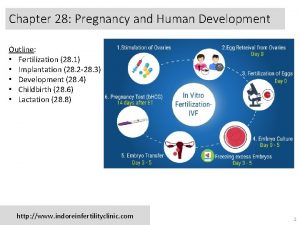
Nutrition during the life cycle Pregnancy and Lactation




- Slides: 84
Nutrition during the life cycle: Pregnancy and Lactation Ms/ Amina Metwaly
Nutrition during pregnancy • Maternal diet and nutritional status have a direct impact on the course of pregnancy and its outcome. • Malnutrition that occurs in the early months of pregnancy affects development and the capacity of the embryo to survive whilst poor nutrition in the latter part of pregnancy affects fetal growth.
Pregnancy physiology that alters nutritional needs 1 - Altered Metabolism: • Increase the basal metabolic rate: by the fourth month of gestation and rises to 15 20% above normal by term. • Altered the metabolism of nutrients: fat becomes the major source of maternal fuel, making glucose available for the fetus.
Pregnancy physiology that alters nutritional needs 2 - Gastrointestinal Changes: • Slow gastrointestinal motility: an advantage of slowed motility is that nutrient absorption increases. • Nausea and vomiting are common in the first trimester and may be related to hypoglycemia, decreased gastric motility, relaxation of the cardiac sphincter, or anxiety.
Pregnancy physiology that alters nutritional needs 2 - Gastrointestinal Changes: • Increases in appetite and thirst are also common. • Heartburn and constipation: due to slow motility or enlarging uterus. .
Pregnancy physiology that alters nutritional needs 3 - Blood Volume Changes: • Increase total body water throughout pregnancy. • Hemodilution or a physiologic anemia of pregnancy: due to the increase in blood volume. • Minor edema: may be considered normal if it is not accompanied by hypertension and proteinuria.
Pregnancy physiology that alters nutritional needs 4 - Ideal Weight Gain: • The average weight gain is about 25 to 30 lb (11. 5 kg to 14. 0 kg). • Weight gain during pregnancy consists of the weight of the fetus and associated fetal tissues (e. g. placenta), plus the weight increases in maternal tissue.
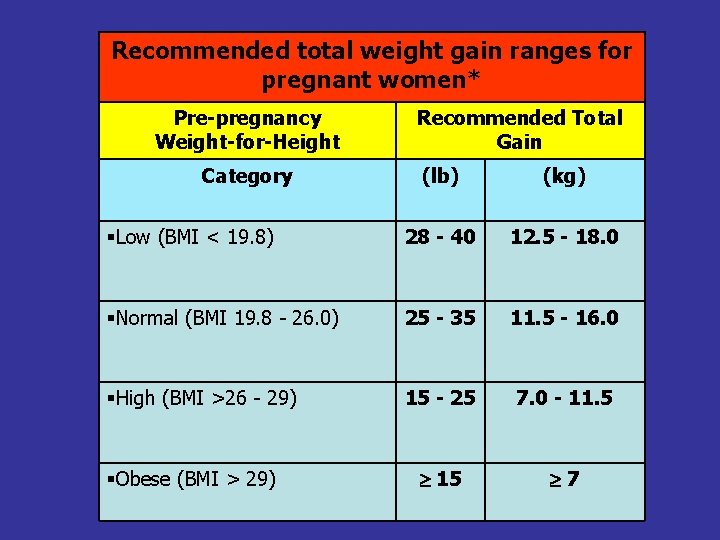
Pregnancy physiology that alters nutritional needs 4 - Ideal Weight Gain: • Recommendations for weight gain are divided into three categories based on the woman’s pre-pregnancy weight. The weight category is determined using body mass index (BMI). • The range for women carrying twins is 35 lb to 45 lb (16 - 20 kg).
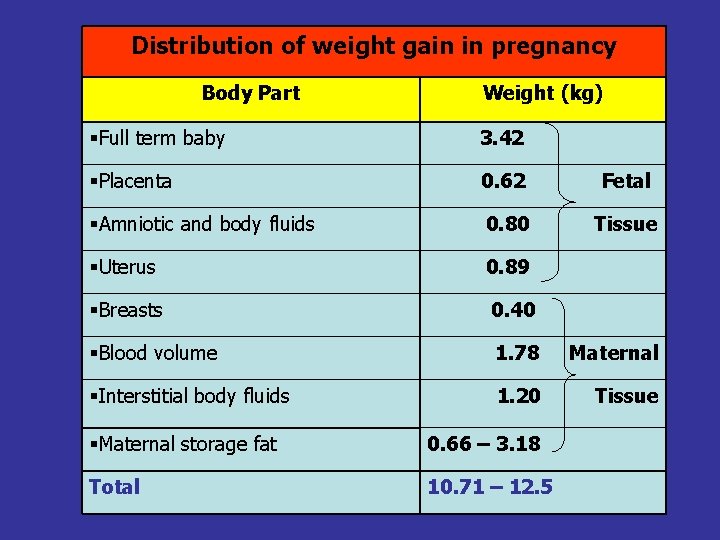
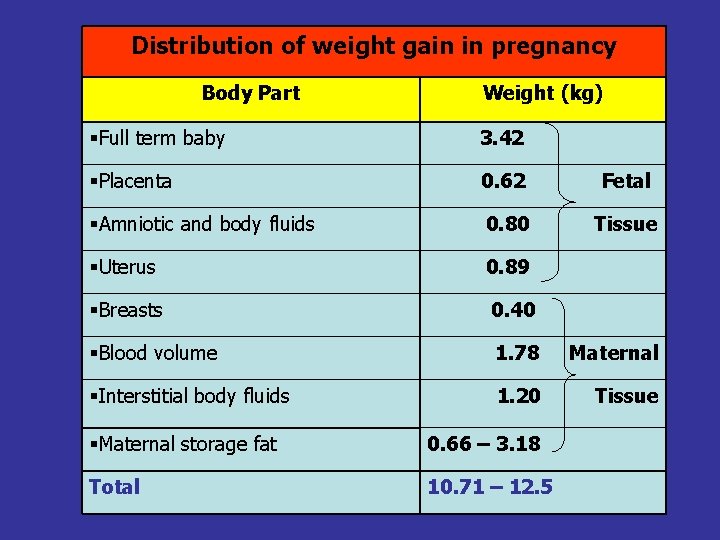
Distribution of weight gain in pregnancy Body Part Weight (kg) Full term baby 3. 42 Placenta 0. 62 Fetal Amniotic and body fluids 0. 80 Tissue Uterus 0. 89 Breasts 0. 40 Blood volume 1. 78 Maternal Interstitial body fluids 1. 20 Tissue Maternal storage fat 0. 66 – 3. 18 Total 10. 71 – 12. 5
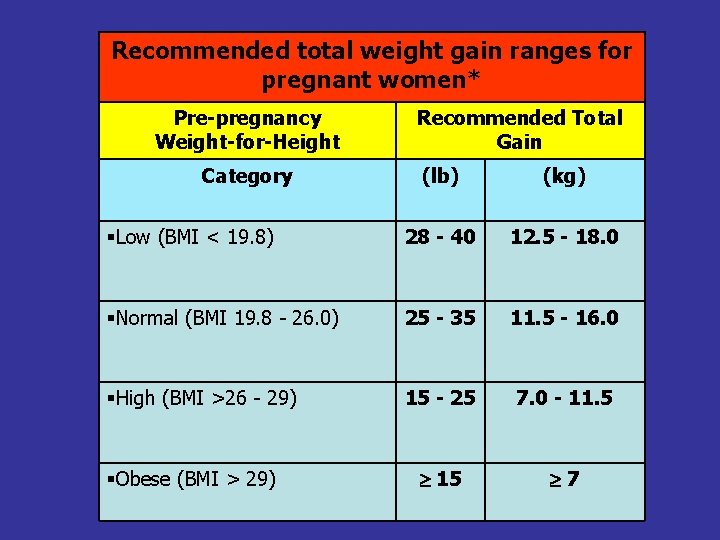
Recommended total weight gain ranges for pregnant women* Pre-pregnancy Weight-for-Height Category Recommended Total Gain (lb) (kg) Low (BMI < 19. 8) 28 - 40 12. 5 - 18. 0 Normal (BMI 19. 8 - 26. 0) 25 - 35 11. 5 - 16. 0 High (BMI >26 - 29) 15 - 25 7. 0 - 11. 5 15 7 Obese (BMI > 29)
Nutrient requirements during pregnancy • Actual requirements during pregnancy are influenced by previous nutritional status and health history, including: chronic illnesses, multiple pregnancies and closely spaced pregnancies. • The requirement for one nutrient may be altered by the intake of another. E. g. , women who do not meet their calorie requirements need higher amounts of protein.
Nutrient requirements during pregnancy • Nutrient needs are not constant throughout the course of pregnancy - nutrient needs change little during the first trimester and are at their highest during the last trimester. • The Food Guide Pyramid can be used to teach women how to make food choices that will provide the balanced intake they need.
Calories • The increased need for calories is 300 extra calories per day, which is @ 15% of a woman’s normal calorie requirement. • The increased need for calories does not occur until the beginning of the second trimester.
Calories Calorie needs increase because of: • The increase in basal metabolic rate. • Weight gain increases the amount of calories burned during activity. • Uses additional calories to store energy in preparation for lactation after delivery.
Protein The RDA for protein increases by 10 g for pregnant women ages 25 and older. Protein needs increase to support : • Fetal growth and development. • The formation of the placenta and amniotic fluid. • The growth of maternal tissues and the expanded blood volume.
Protein Women who fail to consume adequate protein may be at increased risk for: • Development of toxemia. • Anemia. • Poor uterine muscle tone. • Abortion. • Decreased resistance to infection. • Shorter, lighter infants with low Apgar scores.
Folic acid • The Institute of Medicine in U. S. A. recommends that synthetic folic acid intake increase to 600 g daily once pregnancy is confirmed.
Folic acid Importance of folic acid for pregnancy: • Women who consume adequate amounts of folic acid before conception and throughout the first month of pregnancy reduce their risk of having a baby with a neural tube defect (e. g. , spina bifida, anencephaly).
Folic acid sources: • Natural form of folic acid (folate): orange juice, other citrus fruits and juices, green leafy vegetables, dried peas and beans, broccoli, and whole-grain products. • Synthetic folic acid is found in multivitamins, fortified breakfast cereals and enriched grain products.
Other B vitamins • The increased requirement for vitamin B 6 is proportional to the increase in protein because it is involved in protein metabolism. • Because vitamin B 12 is necessary for the metabolism of folate, a slight increase in intake is recommended.
Calcium • The AI for calcium for pregnant women 19 years of age and older is 1000 mg. • The reason why the AI is not higher for pregnant women compared with non pregnant women is that calcium absorption more than doubles early in pregnancy.
Iron • A daily supplement of 30 mg of ferrous iron is recommended for all women during the second and third trimesters. • It is preferably taken between meals or at bedtime on an empty stomach to maximize absorption.
Iron Importance for iron during pregnancy: • To support the increase in maternal blood volume. • To provide iron for fetal liver storage, which will sustain the infant for the first 4 6 months of life.
The advices should be given to a pregnant women concerning her nutrition 1 - Eat in moderation. 2 - Aim for balance. 3 - Eat three meals daily plus two or three snacks. 4 - Drink adequate fluids.
The advices should be given to a pregnant women concerning her nutrition 5 - Do not restrict salt intake. 6 - Moderate Caffeine consumption does not pose a problem. 7 - If you use artificial sweeteners, do so judiciously. 8 - Be aware of food borne risks during pregnancy.
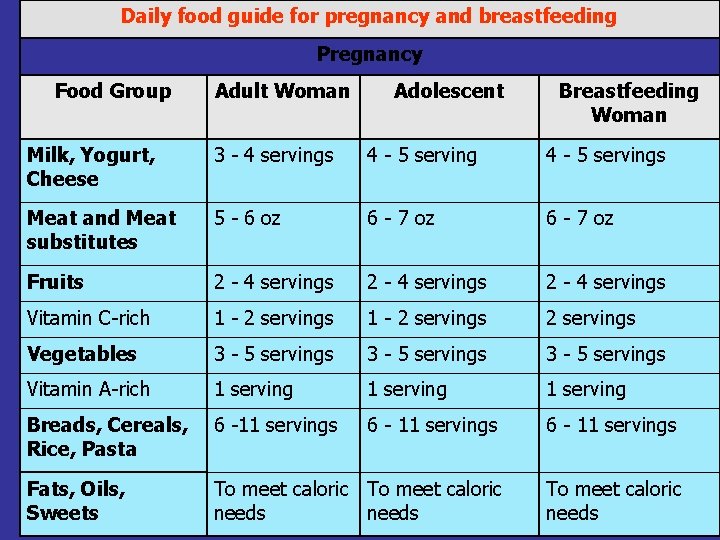
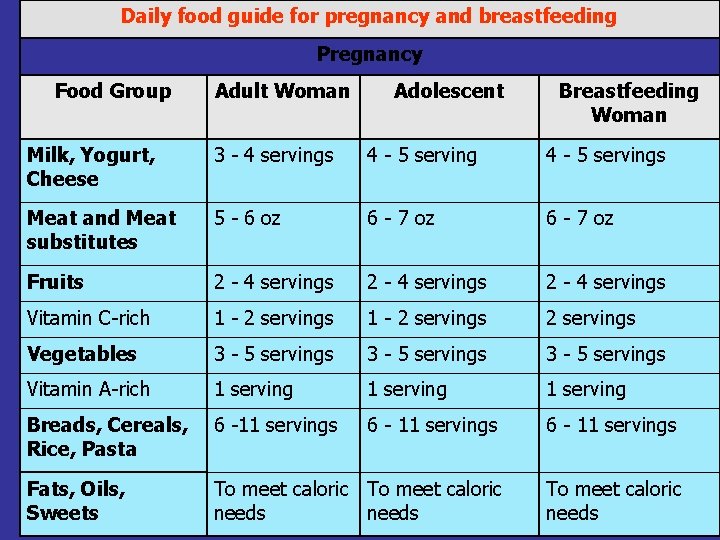
Daily food guide for pregnancy and breastfeeding Pregnancy Food Group Adult Woman Adolescent Breastfeeding Woman Milk, Yogurt, Cheese 3 - 4 servings 4 - 5 servings Meat and Meat substitutes 5 - 6 oz 6 - 7 oz Fruits 2 - 4 servings Vitamin C-rich 1 - 2 servings Vegetables 3 - 5 servings Vitamin A-rich 1 serving Breads, Cereals, Rice, Pasta 6 -11 servings 6 - 11 servings Fats, Oils, Sweets To meet caloric needs
Indications for supplements use during pregnancy • • Heavy smokers. Drug abusers. Those carrying twins. Women who are unlikely to consume an adequate diet despite nutritional advice or nutrition counseling.
Indications for supplements use during pregnancy • Women who do not receive adequate exposure to sunlight. • Women who do not consume adequate calcium.
Indications for supplements use during pregnancy • Complete vegans need daily supplements of vitamin B 12. • Women who take more than 30 mg of iron to treat iron deficiency anemia should take supplements of zinc and copper.
Nutritional intervention for problems during pregnancy 1 - Nausea and Vomiting Women should be advised to: • Eating small, frequent meals every 2 to 3 hours. • Eat carbohydrate foods such as: dry crackers, Melba toast, dry cereal, or hard candy before getting out of bed in the morning.
Nutritional intervention for problems during pregnancy 1 - Nausea and Vomiting Women should be advised to: • Avoid drinking liquids with meals. • Avoid coffee, tea and spicy foods. • Limit high-fat foods, because they delay gastric emptying time. • Eliminate individual intolerances.
Nutritional intervention for problems during pregnancy 2. Constipation, may be caused by: • Relaxation of gastrointestinal muscle tone and motility • Pressure of the fetus on the intestines. • Decrease in physical activity • Inadequate intake of fluid and fiber. • Side effect of the consumption of iron supplements.
Nutritional intervention for problems during pregnancy 2. Constipation Encourage the client to: • Increase fiber intake. • Drink at least eight 8 -ounce glasses of liquid daily. • Try hot water with lemon or prune juice upon waking to help stimulate peristalsis • Participate in regular exercise.
Nutritional intervention for problems during pregnancy 3 - Heartburn: Encourage client to: • Eat small, frequent meals and eliminate liquids immediately before and after meals to avoid gastric distention. • Avoid coffee, high-fat foods and spices. • Eliminate individual intolerances. • Avoid lying down or bending over after eating.
Nutritional intervention for problems during pregnancy 4 - Inadequate Weight Gain: • Inadequate weight gain during pregnancy increases the risk of giving birth to a lowbirth-weight (LBW) infant (i. e. , a baby weighing less than 2500 g).
Nutritional intervention for problems during pregnancy 4 - Inadequate Weight Gain: • The recommended weight gain for normal weight women is @ 0. 44 kg/week, • Underweight women more than 0. 44 kg/week whilst overweight women about 0. 29 kg/week and women pregnant with twins at least 0. 44 kg/week.
Nutritional intervention for problems during pregnancy 4 - Inadequate Weight Gain, may occur secondary to: • Poor appetite related to nausea, vomiting, heartburn or smoking. • From an inadequate intake related to lack of knowledge or fear of gaining weight.
Nutritional intervention for problems during pregnancy 4 - Inadequate Weight Gain • Counsel the client on the recommended rate and quantity of weight gain associated with optimal maternal and infant health and successful breast-feeding. • Explain how the weight gain is distributed among the fetus, placenta and maternal tissues.
Nutritional intervention for problems during pregnancy 4 - Inadequate Weight Gain • Encourage the client to ask questions and verbalize feelings. • Advise the client that extra weight gained during pregnancy is quickly lost during lactation or through dieting after pregnancy.
Nutritional intervention for problems during pregnancy 4 - Inadequate Weight Gain • Advise the client that if her diet is inadequate in calories, it probably is also inadequate in other nutrients. • Advise the client that although the fetus can use maternal nutrient stores if the mother’s diet is inadequate.
Nutritional intervention for problems during pregnancy 4 - Inadequate Weight Gain • Advise the client that an inadequate intake can adversely affect maternal health (e. g. , poor iron intake leading to anemia) and infant health (e. g. , lbw, anemia, other postnatal complications).
Nutritional intervention for problems during pregnancy 5 - Excessive Weight Gain, may be related to: • Overeating. • Stress. • Decrease in physical activity.
Nutritional intervention for problems during pregnancy 5 - Excessive Weight Gain: • Counsel the client on the recommended rate and quantity of weight gain associated with optimal maternal and infant health and successful breast-feeding. • Explain that the weight gain is distributed among the fetus, placenta and maternal tissues.
Nutritional intervention for problems during pregnancy 5 - Excessive Weight Gain: • Set mutually agreeable weight gain goals. • Substitute skim or low-fat milk for whole milk. • Bake, broil or steam foods instead of frying.
Nutritional intervention for problems during pregnancy 5 - Excessive Weight Gain: • Eliminate empty calories: carbonated beverages, candy, rich desserts and traditional snack foods. • Use fats and oils sparingly.
Nutritional interventions for medical complications during pregnancy Diabetes mellitus • It characterized by abnormal glucose tolerance, requires dietary management regardless of whether it was present before conception (established diabetes) or developed during gestation (gestational diabetes) as a result of the metabolic changes of pregnancy.
Nutritional interventions for medical complications during pregnancy Diabetes increases the risk of: • Infection, especially urinary tract infection • Preeclampsia & Eclampsia • Spontaneous abortion • Extrauterine conception • Neonatal death • Congenital abnormalities
Nutritional interventions for medical complications during pregnancy Diabetes • Gestational diabetes does not usually produce maternal complications or birth defects, but it can make delivery difficult, because babies born to gestational diabetics are usually large, which may increase the risk of postpartum hemorrhage.
Nutritional interventions for medical complications during pregnancy Diabetes Management: • Monitor the progress and course of pregnancy of established diabetics. • Screen all women for gestational diabetes between 24 - 28 weeks of pregnancy. • Check for ketonuria regularly. • Diabetic management during pregnancy includes nutrition therapy and, possible, multiple daily doses of insulin.
Nutritional interventions for medical complications during pregnancy Diabetes Advise the client that: • Pregnant diabetics require the same nutrients and weight gain as non diabetic pregnant women. • She is not on a “diet” weight loss and fasting should never be undertaken during pregnancy. • Calorie requirements are based on prepregnancy weight.
Nutritional interventions for medical complications during pregnancy Diabetes Suggested guidelines are as follows: • 30 cal/kg for women of normal weight before conception. • 24 cal/kg for women weighing more than 120% of desirable weight before conception • 36 -40 cal/kg for women weighing less than 90% of desirable weight before conception.
Nutritional interventions for medical complications during pregnancy 2 - Anemia • Non pregnant women (non smokers) who have a hemoglobin below 12 g/d. L are considered anemic. • Pregnant women (non smoker) with a hemoglobin below 11 g/d. L in the first and third trimesters or below 10. 5 g/d. L in the second trimester are considered anemic.
Nutritional interventions for medical complications during pregnancy 2 - Anemia Management: • A therapeutic dose of 60 mg to 120 mg/day of elemental iron is prescribed. • In addition, a low-dose vitamin/mineral supplement is prescribed to ensure adequate amounts of copper and zinc.
Nutritional interventions for medical complications during pregnancy 2 - ANEMIA • The RDA of 400 mcg of folate during pregnancy can be met by a well-chosen diet. Supplements of folate are recommended for pregnant women who are not meeting this level of intake.
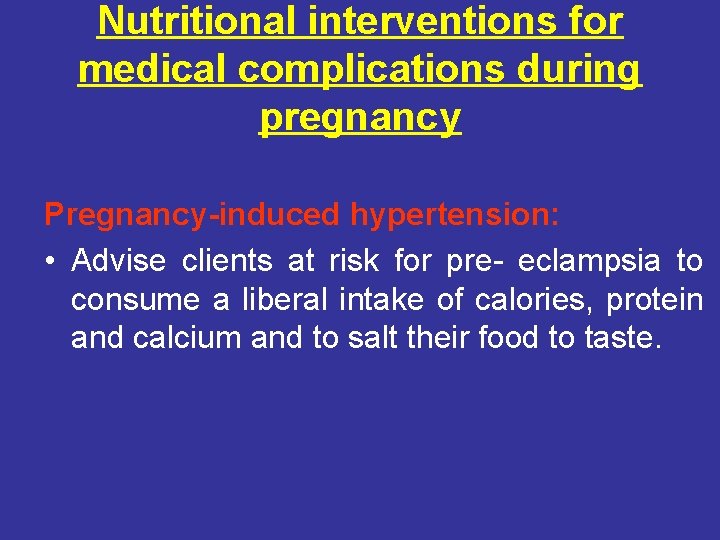
Nutritional interventions for medical complications during pregnancy Pregnancy-induced hypertension: • Pregnancy–induced hypertension (PIH or toxemia) is a hypertensive syndrome that occurs in approximately 6 - 7% of all pregnancies. Severe cases are associated with increased risks of maternal, fetal and neonatal death. • Although the exact cause is unknown.
Nutritional interventions for medical complications during pregnancy Risk factors for pregnancy-induced hypertension: • Poorly nourished. • Primigravida. • Economically deprived. • Very young or very old. • Obese. • Underweight.
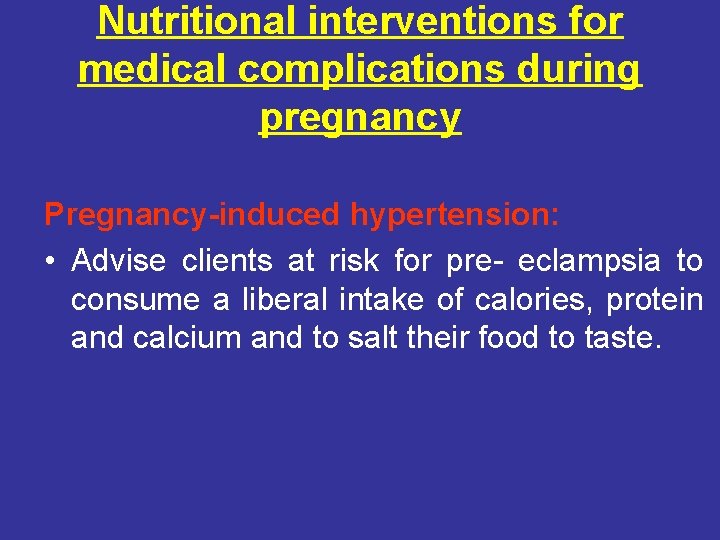
Nutritional interventions for medical complications during pregnancy Pregnancy-induced hypertension: • Advise clients at risk for pre- eclampsia to consume a liberal intake of calories, protein and calcium and to salt their food to taste.
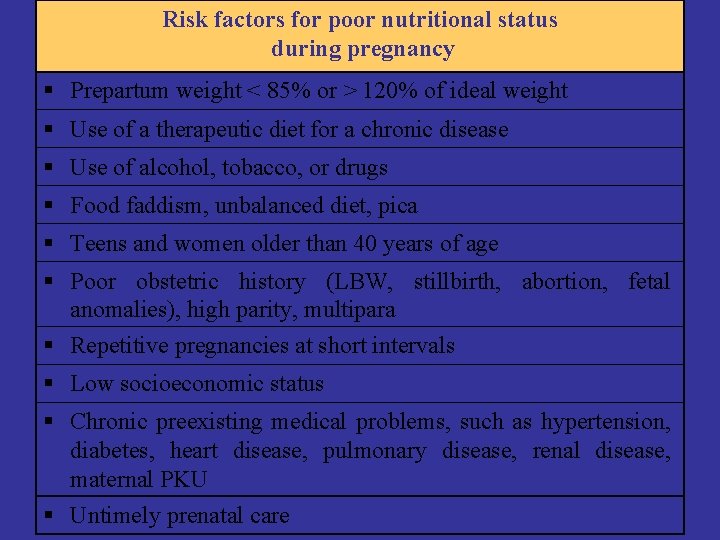
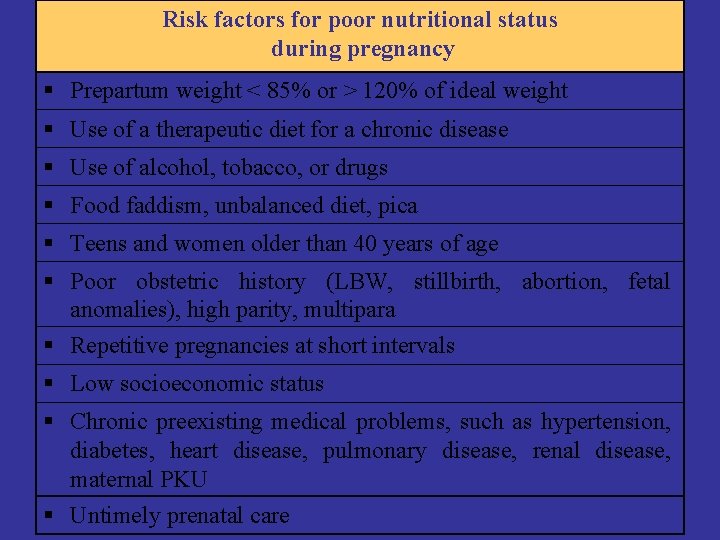
Risk factors for poor nutritional status during pregnancy Prepartum weight < 85% or > 120% of ideal weight Use of a therapeutic diet for a chronic disease Use of alcohol, tobacco, or drugs Food faddism, unbalanced diet, pica Teens and women older than 40 years of age Poor obstetric history (LBW, stillbirth, abortion, fetal anomalies), high parity, multipara Repetitive pregnancies at short intervals Low socioeconomic status Chronic preexisting medical problems, such as hypertension, diabetes, heart disease, pulmonary disease, renal disease, maternal PKU Untimely prenatal care
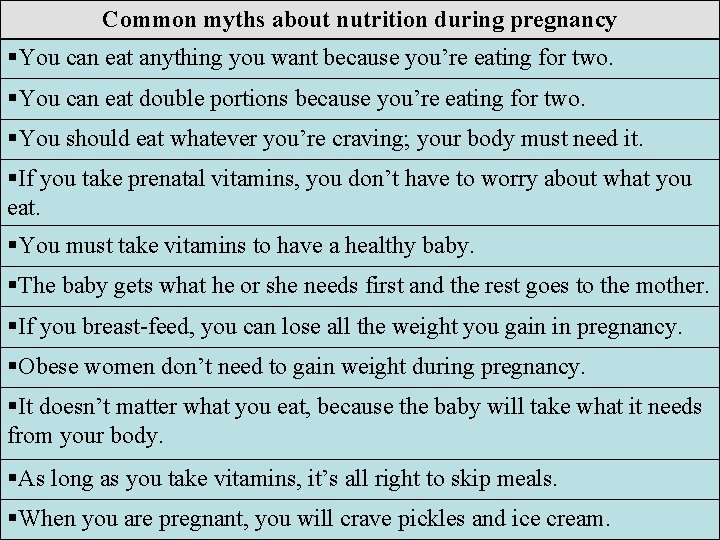
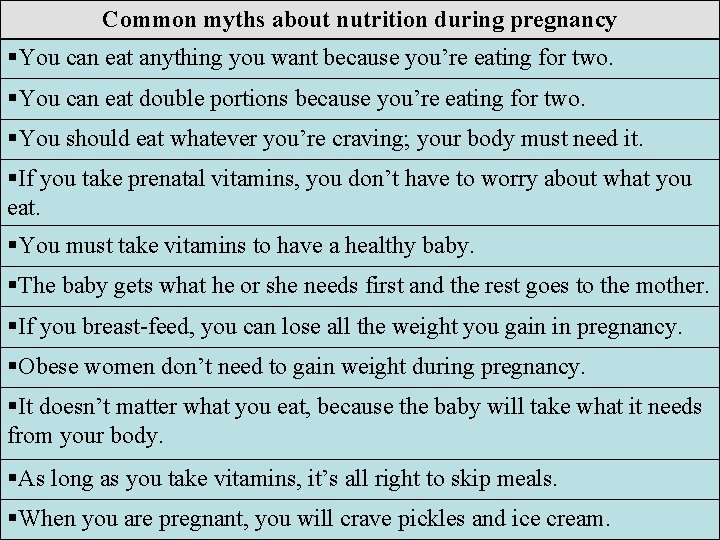
Common myths about nutrition during pregnancy You can eat anything you want because you’re eating for two. You can eat double portions because you’re eating for two. You should eat whatever you’re craving; your body must need it. If you take prenatal vitamins, you don’t have to worry about what you eat. You must take vitamins to have a healthy baby. The baby gets what he or she needs first and the rest goes to the mother. If you breast-feed, you can lose all the weight you gain in pregnancy. Obese women don’t need to gain weight during pregnancy. It doesn’t matter what you eat, because the baby will take what it needs from your body. As long as you take vitamins, it’s all right to skip meals. When you are pregnant, you will crave pickles and ice cream.
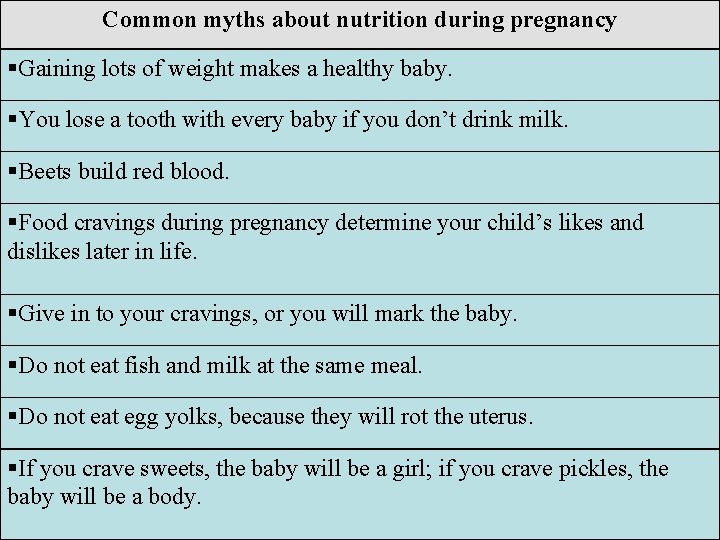
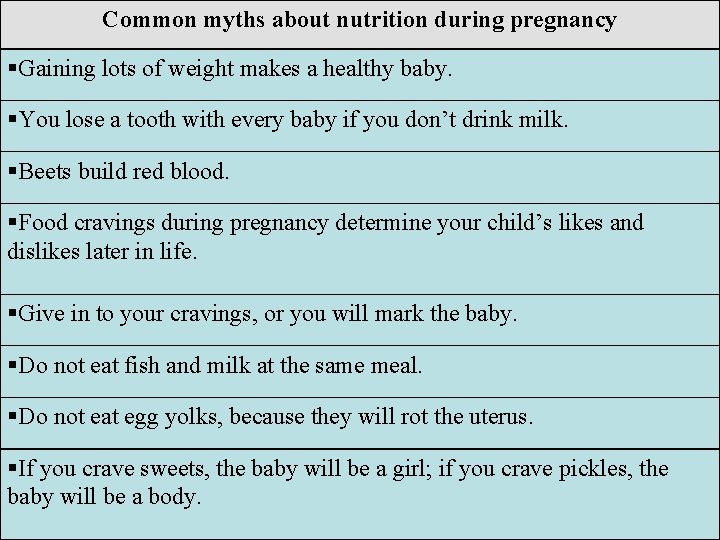
Common myths about nutrition during pregnancy Gaining lots of weight makes a healthy baby. You lose a tooth with every baby if you don’t drink milk. Beets build red blood. Food cravings during pregnancy determine your child’s likes and dislikes later in life. Give in to your cravings, or you will mark the baby. Do not eat fish and milk at the same meal. Do not eat egg yolks, because they will rot the uterus. If you crave sweets, the baby will be a girl; if you crave pickles, the baby will be a body.

Lactation • Because of the unquestionable benefits to both mother and infant, exclusive breastfeeding for the first 4 - 6 months of age is recommended for most full-term infants. • Breast-feeding with weaning to foods is recommended for at least the first 12 months of age.
Benefits of breast feeding For the mother: • Promotes optimal maternal-infant bonding. • Can mobilize fat stores to help women lose weight. • Early breast-feeding stimulates uterine contractions to help control blood loss and regain pregnant size. • Breast milk is readily available and requires no mixing or dilution.

Benefits of breast feeding For the mother: • Is less expensive than purchasing bottles, nipples, sterilizing equipment and formula. • May decrease the risk of thromboembolism, especially after operative deliveries. • Childbirth and breast-feeding may be protective against breast cancer.
Benefits of breast feeding For the infant: • “Breast is best” – breast milk is unique in its types and concentrations of macronutrients, micronutrients, enzymes, hormones, growth factors, inducers/modulators of the immune system and anti-inflammatory agents.
Benefits of breast feeding For the infant: • The infant can easily tolerate and digest and it changes to match the needs of a growing infant. • Is a “natural” food. • Sterile, is at the proper temperature and is readily available.

Benefits of breast feeding For the infant: • Breast-feeding promotes better tooth and jaw development than bottle-feeding because the infant has to suck harder. • Breast-feeding avoids nursing-bottle caries. • Breast-feeding is protective against food allergies.
Benefits of breast feeding For the infant: • Overfeeding is not likely with breast-feeding. • Breast-feeding is associated with decreased frequency of certain chronic diseases later in life, such as non-insulindependent diabetes mellitus & lymphoma.
Variables affecting breast milk composition • • • Stage of lactation. The mother’s diet. The duration of the feeding.
Variables affecting breast milk composition Stage of lactation: • Colostrum, which is secreted during the first few post-partum days, is a thick, yellowish fluid that is higher in protein, minerals and sodium than mature milk, but lower in sugar, fat and calories. • Colostrum is rich in antibodies and antiinfective factors.
Variables affecting breast milk composition Stage of lactation: • Colostrum begins to change to transitional milk about 3 to 6 days after delivery as the protein content decreases and the carbohydrate and fat contents increase. • Major changes in the milk take place by the tenth day and mature milk is stable by the end of the first month.
Variables affecting breast milk composition The mother’s diet: • The vitamin content of breast milk declines as a result of inadequate maternal intake, especially B 6, B 12, A and D.
Variables affecting breast milk composition The duration of the feeding: • The milk secreted as each feeding begins is significantly lower in fat than the milk secreted at the end of each feeding.
Nutritional needs for lactation Calories: • The average woman uses approximately 640 cal/day for the first 6 months and 510 cal/day during the second 6 months to produce a normal amount of milk.
Nutritional needs for lactation Protein • Women need an additional 20 g of protein while breast-feeding. Extra 2 cups of milk provide 16 g of protein.
Nutritional needs for lactation Fluid • It is suggested that nursing mothers drink 2 to 3 liters of fluid daily, preferably in the form of water, milk and fruit juices.
Nutritional needs for lactation Vitamins and minerals: • Foods, rather than supplements, are the preferred source of these nutrients, • women are encouraged to choose a varied diet that includes enriched and fortified grains and cereals, fresh fruits and vegetables and lean meats and dairy products.
Nutritional needs for lactation Vitamins and minerals: • Multivitamin and mineral supplements are not recommended for routine use. However, specific supplements may be indicated when maternal intake is inadequate.
Nutritional needs for lactation Foods to avoid: • Caffeine: consumption of one to two cups of coffee daily does not pose any problems. Intakes higher than this may cause the infant to become irritable and restless. • It usually is not necessary to eliminate any other foods while breast-feeding unless the infant shows intolerance.
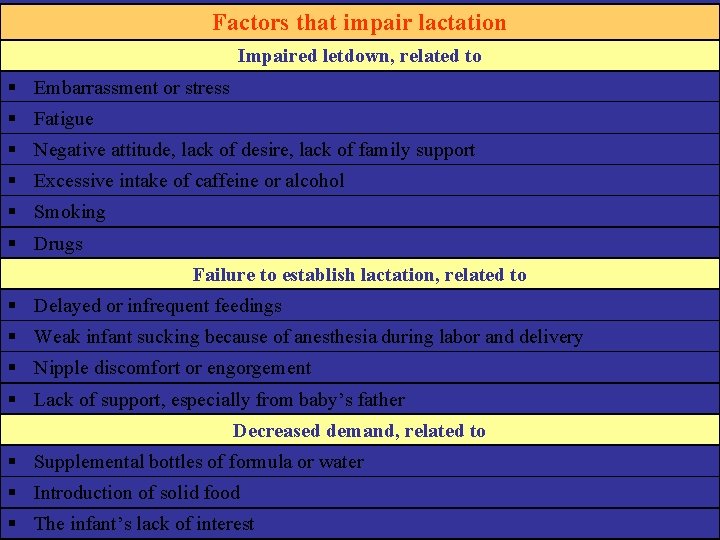
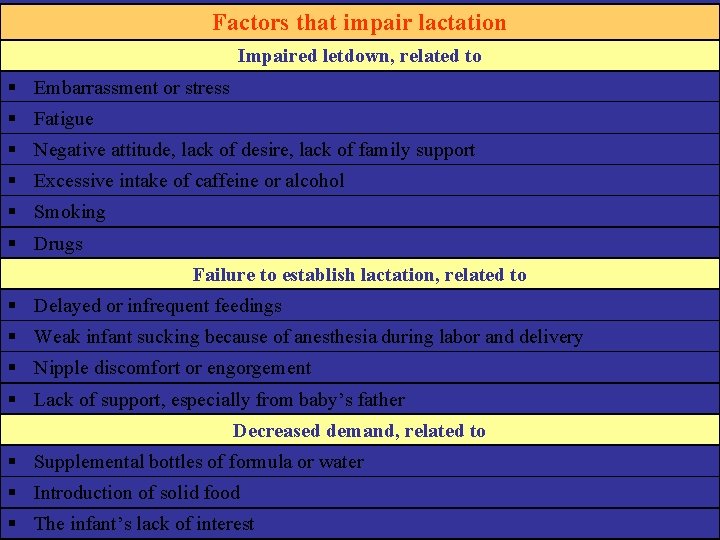
Factors that impair lactation Impaired letdown, related to Embarrassment or stress Fatigue Negative attitude, lack of desire, lack of family support Excessive intake of caffeine or alcohol Smoking Drugs Failure to establish lactation, related to Delayed or infrequent feedings Weak infant sucking because of anesthesia during labor and delivery Nipple discomfort or engorgement Lack of support, especially from baby’s father Decreased demand, related to Supplemental bottles of formula or water Introduction of solid food The infant’s lack of interest
Lactation in the diabetic mother • Breast-feeding complicates blood glucose control in women with type 1 diabetes by inducing hypoglycemia and lowering insulin requirements. • 35 cal/kg is usually recommended to achieve optimal glucose and lipid levels and promote moderate weight loss (4. 5 pounds/month).
Lactation in the diabetic mother Other points to consider include: • Careful and frequent monitoring of blood glucose level is essential. • Frequent snacks are recommended. • Unless breast-feeding occurs within 1 to 2 hours after eating, women should eat a light snack before or during breast-feeding.
Lactation in the diabetic mother Other points to consider include: • Breast care takes on greater importance. • Diabetic women face a higher risk of mastitis. Measures to prevent mastitis include alternating breasts when feeding, cleaning breasts with water and letting them air dry, making sure the baby’s mouth is positioned correctly over the nipple, drinking adequate fluids.
Lactation in the diabetic mother Other points to consider include: • Support groups may be especially helpful. • Encourage participation in appropriate programs that provide support and education.

 Lactation without pregnancy pictures
Lactation without pregnancy pictures Early pregnancy pictures of spotting during pregnancy
Early pregnancy pictures of spotting during pregnancy Nutrition through life cycle
Nutrition through life cycle Lactation drugs
Lactation drugs Lactation physiology
Lactation physiology United states lactation consultant association
United states lactation consultant association Ps12q
Ps12q Milk let down
Milk let down Lactation
Lactation Lactation mastitis treatment
Lactation mastitis treatment Levocetirizine montelukast
Levocetirizine montelukast Lactation curve
Lactation curve Difference between tetanus and tetany
Difference between tetanus and tetany Bacteria
Bacteria Hormones during pregnancy
Hormones during pregnancy Tocolytics
Tocolytics Role of nurse in reproductive health ppt
Role of nurse in reproductive health ppt Components of weight gain during pregnancy
Components of weight gain during pregnancy Sajda during pregnancy
Sajda during pregnancy Sore boobs early pregnancy
Sore boobs early pregnancy Fluticasone furoate pregnancy
Fluticasone furoate pregnancy Pregnancy and infant cohort monitoring and evaluation
Pregnancy and infant cohort monitoring and evaluation Wiggers diagram template
Wiggers diagram template Grade 11 animal nutrition
Grade 11 animal nutrition Nutrition across the lifespan
Nutrition across the lifespan Chapter 7 nutrition for life
Chapter 7 nutrition for life Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Gấu đi như thế nào
Gấu đi như thế nào Tư thế worm breton là gì
Tư thế worm breton là gì Alleluia hat len nguoi oi
Alleluia hat len nguoi oi Các môn thể thao bắt đầu bằng tiếng chạy
Các môn thể thao bắt đầu bằng tiếng chạy Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tiính động năng
Công thức tiính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Phép trừ bù
Phép trừ bù Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng bé xinh thế chỉ nói điều hay thôi
Cái miệng bé xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Giọng cùng tên là
Giọng cùng tên là Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Phối cảnh
Phối cảnh Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Dạng đột biến một nhiễm là
Dạng đột biến một nhiễm là Số nguyên tố là gì
Số nguyên tố là gì Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Hổ đẻ mỗi lứa mấy con
Hổ đẻ mỗi lứa mấy con Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập Sơ đồ cơ thể người
Sơ đồ cơ thể người Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Pregnancy and fetal development brainpop answers
Pregnancy and fetal development brainpop answers Budd-chiari syndrome triad
Budd-chiari syndrome triad Prenatal care and adaptations to pregnancy
Prenatal care and adaptations to pregnancy Chapter 20 reproduction and pregnancy
Chapter 20 reproduction and pregnancy Chapter 13 anatomy and physiology of pregnancy
Chapter 13 anatomy and physiology of pregnancy Trimester graphic organizer
Trimester graphic organizer Icd 10 twin pregnancy
Icd 10 twin pregnancy Adoloscense
Adoloscense Chapter 4 prenatal care and adaptations to pregnancy
Chapter 4 prenatal care and adaptations to pregnancy Pmat
Pmat Gait phases
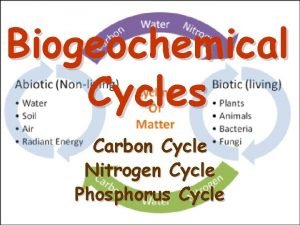
Gait phases Significance of biogeochemical cycle
Significance of biogeochemical cycle Difference between phosphorus cycle and carbon cycle
Difference between phosphorus cycle and carbon cycle Difference between open cycle and closed cycle gas turbine
Difference between open cycle and closed cycle gas turbine Reservation table in computer architecture
Reservation table in computer architecture Chapter 5 principles of engine operation
Chapter 5 principles of engine operation Disadvantages of mhd generator
Disadvantages of mhd generator