Congenital Anomalies Department of Neurosurgery Faculty of Medicine


















- Slides: 79

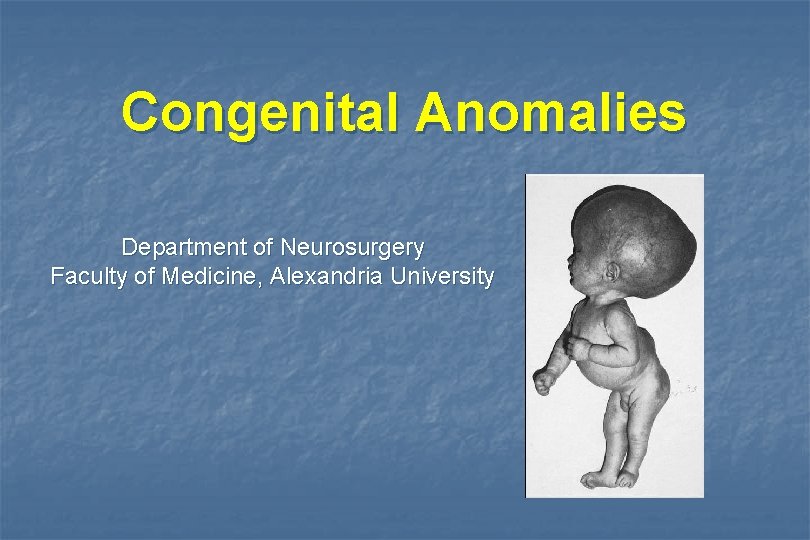
Congenital Anomalies Department of Neurosurgery Faculty of Medicine, Alexandria University
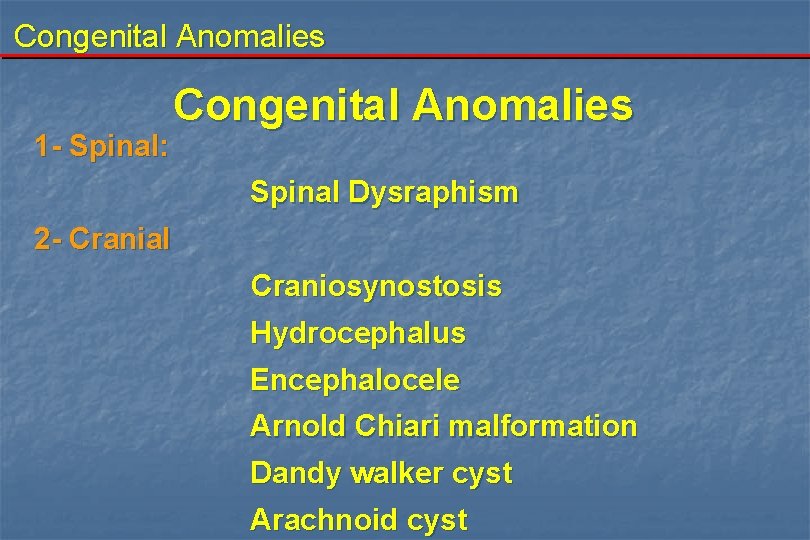
Congenital Anomalies 1 - Spinal: Congenital Anomalies Spinal Dysraphism 2 - Cranial Craniosynostosis Hydrocephalus Encephalocele Arnold Chiari malformation Dandy walker cyst Arachnoid cyst

Congenital Anomalies I. Spinal Dysraphism It is incomplete or faulty closure of the dorsal midline embryological structures abnormal (neural tube and adjacent cutaneous, muscular, and osseous structures) A. Spina bifida occulta B. Spina bifida cystica (aperta)

Congenital Anomalies I. Spinal Dysraphism A. Spina bifida occulta The underlying neural defect is masked by intact overlying skin There is minimal or no abnormality in the back by naked eye. - Diastomatomyelia - Dermoid tumors - Lipomyelomeningocele - Anterior sacral meningocele - Hypertrophic filum terminal
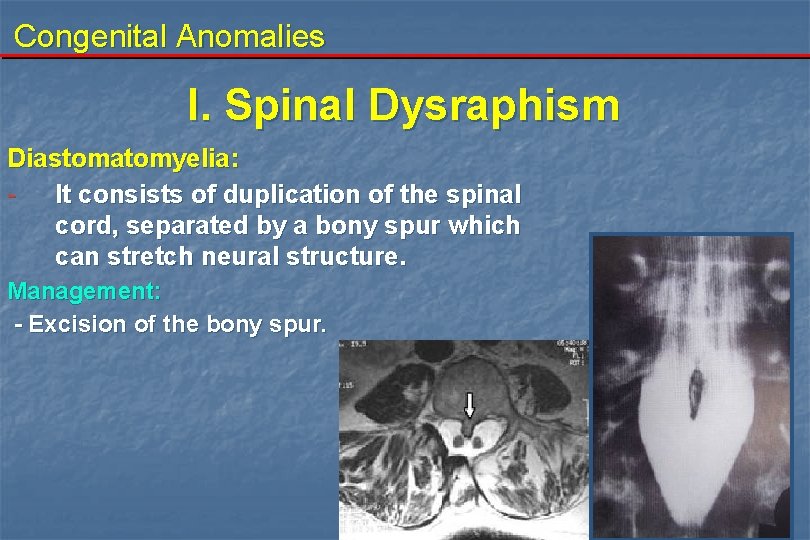
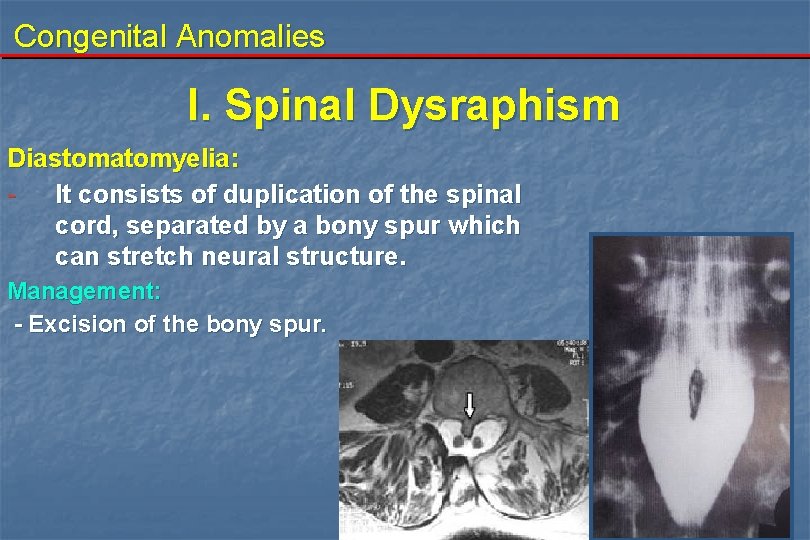
Congenital Anomalies I. Spinal Dysraphism Diastomatomyelia: - It consists of duplication of the spinal cord, separated by a bony spur which can stretch neural structure. Management: - Excision of the bony spur.
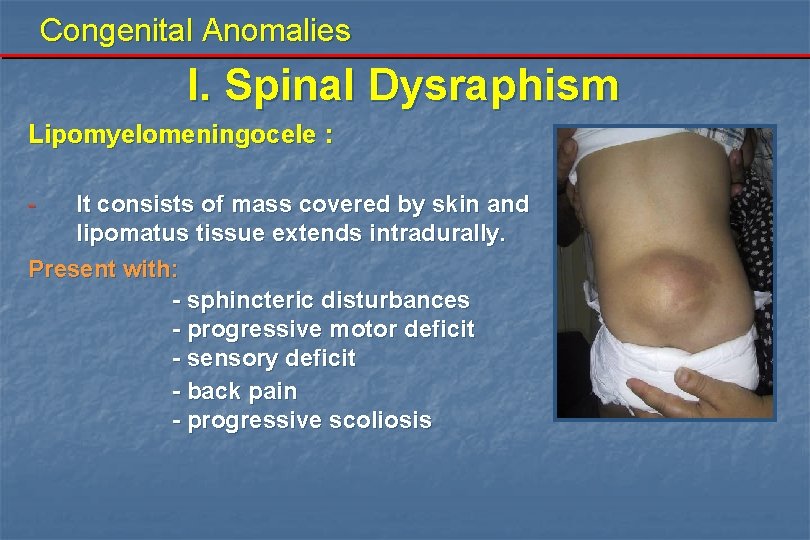
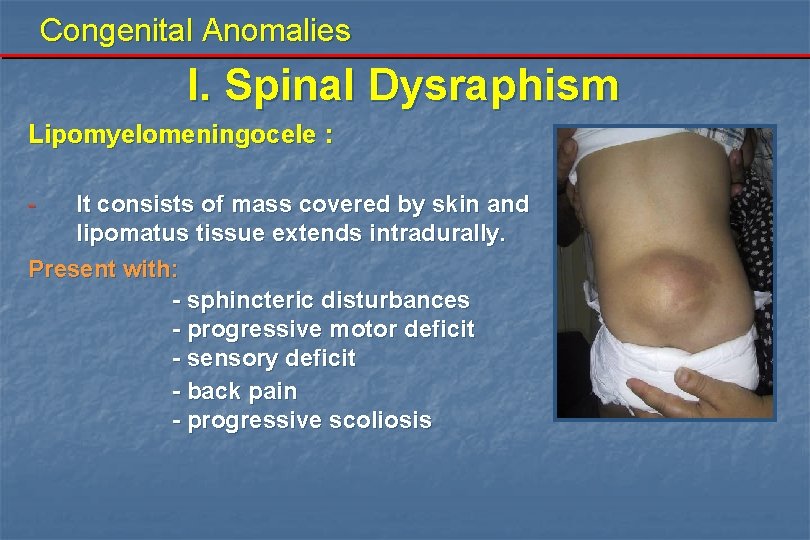
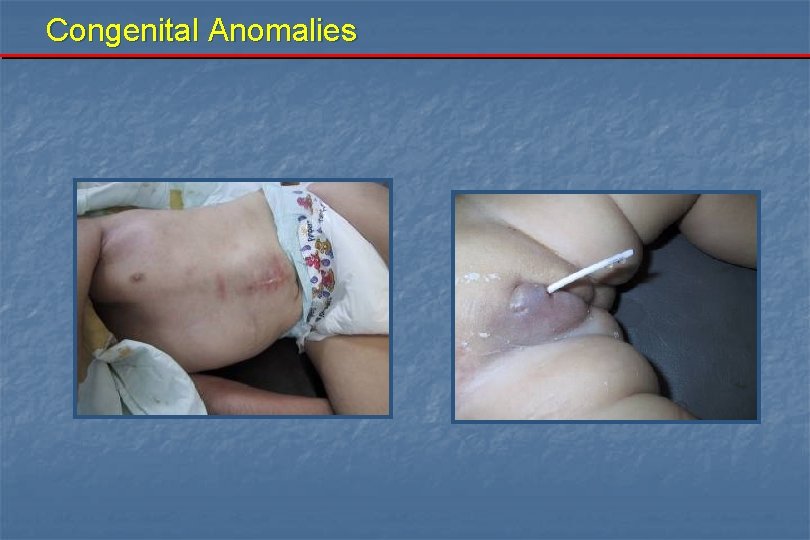
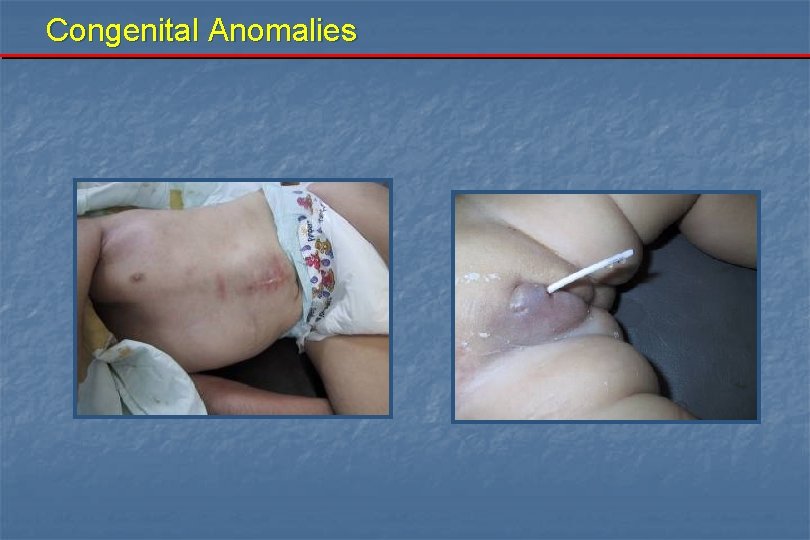
Congenital Anomalies I. Spinal Dysraphism Lipomyelomeningocele : - It consists of mass covered by skin and lipomatus tissue extends intradurally. Present with: - sphincteric disturbances - progressive motor deficit - sensory deficit - back pain - progressive scoliosis
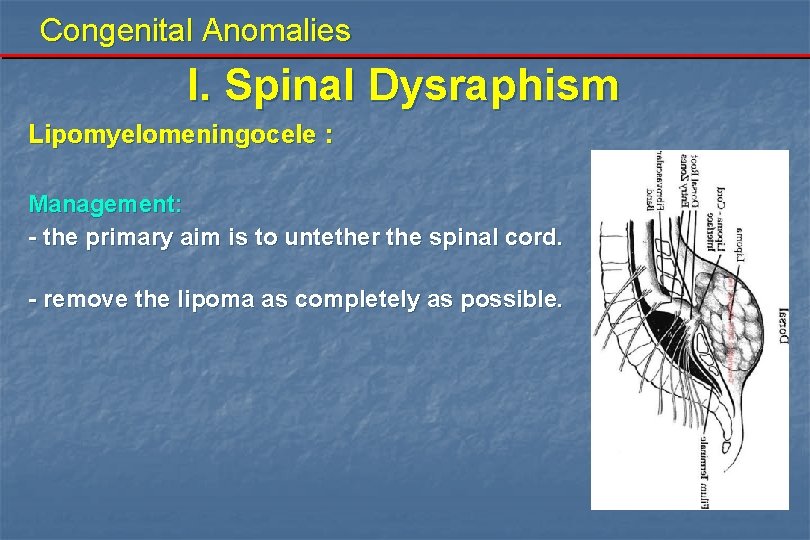
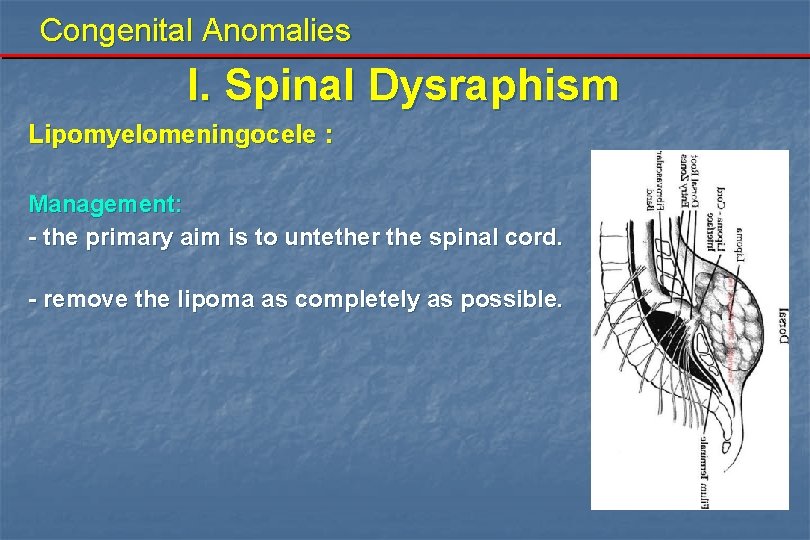
Congenital Anomalies I. Spinal Dysraphism Lipomyelomeningocele : Management: - the primary aim is to untether the spinal cord. - remove the lipoma as completely as possible.
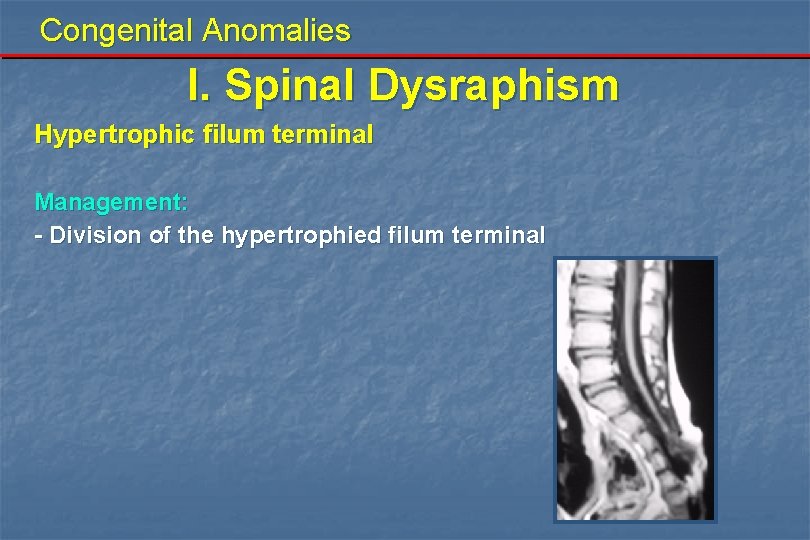
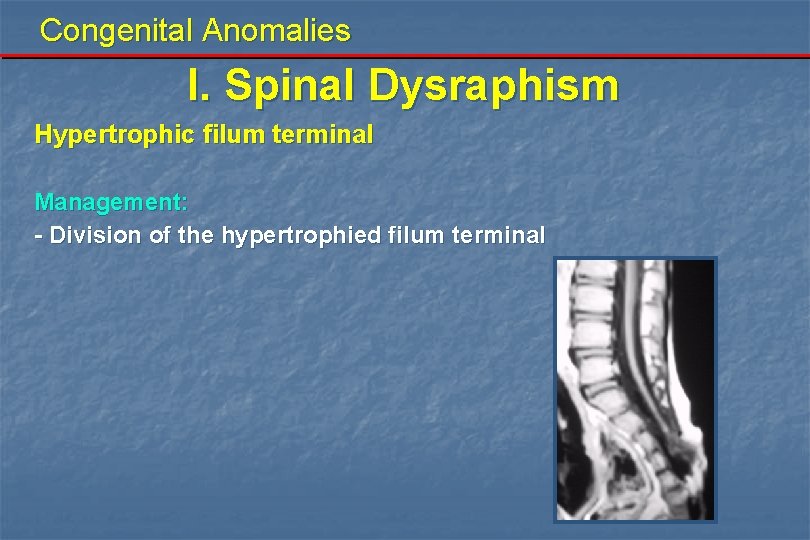
Congenital Anomalies I. Spinal Dysraphism Hypertrophic filum terminal Management: - Division of the hypertrophied filum terminal

Congenital Anomalies I. Spinal Dysraphism Spina bifida A bony defect in the lamina is frequently seen on X ray and is of no significance. May be discovered accidentally, or may be associated with nocturnal enuresis. The skin may show some marks as tuft of hair, or nevus.

Congenital Anomalies I. Spinal Dysraphism B. Spina bifida cystica: Herniation of neural elements through the skin as well as the bony defect. Obvious at birth. This occurs once in 300 live births. It can occur in the midline from the base of the skull to the lumbosacral region. 1 - Meningocele 2 - Meninomyelocele 3 - Rachisis
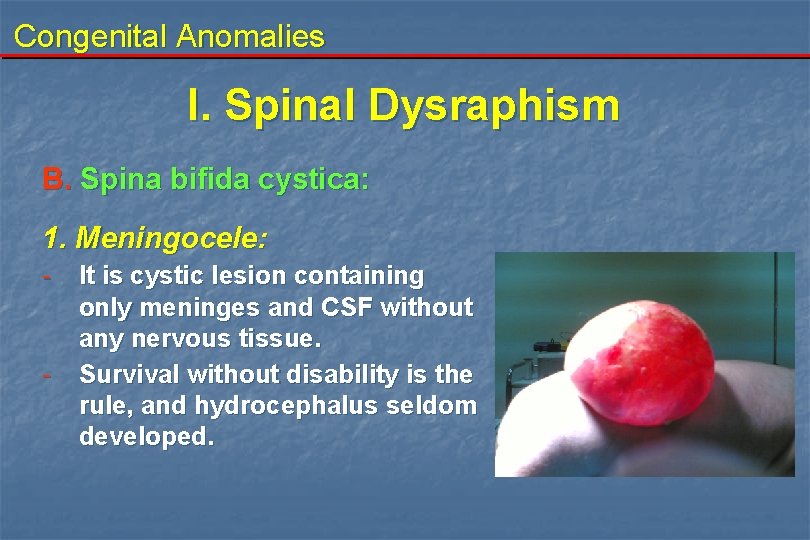
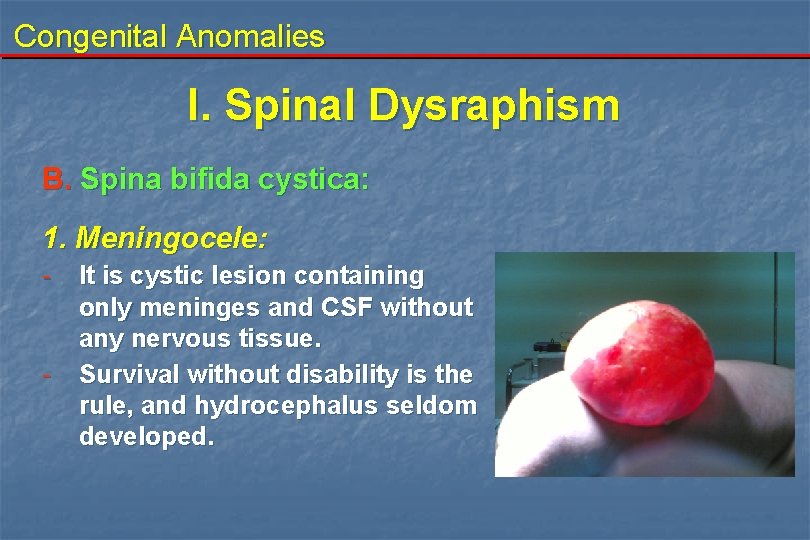
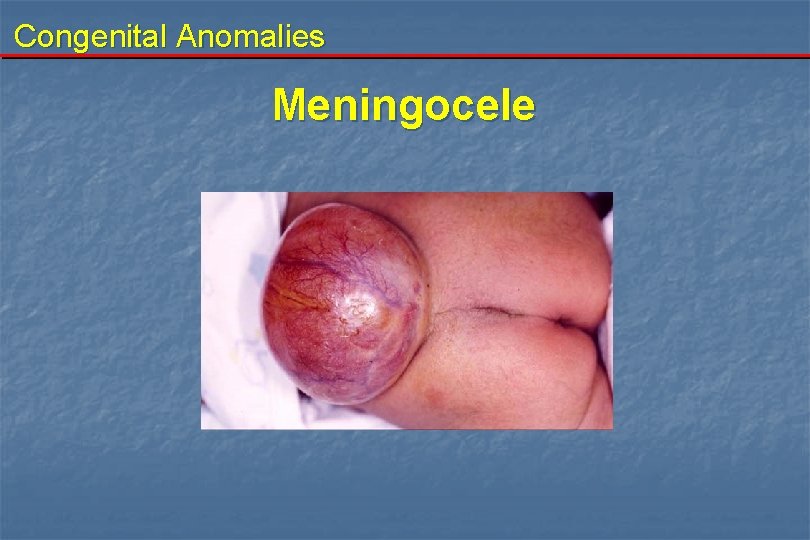
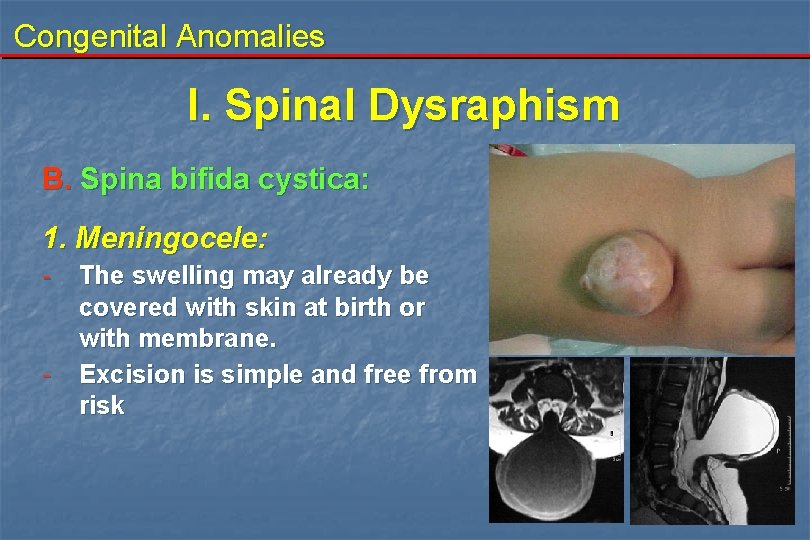
Congenital Anomalies I. Spinal Dysraphism B. Spina bifida cystica: 1. Meningocele: - - It is cystic lesion containing only meninges and CSF without any nervous tissue. Survival without disability is the rule, and hydrocephalus seldom developed.
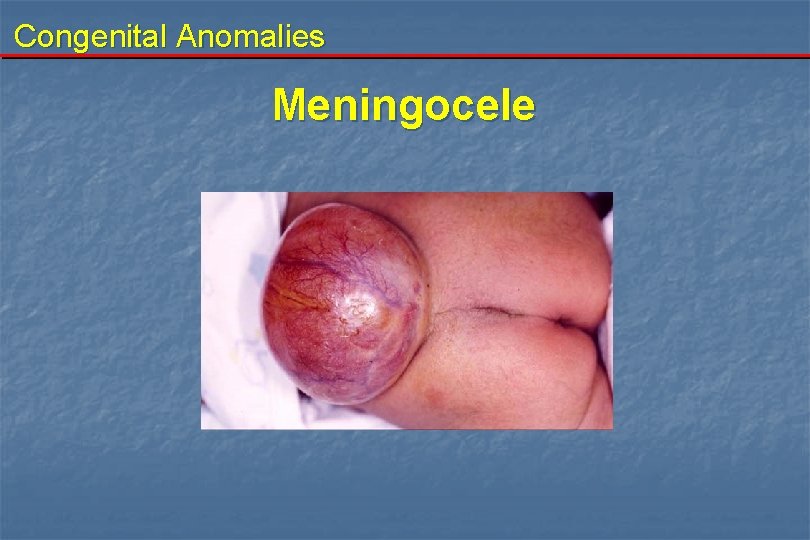
Congenital Anomalies Meningocele
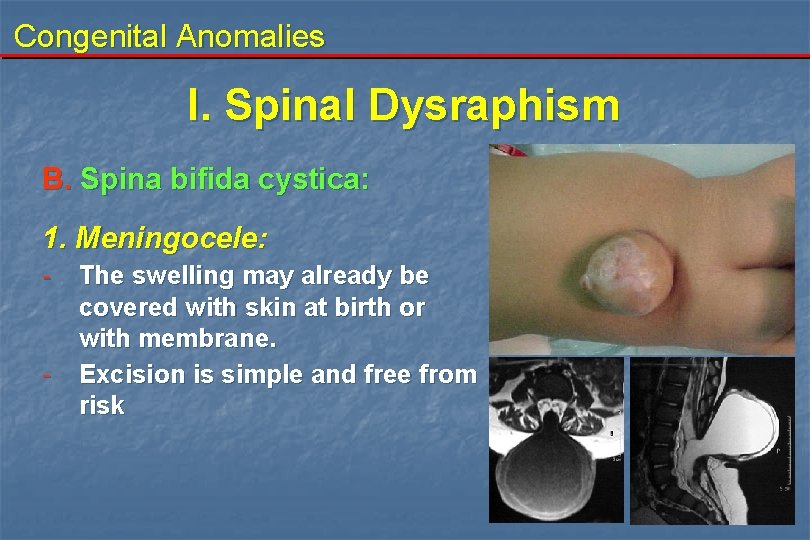
Congenital Anomalies I. Spinal Dysraphism B. Spina bifida cystica: 1. Meningocele: - - The swelling may already be covered with skin at birth or with membrane. Excision is simple and free from risk

Congenital Anomalies I. Spinal Dysraphism B. Spina bifida cystica: 2. Meningomyelocele: - It is much more serious anomaly. The swelling contains neural elements (cord or roots). 80% in the lumbosacral region. Some degree of paralysis of the lower limbs and sphincteric disturbance are present.

Congenital Anomalies I. Spinal Dysraphism B. Spina bifida cystica: 2. Meningomyelocele: - - 65% of the cases develop hydrocephalus with cerebellar ectopia (Chiari malformation). Associated with other congenital anomalies (TEV, PDA)
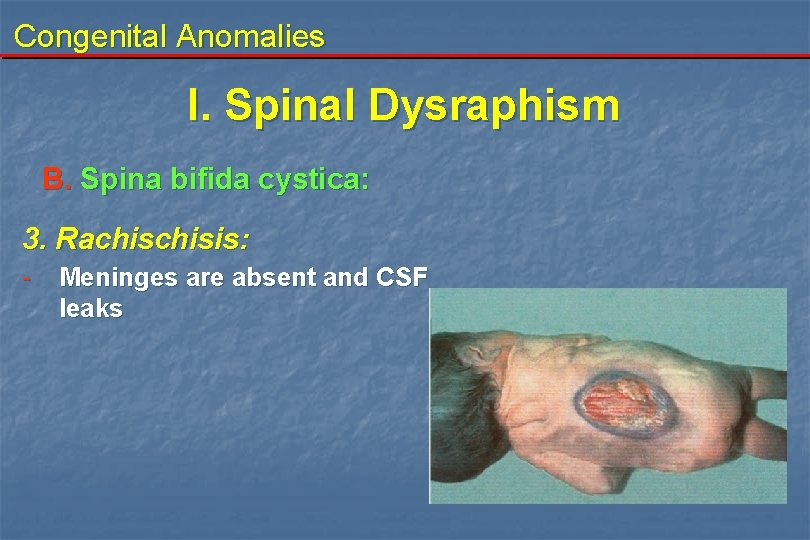
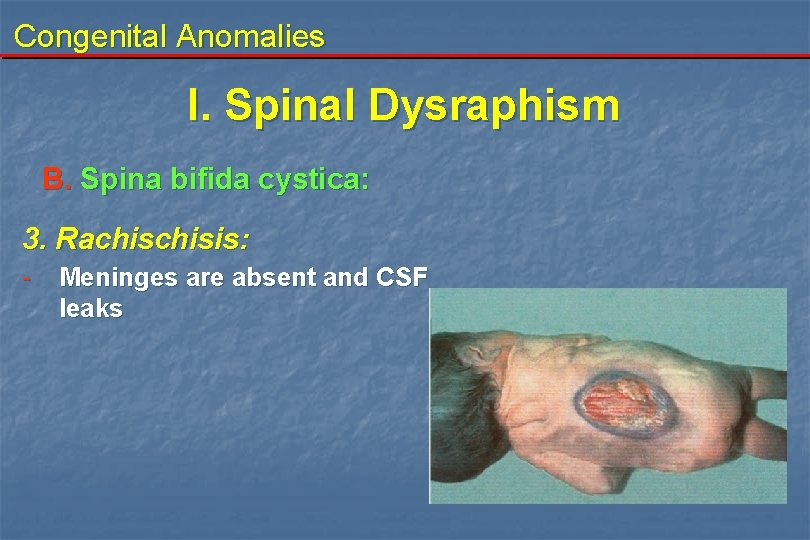
Congenital Anomalies I. Spinal Dysraphism B. Spina bifida cystica: 3. Rachisis: - Meninges are absent and CSF leaks
Congenital Anomalies I. Spinal Dysraphism Examination: 1 - Swelling: - - since birth - cystic swelling - in the midline , moe common in the lumbosacral region - cross flactuation with anterior fontanelle - bulge on crying - ruptures →CSF leak - transillumiation (depends upon the type) - ruptures →CSF leak 2 - Neurological: - motor - sphincteric 3 - Other systems (Head, GIT, GU, CVS, foot)
Congenital Anomalies I. Spinal Dysraphism Investigations: 1. Prenatal diagnosis: - Foetal U/S - alpha foetoprotein measured in: - maternal serum - amniotic fluid 2. Plain X-ray 3. CT scan 4. MRI
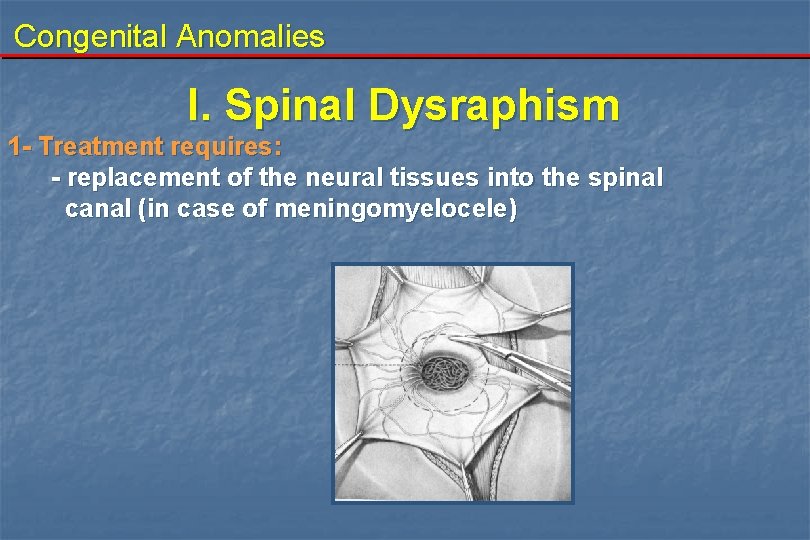
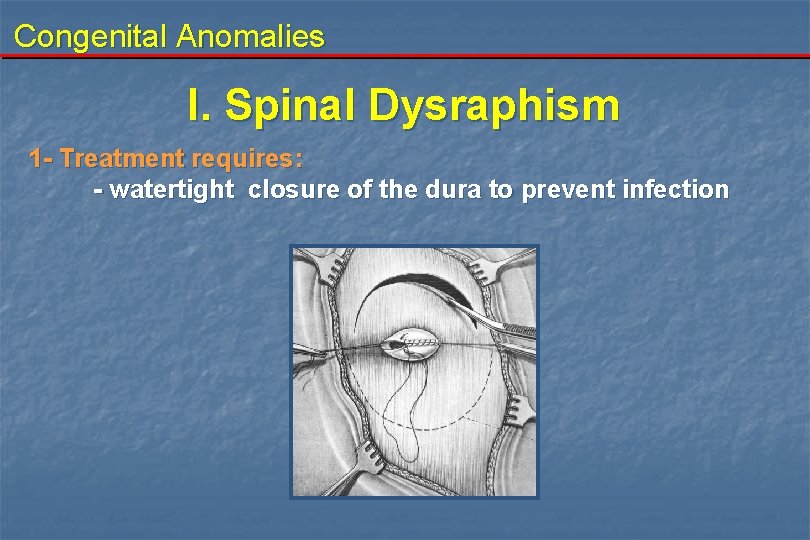
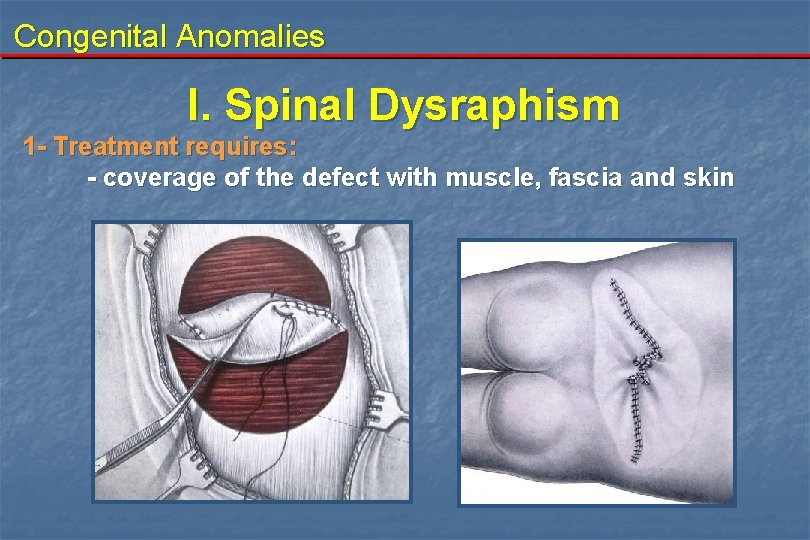
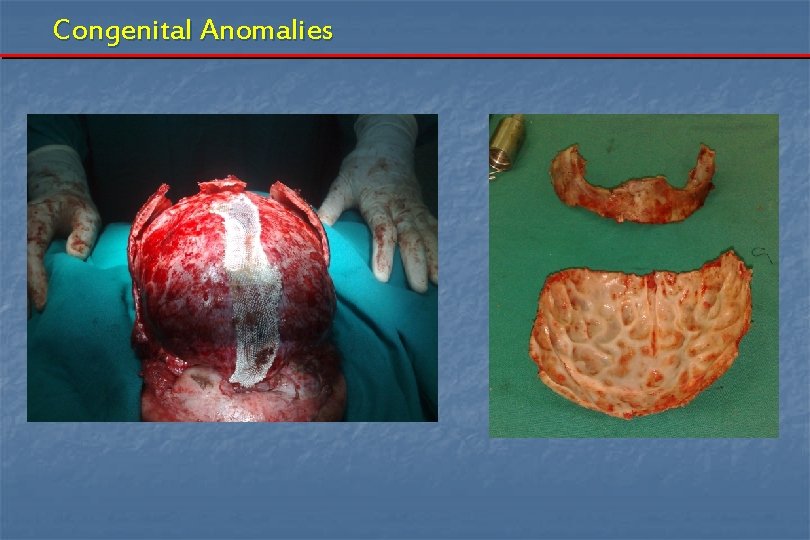
Congenital Anomalies I. Spinal Dysraphism B. Spina bifida cystica: Treatment: 1 - Treatment requires: - excision of the sac - replacement of the neural tissues into the spinal canal (in case of meningomyelocele) - watertight closure of the dura to prevent infection - coverage of the defect with muscle, fascia and skin 2 - Treatment of other associated anomalies 3 - Treatment requires a multidisciplinary approach
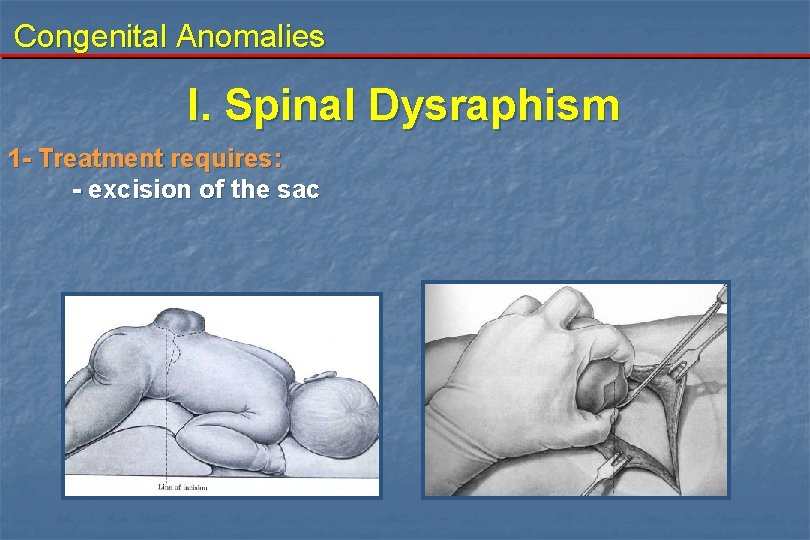
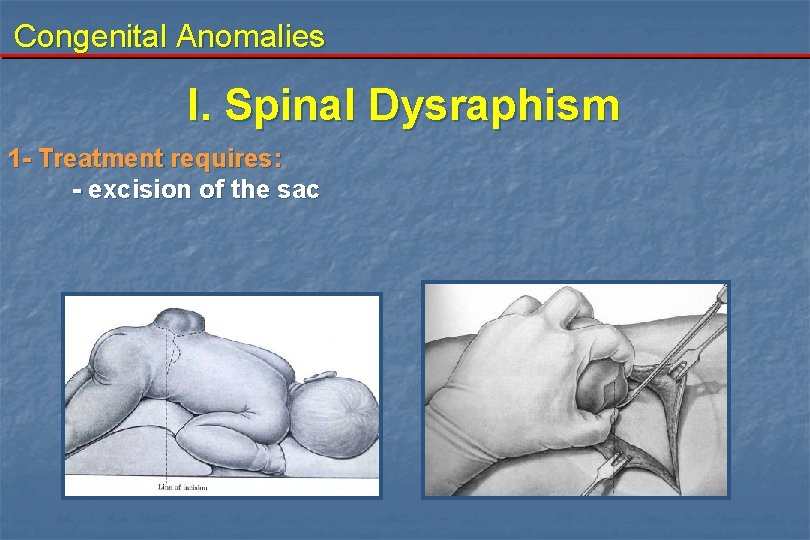
Congenital Anomalies I. Spinal Dysraphism 1 - Treatment requires: - excision of the sac
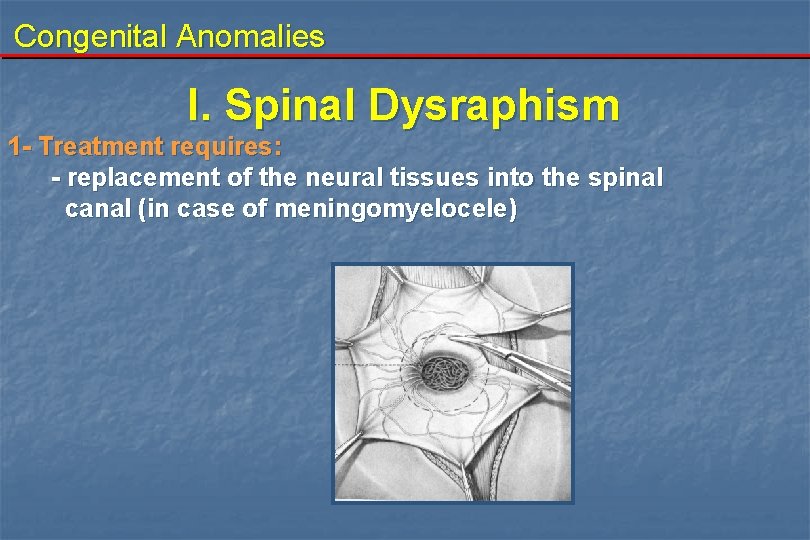
Congenital Anomalies I. Spinal Dysraphism 1 - Treatment requires: - replacement of the neural tissues into the spinal canal (in case of meningomyelocele)
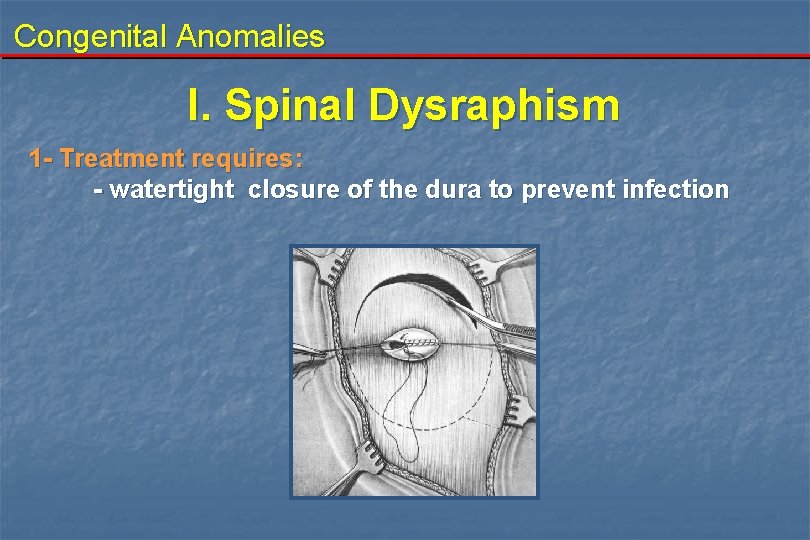
Congenital Anomalies I. Spinal Dysraphism 1 - Treatment requires: - watertight closure of the dura to prevent infection
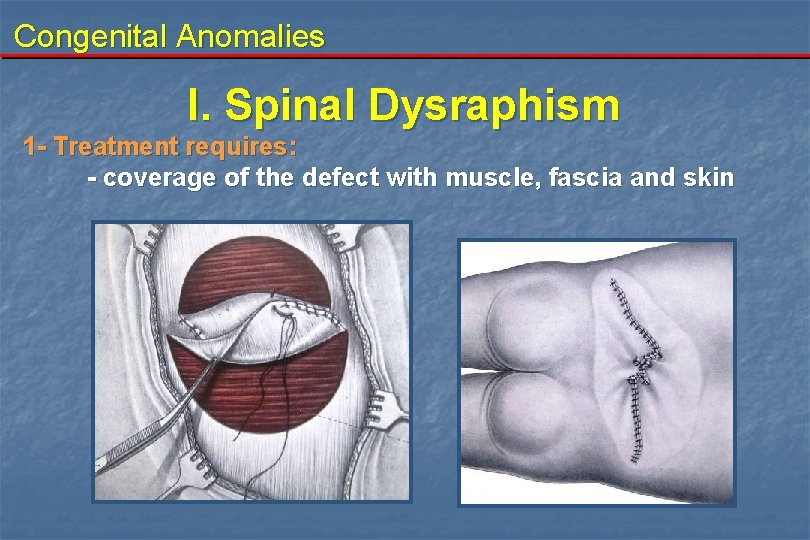
Congenital Anomalies I. Spinal Dysraphism 1 - Treatment requires: - coverage of the defect with muscle, fascia and skin
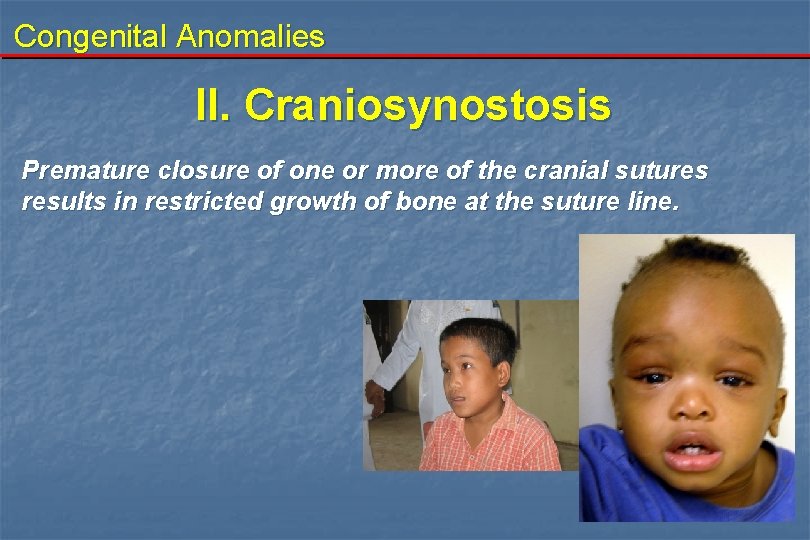
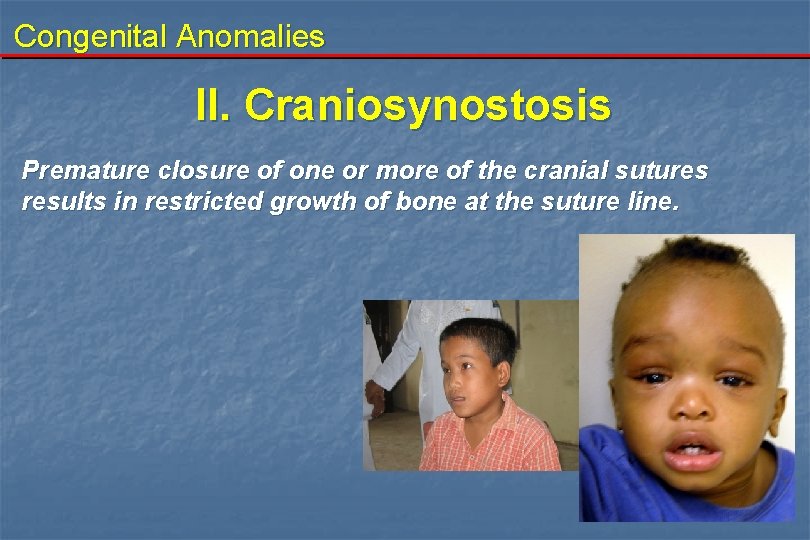
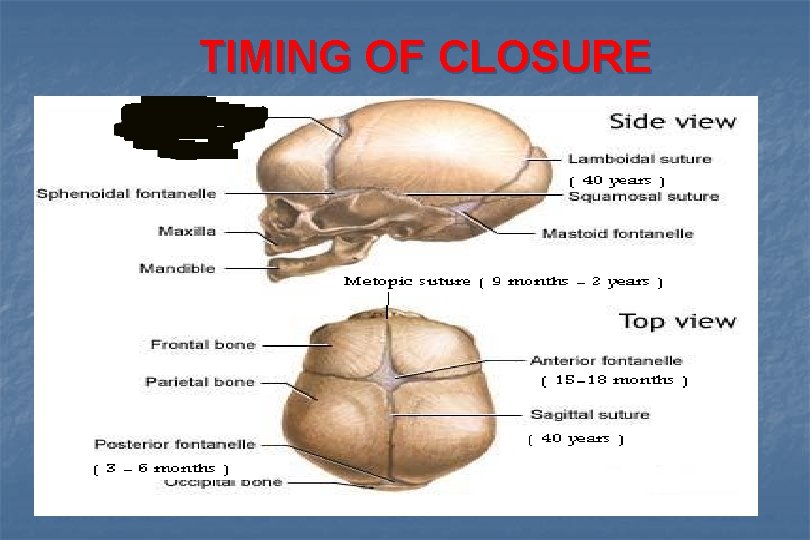
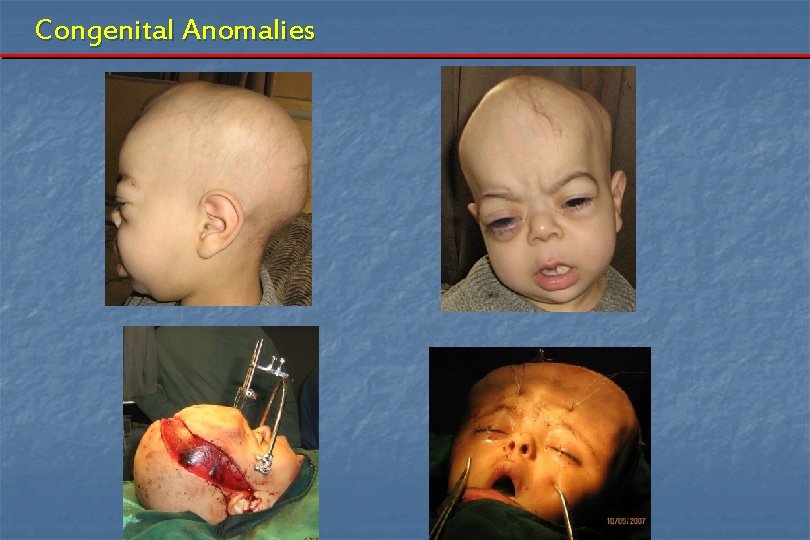
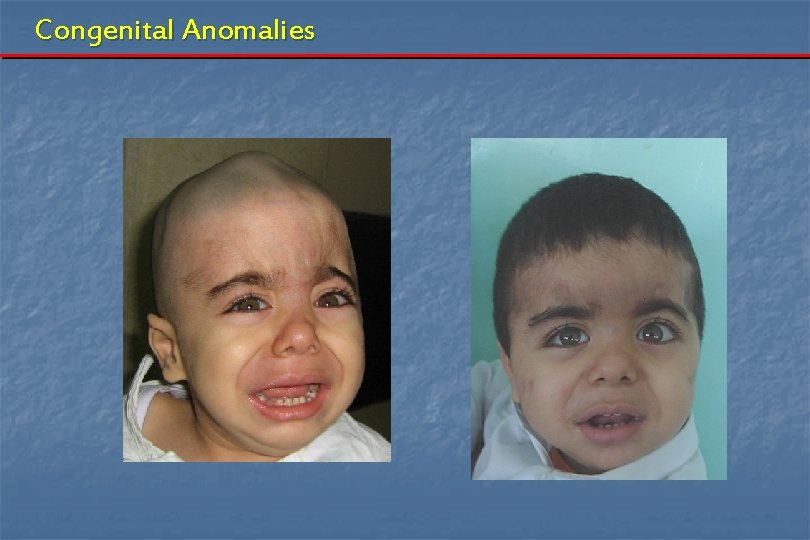
Congenital Anomalies II. Craniosynostosis Premature closure of one or more of the cranial sutures results in restricted growth of bone at the suture line.
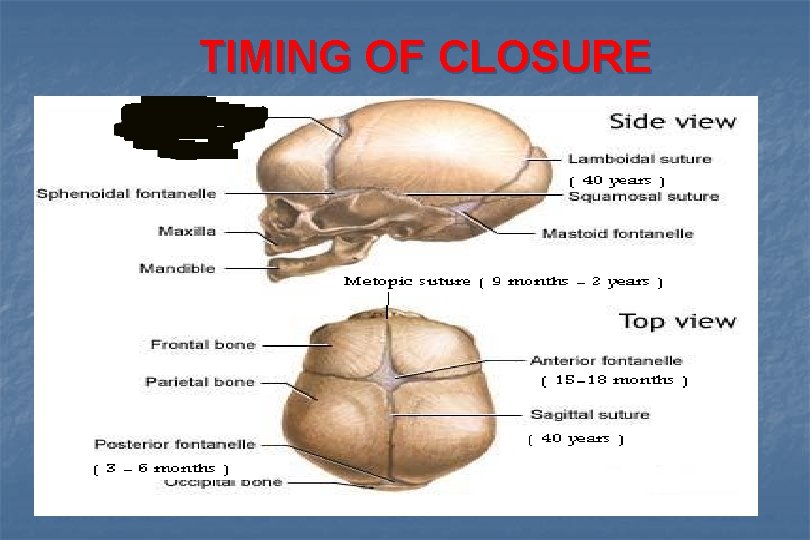
TIMING OF CLOSURE
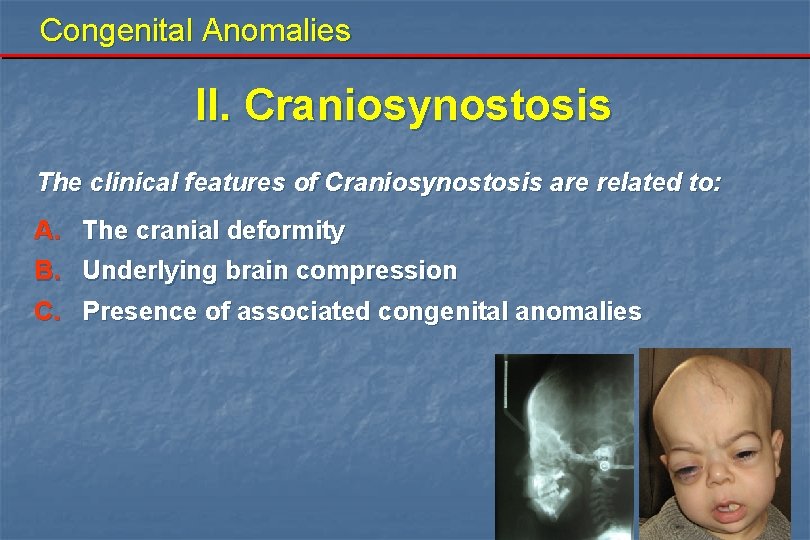
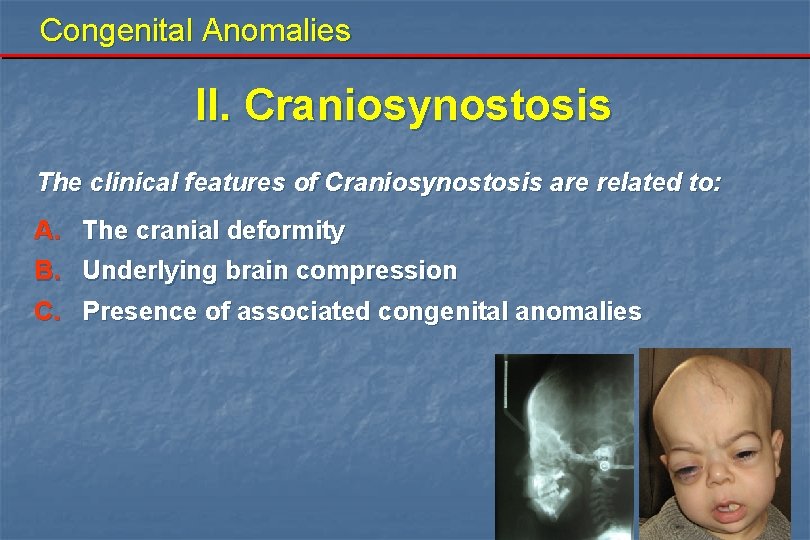
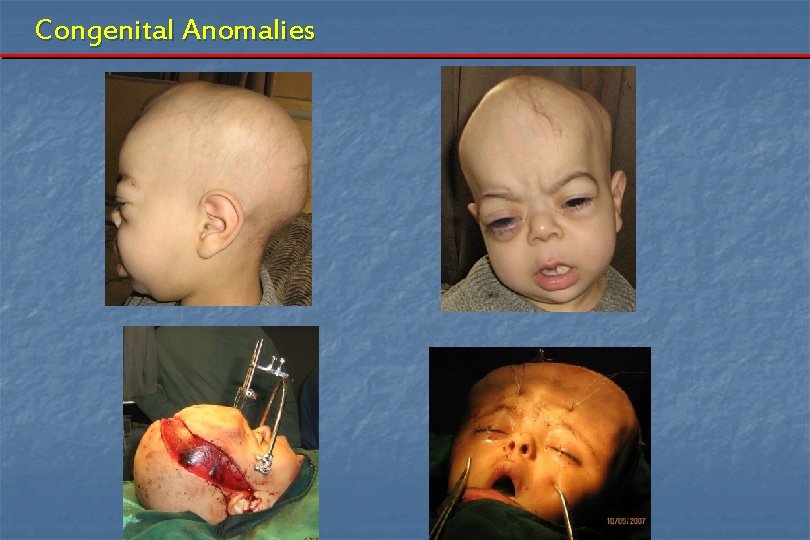
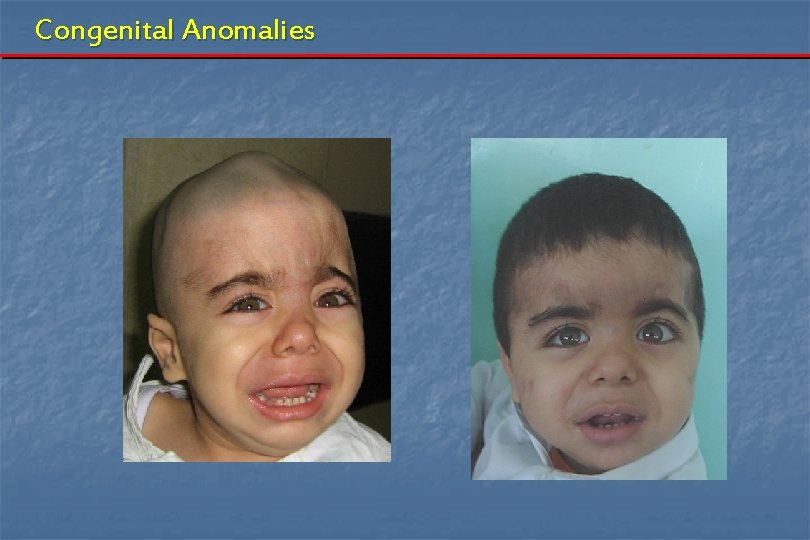
Congenital Anomalies II. Craniosynostosis The clinical features of Craniosynostosis are related to: A. The cranial deformity B. Underlying brain compression C. Presence of associated congenital anomalies
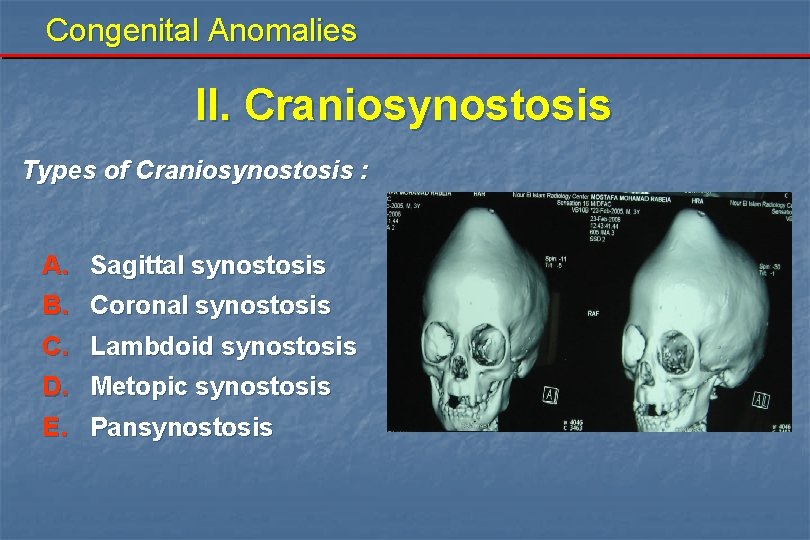
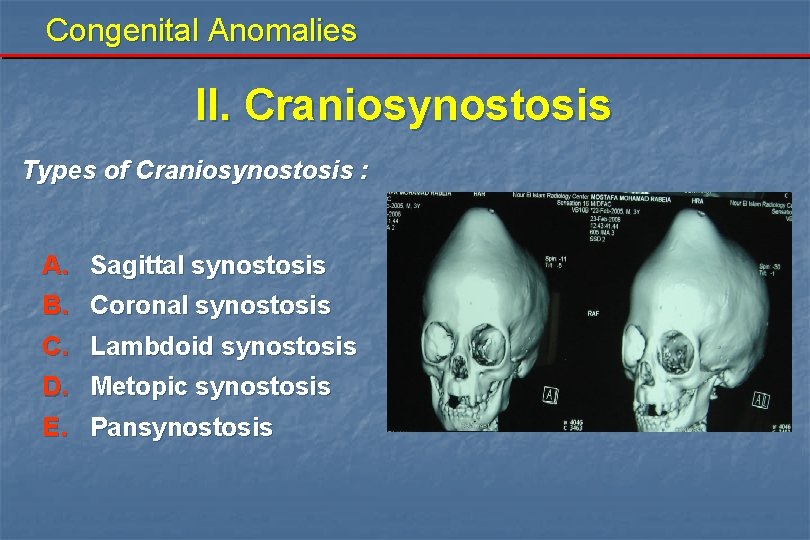
Congenital Anomalies II. Craniosynostosis Types of Craniosynostosis : A. Sagittal synostosis B. Coronal synostosis C. Lambdoid synostosis D. E. Metopic synostosis Pansynostosis
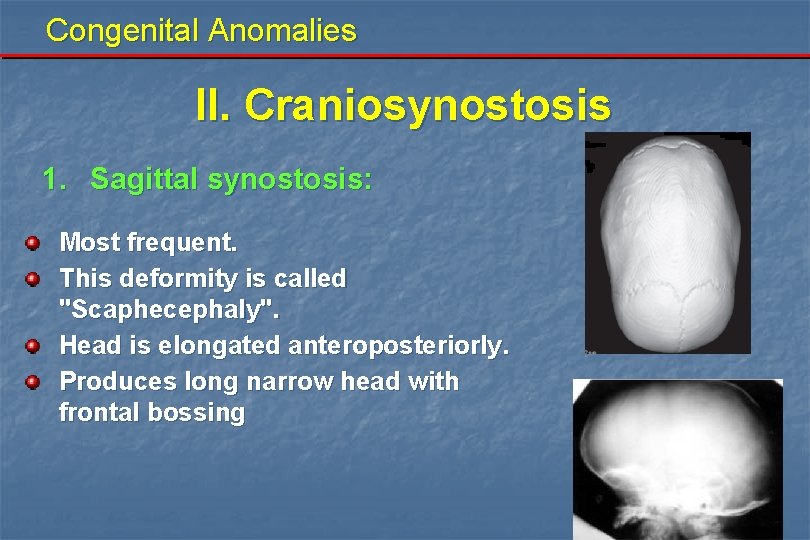
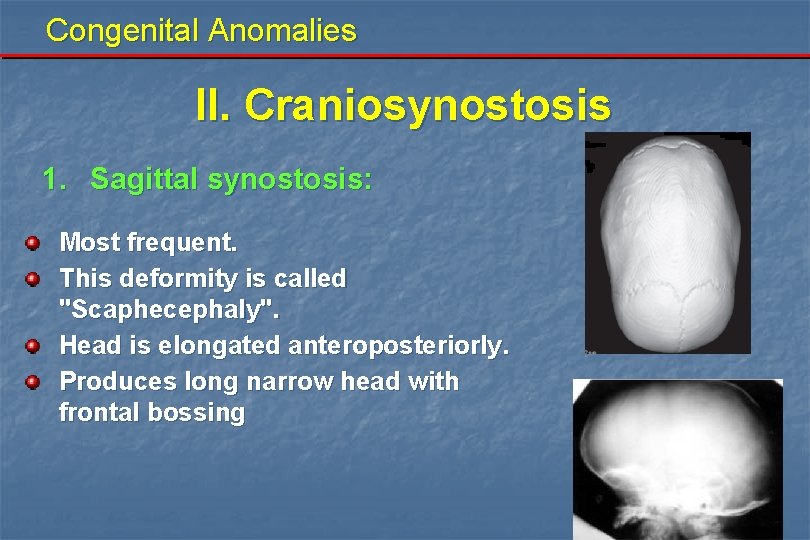
Congenital Anomalies II. Craniosynostosis 1. Sagittal synostosis: Most frequent. This deformity is called "Scaphecephaly". Head is elongated anteroposteriorly. Produces long narrow head with frontal bossing

Congenital Anomalies II. Craniosynostosis 2. Coronal synostosis: It is either bilateral or unilateral. Expansion occurs in the superior and lateral direction. Produces a short anterior cranial fossa, shallow orbits and hypertelorism

Congenital Anomalies II. Craniosynostosis 2. Coronal synostosis: Congenital defects with Crouzon's and Apert's syndromes This deformity is called "Brachycephaly“ if bilateral. “anterior plagiocephaly“ if unilateral.
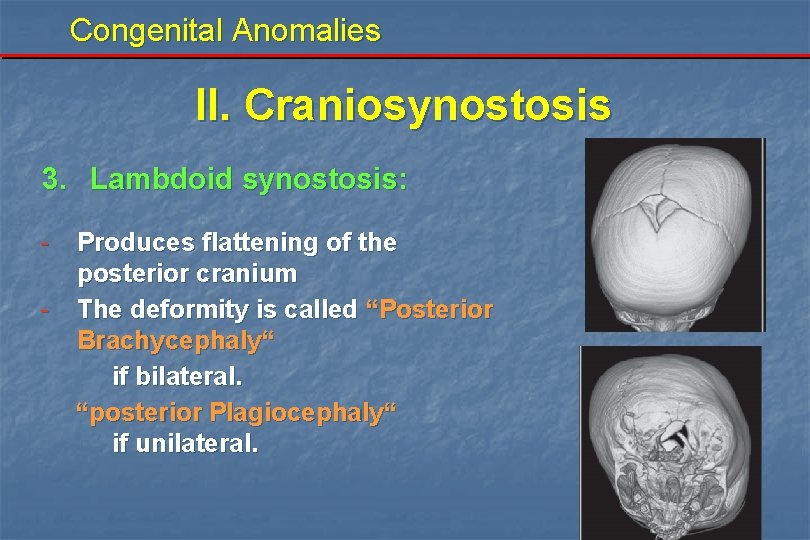
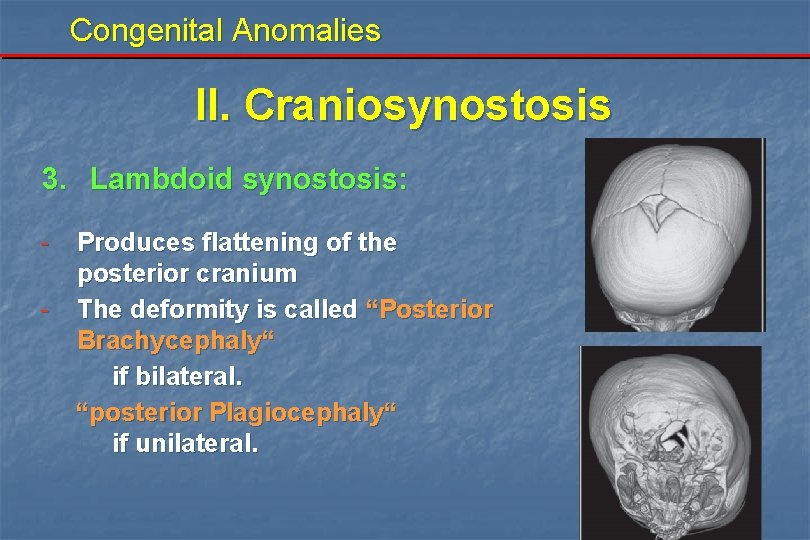
Congenital Anomalies II. Craniosynostosis 3. Lambdoid synostosis: - Produces flattening of the posterior cranium The deformity is called “Posterior Brachycephaly“ if bilateral. “posterior Plagiocephaly“ if unilateral.
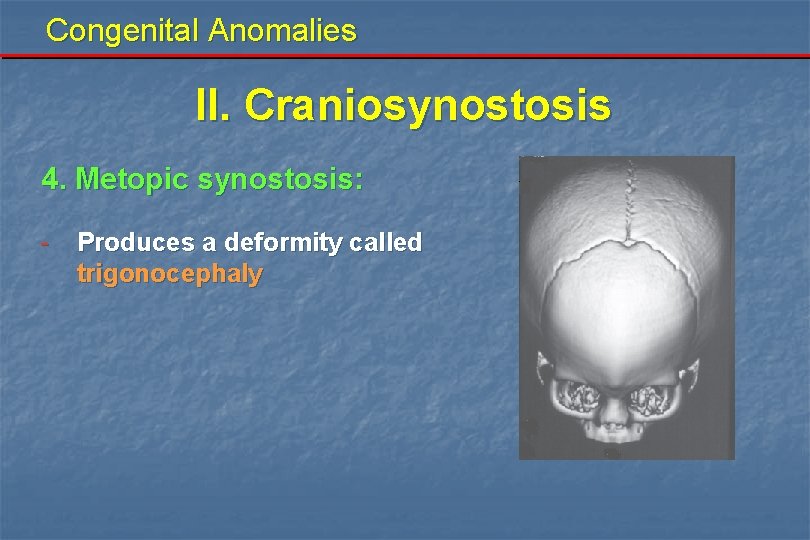
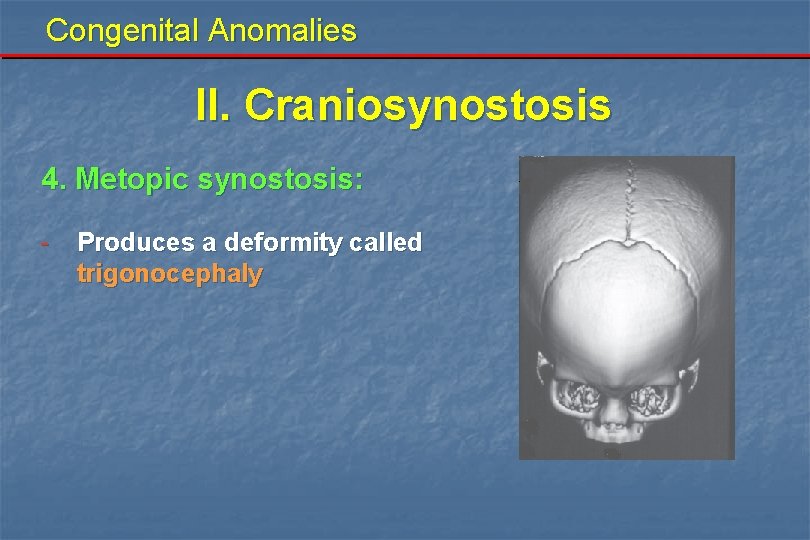
Congenital Anomalies II. Craniosynostosis 4. Metopic synostosis: - Produces a deformity called trigonocephaly
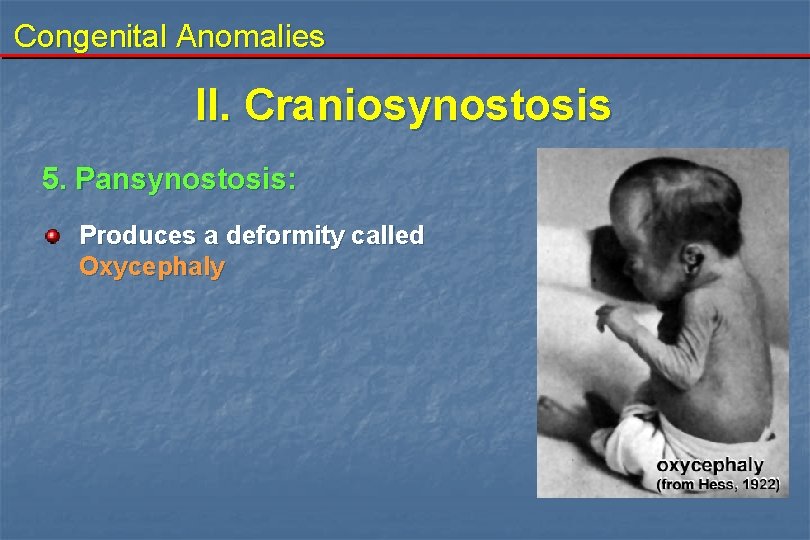
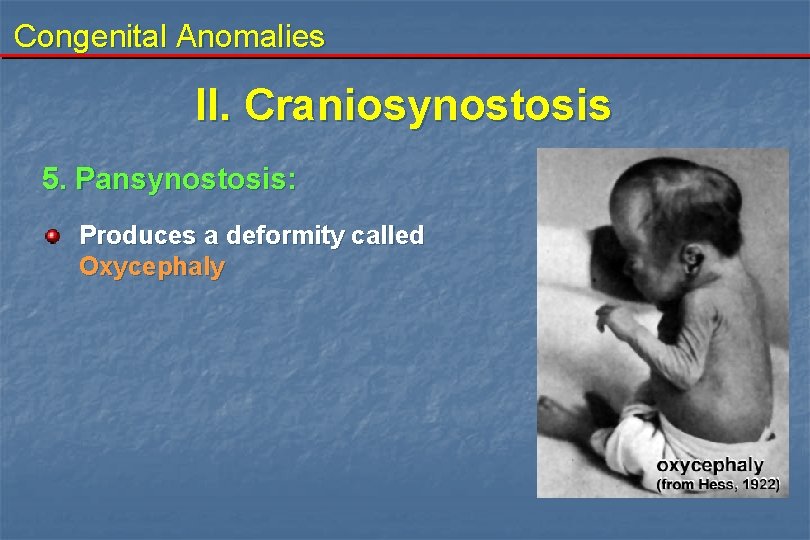
Congenital Anomalies II. Craniosynostosis 5. Pansynostosis: Produces a deformity called Oxycephaly

Congenital Anomalies II. Craniosynostosis Investigations: 1. Prenatal diagnosis: - Foetal U/S - alpha foetoprotein measured in: - maternal serum - amniotic fluid 2. 3. 4. 5. Plain X-ray CT scan (3 D CT) MRI Radioisotpe scanning
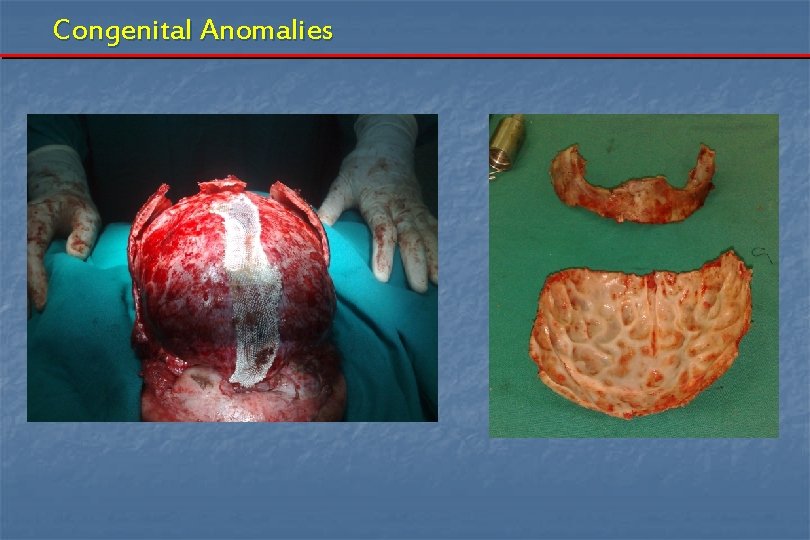
Congenital Anomalies II. Craniosynostosis Treatment: Surgery is performed to: 1 - correct the cranial deformity 2 - relieve the effects of cranial compression Surgery include: 1 - simple ressection of the suture 2 - extensive craniofacial surgery, correcting both cranial and orbital deformities.
Congenital Anomalies
Congenital Anomalies
Congenital Anomalies

Congenital Anomalies
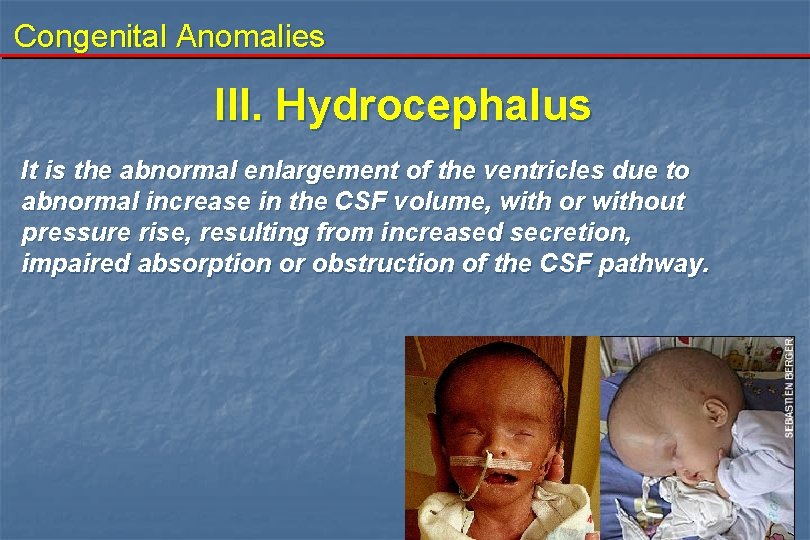
Congenital Anomalies III. Hydrocephalus It is the abnormal enlargement of the ventricles due to abnormal increase in the CSF volume, with or without pressure rise, resulting from increased secretion, impaired absorption or obstruction of the CSF pathway.
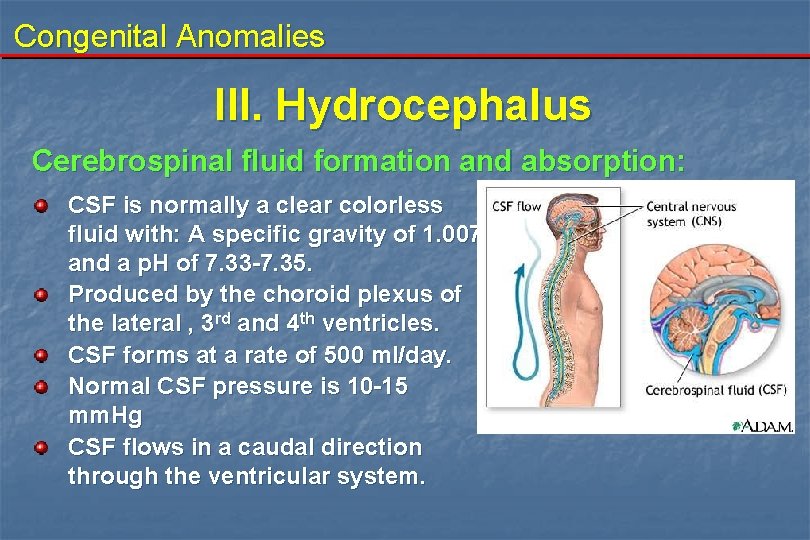
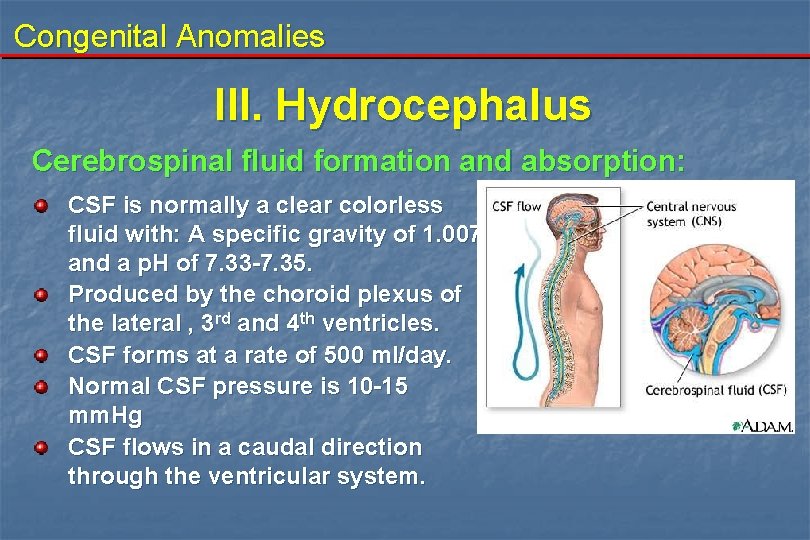
Congenital Anomalies III. Hydrocephalus Cerebrospinal fluid formation and absorption: CSF is normally a clear colorless fluid with: A specific gravity of 1. 007 and a p. H of 7. 33 -7. 35. Produced by the choroid plexus of the lateral , 3 rd and 4 th ventricles. CSF forms at a rate of 500 ml/day. Normal CSF pressure is 10 -15 mm. Hg CSF flows in a caudal direction through the ventricular system.
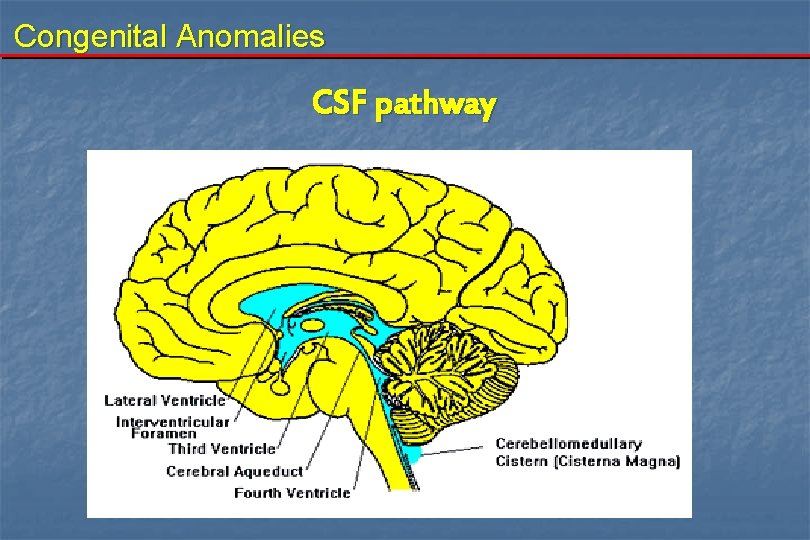
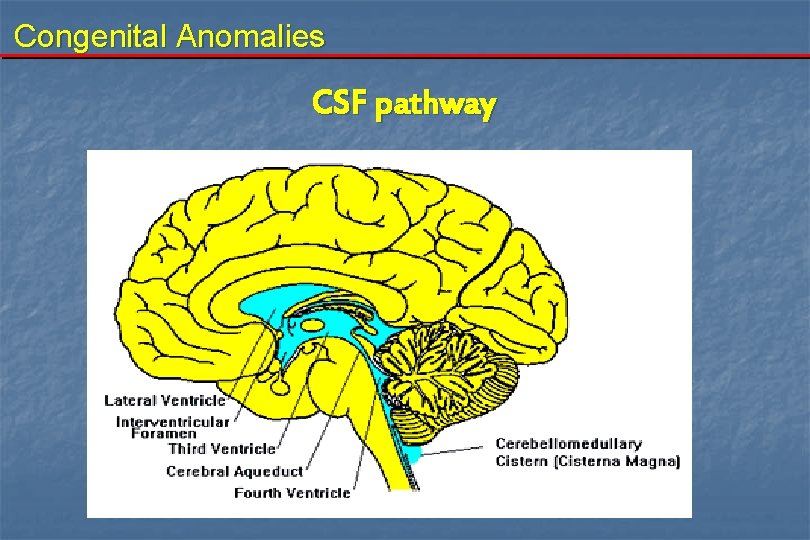
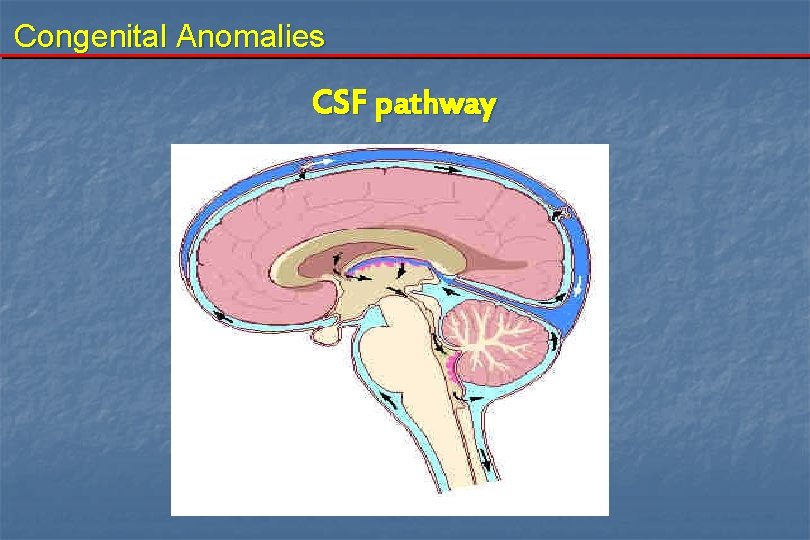
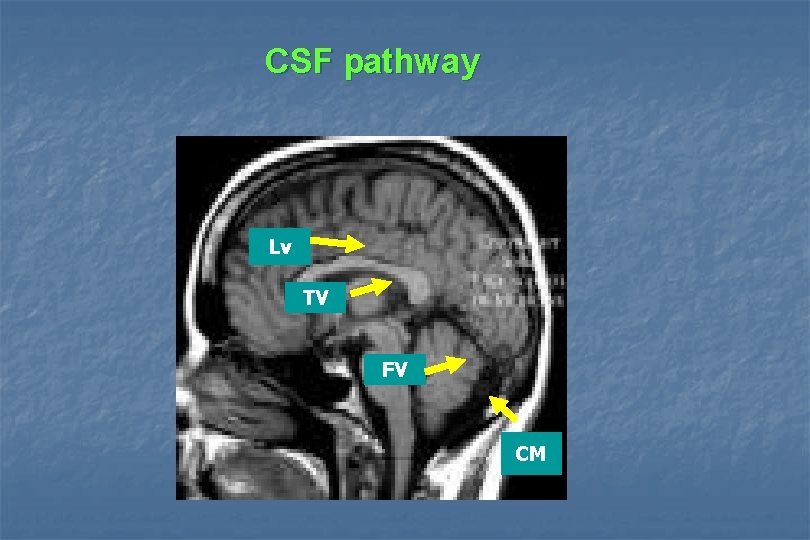
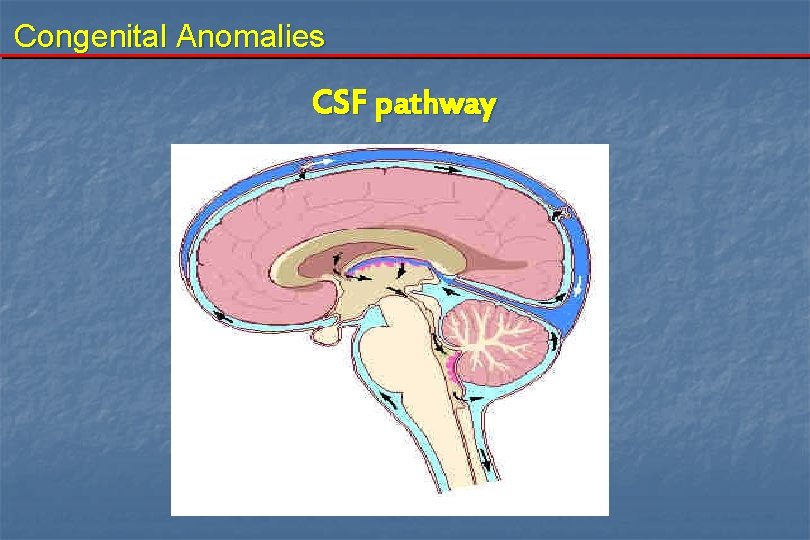
Congenital Anomalies CSF pathway
Congenital Anomalies CSF pathway
Congenital Anomalies III. Hydrocephalus Classification: 1. Obstructive (non communicating) 2. Non obstructive (communicating)
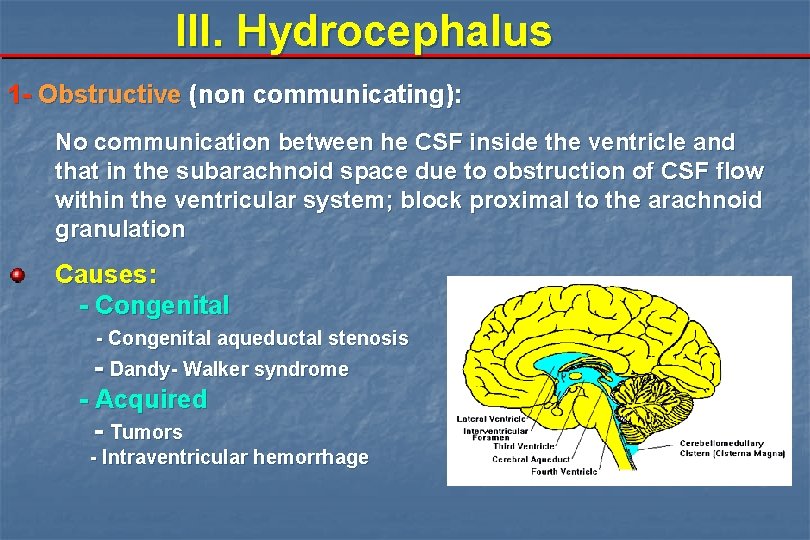
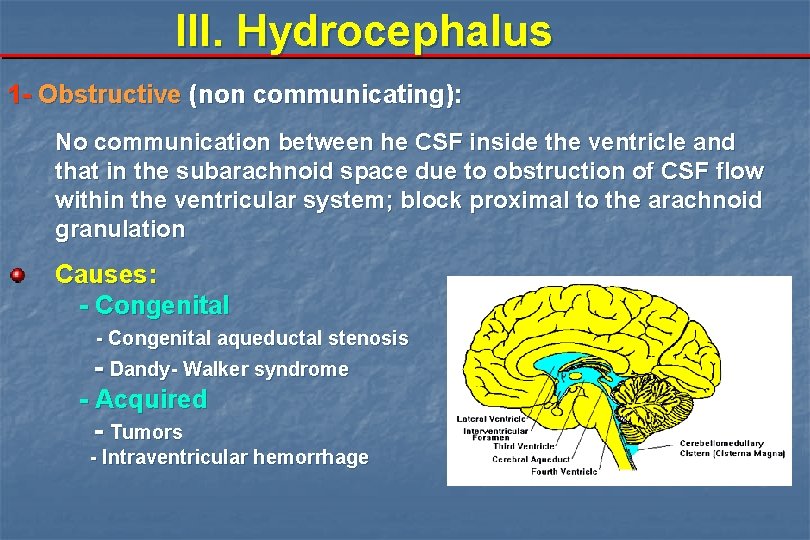
III. Hydrocephalus 1 - Obstructive (non communicating): No communication between he CSF inside the ventricle and that in the subarachnoid space due to obstruction of CSF flow within the ventricular system; block proximal to the arachnoid granulation Causes: - Congenital aqueductal stenosis - Dandy- Walker syndrome - Acquired - Tumors - Intraventricular hemorrhage
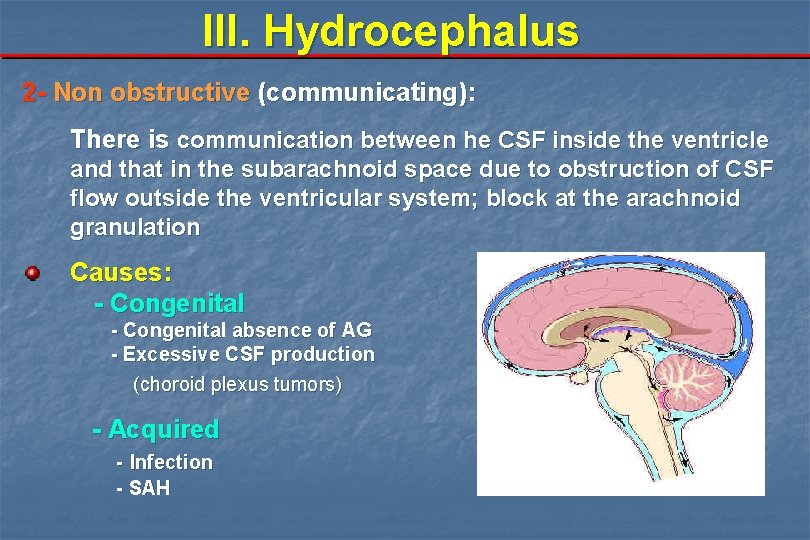
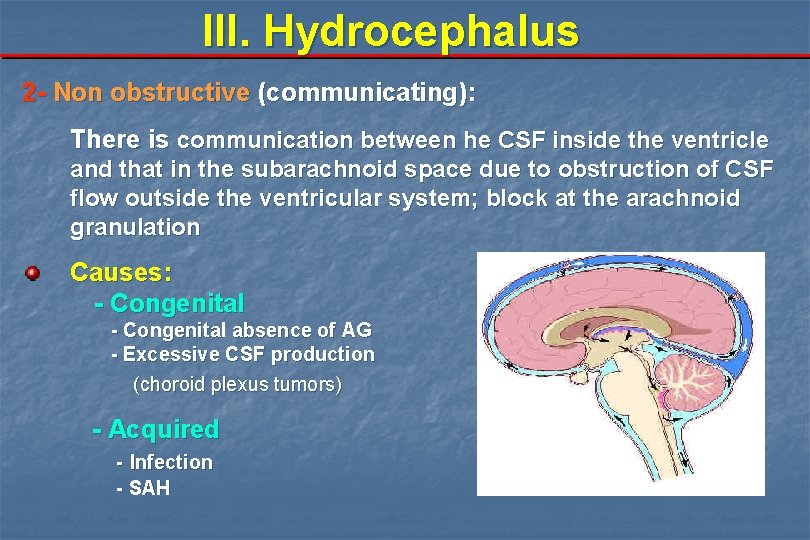
III. Hydrocephalus 2 - Non obstructive (communicating): There is communication between he CSF inside the ventricle and that in the subarachnoid space due to obstruction of CSF flow outside the ventricular system; block at the arachnoid granulation Causes: - Congenital absence of AG - Excessive CSF production (choroid plexus tumors) - Acquired - Infection - SAH
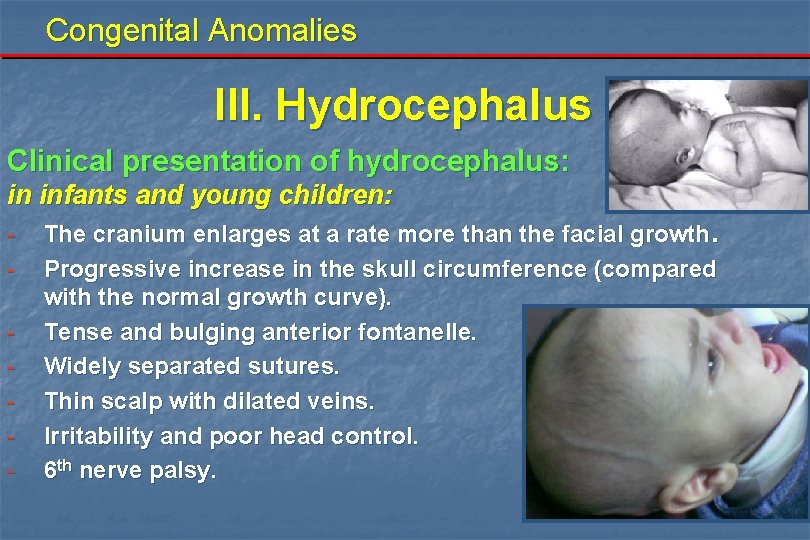
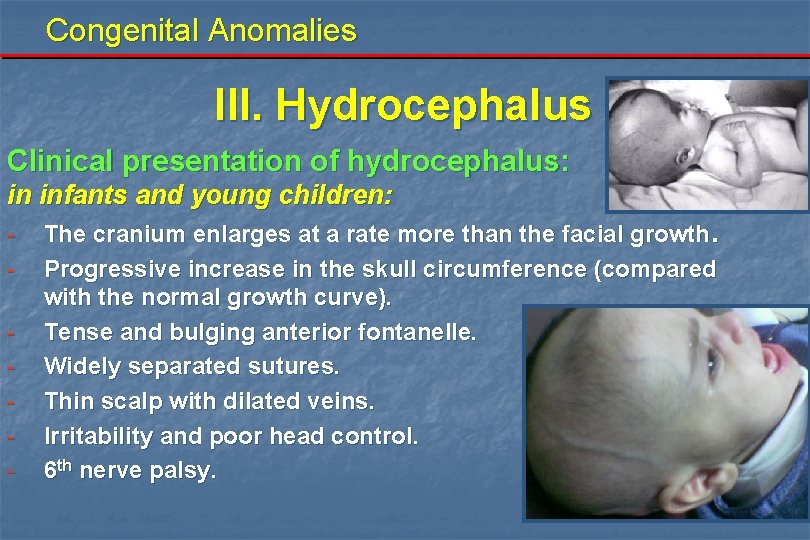
Congenital Anomalies III. Hydrocephalus Clinical presentation of hydrocephalus: in infants and young children: - The cranium enlarges at a rate more than the facial growth. Progressive increase in the skull circumference (compared with the normal growth curve). Tense and bulging anterior fontanelle. Widely separated sutures. Thin scalp with dilated veins. Irritability and poor head control. 6 th nerve palsy.
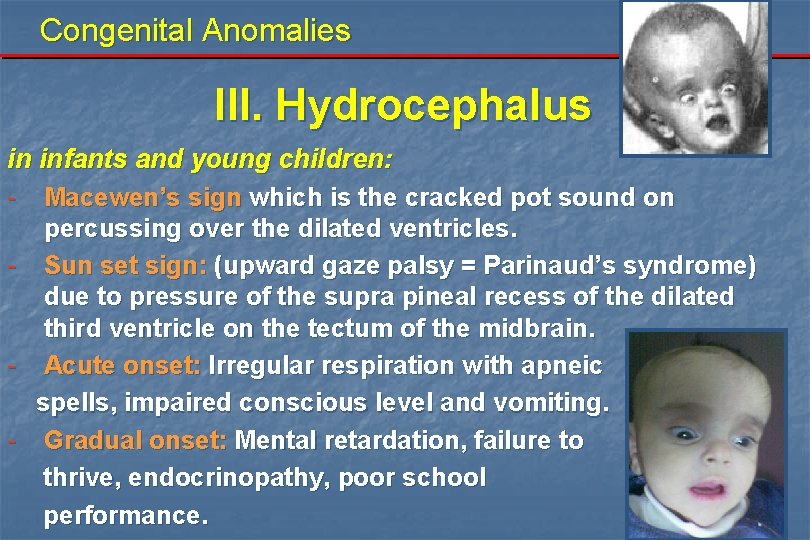
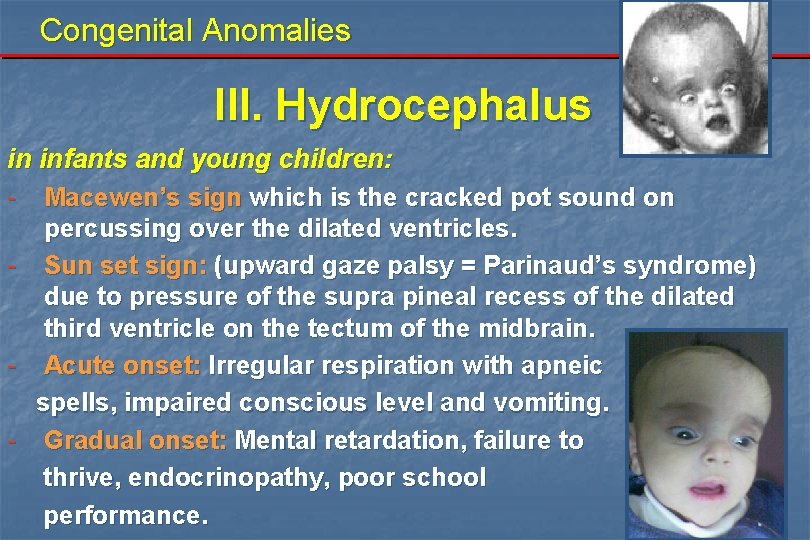
Congenital Anomalies III. Hydrocephalus in infants and young children: - Macewen’s sign which is the cracked pot sound on percussing over the dilated ventricles. - Sun set sign: (upward gaze palsy = Parinaud’s syndrome) due to pressure of the supra pineal recess of the dilated third ventricle on the tectum of the midbrain. - Acute onset: Irregular respiration with apneic spells, impaired conscious level and vomiting. - Gradual onset: Mental retardation, failure to thrive, endocrinopathy, poor school performance.
Congenital Anomalies III. Hydrocephalus Clinical presentation of hydrocephalus: In adults: - Manifestations of increased ICP including: - headache - vomiting - blurring of vision due to papilloedema - drowsiness - gait disturbance, ataxia, nystagmus - diplopia due to 6 th nerve palsy
Congenital Anomalies III. Hydrocephalus Differential diagnosis: Chronic infantile subdural hematoma. Familial. Rickets. Space occupying lesion (tumors, abscess, cyst).
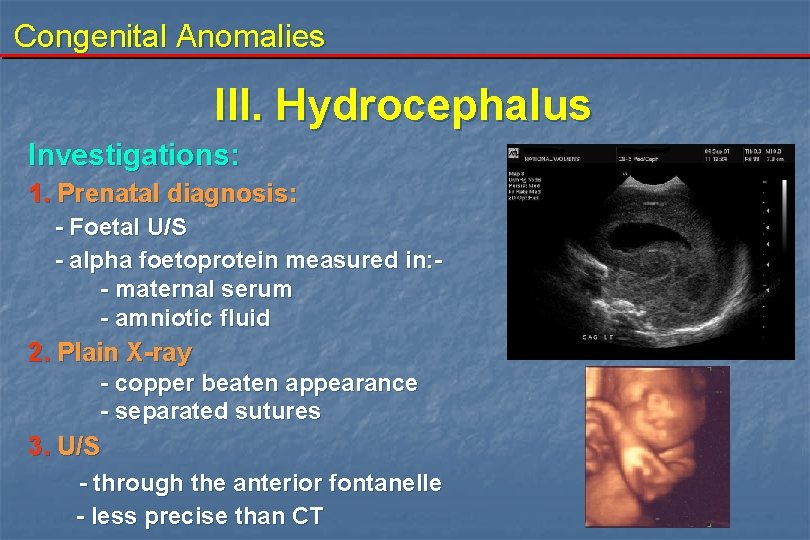
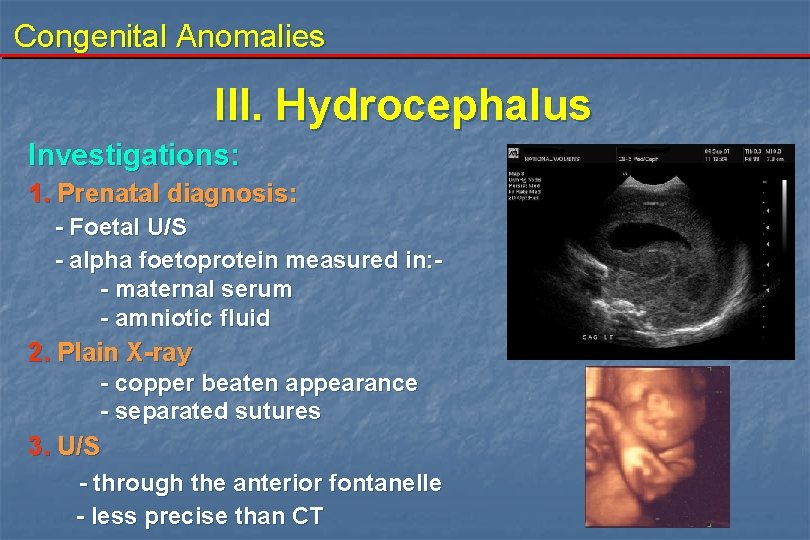
Congenital Anomalies III. Hydrocephalus Investigations: 1. Prenatal diagnosis: - Foetal U/S - alpha foetoprotein measured in: - maternal serum - amniotic fluid 2. Plain X-ray - copper beaten appearance - separated sutures 3. U/S - through the anterior fontanelle - less precise than CT
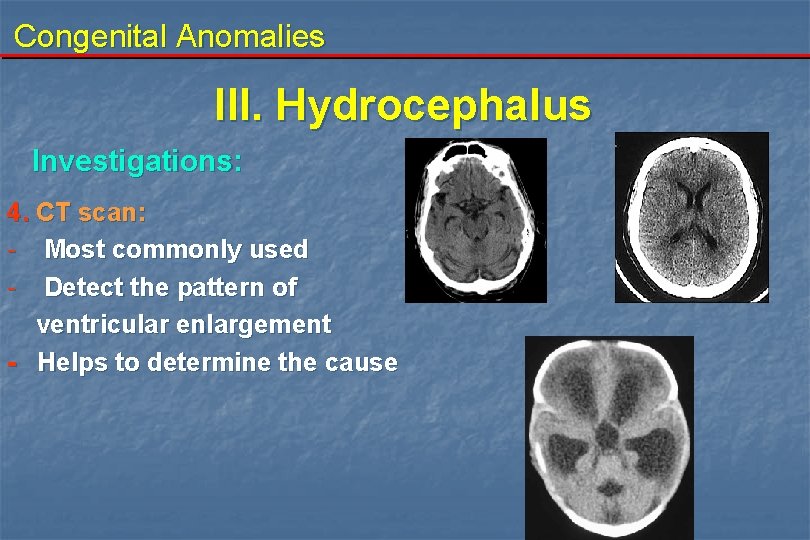
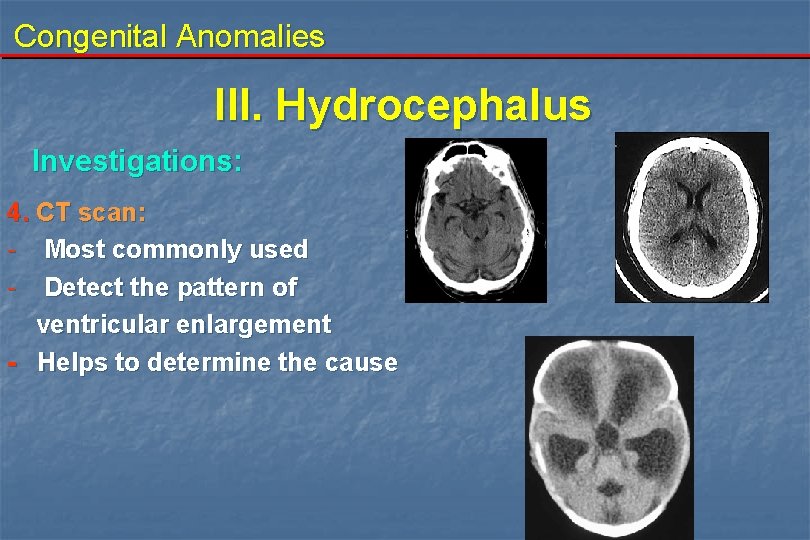
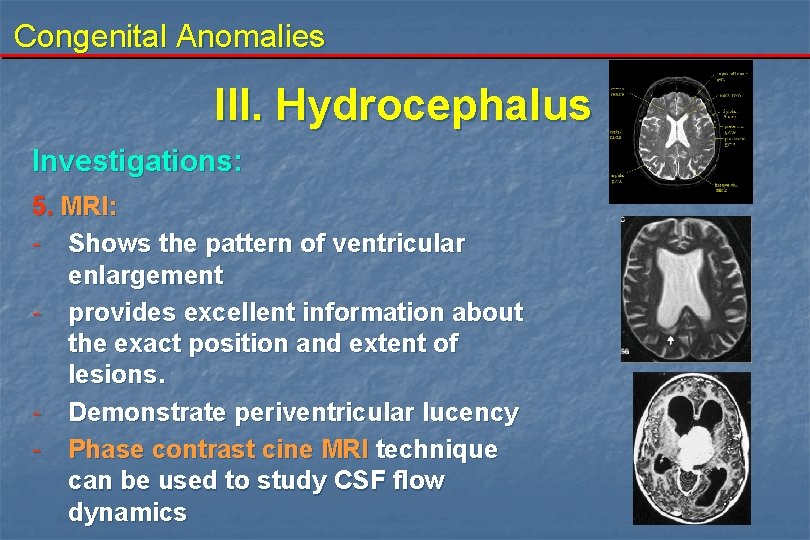
Congenital Anomalies III. Hydrocephalus Investigations: 4. CT scan: - Most commonly used - Detect the pattern of ventricular enlargement - Helps to determine the cause
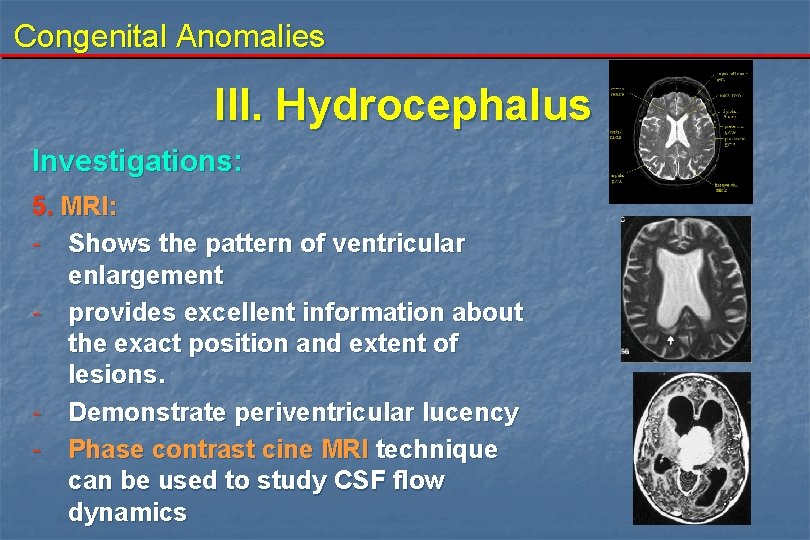
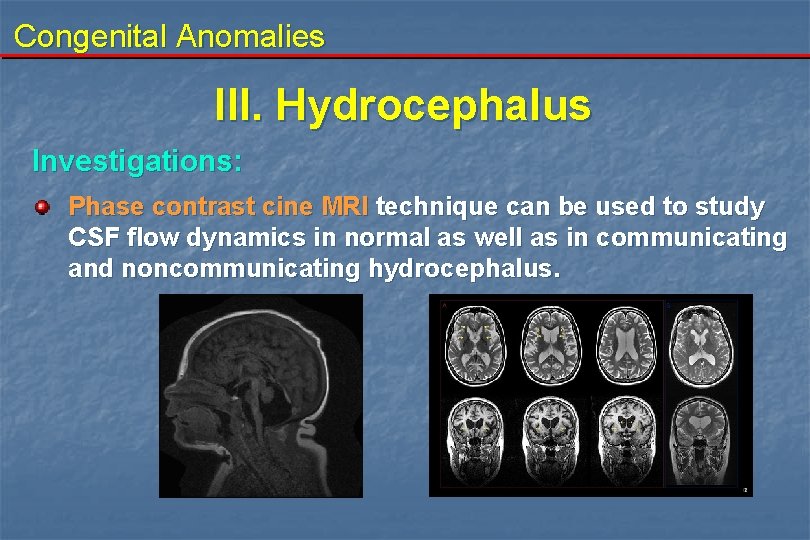
Congenital Anomalies III. Hydrocephalus Investigations: 5. MRI: - Shows the pattern of ventricular enlargement - provides excellent information about the exact position and extent of lesions. - Demonstrate periventricular lucency - Phase contrast cine MRI technique can be used to study CSF flow dynamics

Congenital Anomalies III. Hydrocephalus Investigations: 6 - ICP monitoring 7 - Cerebral angiography
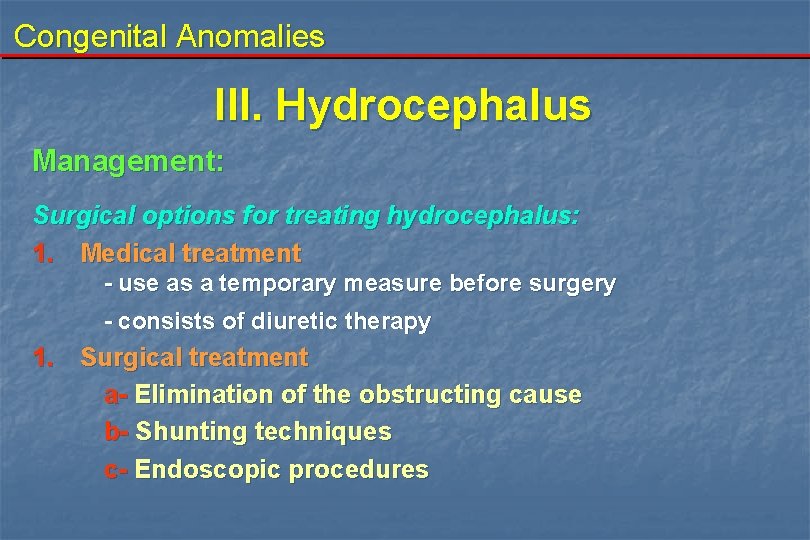
Congenital Anomalies III. Hydrocephalus Management: Surgical options for treating hydrocephalus: 1. Medical treatment - use as a temporary measure before surgery - consists of diuretic therapy 1. Surgical treatment a- Elimination of the obstructing cause b- Shunting techniques c- Endoscopic procedures
Congenital Anomalies III. Hydrocephalus 2. Surgical treatment a. Elimination of the obstructing cause: - For example the removal of the posterior fossa tumor may restore the C S F pathway.
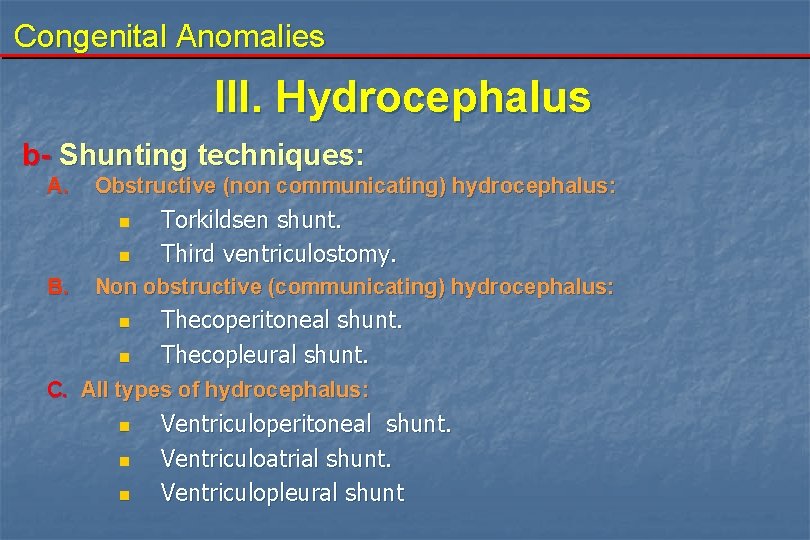
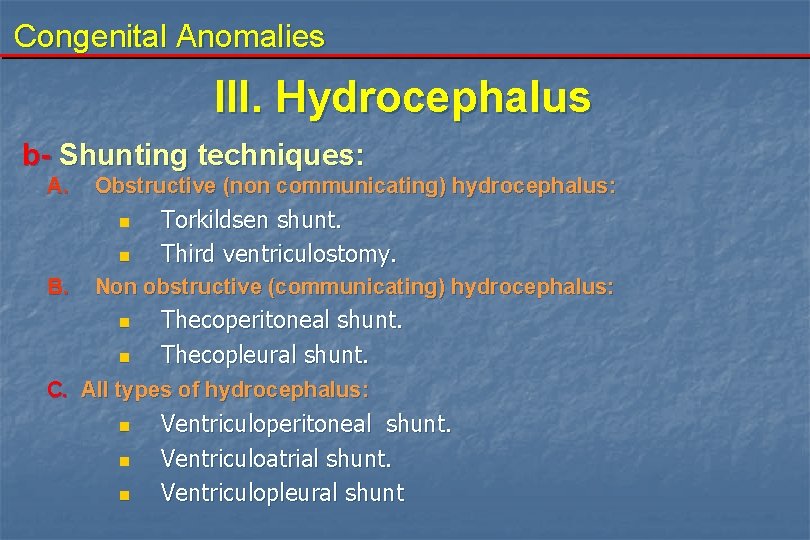
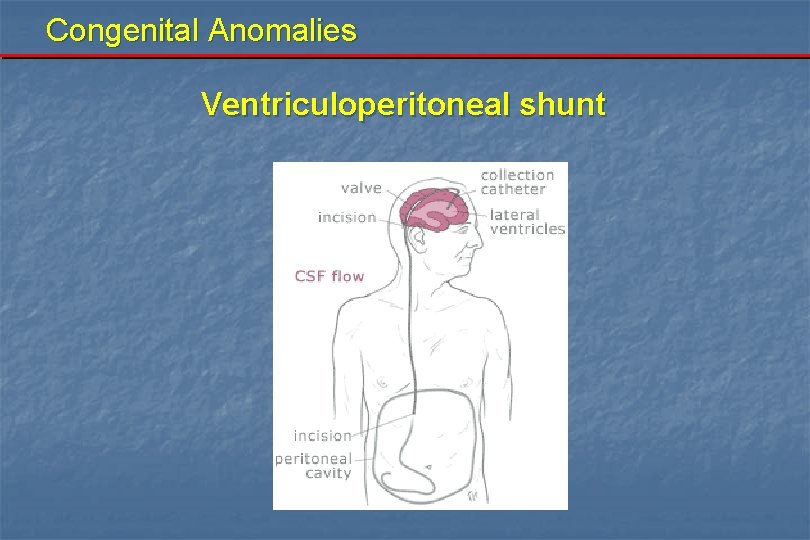
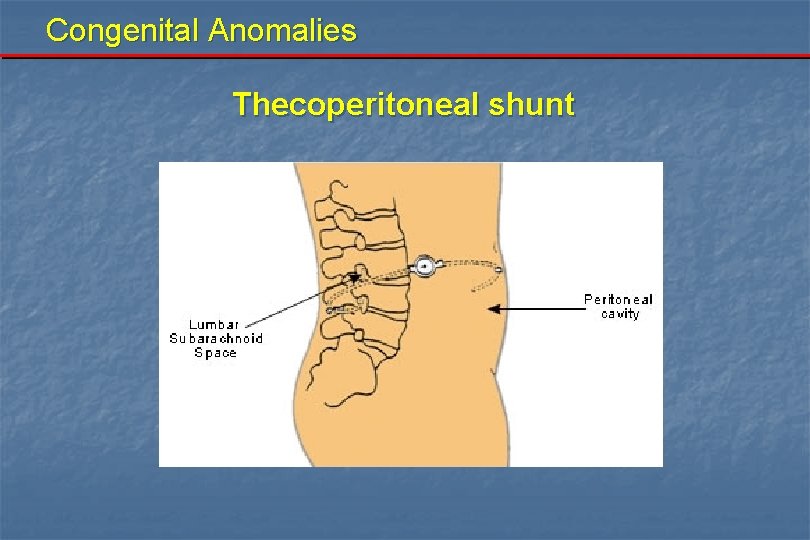
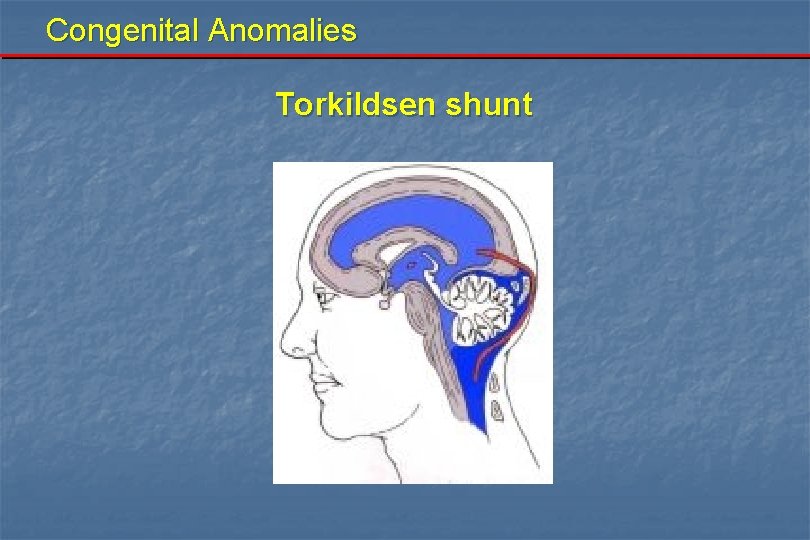
Congenital Anomalies III. Hydrocephalus b- Shunting techniques: A. Obstructive (non communicating) hydrocephalus: n n B. Torkildsen shunt. Third ventriculostomy. Non obstructive (communicating) hydrocephalus: n n Thecoperitoneal shunt. Thecopleural shunt. C. All types of hydrocephalus: n n n Ventriculoperitoneal shunt. Ventriculoatrial shunt. Ventriculopleural shunt
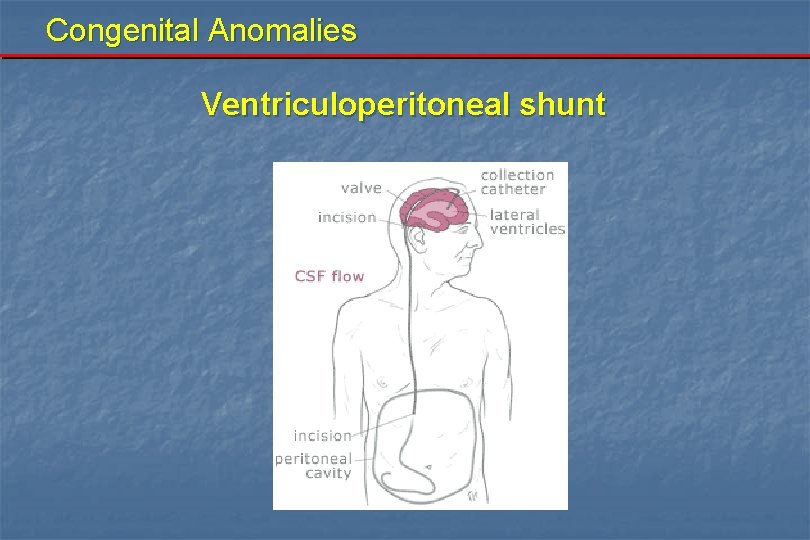
Congenital Anomalies Ventriculoperitoneal shunt
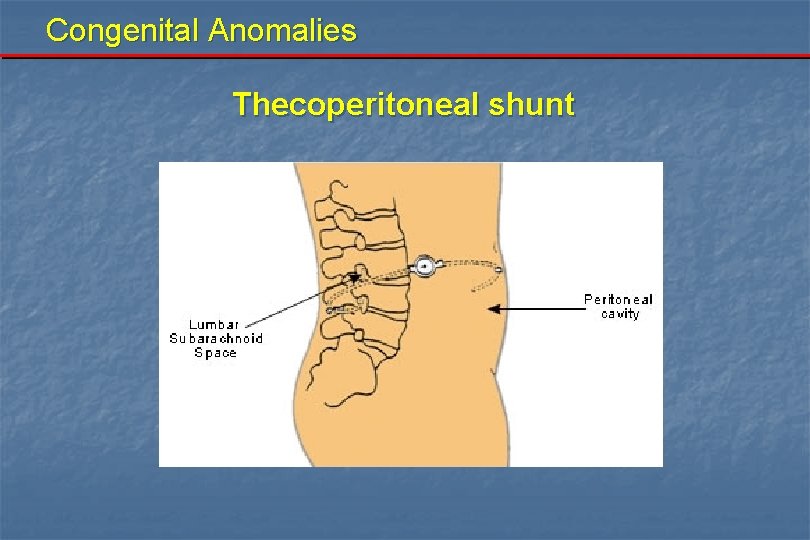
Congenital Anomalies Thecoperitoneal shunt
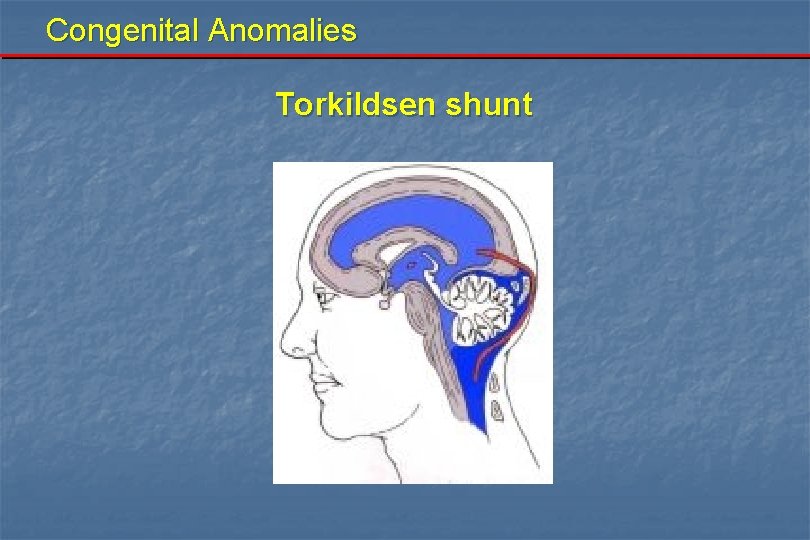
Congenital Anomalies Torkildsen shunt

Congenital Anomalies III. Hydrocephalus Common complications of shunt surgery: 1. 2. 3. 4. Infection Obstruction Intracranial hemorrhage Over drainage complications: - Slit ventricle syndrome - craniosynostosis - subdural hemorrhage 5. Epilepsy 6. Diconnection of the shunt components 7. Shunt metastasis
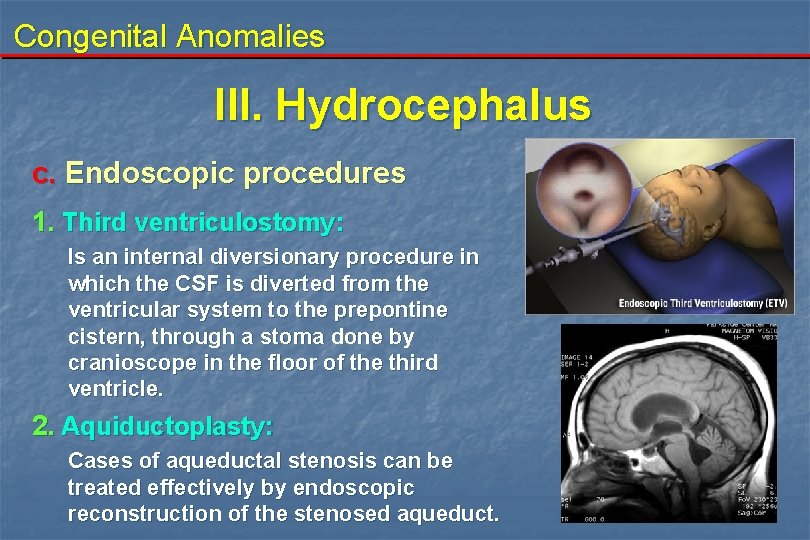
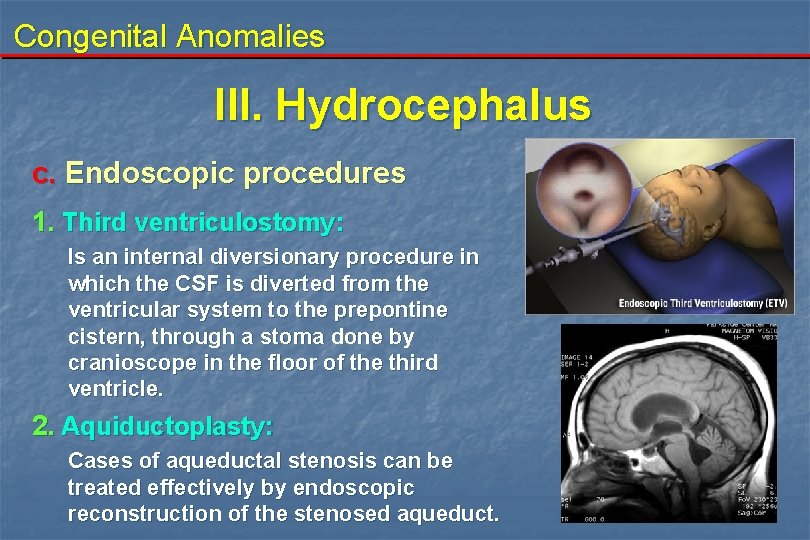
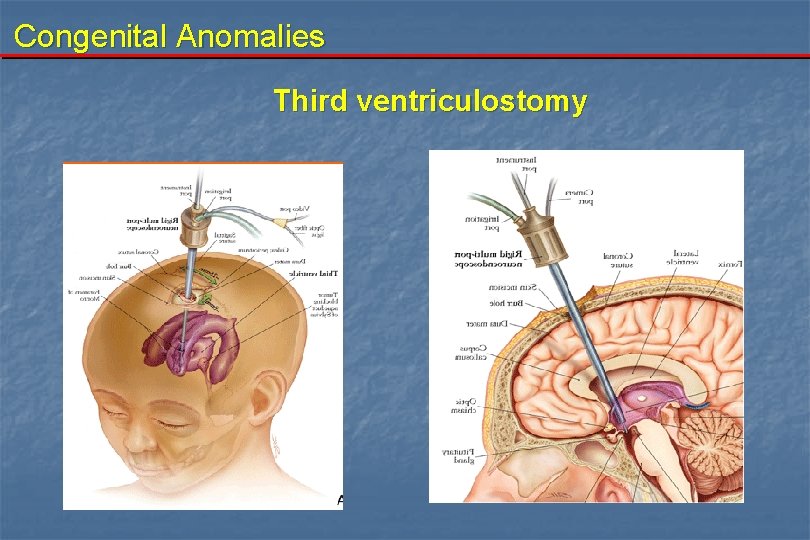
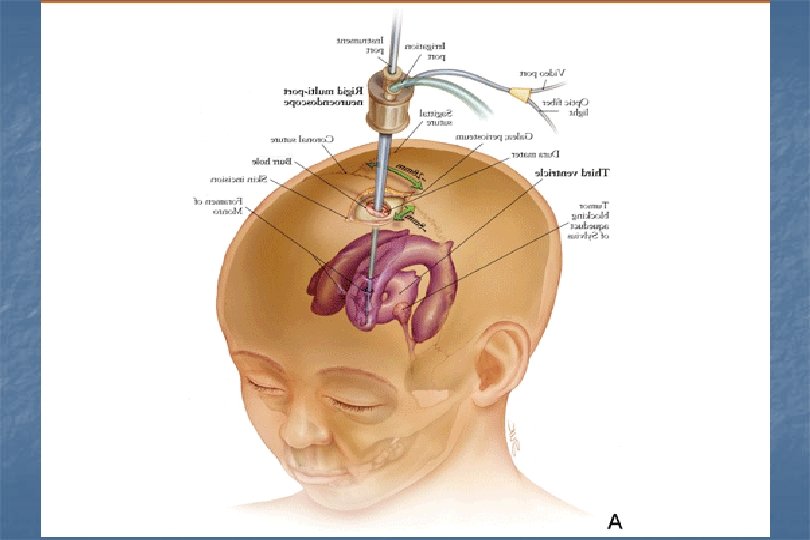
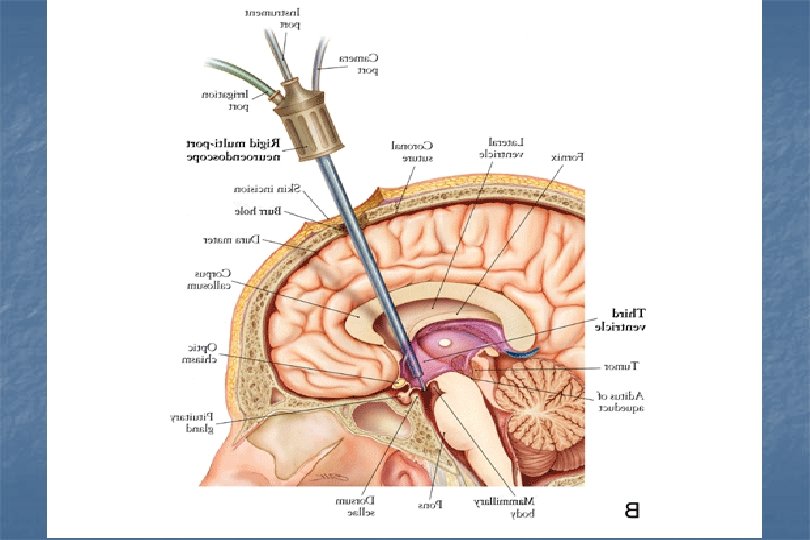
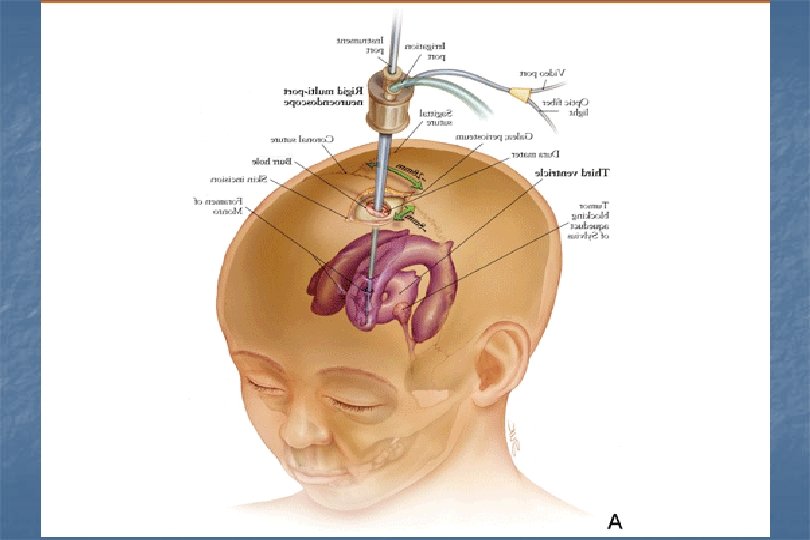
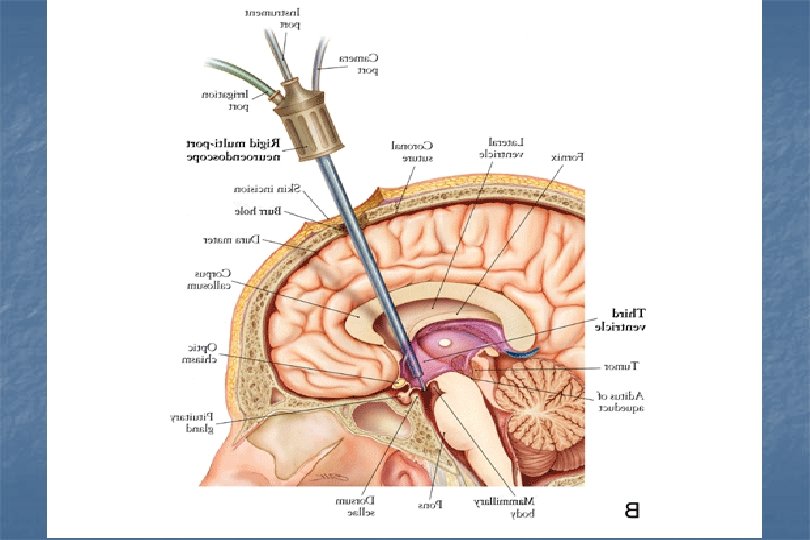
Congenital Anomalies III. Hydrocephalus c. Endoscopic procedures 1. Third ventriculostomy: Is an internal diversionary procedure in which the CSF is diverted from the ventricular system to the prepontine cistern, through a stoma done by cranioscope in the floor of the third ventricle. 2. Aquiductoplasty: Cases of aqueductal stenosis can be treated effectively by endoscopic reconstruction of the stenosed aqueduct.
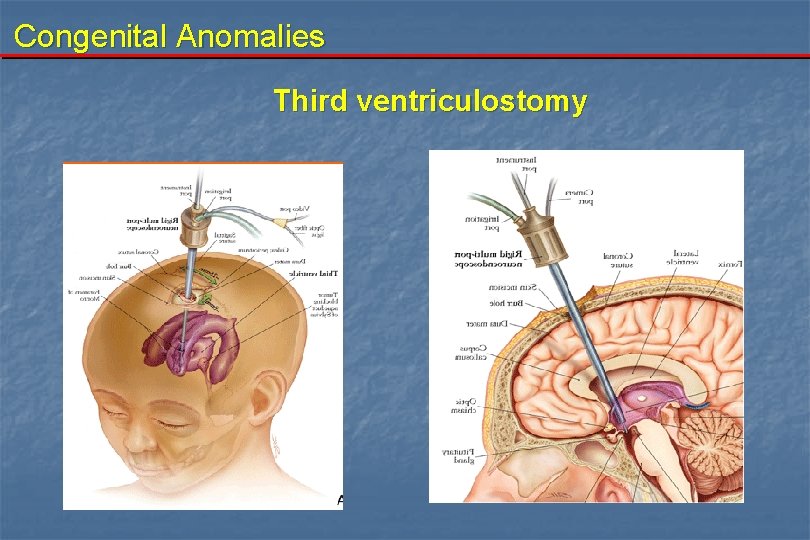
Congenital Anomalies Third ventriculostomy
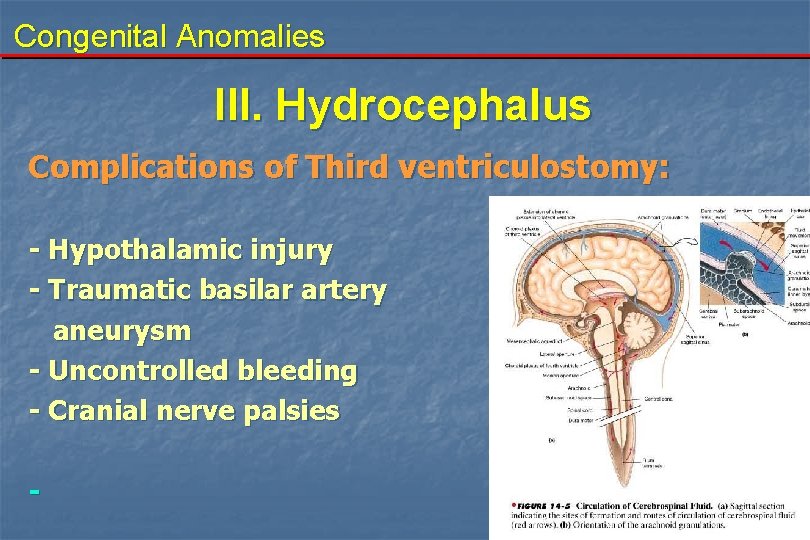
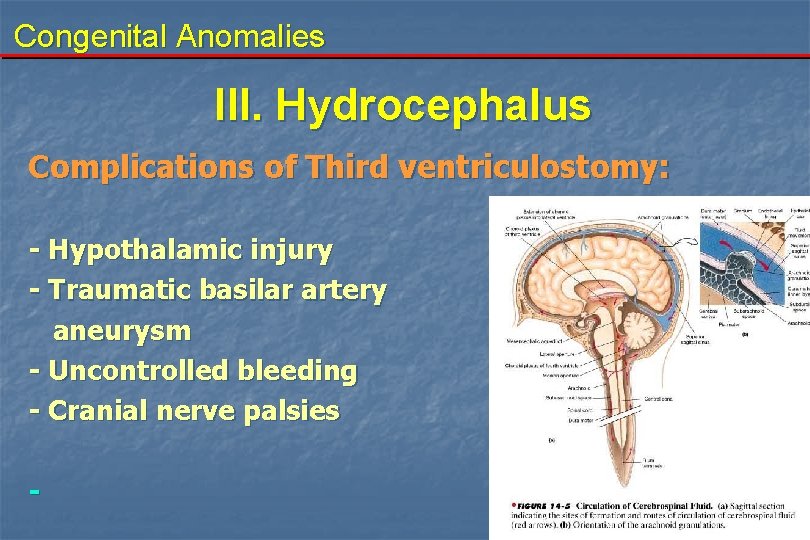
Congenital Anomalies III. Hydrocephalus Complications of Third ventriculostomy: - Hypothalamic injury - Traumatic basilar artery aneurysm - Uncontrolled bleeding - Cranial nerve palsies -

Congenital Anomalies Encephalocele
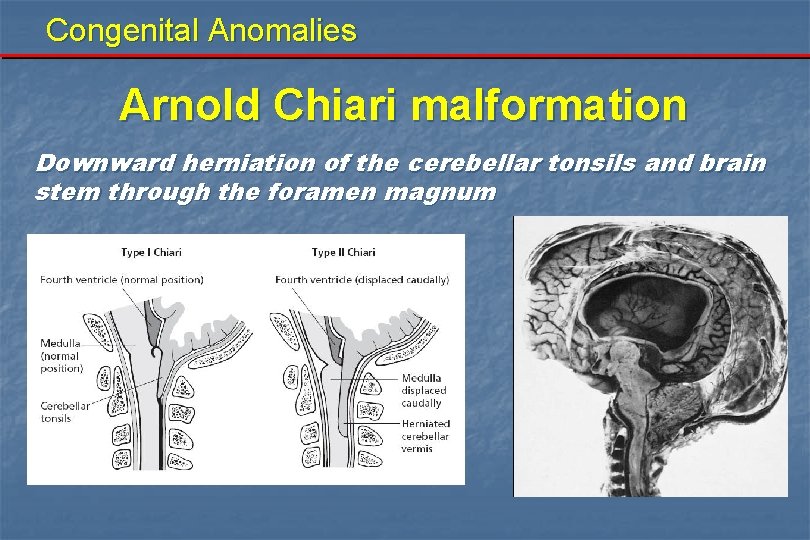
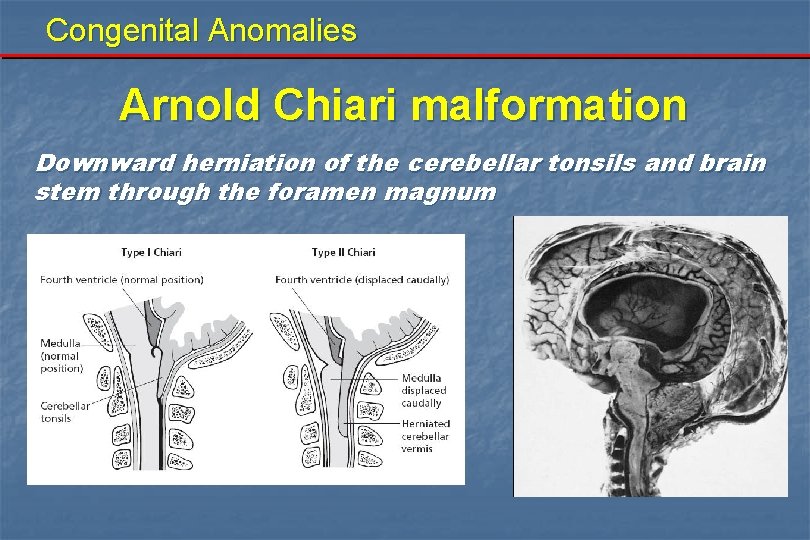
Congenital Anomalies Arnold Chiari malformation Downward herniation of the cerebellar tonsils and brain stem through the foramen magnum
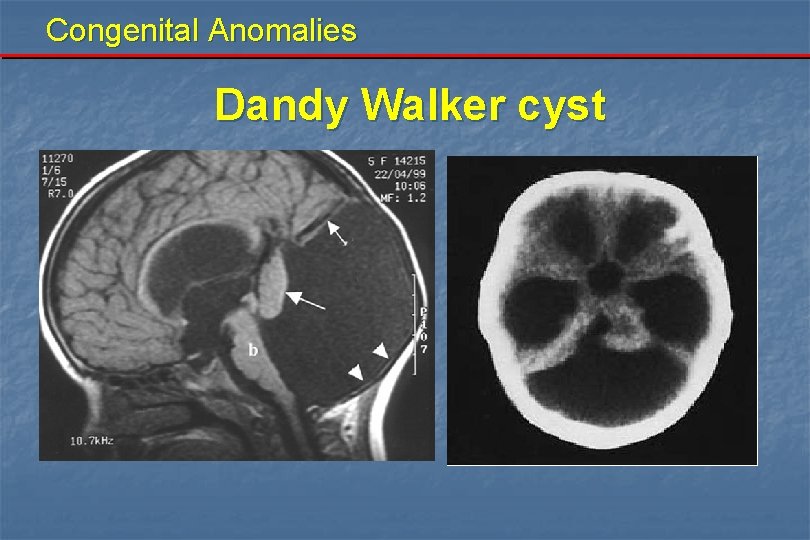
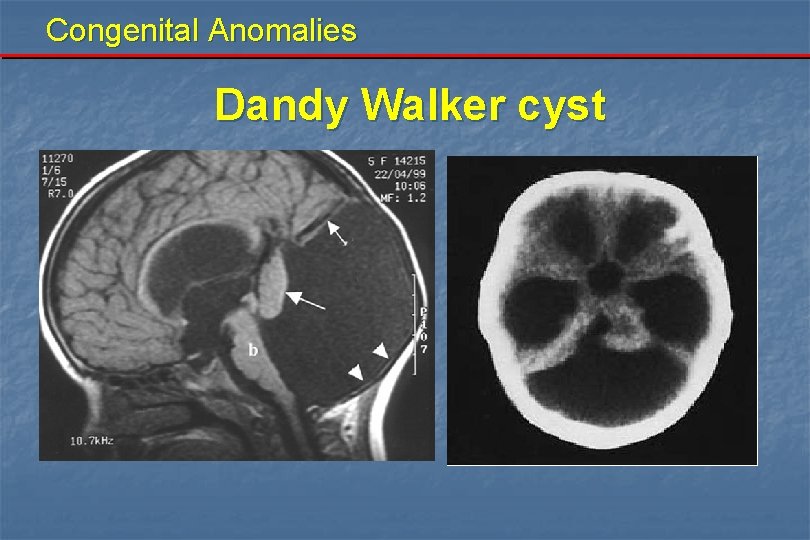
Congenital Anomalies Dandy Walker cyst
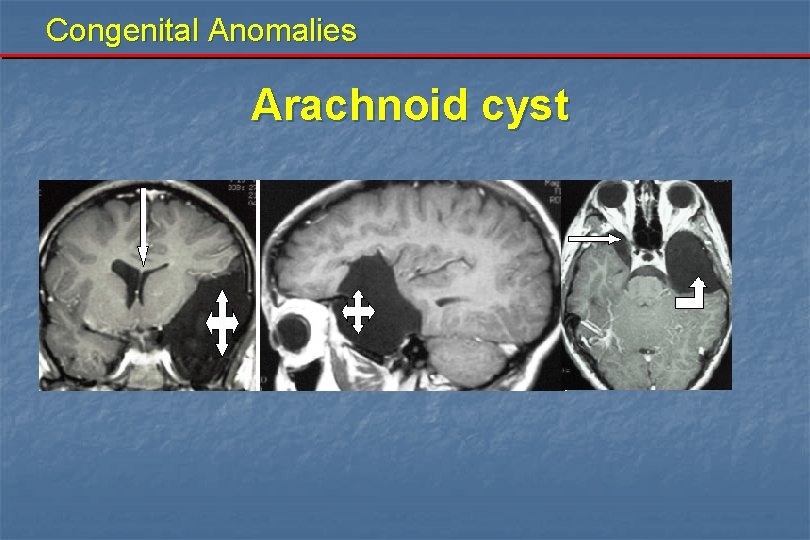
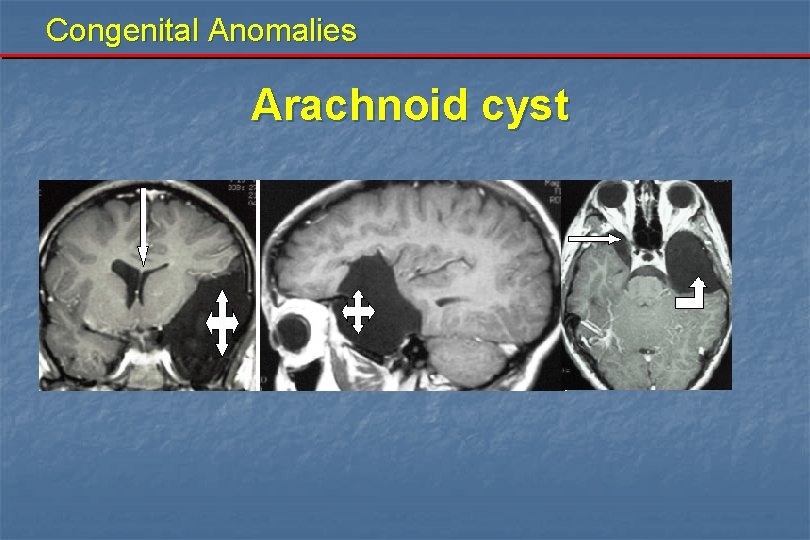
Congenital Anomalies Arachnoid cyst

Data show design & preparation by : Dr. El-Sayed Amr - (012) 3106023

Congenital Anomalies III. Hydrocephalus Pathlogical effects: Raised ICP. White matter damage leading to scaring. Grey matter damage. In infants before sutures fusion; head expansion, massive ventricular dilatation leaving a thin rim of cerebral mantle. Death occurs in untreated cases. Sometimes hydrocephalus arrests.
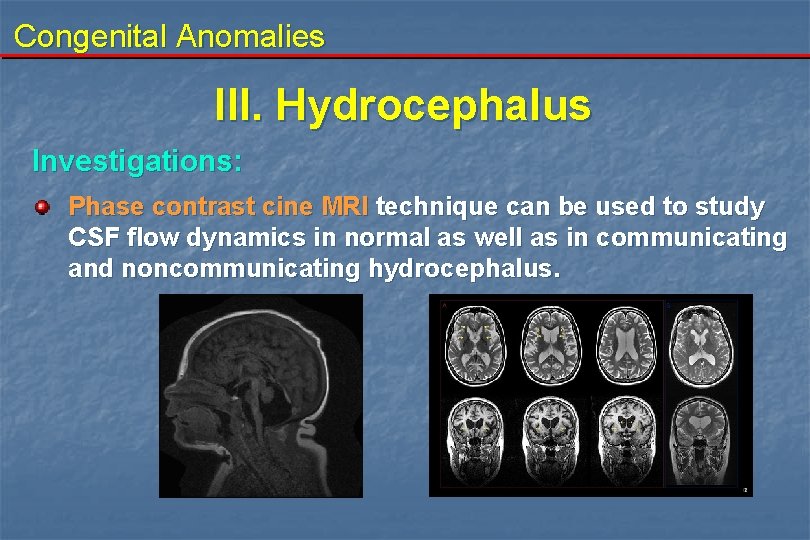
Congenital Anomalies III. Hydrocephalus Investigations: Phase contrast cine MRI technique can be used to study CSF flow dynamics in normal as well as in communicating and noncommunicating hydrocephalus.

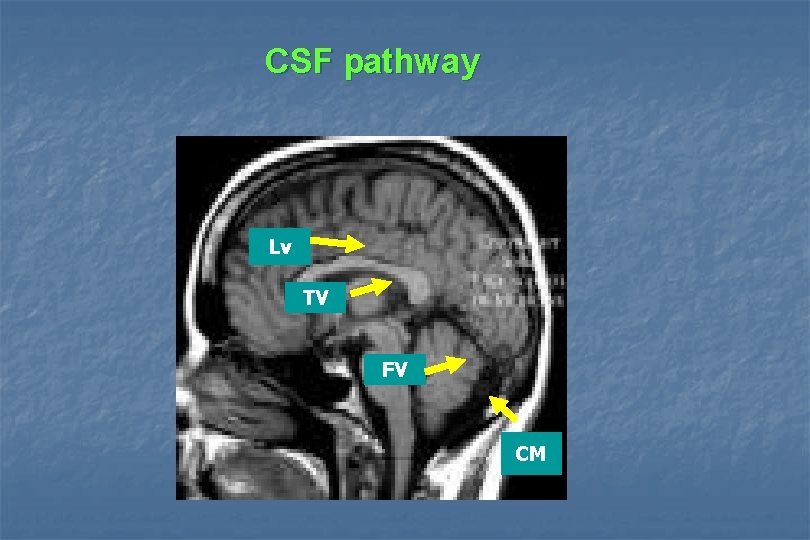
CSF pathway Lv TV FV CM
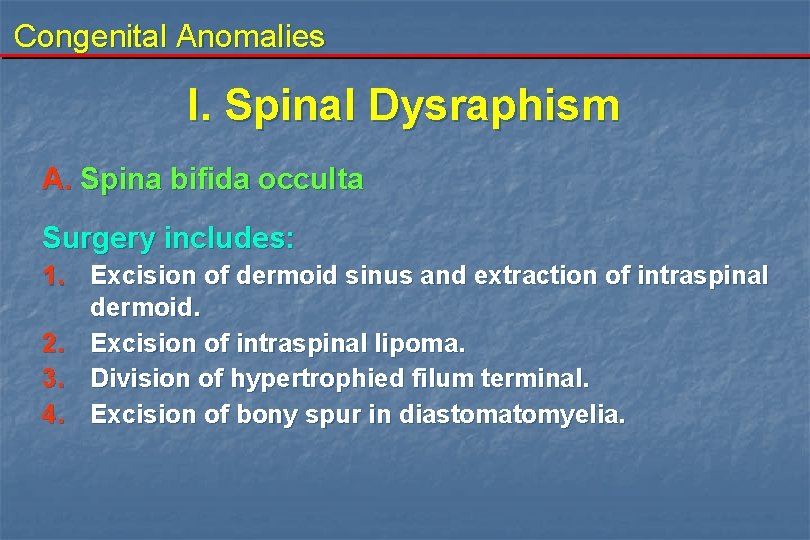
Congenital Anomalies I. Spinal Dysraphism A. Spina bifida occulta Surgery includes: 1. Excision of dermoid sinus and extraction of intraspinal dermoid. 2. Excision of intraspinal lipoma. 3. Division of hypertrophied filum terminal. 4. Excision of bony spur in diastomatomyelia.
Congenital Anomalies

Akher haga khles w Lebanon bingo
 Proboscis lateralis
Proboscis lateralis Causes of congenital anomalies
Causes of congenital anomalies Most common congenital anomalies
Most common congenital anomalies Penis
Penis Kode icd 10 malformasi anorektal
Kode icd 10 malformasi anorektal Causes of congenital anomalies
Causes of congenital anomalies Penn state neurosurgery
Penn state neurosurgery Drug reaction treatment
Drug reaction treatment The walton centre for neurology and neurosurgery
The walton centre for neurology and neurosurgery Neurosurgery
Neurosurgery Alan r cohen
Alan r cohen Norse neurosurgery referral
Norse neurosurgery referral Uw neurosurgery residents
Uw neurosurgery residents Hacettepe university faculty of medicine
Hacettepe university faculty of medicine Faculty of veterinary medicine cairo university
Faculty of veterinary medicine cairo university Applied medical sciences
Applied medical sciences Conus arteriosus
Conus arteriosus Faculty of medicine dentistry and health sciences
Faculty of medicine dentistry and health sciences Semmelweis university faculty of medicine
Semmelweis university faculty of medicine Semmelweis university faculty of medicine
Semmelweis university faculty of medicine Hubert kairuki memorial university faculty of medicine
Hubert kairuki memorial university faculty of medicine Emory dermatology clinic
Emory dermatology clinic Faculty of veterinary medicine cairo university logo
Faculty of veterinary medicine cairo university logo Faculty of medicine mcgill
Faculty of medicine mcgill Faculty of medicine nursing and health sciences
Faculty of medicine nursing and health sciences Solid thyroid nodule
Solid thyroid nodule Cairo university faculty of veterinary medicine
Cairo university faculty of veterinary medicine Nit calicut chemistry department
Nit calicut chemistry department Data redundancy and update anomalies
Data redundancy and update anomalies Anomali refraksi
Anomali refraksi The criminal man
The criminal man Modification anomalies
Modification anomalies Cfsv2 monthly prec anomalies
Cfsv2 monthly prec anomalies Japan population pyramid
Japan population pyramid Anisotrope bois
Anisotrope bois Database anomalies
Database anomalies Attention anomalies finance
Attention anomalies finance Elliptocytosis
Elliptocytosis Anomalies du rcf pendant le travail
Anomalies du rcf pendant le travail Frazzini
Frazzini Vitelline fistula
Vitelline fistula Gynerisq
Gynerisq Oddball: spotting anomalies in weighted graphs
Oddball: spotting anomalies in weighted graphs Department of medicine solna
Department of medicine solna Congenital rubella syndrome triad
Congenital rubella syndrome triad Congenital adrenal hyperplasia characteristics
Congenital adrenal hyperplasia characteristics Congenital malformations
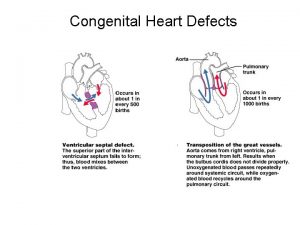
Congenital malformations Congenital heart defect
Congenital heart defect Schlussel urology
Schlussel urology Congenital adrenal hyperplasia characteristics
Congenital adrenal hyperplasia characteristics Juxtaductal position
Juxtaductal position Flat iris insertion in congenital glaucoma
Flat iris insertion in congenital glaucoma Goodsall law fistula
Goodsall law fistula Ttn vs rds cxr
Ttn vs rds cxr Antithyroid drugs mnemonic
Antithyroid drugs mnemonic Canadian congenital heart alliance
Canadian congenital heart alliance Congenital hydronephrosis
Congenital hydronephrosis Endocardial cushion defect
Endocardial cushion defect Congenital voice disorders
Congenital voice disorders Puberty disorder
Puberty disorder Congenital heart disease pda
Congenital heart disease pda Congenital rubella
Congenital rubella Congenital toxoplasmosis
Congenital toxoplasmosis Congenital fibrosis of the extraocular muscles
Congenital fibrosis of the extraocular muscles Cyanotic congenital heart disease
Cyanotic congenital heart disease Congenital
Congenital Piston test for hip dislocation
Piston test for hip dislocation Congenital glaucoma
Congenital glaucoma Vesicoureteral reflux
Vesicoureteral reflux Congenital rubella syndrome triad
Congenital rubella syndrome triad Hypothyroidism classification
Hypothyroidism classification Congenital amusia
Congenital amusia Congenital pneumonia
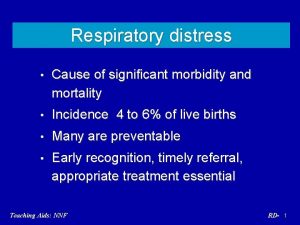
Congenital pneumonia Greater and lesser pelvis
Greater and lesser pelvis Congenital diaphragmatic hernia
Congenital diaphragmatic hernia Congenital toxoplasmosis
Congenital toxoplasmosis Dr dawn lim
Dr dawn lim Congenital rubella syndrome
Congenital rubella syndrome Congenital glaucoma
Congenital glaucoma Horizontal
Horizontal