Medical Therapy in congenital glaucoma complication and follow





![Oral medications �Carbonic anhydrase inhibitors (acetazolamide [Diamox], methazolamide [Neptazane. J). �may be used effectively Oral medications �Carbonic anhydrase inhibitors (acetazolamide [Diamox], methazolamide [Neptazane. J). �may be used effectively](https://slidetodoc.com/presentation_image_h/12fd1eb3fc0426c256527e1187bfacbd/image-19.jpg)



- Slides: 36
Medical Therapy in congenital glaucoma complication and follow up of patients Nasrollahi MD
�Congenital glaucoma is usually managed surgically, and medical therapy play an adjunctive role in this disease.
Where do we use medical therapy Preoperatively, medications may help to clear the cornea to facilitate goniotomy, � and postoperatively, they may help control IOP until the adequacy of the surgical procedure has been verified. � Medical therapy is also indicated in managing difficult cases in which surgery poses life-threatening risks or has incompletely controlled the glaucoma �
In general, the same basic principles of medical therapy apply to the treatment of congenital glaucoma as to adult glaucomas

beta-blocker �Topical beta-blocker therapy has been used in children for more than 30 years. �It usually lowers l. OP 20%-30%. �The major risks of this therapy are respiratory distress caused by apnea or bronchospasm and bradycardia, which occurs mostly in very young infants and in children with a history of bronchospasm.
�Timolol (or its equivalent) or betaxolol is usually used at 0. 25% & 0. 5 % strength twice a day for initial therapy. �Nasolacrimal occlusion at the time of drop placement may increase the efficacy of the drug and decrease its systemic side effects.
Betaxolol �Betaxolol is a cardioselective B 1 antagonist with fewer pulmonary and systemic side effects, � although its pressure-lowering effect may be less than that of the nonselective agents.

Carbonicanhydrase inhibitors �The topical carbonicanhydrase inhibitors(CAls) dorzalamide 2%(Trusopt) and brinzalamide 1% (Azapt) are available as solutions. � �Studies using topical CAls 3 times a day indicate that the drugs can be effective in children, although they produce a smaller reduction in l. OP « 15%). �There is no increased utility in using a topical CAI in a child already taking an oral CAI
combined beta antagonist-CAI �A combined beta antagonist-CAI (Cosopt) combines timolol and dorzalamide in a single eyedrop. � It has been used effectively when administered twice daily in children requiring dual therapy for l. OP control.
Prostaglandin analogues �Prostaglandin analogues latanoprost 0. 005% (Xalatan) and travoprost 0. 004% (Travatan) and a prostamide bimatoprost 0. 03% (Lumigan) have shown effectiveness in some pediatric patients. �Side effects include increased iris pigmentation and eyelash growth. �These medications are not recommended for patients with uveitic glaucoma.


Miotics �Miotics such as pilocarpine (Pilopine gel and Ocusert) and echothiophate (Phospholine. Iodide) are rarely used in children, �although Phospholine Iodide may be effective in the treatment of aphakic glaucoma. �Miotics paradoxically may increase the IOP by collapse of the trabecular meshwork because of the high insertion of uveal tissue into the posterior meshwork.
Adrenergic agents �such as epinephrine or dipivefrin (Propine) are not usually effective in children. �The a 2 -adrenergic agonist apraclonidine (Iopidine) may be useful for short-term l. OP reduction, but it has a high incidence of tachyphylaxis and allergy in young children.
Adrenergic agents �The a 2 -adrenergic agonist brimonidine (Alphagan) effectively reduces l. OP in some cases of pediatric glaucoma, �but this agent can produce profound systemic adverse effects in infants and small children (including lethargy, hypotonia, hypothermia, and serious central nervous system depression) �Therefore this drug is contraindicated in children younger than 2 years.

![Oral medications Carbonic anhydrase inhibitors acetazolamide Diamox methazolamide Neptazane J may be used effectively Oral medications �Carbonic anhydrase inhibitors (acetazolamide [Diamox], methazolamide [Neptazane. J). �may be used effectively](https://slidetodoc.com/presentation_image_h/12fd1eb3fc0426c256527e1187bfacbd/image-19.jpg)
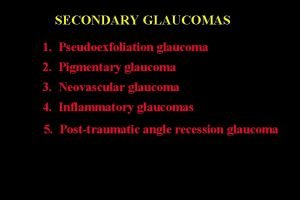
Oral medications �Carbonic anhydrase inhibitors (acetazolamide [Diamox], methazolamide [Neptazane. J). �may be used effectively in children, particularly to delay the need for surgery. �The usefulness of oral CAls may be limited by systemic adverse effects, including weight loss, lethargy‘ and metabolic acidosis.
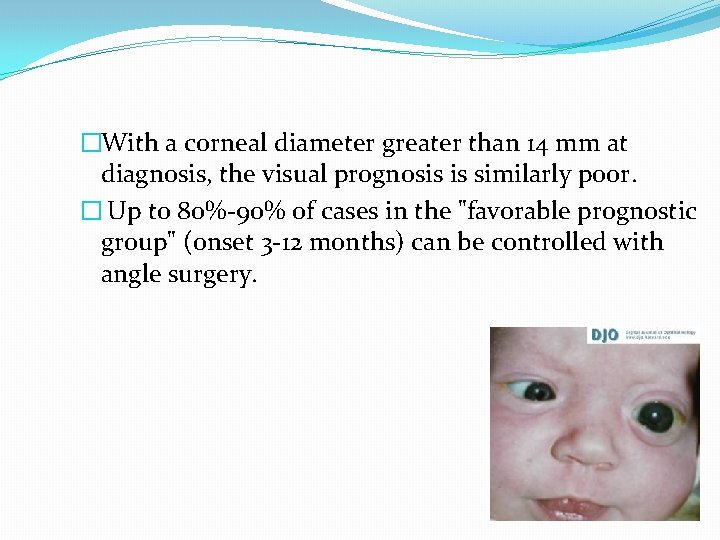
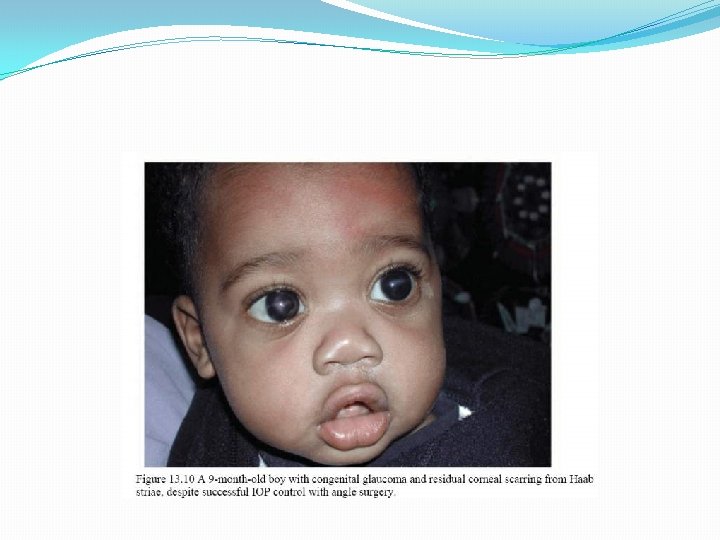
Prognosis and Follow-Up �If PCG presents at birth, the prognosis for l. OP control and visual preservation is poor, with at least half of these patients becoming legally blind.
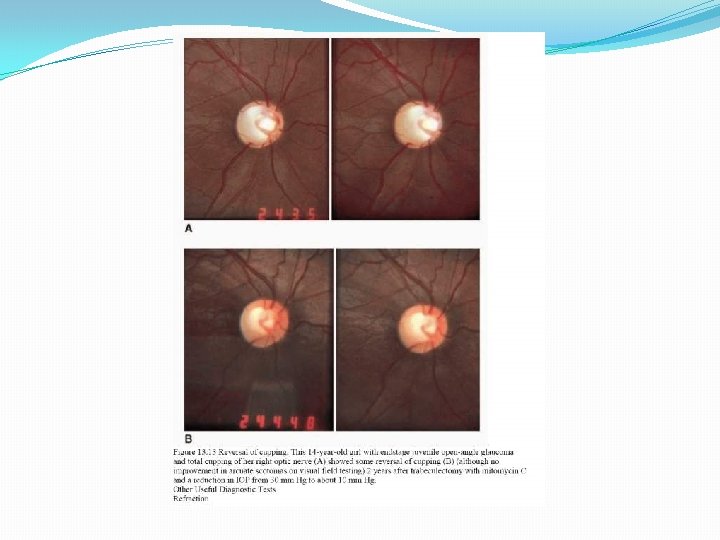
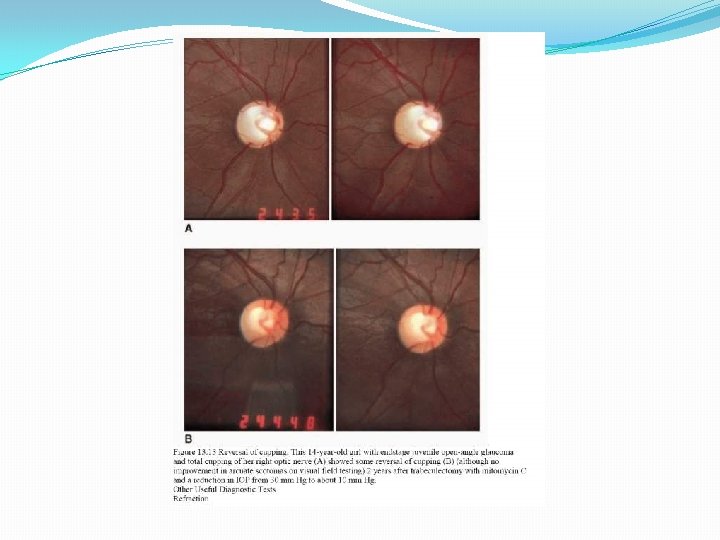
Follow up after surgery In the early postoperative period, close observation is required regarding success of the glaucoma procedure. In addition to IOP reduction, other clinical indicators of successful glaucoma control include: q clearing of corneal edema, q reversal of optic nerve cupping, q and even reduction in myopia in some cases. The IOP has also been related to postoperative visual capacity, with substantially better vision reported among those whose IOP remained no higher than 19 mm Hg in one series 21
�With a corneal diameter greater than 14 mm at diagnosis, the visual prognosis is similarly poor. � Up to 80%-90% of cases in the "favorable prognostic group" (onset 3 -12 months) can be controlled with angle surgery.
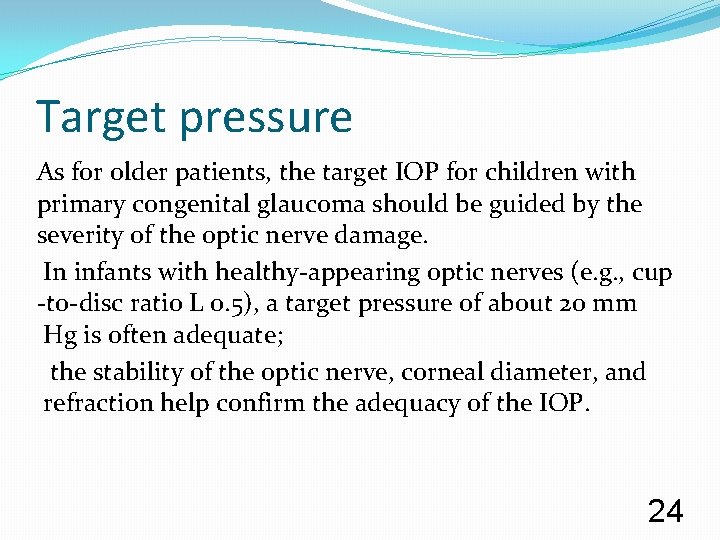
Target pressure As for older patients, the target IOP for children with primary congenital glaucoma should be guided by the severity of the optic nerve damage. In infants with healthy-appearing optic nerves (e. g. , cup -to-disc ratio L 0. 5), a target pressure of about 20 mm Hg is often adequate; the stability of the optic nerve, corneal diameter, and refraction help confirm the adequacy of the IOP. 24

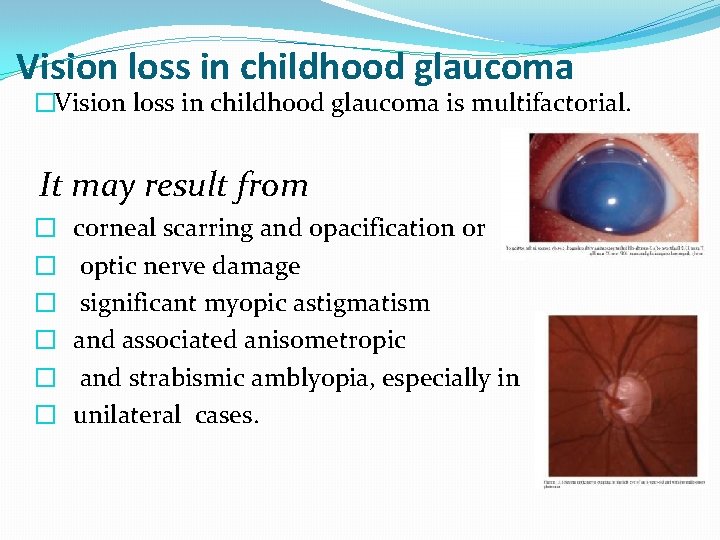
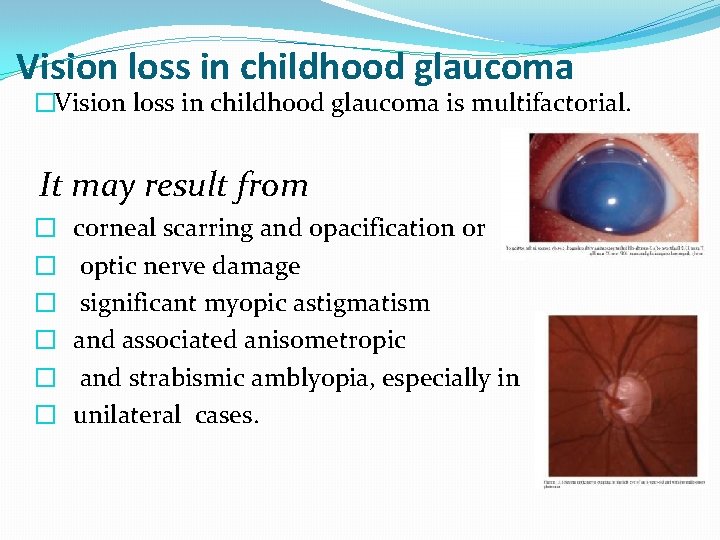
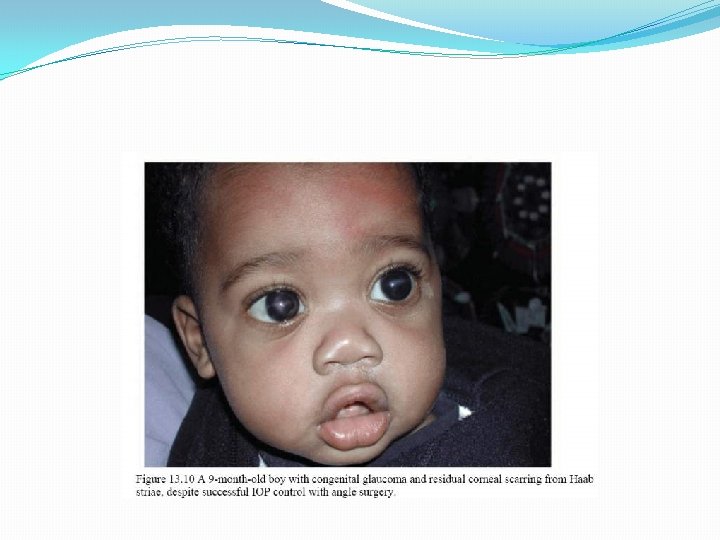
Vision loss in childhood glaucoma �Vision loss in childhood glaucoma is multifactorial. It may result from � � � corneal scarring and opacification or optic nerve damage significant myopic astigmatism and associated anisometropic and strabismic amblyopia, especially in unilateral cases.
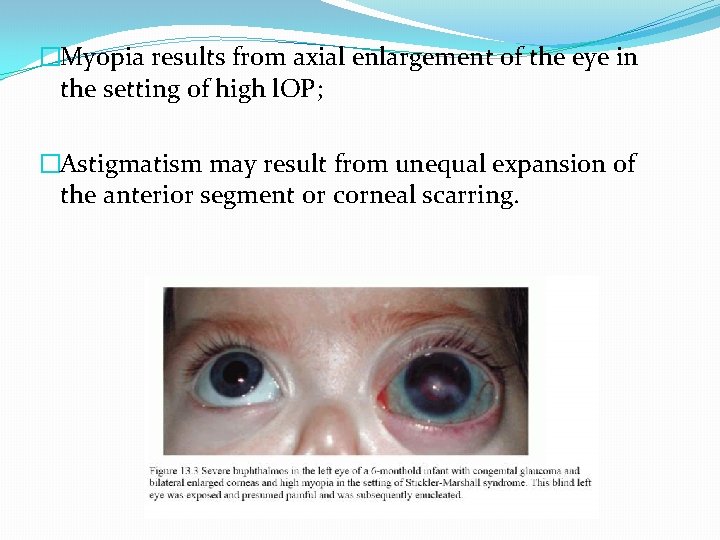
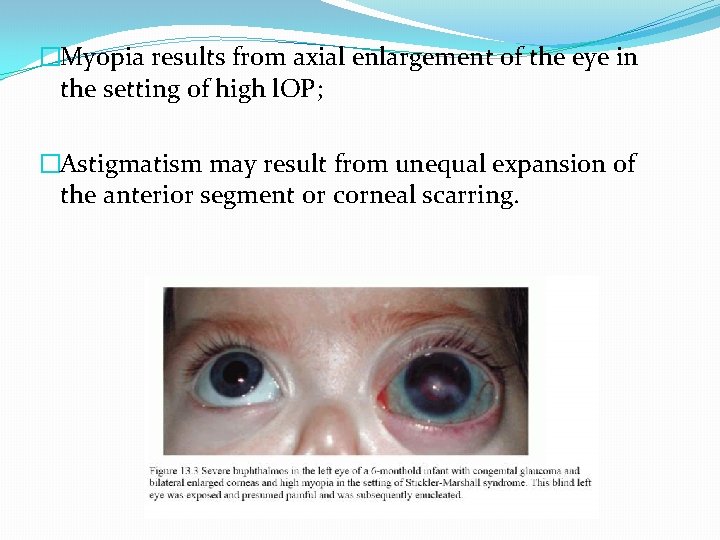
�Myopia results from axial enlargement of the eye in the setting of high l. OP; �Astigmatism may result from unequal expansion of the anterior segment or corneal scarring.

�All cases of childhood glaucoma, as well as suspected but unconfirmed glaucoma, require diligent followup. � After any given surgical intervention or change in medical therapy, control of IOP should be assessed within a few weeks.
�Examination under sedation or anesthesia is often necessary for accurate assessment. �The l. OP should be considered not as an isolated finding but rather in conjunction with other measurements obtained from the examination, �including : refractive error (measured serially), corneal diameter, axial length, and cup-disc ratio.
�evidence shows § persistent corneal edema § or enlargement, progressive optic nerve cupping, § or myopic progression, �further intervention should be pursued despite the l. OP reading.
�In contrast, l. OP of about 20 mm Hg in a young child who shows evidence of clinical improvement may be followed carefully in the short term without any other intervention.
Long-term follow-up of children with glaucoma is important �Even those patients who do well initially after angle surgery can experience relapse years later, with elevated l. OP and subsequent vision loss. �visual fields are rarely reliable in children younger than 6 -8 years. � Optic nerve photographs should be taken whenever possible; these can be helpful for comparison during later examinations.
summary Visual loss due to amblyopia is common and should be aggressively treated. Lifelong follow-up is needed to guard against late loss of IOP control and to detect associated ocular problems such as corneal decompensation, cataract, and progressive optic nerve injury from inadequate IOP. 35

Thanks a lot for your attention
 Stumped cloudy cornea
Stumped cloudy cornea Haab's striae
Haab's striae Congenital glaucoma
Congenital glaucoma Local complications of iv therapy
Local complications of iv therapy Follow you wherever you go
Follow you wherever you go Psychodynamic and humanistic therapies have in common
Psychodynamic and humanistic therapies have in common Bioness integrated therapy system price
Bioness integrated therapy system price Psychoanalytic therapy is to as humanistic therapy is to
Psychoanalytic therapy is to as humanistic therapy is to Hydrocephalus
Hydrocephalus The necklace by guy de maupassant climax
The necklace by guy de maupassant climax Gestational diabetes complications
Gestational diabetes complications Scqa
Scqa Complication of parenteral nutrition
Complication of parenteral nutrition What the purpose of narrative text
What the purpose of narrative text Blood transfusion complications
Blood transfusion complications Dandy walker syndrome
Dandy walker syndrome Complication of liver cirrhosis
Complication of liver cirrhosis Portal hypertension
Portal hypertension Complication of liver cirrhosis
Complication of liver cirrhosis Groshung
Groshung Most common complication of central venous catheter
Most common complication of central venous catheter Massive transfusion complication
Massive transfusion complication Complication of parenteral nutrition
Complication of parenteral nutrition What are the complications of blood transfusion
What are the complications of blood transfusion Complication
Complication What are the complications of blood transfusion
What are the complications of blood transfusion Scqa also called the pyramid principle
Scqa also called the pyramid principle Complication
Complication Diabetes complication
Diabetes complication Diabetic foot
Diabetic foot Pulmonary embolism test
Pulmonary embolism test Perkins timetable of fracture healing
Perkins timetable of fracture healing Pyramid principle situation complication answer solution
Pyramid principle situation complication answer solution Clou de ender
Clou de ender Pars plicata
Pars plicata Triggerfish glaucoma
Triggerfish glaucoma Sampaolesi line
Sampaolesi line