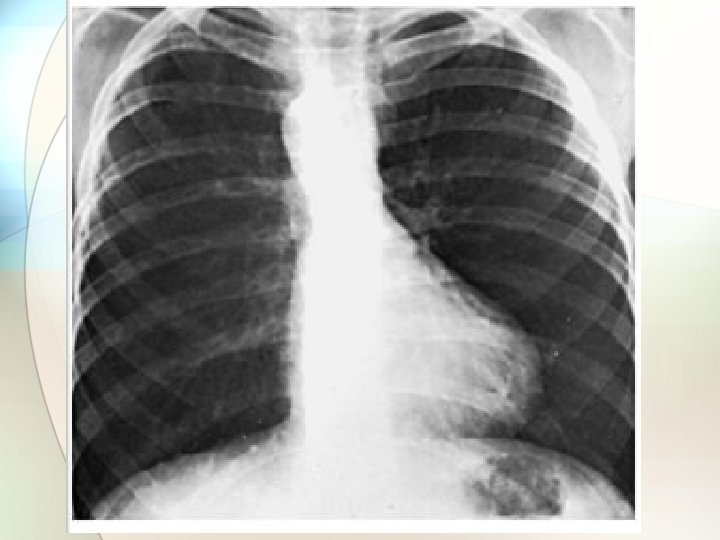
Tetralogy of Fallot: Diagnosis and Treatment • • Tet Spells CXR: Boot-shaped Heart Diagnosed with echocardiography. Surgical correction. • Reparative or Palliative (Blalock-Taussig)
Blalock-Taussig • Something the Lord Made. • Vivien Thomas
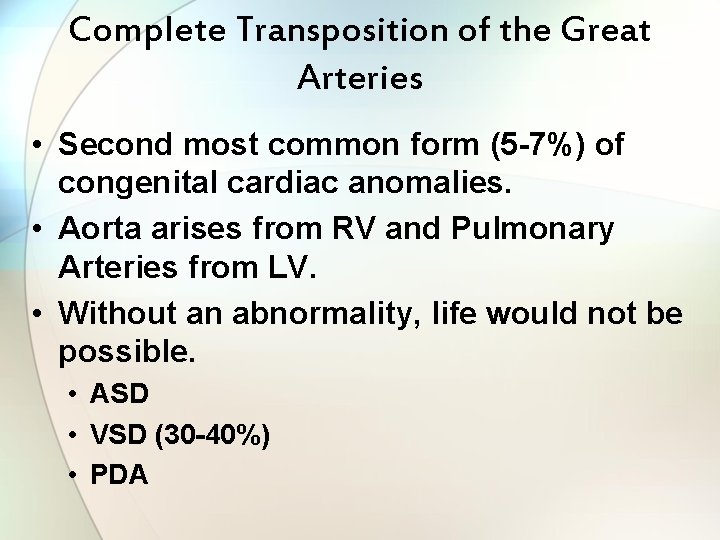
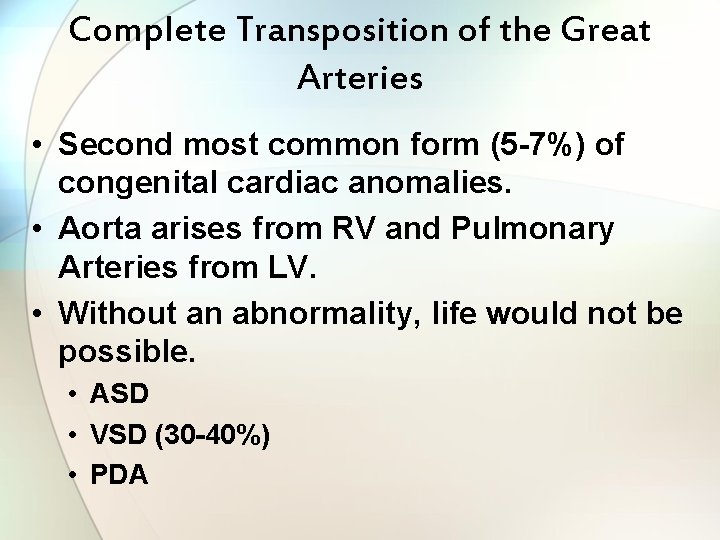
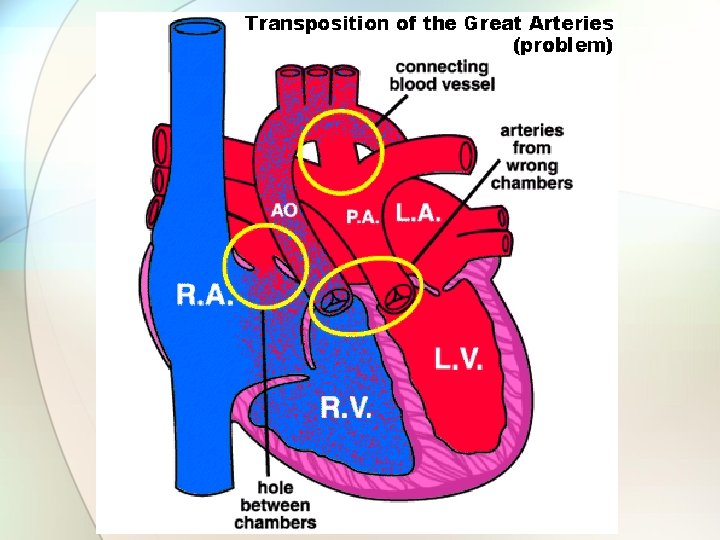
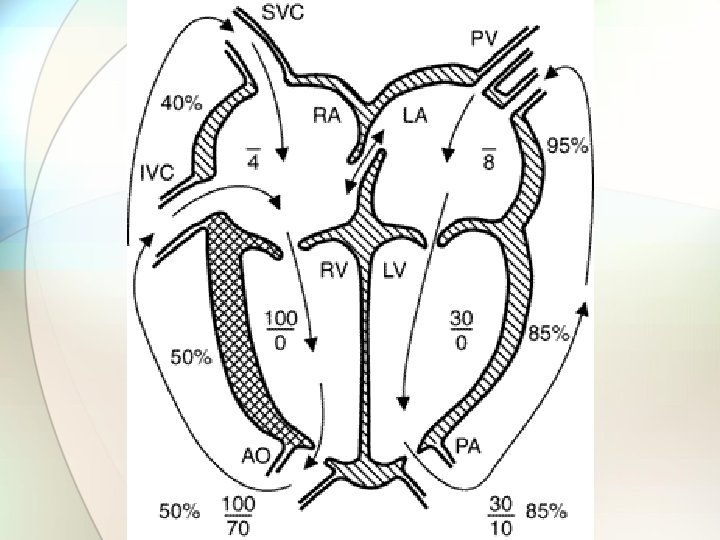
Complete Transposition of the Great Arteries • Second most common form (5 -7%) of congenital cardiac anomalies. • Aorta arises from RV and Pulmonary Arteries from LV. • Without an abnormality, life would not be possible. • ASD • VSD (30 -40%) • PDA
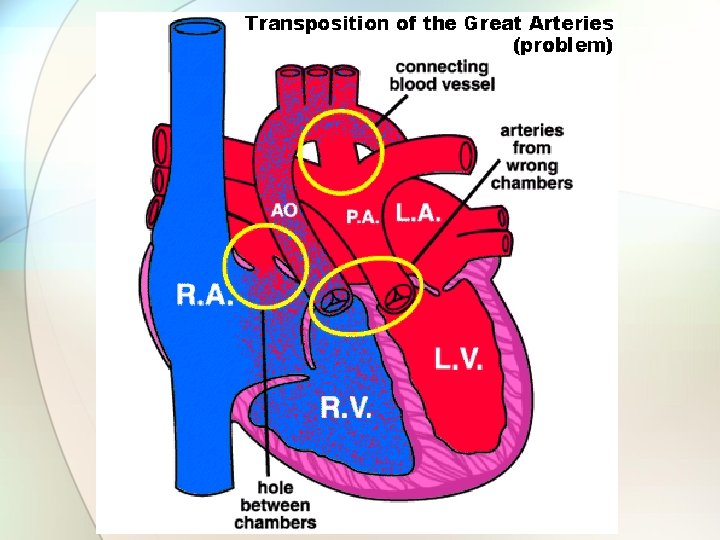
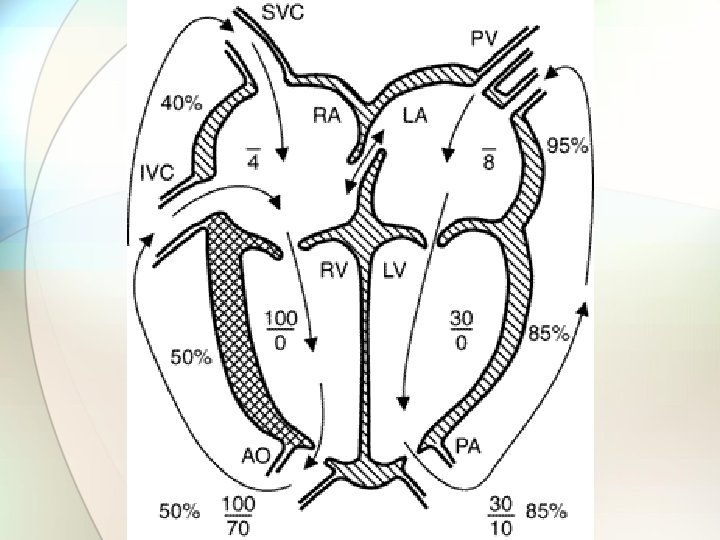
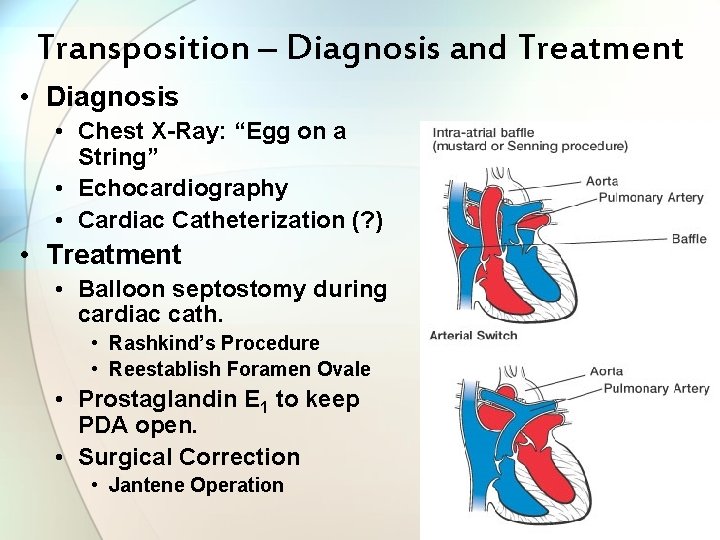
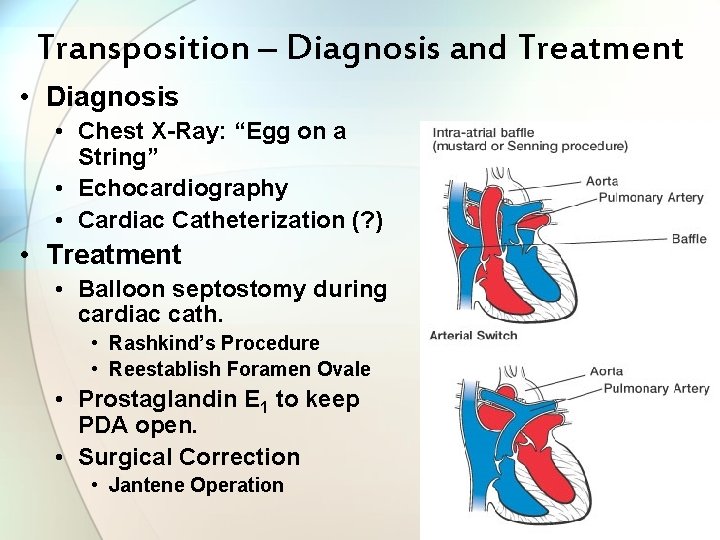
Transposition – Diagnosis and Treatment • Diagnosis • Chest X-Ray: “Egg on a String” • Echocardiography • Cardiac Catheterization (? ) • Treatment • Balloon septostomy during cardiac cath. • Rashkind’s Procedure • Reestablish Foramen Ovale • Prostaglandin E 1 to keep PDA open. • Surgical Correction • Jantene Operation
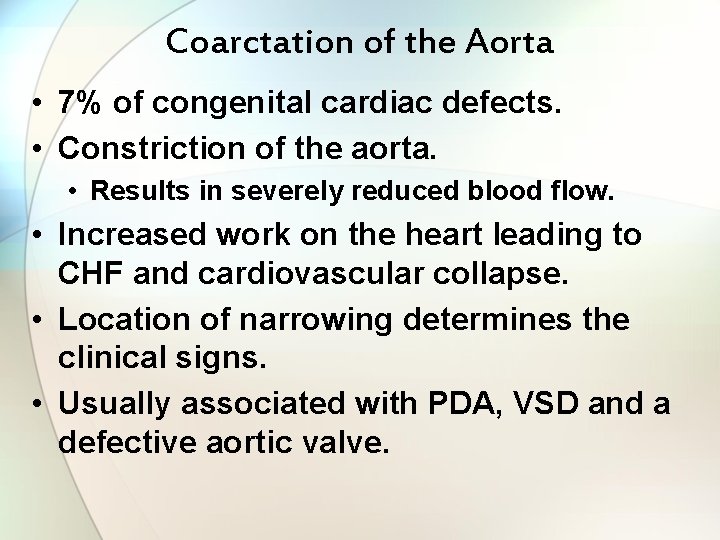
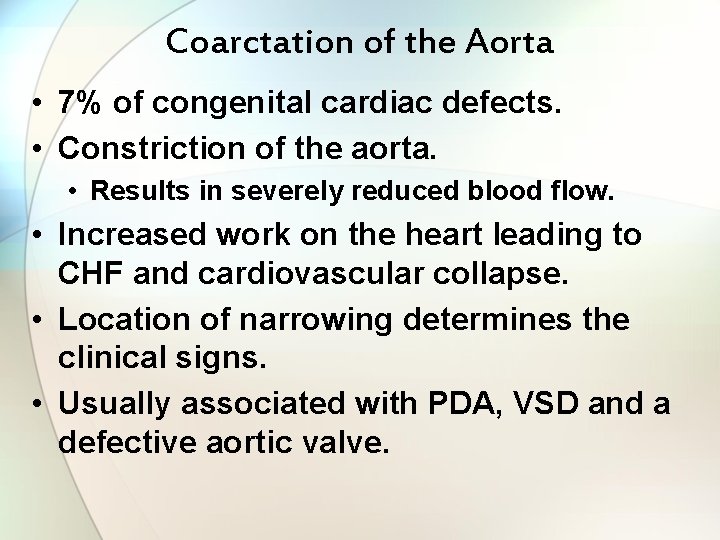
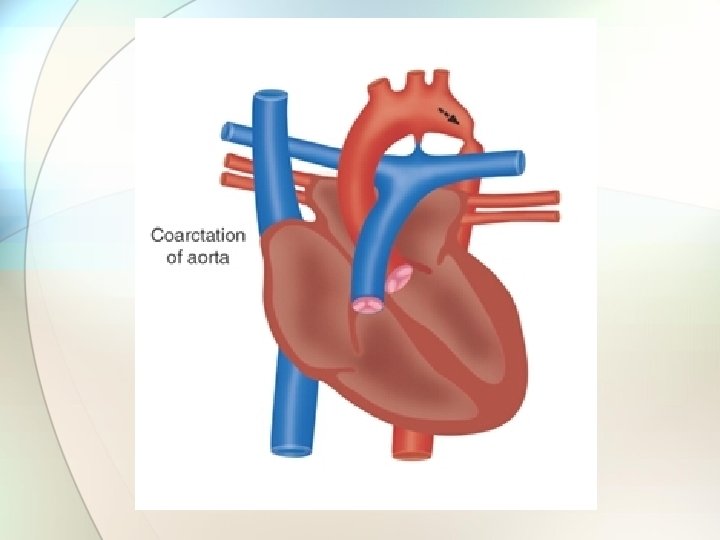
Coarctation of the Aorta • 7% of congenital cardiac defects. • Constriction of the aorta. • Results in severely reduced blood flow. • Increased work on the heart leading to CHF and cardiovascular collapse. • Location of narrowing determines the clinical signs. • Usually associated with PDA, VSD and a defective aortic valve.
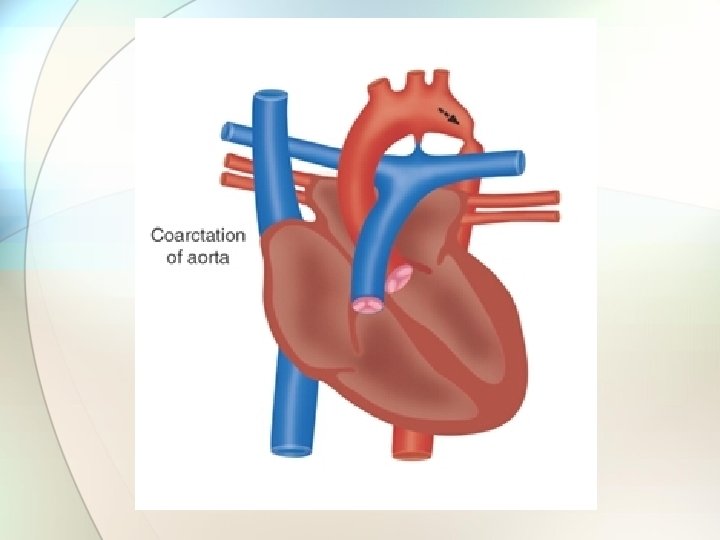
Location of Coarctation • Pre-Ductal • Less common but more serious • Associated with VSD, PDA, Transposition • Post-Ductal • More common • Often associated with collateral circulation beyond coarctation, which minimizes effect. • Diagnosed by a difference in blood pressure between lower extremities and upper ones. • Pressure in upper extremities > lower
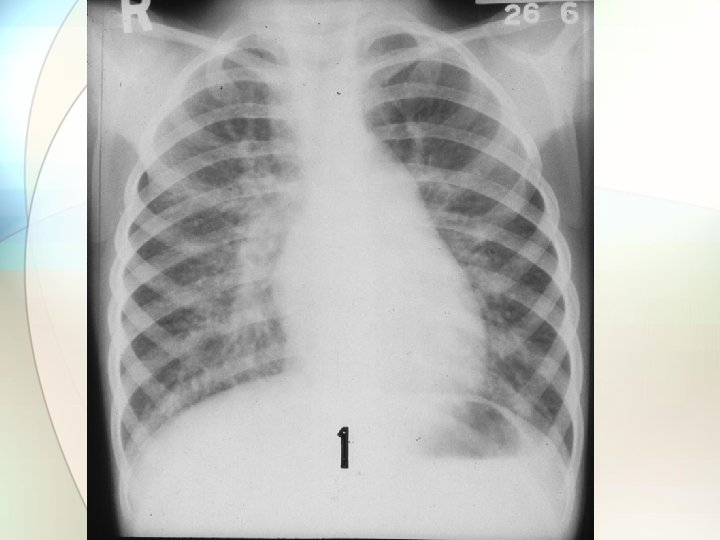
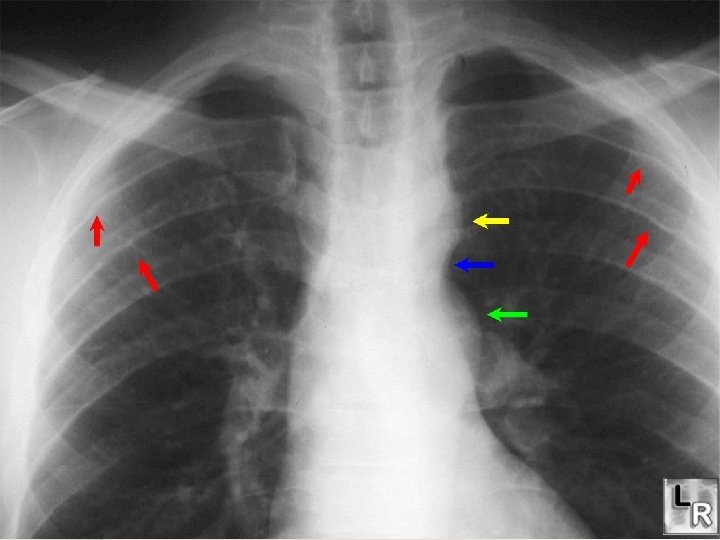
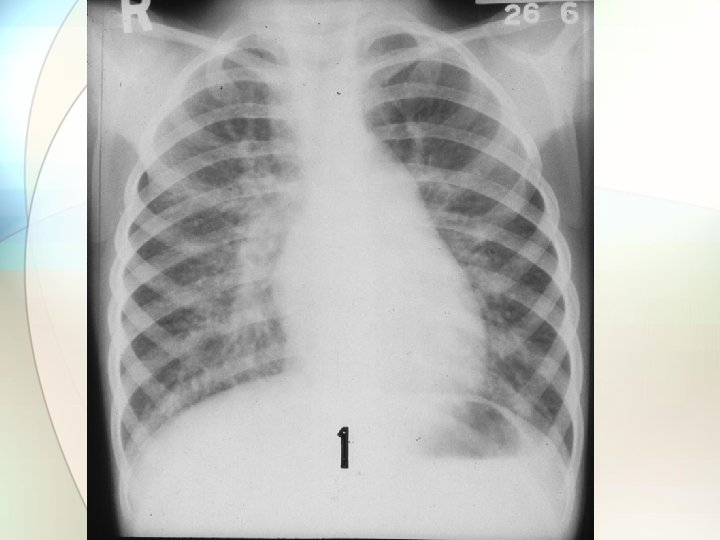
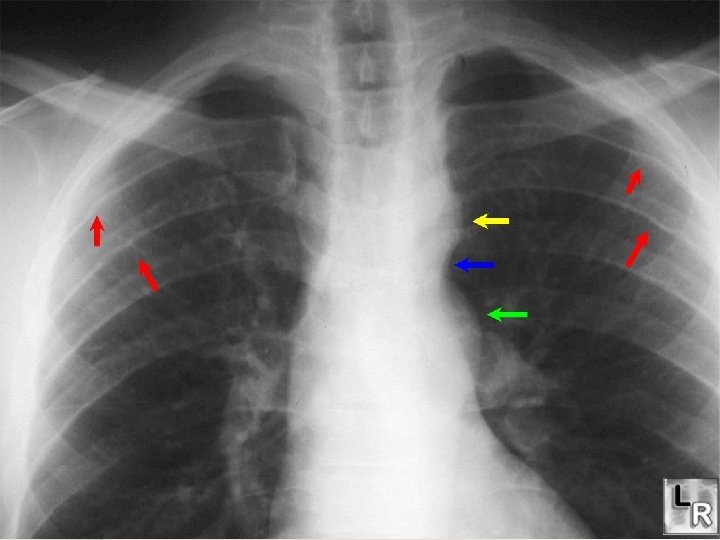
Coarctation – Diagnosis and Treatment • Diagnosis • Chest X-Ray • Echocardiography • Cardiac catheterization • Treatment • Support with inotropic agents (Dopamine). • Prostaglandins to maintain PDA. • Surgical repair

Anomalous Venous Return • Return of pulmonary venous blood to the right atrium instead of the left. • ASD is present to sustain life. • Can also be partial. • Cyanosis usually present. • Diagnosed with echocardiography. • Surgical correction with reimplantation of pulmonary veins.

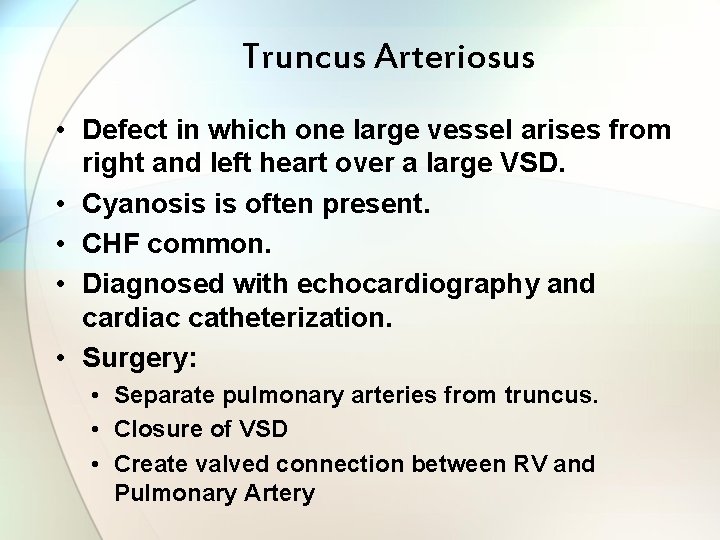
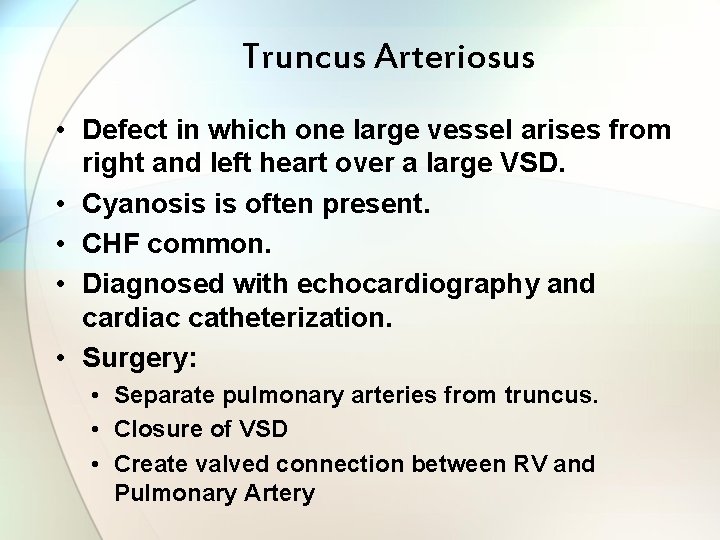
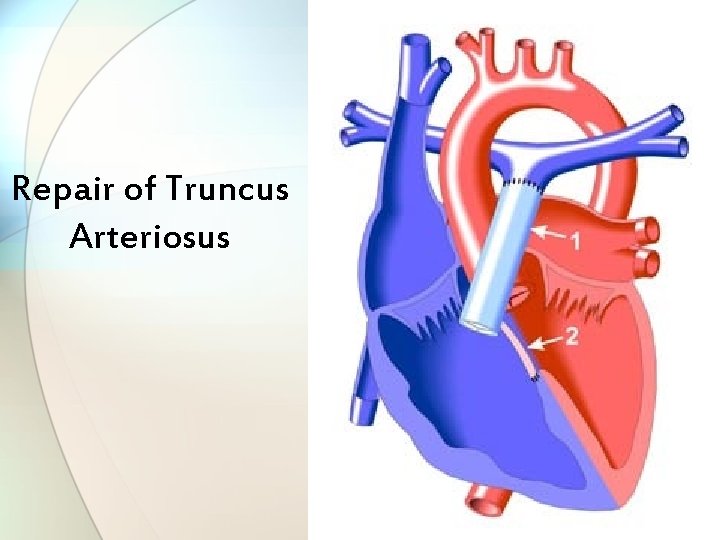
Truncus Arteriosus • Defect in which one large vessel arises from right and left heart over a large VSD. • Cyanosis is often present. • CHF common. • Diagnosed with echocardiography and cardiac catheterization. • Surgery: • Separate pulmonary arteries from truncus. • Closure of VSD • Create valved connection between RV and Pulmonary Artery
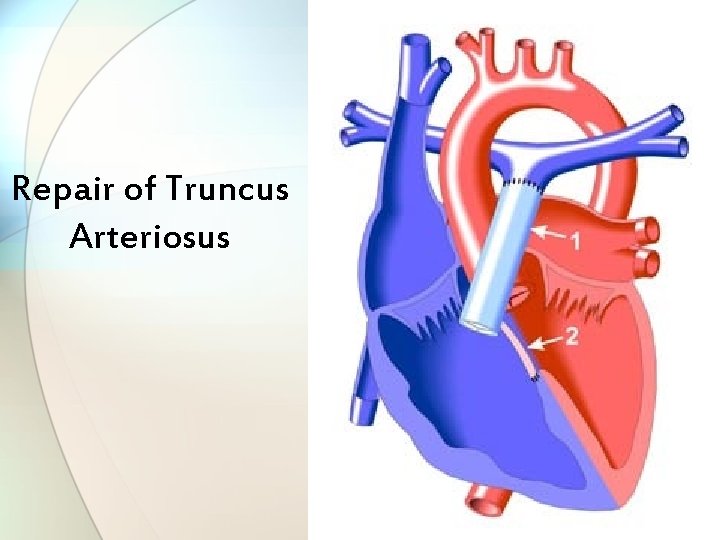
Repair of Truncus Arteriosus
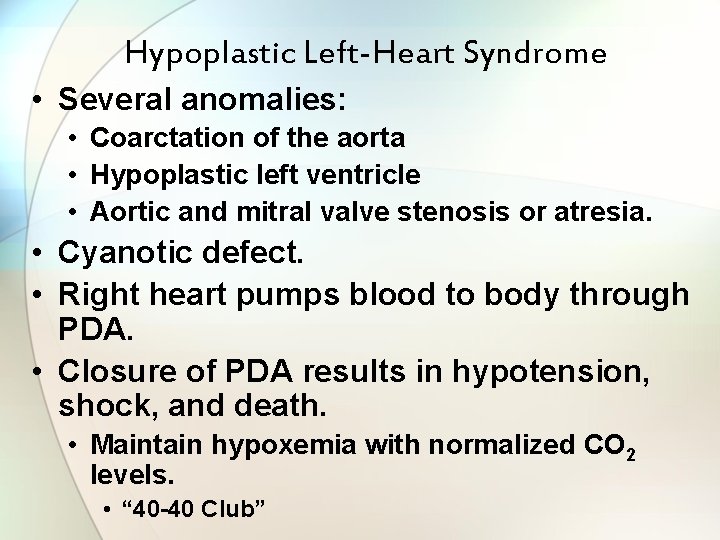
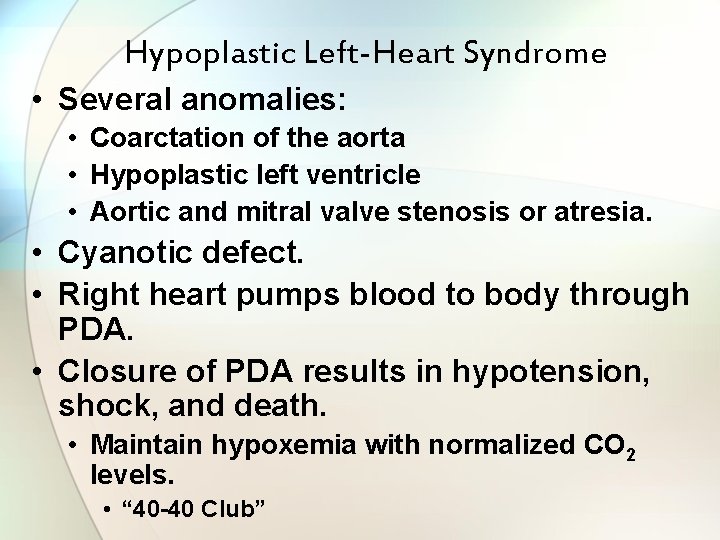
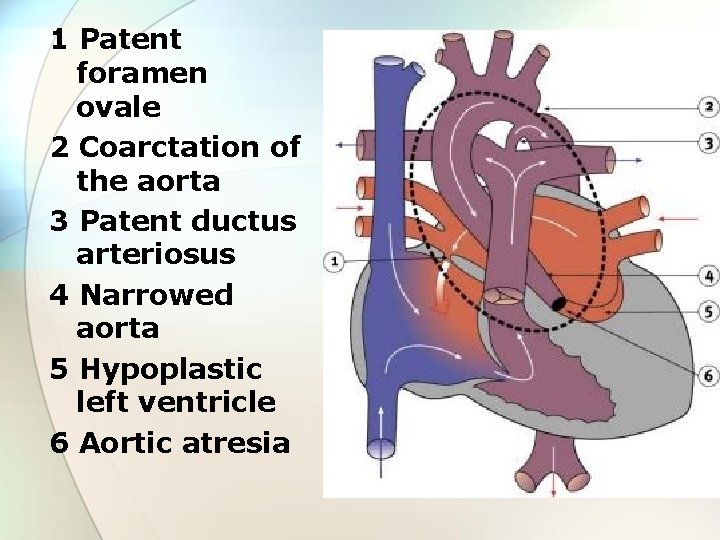
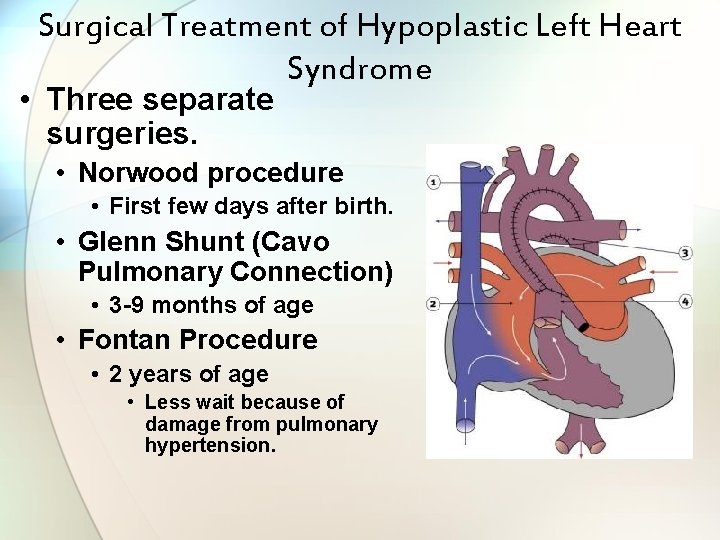
Hypoplastic Left-Heart Syndrome • Several anomalies: • Coarctation of the aorta • Hypoplastic left ventricle • Aortic and mitral valve stenosis or atresia. • Cyanotic defect. • Right heart pumps blood to body through PDA. • Closure of PDA results in hypotension, shock, and death. • Maintain hypoxemia with normalized CO 2 levels. • “ 40 -40 Club”
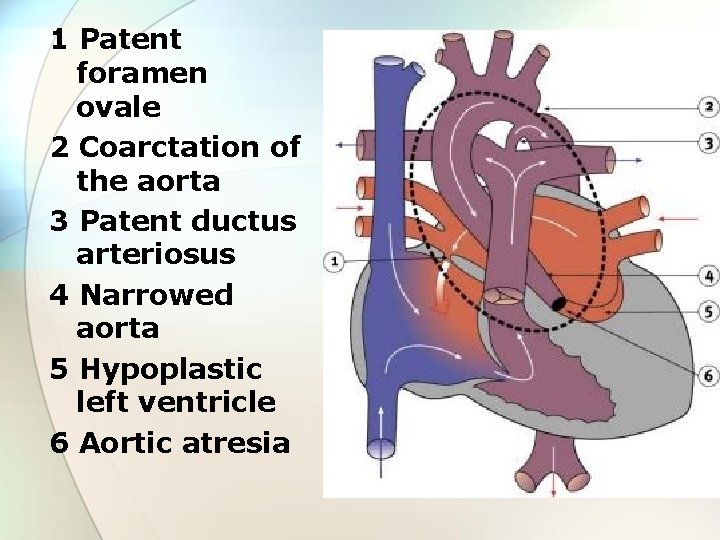
1 Patent foramen ovale 2 Coarctation of the aorta 3 Patent ductus arteriosus 4 Narrowed aorta 5 Hypoplastic left ventricle 6 Aortic atresia
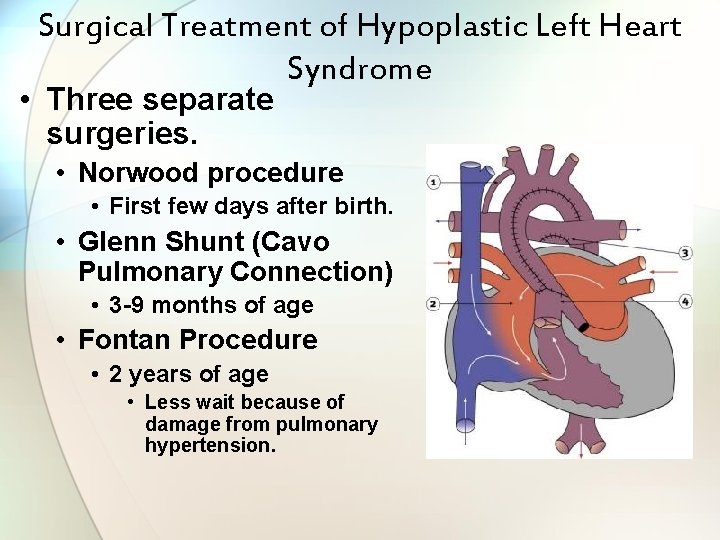
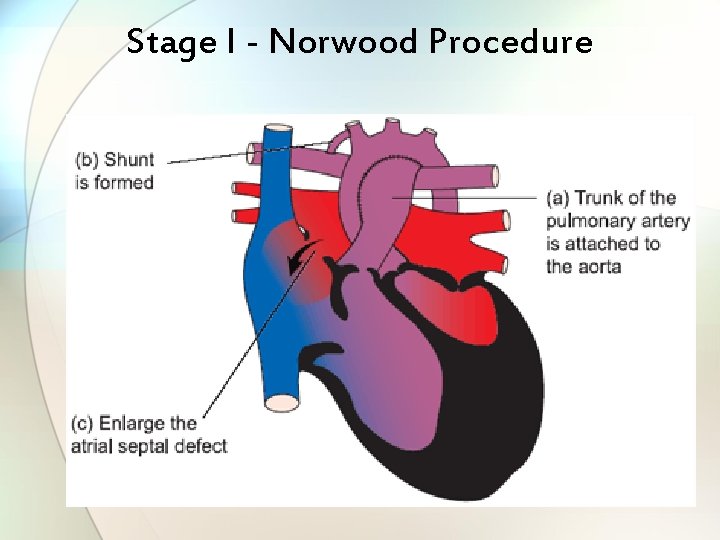
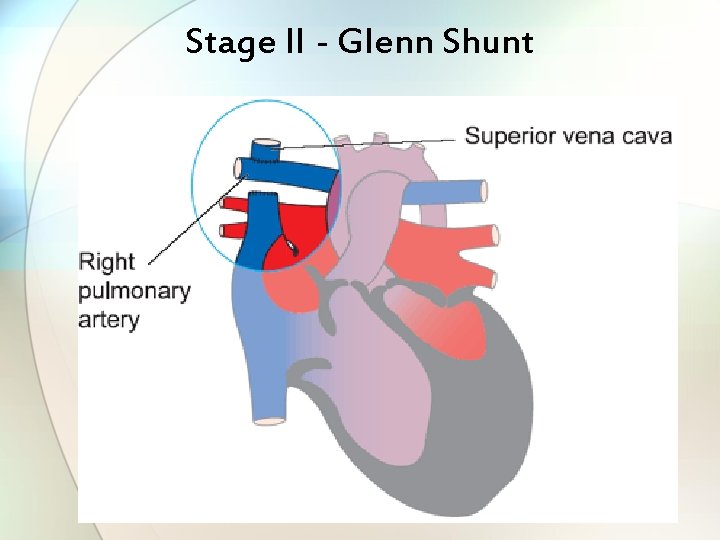
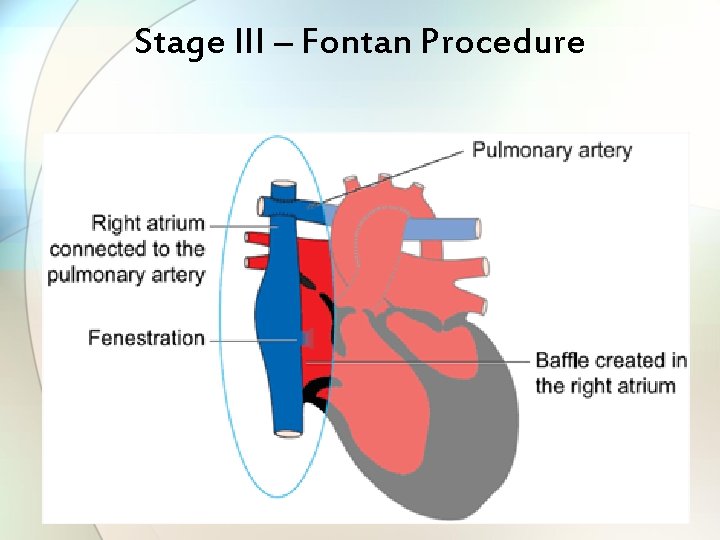
Surgical Treatment of Hypoplastic Left Heart Syndrome • Three separate surgeries. • Norwood procedure • First few days after birth. • Glenn Shunt (Cavo Pulmonary Connection) • 3 -9 months of age • Fontan Procedure • 2 years of age • Less wait because of damage from pulmonary hypertension.
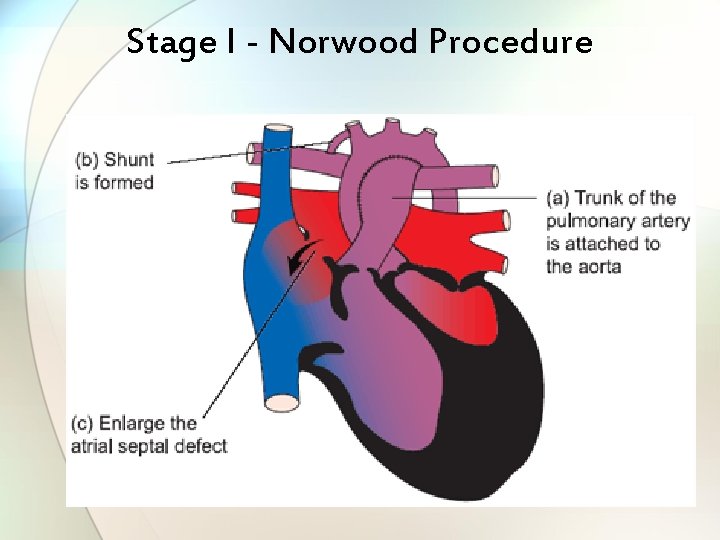
Stage I - Norwood Procedure
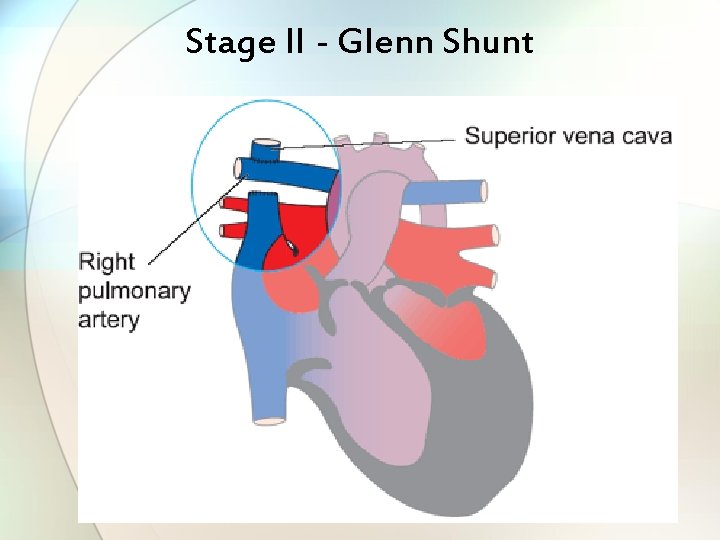
Stage II - Glenn Shunt
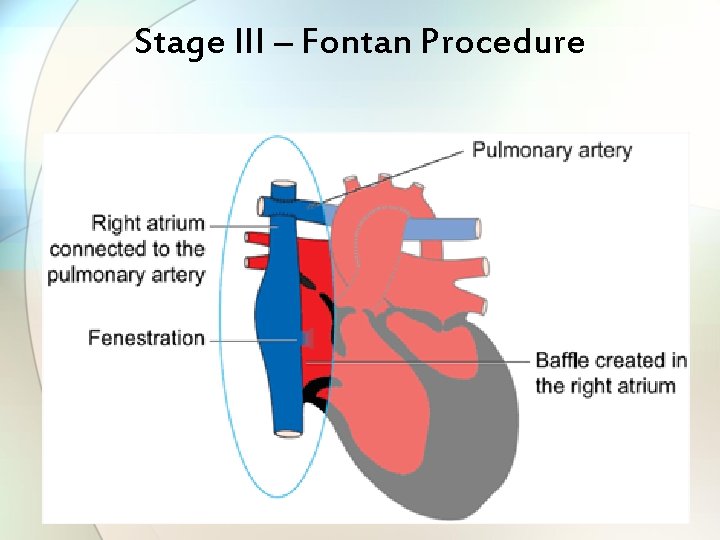
Stage III – Fontan Procedure