DEVELOPMENTAL DYSPLASIA OF THE HIPS Cheryl Parker PAC
- Slides: 16
DEVELOPMENTAL DYSPLASIA OF THE HIPS Cheryl Parker PA-C Department of Orthopedics and Sports Medicine
DEVELOPMENTAL DYSPLASIA OF THE HIP DDH formerly known as CDH A generic term describing abnormalities of the hip that may be congenital, or occur during infancy. Ranges from mild to severe. Abnormal relationship between the femoral head and acetabulum § Dysplasia – shallow/underdeveloped acetabulum § Subluxed – hip that is not reduced
DEVELOPMENTAL DYSPLASIA OF THE HIP Incidence: 1. 5/1000 live births – untreated leads to degenerative arthritis in adulthood § Dysplasia: 1 per 100 § Frank Dislocation: 1. 5 per 1, 000 Most common § (+) FHx § Breech presentation § Girls 4: 1 § Children with joint laxity § L > R hip
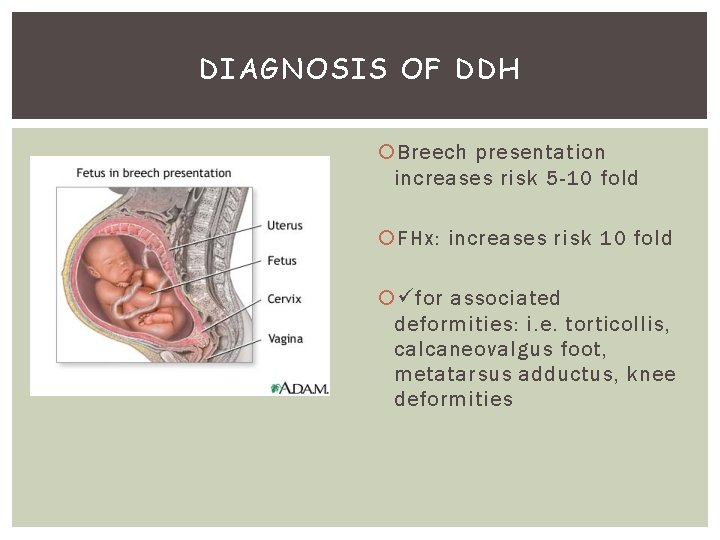
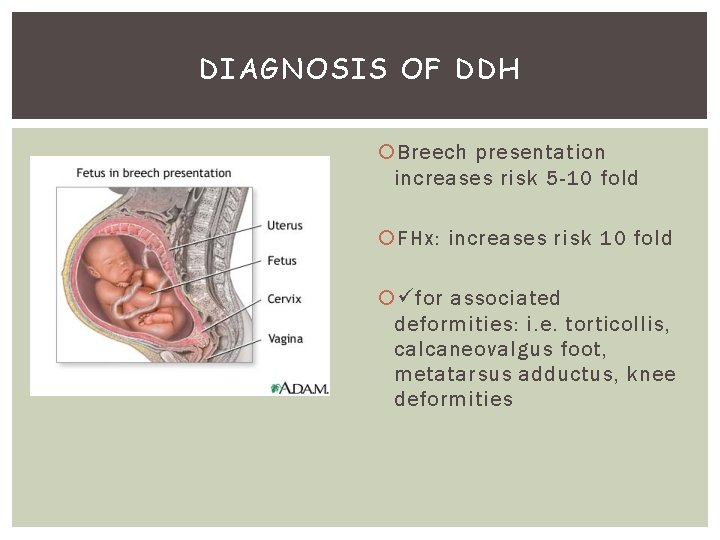
DIAGNOSIS OF DDH Breech presentation increases risk 5 -10 fold FHx: increases risk 10 fold for associated deformities: i. e. torticollis, calcaneovalgus foot, metatarsus adductus, knee deformities
DIAGNOSIS OF DDH Early Diagnosis is critical to successful treatment Signs change with the age of the child, therefore repeat hip exams at each well-child visit Check for asymmetry of legs for pain – DDH is NOT painful – seek other cause
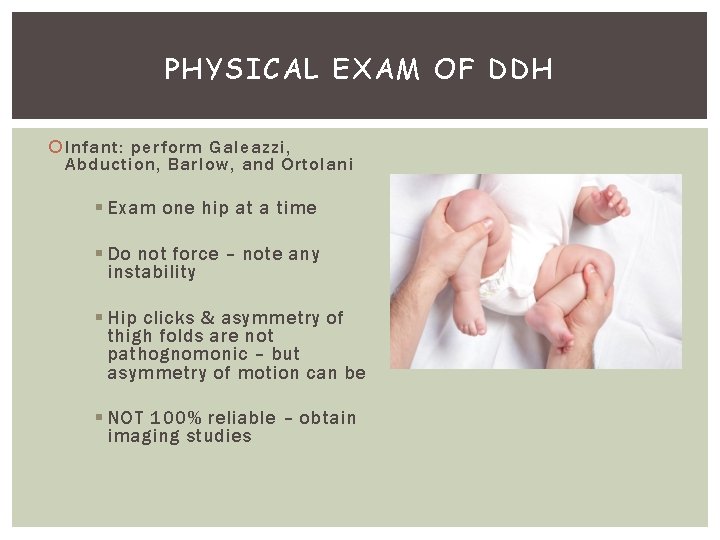
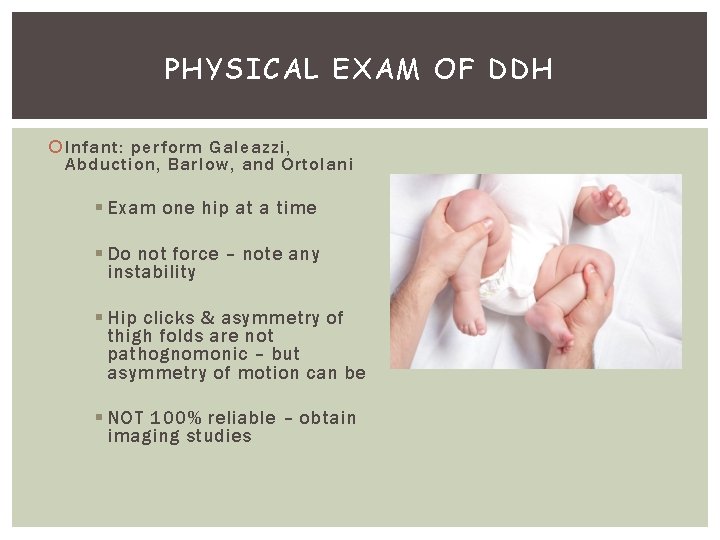
PHYSICAL EXAM OF DDH Infant: perform Galeazzi, Abduction, Barlow, and Ortolani § Exam one hip at a time § Do not force – note any instability § Hip clicks & asymmetry of thigh folds are not pathognomonic – but asymmetry of motion can be § NOT 100% reliable – obtain imaging studies
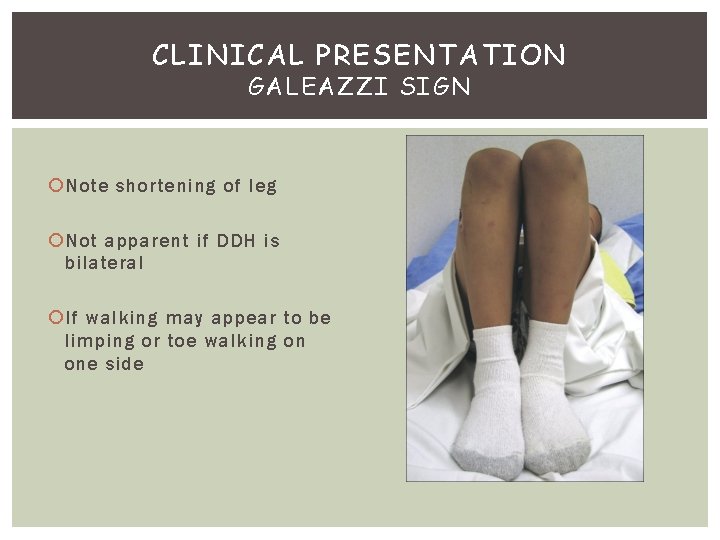
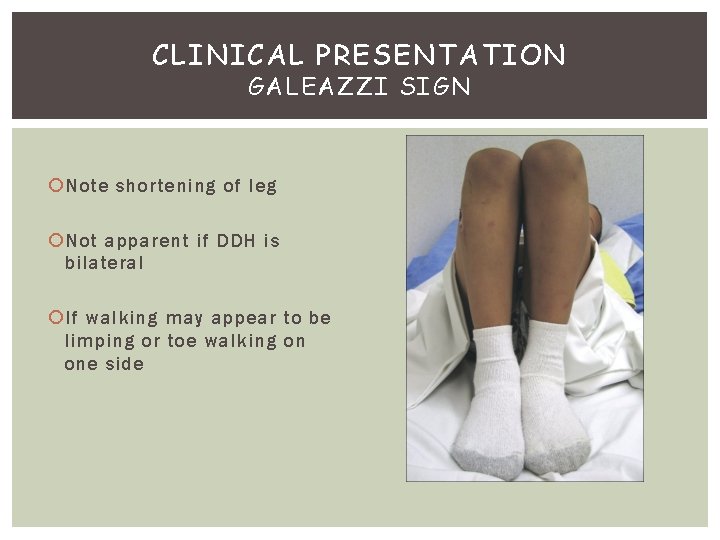
CLINICAL PRESENTATION GALEAZZI SIGN Note shortening of leg Not apparent if DDH is bilateral If walking may appear to be limping or toe walking on one side
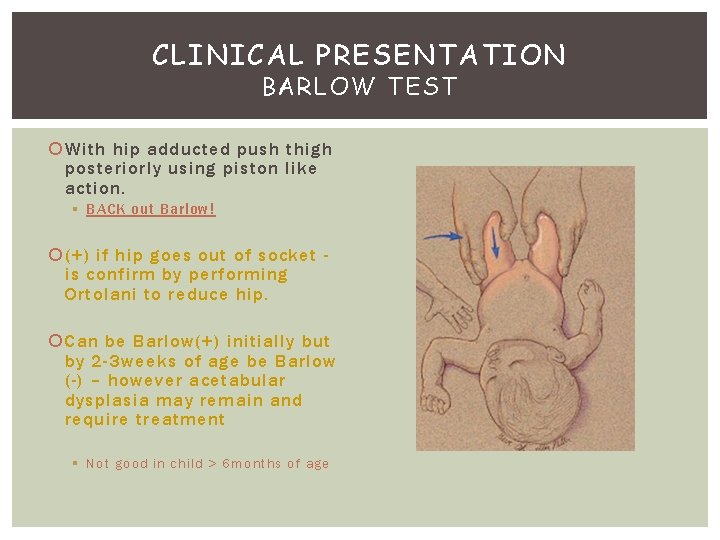
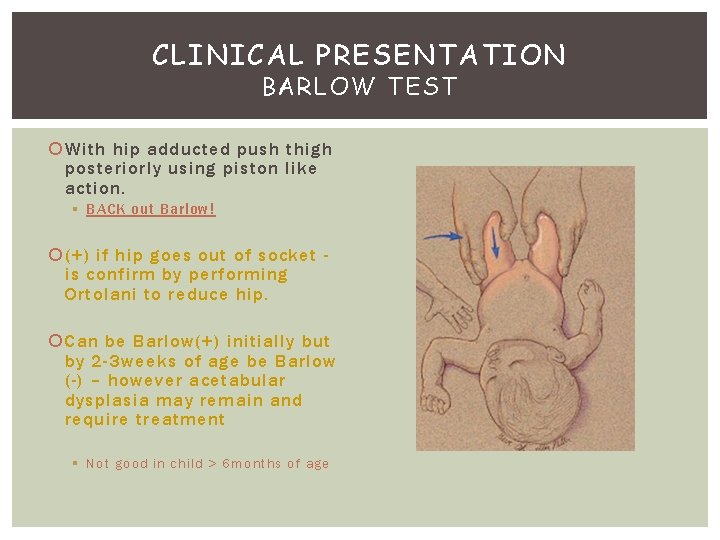
CLINICAL PRESENTATION BARLOW TEST With hip adducted push thigh posteriorly using piston like action. § BACK out Barlow! (+) if hip goes out of socket is confirm by performing Ortolani to reduce hip. Can be Barlow(+) initially but by 2 -3 weeks of age be Barlow (-) – however acetabular dysplasia may remain and require treatment § Not good in child > 6 months of age
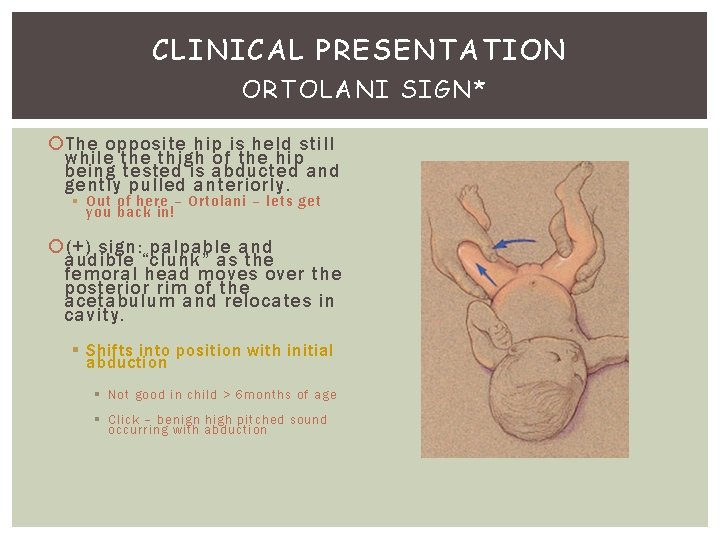
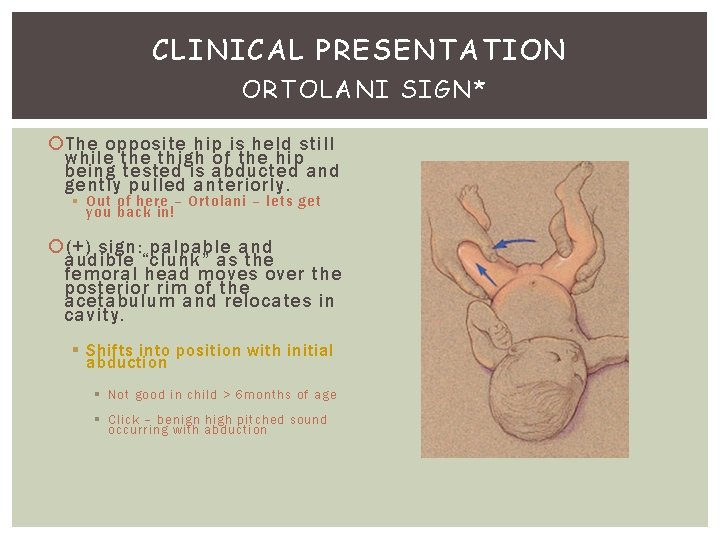
CLINICAL PRESENTATION ORTOLANI SIGN* The opposite hip is held still while thigh of the hip being tested is abducted and gently pulled anteriorly. § Out of here – Ortolani – lets get you back in! (+) sign: palpable and audible “clunk” as the femoral head moves over the posterior rim of the acetabulum and relocates in cavity. § Shifts into position with initial abduction § Not good in child > 6 months of age § Click – benign high pitched sound occurring with abduction
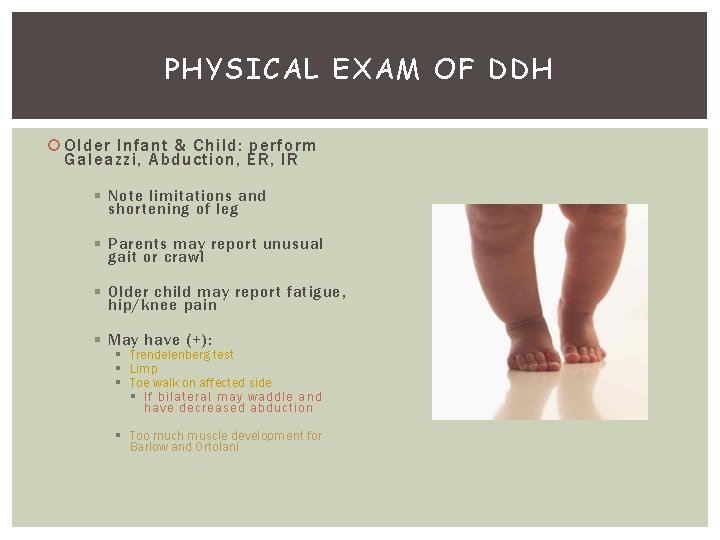
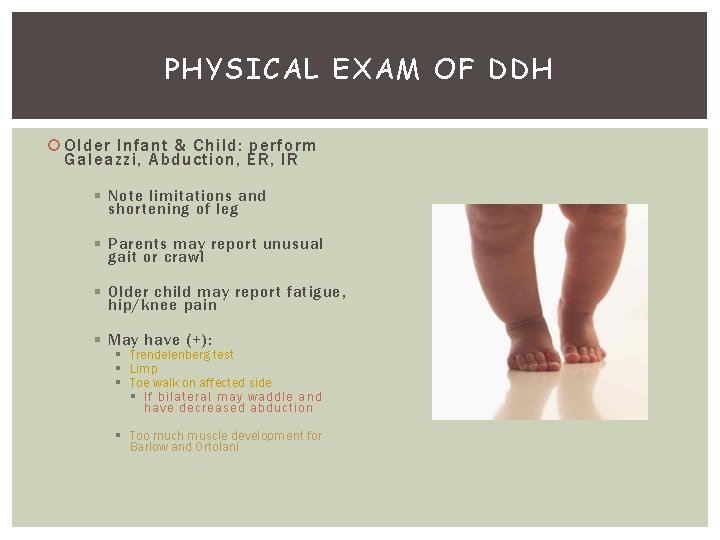
PHYSICAL EXAM OF DDH Older Infant & Child: perform Galeazzi, Abduction, ER, IR § Note limitations and shortening of leg § Parents may report unusual gait or crawl § Older child may report fatigue, hip/knee pain § May have (+): § Trendelenberg test § Limp § Toe walk on affected side § If bilateral may waddle and have decreased abduction § Too much muscle development for Barlow and Ortolani
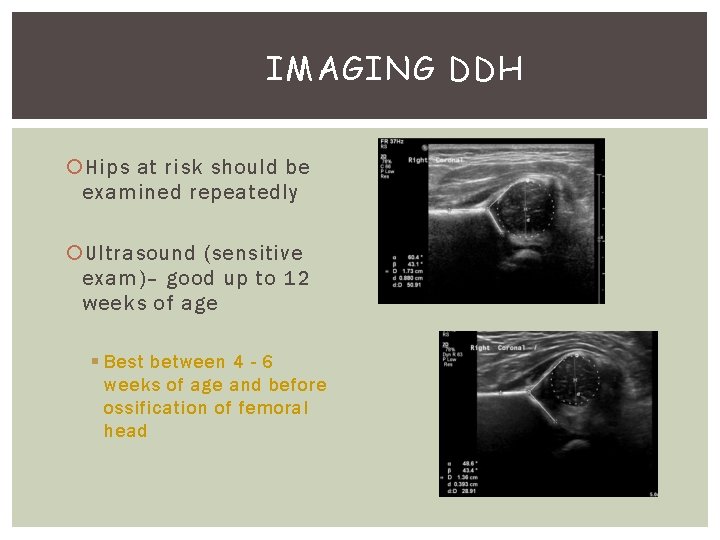
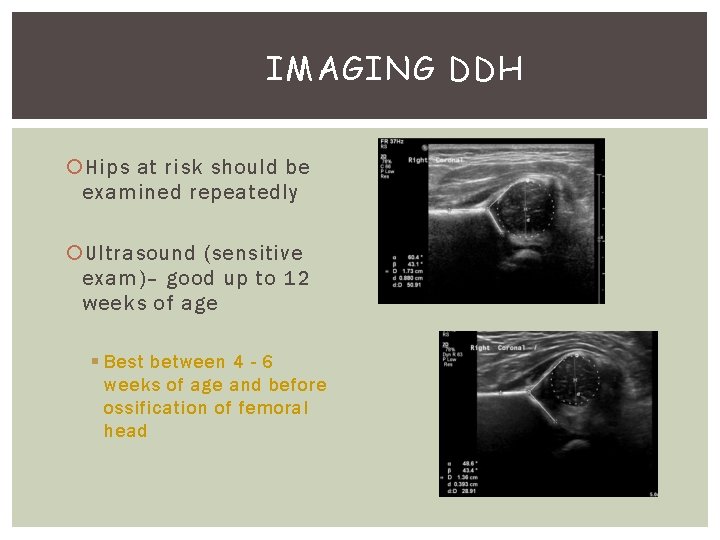
IMAGING DDH Hips at risk should be examined repeatedly Ultrasound (sensitive exam)– good up to 12 weeks of age § Best between 4 - 6 weeks of age and before ossification of femoral head
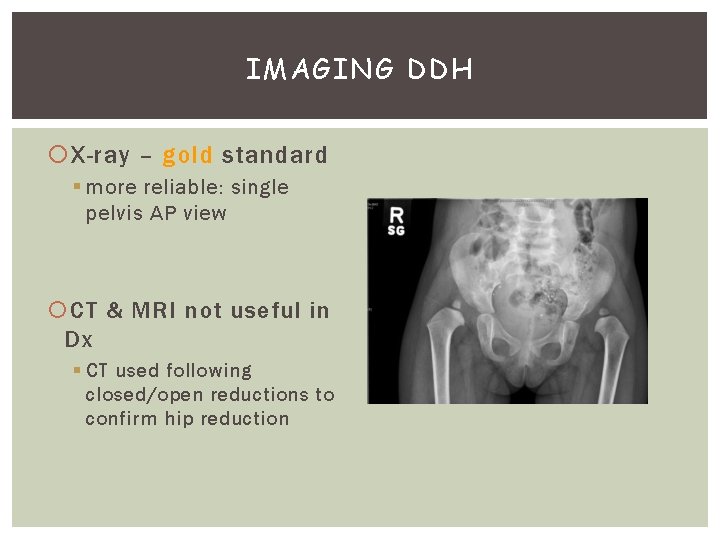
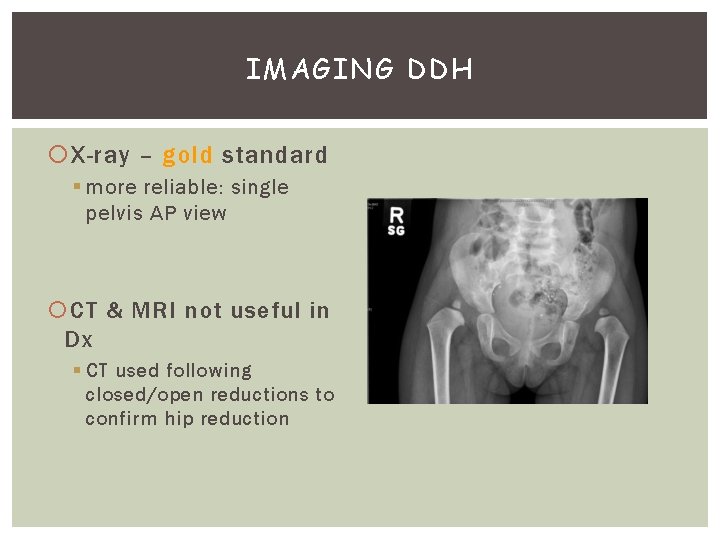
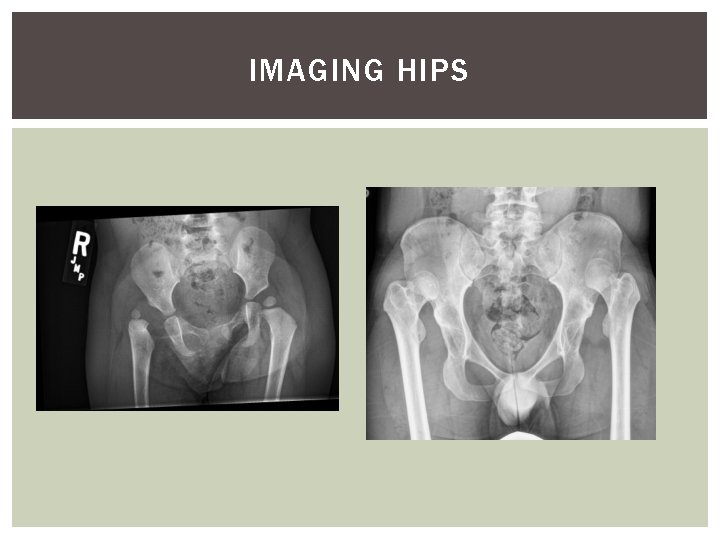
IMAGING DDH X-ray – gold standard § more reliable: single pelvis AP view CT & MRI not useful in Dx § CT used following closed/open reductions to confirm hip reduction
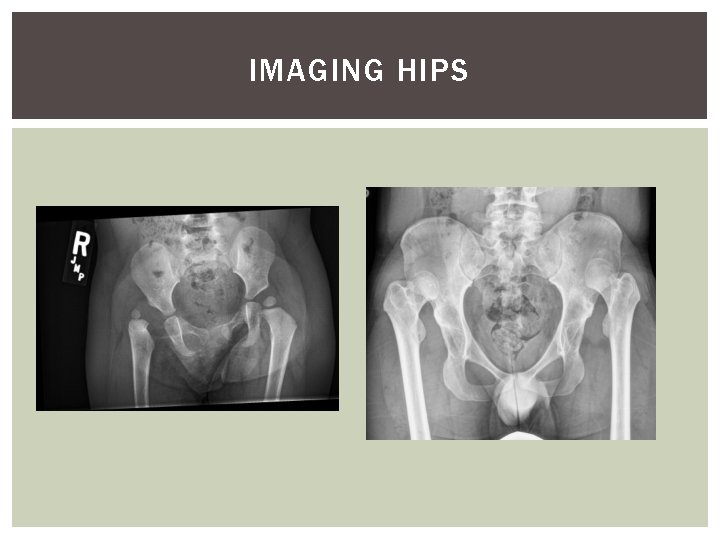
IMAGING HIPS
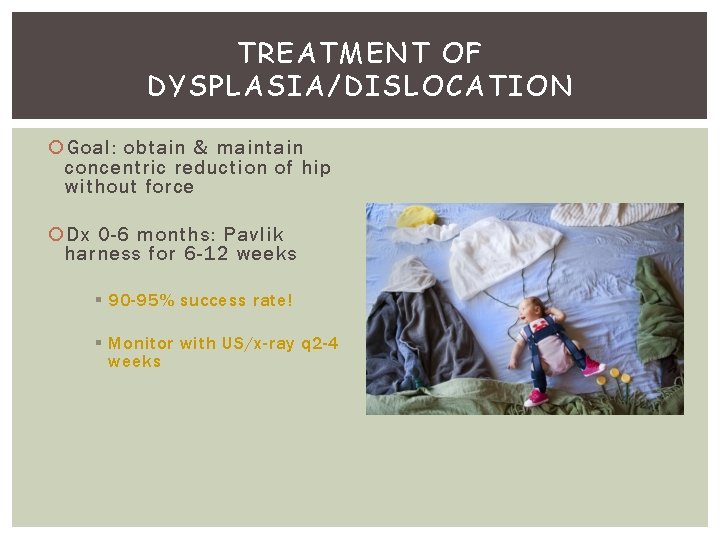
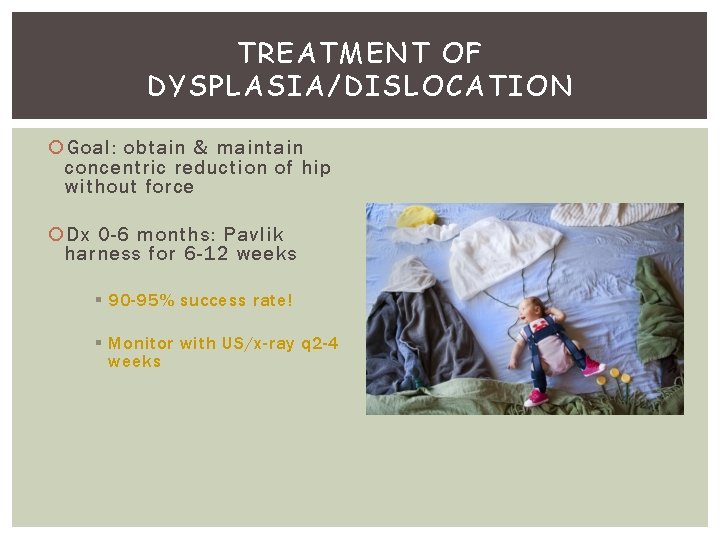
TREATMENT OF DYSPLASIA/DISLOCATION Goal: obtain & maintain concentric reduction of hip without force Dx 0 -6 months: Pavlik harness for 6 -12 weeks § 90 -95% success rate! § Monitor with US/x-ray q 2 -4 weeks
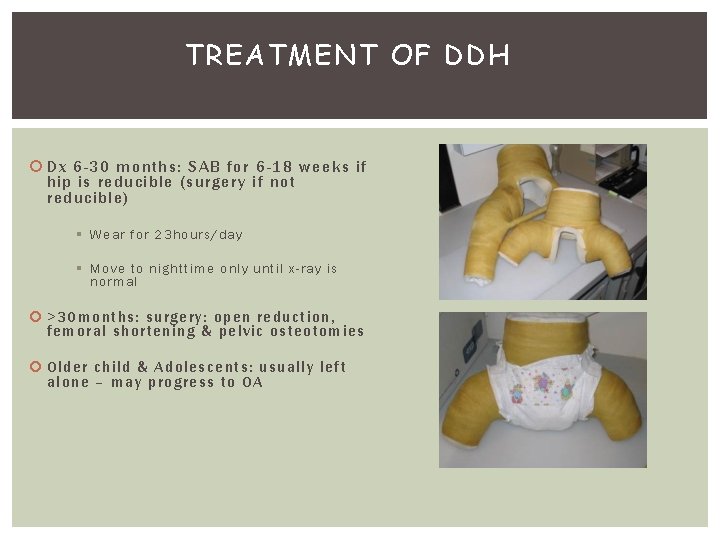
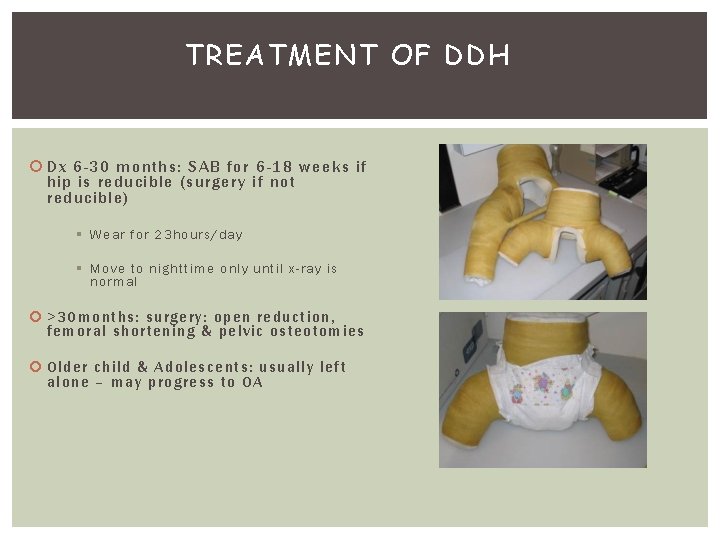
TREATMENT OF DDH Dx 6 -30 months: SAB for 6 -18 weeks if hip is reducible (surgery if not reducible) § Wear for 23 hours/day § Move to nighttime only until x-ray is normal >30 months : surgery: open reduction, femora l sho rtening & pelvic osteotomies Old er child & Adolescents: usu ally left alon e – ma y p rogress to OA
THE END – QUESTIONS? ?
 Piston test for hip dislocation
Piston test for hip dislocation Renal dysplasia
Renal dysplasia Supernumere diş
Supernumere diş Ppt
Ppt Hutchinson triad
Hutchinson triad Periapical
Periapical Hip and elbow dysplasia
Hip and elbow dysplasia Hip usg
Hip usg Epidermal dysplasia verruciformis
Epidermal dysplasia verruciformis Dr ajit nambiar
Dr ajit nambiar Dog kidney
Dog kidney Osmf differential diagnosis
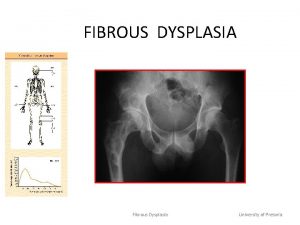
Osmf differential diagnosis Ground glass appearance fibrous dysplasia
Ground glass appearance fibrous dysplasia Norberg szög
Norberg szög Akondroplazi
Akondroplazi Epithelial dysplasia oral
Epithelial dysplasia oral Bowel cancer stages
Bowel cancer stages