INTRAOPERATIVE MANAGEMENT OF CATARACT SURGERY COMPLICATIONS Dr H































- Slides: 95


INTRA-OPERATIVE MANAGEMENT OF CATARACT SURGERY COMPLICATIONS Dr. H. Razmjoo Isfahan University of Medical Sciences
High Risk Cases for VL § 1 - Loose zonules & Phacodonesis § 2 - Lens subluxation § 3 - Miotic pupil § 4 - Glucomatus cases with shallow AC § 5 - Brunescent lenses § 6 - High refractory errors

High Risk Cases for VL § § § § 7 -Pseudoexfoliation Syndrome 8 -Traumatic Cataract 9 - Fellow eye of Complicated Cataract Surgery 10 - Eyes with Transillumination defects in Iris 11 - Previously Vitrectomized eyes 12 - Hypermature cataracts 13 - Very Aged patient 14 - Intra operative floppy iris syndrome
• Management of Phacodonesis § Chopping technique is preferred for phacoemulsification § Use CTR § Lens removal in the presence of severe phacodonesis can be facilitated by temporary suspension of the capsule using iris hooks.

§ A capsular tension ring alone is not sufficient if the zonular defect is larger than 5 h(150 Degree)

Capsule Tension Rings § Dialysis of 2– 3 h (<90°)—CTR is an option, not a necessity. § Dialysis of 3– 5 h (90– 150°)—CTR is required to assure capsular stability and IOL centration. § Dialysis of 5– 7 h (150– 210°)—CTR can be used, but may not be sufficient. The lens or the ring should also sutured to adjacent structures.
§ Dialysis of more than 7 h usually requires complete lens removal and implantation of an AC-IOL (angle or iris supported) or PC-IOL sutured to the sclera and/or iris.
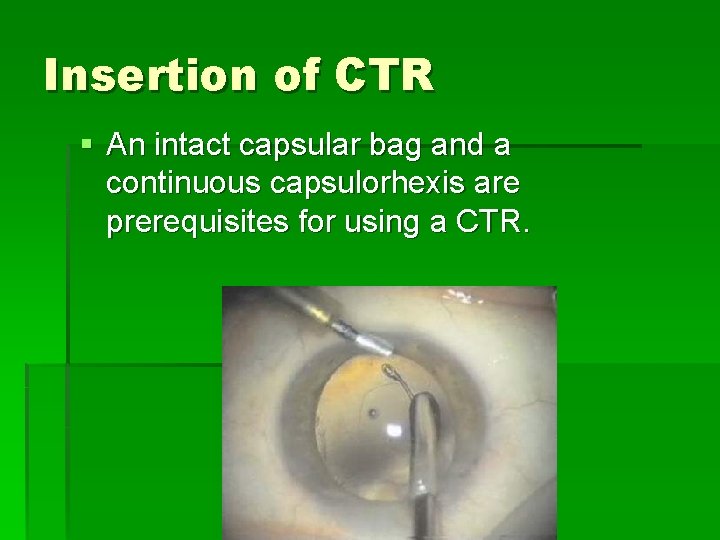
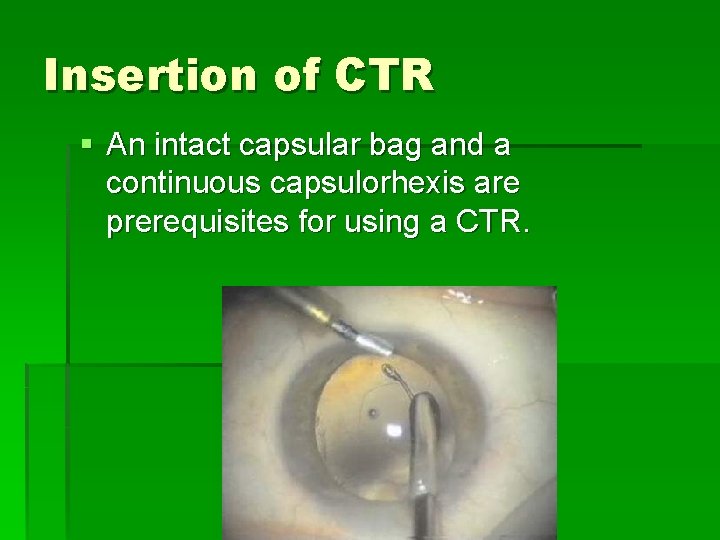
Insertion of CTR § An intact capsular bag and a continuous capsulorhexis are prerequisites for using a CTR.
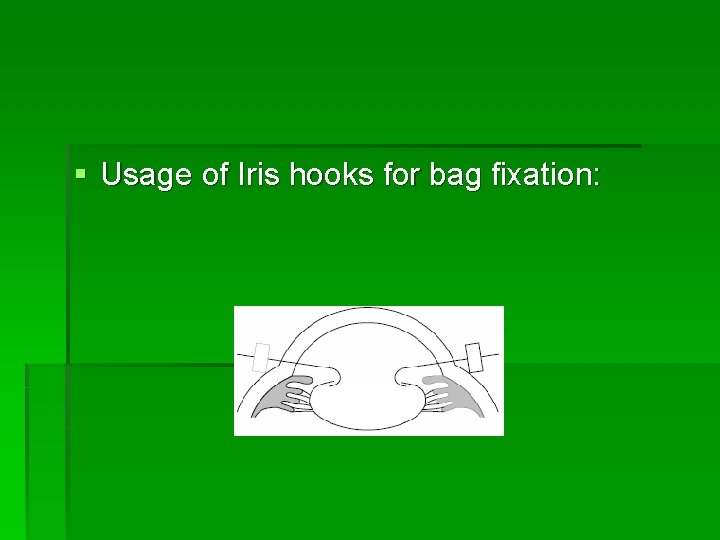
§ Usage of Iris hooks for bag fixation:
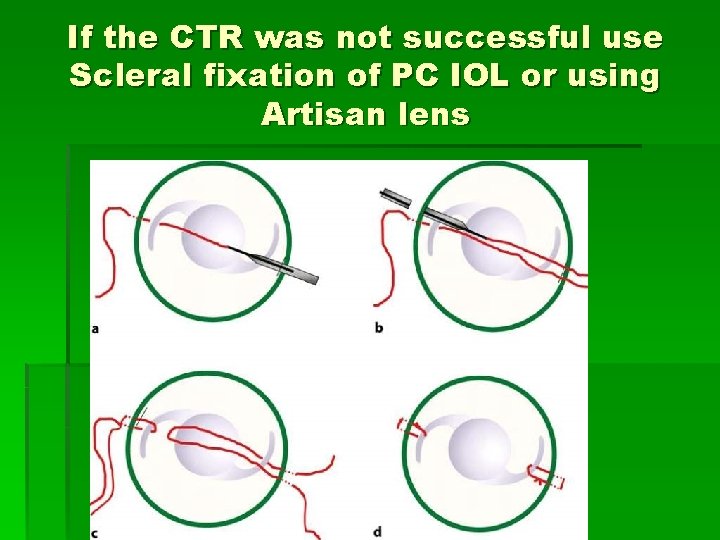
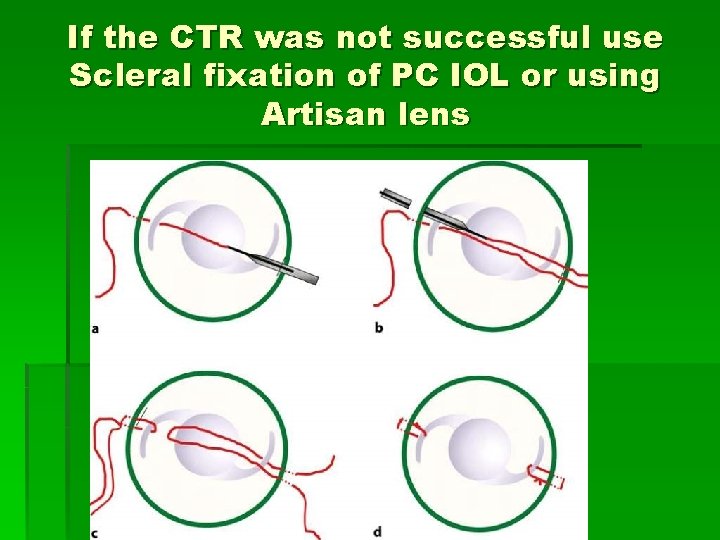
If the CTR was not successful use Scleral fixation of PC IOL or using Artisan lens

MANAGEMENT OF SMALL PUPIL
§ Adequate pupil size is imperative for safe cataract removal.
§ Flomax has led to intraoperative floppy iris syndrome. It will also prolapse into the phaco and side port incisions.

§ Small pupil is generally defined as a pupil less than 4 mm in diameter. § It has been shown that about 1. 6% of cases will fall into this category.
§ The presence of a small pupil is a significant risk factor for the development of complications during cataract surgery.


Starting the surgery § Intracameral 0. 5 cc of unpreserved lidocaine 1% with 1: 100, 000 unpreserved epinephrine. § Injection of viscoelastic. § Inspection of the iris with an instrument to identify synechia.
§ The most common cause of a small surgical pupil is the pseudoexfoliation syndrome.
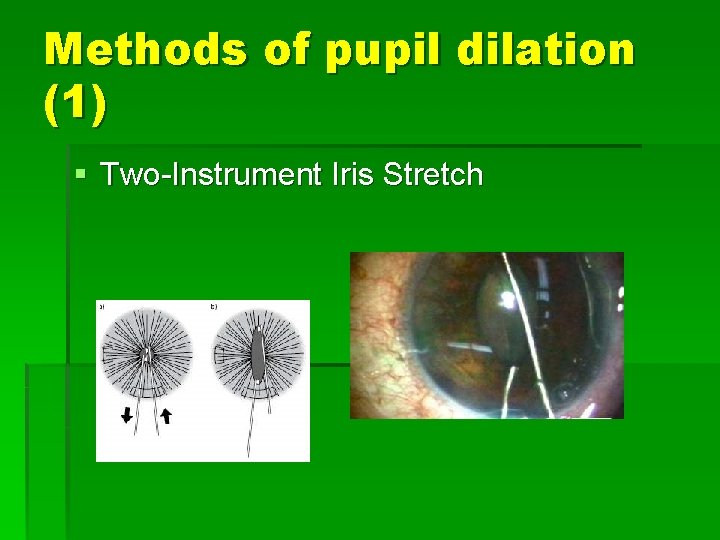
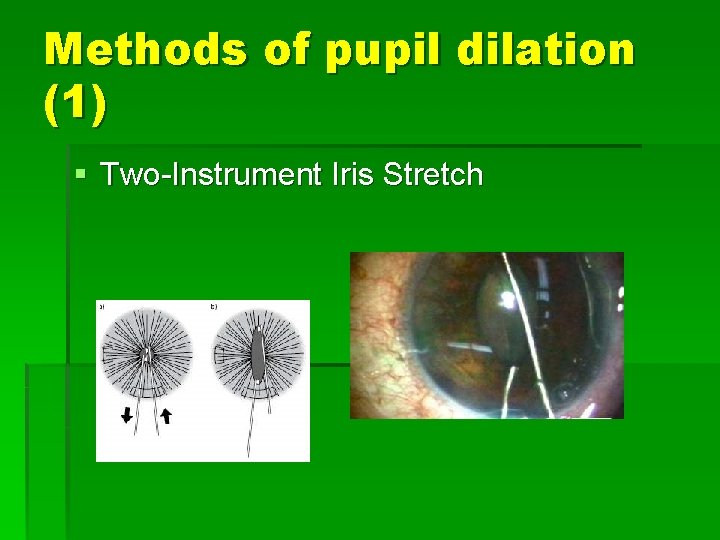
Methods of pupil dilation (1) § Two-Instrument Iris Stretch

Methods of pupil dilation (2) § use of instruments that have been designed to produce a three- or four-point stretch with one hand.
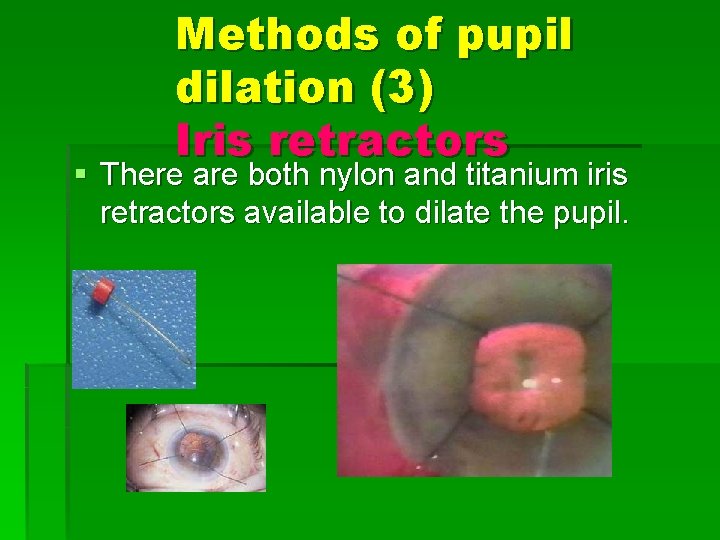
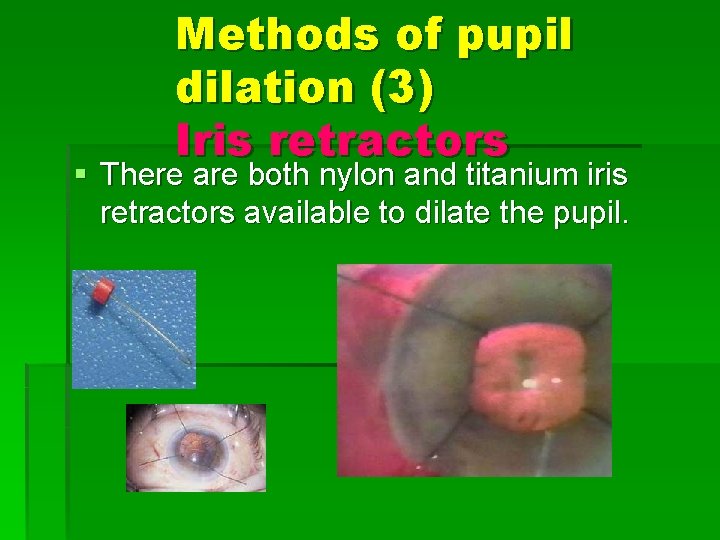
Methods of pupil dilation (3) Iris retractors § There are both nylon and titanium iris retractors available to dilate the pupil.
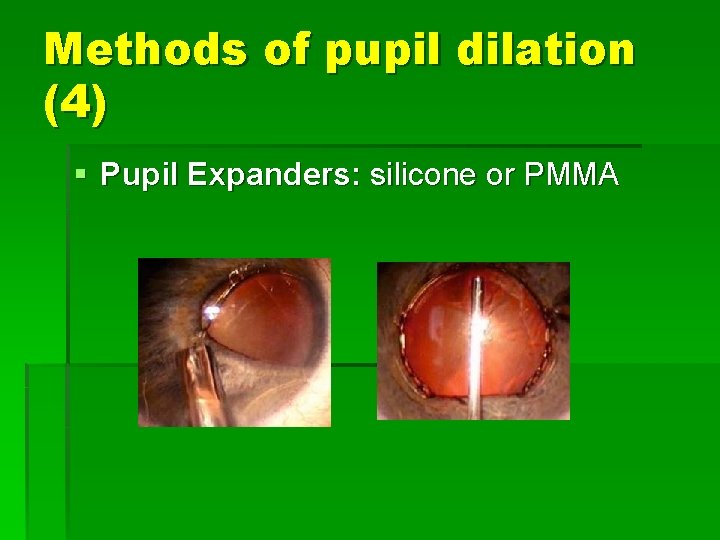
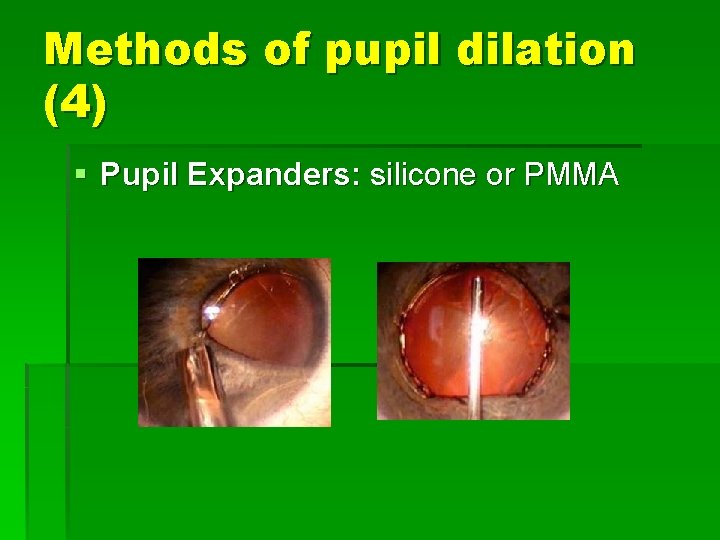
Methods of pupil dilation (4) § Pupil Expanders: silicone or PMMA
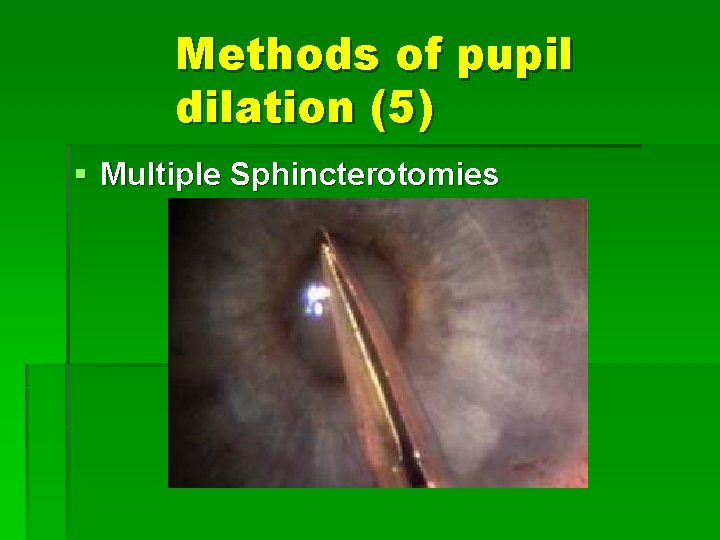
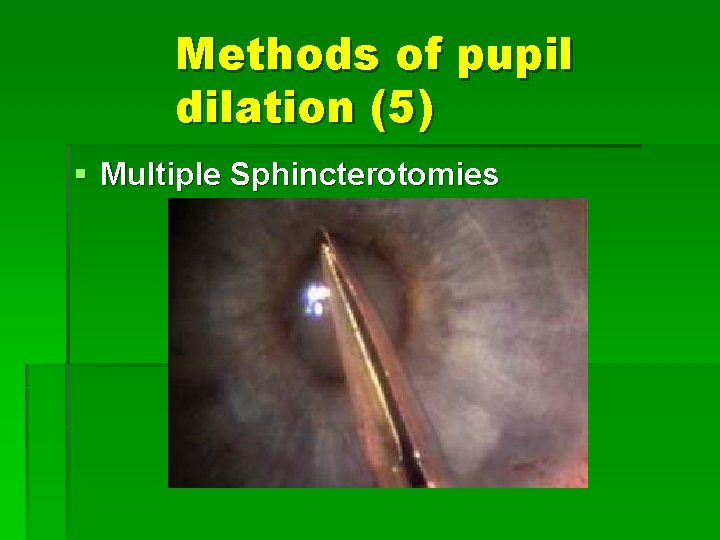
Methods of pupil dilation (5) § Multiple Sphincterotomies

VITREOUS LOSS

Vitreous loss is inevitable
§ Broken capsules occur at a rate between 0. 45% for very experienced surgeons § And up to 14. 7% for residents in training.
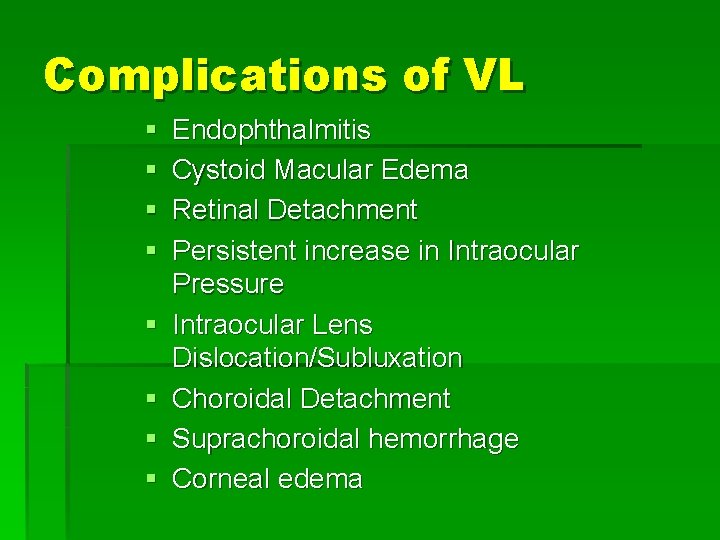
Complications of VL § § § § Endophthalmitis Cystoid Macular Edema Retinal Detachment Persistent increase in Intraocular Pressure Intraocular Lens Dislocation/Subluxation Choroidal Detachment Suprachoroidal hemorrhage Corneal edema

Categories: § Broken capsule with an intact anterior hyaloid. § Vitreous prolapse into AC § Vitreous loss through the incision

SEQUELAE ; RD § RD may occur at the rate of 1% after uncomplicated surgery § Increases up to 8. 6% following VL § RD increases to 14. 5% when lens fragments are retained.
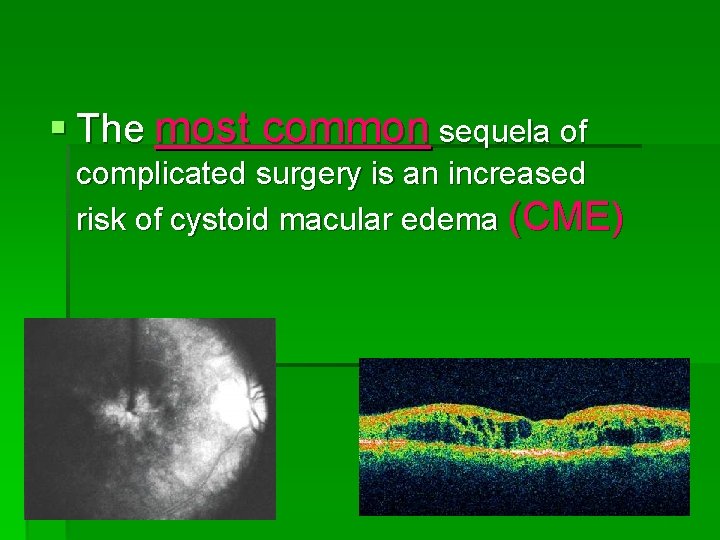
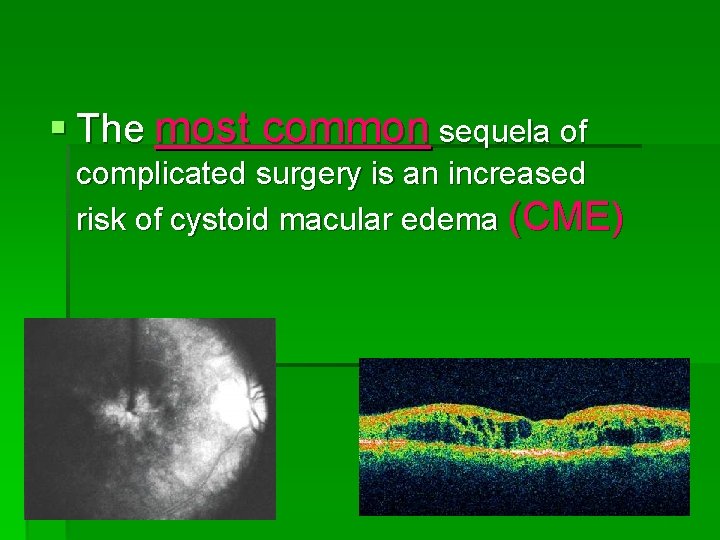
§ The most common sequela of complicated surgery is an increased risk of cystoid macular edema (CME)

EARLY RECOGNITION
Early signs of break in the posterior capsule: § § § A bounce of the iris diaphragm Change in anterior chamber depth Change in pupil size
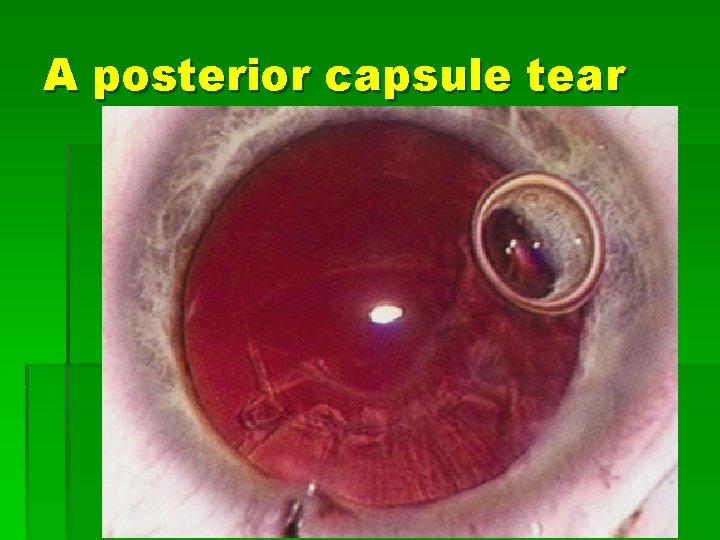
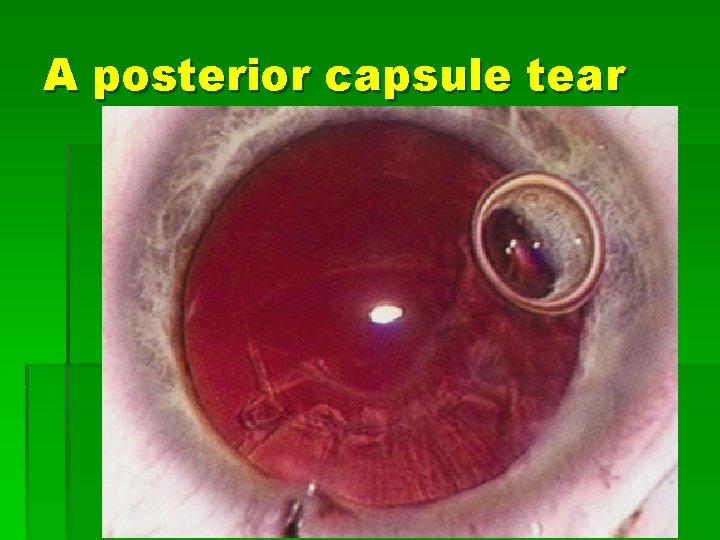
A posterior capsule tear
Loss of followability of lens material Loss of phaco efficiency during surgery are reliable signs that vitreous is present.

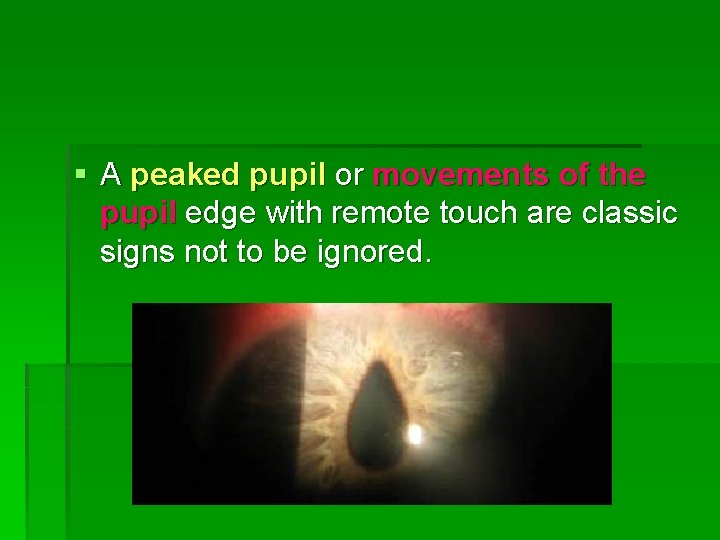
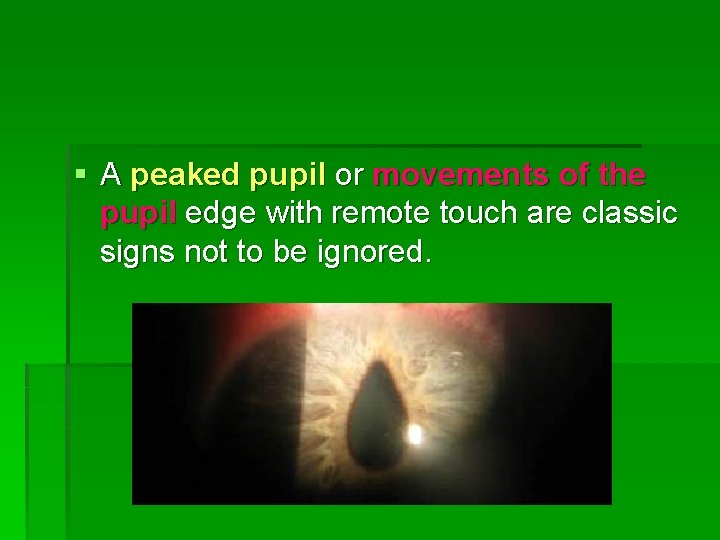
§ A peaked pupil or movements of the pupil edge with remote touch are classic signs not to be ignored.

EARLY RESPONSE
FIRST § Do not pull out of the eye when recognizing a complication. § The phaco tip between the lips of the wound controls the intraocular environment.
§ Upon recognition of a problem go to foot position zero but do not move the phaco tip. § Remove the non-dominant hand instrument from the paracentesis § Prepare to inject OVD (Ophthalmic Viscosurgical Device ) through the paracentesis incision.
§ Only after OVD injection can the phaco tip be withdrawn from the eye. § If not, the chamber will collapse and the stage of complication may progress from capsular rupture to vitreous prolapse or to vitreous loss.
§ Avoid reintroduction of intracameral unpreserved 1% xylocaine with broken zonules or a capsule rupture. § There will be a transient amaurosis, This can be disconcerting or even frightening to both patient and surgeon.
DAMAGE CONTROL
§ compartmentalization with a dispersive OVD. § If the rent in the posterior capsule is central, this must be converted to a circular posterior capsulorhexis

Tear is redirected to a posterior capsulorrhexis

§ Posterior chamber nuclear fragments must be raised above the iris plane into the anterior chamber with OVD.
§ If the lens fragment is below the posterior capsule and has descended into the posterior segment, the fragments should be left in place for later removal with a full three-port pars plana vitrectomy.
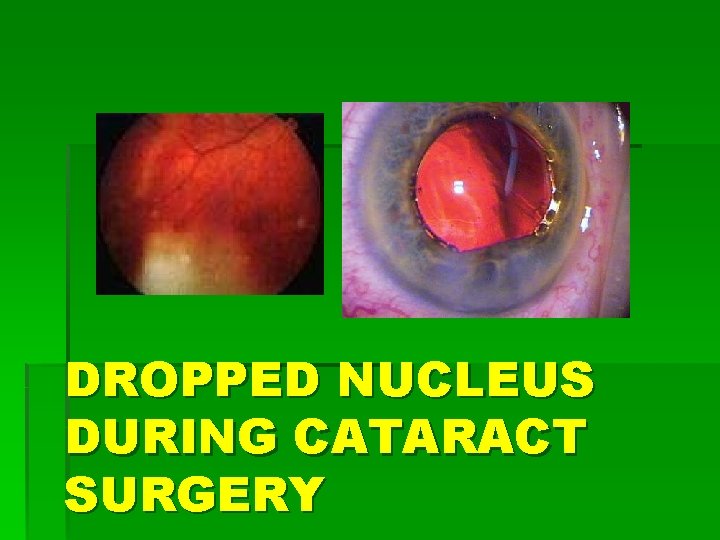
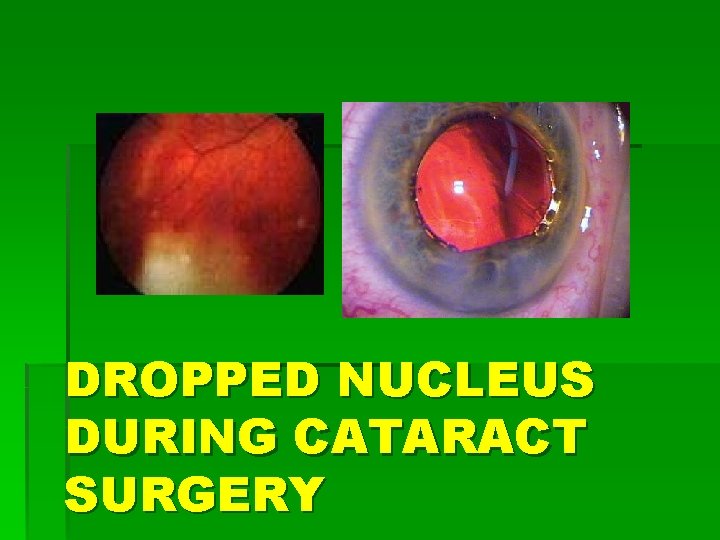
DROPPED NUCLEUS DURING CATARACT SURGERY
§ Lens material cannot damage the retina, unless manipulated by a surgeon. § Posterior assisted levitation to raise a dropped nucleus into the anterior chamber for removal creating unsafe vitreoretinal traction.
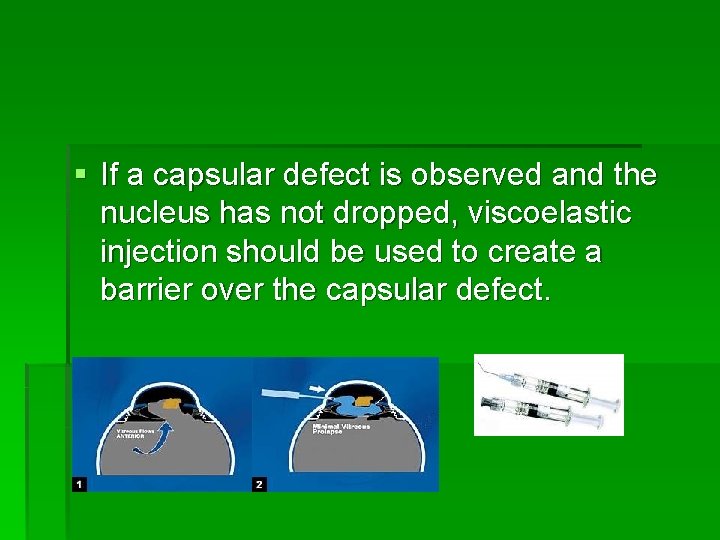
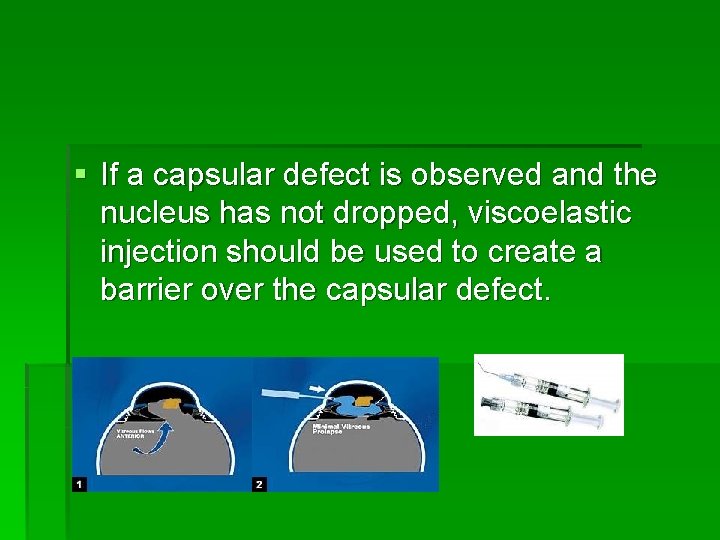
§ If a capsular defect is observed and the nucleus has not dropped, viscoelastic injection should be used to create a barrier over the capsular defect.

If the nucleus drops…. § Focus upon safe management of the vitreous. § Consider lens implantation § Manage the wound § Refer to posterior segment surgeon
§ The timing of the deep vitrectomy is determined on an individual case basis. § Early vitrectomy (fewer than 3 weeks) was associated with better visual results.

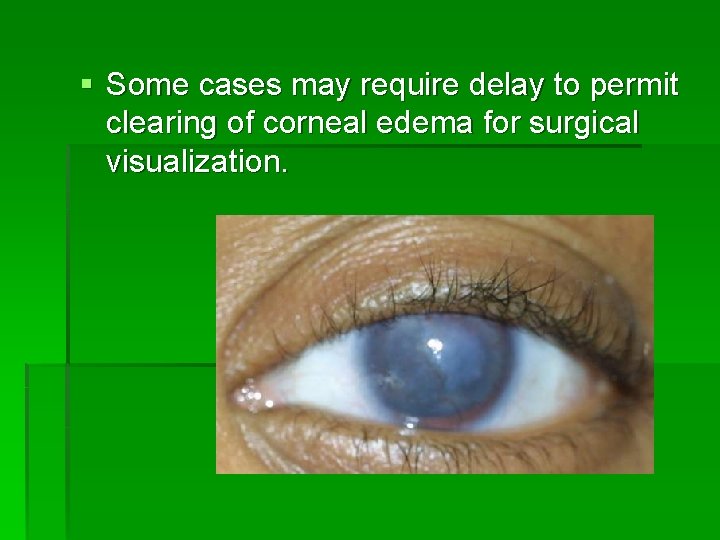
§ Some cases may require delay to permit clearing of corneal edema for surgical visualization.

§ Urgent surgical intervention may be indicated in: Cases with markedly elevated intraocular pressure refractory to medical management.


TO PHACO OR CONVERT TO
Continue Phaco… § It is essential there be no admixture of vitreous and lens material. § vitreous will be attracted to the phaco port displacing nucleus and preventing aspiration of lens material with a high likelihood of retinal tear and detachment.
§ Unless vitreous can be isolated and compartmentalized away from lens fragments, the phaco hand piece should not be used.
In the presence of a controlled capsule tear § Tear must be adequately covered by OVD, or a lens glide to minimize the risk of forcing nuclear fragments posteriorly or displacing vitreous.
Small rent in post capsule Lowering the infusion bottle Full occlusion of the aspiration port Minimal phaco power. Will reduce the risk of further damage to the capsule and aspiration of vitreous.
Capsular rupture If the majority of the nucleus remains and the capsular tear is large further attempts at phaco should be abandoned.
§ A slow motion technique should be employed § with low flow, § moderate vacuum and § appropriate pulses of energy § adequate flow to avoid wound burn to promote follow ability and to minimize chatter.
How convert to ECCE? § Choose the incision based on the size of the remaining fragments. § If the fragment is judged to fit 4 mm, the clear corneal incision can be utilized.
If you need > 4 mm incision § Move superiorly and perform an adequate limbal or scleral tunnel incision appropriate to the fragment size.

Removal of remained lens material. Surgeon should enlarge the incision and remove the nucleus with a lens loop or spoon.
§ Do not express with external pressure § Remove the fragment with a cystotome, forceps or a vectus glide

VITRECTOMY TECHNIQUE
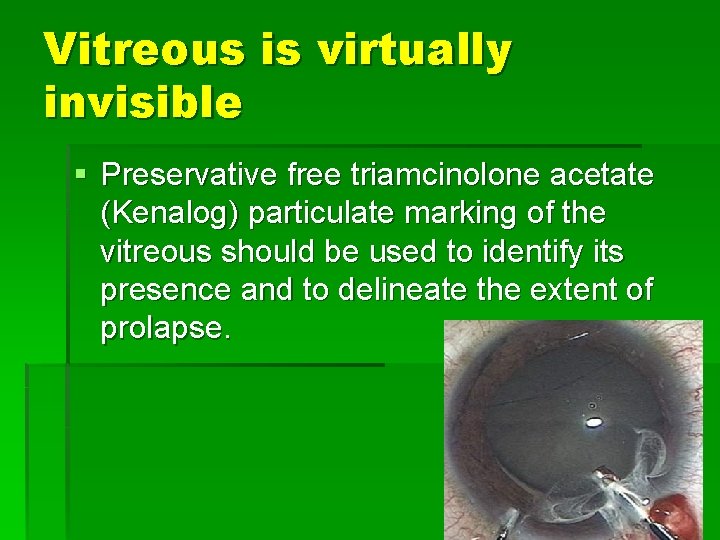
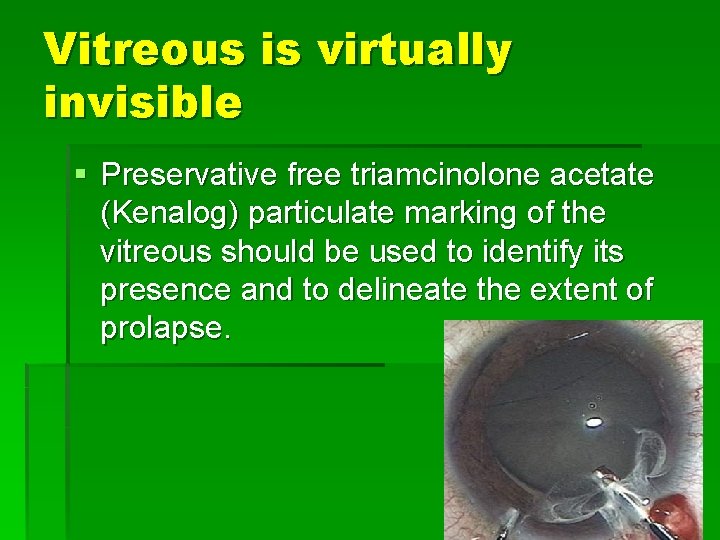
Vitreous is virtually invisible § Preservative free triamcinolone acetate (Kenalog) particulate marking of the vitreous should be used to identify its presence and to delineate the extent of prolapse.
Insertion of a second instrument On lens glide behind the nuclear remnant may help prevent its dislocation in to the vitreous.
§ Remove as much triamcinolone as possible. § Some patients may show a steroid response of ocular hypertension.
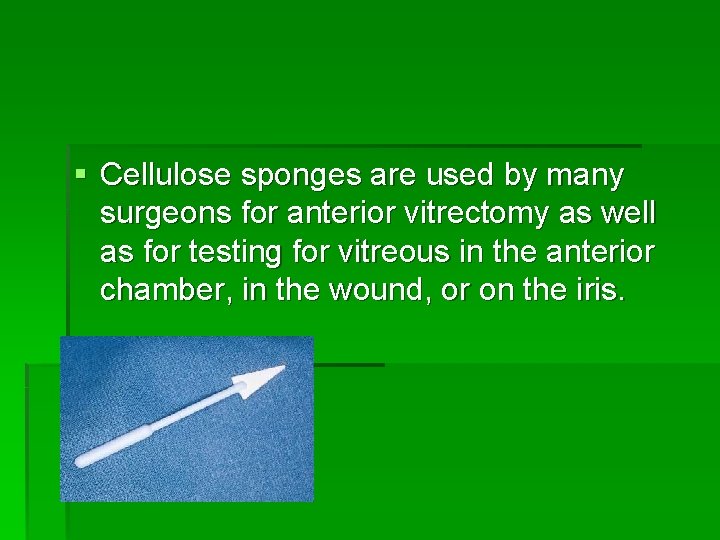
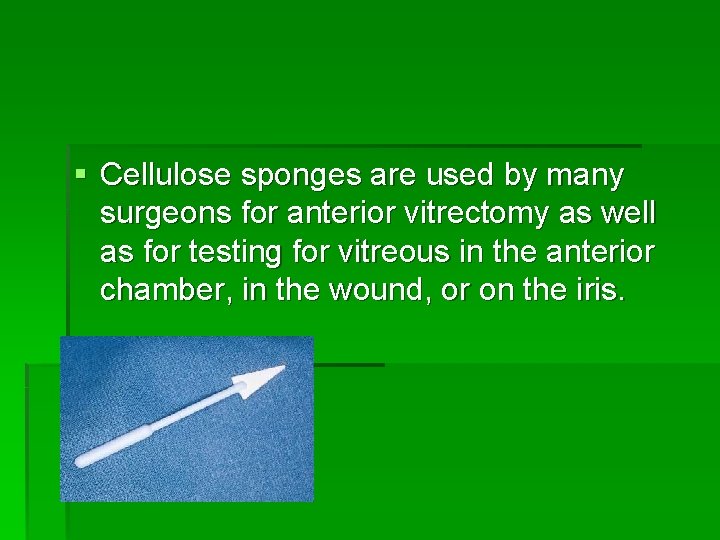
§ Cellulose sponges are used by many surgeons for anterior vitrectomy as well as for testing for vitreous in the anterior chamber, in the wound, or on the iris.
§ It inherently causes marked instantaneous vitreoretinal traction.
§ Traction on the anterior vitreous is particularly dangerous because of § proximity to the vitreoretinal adherence at the vitreous base § peripheral retina is more fragile
§ The vitreous cutter should be used to amputate any posterior connection to wound-entrapped vitreous. § In some instances OVD can be used to reposit vitreous.
Vitrectomy Perform anterior vitrectomy to avoid vitreous prolapse.
Cut rate: § Fast cutting rate reduces vitreoretinal traction. § Fast cut increase fluidic stability
Suction: § Low suction levels and low flow rates are safer. § The suction or flow rate should be slowly increased until vitreous starts being removed.

INSPECTION AND IOL CHOICE
Viscoelastic Can be introduced posteriorly to the fragment in an effort to float it anteriorly and removing.
§ § Be sure the pupil is round. Be certain incisions are sealable. Evaluate the intactness of the CCC Evaluate the extent of the posterior capsule tear and residual sulcus support.
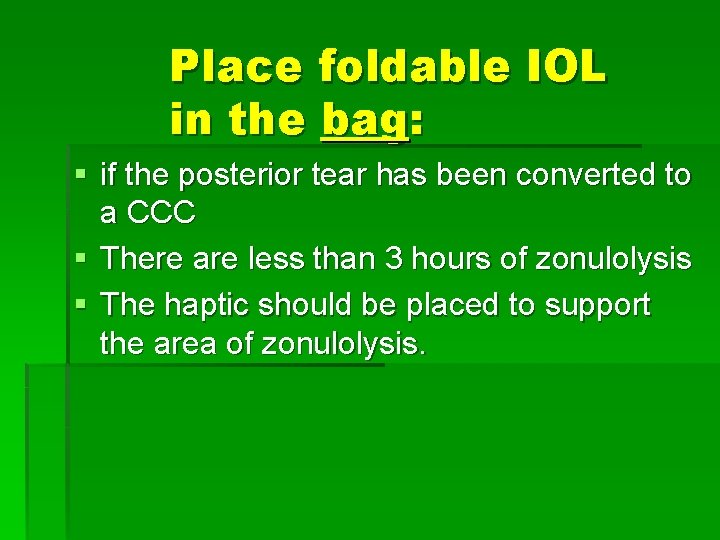
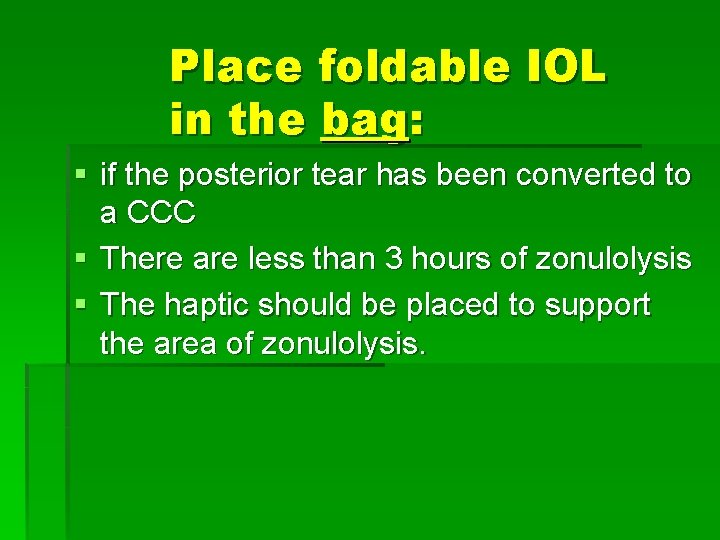
Place foldable IOL in the bag: § if the posterior tear has been converted to a CCC § There are less than 3 hours of zonulolysis § The haptic should be placed to support the area of zonulolysis.
Iol implantation Bag if safe , ciliary sulcus or Artisan lens.

§ If the anterior CCC is intact the foldable lens should have sulcus haptic placement
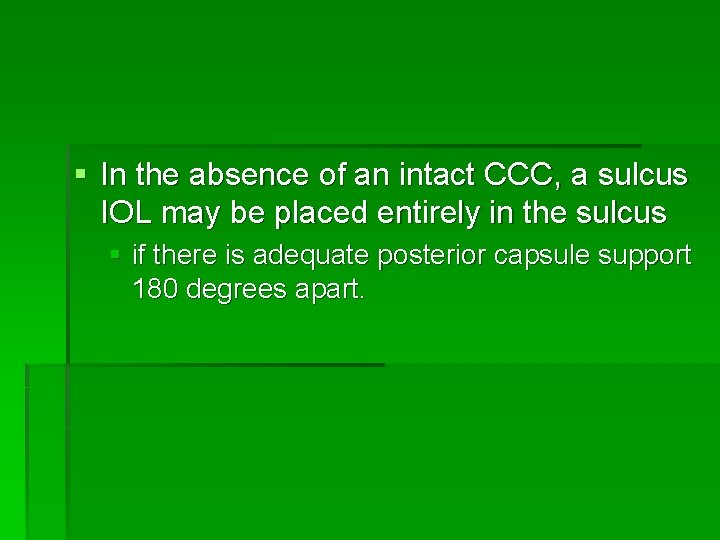
§ In the absence of an intact CCC, a sulcus IOL may be placed entirely in the sulcus § if there is adequate posterior capsule support 180 degrees apart.
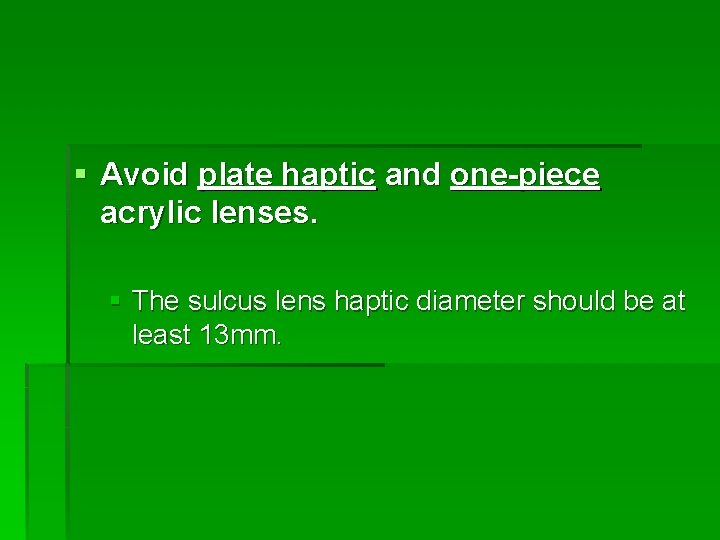
§ Avoid plate haptic and one-piece acrylic lenses. § The sulcus lens haptic diameter should be at least 13 mm.
In the absence of capsular support: § Posterior chamber lens with scleral fixation § Artisan lens § An anterior chamber open loop lens?

POSTOPERATIVE CARE
Post op care. Frequent postop topical steroid , NSAIDS and IOP lowering agents can be used.
Intraocular pressure elevation: § High IOP within the first 24 hours is often due to retained OVD § High pressure secondary to retained lens fragments takes several days

§ the surgeon should anticipate increased post-op inflammation § Require intensive topical steroids § Intracameral antibiotic injection § Non-steroidal anti-inflammatory medications. § Peribulbar steroids
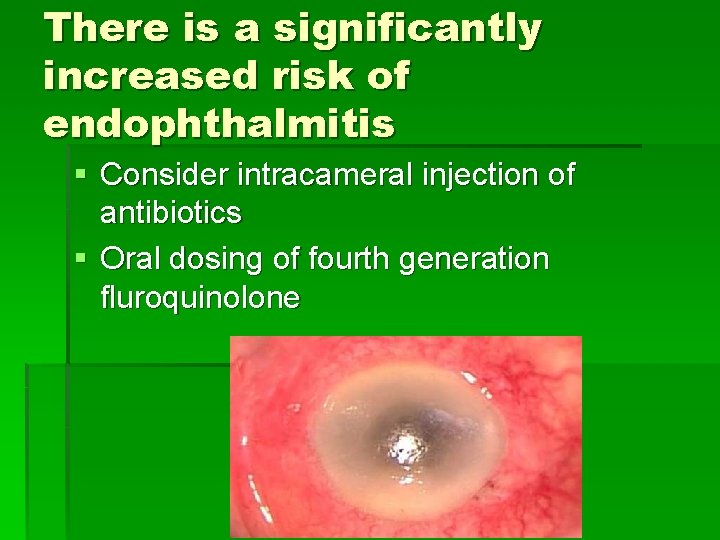
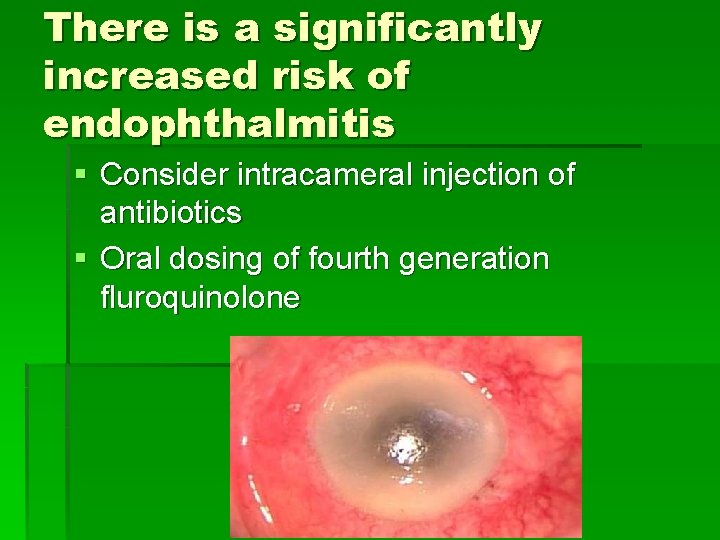
There is a significantly increased risk of endophthalmitis § Consider intracameral injection of antibiotics § Oral dosing of fourth generation fluroquinolone
Conclusion: § Effectively dealing with crisis is a matter of having prepared for it.

Thank You
 Pre and post operative nursing care of cataract
Pre and post operative nursing care of cataract Blended vision
Blended vision Modified monovision
Modified monovision Knapps rule
Knapps rule Intraoperative cholangiogram
Intraoperative cholangiogram Phases of preoperative care
Phases of preoperative care Choledocholithiasis
Choledocholithiasis Perioperative care definition
Perioperative care definition Role of nurse in intraoperative care ppt
Role of nurse in intraoperative care ppt Thyroid
Thyroid Eswl complications
Eswl complications Complications c section
Complications c section Sleeve gastrectomy complications
Sleeve gastrectomy complications Complications of shigellosis
Complications of shigellosis Tracheostomy tube double lumen
Tracheostomy tube double lumen Non atopic asthma
Non atopic asthma Who stroke definition
Who stroke definition Light criteria
Light criteria Eclampsia definicion
Eclampsia definicion Post dated pregnancy complications
Post dated pregnancy complications Post dated pregnancy complications
Post dated pregnancy complications Stitches after birth pictures
Stitches after birth pictures Blood transfusion complications
Blood transfusion complications Bronchoscopy complications
Bronchoscopy complications Neph tubes
Neph tubes Varicella zoster complications
Varicella zoster complications Bronchoscopy complications
Bronchoscopy complications Jim simm
Jim simm Deviated septum
Deviated septum Dialysis in greek
Dialysis in greek Phlegmasia alba dolens definition
Phlegmasia alba dolens definition Portal hypertension
Portal hypertension Abdominal insufflation complications
Abdominal insufflation complications Iliac stent complications
Iliac stent complications Heart failure complications
Heart failure complications Complications of blood transfusion
Complications of blood transfusion Salem sump tube
Salem sump tube Complications of gestational diabetes
Complications of gestational diabetes Complications of c section
Complications of c section Most common complication of central venous catheter
Most common complication of central venous catheter Lower segment caesarean section ppt
Lower segment caesarean section ppt Complications after cesarean section
Complications after cesarean section Complications of blood transfusion
Complications of blood transfusion Complication of blood transfusion
Complication of blood transfusion Complications of blood transfusion
Complications of blood transfusion Hyperlipidemia complications
Hyperlipidemia complications Elemental iron dose
Elemental iron dose Blood transfusion complications
Blood transfusion complications Asthma complications
Asthma complications What is short story definition
What is short story definition Dopamine rash sle
Dopamine rash sle Septic arthritis complications
Septic arthritis complications Glomerulonephritis complications
Glomerulonephritis complications Complications of hydrocephalus
Complications of hydrocephalus Brain hemorrhage
Brain hemorrhage Complications of hydrocephalus
Complications of hydrocephalus Stroke precautions nursing
Stroke precautions nursing Massive transfusion complication
Massive transfusion complication Complications of bacterial meningitis
Complications of bacterial meningitis Septic arthritis complications
Septic arthritis complications Veptr complications
Veptr complications Local complications
Local complications Elements of a setting
Elements of a setting Phlebitis extravasation infiltration
Phlebitis extravasation infiltration Principles of cast application
Principles of cast application Colostomy procedure
Colostomy procedure Gastrostomie complications
Gastrostomie complications Fiksasi internal
Fiksasi internal Incyte
Incyte Hypothyroidism pregnancy
Hypothyroidism pregnancy Indications for blood transfusion
Indications for blood transfusion Otitis media complications
Otitis media complications Chess score syncope
Chess score syncope Complications of respiratory failure
Complications of respiratory failure Complication of gestational diabetes
Complication of gestational diabetes Succussion splash
Succussion splash Adhesive arachnoiditis
Adhesive arachnoiditis Hypothyroidism
Hypothyroidism Dr paul healey
Dr paul healey Nagma vs hagma
Nagma vs hagma Lumbar puncture complications
Lumbar puncture complications Lecture title
Lecture title Perkins timetable fracture healing
Perkins timetable fracture healing Iv site complications
Iv site complications Complications of insulin resistance
Complications of insulin resistance Prefibrotic myelofibrosis
Prefibrotic myelofibrosis Glutaryldehyde,
Glutaryldehyde, Molecular cell biology of diabetic complications
Molecular cell biology of diabetic complications Polychromatic lustre
Polychromatic lustre Glaukomflecken cataract
Glaukomflecken cataract Galctosemia
Galctosemia And now with gleams of half-extinguished thought
And now with gleams of half-extinguished thought Presenile cataract
Presenile cataract Blue dot catract
Blue dot catract Senile incipient cataract
Senile incipient cataract Senile incipient cataract
Senile incipient cataract