Hemorrhagic Stroke The KILLER Headache Intended Audience This



























- Slides: 106
Hemorrhagic Stroke: The KILLER Headache
Intended Audience This course is designed for licensed stroke team members, including: n n n Nurses (RNs/LPNs) CCCs and Social Workers in Care Management Physical Therapists, Occupational Therapists, and Speech & Language Pathologists Pharmacists Clinical Dieticians
Prerequisites/Special Considerations There are no prerequisites for taking this course n There are no special considerations n
Goal n Contribute to increased knowledge about hemorrhagic stroke in members of the stroke team
Objectives By the end of this CBL, the participant will be able to: n n n Define hemorrhagic stroke, including ICH and SAH Discuss risk factors, possible causes, and pathophysiology of hemorrhagic strokes Review treatments and potential complications for patients with hemorrhagic stroke
Key Terms Hemorrhagic stroke n Intracranial hemorrhage (ICH) n Subarachnoid hemorrhage (SAH) n Cerebral aneurysm n Arteriovenous malformation (AVM) n
Menu Lesson 1: Hemorrhagic stroke Lesson 2: Intracranial hemorrhage Lesson 3: Subarachnoid hemorrhage A. Cerebral Aneurysm B. Arteriovenous Malformation
Lesson 1: Hemorrhagic Stroke 1. 2. 3. Define hemorrhagic stroke Discuss risk factors for hemorrhagic stroke Review cerebral circulation and most common sites of hemorrhagic stroke
Hemorrhagic Stroke n DEFINITION: Escape of blood from a ruptured blood vessel within the brain or between the layers covering the brain, causing damage to nearby brain tissue
Morbidity & Mortality Intracranial hemorrhage (ICH) represents 15% of all strokes n More than 75, 000 new hemorrhagic strokes occur each year n 30 -day mortality rate is 2 x – 6 x higher than that of ischemic strokes n More than half will die in the first 2 days n 6% die before reaching the hospital n

Stroke is the 4 th leading cause of death and the #1 cause of disability in the U. S. Although hemorrhagic stroke represents only a small fraction of total strokes, the morbidity is more severe and mortality rates are higher than in ischemic stroke. n Only 20% of patients with hemorrhagic stroke will regain their functional independence n
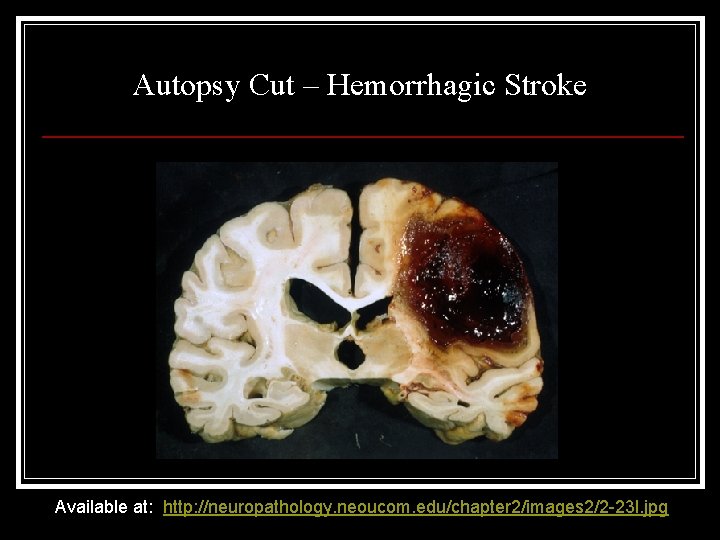
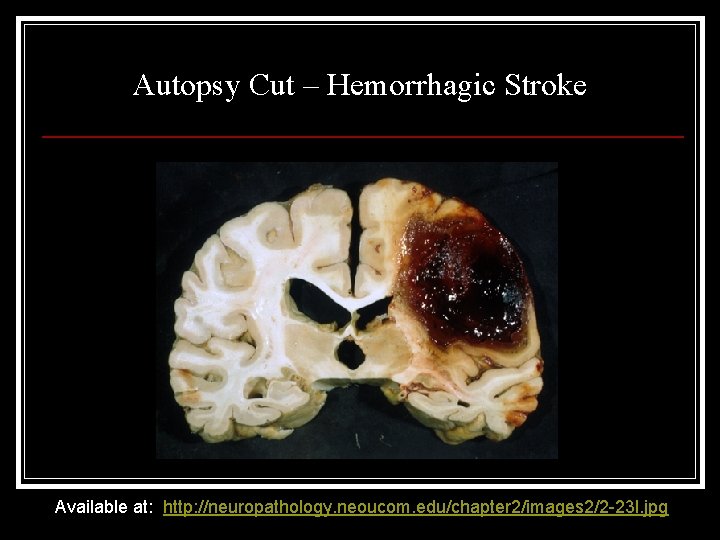
Autopsy Cut – Hemorrhagic Stroke Available at: http: //neuropathology. neoucom. edu/chapter 2/images 2/2 -23 l. jpg
Uncontrollable Risk Factors for Hemorrhagic Stroke Include: Age n Gender n Ethnicity n Genetics (familial aneurysms) n
Age n Older Adults: People most at risk for stroke are older adults, particularly those with high blood pressure, who are sedentary, overweight, smoke, or have diabetes. n Younger Adults: Younger people are not immune. About 28% of stroke victims are under the age of 65.

Gender n In most age groups except in older adults, stroke is more common in men than in women. n However, it kills more women than men at a ratio of 3: 2.
Ethnicity n n All minority groups, including Native Americans, Hispanics, and African-Americans, face a significantly higher risk than Caucasians. The risk is also higher in Asian Americans and the Japanese population. The differences in risk among all groups diminish as people age. Younger African-Americans are two to three times more likely to experience and four times more likely to die from stroke.
Other Risk Factors Include: Hypertension n Smoking n Diabetes n Obesity n Illicit drug use n Stress n Sickle cell anemia n
Pathophysiology n The pathophysiology of a hemorrhagic stroke is associated with an immediate rise in ICP, ischemic cellular responses, cerebral edema, and compromised cerebral perfusion – possibly leading to herniation of the brain
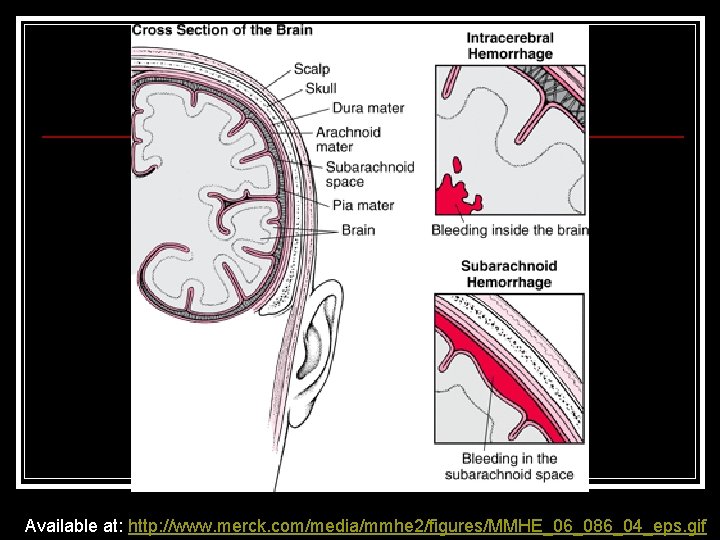
2 Categories of Hemorrhagic Stroke n ICH: Intracranial Hemorrhage – bleeding into brain tissue as a result of bleeding or rupture of a small, deep cortical artery that is damaged by chronic hypertension n SAH: Subarachnoid Hemorrhage – the result of bleeding into the subarachnoid space, most often in relation to a ruptured aneurysm or Arteriovenous Malformation (AVM)
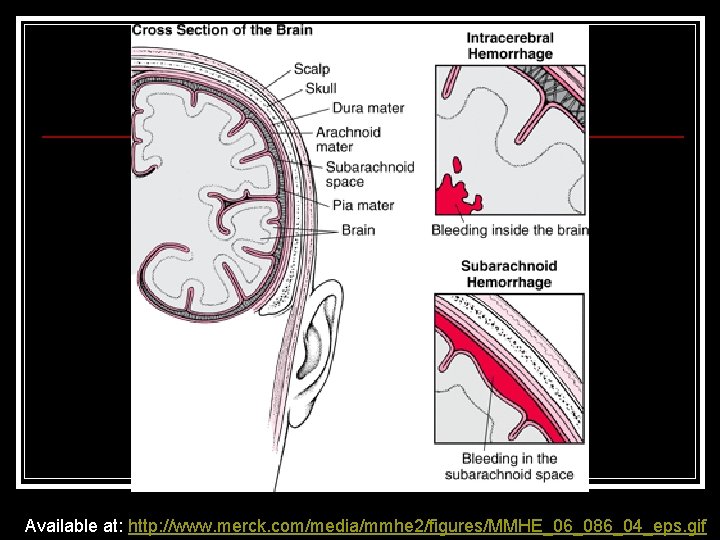
Available at: http: //www. merck. com/media/mmhe 2/figures/MMHE_06_086_04_eps. gif
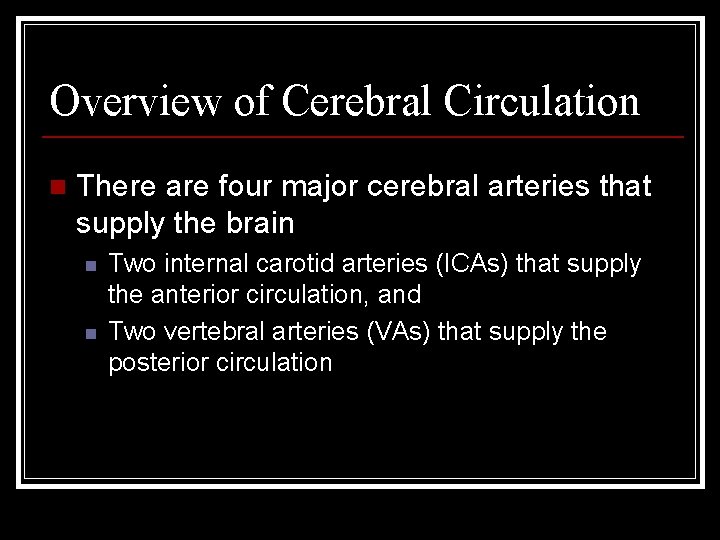
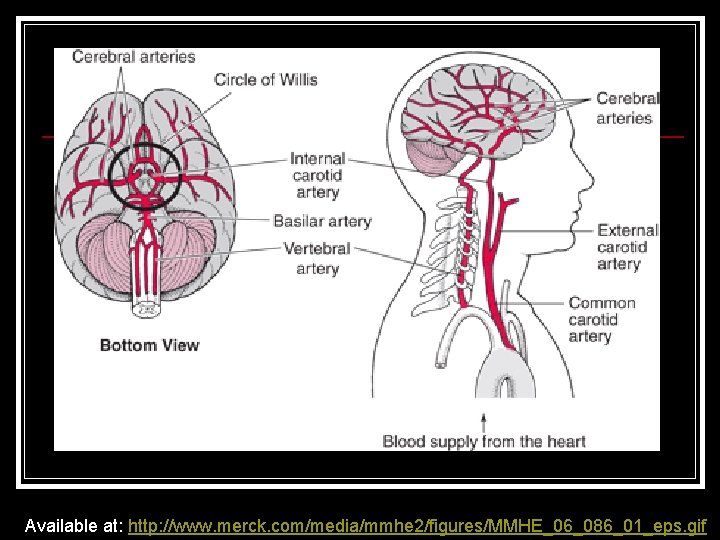
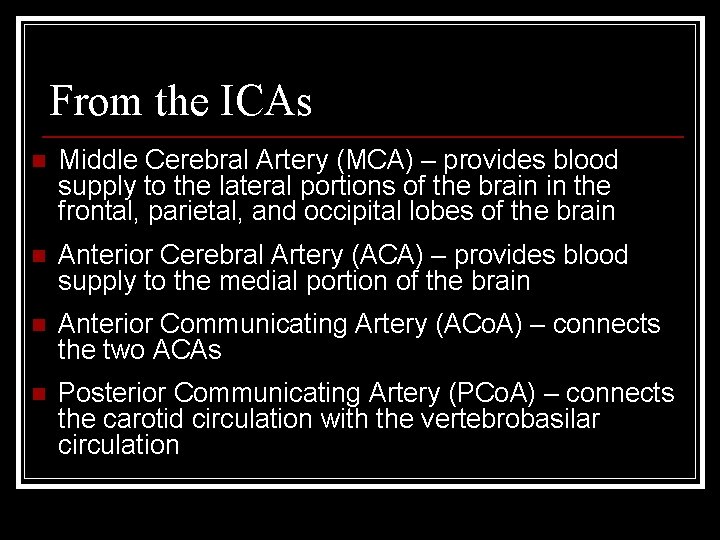
Overview of Cerebral Circulation n There are four major cerebral arteries that supply the brain n n Two internal carotid arteries (ICAs) that supply the anterior circulation, and Two vertebral arteries (VAs) that supply the posterior circulation
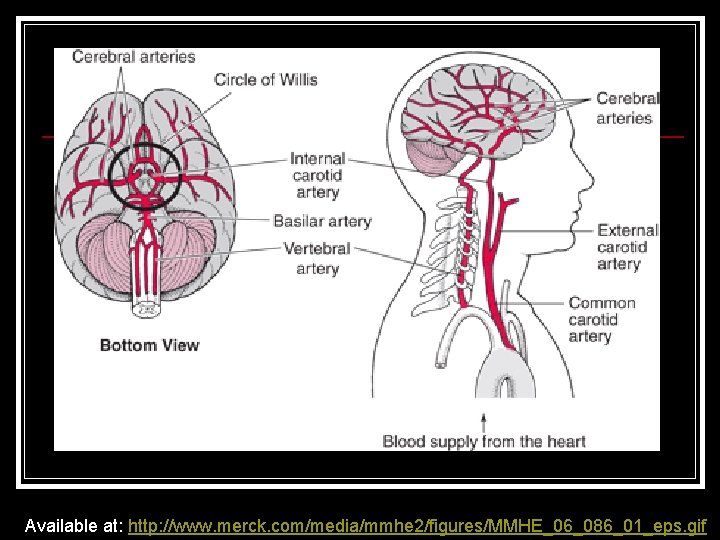
Available at: http: //www. merck. com/media/mmhe 2/figures/MMHE_06_086_01_eps. gif
From the ICAs n Middle Cerebral Artery (MCA) – provides blood supply to the lateral portions of the brain in the frontal, parietal, and occipital lobes of the brain n Anterior Cerebral Artery (ACA) – provides blood supply to the medial portion of the brain n Anterior Communicating Artery (ACo. A) – connects the two ACAs n Posterior Communicating Artery (PCo. A) – connects the carotid circulation with the vertebrobasilar circulation

This figure illustrates the areas of the brain supplied by the major arteries http: //missinglink. ucsf. edu/lm/ids_104_cerebrovasc_neuropath/Case 3 Images/Cer Art. Dist. Blum 1. jpg
The Vertebral Arteries Unite to form the basilar artery (BA) n The BA divides to form the Posterior Cerebral Arteries (PCA) n The PCAs supply blood to the occipital lobe and portions of the temporal lobe n

Vertebral Arteries Available at: http: //graphics 8. nytimes. com/images/2007/08/01/health/adam/18009. jpg

Lesson 1 Review Hemorrhagic stroke is more common in men than in women, except in older adults. n Hemorrhagic stroke kills more women than men. n Younger African-Americans are two to three times more likely to experience a stroke and four times more likely to die from stroke. n
Lesson 1 Review n Two Types of Hemorrhagic Stroke: n n ICH: Intracranial Hemorrhage – Bleeding into brain tissue as a result of bleeding or rupture of a small, deep cortical artery that is damaged by chronic hypertension SAH: Subarachnoid Hemorrhage – The result of bleeding into the subarachnoid space, most often in relation to a ruptured aneurysm or AVM (arteriovenous malformation)

Lesson 1 Review n Risk factors for hemorrhagic stroke include: n n n n Hypertension Smoking Diabetes Obesity Illicit drug use Stress Sickle cell anemia
Lesson 1 Review n There are four major cerebral arteries that supply the brain n Two internal carotid arteries (ICAs) that supply the anterior circulation, and Two vertebral arteries (VAs) that supply the posterior circulation The divisions and deep branches of the Middle Cerebral Artery (MCA) supply the largest territory of brain
Lesson 2: Intracranial Hemorrhage Identify classic symptoms (presentation) of a patient experiencing intracranial hemorrhage (ICH) n Review common sites of ICH n Discuss possible causes of ICH n
Intracranial Hemorrhage (ICH) ICH that is massive or near vital brain centers constitutes a medical emergency that requires immediate diagnosis and intervention to prevent death n However, ICH in small penetrating vessels can mimic the evolution of an ischemic stroke, which complicates diagnosis and treatment n
Presentation Symptoms vary depending on the area of the brain affected and the extent of the bleeding n Headache, vomiting, altered level of consciousness (LOC), seizure at onset (or within 24 hours) n May present as new onset of seizure n Hypertension is commonly a prominent finding n
Presentation Is: n Characterized by sudden loss of consciousness that usually occurs without warning and while the person is active n Typical situation: an older person with a long history of poorly controlled hypertension straining at stool develops a severe headache, decreased LOC, hemiplegia, nausea/vomiting, and possibly a focal seizure
ICH Symptoms and Syndromes In addition to altered LOC, headache, nausea/vomiting, nuchal rigidity, hypertension and bradycardia that occur related to increased intracranial pressure (ICP), there are ICH syndromes. n Depending on the location of the ICH, each syndrome has distinguishing characteristics n
Intracranial Hemorrhage With ICH, the usual hemorrhage sites are small, deep cortical arteries n The most common sites are: n n n Putamen (50%) Thalamus (30%) Cerebellum (10%) Pons (10%)

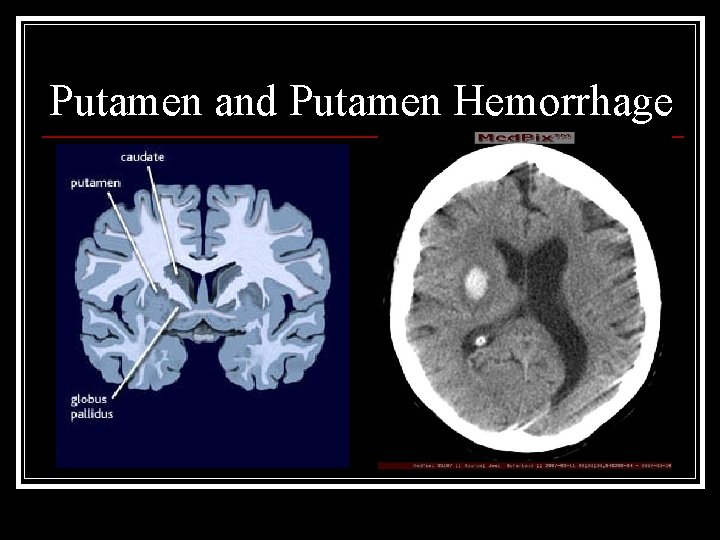
ICH: Deep Cortical Syndromes The Putamen is involved in sensorimotor integration and motor control. n Putamen hemorrhage accounts for 50% of ICH n Symptoms include: n n n Contralateral hemiplegia Contralateral hemisensory deficits Hemianopsia Slurred speech
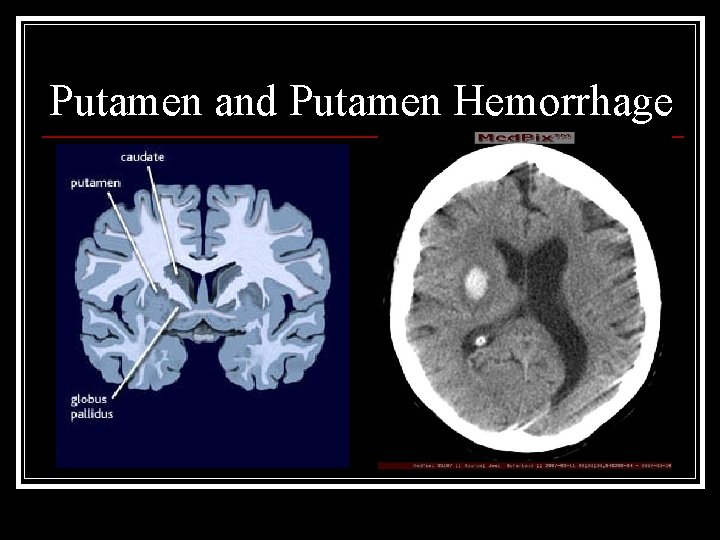
Putamen and Putamen Hemorrhage

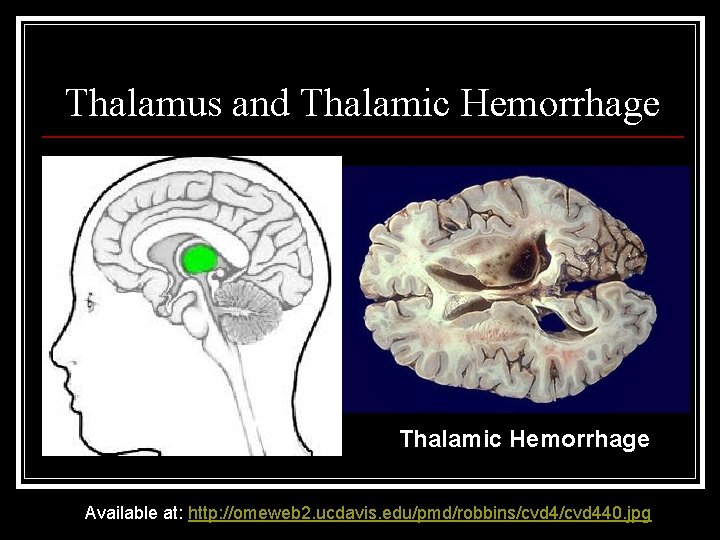
ICH: Deep Cortical Syndromes The Thalamus relays sensory information to various parts of the cerebral cortex n Thalamic Hemorrhage accounts for 30% of ICH n This syndrome is characterized by: n n Contralateral hemiplegia Contralateral hemisensory deficits Deficit of vertical and lateral gaze
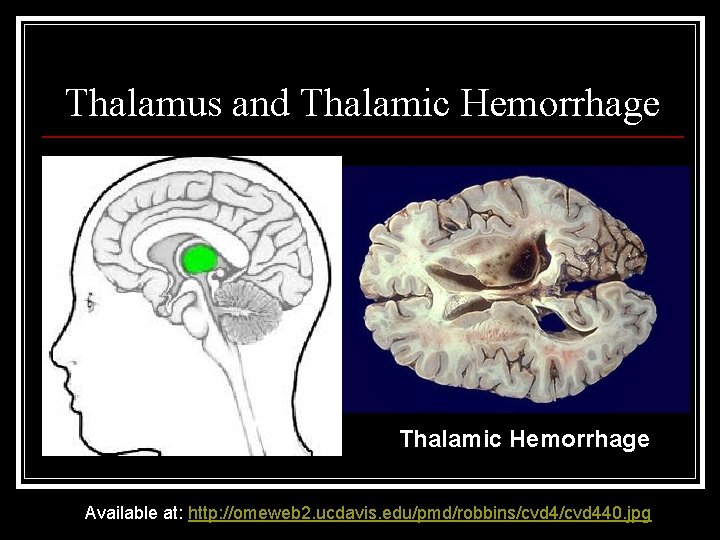
Thalamus and Thalamic Hemorrhage Available at: http: //omeweb 2. ucdavis. edu/pmd/robbins/cvd 440. jpg
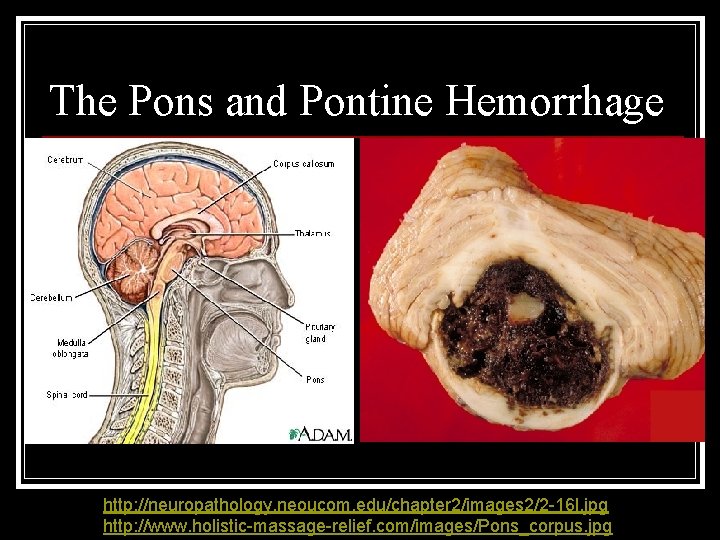
ICH: Deep Cortical Syndromes The Pons relays sensory info between the cerebellum and cerebrum, controls arousal, and regulates respiration n Pontine hemorrhage accounts for 10% of ICH n It is characterized by: n n n “Locked in” syndrome Deficits in lateral eye movements
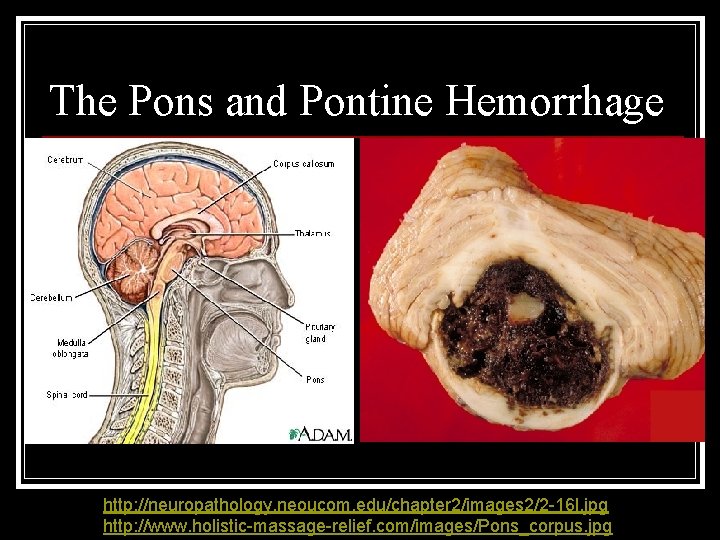
The Pons and Pontine Hemorrhage http: //neuropathology. neoucom. edu/chapter 2/images 2/2 -16 l. jpg http: //www. holistic-massage-relief. com/images/Pons_corpus. jpg
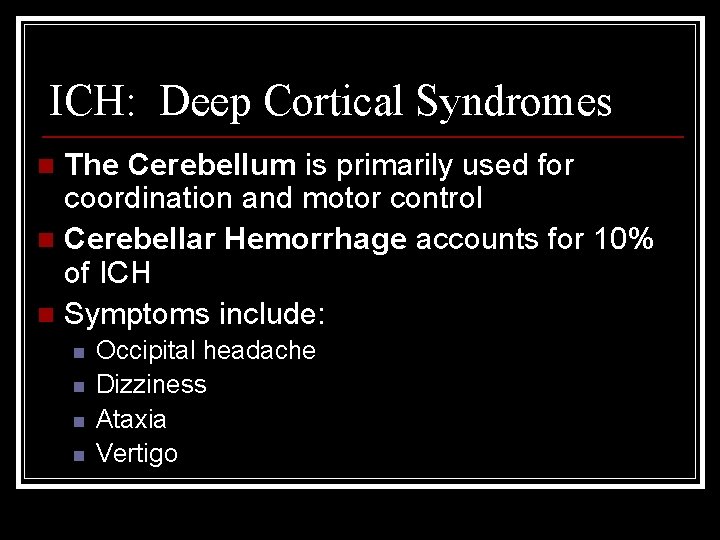
ICH: Deep Cortical Syndromes The Cerebellum is primarily used for coordination and motor control n Cerebellar Hemorrhage accounts for 10% of ICH n Symptoms include: n n n Occipital headache Dizziness Ataxia Vertigo

Cerebellum and Cerebellar Hemorrhage Available at: http: //pathcuric 1. swmed. edu/Path. Demo/cns 1190. jpg
Causes of ICH Hypertension n Aneurysm n Arteriovenous Malformation (AVM) n Trauma n Coagulopathies n Cocaine use n
Cocaine Abuse Creates a high risk for hemorrhagic stroke as a result of a sudden rise in blood pressure, heart rate, and contractions of the left ventricle of the heart n Cocaine also tightly constricts coronary and cerebral arteries n

Lesson 2 Review n Symptoms of hemorrhagic stroke vary depending on the area of the brain affected, but can include: n n n Headache Nausea/vomiting Altered level of consciousness (LOC) Seizure at onset (or within 24 hours) Hypertension
Lesson 2 Review n Possible Causes of ICH include: n n n Hypertension Aneurysm Arteriovenous Malformation (AVM) Trauma Coagulopathies Cocaine use
Lesson 2 Review n With ICH, the usual hemorrhage sites are small, deep cortical arteries; most commonly: n n Putamen (50%) Thalamus (30%) Cerebellum (10%) Pons (10%)
Lesson 3: Cerebral Aneurysm Define cerebral aneurysm n Identify warning signs of aneurysm rupture n Discuss two treatment options for cerebral aneurysm n Review patient care strategies and potential complications in cerebral aneurysm n
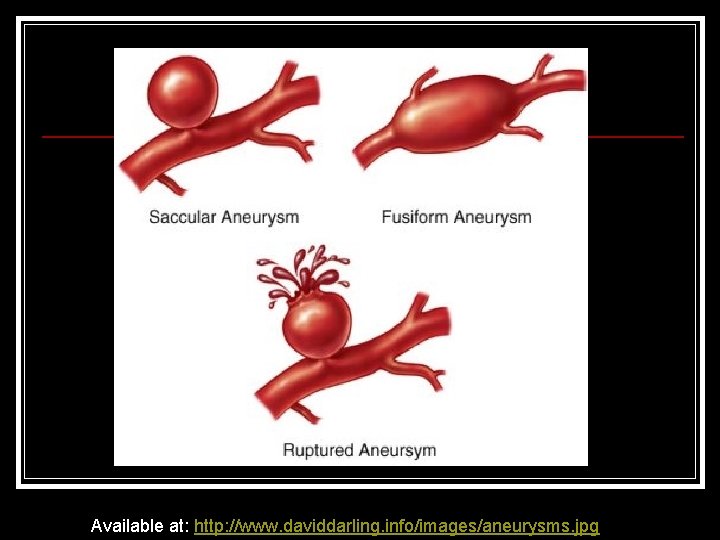
Cerebral Aneurysm A cerebral aneurysm is a saccular outpouching of a cerebral artery n Aneurysm rupture is the most common cause of non-traumatic subarachnoid hemorrhage (SAH) n Aneurysm usually occurs at arterial bifurcations in the Circle of Willis n
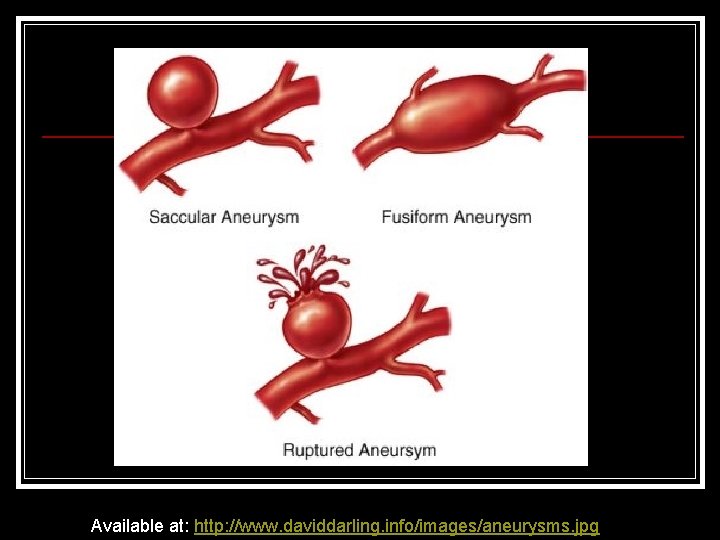
Available at: http: //www. daviddarling. info/images/aneurysms. jpg
Incidence of Cerebral Aneurysm There are 30, 000 new cases of SAH secondary to aneurysm rupture each year n It is most prevalent in 35 – 60 year olds n Occurs more often in women at a 3: 2 ratio n Only one third recover without major disability n
Incidence Cont’d n n n Autopsy studies show that the overall frequency of un-ruptured aneurysms in the general population is about 5% It is estimated that 10 -15 million Americans have a cerebral aneurysm (most of them are small, though, and do not bleed throughout life) Although advanced imaging techniques have allowed for noninvasive detection of an aneurysm, most are found following rupture
The Chance of Aneurysm Rupture n Influenced by: n n n History of smoking Age Gender Hypertension Number of existing aneurysms Aneurysm size > 3 – 5 cm

Aneurysm Rupture n The occurrence, growth and rupture of aneurysms can be directly related to the effect of hemodynamic forces n n n Blood pressure Stress on the arterial wall Impingement forces
Prodromal Signs present 10 – 20 days prior to rupture n 50% experience warning signs that are either ignored or attributed to other causes n n n n Headache (48%) Dizziness (10%) Pain above & behind the eye (7%) Sensory or motor disturbance (6%) Photophobia, diplopia, or vision loss (4%) Bruits (3%) Impaired extra ocular movements (EOMs) or ptosis

Pathophysiology of Aneurysm Rupture n n n At the time of rupture, blood under high pressure is forced into the subarachnoid (SA) space Pressure in the surrounding tissue actually controls or stops the bleeding Fibrin, platelets and fluid form a plug that seals off the site of bleeding The resulting clot can occlude the area & interfere with CSF absorption, leading to hydrocephalus The blood released irritates the brain tissue, setting up an inflammatory response & cerebral edema (increased ICP and decreased cerebral perfusion)

Presentation The patient experiences a characteristic, intense, unrelenting headache of sudden onset often described as “the worst headache of my life!” n Patients with history of headaches including migraines typically describe SAH headache as different, being more severe and accompanied by a feeling of impending doom n Transient loss of or altered consciousness n

Intracranial Pressure (ICP) Increases n Signs of elevated ICP: n Cushing’s Triad: n n n Hypertension Bradycardia Widening pulse pressure Seizures Nausea and vomiting
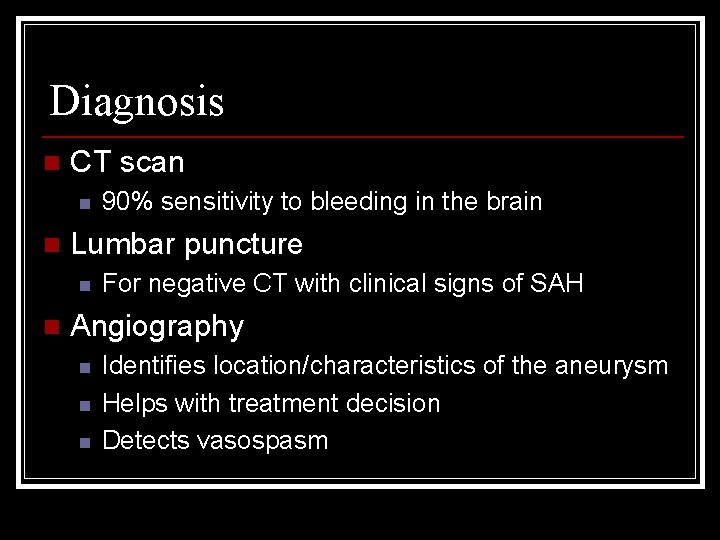
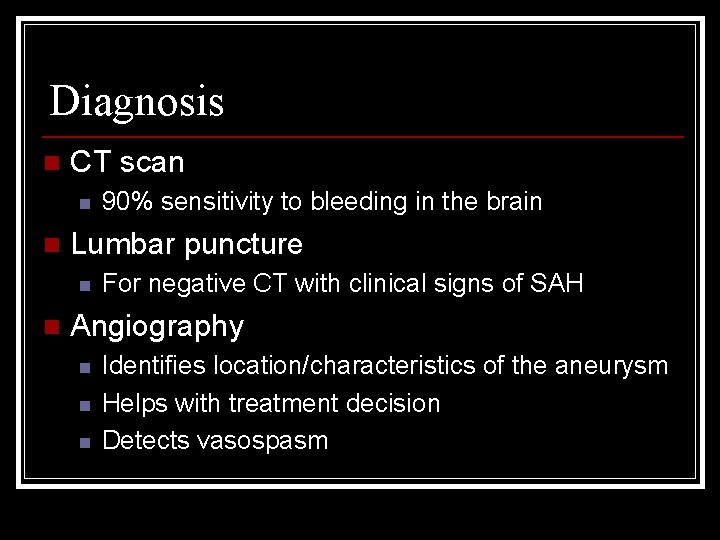
Diagnosis n CT scan n n Lumbar puncture n n 90% sensitivity to bleeding in the brain For negative CT with clinical signs of SAH Angiography n n n Identifies location/characteristics of the aneurysm Helps with treatment decision Detects vasospasm

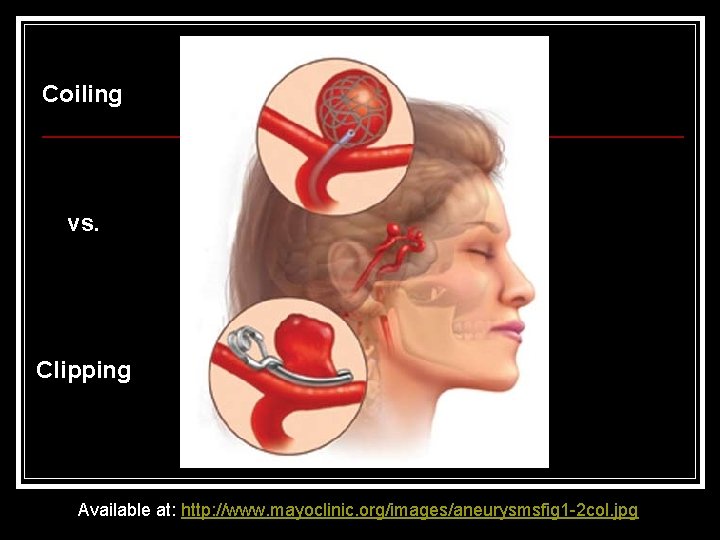
Treatment Options for Aneurysm n n n Craniotomy with aneurysm neck clipping Endovascular embolization, also called coiling The stroke team considers several factors when deciding which treatment option is best for a particular patient. These include: n n n Size of Aneurysm Location of Aneurysm Type of Aneurysm Condition of Patient Medical History
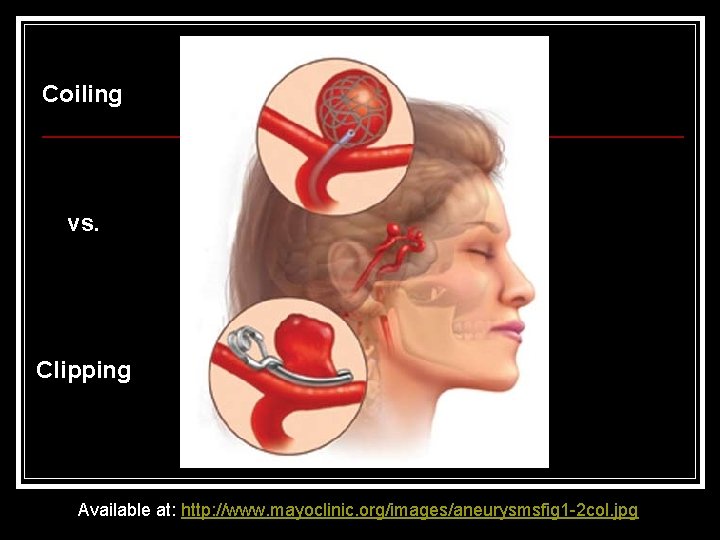
Coiling vs. Clipping Available at: http: //www. mayoclinic. org/images/aneurysmsfig 1 -2 col. jpg
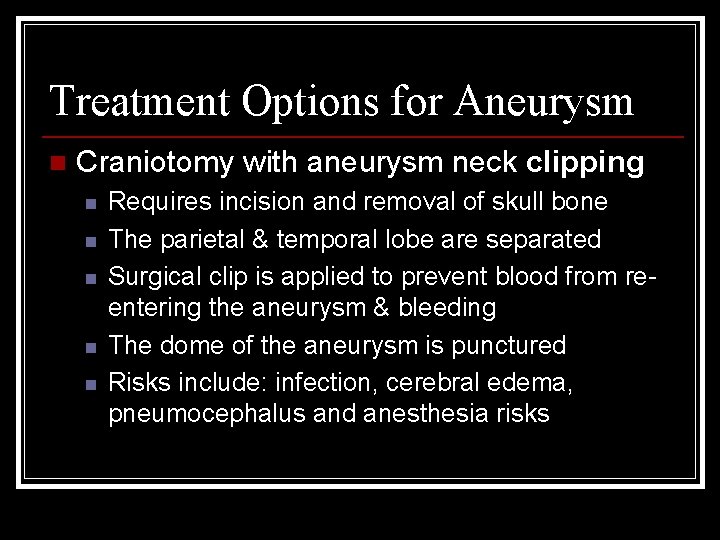
Treatment Options for Aneurysm n Craniotomy with aneurysm neck clipping n n n Requires incision and removal of skull bone The parietal & temporal lobe are separated Surgical clip is applied to prevent blood from reentering the aneurysm & bleeding The dome of the aneurysm is punctured Risks include: infection, cerebral edema, pneumocephalus and anesthesia risks
Treatment Options for Aneurysm n Endovascular embolization (coiling) n n n Approved in 1995 by the FDA Coiling is associated with improved outcomes Uses angio techniques to guide a catheter to the location of the aneurysm Coils are packed into the aneurysm until filled Blood can no longer enter the aneurysm and there is no further risk of re-bleed Risks: perforation of vasculature; bleeding at site

Imaging of an aneurysm that had previously undergone coiling
Potential Complications: RE-BLEEDING n Re-bleeding n n n Of the 18, 000 victims that survive annually, 3, 000 will die or be disabled from re-bleed The highest incidence of re-bleeding is in the first two weeks Symptoms are related to increased ICP – increase in headache, decrease in LOC & new onset of focal (stroke-like) symptoms
Potential Complications: HYDROCEPHALUS n Hydrocephalus n n Occurs in 65% of SAH patients Can be life-threatening Acute signs: drowsiness, abrupt mental status and behavioral changes Treatment: Ventriculostomy, Lumbar drain and/or VP shunt

Available at: http: //www. lowback-pain. com/imagesfolder/nph 6. jpg
Potential Complications: SEIZURE Seizures can occur in as many as 25% of patients n Most common after MCA ruptures n Lead to increased cerebral blood flow, increased ICP and hypertension n Escalate the risk of aneurysm re-bleed and neurologic deterioration n

Potential Complications: FEVER and Secondary INFECTION n Patients are at risk for developing both infectious and noninfectious fever and often do not respond to treatment n Fever occurs in as many as 54% of patients recovering from SAH and is a predictor of poor prognosis n Fever increases cerebral metabolic rate, releases excitatory neurotransmitters, increases production of free radicals and breakdown of the blood-brain barrier – all result in an increased risk for ischemia
Potential Complications: VASOSPASM Definition: the narrowing of a cerebral blood vessel causing decreased cerebral perfusion initially; leading to delayed ischemic deficit, infarction & brain damage if untreated n 40% of patients will experience vasospasm n Etiology of this phenomenon is unknown n If patient’s condition deteriorates after 3 -14 days, vasospasm should be considered n

Vasospasm – the narrowing of a cerebral blood vessel is depicted in this image Available at: http: //www. keithandgina. com/aneurysm/ang 3. jpg
Vasospasm n Signs: n n Gradual neurological deterioration Confusion Decreased LOC Mimics ischemic stroke as new focal neurologic deficits (hemiplegia, CN deficits, & aphasia)
Treatment of Vasospasm n Aimed at increasing cerebral perfusion (Triple H Therapy) n n Hypervolemia Hypertension Hemodilution Triple H Therapy helps to maintain a stable, slightly higher blood pressure, which increases and maintains cerebral perfusion pressure.
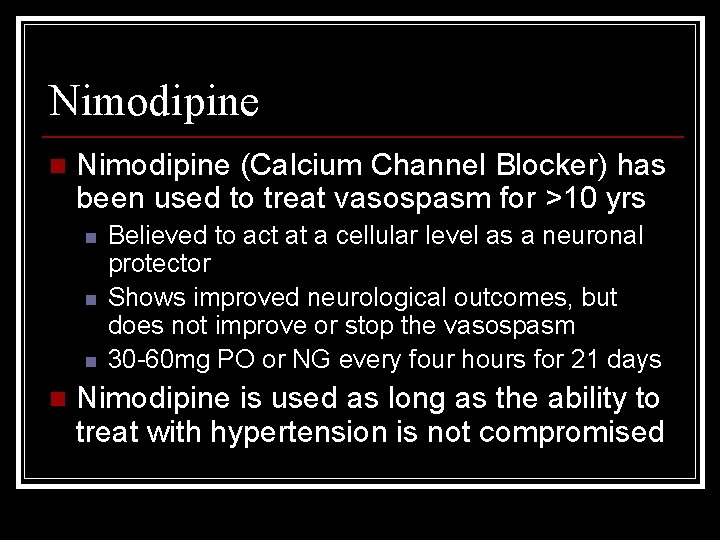
Nimodipine n Nimodipine (Calcium Channel Blocker) has been used to treat vasospasm for >10 yrs n n Believed to act at a cellular level as a neuronal protector Shows improved neurological outcomes, but does not improve or stop the vasospasm 30 -60 mg PO or NG every four hours for 21 days Nimodipine is used as long as the ability to treat with hypertension is not compromised

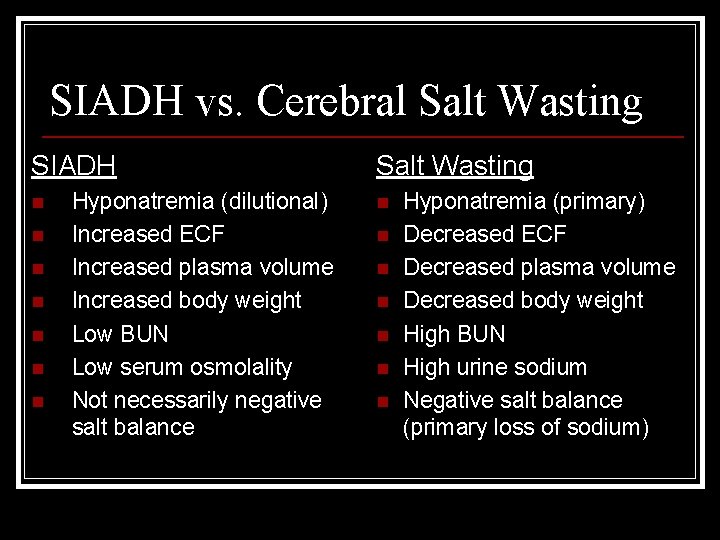
Potential Complications: HYPONATREMIA n n n Low sodium levels create a high risk for vasospasm when combined with hypovolemia Hyponatremia can be caused by SIADH (Syndrome of In-Appropriate Diuretic Hormone) or Cerebral Salt Wasting (CSW). The cause must be distinguished because the treatment is so different: n n n If caused by true SIADH – fluid restriction If caused by salt wasting – fluid replacement Fluid restriction in a patient with salt wasting places them at high risk for vasospasm and ischemia
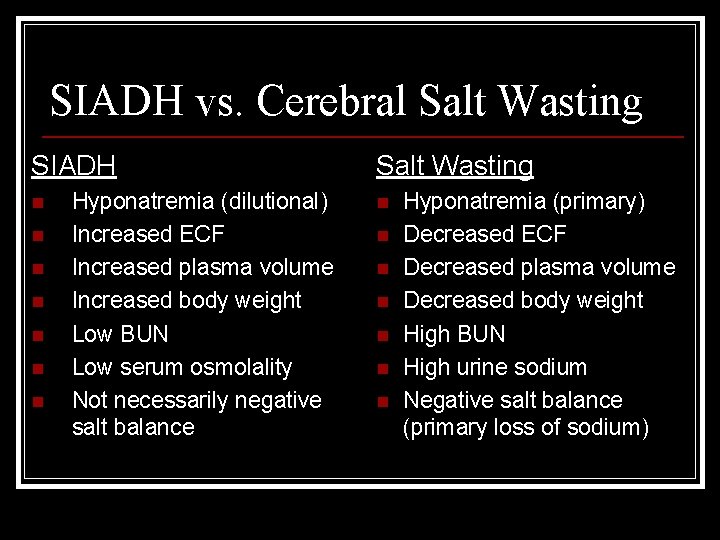
SIADH vs. Cerebral Salt Wasting SIADH n n n n Hyponatremia (dilutional) Increased ECF Increased plasma volume Increased body weight Low BUN Low serum osmolality Not necessarily negative salt balance Salt Wasting n n n n Hyponatremia (primary) Decreased ECF Decreased plasma volume Decreased body weight High BUN High urine sodium Negative salt balance (primary loss of sodium)
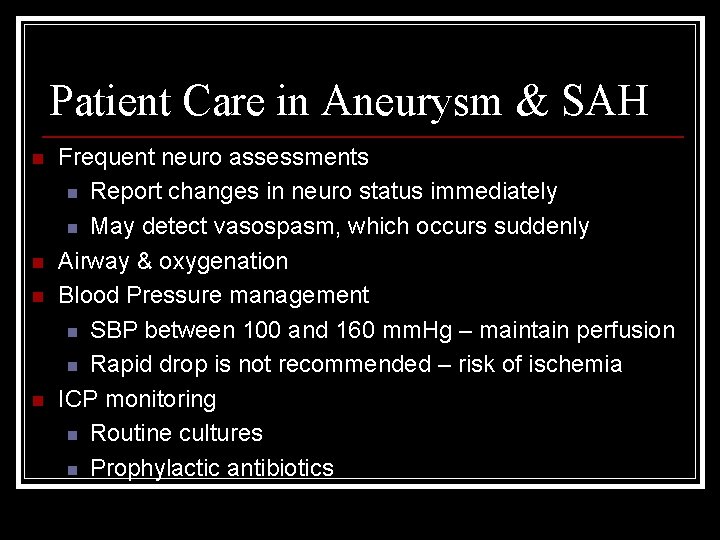
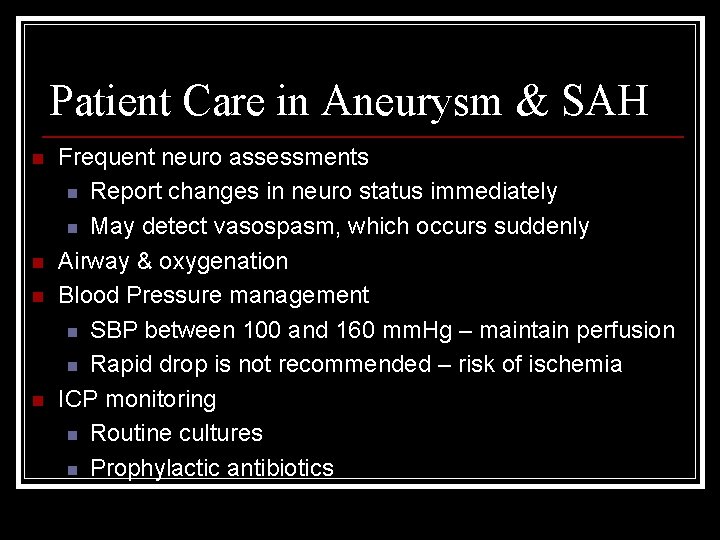
Patient Care in Aneurysm & SAH n n Frequent neuro assessments n Report changes in neuro status immediately n May detect vasospasm, which occurs suddenly Airway & oxygenation Blood Pressure management n SBP between 100 and 160 mm. Hg – maintain perfusion n Rapid drop is not recommended – risk of ischemia ICP monitoring n Routine cultures n Prophylactic antibiotics
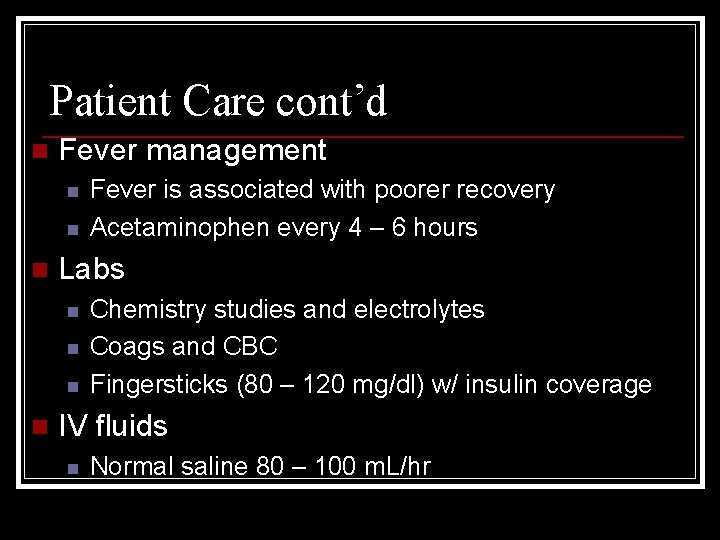
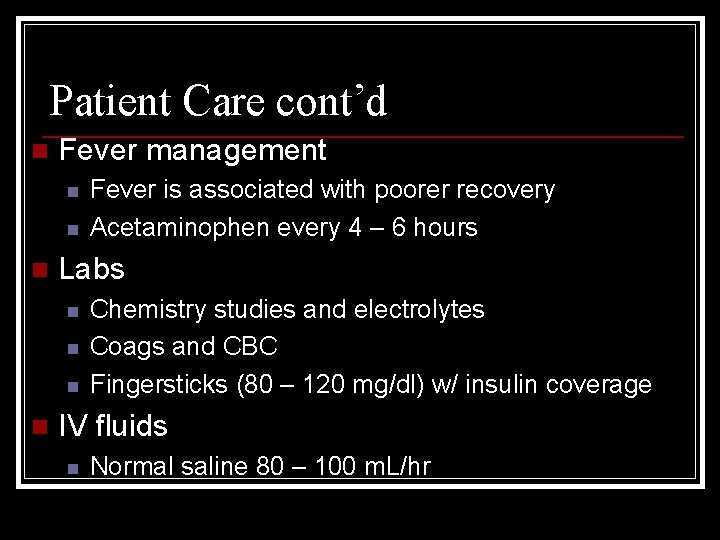
Patient Care cont’d n Fever management n n n Labs n n Fever is associated with poorer recovery Acetaminophen every 4 – 6 hours Chemistry studies and electrolytes Coags and CBC Fingersticks (80 – 120 mg/dl) w/ insulin coverage IV fluids n Normal saline 80 – 100 m. L/hr
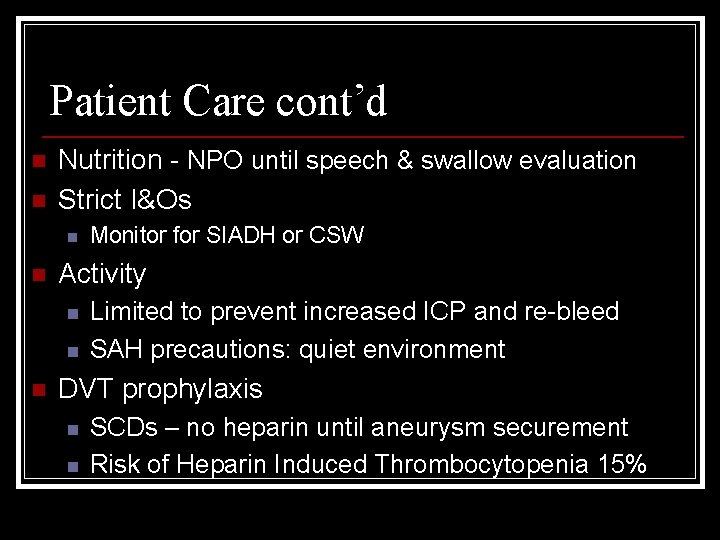
Patient Care cont’d n n Nutrition - NPO until speech & swallow evaluation Strict I&Os n n Activity n n n Monitor for SIADH or CSW Limited to prevent increased ICP and re-bleed SAH precautions: quiet environment DVT prophylaxis n n SCDs – no heparin until aneurysm securement Risk of Heparin Induced Thrombocytopenia 15%
Medications Seizure prophylaxis n Blood pressure management n Stool softeners – should not strain at BM n Pain management – headache n Antiemetic – n/v increases ICP & re-bleed n GI prophylaxis n Nimodipine – prevention of vasospasm n
Lesson 3 Review A cerebral aneurysm is a saccular outpouching of a cerebral artery n Aneurysm rupture is the most common cause of non-traumatic subarachnoid hemorrhage (SAH) n Although advanced imaging has allowed for noninvasive detection of an aneurysm, most are found following rupture n
Lesson 3 Review n 50% of patients experience prodromal (warning) signs 10 -20 days prior to aneurysm rupture: n n n n Headache (48%) Dizziness (10%) Pain above & behind the eye (7%) Sensory or motor disturbance (6%) Photophobia, diplopia, or vision loss (4%) Bruits (3%) Impaired extra ocular movements (EOMs) or ptosis
Lesson 3 Review n Initial presentation with aneurysm rupture: n n Intense, unrelenting headache of sudden onset, described as “the worst headache of my life!” Transient loss of or altered consciousness Feelings of impending doom Treatment options for aneurysm include: n n Craniotomy with aneurysm neck clipping Endovascular embolization, also called coiling

Lesson 4: Arteriovenous Malformation (AVM) Define Arteriovenous Malformation (AVM) and associated terms n List medical manifestations of AVM n Discuss treatment options for AVMs n

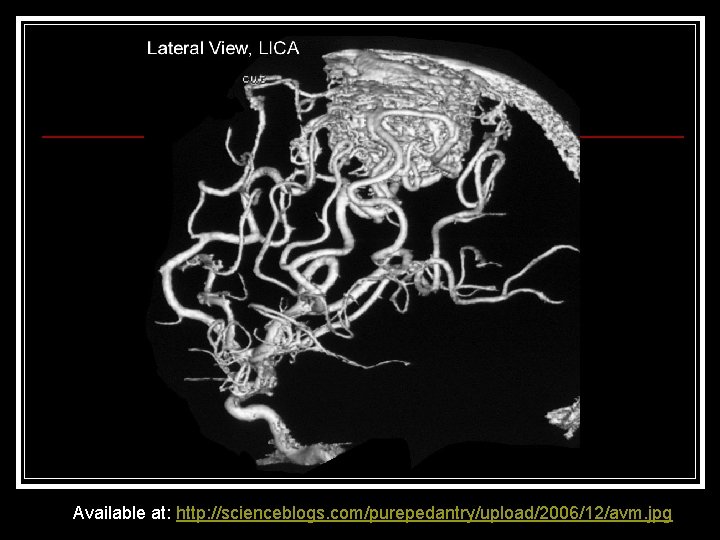
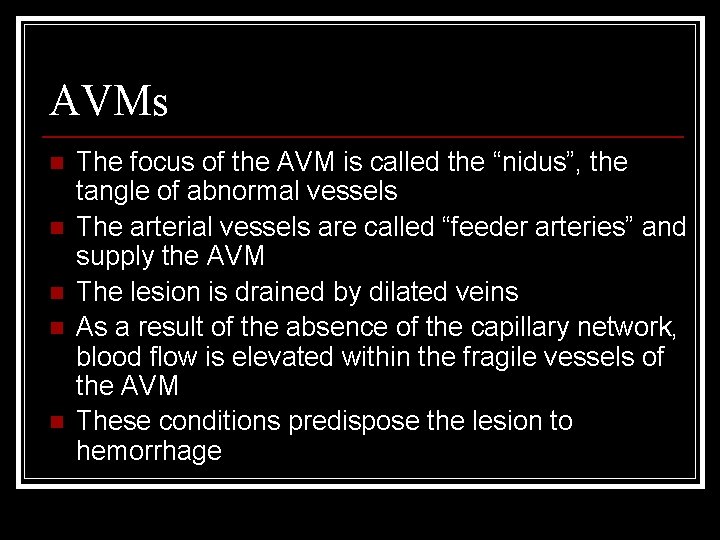
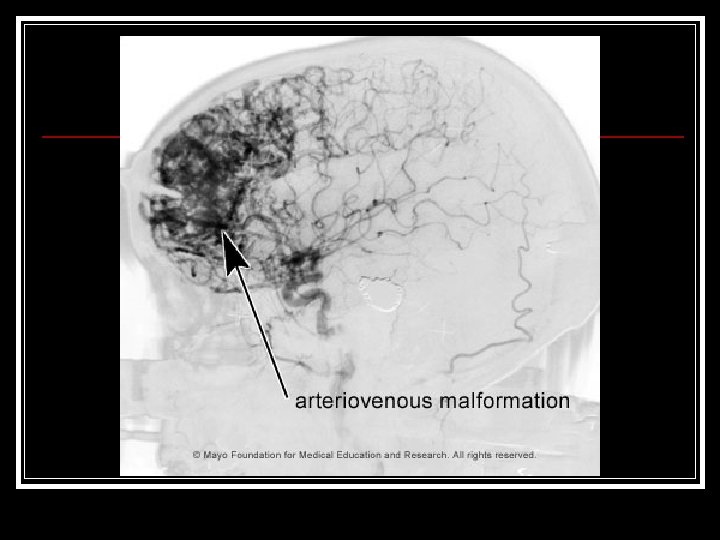
Arteriovenous Malformation (AVM) Composed of a tightly tangled collection of abnormal, thin-walled, dilated blood vessels that directly shunt arterial blood into the venous system without the usual connecting capillary network n Found in children and adults n Believed to be congenital (embryonic vascular network did not develop properly) n
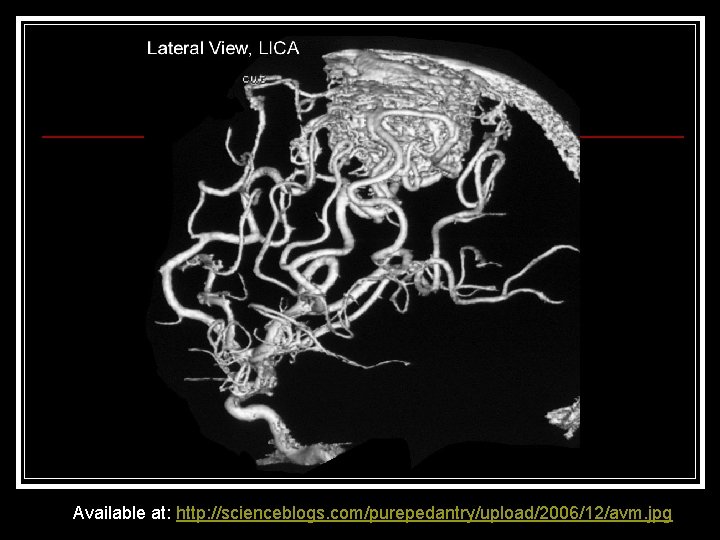
Available at: http: //scienceblogs. com/purepedantry/upload/2006/12/avm. jpg
AVMs n n n The focus of the AVM is called the “nidus”, the tangle of abnormal vessels The arterial vessels are called “feeder arteries” and supply the AVM The lesion is drained by dilated veins As a result of the absence of the capillary network, blood flow is elevated within the fragile vessels of the AVM These conditions predispose the lesion to hemorrhage
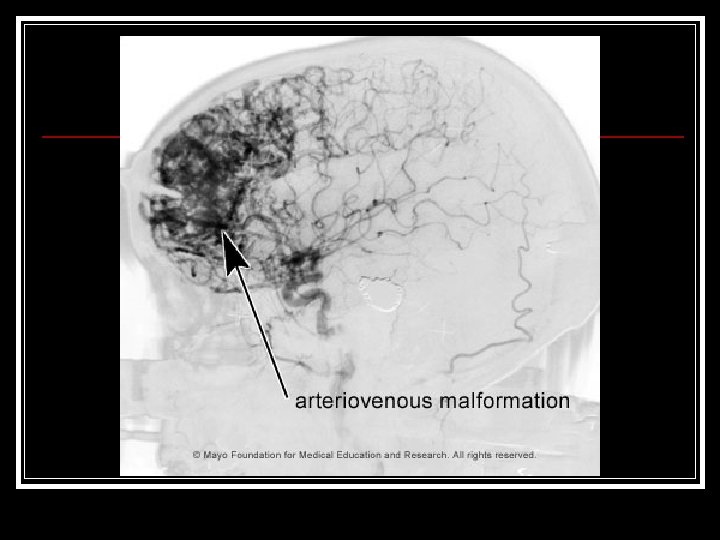
Incidence of AVM Account for 8. 6% of SAHs and 1% of strokes n Clinically significant because AVM is the most common cerebrovascular lesion that causes symptoms n 80% develop symptoms between 20 -40 years of age n

Vascular Steal Phenomenon There is an effect of impaired perfusion of the cerebral tissue surrounding the AVM n The diversion of blood to the AVM is called “vascular steal” phenomenon n Vascular steal is said to be the cause of progressive neuro deficits and psychiatric behaviors/manifestations seen in some AVM patients n

Major Clinical Manifestions of AVM 50% present with hemorrhage n 70% have a seizure at some point n 15% have migraine-like headaches that do not respond to usual drug therapy n Progressive neuro deficits – depend on the area of the brain with vascular steal n Psychiatric manifestions/behaviors n
Diagnosis of AVM CT scan n MRI/MRA n Angiography – n n n Definitive Demonstrates the feeding arteries, the nidus and the draining veins
Treatment of AVMs Surgery – usually elective; delayed for 3 weeks after hemorrhage to allow the patient to be stabilized and for the brain to recover from the effects of hemorrhage n Endovascular Tx – may be needed in multiple stages to reduce blood supply to the AVM and/or in combination with surgery n

Treatment of AVMs cont’d n Embolization – permanent occlusion of the nidus and feeding vessels n n Surgically inaccessible lesions Facilitate surgical excision Promote thrombosis of the nidus Radiation (Gamma Knife)
Key Assessment Points Level of Consciousness n Pupil checks n Motor function n Sensory function n Meningeal irritation signs (headache, stiff neck, photophobia) n CN deficits (blurred vision, diplopia, EOMs, ptosis, dysarthria, facial droop, etc) n

Caution! Alterations in assessment could be the result of : Potential complications such as n re-bleed, n hydrocephalus, n ischemia, n vasospasm, n hypoxia, n focal seizures, n increased ICP, or n electrolyte imbalances
However, n Alterations may also be caused by: n n n Effects of immobility (DVT, PE, constipation, atelectasis) Sensory deprivation (depression, psychological effects/behaviors) Infections (aspiration or bacterial pneumonia, UTIs)
Additional Points of Care n n Recognition of common complications Prevention of other complications n n n n n Monitoring blood pressure and lab values Adequate oxygenation Bowel and bladder management Dysphagia/nutritional compromise DVT prophylaxis Aseptic technique Skin breakdown Seizure precautions and prophylaxis Drug therapy (Nimodipine, pain control, etc) Patient Education (disease process & treatment)
Lesson 4 Review n An AVM is: n n n composed of a tightly tangled collection of abnormal, thin-walled, dilated blood vessels that directly shunt arterial blood into the venous system without the usual connecting capillary network believed to be congenital most commonly found at 20 -40 years of age
Lesson 4 Review n Major medical manifestations of AVM n n n Hemorrhage Seizures Migraine-like headaches Progressive neuro deficits Psychiatric manifestions/behaviors
Lesson 4 Review n Treatment options for AVM include: n n Surgery Embolization Radiation (Gamma-knife) Combinations of these

Summary n n n Although hemorrhagic strokes constitute only a fraction of total strokes, the effects can be devastating or deadly New research and technical advances have led to less traumatic and safer methods of treatment for patients Recovery is often complicated by secondary injuries When a patient suffers hemorrhagic stroke, each team member plays an important role in patient monitoring, therapies and management of care to prevent secondary injury and complications Nursing can directly impact care, patient outcomes and quality of life with thorough assessment, early recognition of complications, patient education and advocacy
References n n n American Association of Neuroscience Nurses. (2007). Care of the patient with aneurysmal subarachnoid hemorrhage [AANN Clinical Practice Guideline]. Glenview, IL: Sheila Alexander. Barker, E (2002). Neuroscience nursing - A spectrum of care. St. Louis, MO: Mosby. Hickey, J (2003). The clinical practice of neurological and neurosurgical nursing. Philadelphia, PA: Lippincott, Williams & Wilkins.
 Ischemic vs hemorrhagic stroke
Ischemic vs hemorrhagic stroke Different types of serial killers
Different types of serial killers Intended audience
Intended audience Hippo document analysis
Hippo document analysis Intended audience
Intended audience Who is the intended audience?
Who is the intended audience? Intended audience of the declaration of independence
Intended audience of the declaration of independence Intended audience
Intended audience Who was the intended audience
Who was the intended audience Intended audience
Intended audience What is the purpose of the media
What is the purpose of the media Your turn next
Your turn next Anterior stroke vs posterior stroke
Anterior stroke vs posterior stroke Hypovolemic shock classification
Hypovolemic shock classification Types of haemorrhage
Types of haemorrhage Reactionary hemorrhage definition
Reactionary hemorrhage definition Hemorrhagic
Hemorrhagic Causes of viral hemorrhagic fever
Causes of viral hemorrhagic fever Acute pancreatitis treatment
Acute pancreatitis treatment Hemorrhagic diathesis
Hemorrhagic diathesis Icp monitoring
Icp monitoring Stages of hemorrhagic shock
Stages of hemorrhagic shock Functions of vitamin k
Functions of vitamin k Andy rekito
Andy rekito Childrens temperature chart
Childrens temperature chart Hantavirus humans
Hantavirus humans Necrotizing fasciitis hemorrhagic bullae
Necrotizing fasciitis hemorrhagic bullae Audience addressed audience invoked
Audience addressed audience invoked Headache
Headache Post-ictal
Post-ictal How to apply sick leave in infosys
How to apply sick leave in infosys Left side low abdominal pain
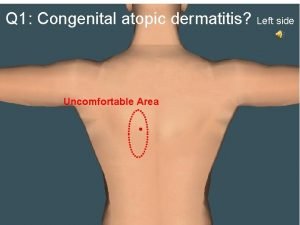
Left side low abdominal pain Headache
Headache Headache
Headache Ophthalmoplegic migraine
Ophthalmoplegic migraine European headache federation
European headache federation Nursing management of encephalitis
Nursing management of encephalitis Pumcture
Pumcture Ottohrea
Ottohrea ı have a headache song
ı have a headache song Headache
Headache Headache pain chart
Headache pain chart Meao mudra
Meao mudra Improved
Improved Dr alexander mauskop
Dr alexander mauskop Anxiety headache
Anxiety headache Pediatric headache red flags
Pediatric headache red flags Red flags headache
Red flags headache Rasmussen syndrome
Rasmussen syndrome Snoop headache
Snoop headache Migraine hangover symptoms
Migraine hangover symptoms Composition is the arrangement of
Composition is the arrangement of Direct voluntary act examples in school
Direct voluntary act examples in school What is intended benefit
What is intended benefit Great gatsby vocabulary
Great gatsby vocabulary Usability specification in hci
Usability specification in hci It is the intended height of the function?
It is the intended height of the function? A humorous scene or speech intended to lighten the mood
A humorous scene or speech intended to lighten the mood Fuses and circuit breakers are intended primarily for the
Fuses and circuit breakers are intended primarily for the Simulate or animate some features of intended system
Simulate or animate some features of intended system The text is intended for
The text is intended for Births deaths and marriages tasmania
Births deaths and marriages tasmania In her statement (lines 53-54) miss nightingale intended to
In her statement (lines 53-54) miss nightingale intended to A specially waxed carbon paper
A specially waxed carbon paper Stabilizing community lifelines is primary effort during
Stabilizing community lifelines is primary effort during Destructive event or prank a virus was created to deliver
Destructive event or prank a virus was created to deliver Fuses and circuit breakers are intended primarily for
Fuses and circuit breakers are intended primarily for Intended message
Intended message Intended outcome
Intended outcome Most inhalants are actually intended to be
Most inhalants are actually intended to be A long uninterrupted speech
A long uninterrupted speech What was trench warfare intended to accomplish
What was trench warfare intended to accomplish The poster was intended to
The poster was intended to Intended curriculum
Intended curriculum 101012 bằng
101012 bằng Thể thơ truyền thống
Thể thơ truyền thống Hát lên người ơi alleluia
Hát lên người ơi alleluia Hươu thường đẻ mỗi lứa mấy con
Hươu thường đẻ mỗi lứa mấy con đại từ thay thế
đại từ thay thế Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Công của trọng lực
Công của trọng lực Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Lời thề hippocrates
Lời thề hippocrates Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Phản ứng thế ankan
Phản ứng thế ankan Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Môn thể thao bắt đầu bằng từ chạy
Môn thể thao bắt đầu bằng từ chạy Khi nào hổ mẹ dạy hổ con săn mồi
Khi nào hổ mẹ dạy hổ con săn mồi điện thế nghỉ
điện thế nghỉ Các loại đột biến cấu trúc nhiễm sắc thể
Các loại đột biến cấu trúc nhiễm sắc thể Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Một số thể thơ truyền thống
Một số thể thơ truyền thống Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Ng-html
Ng-html Sơ đồ cơ thể người
Sơ đồ cơ thể người Tư thế ngồi viết
Tư thế ngồi viết Số nguyên là gì
Số nguyên là gì đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Tư thế worms-breton
Tư thế worms-breton