Wound Complications of VEPTR Incisions Sumeet Garg Jaren



- Slides: 15
Wound Complications of VEPTR Incisions Sumeet Garg, Jaren La. Greca, Dexiang Gao, Tricia St. Hilaire, Michael Glotzbecker, Ying Li, John T. Smith, Jack Flynn, Jeffrey Sawyer, Michael G. Vitale, Ron El-Hawary, John M. Flynn

Disclosure • B) Consulting - De. Puy Synthes Spine – teaching at educational course for residents • • • La. Greca – none Gao – none St. Hilaire – none Glotzbecker – A) Synthes, via CWSDRF Li – none Smith – A) CWSDRF B) Synthes Flynn – F) Biomet, Wolters Kluwer Health – Lippincott Williams & Wilkins Sawyer – F) Mosby, Wolters Kluwer Health – Lippincott Williams & Wilkins Vitale – A) Synthes B) Biomet, Stryker F) Biomet El-Hawary – A) De. Puy, Medtronic B) De. Puy, Halifax Biomedical Inc, Medtronic, Synthes Flynn – none 2
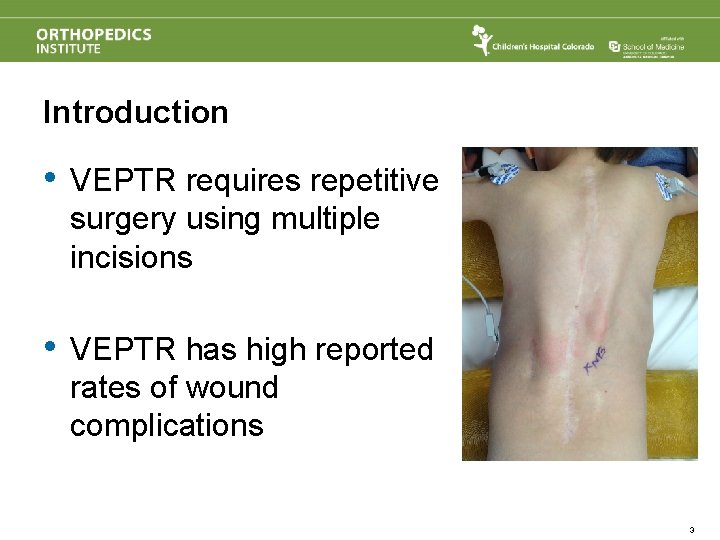
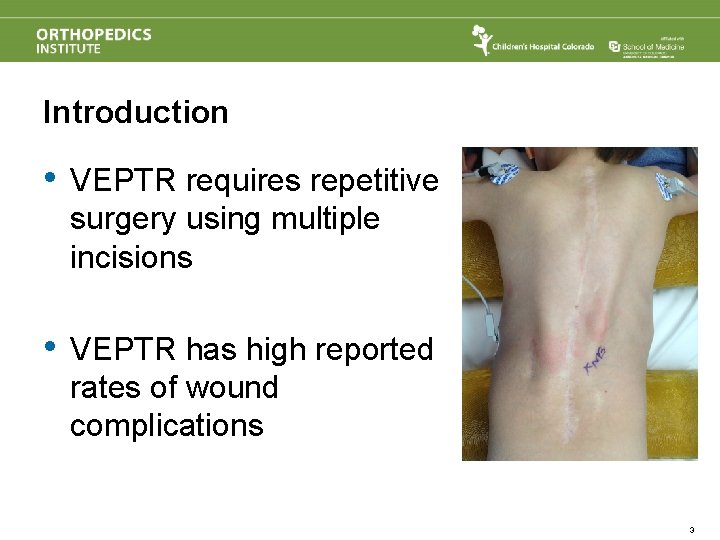
Introduction • VEPTR requires repetitive surgery using multiple incisions • VEPTR has high reported rates of wound complications 3
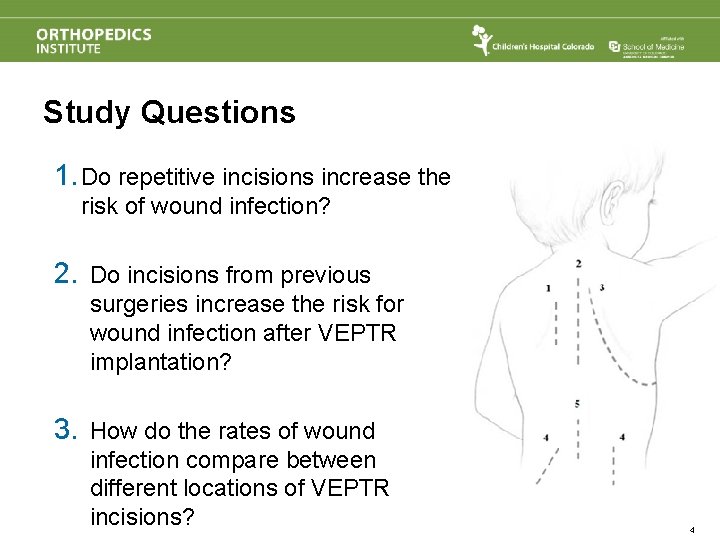
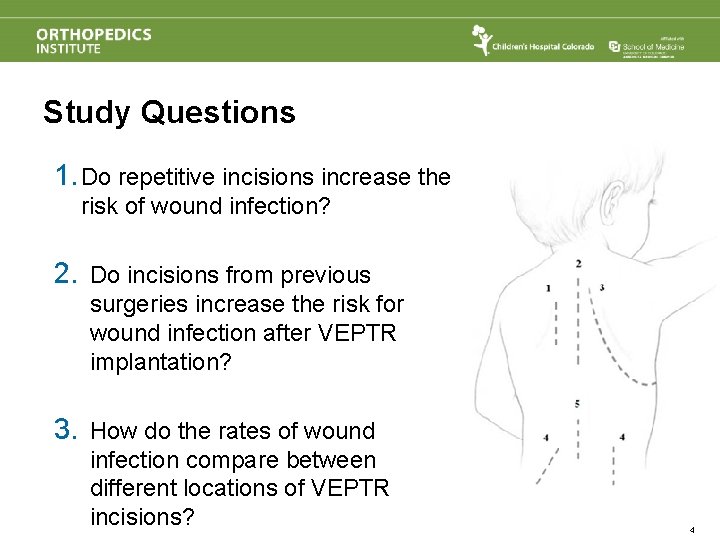
Study Questions 1. Do repetitive incisions increase the risk of wound infection? 2. Do incisions from previous surgeries increase the risk for wound infection after VEPTR implantation? 3. How do the rates of wound infection compare between different locations of VEPTR incisions? 4

Methods • Multicenter retrospective review • 9 participating institutions • Inclusion Criteria: • Minimum 4 expansion procedures • 20 most recent patients treated with VEPTR from each institution • Wound complication requiring return to the OR • Outcome Variables • infecting procedure (implant vs. expansion vs. revision), time to infection, total incisions prior to infection, total incisions per incision type Final Study Cohort: 103 subjects 5
Infection Rate • Infection Rate: 24% • 25/103 patients developed infection during VEPTR treatment • 6 with multiple infection events 6
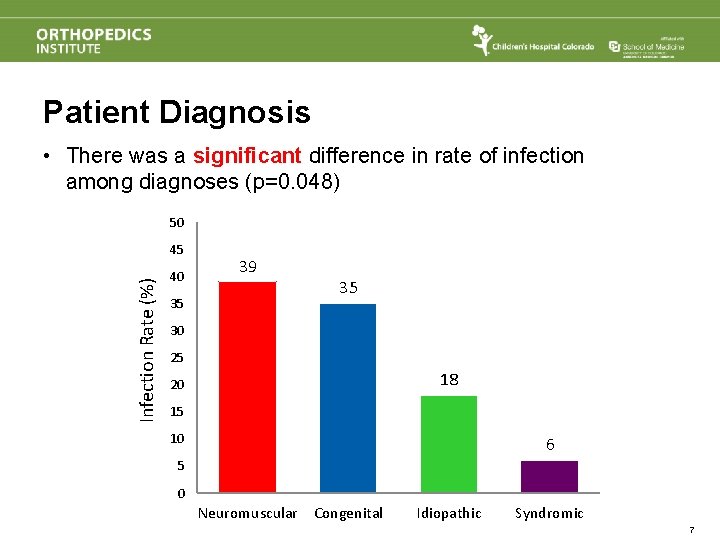
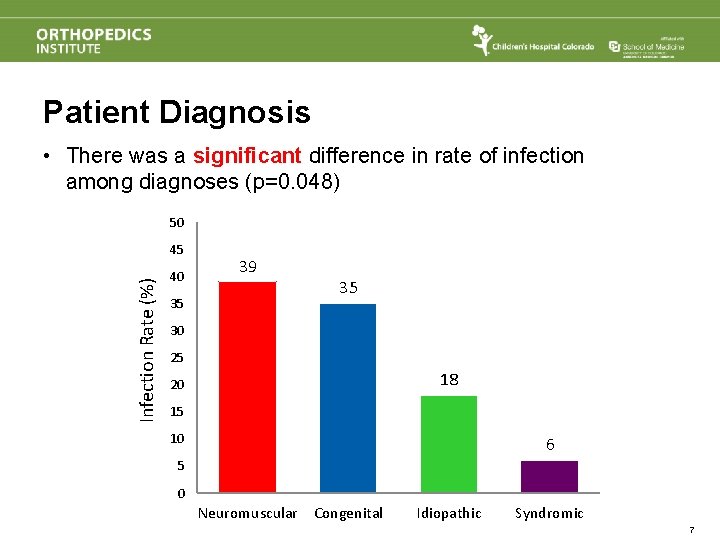
Patient Diagnosis • There was a significant difference in rate of infection among diagnoses (p=0. 048) 50 Infection Rate (%) 45 40 35 39 35 30 25 18 20 15 10 6 5 0 Neuromuscular Congenital Idiopathic Syndromic 7
Deformity Magnitude • There was no significant difference in average preoperative Cobb angle between infected (68º) and non-infected patients (62º) (p=0. 17) 8
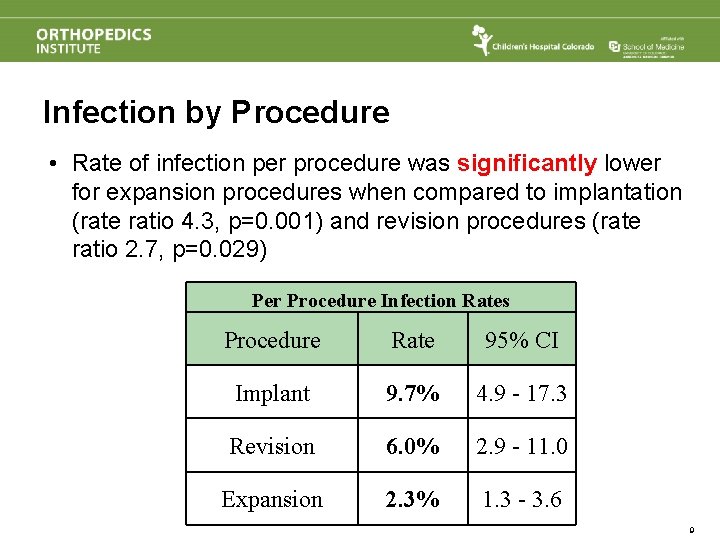
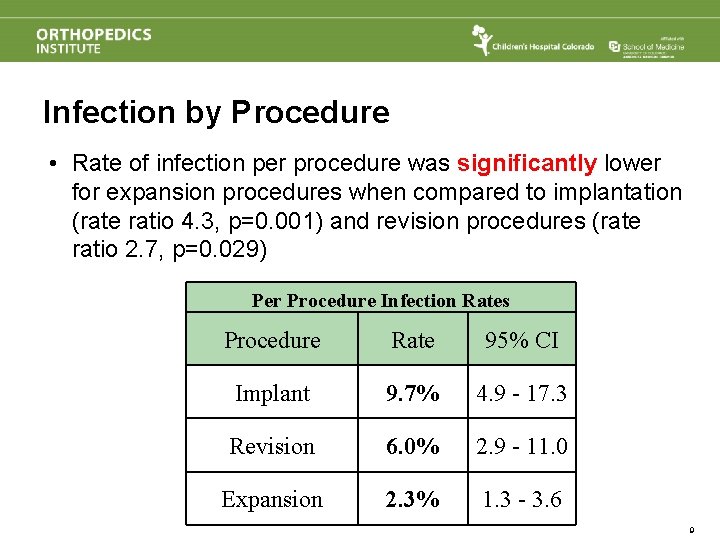
Infection by Procedure • Rate of infection per procedure was significantly lower for expansion procedures when compared to implantation (rate ratio 4. 3, p=0. 001) and revision procedures (rate ratio 2. 7, p=0. 029) Per Procedure Infection Rates Procedure Rate 95% CI Implant 9. 7% 4. 9 - 17. 3 Revision 6. 0% 2. 9 - 11. 0 Expansion 2. 3% 1. 3 - 3. 6 9
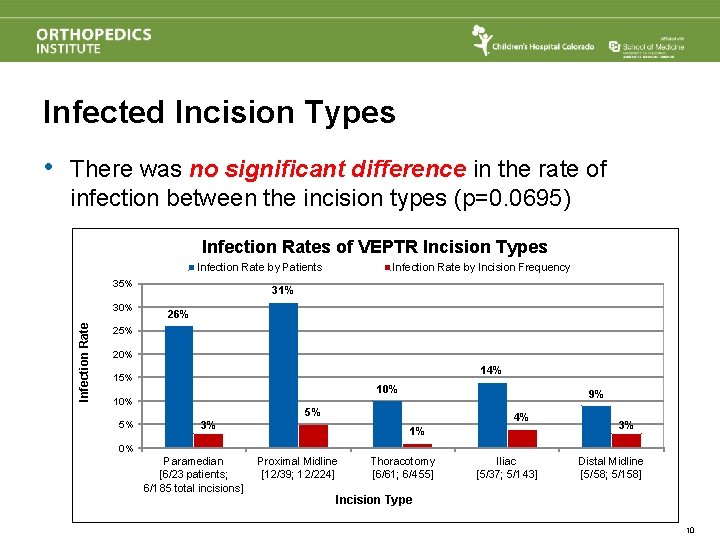
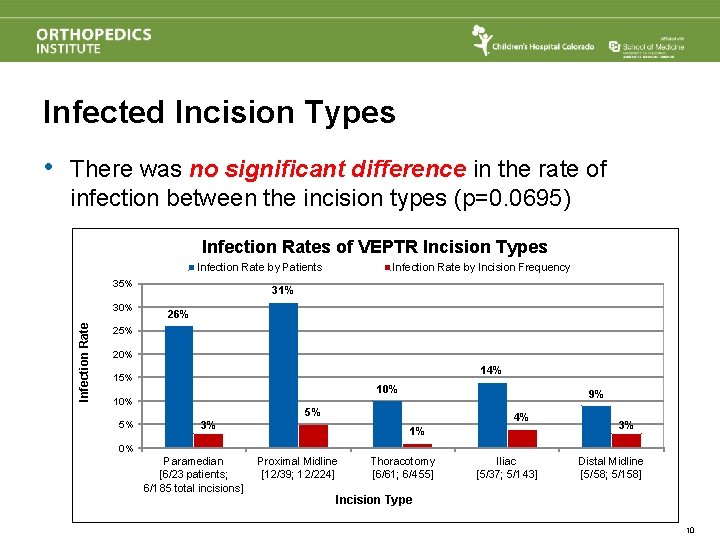
Infected Incision Types • There was no significant difference in the rate of infection between the incision types (p=0. 0695) Infection Rates of VEPTR Incision Types Infection Rate by Patients 35% Infection Rate 30% Infection Rate by Incision Frequency 31% 26% 25% 20% 14% 15% 10% 5% 3% 9% 5% 4% 1% 3% 0% Paramedian [6/23 patients; 6/185 total incisions] Proximal Midline [12/39; 12/224] Thoracotomy [6/61; 6/455] Iliac [5/37; 5/143] Distal Midline [5/58; 5/158] Incision Type 10
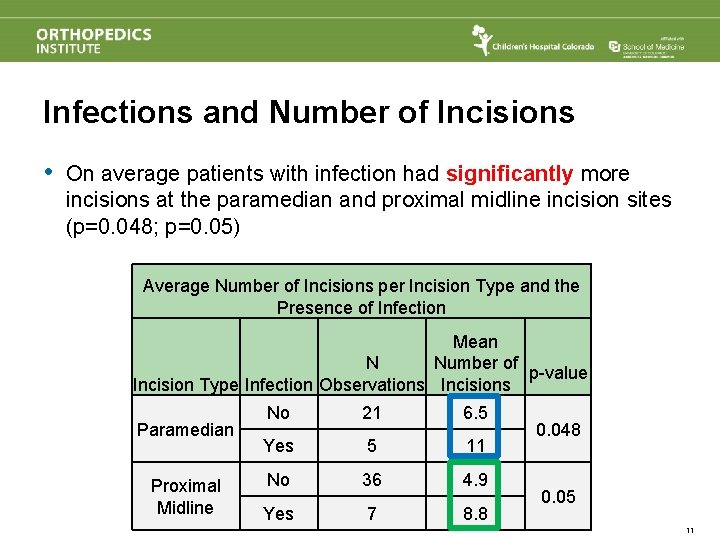
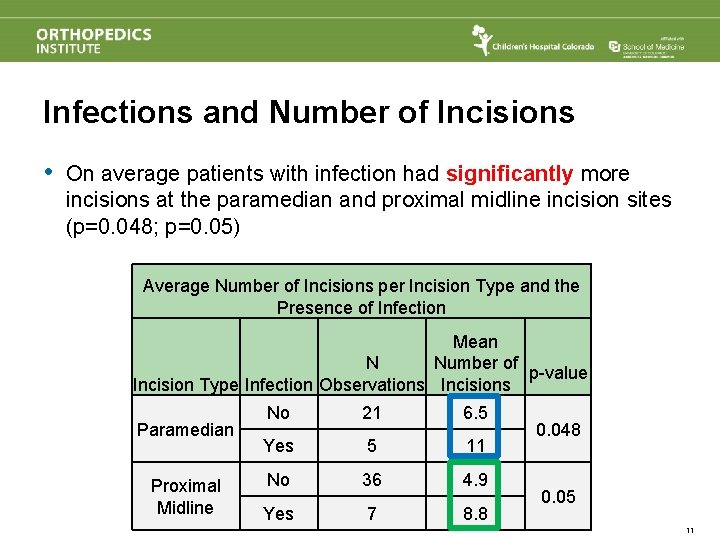
Infections and Number of Incisions • On average patients with infection had significantly more incisions at the paramedian and proximal midline incision sites (p=0. 048; p=0. 05) Average Number of Incisions per Incision Type and the Presence of Infection Mean N Number of p-value Incision Type Infection Observations Incisions Paramedian Proximal Midline No 21 6. 5 Yes 5 11 No 36 4. 9 Yes 7 8. 8 0. 048 0. 05 11
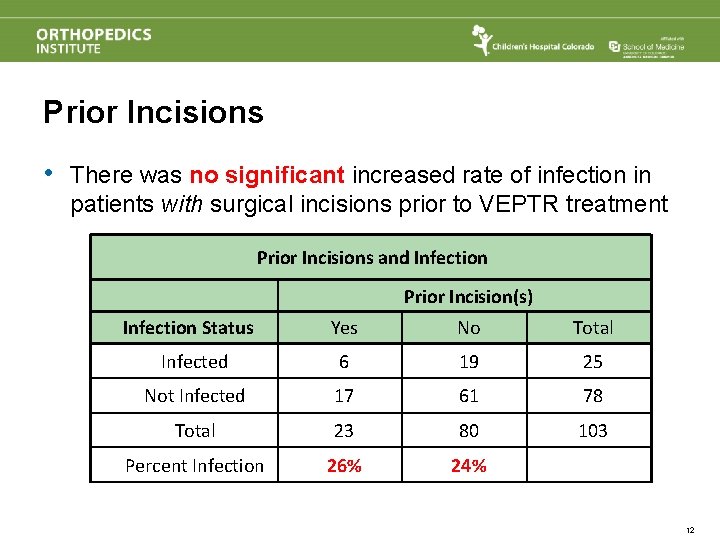
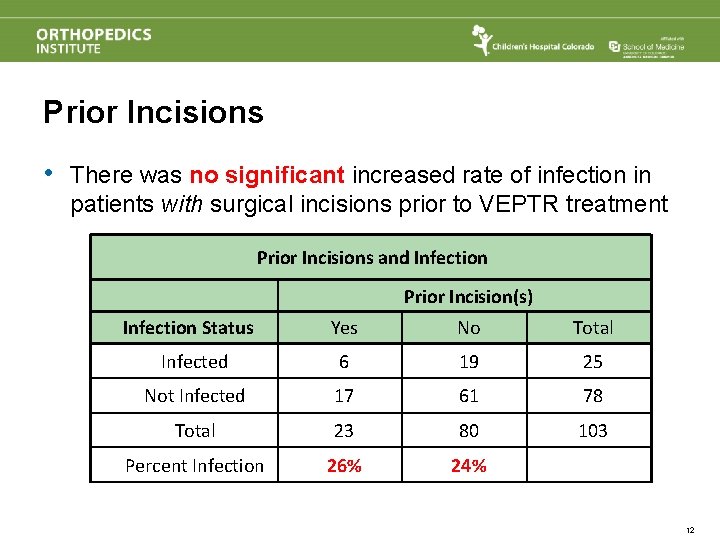
Prior Incisions • There was no significant increased rate of infection in patients with surgical incisions prior to VEPTR treatment Prior Incisions and Infection Prior Incision(s) Infection Status Yes No Total Infected 6 19 25 Not Infected 17 61 78 Total 23 80 103 Percent Infection 26% 24% 12
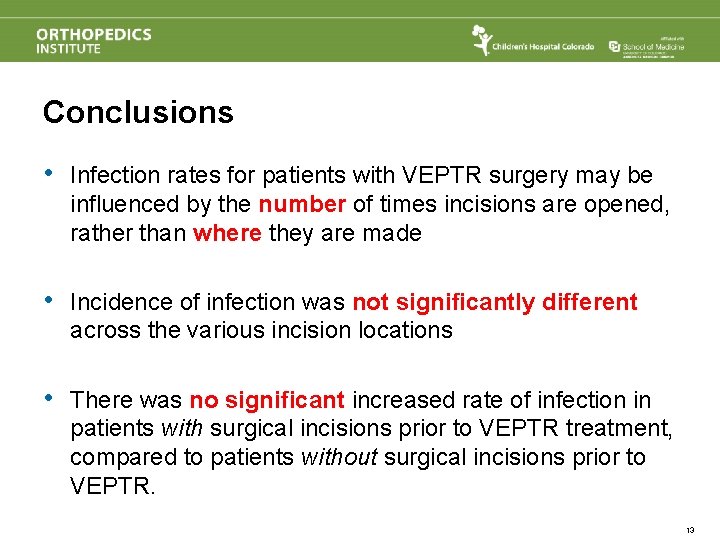
Conclusions • Infection rates for patients with VEPTR surgery may be influenced by the number of times incisions are opened, rather than where they are made • Incidence of infection was not significantly different across the various incision locations • There was no significant increased rate of infection in patients with surgical incisions prior to VEPTR treatment, compared to patients without surgical incisions prior to VEPTR. 13
Recommendation Surgeons should utilize the most appropriate incision in relation to their patient’s pathology when using VEPTR 14

Thank You 15
 Sumeet garg
Sumeet garg Compound measures dr frost
Compound measures dr frost Bermtoerisme jaren 60
Bermtoerisme jaren 60 Veptr growing rods
Veptr growing rods Fietsen alle jaren
Fietsen alle jaren Jazz oervorm van de jamaicaanse reggae
Jazz oervorm van de jamaicaanse reggae James bond door de jaren heen
James bond door de jaren heen Singkatan latin farmasi
Singkatan latin farmasi Prakhar garg stony brook
Prakhar garg stony brook Trebaculation
Trebaculation Amit garg irse
Amit garg irse Naveen garg iit delhi
Naveen garg iit delhi Indu garg
Indu garg Naveen garg iit delhi
Naveen garg iit delhi Akansha jahangir
Akansha jahangir Dr rajesh garg
Dr rajesh garg