Management of neonatal hydronephrosis diagnosed in antenatal period






















- Slides: 94
Management of neonatal hydronephrosis diagnosed in antenatal period By: Dr behzad barekatain, MD Assistant professor of pediatrics Neonatologist Isfahan university of medical sciences
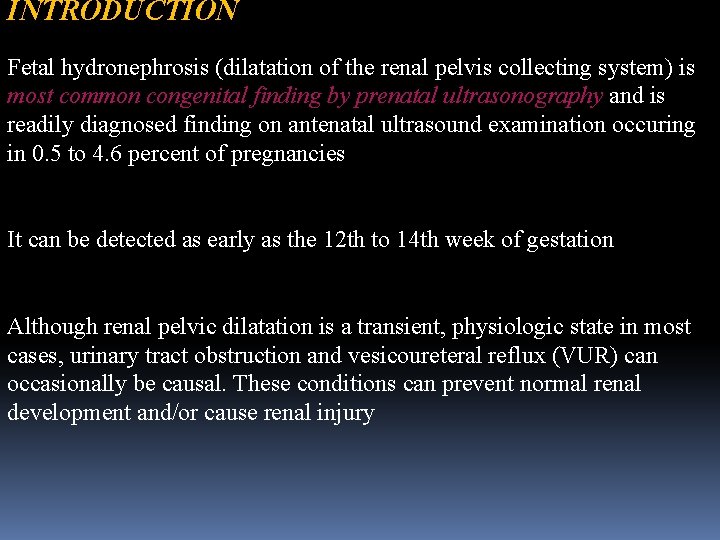
INTRODUCTION Fetal hydronephrosis (dilatation of the renal pelvis collecting system) is most common congenital finding by prenatal ultrasonography and is readily diagnosed finding on antenatal ultrasound examination occuring in 0. 5 to 4. 6 percent of pregnancies It can be detected as early as the 12 th to 14 th week of gestation Although renal pelvic dilatation is a transient, physiologic state in most cases, urinary tract obstruction and vesicoureteral reflux (VUR) can occasionally be causal. These conditions can prevent normal renal development and/or cause renal injury
However, the majority of cases of antenatal hydronephrosis are not clinically significant leading to unnecessary testing of the newborn baby and anxiety for patients and healthcare providers The goal of prenatal management is to detect those cases of antenatal hydronephrosis that will impact the health of the infant and require antenatal and postnatal evaluation, timely referral to a pediatric urologist if required, and possible intervention to minimize adverse outcomes

DEFINITION AND GRADING Several systems have been developed to diagnosis and grade the severity of antenatal hydronephrosis
Scoring systems differ based upon the fetal ultrasound criteria used, as follows: 1. Society of Fetal Urology (SFU) criteria SFU criteria for the diagnosis and grading of antenatal hydronephrosis are based upon the 1. degree of pelvic dilation 2. presence of caliceal dilation 3. the presence and severity of parenchymal thinning or atrophy.
The SFU developed criteria for the diagnosis and grading of antenatal hydronephrosis based upon the degree of pelvic dilatation, number of calyces seen, and the presence and severity of parenchymal atrophy. • Grade 0 — Normal examination with no dilatation of the renal pelvis • Grade 1 — Mild dilatation of the renal pelvis only • Grade II — Moderate dilatation of the renal pelvis including a few calyces • Grade III — Dilatation of the renal pelvis with visualization of all the calyces, which are uniformly dilated, and normal renal parenchyma. • Grade IV — Similar appearance of the renal pelvis and calyces as Grade III plus thinning of the renal parenchyma.
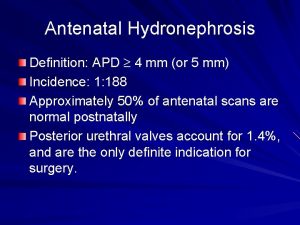
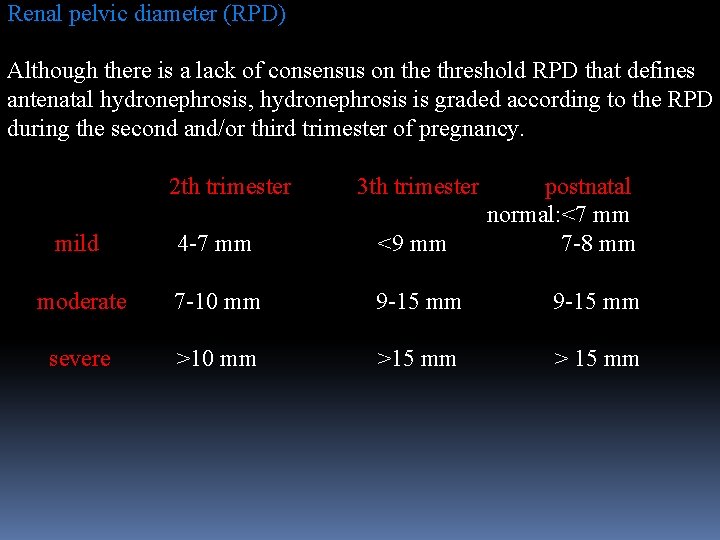
2. Renal pelvic diameter Measurement of the maximum anteroposterior diameter of the renal pelvis (APPD), also referred to as renal pelvic diameter (RPD), is the most generally accepted method to define antenatal hydronephrosis. Several studies have established normative data for fetal renal size based upon gestational age. However, despite these data, there remains a lack of consensus on the threshold RPD that defines clinically significant antenatal hydronephrosis.
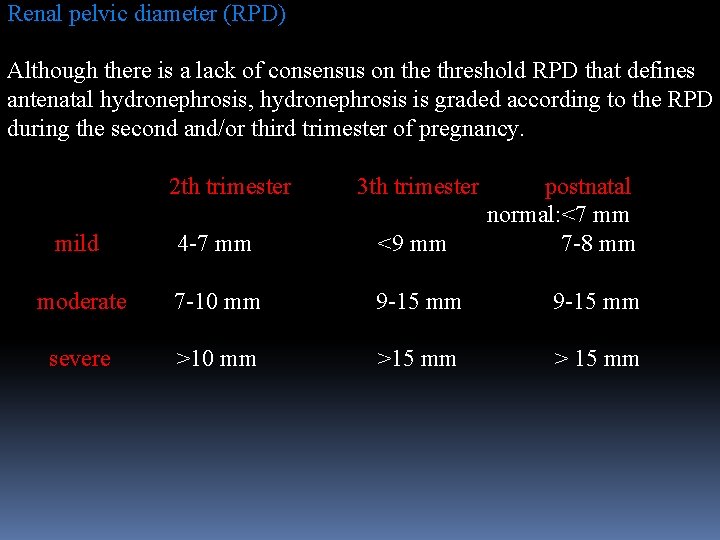
Renal pelvic diameter (RPD) Although there is a lack of consensus on the threshold RPD that defines antenatal hydronephrosis, hydronephrosis is graded according to the RPD during the second and/or third trimester of pregnancy. 2 th trimester 3 th trimester postnatal normal: <7 mm mild 4 -7 mm <9 mm 7 -8 mm moderate 7 -10 mm 9 -15 mm severe >10 mm >15 mm > 15 mm
3. Changes in the degree of hydronephrosis The relative change in hydronephrosis compared to subsequent prenatal ultrasound or the first postnatal ultrasound has been used in the clinical research setting. However, testing its clinical applicability has been limited. As a result, relative changes in antenatal hydronephrosis are not generally used clinically.

Despite numerous studies in neonates with antenatal hydronephrosis , there remains considerable debate on the accepted RPD threshold that predicts clinically significant disease in the neonate. Currently, no criteria have been identified that can identify all neonates with significant pathology and exclude those infants with transient or physiologic hydronephrosis.
Thus, although a low threshold (eg, RPD >4 mm) in the second trimester will have a greater sensitivity of detecting infants with CAKUT, it would also include a large number of patients without renal disease who would undergo unnecessary testing.
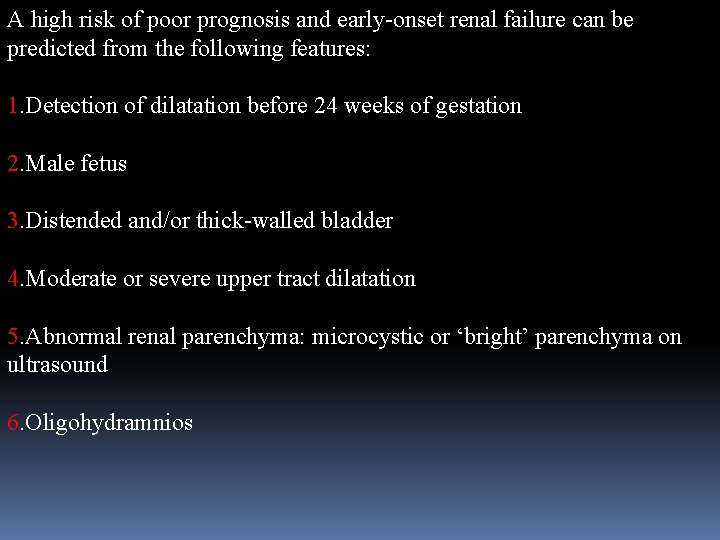
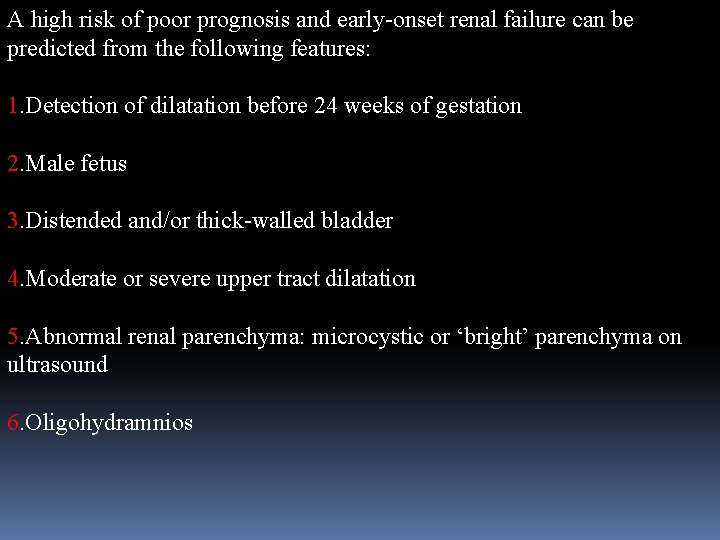
A high risk of poor prognosis and early-onset renal failure can be predicted from the following features: 1. Detection of dilatation before 24 weeks of gestation 2. Male fetus 3. Distended and/or thick-walled bladder 4. Moderate or severe upper tract dilatation 5. Abnormal renal parenchyma: microcystic or ‘bright’ parenchyma on ultrasound 6. Oligohydramnios
EPIDEMIOLOGY . Hydronephrosis occurs approximately twice as often in males than in females. . It is bilateral in 20 to 40 percent of cases. . The reported incidence of antenatal hydronephrosis ranges from 0. 6 to 4. 5 percent of pregnancies. Differences in reported data may be due to different criteria used to define the disorder and the level of attention to the urinary system by the ultrasonographer.
ETIOLOGY . In a one review, causes of antenatal hydronephrosis and their relative frequency were determined as follows : • Transient — 48 percent • Physiologic — 15 percent • UPJ obstruction — 11 percent • VUR — 9 percent • Megaureter — 4 percent • Multicystic dysplastic kidney — 2 percent • Ureterocele — 2 percent • Posterior urethral valves — 1 percent Less common causes included ectopic ureter, prune belly, urachal cyst, duplex collecting system and urethral atresia
PRENATAL ISSUES Detection of antenatal hydronephrosis usually occurs in the second trimester with a RPD cutoff of ≥ 4 mm. Mild hydronephrosis (RPD of 4 to 9 mm or SFU grade 1 or 2) can be associated with Down syndrome and an increased risk of other chromosome anomalies. More severe dilatation increases the risk of renal/urinary tract disorders. Down syndrome — Mild hydronephrosis is a common finding in fetuses with Down syndrome. Studies that defined hydronephrosis as RPD ≥ 4 mm demonstrated hydronephrosis is greater in Down syndrome compared to normal control fetuses (18 versus 0 to 3 percent, respectively).
The finding of mild hydronephrosis requires a detailed assessment of fetal anatomy and review of clinical risk factors for Down syndrome. However, genetic amniocentesis is not warranted based solely on the isolated finding of hydronephrosis, because the incidence of Down syndrome remains low (<1 in 300 pregnancies) in fetuses with no maternal risk factors (eg, advanced age or abnormal maternal serum screen) or without any other sonographic features suggestive for Down syndrome
The likelihood that an infant postnatally will have a significant CAKUT increases with the severity of hydronephrosis. This was illustrated in a meta-analysis of 1678 infants that demonstrated that the severity of antenatal hydronephrosis defined by RPD increased the risk of renal/urinary tract pathology, as follows: • Mild hydronephrosis (≤ 7 mm in the second trimester and/or ≤ 9 mm in the third trimester) — 12 percent • Moderate hydronephrosis (7 to 10 mm in the second trimester and/or 9 to 15 mm in the third trimester) — 45 percent • Severe hydronephrosis (>10 mm in the second trimester and/or >15 mm in the third trimester) — 88 percent
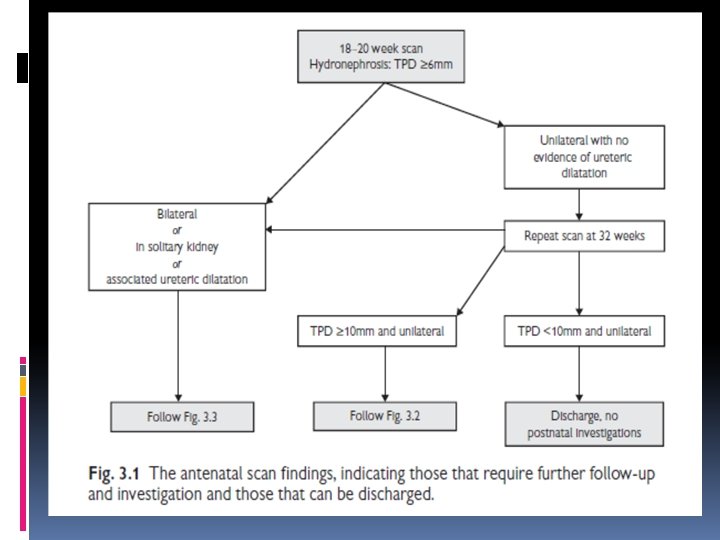
Timing of prenatal ultrasonography is important in optimal detection of CAKUT. Ultrasonography performed before the 18 to 24 th week of gestation can fail to detect significant disease. In addition, studies performed in the third trimester have been suggested to be more helpful in predicting postnatal outcome than screening earlier in the pregnancy. Thus, most authors agree that a repeat scan in the third trimester (28 to 34 weeks gestation) be performed to identify those fetuses potentially requiring postnatal intervention

Ultrasound follow-up . Fetuses with mild hydronephrosis should have a follow-up ultrasound scan in the third trimester (32 to 34 weeks of gestation). Those with resolution have a low risk of clinically significant pathology, and do not need further antenatal or postnatal evaluation. . By comparison, serial follow-up ultrasounds are indicated for fetuses with: - Moderate or severe hydronephrosis - Bilateral involvement - Progression and/or persistence of hydronephrosis - Oligohydramnios. The interval for follow-up examination and management are dictated by the initial findings and the amount of amniotic fluid.

. If fetal hydronephrosis is detected, the following parameters need to be evaluated by ultrasonography as they guide further need for evaluation and are helpful in determining the cause of hydronephrosis: • Severity of hydronephrosis • Unilateral versus bilateral involvement Bilateral involvement increases the risk of a significant abnormality and the risk of impaired postnatal renal function. • Ureter Dilatation of the ureter can be consistent with VUR or obstructive uropathy distal to the ureteropelvic junction [eg, ureterocoele, megaureter, or posterior urethral valves (PUV)].
• Bladder Abnormalities of the bladder such as increased thickness and trabeculation of the bladder wall are consistent with obstructive uropathy distal to the bladder (eg, PUV). In addition, dilatation of the proximal urethra (key-hole sign) may indicate PUV in male fetuses patients with a thickened bladder wall and hydronephrosis. • Amniotic fluid Oligohydramnios is consistent with impaired renal function resulting in a decreased production of fetal urine (amniotic fluid). It is a consistent feature of severe renal disease affecting both kidneys or a solitary kidney. • Renal parenchyma Thinning of the parenchyma indicates injury or impaired development of the renal cortex. An echogenic renal cortex may indicate abnormal renal parenchymal development (dysplasia), which may be associated with vesicoureteral reflux.
Other anomalies . Other non-renal/urinary tract congenital abnormalities are associated with antenatal hydronephrosis. . In one case series of 104 fetuses with hydronephrosis, the three other major birth defects detected were ventricular septal defect in a patient with Down syndrome, microcephaly and omphalocele. . Hydronephrosis also has been reported as part of a multiple malformation syndrome in more than 60 genetic and sporadic malformation syndromes. . In one case series, a chromosomal abnormality was detected in 7 of 81 fetuses that had karyotyping. Of those, only two had isolated renal malformations.
OVERVIEW OF MANAGEMENT Decisions regarding evaluation and care dependent on the: 1. presence and nature of associated renal and extrarenal anomalies 2. severity of hydronephrosis 3. unilateral versus bilateral involvement 4. gestational age 5. the amniotic fluid volume

Antenatal management: In fetuses with mild hydronephrosis and normal amniotic fluid, a careful examination for genitourinary and extrarenal abnormalities should be performed. Clinical risk factors and ultrasound markers of Down syndrome should be evaluated. Assessment of the fetal karyotype should be offered if additional fetal anomalies are detected, in women of advanced maternal age, and women with abnormal maternal serum screening tests for Down syndrome.
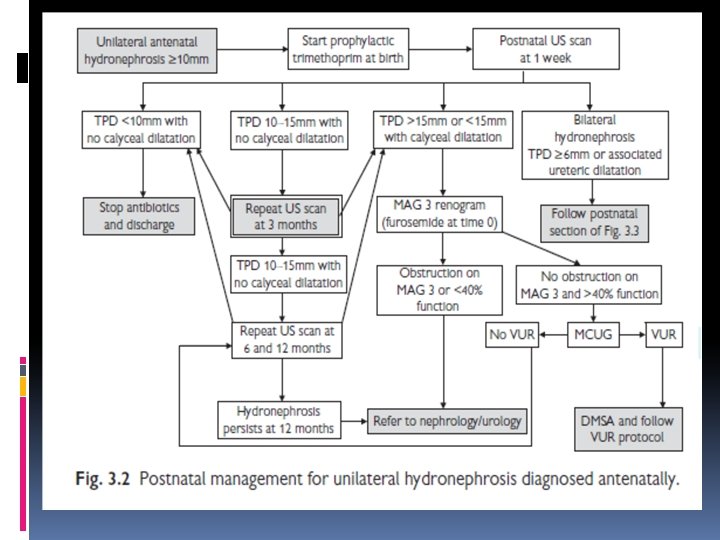
Post natal management: Evaluation includes: 1. physical examination 2. use of radiologic studies to detect renal and urinary tract abnormalities including obstructive uropathy or vesicoureteral reflux (VUR).
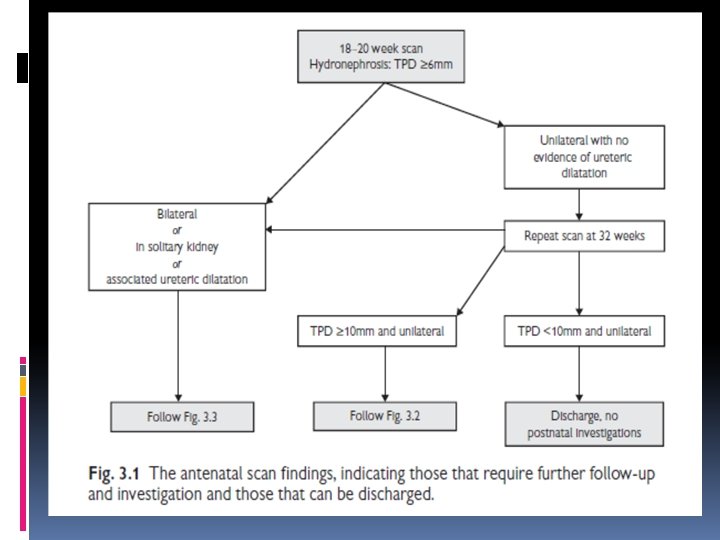
. Currently, there is not a single test or finding that accurately differentiates infants with significant disease from those who are normal or have insignificant findings. . In practice, usually use an algorithm based upon the presence of predicative factors (bilateral involvement and severity of hydronephrosis) for postnatal management that limits unnecessary radiographic studies and minimizes parental distress.

PHYSICAL EXAMINATION. The physical examination of the newborn can detect abnormalities that suggest genitourinary abnormalities associated with antenatal hydronephrosis. These include the following: 1. The presence of an abdominal mass that could represent an enlarged kidney due to obstructive uropathy or multicystic dysplastic kidney (MCDK).
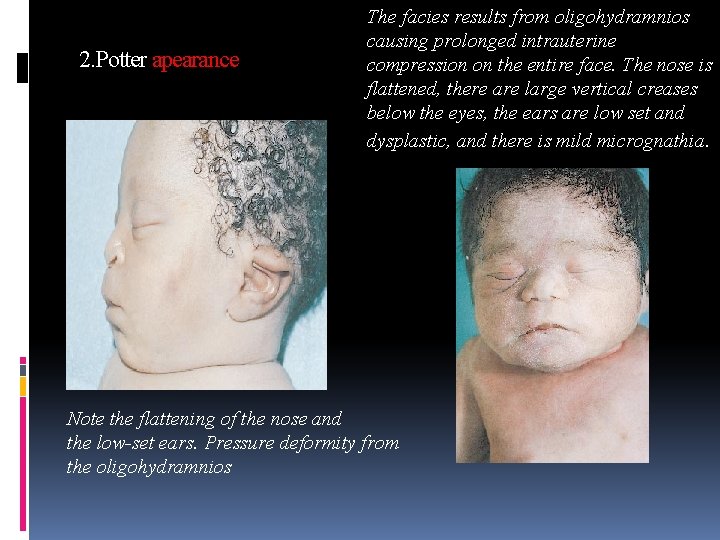
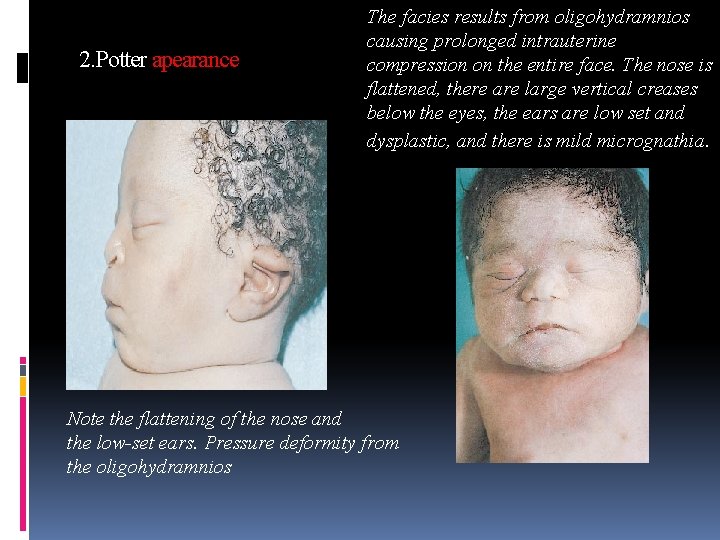
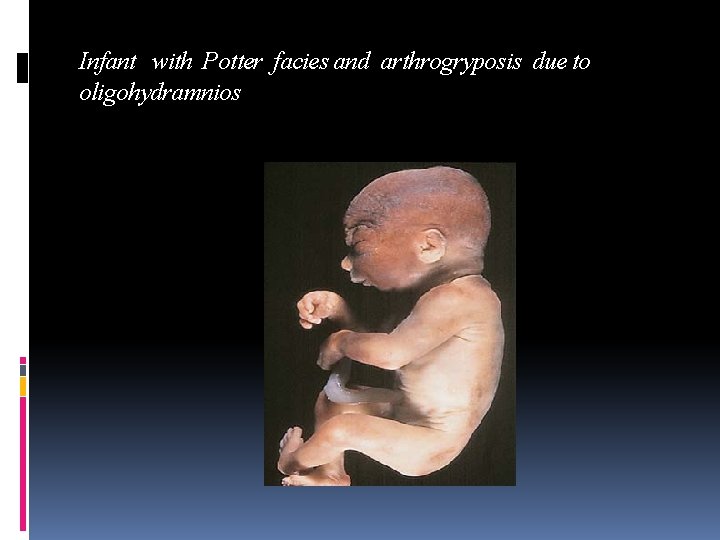
2. Potter apearance The facies results from oligohydramnios causing prolonged intrauterine compression on the entire face. The nose is flattened, there are large vertical creases below the eyes, the ears are low set and dysplastic, and there is mild micrognathia. Note the flattening of the nose and the low-set ears. Pressure deformity from the oligohydramnios
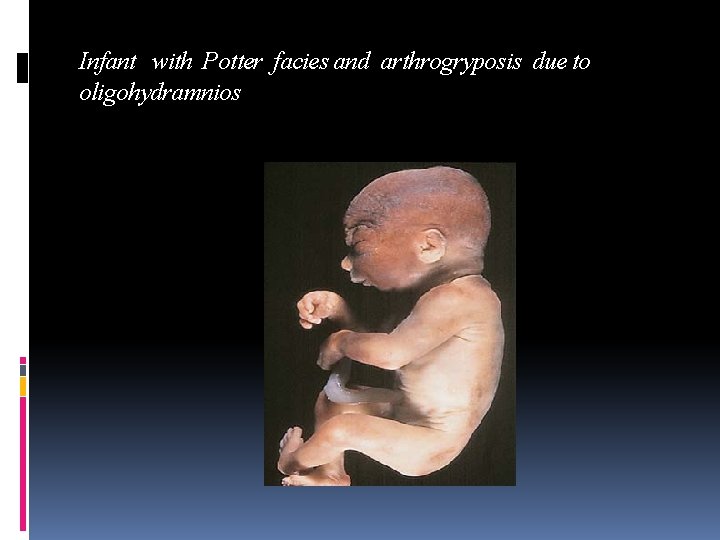
Infant with Potter facies and arthrogryposis due to oligohydramnios
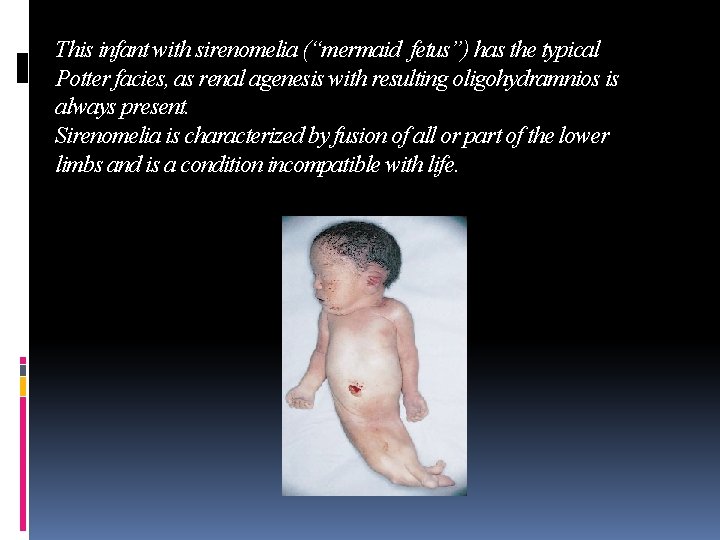
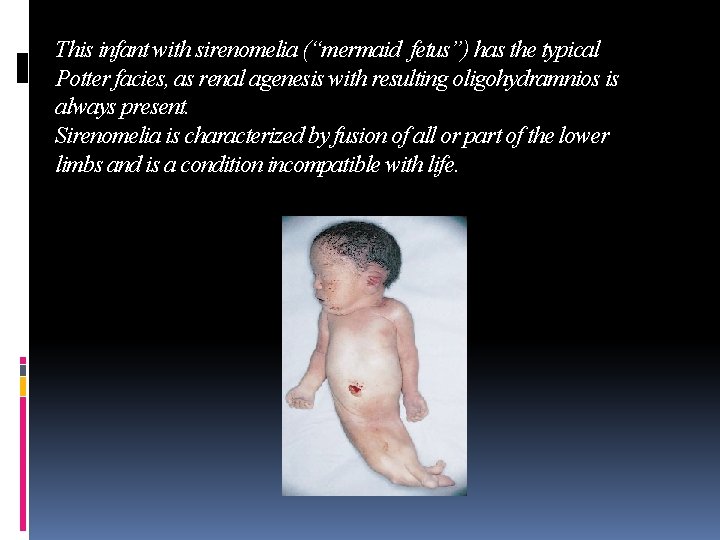
This infant with sirenomelia (“mermaid fetus”) has the typical Potter facies, as renal agenesis with resulting oligohydramnios is always present. Sirenomelia is characterized by fusion of all or part of the lower limbs and is a condition incompatible with life.
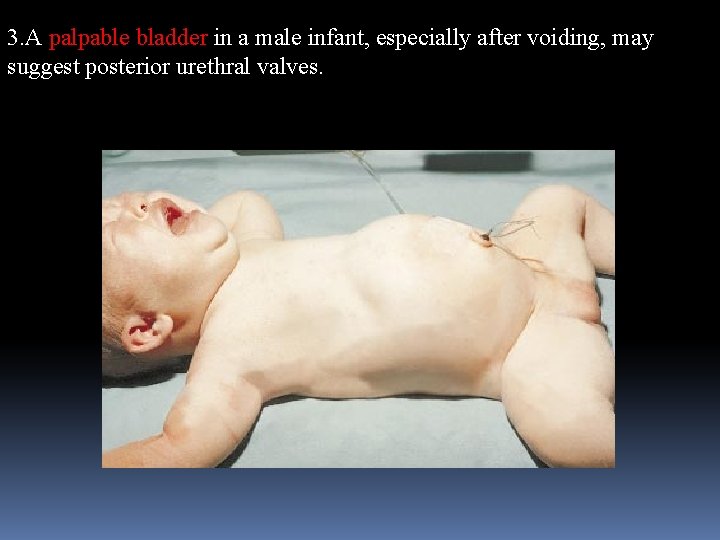
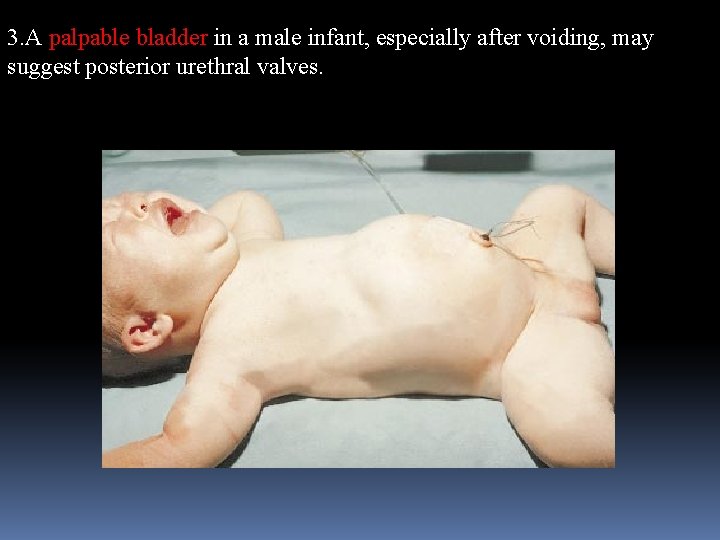
3. A palpable bladder in a male infant, especially after voiding, may suggest posterior urethral valves.
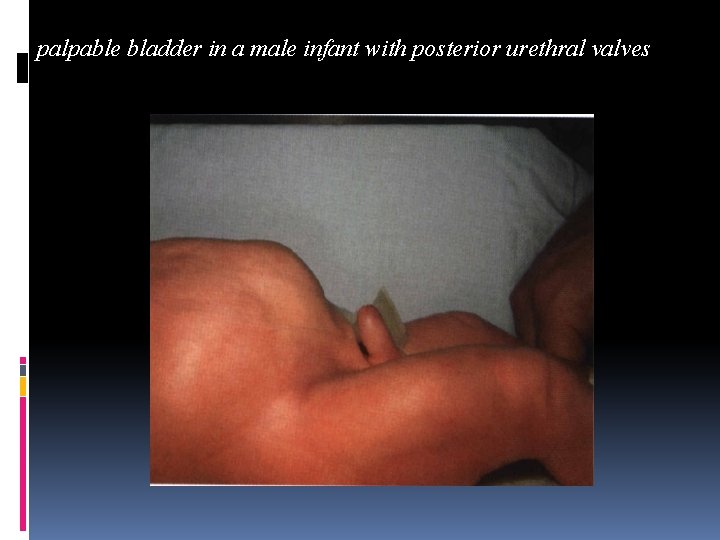
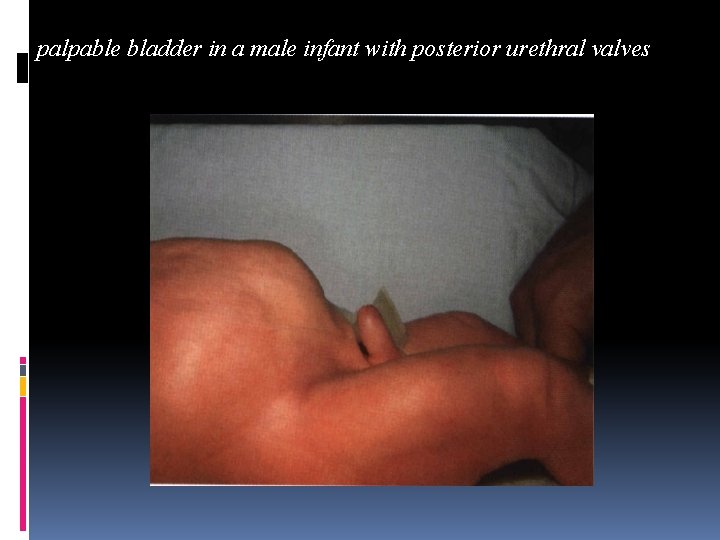
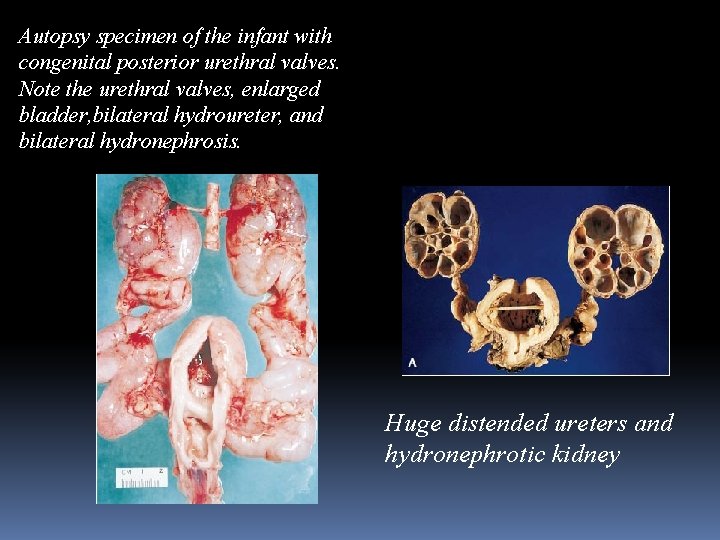
palpable bladder in a male infant with posterior urethral valves
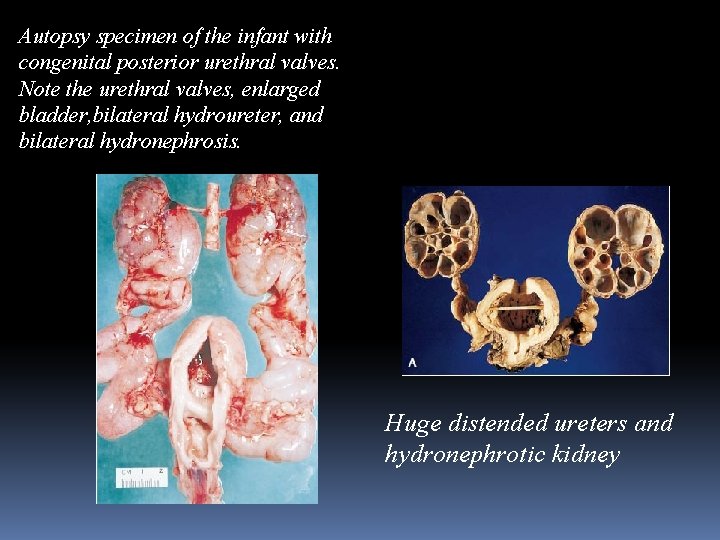
Autopsy specimen of the infant with congenital posterior urethral valves. Note the urethral valves, enlarged bladder, bilateral hydroureter, and bilateral hydronephrosis. Huge distended ureters and hydronephrotic kidney
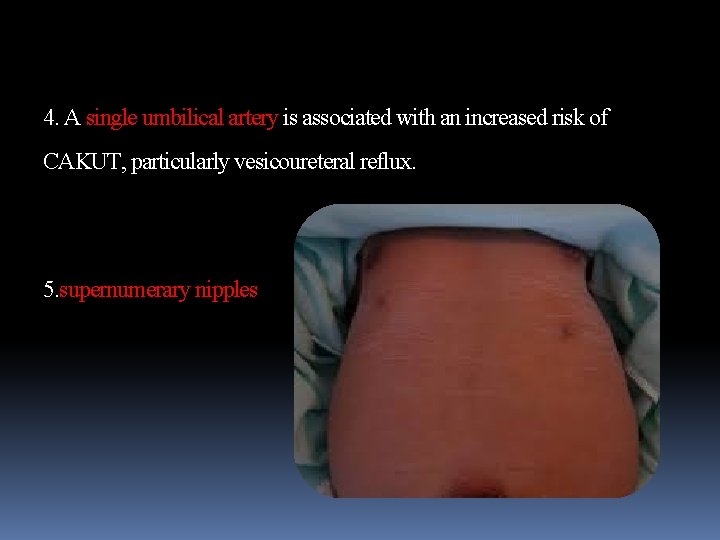
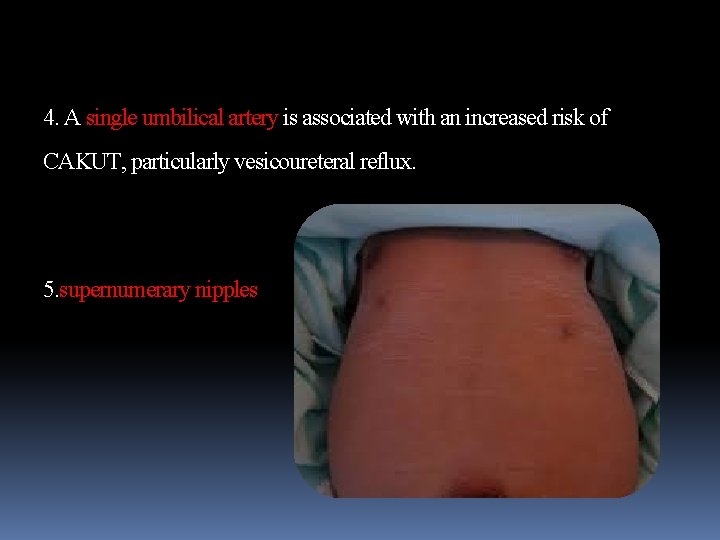
4. A single umbilical artery is associated with an increased risk of CAKUT, particularly vesicoureteral reflux. 5. supernumerary nipples
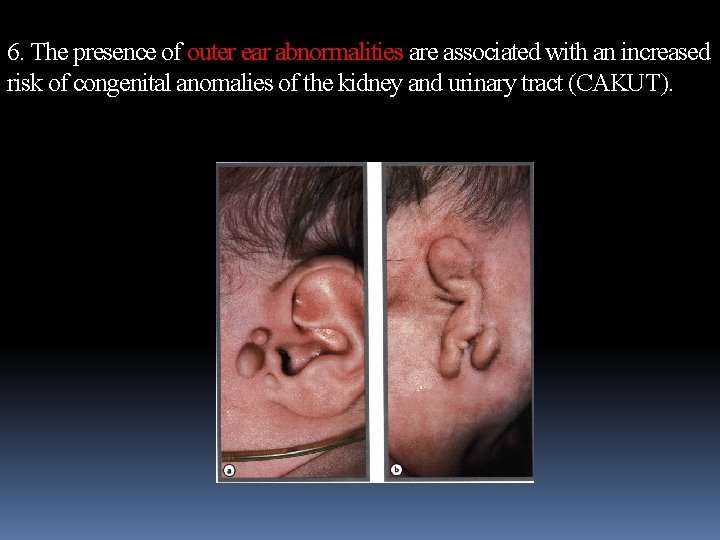
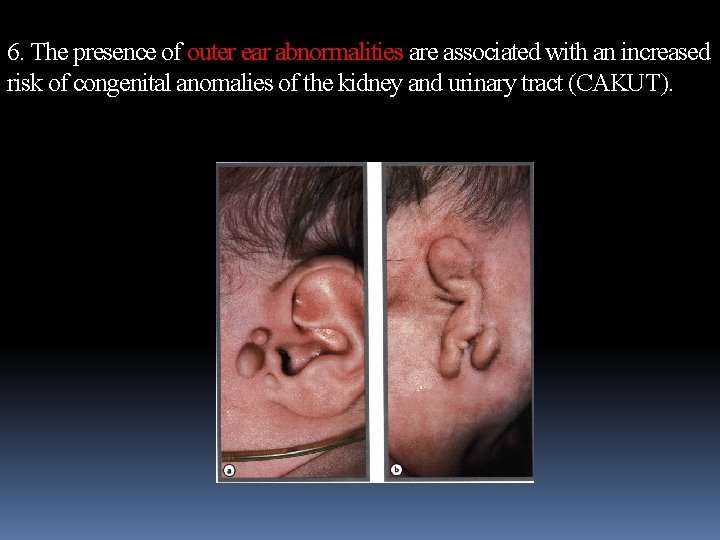
6. The presence of outer ear abnormalities are associated with an increased risk of congenital anomalies of the kidney and urinary tract (CAKUT).
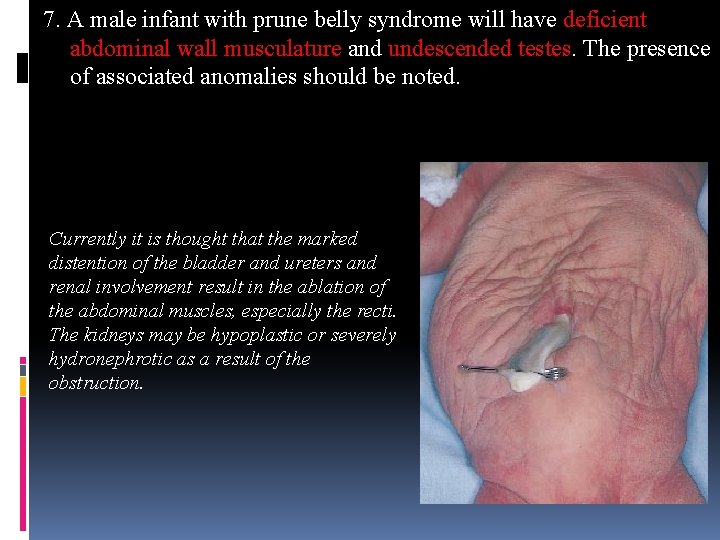
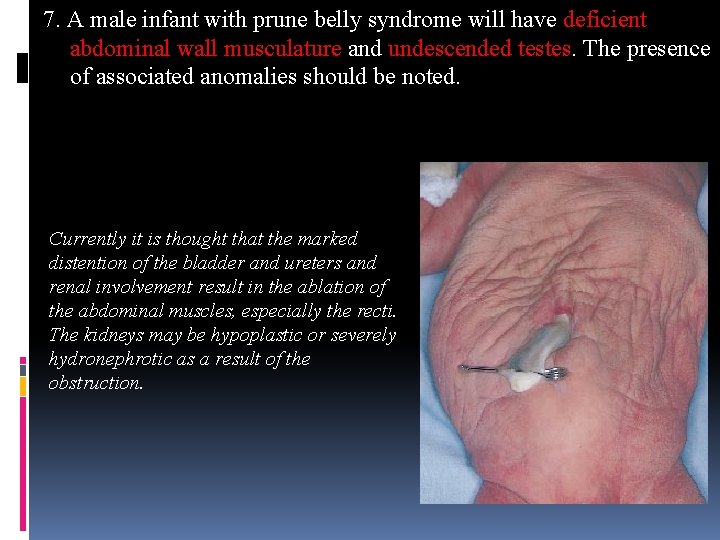
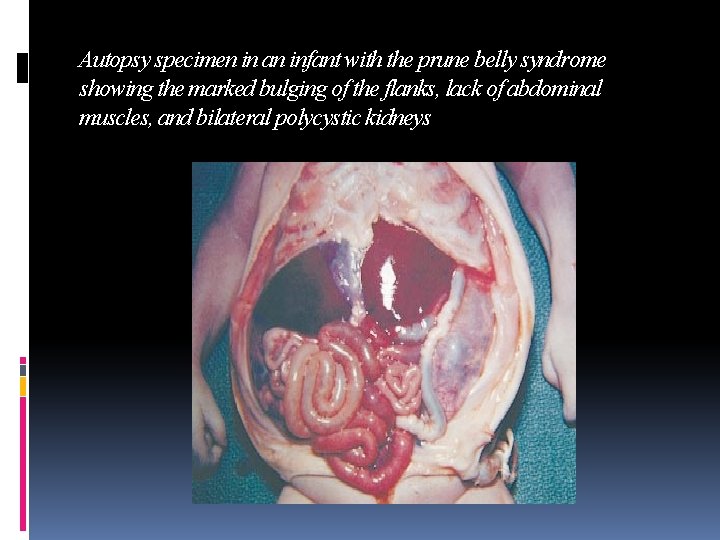
7. A male infant with prune belly syndrome will have deficient abdominal wall musculature and undescended testes. The presence of associated anomalies should be noted. Currently it is thought that the marked distention of the bladder and ureters and renal involvement result in the ablation of the abdominal muscles, especially the recti. The kidneys may be hypoplastic or severely hydronephrotic as a result of the obstruction.
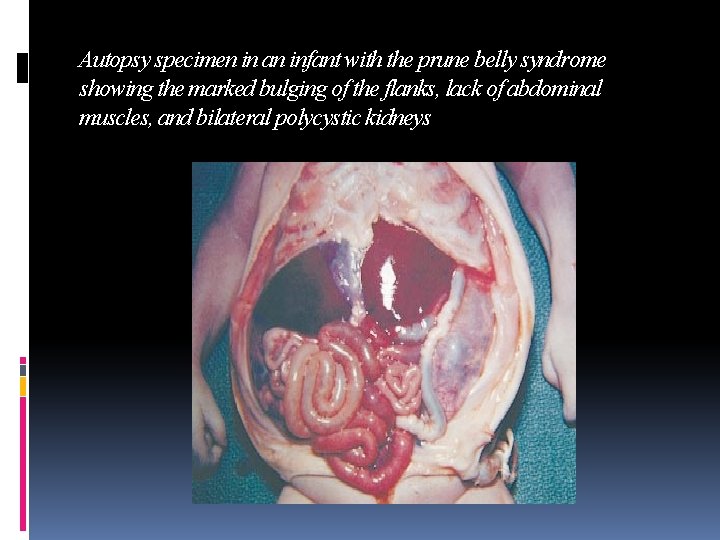
Autopsy specimen in an infant with the prune belly syndrome showing the marked bulging of the flanks, lack of abdominal muscles, and bilateral polycystic kidneys

8. ascit Marked abdominal distention in an infant with urinary ascites and bilateral multicystic kidneys

Transillumination of the abdomen showing the large amount of ascitic fluid.
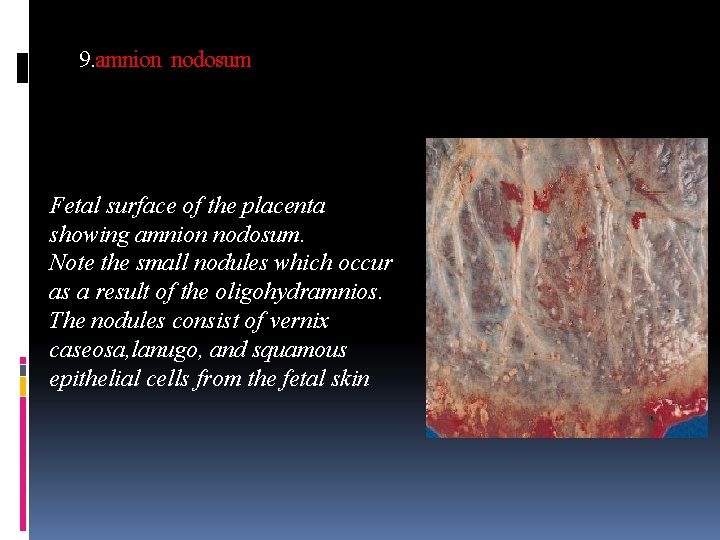
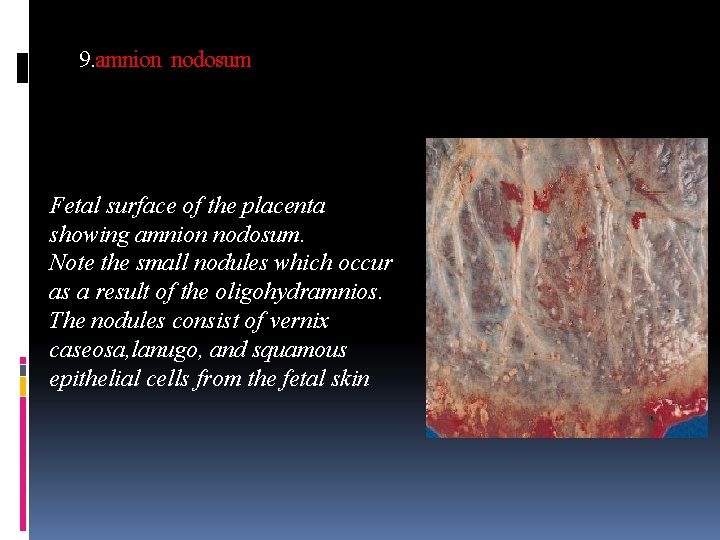
9. amnion nodosum Fetal surface of the placenta showing amnion nodosum. Note the small nodules which occur as a result of the oligohydramnios. The nodules consist of vernix caseosa, lanugo, and squamous epithelial cells from the fetal skin
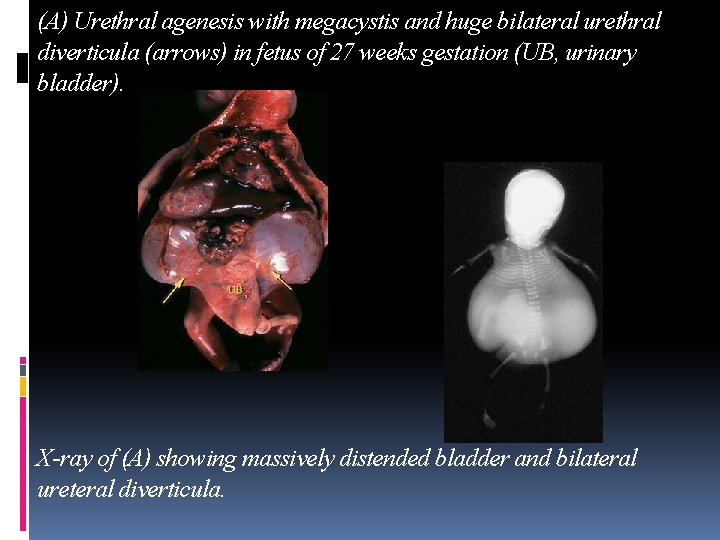
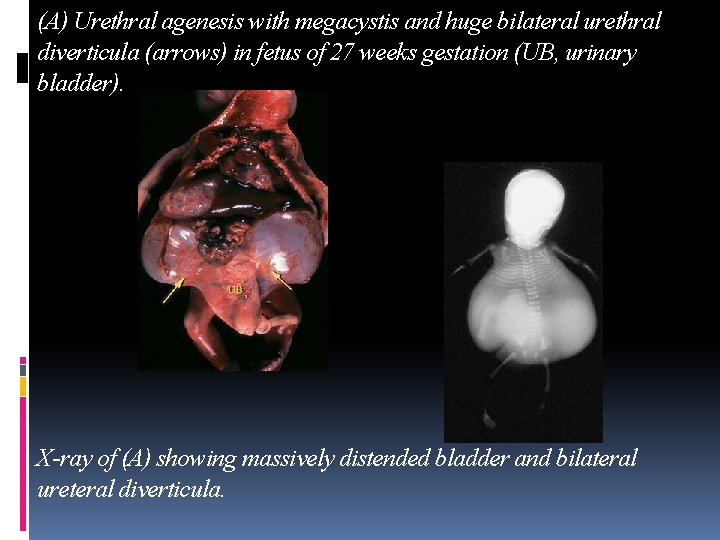
(A) Urethral agenesis with megacystis and huge bilateral urethral diverticula (arrows) in fetus of 27 weeks gestation (UB, urinary bladder). X-ray of (A) showing massively distended bladder and bilateral ureteral diverticula.
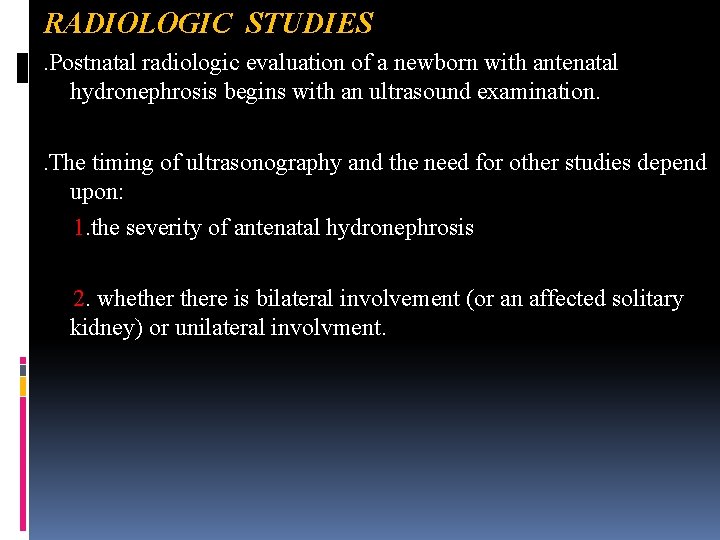
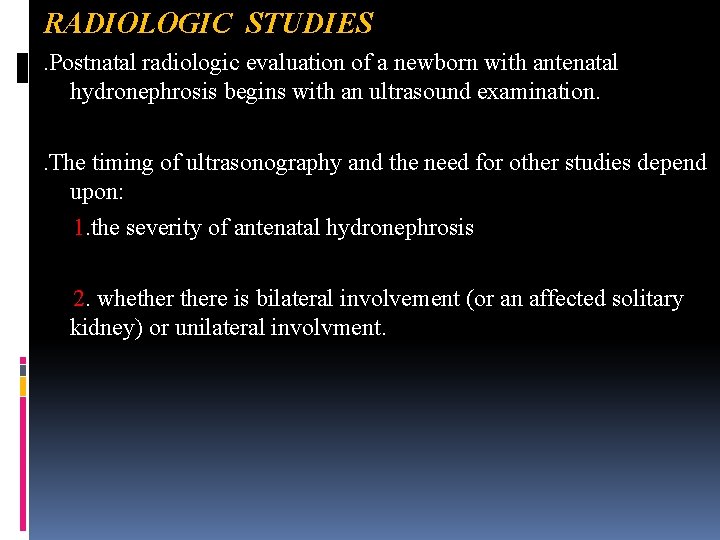
RADIOLOGIC STUDIES . Postnatal radiologic evaluation of a newborn with antenatal hydronephrosis begins with an ultrasound examination. . The timing of ultrasonography and the need for other studies depend upon: 1. the severity of antenatal hydronephrosis 2. whethere is bilateral involvement (or an affected solitary kidney) or unilateral involvment.
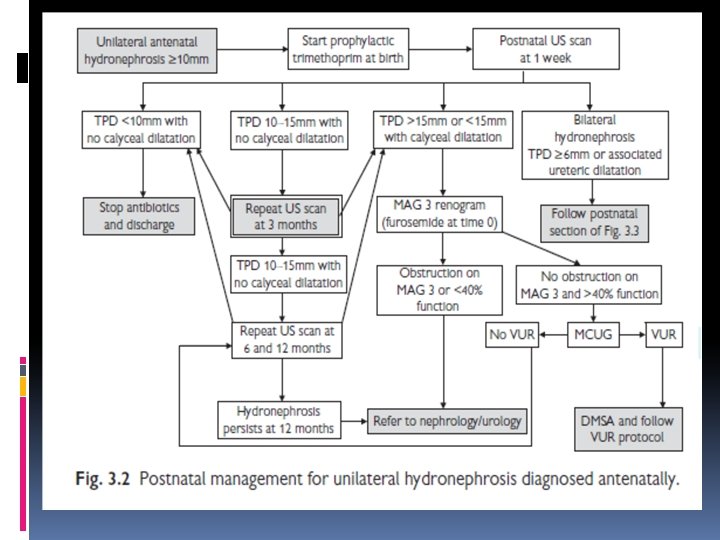
Ultrasonography . Affected infants should have an ultrasound examination of the kidneys and bladder in the postnatal period. . The timing of the study depends upon the severity of the antenatal hydronephrosis. . In general, examination should be avoided in the first two days after birth because hydronephrosis may not be detected because of extracellular fluid shifts that will underestimate the degree of hydronephrosis.
. However: 1. infants with bilateral hydronephrosis 2. those with a severe hydronephrotic solitary kidney require urgent evaluation on the first postnatal day because of the increased likelihood of significant disease and a possible need for early intervention. . For unilateral hydronephrosis without antenatal bladder pathology, we recommend that the postnatal sonogram be done at one to four weeks after birth. (in some refrence 1014 th day after birth)
Voiding cystourethogram . A voiding cystourethogram (VCUG) is performed to detect VUR and in boys, to evaluate the posterior urethra. . For this procedure, a urinary catheter is inserted into the bladder and contrast material is instilled. Fluoroscopic monitoring is performed while the bladder is filling and during voiding. Although the duration of fluoroscopy is minimized, the gonads, especially the ovaries, are exposed to radiation.
The role of the VCUG in the routine postnatal evaluation of infants with prenatally detected dilatation remains controversial, with practice varying considerably between different centres. However, the following conditions are generally regarded as being definite indications for a postnatal VCUG: 1. abnormal bladder (particularly a thick-walled bladder or other evidence of outflow obstruction) 2. bilateral upper tract dilatation 3. dilatation of one or both ureters seen on either on pre- or postnatal ultrasound 4. duplex kidneys (in view of the high incidence of lower pole reflux).
the VCUG is an invasive and potentially distressing procedure which carries some risk of morbidity in its own right (predominantly infection). For these reasons, many neonatologist no longer advocate routine VCUG if dilatation is confined to the renal pelvis (i. e. no evidence of ureteric and/or calyceal dilatation), and the AP diameter of the pelvis is <15 mm. Some cases of low-grade VUR will be missed by this approach, but this is outweighed by the benefit of a greatly reduced burden of unnecessary investigation into healthy infants. If an VCUG is not undertaken, the child’s parents and general practitioner should, nevertheless, be alerted to the importance of having the urine checked for possible infection in the event of an unexplained febrile illness or more specific features of urinary infection.
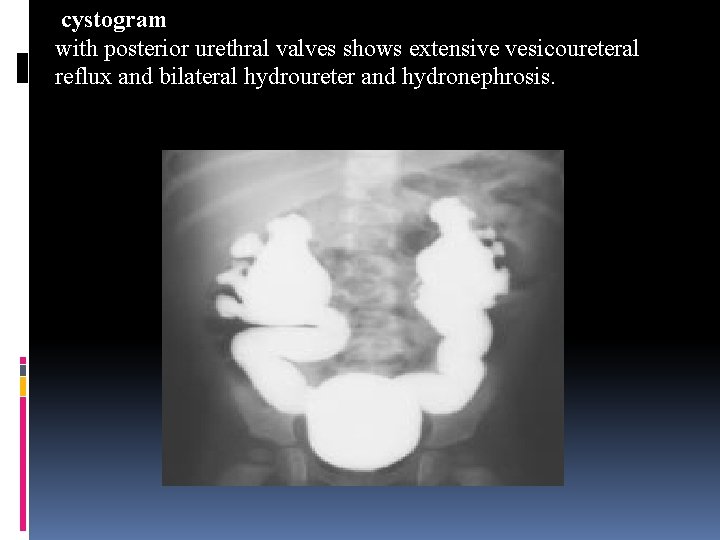
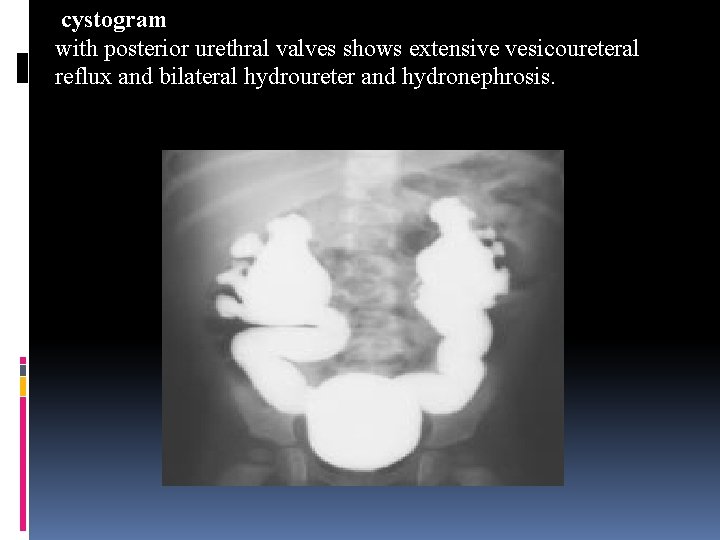
cystogram with posterior urethral valves shows extensive vesicoureteral reflux and bilateral hydroureter and hydronephrosis.
Diuretic renography (renal scan and the administration of a diuretic) is used to diagnose urinary tract obstruction in infants with persistent hydronephrosis, usually ordered after a VCUG has demonstrated no vesicoureteral reflux. . It measures the drainage time from the renal pelvis and assesses total and each individual kidney's renal function. . Since the information derived from DMSA scintigraphy or diuretic renography rarely influences practical management in the first few weeks or months of life, isotope imaging is best deferred until 1– 3 months of age.
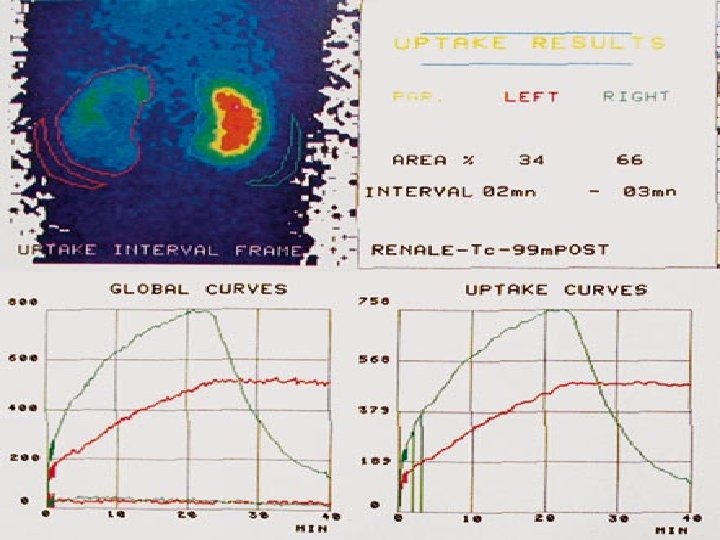
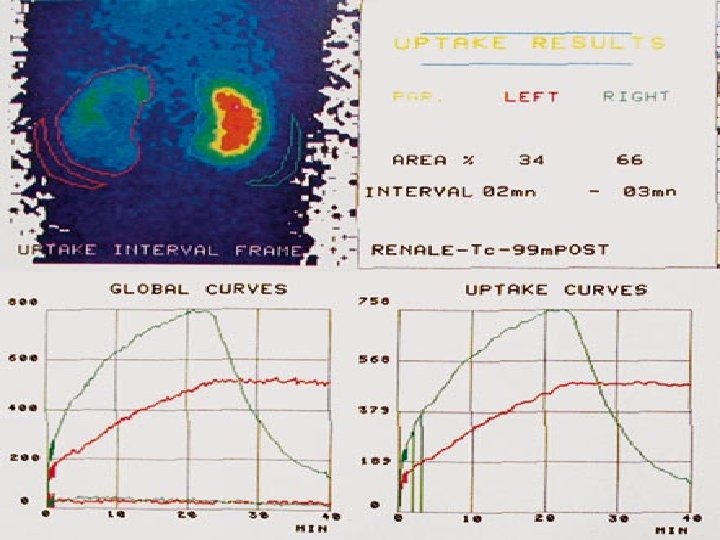
. Renal scintigraphy is used to assess renal anatomy and function. The two most commonly used radiopharmaceuticals are 1. mercaptoacetyl triglycine (MAG-3) 2. technetium-99 m-labeled dimercaptosuccinic acid (DMSA). . MAG-3, which is excreted by renal tubular secretion, is used to assess differential renal function, and, when furosemide is administered, drainage also can be measured. An alternative to MAG-3 is diethylene tetrapentaacetic acid (DTPA), which is cleared by glomerular filtration. The background activity of DTPA is much higher than that of MAG-3. . DMSA is a renal cortical imaging agent and is used to assess differential renal function and to demonstrate whether renal scarring is present. It is used infrequently in children with obstructive uropathy.
. In a MAG-3 diuretic renogram, a small dose of technetium-labeled MAG-3 is injected intravenously. During the first 2– 3 min, renal parenchymal uptake is analyzed and compared, allowing computation of differential renal function. Subsequently, excretion is evaluated. After 20– 30 min, furosemide is injected intravenously, and the rapidity and pattern of drainage from the kidneys to the bladder are analyzed. a. If no obstruction is present, half of the radionuclide should be cleared from the renal pelvis within 10– 15 min, termed the halflife (t½). b. If there is significant upper tract obstruction, the t½ usually is >20 min. c. A t½ between 15– 20 min is indeterminate.
. The images generated usually provide an accurate assessment of the site of obstruction. . Numerous variables affect the outcome of the diuretic renogram. 1. Newborn kidneys are functionally immature, and, in some cases, normal kidneys may not demonstrate normal drainage after diuretic administration. 2. Dehydration prolongs parenchymal transit and can blunt the diuretic response. 3. Giving an insufficient dose of furosemide may result in inadequate drainage. 4. If vesicoureteral reflux is present, continuous catheter drainage is mandatory to prevent the radionuclide from refluxing from the bladder into the dilated upper tract, which would prolong the washout phase.
. In response to the numerous variables, the Society for Fetal Urology and the Pediatric Nuclear Medicine Club jointly developed a standardized method for performing diuretic renography in infants and children, termed the well-tempered renogram
. The test requires insertion of a bladder catheter to relieve any pressure that can be transmitted to the ureters and kidneys. Intravenous access is needed for hydration and the administration of the radioisotope and diuretic. The preferred radioisotope is technetium-99 m-mercaptoacetyltriglycine (Tc 99 m. MAG 3), which is taken up by the renal cortex, filtered across the glomerular basement membrane to the renal tubules, and excreted into the renal pelvis and urinary tract.
. The study includes two phases: Initial phase Radioisotope is injected intravenously and renal parenchymal (cortical) uptake is measured during the first two to three minutes. The relative contribution of each kidney to overall renal function (called the split renal function) is assessed quantitatively and is useful as a baseline study. Subsequent studies can be compared to assess whether kidney function remains stable or has deteriorated, suggesting true obstruction.
Second phase . In the second phase at peak renal uptake, intravenous furosemide is administered and the excretion of isotope from the kidney is measured referred to as the "washout curve". This phase indicates the extent of obstruction, if present. . In the normal kidney: the administration of furosemide results in a prompt washout. . In a dilated system: a. if washout occurs rapidly after diuretic administration (<15 minutes), the system is not obstructed. b. if washout is delayed beyond 20 minutes, the pattern is consistent with obstructive uropathy.
. However, a delayed washout must be interpreted with caution. As an example, in a series of 39 infants with antenatal unilateral hydronephrosis followed without surgery, diuretic renography indicated obstruction in 24 patients whose renal function never decreased and thus could not have been obstructed. These results may be in part be due to the normally low neonatal glomerular filtration rate that can be refractory to diuretic therapy. . If washout is between 15 and 20 minutes, the study is indeterminate.
Split renal function . The split renal function is the most useful criteria to evaluate a decrease in renal function. In patients with unilateral hydronephrosis (which is the most common clinical scenario), if the normal nonhydronephrotic kidney and hydronephrotic kidney both have equal function, conservative management without surgery is a safe option.
. In a cohort of 831 cases of antenatal hydronephrosis, renal scans performed in 229 newborns demonstrated 16 percent of patients had significant decrease in renal function of one kidney defined as ≤ 35 percent or less differential renal function. . A decrease in differential renal function was associated with severe antenatal hydronephrosis (ie, renal pelvic diameter >10 mm in at 20 to 24 weeks gestation and >16 mm greater than 33 weeks gestation).
. The characteristics of the uptake and drainage curves, as defined by O’Reilly and associates, fall into four patterns : Type 1. Normal uptake with prompt washout. Type 2. Rising uptake curve; no response to diuretic (obstruction). Type 3 a. Initially rising curve, that falls rapidly in response to diuretic (non-obstructive dilatation). Type 3 b. Initially rising curve which neither falls promptly nor continues to rise.

. Whereas type 1 and type 3 a curves are normal and non obstructed, the clinical significance of type 2 and type 3 b curves remains problematic. . Drainage curves can be particularly difficult to interpret in the first few months of life (the period of so-called ‘transitional nephrology’) when immaturity of the renal tubules may impair the response of the kidney to diuretic stimulation.

IVP(intra venous pyelogram) The MAG-3 diuretic renogram is considered superior to the excretory urogram in infants and children with hydronephrosis, because bowel gas and immaturity of renal function often cause the intravenous pyelogram (IVP) images to be suboptimal.


Magnetic resonance urography (MRU) in children is becoming more commonly used in the diagnosis and management of congenital uropathies, such as ureteropelvic junction obstruction. . MRU is especially useful in the management of obstructed kidneys that have rotation or ascent anomalies, or are solitary. . MRU can more clearly define the anatomy and delineate the proper surgical approach (ie, retroperitoneal versus transperitoneal).
. The disadvantage of MRU is that they study often requires a general anesthesia or heavy conscious sedation in children. Furthermore, the contrast agent gadolinium can only be used if the renal function is normal (requiring a preprocedure serum creatinine test) because of reports of irreversible renal fibrosis in patients with renal insufficiency. . Newer MRU technology may even define obstruction, eliminating the need for diuretic renal scans.
APPROACH . The goal of evaluation is to identify all infants with significant renal or urinary tract abnormalities but limit unnecessary radiographic studies and minimize parental distress in infants with clinically insignificant findings or normal infants. . The risk of renal and urinary tract abnormality increases with the 1. severity of hydronephrosis 2. persistence of hydronephrosis into the third trimester 3. bilateral involvement 4. presence of oligohydramnios.
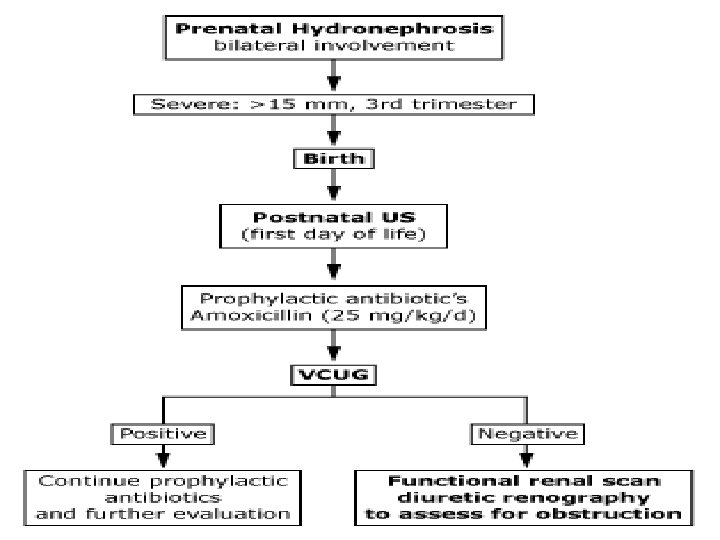
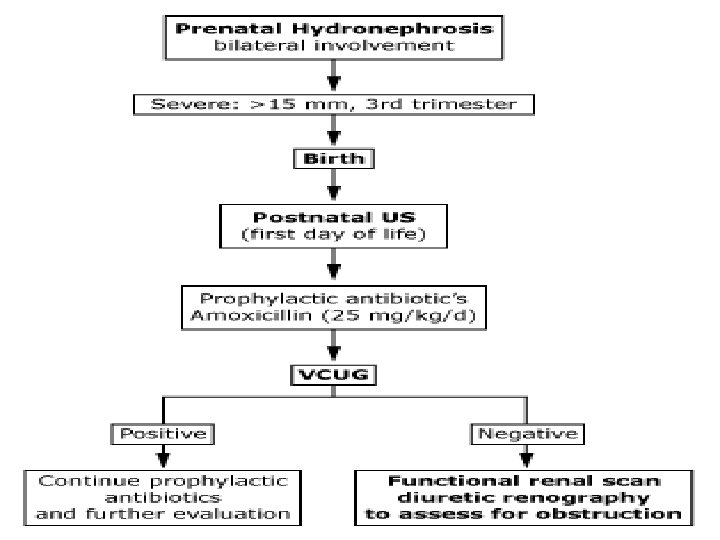
Severe Bilateral hydronephrosis . Infants with severe bilateral antenatal hydronephrosis and/or bladder distension are at increased likelihood to have significant disease. These infants and those with a severe hydronephrotic solitary kidney should be evaluated initially by ultrasonography on the first postnatal day. Bilateral hydronephrosis suggests an obstructive process at the level or distal to the bladder such as ureterocele or posterior urethral valves (PUV) in a male infant, which can be associated with impaired renal function and ongoing renal injury.
. If the postnatal ultrasound demonstrates persistent hydronephrosis, a VCUG should be performed. In male infants, the posterior urethra should be fully evaluated to detect possible posterior urethral valves. Mild & moderate bilateral hydronephrosis. Infants with mild or moderate hydronephrosis can be evaluated after 7 days of life.
Severe unilateral hydronephrosis . In newborns with severe antenatal unilateral hydronephrosis (renal pelvic diameter >15 mm in the third trimester), ultrasonography should be performed after the infant returns to birth weight (after 48 hours of age and within the first two weeks of life).
Moderate and mild unilateral hydronephrosis . In newborns with less severe antenatal unilateral hydronephrosis (renal pelvic diameter <15 mm during third trimester), ultrasonography can be performed after they reach seven days of age to see if the hydronephrosis is persistent postnatally. The majority of cases with moderate hydronephrosis appear to resolve by 18 months of age. . This was illustrated by a prospective study of 282 infants (two months of age) with renal pelvic diameters between 10 and 15 mm, which resolved (defined as renal pelvic diameter ≤ 5 mm on two consecutive ultrasounds) in 94% of patients by 12 to 14 months of age. Of the 18 patients(6%) with persistent hydronephrosis, 14 had UPJ obstruction and 4 had VUR.
Antibiotic prophylaxis . Higher rates of urinary tract infections have been reported in children with prenatally diagnosed hydronephrosis compare to the general pediatric population. . The risk of infection rises if there is an underlying urologic abnormality, such as VUR or obstructive uropathy, and is greater in girls compared to boys. . As a result, in infants with severe hydronephrosis who are at greater risk for an underlying urologic abnormality, antibiotic prophylaxis (amoxicillin, 12 to 25 mg/kg PO daily) is started after delivery until the diagnosis of VUR or obstructive uropathy is excluded.
. Antibiotic prophylaxis in children with mild or moderate hydronephrosis confirmed postnatally has not been studied prospectively. In one retrospective study of 1514 with mild persistent hydronephrosis, the use of prophylactic antibiotics reduced the risk of febrile UTI in patients who had VUR. . Until further prospective studies are conducted, antibiotic prophylaxis should be considered until a VCUG has been performed and either the diagnosis of VUR has been made or eliminated. . Antiobiotic prophylaxis is not needed in infants with a normal postnatal ultrasound.
There is very little evidence on which to base reliable guidelines. As a rule, however, antibiotic prophylaxis is a prudent precaution for all newborn infants with prenatally detected uropathies, pending the outcome of postnatal investigations (particularly VCU). However, antibiotic prophylaxis may not be required for the following, although it is still generally prescribed: 1. isolated renal dilatation with an AP diameter of 10 mm or less 2. unilateral multicystic dysplastic kidney with a normal contralateral kidney and no evidence of contralateral or ipsilateral ureteric dilatation 3. an ectopic but otherwise normal kidney.
Further evaluation Persistent postnatal ultrasound findings Infants with persistent hydronephrosis should have a VCUG to detect vesicoureteral reflux (VUR). . VUR accounts for approximately 9 percent of cases of antenatal hydronephrosis, but it is a more common and severe in infants with persistent postnatal hydronephrosis (13 to 30 percent) . This was illustrated in a prospective study of 106 fetuses with renal pelvic diameter ≥ 5 mm. Two postnatal ultrasounds were performed at 5 to 7 days of age and during the third week of life, and a VCUG at 6 to 8 weeks of life. The following findings were noted:
. Of the 103 infants with complete data, 53 had normal postnatal ultrasounds, defined as pelvic diameter ≤ 7 mm without evidence of calyceal or ureteric dilatation, renal dysplasia, or other renal anomalies. VUR was detected in only three infants with normal postnatal ultrasounds, which was grade I in all three cases. . Fifty infants had an abnormal postnatal ultrasound. Thirteen had evidence of calyceal/ureteric dilatation but a normal renal pelvic diameter (≤ 7 mm), of which one infant had grade IV VUR. . Thirty-seven patients had persistent hydronephrosis (renal pelvic diameter >7 mm), of which five infants had VUR (Grade IV and V in three cases, and Grade II in two cases).
. Infants who have VUR demonstrated on VCUG should remain on antibiotic prophylaxis until therapeutic options can be discussed with the family and care providers. Options include observation, medical management including antibiotic prophylaxis, or surgical correction.
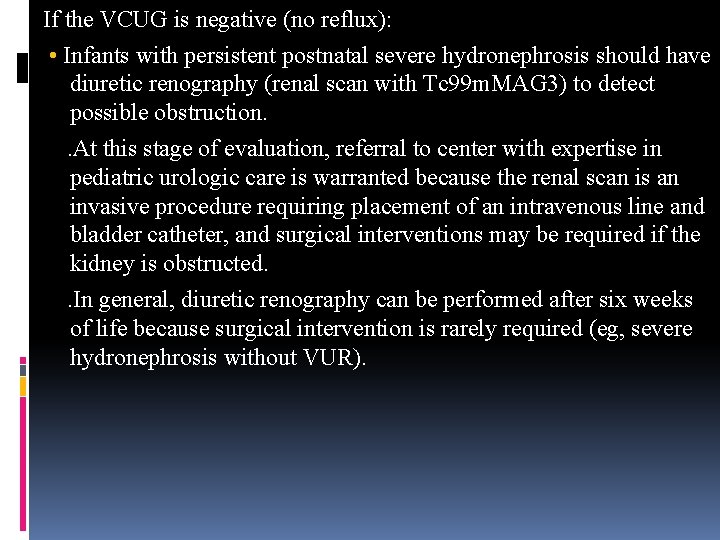
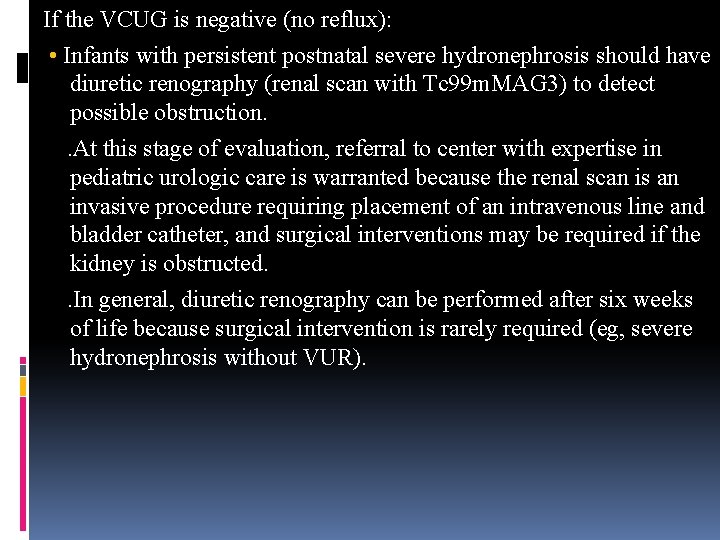
If the VCUG is negative (no reflux): • Infants with persistent postnatal severe hydronephrosis should have diuretic renography (renal scan with Tc 99 m. MAG 3) to detect possible obstruction. . At this stage of evaluation, referral to center with expertise in pediatric urologic care is warranted because the renal scan is an invasive procedure requiring placement of an intravenous line and bladder catheter, and surgical interventions may be required if the kidney is obstructed. . In general, diuretic renography can be performed after six weeks of life because surgical intervention is rarely required (eg, severe hydronephrosis without VUR).
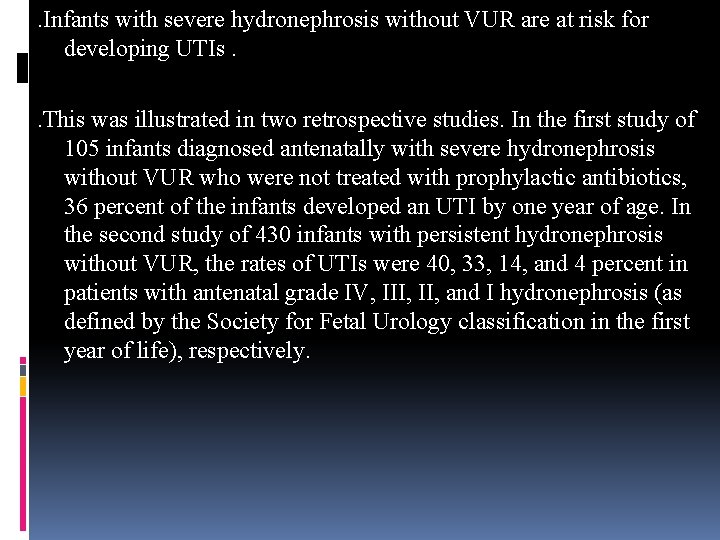
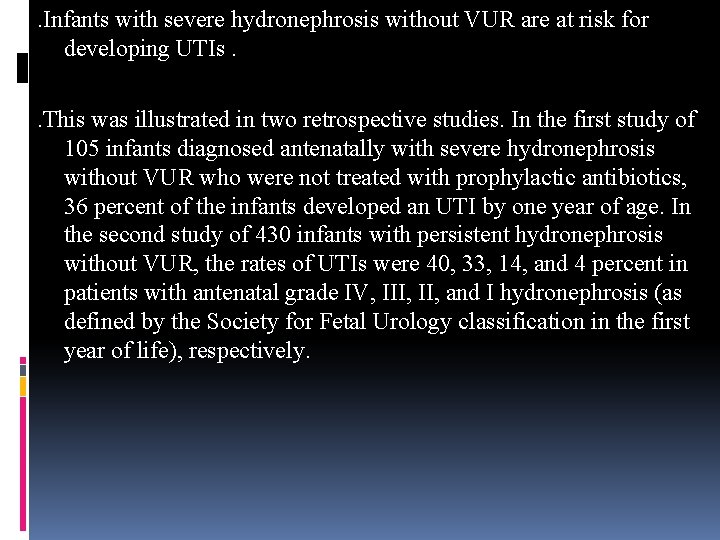
. Infants with severe hydronephrosis without VUR are at risk for developing UTIs. . This was illustrated in two retrospective studies. In the first study of 105 infants diagnosed antenatally with severe hydronephrosis without VUR who were not treated with prophylactic antibiotics, 36 percent of the infants developed an UTI by one year of age. In the second study of 430 infants with persistent hydronephrosis without VUR, the rates of UTIs were 40, 33, 14, and 4 percent in patients with antenatal grade IV, III, and I hydronephrosis (as defined by the Society for Fetal Urology classification in the first year of life), respectively.

. Nevertheless, the use of antibiotic prophylaxis in patients with prenatally diagnosed hydronephrosis that is subsequently confirmed to be ureteropelvic junction (UPJ) type hydronephrosis remains controversial. In general, antibiotic prophylaxis is given until the time of the VCUG. If the VCUG does not show reflux in general antibiotics are discontinued. However, in cases of the most severe grade IV hydronephrosis or in patients with a solitary kidney antibiotics are continued until surgical correction is performed or a decrease in the severity of hydronephrosis is detected by ultrasonography. It's prudent to remember that prior to the era of prenatal sonography, UPJ obstruction typically presented with urosepsis. . In general, antibiotic prophylaxis is given until the time of the VCUG. If the VCUG does not show reflux the antibiotics are discontinued.
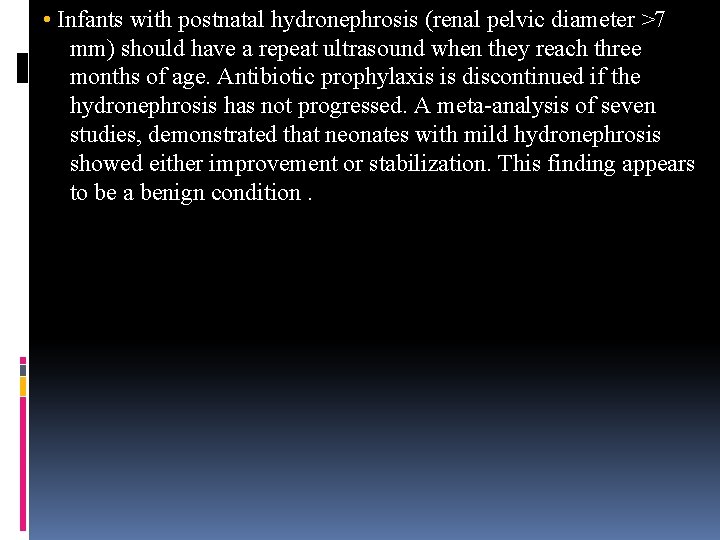
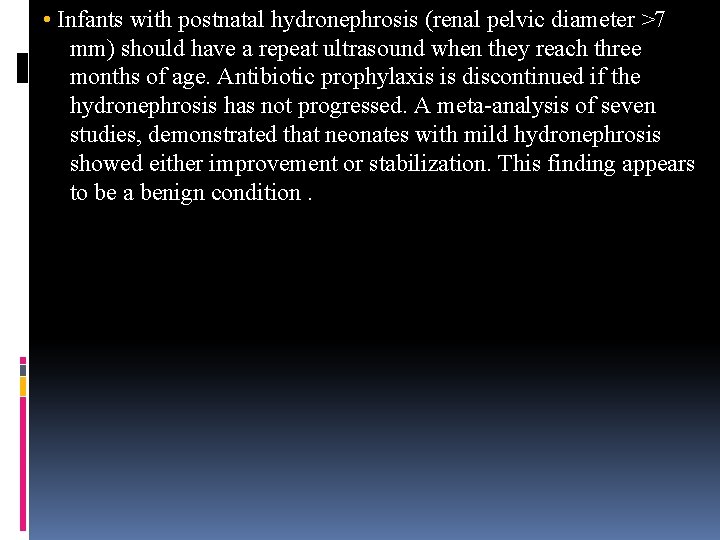
• Infants with postnatal hydronephrosis (renal pelvic diameter >7 mm) should have a repeat ultrasound when they reach three months of age. Antibiotic prophylaxis is discontinued if the hydronephrosis has not progressed. A meta-analysis of seven studies, demonstrated that neonates with mild hydronephrosis showed either improvement or stabilization. This finding appears to be a benign condition.

. However, in a small number of patients, hydronephrosis may worsen after initial improvement. In a retrospective review, four of 394 kidneys with hydronephrosis followed nonoperatively worsened after initial spontaneous improvement on renal ultrasonography. All four patients presented with clinical symptoms including abdominal pain, gross hematuria, and vomiting at a mean age of 40 months of age (range 22 to 60 months) consistent with a diagnosis of intermittent uretero pelvic junction obstruction requiring pyeloplasty.

Normal postnatal ultrasound Infants with a normal postnatal examination (defined as a renal pelvic diameter ≤ 7 mm without any evidence of calyceal or ureteric dilatation, or signs of renal dysplasia or anomalies) require no further evaluation. This was supported in one study of patients with antenatal hydronephrosis and normal postnatal ultrasounds that demonstrated normal DMSA scans in 49 of the 103 children available for evaluation at two-years of age. Renal ultrasound was normal in three additional children whose families refused a follow-up DMSA scan.







 Nursing management of hydronephrosis
Nursing management of hydronephrosis Nursing management of hydronephrosis
Nursing management of hydronephrosis Hydronephrosis
Hydronephrosis Congenital hydronephrosis
Congenital hydronephrosis Vesicoureteral reflux
Vesicoureteral reflux Intraluminal intramural extramural
Intraluminal intramural extramural Hydronephrosis radiopedia
Hydronephrosis radiopedia Neonatal period is defined as
Neonatal period is defined as Lisa has a diagnosed learning disability
Lisa has a diagnosed learning disability How is progeria diagnosed
How is progeria diagnosed How is progeria diagnosed
How is progeria diagnosed How is crohn's disease diagnosed
How is crohn's disease diagnosed Two years ago jenny was diagnosed with schizophrenia
Two years ago jenny was diagnosed with schizophrenia Total bilirubin newborn chart
Total bilirubin newborn chart Tetanus
Tetanus Antenatal card
Antenatal card Antenatal class adalah
Antenatal class adalah Role of antenatal care
Role of antenatal care Antenatal card template south africa
Antenatal card template south africa Conclusion for antenatal care
Conclusion for antenatal care Antenatal visits
Antenatal visits Antenatal care definition
Antenatal care definition Etiolgy
Etiolgy Antenatal care summary
Antenatal care summary Antenatal intrapartum and postnatal
Antenatal intrapartum and postnatal Antenatal examination grips
Antenatal examination grips Whooley questions nice
Whooley questions nice 3 weeks pregnant ultrasound
3 weeks pregnant ultrasound Antenatal care definition
Antenatal care definition Mcug
Mcug The development of children 7th edition
The development of children 7th edition Absolute refractory period and relative refractory period
Absolute refractory period and relative refractory period Is hyperpolarization the same as refractory period
Is hyperpolarization the same as refractory period Critical period vs sensitive period
Critical period vs sensitive period Critical period
Critical period Critical period vs sensitive period
Critical period vs sensitive period Classic period
Classic period Non-metal halogen family atomic mass 35
Non-metal halogen family atomic mass 35 1970 1972
1970 1972 Stability period vs measurement period
Stability period vs measurement period Trustee period and royal period
Trustee period and royal period Prehistory vs history
Prehistory vs history Yorkshire neonatal network
Yorkshire neonatal network Vasculopatía lenticuloestriada neonatal
Vasculopatía lenticuloestriada neonatal Circulação neonatal
Circulação neonatal Circulação neonatal
Circulação neonatal Tamiz neonatal
Tamiz neonatal Ambiente termico neutro
Ambiente termico neutro Epizod hızı
Epizod hızı Neonatal sepsis pathophysiology diagram
Neonatal sepsis pathophysiology diagram Sepsis temprana
Sepsis temprana Fisiopatologia de ictericia neonatal
Fisiopatologia de ictericia neonatal Equation
Equation Poliglobulia neonatal
Poliglobulia neonatal Nomograma de rawlings
Nomograma de rawlings Phototherapy unit uses
Phototherapy unit uses Parâmetros iniciais ventilação mecânica neonatal
Parâmetros iniciais ventilação mecânica neonatal Child pain scale
Child pain scale Halo oxigenoterapia alto flujo
Halo oxigenoterapia alto flujo Example of community health nursing diagnosis statement
Example of community health nursing diagnosis statement Storch infection
Storch infection L
L Dope neonatal resuscitation
Dope neonatal resuscitation Iap slides
Iap slides Neonatal resuscitation definition
Neonatal resuscitation definition Zonas de kramer ictericia neonatal
Zonas de kramer ictericia neonatal Bilirrubina total valores normales
Bilirrubina total valores normales Hemoglucotest en neonatos
Hemoglucotest en neonatos Escala kramer modificada
Escala kramer modificada Diagnostico de hiperbilirrubinemia neonatal
Diagnostico de hiperbilirrubinemia neonatal Zonas de kramer ictericia neonatal
Zonas de kramer ictericia neonatal Ascites veins
Ascites veins Zona de kramer
Zona de kramer Cuidados de enfermería en oxigenoterapia neonatal
Cuidados de enfermería en oxigenoterapia neonatal Circulação neonatal
Circulação neonatal Tetralogy of fallot heart sounds
Tetralogy of fallot heart sounds Hiponatremia neonatal
Hiponatremia neonatal Pacto pela redução da mortalidade materna e neonatal
Pacto pela redução da mortalidade materna e neonatal Aig gig pig
Aig gig pig Kukonmaz
Kukonmaz Neonatal sepsis symptoms
Neonatal sepsis symptoms Nelson nec
Nelson nec Neonatal cholestasis definition
Neonatal cholestasis definition Neonatal progeria
Neonatal progeria Icterícia neonatal tratamento
Icterícia neonatal tratamento Nanda hipertension
Nanda hipertension Hepatocytolyse
Hepatocytolyse Neonatal cholestasis naspghan
Neonatal cholestasis naspghan Hiperbilirrubinemia mixta
Hiperbilirrubinemia mixta Pathologic jaundice
Pathologic jaundice Neonatal hlr
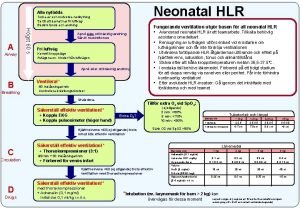
Neonatal hlr Vasculopatia lenticulo estriada
Vasculopatia lenticulo estriada Reflejos en el período neonatal
Reflejos en el período neonatal Hepatomogaly
Hepatomogaly Warm chain
Warm chain