Nutrition Support of the Surgical Patient Randa Jaroudi






















- Slides: 90
Nutrition Support of the Surgical Patient Randa Jaroudi, Pharm. D Clinical Coordinator TPN Coordinator KKUH
Nutrition n Nutrition allows the body to be provided with all basic nutrients substrates and energy required for maintaining or restoring all vital body functions from carbohydrate and fat and for building up body mass from amino acid.
Malnutrition n Malnutrition—come from extended inadequate intake of nutrient or severe illness burden on the body composition and function—affect all systems of the body
Type of Malnutrition Marasmus Protein – calorie malnutrition The patient's oral diet may include an acceptable protein: calorie ratio but is inadequate in quantity and calories. n (depleted somatic proteins, normal visceral proteins) Normal Albumin and transferrin Patients look thin and malnourished. e. g. Patients with mild to moderate starvation, common severe burns, injuries, systemic infections, cancer etc or conditions where patient does not eat like anorexia nervosa
Clinical Manifestations n Weight loss n Reduced basal metabolism n Depletion skeletal muscle and adipose (fat) stores n Decrease tissue turgor n Bradycardia n Hypothermia

Type of Malnutrition n Kwashiorkor (Kwa-shior-kor) Protein malnutrition the diet contains various amounts of nonprotein calories (inadequate, or excessive) from carbohydrates and fats, but is deficient in total protein and essential amino acids. (normal somatic proteins depleted visceral proteins) ↓ Serum Albumin and transferrin Patients appear normal or overweight e. g. Hypercatabolic critical care patients, chronic diarrhea, chronic kidney disease, trauma , burns, hemorrhage, and liver cirrhosis
Clinical Manifestations n Marked hypoalbuminemia n Anemia n Edema and ascites n Muscle atrophy n Delayed wound healing n Impaired immune function

Diagnosis Mixed Marasmus-Kwashiorkor: (depleted somatic and visceral proteins) All above data are reduced Patients appear cachexic and severely malnourished. e. g. *Chronic hypercatabolic patients (250 to 500 g loss of weight) *Prolonged starvation n Marasmic-kwashiorkor is a mixed form of any PCM symptoms. It frequently occurs when the marasmic patient experiences the catabolic stress of illness or trauma.
Medical causes (Risk factors for malnutrition) n n n Recent surgery or trauma Sepsis Chronic illness Gastrointestinal disorders Anorexia, other eating disorders Dysphagia Recurrent nausea, vomiting, or diarrhea Pancreatitis Inflammatory bowel disease Gastrointestinal fistulas Cancer
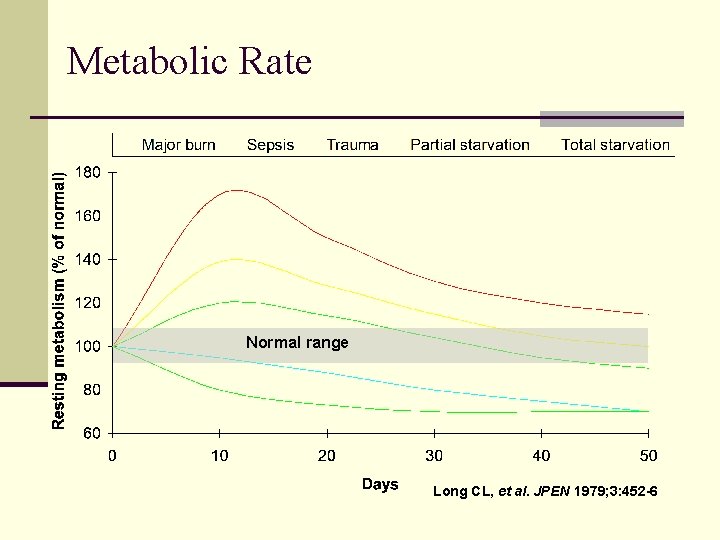
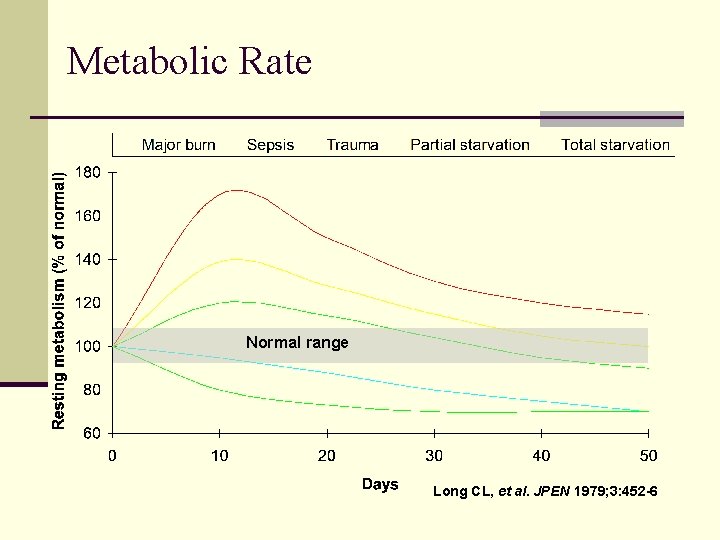
Metabolic Rate Normal range Long CL, et al. JPEN 1979; 3: 452 -6

Protein Catabolism Normal range Long CL. Contemp Surg 1980; 16: 29 -42
The Goals of Preoperative Nutrition Support n ↓ surgical mortality n ↓surgical complications and infection n Reduce the catabolic state and restore anabolism n ↓the hospital length of stay n Speed the healing/recovery process

Indications Aggressive nutritional support (enteral or parenteral) should be considered in minimum 3 of: n n n Looks clinically malnourished. Has a low serum albumin <3. 5 g/d. L. Has a recent loss of 10% or greater within Has a history of recent poor intake. Who as a consequence of his illness is going to be or has been NPO for 5 -7 days. The term “If gut works, use it” remains the golden rule. However, recently this was changed to: If gut works use it; and if gut works partially, use it partially.
Preoperative Nutrition Assessment-1 1. Medical & Nutritional History Medical history includes acute or chronic disease, medication, surgeries, & otherapies (i. e. , chemotherapeutics, immunosuppressive) Nutrition History includes recent changes in appetite or weight, activity level, use of diet. Subject Global Assessment (SGA)
Preoperative Nutrition Assessment-2 2. Physical examination Logical assessment from head to toe 3. Anthropometric parameters % of IBW = Actual weight x 100/Ideal body weight n Triceps Skinfold Thickness (TSF) for assessing fat reserve. It is decreased when fat stores are depleted. n Midarm muscle circumference (MAC) to assess the degree of somatic protein depletion. TSF and Mid Arm Circumference are no more recommended as an accurate measurement. n Creatinine Height Index (CHI) to assess somatic protein stores. Serum Protein Determination to assess the degree of visceral protein depletion, e. g. Albumin, Transferring, Prealbumin. n Measure Total Lymphocyte Count (TLC) to assess Immune function becomes impaired n 4. Lab assessment
Fat, Anthropometric parameters Assessment of body fat Triceps Skinfold Thickness (TSF) for assessing fat reserve. It is decreased when fat stores are depleted.
Protein (Somatic Protein) n Assessment of the fat-free muscle mass (Somatic Protein) depletion n Mid-upper-arm circumference (MAC) TSF and MAC are no more recommended as an accurate measurement
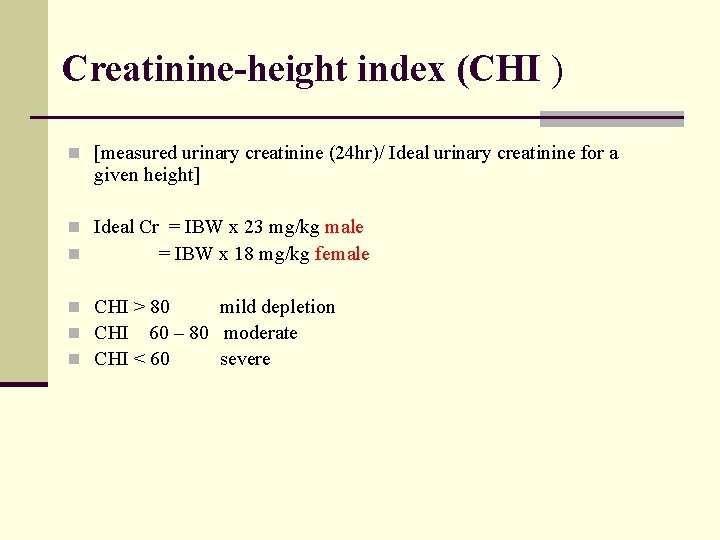
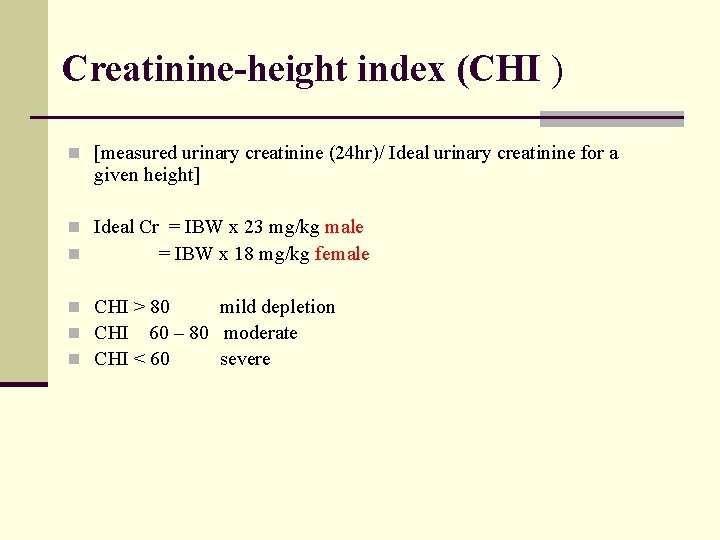
Creatinine-height index (CHI ) n [measured urinary creatinine (24 hr)/ Ideal urinary creatinine for a given height] n Ideal Cr = IBW x 23 mg/kg male n = IBW x 18 mg/kg female n CHI > 80 mild depletion n CHI 60 – 80 moderate n CHI < 60 severe
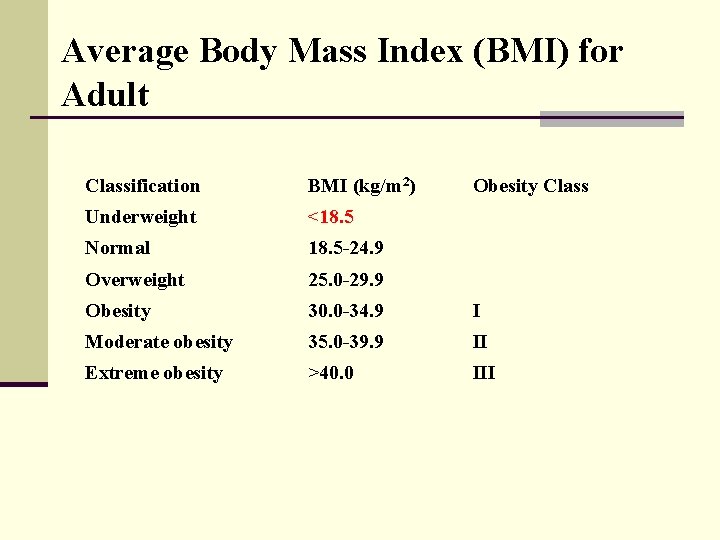
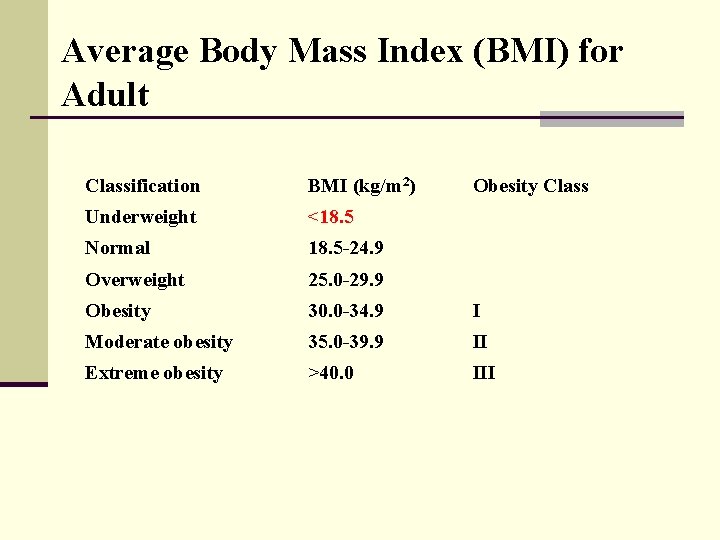
Average Body Mass Index (BMI) for Adult Classification BMI (kg/m 2) Obesity Class Underweight <18. 5 Normal 18. 5 -24. 9 Overweight 25. 0 -29. 9 Obesity 30. 0 -34. 9 I Moderate obesity 35. 0 -39. 9 II Extreme obesity >40. 0 III

Nutrition Provides n Energy n Amino Acid n Fluid & Electrolyte n Trace minerals (elements) n Vitamin n Certain drugs
Fluid Requirement
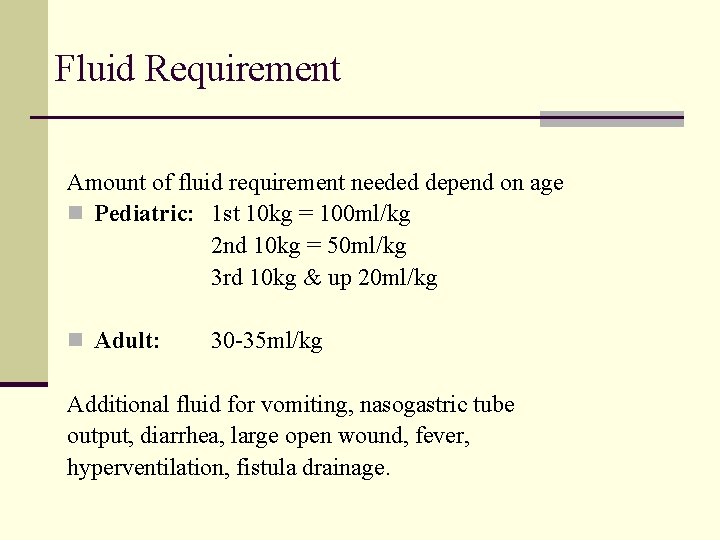
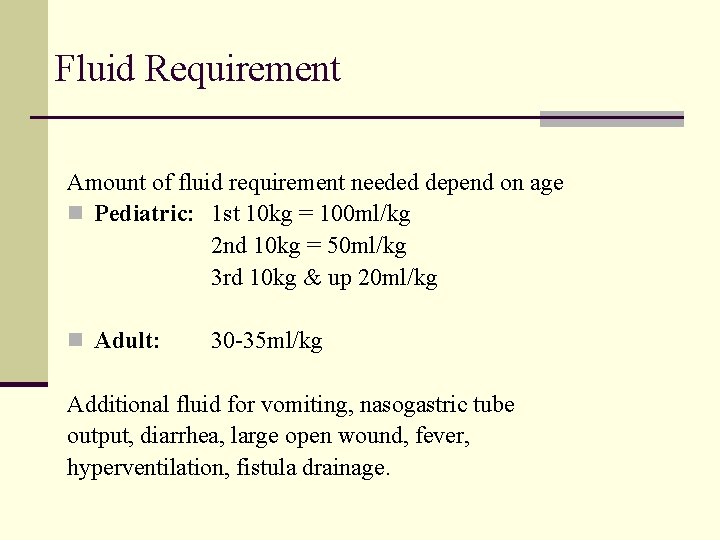
Fluid Requirement Amount of fluid requirement needed depend on age n Pediatric: 1 st 10 kg = 100 ml/kg 2 nd 10 kg = 50 ml/kg 3 rd 10 kg & up 20 ml/kg n Adult: 30 -35 ml/kg Additional fluid for vomiting, nasogastric tube output, diarrhea, large open wound, fever, hyperventilation, fistula drainage.

Fluid Requirements Special situation for fluid restriction: Fluid overload, n Cardiac, Renal, or Liver failure n Elderly n Medication NRC* recommends 1 to 2 ml of water for each kcal of energy expenditure n *NRC= National research council
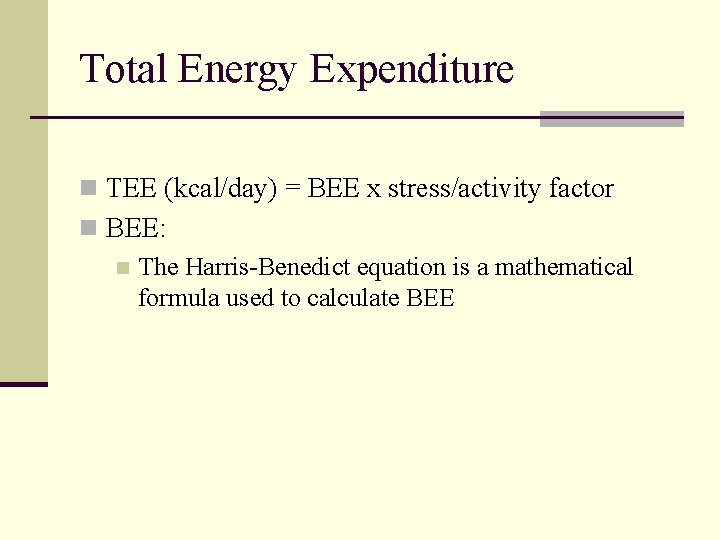
Energy Requirements
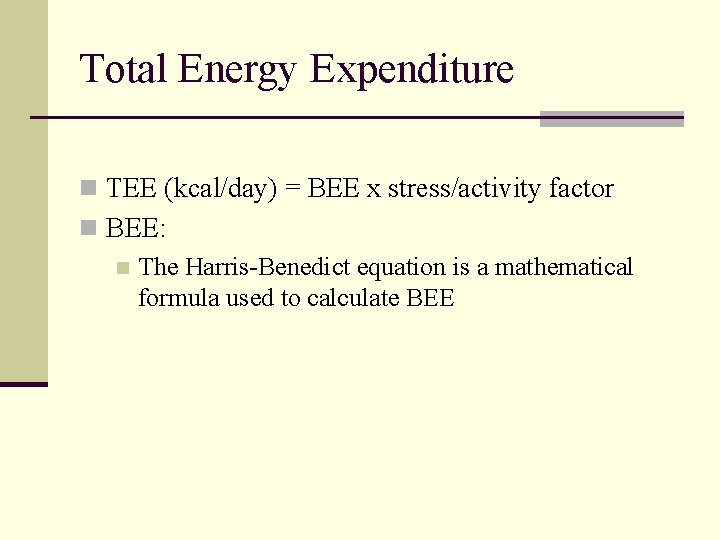
Total Energy Expenditure n TEE (kcal/day) = BEE x stress/activity factor n BEE: n The Harris-Benedict equation is a mathematical formula used to calculate BEE
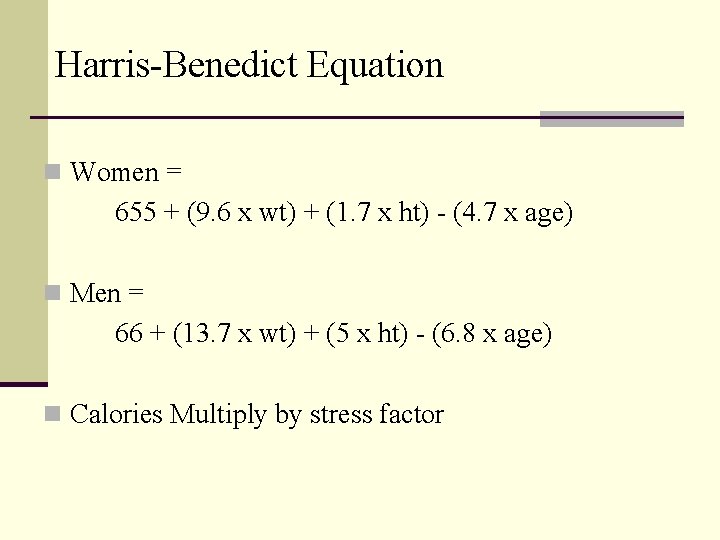
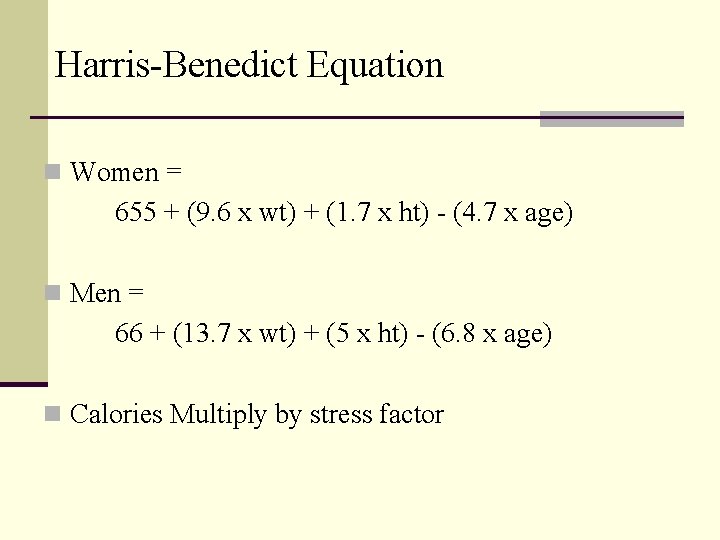
Harris-Benedict Equation n Women = 655 + (9. 6 x wt) + (1. 7 x ht) - (4. 7 x age) n Men = 66 + (13. 7 x wt) + (5 x ht) - (6. 8 x age) n Calories Multiply by stress factor
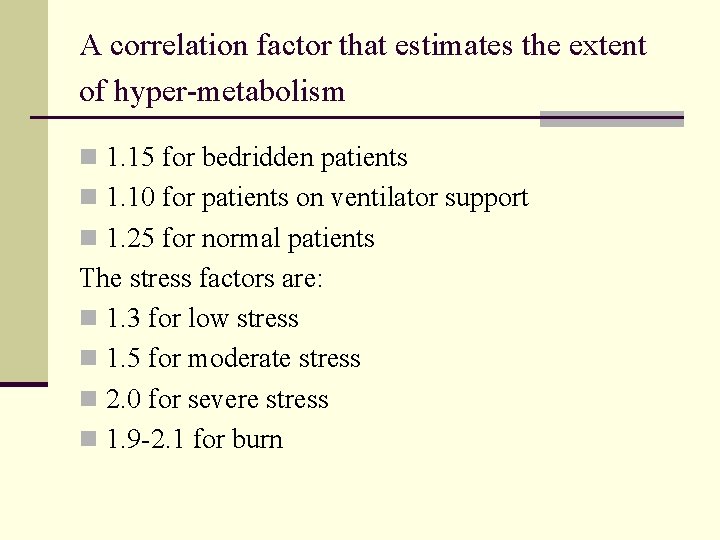
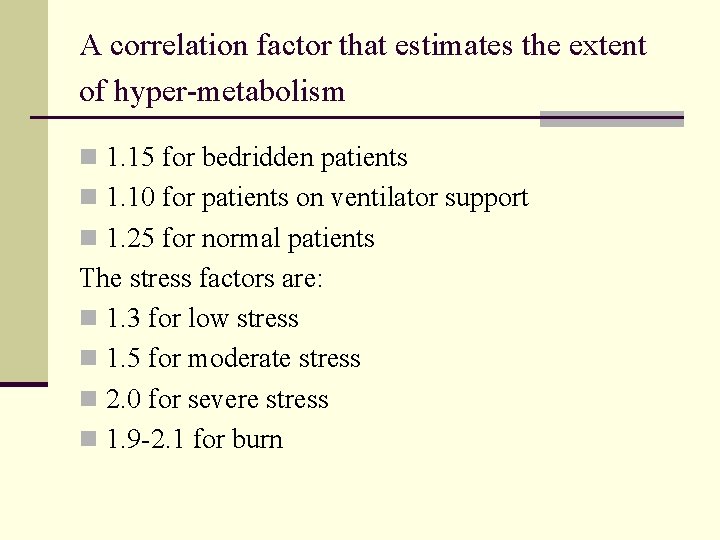
A correlation factor that estimates the extent of hyper-metabolism n 1. 15 for bedridden patients n 1. 10 for patients on ventilator support n 1. 25 for normal patients The stress factors are: n 1. 3 for low stress n 1. 5 for moderate stress n 2. 0 for severe stress n 1. 9 -2. 1 for burn
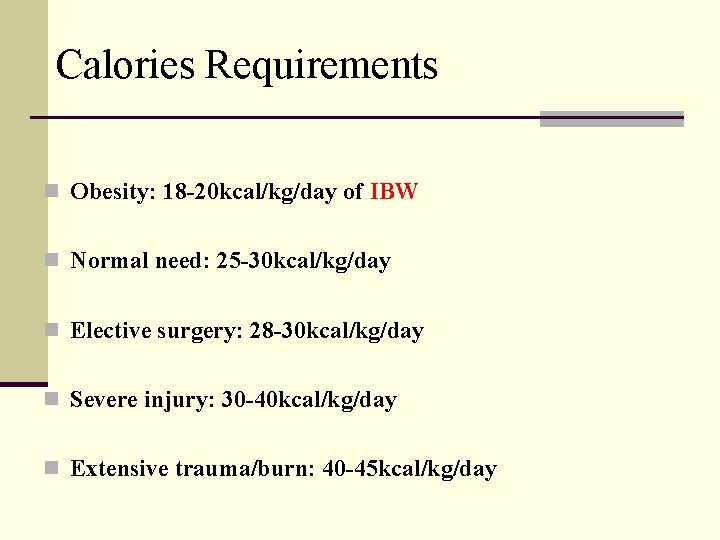
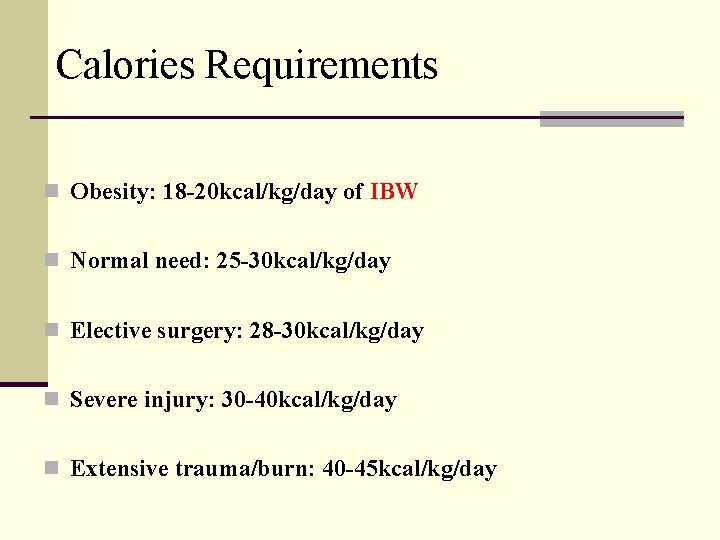
Calories Requirements n Obesity: 18 -20 kcal/kg/day of IBW n Normal need: 25 -30 kcal/kg/day n Elective surgery: 28 -30 kcal/kg/day n Severe injury: 30 -40 kcal/kg/day n Extensive trauma/burn: 40 -45 kcal/kg/day
Carbohydrate n Primary energy substrate n The amount of carbohydrate is determined by n patient’s calorie requirement n glucose oxidation rate n optimal balance of carbohydrate and fat n Maximum oxidized rate 4 - 7 mg/kg/min (adult).
Carbohydrate n Provide from a non nitrogen source n Energy requirement depends on number of factors! n Stress factors, increase calories requirements n 60% - 80% of caloric requirement as glucose
CHO Oxidation Rate n 1 gm = 3. 4 kcal n Kcl ÷ 3. 4 x 1000 ÷ 1440 ÷ wt kg = not more than 5 mg/kg/min e. g. 1700 ÷ 3. 4 x 1000 ÷ 1440 ÷ 70 = 4. 9 mg/kg/min or n 5 mg x 3. 4 ÷ 1000 x wt x 1440 n 5 x 3. 4 ÷ 1000 x 70 x 1440 = ~ 1700 kcal
Carbohydrate Source Starting with: n 200 - 250 gm or 15% dextrose solution started or 2. 5 mg/kg/min n 100 - 150 gm or 10% - 15% dextrose solution in stress & DM n Increase gradually up to 5 mg/kg/min, n Max 7 mg/kg/min
How to Calculate Percentage n Total volume of fluid x 3. 4 x % n e. g. 2000 ml x 3. 4 x 0. 20 = 1360 kcal. Or n 1400 ÷ 3. 4 ÷ 2000 ml = 20% as started then n 1700 ÷ 3. 4 ÷ 2000 ml = 25% full requirement
Protein (Amino Acid) AAs are the vital components of body protein. The primary aim of providing AAs to the body is to prevent: n Disease related catabolic state. n The development of manifest protein deficiency with subsequent impaired wound healing. n Disturbances of blood clotting. n The impairment of hepatic and renal function. n A reduced immuno-competence.
Protein (Amino Acid) n 1 g of protein = 4 Kcal n 1 g of nitrogen is equivalent to 6. 3 g of protein n Non-protein k. cal: nitrogen n 150 -200: 1 (normal patient) Note: In renal and hepatic failure the ratio is 1: 300 -400. Adult dose: Normal patients requirement 0. 8 -1. 0 g/kg max. 2. 5 g/kg depend on patient status Renal failure patient 0. 6 g/kg
Protein (Amino Acid) 12% - 16% of calories as protein Note: n Products containing only essential Aas have been formulated for renal failure. n BCAA (Branched Chain Amino Acids) are used for Hepatic Encephalopathy or in severely stressed patients.
Fat Emulsion n Essential linoleic acid stabilized by egg yolk phospholipids n Delivered in the form of an emulsion n fat emulsion has no isotonicity by itself, glycerol is added to render emulsion isotonic (300 mosm/l). n Concentrated source of calories n Source of essential fatty acids (EFAs) n Substitute for carbohydrate in diabetic & fluid restricted patients

Fat Emulsion n Fat should provide 20 -40% of total calories. n Fat provides a concentrated caloric source. 1 g provide 10 Kcal. n Also fat is an alternative source to dextrose to the patients with compromised respiration since it does produce little CO 2 in its metabolism. While dextrose, when oxidized, it produces CO 2 which must be eliminated via lungs. n Start with 0. 5 g/kg/d gradually up to 1. 5 g/kg/d.

Fat Emulsion n The caloric density § 10% FE is 1. 1 kcal/ml § 20% FE is 2 kcal/ml § 30% FE is 3 kcal/ml n There is LCT, and MCT/LCT products n 1 gm = 9 kcal of fat n Each 1 ml = 2 kcal n Lipid emulsions contain glycerol, so lipid emulsion does not have 9 kcal per gram as it would if it were pure fat. Some use 10 kcal/gm for lipid emulsions. n Propofol: Soybean oil in water emulsion, 1 ml - 1. 112 kcal randa 911@yahoo. com
Fat Emulsion Contraindications n Hyperlipdemia n Acute pancreatitis n Previous history of fat embolism n Severe liver disease n Allergies to egg, soybean oil or safflower oil

Electrolytes n Na, K, CL, Ca, Mg, PO 4, & acetate. n Electrolytes given to maintain normal serum concentration or to correct deficit. n Requirements for specific electrolytes will vary according to the patients disease state randa 911@yahoo. com

Restrict electrolytes n Severe renal dysfunction. n Edema & congestive heart failure. n Patients on corticosteroids. n Metabolic acidosis, acute pancreatitis fistulas, or diarrhea. n Metabolic alkalosis, vomiting. randa 911@yahoo. com
Multivitamins B – Complex: Co-enzyme in absorptive and metabolic processes, transfer of energy from protein, fat and carbohydrate to the cells and their storage as ATP. Ascorbic Acid: Required for collagen synthesis, wound healing. An additional amount may be required in major burns, traumas, and extensive surgeries. Vitamin A: Essential for vision, the production of mucus-secreting epithelial cells and bone growth. Vitamin D: For calcium and phosphate hemeostasis and boncalcification. Vitamin K: For prothrombin generation (Fibrinogen).
Vitamin K n TPN solution does not contain vitamin K and it can predispose patient to deficiency n Vitamin K 10 mg should be given weekly IV or IM if patient is on long-term TPN
Multivitamin and Trace Minerals n Standard form of multivitamin & trace mineral use. n Zinc, copper, manganese & chromium. n Additional of trace mineral required depend on GI losses. n Renal failure patients reduce dose n Biliary stasis disease, avoid copper & manganese randa 911@yahoo. com

Additives n INSULIN: For hyperglycemia when glucose is spilling in urine. n HEPARIN: To promote blood circulation (especially with peripheral TPN) and to prevent thrombophlebitis. n HYDROCORTISONE: To prevent thrombophlebitis in patients receiving peripheral TPN. n ACETATE: For acidosis. n ZINC: Extra amount is needed for patient with severe stress, diarrhea, and ileostomy.
Status of Organic failure n Hypermetabolism n Tachycardia, Tachypnea, Fever, Leucocytosis n Hypercatabolism n Hyperglycemia, Uremia, Hypertriglyceridemia, -NB
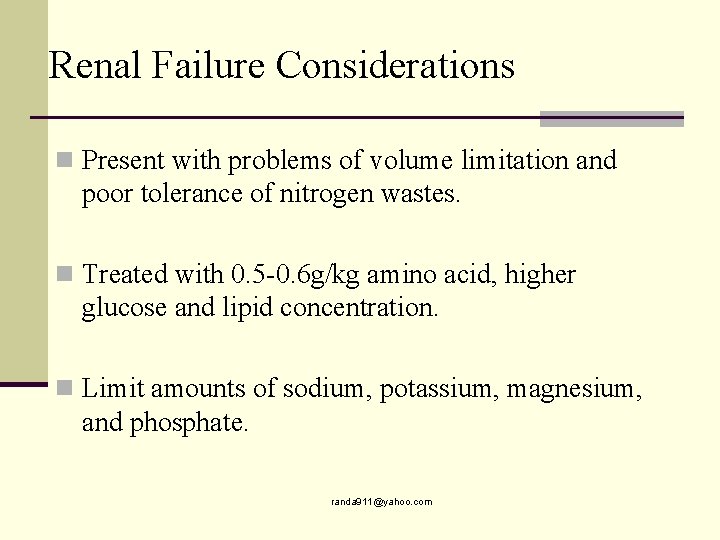
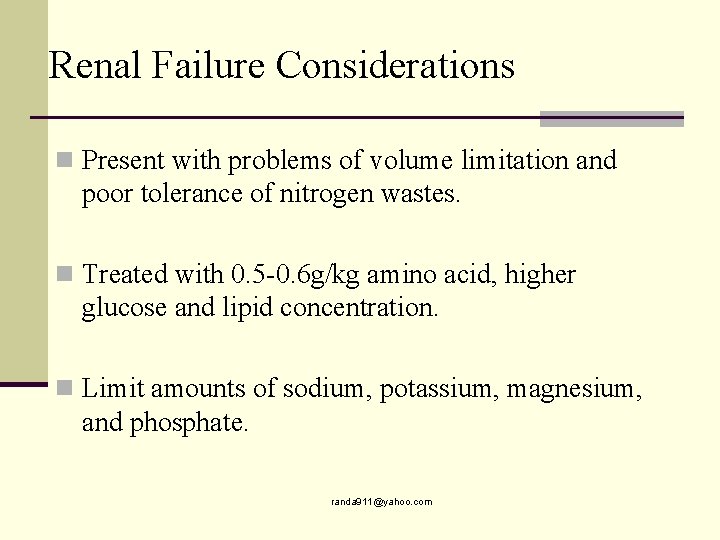
Renal Failure Considerations n Present with problems of volume limitation and poor tolerance of nitrogen wastes. n Treated with 0. 5 -0. 6 g/kg amino acid, higher glucose and lipid concentration. n Limit amounts of sodium, potassium, magnesium, and phosphate. randa 911@yahoo. com
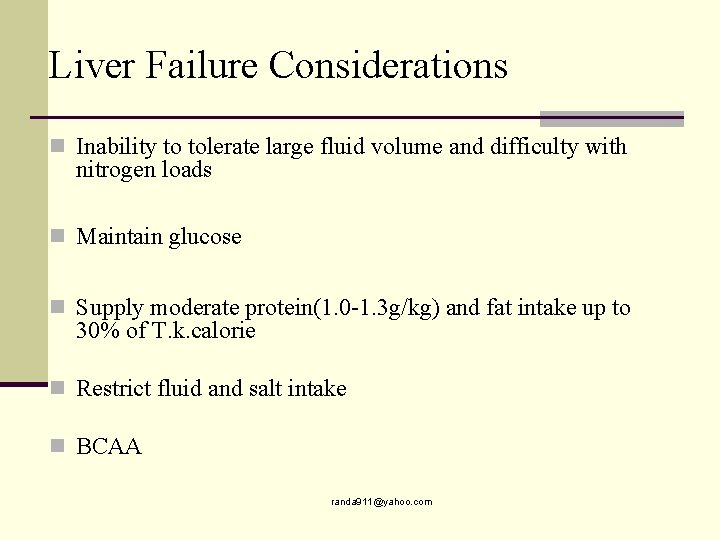
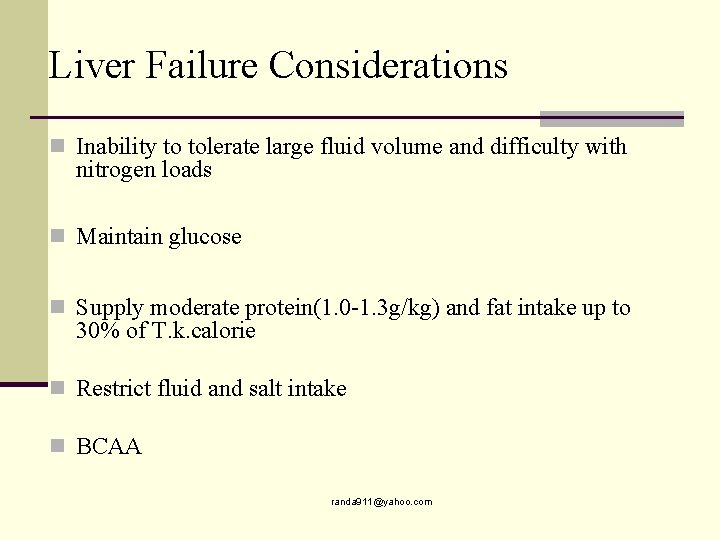
Liver Failure Considerations n Inability to tolerate large fluid volume and difficulty with nitrogen loads n Maintain glucose n Supply moderate protein(1. 0 -1. 3 g/kg) and fat intake up to 30% of T. k. calorie n Restrict fluid and salt intake n BCAA randa 911@yahoo. com

Fluid Restricted Considerations n As pulmonary, cardiac failure, head injuries, and elderly. n Special concentrated TPN solution. n High fat emulsion, low glucose. n Normal protein requirement. n Normal electrolyte. randa 911@yahoo. com

Respiratory Failure n Non-protein calories to nitrogen ration is not a major consideration. n Major problem total calories, either from CHO or fat or both n Protein increases oxygen consumption demands and that is not indicated to reducing protein randa 911@yahoo. com
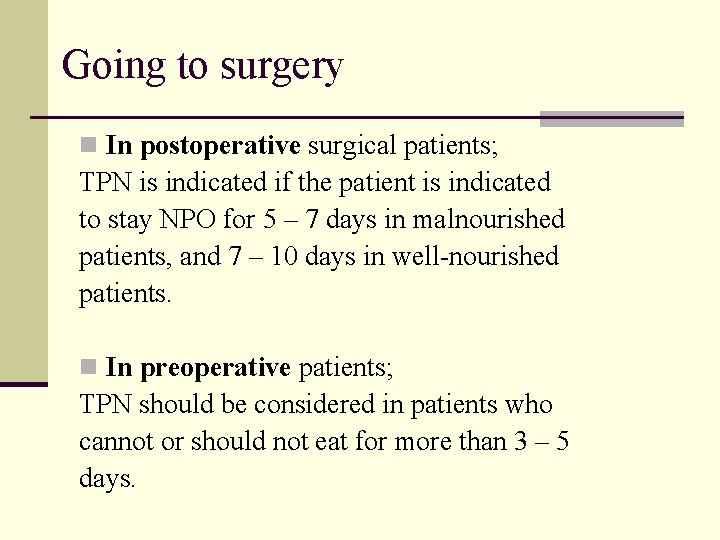
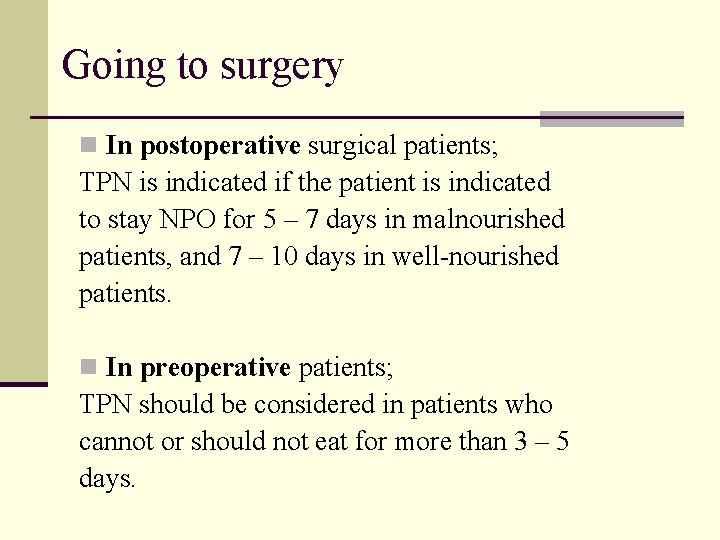
Going to surgery n In postoperative surgical patients; TPN is indicated if the patient is indicated to stay NPO for 5 – 7 days in malnourished patients, and 7 – 10 days in well-nourished patients. n In preoperative patients; TPN should be considered in patients who cannot or should not eat for more than 3 – 5 days.

Practice Guidelines Preoperative n NS should be administered for 7 -14 days to moderately or severely malnourished patients undergoing major GI surgery n PN should NOT be routinely given in the immediate postoperative period to patients undergoing major GI procedures
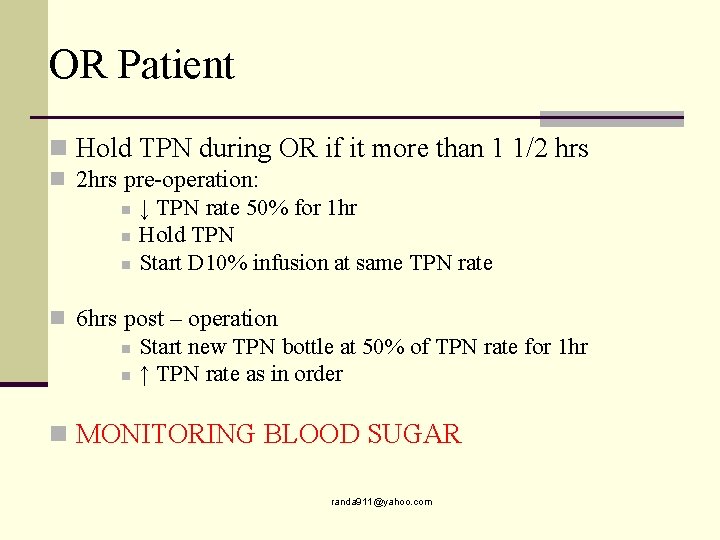
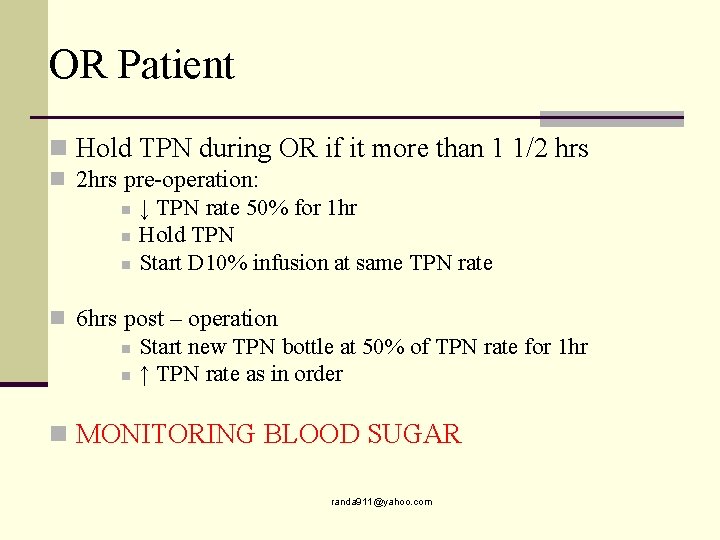
OR Patient n Hold TPN during OR if it more than 1 1/2 hrs n 2 hrs pre-operation: n ↓ TPN rate 50% for 1 hr n Hold TPN n Start D 10% infusion at same TPN rate n 6 hrs post – operation n Start new TPN bottle at 50% of TPN rate for 1 hr n ↑ TPN rate as in order n MONITORING BLOOD SUGAR randa 911@yahoo. com
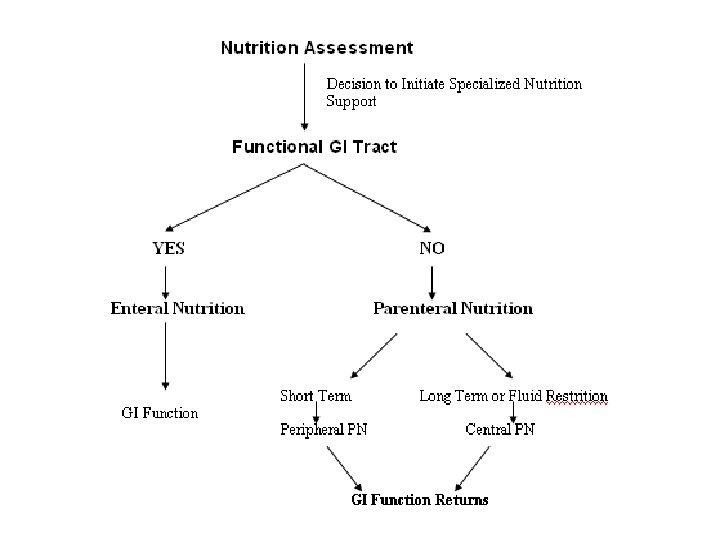
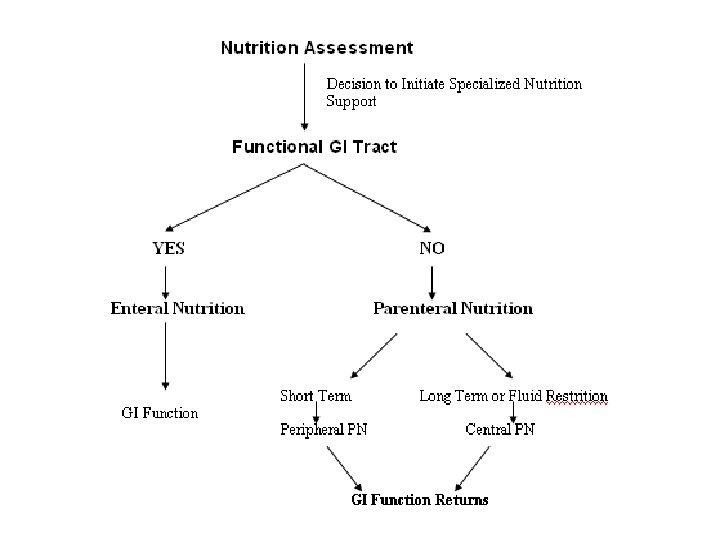
Routes of Nutrition Support
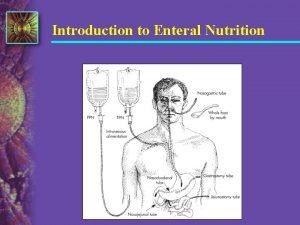
Enteral Nutrition
Enteral Nutrition Indication n Inability to consume or absorb adequate nutrition e. g. who do not eat or receive nutrition support for ≥ 10 -14 days after hospital admission n Functional or partially functional gut e. g. who are unable or not allowed to eat, or partial functional gut
Potential benefits of EN over PN n Nutrients are metabolized and utilized more effectively via the enteral than parenteral route n Gut and liver process EN before their release into systemic circulation n Gut and liver help maintain the homeostasis of the AA pool and skeletal muscle tissue
EN (Immunologic) n Gut integrity is maintained by enteral feeding and prevent the bacterial translocation from the gut and minimize risk of gut related sepsis

Enteral nutrition (EN) Long-term nutrition: n Gastrostomy n Jejunostomy Short-term nutrition: n Nasogastric feeding n Nasoduodenal feeding n Nasojejunal feeding

Benefits of EN n Physiological/metabolic benefits The gut can be used for administration of complex nutrients that cannot be given intravenously e. g. intact protein, peptides, fiber n Safety benefits Safer than PN and less side effects n Cost benefits
Contraindication to EN n Terminal illness n Short bowel n Obstruction n GI bleeding n Vomiting and diarrhea n Fistulas n GI ischemia n Illues n GI inflammation n A. pancreatitis
Enteral Nutrition Complications n Mechanical complication n During placement of feeding tube § Airway injury, infection, ↑ICP n n Presence of a feeding tube Tube clogging Declogging methods Aspiration n GI complication n Gastroesophageal reflux duodenal gastric reflux Diarrhea Metabolic complication
Enteral Nutrition Complications n Metabolic complication n Hyperglycemia Electrolyte and mineral deficiences Refeeding syndrome
Total Parentral Nutrition

Total Parenteral Nutrition Indication n When normal oral feeding is not possible. e. g. : Chron’s disease, gastric & esophageal carcinoma, paralytic ileus, generalized peronitis, GI. obstruction, intractable vomiting. n When food is incompletely absorbed. e. g. : Major burns, multiple injuries, radiation therapy, ulcerative colitis, chemotherapy treatment, short bowel syndrome. n When food intake is undesirable, in case it is prudent to rest the bowel. e. g. : Post GIT surgery, chronic inflammatory diseases, intractable diarrhea.
Total Parenteral Nutrition Indication n In patients who are able to ingest food, but refuse to do so. e. g. : Geriatric post-operative patients, adolescents with anorexia nervosa, some psychiatric patients with prolonged depression. n In patients who, as a consequence of their illness are going to be, or have been NPO for 5 – 7 days.
Administration

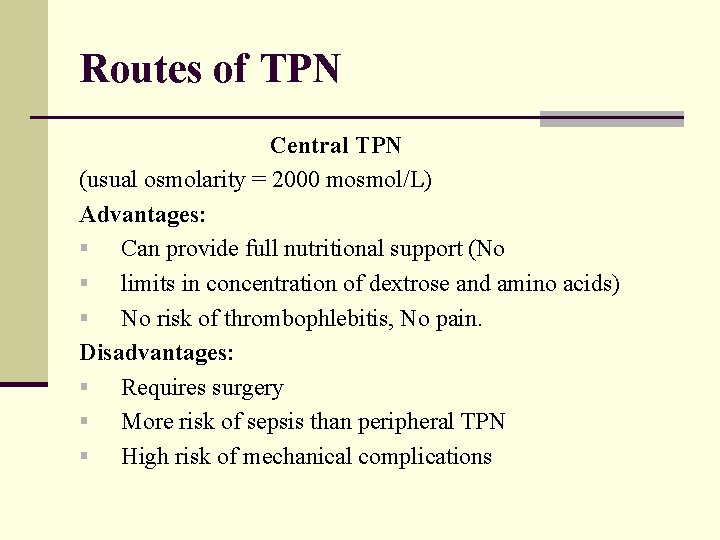
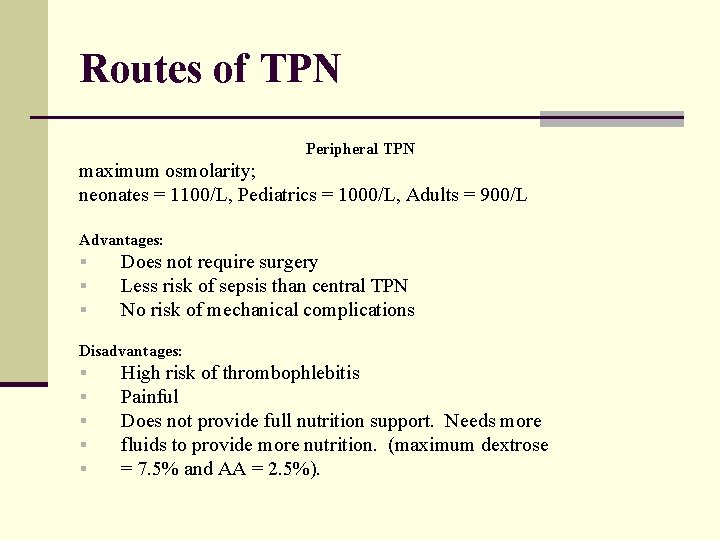
Parenteral Nutrition n n n Central Nutrition Subclavian line Long period Hyperosmolar solution Full requirement Minimum volume Expensive More side effect Peripheral nutrition n Peripheral line n Short period < 14 days n Low osmolality < 900 m. Osm/L n Min. requirement n Large volume n Thrombophlebitis
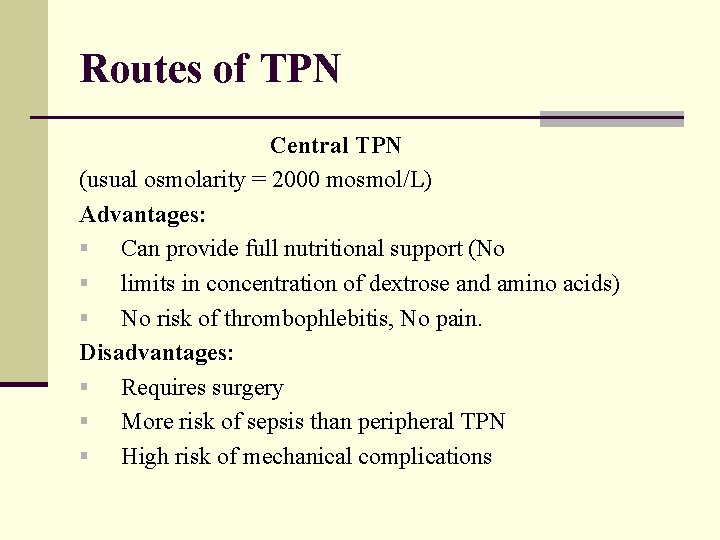
Routes of TPN Central TPN (usual osmolarity = 2000 mosmol/L) Advantages: § Can provide full nutritional support (No § limits in concentration of dextrose and amino acids) § No risk of thrombophlebitis, No pain. Disadvantages: § Requires surgery § More risk of sepsis than peripheral TPN § High risk of mechanical complications
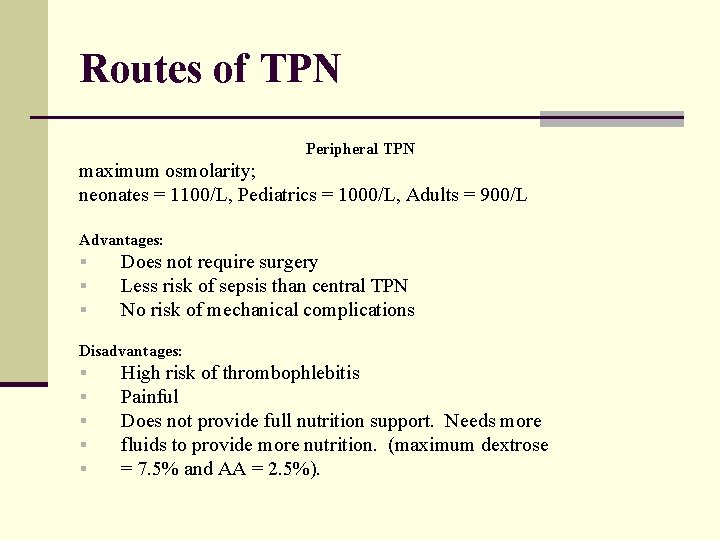
Routes of TPN Peripheral TPN maximum osmolarity; neonates = 1100/L, Pediatrics = 1000/L, Adults = 900/L Advantages: § § § Does not require surgery Less risk of sepsis than central TPN No risk of mechanical complications Disadvantages: § § § High risk of thrombophlebitis Painful Does not provide full nutrition support. Needs more fluids to provide more nutrition. (maximum dextrose = 7. 5% and AA = 2. 5%).
Note PPN can infuse through central line but central TPN can NOT infuse through the peripheral line

Calculating the Osmolarity of a Parenteral Nutrition Solution Multiply the grams of dextrose per liter by 5. Example: 100 g of dextrose x 5 = 500 m. Osm/L Multiply the grams of protein per liter by 10. Example: 30 g of protein x 10 = 300 m. Osm/L Multiply the (m. Eq per L sodium + potassium + calcium + magnesium) X 2 Example: 80 X 2 = 160 Total osmolarity = 500 + 300 + 160 = 960 m. Osm/L randa 911@yahoo. com
Monitoring
Monitoring n Avoid overfeeding n Avoid respiratory problem n Promote nitrogen retention n Triglyceride clearance n Fluid and electrolyte n Weight n Liver function randa 911@yahoo. com
Monitoring for Complications n Malnourished patients at risk for refeeding syndrome should have serum phosphorus, magnesium, potassium, and glucose levels monitored closely n In patients with diabetes or risk factors for glucose intolerance, insulin infusion should be initiated with a low dextrose infusion rate and blood and urine glucose monitored closely. n Blood glucose should be monitored frequently upon initiation, any change in insulin dose, and until measurements are stable. randa 911@yahoo. com
Monitoring for Complications n Serum electrolytes (sodium, potassium, chloride, and bicarbonate) should be monitored frequently until measurements are stable. n Patients receiving intravenous fat emulsions should have serum triglyceride levels monitored until stable and when changes are made in the amount of fat administered. n Liver function tests should be monitored periodically in patients receiving PN. randa 911@yahoo. com
Complications of TPN

Complication n Mechanical: occlusion, catheter removal, improper rate, thromboses, pneumothorax. n Infection: catheter related n Metabolic: re-feeding syndrome, hyperglycemia, fluid & electrolyte disturbance (cont. . ) randa 911@yahoo. com

Complication n Organic system: n n hepatobiliary complication respiratory cardiovascular renal randa 911@yahoo. com
Transitional Feeding n Maintain full PN support until pt is tolerating 1/3 of needs via enteral route n Decrease TPN by 50% and continue to taper as the enteral feeding is advanced to total n TPN can reduce appetite if >25% of calorie needs are met via PN n TPN can be tapered when pt is consuming greater than 500 calories/d and d-c’d when meeting 60% of goal n TPN can be rapidly d-c’d if pt is receiving enteral feeding in amount great enough to maintain blood glucose levels randa 911@yahoo. com

Defense Against NS Complications n Select appropriate patients to appropriate nutrition n Aseptic technique n Do not overfeed n n n Maintain glycemic control <150 -170 mg/dl Limit lipids to 1 gm/kg and monitor TG levels Adjust protein based on metabolic demand organ function n Monitor fluid/electrolyte/mineral status n Provide standard vitamin and trace element preps daily randa 911@yahoo. com
Thank you
 Care of critically ill surgical patient
Care of critically ill surgical patient Durodgorlik ustaxonasida
Durodgorlik ustaxonasida Randa tower
Randa tower Randa stringer
Randa stringer Randa login
Randa login Randa tower
Randa tower Randa sawires
Randa sawires South carolina teacher evaluation system
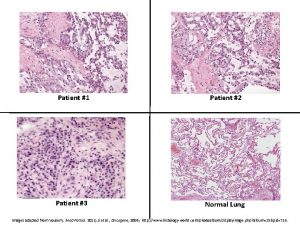
South carolina teacher evaluation system Patient 2 patient
Patient 2 patient Enteral parenteral beslenme
Enteral parenteral beslenme Patient support manager
Patient support manager Signal words example
Signal words example Hươu thường đẻ mỗi lứa mấy con
Hươu thường đẻ mỗi lứa mấy con đại từ thay thế
đại từ thay thế Quá trình desamine hóa có thể tạo ra
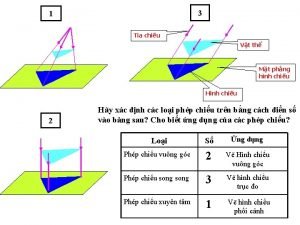
Quá trình desamine hóa có thể tạo ra Vẽ hình chiếu vuông góc của vật thể sau
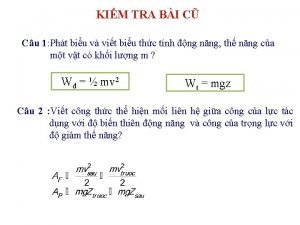
Vẽ hình chiếu vuông góc của vật thể sau Cong thức tính động năng
Cong thức tính động năng Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Dot
Dot Lời thề hippocrates
Lời thề hippocrates Bổ thể
Bổ thể Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể độ dài liên kết
độ dài liên kết Các môn thể thao bắt đầu bằng tiếng chạy
Các môn thể thao bắt đầu bằng tiếng chạy Sự nuôi và dạy con của hổ
Sự nuôi và dạy con của hổ điện thế nghỉ
điện thế nghỉ Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Chó sói
Chó sói Các số nguyên tố là gì
Các số nguyên tố là gì Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Tia chieu sa te
Tia chieu sa te Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Một số thể thơ truyền thống
Một số thể thơ truyền thống Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Hệ hô hấp
Hệ hô hấp Tư thế ngồi viết
Tư thế ngồi viết Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Tư thế worm breton là gì
Tư thế worm breton là gì ưu thế lai là gì
ưu thế lai là gì Thẻ vin
Thẻ vin Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Cái miệng bé xinh thế chỉ nói điều hay thôi
Cái miệng bé xinh thế chỉ nói điều hay thôi Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Diễn thế sinh thái là
Diễn thế sinh thái là Tư thế ngồi viết
Tư thế ngồi viết V cc cc
V cc cc Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 Chúa yêu trần thế
Chúa yêu trần thế Qrc surgical
Qrc surgical Surgical plume evacuator tool
Surgical plume evacuator tool Chapter 22 surgical asepsis
Chapter 22 surgical asepsis Corrective phase periodontal therapy
Corrective phase periodontal therapy Acute specific surgical infection
Acute specific surgical infection Joint hospital surgical grand round
Joint hospital surgical grand round Surgical metabolism
Surgical metabolism What part of the surgical gown is considered sterile
What part of the surgical gown is considered sterile Voluntary surgical contraception
Voluntary surgical contraception Surgical hand scrub products
Surgical hand scrub products Color coding of sutures
Color coding of sutures Conclusion of oral medication
Conclusion of oral medication A nurse floats to a busy surgical unit
A nurse floats to a busy surgical unit Cpt surgical package
Cpt surgical package A newly admitted patient was found wandering
A newly admitted patient was found wandering Grasping and clamping instruments
Grasping and clamping instruments Cloroprep
Cloroprep Surgical audit cycle
Surgical audit cycle Surgical bandage types
Surgical bandage types Medical asepsis hand washing
Medical asepsis hand washing Deltoid tuberosity
Deltoid tuberosity Weilaner
Weilaner Surgical prep
Surgical prep Managing surgical smoke
Managing surgical smoke Clasis a suffix denoting break, fracture
Clasis a suffix denoting break, fracture Surgical planning laboratory
Surgical planning laboratory Difference between medical and surgical asepsis
Difference between medical and surgical asepsis Uterine prolapse treatment non surgical
Uterine prolapse treatment non surgical Gordochom precio
Gordochom precio Surgical bandage types
Surgical bandage types Maintenance of surgical instruments
Maintenance of surgical instruments Imaging at lafayette surgical specialty hospital
Imaging at lafayette surgical specialty hospital Svv cardiac
Svv cardiac Aseptic technique clipart
Aseptic technique clipart Surgical staples
Surgical staples Inductive vs deductive learning
Inductive vs deductive learning Horizontal position patient
Horizontal position patient