N 107 Essentials of Nursing Care Reproductive Health






















- Slides: 75
N 107 Essentials of Nursing Care: Reproductive Health Chapter 3: Needs of the Childbearing Family: Antepartal
Chapter Objectives Understand the S&S of Pregnancy n ID the physiological changes that take place during pregnancy n Know the discomforts of pregnancy and know appropriate interventions to help with discomforts n Describe psychosocial changes in the expectant family n

Chapter Objectives n n n Know what a nurse could tell a patient to promote self-care during pregnancy Know when a pregnancy is at risk due to chronic health problems Be knowledgeable of different medications used during pregnancy Be familiar with diagnostic tests and possible medical interventions used during pregnancy Be knowledgeable about the process of conception and implantation

Chapter Objectives Know about embryonic/fetal development n Understand the details and importance of the umbilical cord and placenta n Describe factors that influence fetal growth and well-being n Be knowledgeable of diagnostic test used during pregnancy n
Signs and Symptoms of Pregnancy n Antepartal – beginning of pregnancy to beginning of labor n Pregnancy made possible by the hypothalamic stimulation of the anterior pituitary hormones: follicle stimulating hormone (FSH), which stimulates follicle growth within the ovary, and luteinizing hormone (LH) which affects ovulation n 3 categories of S&S of pregnancy ¨ ¨ ¨ n n Presumptive – those felt by the woman Probable – those changes observed by the examiner Positive Signs – those signs credited only to the presence of the fetus Presumptive and probable could have other causes for their occurrences. Positive signs are completely objective and cannot be caused by other pathologic states
Signs and Symptoms of Pregnancy n Presumptive Signs ¨ ¨ ¨ Referred to as subjective Earliest is usually amenorrhea (in those with regular cycles) Morning sickness (can occur any time during day) n Due to elevated h. CG levels and changed CHO metabolism ¨ ¨ ¨ h. CG is biological marker on which all pregnancy test are based h. CG can be detected in the blood as early as 6 days after conception (or about 20 days since LMP) h. CG secreted by trophoblast (outer layer of uterus) Excessive fatigue Urinary frequency n n n Enlarging uterus putting pressure on bladder Symptoms decrease during 2 nd trimester as uterus becomes an abdominal organ Reappears during 3 rd trimester as fetus descends into pelvic region
Signs and Symptoms of Pregnancy n Presumptive Signs (Cont’d) ¨ Breast changes (enlargement, tenderness & tingling) May occur prior to missing 1 st menses n Growth due to hormones and growth of secretory ductal system. Tenderness and tingling most noticeable around nipple area n ¨ Quickening (fetal movements) Week 14 – 16 in a multigravida woman n Week 18 or later in primagravida woman n

Signs and Symptoms of Pregnancy n Probable Signs (Objective) ¨ Observed through inspection or palpation ¨ Changes in pelvic organs caused by increased vascular congestion n Only physical signs detectable with the first 3 months of pregnancy ¨ ¨ ¨ Goodell’s sign – softening of cervix Chadwick’s sign – deep red to purple bluish coloration of the mucous membranes of cervix, vagina and vulva Hegar’s Sign – softening and compressibility of the lower uterine segment Mc. Donald's Sign – easy flexion of the fundus on the cervix Braun von Fernwald’s Sign – Softening and slight fullness of the fundus near the area of implantation Piskacek’s Sign – a soft lateral bulge with corneal implantation
Signs and Symptoms of Pregnancy n Probable Signs (Cont’d) ¨ Ultrasound n Uterine soufflé (bruit) – sound of maternal blood flowing through uterine arteries to placenta ¨ n Synchronous with maternal pulse Funic soufflé – caused by fetal blood coursing though the umbilical cord ¨ n or fetal stethoscope Synchronous with fetal heart tone Fetal heart tone – actual heartbeat of fetus
Signs and Symptoms of Pregnancy n Other manifestations ¨ Facial chloasma, melasma (mask of pregnancy) n Blotchy, brownish hyperpigmentation of the skin over cheeks, nose & forehead ¨ Accentuated by sun exposure ¨ Linea nigra – pigmented line down midline of abdomen ¨ Striae gravidarum – stretch marks n Abdomen & buttocks Ballotment – examiner pushes up against cervix with 2 fingers to elicit a passive rebound fetal movement. ID’d between week 16 - 18

Signs & Symptoms of Pregnancy n Positive signs of pregnancy (definitive) ¨ Visualization n of fetus via US Weeks 5 – 6 ¨ Fetal heart tones heard at 6 weeks ¨ Fetal heart tones heard by doppler at 10 -17 weeks ¨ Fetal heart tones heard by stethoscope at weeks 17 – 19 ¨ Fetal movements palpated at weeks 19 - 22
Physiological Changes During Pregnancy n Uterine Growth ¨ Response to hormonal stimulus n High levels of estrogen and progesterone ¨ Fundal height n Uterus enlarges at predictable rate. Measurement used to estimate the duration of pregnancy Palpable at symphis pubis between week 12 – 14 ¨ Palpable at umbilicus level at week 22 – 24 ¨ At level of xyphoid process at term ¨ n Lightening – fundal height decreases weeks 38 – 40 as fetus descends and engages the pelvis
Physiological Changes During Pregnancy ¨ Braxton Hicks contractions – irregular painless contractions of the uterus that occur intermittently throughout pregnancy starting soon after 4 th month Contractions stimulate the movement of blood through the placenta and promote oxygen delivery to the fetus. n Increase in frequency during late pregnancy. n Not true labor contractions n
Physiological Changes During Pregnancy n Breast Changes ¨ Result of increased levels of estrogen and progesterone ¨ Development of mammary glands is complete by mid pregnancy ¨ Lactation does not occur until birth of baby and placenta n Estrogen levels decrease ¨ Colostrum n Creamy, white to yellow pre-milk fluid expressed from nipples as early as week 16
Physiological Changes During Pregnancy n Skin ¨ Changes thought to occur due to increased estrogen, progesterone and alpha-melanocyte-stimulating hormone levels ¨ Sweat and sebaceous glands usually hyperactive ¨ Angiomas (telangiectasias) - Vascular spider nevi may appear on the chest, neck, face, arms and legs. Of no clinical significance and disappear after pregnancy. Due to increased levels of estrogen ¨ Palmar erythema – color changes which occur over the palmer surface of the hands. Due to increased levels of estrogen and progesterone
Physiological Changes During Pregnancy n Hormones ¨ Thyroid – moderate enlargement; increased vascularity n n T 4 levels decrease in response to increased estrogen Oxygen consumption and basic metabolic rate (BMR) increase as much as 20 -25% secondary to fetal metabolic activity ¨ Parathyroid n n n Slight secondary hyperparathyroidism Plasma parathormone are elevated Coincides with fetal skeletal growth ¨ The increased requirements for calcium and Vitamin D
Physiological Changes During Pregnancy ¨ Pituitary n Prolactin responsible for initial lactation ¨ Posterior Pituitary Releases oxytocin which promotes uterine contractility and the stimulation of milk ejection from the breasts n Releases vasopressin which results in increased BP by vasoconstriction and has an antidiuretic effect to maintain water balance. n
Physiological Changes During Pregnancy n Adrenals Glands ¨ Secrete increased levels of aldosterone by the early part of 2 nd trimester in a protective response to the increased sodium excretion associated with progesterone. ¨ Cortisol production increases which increases production of insulin but also increases mother peripheral resistance to insulin n This decreases mother’s ability to use her own insulin, thus ensuring ample supply of glucose for fetoplacental unit
Physiological Changes During Pregnancy n Pancreas ¨ Responsible for insulin production to lower glucose levels ¨ The fetus requires ample amount of glucose for growth and development ¨ The islet of Langerhans (beta cells) are stressed to meet the mother’s increased needs for insulin n Deficiency produces S&S of gestational diabetes
Physiological Changes During Pregnancy n Hormones Required to Maintain Pregnancy ¨ h. CG n n ¨ Secreted early in pregnancy Stimulates progesterone and estrogen production by the corpus luteum to maintain pregnancy until placenta has developed sufficiently enough to support it Human Placental Lactogen n Increases the amount of circulating free fatty acids for maternal metabolic needs and decreases maternal metabolism of glucose to favor fetal grown

Physiological Changes During Pregnancy n Hormones Required to Maintain Pregnancy ¨ Estrogen n Stimulates uterine development to provide a suitable environment for the fetus while helping to develop the ductal system of the breast in preparation for lactation ¨ Progesterone n Maintains the endometrium, inhibiting spontaneous abortion n Helps development of acini & lobules of the breasts in preparation for lactation ¨ Relaxin n Inhibits uterine activity n Diminishes the strength of uterine contractions n Aids in the softening of the cervix n Has long-term effect of remodeling collagen
Physiological Changes During Pregnancy n Other Hormones ¨ Prostaglandins n Lipid substances that occur in high concentrations in female reproductive tract n Present in the endometrium or lining of uterus during pregnancy n Present in the tissue around the ectopically located fertilized ovum during pregnancy n Exact functions unknown n Decreased levels may contribute to HTN and pregnancy induced HTN (PID)

Physiological Changes During Pregnancy n Other Hormones ¨ Mucus Plug Result of secretions from endocervical glands n Plug seals the endocervical canal & prevents invasion of bacteria or other substances into uterus n Secretions favor the growth of yeast organisms monilasis, a common vaginal infection during pregnancy n
Physiological Changes During Pregnancy n Metabolic The expectant mother must meet her own tissue replacement needs, those of the fetus, and those preparatory for labor and lactation ¨ Recommended weight gain ¨ n n n ¨ Woman of normal wt = 25 – 35 pounds Overweight woman = 15 – 25 pounds Underweight woman = 28 – 40 pounds Avg increases n n n 3. 5 – 5 pounds 1 st trimester 12 – 16 pounds 2 nd trimester 10 – 13 pounds 3 rd trimester
Physiological Changes During Pregnancy n Metabolic (Cont’d) ¨ Water retention is a basic chemical alteration of pregnancy; caused by an increased level of steroid sex hormones, lowered serum protein and increased intracapillary pressure permeability. The extra water is needed for the fetus, placenta, and amniotic fluid, in addition to the mother’s increased blood volume, interstitial fluids, and enlarged organs.
Physiological Changes During Pregnancy n BMR (Basic Metabolic Rate) is increased by 15 -20% by term ¨ Reflects increased oxygen demand of uterineplacental-fetal unit as well as oxygen consumption from increased maternal cardiac work ¨ High risk for heat intolerance ¨ During early pregnancy may report feeling hot & fatigued after slight exertion. ¨ Greater need for sleep
Physiological Changes During Pregnancy n Cardiovascular System ¨ Growing fetus pushes heart upward and left ¨ Blood volume increases throughout pregnancy; 45% increase in 3 rd trimester ¨ Cardiac hypertrophy n n about Increase in blood volume and cardiac output Both plasma and erythrocytes increase ¨ Systemic Vascular Resistance & Pulmonary Vascular Resistance decrease enabling circulation to adapt to higher blood volume while maintaining normal vessel pressures
Physiological Changes During Pregnancy n CV System (cont’d) ¨ CO increases due to increased tissue demand for oxygen ¨ CO higher when lying in lateral recumbent position; lower when in supine position ¨ CO increased with labor and birth ¨ Organ systems receive additional blood flow according to their increased workload ¨ Heart rate increases about 10 -15 BPM ¨ Palpitations and dysrhythmias may occur. n If no underlying pathology, no treatment required
Physiological Changes During Pregnancy n CV (cont’d) ¨ BP n considerations Same position, same arm, correct cuff size ¨ Dependent edema, varicose veins, hemorrhoids due to uterus compressing iliac veins and inferior vena cava increased venous pressure and reduced blood flow to lower extremities n More prone to postural hypotension

Physiological Changes During Pregnancy n CV (cont’d) ¨ Venal Caval Syndrome (Supine hypotensive syndrome/autocaval compression) n Enlarging uterus putting pressure on the vena cava when in supine position Interferes with blood return ¨ Significant decrease in BP with symptoms § Dizziness, pallor, clamminess § Corrected by placing in left side-lying position ¨
Physiological Changes During Pregnancy n CV (cont’d) ¨ Blood n volume increases 40 -50% Peripheral vasodilation maintains normal BP ¨ Total erythrocyte volume increases about 30% in women who receive iron supplementation; only 18% in those without iron supplementation ¨ Plasma increase > RBC production decrease in Hematocrit (psuedoanemia) n Elevated erythrocyte production increases need for iron, because iron is necessary for the formation of hemoglobin (oxygen carrying component of erythrocytes)

Physiological Changes During Pregnancy n CV (cont’d) ¨ Higher risk for hypercoagulation (clot formation) Various clotting factors increase during pregnancy n Fibrinolytic activity (dissolving actions of clots) decreased n Venous stasis DVT formation n
Physiological Changes During Pregnancy n Respiratory System ¨ Maternal oxygen requirements increase n n n ¨ Increase in BMR Need to add tissue mass in uterus and breast Fetus requires oxygen and needs to dispose of carbon monoxide Elevated estrogen levels n n cause ligaments of rib cage to relax which allows increased chest expansion Cause an increase in vascularization in upper respiratory tract ¨ ¨ capillary congestion nasal & sinus congestion, nosebleeds, changes in voice, changes in respiratory center (a lower threshold for CO 2) During advanced pregnancy, increased awareness of the need to breathe evident; some complain of SOB; some complain of dyspnea at rest
Physiological Changes During Pregnancy n Gastrointestinal (GI) ¨ During pregnancy n Appetite increases, intestinal secretions reduced, liver function is altered, absorption of nutrients is enhanced, colon is displaced, GI motility decreases n Bowel sounds decrease, nausea and vomiting are common n An increase in blood flow and pressure on pelvic areas (later in pregnancy) places pregnant woman at increased risk for hemorrhoids
Physiological Changes During Pregnancy n GI (cont’d) ¨ Early in pregnancy n Morning sickness (with or with vomiting) Can occur at any time of day/night ¨ Usually appears 4 -6 weeks & subsides after 1 st trimester ¨ Triggered by sight or odors ¨ Appetite may be decreased ¨ h. CG has depressant effect on appetite ¨ n Hyperemesis (severe vomiting) Should not continue beyond 1 st trimester ¨ Should not be accompanied by fever, pain or weight loss ¨ If either occurs, medical intervention necessary ¨
Physiological Changes During Pregnancy n GI (cont’d) ¨ Morning sickness rarely has harmful effects on mother or fetus ¨ Rising levels of estrogen cause selective increase in vascularity and connective tissue proliferation (gingivitis) and causes gums to bleed ¨ Hiatal hernia n n Can occur after 7 th month of pregnancy Usually due to displacement of stomach
Physiological Changes During Pregnancy n GI (cont’d) ¨ increased progesterone production causes: Esophageal regurgitation, slower emptying of stomach and reverse peristalsis from decreased tone and motility of smooth muscles n Increase in water absorption from colon constipation n ¨ Increased risk for gallstones
Physiological Changes During Pregnancy n Genitourinary System(GU) ¨ Affected by pressure from bladder, increased blood flow & increased filtration in the tubules n 1 st trimester ¨ n 2 nd trimester ¨ n Bladder irritability, nocturia, frequency due to growing uterus placing pressure on bladder Bladder is pulled up and out of pelvis into abdomen 3 rd trimester ¨ Due to pressure from presenting part, impaired drainage of blood and lymph, bladder more susceptible to infection and trauma
Physiological Changes During Pregnancy n GU (cont’d) ¨ Susceptibility to infection n ¨ Greater glucose content More alkaline (p. H increased) Stagnated urine (takes longer to reach bladder) Renal function n n Glomerular Filtration Rate (GFR) increases Renal Plasma Flow (RPF) increases Least efficient when in the supine position Most efficient in lateral recumbent position ¨ n Side lying increases renal perfusion, increases UOP, and decreases edema Due to vena cava syndrome and compression of aorta, CO drops as does renal perfusion
Physiological Changes During Pregnancy n GU (cont’d) ¨ Renal system can overstressed by excessive sodium intake or restriction or by using diuretics ¨ Extra sodium is needed for both mother and fetus during pregnancy ¨ Selective renal tubular reabsorption maintains sodium and water balance regardless of changes in dietary intake and losses ¨ Severe hypovolemia and reduced placental perfusion are consequences of using diuretics during pregnancy
Physiological Changes During Pregnancy n GU (cont’d) ¨ Glucose n reabsorption is impaired Glucosuria varies in time and degree ¨ Proteinuria does not usually occur in normal pregnancy except during labor or after birth The amount of protein excreted does not indicate the severity of renal disease n Values of 1+ protein (per dipstick) is acceptable n
Physiological Changes During Pregnancy n Musculoskeletal Alterations in posture and gait due to weight gain ¨ Spinal curvatures are re-aligned ¨ Lordosis develops ¨ n n ¨ Pelvic joints become more mobile and relaxed due to increased estrogen & other circulating hormones (relaxin) n ¨ An increase in curvature of spine The head is held Lordly, like a King to maintain balance This also allows an increase in pelvic dimensions preparing for labor and birth Abdominal walls stretch and loose tone

Discomforts of Pregnancy n First Trimester ¨ Breast Changes ¨ Urgency/Frequency ¨ Languor & Malaise/Fatigue ¨ Nausea/Vomiting (Morning Sickness ¨ Ptyalism (Excessive Salivation) ¨ Psychological Effects; Mood Swings; Mixed Feelings
Discomforts of Pregnancy n Second Trimester ¨ Skin changes ¨ Spider Nevi (Telangiectasias ¨ Palmar Erythema ¨ Pruritus ¨ Palpitations ¨ Supine Hypotension (Vena Cava Syndrome) ¨ Orthostatic Hypotension

Discomforts of Pregnancy n 2 nd Trimester (Cont’d) ¨ Food Cravings ¨ Heartburn/Indigestion ¨ Constipation ¨ Flatulence/Bloating/Belching ¨ Varicose Veins ¨ Leukorrhea ¨ Headaches
Discomforts of Pregnancy n 2 nd Trimester (Cont’d) ¨ Carpal Tunnel Syndrome ¨ Acrodysesthesia (Numbness/Tingling of Fingers ¨ Round Ligament Pain/Tenderness ¨ Joint Pain/Backache/Pelvic Pressure Hypermobility of Joints

Discomforts of Pregnancy n Third Trimester ¨ Respiratory Discomforts ¨ Insomnia ¨ Psychological Responses/Mood Swings Mixed Feelings/Anxiety ¨ Hyperemia, Hypertrophy, Bleeding Tendencies ¨ Return of GU Symptoms

Discomforts of Pregnancy n 3 rd Trimester (Cont’d) ¨ Perineal Discomfort and Pressure ¨ Braxton Hicks Contractions ¨ Leg Cramps ¨ Marked Edema ¨ Nasal Stuffiness
The Expectant Family n Psychosocial Changes ¨ Pregnancy represents a turning point in the affected individuals’ lives ¨ Support system ¨ Altered routines and family dynamics ¨ Financial issues n n Will expectant mother work during pregnancy? Will expectant mother work after baby is born? Who will provide childcare if mother does work? Will housework & care for the child at home be divided?
The Expectant Family n Emotional Responses ¨ Ambivalence, introversion, mood swings & changes in body image ¨ Ambivalence may be related to many things (See page 73) ¨ Indirect evidence of ambivalence n n n c/o prolonged or frequent depression Physical discomforts Body image Excessive mood swings Difficulty accepting life changes resulting from pregnancy
The Expectant Family n Emotional Responses (cont’d) ¨ Women with unplanned or unwanted pregnancies experience: Increased depression n Increased stress n Decreased support from the father n Decreased overall satisfaction with life n
The Expectant Family n Emotional Responses ¨ Women with planned pregnancies n n n tend to be happier Experience less physical discomforts Tolerate discomforts associated with 3 rd trimester Introversion is common during pregnancy ¨ Mood swings ¨ Need increased love and affection from partner ¨ Concerns about body image ¨ n Personality traits, values, social network responses and attitude toward pregnancy are thought to influence her body image
The Expectant Family n Role Transition ¨ Four psychological tasks the expectant mother undertakes to maintain her intactness and that of her family while also incorporating her new child into the family system: n n Prenatal care Seeking partner’s acceptance and support Preparing herself to protect fetus and child once born Learning to delay immediate gratification to meet the needs of another

The Expectant Family n The Expectant Father ¨ May experience ambivalence and stress also n n n ¨ Reality of new role Financial issues Unexpected events Health of baby His role during labor and birth The successful father: n n n Likes children Excited about fatherhood Want to nurture Have parenting confidence Share experience of pregnancy and childbirth with their parents
The Expectant Family n The Expectant Father ¨ 1 st trimester n n ¨ 2 nd trimester n n n ¨ Confused by woman’s mood swings Resentful of attention given to mother-to-be Feel more involved by feeling fetal movements See fetus on US Plans parenting style 3 rd trimester n n Afraid of hurting unborn child during intercourse Have increased anxiety over outcome of partner and baby during labor and birth

Promotion of Self-Care During Pregnancy n Estimated Date of Birth ¨ AKA n n Estimated Date of Confinement (EDC) Due Date Most common method = Nagele’s Rule ¨ ¨ ¨ n LMP – 3 months + 7 days LMP (5/8/2011) – 3 months = 2/8/11 + 7 days = EDC of 2/15/2012 Rule can be adjusted for those who have irregular menstrual cycles ¨ Fundal Height (See page 77)

Promotion of Self-Care During Pregnancy n Nutrition/Supplements Pregnant woman need additional 300 kilocalories per day during 2 nd & 3 rd trimesters ¨ Lactating mother needs additional 500 kilocalories per day ¨ Factors that increase nutrient needs: n Uterine-placental unit n Maternal blood volume and constituents, n Maternal mammary changes n Metabolic needs (BMR increases) ¨ Daily food plan should include all food groups + Vitamins + Minerals n See page 77 -80 n PICA (non food sources) or non-nutritional food should be avoided as much as possible ¨ Nurse should be non-judgmental when assessing for PICA ¨
Promotion of Self-Care During Pregnancy n Teratogenic Substances that cause abnormal development of the embryo n Alcohol fetal alcohol syndrome ¨ Maternal alcohol use spontaneous abortion n Smoking IUGR ¨ Increase risks for preterm labor, premature rupture of membrane (PROM), abruption placentae, placenta previa and fetal death R/T decreased placental perfusion ¨ Illegal or Controlled Substance Abuse n IUGR and developmental delay ¨ Focus for mother with any detrimental habit should be Good Nutrition ¨
Promotion of Self-Care During Pregnancy n Teratogenic Substances ¨ Congenital anomaly n Condition present at birth ¨ Known human teratogens n Drugs, chemicals, infections, radiation, DM, PKU n Greatest impact during periods of rapid differentiation Embryonic period (days 15 – 60) ¨ Fetus unable to use maternal reserves, subsequently all nutrients come directly from mother’s diet ¨
Promotion of Self-Care During Pregnancy n Activity and Exercise ¨ Consult physician before starting an exercise regimen ¨ Exercise should be moderate and consistent ¨ Fluid intake should be increased before during and after exercise to prevent dehydration n Dehydration preterm labor ¨ Aerobic 140 n exercise recommended with maternal HR<or= Do NOT proceed to fatigue or exhaustion decrease uterine profusion &/or fetoplacental deoxygenation
Promotion of Self-Care During Pregnancy n Screenings and Lab Test ¨ Numerous Labs, blood type & Rh, rubella, TB, urine, renal function, pap smear, STD/HIV. n Alpha-fetoprotein is done at 16 weeks n Triple Marker Test (Triple Screen) n Group B Streptococci n
Promotion of Self-Care During Pregnancy n Screenings and Lab Test ¨ HIV (Human Immunodeficiency Virus) n causes Acquired Immune Deficiency Disease [AIDS] n Should be tested during prenatal period n Pregnancy is discouraged n Common presenting problems ¨ Chronic vaginitis & candidiasis (thrush) n Treatment started prior to 14 th week of pregnancy has shown a 66% decrease in lateral transmission to fetus with caesarian section ¨ Treatment is Zidovudine (AZT) ¨ n Fetus will test positive for HIV antibody for up to 18 months even if not infected HIV can be transmitted through breast milk

Promotion of Self-Care During Pregnancy n Screenings and Lab Test ¨ TORCH Infections Toxoplasmosis n Other infections n Rubella Virus n Cytomegalovirus n Herpes simplex Virus n
Promotion of Self-Care During Pregnancy n Screenings and Lab Test ¨ TORCH Infections n Toxoplasmosis n Cause ¨ ¨ n n Consumption of infected raw or undercooked meat or handling infection cat litter Can cause spontaneous abortions &/or congenital infections Diagnosis: Serologic testing Treatment: Pyrimethamin and sulfadiazine ¨ Can reduce risk to fetus by 60%
Promotion of Self-Care During Pregnancy n Screenings and Lab Test ¨ TORCH Infections n Other Infections Hepatitis A, B, C, D ¨ Causes: § Hep A – feces § Hep B – blood products & body fluids § Hep C – direct blood contact (IV drug users, receivers of blood products) § Hep D – same as Hep B; ¨
Promotion of Self-Care During Pregnancy n Screenings and Lab Test ¨ TORCH Infections n Rubella (German Measles) ¨ ¨ ¨ Cause: contact with droplets Clinical Signs § Heart Dz, IUGR, cataracts Complications: spontaneous abortions, heart damage, cataracts, mental retardation Infants are infectious and require isolation Prevention: Rubella vaccine (prenatal assessment) § Serious fetal consequences; vaccination not warranted during pregnancy
Promotion of Self-Care During Pregnancy n Screenings and Lab Test ¨ TORCH Infections n Cytomegalovirus ¨ ¨ ¨ Cause: Herpes Virus § Transmitted by respiratory droplets or body fluids (less likely) § Women who have + titer usually have chronic or recurrent infections § Not normally harmful to mothers with intact immune systems Treatment: No known treatment Complications: Primary cause of congenital infection in fetus and neonate Most common infectious cause of mental retardation Most at Risk: women who work or have children in daycare, mental health facilities or certain health care settings
Promotion of Self-Care During Pregnancy n Screenings and Lab Test ¨ TORCH Infections n Herpes Simplex Virus (HSV) ¨ ¨ n n Type I – contact with oral secretions Type II –contact with genital secretions Treatment: Acyclovir Prevention of lateral transfer: Cesarean birth within 4 hours of ruptured membranes ¨ ¨ Neonate and fetal effects are profound Good hand washing especially if lesions are present Healthcare providers with oral lesions present should practice good hand hygiene and wear masks when in contact with newborns Anyone with skin lesions should not give direct care until lesions are dried and crusted.






 Essentials of health care marketing
Essentials of health care marketing Nursing diagnosis for ocd
Nursing diagnosis for ocd Nursing diagnosis for vision impairment
Nursing diagnosis for vision impairment Primary secondary tertiary care nursing
Primary secondary tertiary care nursing Family care plan in community health nursing
Family care plan in community health nursing Essentials of nursing leadership & management
Essentials of nursing leadership & management Care value base health and social care
Care value base health and social care Scottish patient safety programme
Scottish patient safety programme Health and social care component 3 health and wellbeing
Health and social care component 3 health and wellbeing Focus on pharmacology essentials for health professionals
Focus on pharmacology essentials for health professionals Lomotib
Lomotib Nursing management of reproductive tract infection
Nursing management of reproductive tract infection How to care reproductive system
How to care reproductive system Inguinal hernia are a female reproductive health issue
Inguinal hernia are a female reproductive health issue Rch programme definition
Rch programme definition What is the definition of reproductive health
What is the definition of reproductive health Interconception definition
Interconception definition Height of fundus during pregnancy
Height of fundus during pregnancy Reproductive and child health programme phase 1
Reproductive and child health programme phase 1 Psalm 107:23–32
Psalm 107:23–32 Dpr 80 2013 sintesi
Dpr 80 2013 sintesi Prime number 105
Prime number 105 Ilang pulo binubuo ang pilipinas
Ilang pulo binubuo ang pilipinas Grande barrio central
Grande barrio central 107/2010
107/2010 Doc 107
Doc 107 Fas 105
Fas 105 Quanto devo aplicar hoje a taxa de 51 107 ao ano
Quanto devo aplicar hoje a taxa de 51 107 ao ano Cs 107
Cs 107 Pl 107-208
Pl 107-208 Cbtis 107
Cbtis 107 Psalm 107:12
Psalm 107:12 Tom sensky
Tom sensky Legge 107 del 2015
Legge 107 del 2015 Mont 107
Mont 107 The verb estar (p. 107)
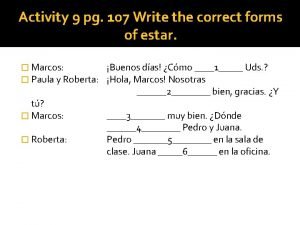
The verb estar (p. 107) Cornell cooperative extension schenectady
Cornell cooperative extension schenectady Marta and berta are getting ready for school
Marta and berta are getting ready for school 107 108 109
107 108 109 Przedszkole 107 warszawa
Przedszkole 107 warszawa Legge n. 107 del 2015
Legge n. 107 del 2015 101 102 103 104 105 106 107 108
101 102 103 104 105 106 107 108 Psalm 107:4-9
Psalm 107:4-9 Manifestação da vontade
Manifestação da vontade -2x^2-9=-107
-2x^2-9=-107 Ppt 107
Ppt 107 12*107
12*107 Fondo colores
Fondo colores Gylot 107
Gylot 107 Legge 13 luglio 2015 n. 107 sintesi
Legge 13 luglio 2015 n. 107 sintesi Alex kroll
Alex kroll Pag 107
Pag 107 Ac 20-107
Ac 20-107 107 1 fm
107 1 fm 105 106 107
105 106 107 Patient care delivery models
Patient care delivery models Nursing care plan evaluation examples
Nursing care plan evaluation examples Nursing process in psychiatric nursing
Nursing process in psychiatric nursing As evidenced by nursing examples
As evidenced by nursing examples Primary nursing care model
Primary nursing care model Associative looseness
Associative looseness High fowlers position
High fowlers position Definition of perioperative nursing
Definition of perioperative nursing Intraoperative care definition
Intraoperative care definition Nursing care of hospitalized child
Nursing care of hospitalized child Post operative nursing care
Post operative nursing care Nail care procedure in nursing
Nail care procedure in nursing Nursing care plan for gingivitis
Nursing care plan for gingivitis Hernia nursing care plan
Hernia nursing care plan Chapter 41 rehabilitation and restorative nursing care
Chapter 41 rehabilitation and restorative nursing care Angina pectoris care plan
Angina pectoris care plan Post operative nursing care
Post operative nursing care Atraumatic care meaning
Atraumatic care meaning Atraumatic care definition
Atraumatic care definition Virginia henderson conclusion
Virginia henderson conclusion Somatoform disorder nursing diagnosis
Somatoform disorder nursing diagnosis