Early Indicators of Schizophrenia Dr Jim Simm FRCPC





- Slides: 45

Early Indicators of Schizophrenia • Dr Jim Simm*, FRCPC; CCSAM • Dr Richard Tachere*, MD; MPH *Dept. of Psychiatry, University of Manitoba. CAPA Annual Conference October 30 th, 2016
Disclosure • Dr. Simm has received honorarium payments for speaking on behalf of Janssen pharmaceuticals on the treatment of schizophrenia. • Dr. Tachere has no conflict of interest to declare.
Stay Awake. . . WHY ? ? ?
Introduction: • Schizophrenia can be a terrible mental illness: Ø robs young people of their potentials; Ø tears families apart; Ø has an enormous burden on our society (financial, legal, social, etc. )
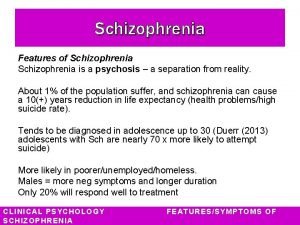
Facts: • Among the top 25 leading causes of disability globally • ~ 3% of the total burden of human disease • ~ 1% point prevalence • > 60% of patients with the first episode of the illness have persistence of symptoms & impairment in various domains of functioning.
Facts: • In Canada: - hospital bed occupancy: 1 in 12 (higher than any other single disease) - direct health & non-health care costs ~ $2 billion/yr. - indirect costs ~ $1. 4 billion/yr.
Facts: • Peak age of onset for first psychotic episode: - Males: early to mid-20 s; - Females: the late-20 s. • Early recognition and uninterrupted treatment can lead to optimal outcomes.
Outline: • Meaning of psychosis and schizophrenia; • Approaches to Assessment, Diagnosis & Treatment; • The importance of early continuous treatment; • Conclusion.
Overview • Schizophrenia is a major mental illness - the most well-known of the ‘psychotic’ disorders. • Most common age of onset is 15 -25 yrs • It affects ~ 1% of the population Ø But what exactly is “psychosis”?
Psychosis… • The term “psychosis” refers to an impairment in reality testing. • Symptoms: hallucinations, delusions, disorganized speech, behavior, etc.
The contemporary concept of psychosis (DSM 5): Abnormalities in one or more of 5 domains: • delusions, • hallucinations, • disorganized thinking (speech), • grossly disorganized or abnormal motor behavior (including catatonia), and • negative symptoms
Signs and Symptoms of Psychosis • Delusions • Hallucinations • Replaying or rehearsing conversations out loud- i. e. talking to yourself (very common sign) • Inappropriate responses - laughing or smiling when talking of a sad event, making irrational statements.
Signs and Symptoms of Psychosis • Catatonia - staying in the same rigid position for a long time, as if in a daze. • Intense & excessive preoccupation with religion or spirituality • Hypergraphia, bizarre writing with paranoid themes, conspiracy theories, etc • Frequent moves, trips, or walks that lead nowhere
Delusions • Usually paranoid: others are plotting to harm you, are monitoring you, can read your thoughts, etc. • Often accompanied by ideas of reference: events or occurrences have a special meaning to you. • Grandiose delusions, often religious in nature (more common in mania) • Somatic - infestation, bizarre somatic complaints (e. g. in psychotic depression) • Jealousy – Often delusional disorder.
Hallucinations • Auditory: most common; generally commenting on behavior, insulting comments or command hallucinations. • Often source is attributed to “talking through the wall”, radio waves; almost always human voices • These can be either inside the person's head or externally. • When external, they sound as real as an actual voice. Sometimes they come from no apparent source; at other times they come from real people who don't actually say anything.
Hallucinations… • Visual: 2 nd most common; usually misinterpretation of real objects (i. e. illusions) • Olfactory/gustatory: less common but usually of foul odour or food is spoiled or tainted. (Consider psychotic depression if this is a prominent feature). • Tactile hallucinations: rare; often of being sexually violated.
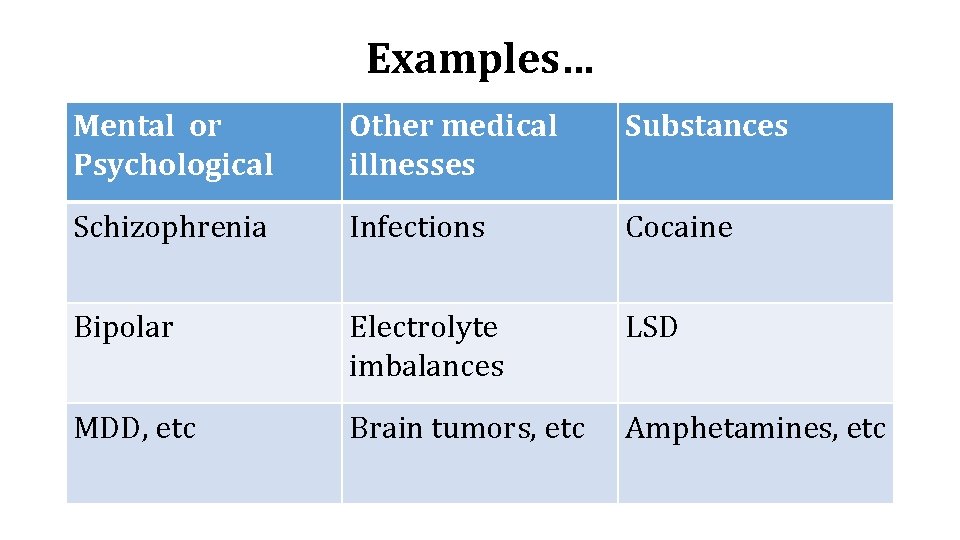
Differential Diagnosis: 3 broad groups • Psychoses: (a) due to a mental or psychological disorder (b) due to a general medical condition (c) due to a substance (medication or drug of abuse)
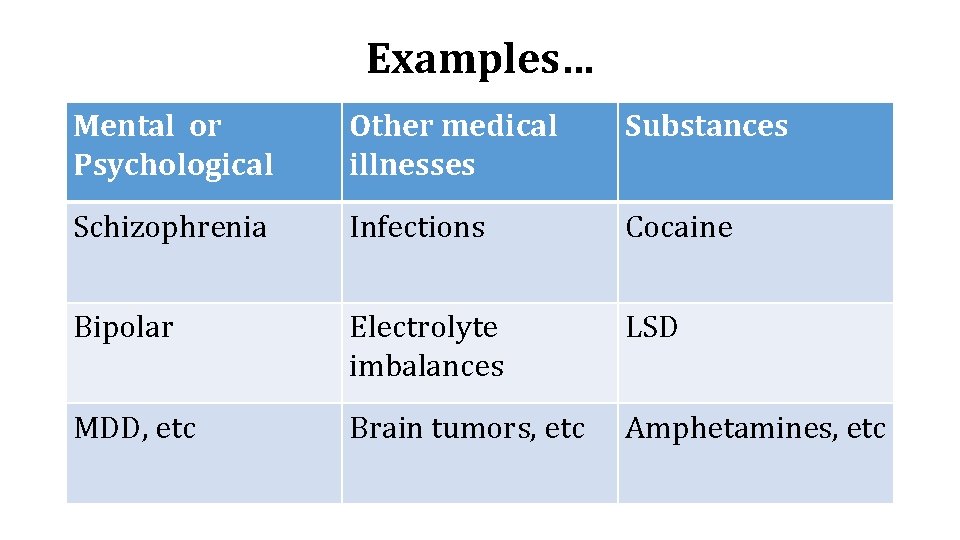
Examples… Mental or Psychological Other medical illnesses Substances Schizophrenia Infections Cocaine Bipolar Electrolyte imbalances LSD MDD, etc Brain tumors, etc Amphetamines, etc
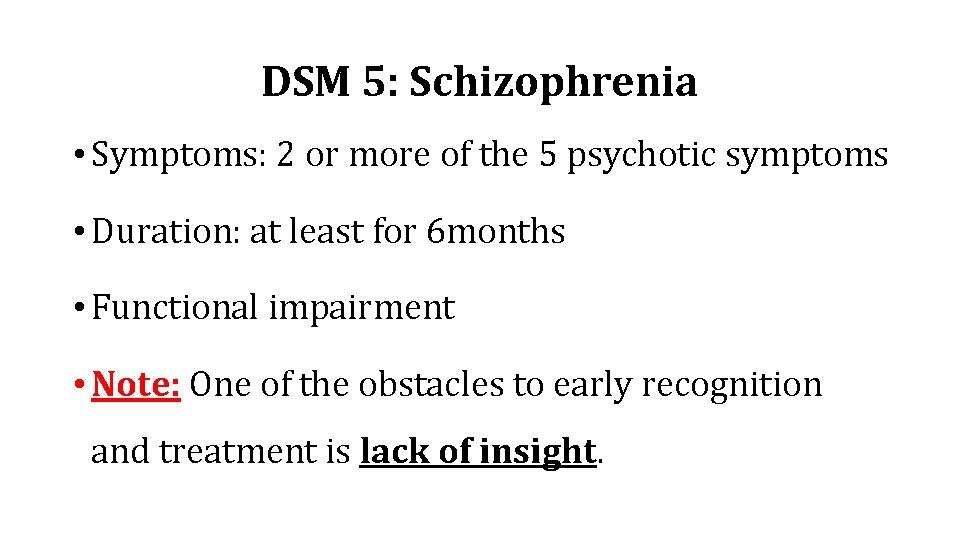
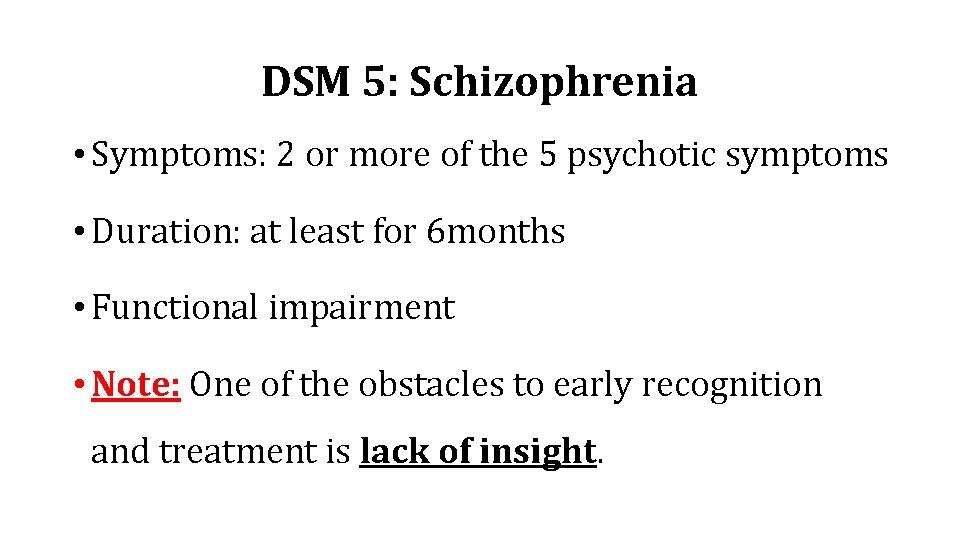
DSM 5: Schizophrenia • Symptoms: 2 or more of the 5 psychotic symptoms • Duration: at least for 6 months • Functional impairment • Note: One of the obstacles to early recognition and treatment is lack of insight.
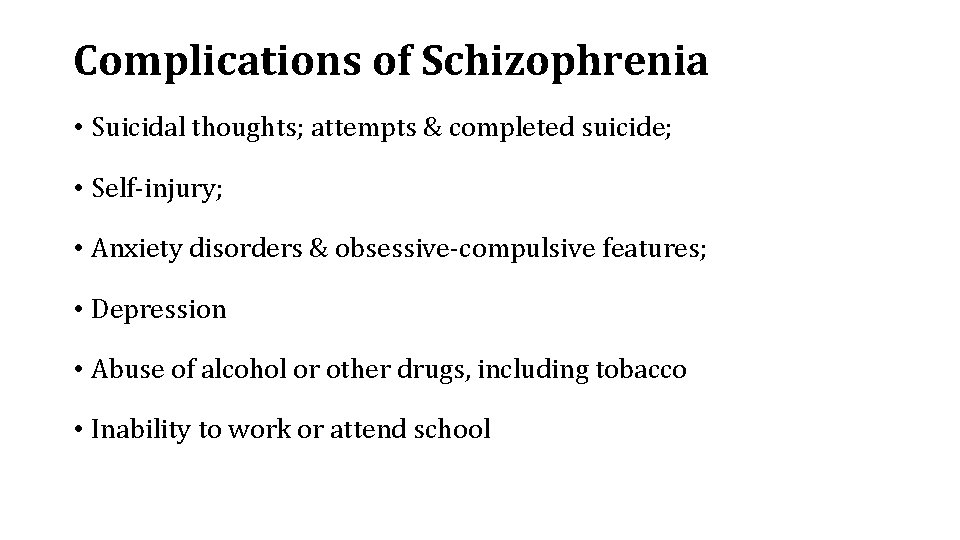
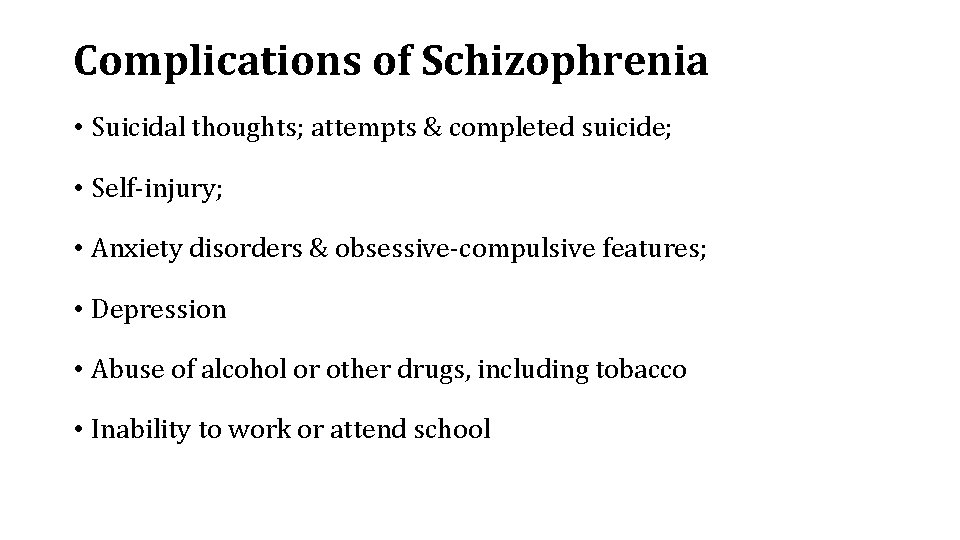
Complications of Schizophrenia • Suicidal thoughts; attempts & completed suicide; • Self-injury; • Anxiety disorders & obsessive-compulsive features; • Depression • Abuse of alcohol or other drugs, including tobacco • Inability to work or attend school
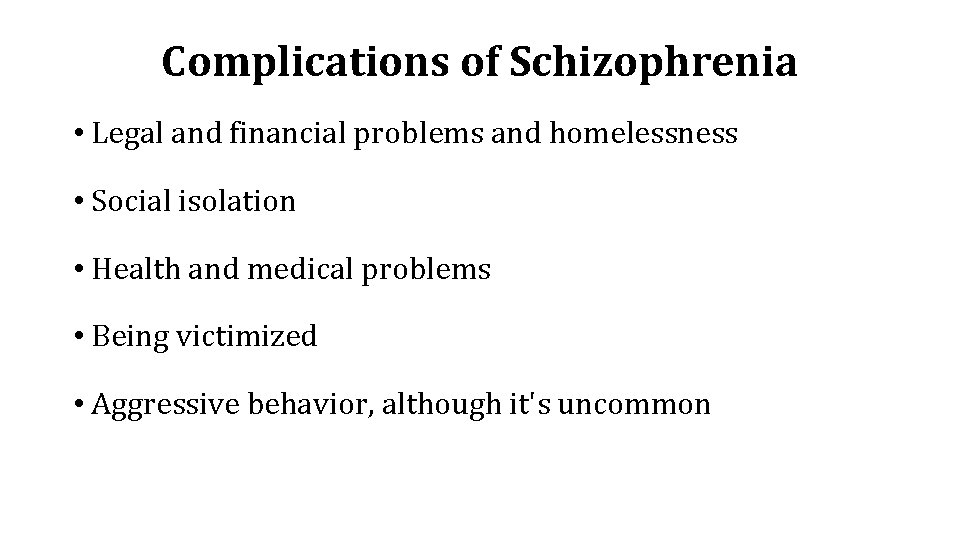
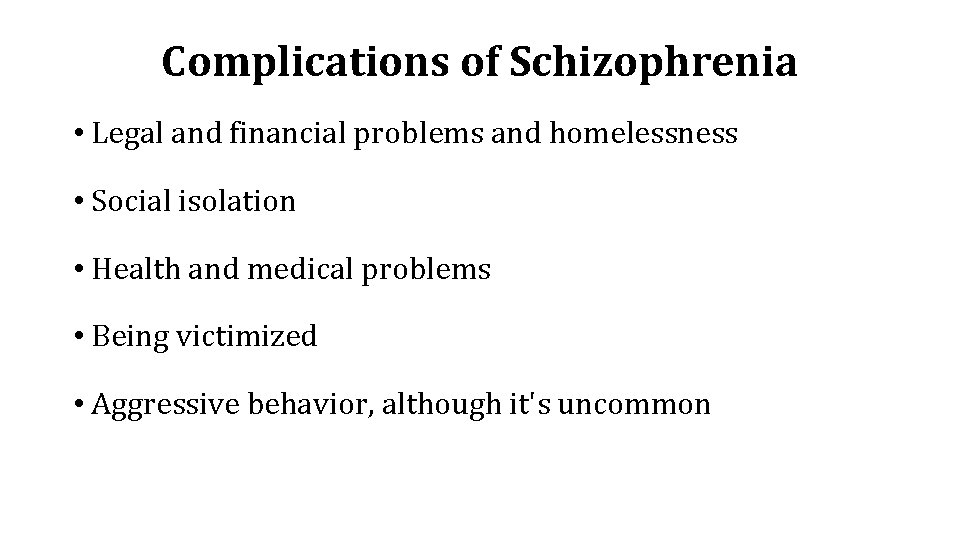
Complications of Schizophrenia • Legal and financial problems and homelessness • Social isolation • Health and medical problems • Being victimized • Aggressive behavior, although it's uncommon

So now that I’ve established that the most likely diagnosis is schizophrenia, What should I do?
Assessment • Goals of initial evaluation include: Ødevelopment of a therapeutic alliance; Øobtaining information required for diagnosis; Øidentifying factors that can assist or impede recovery
Assessment • Should include risk of: Ø suicide & deliberate self-harm Ø violence Ø neglect Ø victimization
Assessment • Should include supports available: Ø Engagement with families Ø Other relevant social networks Ø Community mental health resources available Ø Non-adherence to treatment & service disengagement.
Assessment • Goals of full medical work-up include: ØDetection of medical etiologies and/or comorbidities; ØIdentification of risk factors for possible medical disorders; ØProviding a baseline against which pharmacological complications & side-effects can be assessed.
Assessment • History is key especially family history; • Physical exam; • Investigations: ØComprehensive drug screen ØImaging: specific findings are quite rare without a neurological finding on exam; but family or patient will often insist and be unwilling to accept diagnosis until done. ØWeight, glucose, lipid profile as baseline.
Some non-specific physical findings on exam • A blank, vacant facial expression; e. g. staring while in deep thought, with infrequent blinking, etc. • Clumsy, inexact motor skills • Abnormal eye movements, e. g. difficulty focusing on slow moving objects • Unusual gestures or postures • Constant pacing • Movement could be slowed down - staying in bed (in extreme cases, catatonia)
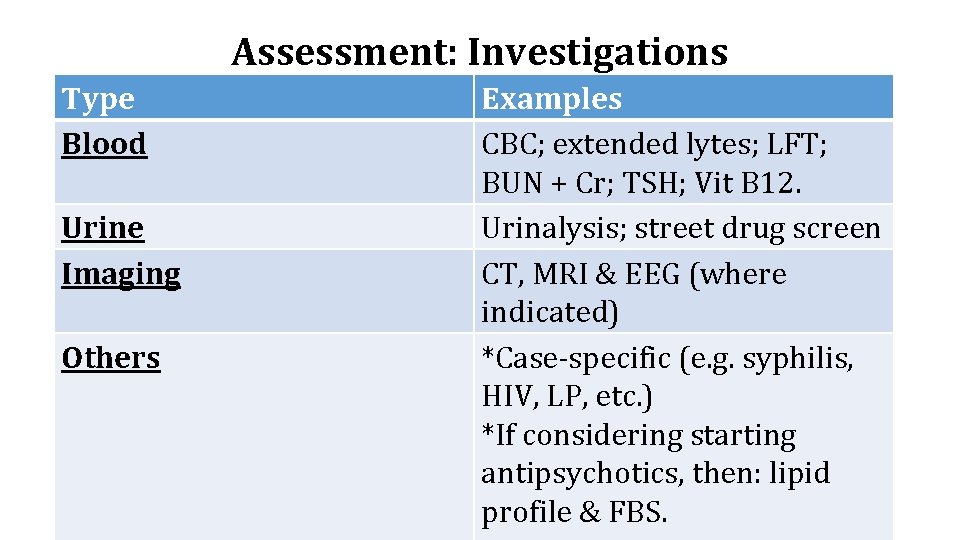
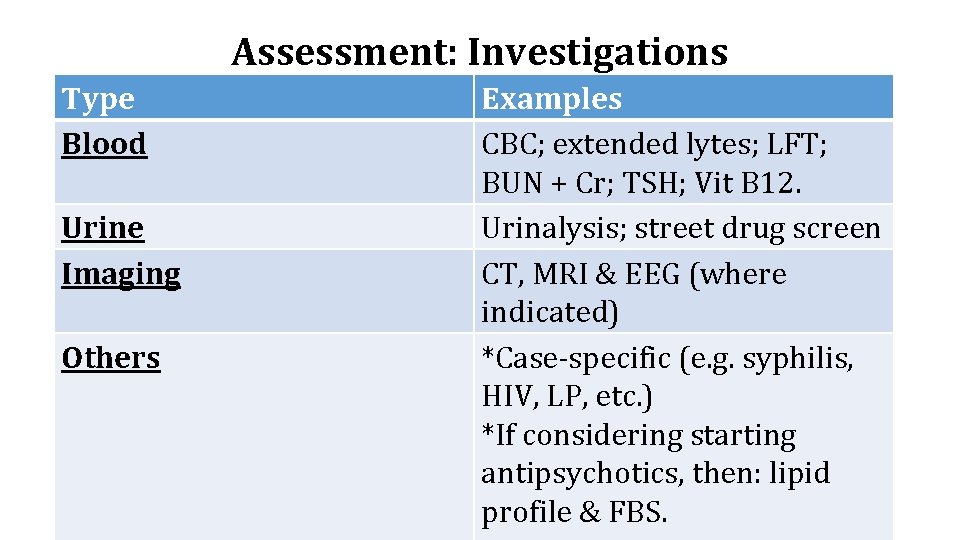
Assessment: Investigations Type Blood Urine Imaging Others Examples CBC; extended lytes; LFT; BUN + Cr; TSH; Vit B 12. Urinalysis; street drug screen CT, MRI & EEG (where indicated) *Case-specific (e. g. syphilis, HIV, LP, etc. ) *If considering starting antipsychotics, then: lipid profile & FBS.
Non-specific early symptoms • Withdrawal from friends and family • A drop in performance at school • Trouble sleeping • Irritability or depressed mood • Lack of motivation
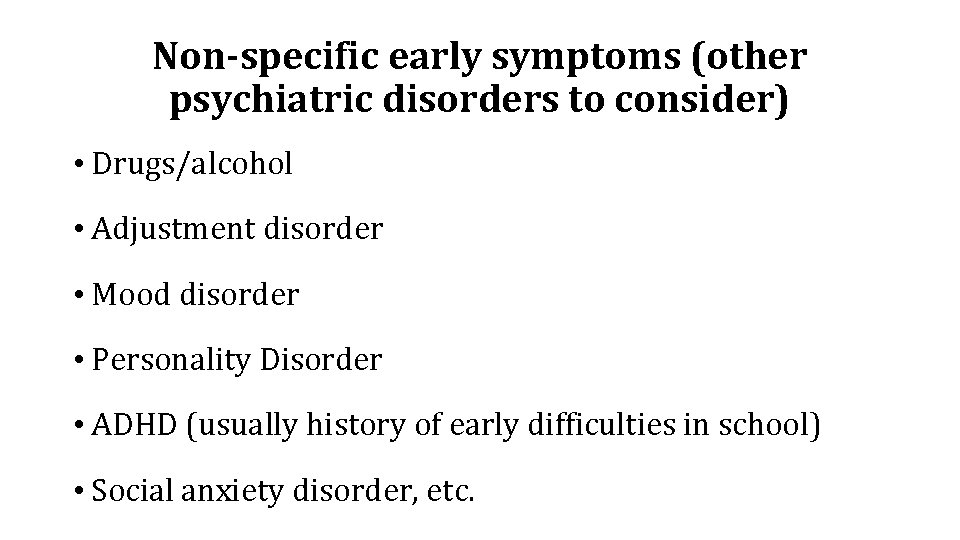
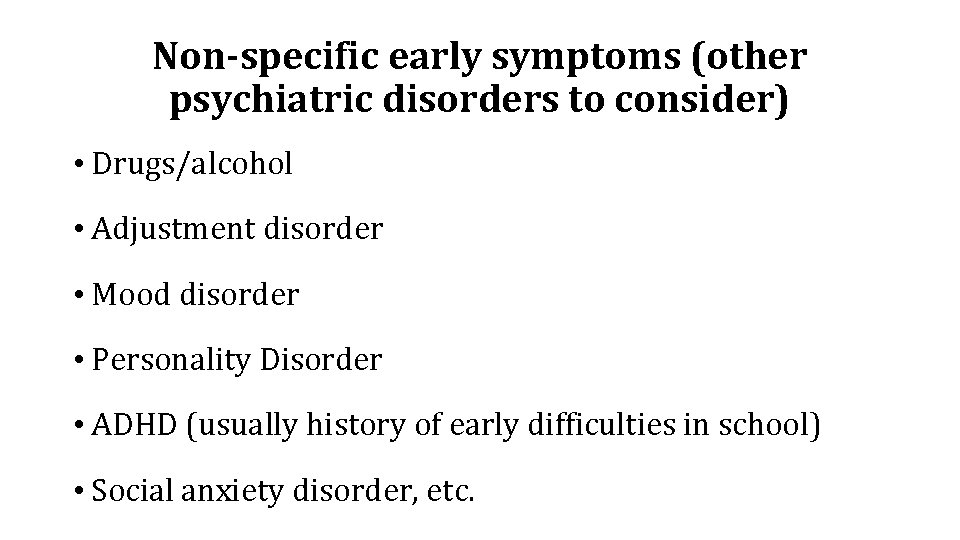
Non-specific early symptoms (other psychiatric disorders to consider) • Drugs/alcohol • Adjustment disorder • Mood disorder • Personality Disorder • ADHD (usually history of early difficulties in school) • Social anxiety disorder, etc.

• Early recognition and uninterrupted treatment can lead to optimal outcomes.
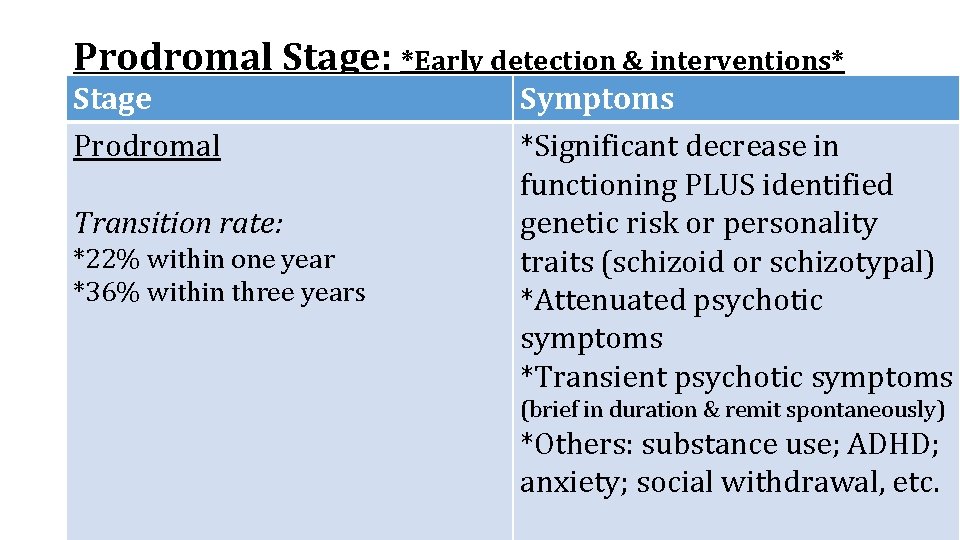
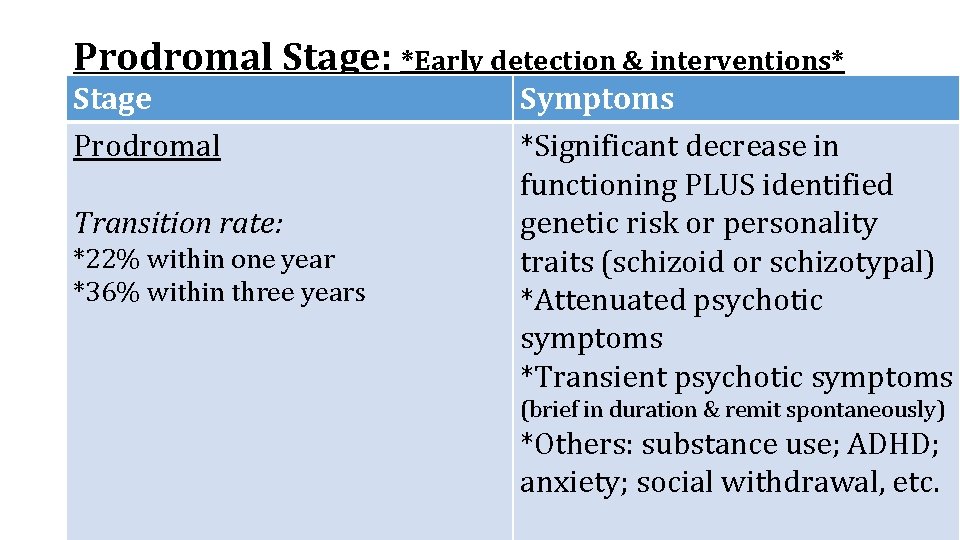
Prodromal Stage: *Early detection & interventions* Stage Prodromal Transition rate: *22% within one year *36% within three years Symptoms *Significant decrease in functioning PLUS identified genetic risk or personality traits (schizoid or schizotypal) *Attenuated psychotic symptoms *Transient psychotic symptoms (brief in duration & remit spontaneously) *Others: substance use; ADHD; anxiety; social withdrawal, etc.
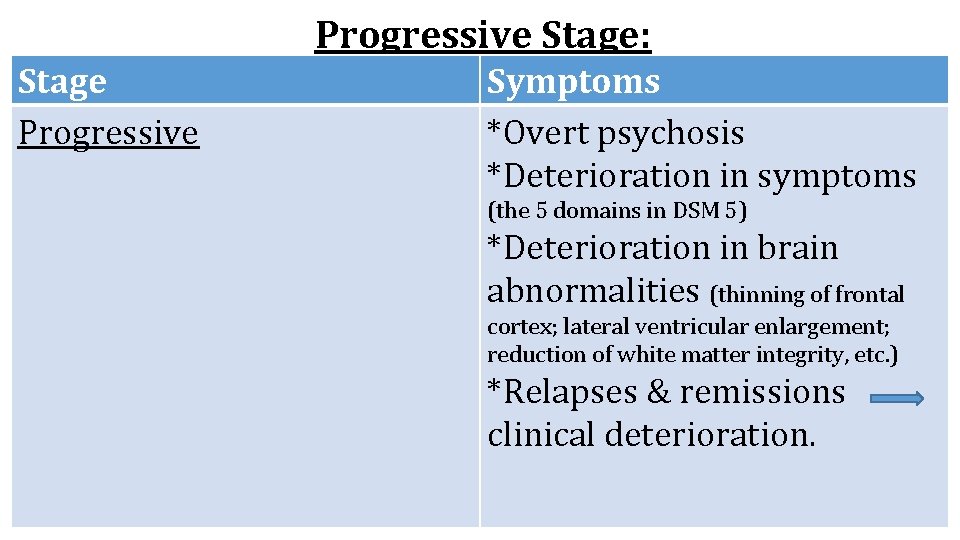
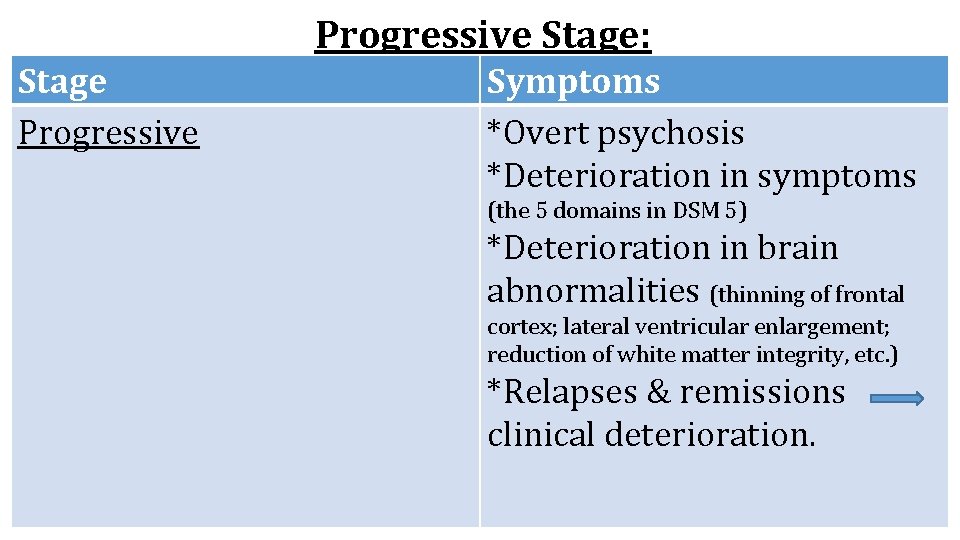
Progressive Stage: Stage Progressive Symptoms *Overt psychosis *Deterioration in symptoms (the 5 domains in DSM 5) *Deterioration in brain abnormalities (thinning of frontal cortex; lateral ventricular enlargement; reduction of white matter integrity, etc. ) *Relapses & remissions clinical deterioration.
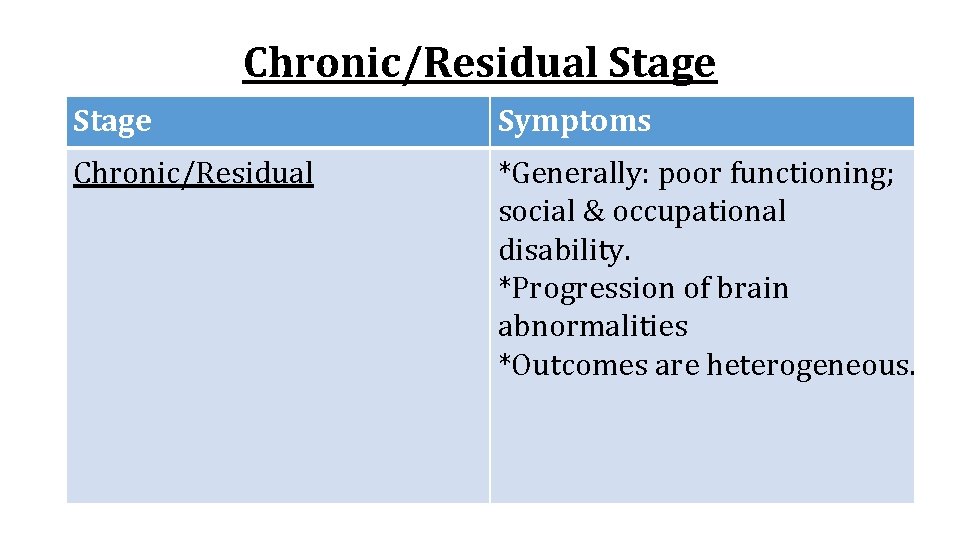
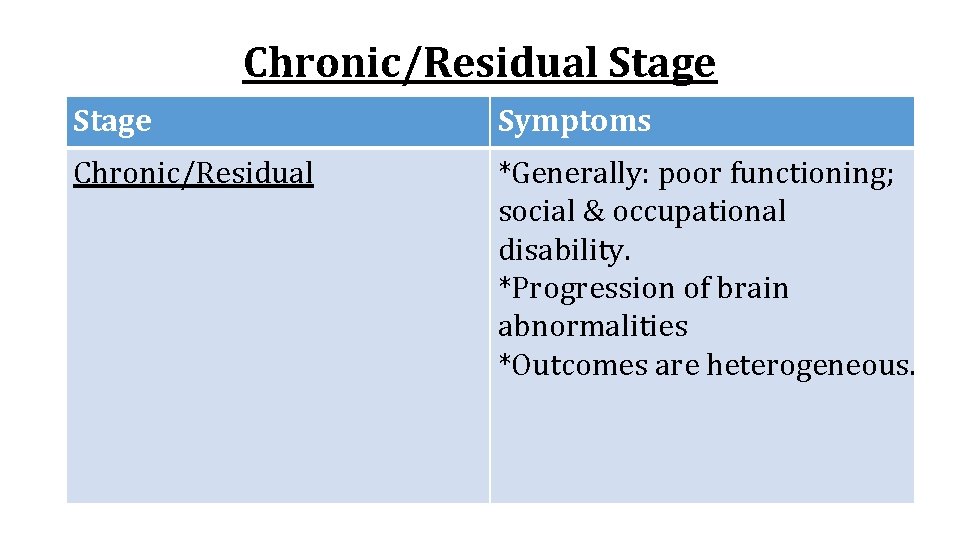
Chronic/Residual Stage Symptoms Chronic/Residual *Generally: poor functioning; social & occupational disability. *Progression of brain abnormalities *Outcomes are heterogeneous.

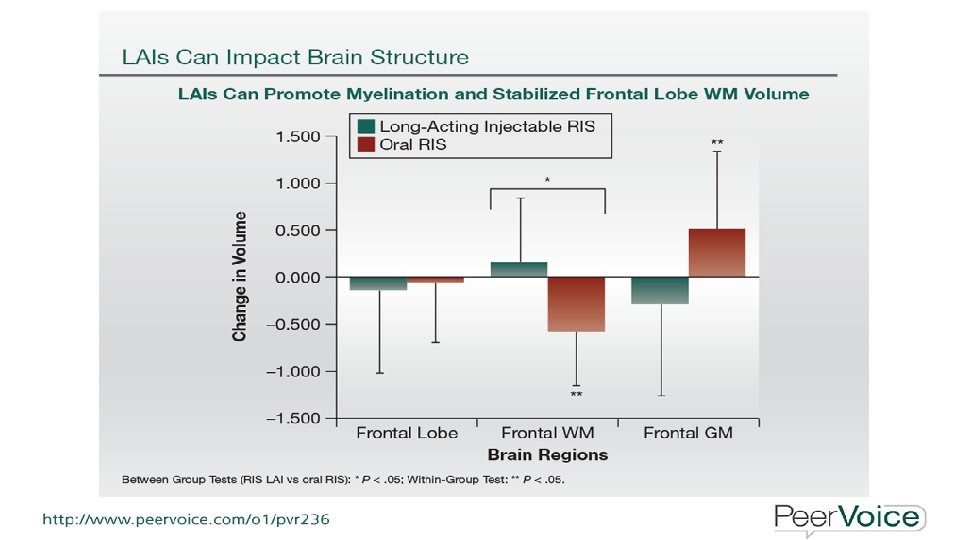
Clear evidence that early uninterrupted intervention decreases the burden of illness v. Reduces # of relapses & hospitalizations v. Higher functioning v. Preservation of grey matter

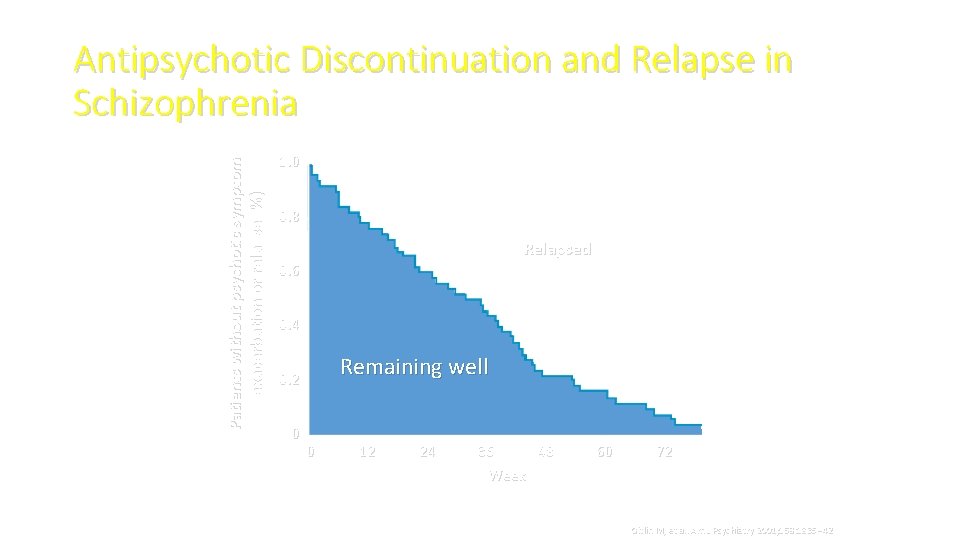
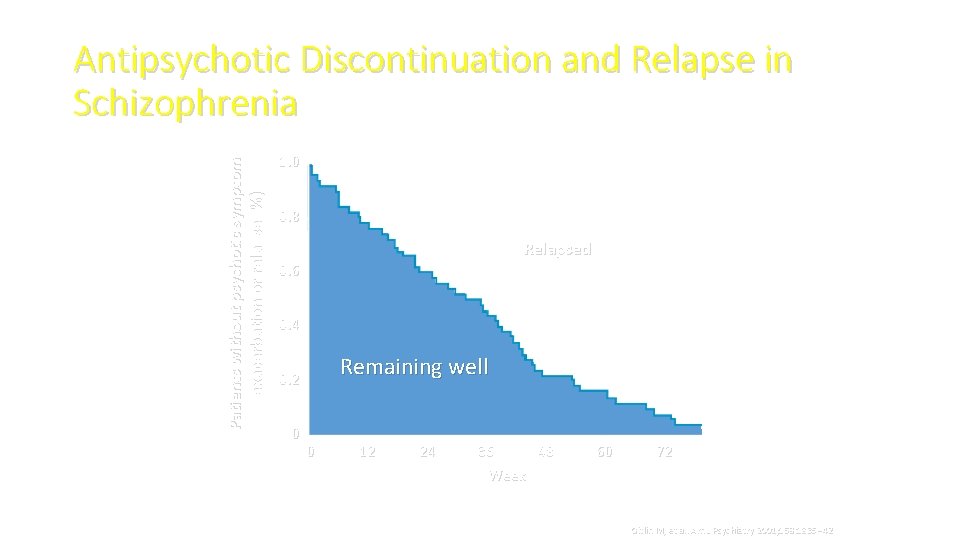
Patients without psychotic symptom exacerbation or relapse (%) Antipsychotic Discontinuation and Relapse in Schizophrenia 1. 0 0. 8 Relapsed 0. 6 0. 4 Remaining well 0. 2 0 0 12 24 36 48 Week 60 72 Gitlin M, et al. Am J Psychiatry 2001; 158: 1835– 42
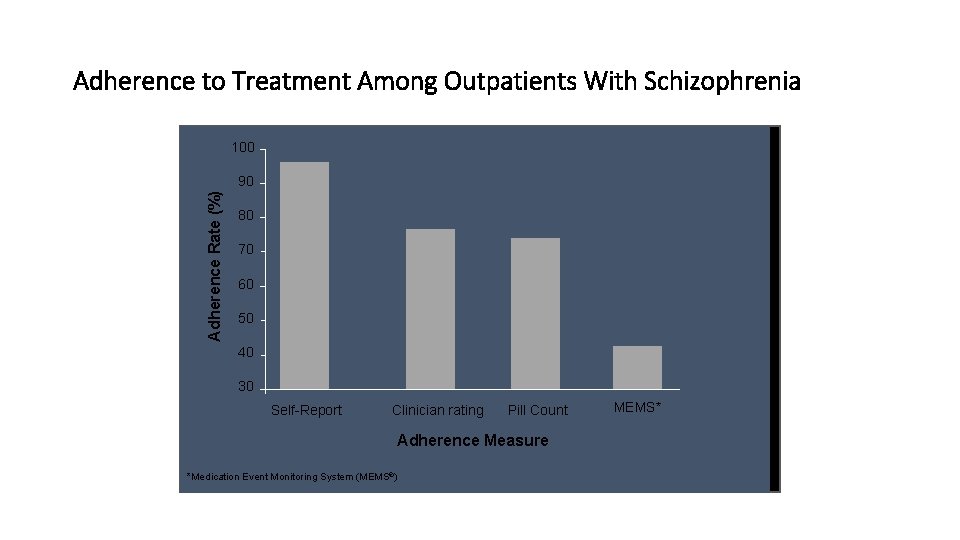
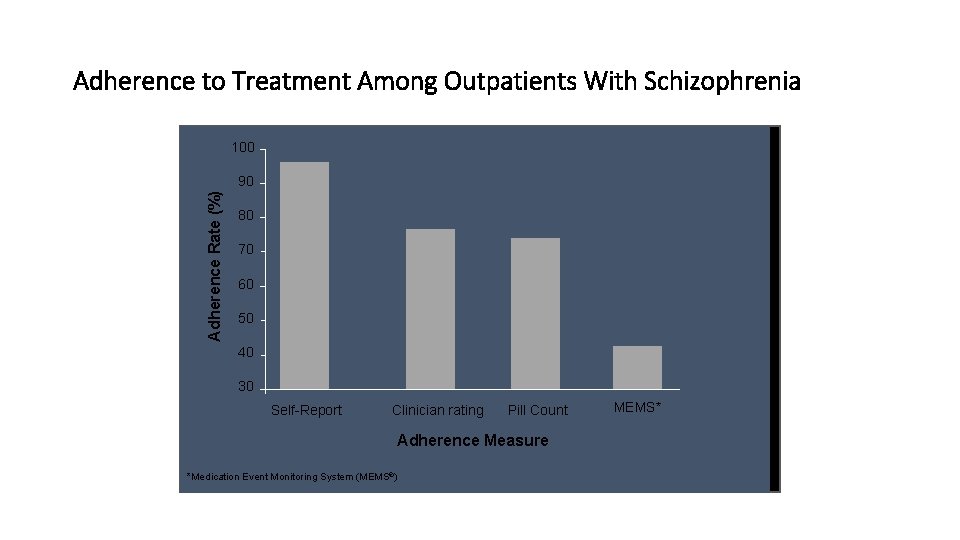
Adherence to Treatment Among Outpatients With Schizophrenia 100 Adherence Rate (%) 90 80 70 60 50 40 30 Self-Report Clinician rating Pill Count Adherence Measure *Medication Event Monitoring System (MEMS®) Remington G. et al. Scz Res 2007. MEMS*
Enhancing Adherence • Patient engagement and active involvement; • Clear, simple instructions; (people recall at best 50% of what was said during appointments, and the 50% recalled is often not the same 50% as the clinician wanted to emphasize); • No blame environment; • Enquire about financial barriers.
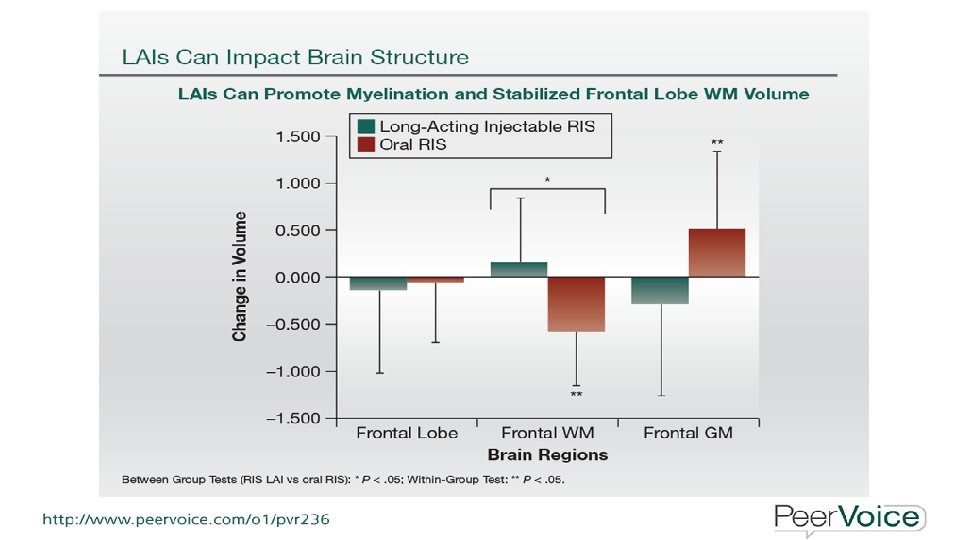
Enhancing Adherence • If you give out reading material, make sure that the patient and family can understand it; • The best results are seen with Long Acting Injectables.
Conclusions • Schizophrenia can be a devastating illness for the patient, family & society; • Early recognition AND early uninterrupted treatment are crucial to long term positive outcomes.
 Dr tachere
Dr tachere Malignant neoplasm
Malignant neoplasm Polyp
Polyp Birgit simm
Birgit simm Janno simm
Janno simm Early cpr and early defibrillation can: *
Early cpr and early defibrillation can: * Thesis statement about schizophrenia
Thesis statement about schizophrenia Example of an epic poem
Example of an epic poem What causes schizophrenia
What causes schizophrenia Loose associations
Loose associations Schizophrenia types
Schizophrenia types Schizophrenia def
Schizophrenia def Two years ago jenny was diagnosed with schizophrenia
Two years ago jenny was diagnosed with schizophrenia Nursing care plan for hallucination
Nursing care plan for hallucination Catatonia
Catatonia Schizophrenia relapse
Schizophrenia relapse Schizophrenia disorganized behavior
Schizophrenia disorganized behavior Ashley baldwin
Ashley baldwin What is schizophrenia
What is schizophrenia Genes schizophrenia
Genes schizophrenia Schizophrenia def
Schizophrenia def Akathisea
Akathisea Cognitive explanations of schizophrenia
Cognitive explanations of schizophrenia Tanya kraus
Tanya kraus Schizophrenia types
Schizophrenia types Double bind
Double bind Types of schizophrenia
Types of schizophrenia Types of schizophrenia
Types of schizophrenia Definition of schizophrenia
Definition of schizophrenia Dopamine hypothesis psychosis
Dopamine hypothesis psychosis First-line treatment for schizophrenia
First-line treatment for schizophrenia Is schizophrenia hereditary
Is schizophrenia hereditary Example of loose associations in schizophrenia
Example of loose associations in schizophrenia Signs of schizophrenia in children
Signs of schizophrenia in children Module 68 schizophrenia
Module 68 schizophrenia Schizophrenia dsm 5
Schizophrenia dsm 5 Example of loose associations in schizophrenia
Example of loose associations in schizophrenia Youtube crash course psychology
Youtube crash course psychology Symptoms of schizophrenia
Symptoms of schizophrenia Is schizophrenia on a spectrum
Is schizophrenia on a spectrum Chapter 12 schizophrenia spectrum disorders
Chapter 12 schizophrenia spectrum disorders Hebephrenic schizophrenia
Hebephrenic schizophrenia Example of loose associations in schizophrenia
Example of loose associations in schizophrenia Acute dystonia pathophysiology
Acute dystonia pathophysiology Psychosis
Psychosis Negative explanatory style
Negative explanatory style