Developmental dysplasia of the hip DDH Definition Dysplasia

![Graf classification of DDH [ simplified] class Alpha angle Beta angle description 1 Graf classification of DDH [ simplified] class Alpha angle Beta angle description 1](https://slidetodoc.com/presentation_image/30c2513983aadfc80f250d898f2fbd78/image-31.jpg)





- Slides: 58
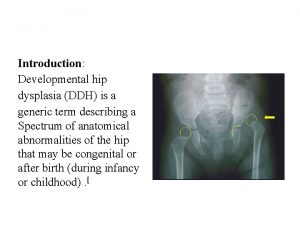
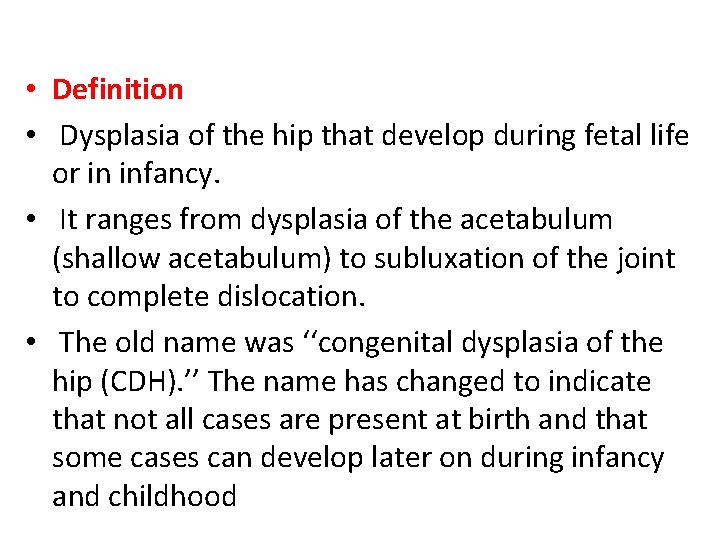
Developmental dysplasia of the hip (DDH)
• Definition • Dysplasia of the hip that develop during fetal life or in infancy. • It ranges from dysplasia of the acetabulum (shallow acetabulum) to subluxation of the joint to complete dislocation. • The old name was ‘‘congenital dysplasia of the hip (CDH). ’’ The name has changed to indicate that not all cases are present at birth and that some cases can develop later on during infancy and childhood
Types: DDH is classified into two major groups : Typical and teratologic. Typical DDH occurs in otherwise normal patients or those without defined syndromes or genetic conditions. • Teratologic hip dislocations usually have identifiable causes such as arthrogyposis or a genetic syndrome and occur before birth. • •
Developmental Dysplasia of the Hip 1. Complete hip dislocation. 2. Partial hip subluxation. 3. Hip dysplasia (incomplete development).
Incidence • Most newborn screening studies suggest that some degree of hip instability can be detected in 1/100 to 1/250 babies, actual dislocated or dislocatable hips are much less common, being found in 1 -1. 5 of 1000 live births. • There is marked geographic and racial variation in the incidence of DDH. • More inidence of DDH IN Sweden, Yugoslavia and Canada.
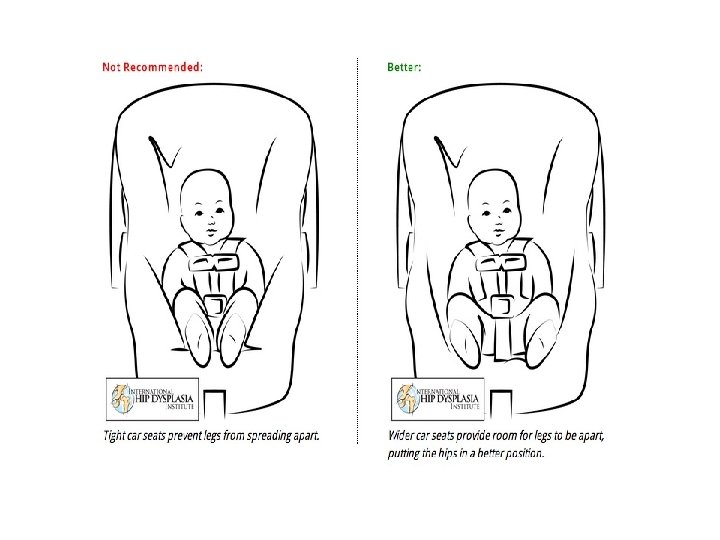
• Children in Native American • African and Asian caregivers and Eastern European have traditionally carried cultures, which have a babies against their bodies in a relatively high incidence of shawl so that a child ’s hips are DDH, have historically been flexed, abducted, and free to swaddled in confining move. clothes that bring their hips • This keeps the hips in the into extension. optimal position for stability • This position increases the and for dynamic molding of tension of the psoas muscle the developing acetabulum by -tendon unit and might the cartilaginous femoral head. predispose the hips to displace and eventually dislocate laterally and superiorly.

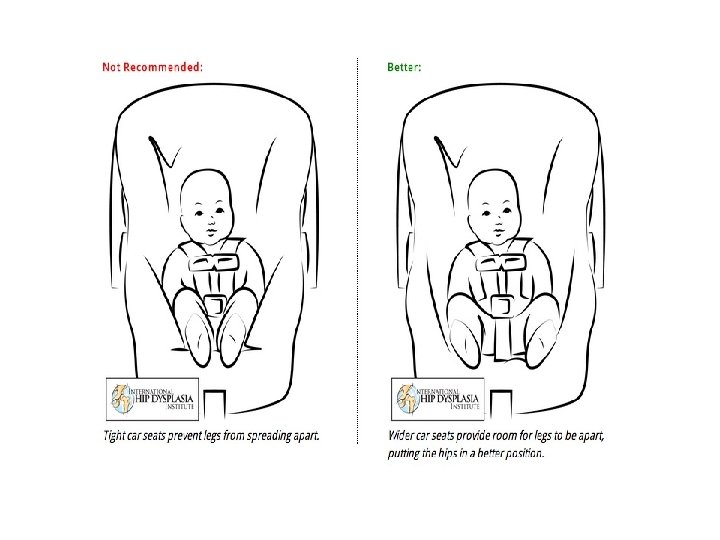
Recommended Not recommended
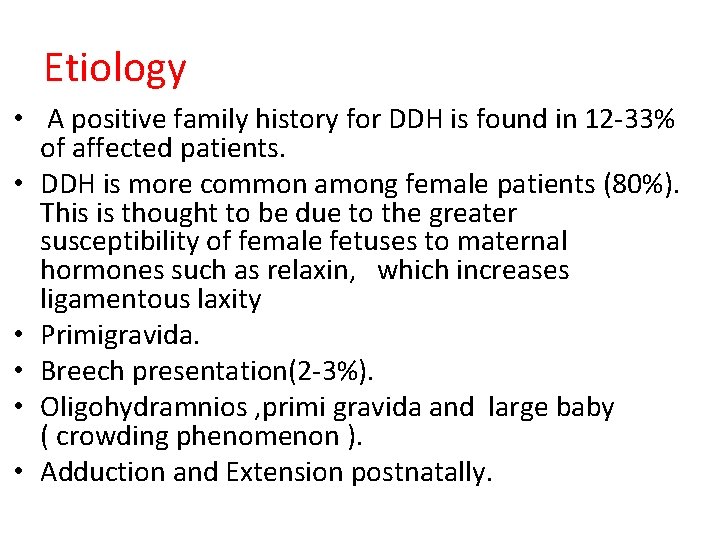
Etiology • A positive family history for DDH is found in 12 -33% of affected patients. • DDH is more common among female patients (80%). This is thought to be due to the greater susceptibility of female fetuses to maternal hormones such as relaxin, which increases ligamentous laxity • Primigravida. • Breech presentation(2 -3%). • Oligohydramnios , primi gravida and large baby ( crowding phenomenon ). • Adduction and Extension postnatally.
Associated conditions • Torticollis • metatarsus adductus • calcaneovalgus feet
• The left hip is the most commonly affected hip • In the most common fetal position, this is the hip that is usually forced into adduction against the mother’s sacrum. • Girls are affected 5 times more than boys.
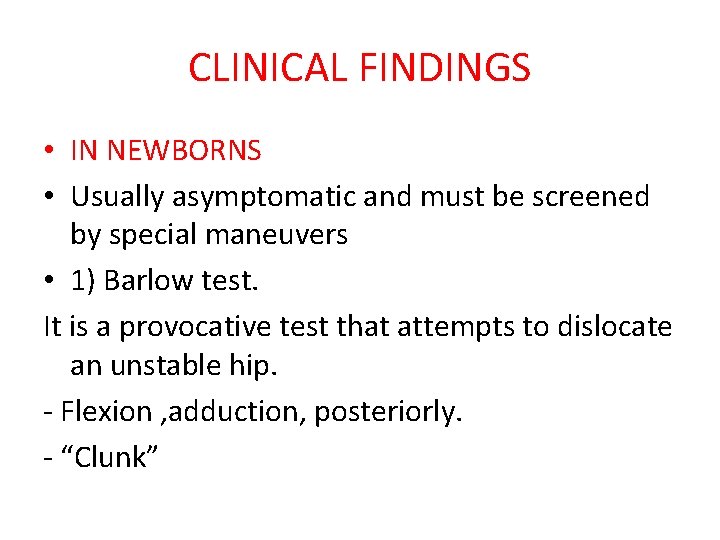
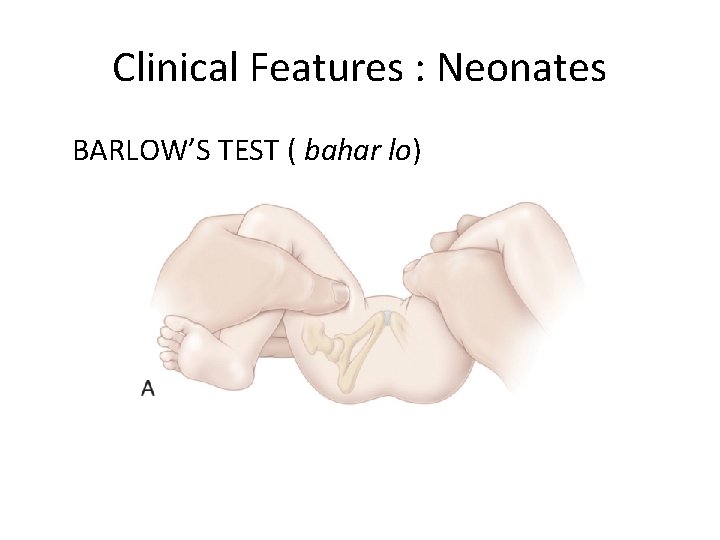
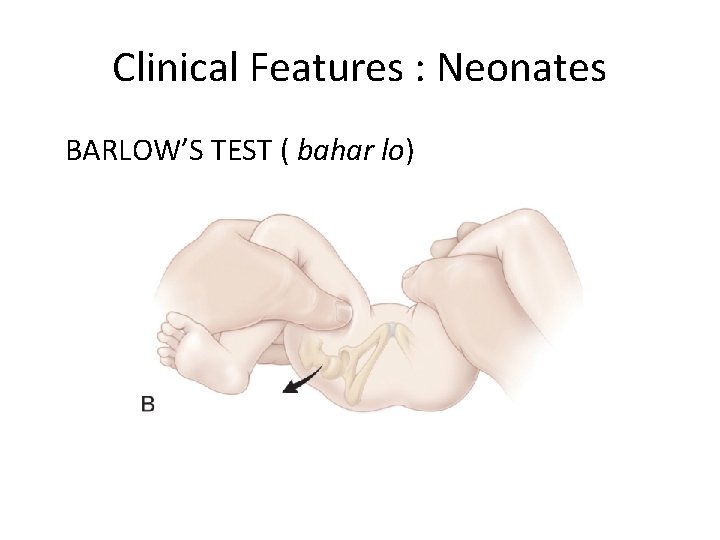
CLINICAL FINDINGS • IN NEWBORNS • Usually asymptomatic and must be screened by special maneuvers • 1) Barlow test. It is a provocative test that attempts to dislocate an unstable hip. - Flexion , adduction, posteriorly. - “Clunk”
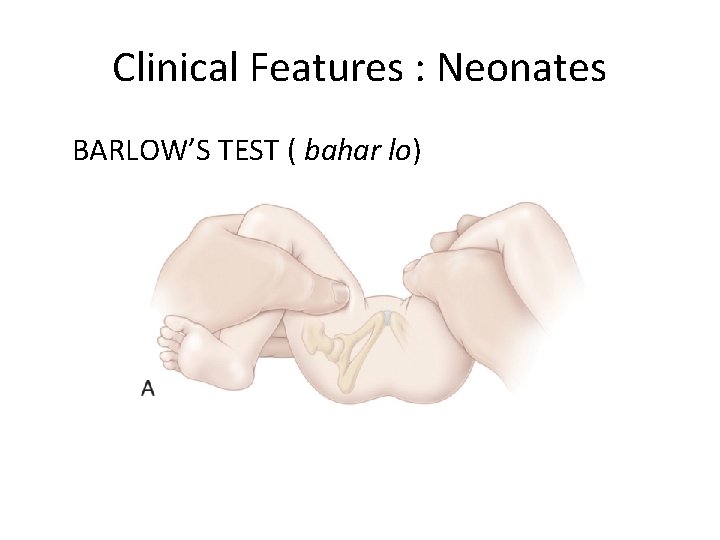
Clinical Features : Neonates BARLOW’S TEST ( bahar lo)
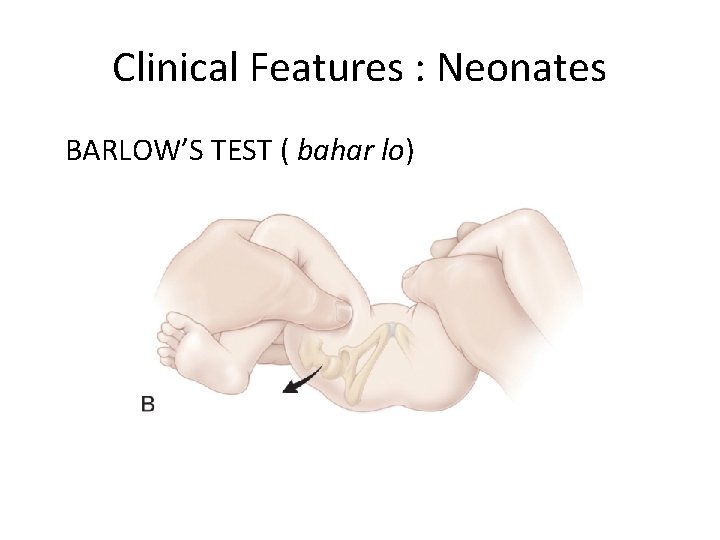
Clinical Features : Neonates BARLOW’S TEST ( bahar lo)
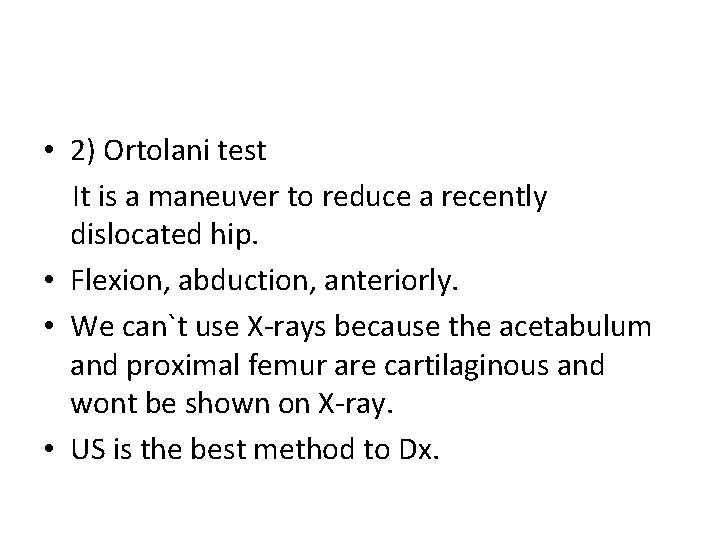
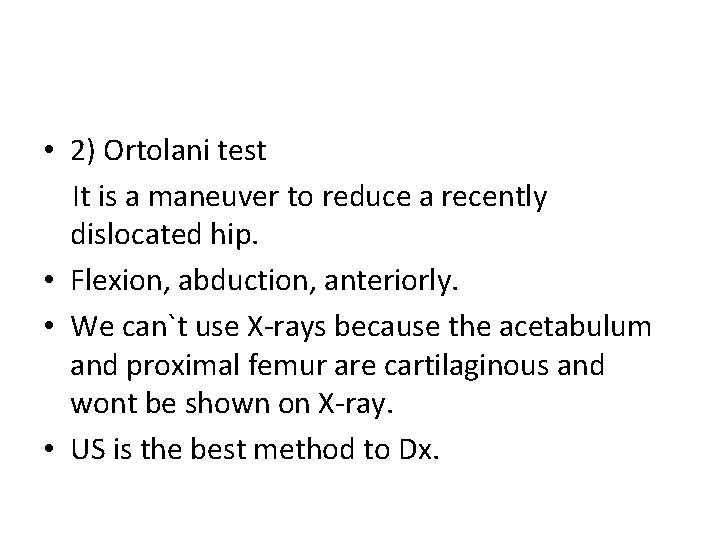
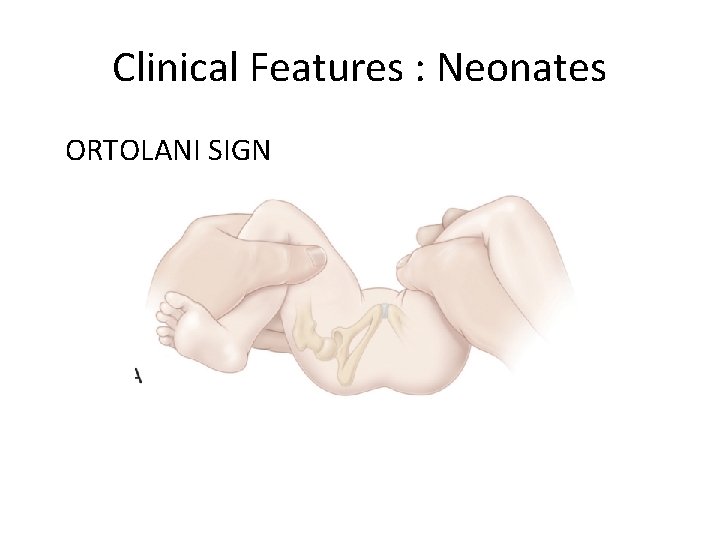
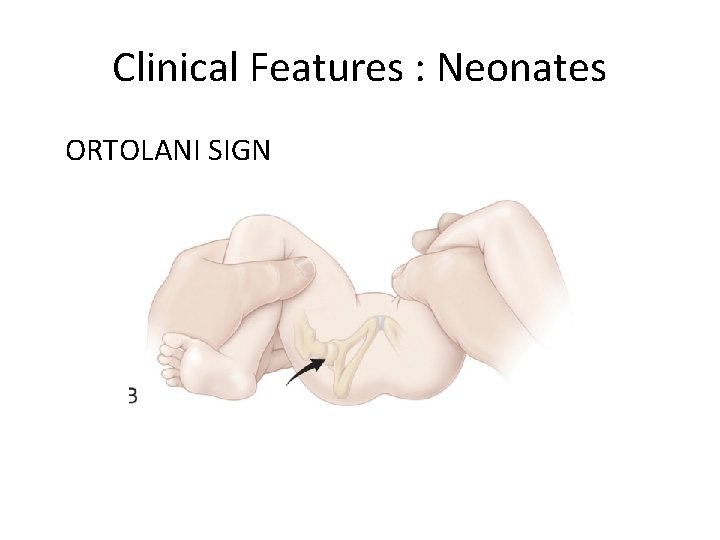
• 2) Ortolani test It is a maneuver to reduce a recently dislocated hip. • Flexion, abduction, anteriorly. • We can`t use X-rays because the acetabulum and proximal femur are cartilaginous and wont be shown on X-ray. • US is the best method to Dx.
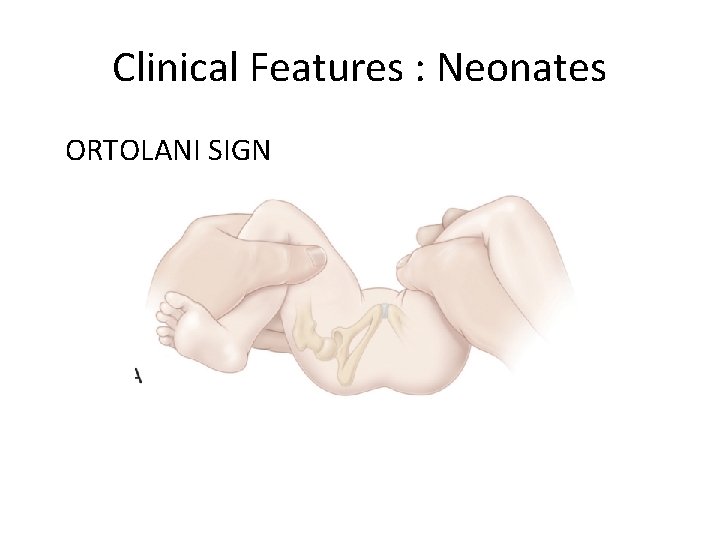
Clinical Features : Neonates ORTOLANI SIGN
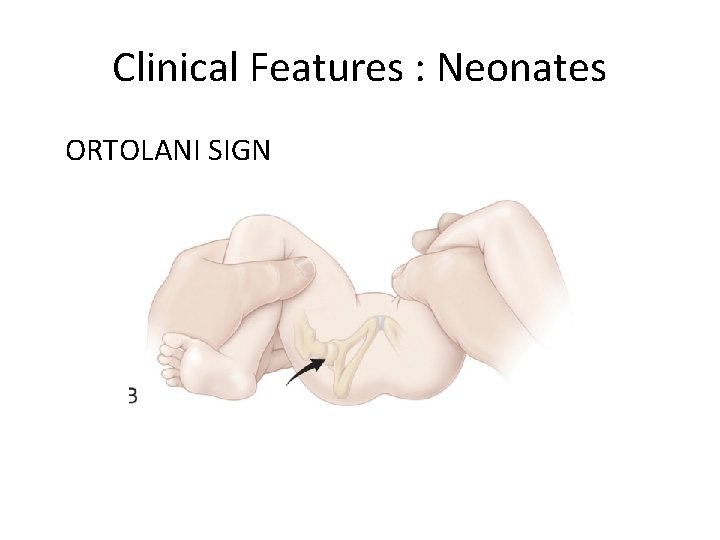
Clinical Features : Neonates ORTOLANI SIGN
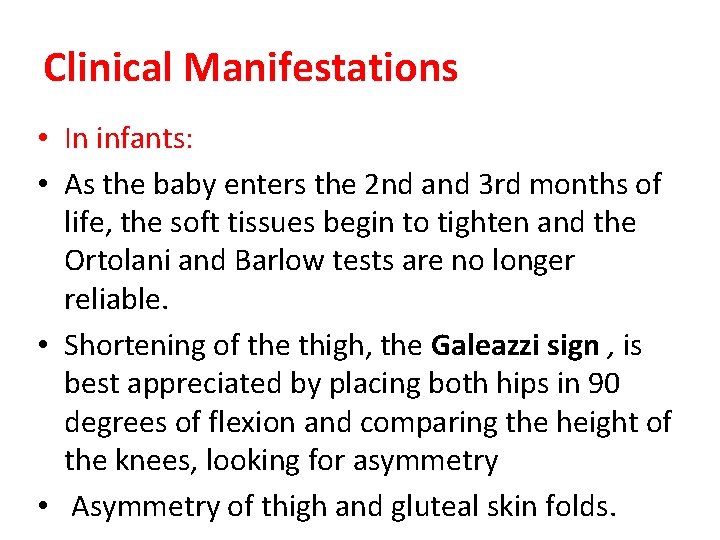
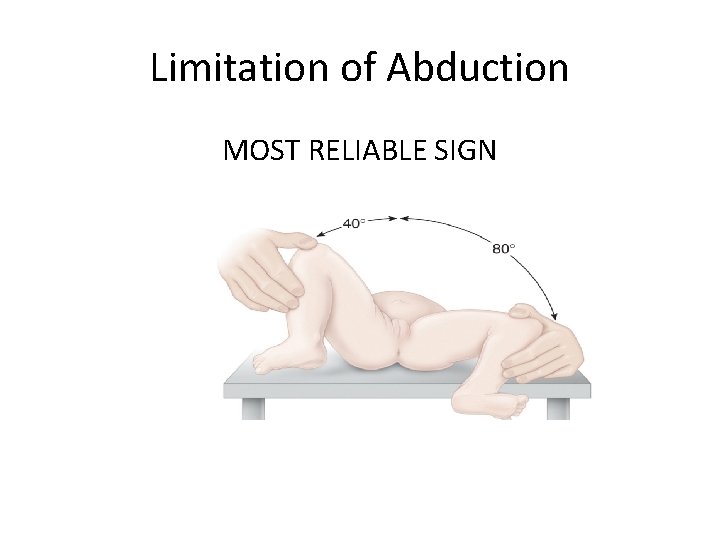
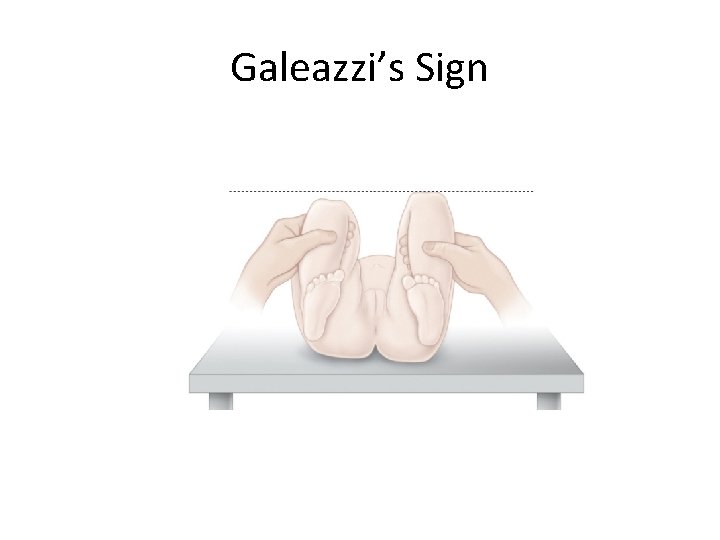
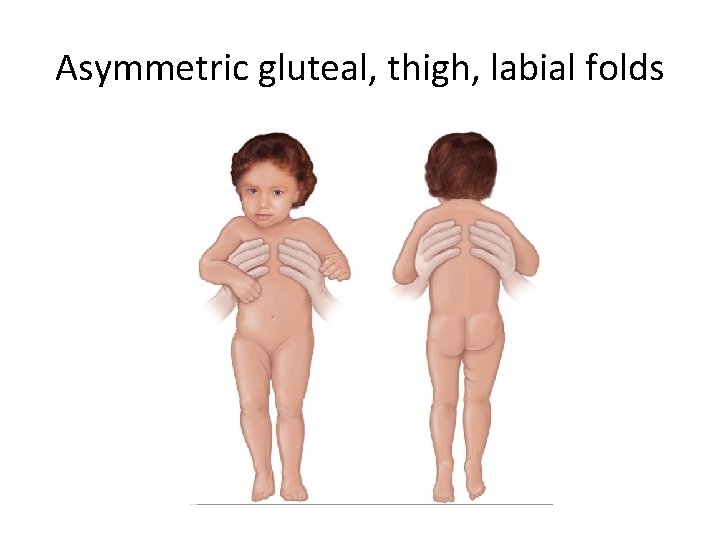
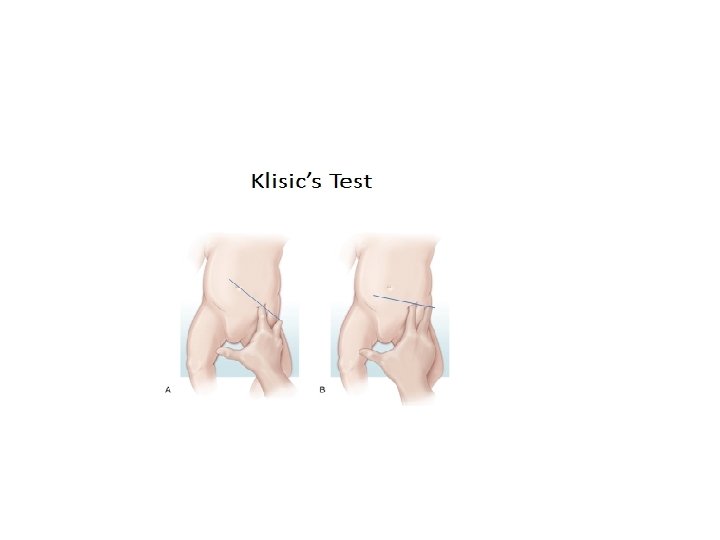
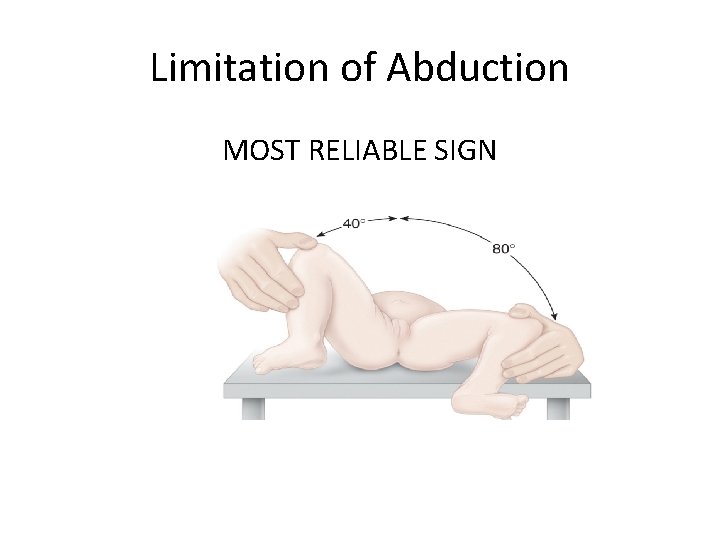
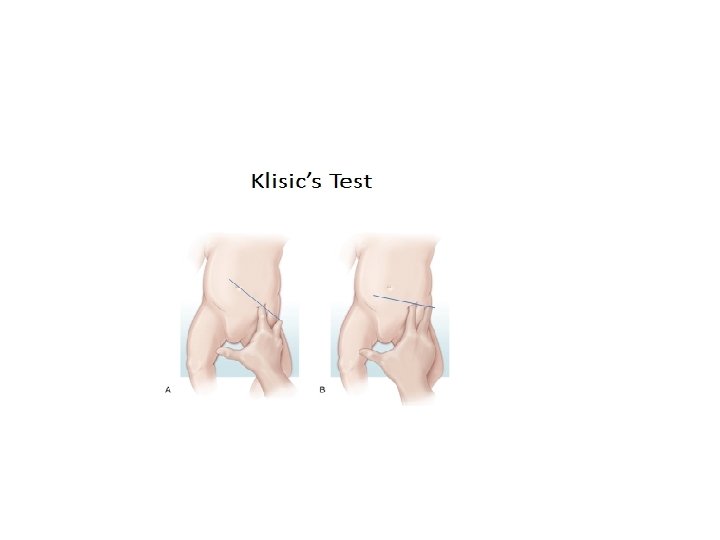
Clinical Manifestations • In infants: • As the baby enters the 2 nd and 3 rd months of life, the soft tissues begin to tighten and the Ortolani and Barlow tests are no longer reliable. • Shortening of the thigh, the Galeazzi sign , is best appreciated by placing both hips in 90 degrees of flexion and comparing the height of the knees, looking for asymmetry • Asymmetry of thigh and gluteal skin folds.
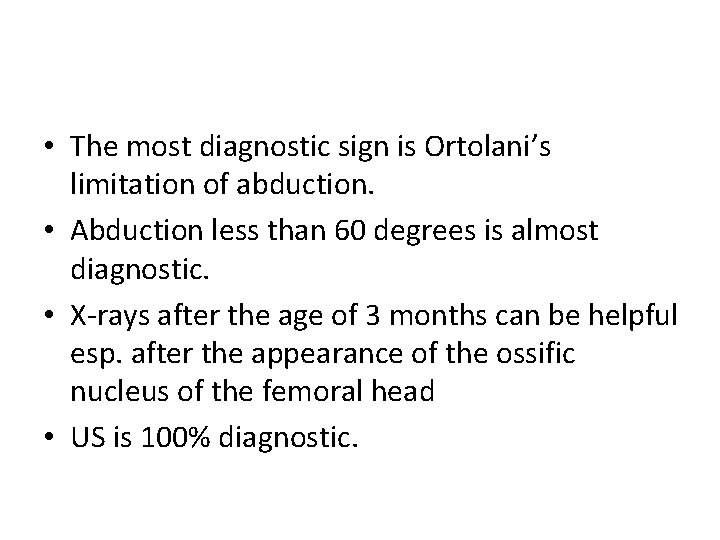
• The most diagnostic sign is Ortolani’s limitation of abduction. • Abduction less than 60 degrees is almost diagnostic. • X-rays after the age of 3 months can be helpful esp. after the appearance of the ossific nucleus of the femoral head • US is 100% diagnostic.
Limitation of Abduction MOST RELIABLE SIGN
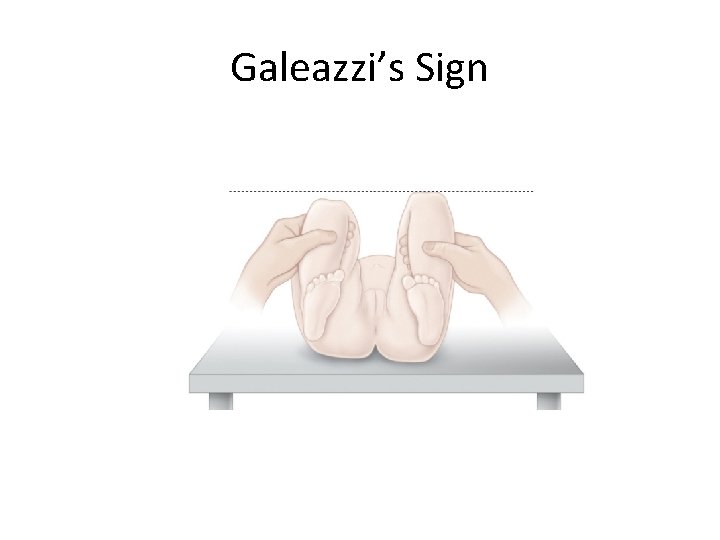
Galeazzi’s Sign
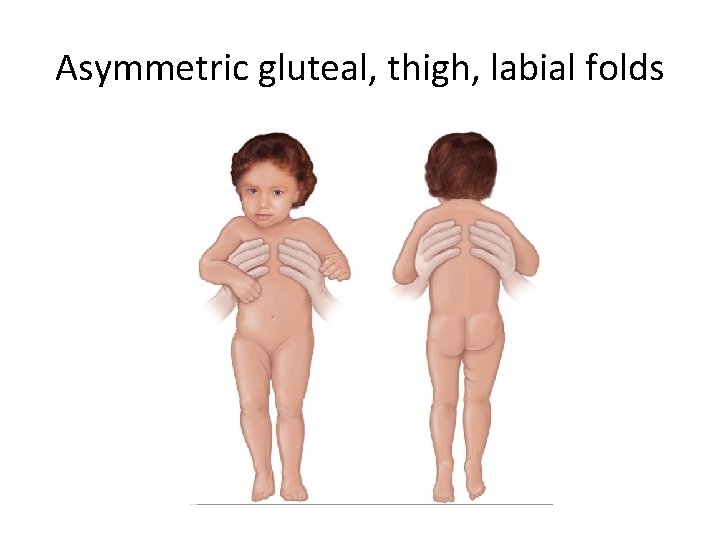
Asymmetric gluteal, thigh, labial folds
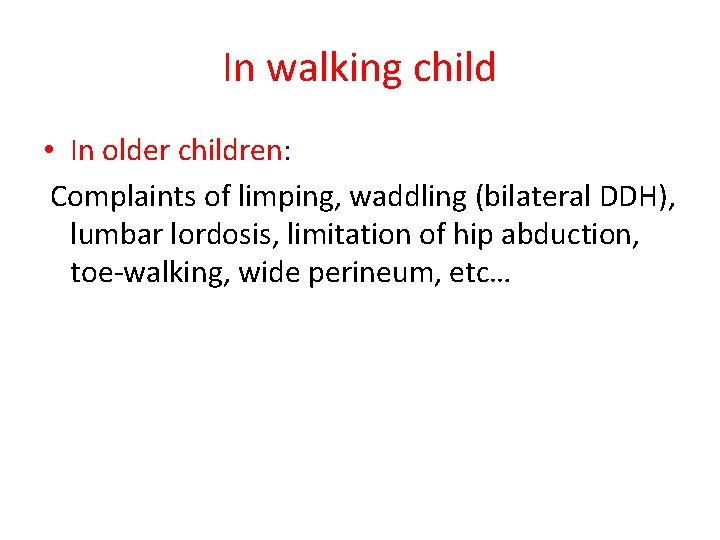
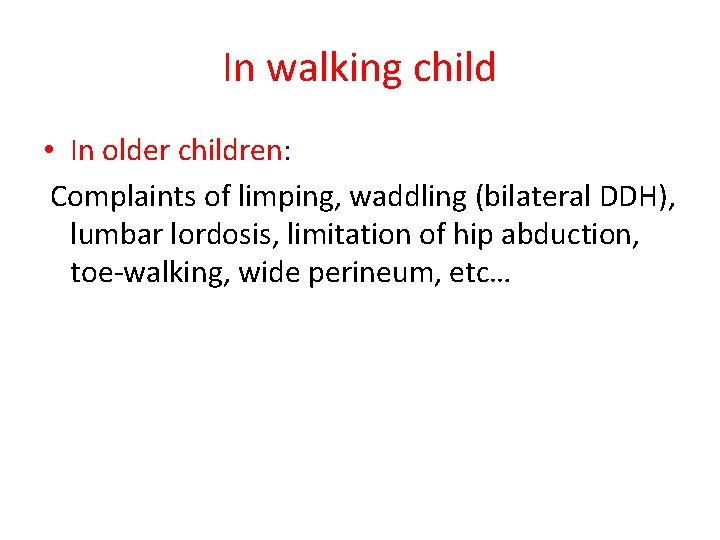
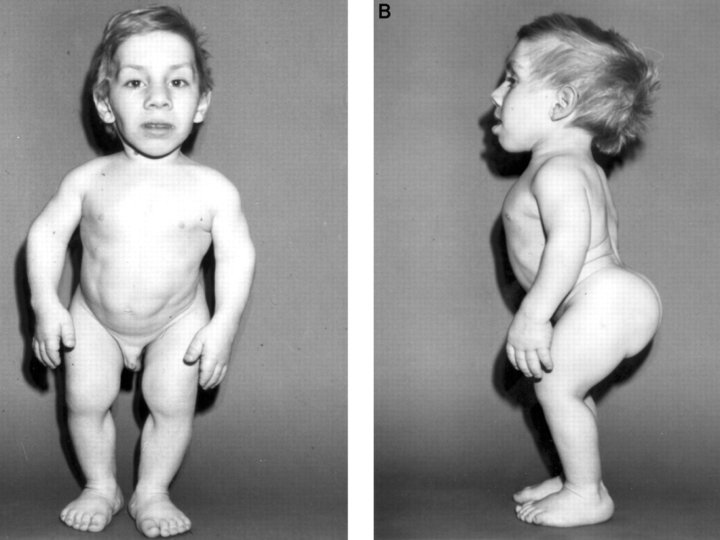
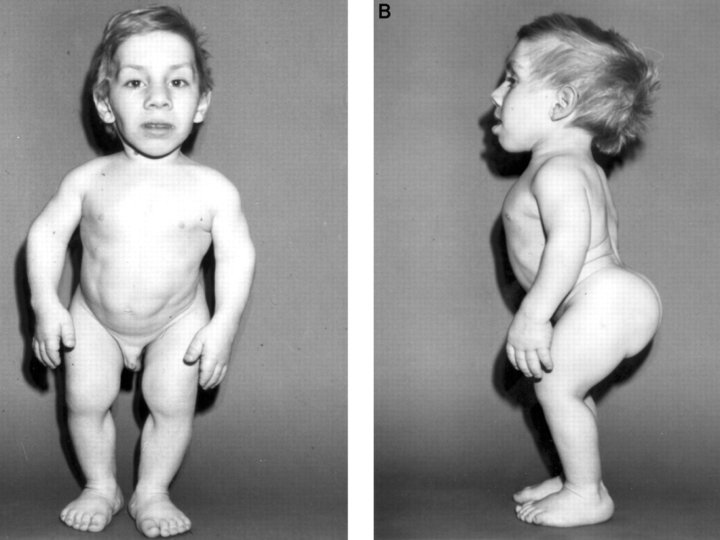
In walking child • In older children: Complaints of limping, waddling (bilateral DDH), lumbar lordosis, limitation of hip abduction, toe-walking, wide perineum, etc…
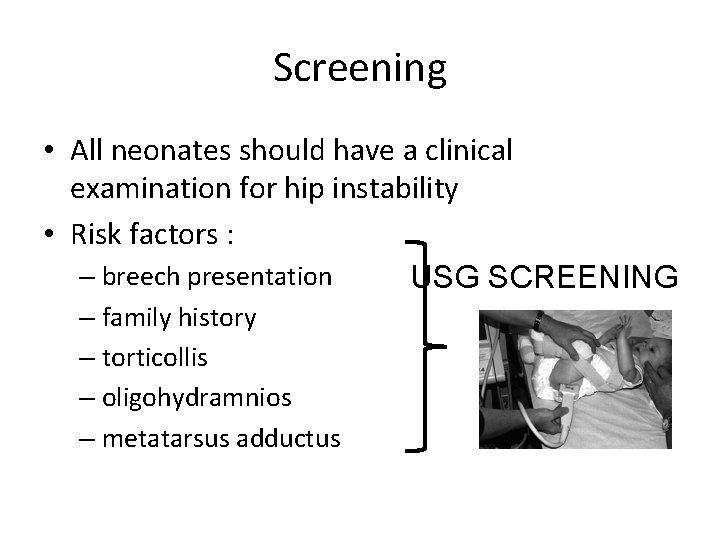
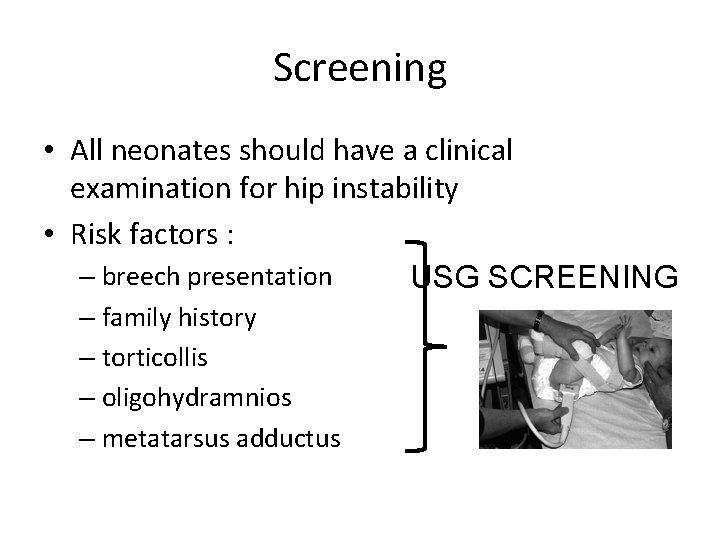
Screening • All neonates should have a clinical examination for hip instability • Risk factors : – breech presentation USG SCREENING – family history – torticollis – oligohydramnios – metatarsus adductus
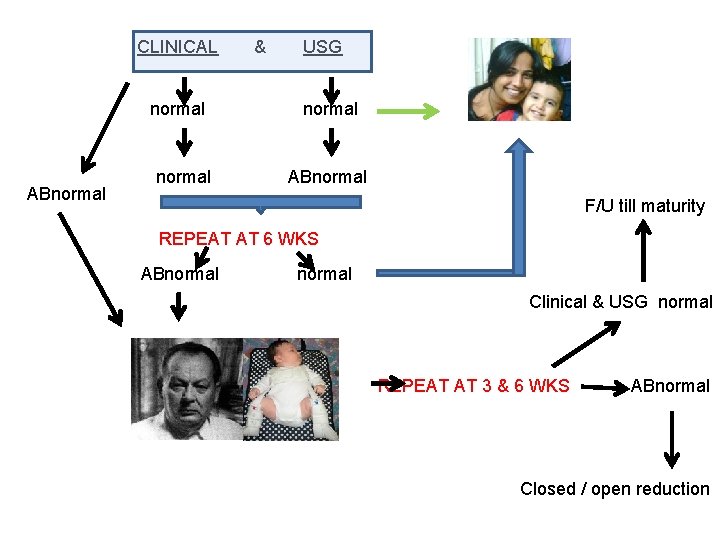
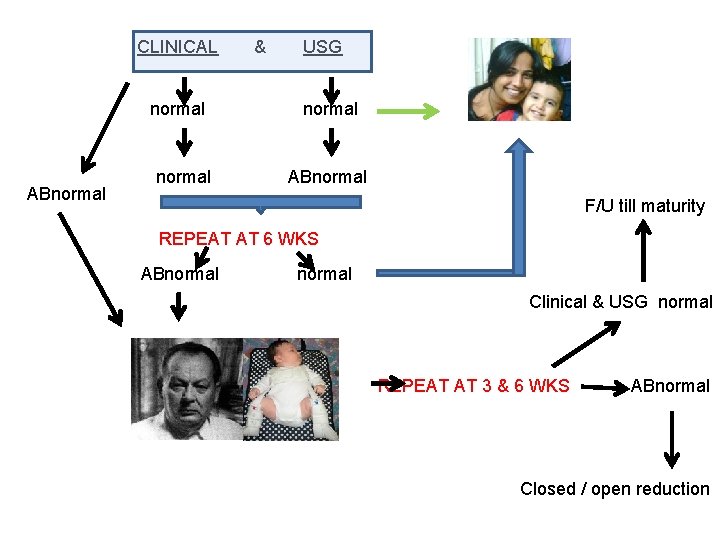
CLINICAL normal ABnormal & USG normal ABnormal F/U till maturity REPEAT AT 6 WKS ABnormal Clinical & USG normal REPEAT AT 3 & 6 WKS ABnormal Closed / open reduction
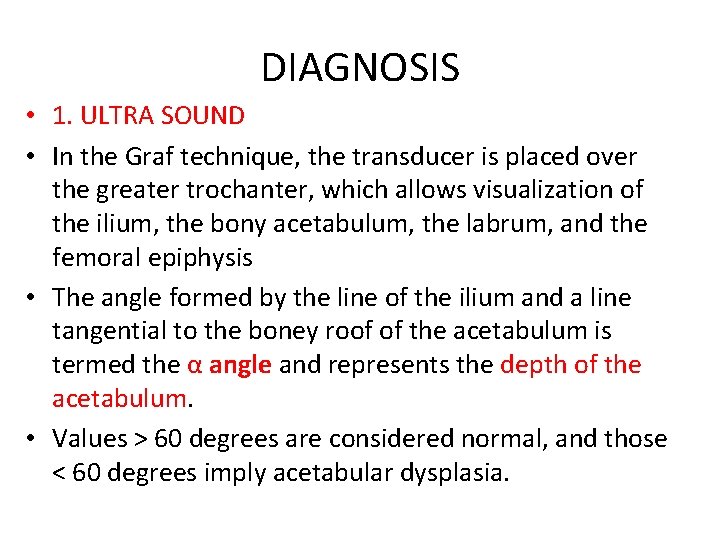
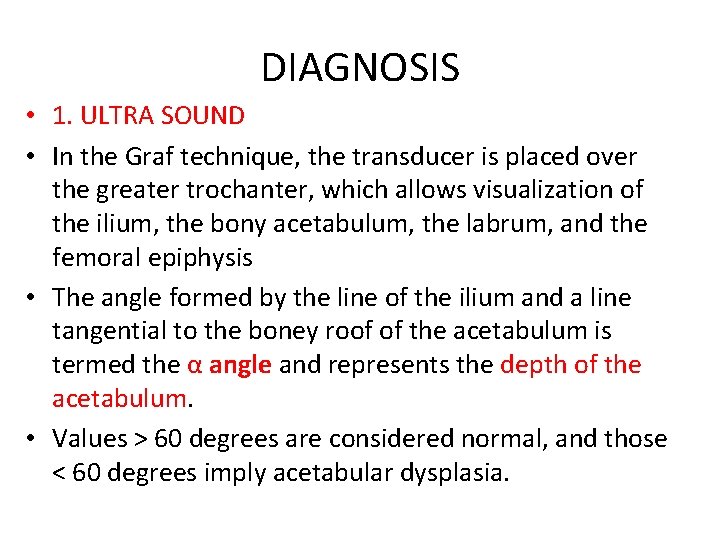
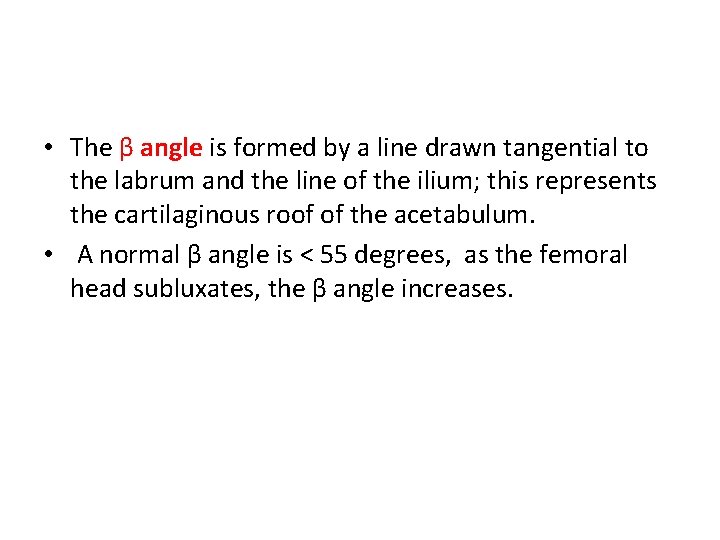
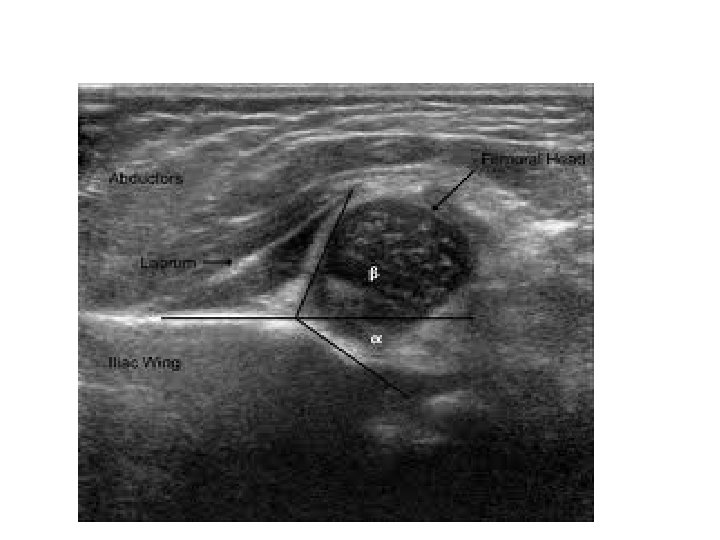
DIAGNOSIS • 1. ULTRA SOUND • In the Graf technique, the transducer is placed over the greater trochanter, which allows visualization of the ilium, the bony acetabulum, the labrum, and the femoral epiphysis • The angle formed by the line of the ilium and a line tangential to the boney roof of the acetabulum is termed the α angle and represents the depth of the acetabulum. • Values > 60 degrees are considered normal, and those < 60 degrees imply acetabular dysplasia.
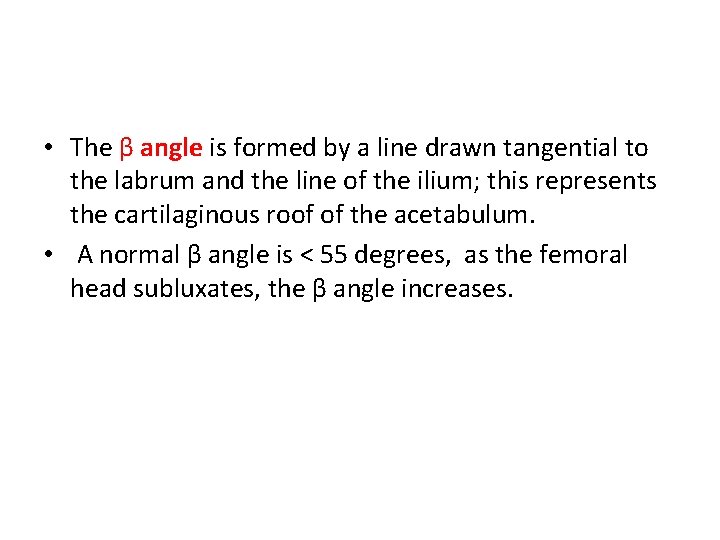
• The β angle is formed by a line drawn tangential to the labrum and the line of the ilium; this represents the cartilaginous roof of the acetabulum. • A normal β angle is < 55 degrees, as the femoral head subluxates, the β angle increases.
![Graf classification of DDH simplified class Alpha angle Beta angle description 1 Graf classification of DDH [ simplified] class Alpha angle Beta angle description 1](https://slidetodoc.com/presentation_image/30c2513983aadfc80f250d898f2fbd78/image-31.jpg)
Graf classification of DDH [ simplified] class Alpha angle Beta angle description 1 >60 <55 normal 2 43 -60 55 -77 3 <43 >77 Delayed ossification lateralization 4 unmeasurable dislocated
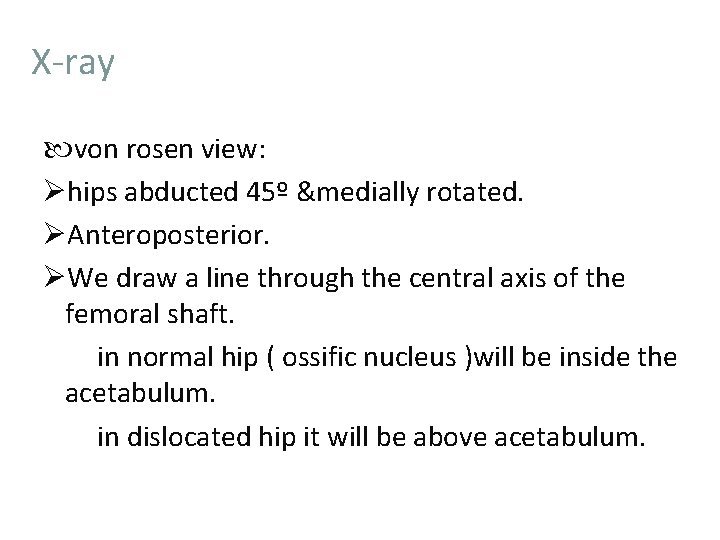
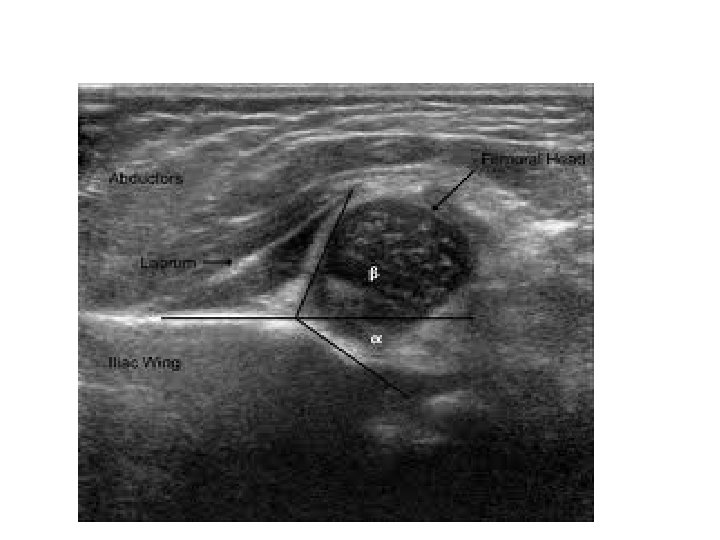
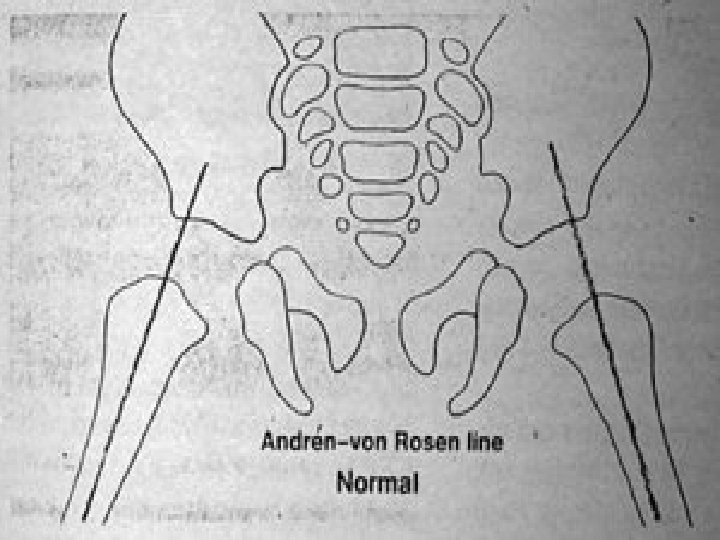
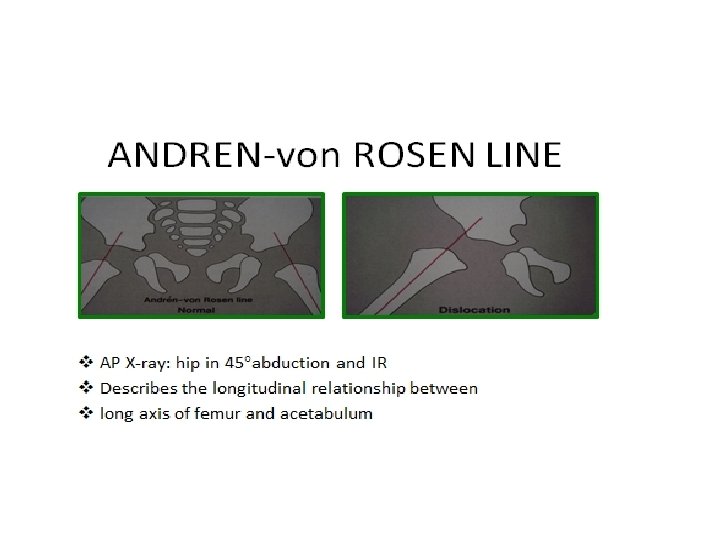
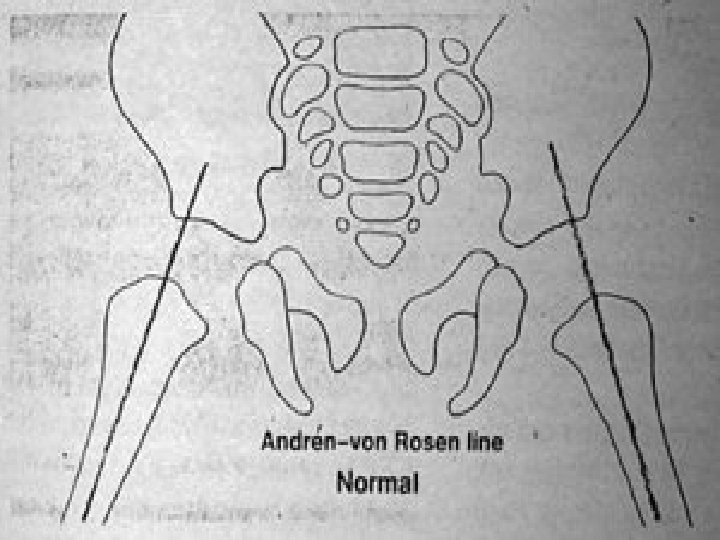
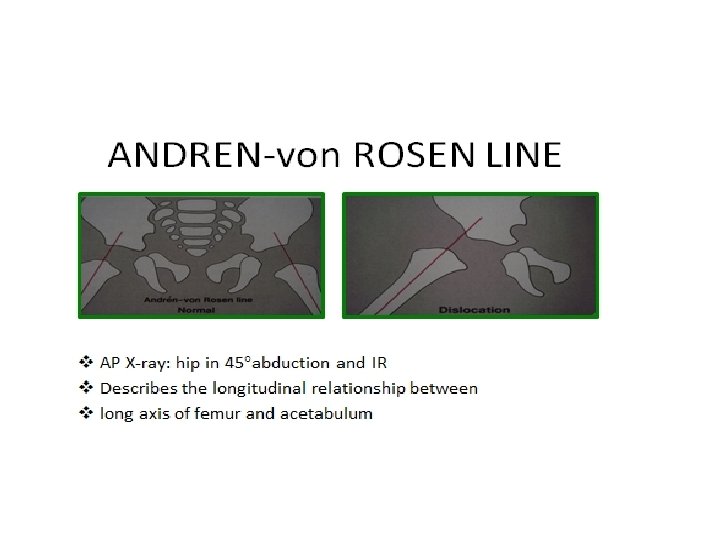
X-ray von rosen view: Øhips abducted 45º &medially rotated. ØAnteroposterior. ØWe draw a line through the central axis of the femoral shaft. in normal hip ( ossific nucleus )will be inside the acetabulum. in dislocated hip it will be above acetabulum.
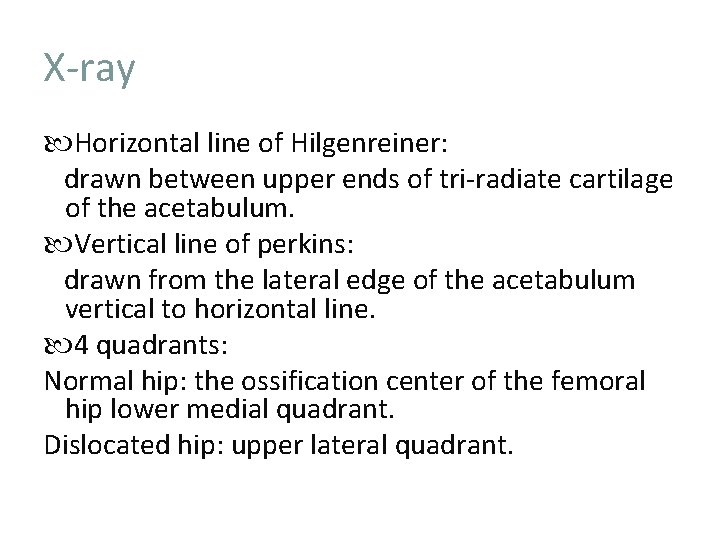
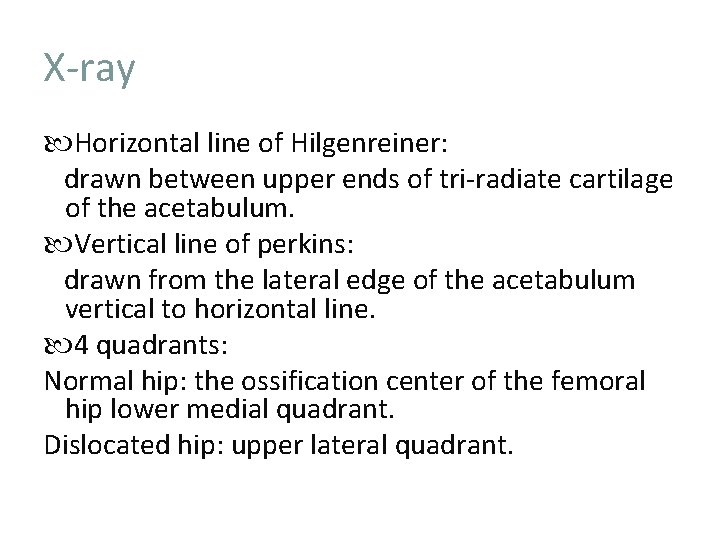
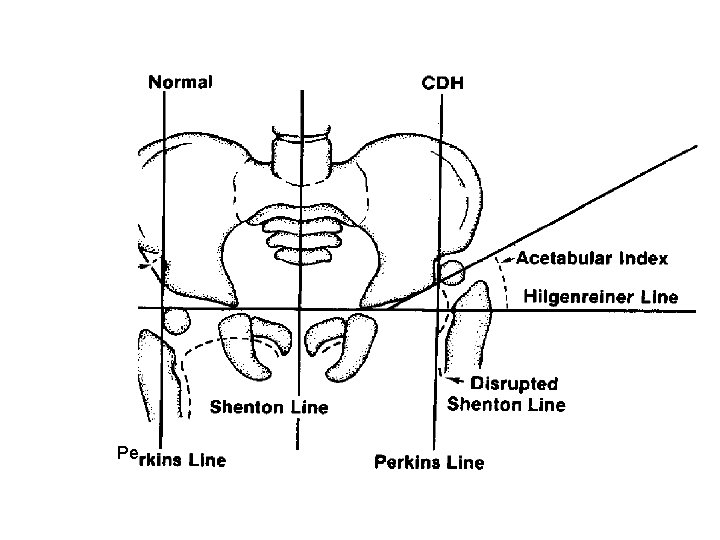
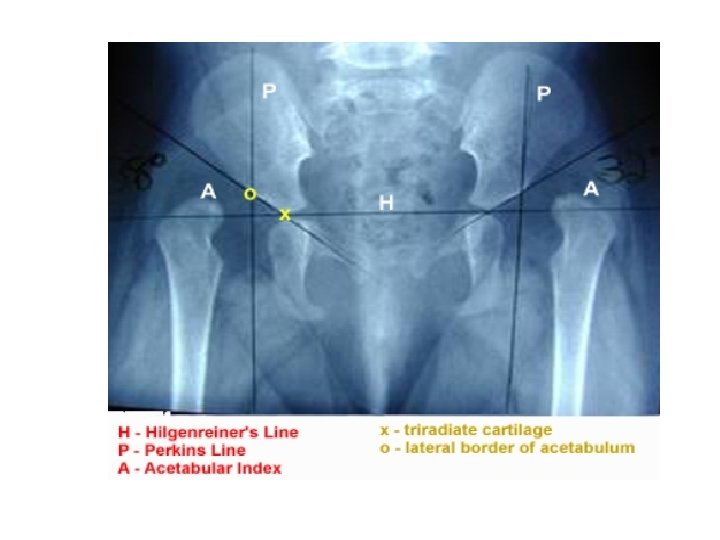
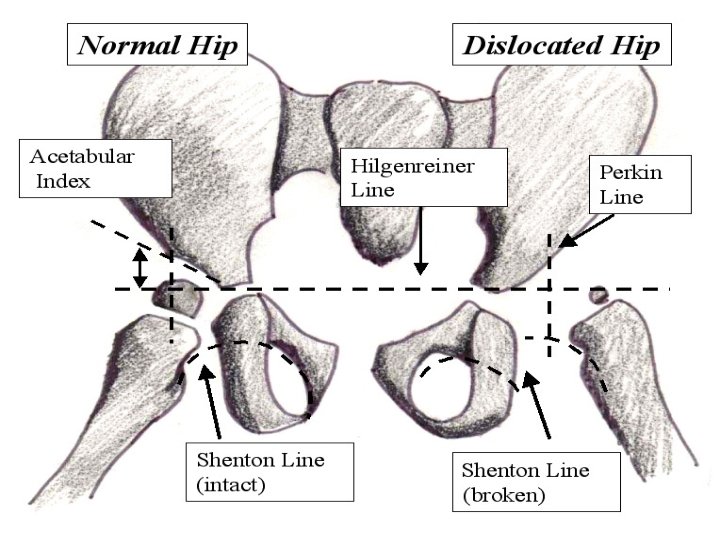
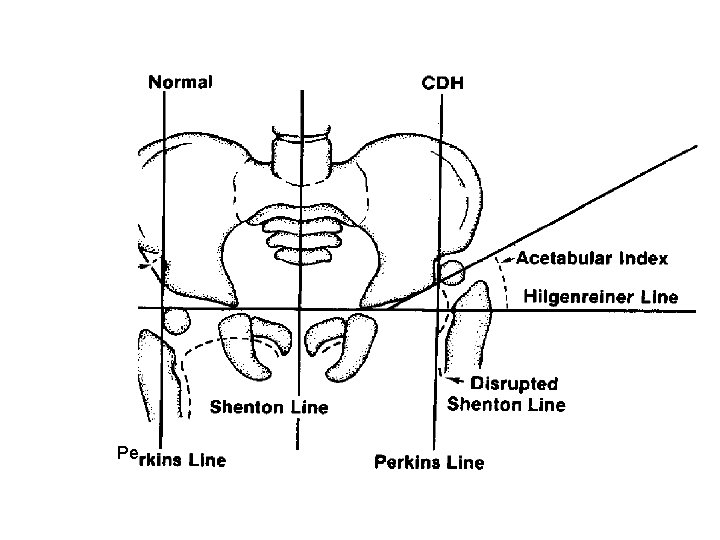
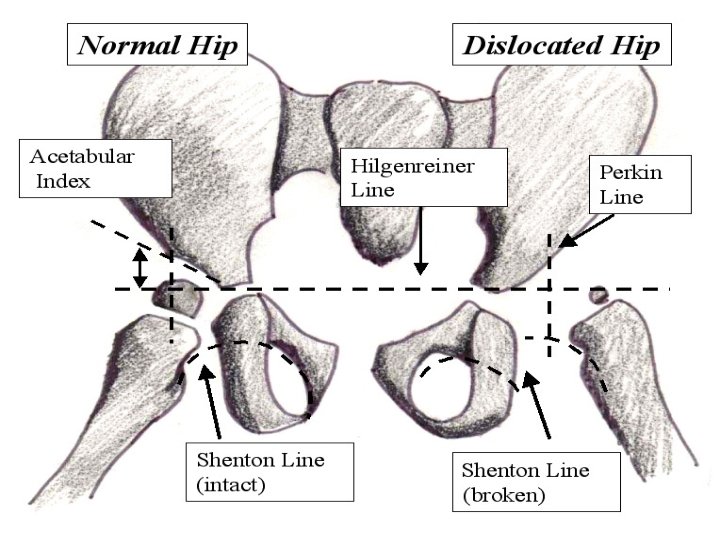
X-ray Horizontal line of Hilgenreiner: drawn between upper ends of tri-radiate cartilage of the acetabulum. Vertical line of perkins: drawn from the lateral edge of the acetabulum vertical to horizontal line. 4 quadrants: Normal hip: the ossification center of the femoral hip lower medial quadrant. Dislocated hip: upper lateral quadrant.
Pe

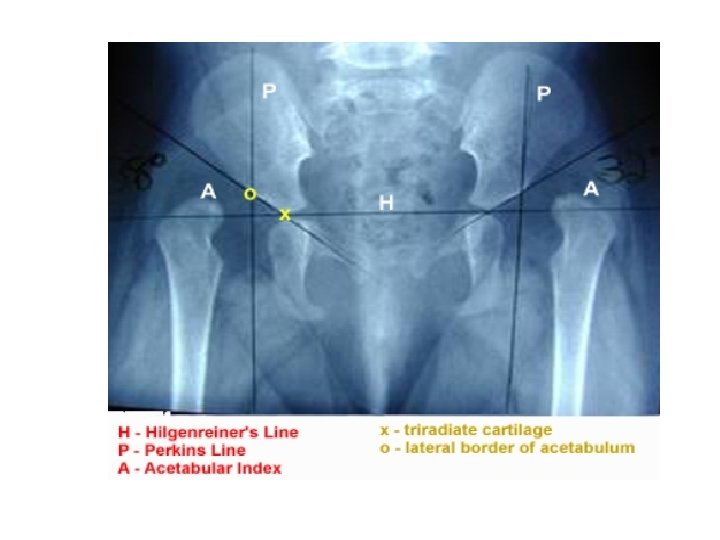
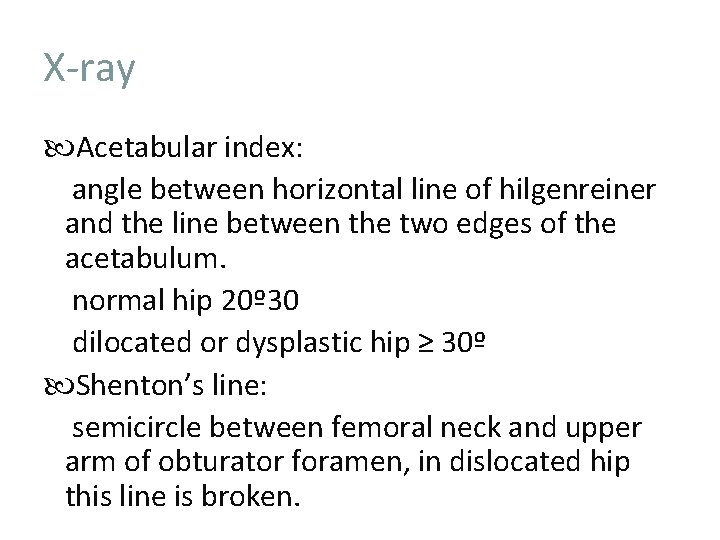
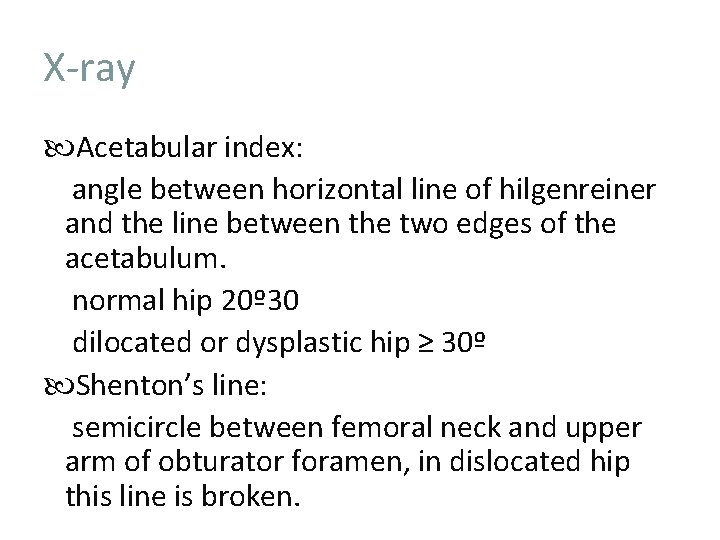
X-ray Acetabular index: angle between horizontal line of hilgenreiner and the line between the two edges of the acetabulum. normal hip 20º 30 dilocated or dysplastic hip ≥ 30º Shenton’s line: semicircle between femoral neck and upper arm of obturator foramen, in dislocated hip this line is broken.
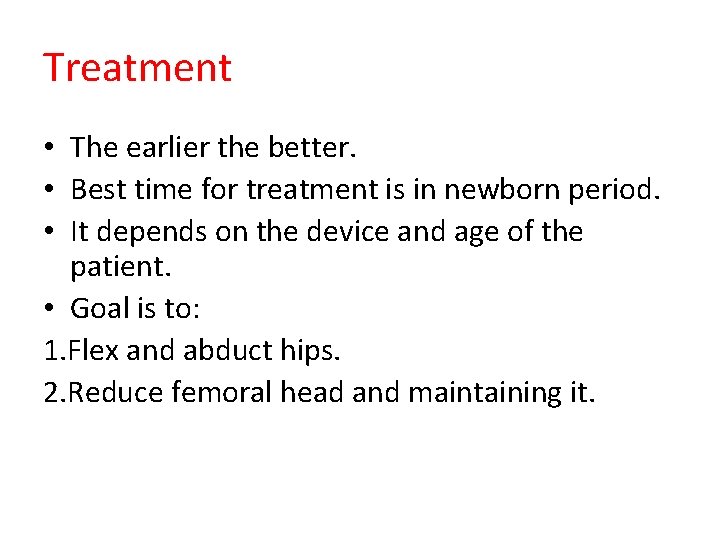
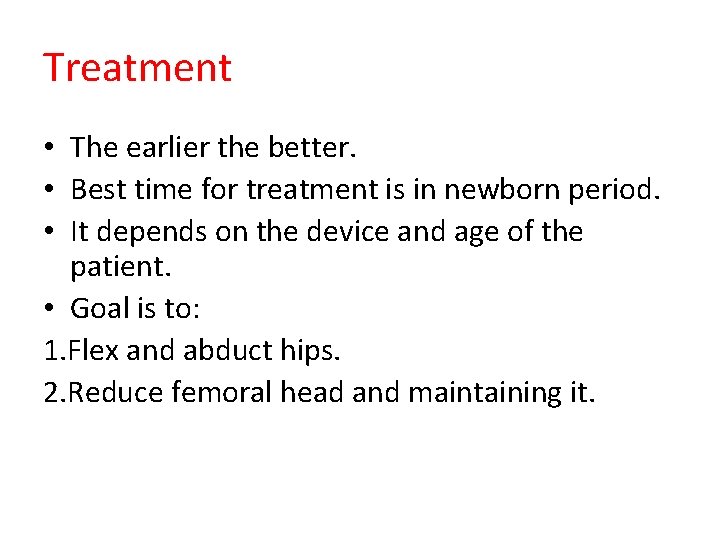
Treatment • The earlier the better. • Best time for treatment is in newborn period. • It depends on the device and age of the patient. • Goal is to: 1. Flex and abduct hips. 2. Reduce femoral head and maintaining it.
• The goals in the management of DDH are to obtain and maintain a concentric reduction of the femoral head within the acetabulum to provide the optimal environment for the normal development of both the femoral head and acetabulum. • The later the diagnosisof DDH is made, the more difficult it is to achieve these goals, the less potential there is for acetabular and proximal femoral remodeling, and the more complex are the required treatments
Treatment • From (1 -6 months) use Pavlik Harness. • From 6 months -2 year use hip spica. • From the age of >2 year traction , adductor tenotomy , surgical closed reduction, salter innominate osteotomy.
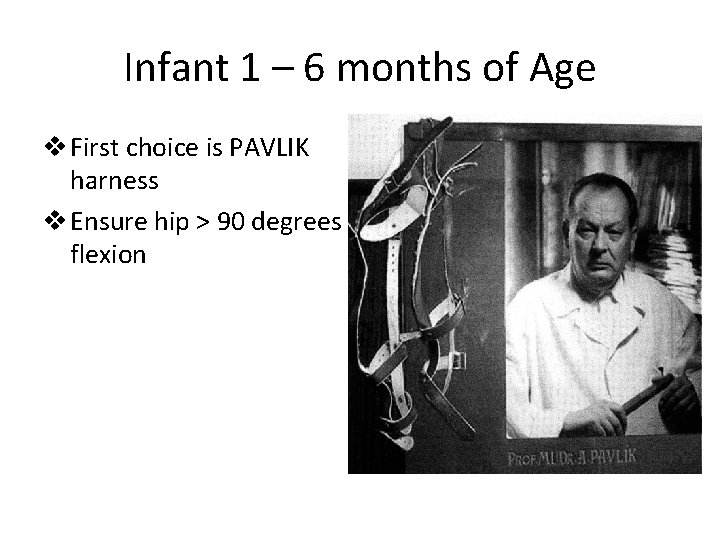
Infant 1 – 6 months of Age v First choice is PAVLIK harness v Ensure hip > 90 degrees flexion
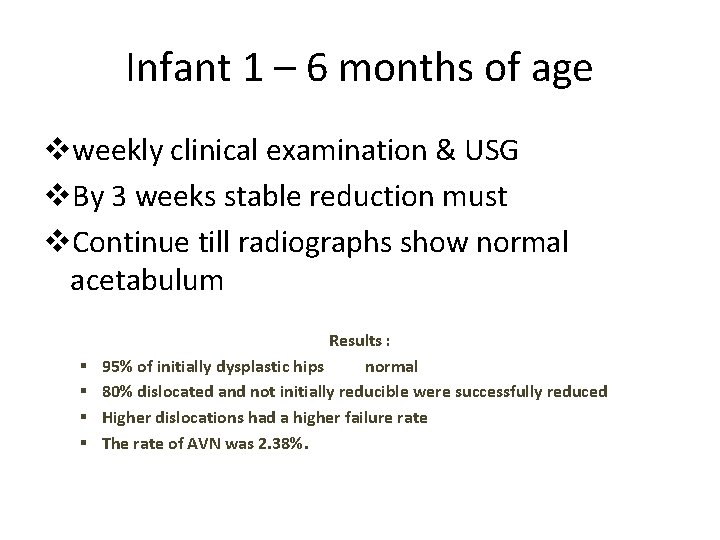
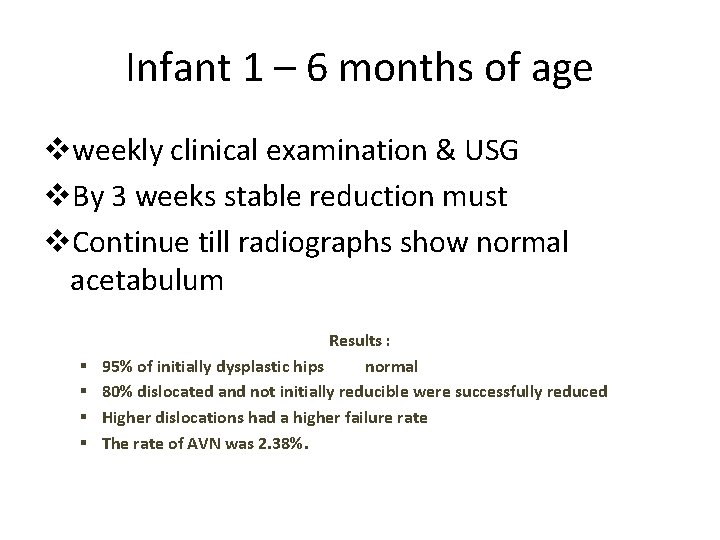
Infant 1 – 6 months of age vweekly clinical examination & USG v. By 3 weeks stable reduction must v. Continue till radiographs show normal acetabulum § § Results : 95% of initially dysplastic hips normal 80% dislocated and not initially reducible were successfully reduced Higher dislocations had a higher failure rate The rate of AVN was 2. 38%.
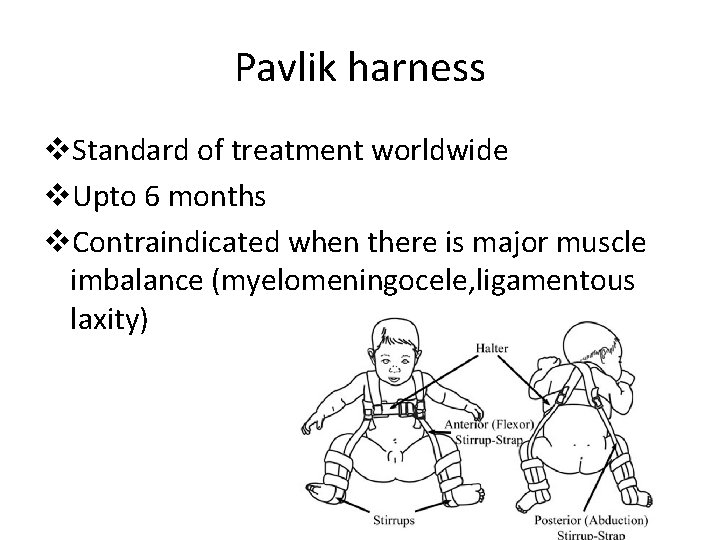
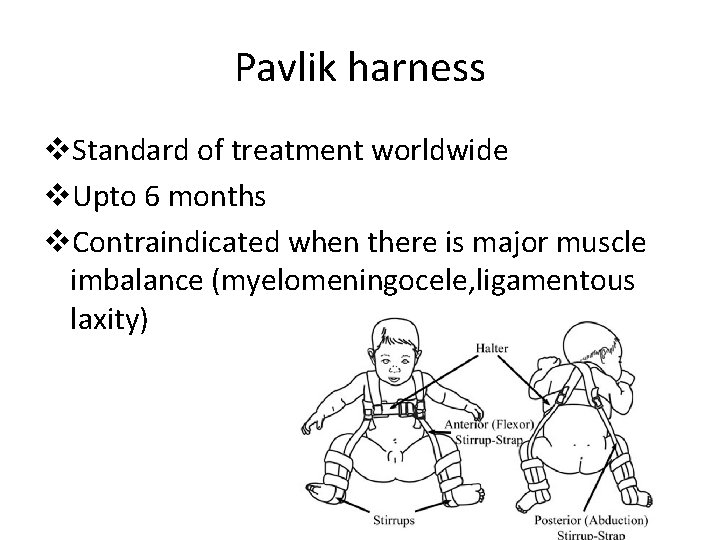
Pavlik harness v. Standard of treatment worldwide v. Upto 6 months v. Contraindicated when there is major muscle imbalance (myelomeningocele, ligamentous laxity)

Complications of Pavlik Harness • AVN • Failure to reduce • Femoral nerve neuropathy • Inferior dislocation • Pavlik’s disease (flattening posterolateral acetabulum)
Von Rosens splint
Child 6 months to 2 years of age • Closed or open reduction + adductor tenotomy • If closed reduction fails then surgeon should be prepared for an open procedure
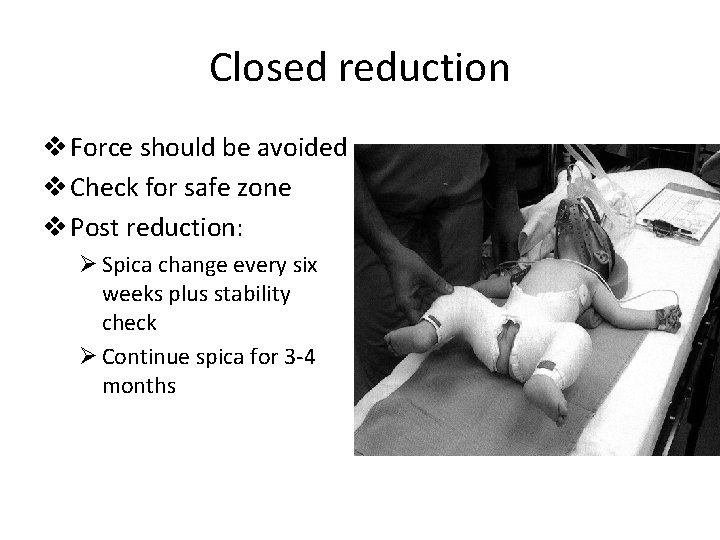
Closed reduction v Force should be avoided v Check for safe zone v Post reduction: Ø Spica change every six weeks plus stability check Ø Continue spica for 3 -4 months
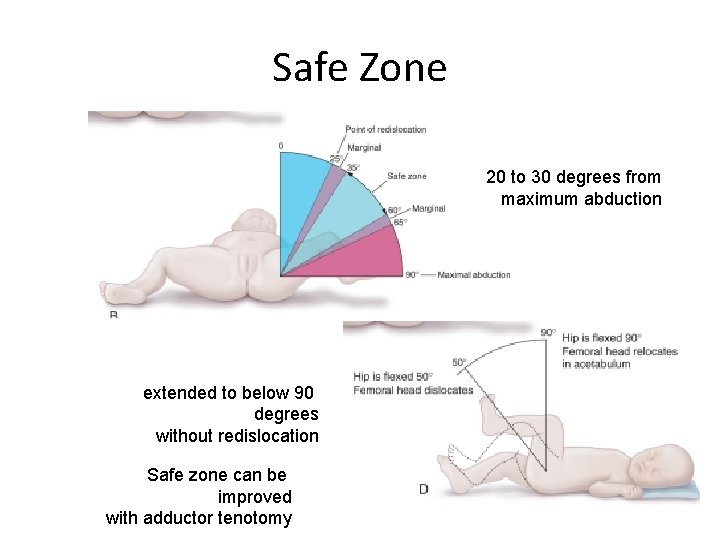
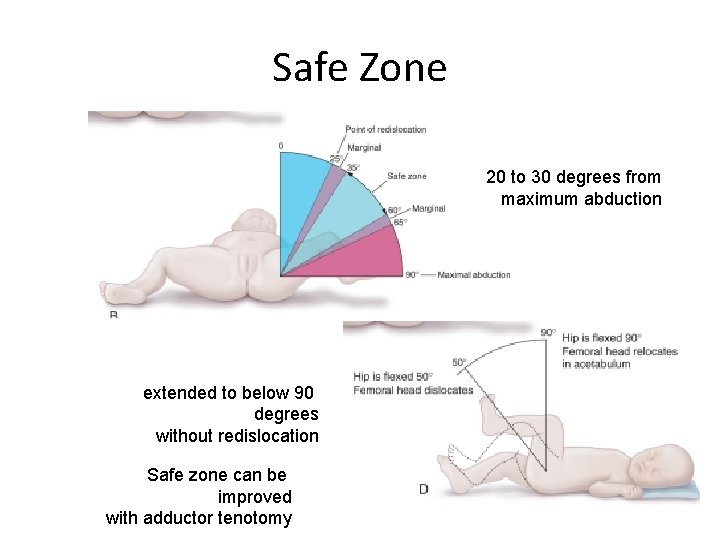
Safe Zone 20 to 30 degrees from maximum abduction extended to below 90 degrees without redislocation Safe zone can be improved with adductor tenotomy
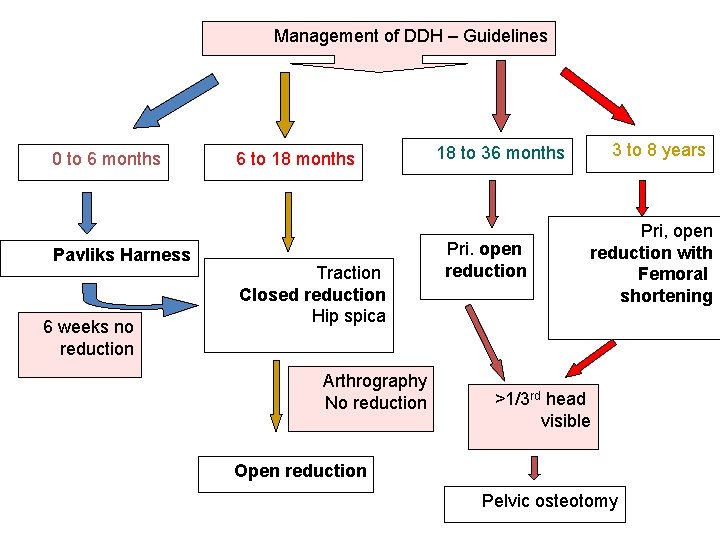
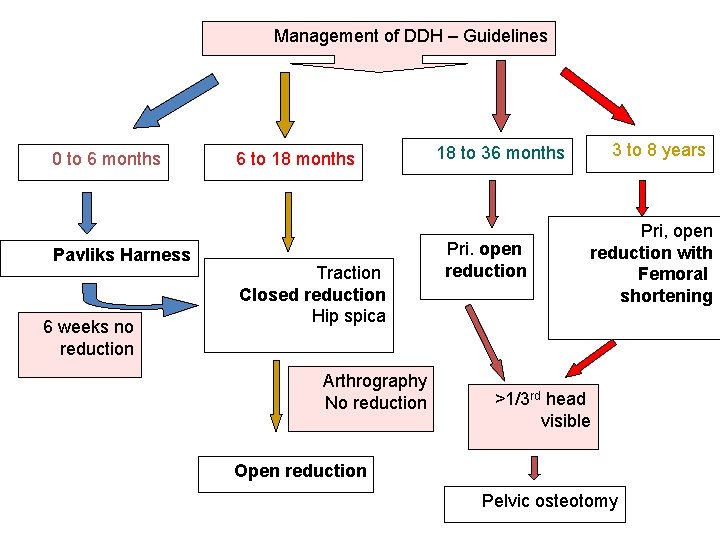
Management of DDH – Guidelines 0 to 6 months Pavliks Harness 6 weeks no reduction 6 to 18 months Traction Closed reduction Hip spica Arthrography No reduction 3 to 8 years 18 to 36 months Pri. open reduction Pri, open reduction with Femoral shortening >1/3 rd head visible Open reduction Pelvic osteotomy
• A 6 -week-old female infant is referred to your practice for concerns of developmental dysplasia of the hip. On physical exam, you note a positive Ortolani test on the left side. Pavlik harness treatment is initiated. Which of the following imaging modalities should be utilized at the two week follow-up visit? • • • 1. Magnetic Resonance Imaging (MRI) 2. Computed Tomography (CT) 3. Ultrasound (US) 4. Plain Radiographs 5. Arthrogram and Dynamic Fluroscopy Which of the following concepts regarding pediatric hips is true? Review Topic • • • 1. The proximal femoral physis and greater trochanteric apophysis develop from different cartilaginous physes 2. The proximal femoral physis grows at a rate of 9 mm per year 3. Normal infant femoral anteversion is between 10 -20 degrees 4. The ossific nucleus of the proximal femur is visible on radiographs by 6 months of age in most children 5. Slipped capital femoral epiphysis (SCFE) typically occurs through the zone of proliferation Failure to achieve reduction of a dislocated hip in an otherwise healthy 4 month old infant which did not reduce after 3 weeks in a Pavlik harness and 3 weeks in an abduction brace is best treated with which of the following? Review Topic • • • 1. Adjusting the harness to 75 degrees of abduction and maintaing 90 degrees of hip flexion 2. Adjusting the harness to 75 degrees of abduction and increasing hip flexion to 120 degrees 3. Closed reduction with hip arthrogram, adductor tenotomy if necessary, and hip spica casting 4. Open reduction and femoral shortening osteotomy 5. Open reduction, femoral shortening osteotomy, and pelvic acetabular osteotomy
• In patients older than 12 -months of age with developmental dysplasia of the hip, all of the following physical exam findings are likely present EXCEPT? Review Topic • • • 1. Limited hip abduction 2. Positive Ortolani maneuver 3. Abnormal leg lengths on Galeazzi testing 4. Trendelenburg gait 5. Pelvic obliquity n infants with developmental dysplasia of the hip (DDH), anatomic closed reduction may be prevented by all of the following anatomic structure EXCEPT. Review Topic • • • 1. Interposition of gluteus medius 2. Limbus formed by fibrous tissue and hyaline cartilage 3. Ligamentum teres and prominent fibrofatty pulvinar tissue 4. Contracted transverse acetabular ligament 5. Inverted acetabular labrum A five-year-old boy with cerebral palsy presents to the clinic with a dislocated right hip, what quadrant of the acetabulum is most likely deficient? Review Topic • • • 1. Anterior-inferior 2. Anterior-superior 3. Posterior-superior 4. Posterior-inferior 5. Anterior-inferior and anterior-superior



 Barlow y ortolani
Barlow y ortolani Alpha and beta angle in ddh
Alpha and beta angle in ddh Strart
Strart Hip and elbow dysplasia
Hip and elbow dysplasia Ppt
Ppt Hip hop hip to the hippity
Hip hop hip to the hippity Hip hop hip the hippity
Hip hop hip the hippity Shenton line
Shenton line Ddh
Ddh Galeazzi sign
Galeazzi sign Alpha and beta angle in ddh
Alpha and beta angle in ddh Epithelial dysplasia
Epithelial dysplasia Hiperdonti nedir
Hiperdonti nedir Ground glass appearance fibrous dysplasia
Ground glass appearance fibrous dysplasia Supernumeray
Supernumeray Renal dysplasia
Renal dysplasia Diastrophic dysplasia
Diastrophic dysplasia Renal dysplasia
Renal dysplasia Epithelial dysplasia
Epithelial dysplasia Epithelial dysplasia
Epithelial dysplasia Craniodiaphyseal dysplasia
Craniodiaphyseal dysplasia Epidermal dysplasia verruciformis
Epidermal dysplasia verruciformis Osteofytes
Osteofytes Ununited anconeal process
Ununited anconeal process Periapical cemento-osseous dysplasia
Periapical cemento-osseous dysplasia Developmentally inappropriate practices definition
Developmentally inappropriate practices definition Developmental assets definition
Developmental assets definition Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Frameset trong html5
Frameset trong html5 Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Chụp tư thế worms-breton
Chụp tư thế worms-breton Chúa sống lại
Chúa sống lại Kể tên các môn thể thao
Kể tên các môn thể thao Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
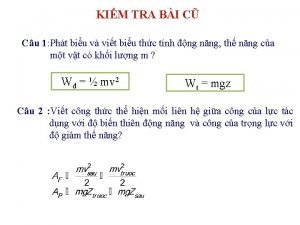
Các châu lục và đại dương trên thế giới Công thức tính thế năng
Công thức tính thế năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng bé xinh thế chỉ nói điều hay thôi
Cái miệng bé xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
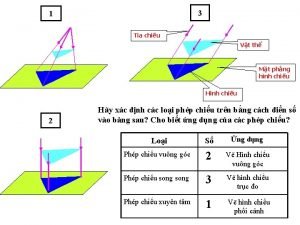
Vẽ hình chiếu vuông góc của vật thể sau Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Giọng cùng tên là
Giọng cùng tên là Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Fecboak
Fecboak Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Các loại đột biến cấu trúc nhiễm sắc thể
Các loại đột biến cấu trúc nhiễm sắc thể