Central Venous Access Approach and Complications Introduction l
















- Slides: 46
Central Venous Access: Approach and Complications

Introduction l Options – Peripheral venous catheters – Central venous catheters l Central Venous access: Internal Jugular, Subclavian, Femoral l Arterial Line access: Radial artery, Femoral artery, Axillary artery.
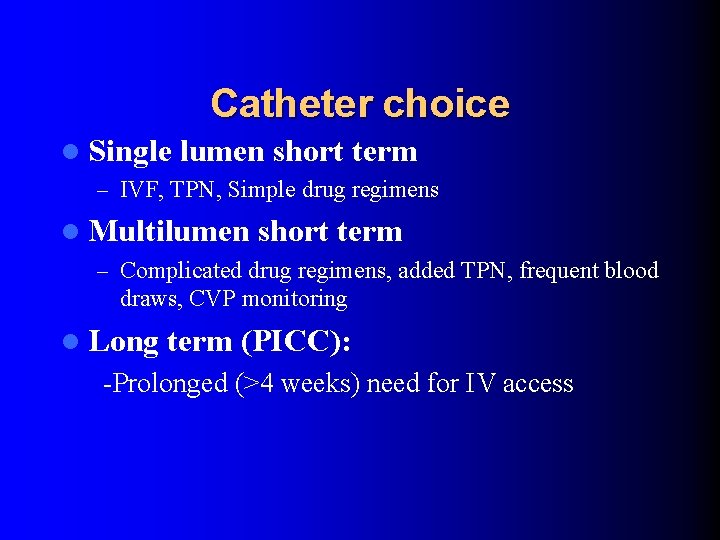
Catheter choice l Single lumen short term – IVF, TPN, Simple drug regimens l Multilumen short term – Complicated drug regimens, added TPN, frequent blood draws, CVP monitoring l Long term (PICC): -Prolonged (>4 weeks) need for IV access
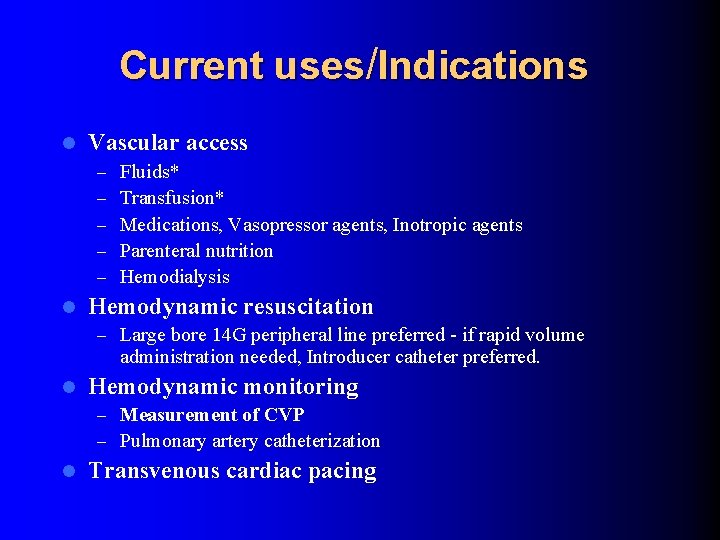
Current uses/Indications l Vascular access – – – l Fluids* Transfusion* Medications, Vasopressor agents, Inotropic agents Parenteral nutrition Hemodialysis Hemodynamic resuscitation – Large bore 14 G peripheral line preferred - if rapid volume administration needed, Introducer catheter preferred. l Hemodynamic monitoring – Measurement of CVP – Pulmonary artery catheterization l Transvenous cardiac pacing

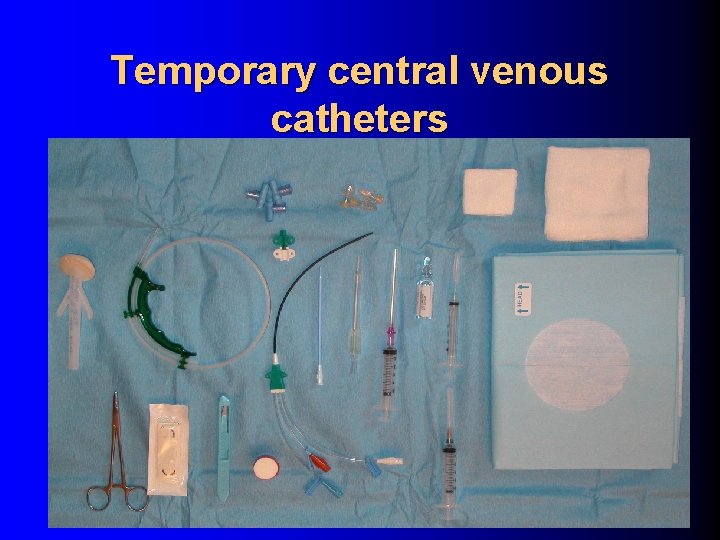
Temporary central venous catheters Procedures and Monitoring for the Critically Ill, Saunders, 2002
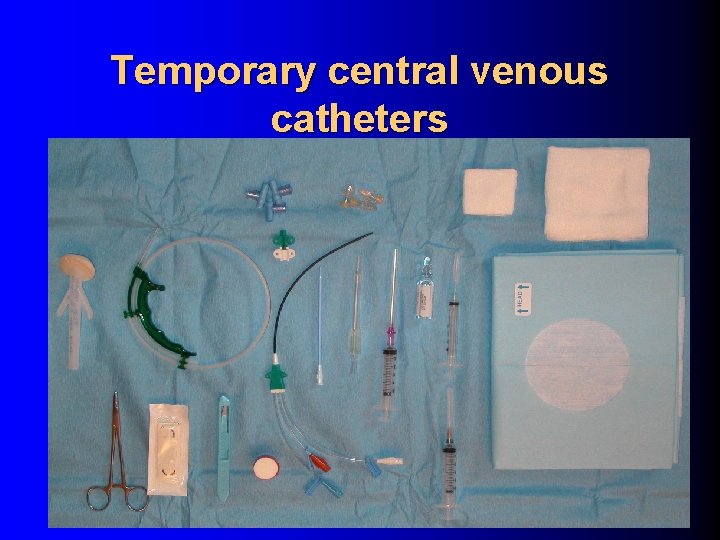
Temporary central venous catheters

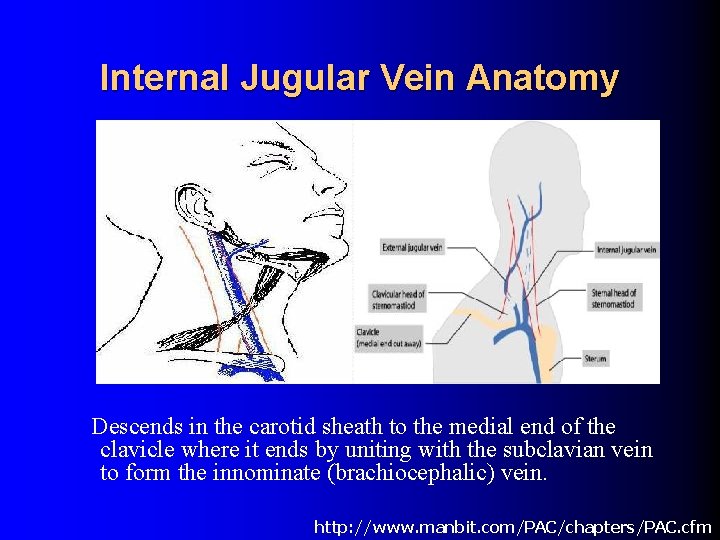
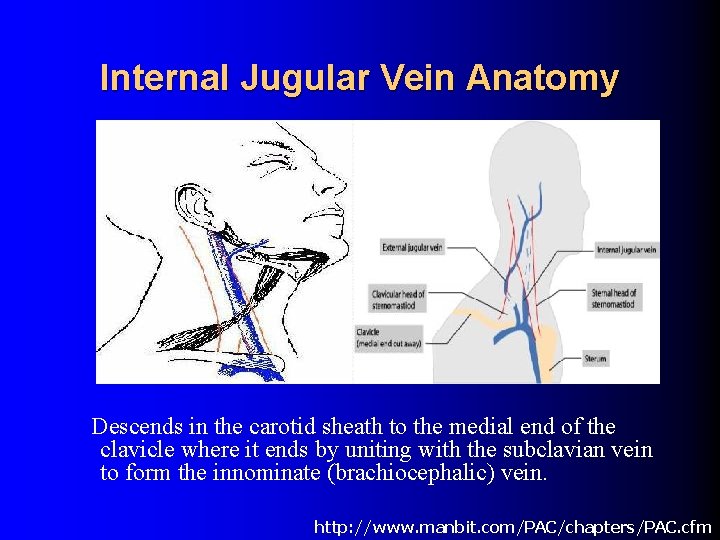
Internal Jugular Vein Anatomy Descends in the carotid sheath to the medial end of the clavicle where it ends by uniting with the subclavian vein to form the innominate (brachiocephalic) vein. http: //www. manbit. com/PAC/chapters/PAC. cfm

Internal Jugular Vein Anatomy The carotid artery and internal jugular vein are well seen. The IJV is much larger than the artery. Variable relationship of Internal Jugular Vein and Carotid Artery
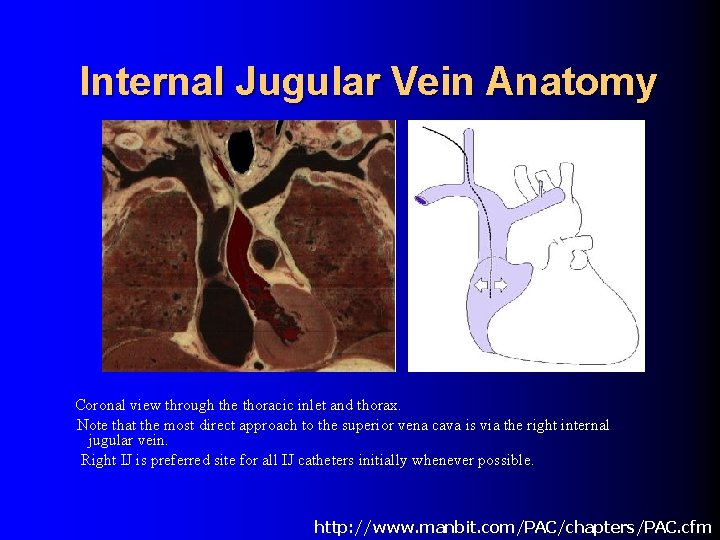
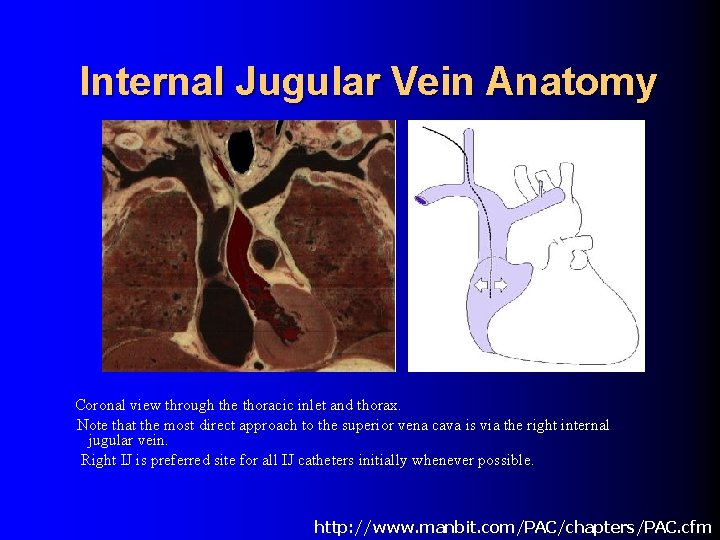
Internal Jugular Vein Anatomy Coronal view through the thoracic inlet and thorax. Note that the most direct approach to the superior vena cava is via the right internal jugular vein. Right IJ is preferred site for all IJ catheters initially whenever possible. http: //www. manbit. com/PAC/chapters/PAC. cfm
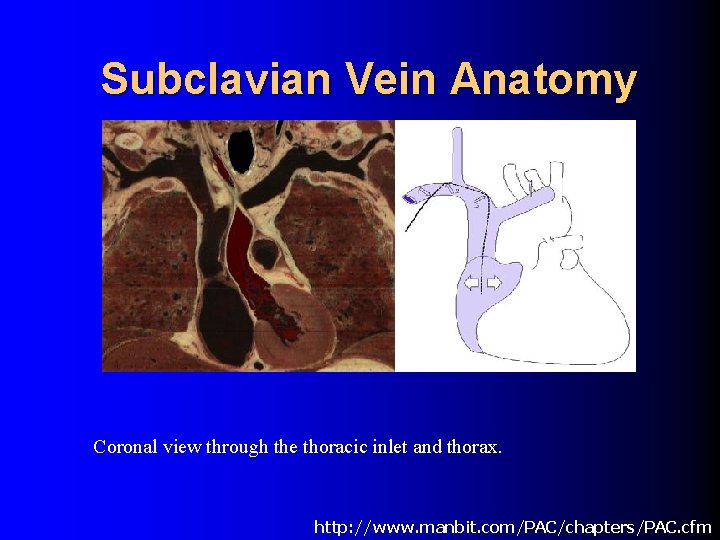
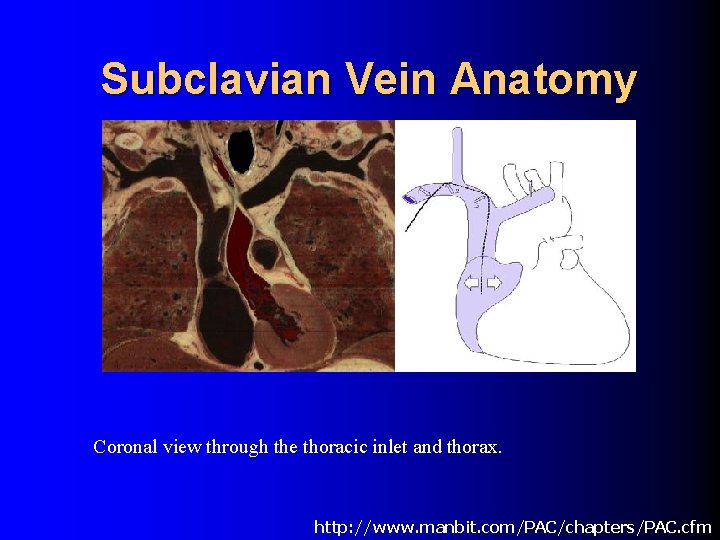
Subclavian Vein Anatomy Coronal view through the thoracic inlet and thorax. http: //www. manbit. com/PAC/chapters/PAC. cfm
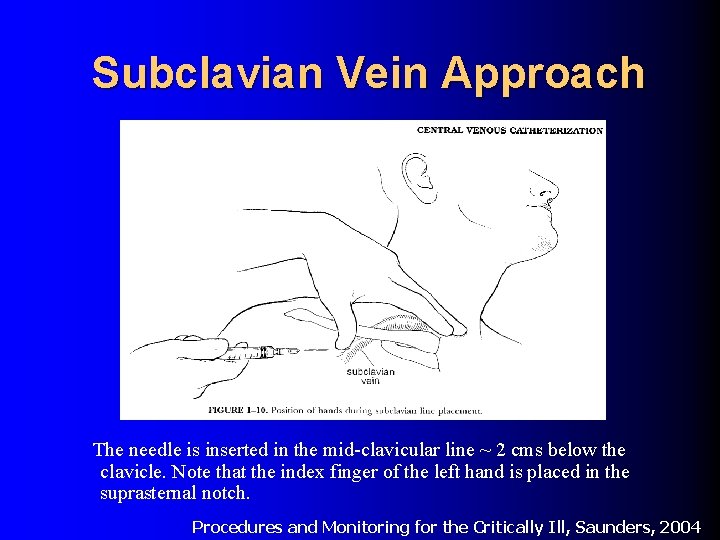
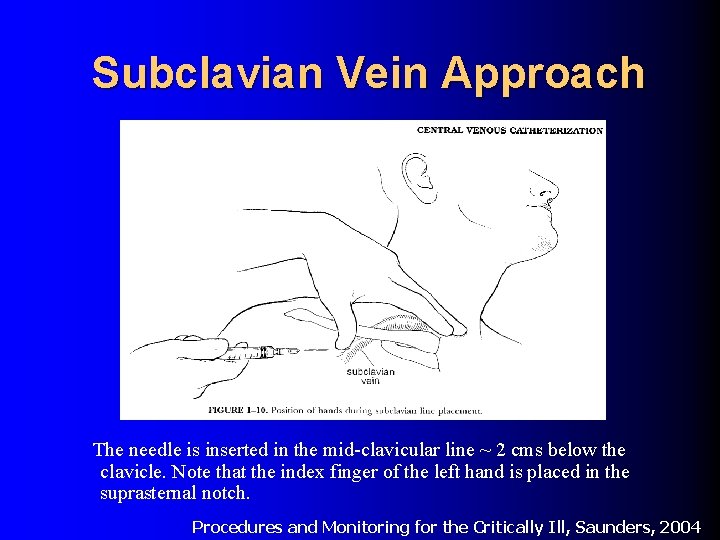
Subclavian Vein Approach The needle is inserted in the mid-clavicular line ~ 2 cms below the clavicle. Note that the index finger of the left hand is placed in the suprasternal notch. Procedures and Monitoring for the Critically Ill, Saunders, 2004

Relation to thoracic duct The confluence of the thoracic duct and the left subclavian vein is shown in this diagram. The duct loops behind the internal jugular vein to enter the subclavian vein in the region of its joining with the internal jugular vein. Thus it can be injured in left sided approach.
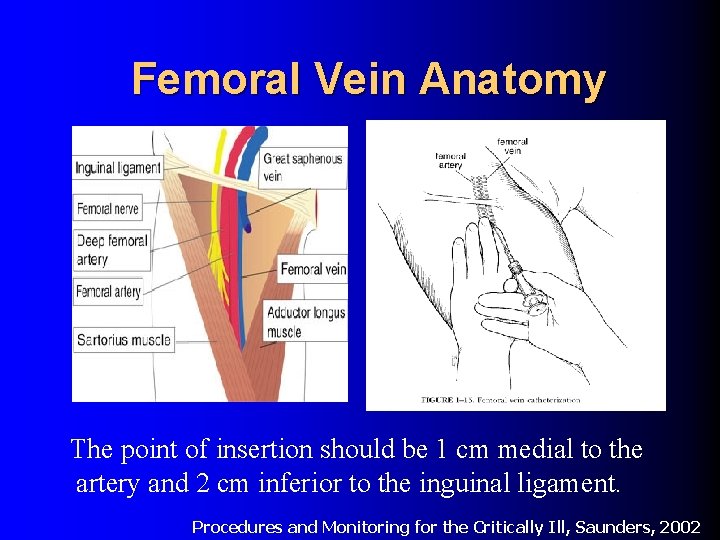
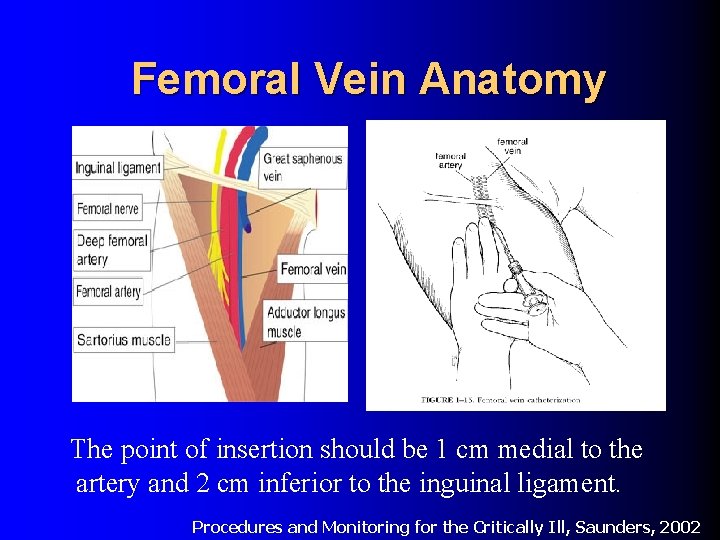
Femoral Vein Anatomy The point of insertion should be 1 cm medial to the artery and 2 cm inferior to the inguinal ligament. Procedures and Monitoring for the Critically Ill, Saunders, 2002
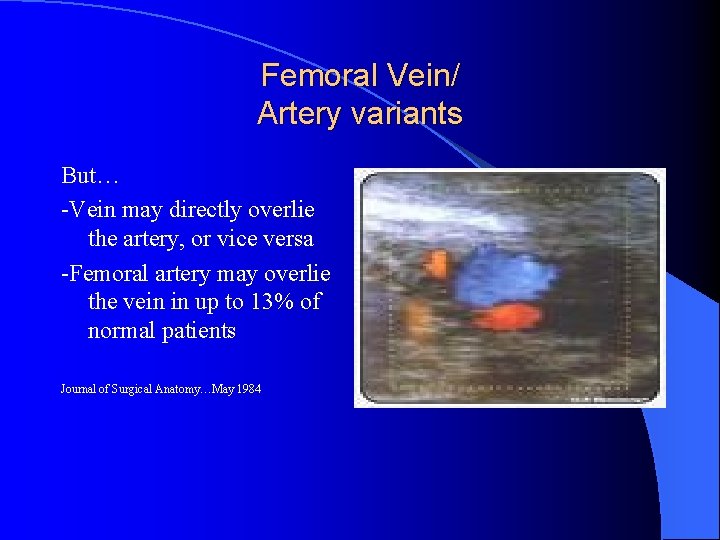
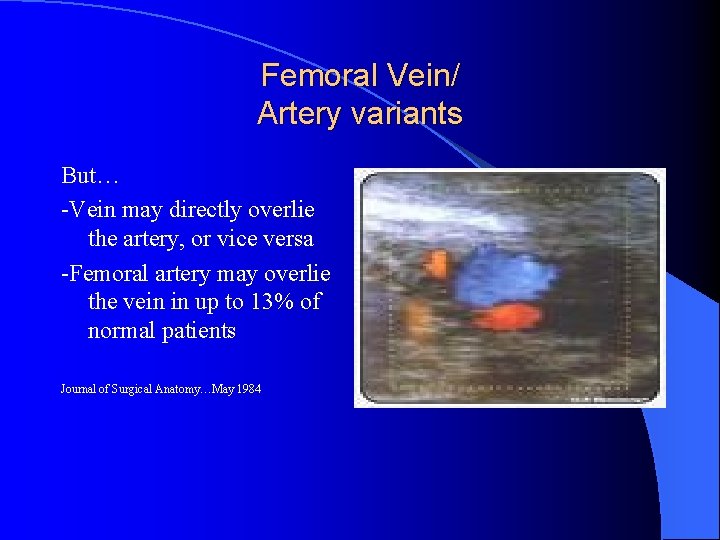
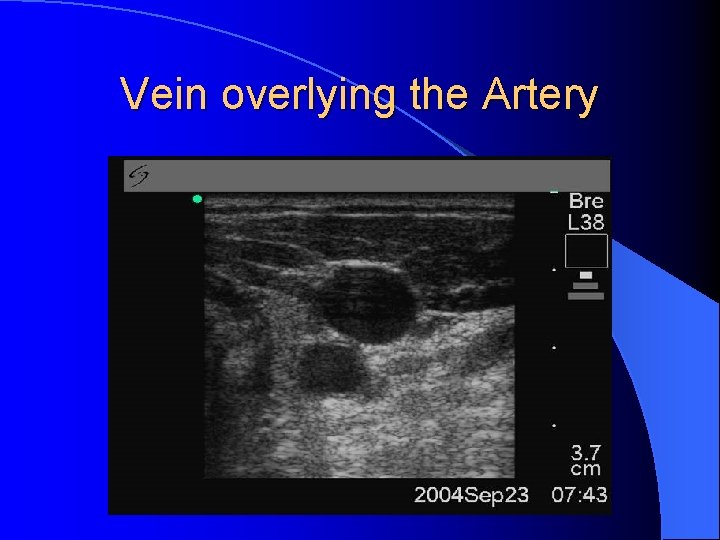
Femoral Vein/ Artery variants But… -Vein may directly overlie the artery, or vice versa -Femoral artery may overlie the vein in up to 13% of normal patients Journal of Surgical Anatomy…May 1984
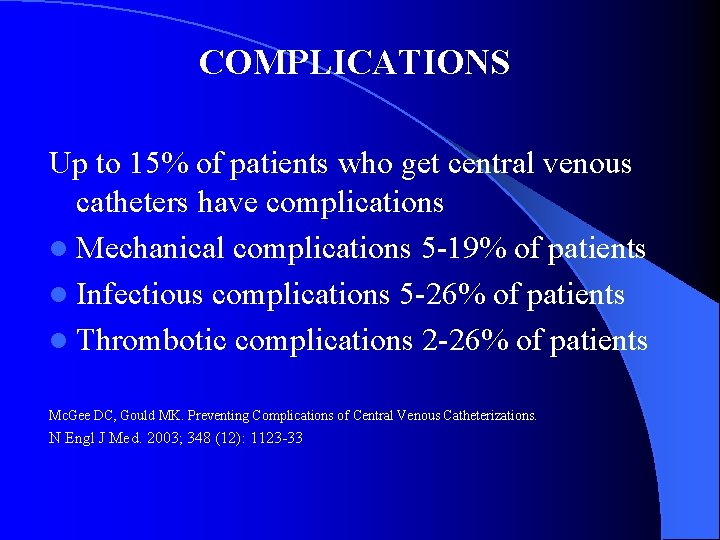
COMPLICATIONS Up to 15% of patients who get central venous catheters have complications l Mechanical complications 5 -19% of patients l Infectious complications 5 -26% of patients l Thrombotic complications 2 -26% of patients Mc. Gee DC, Gould MK. Preventing Complications of Central Venous Catheterizations. N Engl J Med. 2003; 348 (12): 1123 -33
Factors associated with Mechanical complications l l l Extremes of BMI (very low or high) Multiple prior catheterizations Advanced age Time needed to place catheter (multiple attempts) Prior radiotherapy, known history of vascular disease NEJM… 2003; 348; 1123 Intensive care Med… 2002; 28: 1036

Patient assessment l History: – Bleeding history, Previous access, Radiation, Peripheral vascular disease, Existing catheters in place: PICC, HD access, AICD, Pacemaker, etc. l Medications: – Anticoagulants Physical: – Clavicular anatomy, Flexibility, Trendelenberg positioning -- Can the patient be properly positioned? l Labs: – Platelets, PTT/PT INR l Ultrasound: – Vein compressible? Too close to the artery? Too small? Clot within the vessel? l Proper Site Selection
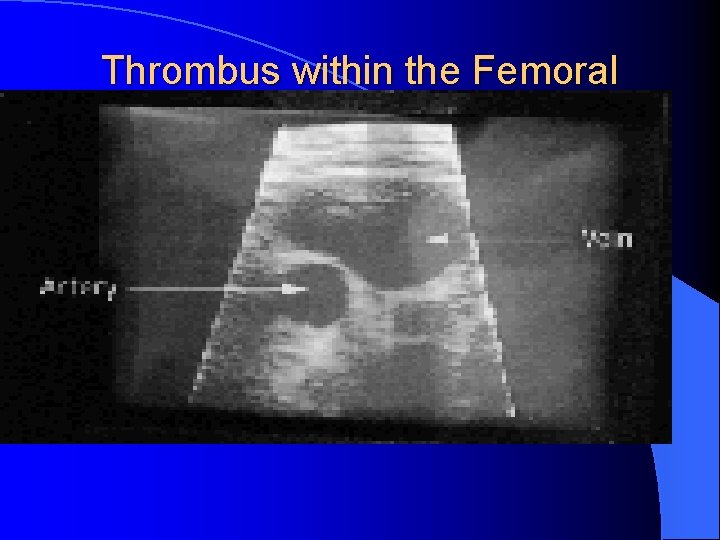
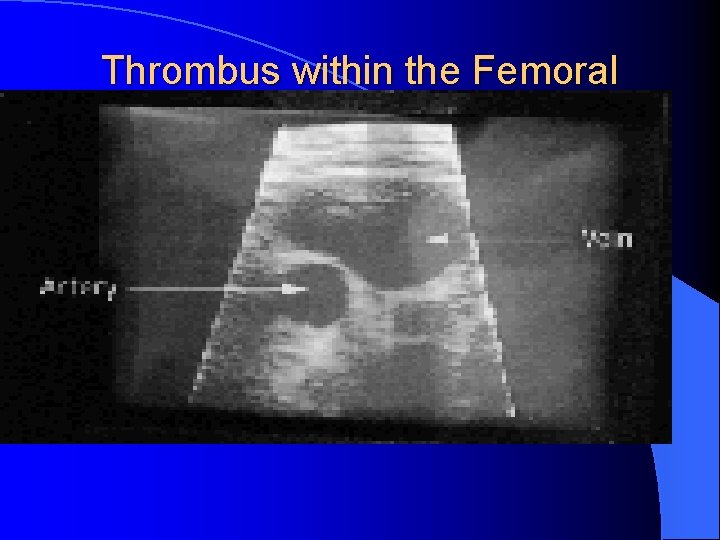
Thrombus within the Femoral Vein
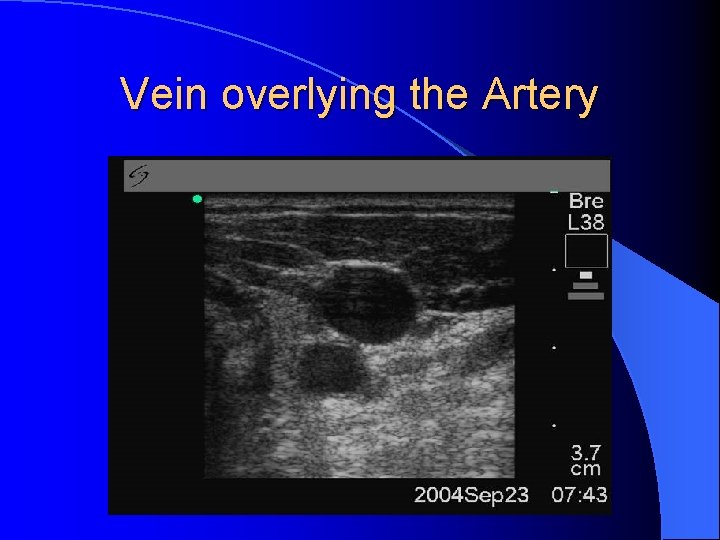
Vein overlying the Artery
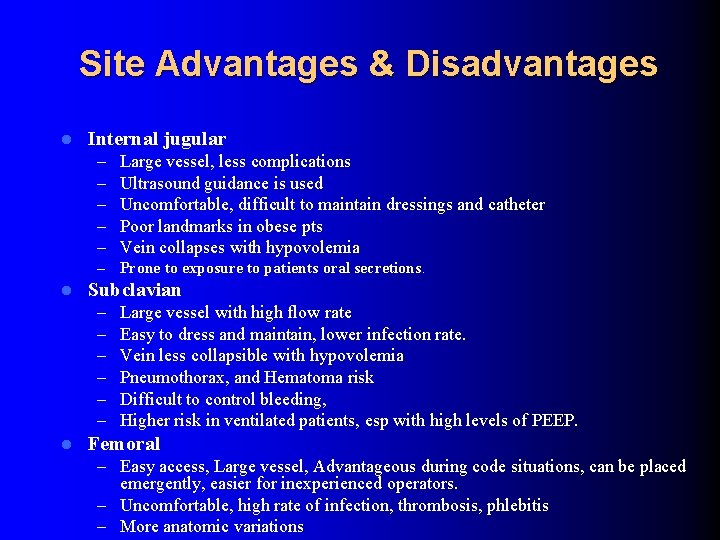
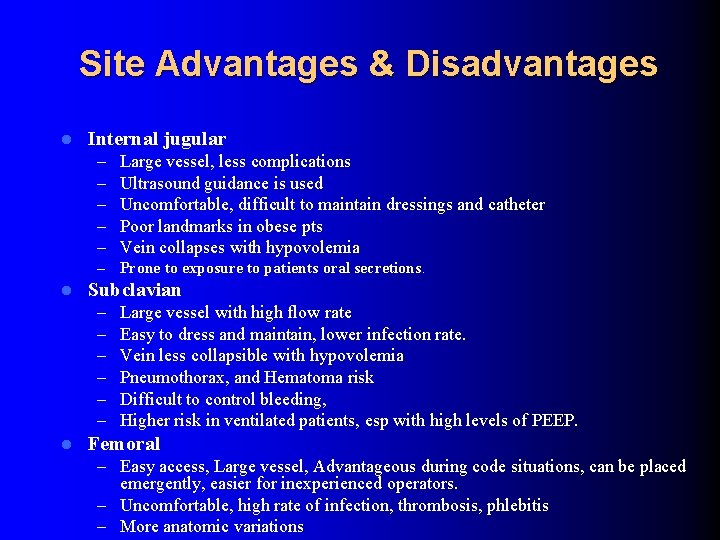
Site Advantages & Disadvantages l l Internal jugular – – – Large vessel, less complications Ultrasound guidance is used Uncomfortable, difficult to maintain dressings and catheter Poor landmarks in obese pts Vein collapses with hypovolemia – Prone to exposure to patients oral secretions. Subclavian – – – l Large vessel with high flow rate Easy to dress and maintain, lower infection rate. Vein less collapsible with hypovolemia Pneumothorax, and Hematoma risk Difficult to control bleeding, Higher risk in ventilated patients, esp with high levels of PEEP. Femoral – Easy access, Large vessel, Advantageous during code situations, can be placed emergently, easier for inexperienced operators. – Uncomfortable, high rate of infection, thrombosis, phlebitis – More anatomic variations

Common Insertion Mistakes l Multiple attempts at the same site – Max 3 attempts. Greater than 3 attempts is associated with increased complication rates, regardless of operator skill. – Use Ultrasound when experienced operator available Pushing the guidewire in too far l Pushing the guidewire or catheter against resistance l – False passage can be created – Vessel can be torn – Guidewire can become entrapped l Pulling the guidewire or catheter against resistance – Entangled by other intravenous devices- AICD, PM, Vascath, etc – Knot formation

How much guidewire is too much? Average Distance of atrio-caval junction from skin puncture site: Right Internal Jugular Vein to Atrio-caval junction 16. 0 cms Right Subclavian Vein to Atrio-caval Junction 18. 4 cms Left Internal Jugular Vein to Atrio-caval Junction 19. 1 cms Left Subclavian Vein to Atrio-caval Junction 20 cm 16. 5 cm should be considered the upper limit for most neck lines Crit Care Med 2000 Jan; 28(1): 138 -42
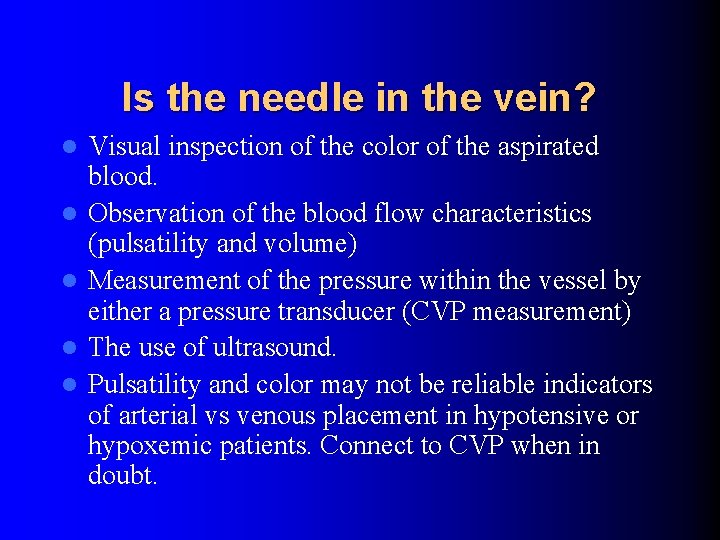
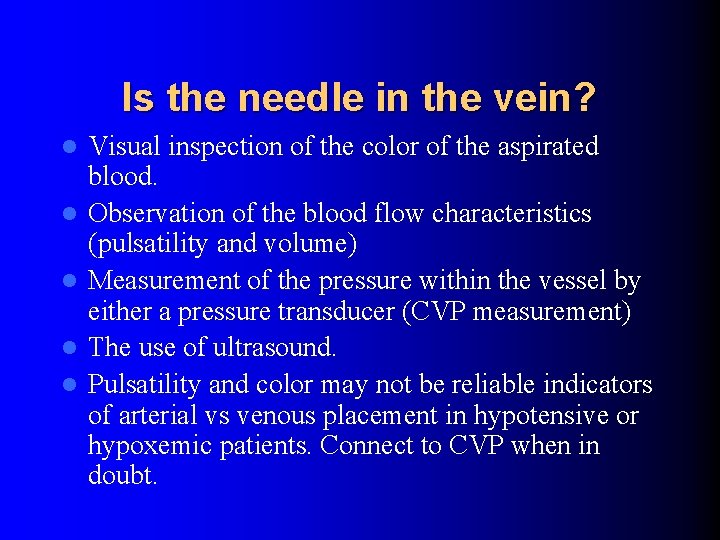
Is the needle in the vein? l l l Visual inspection of the color of the aspirated blood. Observation of the blood flow characteristics (pulsatility and volume) Measurement of the pressure within the vessel by either a pressure transducer (CVP measurement) The use of ultrasound. Pulsatility and color may not be reliable indicators of arterial vs venous placement in hypotensive or hypoxemic patients. Connect to CVP when in doubt.


Catheter complications: Early l Injuries – – l Cardiac - arrhythmia Lymphatic - Chylothorax Great vessel perforation, Vessel perforation or tears due to dilator or stiff catheter Malposition – 5% on post procedure CXR l Air embolism – Occurs during Insertion and removal – Cardiovascular collapse, wheel mill murmur – Rx: Left lateral decubitus positioning, air aspiration if possible.

Catheter complications: Early l Catheter embolism – Needs Radiologic retrieval l Guidewire complications – IVC filter entrapment – Guidewire entrapment on existing hardware – Loss of Guidewire l Pneumothorax – – 2 -10% with subclavian cannulation 1 -2% with internal jugular Post procedure CXR mandatory CXR needed before bilateral attempts!!

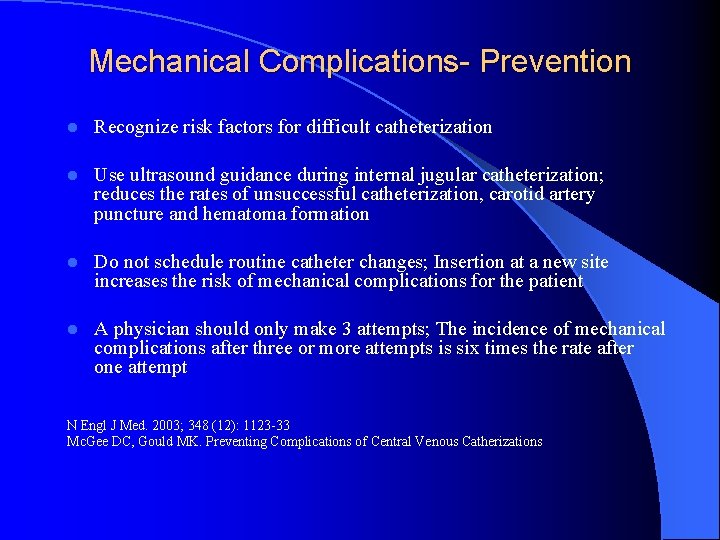
Mechanical Complications- Prevention l Recognize risk factors for difficult catheterization l Use ultrasound guidance during internal jugular catheterization; reduces the rates of unsuccessful catheterization, carotid artery puncture and hematoma formation l Do not schedule routine catheter changes; Insertion at a new site increases the risk of mechanical complications for the patient l A physician should only make 3 attempts; The incidence of mechanical complications after three or more attempts is six times the rate after one attempt N Engl J Med. 2003; 348 (12): 1123 -33 Mc. Gee DC, Gould MK. Preventing Complications of Central Venous Catherizations
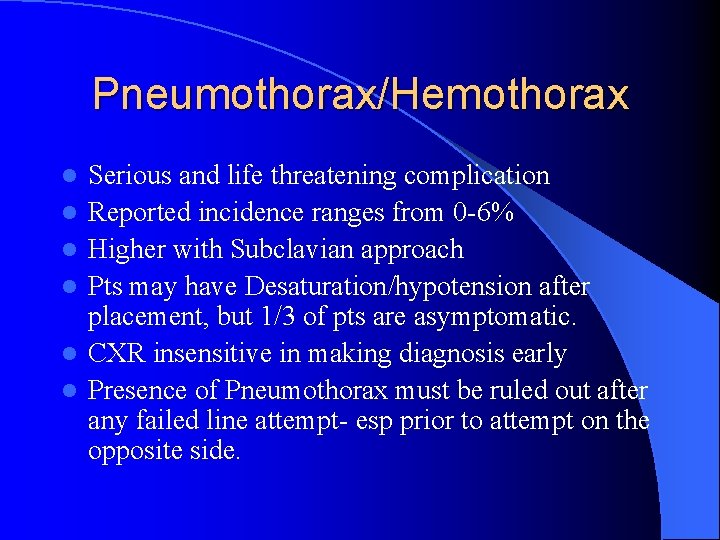
Pneumothorax/Hemothorax l l l Serious and life threatening complication Reported incidence ranges from 0 -6% Higher with Subclavian approach Pts may have Desaturation/hypotension after placement, but 1/3 of pts are asymptomatic. CXR insensitive in making diagnosis early Presence of Pneumothorax must be ruled out after any failed line attempt- esp prior to attempt on the opposite side.
Prevention l l l Optimal position Operator skill Alternate approach to subclavian site in high risk patients- COPD, bullous disease, PEEP. Avoid multiple attempts Tredelenberg position Bowyer MW, Bonar JP. Non-infectious complications of invasive hemodynamic monitering in the intensive care unit. In Complications in the ICU: recognition, prevention and management. 1997
Arterial Puncture l Incidence ranges from 1 -19% l Easy to identify in pts with normal BP and pa. O 2. More obscure in hypoxemic, hypotensive pts. l Results in hematoma formation. Large hematoma formation in the neck can potentially cause airway compromise.
Prevention l l l Avoid multiple attempts Ultrasound guidance Correction of coagulopathies Use of small finder needle Do not use dilator when in doubt CVP/ABG for confirmation Bowyer MW, Bonar JP. Non-infectious complications of invasive hemodynamic monitering in the intensive care unit. In Complications in the ICU: recognition, prevention and management. 1997

Arrhythmias Atrial and ventricular arrhythmias frequently accompany the insertion of CVP lines l These arrhythmias occur as a direct result of myocardial stimulation by the guidewire or catheter that has been advanced too far l Can be minimized by using the shortest catheter that will place the tip of the CVP catheter into the SVC just above the right atrium; l Bowyer MW, Bonar JP. Non-infectious complications of invasive hemodynamic monitering in the intensive care unit. In Complications in the ICU: recognition, prevention and management. 1997
Air Embolism l Air may enter the great vessels directly when a needle is inserted l Most cases occur during use or catheter maintenance l Negative intrathoracic pressure in a spontaneously breathing pt can draw air into the vein
Prevention l Occlude hubs at all times l Clear air bubbless l Flush all catheter ports!! l Trendelenberg postion increases CVP and reduces likelihood of air entry
Thoracic duct injury l The thoracic duct arches over the dome of the left lung lateral to the left internal jugular vein and joins the subclavian vein at the internal jugular-subclavian angle l Reported incidence of injury is 1% l Most commonly occurs with left sided subclavian cannulation
Catheter malposition l CXR confirms malposition l Repeat CXR can show migration of catheter

Radiographic assessment of implanted catheter Tip of subclavian catheter at atriocaval junction
Central Venous Catheter Tip Position l In the distal tip in the SVC for routine applications l In the upper right atrium, to achieve optimal performance of a hemodialysis or plasmapheresis catheter l The right tracheobronchial angle landmark Journal Of Intensive Care. . Feb 1999

Other Complications l l l Loss of Guidewire perforation of vessel Guidewire kinking Dislodgement of IVC filters Guidewire fragmentation/embolization Rx: Management of most of these complications will require interventional radiology or vascular surgery intervention.
Catheter Infection l Common (10%) and expensive (7 hospital days per infection, $6000 -10, 000) l 10 to 20% mortality. l Exit site, tunnel, catheter related sepsis, septic thrombophebitis, metastatic bacteremia
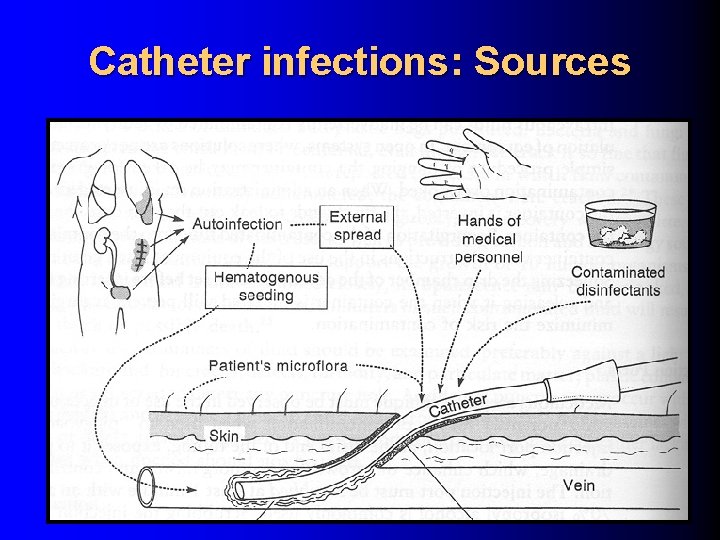
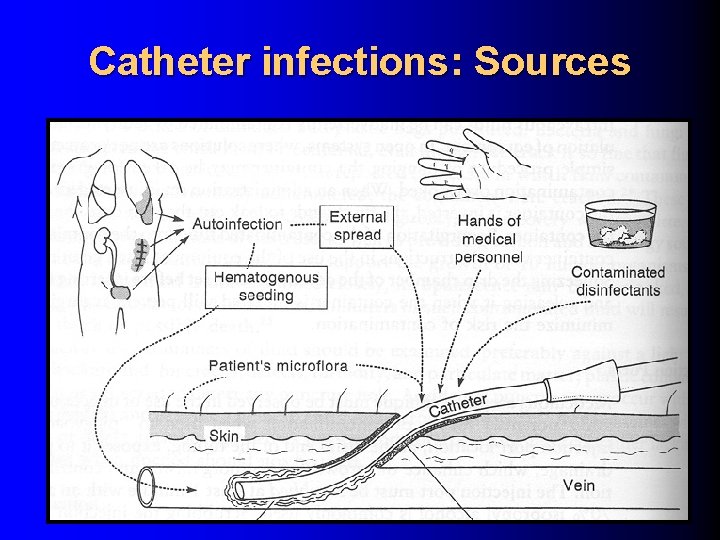
Catheter infections: Sources
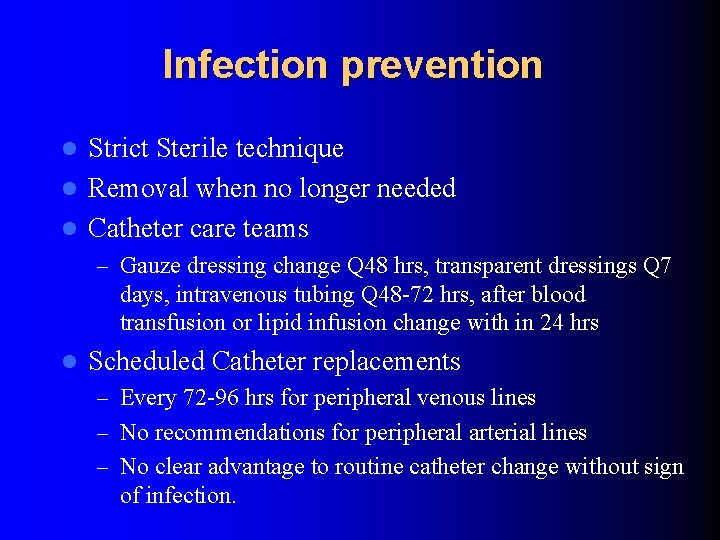
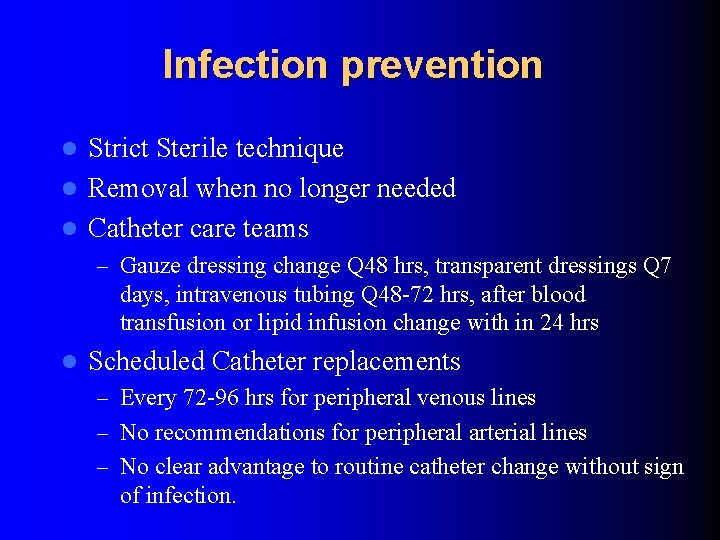
Infection prevention Strict Sterile technique l Removal when no longer needed l Catheter care teams l – Gauze dressing change Q 48 hrs, transparent dressings Q 7 days, intravenous tubing Q 48 -72 hrs, after blood transfusion or lipid infusion change with in 24 hrs l Scheduled Catheter replacements – Every 72 -96 hrs for peripheral venous lines – No recommendations for peripheral arterial lines – No clear advantage to routine catheter change without sign of infection.
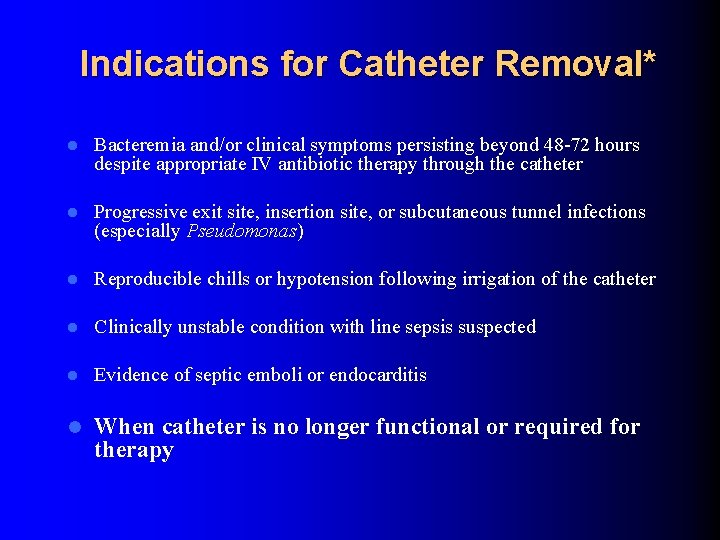
Indications for Catheter Removal* l Bacteremia and/or clinical symptoms persisting beyond 48 -72 hours despite appropriate IV antibiotic therapy through the catheter l Progressive exit site, insertion site, or subcutaneous tunnel infections (especially Pseudomonas) l Reproducible chills or hypotension following irrigation of the catheter l Clinically unstable condition with line sepsis suspected l Evidence of septic emboli or endocarditis l When catheter is no longer functional or required for therapy

Removal of Central Catheters l Neck Lines – Trendelenberg position advised l Risk of air embolism is highest during removal – Pressure l Limb lines – Reverse Trendenlenburg for femoral lines – Pressure – Occlusive dressing