Role of Anesthesiologist in PeriOperative Period essam manaa



- Slides: 35
ﺑﺴﻢ ﺍﻟﻠﻪ ﺍﻟﺮﺣﻤﻦ ﺍﻟﺮﺣﻴﻢ Role of Anesthesiologist in Peri-Operative Period essam manaa assistant professor & consultant anesthesia dept. , kkuh e_manaa@yahoo. com
Lecture Objectives. . Students at the end of the lecture will be able to: a) Obtain a full history and physical examination including allergies, current medications, past anesthetic history, family anesthetic history b) Understand how patient co-morbidities can affect the anesthetic plan c) Able to plan an anesthetic for a basic surgical procedure d) Understand risk stratification of a patient undergoing anesthesia
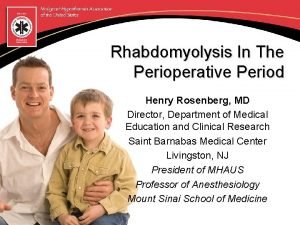
An Anesthesiologist or Anaesthetist is a physician trained in anesthesia and perioperative medicine. They provide medical care to patients in a wide variety of (usually acute) situations. Anesthesiologists are responsible for ensuring the delivery of anesthesia safely to patients in virtually all health care settings, including all major medical and tertiary care facilities.
Pre-Anesthesia Clinic KKUH
Stages of the Peri-Operative Period Pre-Operative From time of decision to have surgery until admitted into the OR theatre.
Intra-Operative Time from entering the OR theatre to entering the Recovering Room or Post Anesthetic Care Unit (PACU)
Post-Operative Time from leaving the RR or PACU until time of follow-up evaluation (often as out-patient)

Preoperative visit Preoperative Preparation Preoperative Evaluation Preoperative Medication
Preoperative Preparation To educate about anesthesia , perioperative care and pain management to reduce anxiety To determine which lab test or further medical consultation are needed To choose care plan guided by patient's choice and risk factors Benefits from surgery ← → Risk of complications
Preoperative Evaluation & Medication Evaluation - A thorough history - Habits (smoking, alcohol) - Medications (herbals, Drugs) and allergies Physical exam - Complete review of systems i. e. Functional Status (METs) Pre-op medication
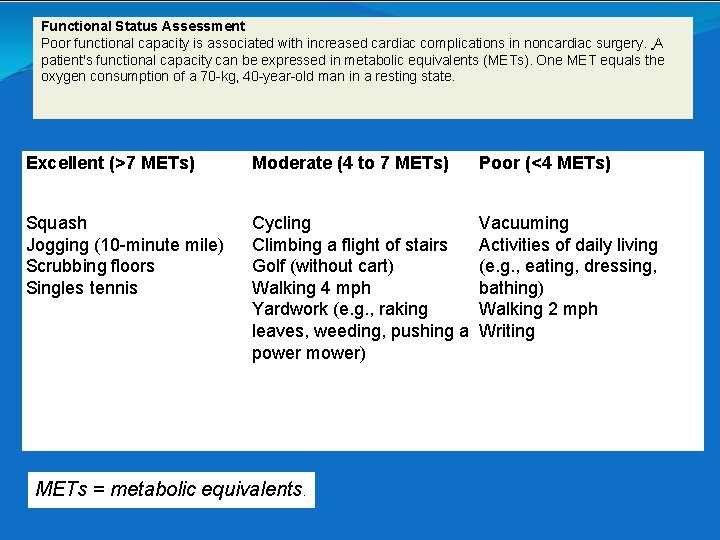
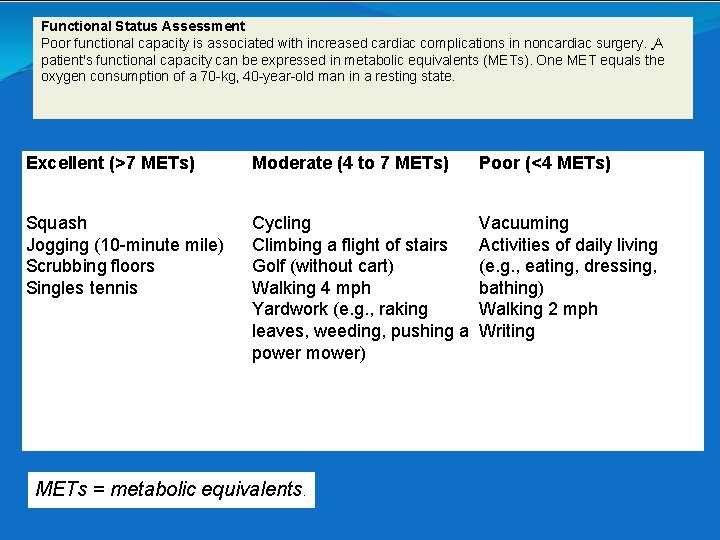
Functional Status Assessment Poor functional capacity is associated with increased cardiac complications in noncardiac surgery. A patient's functional capacity can be expressed in metabolic equivalents (METs). One MET equals the oxygen consumption of a 70 -kg, 40 -year-old man in a resting state. Excellent (>7 METs) Moderate (4 to 7 METs) Squash Jogging (10 -minute mile) Scrubbing floors Singles tennis Cycling Vacuuming Climbing a flight of stairs Activities of daily living Golf (without cart) (e. g. , eating, dressing, Walking 4 mph bathing) Yardwork (e. g. , raking Walking 2 mph leaves, weeding, pushing a Writing power mower) METs = metabolic equivalents. Poor (<4 METs)
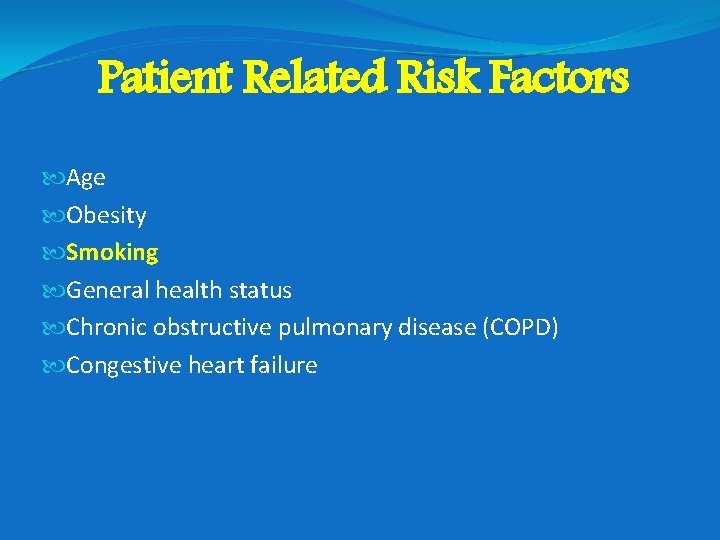
Patient Related Risk Factors Age Obesity Smoking General health status Chronic obstructive pulmonary disease (COPD) Congestive heart failure
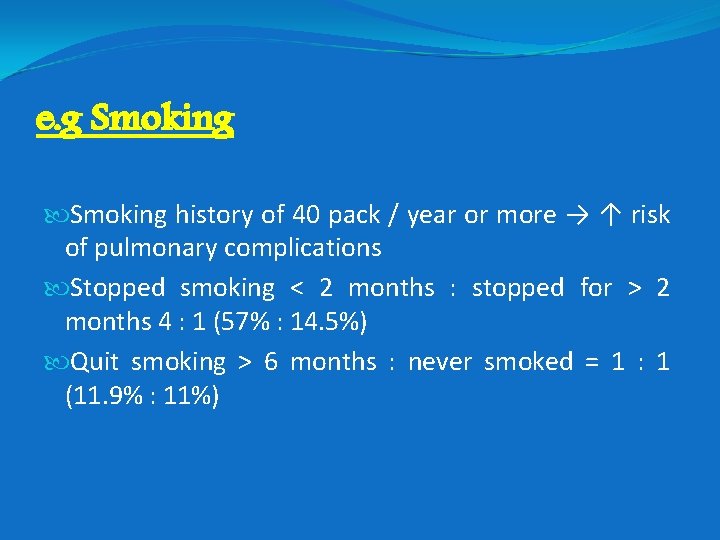
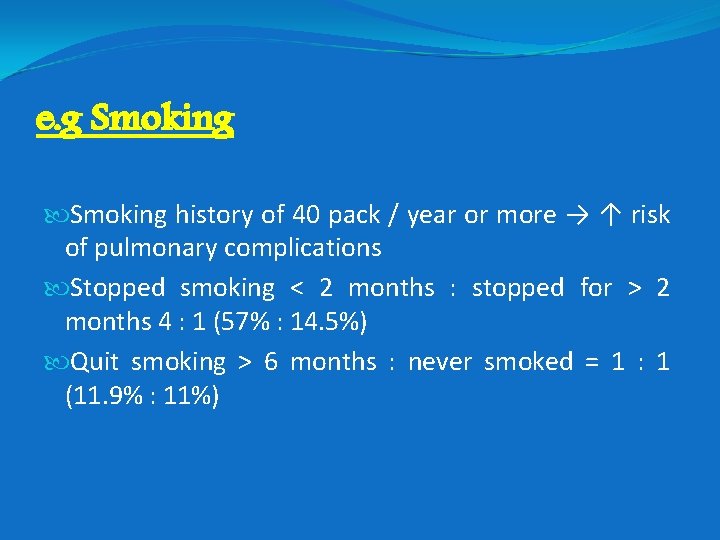
e. g Smoking history of 40 pack / year or more → ↑ risk of pulmonary complications Stopped smoking < 2 months : stopped for > 2 months 4 : 1 (57% : 14. 5%) Quit smoking > 6 months : never smoked = 1 : 1 (11. 9% : 11%)
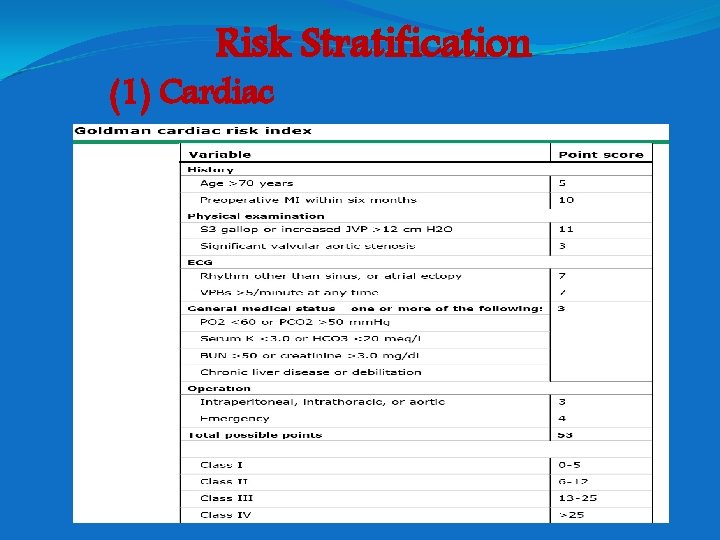
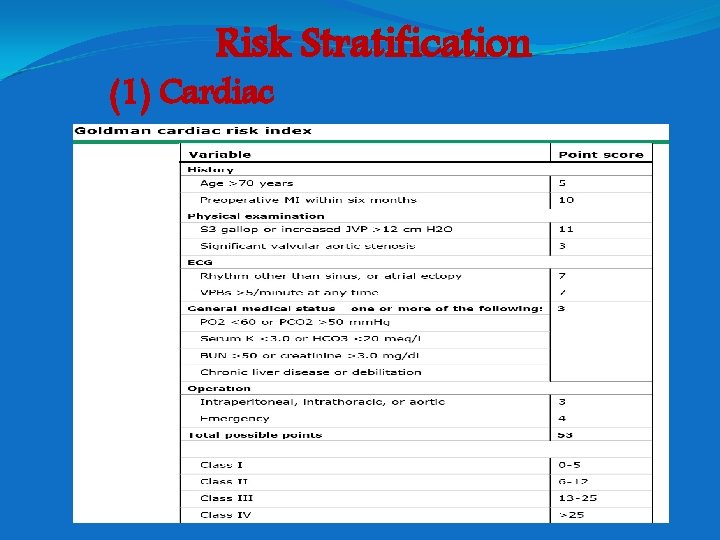
Risk Stratification (1) Cardiac
This is a multi-factorial index of cardiac risk in the non-cardiac surgical setting. It was developed for preoperative identification of patients at risk from major perioperative cardiovascular complications. The data were derived retrospectively in 1977 from 1001 patients undergoing non-cardiac surgery. Patients with scores >25 had a 22% incidence of death, with a 56% incidence of severe cardiovascular complications. Patients with scores <26 had a 4% incidence of death, with a 17% incidence of severe cardiovascular complications. Patients with scores <6 had a 0. 2% incidence of death, with a 0. 7% incidence of severe cardiovascular complications. Multifactorial index of cardiac risk in noncardiac surgical procedures Goldman L, Caldera DL, Nussbaum SR N Engl J Med 1977; 297: 845 -50
(2) ASA Physical Status (Br J Anaesth 2004; 93: 393– 399. ) ASA 1 Healthy patient without organic biochemical or psychiatric disease. ASA 2 A Patient with mild systemic disease (controlled hypertension or diabetes without systemic effects). No significant impact on daily activity. Unlikely impact on anesthesia and surgery. ASA 3 Significant or severe systemic disease that limits normal activity (controlled congestive heart failure (CHF), stable angina, old heart attack, poorly controlled hypertension, morbid obesity, chronic renal failure). Significant impact on daily activity. Likely impact on anesthesia and surgery. ASA 4 Severe disease that is a constant threat to life or requires intensive therapy (symptomatic COPD, symptomatic CHF, hepatorenal failure). Serious limitation of daily activity. ASA 5 Moribund patient who is equally likely to die in the next 24 hours with or without surgery (multiorgan failure, sepsis syndrome). ASA 6 Brain-dead organ donor “E” Added to the classifications indicates emergency surgery. **Mortality rates of the individual classes showed considerable variation, with 0 -0. 3% for ASA I, 0. 3 -1. 4% for ASA II, 1. 8 -4. 5% for ASA III, 7. 8 -25. 9% for ASA IV and 9. 457. 8% ASA V
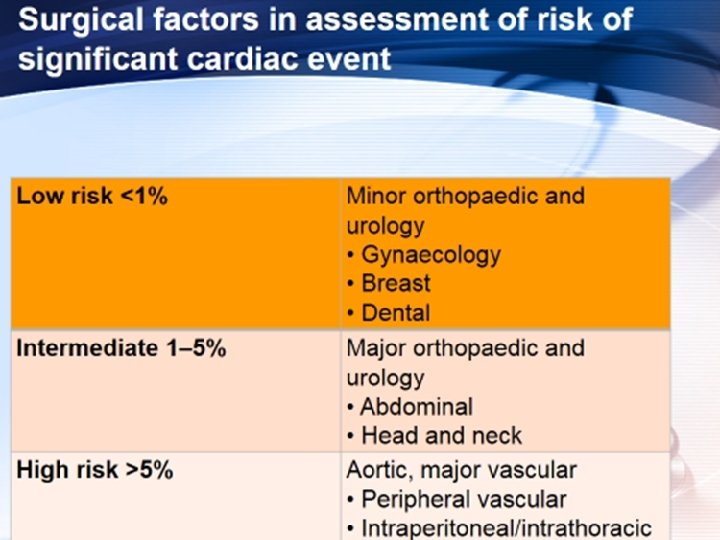
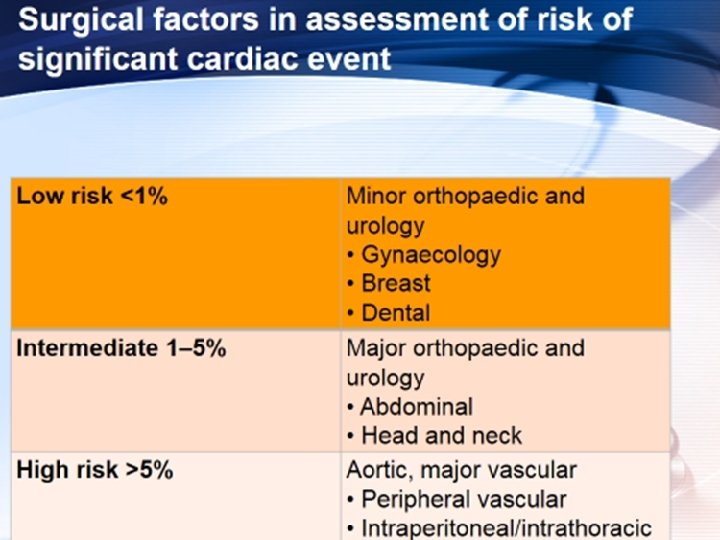
#: Surgery Low Risk* Low risk surgery confirmed Operating room 1. 2. 3. 4. 5. Endoscopic procedures Superficial procedures Cataract surgery Breast surgery Ambulatory surgery *Cardiac risk <1% Testing does not change management
#: Active Cardiac Conditions Active Cardiac conditions Evaluate and treat per current guidelines (Many patients need a cardiac cath. ) Consider Operating Room 1 - Unstable coronary syndromes 2 - Decompensated heart failure 3 - Significant arrhythmias 4 - Severe valvular disease
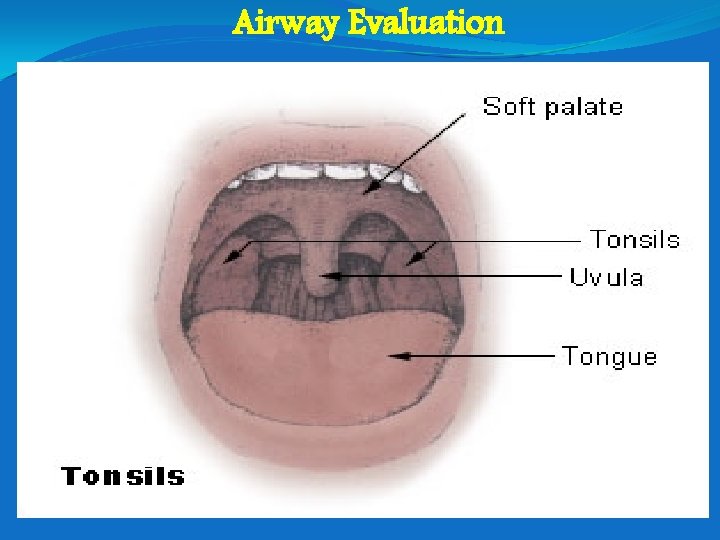
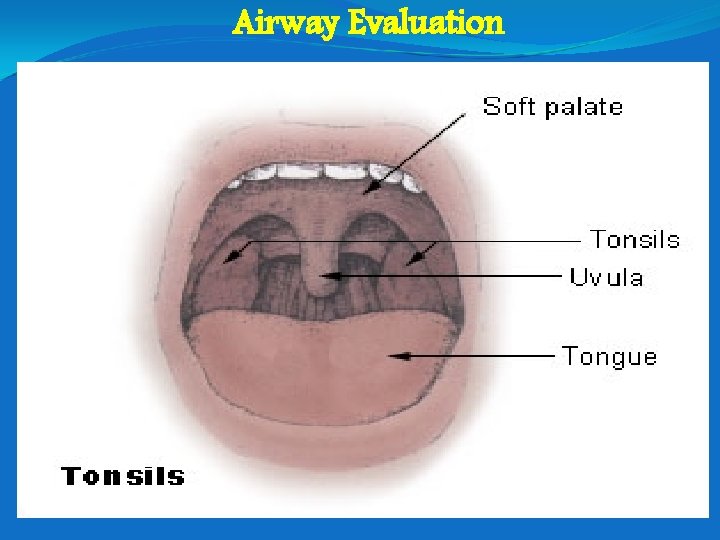
Airway Evaluation
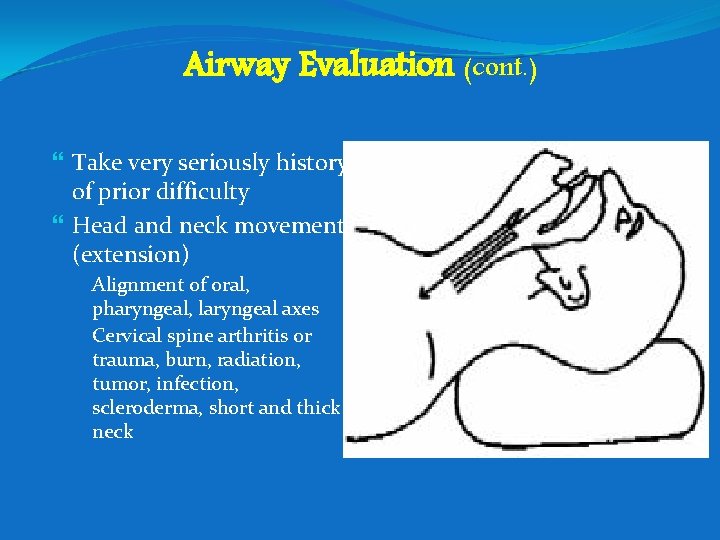
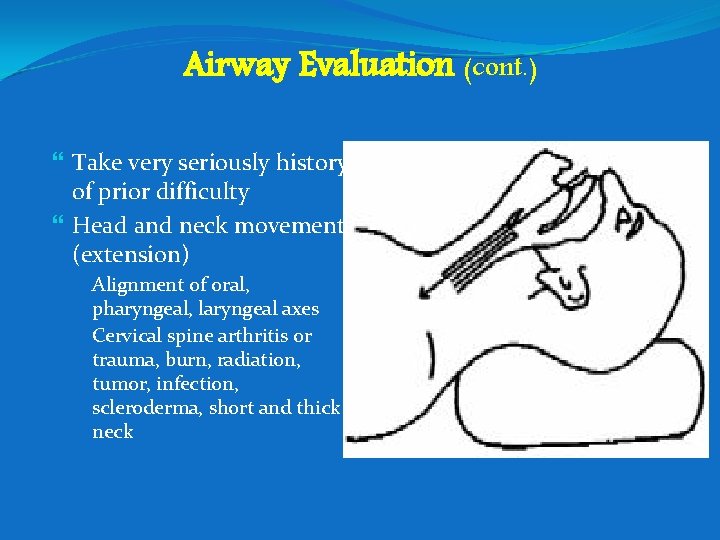
Airway Evaluation (cont. ) Take very seriously history of prior difficulty Head and neck movement (extension) ◦ Alignment of oral, pharyngeal, laryngeal axes ◦ Cervical spine arthritis or trauma, burn, radiation, tumor, infection, scleroderma, short and thick neck
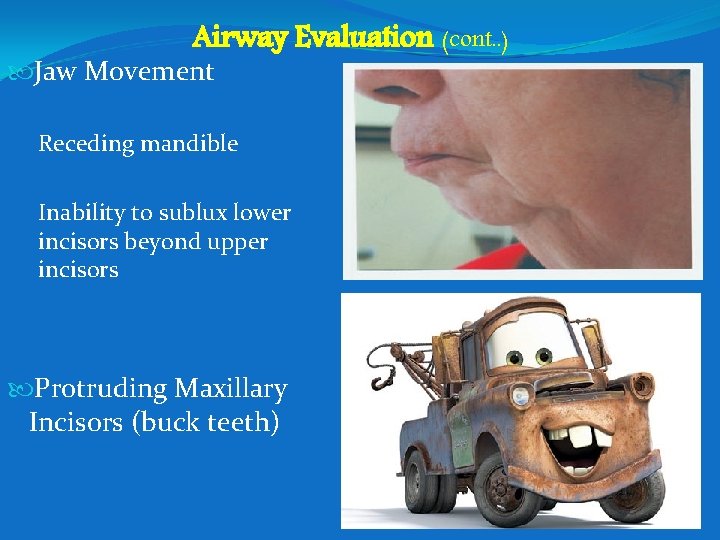
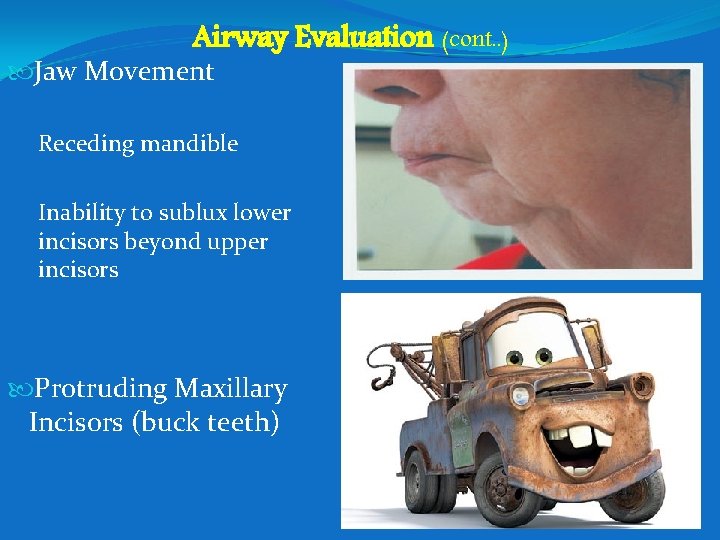
Airway Evaluation (cont. . ) Jaw Movement Receding mandible Inability to sublux lower incisors beyond upper incisors Protruding Maxillary Incisors (buck teeth)
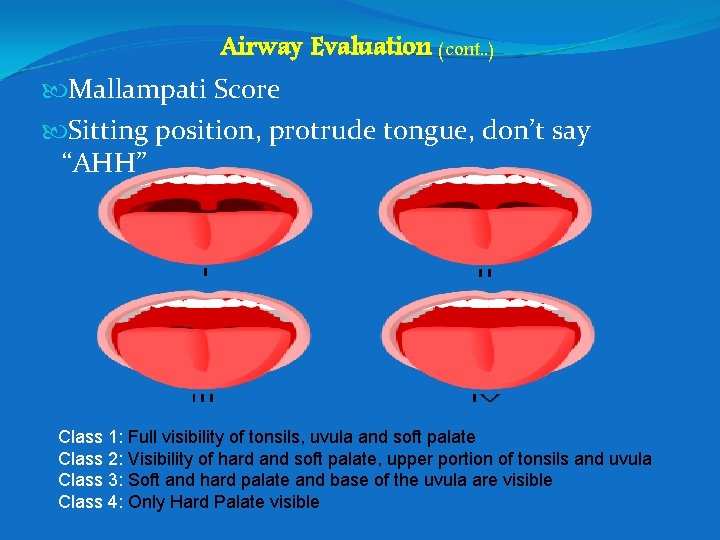
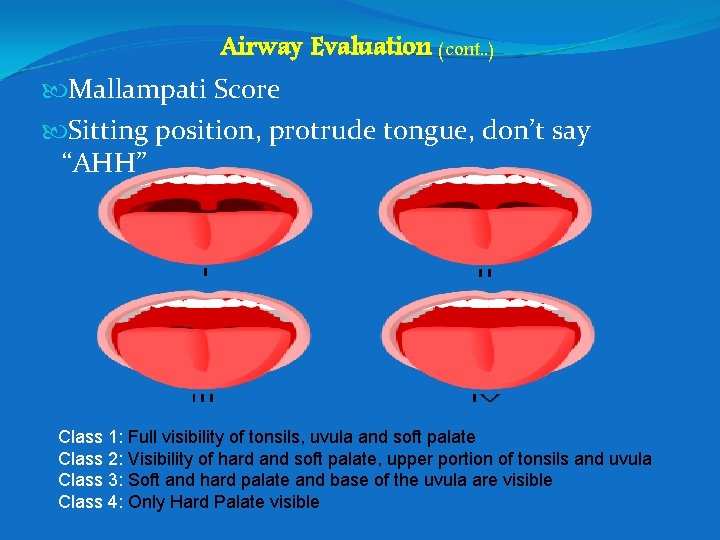
Airway Evaluation (cont. . ) Mallampati Score Sitting position, protrude tongue, don’t say “AHH” Class 1: Full visibility of tonsils, uvula and soft palate Class 2: Visibility of hard and soft palate, upper portion of tonsils and uvula Class 3: Soft and hard palate and base of the uvula are visible Class 4: Only Hard Palate visible

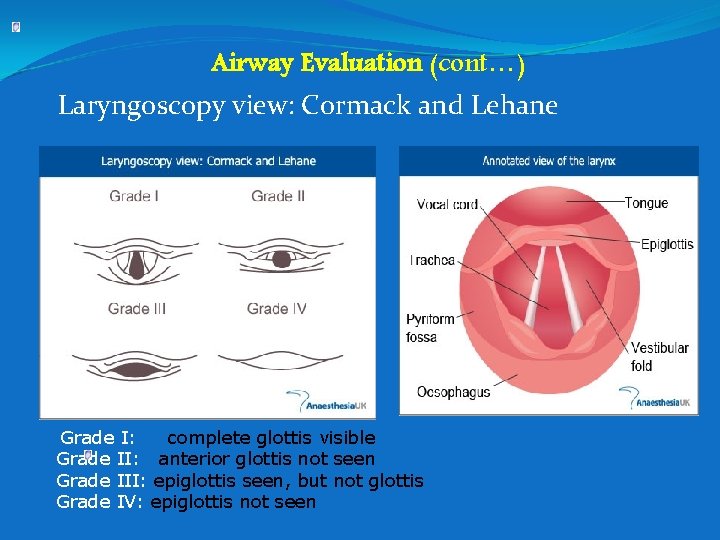
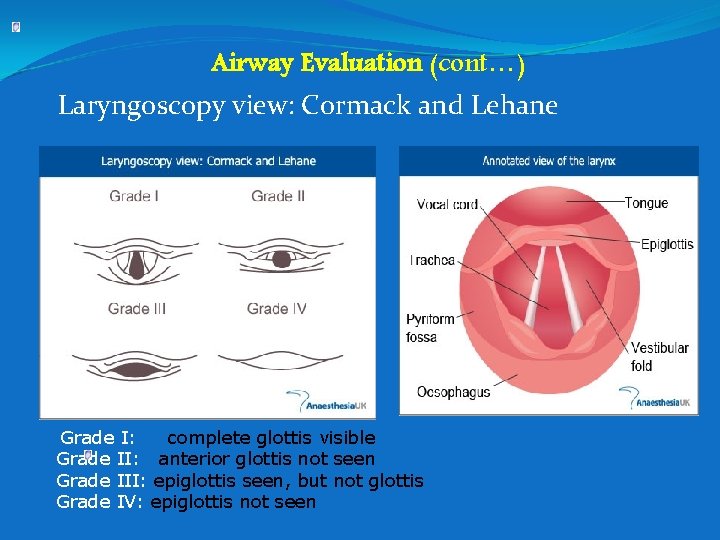
Airway Evaluation (cont…) Laryngoscopy view: Cormack and Lehane Grade I: complete glottis visible Grade II: anterior glottis not seen Grade III: epiglottis seen, but not glottis Grade IV: epiglottis not seen
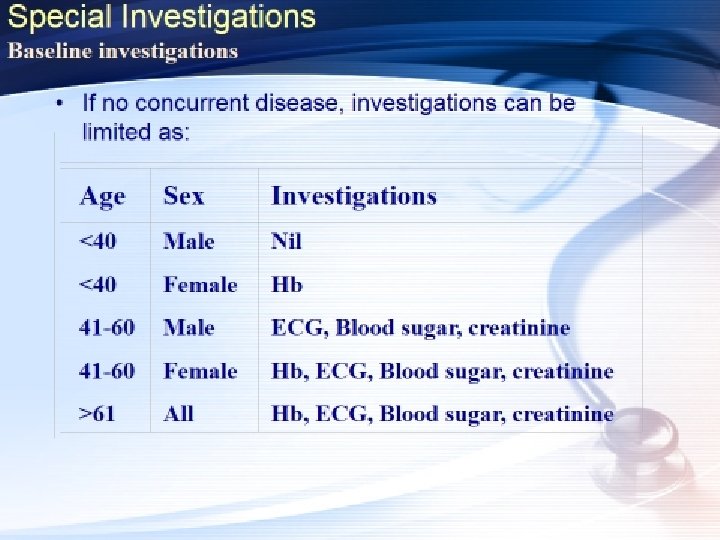
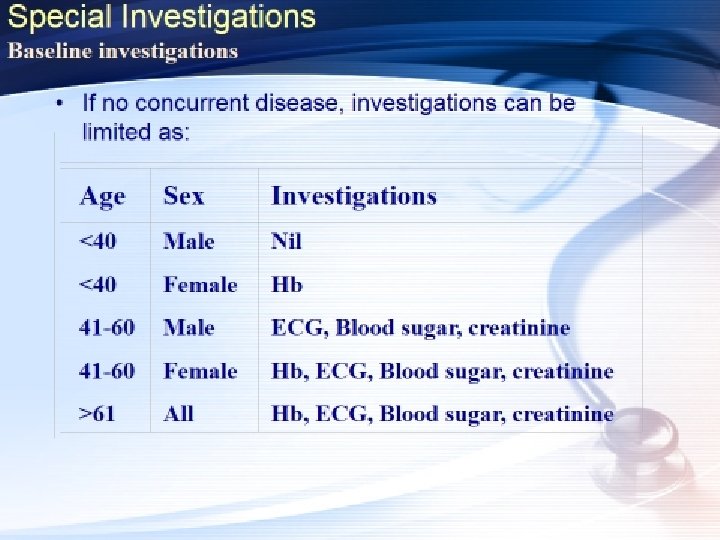
Preoperative Lab. Testing Routine preoperative testing should not be ordered. Preoperative testing should be performed on a selective basis for purposes of guiding or optimizing perioperative management.
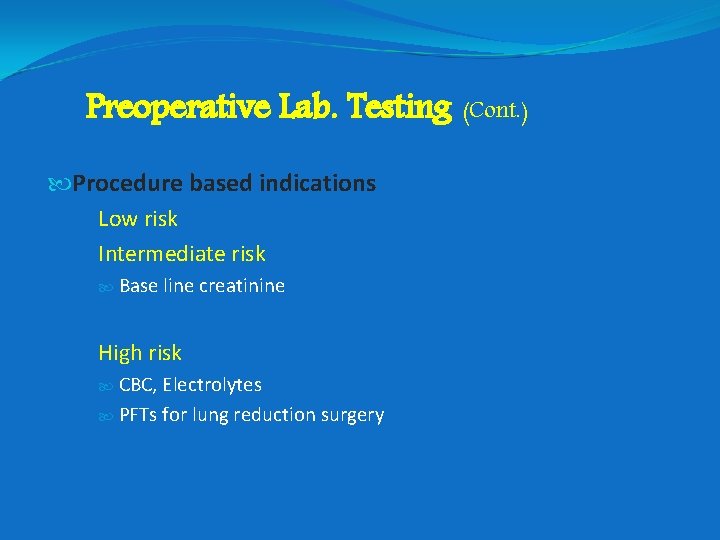
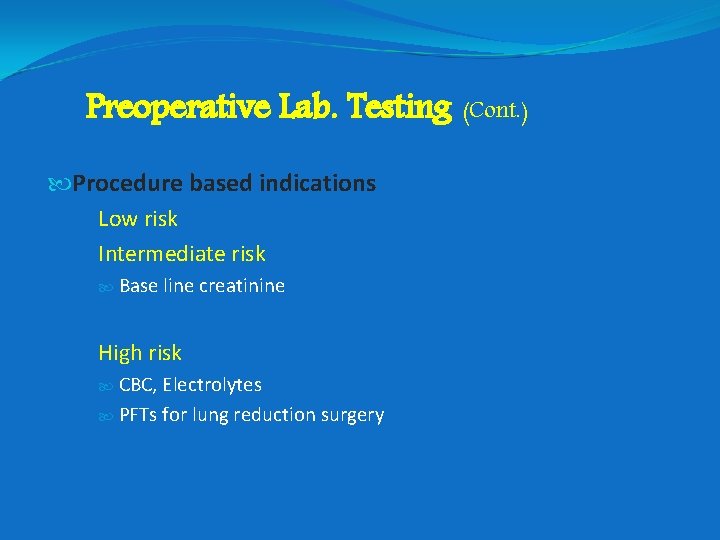
Preoperative Lab. Testing (Cont. ) Procedure based indications Low risk Intermediate risk Base line creatinine High risk CBC, Electrolytes PFTs for lung reduction surgery
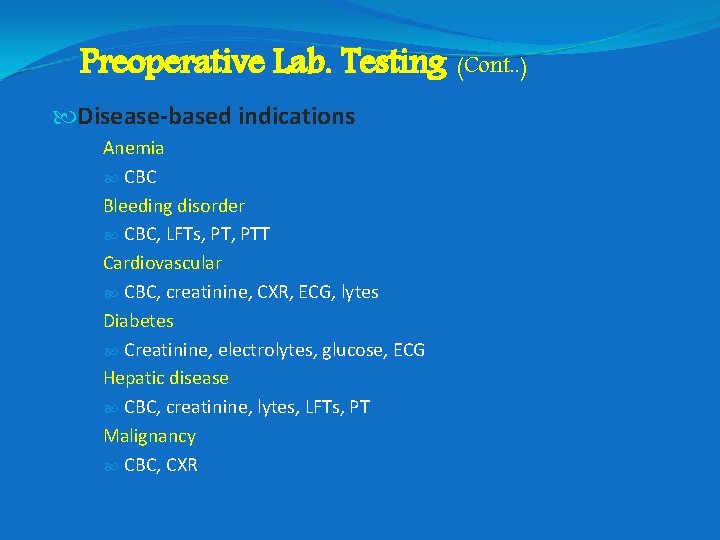
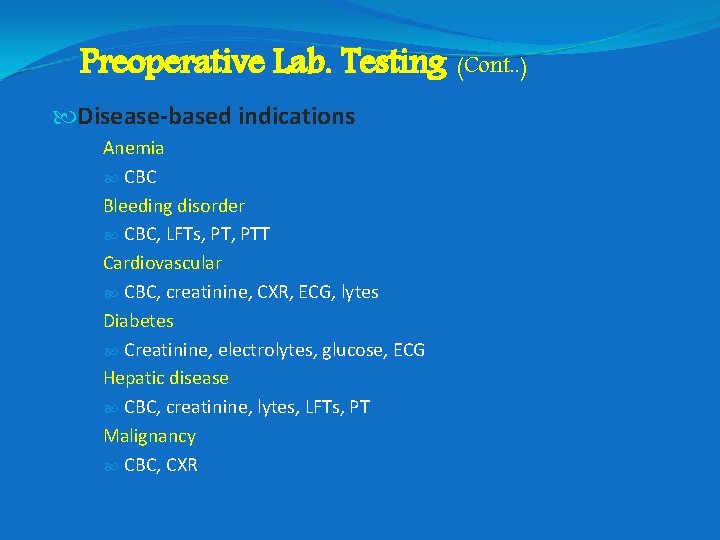
Preoperative Lab. Testing (Cont. . ) Disease-based indications Anemia CBC Bleeding disorder CBC, LFTs, PTT Cardiovascular CBC, creatinine, CXR, ECG, lytes Diabetes Creatinine, electrolytes, glucose, ECG Hepatic disease CBC, creatinine, lytes, LFTs, PT Malignancy CBC, CXR
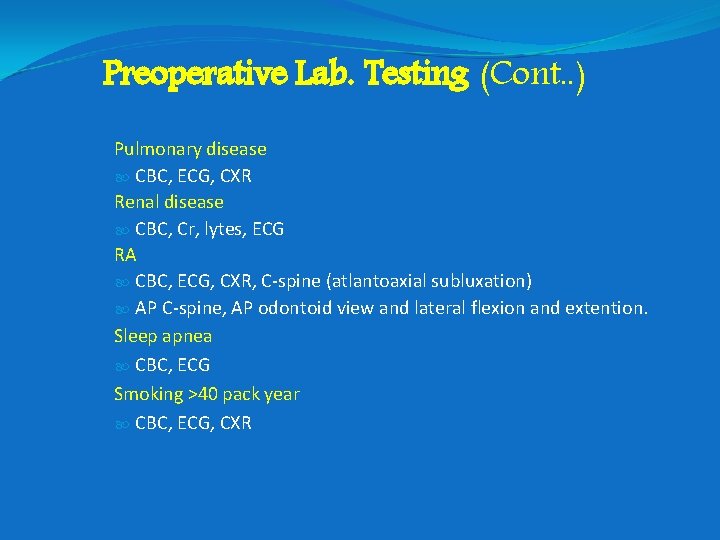
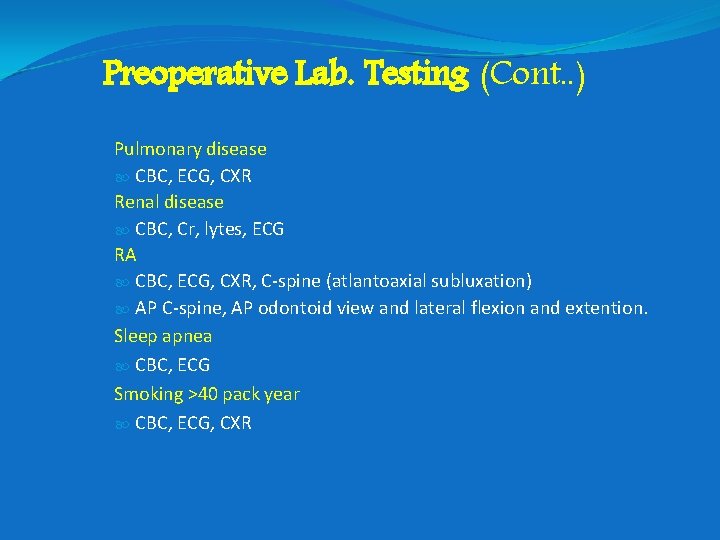
Preoperative Lab. Testing (Cont. . ) Pulmonary disease CBC, ECG, CXR Renal disease CBC, Cr, lytes, ECG RA CBC, ECG, CXR, C-spine (atlantoaxial subluxation) AP C-spine, AP odontoid view and lateral flexion and extention. Sleep apnea CBC, ECG Smoking >40 pack year CBC, ECG, CXR
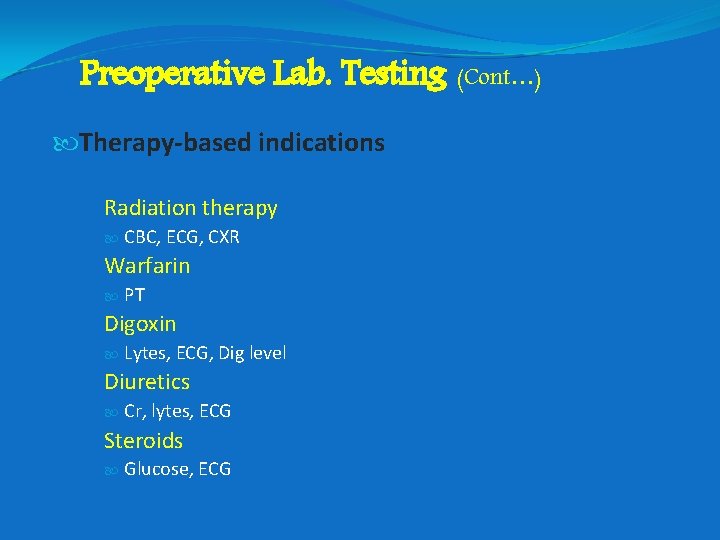
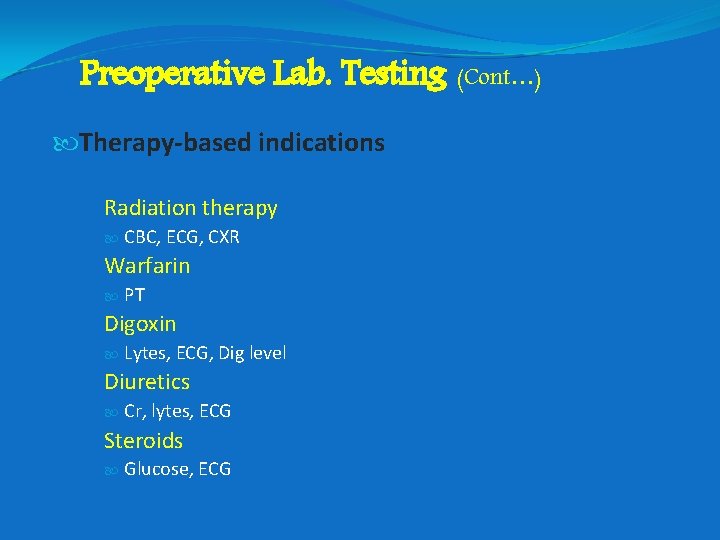
Preoperative Lab. Testing (Cont…) Therapy-based indications Radiation therapy CBC, ECG, CXR Warfarin PT Digoxin Lytes, ECG, Dig level Diuretics Cr, lytes, ECG Steroids Glucose, ECG

Thank You
 Dr. essam hamza
Dr. essam hamza Perioperative case study nursing
Perioperative case study nursing Ccs perioperative guidelines
Ccs perioperative guidelines What are the 3 phases of perioperative nursing?
What are the 3 phases of perioperative nursing? Preoperative checklist definition
Preoperative checklist definition Preoperative nursing definition
Preoperative nursing definition Azure worker role
Azure worker role Krappmann schaubild
Krappmann schaubild Role conflict occurs when fulfilling the role expectations
Role conflict occurs when fulfilling the role expectations Stability period vs measurement period
Stability period vs measurement period Absolute refractory period and relative refractory period
Absolute refractory period and relative refractory period 1750s music
1750s music Approaches to child development
Approaches to child development Trustee period and royal period
Trustee period and royal period When is the relative refractory period
When is the relative refractory period Mass less than 30, not neon, noble gas
Mass less than 30, not neon, noble gas Ce vs ad
Ce vs ad Critical period vs sensitive period
Critical period vs sensitive period Bloody placards
Bloody placards The development of children 7th edition
The development of children 7th edition Critical period
Critical period Role of herbarium
Role of herbarium Role of taxation
Role of taxation Your role in society
Your role in society Role of government in correcting market failure
Role of government in correcting market failure Objectives of family planning
Objectives of family planning Pcn role conception
Pcn role conception How does the local church help the community
How does the local church help the community Oxhmoron
Oxhmoron Bandura ross and ross 1961 evaluation
Bandura ross and ross 1961 evaluation Supply chain management system
Supply chain management system Role of health psychologist
Role of health psychologist Criteria for performance task
Criteria for performance task Role of nurse in patient teaching ppt
Role of nurse in patient teaching ppt Sport instruction
Sport instruction Shrm vs hrm
Shrm vs hrm